m Laryngospas and Negative Pressure Pulmonary Edema v

- Slides: 23
m Laryngospas and Negative Pressure Pulmonary Edema ��. ���������
v Laryngospasm is a form of airway obstruction. v Laryngospasm is usually easily detected and managed, but may present atypically and/or be precipitated by factors which are not immediately recognized. v If poorly managed, it has the potential to cause morbidity and mortality such as severe hypoxaemia, pulmonary aspiration, and post-obstructive
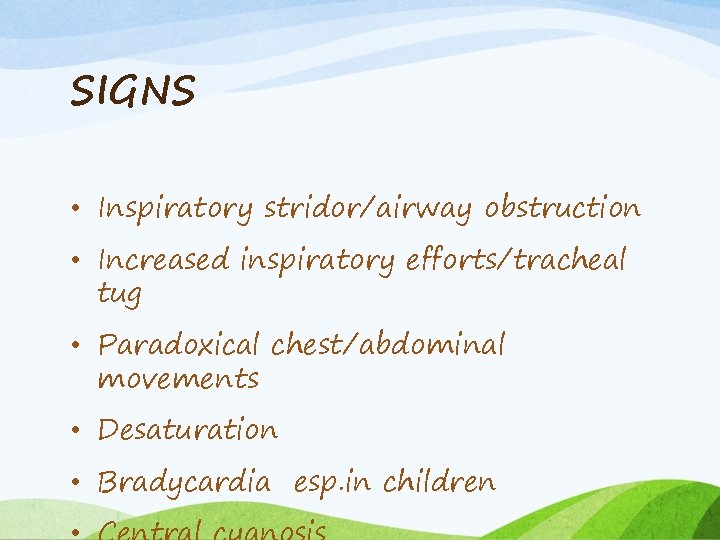
SIGNS • Inspiratory stridor/airway obstruction • Increased inspiratory efforts/tracheal tug • Paradoxical chest/abdominal movements • Desaturation • Bradycardia esp. in children
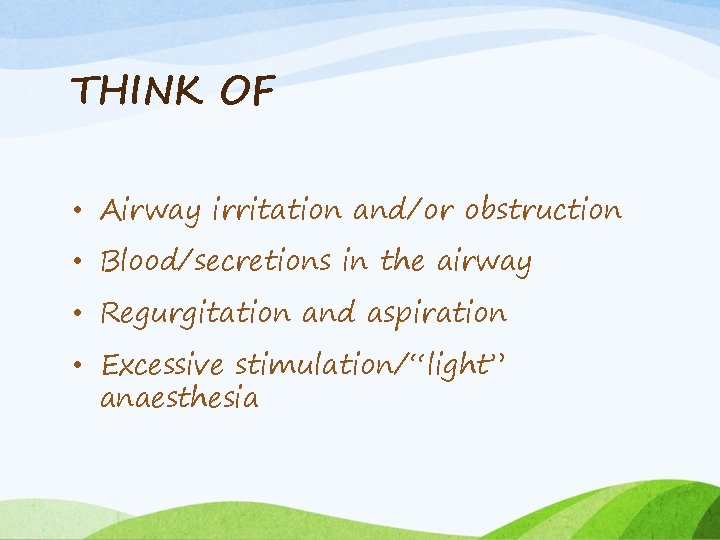
THINK OF • Airway irritation and/or obstruction • Blood/secretions in the airway • Regurgitation and aspiration • Excessive stimulation/“light” anaesthesia
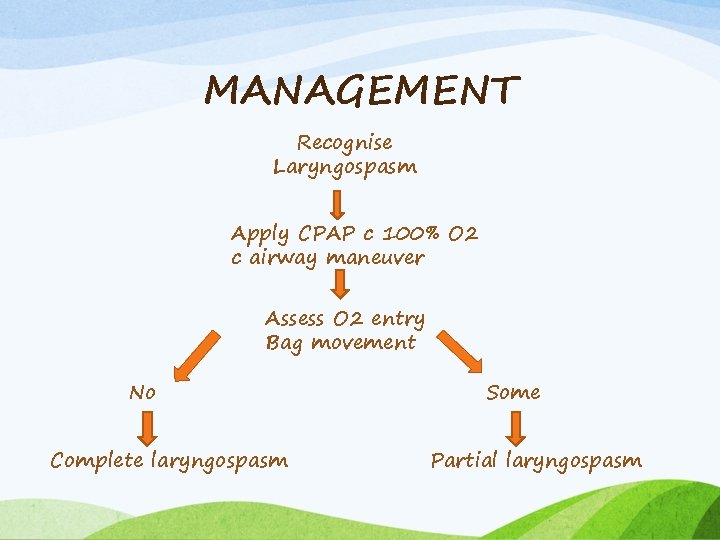
