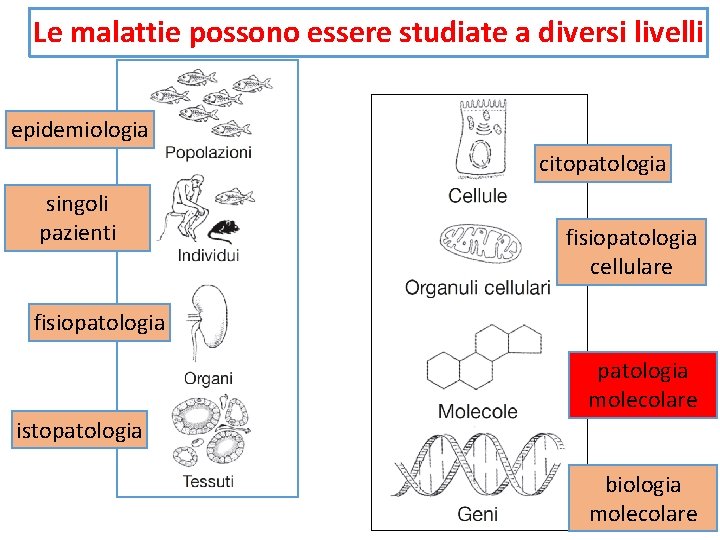
Le malattie possono essere studiate a diversi livelli
![Damage-Associated Molecular Patterns ● DAMPs: [allarmins] ● intracellular proteins, such as heat-shock proteins (HSP) Damage-Associated Molecular Patterns ● DAMPs: [allarmins] ● intracellular proteins, such as heat-shock proteins (HSP)](https://slidetodoc.com/presentation_image_h2/8366cdaa04e85ad637c54415e21b2b62/image-25.jpg)
- Slides: 35
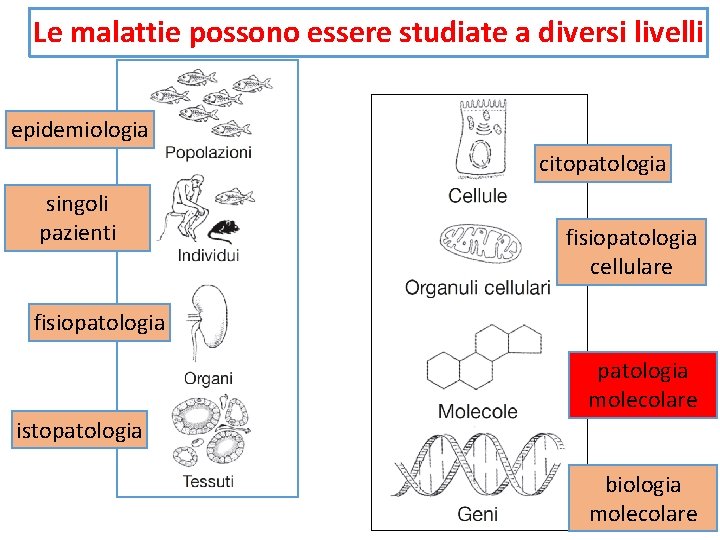
Le malattie possono essere studiate a diversi livelli epidemiologia citopatologia singoli pazienti fisiopatologia cellulare fisiopatologia molecolare istopatologia biologia molecolare
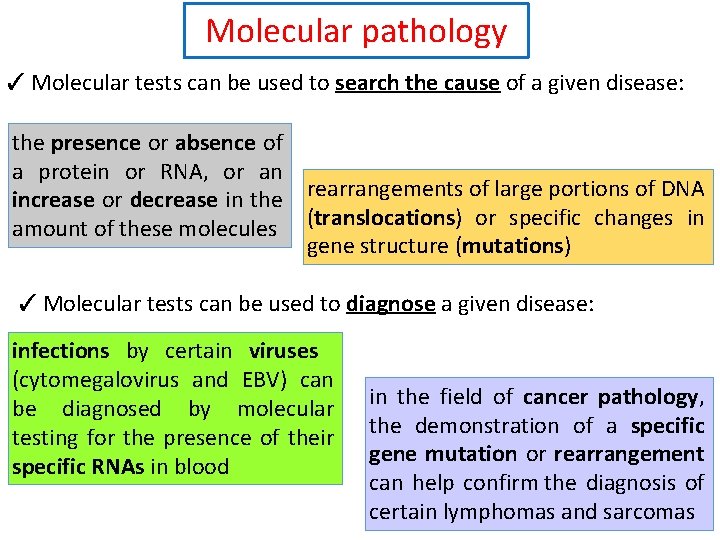
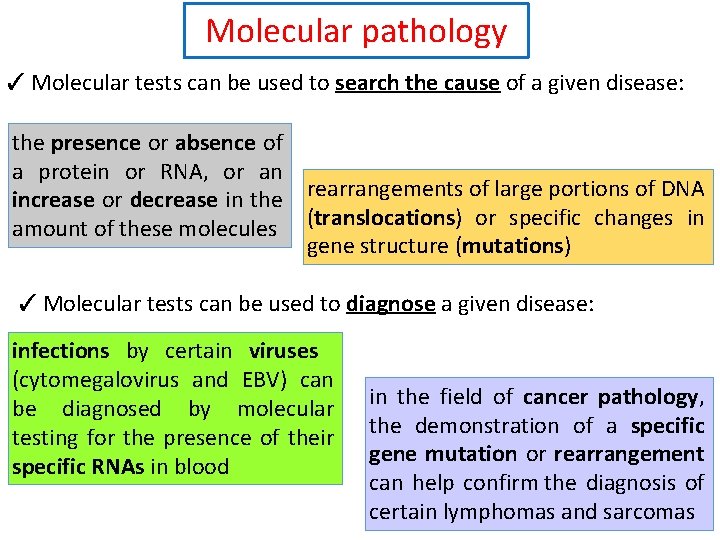
Molecular pathology ✓ Molecular tests can be used to search the cause of a given disease: the presence or absence of a protein or RNA, or an increase or decrease in the rearrangements of large portions of DNA amount of these molecules (translocations) or specific changes in gene structure (mutations) ✓ Molecular tests can be used to diagnose a given disease: infections by certain viruses (cytomegalovirus and EBV) can be diagnosed by molecular testing for the presence of their specific RNAs in blood in the field of cancer pathology, the demonstration of a specific gene mutation or rearrangement can help confirm the diagnosis of certain lymphomas and sarcomas
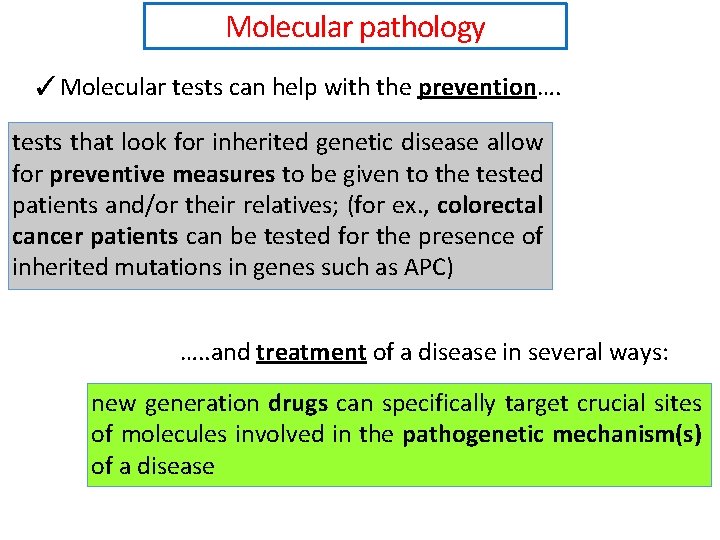
Molecular pathology ✓Molecular tests can help with the prevention…. tests that look for inherited genetic disease allow for preventive measures to be given to the tested patients and/or their relatives; (for ex. , colorectal cancer patients can be tested for the presence of inherited mutations in genes such as APC) …. . and treatment of a disease in several ways: new generation drugs can specifically target crucial sites of molecules involved in the pathogenetic mechanism(s) of a disease
