Ischemia Guided Strategy in NSTEACS When to go


- Slides: 81
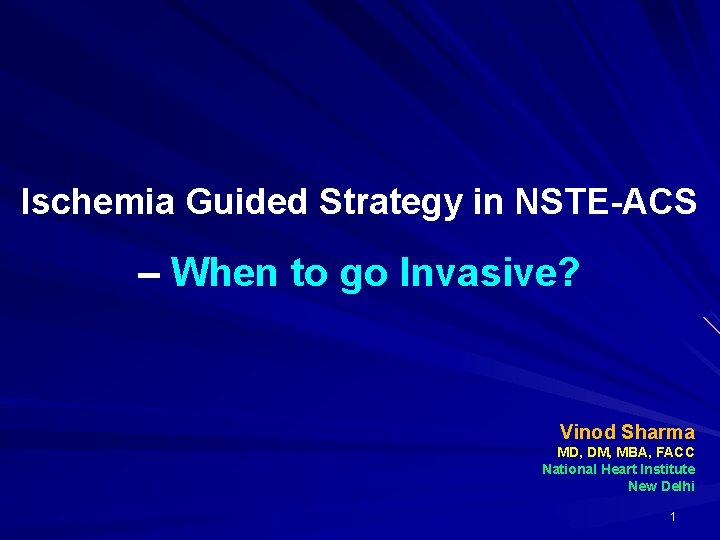
Ischemia Guided Strategy in NSTE-ACS – When to go Invasive? Vinod Sharma MD, DM, MBA, FACC National Heart Institute New Delhi 1
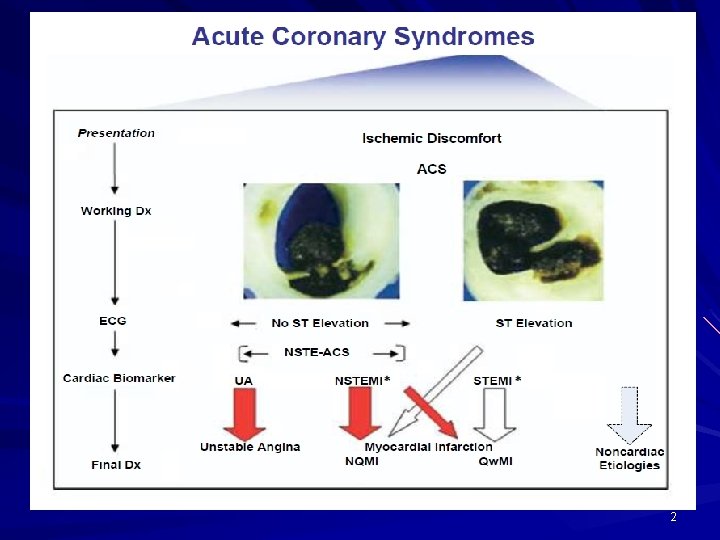
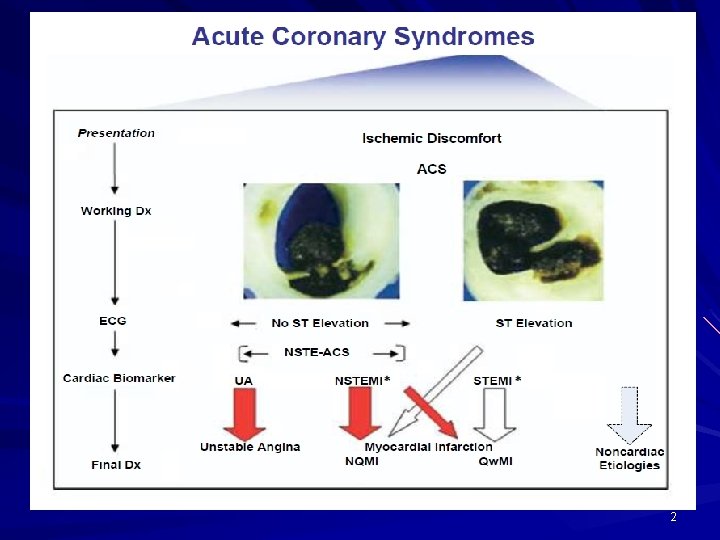
2
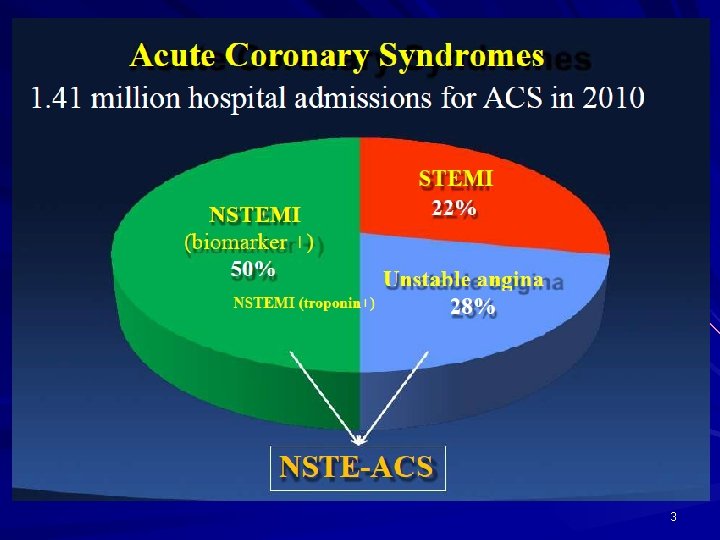
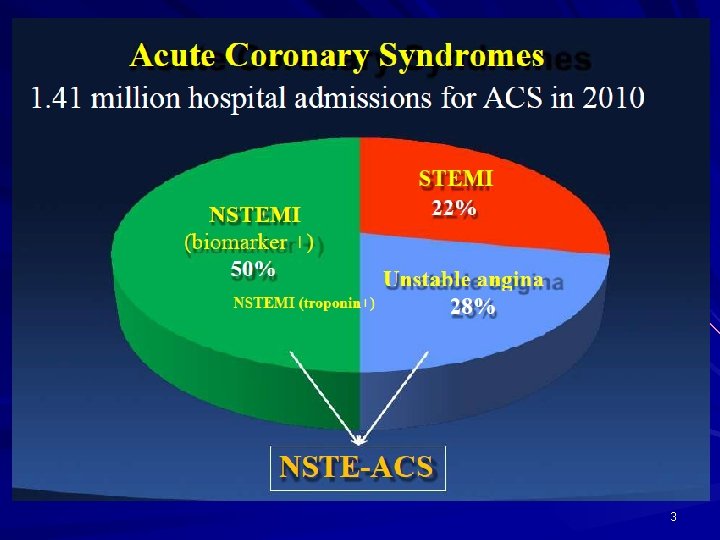
3
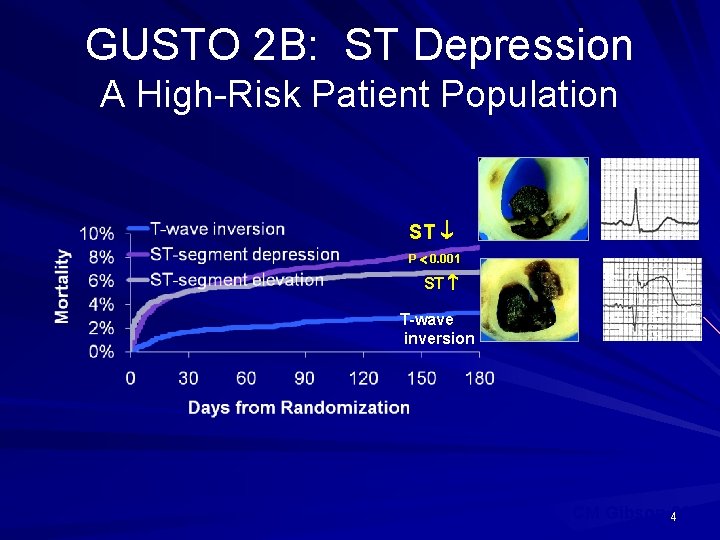
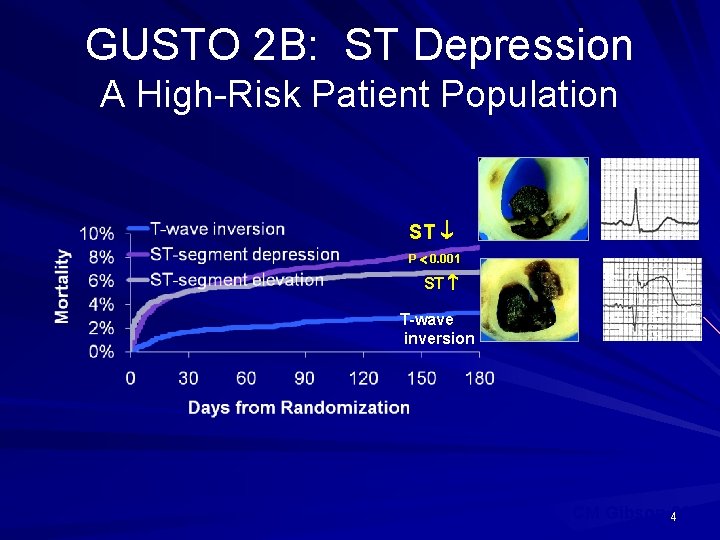
GUSTO 2 B: ST Depression A High-Risk Patient Population ST P 0. 001 ST T-wave inversion CM Gibson 42002
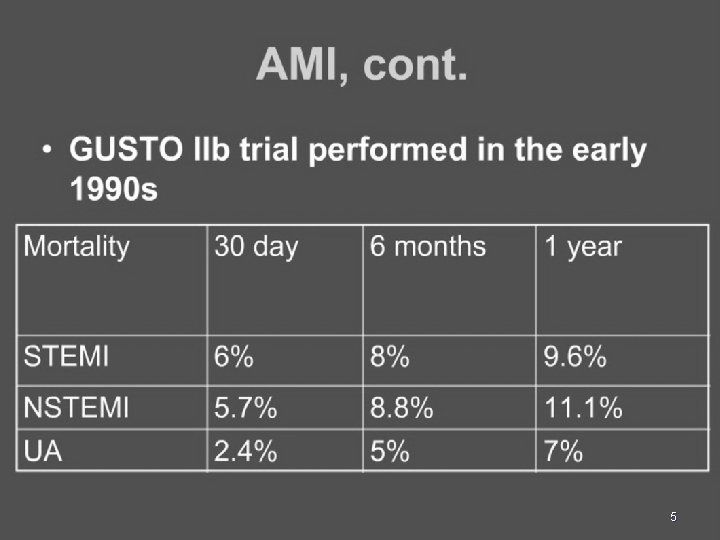
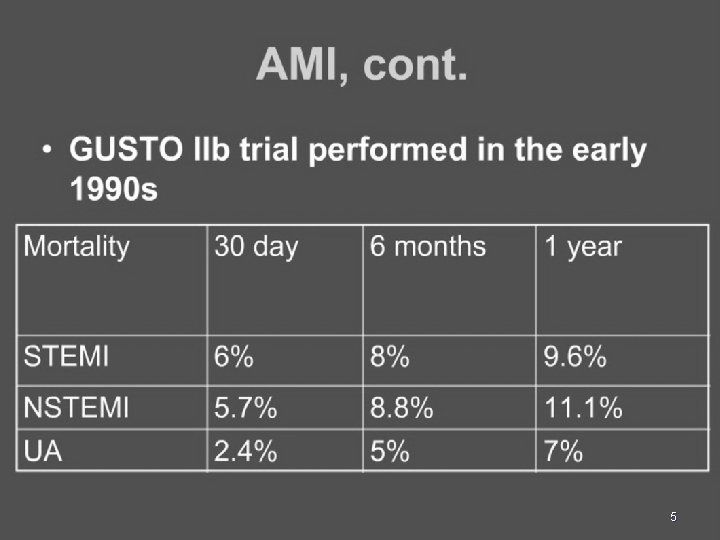
5
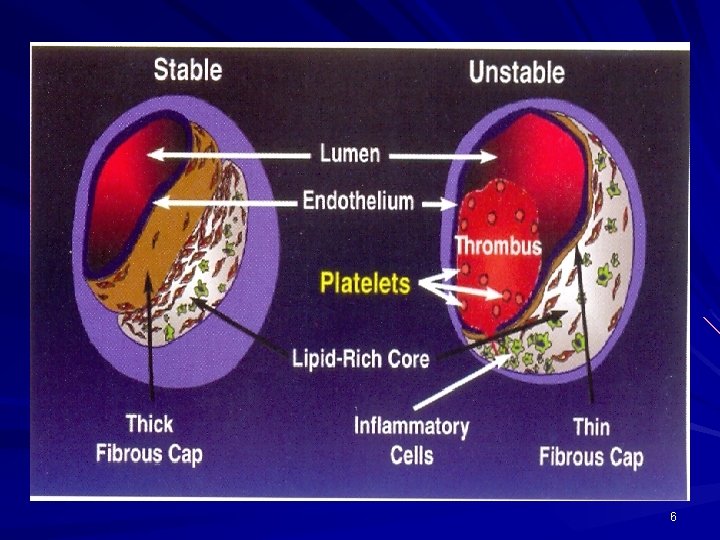
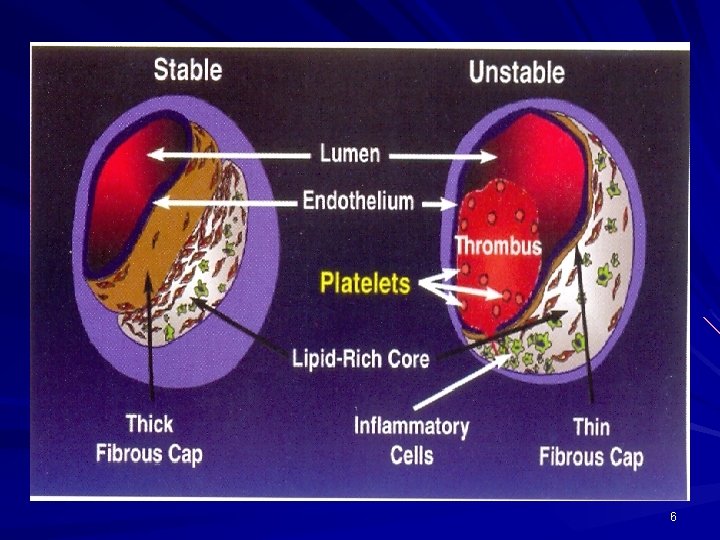
6
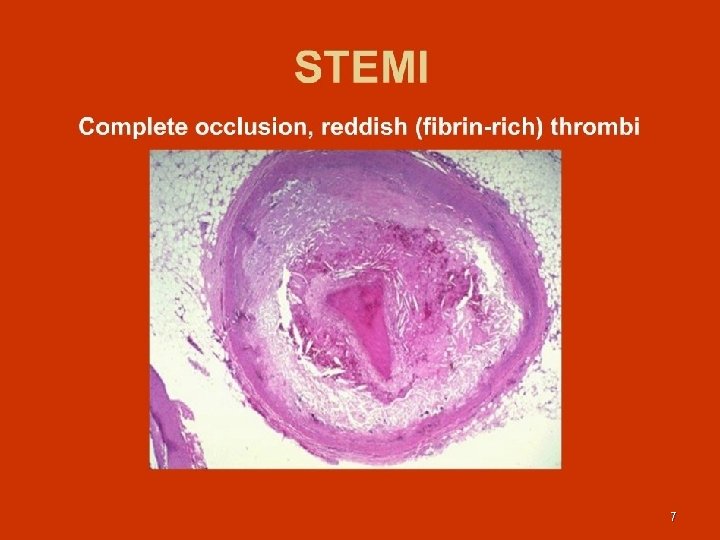
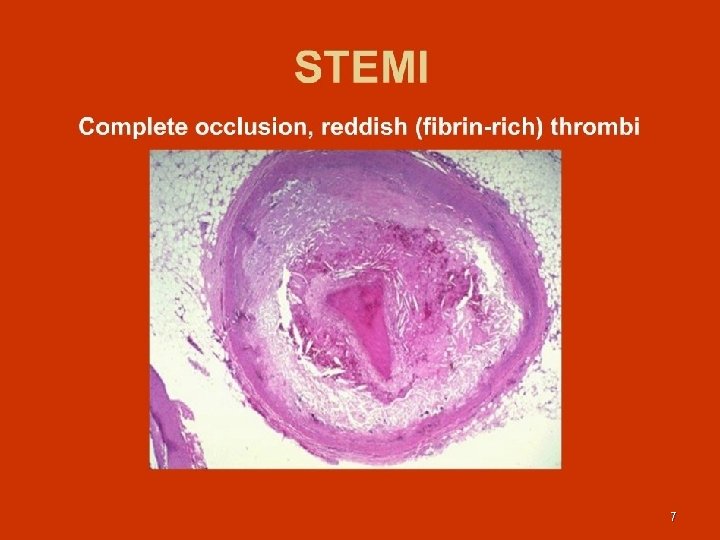
7
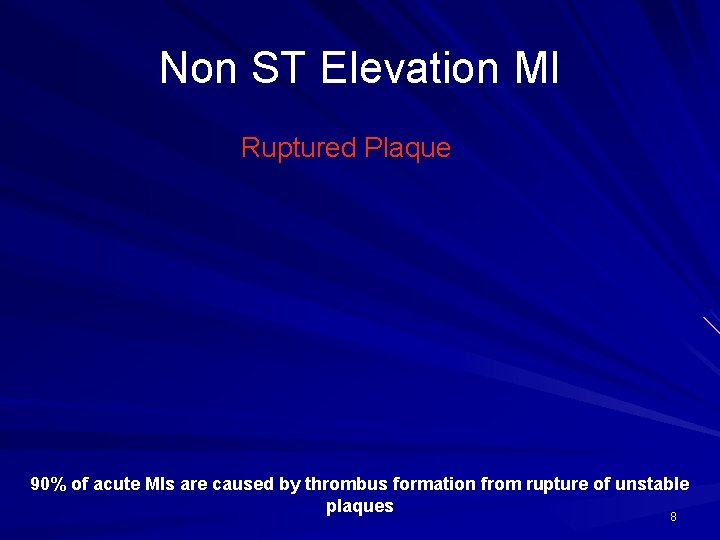
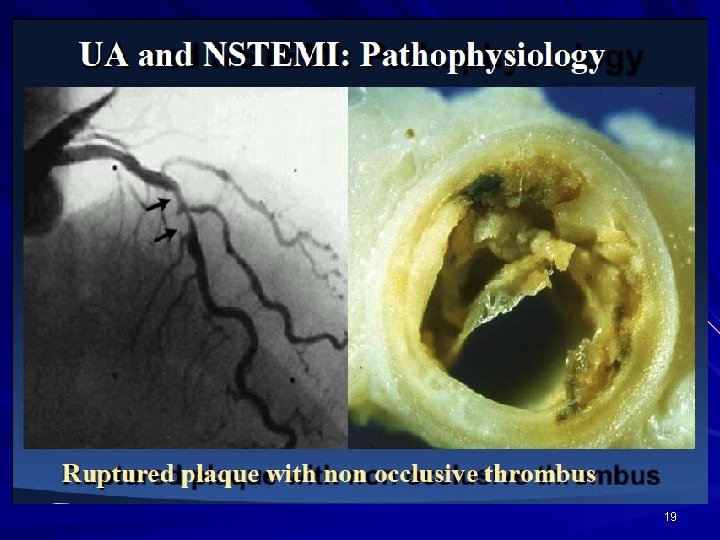
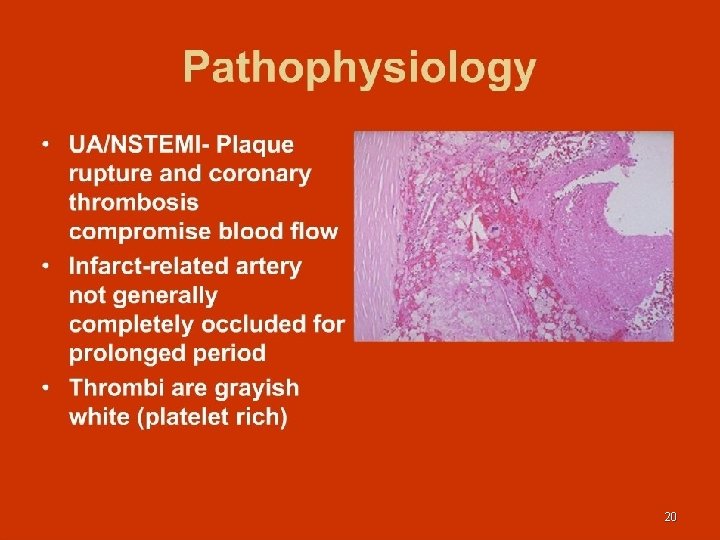
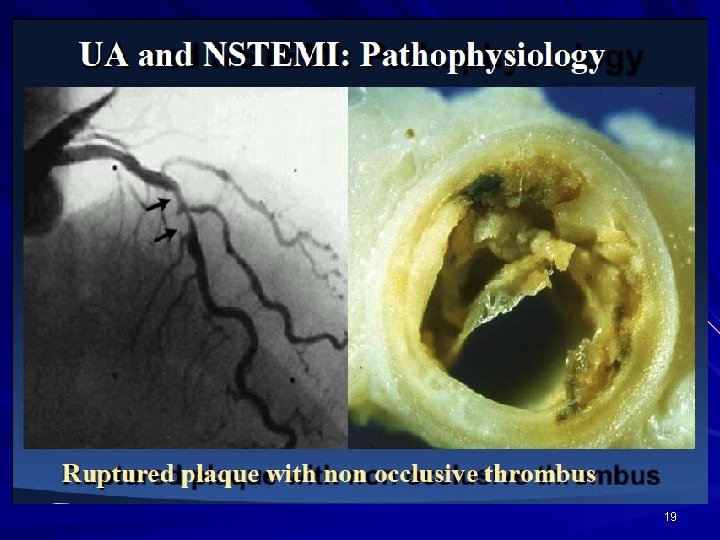
Non ST Elevation MI Ruptured Plaque 90% of acute MIs are caused by thrombus formation from rupture of unstable plaques 8
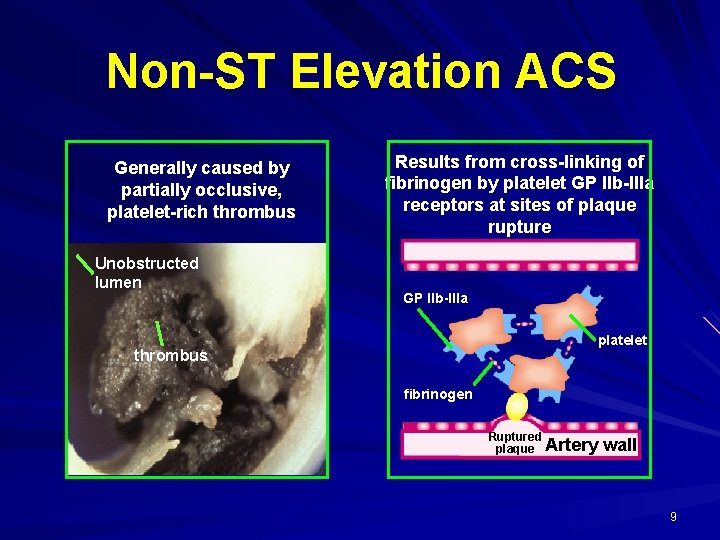
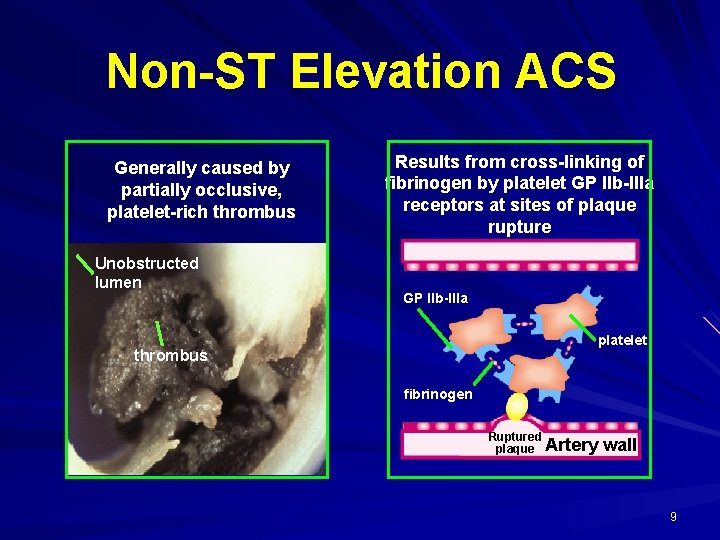
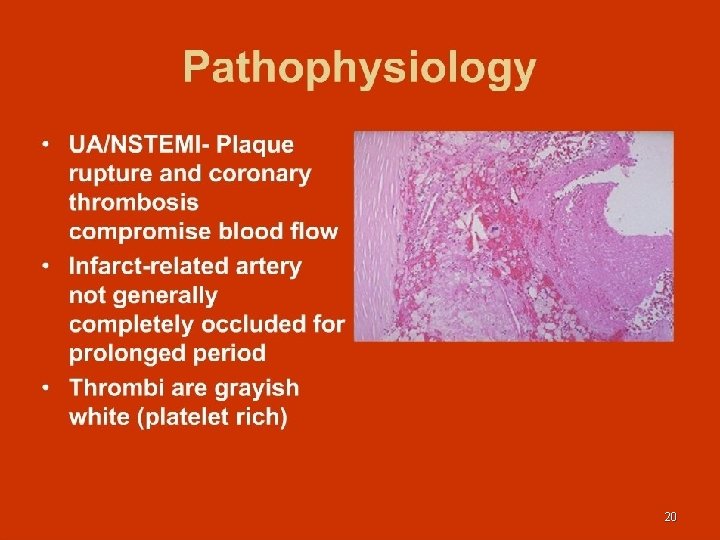
Non-ST Elevation ACS Generally caused by partially occlusive, platelet-rich thrombus Unobstructed lumen Results from cross-linking of fibrinogen by platelet GP IIb-IIIa receptors at sites of plaque rupture GP IIb-IIIa platelet thrombus fibrinogen Ruptured plaque Artery wall 9
Red Vs White Thrombus …… 10
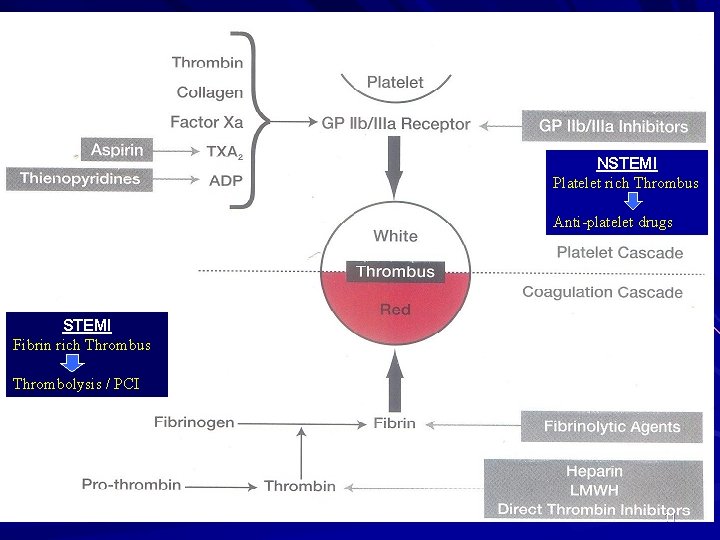
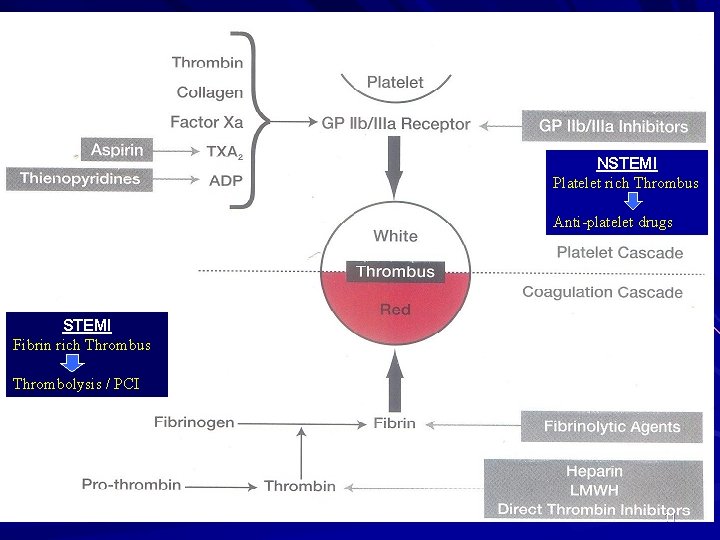
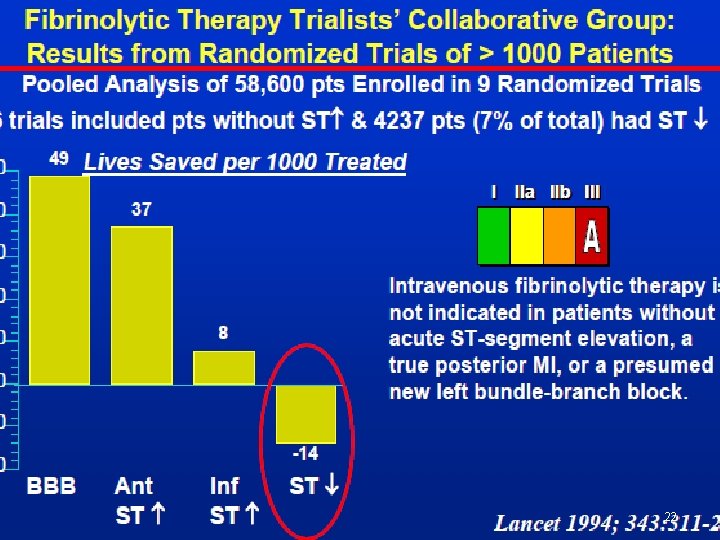
NSTEMI Platelet rich Thrombus Anti-platelet drugs STEMI Fibrin rich Thrombus Thrombolysis / PCI 11
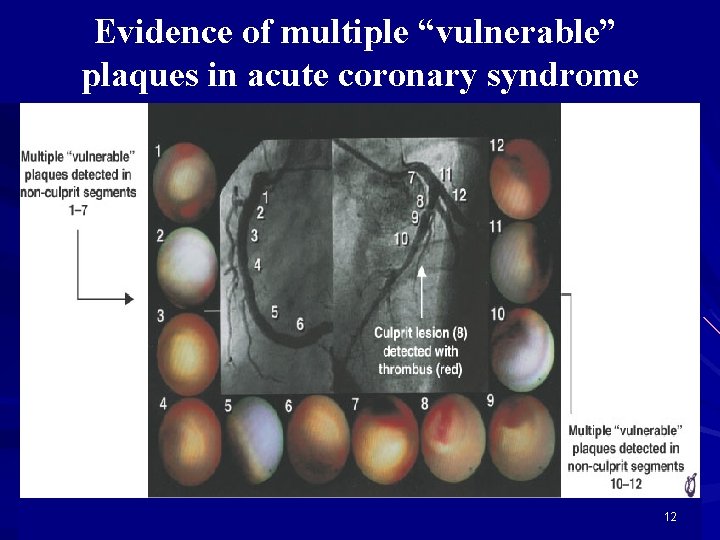
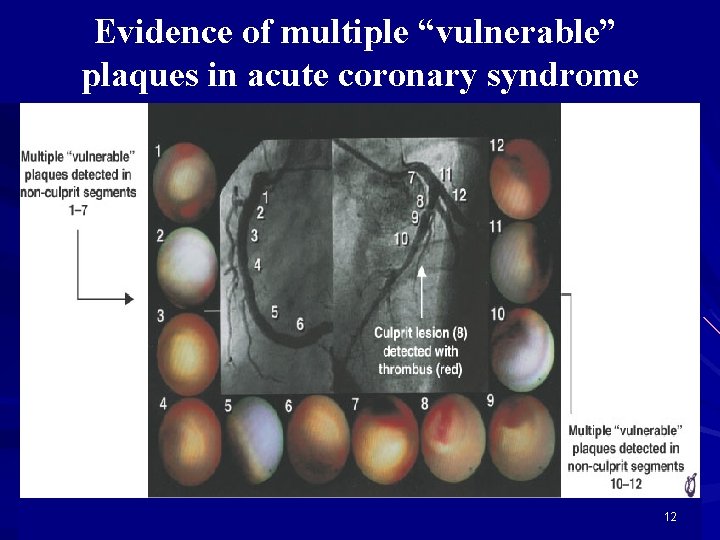
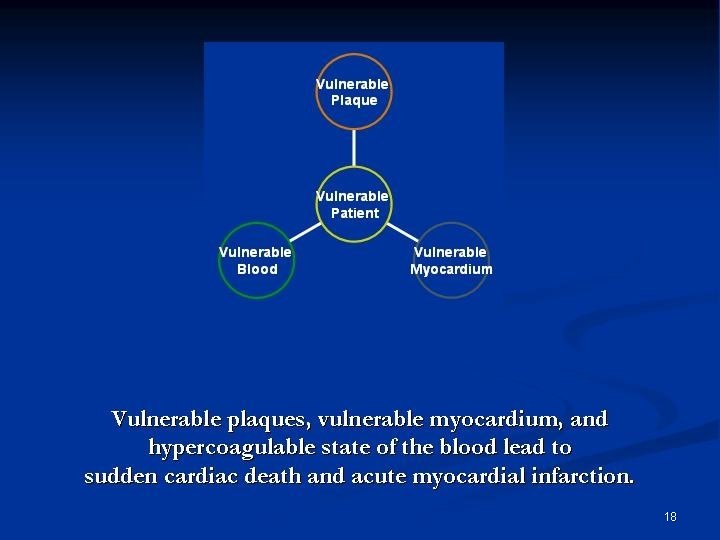
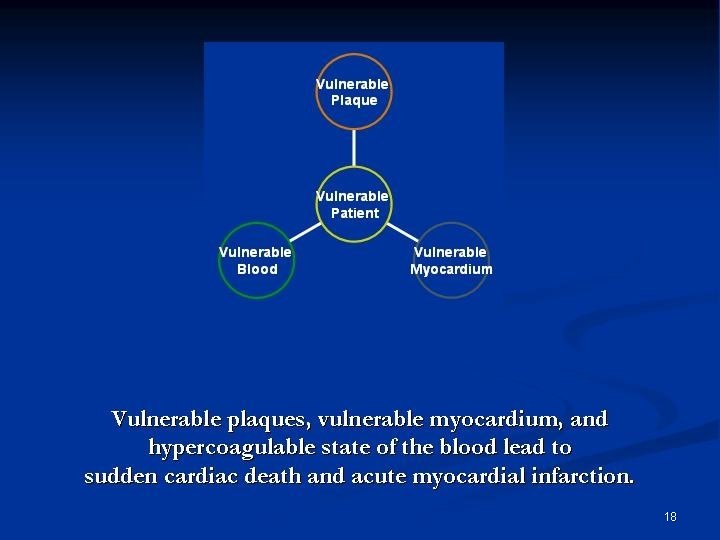
Evidence of multiple “vulnerable” plaques in acute coronary syndrome 12
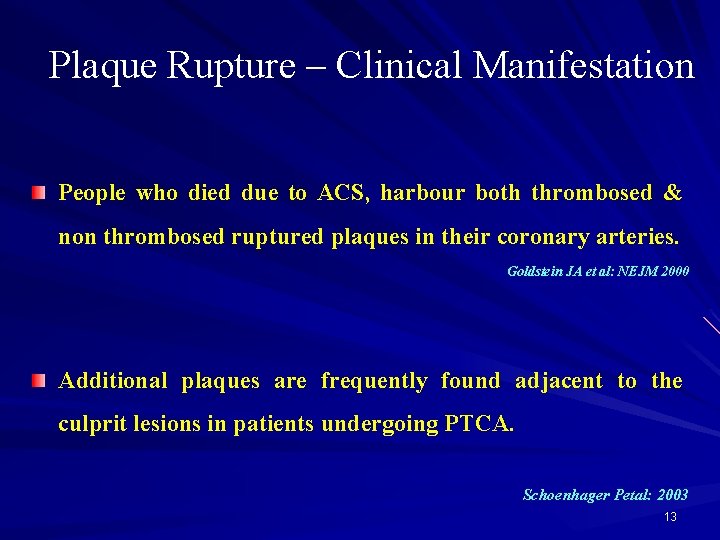
Plaque Rupture – Clinical Manifestation People who died due to ACS, harbour both thrombosed & non thrombosed ruptured plaques in their coronary arteries. Goldstein JA et al: NEJM 2000 Additional plaques are frequently found adjacent to the culprit lesions in patients undergoing PTCA. Schoenhager Petal: 2003 13
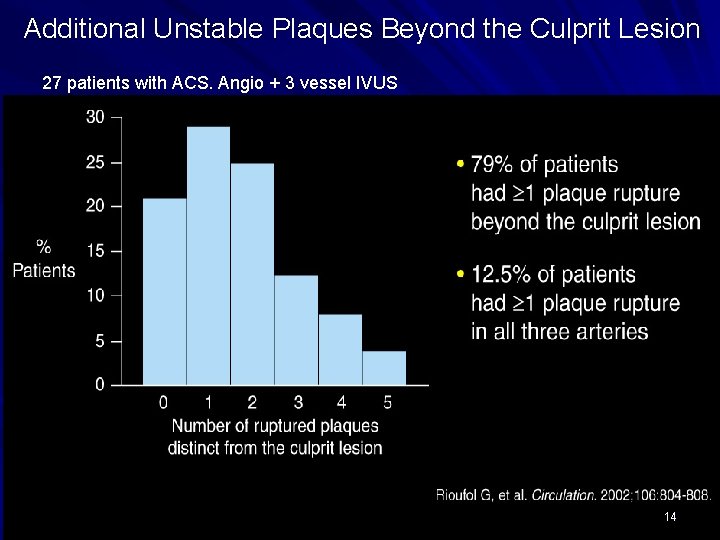
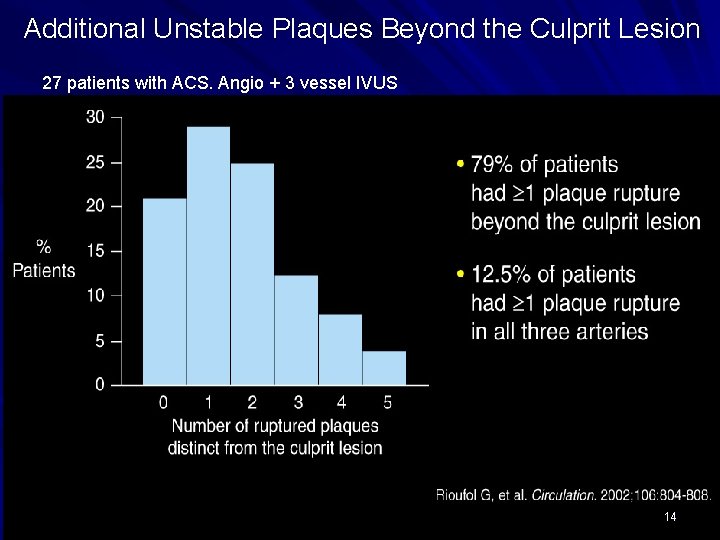
Additional Unstable Plaques Beyond the Culprit Lesion 27 patients with ACS. Angio + 3 vessel IVUS 14
Acute Coronary Syndrome a “PANCORONITIS” ? Local manifestation of systemic disease 15