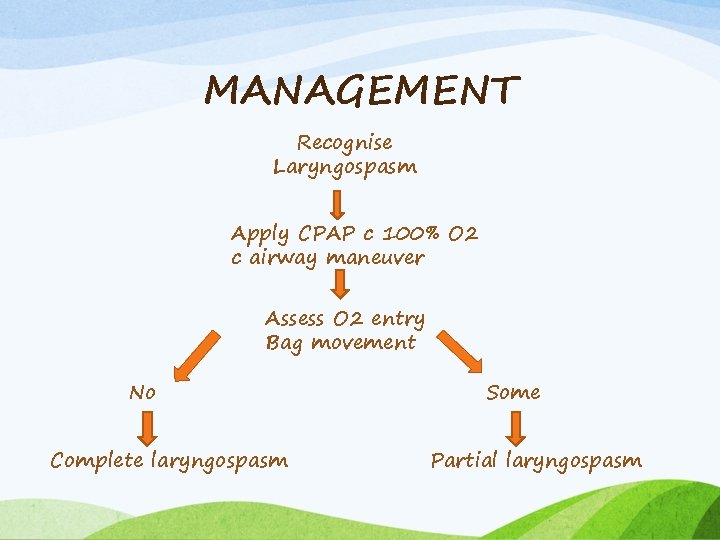
MANAGEMENT Recognise Laryngospasm Apply CPAP c 100% O 2 c airway maneuver Assess O 2 entry Bag movement No Complete laryngospasm Some Partial laryngospasm
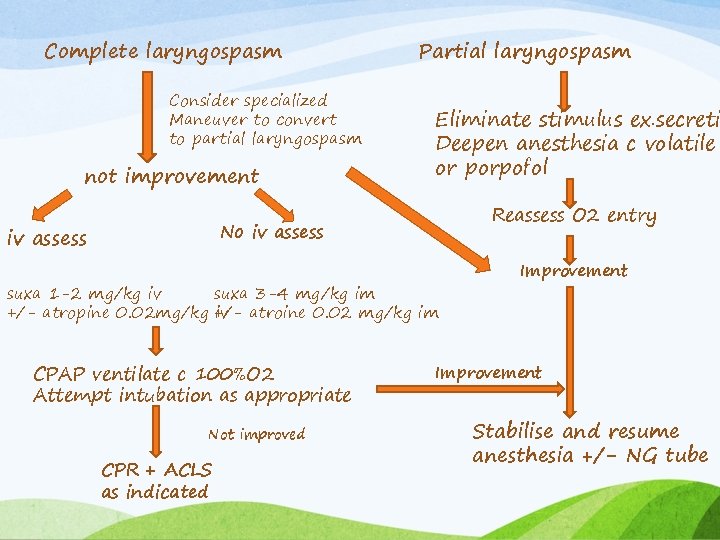
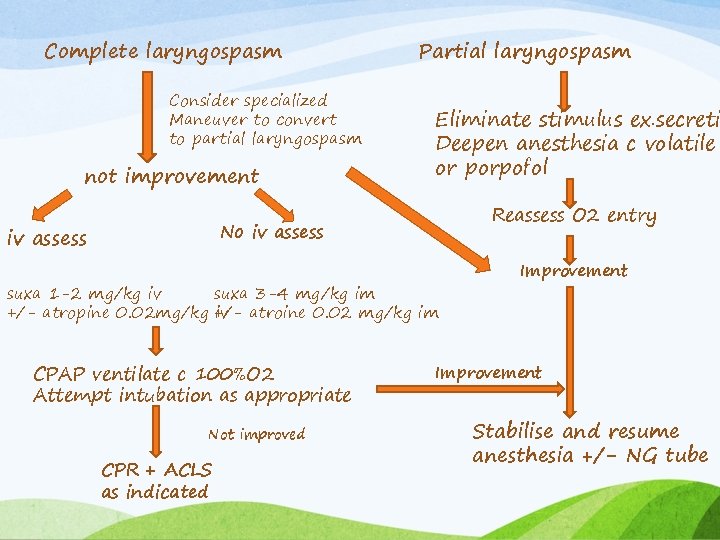
Complete laryngospasm Consider specialized Maneuver to convert to partial laryngospasm not improvement Partial laryngospasm Eliminate stimulus ex. secreti Deepen anesthesia c volatile or porpofol Reassess O 2 entry No iv assess suxa 1 -2 mg/kg iv suxa 3 -4 mg/kg im +/- atropine 0. 02 mg/kg +/iv atroine 0. 02 mg/kg im CPAP ventilate c 100%O 2 Attempt intubation as appropriate Not improved CPR + ACLS as indicated Improvement Stabilise and resume anesthesia +/- NG tube
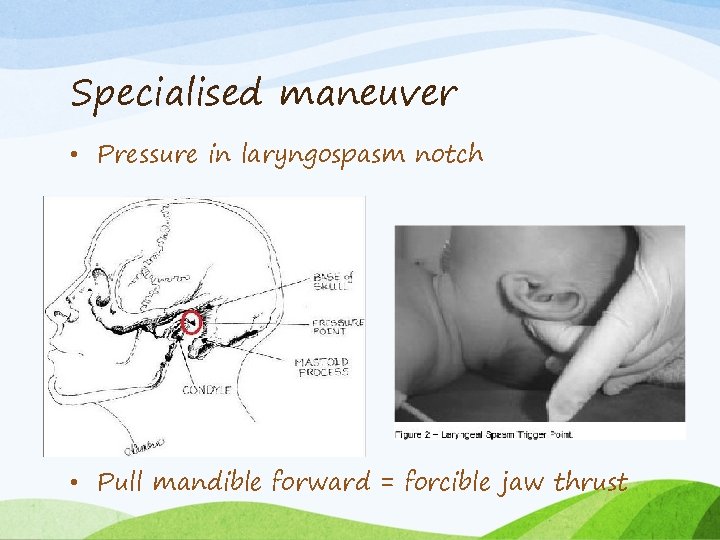
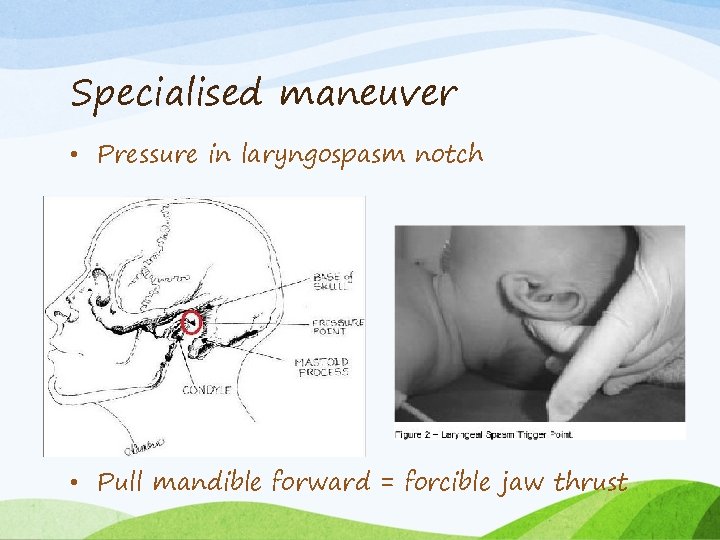
Specialised maneuver • Pressure in laryngospasm notch • Pull mandible forward = forcible jaw thrust
Negative Pressure Pulmonary Edema
