Office of Research Integrity Assurance ORIA The future










- Slides: 38
Office of Research Integrity & Assurance (ORIA) The future of global health: Navigating a complex ethical terrain Mary Simmerling, Ph. D Assistant Professor of Research Integrity in Medicine Office of Research Integrity
Global Health at Weill Cornell Medical College Service, training, and research to address health problems that transcend national boundaries, disproportionately affect the resource poor, and are best addressed by multidisciplinary solutions. Goal is to create a sustainable and innovative research and training program that engage students and faculty at all levels and from multiple disciplines to solve problems of global health.
Major Global Health Initiatives at WCMC Australia: University of Sydney Medical School Brazil: UFBa and FIOCRUZ India: Christian Medical College India: Narayana Hrudayalaya and Mazumdar-Shaw Cancer Center Peru: San Marcos Medical College Qatar: Weill Cornell in Qatar Tanzania: Weill Bugando Haiti: GHESKIO Centers

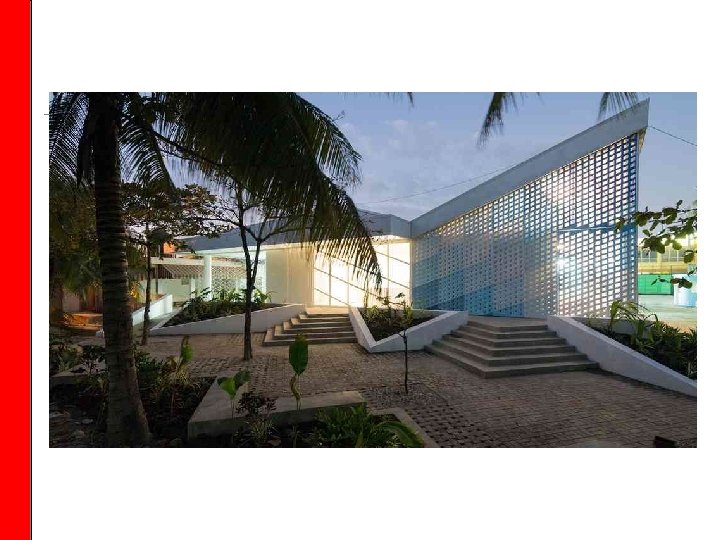
GHESKIO (Groupe Haitien d’Etude du Sarcome de Kaposi et des Infection Opportunistes) Centers



* 'Managing Conflicts of Interest in Clinical Care: The 'Race to the Middle' at US Medical Schools' appeared in the October 2013 edition of Academic Medicine, Vol. 88, No. 10 – data based on September 2011 Policies

* 'Managing Conflicts of Interest in Clinical Care: The 'Race to the Middle' at US Medical Schools' appeared in the October 2013 edition of Academic Medicine, Vol. 88, No. 10 – data based on September 2011 Policies

* 'Managing Conflicts of Interest in Clinical Care: The 'Race to the Middle' at US Medical Schools' appeared in the October 2013 edition of Academic Medicine, Vol. 88, No. 10 – data based on September 2011 Policies

1982 2014
How do we respond when things don’t go that well? What happens at the intersection of longstanding cultural norms and moral disagreements/disharmonies? What happens when we are faced with conflicting demands (internal or external)?
Philosophical considerations Principles based framework for establishing: What is morally permissible/justifiable What is morally required (eg, as a duty or obligation) What is morally unjustifiable
Guiding/foundational moral principles Beneficence Do good, don’t harm Respect for persons Treat people as autonomous agents (with limitations) Allow them to make their own decisions Put them in a good position to make those decisions in a well-informed way (power differential, knowledge differential) Justice Fairness (not necessarily equality, but consistency)
With hard questions…. . Do we need to respect everyone and everything? What does it mean to do good? Towards what end? How do we resolve competing moral – and practical - demands?
Beneficence What maximizes benefits? Whose benefits? Who gets to decide?
Respect for Persons Who gets to choose (be a chooser)? Under what circumstances?
Justice Fairly sharing benefits and burdens – should geographic lines matter? Are they morally relevant? Defining the standard of care: is it where one stands at the time, or is it defined by the best (available) options? Does this mean the poor should get less, because they have less? (and if so, how could THAT be fair? )
Case for consideration/discussion Organ transplantation in China January 2007 – Vice Minister of Health publicly admits that China uses organs from executed prisoners for transplantation

How should we respond?
