Nutrition of the Medical Surgical Patient Todays Content








- Slides: 41

Nutrition of the Medical. Surgical Patient
Today’s Content • Nutrition Therapy in the acute health-care setting – For medical patients – For surgical patients

MEDICAL NUTRITION THERAPY IN A HEALTH CARE SETTING • Provided to: – Aid in recovery – To stabilize the health condition – ↑ nutritional status – Prepare for surgery • ↓ surgical risk • Help with healing
Involves: • Physical assessment • Nutritional assessment – Usually done 24 -72 hours after admission • Labs – Albumin – Na, K – Ca – Hbg, Hct
Special Diets • • For patients with certain diseases To prepare for special test For surgery To increase or decrease weight

Diets are modified: • • • Texture Calories Specific nutrients Seasonings Consistency
Common diets seen in acute care setting: • • NPO (nothing by mouth) Clear liquid Full liquid Soft Diet as tolerated Regular diet Other diets
NPO • Nothing by mouth – Before anethesia or after surgery until bowel sounds return • Most patients ok with NPO for several days • Some patients may require nutrition and fluids per IV
Clear Liquid • Next step after NPO • How do we know when a patient is ready for this next step? – – Bowel sounds Passing flatus
Clear Liquid • Supplies patient with: – Fluid – CHO (as sugar) – 600 kcal/day • Short term; about 24 -36 hours
Clear Liquid • Major goals of this diet: – relieve thirst – prevent dehydration – minimize stimulation of GI tract
Clear Liquid • Includes: – Water – Tea – Coffee – Clear broths – Carbonated beverages – Strained and clear juices – Plain gelatin
Full liquid diet • Next step after clear liquids • Liquids or foods that turn to liquid at body temperatur • For patients with: – GI problems – Unable to tolerate solid or semisolid foods – Post-surgery
Full liquid diet • Low in: – Iron – Protein – Calories • High in – Cholesterol
Full liquid diet includes: • Clear liquids plus: – Milk and milk drinks – Puddings, custards – Ice cream, sherbet, yogurt – Vegetable juices – Strained cereals – Cream, butter, margarine
Soft diet (soft mechanical diet) • Easily chewed and digested • For patients who have difficulty chewing and swallowing (ex: _______) • Also for some patients after surgery – from clear to full liquid to soft diet • Low-residue (fiber) diet containing very few uncooked foods • Can be modified Pureed diet

Diet as Tolerated •
Regular • • For patients with no special needs A balanced diet about 2000 kcals “light” diet – for postoperative patients not quite ready for regular diet
Diets Modified for Disease • Diabetes (ADA) • Heart disease (prudent diet, low sodium) • GI alterations (bland diets)