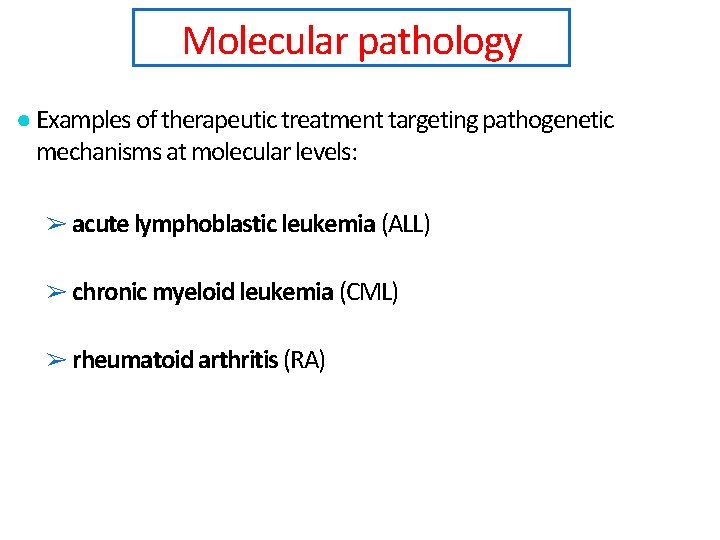
Molecular pathology ● Examples of therapeutic treatment targeting pathogenetic mechanisms at molecular levels: ➢ acute lymphoblastic leukemia (ALL) ➢ chronic myeloid leukemia (CML) ➢ rheumatoid arthritis (RA)
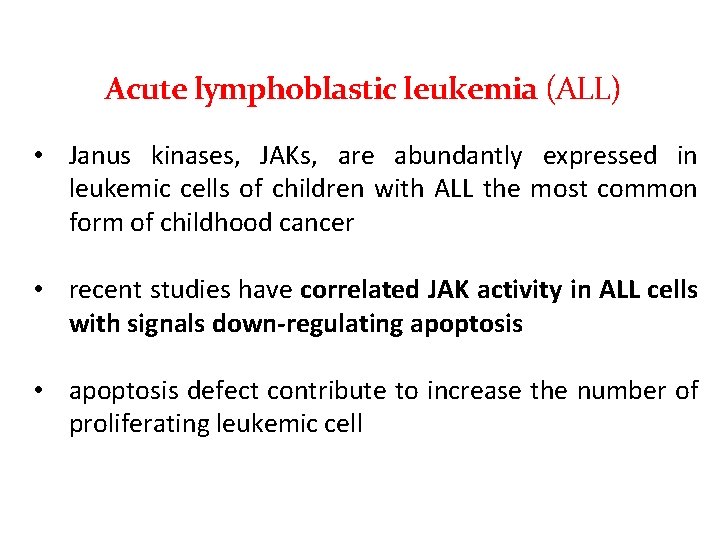
Acute lymphoblastic leukemia (ALL) • Janus kinases, JAKs, are abundantly expressed in leukemic cells of children with ALL the most common form of childhood cancer • recent studies have correlated JAK activity in ALL cells with signals down-regulating apoptosis • apoptosis defect contribute to increase the number of proliferating leukemic cell
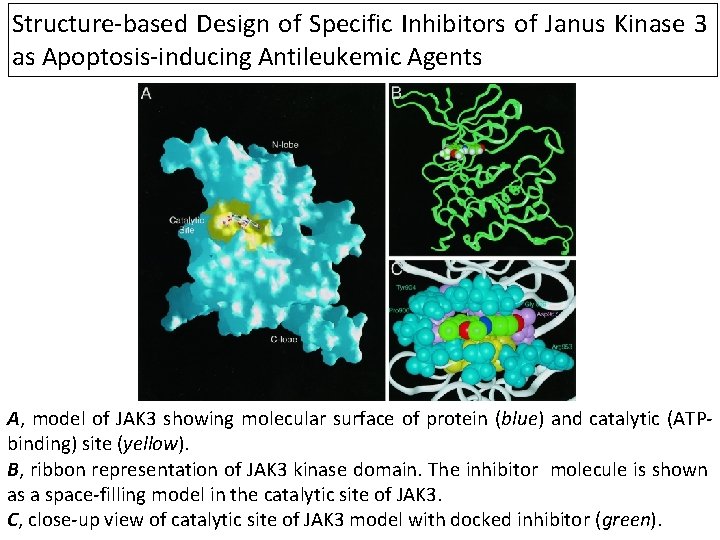
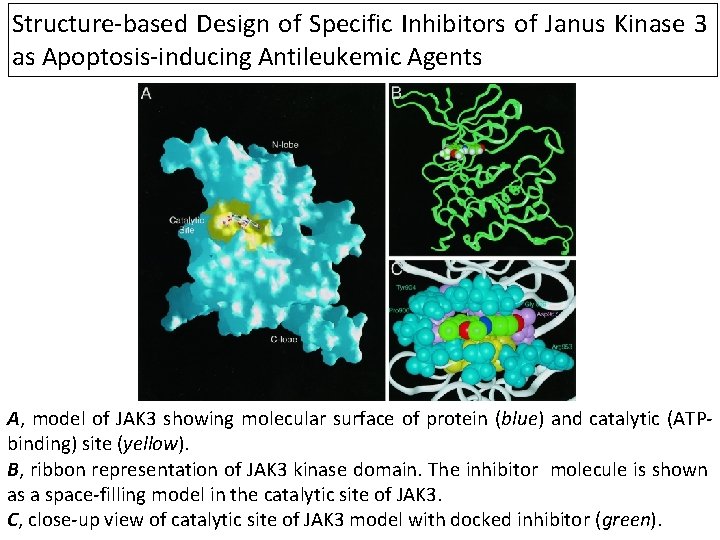
Structure-based Design of Specific Inhibitors of Janus Kinase 3 as Apoptosis-inducing Antileukemic Agents A, model of JAK 3 showing molecular surface of protein (blue) and catalytic (ATPbinding) site (yellow). B, ribbon representation of JAK 3 kinase domain. The inhibitor molecule is shown as a space-filling model in the catalytic site of JAK 3. C, close-up view of catalytic site of JAK 3 model with docked inhibitor (green).
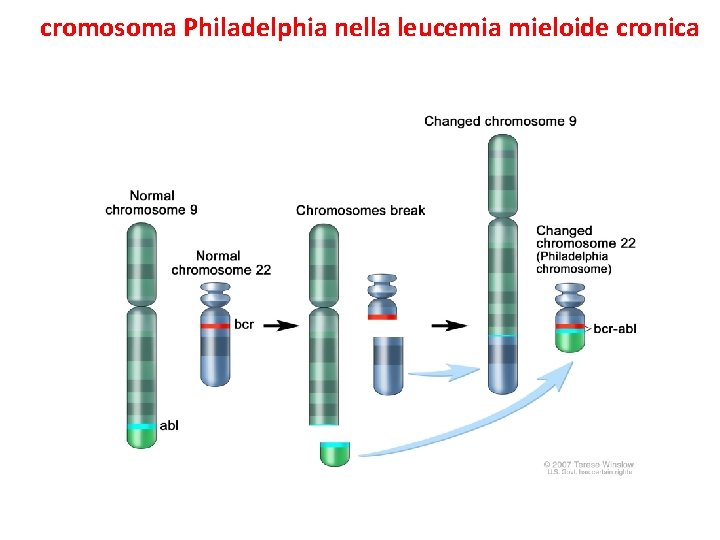
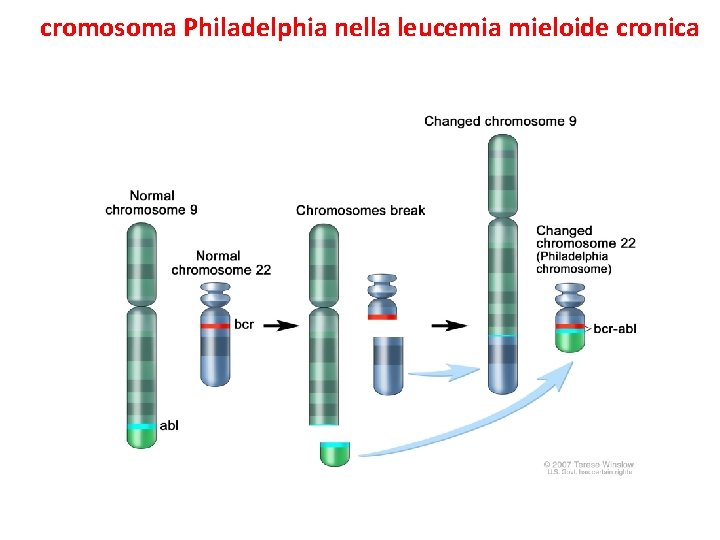
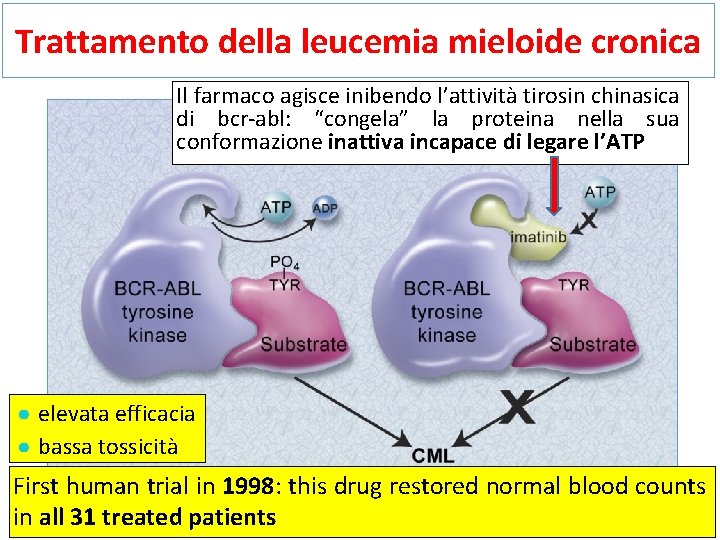
Il cromosoma Philadelphia nella leucemia mieloide cronica Il gene di fusione ABL-BCR produce una proteina ad attività tirosin chinasica che non risponde più ai normali controlli (loss of negative regulatory domains)
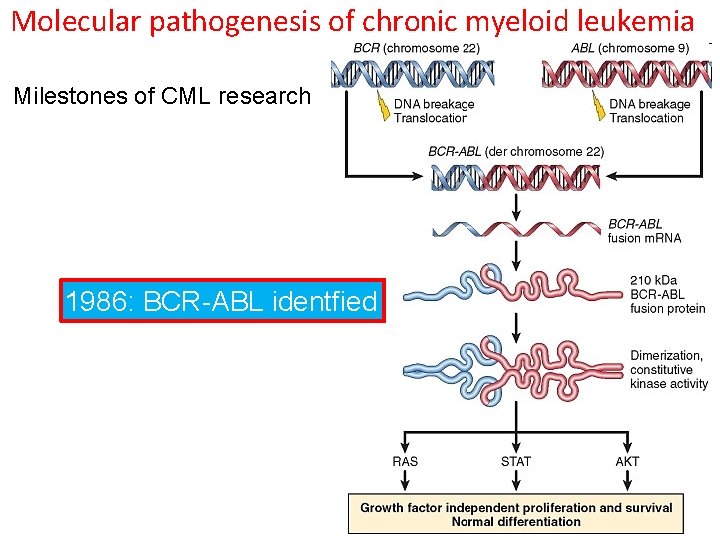
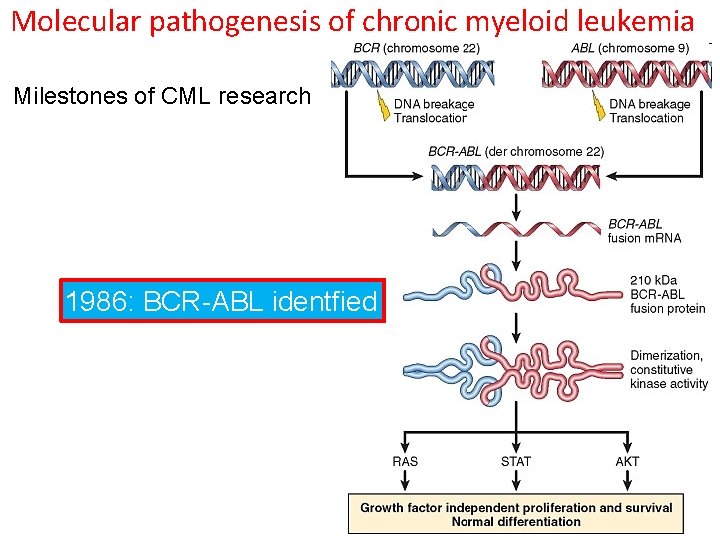