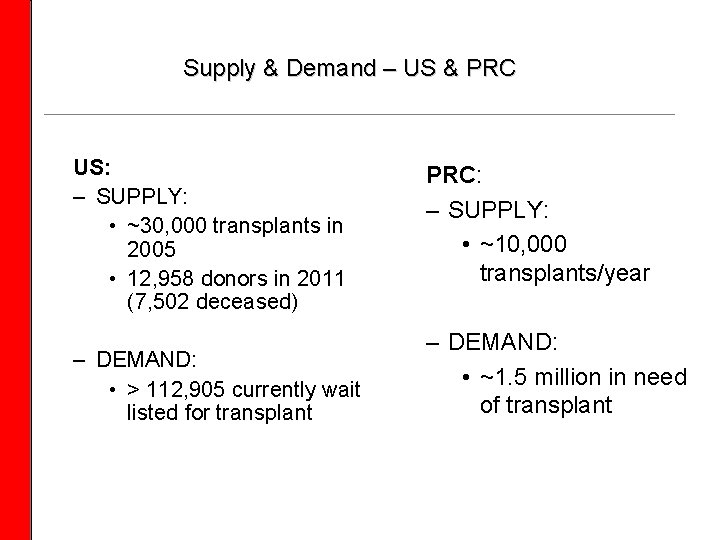
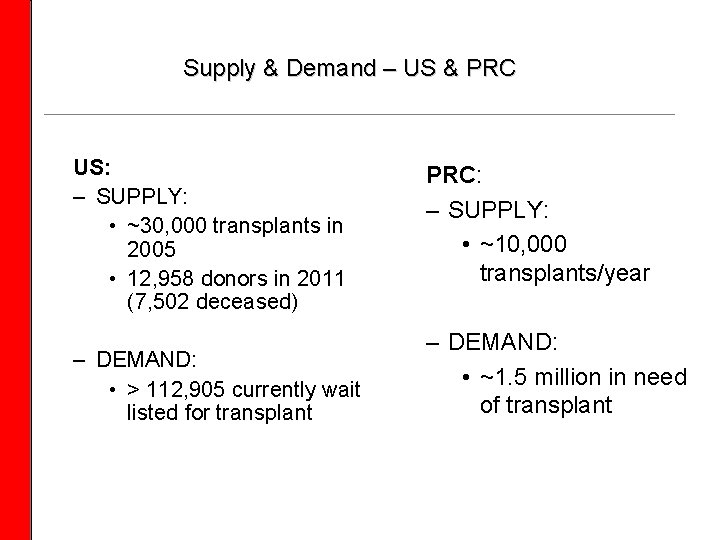
Supply & Demand – US & PRC US: – SUPPLY: • ~30, 000 transplants in 2005 • 12, 958 donors in 2011 (7, 502 deceased) – DEMAND: • > 112, 905 currently wait listed for transplant PRC: – SUPPLY: • ~10, 000 transplants/year – DEMAND: • ~1. 5 million in need of transplant
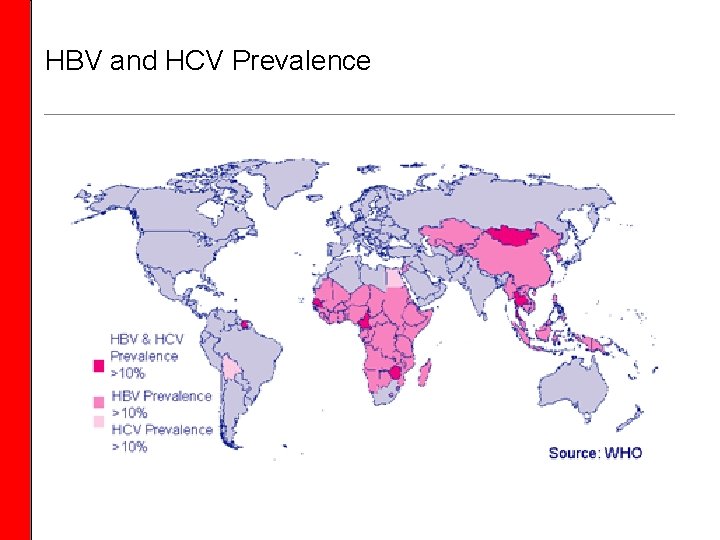
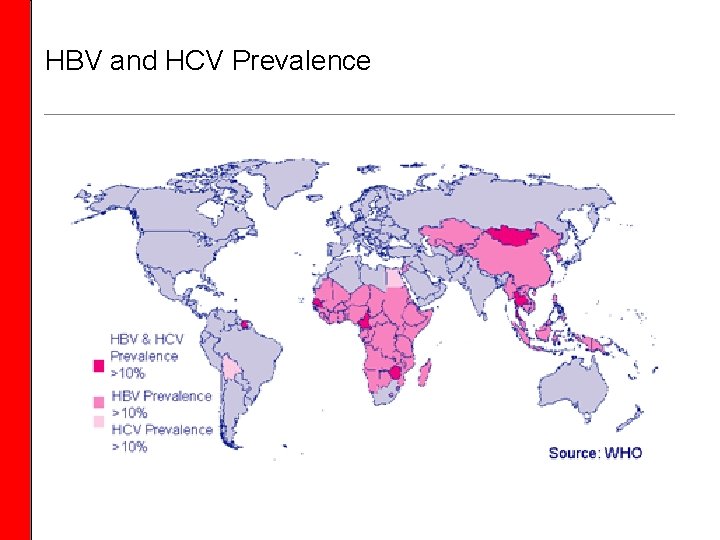
HBV and HCV Prevalence
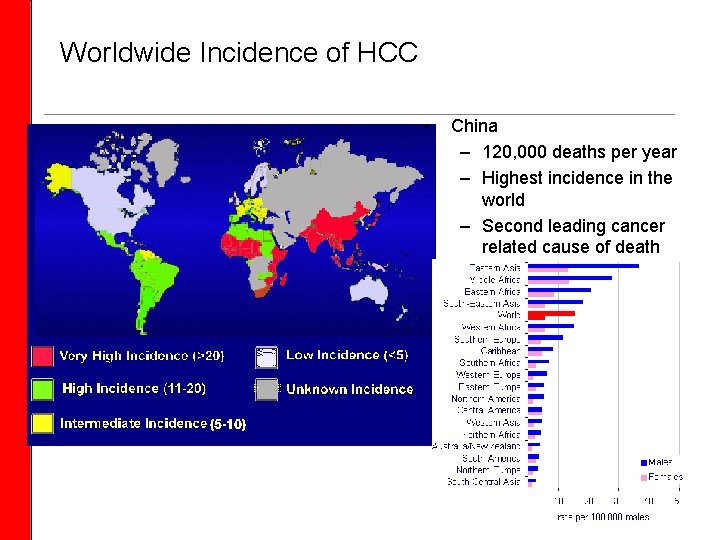
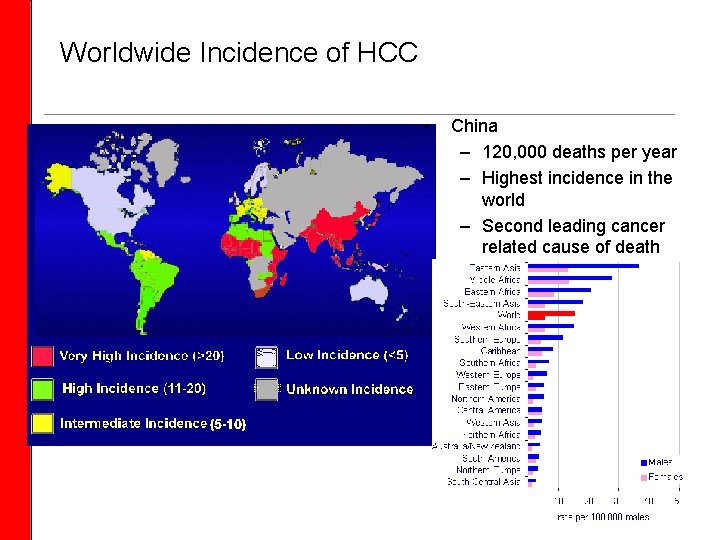
Worldwide Incidence of HCC • China – 120, 000 deaths per year – Highest incidence in the world – Second leading cancer related cause of death
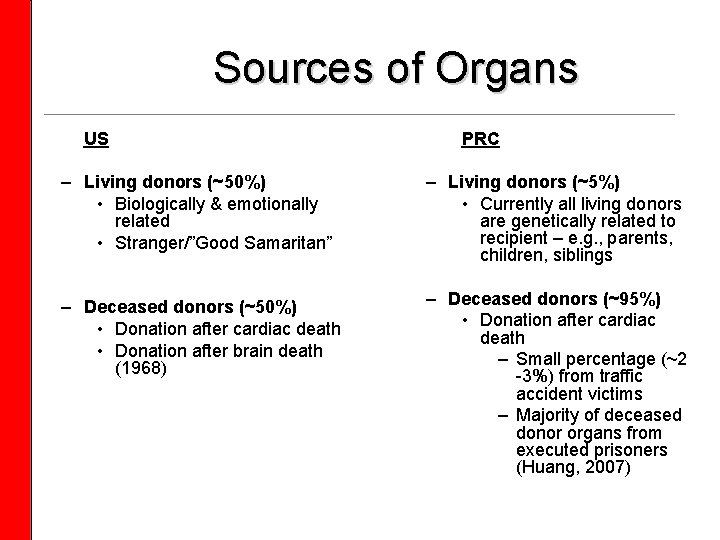
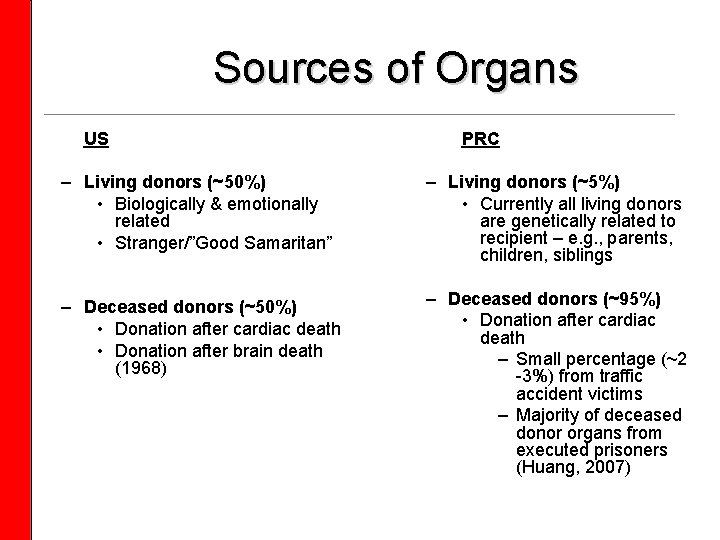
Sources of Organs US PRC – Living donors (~50%) • Biologically & emotionally related • Stranger/”Good Samaritan” – Living donors (~5%) • Currently all living donors are genetically related to recipient – e. g. , parents, children, siblings – Deceased donors (~50%) • Donation after cardiac death • Donation after brain death (1968) – Deceased donors (~95%) • Donation after cardiac death – Small percentage (~2 -3%) from traffic accident victims – Majority of deceased donor organs from executed prisoners (Huang, 2007)