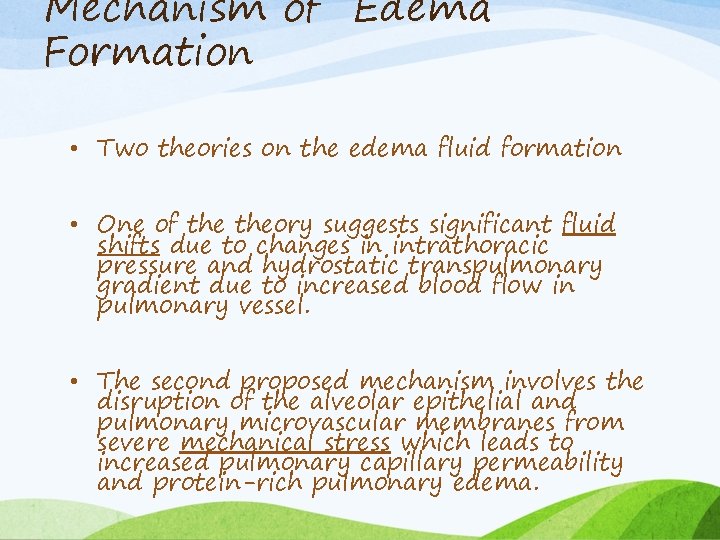
Mechanism of Edema Formation • Two theories on the edema fluid formation • One of theory suggests significant fluid shifts due to changes in intrathoracic pressure and hydrostatic transpulmonary gradient due to increased blood flow in pulmonary vessel. • The second proposed mechanism involves the disruption of the alveolar epithelial and pulmonary microvascular membranes from severe mechanical stress which leads to increased pulmonary capillary permeability and protein-rich pulmonary edema.
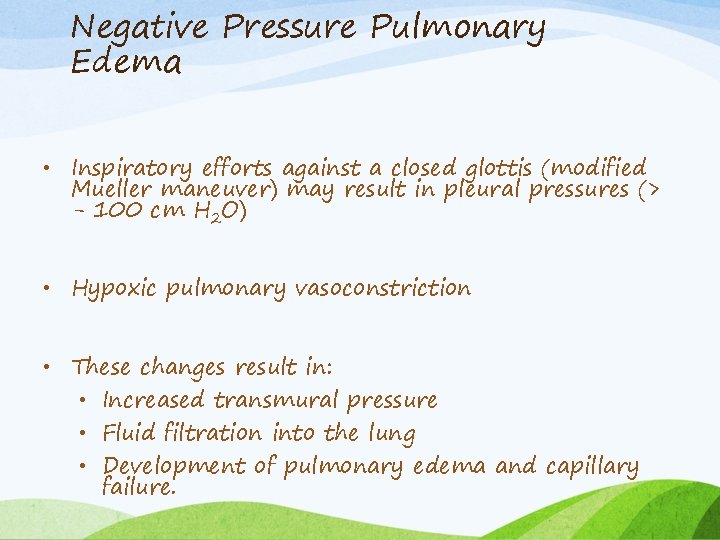
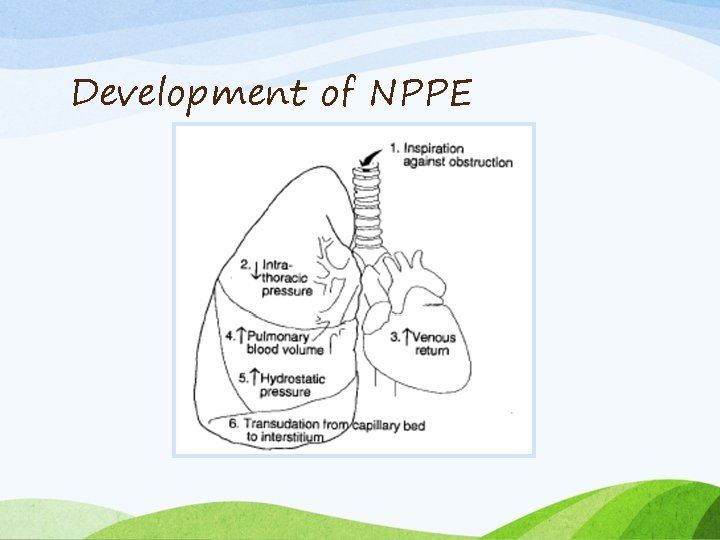
Negative Pressure Pulmonary Edema • Inspiratory efforts against a closed glottis (modified Mueller maneuver) may result in pleural pressures (> - 100 cm H 2 O) • Hypoxic pulmonary vasoconstriction • These changes result in: • Increased transmural pressure • Fluid filtration into the lung • Development of pulmonary edema and capillary failure.
