Inflammation Coagulation Dr Rex Lam ICU Friday Seminar



- Slides: 40
Inflammation & Coagulation Dr Rex Lam ICU Friday Seminar PYNEH 21 st July, 2006
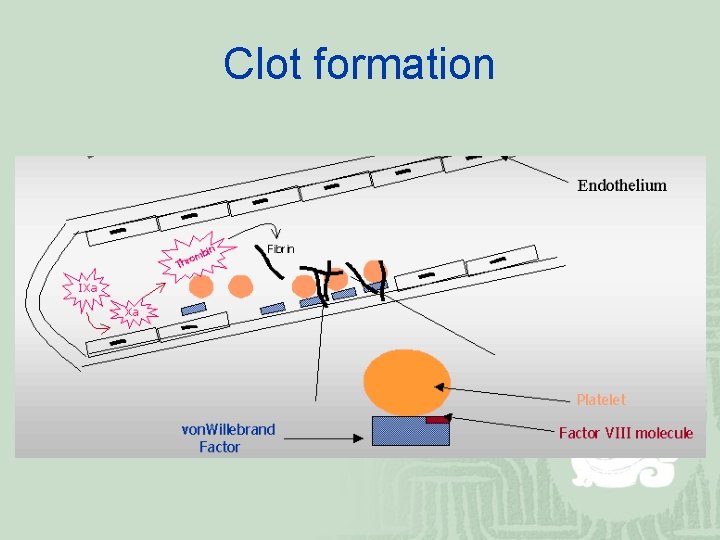
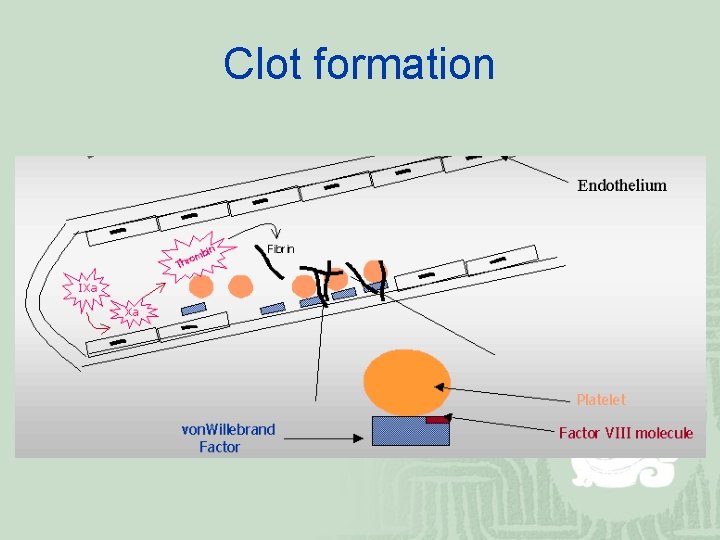
Clot formation
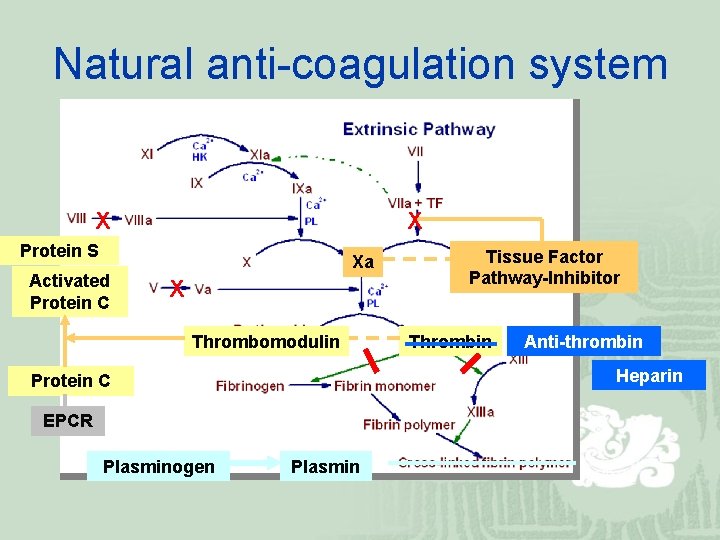
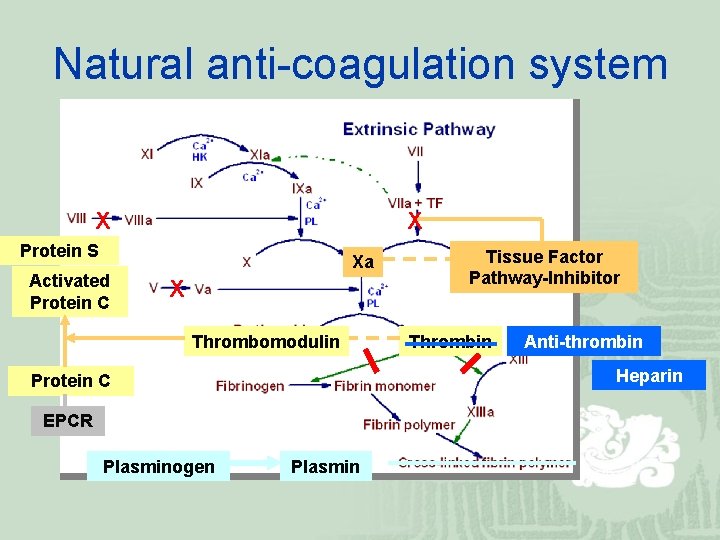
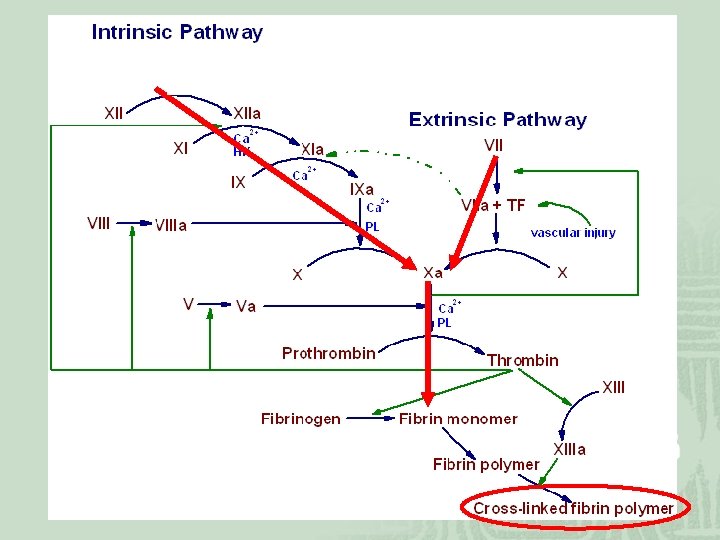
Natural anti-coagulation system X X Protein S Activated Protein C Xa X Thrombomodulin Thrombin Anti-thrombin Heparin Protein C EPCR Plasminogen Tissue Factor Pathway-Inhibitor Plasmin
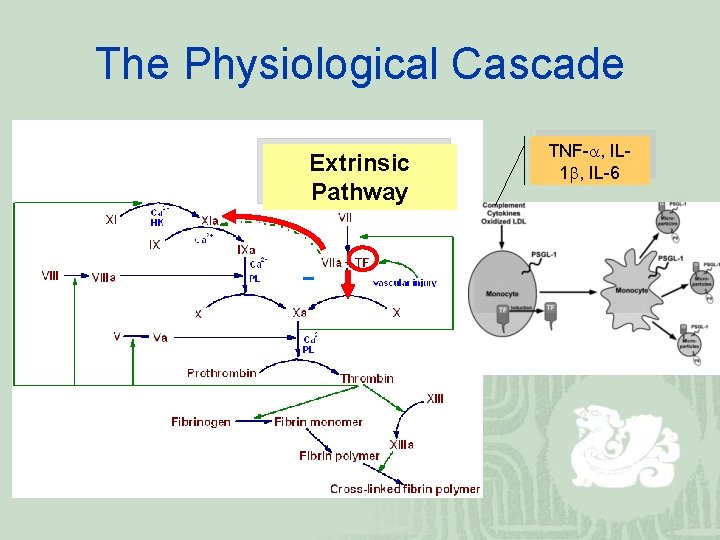
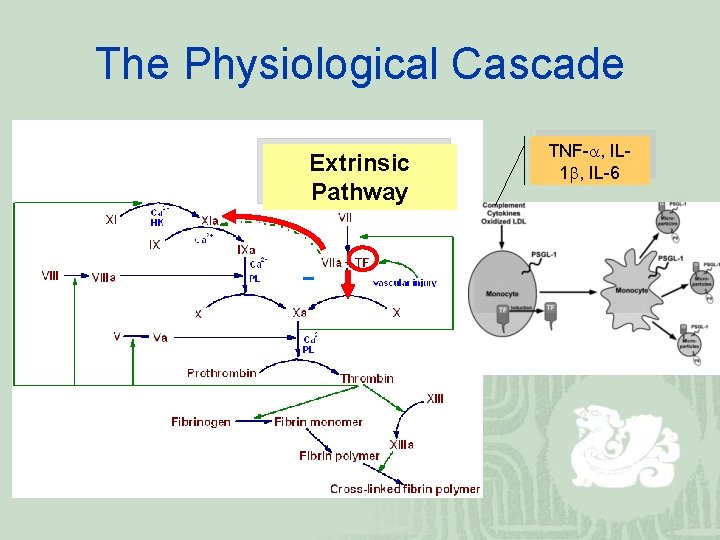
The Physiological Cascade Extrinsic Pathway TNF- , IL 1 , IL-6
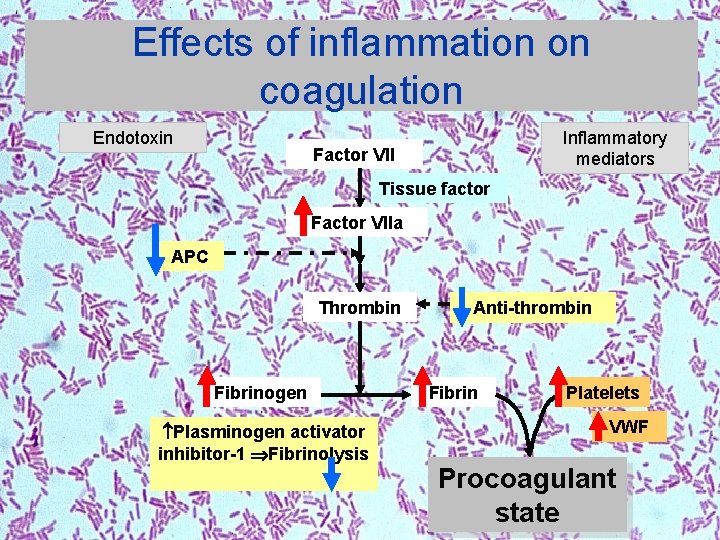
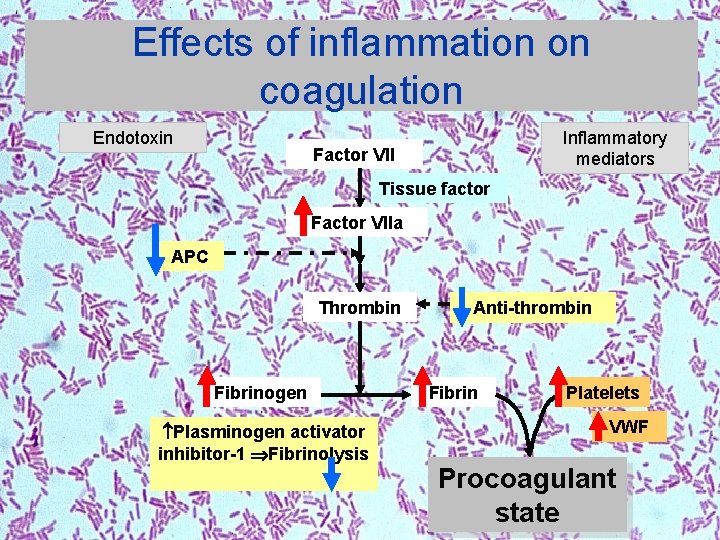
Effects of inflammation on coagulation Endotoxin Inflammatory mediators Factor VII Tissue factor Factor VIIa APC Thrombin Fibrinogen Plasminogen activator inhibitor-1 Fibrinolysis Anti-thrombin Fibrin Platelets VWF Procoagulant state
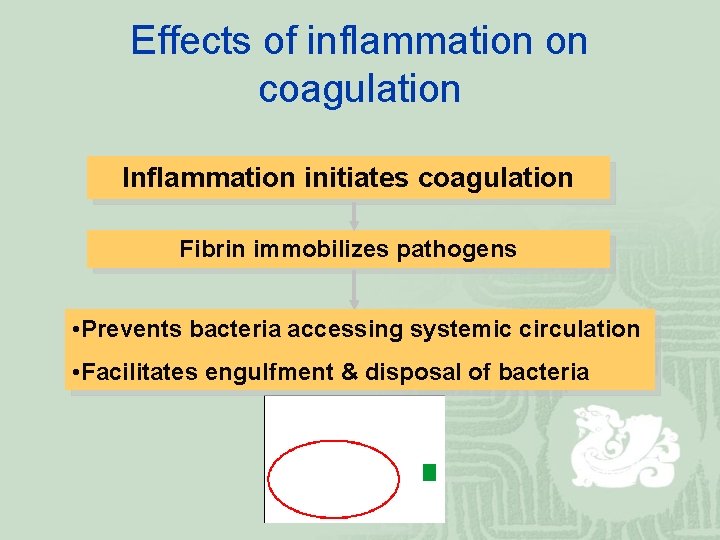
Effects of inflammation on coagulation Inflammation initiates coagulation Fibrin immobilizes pathogens • Prevents bacteria accessing systemic circulation • Facilitates engulfment & disposal of bacteria
