KIDNEY DISEASE 1 Nephritic syndrome acute onset characterized
- Slides: 24
KIDNEY DISEASE 1
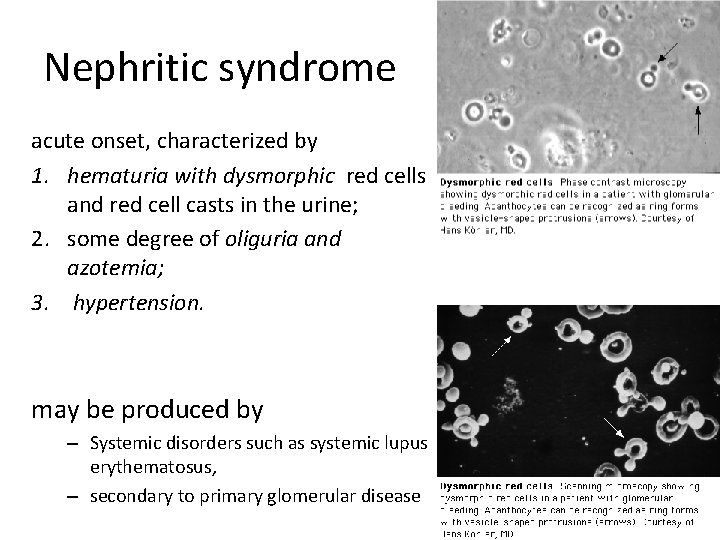
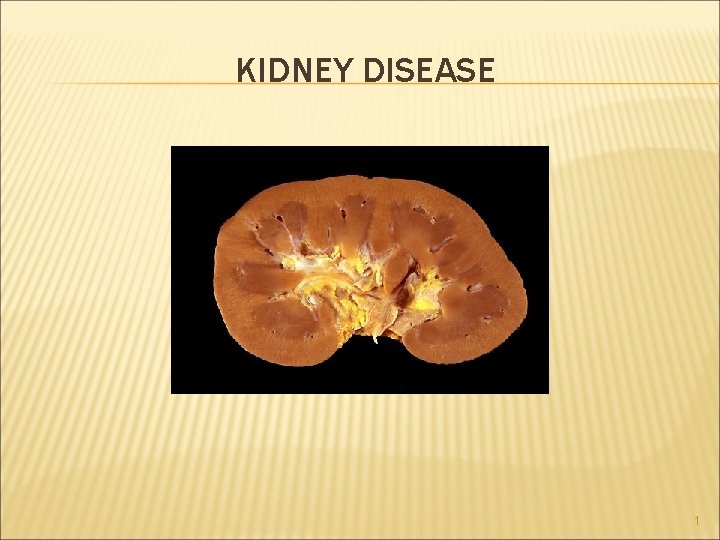
Nephritic syndrome acute onset, characterized by 1. hematuria with dysmorphic red cells and red cell casts in the urine; 2. some degree of oliguria and azotemia; 3. hypertension. may be produced by – Systemic disorders such as systemic lupus erythematosus, – secondary to primary glomerular disease 2
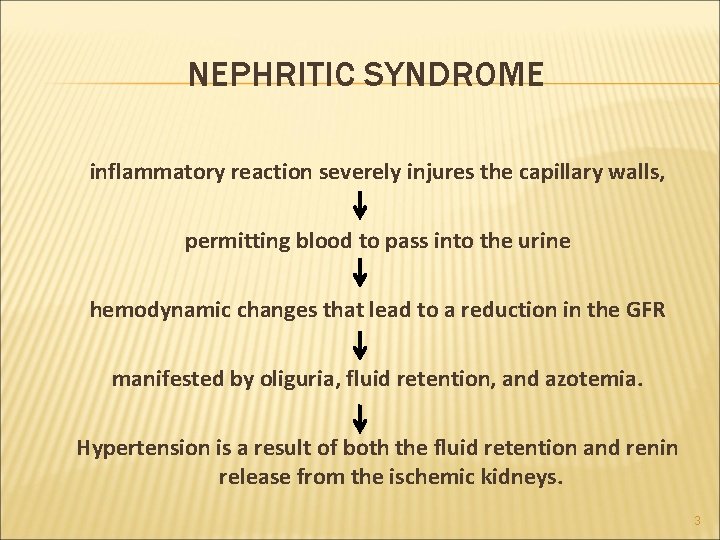
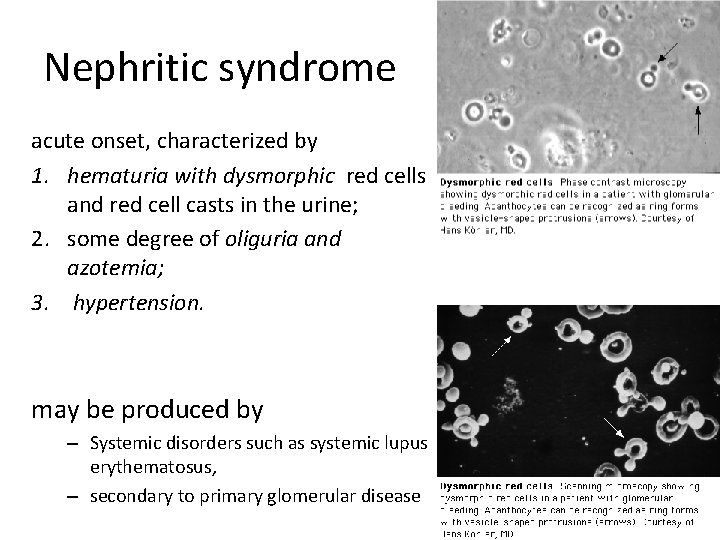
NEPHRITIC SYNDROME inflammatory reaction severely injures the capillary walls, permitting blood to pass into the urine hemodynamic changes that lead to a reduction in the GFR manifested by oliguria, fluid retention, and azotemia. Hypertension is a result of both the fluid retention and renin release from the ischemic kidneys. 3
+ 4 Acute GN They are characterized by n Anatomically by inflammatory alterations in the glomeruli especially neutrophils. n Clinically by the acute nephritic syndrome These lesions are typically caused by immune complexes , The inciting antigen may be n Exogenous: post infectious glomerulonephritis, The most common infections are streptococcal n Endogenous : the nephritis of systemic lupus erythematosus
ACUTE POSTINFECTIOUS (POSTSTREPTOCOCCAL) GLOMERULONEPHRITIS 5