Molecular pathogenesis of chronic myeloid leukemia Milestones of CML research 1845: CML described 1960: 22 Ph’ identified 1973: t(9: 22) identified 1986: BCR-ABL identfied 1998: BCR-ABL inhibitor tested in CML patients 2001: Gleevec (Imatinib) approved by FDA
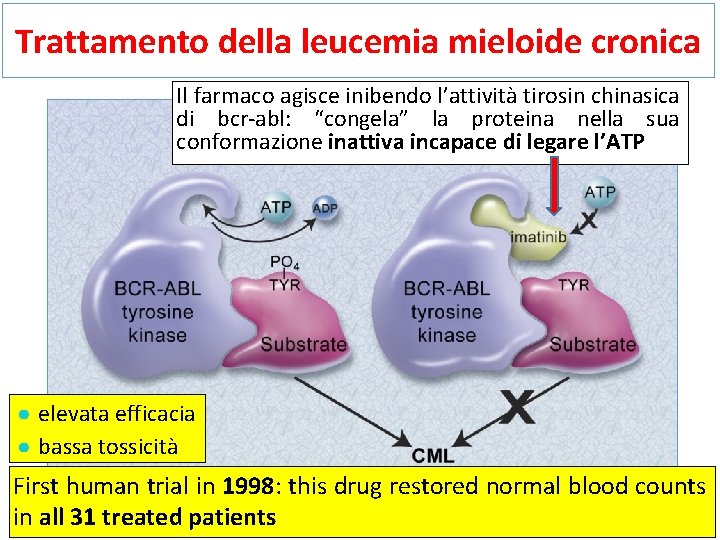
Trattamento della leucemia mieloide cronica Il farmaco agisce inibendo l’attività tirosin chinasica di bcr-abl: “congela” la proteina nella sua conformazione inattiva incapace di legare l’ATP ● elevata efficacia ● bassa tossicità First human trial in 1998: this drug restored normal blood counts in all 31 treated patients
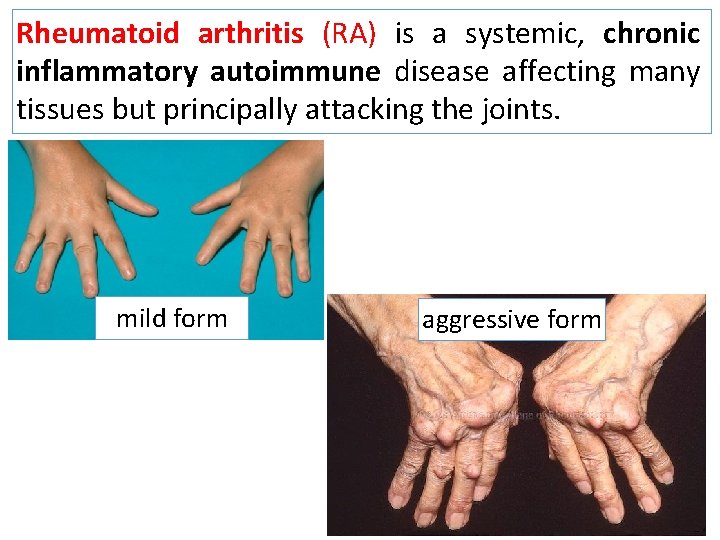
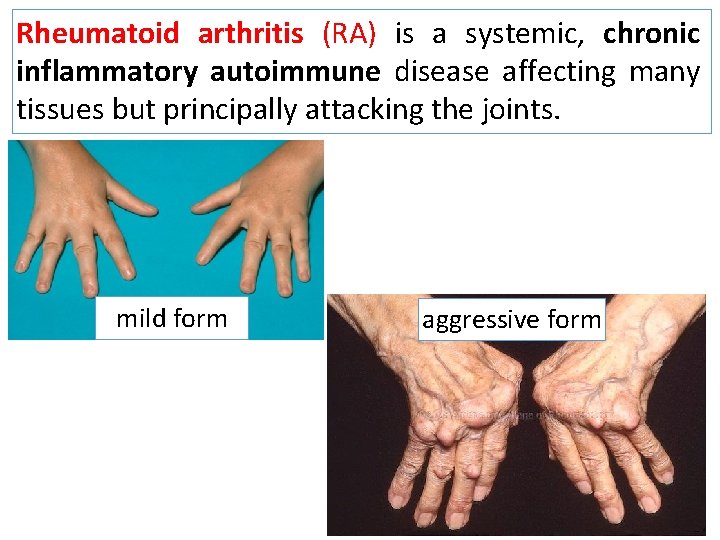
Rheumatoid arthritis (RA) is a systemic, chronic inflammatory autoimmune disease affecting many tissues but principally attacking the joints. mild form aggressive form
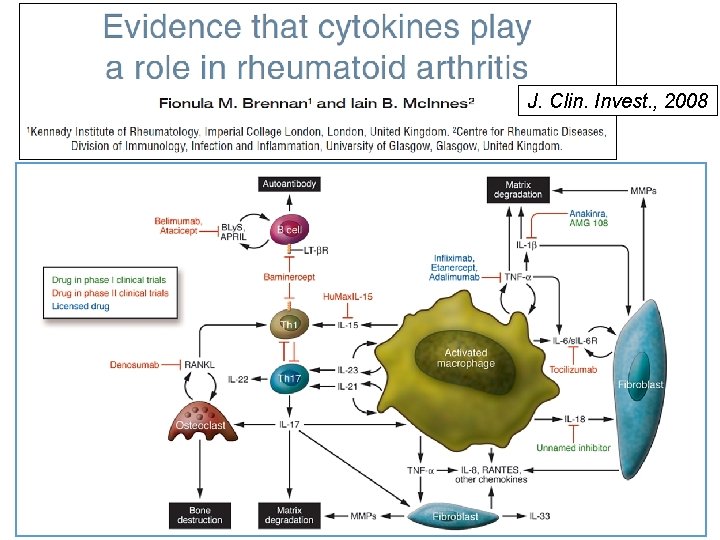
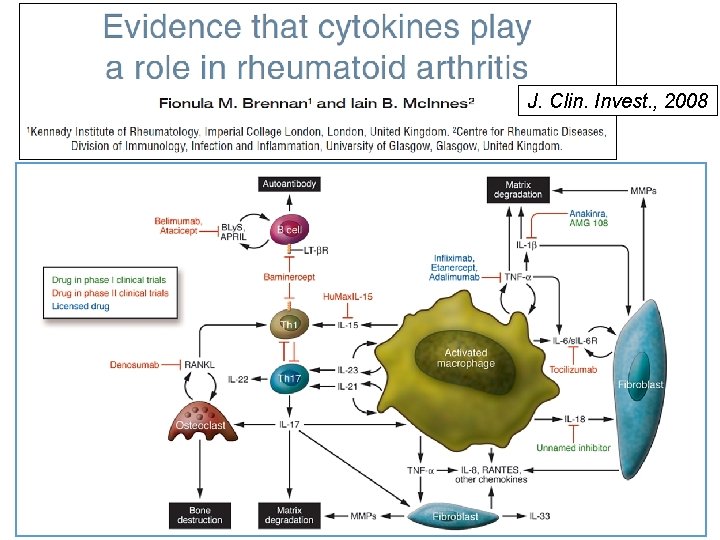
J. Clin. Invest. , 2008
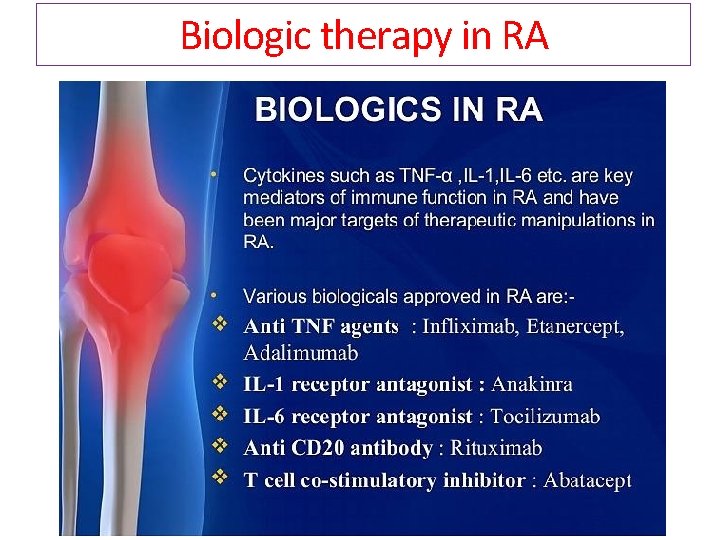
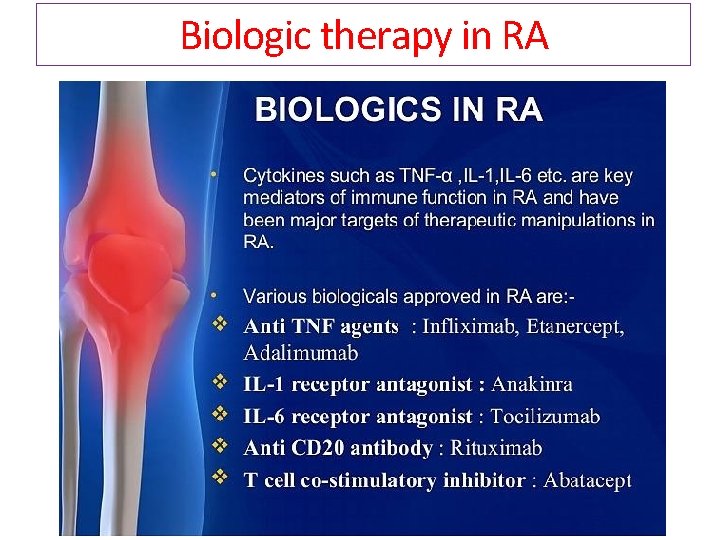
Biologic therapy in RA
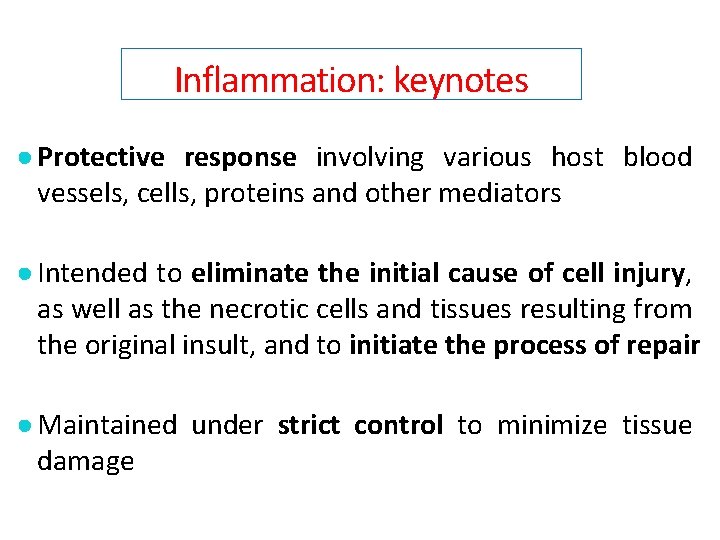
Inflammation: keynotes ● Protective response involving various host blood vessels, cells, proteins and other mediators ● Intended to eliminate the initial cause of cell injury, as well as the necrotic cells and tissues resulting from the original insult, and to initiate the process of repair ● Maintained under strict control to minimize tissue damage
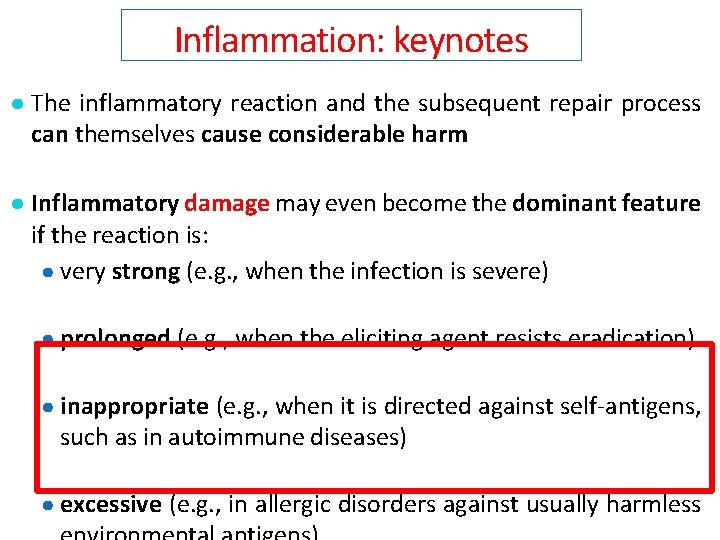
Inflammation: keynotes ● The inflammatory reaction and the subsequent repair process can themselves cause considerable harm ● Inflammatory damage may even become the dominant feature if the reaction is: ● very strong (e. g. , when the infection is severe) ● prolonged (e. g. , when the eliciting agent resists eradication) ● inappropriate (e. g. , when it is directed against self-antigens, such as in autoimmune diseases) ● excessive (e. g. , in allergic disorders against usually harmless