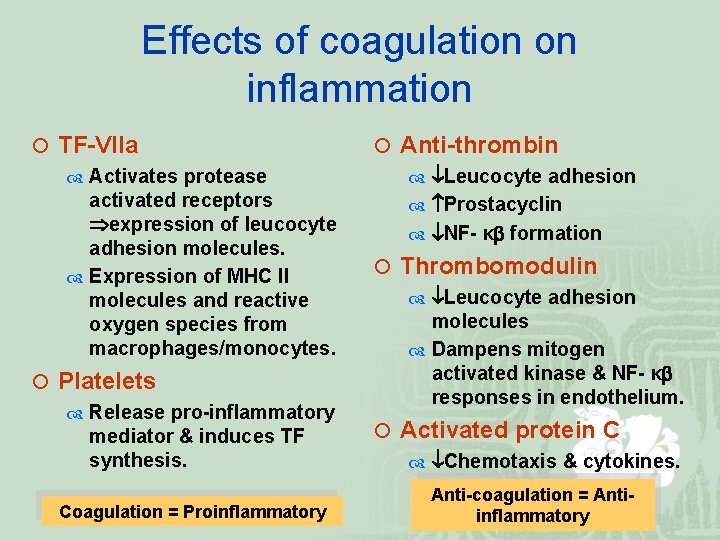
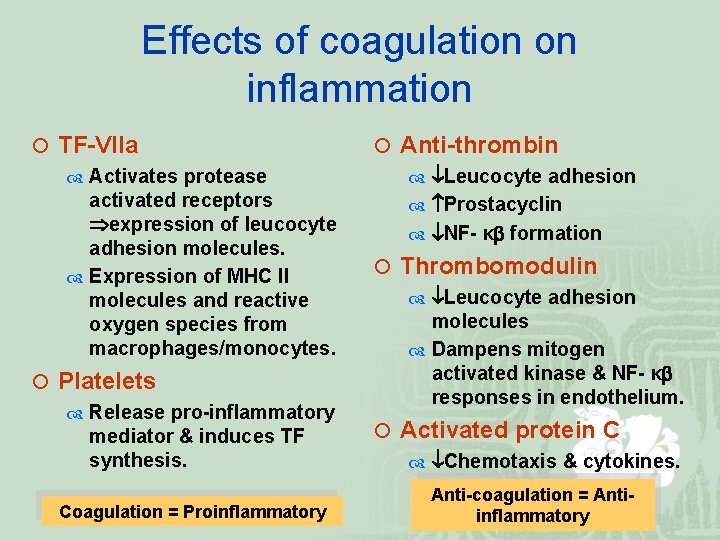
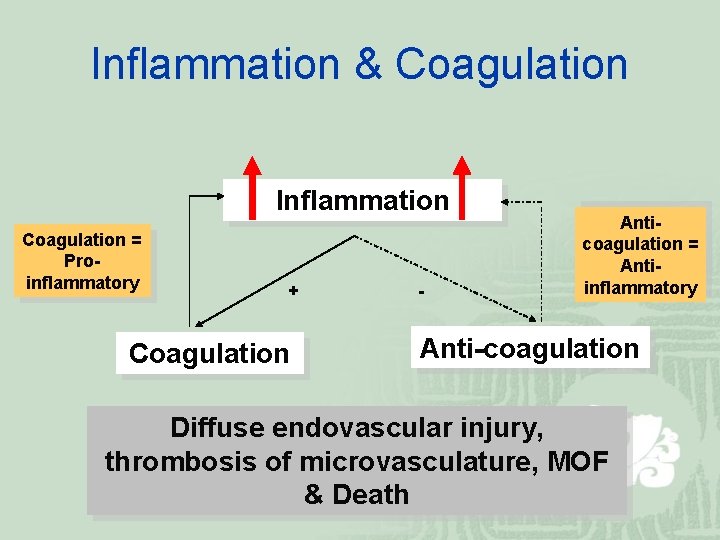
Effects of coagulation on inflammation ¡ TF-VIIa Activates protease activated receptors expression of leucocyte adhesion molecules. Expression of MHC II molecules and reactive oxygen species from macrophages/monocytes. ¡ Platelets Release pro-inflammatory mediator & induces TF synthesis. Coagulation = Proinflammatory ¡ Anti-thrombin Leucocyte adhesion Prostacyclin NF- κ formation ¡ Thrombomodulin Leucocyte adhesion molecules Dampens mitogen activated kinase & NF- κ responses in endothelium. ¡ Activated protein C Chemotaxis & cytokines. Anti-coagulation = Antiinflammatory
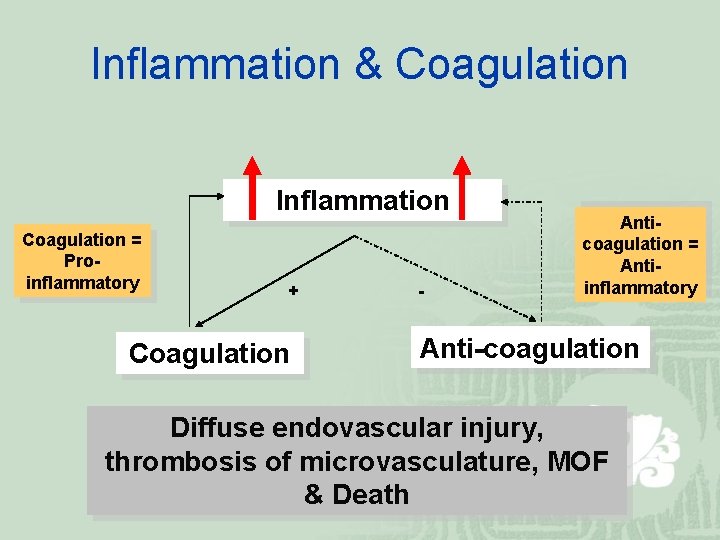
Inflammation & Coagulation Inflammation Coagulation = Proinflammatory + Coagulation - Anticoagulation = Antiinflammatory Anti-coagulation Diffuse endovascular injury, thrombosis of microvasculature, MOF & Death
Sepsis ¡ Despite improvements in standards of care & antibiotic therapy, sepsis still remains the commonest cause of death among hospitalized patients in non-cardiac ICUs. ¡ Mortality of severe sepsis 30 -50%.