Culprit is vulnerability …… 16
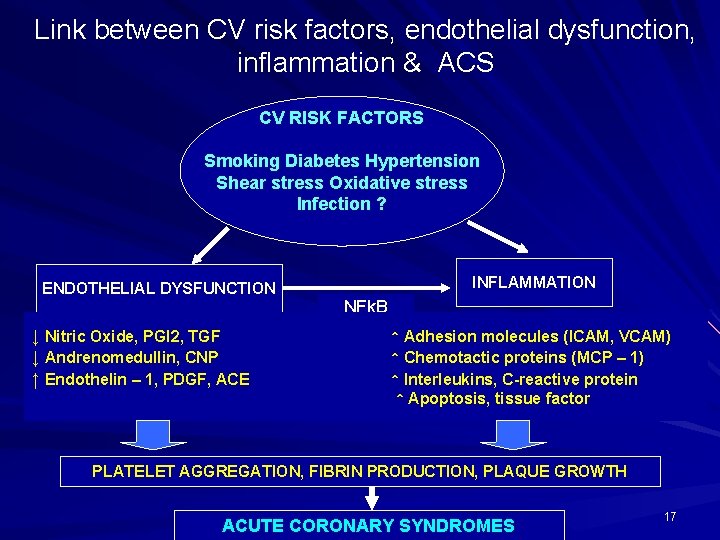
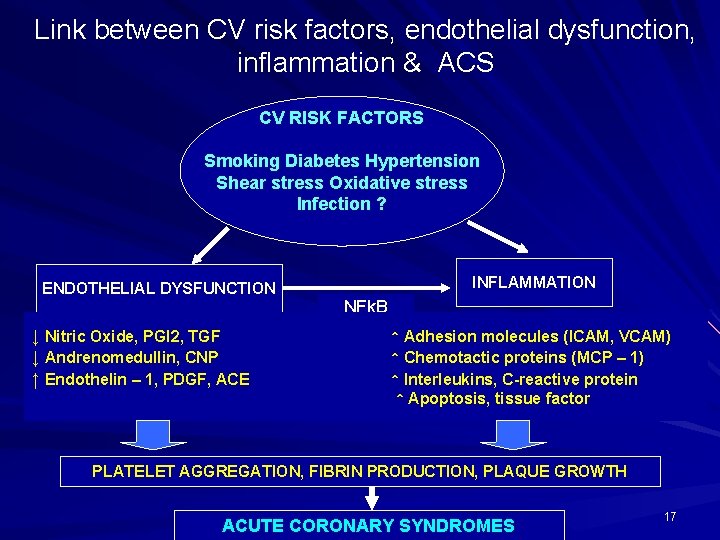
Link between CV risk factors, endothelial dysfunction, inflammation & ACS CV RISK FACTORS Smoking Diabetes Hypertension Shear stress Oxidative stress Infection ? ENDOTHELIAL DYSFUNCTION ↓ Nitric Oxide, PGI 2, TGF ↓ Andrenomedullin, CNP ↑ Endothelin – 1, PDGF, ACE INFLAMMATION NFk. B ↑ Adhesion molecules (ICAM, VCAM) ↑ Chemotactic proteins (MCP – 1) ↑ Interleukins, C-reactive protein ↑ Apoptosis, tissue factor PLATELET AGGREGATION, FIBRIN PRODUCTION, PLAQUE GROWTH ACUTE CORONARY SYNDROMES 17
18
19
20
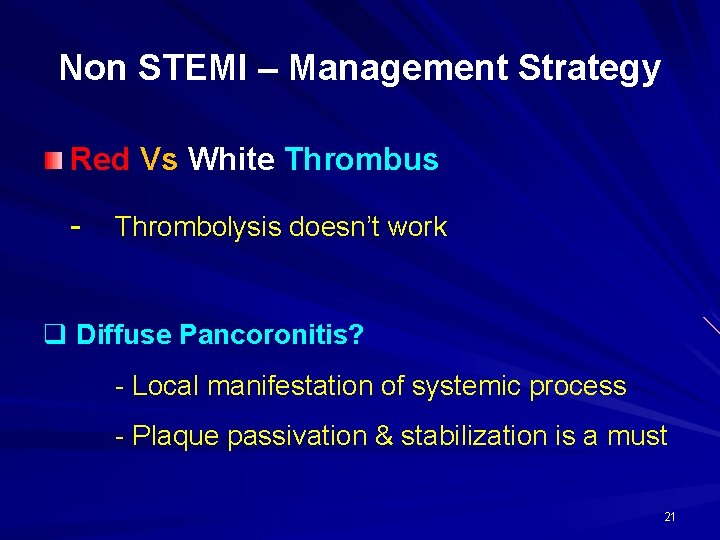
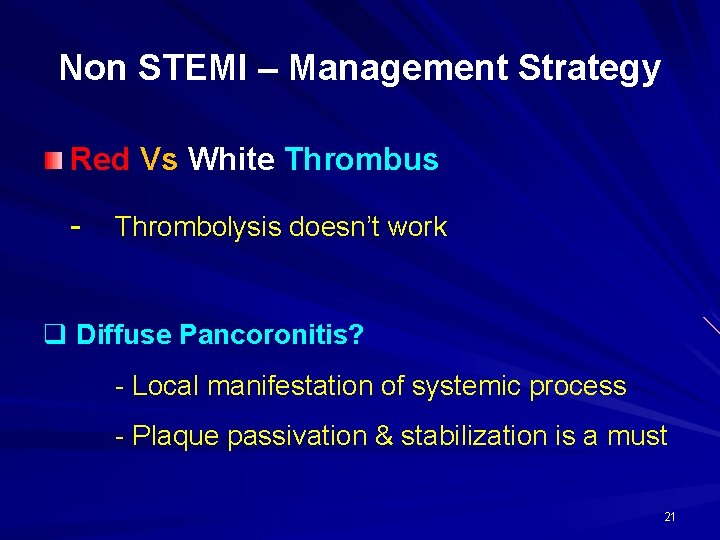
Non STEMI – Management Strategy Red Vs White Thrombus - Thrombolysis doesn’t work q Diffuse Pancoronitis? - Local manifestation of systemic process - Plaque passivation & stabilization is a must 21
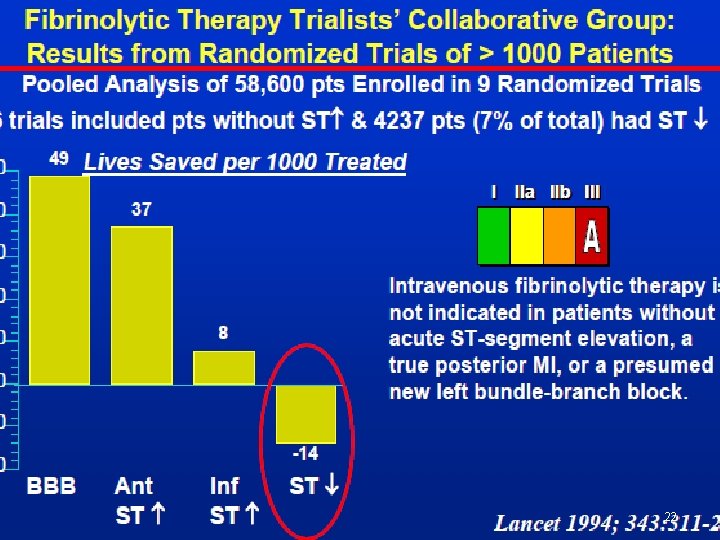
22
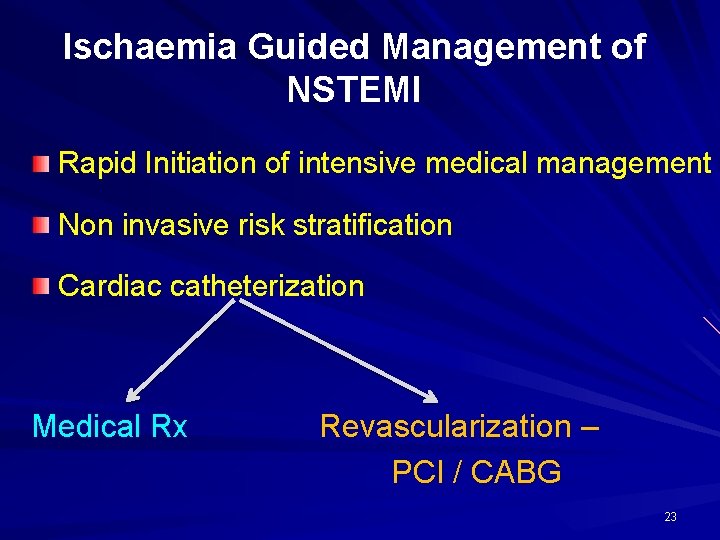
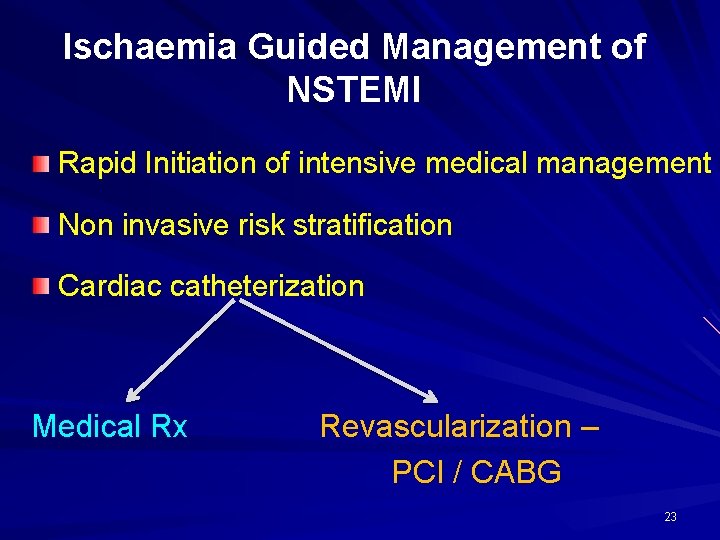
Ischaemia Guided Management of NSTEMI Rapid Initiation of intensive medical management Non invasive risk stratification Cardiac catheterization Medical Rx Revascularization – PCI / CABG 23
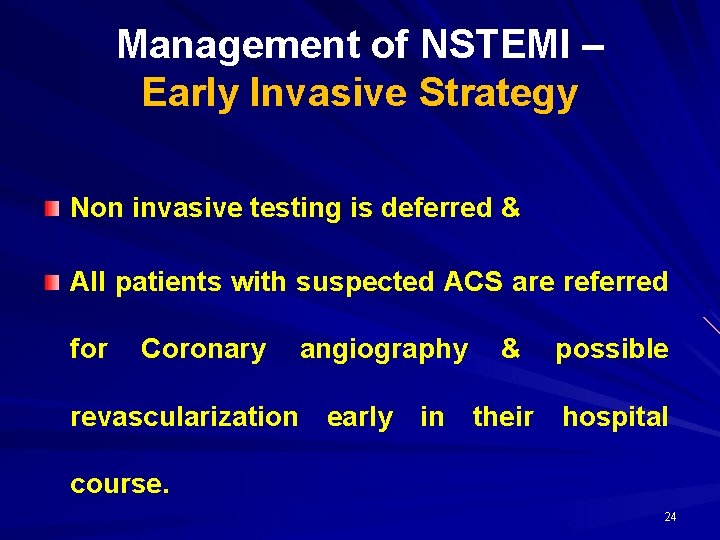
Management of NSTEMI – Early Invasive Strategy Non invasive testing is deferred & All patients with suspected ACS are referred for Coronary angiography & possible revascularization early in their hospital course. 24
Management of NSTEMI – Early Invasive Approach Helps in determining coronary anatomy early in the hospital course. Avoid lengthy delays & possible ambiguities associated with noninvasive testing. Specific anatomical subgroups expeditiously identified & treated. can be Early hospital discharge for low risk cases. 25
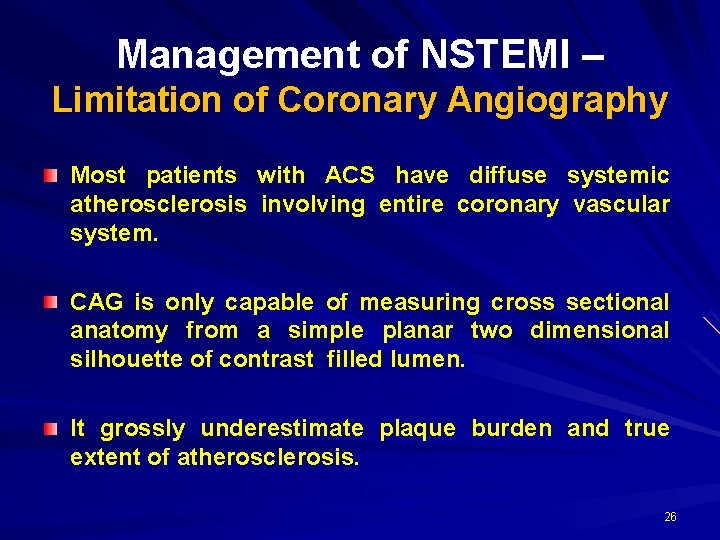
Management of NSTEMI – Limitation of Coronary Angiography Most patients with ACS have diffuse systemic atherosclerosis involving entire coronary vascular system. CAG is only capable of measuring cross sectional anatomy from a simple planar two dimensional silhouette of contrast filled lumen. It grossly underestimate plaque burden and true extent of atherosclerosis. 26

Management of NSTEMI – Limitation of Coronary Angiography (contd) Individual lesion assessment may be difficult, if the adjacent “normal” coronary segment is diffusely diseased or if there is coronary remodeling with development of “extra CONTINUED NEED luminal plaque”. FOR AGGRESSIVE MEDICAL THERAPY is incapable of assessing plaque CAG vulnerability & sub-segment risk for plaque rupture. 27
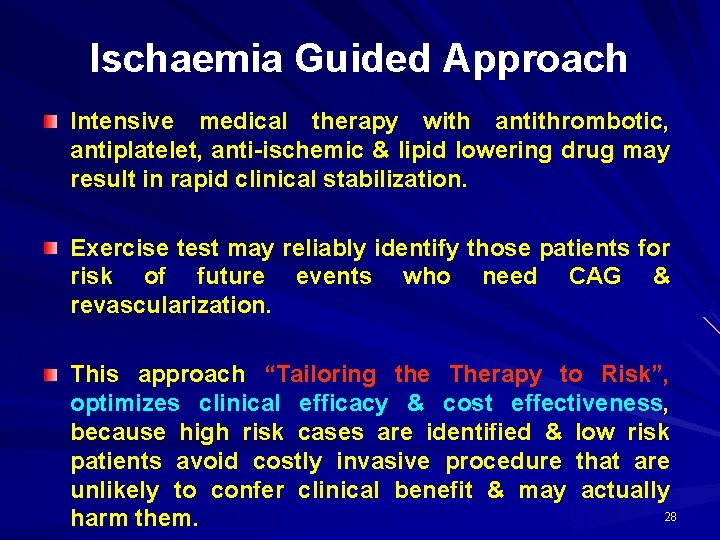