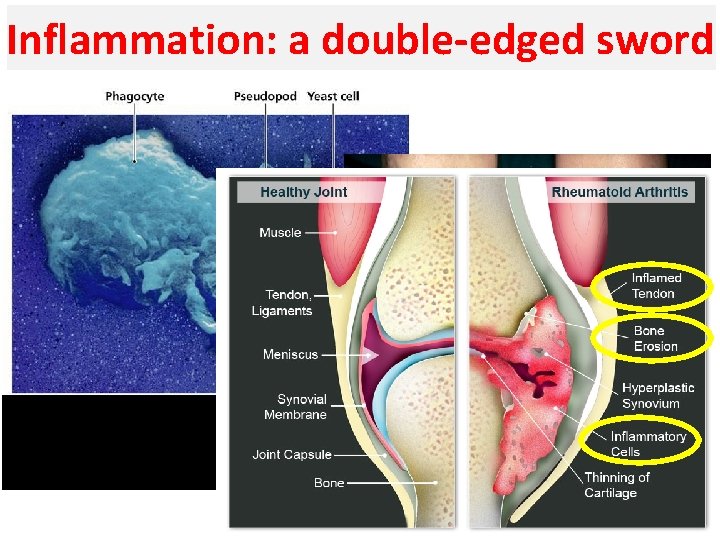
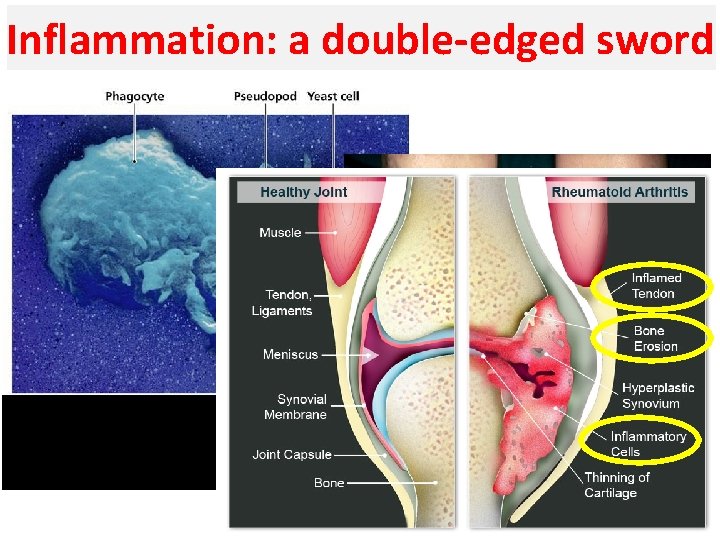
Inflammation: a double-edged sword During the inflammatory response, the phagocytes eliminate the invading pathogens
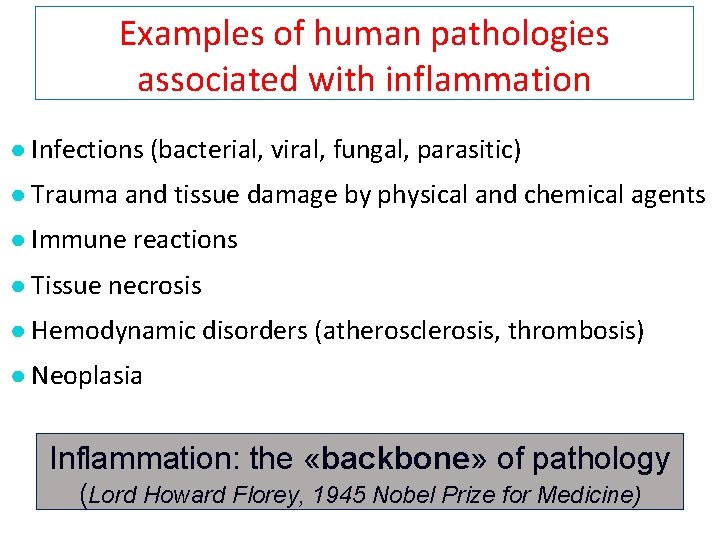
Examples of human pathologies associated with inflammation ● Infections (bacterial, viral, fungal, parasitic) ● Trauma and tissue damage by physical and chemical agents ● Immune reactions ● Tissue necrosis ● Hemodynamic disorders (atherosclerosis, thrombosis) ● Neoplasia Inflammation: the «backbone» of pathology (Lord Howard Florey, 1945 Nobel Prize for Medicine)
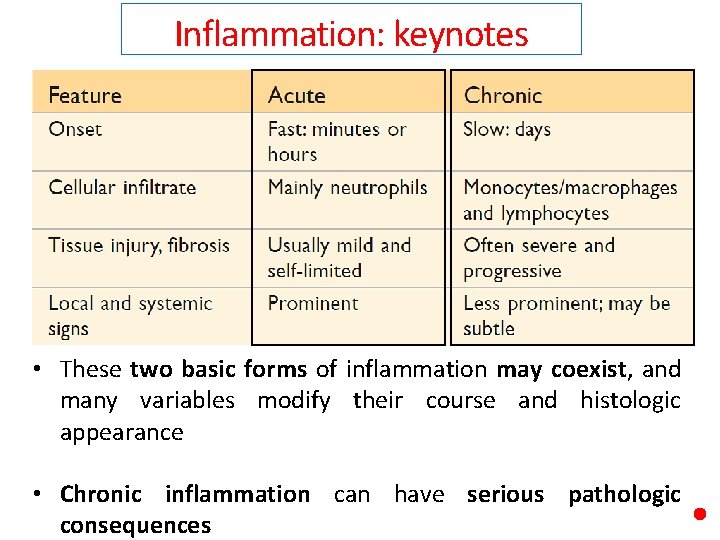
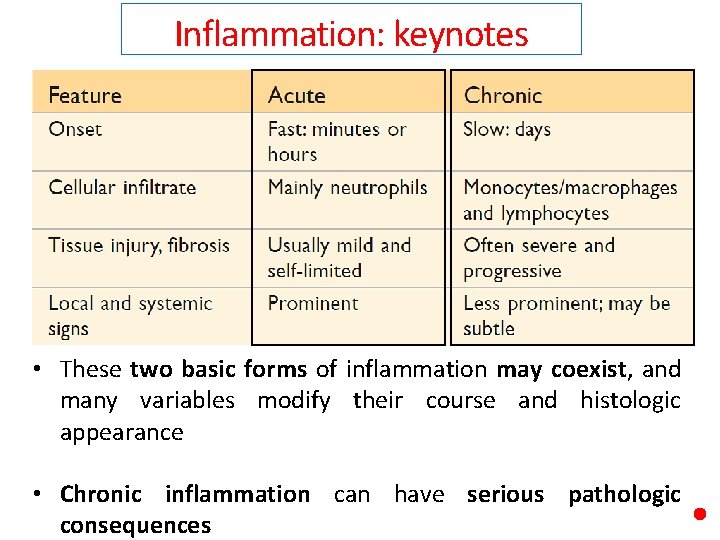
Inflammation: keynotes • These two basic forms of inflammation may coexist, and many variables modify their course and histologic appearance • Chronic inflammation can have serious pathologic consequences
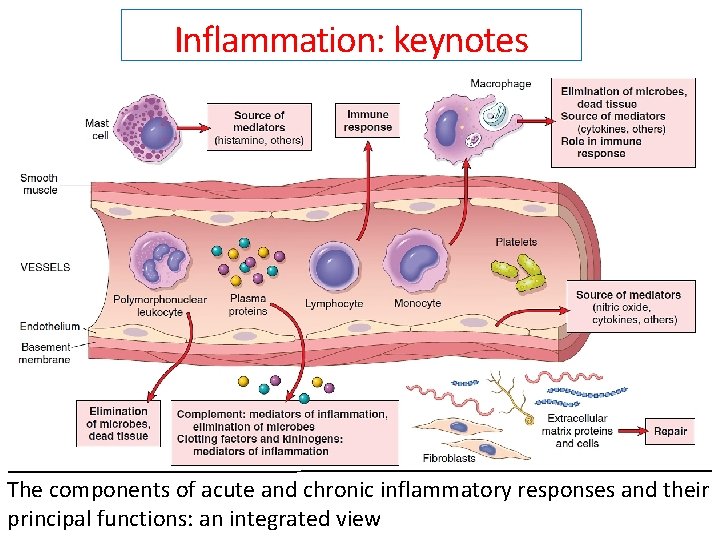
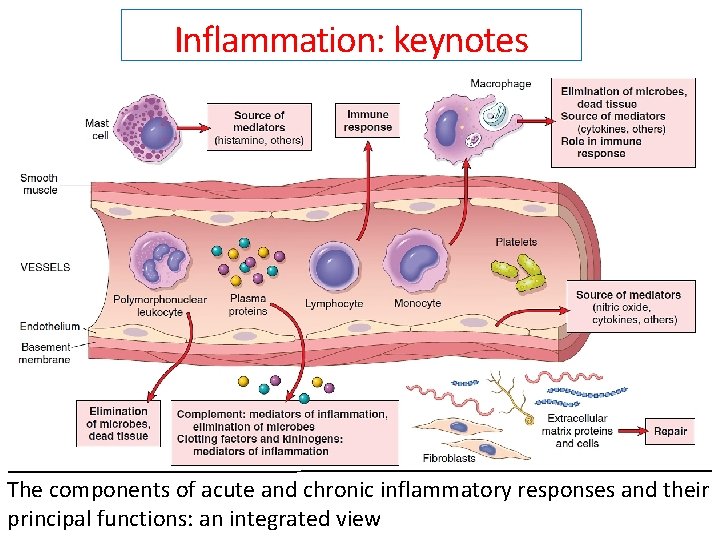
Inflammation: keynotes The components of acute and chronic inflammatory responses and their principal functions: an integrated view
Acute inflammation
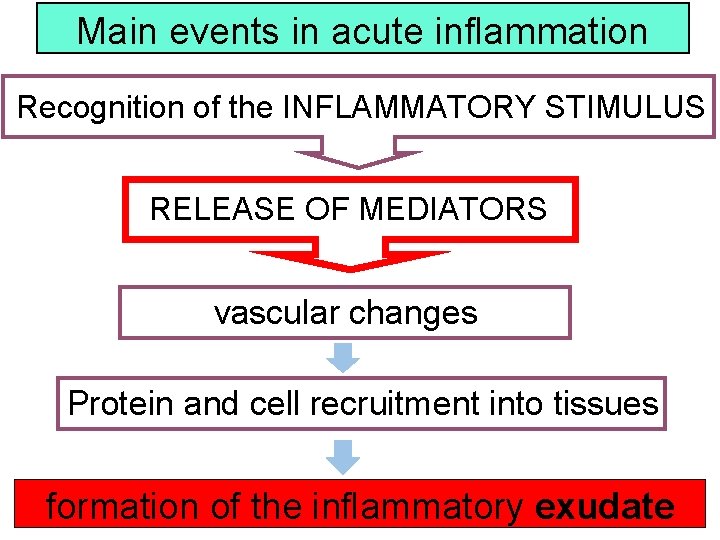
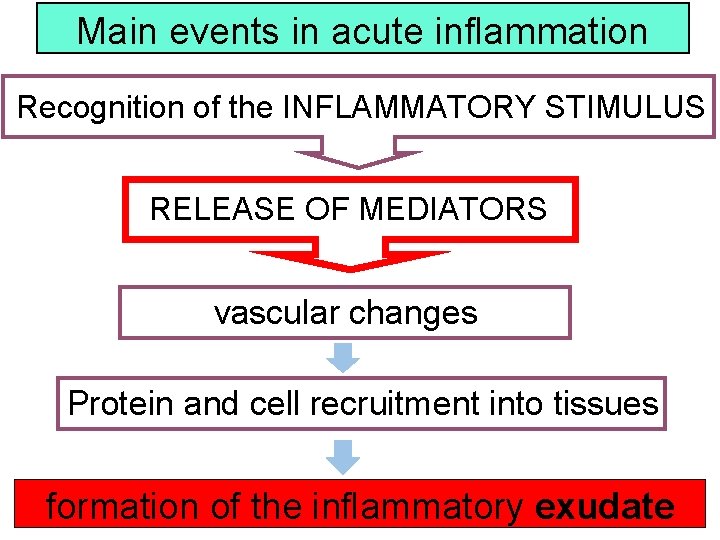
Main events in acute inflammation Recognition of the INFLAMMATORY STIMULUS RELEASE OF MEDIATORS vascular changes Protein and cell recruitment into tissues formation of the inflammatory exudate
Main events in acute inflammation Recognition of the INFLAMMATORY STIMULUS
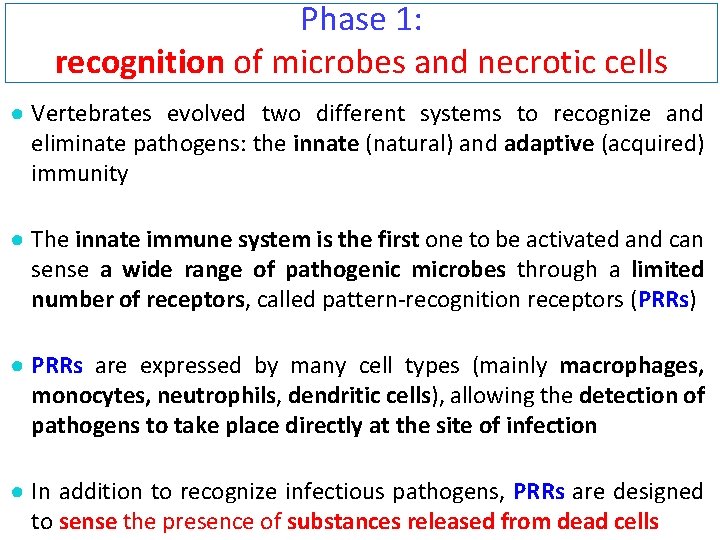