PSGN It usually appears 1 to 4 weeks after a streptococcal infection of the pharynx or skin (impetigo). In children 6 to 10 years of age, but adults of any age can be affected. Etiology and Pathogenesis. Only certain "nephritogenic" strains of β-hemolytic streptococci evoke glomerular disease. 6
PATHOGENESIS • an immune complex disease caused by complement activation by the classical pathway. • Specific antigens implicated in pathogenesis include streptococcal exotoxin B (Spe B) and streptococcal GAPDH. Both activate the alternative complement pathway and have affinity for glomerular proteins and plasmin. • It is not clear if immune complexes are formed mainly in the circulation or in situ ( by binding of antibodies to bacterial antigens "planted“ in the GBM). (glyceraldehyde-3 -phosphate dehydrogenase[GAPDH]) 7
PSGN is an immunologically mediated disease Elevated titers of antibodies against one or more streptococcal antigens Activation of the complement system and consumption of its components. Serum complement levels are low 8
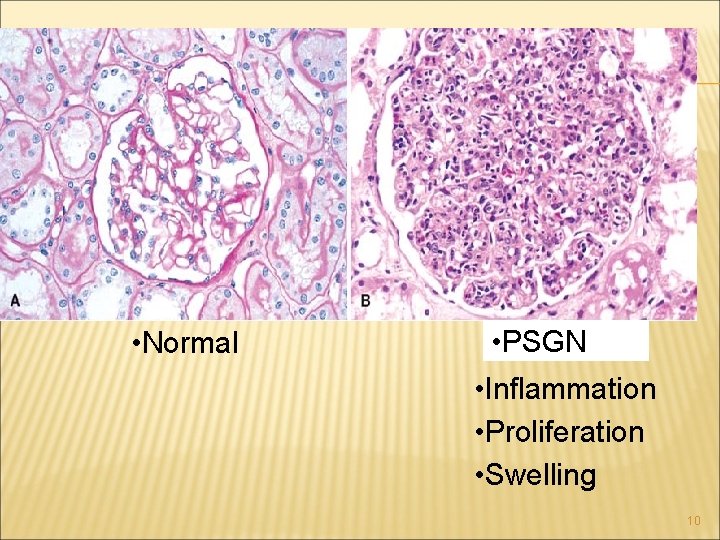
In light microscopy of PSGN the most characteristic change in postinfectious GN is increased cellularity of the glomerular tufts that affects nearly all glomeruli-hence the term diffuse. The increased cellularity is caused both by proliferation and swelling of endothelial and mesangial cells and by infiltrating neutrophils and monocytes. Sometimes there is necrosis of the capillary walls 9
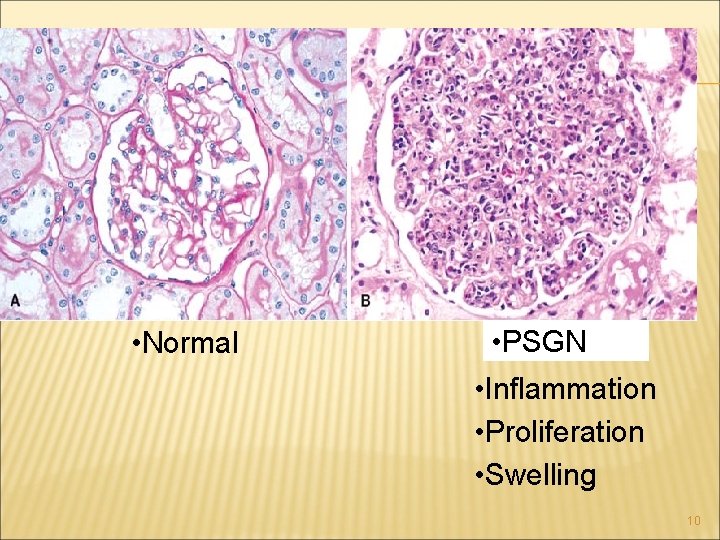
• Normal • PSGN • Inflammation • Proliferation • Swelling 10