Ischaemia Guided Approach Intensive medical therapy with antithrombotic, antiplatelet, anti-ischemic & lipid lowering drug may result in rapid clinical stabilization. Exercise test may reliably identify those patients for risk of future events who need CAG & revascularization. This approach “Tailoring the Therapy to Risk”, optimizes clinical efficacy & cost effectiveness, because high risk cases are identified & low risk patients avoid costly invasive procedure that are unlikely to confer clinical benefit & may actually 28 harm them.
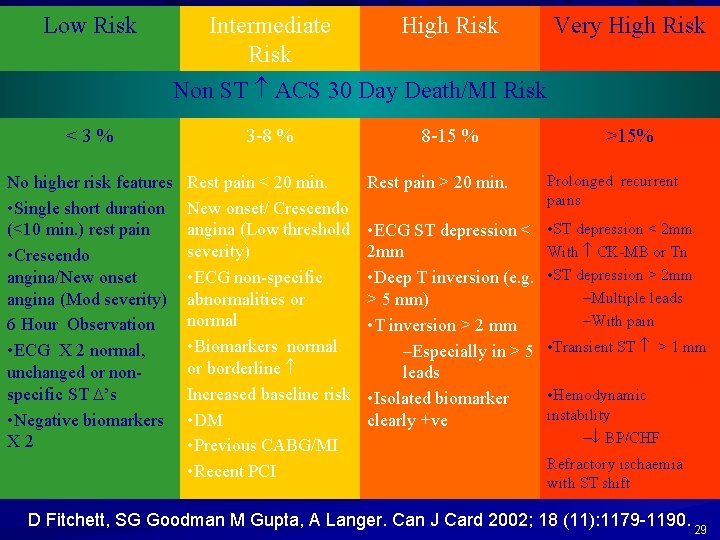
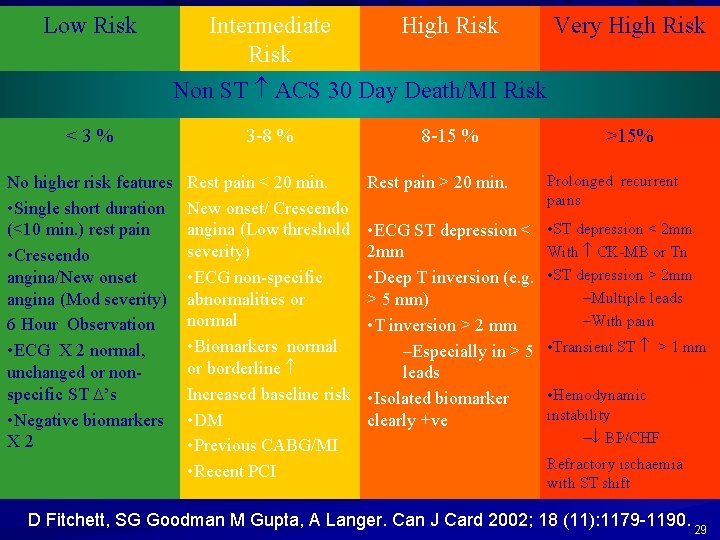
Low Risk Intermediate Risk High Risk Very High Risk Non ST ACS 30 Day Death/MI Risk <3% 3 -8 % No higher risk features • Single short duration (<10 min. ) rest pain • Crescendo angina/New onset angina (Mod severity) 6 Hour Observation • ECG X 2 normal, unchanged or nonspecific ST ’s • Negative biomarkers X 2 Rest pain < 20 min. New onset/ Crescendo angina (Low threshold severity) • ECG non-specific abnormalities or normal • Biomarkers normal or borderline Increased baseline risk • DM • Previous CABG/MI • Recent PCI 8 -15 % >15% Rest pain > 20 min. Prolonged recurrent pains • ECG ST depression < 2 mm • Deep T inversion (e. g. > 5 mm) • T inversion > 2 mm –Especially in > 5 leads • Isolated biomarker clearly +ve • ST depression < 2 mm With CK-MB or Tn • ST depression > 2 mm –Multiple leads –With pain • Transient ST > 1 mm • Hemodynamic instability – BP/CHF Refractory ischaemia with ST shift D Fitchett, SG Goodman M Gupta, A Langer. Can J Card 2002; 18 (11): 1179 -1190. 29
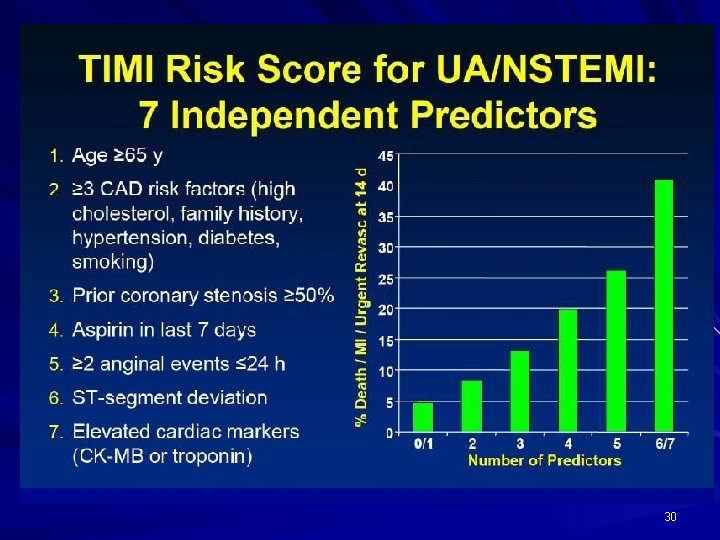
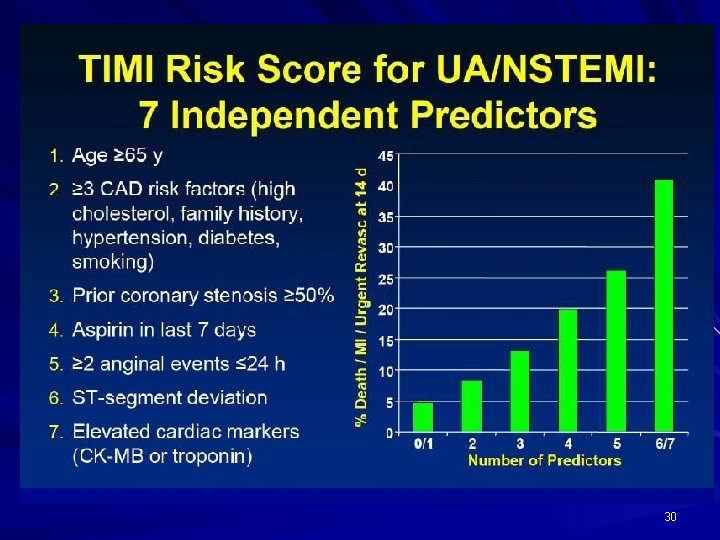
30
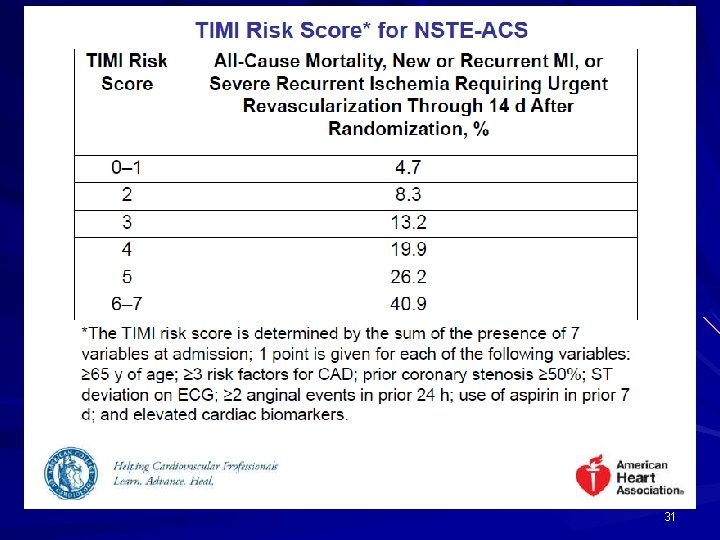
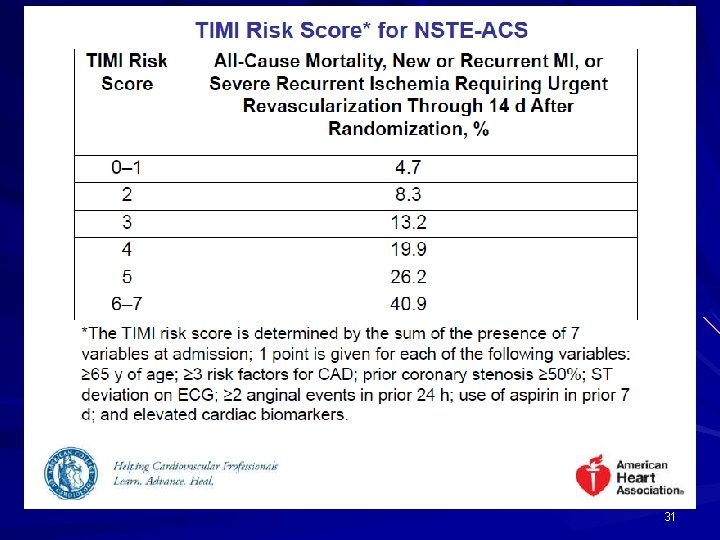
31
32
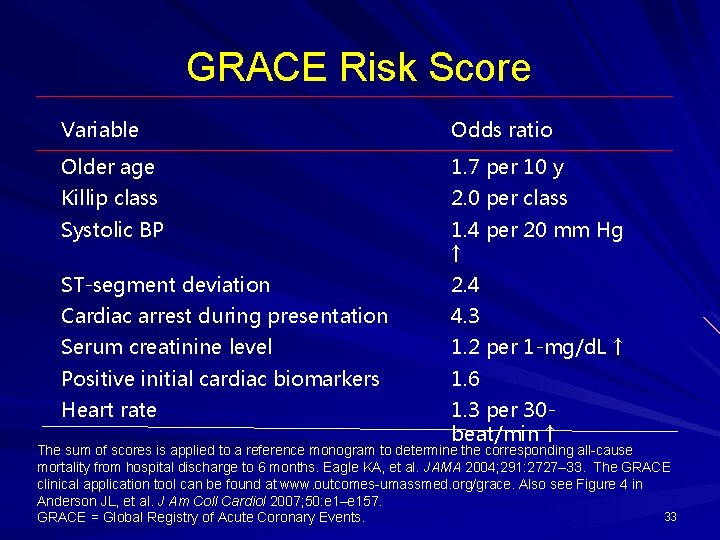
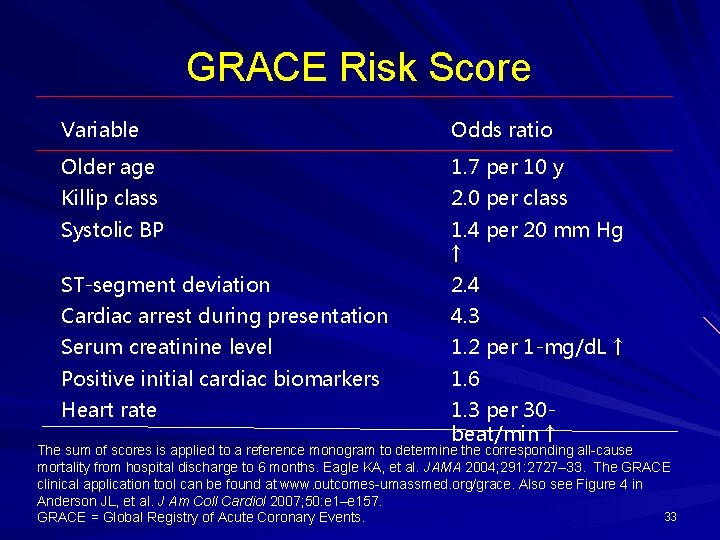
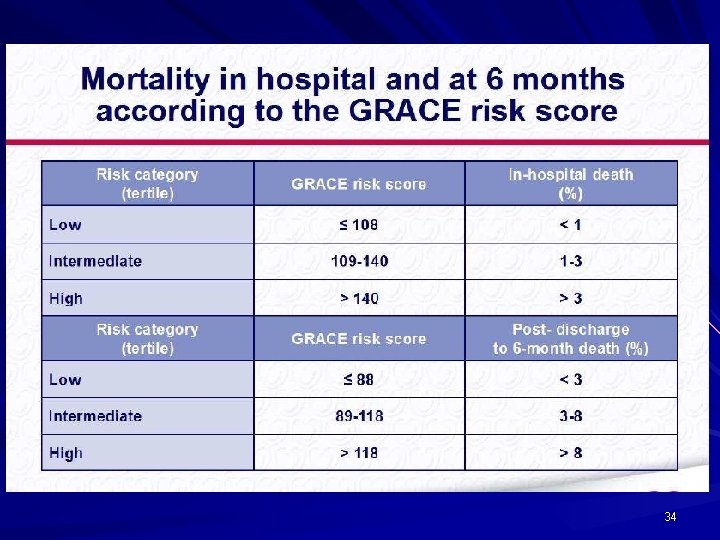
GRACE Risk Score Variable Odds ratio Older age 1. 7 per 10 y Killip class 2. 0 per class Systolic BP 1. 4 per 20 mm Hg ↑ ST-segment deviation 2. 4 Cardiac arrest during presentation 4. 3 Serum creatinine level 1. 2 per 1 -mg/d. L ↑ Positive initial cardiac biomarkers 1. 6 Heart rate 1. 3 per 30 beat/min ↑ The sum of scores is applied to a reference monogram to determine the corresponding all-cause mortality from hospital discharge to 6 months. Eagle KA, et al. JAMA 2004; 291: 2727– 33. The GRACE clinical application tool can be found at www. outcomes-umassmed. org/grace. Also see Figure 4 in Anderson JL, et al. J Am Coll Cardiol 2007; 50: e 1–e 157. 33 GRACE = Global Registry of Acute Coronary Events.