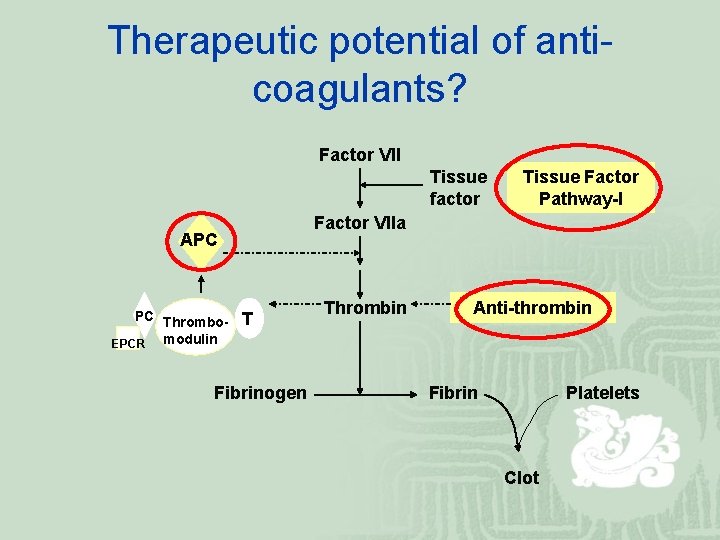
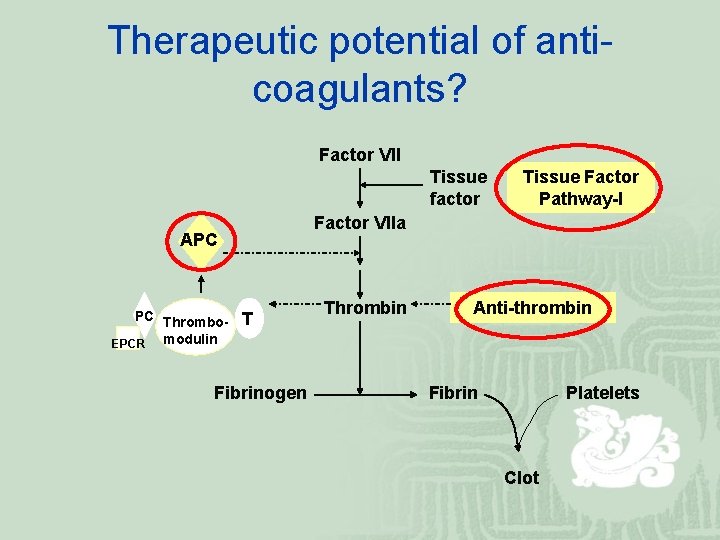
Therapeutic potential of anticoagulants? Factor VII Tissue factor Factor VIIa APC PC Thrombo. EPCR modulin Tissue Factor Pathway-I T Fibrinogen Thrombin Anti-thrombin Fibrin Platelets Clot
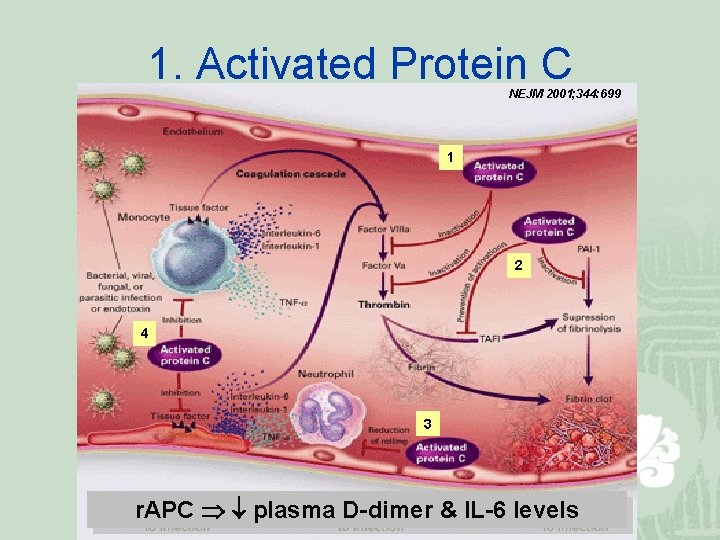
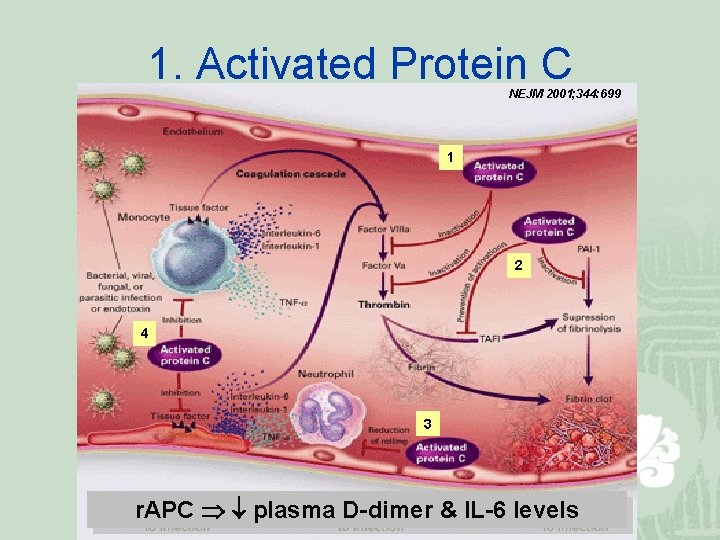
1. Activated Protein C NEJM 2001; 344: 699 1 2 4 3 APC r. APC during sepsis plasma&D-dimer associated & IL-6 with levels death.
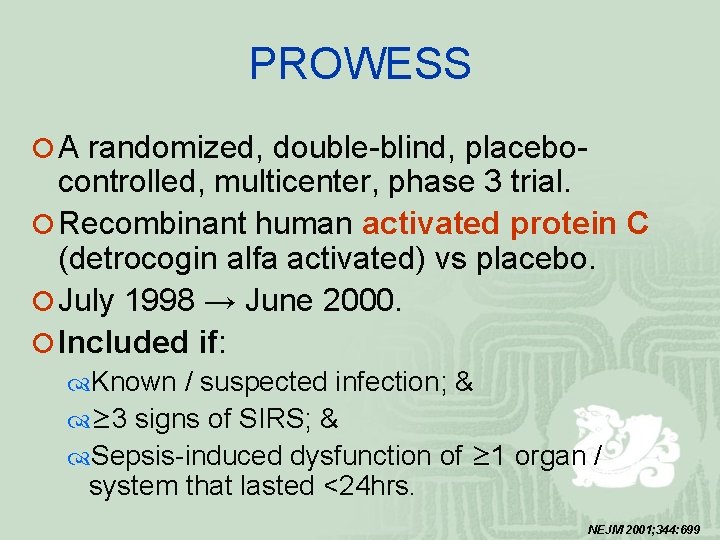
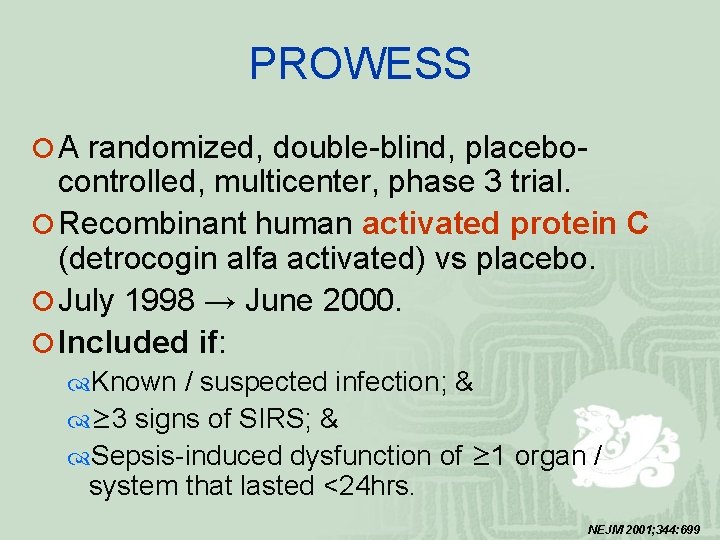
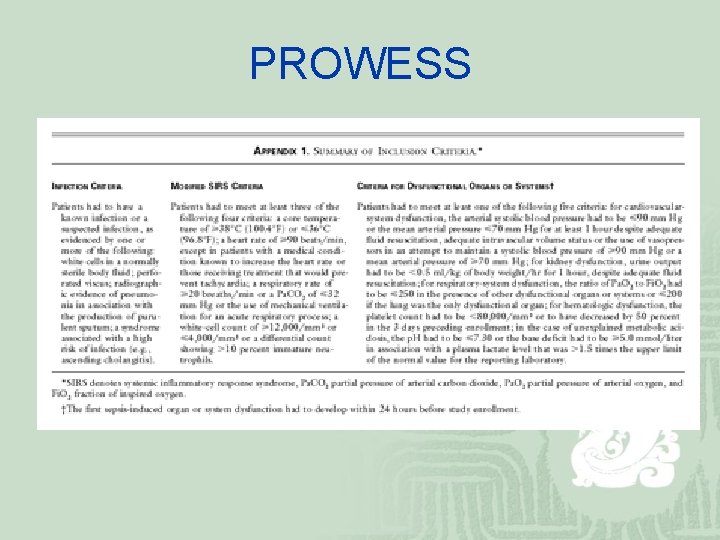
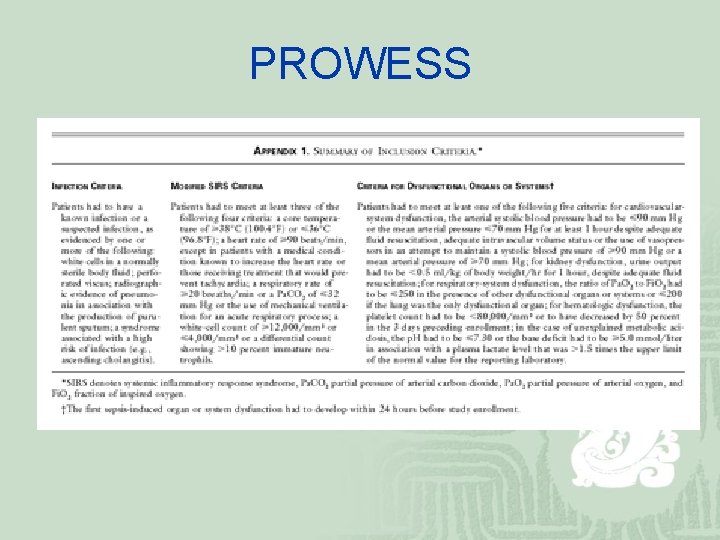
PROWESS ¡ A randomized, double-blind, placebo- controlled, multicenter, phase 3 trial. ¡ Recombinant human activated protein C (detrocogin alfa activated) vs placebo. ¡ July 1998 → June 2000. ¡ Included if: Known / suspected infection; & ≥ 3 signs of SIRS; & Sepsis-induced dysfunction of ≥ 1 organ / system that lasted <24 hrs. NEJM 2001; 344: 699
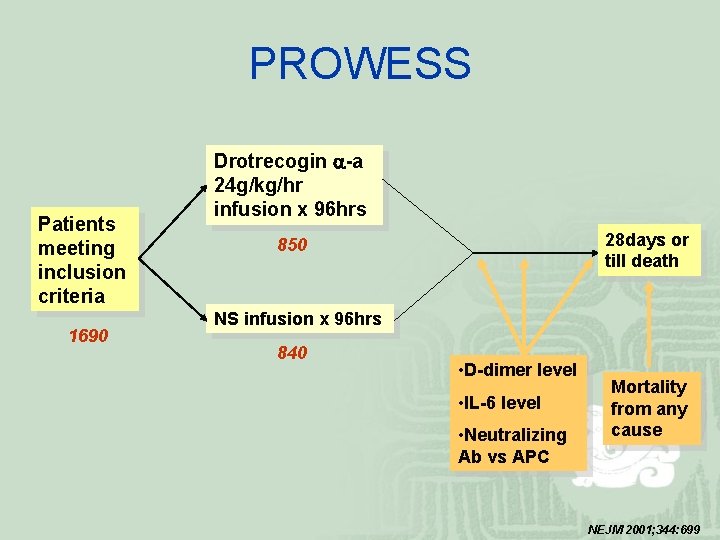