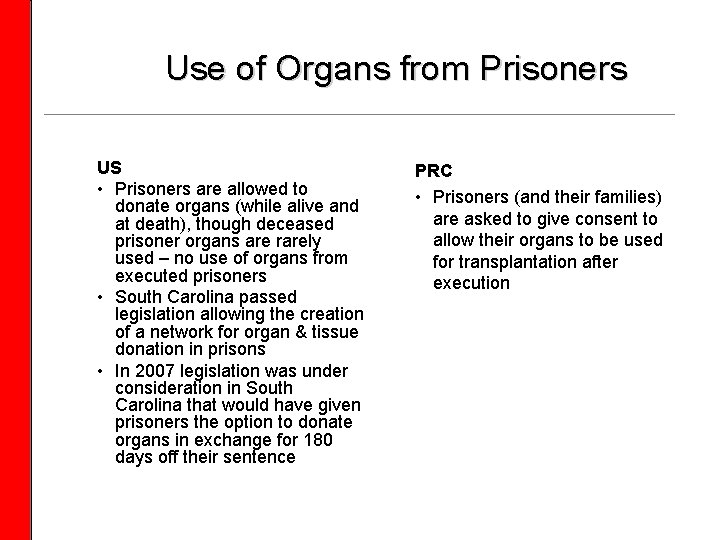
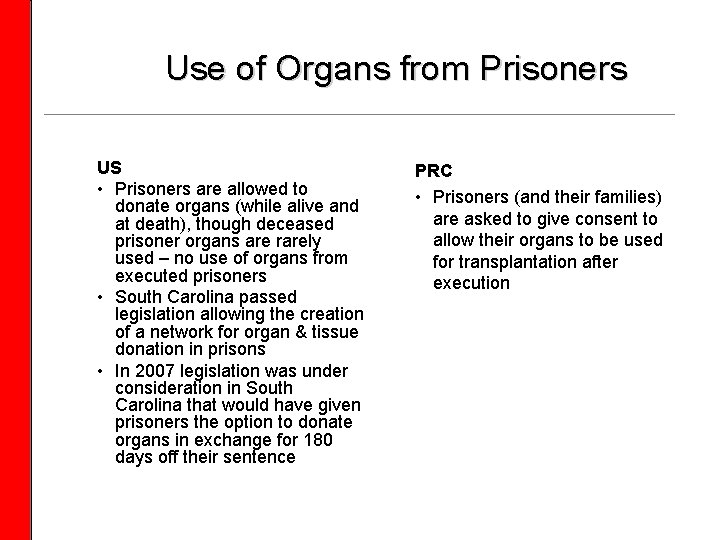
Use of Organs from Prisoners US • Prisoners are allowed to donate organs (while alive and at death), though deceased prisoner organs are rarely used – no use of organs from executed prisoners • South Carolina passed legislation allowing the creation of a network for organ & tissue donation in prisons • In 2007 legislation was under consideration in South Carolina that would have given prisoners the option to donate organs in exchange for 180 days off their sentence PRC • Prisoners (and their families) are asked to give consent to allow their organs to be used for transplantation after execution
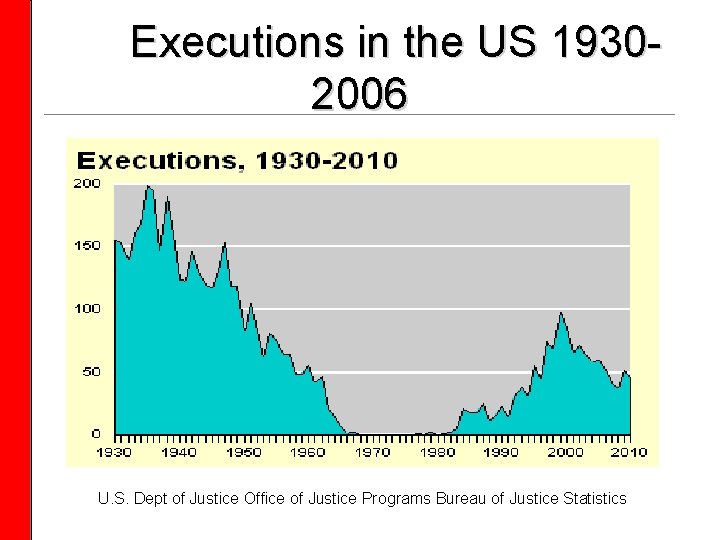
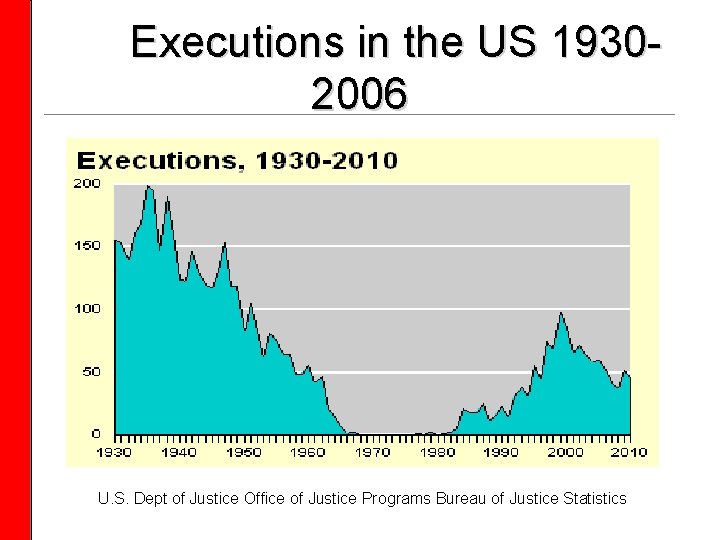
Executions in the US 19302006 U. S. Dept of Justice Office of Justice Programs Bureau of Justice Statistics
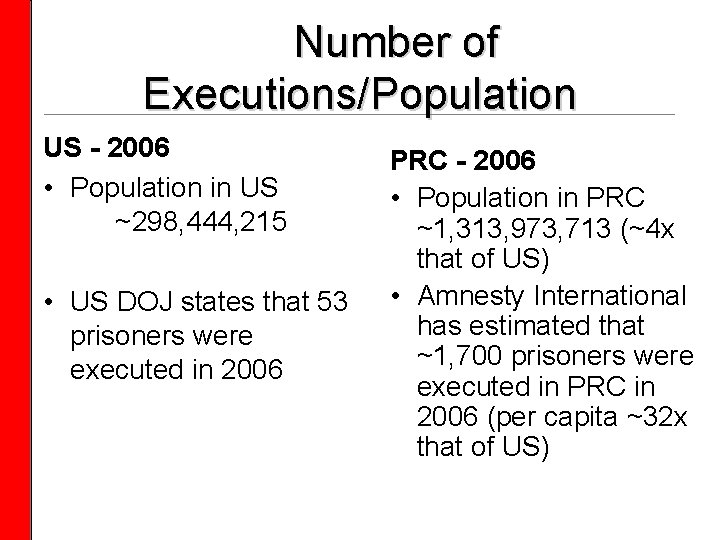
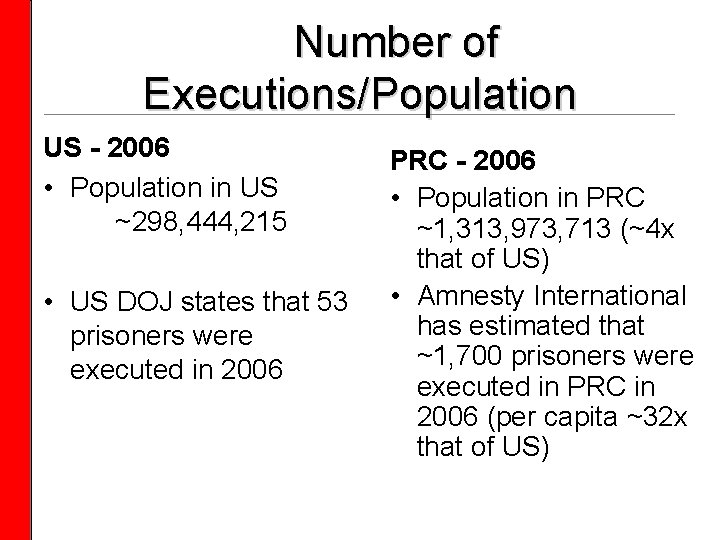