Phase 1: recognition of microbes and necrotic cells ● Vertebrates evolved two different systems to recognize and eliminate pathogens: the innate (natural) and adaptive (acquired) immunity ● The innate immune system is the first one to be activated and can sense a wide range of pathogenic microbes through a limited number of receptors, called pattern-recognition receptors (PRRs) ● PRRs are expressed by many cell types (mainly macrophages, monocytes, neutrophils, dendritic cells), allowing the detection of pathogens to take place directly at the site of infection ● In addition to recognize infectious pathogens, PRRs are designed to sense the presence of substances released from dead cells
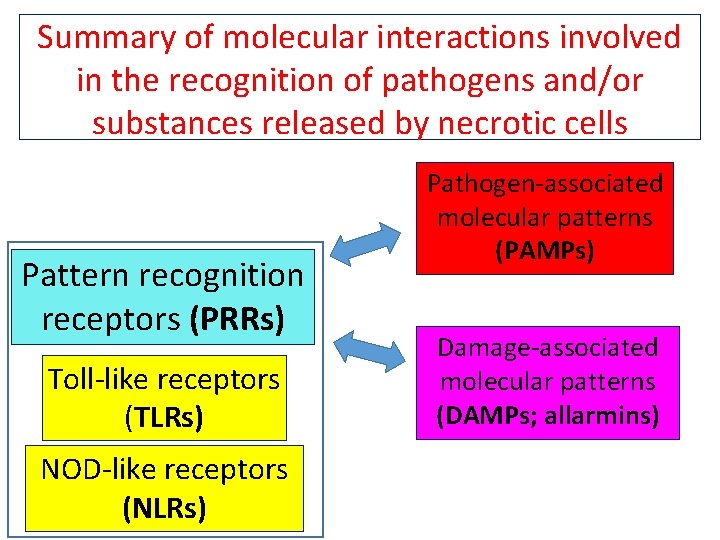
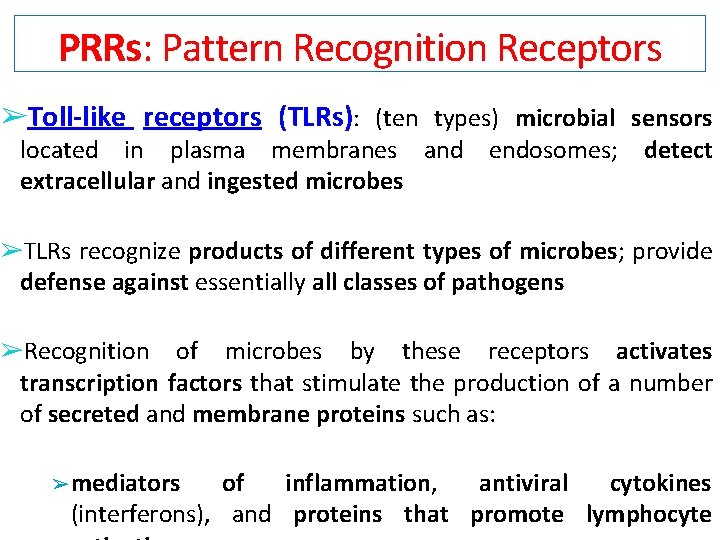
Phase 1: recognition of microbes and necrotic cells ● Microbes and necrotic cells elicit “danger signals” that distinguish them from normal tissues and mobilize the host response ● PRRs recognize structures (i. e. , molecular patterns) common to: ➢ many microbes (Pathogen-Associated Molecular Patterns, PAMPs) ➢ dead cells (Damage-Associated Molecular Patterns, DAMPs)
Phase 1: recognition of microbes and necrotic cells ● Once activated by PRRs – PAMPs interaction, the cells of the innate immune system initiates the inflammatory response by secreting cytokines and chemokines ● This leads to the expression of adhesion and co-stimulatory molecules able to (1) recruit immune cells and (2) stimulate the adaptive immune response ● Because of the need to distinguish between pathogenic and non-pathogenic (or commensal) microbes, it has been proposed that the innate immune system is activated by the recognition of an antigen, but only in presence of danger signals released by cells (DAMPs).