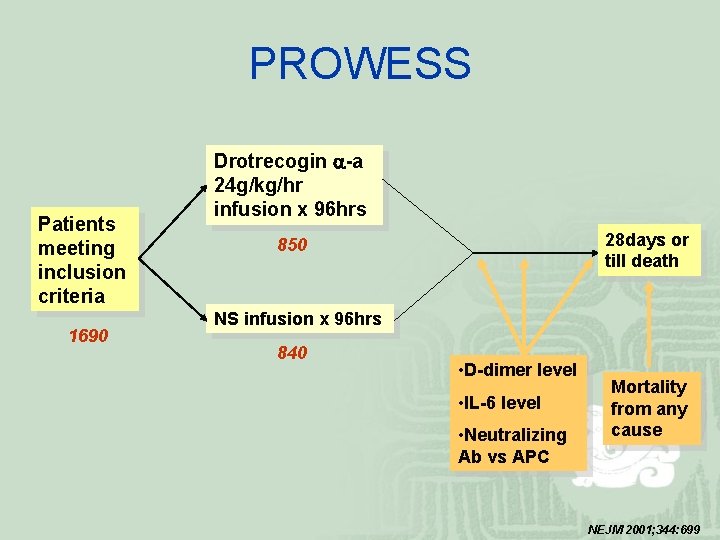
PROWESS Patients meeting inclusion criteria 1690 Drotrecogin -a 24 g/kg/hr infusion x 96 hrs 28 days or till death 850 NS infusion x 96 hrs 840 • D-dimer level • IL-6 level • Neutralizing Ab vs APC Mortality from any cause NEJM 2001; 344: 699
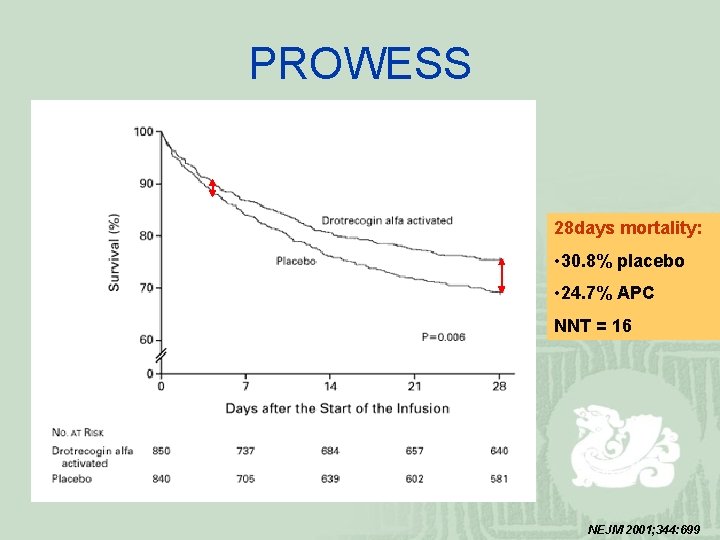
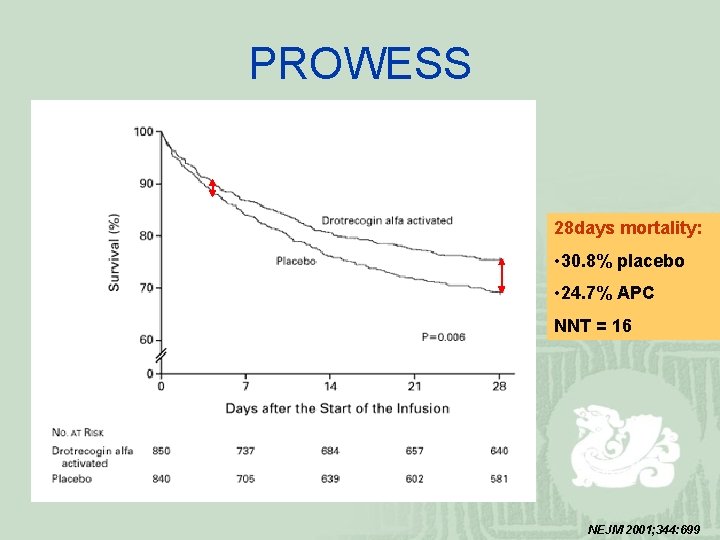
PROWESS 28 days mortality: • 30. 8% placebo • 24. 7% APC NNT = 16 NEJM 2001; 344: 699

PROWESS In November 2001, FDA approved Drot. AA for adults with severe sepsis & a high risk of death i. e. APACHE ≥ 25 or MOF Neutralizing Ab vs APC was not detected in any patient. NEJM 2001; 344: 699
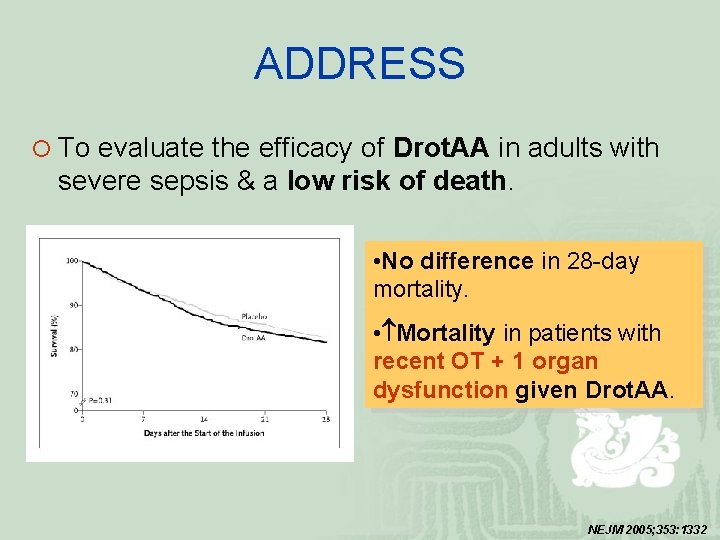
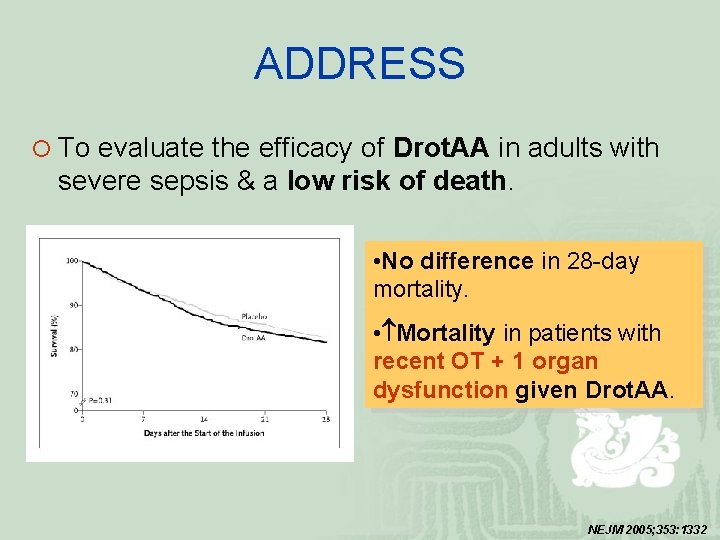
ADDRESS ¡ To evaluate the efficacy of Drot. AA in adults with severe sepsis & a low risk of death. • No difference in 28 -day mortality. • Mortality in patients with recent OT + 1 organ dysfunction given Drot. AA. NEJM 2005; 353: 1332
2. Anti-thrombin III
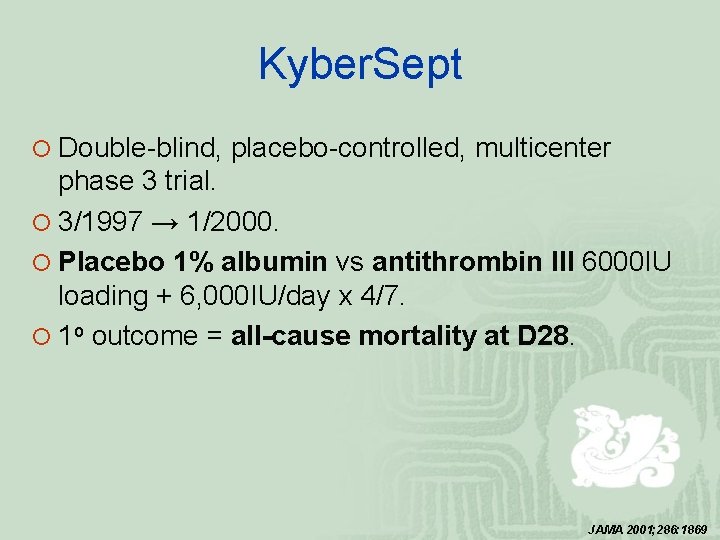