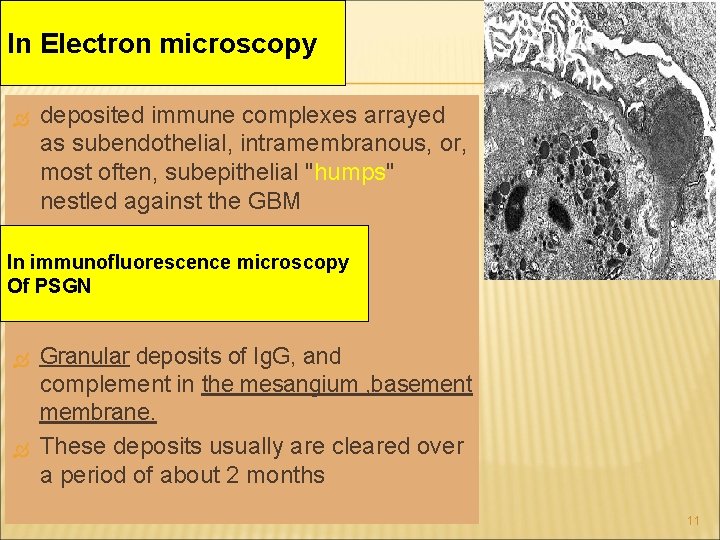
In Electron microscopy deposited immune complexes arrayed as subendothelial, intramembranous, or, most often, subepithelial "humps" nestled against the GBM In immunofluorescence microscopy Of PSGN Granular deposits of Ig. G, and complement in the mesangium , basement membrane. These deposits usually are cleared over a period of about 2 months 11
CLINICAL COURSE OF PSGN In adults 15% to 50% of affected persons develop end -stage renal disease In children the prevalence of chronicity after sporadic cases of acute postinfectious GN is much lower. 12
Nonstreptococcal Acute Glomerulonephritis (Postinfectious Glomerulonephritis) 13
NONSTREPTOCOCCAL ACUTE GLOMERULONEPHRITIS • Bacterial infections : staphylococcal endocarditis Pneumococcal pneumonia , meningococcemia • Viral disease: hepatitis B, hepatitis C, mumps, chickenpox, varicella, infectious mononucleosis • Parasitic infections (malaria, toxoplasmosis) • In this setting, granular immunofluorescent deposits and subepithelial humps characteristic of immune complex nephritis are present. 14
Ig. A NEPHROPATHY (BERGER DISEASE) the most common cause of the nephritic syndrome worldwide probably the most common type of glomerulonephritis revealed by renal biopsy worldwide one of the most common causes of recurrent microscopic or gross hematuria The hallmark of the disease is the deposition of 15 Ig. A in the mesangium in immunofluorescence microscopy.