![DamageAssociated Molecular Patterns DAMPs allarmins intracellular proteins such as heatshock proteins HSP Damage-Associated Molecular Patterns ● DAMPs: [allarmins] ● intracellular proteins, such as heat-shock proteins (HSP)](https://slidetodoc.com/presentation_image_h2/8366cdaa04e85ad637c54415e21b2b62/image-25.jpg)
Damage-Associated Molecular Patterns ● DAMPs: [allarmins] ● intracellular proteins, such as heat-shock proteins (HSP) or HMGB 1 (high-mobility group box 1), Ca++ binding proteins ● non-protein DAMPs: ATP, uric acid, DNA, RNA, altered phospholipids ● proteins derived from the extracellular matrix generated upon tissue injury, such as hyaluronan fragments
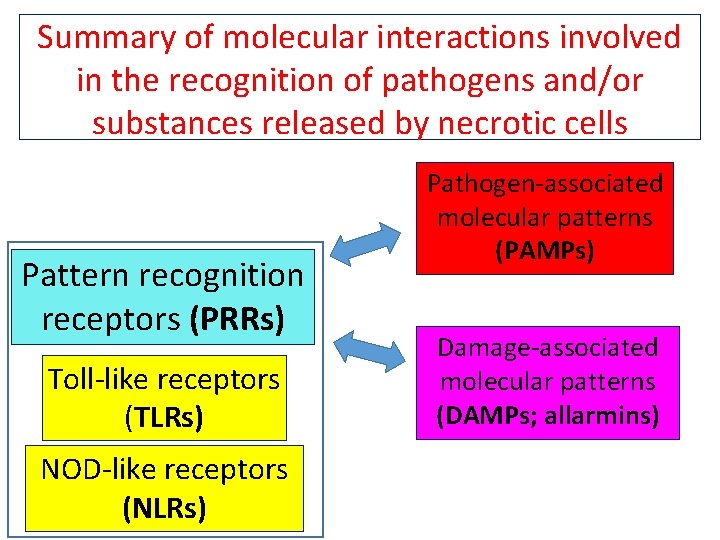
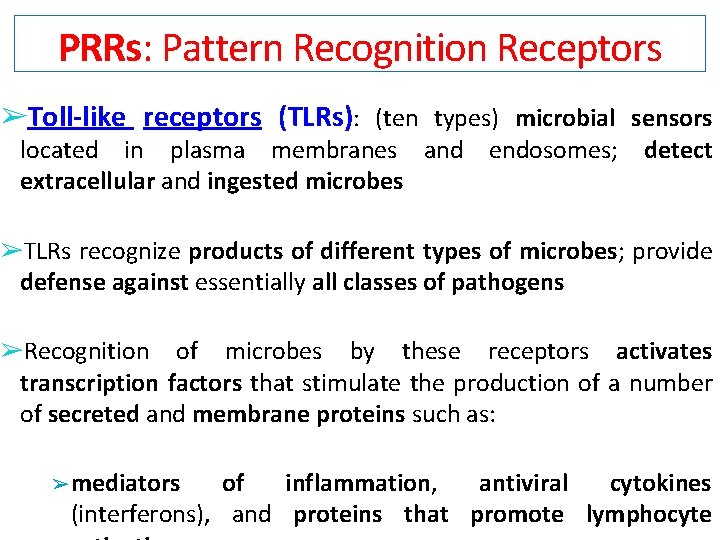
Summary of molecular interactions involved in the recognition of pathogens and/or substances released by necrotic cells Pattern recognition receptors (PRRs) Toll-like receptors (TLRs) NOD-like receptors (NLRs) Pathogen-associated molecular patterns (PAMPs) Damage-associated molecular patterns (DAMPs; allarmins)
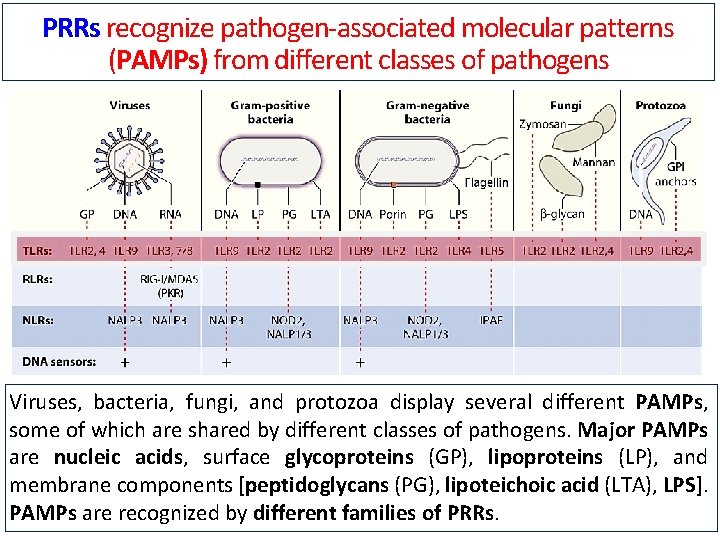
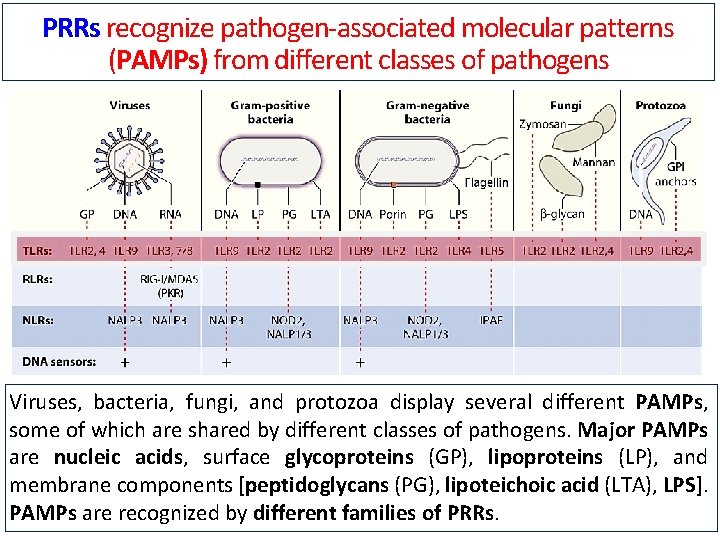
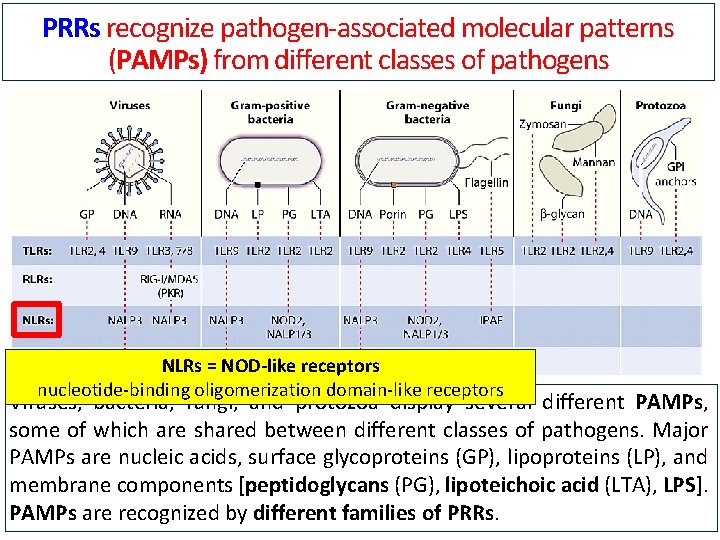
PRRs recognize pathogen-associated molecular patterns (PAMPs) from different classes of pathogens Viruses, bacteria, fungi, and protozoa display several different PAMPs, some of which are shared by different classes of pathogens. Major PAMPs are nucleic acids, surface glycoproteins (GP), lipoproteins (LP), and membrane components [peptidoglycans (PG), lipoteichoic acid (LTA), LPS]. PAMPs are recognized by different families of PRRs.