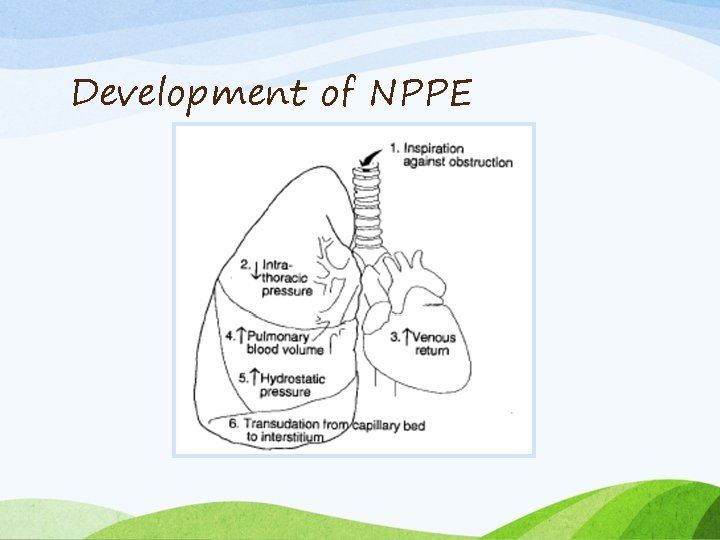
Development of NPPE
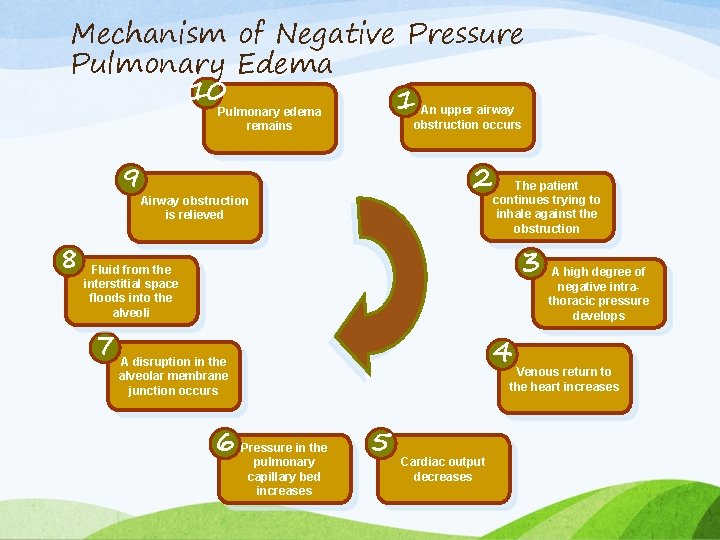
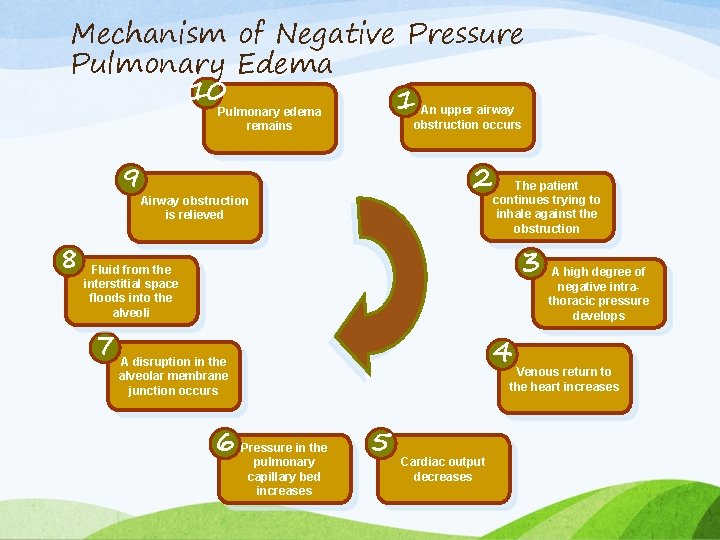
Mechanism of Negative Pressure Pulmonary Edema 10 1 An upper airway obstruction occurs Pulmonary edema remains 9 2 Airway obstruction is relieved 8 The patient continues trying to inhale against the obstruction 3 Fluid from the interstitial space floods into the alveoli 7 A disruption in