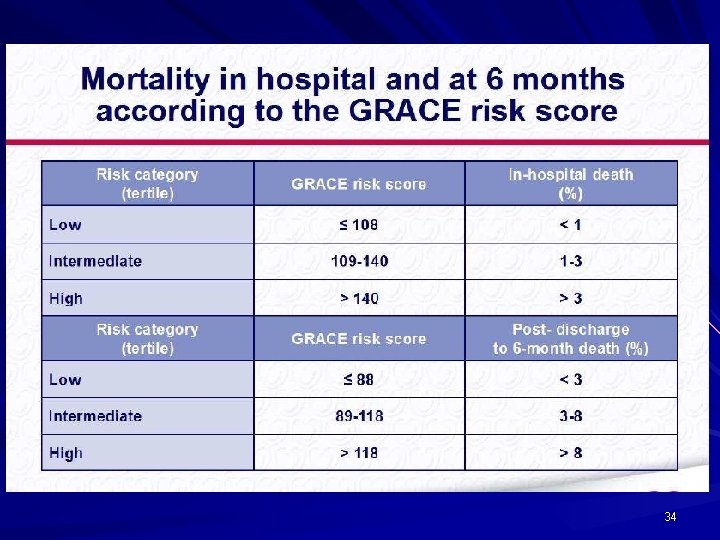
34
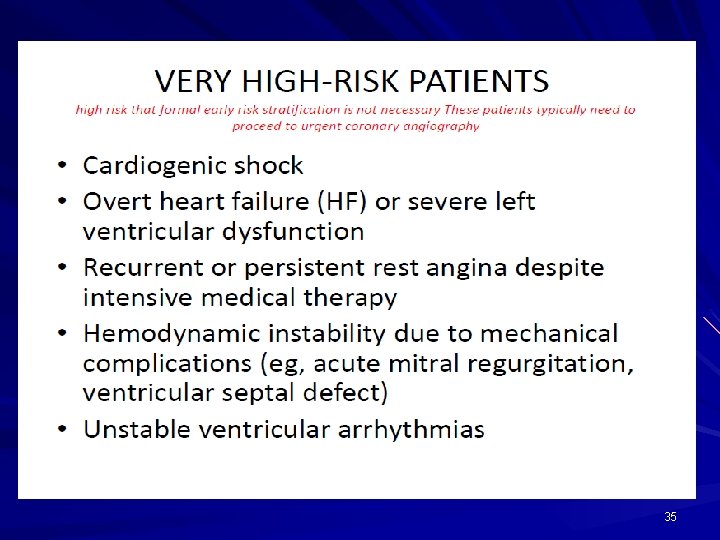
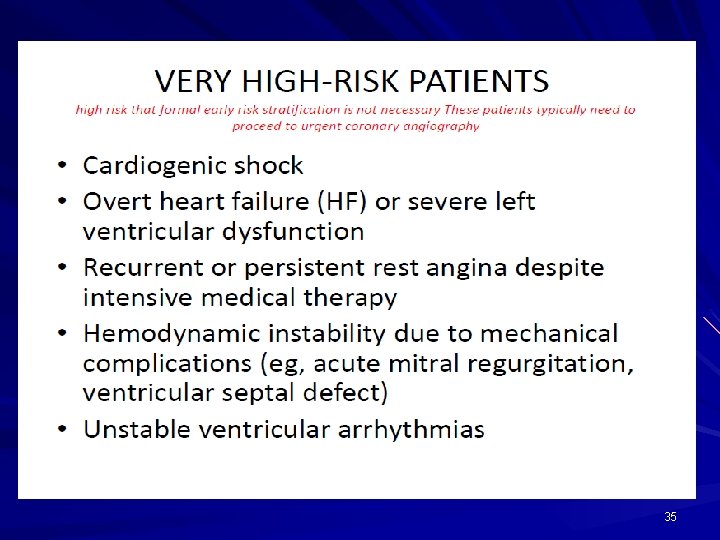
35
36
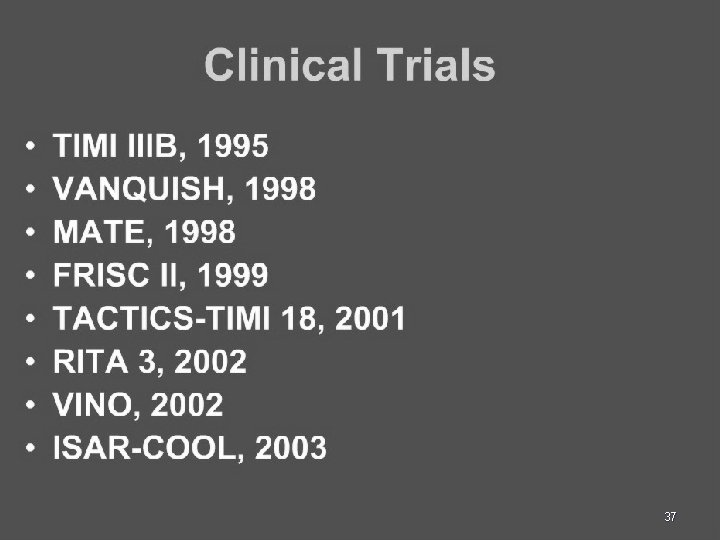
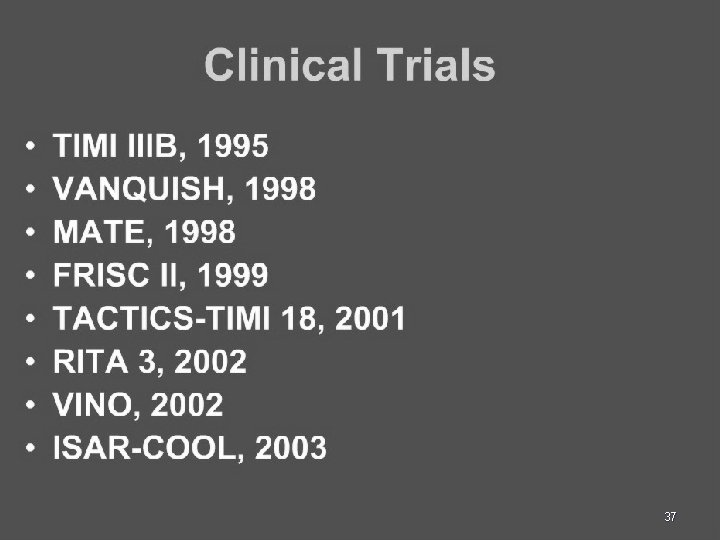
37
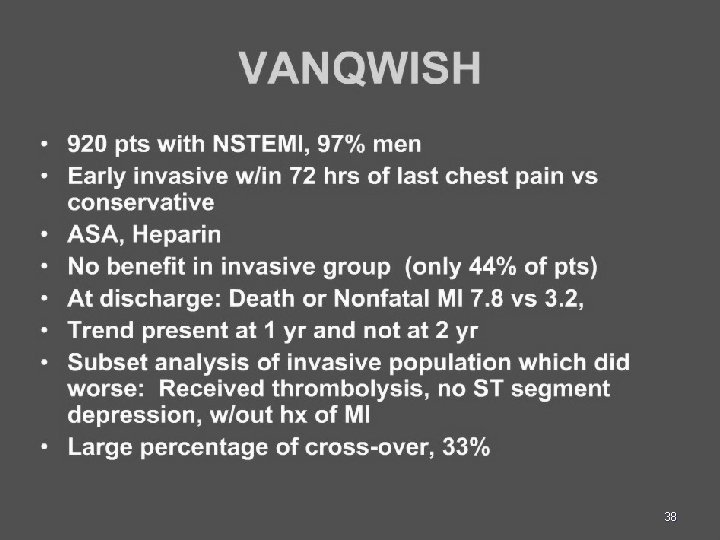
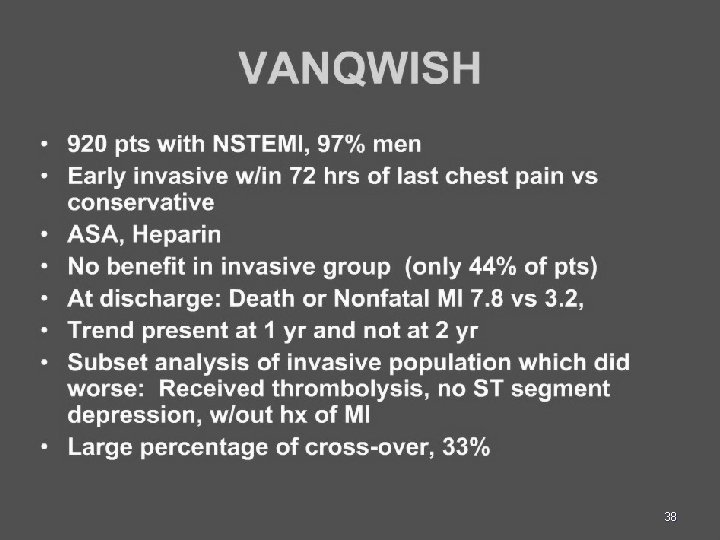
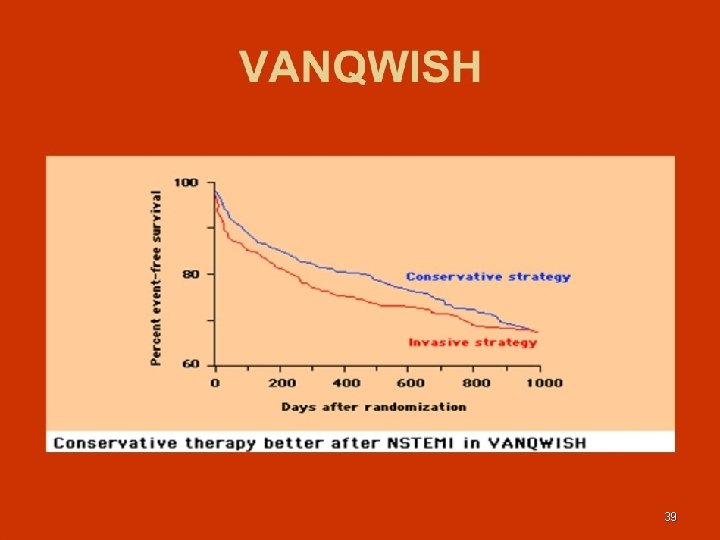
38
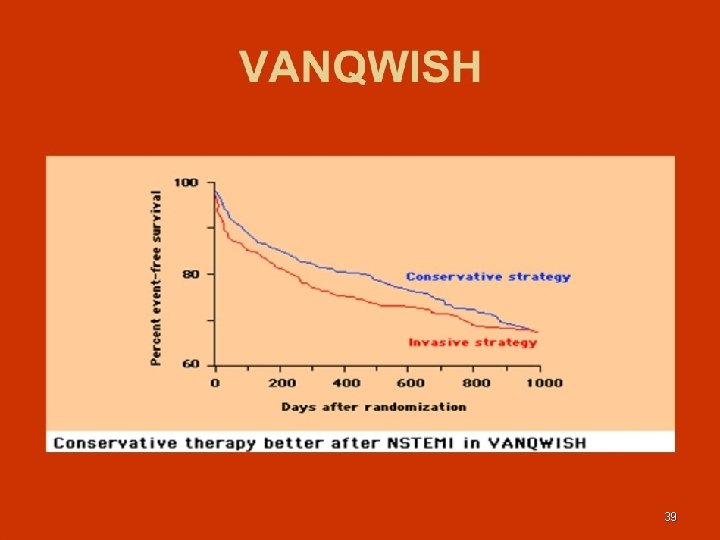
39
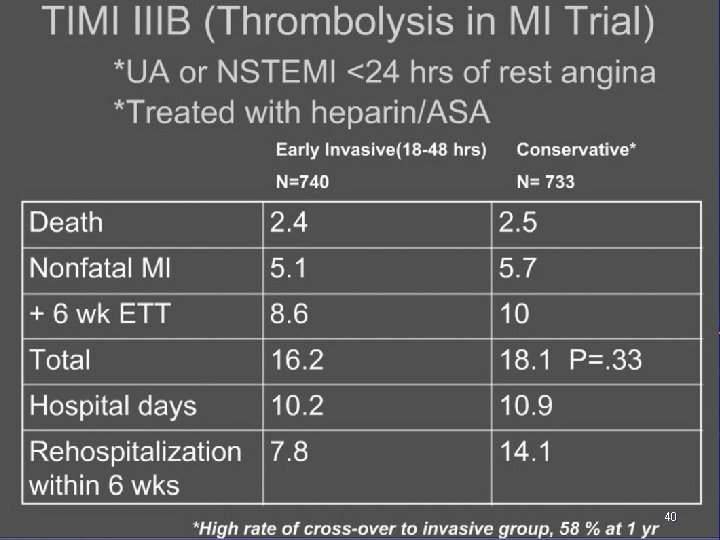
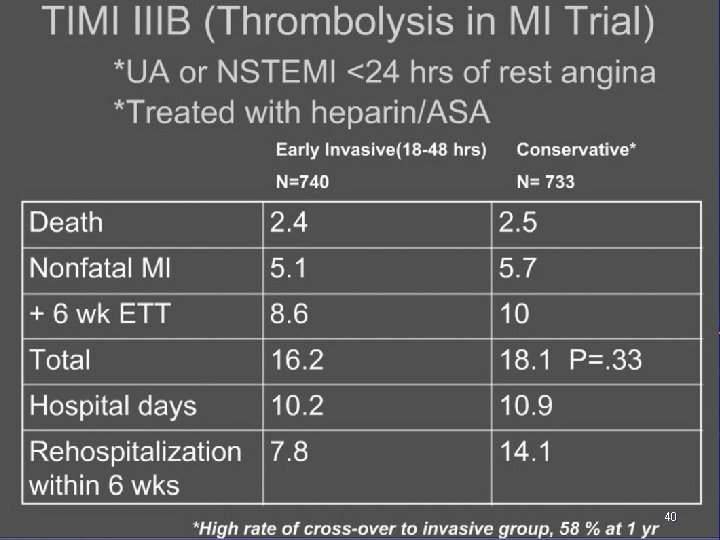
40
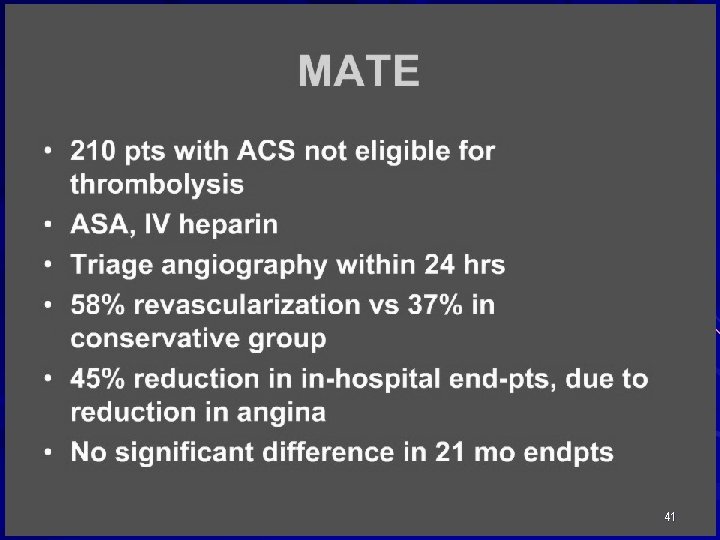
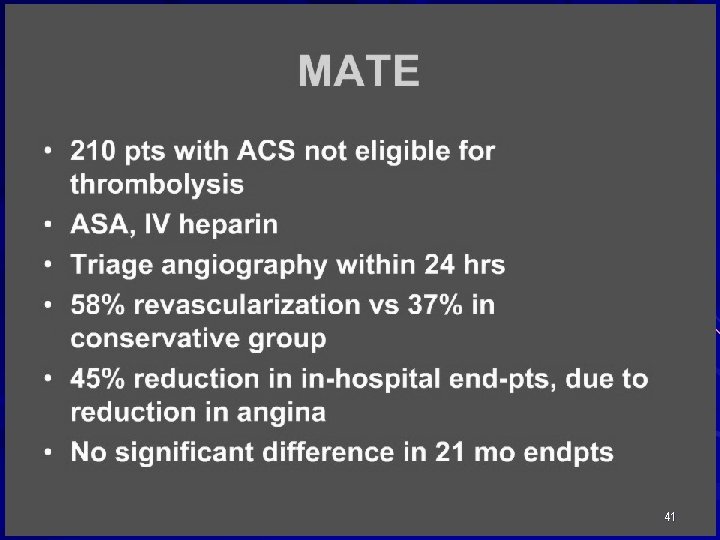
41
ICTUS Trial Invasive versus conservative treatment in unstable coronary syndromes Presented at European Society of Cardiology Congress 2004 Presented by Dr. R. J. De Winter 42
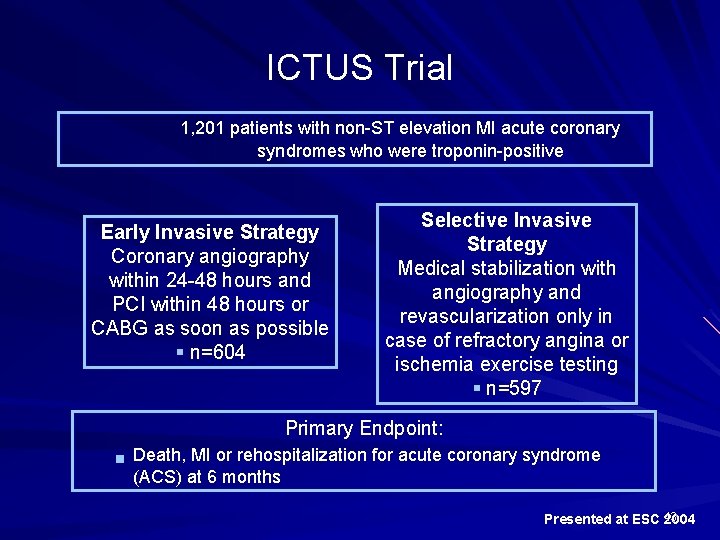
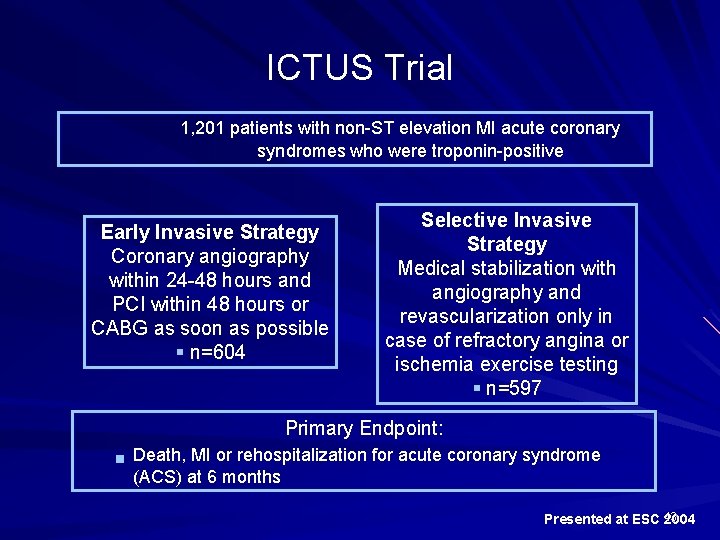
ICTUS Trial 1, 201 patients with non-ST elevation MI acute coronary syndromes who were troponin-positive Early Invasive Strategy Coronary angiography within 24 -48 hours and PCI within 48 hours or CABG as soon as possible § n=604 Selective Invasive Strategy Medical stabilization with angiography and revascularization only in case of refractory angina or ischemia exercise testing § n=597 Primary Endpoint: g Death, MI or rehospitalization for acute coronary syndrome (ACS) at 6 months Presented at ESC 43 2004
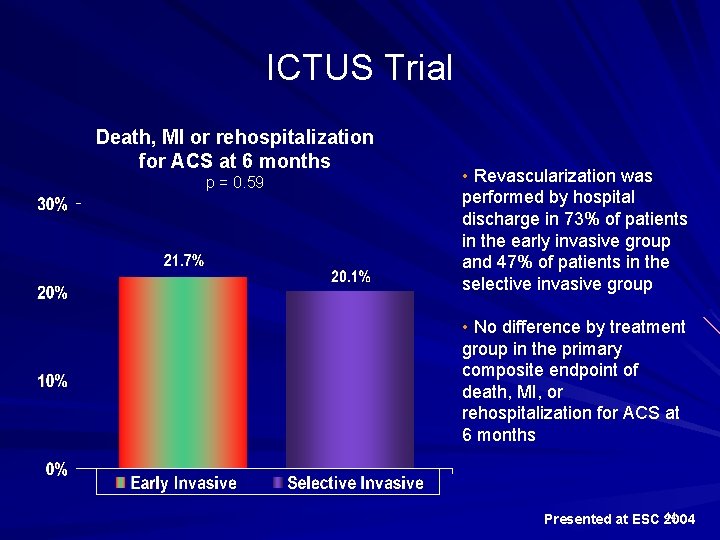
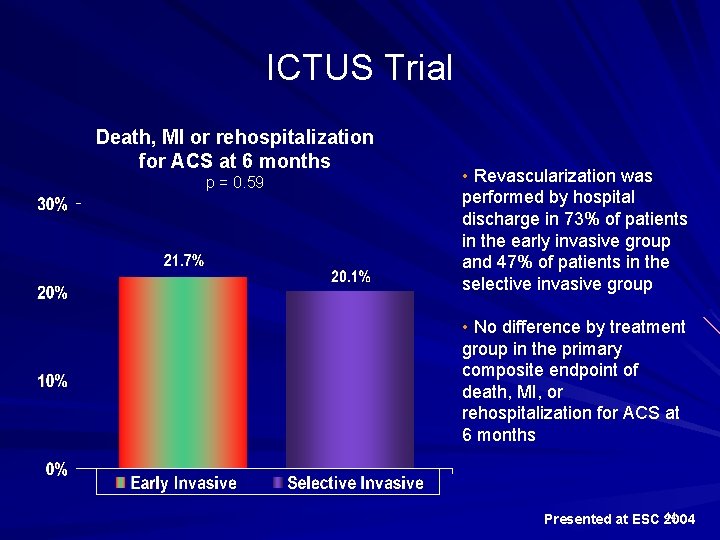