Number of Executions/Population US - 2006 • Population in US ~298, 444, 215 • US DOJ states that 53 prisoners were executed in 2006 PRC - 2006 • Population in PRC ~1, 313, 973, 713 (~4 x that of US) • Amnesty International has estimated that ~1, 700 prisoners were executed in PRC in 2006 (per capita ~32 x that of US)
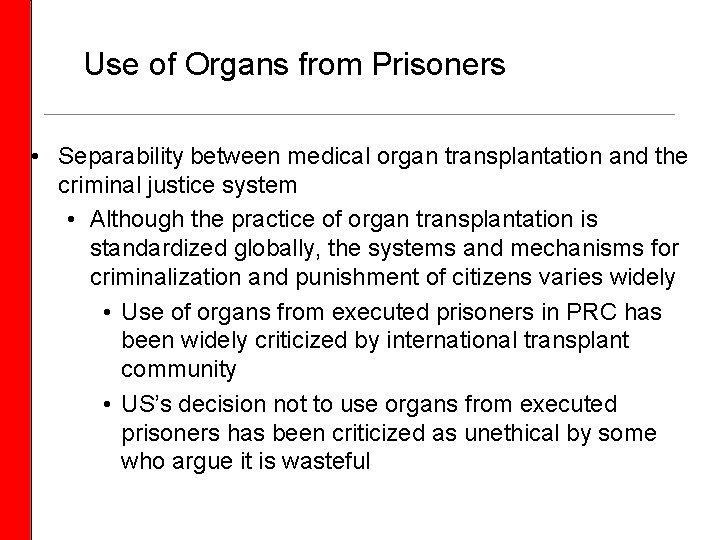
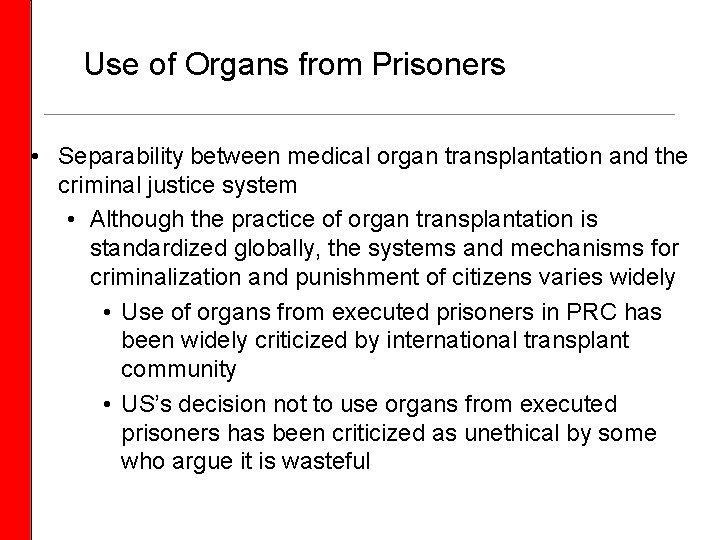
Use of Organs from Prisoners • Separability between medical organ transplantation and the criminal justice system • Although the practice of organ transplantation is standardized globally, the systems and mechanisms for criminalization and punishment of citizens varies widely • Use of organs from executed prisoners in PRC has been widely criticized by international transplant community • US’s decision not to use organs from executed prisoners has been criticized as unethical by some who argue it is wasteful
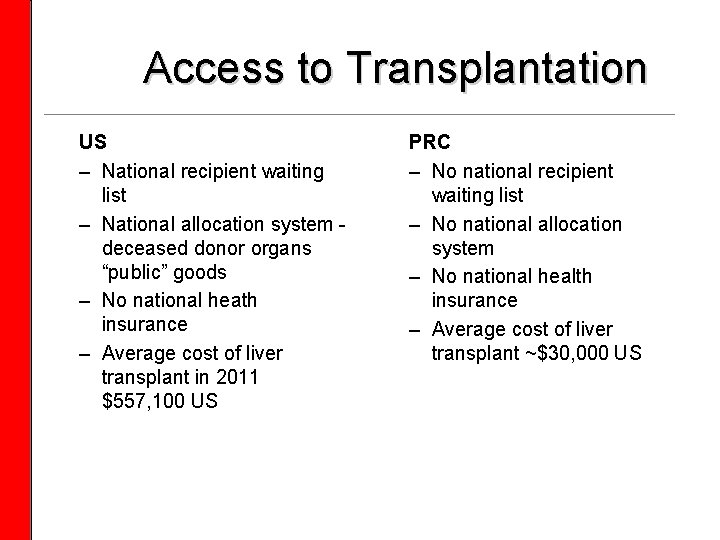
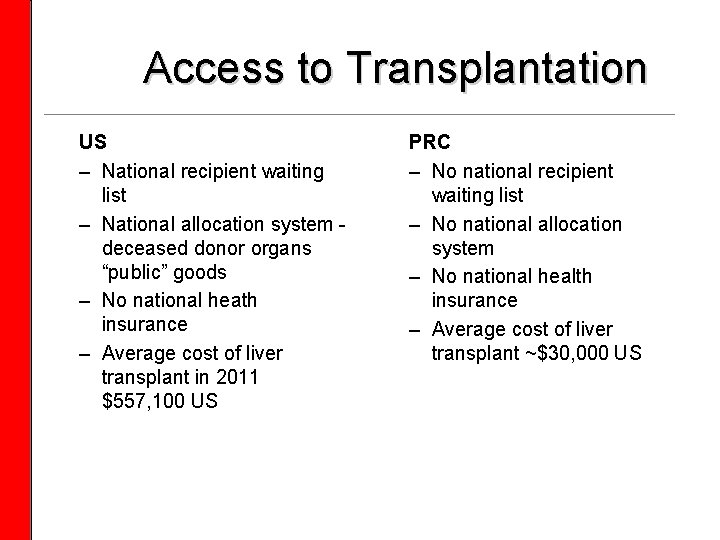
Access to Transplantation US – National recipient waiting list – National allocation system - deceased donor organs “public” goods – No national heath insurance – Average cost of liver transplant in 2011 $557, 100 US PRC – No national recipient waiting list – No national allocation system – No national health insurance – Average cost of liver transplant ~$30, 000 US