the 4 A high degree of negative intrathoracic pressure develops Venous return to the heart increases alveolar membrane junction occurs 6 Pressure in the pulmonary capillary bed increases 5 Cardiac output decreases
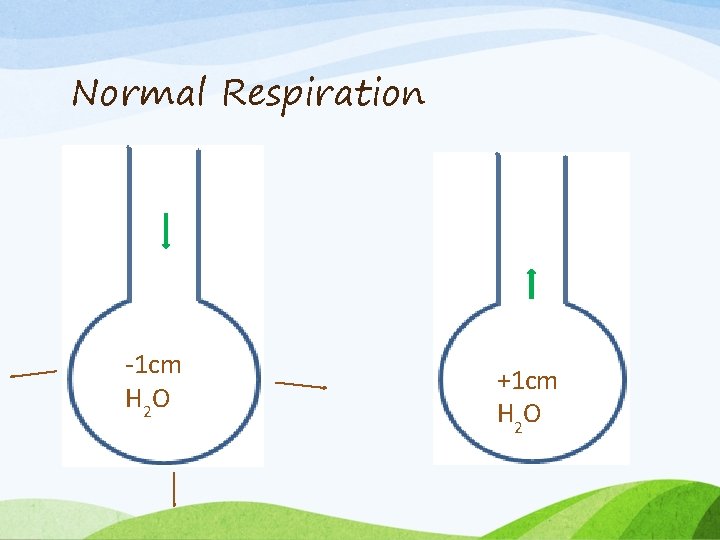
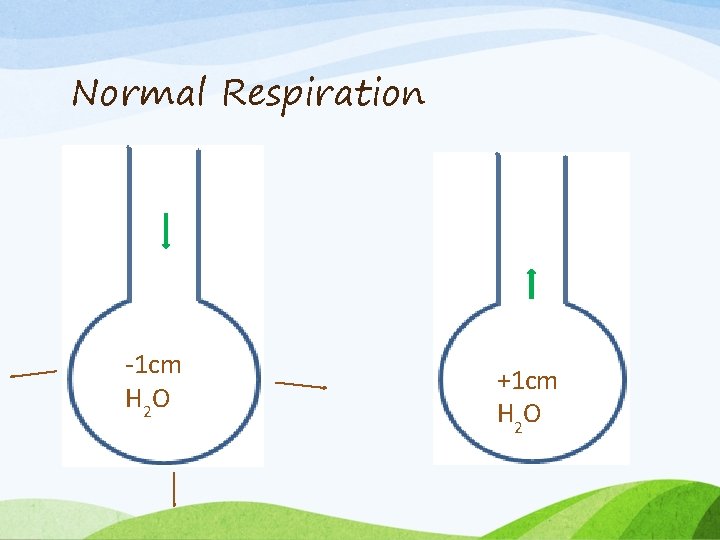
Normal Respiration -1 cm H 2 O +1 cm H 2 O
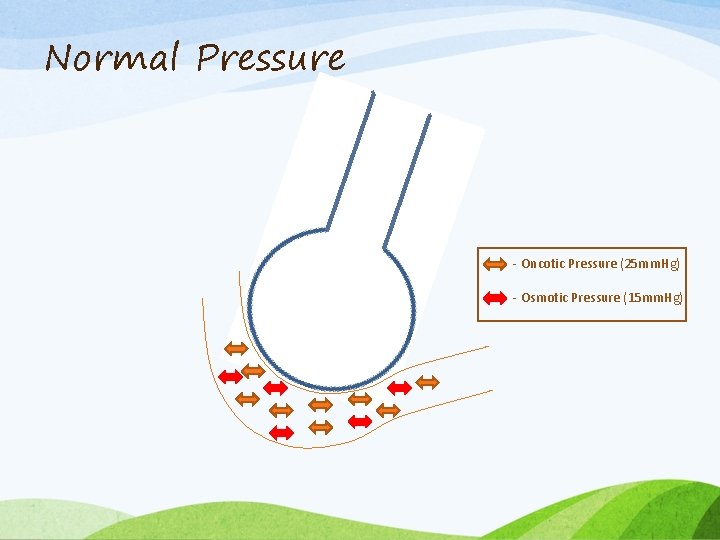
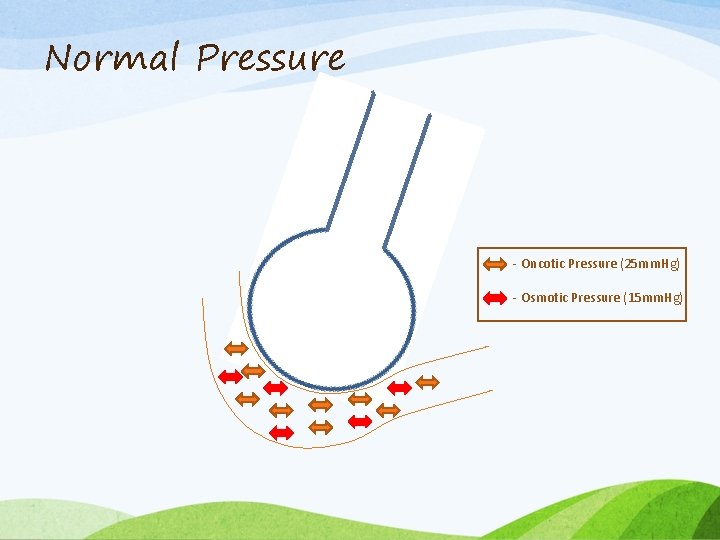