PRRs: Pattern Recognition Receptors ➢Toll-like receptors (TLRs): (ten types) microbial sensors located in plasma membranes and endosomes; extracellular and ingested microbes detect ➢TLRs recognize products of different types of microbes; provide defense against essentially all classes of pathogens ➢Recognition of microbes by these receptors activates transcription factors that stimulate the production of a number of secreted and membrane proteins such as: ➢ mediators of inflammation, antiviral cytokines (interferons), and proteins that promote lymphocyte
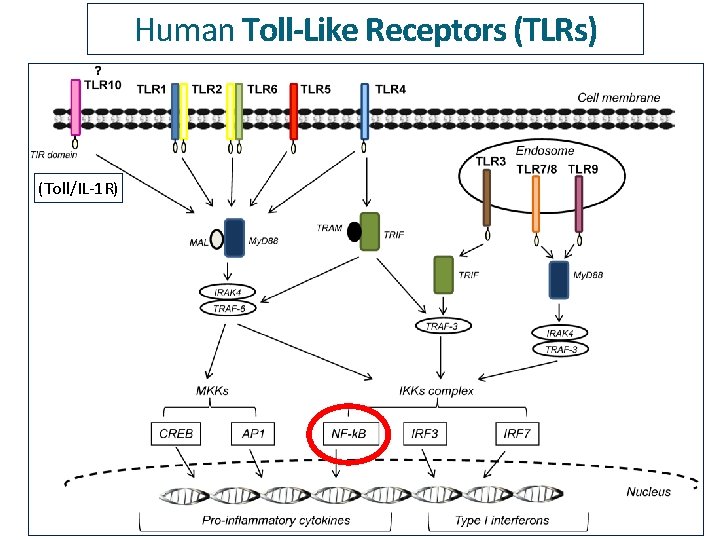
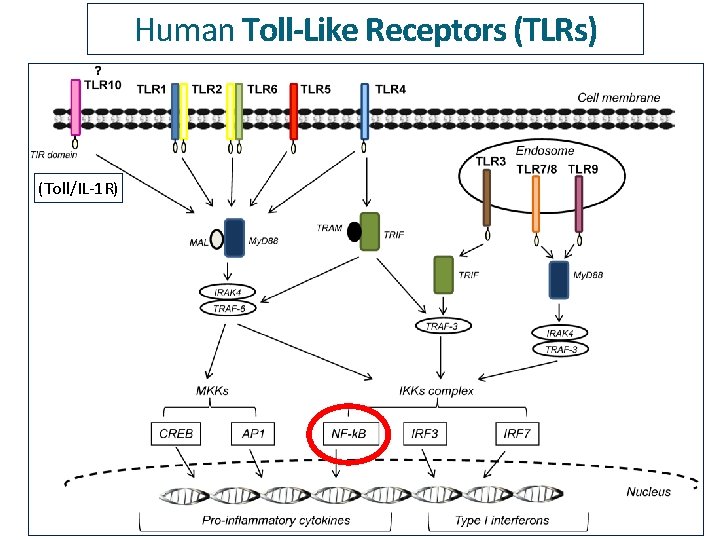
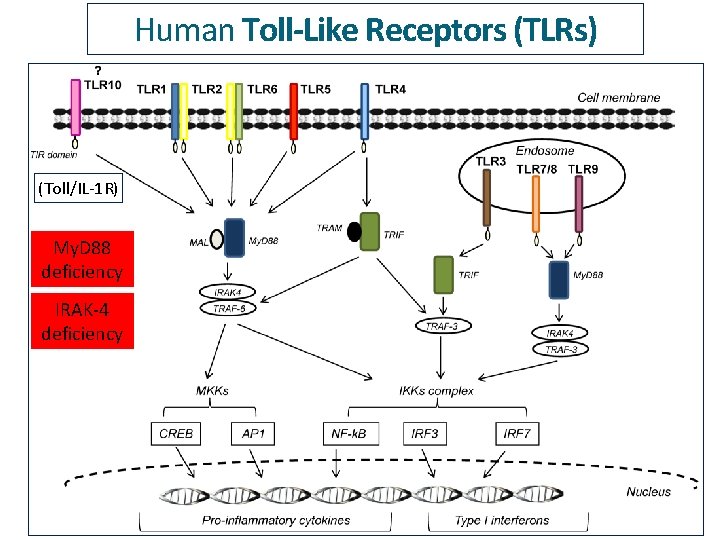
Human Toll-Like Receptors (TLRs) (Toll/IL-1 R)
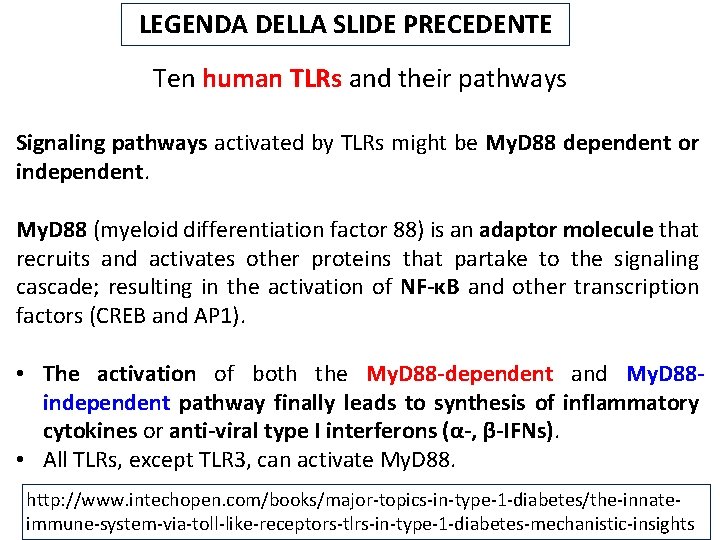
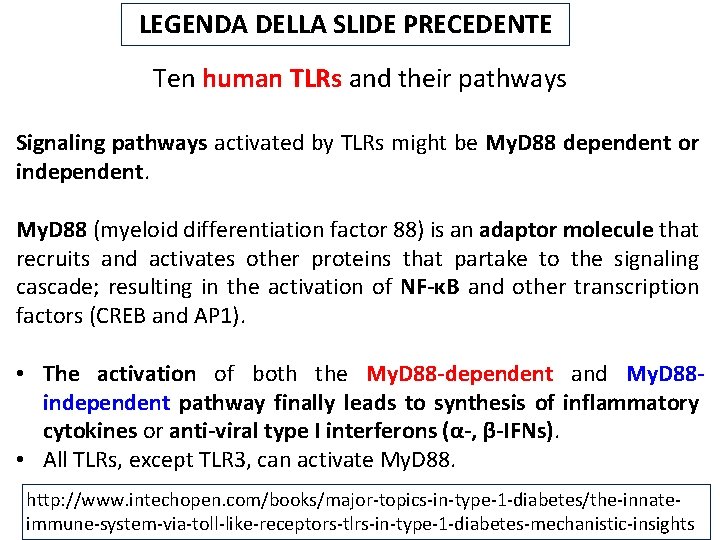
LEGENDA DELLA SLIDE PRECEDENTE Ten human TLRs and their pathways Signaling pathways activated by TLRs might be My. D 88 dependent or independent. My. D 88 (myeloid differentiation factor 88) is an adaptor molecule that recruits and activates other proteins that partake to the signaling cascade; resulting in the activation of NF-κB and other transcription factors (CREB and AP 1). • The activation of both the My. D 88 -dependent and My. D 88 independent pathway finally leads to synthesis of inflammatory cytokines or anti-viral type I interferons (α-, β-IFNs). • All TLRs, except TLR 3, can activate My. D 88. http: //www. intechopen. com/books/major-topics-in-type-1 -diabetes/the-innateimmune-system-via-toll-like-receptors-tlrs-in-type-1 -diabetes-mechanistic-insights
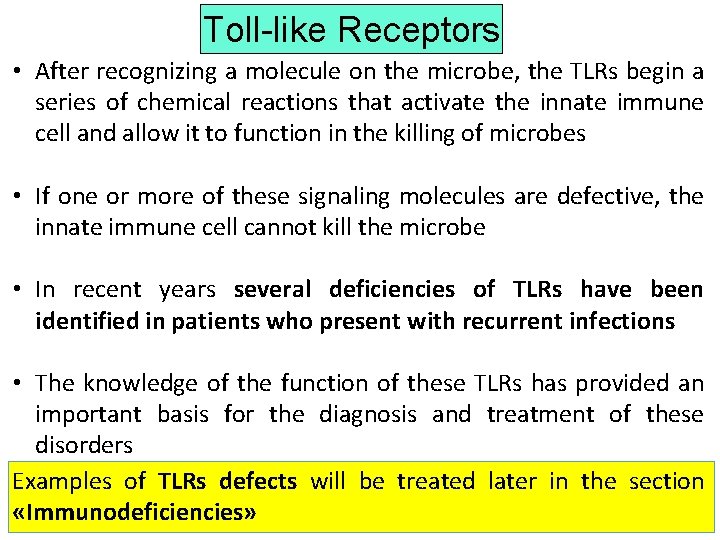
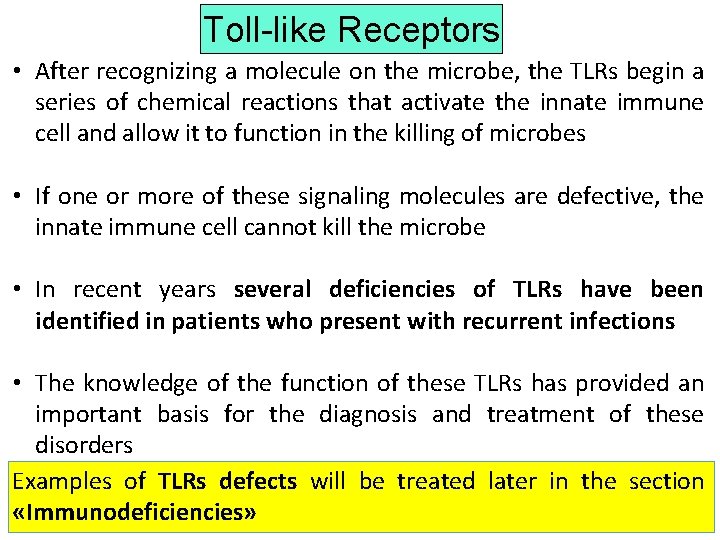
Toll-like Receptors • After recognizing a molecule on the microbe, the TLRs begin a series of chemical reactions that activate the innate immune cell and allow it to function in the killing of microbes • If one or more of these signaling molecules are defective, the innate immune cell cannot kill the microbe • In recent years several deficiencies of TLRs have been identified in patients who present with recurrent infections • The knowledge of the function of these TLRs has provided an important basis for the diagnosis and treatment of these disorders Examples of TLRs defects will be treated later in the section «Immunodeficiencies»