Ig. A NEPHROPATHY (BERGER DISEASE) usually affects children and young adults 1 or 2 days after a nonspecific upper respiratory tract infection gross hematuria happenes. Typically, the hematuria lasts several days and then subsides, only to recur every few months. It may be associated with local pain. 16
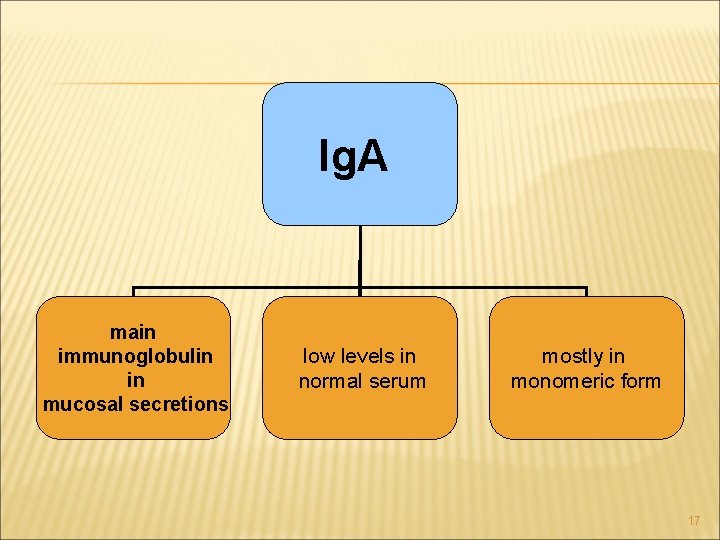
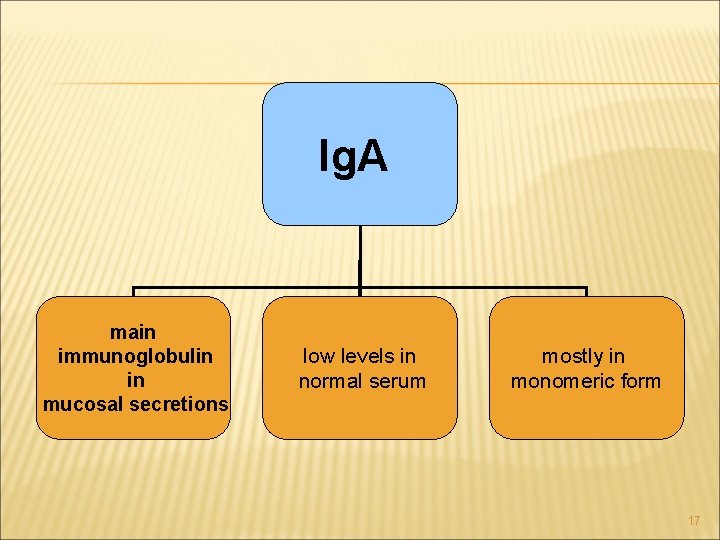
Ig. A main immunoglobulin in mucosal secretions low levels in normal serum mostly in monomeric form 17
18 IGA nephropathy primary secondary
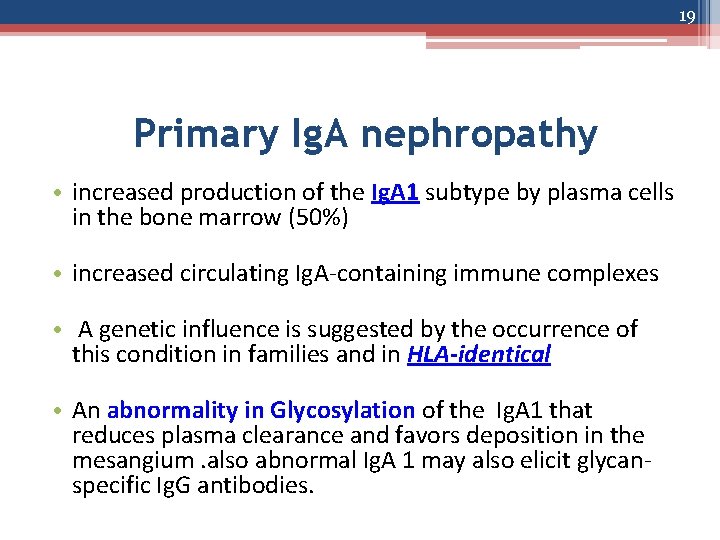
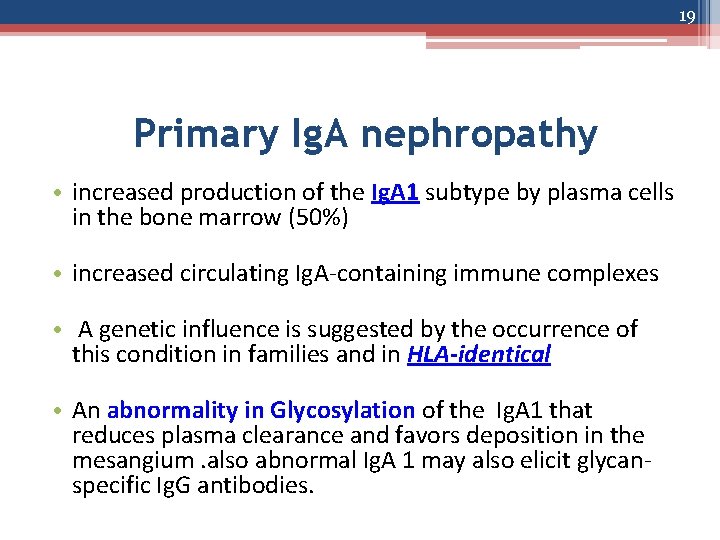
19 Primary Ig. A nephropathy • increased production of the Ig. A 1 subtype by plasma cells in the bone marrow (50%) • increased circulating Ig. A-containing immune complexes • A genetic influence is suggested by the occurrence of this condition in families and in HLA-identical • An abnormality in Glycosylation of the Ig. A 1 that reduces plasma clearance and favors deposition in the mesangium. also abnormal Ig. A 1 may also elicit glycanspecific Ig. G antibodies.
Secondary Ig. A nephropathy in celiac disease, ( in whom intestinal mucosal defects) in liver disease, (with defective hepatobiliary clearance of Ig. A complexes) 20