Normal Pressure - Oncotic Pressure (25 mm. Hg) - Osmotic Pressure (15 mm. Hg)
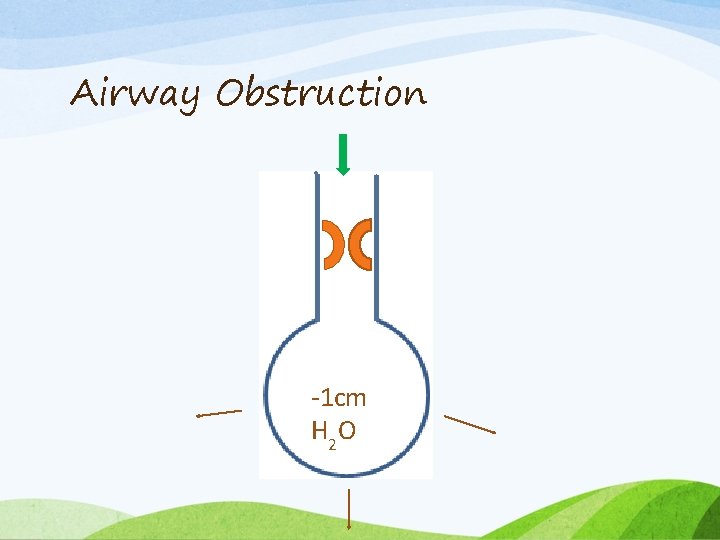
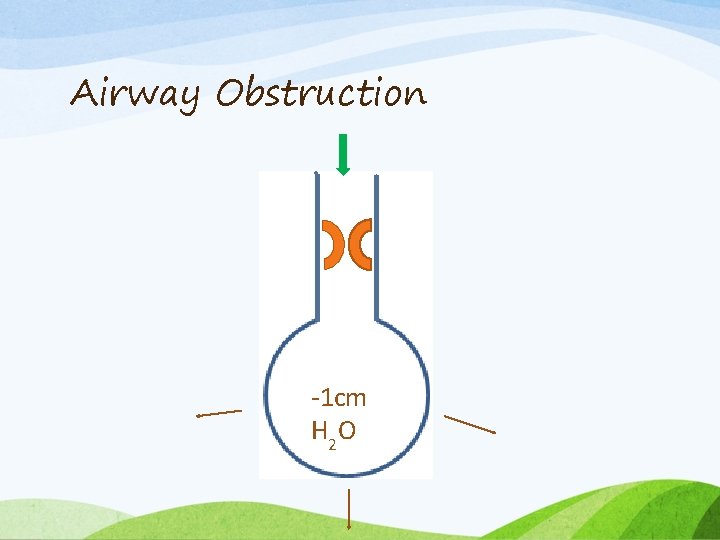
Airway Obstruction -1 cm H 2 O
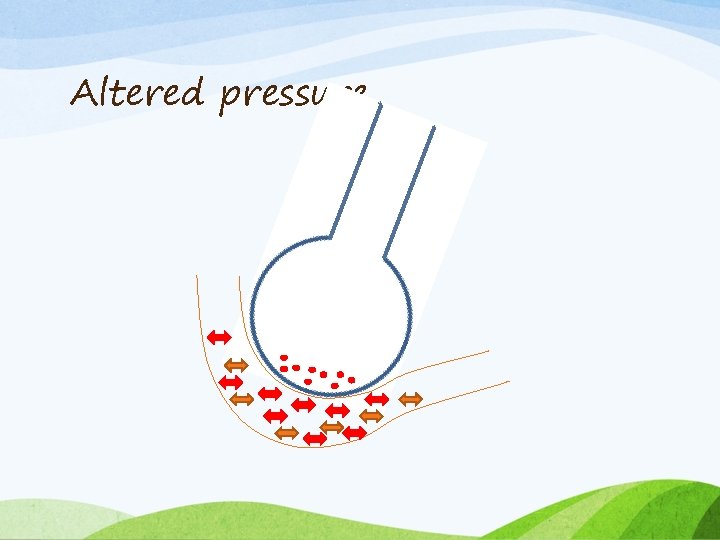
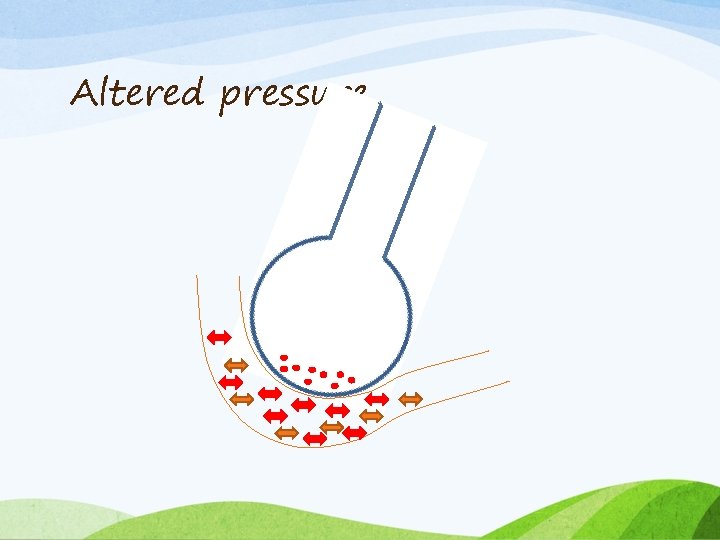
Altered pressure
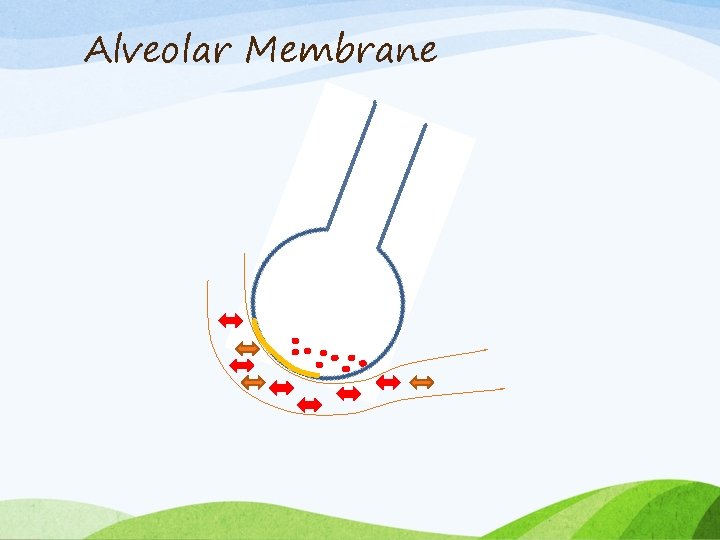
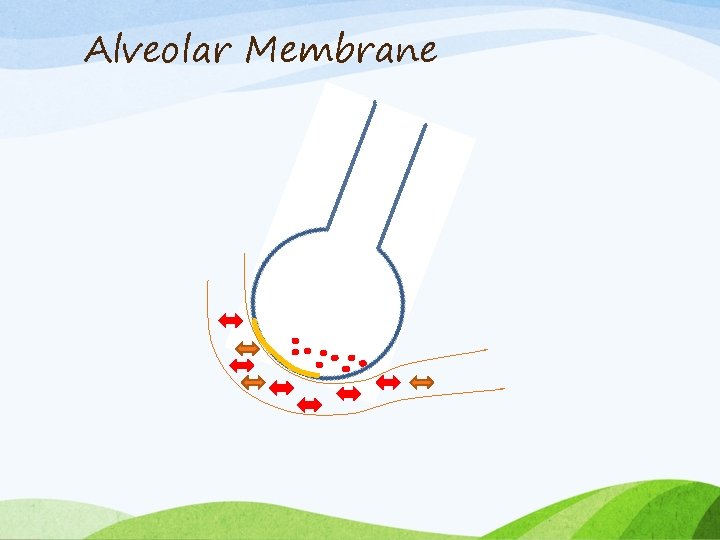
Alveolar Membrane
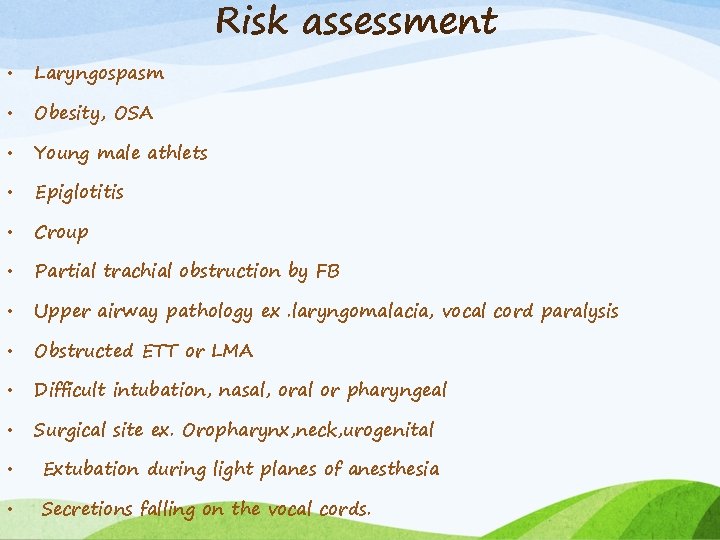