ICTUS Trial Death, MI or rehospitalization for ACS at 6 months p = 0. 59 • Revascularization was performed by hospital discharge in 73% of patients in the early invasive group and 47% of patients in the selective invasive group • No difference by treatment group in the primary composite endpoint of death, MI, or rehospitalization for ACS at 6 months Presented at ESC 44 2004
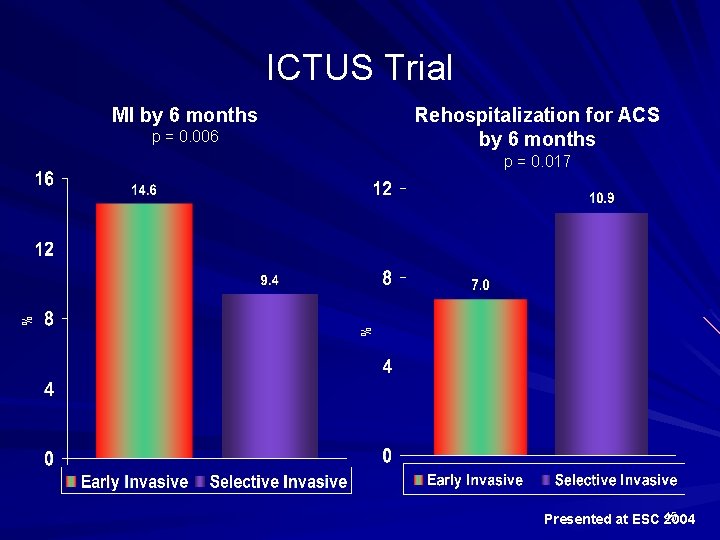
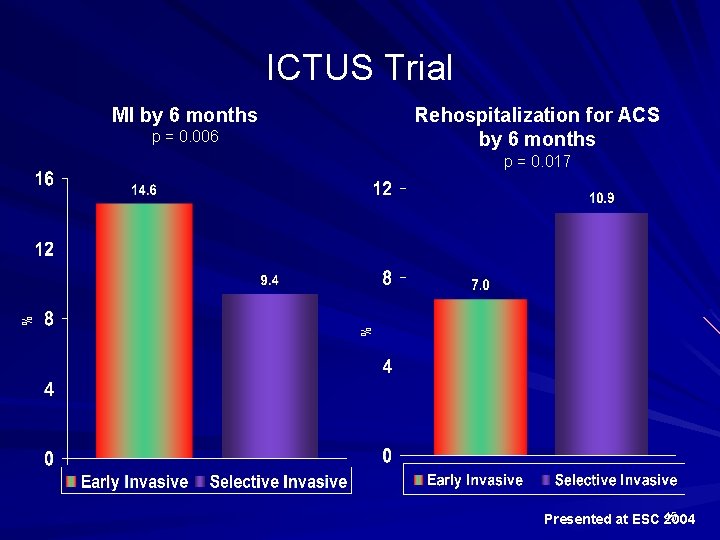
ICTUS Trial MI by 6 months Rehospitalization for ACS by 6 months p = 0. 006 % % p = 0. 017 Presented at ESC 45 2004
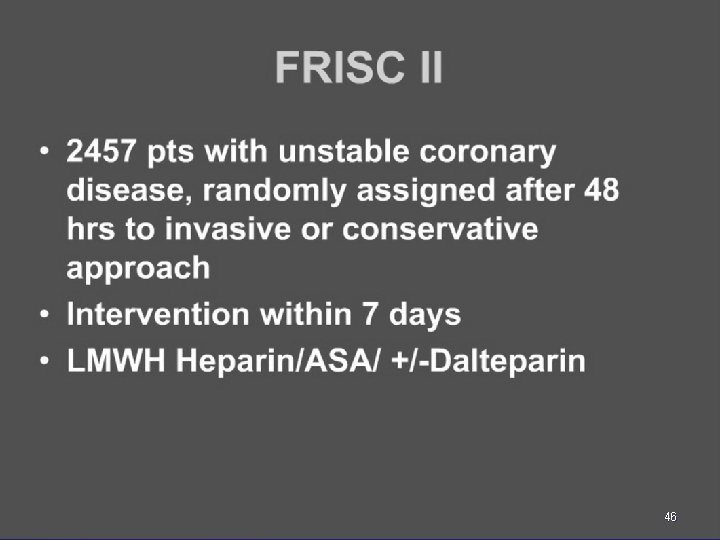
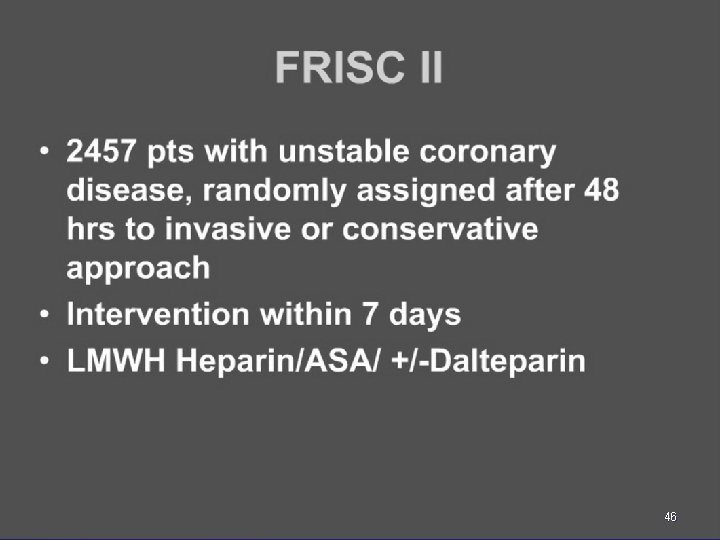
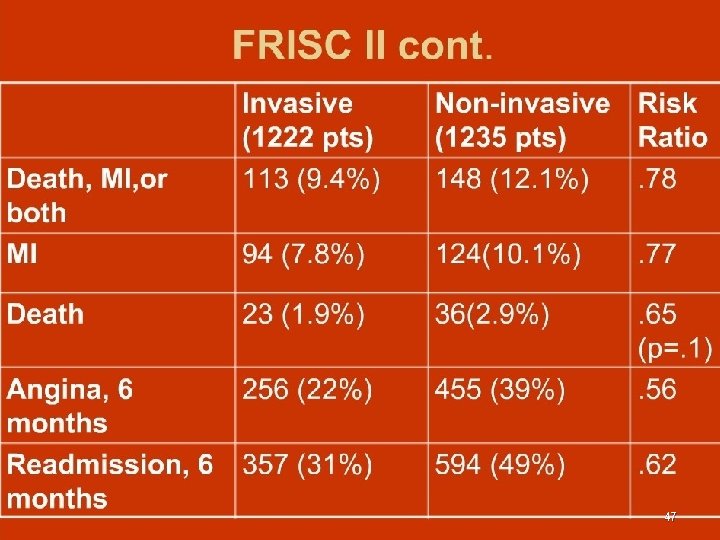
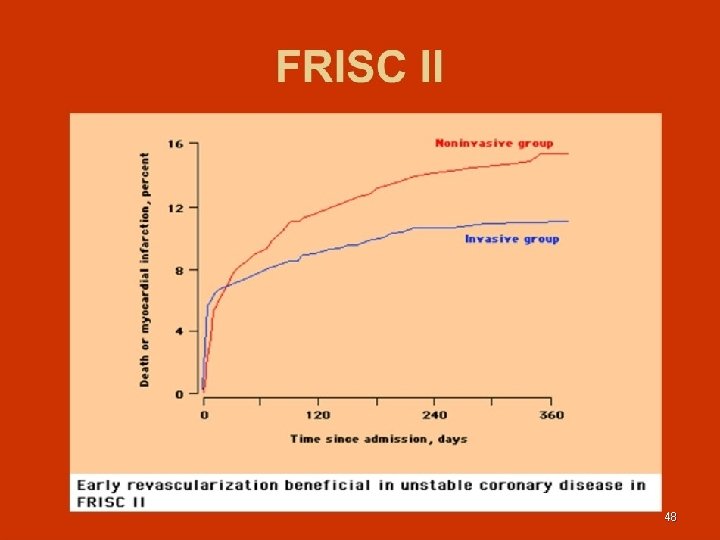
46
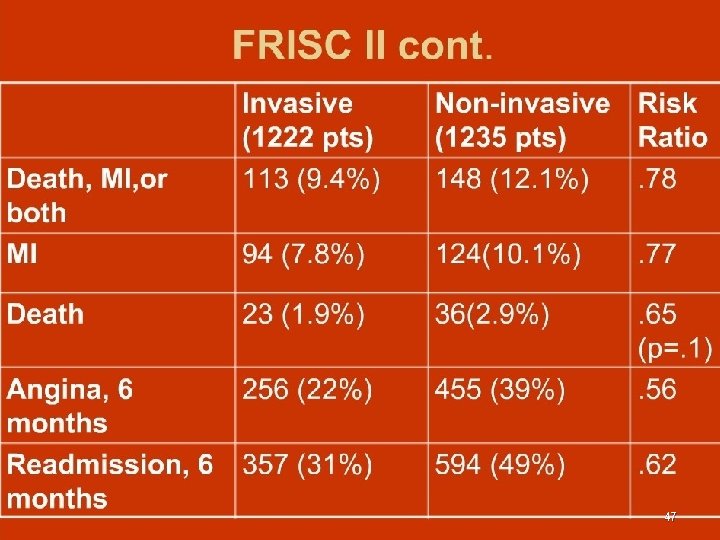
47
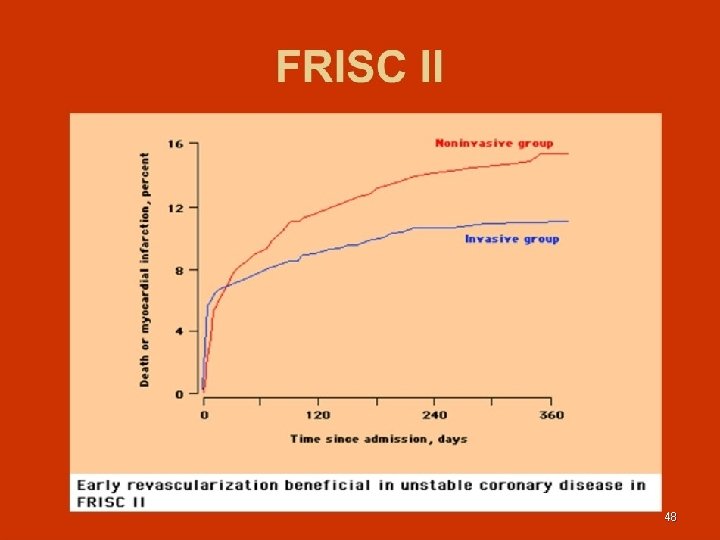
48

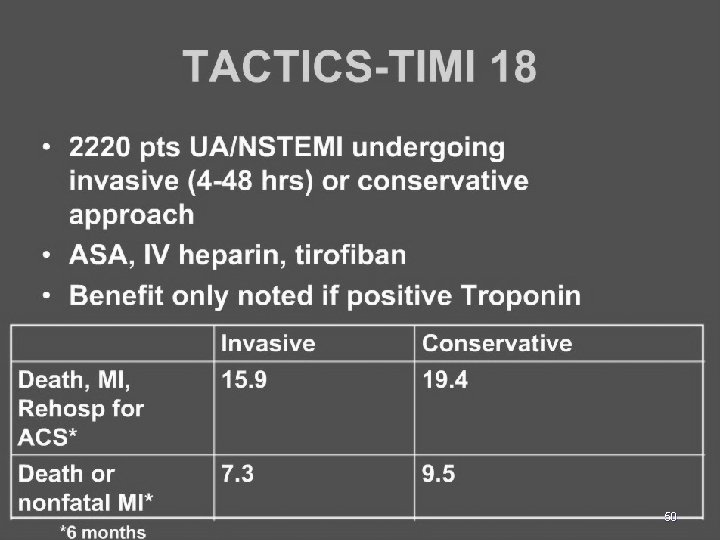
TACTICS-TIMI 18 Treat Angina with Aggrastat + Determine Cost of Therapy with an Invasive or Conservative Strategy TIMI 18 As presented by Dr. Cannon at AHA 2000. 49
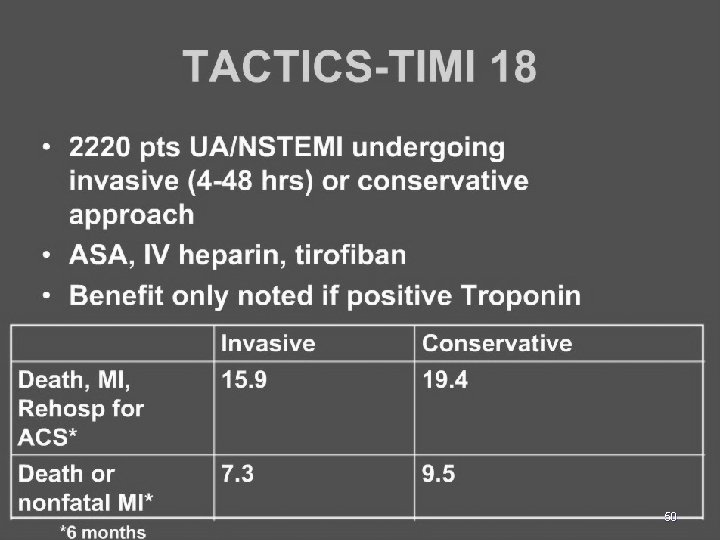
50
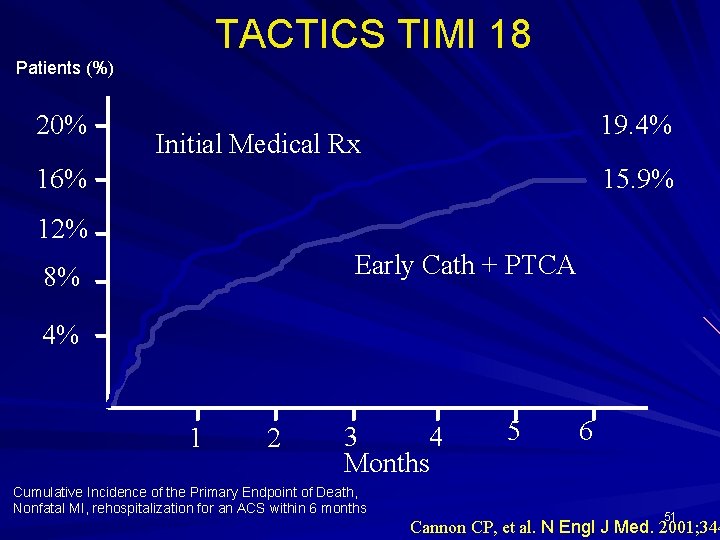
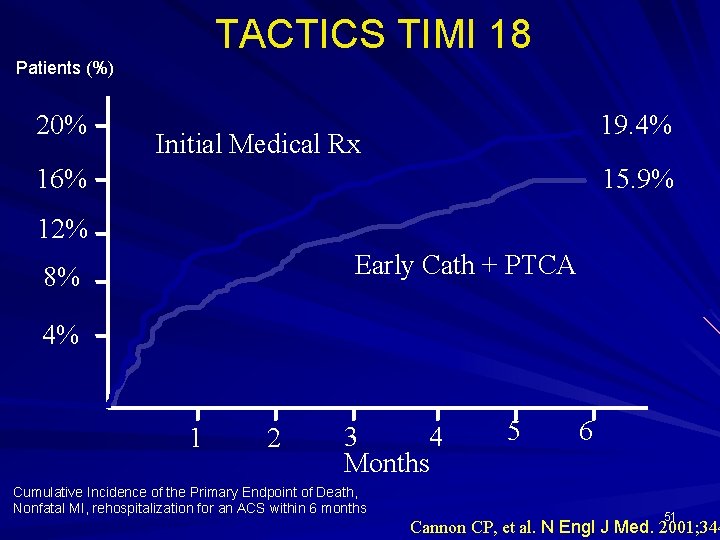
TACTICS TIMI 18 Patients (%) 20% 19. 4% Initial Medical Rx 16% 15. 9% 12% Early Cath + PTCA 8% 4% 1 2 3 4 Months Cumulative Incidence of the Primary Endpoint of Death, Nonfatal MI, rehospitalization for an ACS within 6 months 5 6 51 Cannon CP, et al. N Engl J Med. 2001; 344
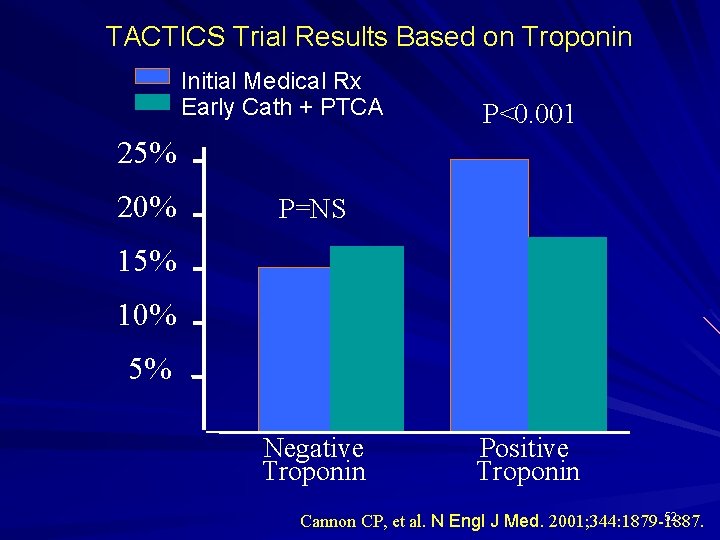
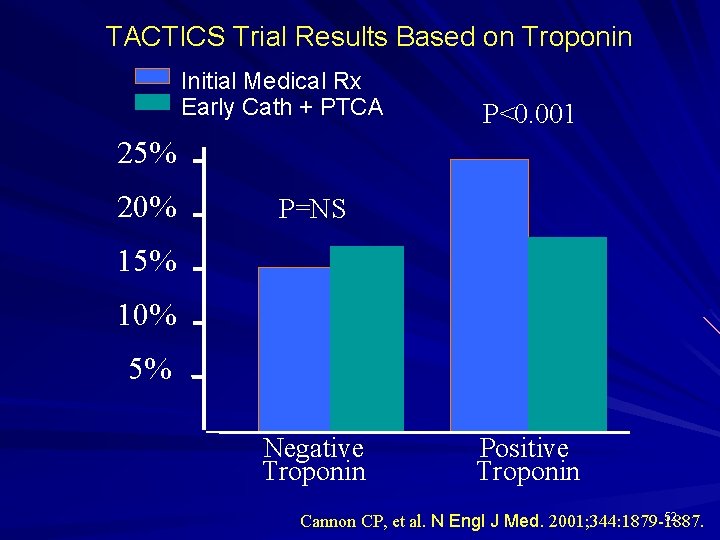
TACTICS Trial Results Based on Troponin Initial Medical Rx Early Cath + PTCA P<0. 001 25% 20% P=NS 15% 10% 5% Negative Troponin Positive Troponin 52 Cannon CP, et al. N Engl J Med. 2001; 344: 1879 -1887.