Ethical Challenges • Historical Challenges • Feasibility • Risks & Benefits • Scarcity, Supply & Demand • Access & Allocation • Informed Consent • Use of prisoner organs • Organ sales • Continuing/Emerging Challenges • Risks & Benefits • Scarcity, Supply & Demand • Access & Allocation • Informed Consent • Use of prisoner organs • Organ sales • Transplant tourism
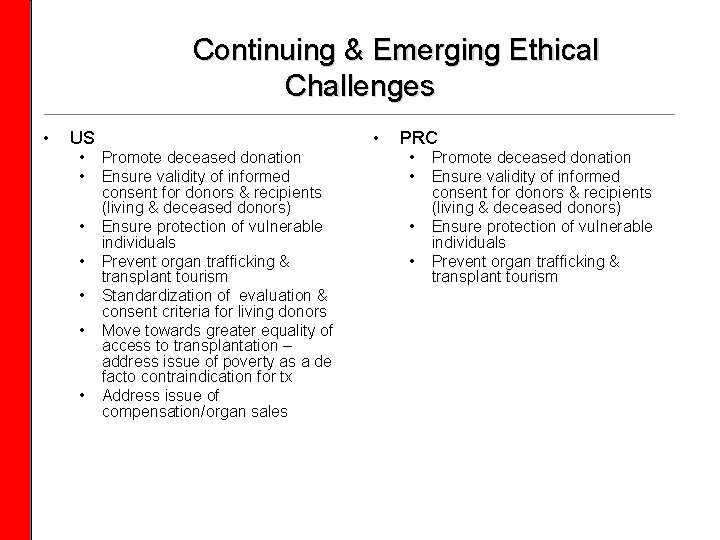
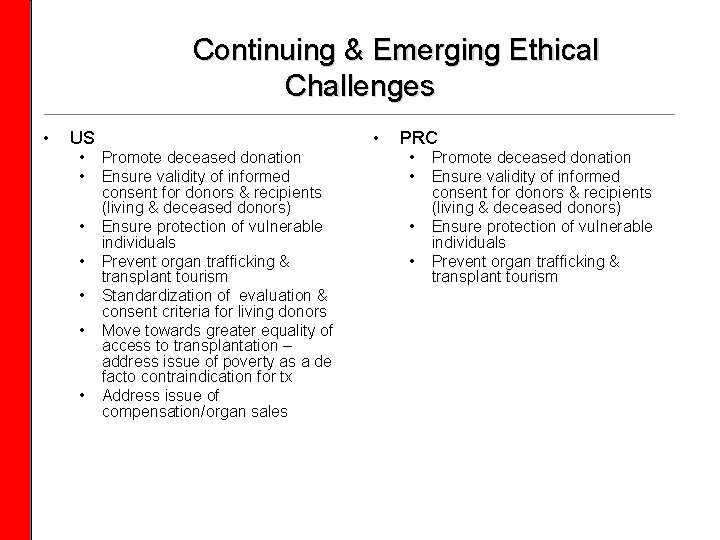
Continuing & Emerging Ethical Challenges • • US • • Promote deceased donation Ensure validity of informed consent for donors & recipients (living & deceased donors) Ensure protection of vulnerable individuals Prevent organ trafficking & transplant tourism Standardization of evaluation & consent criteria for living donors Move towards greater equality of access to transplantation – address issue of poverty as a de facto contraindication for tx Address issue of compensation/organ sales PRC • • Promote deceased donation Ensure validity of informed consent for donors & recipients (living & deceased donors) Ensure protection of vulnerable individuals Prevent organ trafficking & transplant tourism
