End of Life Care in the ICU Goals


- Slides: 29
End of Life Care in the ICU
Goals in Critical Care and Medicine • Save the lives of salvageable patients, restore health, relieve suffering and offer the dying a peaceful and dignified death. • Patients should expect excellence in all treatments, humanity and compassion, respect for autonomy.
End-of-life in the ICU Use of intensive care at the end of life in the U. S. RWJ ICU End-of-Life Peer Group. Crit Care Med 2004 – Projection: 540, 000 people die after receiving ICU care each year. Of hospital deaths, half associated with ICU – 1 in 5 Americans die in/after ICU hospitalization • Deaths in ICU: majority of deaths expected – >70% are preceded by withholding or withdrawing of life support – Intensivists actively manage deaths in ICU • Institute of Medicine – national priority • Society of Critical Care Medicine supports palliative model
Palliative Care • Patient and family-centered • Alleviate suffering caused by illness - control symptoms • Communicate effectively about appropriate goals of treatment • Promote concordance of treatment with patient preferences • Promote quality of life – Quality of life as the outcome rather than morbidity/mortality – Does not hasten or prolong death, affirms life
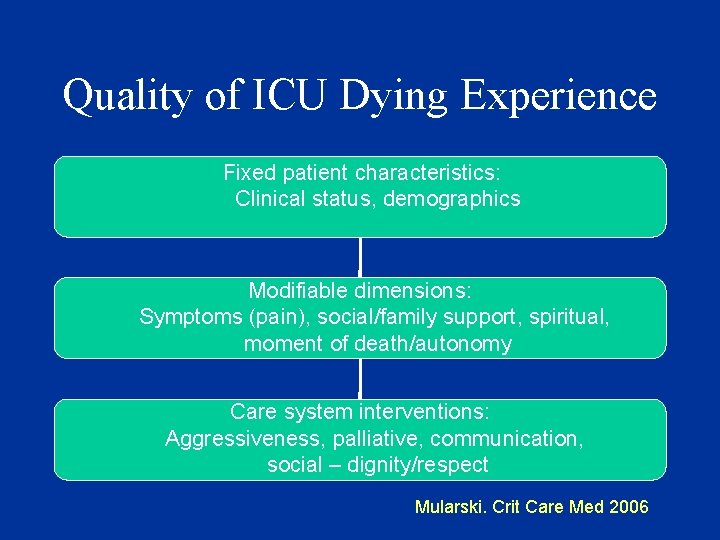
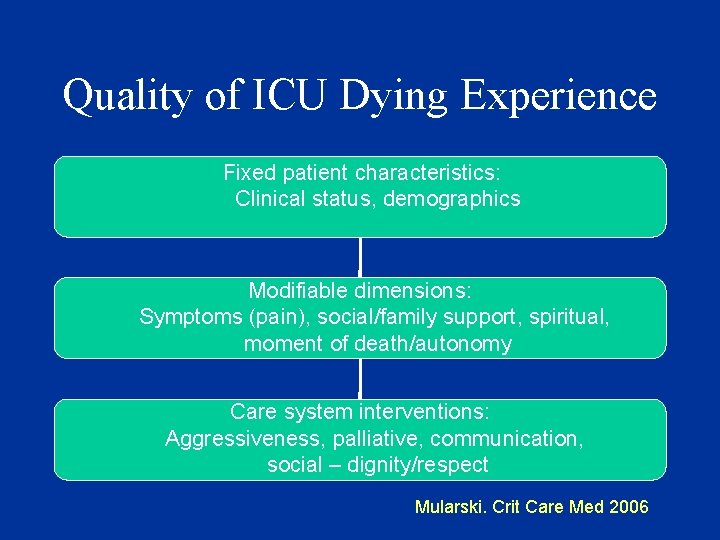
Quality of ICU Dying Experience Fixed patient characteristics: Clinical status, demographics Modifiable dimensions: Symptoms (pain), social/family support, spiritual, moment of death/autonomy Care system interventions: Aggressiveness, palliative, communication, social – dignity/respect Mularski. Crit Care Med 2006
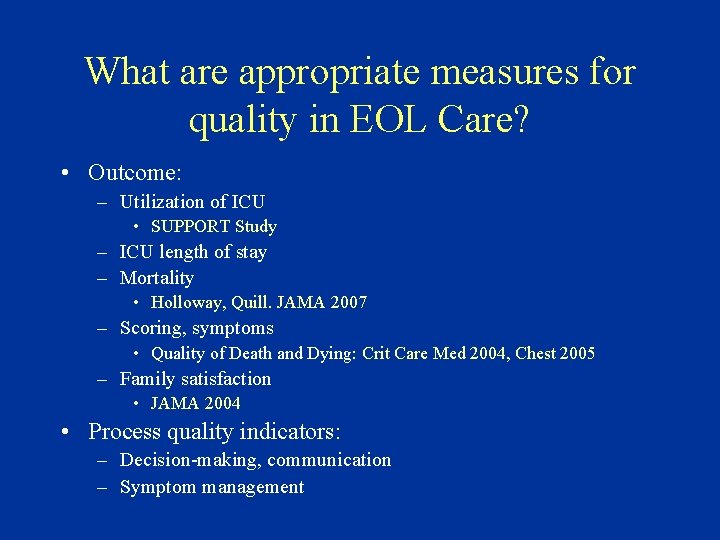
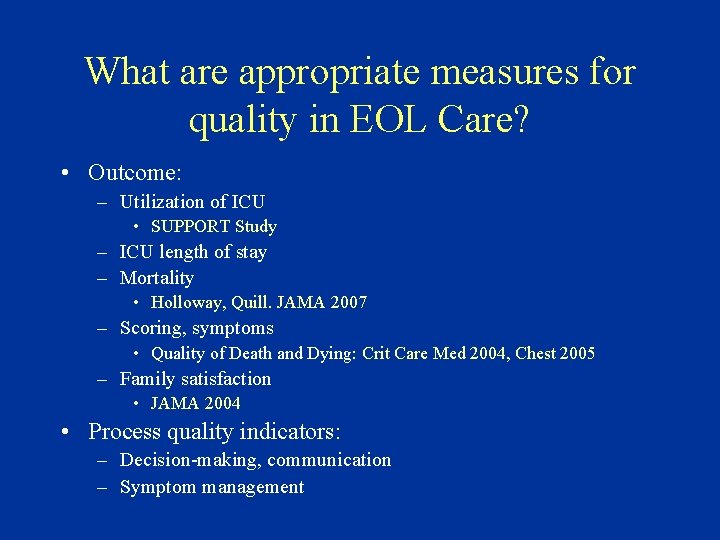