Kyber. Sept ¡ Double-blind, placebo-controlled, multicenter phase 3 trial. ¡ 3/1997 → 1/2000. ¡ Placebo 1% albumin vs antithrombin III 6000 IU loading + 6, 000 IU/day x 4/7. ¡ 1 o outcome = all-cause mortality at D 28. JAMA 2001; 286: 1869
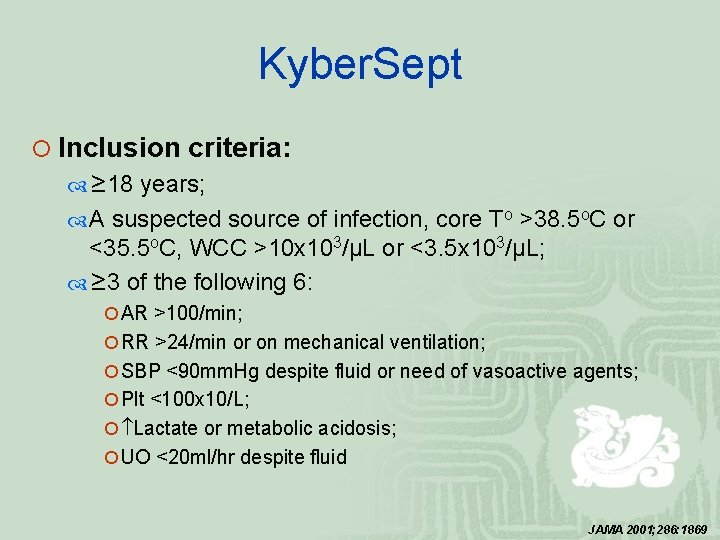
Kyber. Sept ¡ Inclusion criteria: ≥ 18 years; A suspected source of infection, core To >38. 5 o. C or <35. 5 o. C, WCC >10 x 103/μL or <3. 5 x 103/μL; ≥ 3 of the following 6: ¡ AR >100/min; ¡ RR >24/min or on mechanical ventilation; ¡ SBP <90 mm. Hg despite fluid or need of vasoactive agents; ¡ Plt <100 x 10/L; ¡ Lactate or metabolic acidosis; ¡ UO <20 ml/hr despite fluid JAMA 2001; 286: 1869
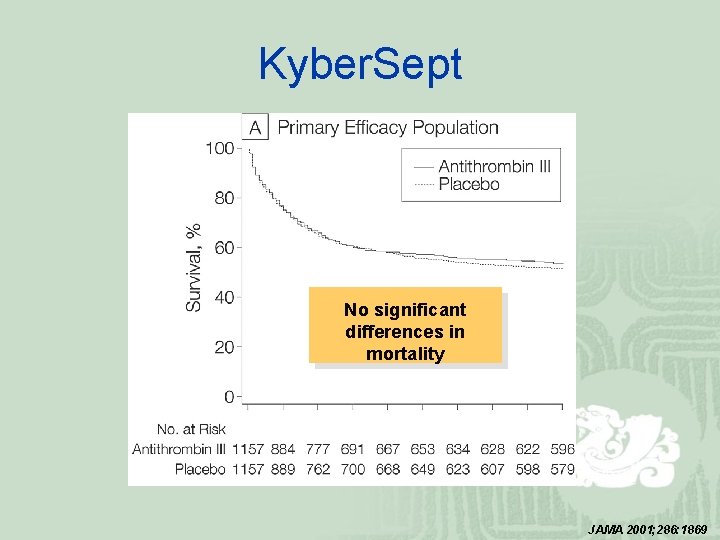
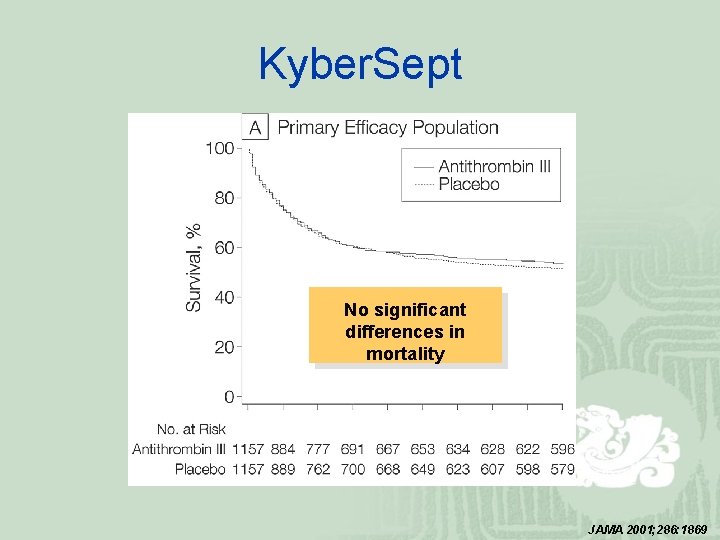
Kyber. Sept No significant differences in mortality JAMA 2001; 286: 1869
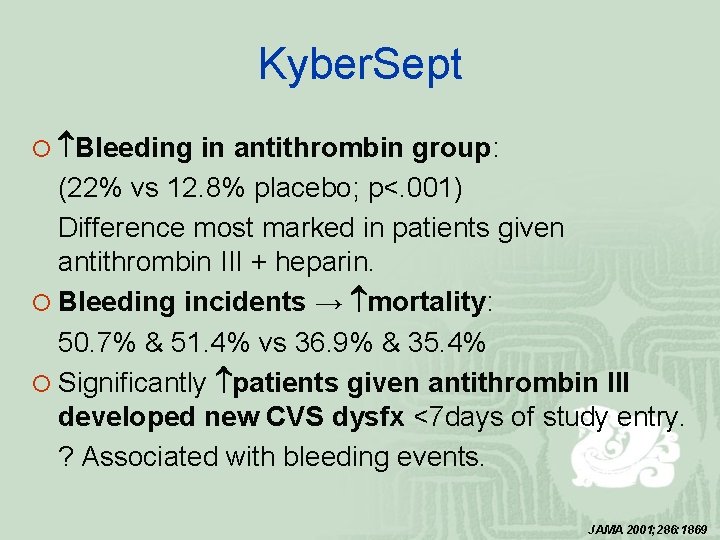