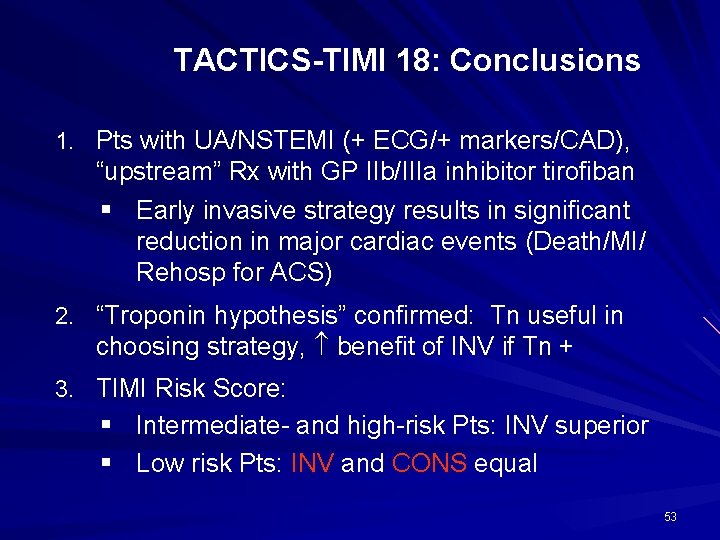
TACTICS-TIMI 18: Conclusions 1. Pts with UA/NSTEMI (+ ECG/+ markers/CAD), “upstream” Rx with GP IIb/IIIa inhibitor tirofiban § Early invasive strategy results in significant reduction in major cardiac events (Death/MI/ Rehosp for ACS) 2. “Troponin hypothesis” confirmed: Tn useful in choosing strategy, benefit of INV if Tn + 3. TIMI Risk Score: § Intermediate- and high-risk Pts: INV superior § Low risk Pts: INV and CONS equal 53
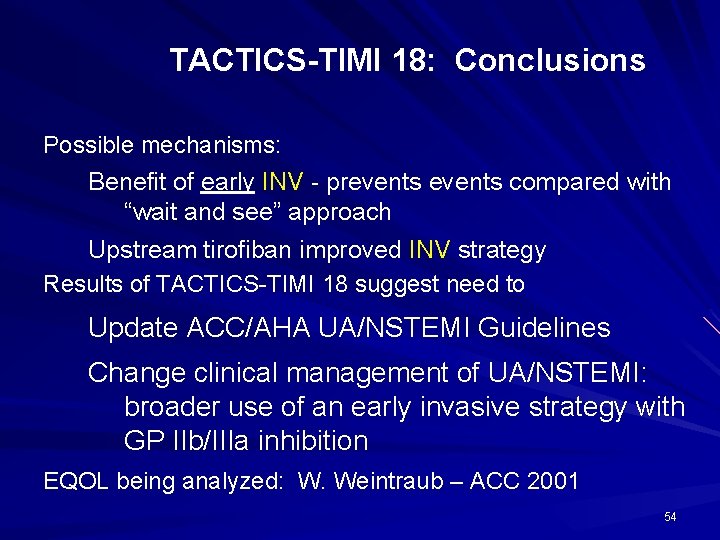
TACTICS-TIMI 18: Conclusions Possible mechanisms: Benefit of early INV - prevents compared with “wait and see” approach Upstream tirofiban improved INV strategy Results of TACTICS-TIMI 18 suggest need to Update ACC/AHA UA/NSTEMI Guidelines Change clinical management of UA/NSTEMI: broader use of an early invasive strategy with GP IIb/IIIa inhibition EQOL being analyzed: W. Weintraub – ACC 2001 54
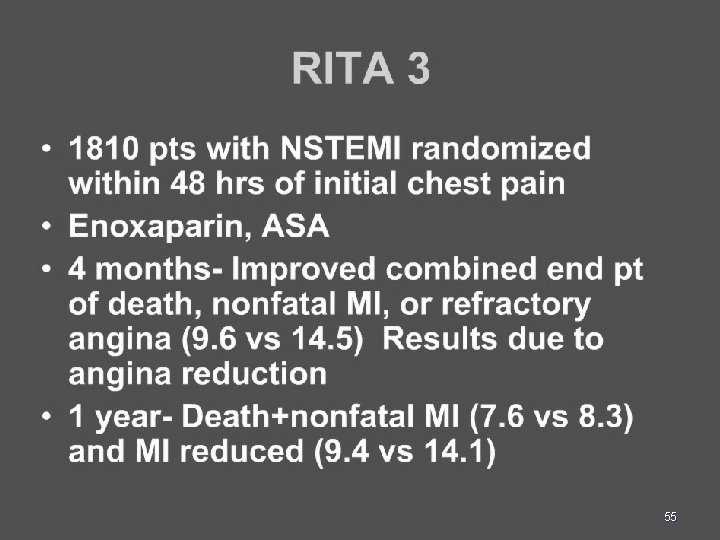
55
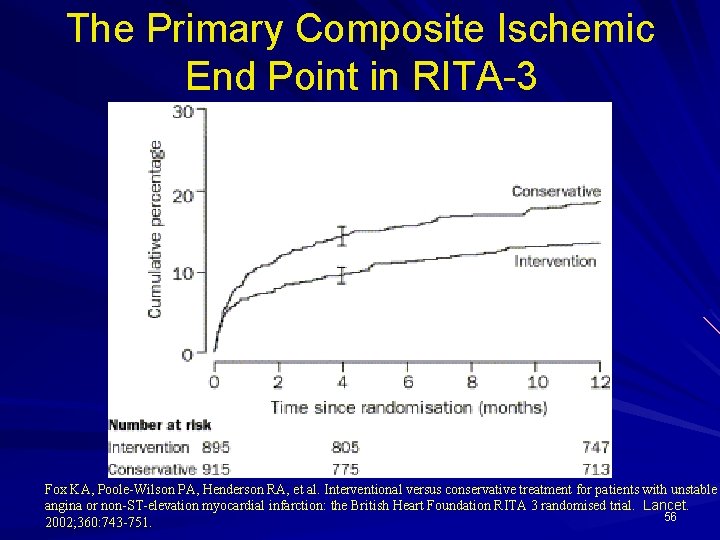
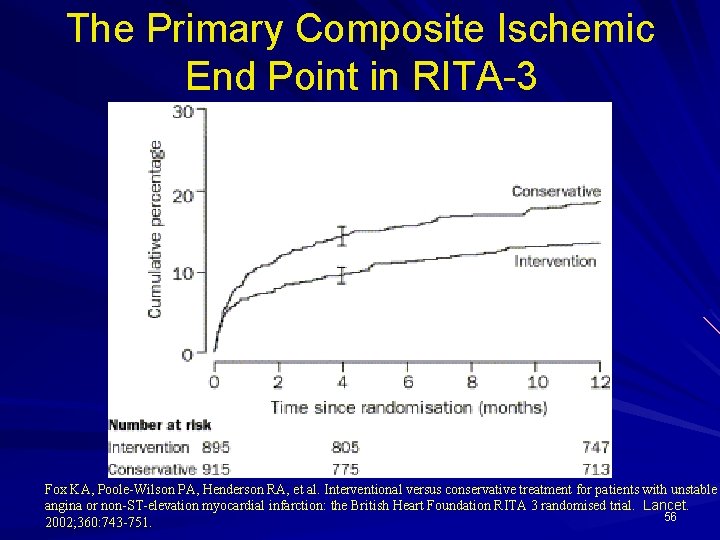
The Primary Composite Ischemic End Point in RITA-3 Fox KA, Poole-Wilson PA, Henderson RA, et al. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomised trial. Lancet. 56 2002; 360: 743 -751.
57
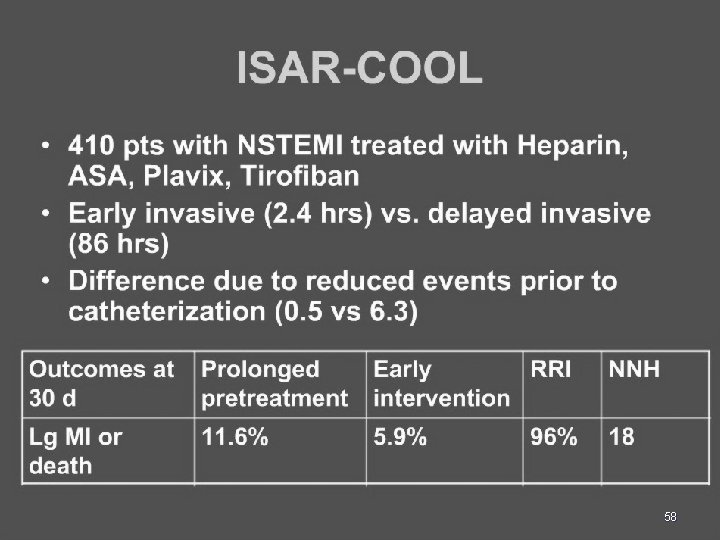
58
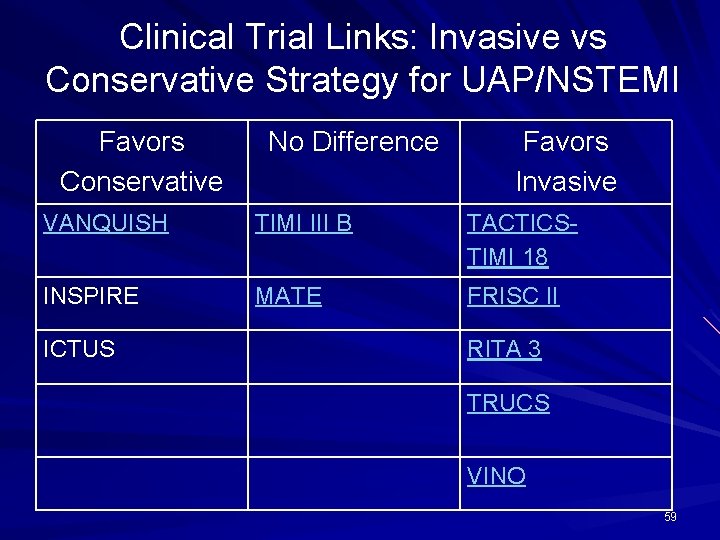
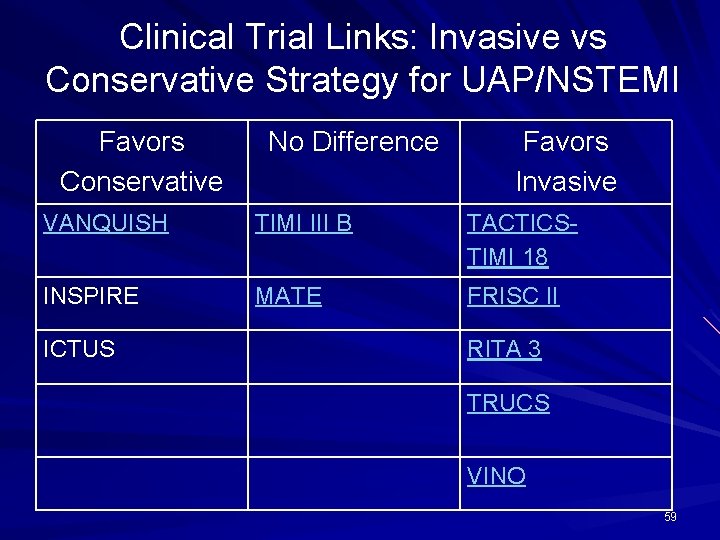
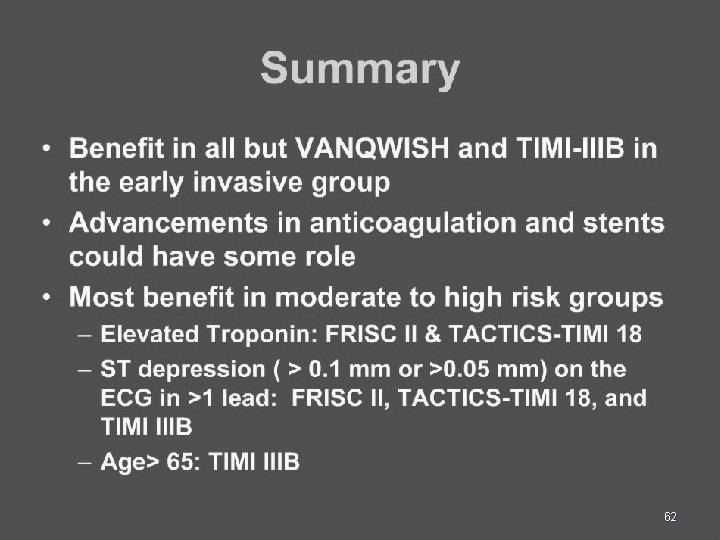
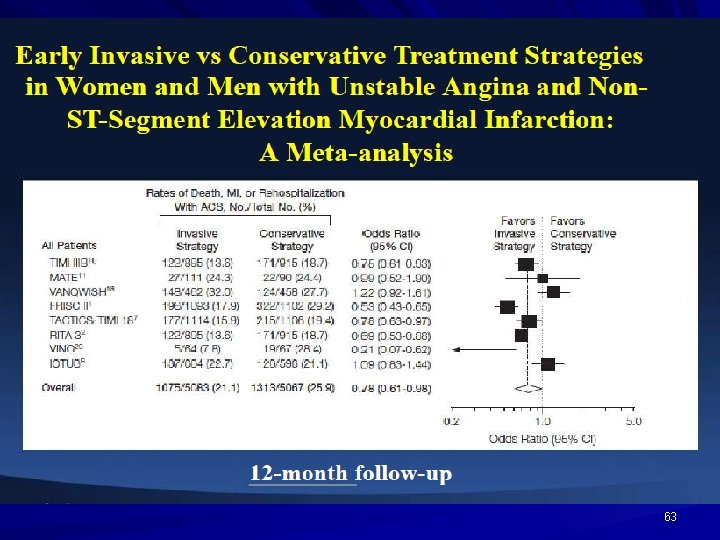
Clinical Trial Links: Invasive vs Conservative Strategy for UAP/NSTEMI Favors Conservative No Difference Favors Invasive VANQUISH TIMI III B TACTICSTIMI 18 INSPIRE MATE FRISC II ICTUS RITA 3 TRUCS VINO 59
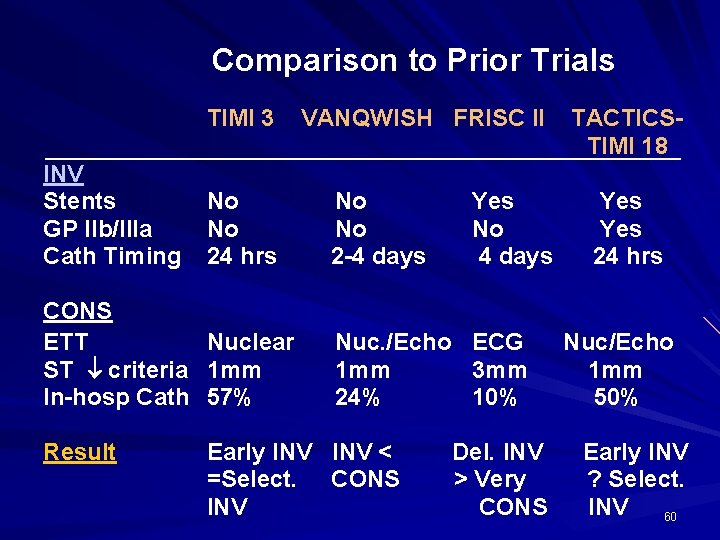
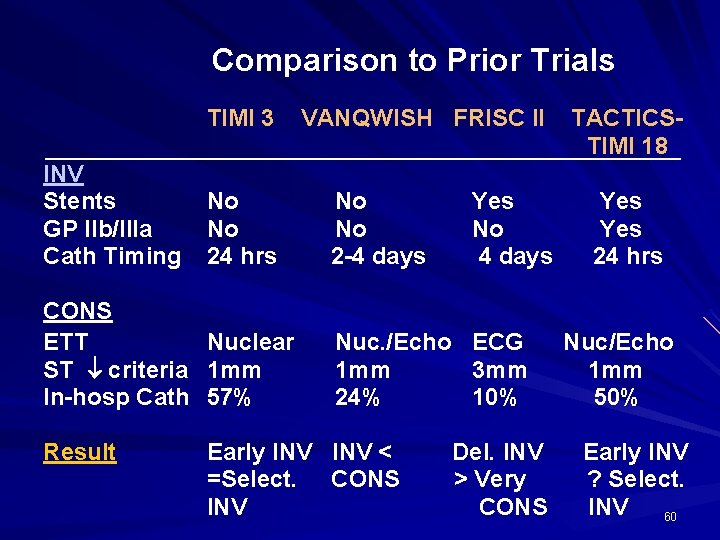
Comparison to Prior Trials TIMI 3 INV Stents GP IIb/IIIa Cath Timing No No 24 hrs CONS ETT Nuclear ST criteria 1 mm In-hosp Cath 57% Result VANQWISH FRISC II No No 2 -4 days Yes No 4 days Nuc. /Echo ECG 1 mm 3 mm 24% 10% Early INV < =Select. CONS INV Del. INV > Very CONS TACTICSTIMI 18 Yes 24 hrs Nuc/Echo 1 mm 50% Early INV ? Select. INV 60
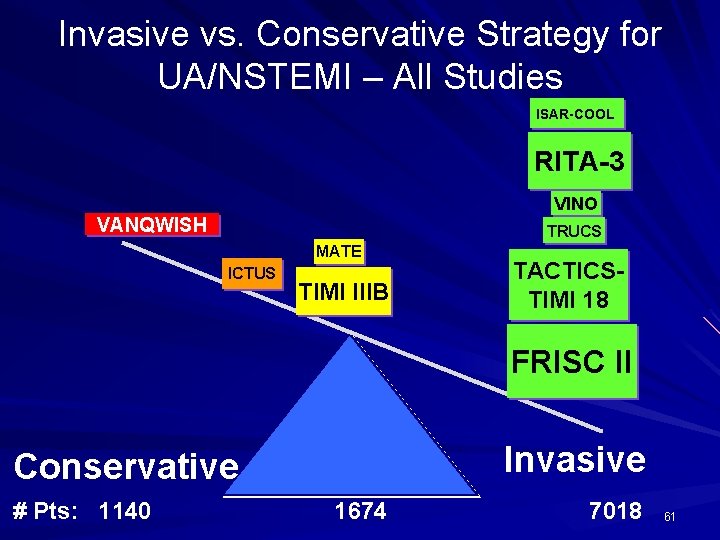
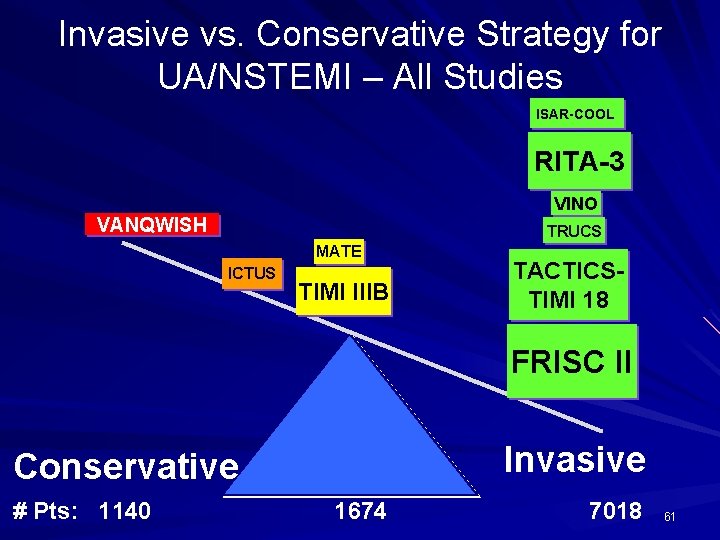
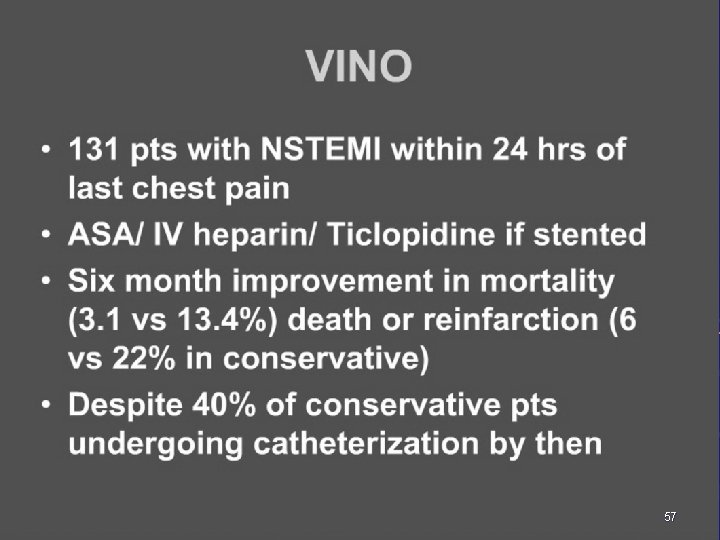
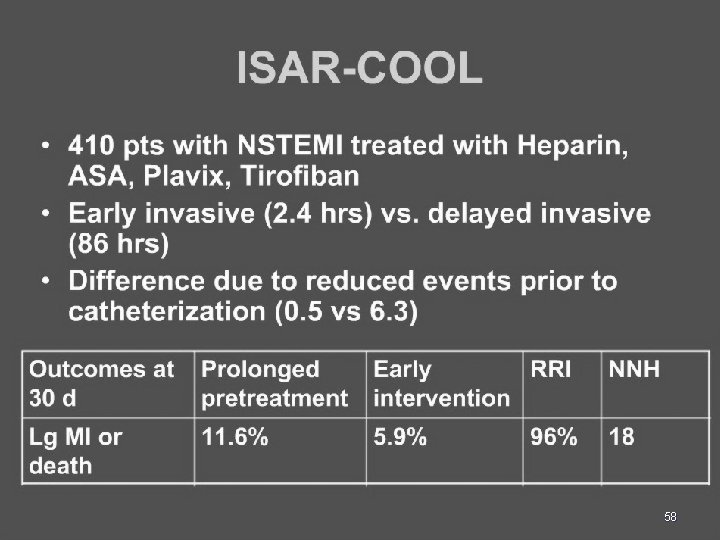
Invasive vs. Conservative Strategy for UA/NSTEMI – All Studies ISAR-COOL RITA-3 VINO VANQWISH TRUCS MATE ICTUS TIMI IIIB TACTICSTIMI 18 FRISC II Invasive Conservative # Pts: 1140 1674 7018 61
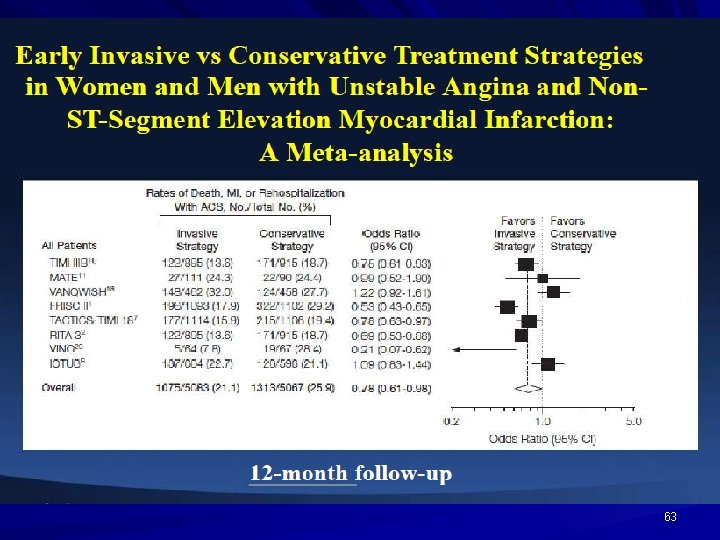
62
63
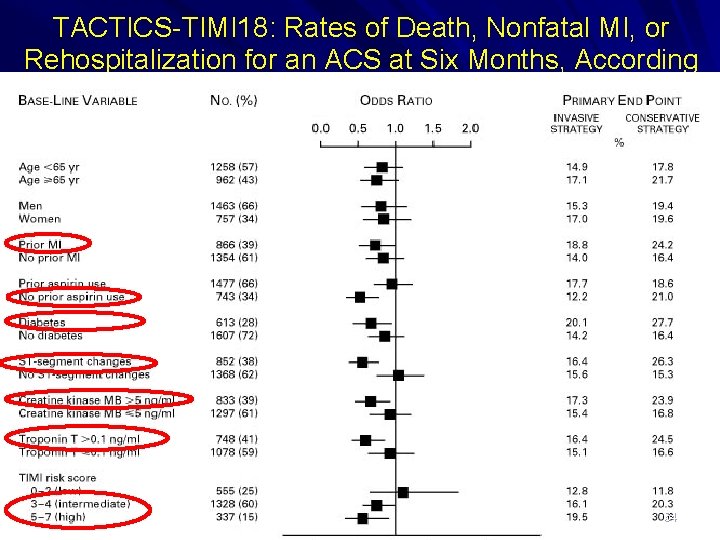
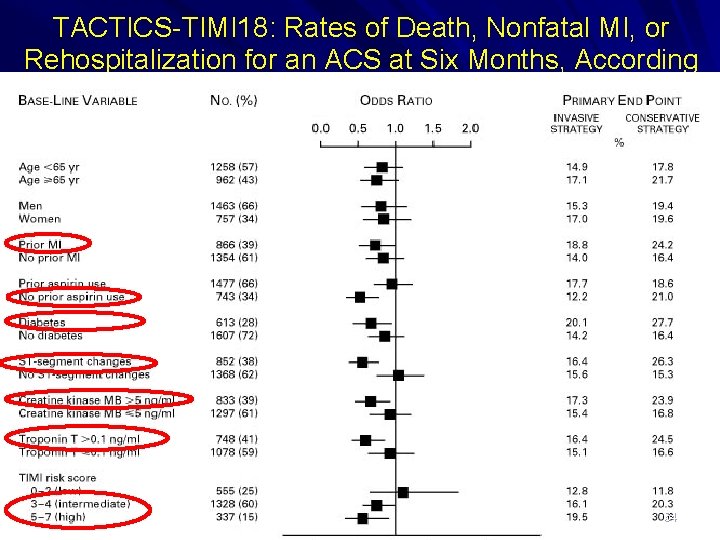