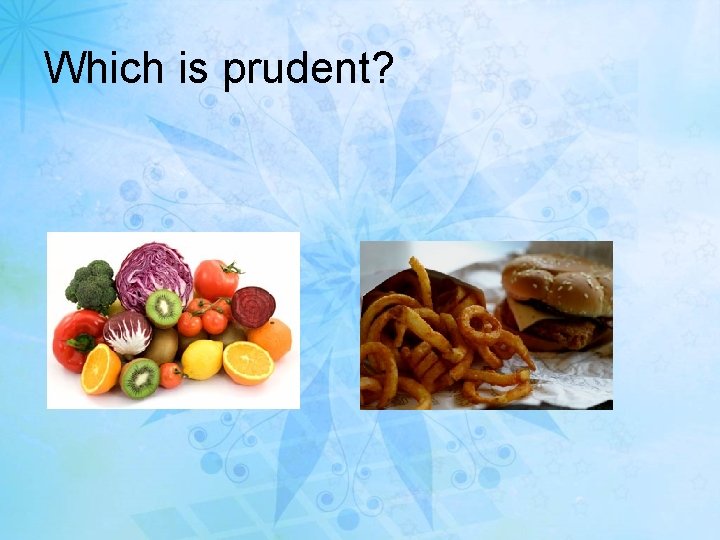
Prudent diet (low cholesterol and sodium) • To lower the LDL cholesterol levels and sodium intake • For heart disease, atherosclerosis, hyperlipidemia
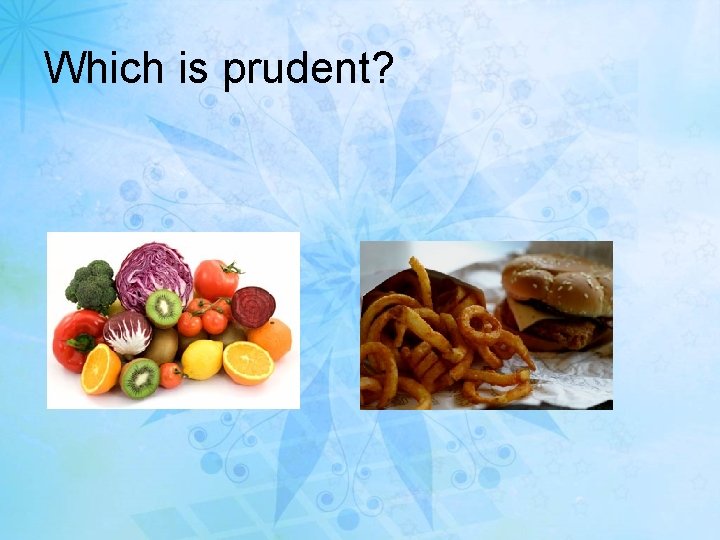
Which is prudent?
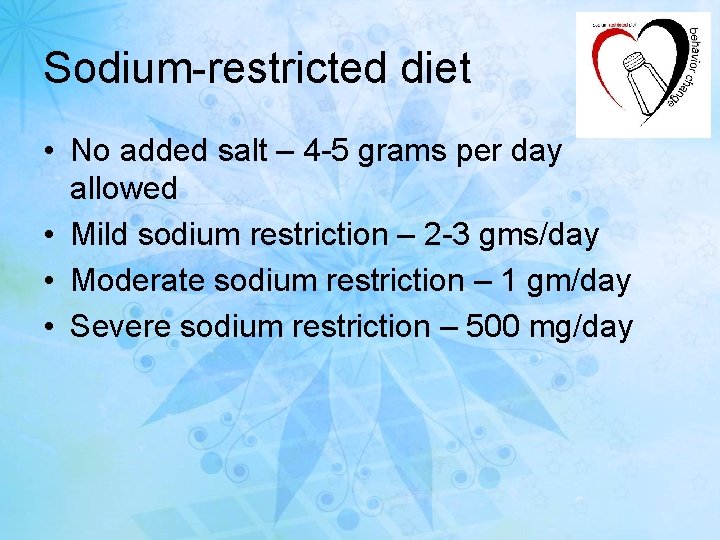
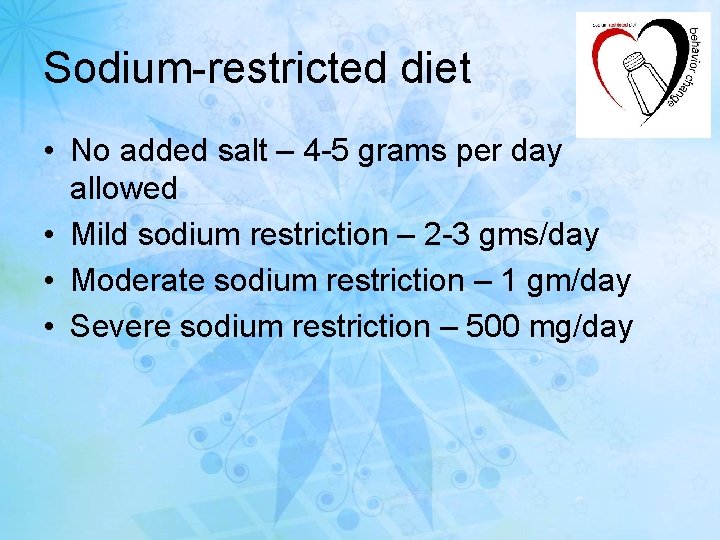
Sodium-restricted diet • No added salt – 4 -5 grams per day allowed • Mild sodium restriction – 2 -3 gms/day • Moderate sodium restriction – 1 gm/day • Severe sodium restriction – 500 mg/day
• High sodium foods include: – pickles, olives – salted nuts – soy sauce – hot dogs, bacon, sausage – processed cheese
– canned soups – potato chips – canned fish and meats – luncheon meats, ham – mustard and ketchup