Kyber. Sept ¡ Bleeding in antithrombin group: (22% vs 12. 8% placebo; p<. 001) Difference most marked in patients given antithrombin III + heparin. ¡ Bleeding incidents → mortality: 50. 7% & 51. 4% vs 36. 9% & 35. 4% ¡ Significantly patients given antithrombin III developed new CVS dysfx <7 days of study entry. ? Associated with bleeding events. JAMA 2001; 286: 1869
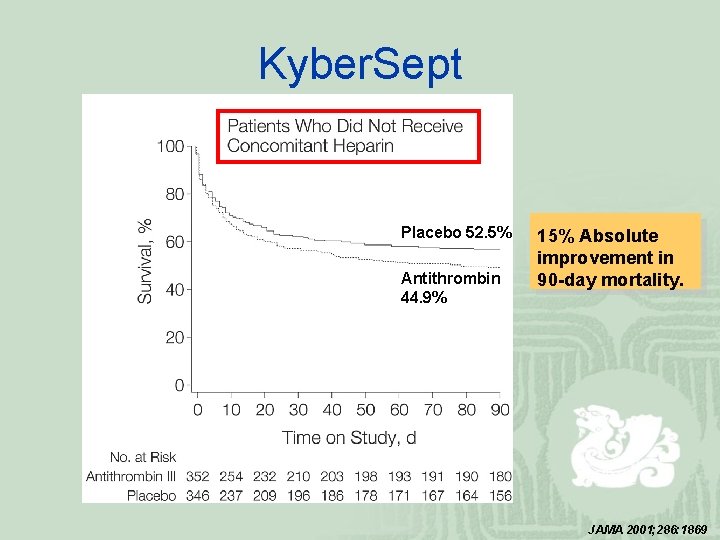
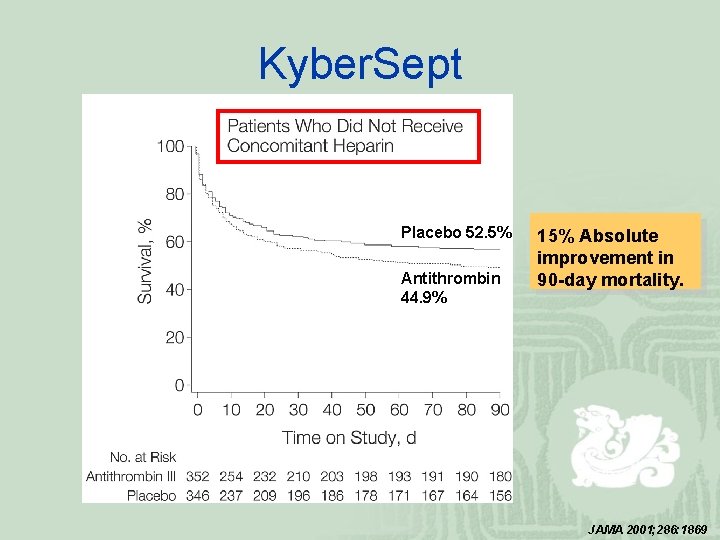
Kyber. Sept Placebo 52. 5% Antithrombin 44. 9% 15% Absolute improvement in 90 -day mortality. JAMA 2001; 286: 1869
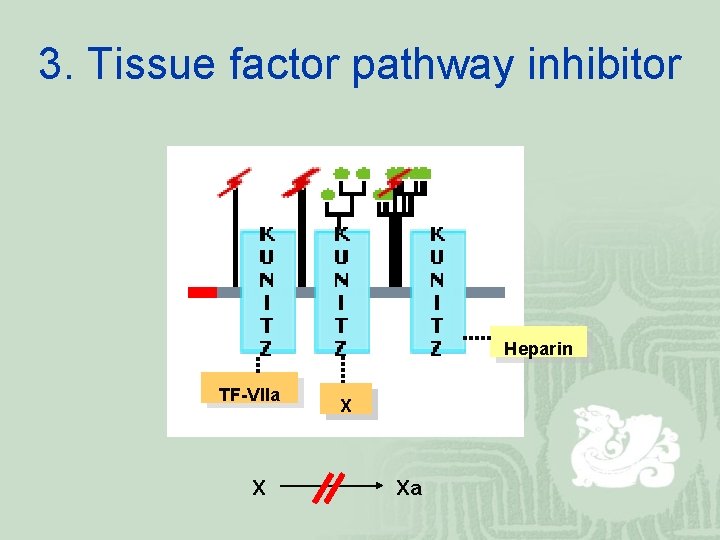
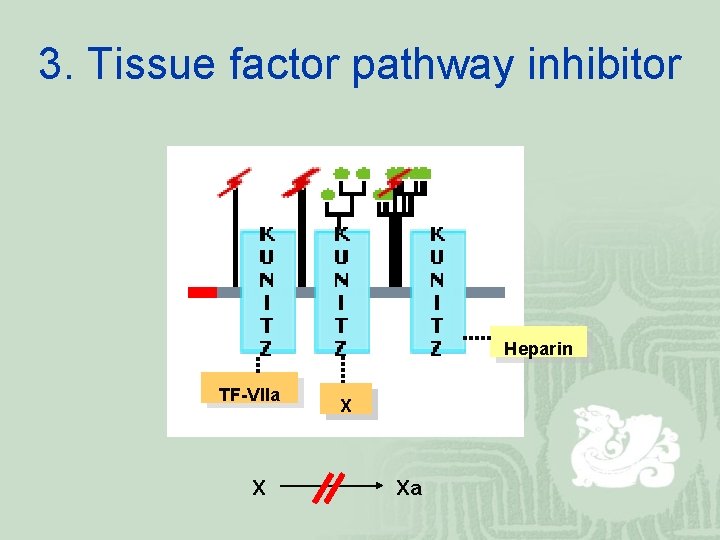
3. Tissue factor pathway inhibitor Heparin TF-VIIa X Xa
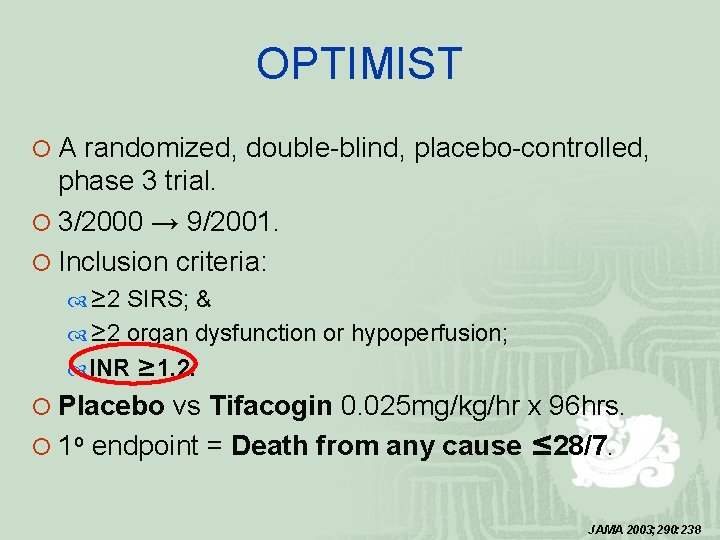
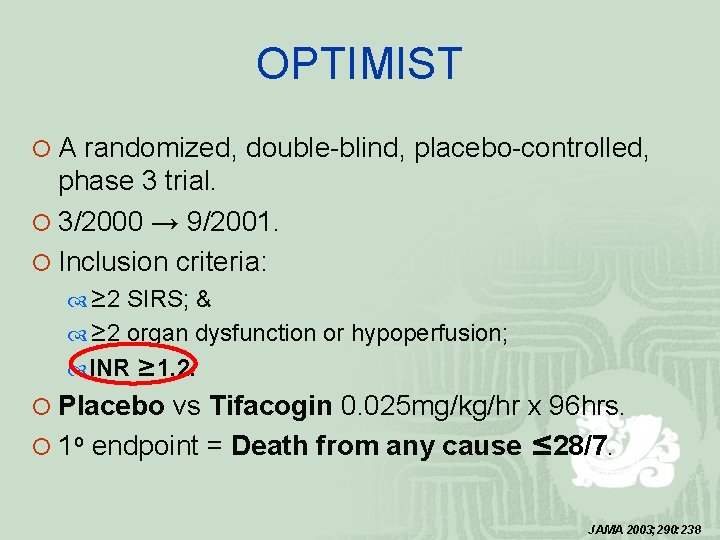
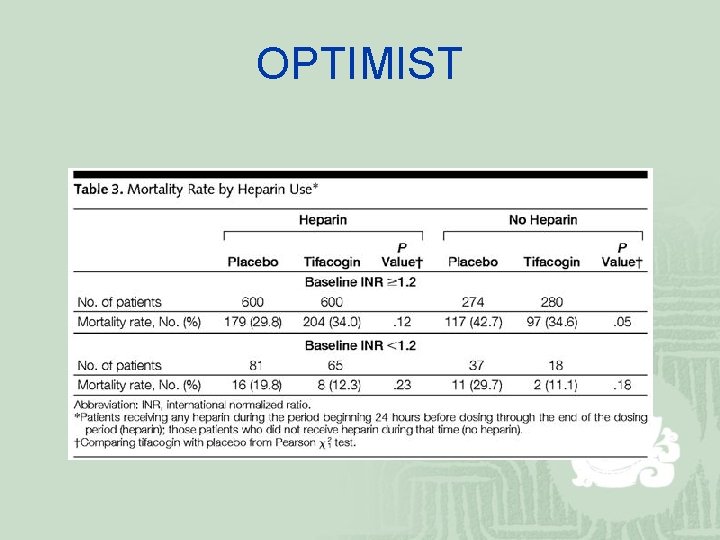
OPTIMIST ¡ A randomized, double-blind, placebo-controlled, phase 3 trial. ¡ 3/2000 → 9/2001. ¡ Inclusion criteria: ≥ 2 SIRS; & ≥ 2 organ dysfunction or hypoperfusion; INR ≥ 1. 2. ¡ Placebo vs Tifacogin 0. 025 mg/kg/hr x 96 hrs. ¡ 1 o endpoint = Death from any cause ≤ 28/7. JAMA 2003; 290: 238
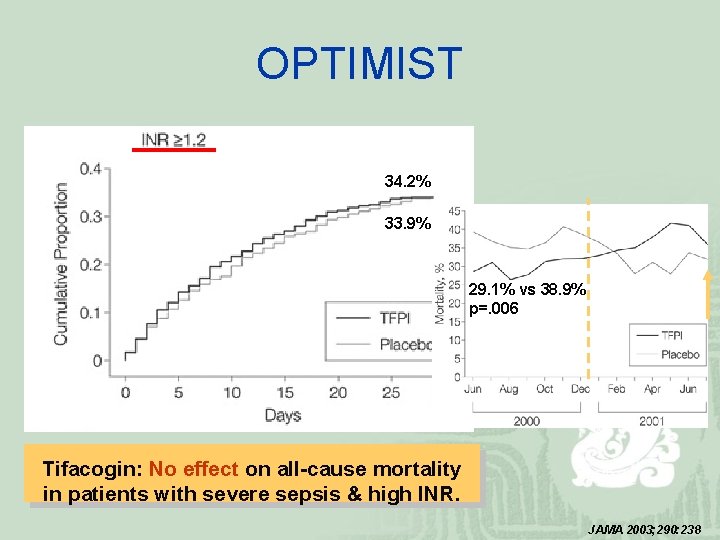