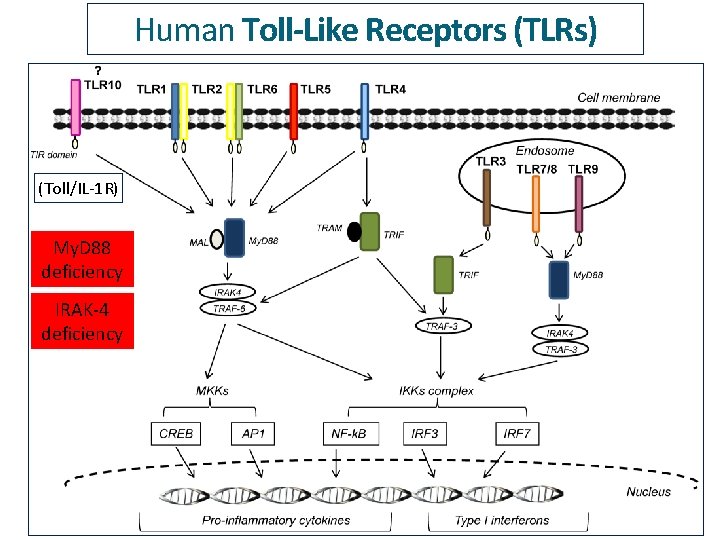
Human Toll-Like Receptors (TLRs) (Toll/IL-1 R) My. D 88 deficiency IRAK-4 deficiency
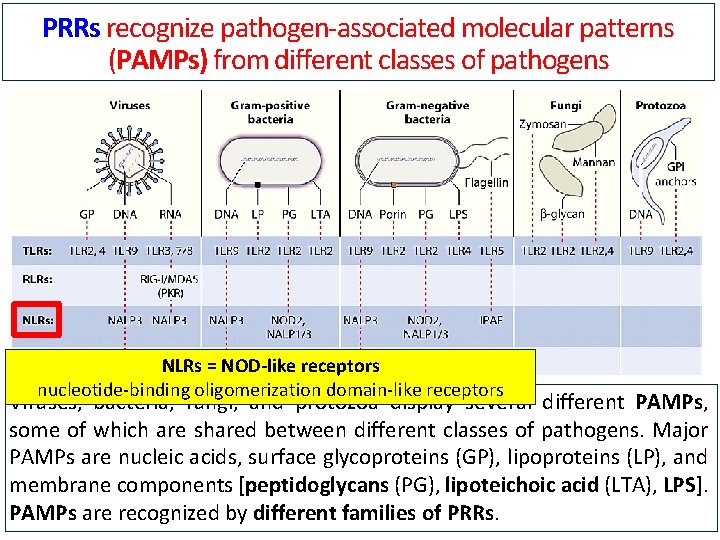
PRRs recognize pathogen-associated molecular patterns (PAMPs) from different classes of pathogens NLRs = NOD-like receptors nucleotide-binding oligomerization domain-like receptors Viruses, bacteria, fungi, and protozoa display several different PAMPs, some of which are shared between different classes of pathogens. Major PAMPs are nucleic acids, surface glycoproteins (GP), lipoproteins (LP), and membrane components [peptidoglycans (PG), lipoteichoic acid (LTA), LPS]. PAMPs are recognized by different families of PRRs.
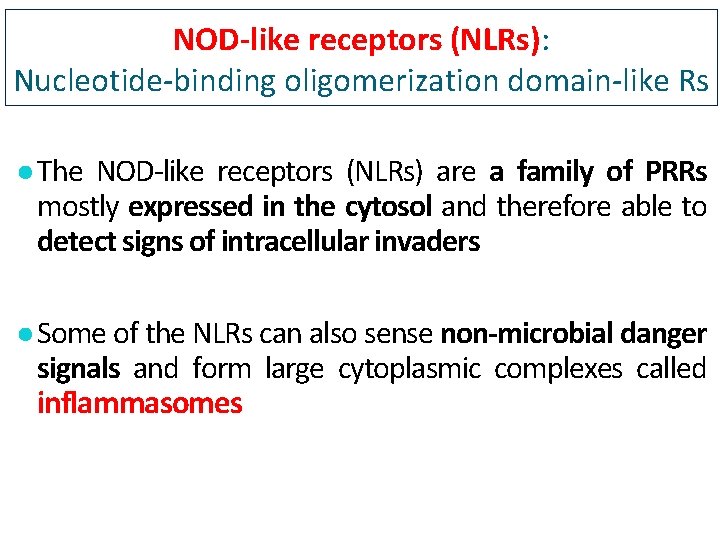
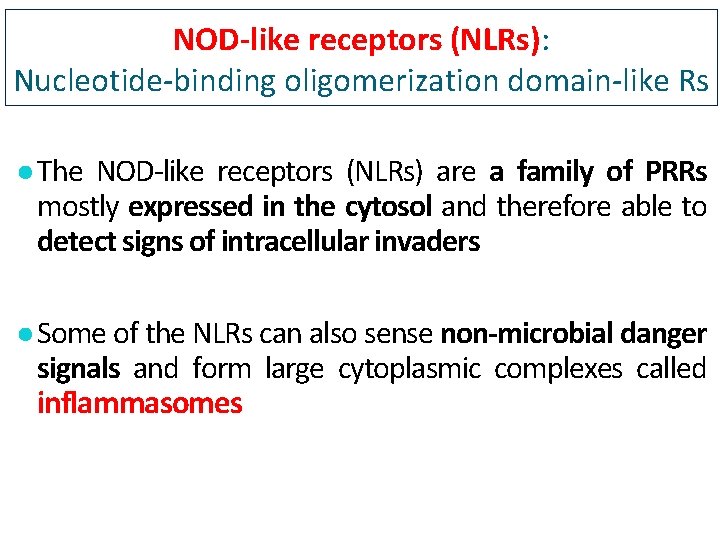
NOD-like receptors (NLRs): Nucleotide-binding oligomerization domain-like Rs ● The NOD-like receptors (NLRs) are a family of PRRs mostly expressed in the cytosol and therefore able to detect signs of intracellular invaders ● Some of the NLRs can also sense non-microbial danger signals and form large cytoplasmic complexes called inflammasomes
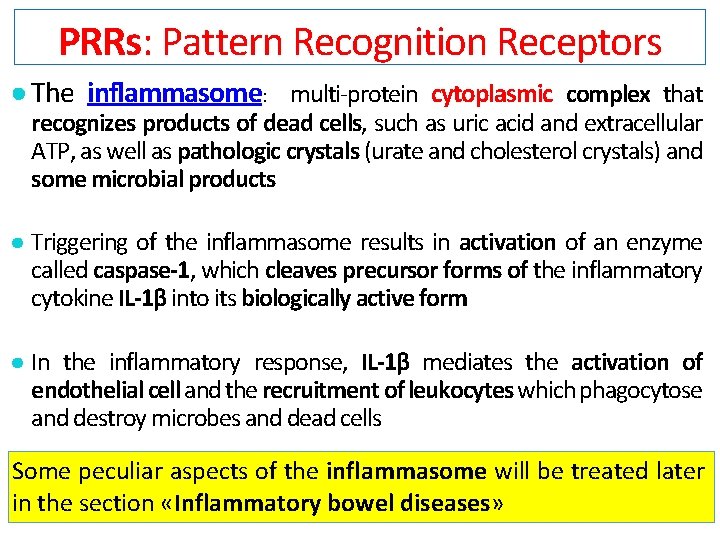
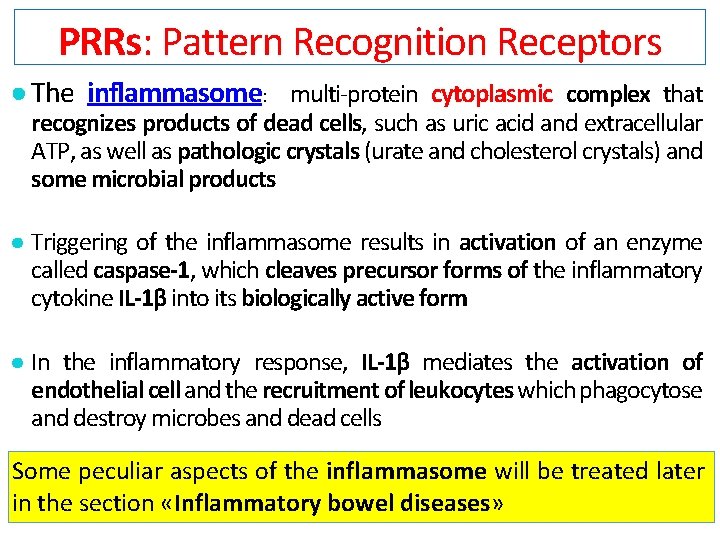
PRRs: Pattern Recognition Receptors ● The inflammasome: multi-protein cytoplasmic complex that recognizes products of dead cells, such as uric acid and extracellular ATP, as well as pathologic crystals (urate and cholesterol crystals) and some microbial products ● Triggering of the inflammasome results in activation of an enzyme called caspase-1, which cleaves precursor forms of the inflammatory cytokine IL-1β into its biologically active form ● In the inflammatory response, IL-1β mediates the activation of endothelial cell and the recruitment of leukocytes which phagocytose and destroy microbes and dead cells Some peculiar aspects of the inflammasome will be treated later in the section «Inflammatory bowel diseases»