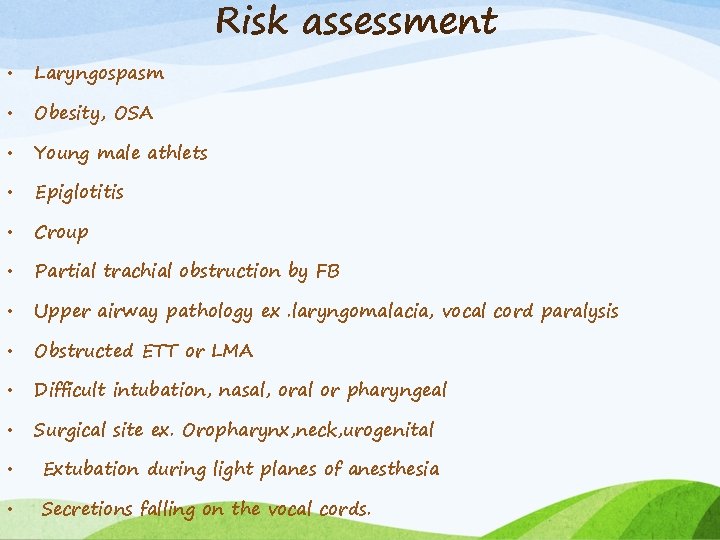
Risk assessment • Laryngospasm • Obesity, OSA • Young male athlets • Epiglotitis • Croup • Partial trachial obstruction by FB • Upper airway pathology ex. laryngomalacia, vocal cord paralysis • Obstructed ETT or LMA • Difficult intubation, nasal, oral or pharyngeal • Surgical site ex. Oropharynx, neck, urogenital • Extubation during light planes of anesthesia • Secretions falling on the vocal cords.