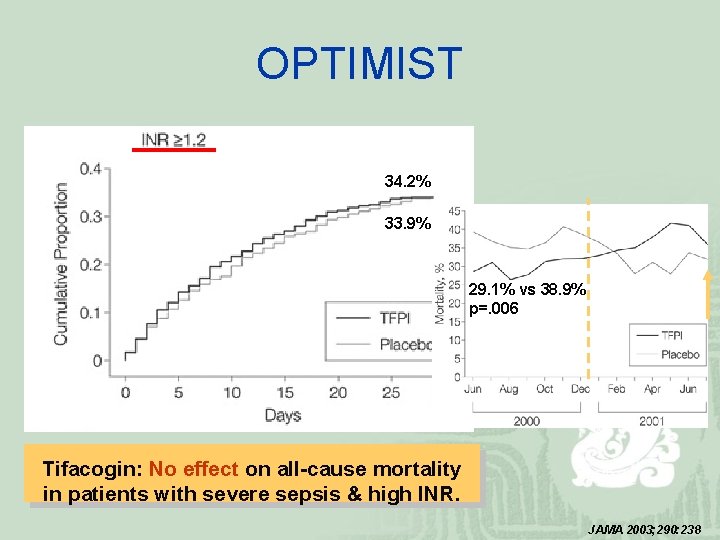
OPTIMIST 34. 2% 33. 9% 29. 1% vs 38. 9% p=. 006 Tifacogin: No effect on all-cause mortality in patients with severe sepsis & high INR. JAMA 2003; 290: 238
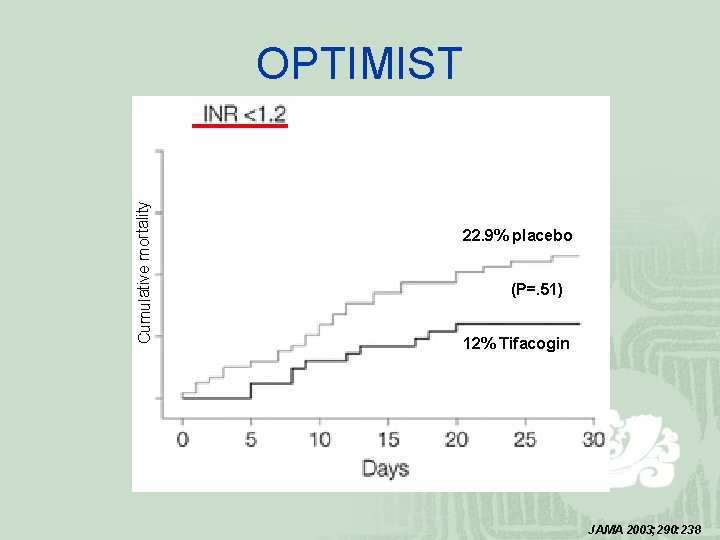
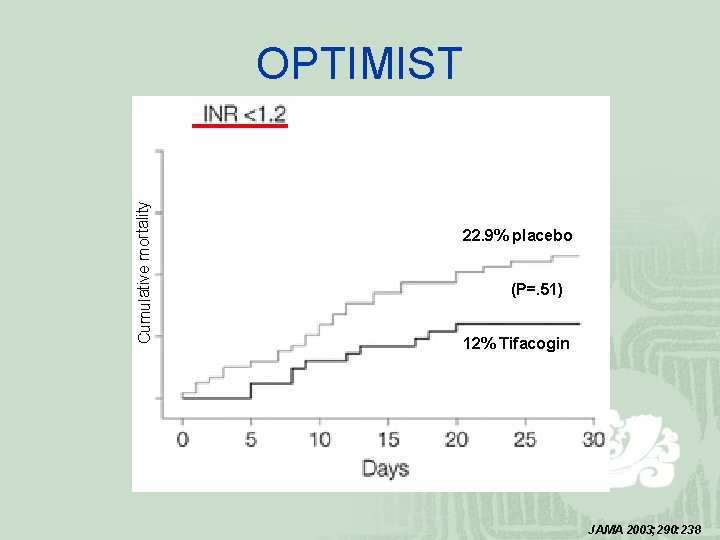
Cumulative mortality OPTIMIST 22. 9% placebo (P=. 51) 12% Tifacogin JAMA 2003; 290: 238
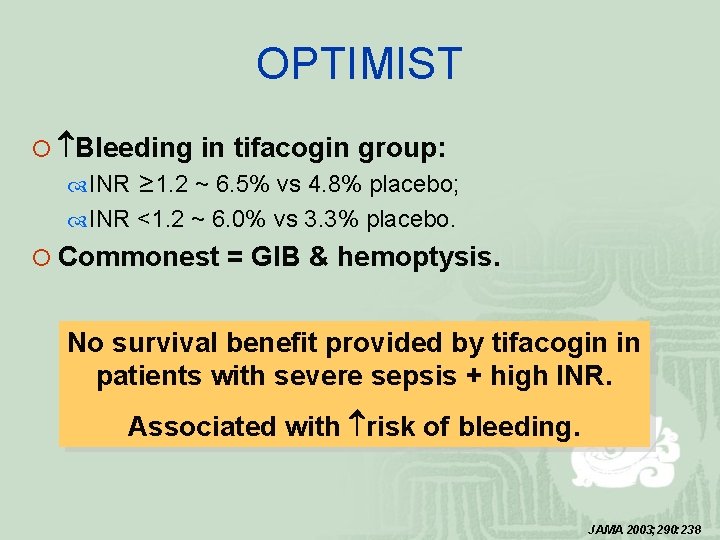
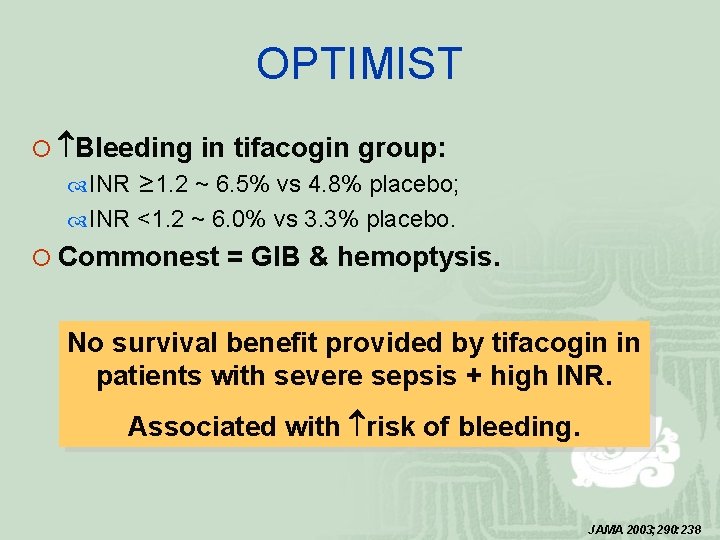
OPTIMIST ¡ Bleeding in tifacogin group: INR ≥ 1. 2 ~ 6. 5% vs 4. 8% placebo; INR <1. 2 ~ 6. 0% vs 3. 3% placebo. ¡ Commonest = GIB & hemoptysis. No survival benefit provided by tifacogin in patients with severe sepsis + high INR. Associated with risk of bleeding. JAMA 2003; 290: 238
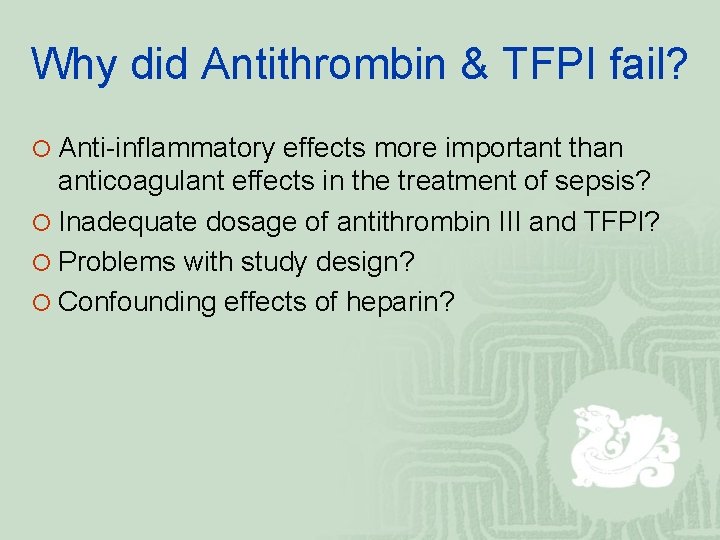
Why did Antithrombin & TFPI fail? ¡ Anti-inflammatory effects more important than anticoagulant effects in the treatment of sepsis? ¡ Inadequate dosage of antithrombin III and TFPI? ¡ Problems with study design? ¡ Confounding effects of heparin?