TACTICS-TIMI 18: Rates of Death, Nonfatal MI, or Rehospitalization for an ACS at Six Months, According to Base-Line Characteristics Cannon C et al. N Engl J Med 2001; 344: 1879 -1887 64
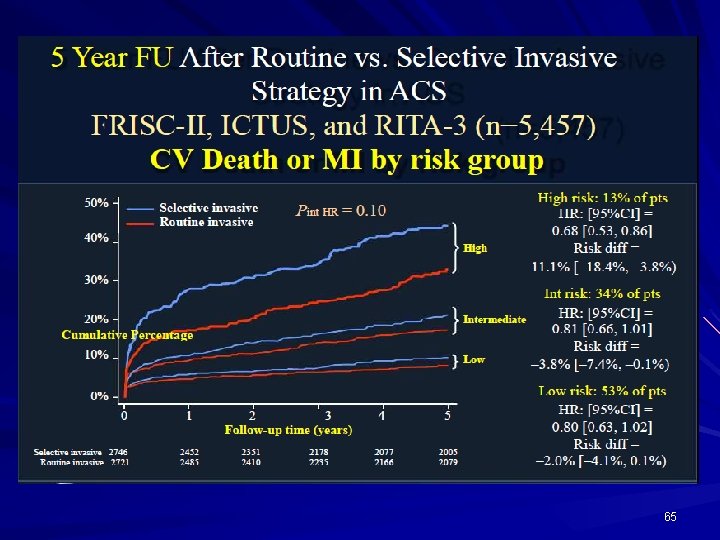
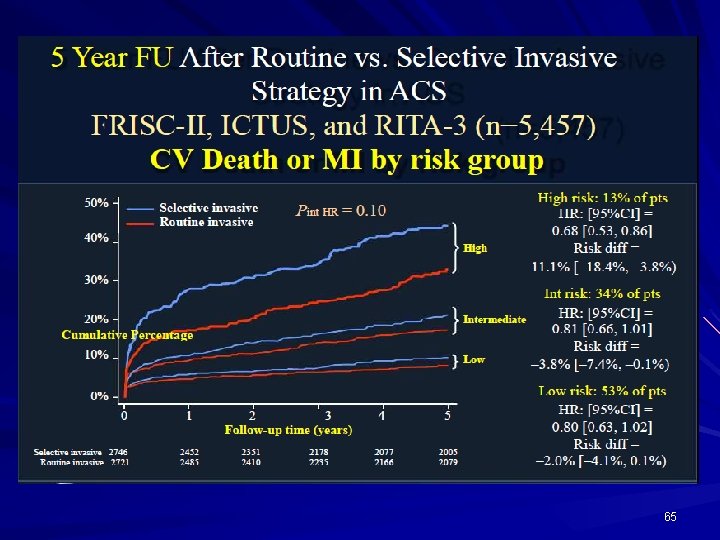
65
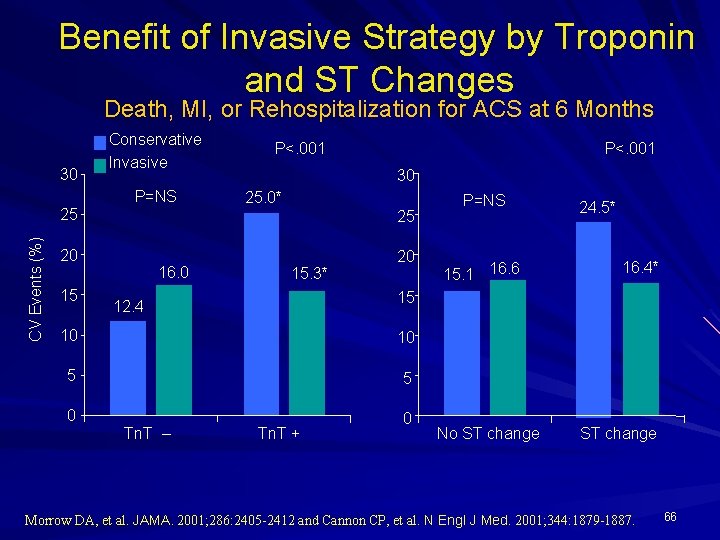
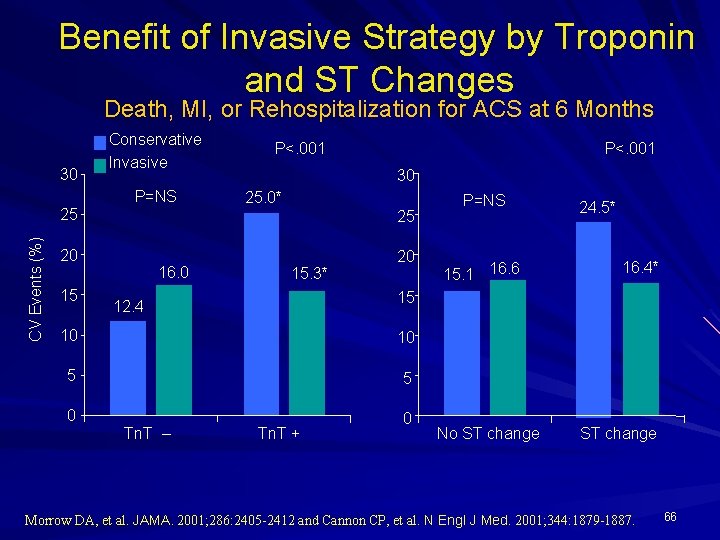
Benefit of Invasive Strategy by Troponin and ST Changes Death, MI, or Rehospitalization for ACS at 6 Months 30 CV Events (%) 25 Conservative Invasive P=NS P<. 001 30 25. 0* 25 20 15 P<. 001 16. 0 15. 3* 20 15. 1 16. 6 24. 5* 16. 4* 15 12. 4 10 10 5 5 0 0 Tn. T – P=NS Tn. T + No ST change Morrow DA, et al. JAMA. 2001; 286: 2405 -2412 and Cannon CP, et al. N Engl J Med. 2001; 344: 1879 -1887. 66
Timing of Intervention in Patients with Acute Coronary Syndromes (TIMACS) AHA, 2008
Background For UA/NSTEMI pts that are treated with an invasive strategy, the timing of catheterization has not been rigorously investigated.
TIMACS: Methods Pts with UA/NSTEMI randomized to early invasive strategy (angiography within 24 hrs) or delayed invasive strategy (angiography any time after 36 hrs). Primary endpoint: - composite of death, new MI, or CVA at 6 months. Secondary endpoints: - death, new MI, or refractory ischemia - death, new MI, CVA, refractory ischemia, repeat revascularization - CVA
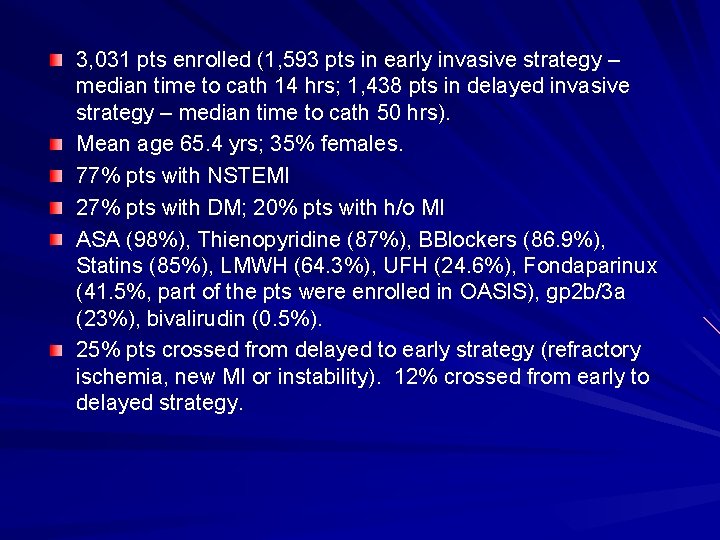
3, 031 pts enrolled (1, 593 pts in early invasive strategy – median time to cath 14 hrs; 1, 438 pts in delayed invasive strategy – median time to cath 50 hrs). Mean age 65. 4 yrs; 35% females. 77% pts with NSTEMI 27% pts with DM; 20% pts with h/o MI ASA (98%), Thienopyridine (87%), BBlockers (86. 9%), Statins (85%), LMWH (64. 3%), UFH (24. 6%), Fondaparinux (41. 5%, part of the pts were enrolled in OASIS), gp 2 b/3 a (23%), bivalirudin (0. 5%). 25% pts crossed from delayed to early strategy (refractory ischemia, new MI or instability). 12% crossed from early to delayed strategy.
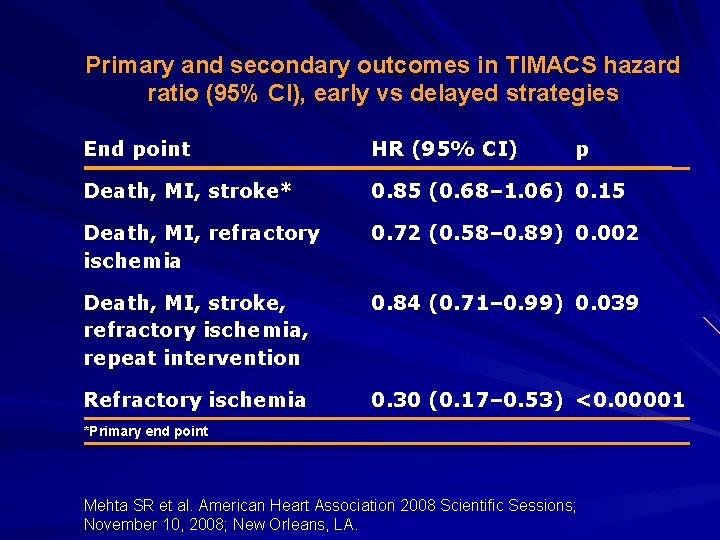
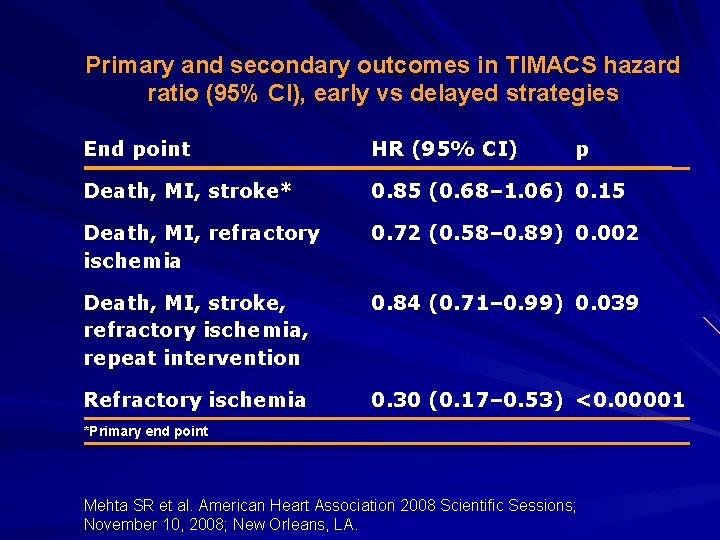
Primary and secondary outcomes in TIMACS hazard ratio (95% CI), early vs delayed strategies End point HR (95% CI) p Death, MI, stroke* 0. 85 (0. 68– 1. 06) 0. 15 Death, MI, refractory ischemia 0. 72 (0. 58– 0. 89) 0. 002 Death, MI, stroke, refractory ischemia, repeat intervention 0. 84 (0. 71– 0. 99) 0. 039 Refractory ischemia 0. 30 (0. 17– 0. 53) <0. 00001 *Primary end point Mehta SR et al. American Heart Association 2008 Scientific Sessions; November 10, 2008; New Orleans, LA.