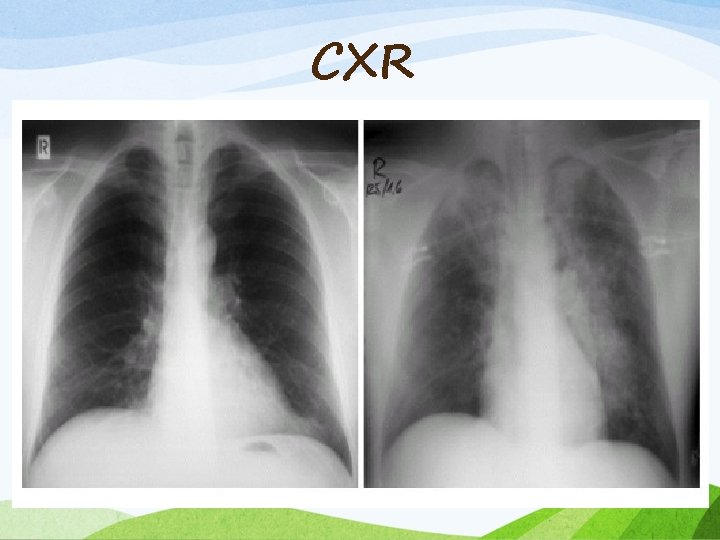
Signs and Symptoms • Frothy pink pulmonary secretions : Hallmark sign • Tachycardia, hypertension • Diaphoresis • Auscultation : Rales, Occasionally wheezing • Hypoxemia on pulse oximetry or ABG • Bilateral, alveolar infiltrates on chest x-ray
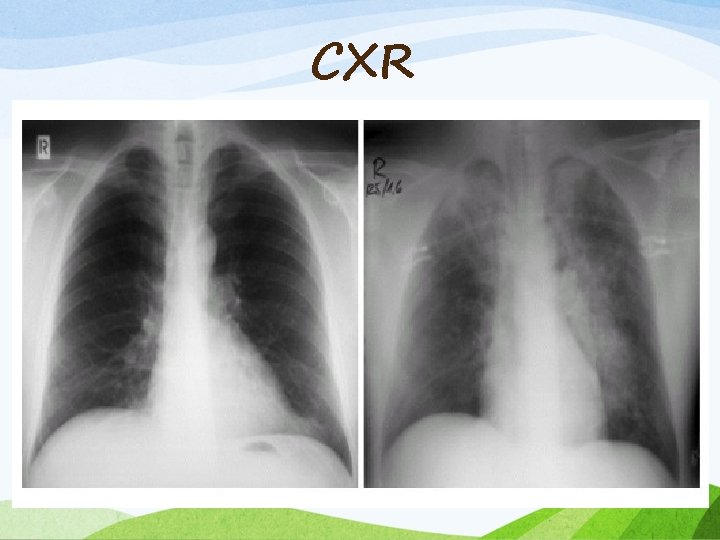
CXR
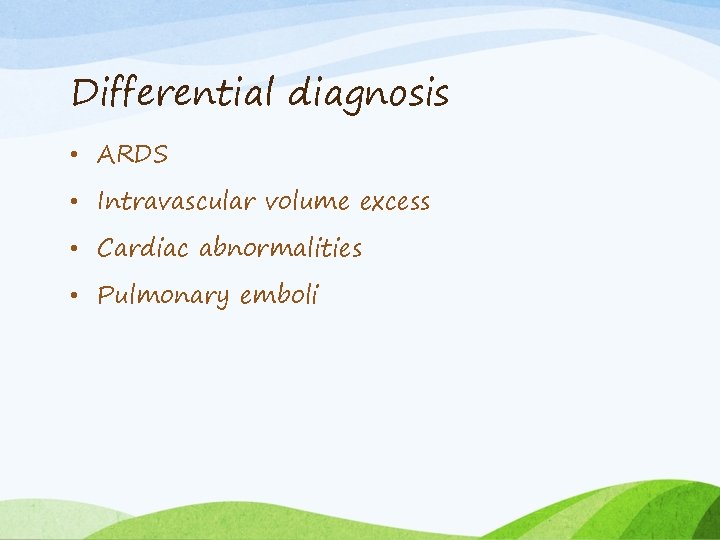
Differential diagnosis • ARDS • Intravascular volume excess • Cardiac abnormalities • Pulmonary emboli
Treatment • Early diagnosis • Reestablishment of the airway • Adequate oxygenation • Application of positive airway pressure • Via face mask or LMA • Endotracheal intubation with vent support • Although NPPE does not result from fluid overload, most authors recommend gentle diuresis using low-dose furosemide(1 mg/kg).
Prevention • Early recognition • Avoid potential obstruction • Ensure adequate depth of anesthesia during use of facemask or LMA • Consider the use of Bite block to ensure patency of artificial airway during emergence from anesthesia • Perform trachial extubation in fully awake Pt.
 Pulmonary edema
Pulmonary edema Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Pa systolic pressure range
Pa systolic pressure range Mean pulmonary arterial pressure
Mean pulmonary arterial pressure Dynamic pressure formula
Dynamic pressure formula Osmolality vs osmolarity
Osmolality vs osmolarity High pressure and low pressure
High pressure and low pressure Low atmospheric pressure
Low atmospheric pressure Difference between renal and cardiac edema
Difference between renal and cardiac edema Patella type 3
Patella type 3 Pressure support vs pressure control
Pressure support vs pressure control Continuous bedside pressure mapping
Continuous bedside pressure mapping Intrapleural pressure
Intrapleural pressure Oncotic pressure vs osmotic pressure
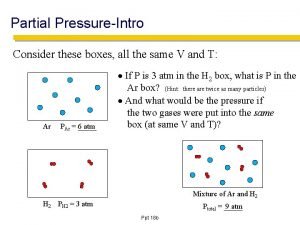
Oncotic pressure vs osmotic pressure Partial pressure formula
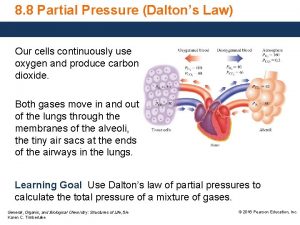
Partial pressure formula Intra plural pressure
Intra plural pressure Metamorphic
Metamorphic ütube
ütube Oncotic pressure vs hydrostatic
Oncotic pressure vs hydrostatic Oncotic pressure
Oncotic pressure Oncotic pressure vs hydrostatic pressure
Oncotic pressure vs hydrostatic pressure Dynamothermal
Dynamothermal Mean arterial pressure
Mean arterial pressure How to find partial pressure
How to find partial pressure