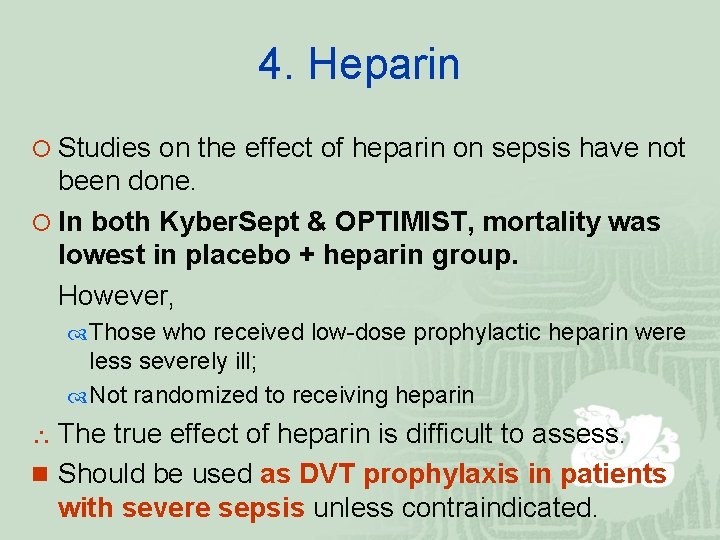
4. Heparin ¡ Studies on the effect of heparin on sepsis have not been done. ¡ In both Kyber. Sept & OPTIMIST, mortality was lowest in placebo + heparin group. However, Those who received low-dose prophylactic heparin were less severely ill; Not randomized to receiving heparin The true effect of heparin is difficult to assess. n Should be used as DVT prophylaxis in patients with severe sepsis unless contraindicated.
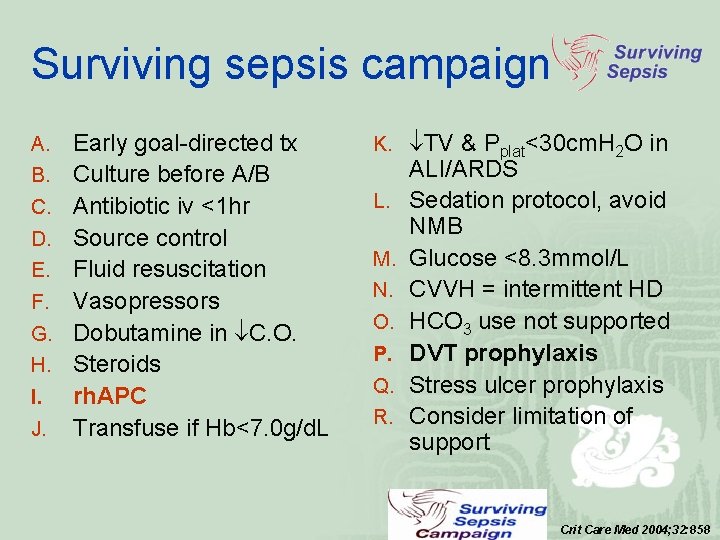
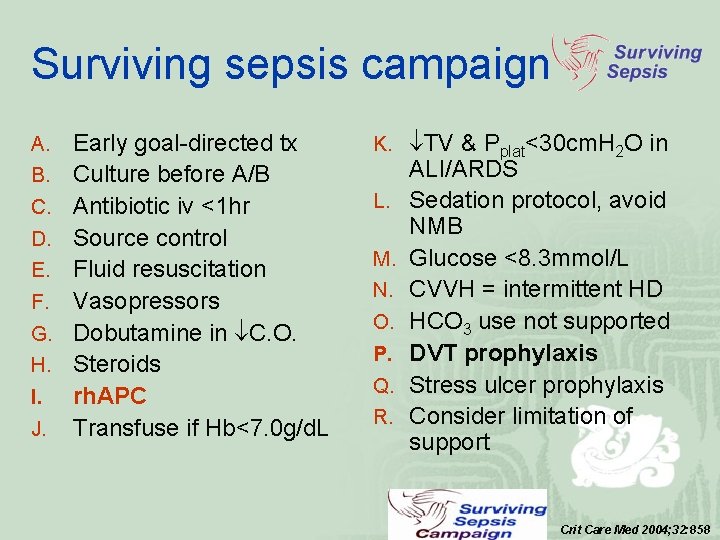
Surviving sepsis campaign A. B. C. D. E. F. G. H. I. J. Early goal-directed tx Culture before A/B Antibiotic iv <1 hr Source control Fluid resuscitation Vasopressors Dobutamine in C. O. Steroids rh. APC Transfuse if Hb<7. 0 g/d. L K. TV & Pplat<30 cm. H 2 O in L. M. N. O. P. Q. R. ALI/ARDS Sedation protocol, avoid NMB Glucose <8. 3 mmol/L CVVH = intermittent HD HCO 3 use not supported DVT prophylaxis Stress ulcer prophylaxis Consider limitation of support Crit Care Med 2004; 32: 858
Prevention of nosocomial infections ¡ Head tilt in ventilated patients; ¡ Appropriate stress ulcer prophylaxis; ¡ Sterile precautions during CVC insertion; ¡ Hand washing.
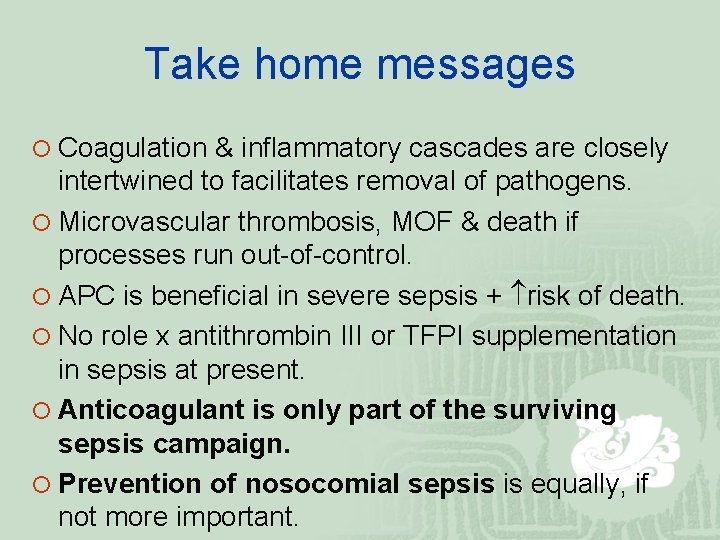
Take home messages ¡ Coagulation & inflammatory cascades are closely intertwined to facilitates removal of pathogens. ¡ Microvascular thrombosis, MOF & death if processes run out-of-control. ¡ APC is beneficial in severe sepsis + risk of death. ¡ No role x antithrombin III or TFPI supplementation in sepsis at present. ¡ Anticoagulant is only part of the surviving sepsis campaign. ¡ Prevention of nosocomial sepsis is equally, if not more important.
References ¡ Br J Haematol 2005; 131: 417 -430. ¡ Blood 2003; 101(10): 3765 -3777. ¡ NEJM 2001; 344(10): 699 -709. ¡ NEJM 2005; 353(13): 1332 -1341. ¡ JAMA 2003; 290(2): 238 -247. ¡ JAMA 2003; 290(2): 256 -258. ¡ JAMA 2001; 286(15): 1869 -1878. ¡ JAMA 2001; 286(15): 1894 -1896. ¡ Crit Care Med 2004; 32(3): 858 -873.
The end Thank you

PROWESS

PROWESS
2. Anti-thrombin III
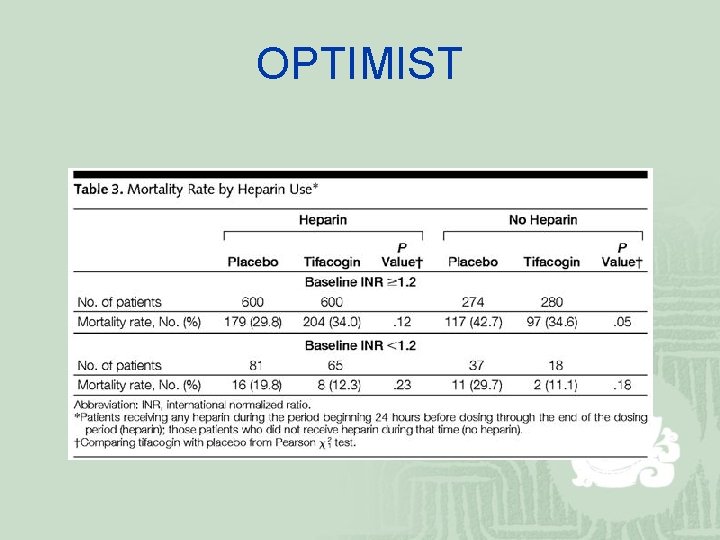
OPTIMIST