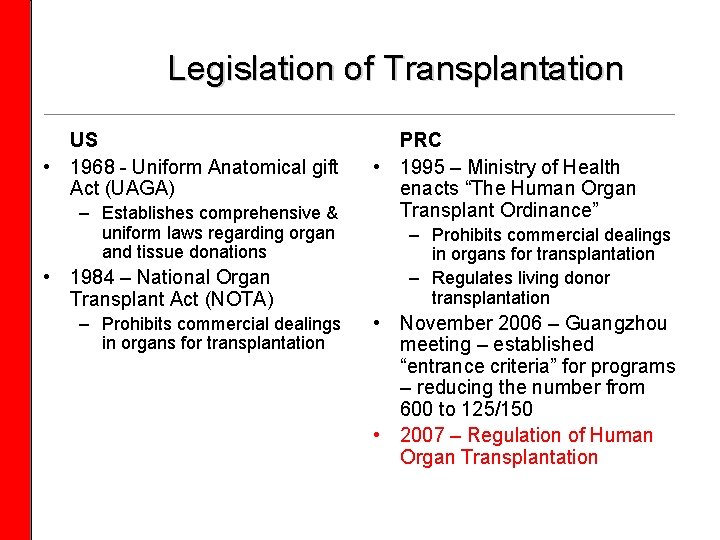
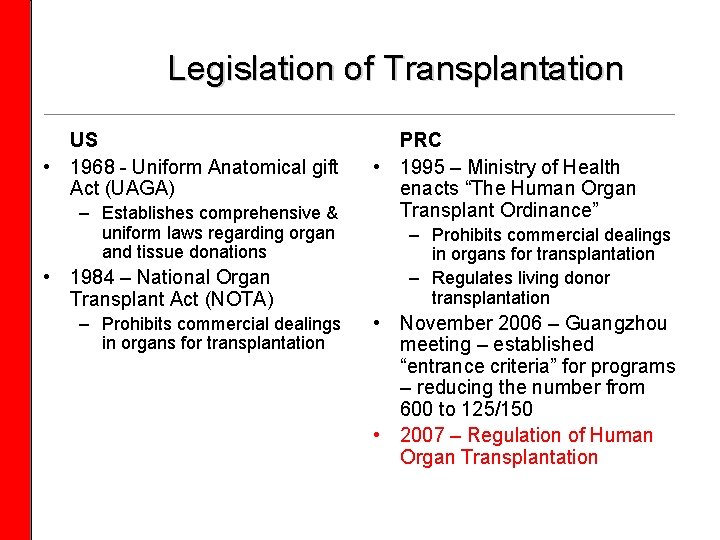
Legislation of Transplantation US • 1968 - Uniform Anatomical gift Act (UAGA) – Establishes comprehensive & uniform laws regarding organ and tissue donations • 1984 – National Organ Transplant Act (NOTA) – Prohibits commercial dealings in organs for transplantation PRC • 1995 – Ministry of Health enacts “The Human Organ Transplant Ordinance” – Prohibits commercial dealings in organs for transplantation – Regulates living donor transplantation • November 2006 – Guangzhou meeting – established “entrance criteria” for programs – reducing the number from 600 to 125/150 • 2007 – Regulation of Human Organ Transplantation
Challenges • Abolishing & criminalizing transplant tourism • China has already taken a clear and strong position against this human rights abuse, however there is still a need to enforce it • Utilizing living organ donors without contributing to the organ trafficking problem • Establishing an ethical framework for transplantation that reflects China’s history, culture, and beliefs