Low sodium foods

High Fiber diet • Includes: – whole-wheat breads and cereals – Bran – Oatmeal – fresh fruits and vegetables with skins – and more!
NUTRITIONAL NEEDS OF SURGICAL PATIENT • Needs vary based on: – Patient’s disease process – Other chronic illnesses – Baseline nutritional status
Immediate Preoperative Period • NPO 8 – 12 hours before surgery – Ensures empty stomach to prevent: • Vomiting • Aspiration – Can impair patient’s ability to respond to metabolic stress of surgery
Postoperative Nutrition • Goal: – Maintain current lean body mass • Several factors to consider: – Surgical procedure – Expected time to resume oral intake – Complications of surgery – Preop nutritional status
Energy & Protein Requirements • Most common nutritional deficiency after surgery is protein
Energy & Protein Requirements • Protein: – Required to build new and maintain existing body tissue – Wound healing – Control edema – Bone healing – Resistance to infection
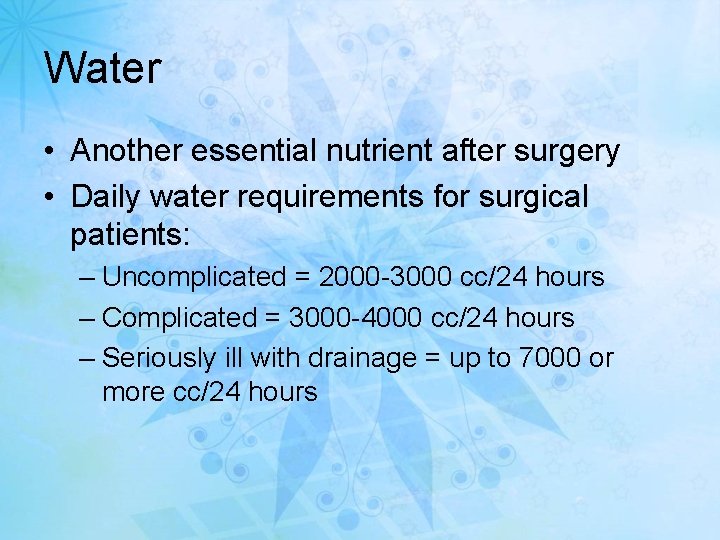
Water • Another essential nutrient after surgery • Daily water requirements for surgical patients: – Uncomplicated = 2000 -3000 cc/24 hours – Complicated = 3000 -4000 cc/24 hours – Seriously ill with drainage = up to 7000 or more cc/24 hours
Energy Needs • 2800 kcals/day needed before protein can be used in the body to repair tissue
Vitamins • Vitamin C • B- vitamins – Provide coenzyme function • Vitamin K
Minerals • Potassium lost with tissue breakdown • Other electrolyte losses – Na and Cl • Blood loss iron loss – H/H
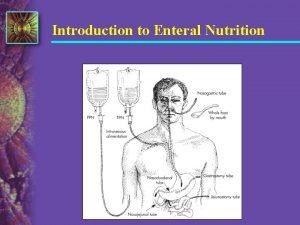
How does a surgical patient have nutritional needs met? • • IV infusing? Eats as soon as possible? Is this enough? What if a patient has an NG tube for 3 -5 days? How will that person’s nutritional needs be met?
What do IV fluids provide? • Simple IV fluids used routinely after surgery: – Provide: water, dextrose, electrolytes – Do not provide many calories or fat – Do not provide protein
If NPO for 5 days or more …. • TPN (Total Parenteral Nutrition) is usually started – Higher amount of dextrose – Amino acids – Vitamins, minerals – Lipids (fat emulsions) can be infused with TPN
Routine Postoperative Diets • Begun after adequate bowel function returns: – Flatus – Bowel sounds present • Begins with clear liquids • Advanced to full liquids • Soft/regular
Specialized Nutrition Support • Used if oral diet is not tolerated • Includes: – Tube feeding (enteral) – Parenteral nutrition • • Bowel obstructions Unable to tolerate tube feedings Ileus Major upper GI bleed

Institutional Meal Concerns & Considerations • Mealtime is often major event of the day. – Make food attractive – Have patient brush teeth or rinse out mouth – Comfortable room temperature – Comfortable lighting – Get rid of odors
 Care of the critically ill surgical patient
Care of the critically ill surgical patient Conclusion of medical surgical nursing
Conclusion of medical surgical nursing N
N Ogden surgical medical society
Ogden surgical medical society Difference between medical and surgical asepsis
Difference between medical and surgical asepsis Bibliography of medical surgical nursing
Bibliography of medical surgical nursing Patient 2 patient
Patient 2 patient What is esp
What is esp Static content vs dynamic content
Static content vs dynamic content Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction nutrition management
Small bowel obstruction nutrition management Patient centered medical home conference
Patient centered medical home conference Patient centered medical home
Patient centered medical home Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Heaton moor health centre
Heaton moor health centre Chafford hundred medical centre book an appointment
Chafford hundred medical centre book an appointment Generations
Generations In todays lesson
In todays lesson Todays with apostrophe
Todays with apostrophe Todays worldld
Todays worldld Whats thermal energy
Whats thermal energy Todays globl
Todays globl Whats todays wordlw
Whats todays wordlw Chapter 13 marketing in todays world
Chapter 13 marketing in todays world Todays plan
Todays plan Todays sabbath lesson
Todays sabbath lesson Welcome for sabbath school
Welcome for sabbath school Walsall rugby club
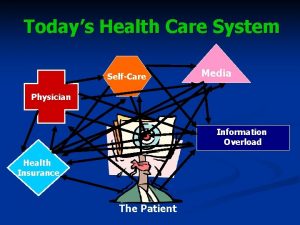
Walsall rugby club Todays health
Todays health Today's objective
Today's objective Todays objective
Todays objective Todays objective
Todays objective Todays whether
Todays whether Todays vision
Todays vision Todays objective
Todays objective Todays planetary position
Todays planetary position Mla title page
Mla title page 3 statements of cell theory
3 statements of cell theory Handcuff nomenclature quiz
Handcuff nomenclature quiz Todays weather hull
Todays weather hull Todays objective
Todays objective