What are appropriate measures for quality in EOL Care? • Outcome: – Utilization of ICU • SUPPORT Study – ICU length of stay – Mortality • Holloway, Quill. JAMA 2007 – Scoring, symptoms • Quality of Death and Dying: Crit Care Med 2004, Chest 2005 – Family satisfaction • JAMA 2004 • Process quality indicators: – Decision-making, communication – Symptom management
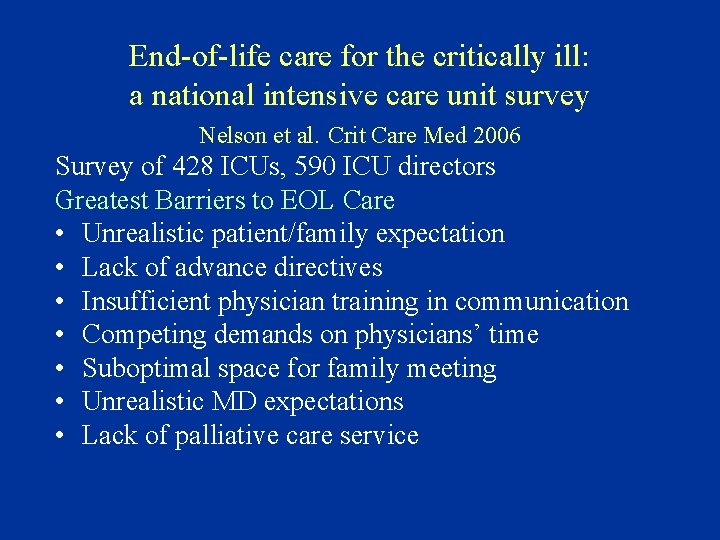
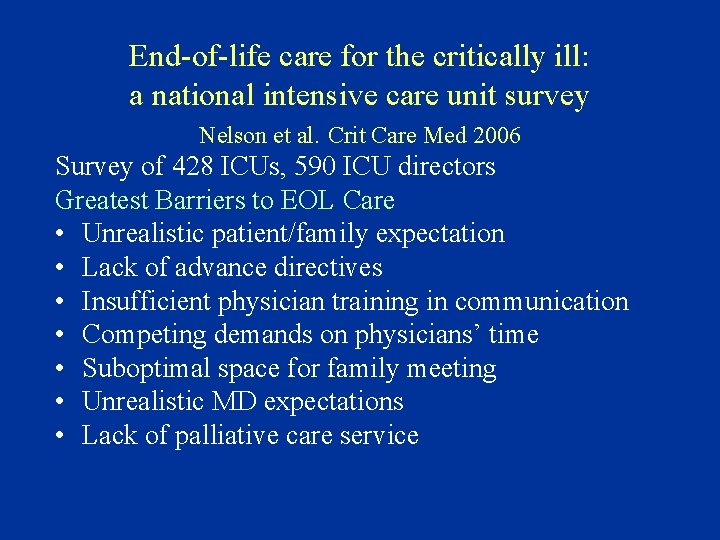
End-of-life care for the critically ill: a national intensive care unit survey Nelson et al. Crit Care Med 2006 Survey of 428 ICUs, 590 ICU directors Greatest Barriers to EOL Care • Unrealistic patient/family expectation • Lack of advance directives • Insufficient physician training in communication • Competing demands on physicians’ time • Suboptimal space for family meeting • Unrealistic MD expectations • Lack of palliative care service
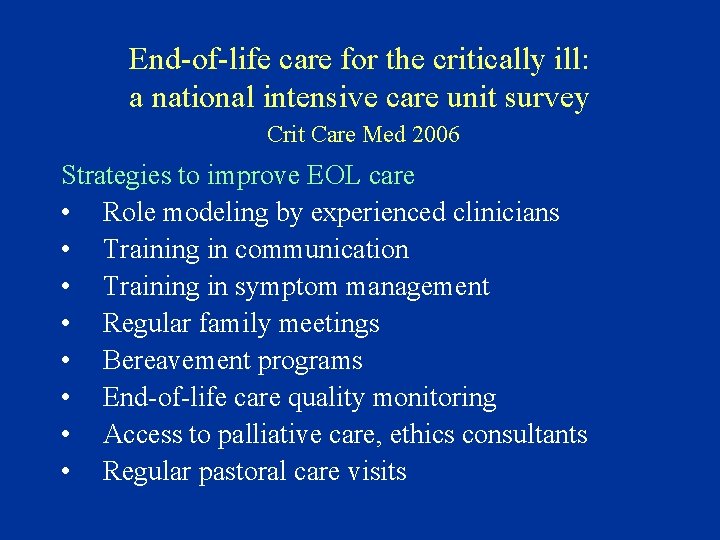
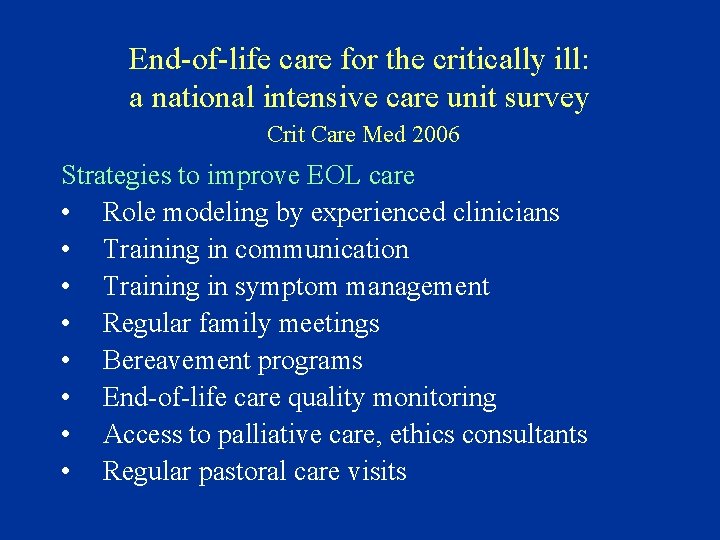
End-of-life care for the critically ill: a national intensive care unit survey Crit Care Med 2006 Strategies to improve EOL care • Role modeling by experienced clinicians • Training in communication • Training in symptom management • Regular family meetings • Bereavement programs • End-of-life care quality monitoring • Access to palliative care, ethics consultants • Regular pastoral care visits
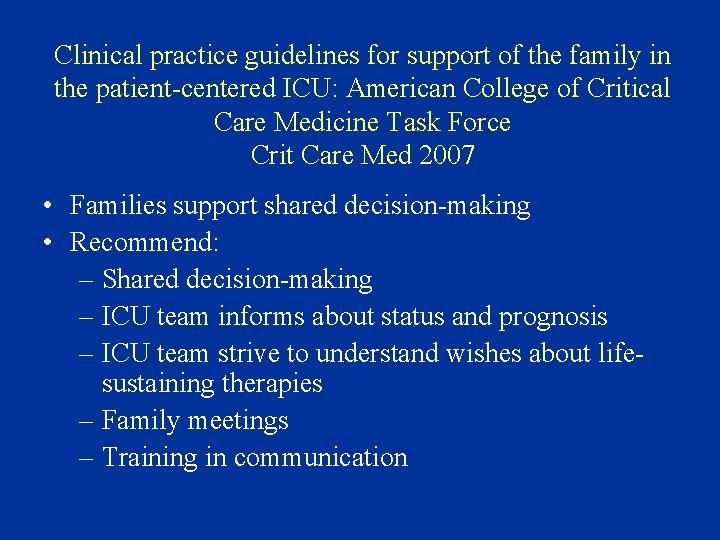
Clinical practice guidelines for support of the family in the patient-centered ICU: American College of Critical Care Medicine Task Force Crit Care Med 2007 • Families support shared decision-making • Recommend: – Shared decision-making – ICU team informs about status and prognosis – ICU team strive to understand wishes about lifesustaining therapies – Family meetings – Training in communication
Decision making depends on communication • Goal is to use patient preferences in order to establish goals of care • The physician must provide information about the illness, treatments, and prognosis • Decisions depend on the patient’s values attached to life-prolongation, functioning, and comfort
Communication with Family • Communication with family: informal, family meetings • Provide information, understanding patient preferences, setting goals • Families: information, understanding – Crit Care Med 2000. over 50% of 102 ICU families failed to identify 1 failing organ, any treatment or prognosis – Chest 2006. 440 hospitalized patients, 160 caregivers. Poor knowledge of CPR – treatments and outcome
Communication - Family conferences • Study of family conferences, Seattle, 2000 -2002, Curtis et al – 51/111 eligible conferences- audiotaped, family questionnaire – Mainly white patient/family and physicians, Englishspeaking – 80% of patients died, WH/WDLS discussed in 86% of conferences • Family satisfaction with family conferences about end-of-life care in the ICU. Crit Care Med 2004 – Conference time 32 minutes, clinicians 70% of time talking. Increased proportion of family speech was associated with increased satisfaction
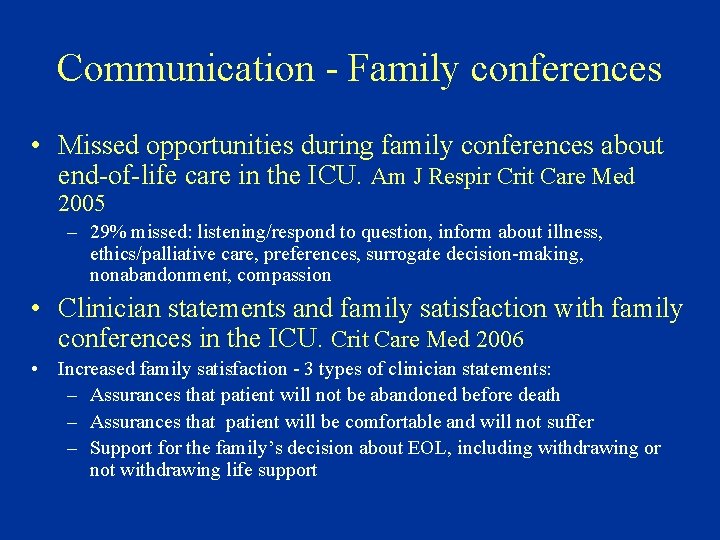
Communication - Family conferences • Missed opportunities during family conferences about end-of-life care in the ICU. Am J Respir Crit Care Med 2005 – 29% missed: listening/respond to question, inform about illness, ethics/palliative care, preferences, surrogate decision-making, nonabandonment, compassion • Clinician statements and family satisfaction with family conferences in the ICU. Crit Care Med 2006 • Increased family satisfaction - 3 types of clinician statements: – Assurances that patient will not be abandoned before death – Assurances that patient will be comfortable and will not suffer – Support for the family’s decision about EOL, including withdrawing or not withdrawing life support
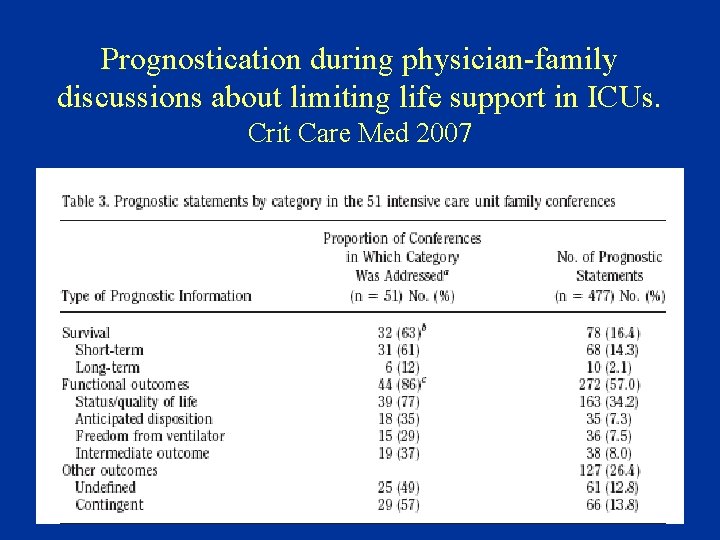
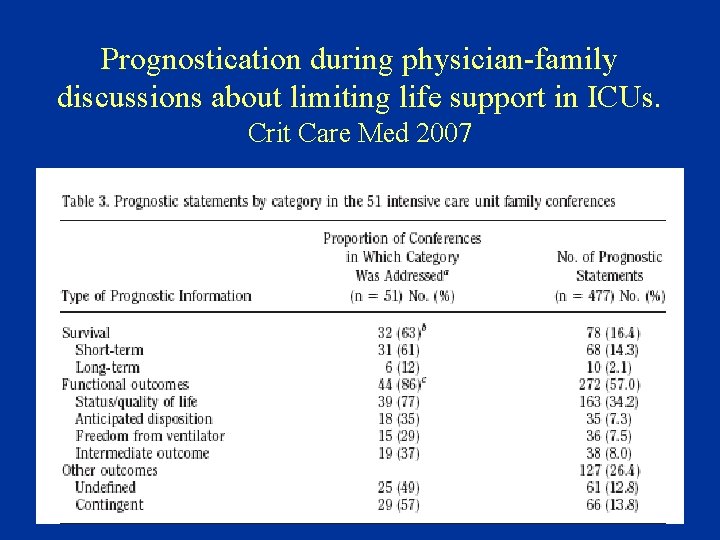
Prognostication during physician-family discussions about limiting life support in ICUs. Crit Care Med 2007
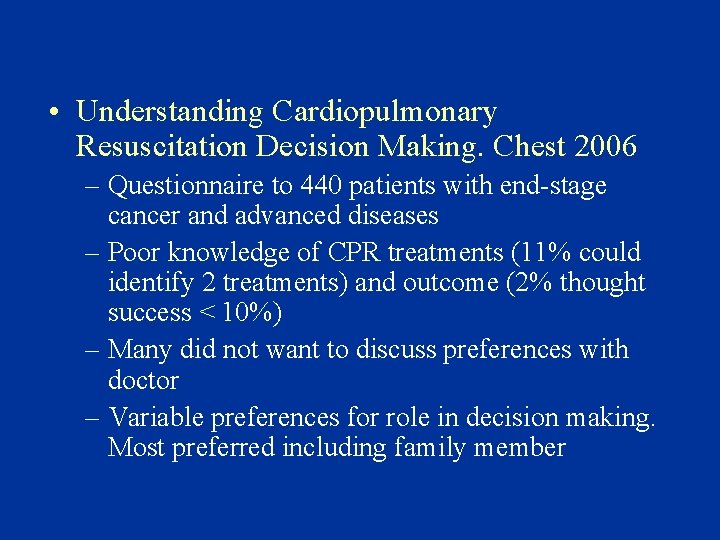
• Understanding Cardiopulmonary Resuscitation Decision Making. Chest 2006 – Questionnaire to 440 patients with end-stage cancer and advanced diseases – Poor knowledge of CPR treatments (11% could identify 2 treatments) and outcome (2% thought success < 10%) – Many did not want to discuss preferences with doctor – Variable preferences for role in decision making. Most preferred including family member
Advance Directives • Health care proxy, living will • Permit patients to make informed decisions about their health care • Promote patient autonomy: patients have the right to make decisions and this right is protected when conscious capacity is lost. • The Patient Self-Determination Act of 1991 requires hospitals to ask patients whether they have an advance directive
• Patient with capacity to make health care decisions has the authority to decline life-sustaining treatment or ask that such treatment be withdrawn • Surrogate decision maker: patient’s representative to make decisions when the patient is incapable of making health care decisions • Substituted judgment: learn what the patient would have wanted if he or she had been able to understand participate in the decisions
Do Not Resuscitate Order • A “Do Not Resuscitate (DNR)” order is one advance directive that concerns interventions in the setting of a cardiopulmonary arrest • A DNR order means that if the patient suffers a cardiopulmonary arrest, the interventions of intubation, CPR and ACLS will be withheld
Decision to Withdraw Life Support • Patient’s expressed wishes • Health care proxy or living will • Oral advance directive – requires Ethics Consultation
Withholding and Withdrawing Life. Sustaining Treatments • Based on the individual patient’s goals of therapy, withholding an intervention may be appropriate • As well, a trial of therapy with clear goals may be undertaken. If the goals are not achieved, withdrawing an intervention is acceptable • The motivation must be respect for patient preferences and avoiding burdensome interventions
Withdrawal of Life Support • Majority of physicians withdraw/withhold life support Am J Respir Crit Care Med 1995 • Life-sustaining treatments: ventilation, vasopressors, dialysis, blood products, nutrition, hydration • >70% of ICU deaths are preceded by decision to WH/WD – Am J Respir Crit Care Med 1998

Withdrawal of Mechanical Ventilation in Anticipation of Death in the ICU Cook et al. N Engl J Med 2003 • 15 medical-surgical ICUs, 851 patients receiving mechanical ventilation • 63% weaned, 17% died while receiving MV • 19. 5% died after withdrawal of MV Determinants of withdrawal • Physicians’ perception of patient preference • Physician prediction of low likelihood of ICU survival and high likelihood of poor cognitive function • Dependency on inotropes and vasopressors
Symptoms in the Critically Ill • Patients die with treatable pain • The symptom burden of chronic critical illness. Crit Care Med 2004 – Patient report: 50 patients with tracheostomy – 40 -50% of patients experienced pain at the highest levels of intensity, 60% dyspnea – Studied communicative patients so likely underestimate symptoms and relief – Half of patients died by 3 months
Nursing - Front Line • Nurse is the main caregiver – ICU, Palliative unit • Improve EOL care – MD/RN Communication • Differences in ideas of EOL, processes, good death, predicting outcomes of critically ill patients – Crit Care Med 2003: 1900 judgments by MD and RNs, disagreements in 63% of dying patients • MD and RN: Different experiences and burdens
Factors associated with nurse assessment of the quality of dying and death in the intensive care unit. Crit Care Med 2004. • 178 patients • QODD: Control of pain, situation, breathing, dignity, time with family, spiritual/religious, someone present at death, on ventilator, proper amount of sedation • Independent predictors of QODD score: – CPR performed in last 8 hours of life – negative – Someone present at moment of death – positive
Quality of Dying in the ICU Chest 2005 • • Ratings by families of 38 decedents, QODD <50% had pain controlled 3% breathing comfortably 32% kept dignity and self-respect
Family Perspectives • Family perspectives on end-of-life care at the last place of care. JAMA 2004 • Family follow-up after 1578 deaths • 67% institution, 32% death at home • Unmet needs in institutions (more than 1/3 reported): inadequate treatment for pain or dyspnea, emotional support, respect, physician communication

How we can improve EOL care • Recognize end of life, preferences, goals of care for the patient • Process of ICU care: decision-making, communication, symptom management • Education, teaching communication skills • For ICU Nurses: involvement in EOL decisions • Communicate - MD, RN, family • Use resources: Nursing, Palliative, Critical Care, Geriatrics, Pastoral Care, Ethics, Social Work
 End of life care in icu
End of life care in icu Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals End to end accounting life cycle tasks
End to end accounting life cycle tasks End-to-end procurement life cycle
End-to-end procurement life cycle Chapter 55 end of life care
Chapter 55 end of life care North west end of life care model
North west end of life care model End of life care in south tyneside
End of life care in south tyneside Primary secondary and tertiary care
Primary secondary and tertiary care General goals and specific goals
General goals and specific goals Motivation in consumer behaviour
Motivation in consumer behaviour Guiding principles of mtb-mle
Guiding principles of mtb-mle Menghitung kebutuhan perawat dengan gillies
Menghitung kebutuhan perawat dengan gillies Caso clínico
Caso clínico Icu localization
Icu localization Klasifikasi pelayanan icu
Klasifikasi pelayanan icu Information and communication university zambia location
Information and communication university zambia location Icu indication
Icu indication Sean forsythe
Sean forsythe Estado de conciencia alterado
Estado de conciencia alterado Language
Language Cam icu escala
Cam icu escala Cheetah nicom monitor
Cheetah nicom monitor Abcde methode ehbo
Abcde methode ehbo Icu unit meaning
Icu unit meaning Icu orientation
Icu orientation Icu for dummies
Icu for dummies List of lecturers at icu zambia
List of lecturers at icu zambia Icu acuity tool
Icu acuity tool Icu library
Icu library