Ig. A nephropathy to be a localized variant of Henoch- Schonlein purpura In contrast with Ig. A nephropathy, which is purely a renal disorder, Henoch-Schonlein purpura is a systemic syndrome involving the *skin (purpuric rash), *Gastrointestinal tract (abdominal pain), * joints (arthritis), * and kidneys (Ig. A deposition in the mesangium. ) 21
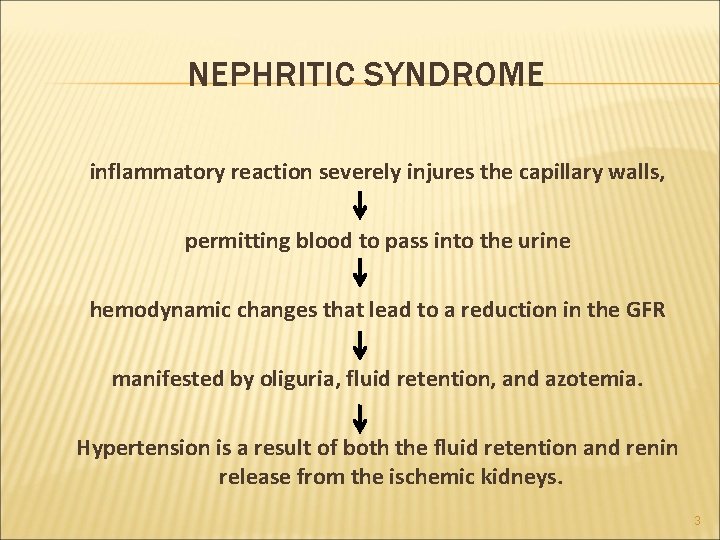
On histologic examination, the lesions vary considerably. The glomeruli may be normal Mesangial widening and segmental inflammation confined to some glomeruli (focal proliferative GN) diffuse mesangial proliferation (mesangioproliferative GN) or (rarely) overt crescentic GN. Electron microscopy confirms the presence of electron-dense deposits in the mesangium 22
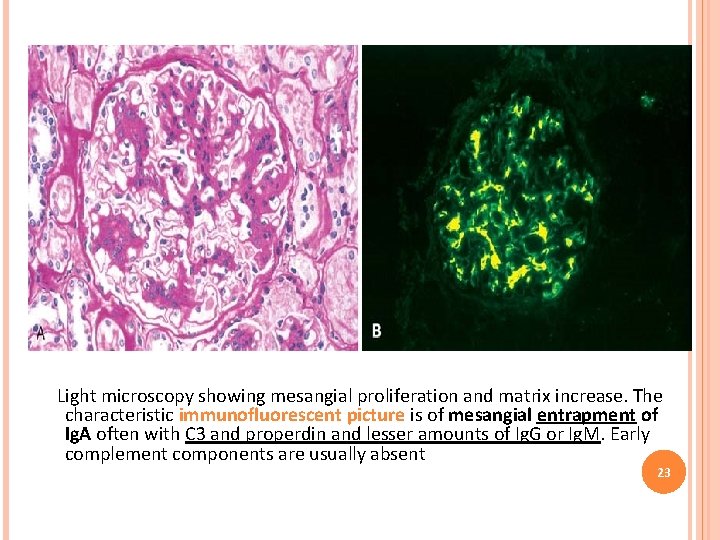
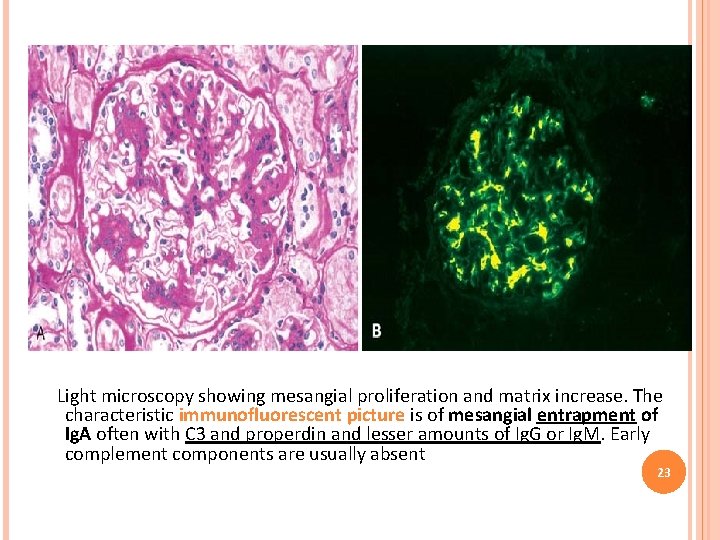
Light microscopy showing mesangial proliferation and matrix increase. The characteristic immunofluorescent picture is of mesangial entrapment of Ig. A often with C 3 and properdin and lesser amounts of Ig. G or Ig. M. Early complement components are usually absent 23
Renal biopsy findings may help identify those with worse prognosis, as indicated by diffuse mesangial proliferation, segmental sclerosis, endocapillary proliferation, tubulointerstitial fibrosis 24
 Dr kriti mohan
Dr kriti mohan Nephritic syndrome triad
Nephritic syndrome triad Skt aki
Skt aki Natremia
Natremia Nemo dialysis
Nemo dialysis Albumin kidney disease
Albumin kidney disease Nih stroke scale
Nih stroke scale Albumin kidney disease
Albumin kidney disease Sighns of kidney disease
Sighns of kidney disease Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Nephrology near atwater
Nephrology near atwater Diabetes mellitus is a metabolic disease characterized by
Diabetes mellitus is a metabolic disease characterized by An acute highly contagious viral disease
An acute highly contagious viral disease Acute radiation syndrome
Acute radiation syndrome Acute coronary syndrome
Acute coronary syndrome Acute aortic syndrome
Acute aortic syndrome Communicable disease and non communicable disease
Communicable disease and non communicable disease Nursing management of adrenal tumor
Nursing management of adrenal tumor Maximal onset principle example
Maximal onset principle example Nph onset and peak
Nph onset and peak Hindi transliteration
Hindi transliteration Onset offset trial
Onset offset trial Maximal onset principle example
Maximal onset principle example Assimilation in phonetics
Assimilation in phonetics Early onset scoliosis classification
Early onset scoliosis classification