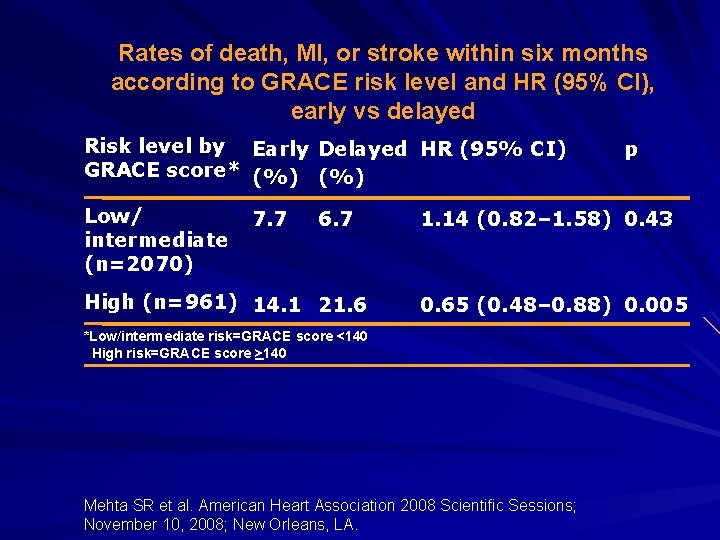
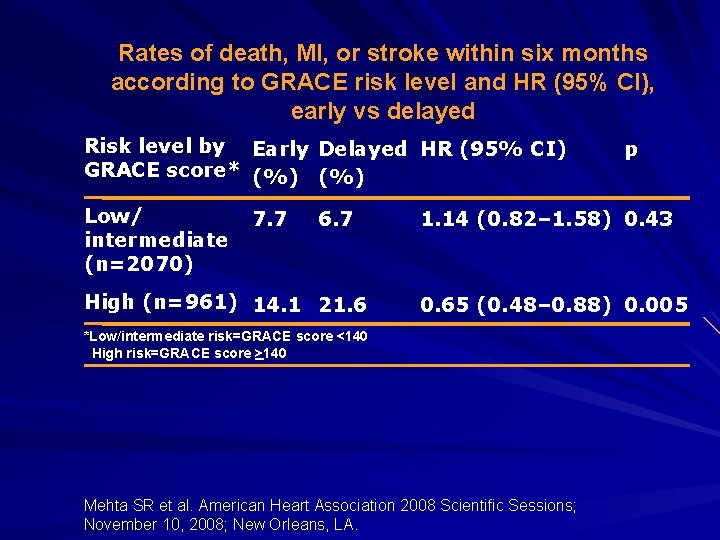
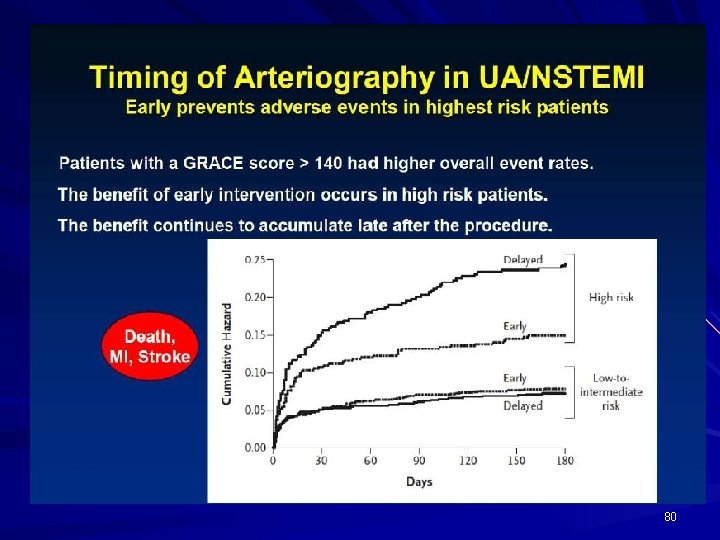
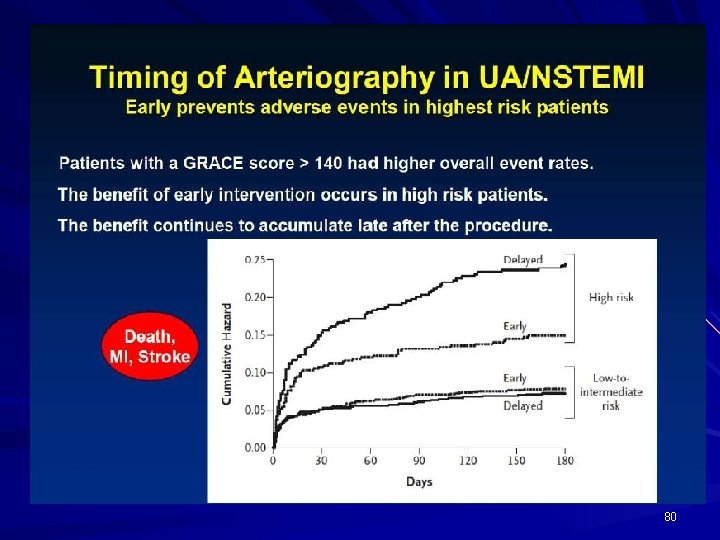
Rates of death, MI, or stroke within six months according to GRACE risk level and HR (95% CI), early vs delayed Risk level by Early Delayed HR (95% CI) GRACE score* (%) Low/ intermediate (n=2070) 7. 7 6. 7 High (n=961) 14. 1 21. 6 p 1. 14 (0. 82– 1. 58) 0. 43 0. 65 (0. 48– 0. 88) 0. 005 *Low/intermediate risk=GRACE score <140 High risk=GRACE score >140 Mehta SR et al. American Heart Association 2008 Scientific Sessions; November 10, 2008; New Orleans, LA.
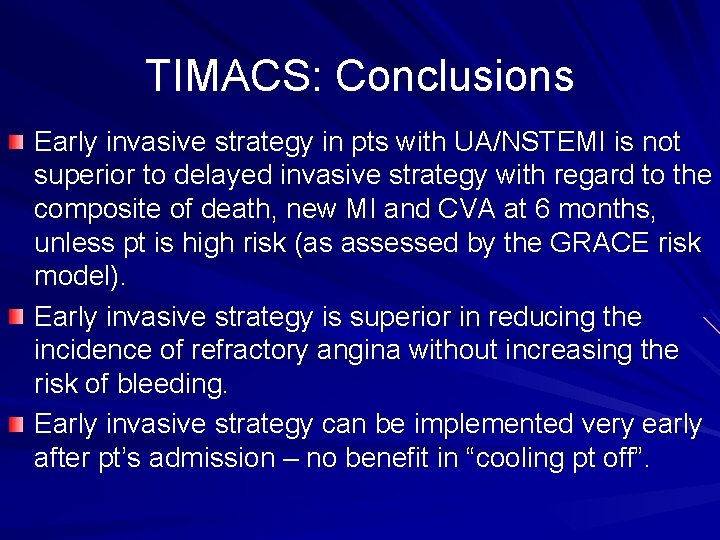
TIMACS: Conclusions Early invasive strategy in pts with UA/NSTEMI is not superior to delayed invasive strategy with regard to the composite of death, new MI and CVA at 6 months, unless pt is high risk (as assessed by the GRACE risk model). Early invasive strategy is superior in reducing the incidence of refractory angina without increasing the risk of bleeding. Early invasive strategy can be implemented very early after pt’s admission – no benefit in “cooling pt off”.
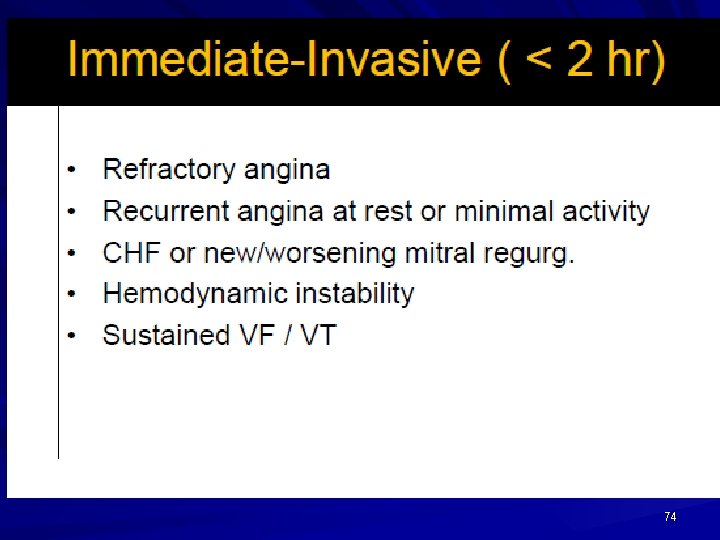
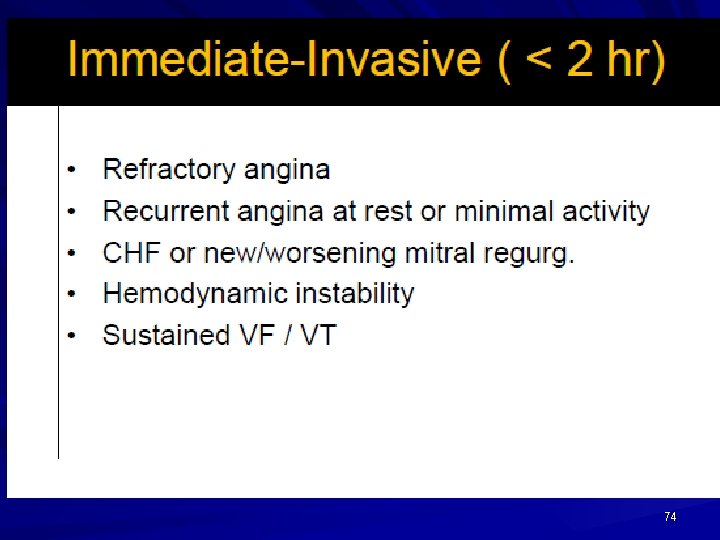
74
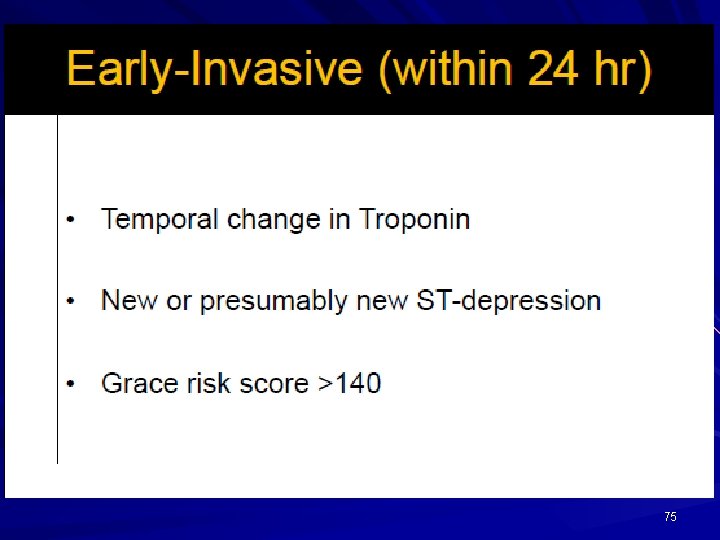
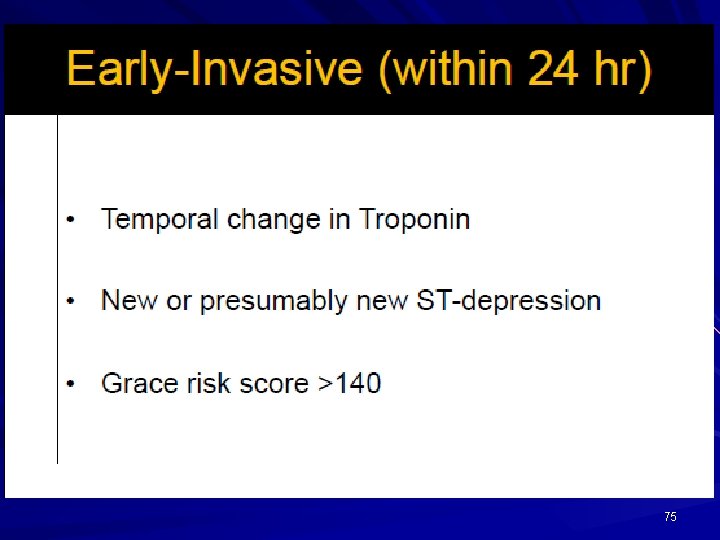
75
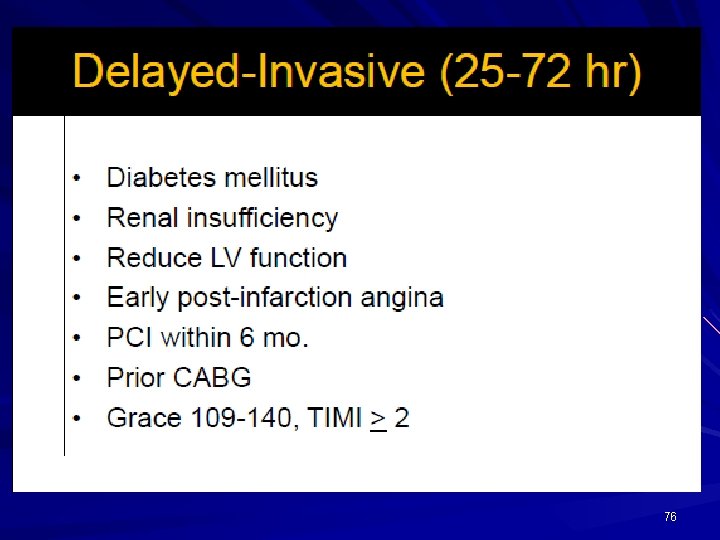
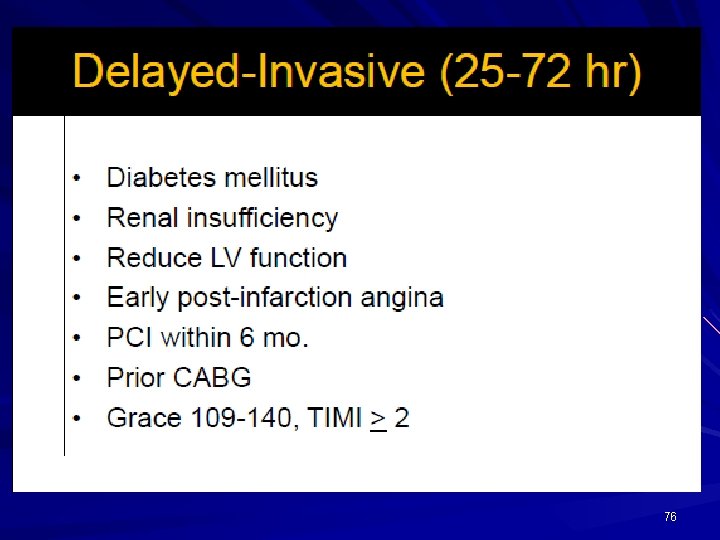
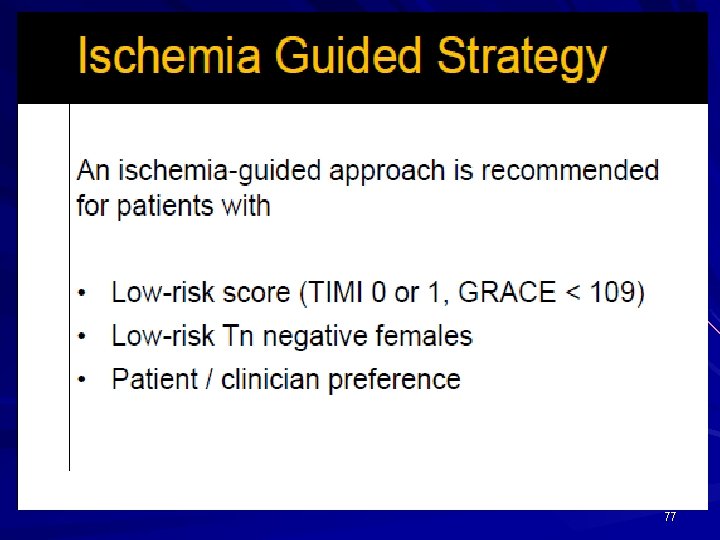
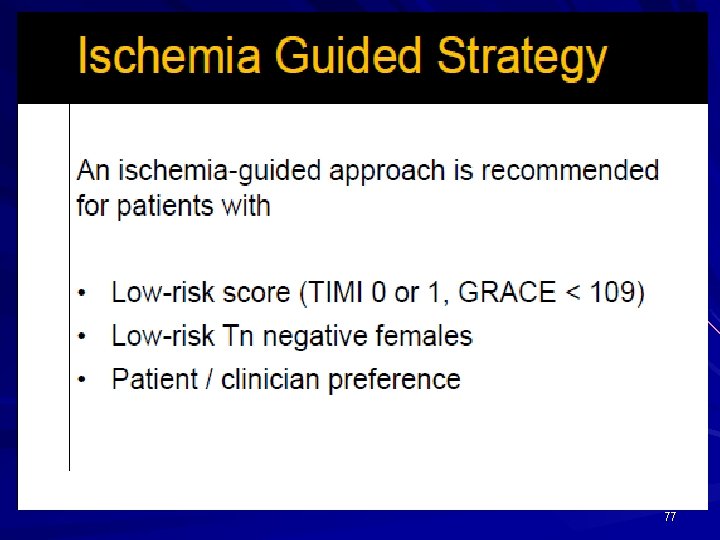
76
77
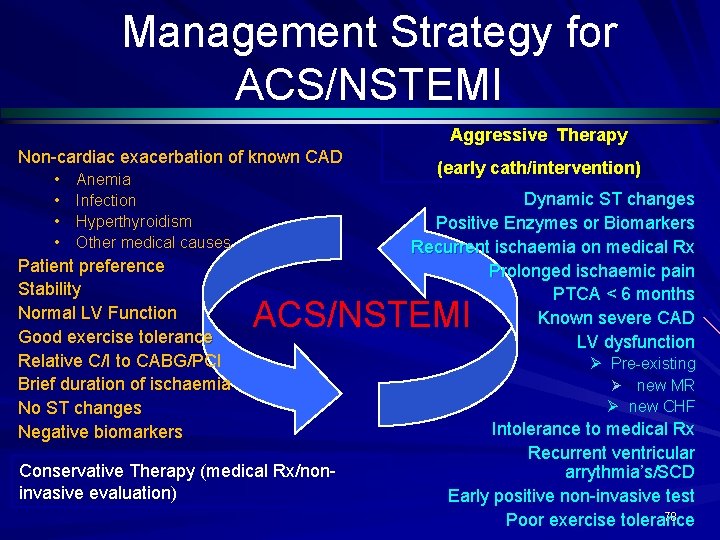
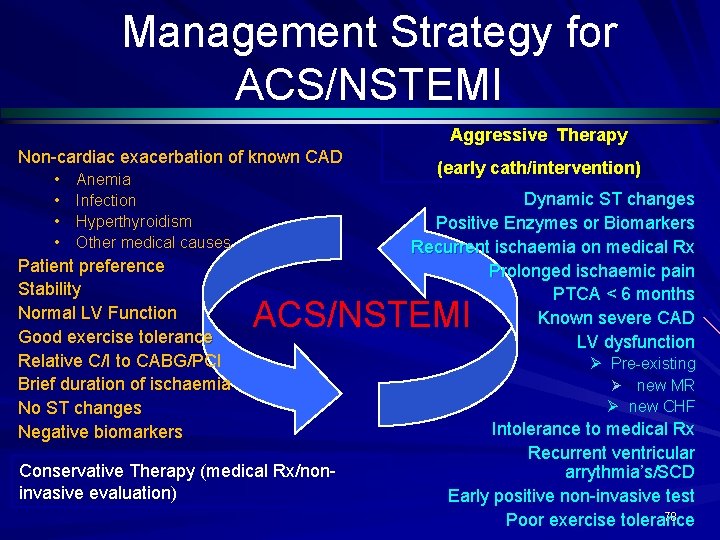
Management Strategy for ACS/NSTEMI Aggressive Therapy Non-cardiac exacerbation of known CAD • • Anemia Infection Hyperthyroidism Other medical causes Patient preference Stability Normal LV Function Good exercise tolerance Relative C/I to CABG/PCI Brief duration of ischaemia No ST changes Negative biomarkers (early cath/intervention) Dynamic ST changes Positive Enzymes or Biomarkers Recurrent ischaemia on medical Rx Prolonged ischaemic pain PTCA < 6 months Known severe CAD LV dysfunction ACS/NSTEMI Conservative Therapy (medical Rx/noninvasive evaluation) Ø Pre-existing Ø new MR Ø new CHF Intolerance to medical Rx Recurrent ventricular arrythmia’s/SCD Early positive non-invasive test 78 Poor exercise tolerance
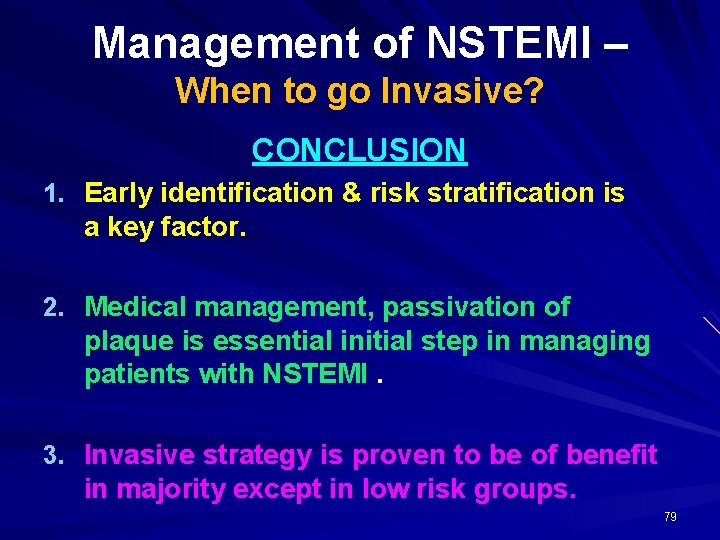
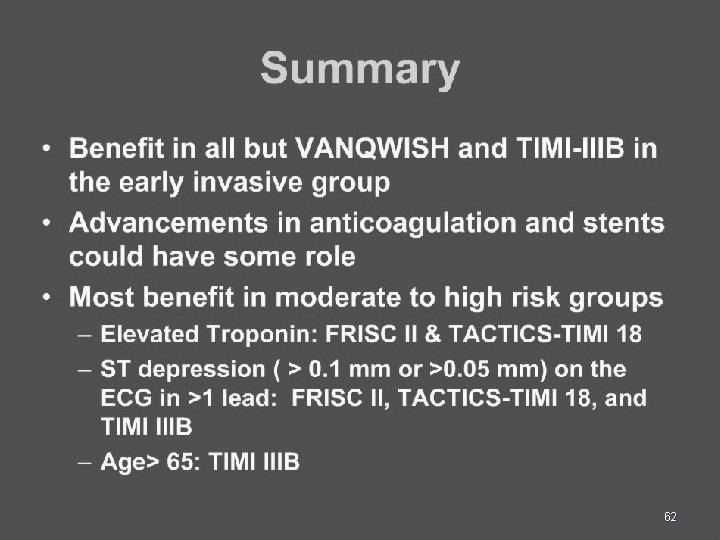
Management of NSTEMI – When to go Invasive? CONCLUSION 1. Early identification & risk stratification is a key factor. 2. Medical management, passivation of plaque is essential initial step in managing patients with NSTEMI. 3. Invasive strategy is proven to be of benefit in majority except in low risk groups. 79
80
THANK YOU 81