Opportunities • Use of brain dead donors in PRC • Establishment of a national system for access and allocation of organs • Further improvement of procedures for informed consent for living & deceased donation
Support, and sanctions • The global transplant community has supported China’s efforts to establish an ethical framework for transplantation that reflects China’s history culture, beliefs, and values - simply imposing a distinctively Western ethic on China would be disrespectful & may be damaging to China’s efforts. • At the same time, initiated sanctions by barring publication of articles utilizing organs from executed prisoners
Moral engagement Be humble, curious, and creative Approach issues with humility, gravitas, and honesty Recognize these are complex and serious issues that can’t be solved alone, and often are not completely solvable Don’t be a moral bystander – take the opportunity to tune your moral compass

 Future continuous tense rules
Future continuous tense rules Future continuous and future perfect
Future continuous and future perfect Vincent oria
Vincent oria Ceip cardenal herrera oria
Ceip cardenal herrera oria Doctor eugenio oria
Doctor eugenio oria Colegio concertado cardenal herrera oria
Colegio concertado cardenal herrera oria Ceip cardenal cisneros boceguillas
Ceip cardenal cisneros boceguillas Methodological integrity in qualitative research
Methodological integrity in qualitative research Uq research integrity module
Uq research integrity module Epigeum research integrity training
Epigeum research integrity training Future vs future perfect
Future vs future perfect Rules of tense
Rules of tense Future perfect and future continuous examples
Future perfect and future continuous examples Future nurse programme
Future nurse programme Future continuous tense sentences
Future continuous tense sentences How to use present continuous for future
How to use present continuous for future Future tenses summary
Future tenses summary Future plans and finished future actions
Future plans and finished future actions Future continuous and future perfect
Future continuous and future perfect Nulti kondicional
Nulti kondicional Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Kể tên các môn thể thao
Kể tên các môn thể thao Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
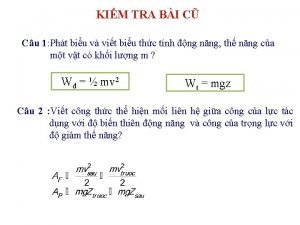
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống