In vitro fertilization Dr Kamal Kumar Gupta Louise




















- Slides: 45

In vitro fertilization Dr. Kamal Kumar Gupta
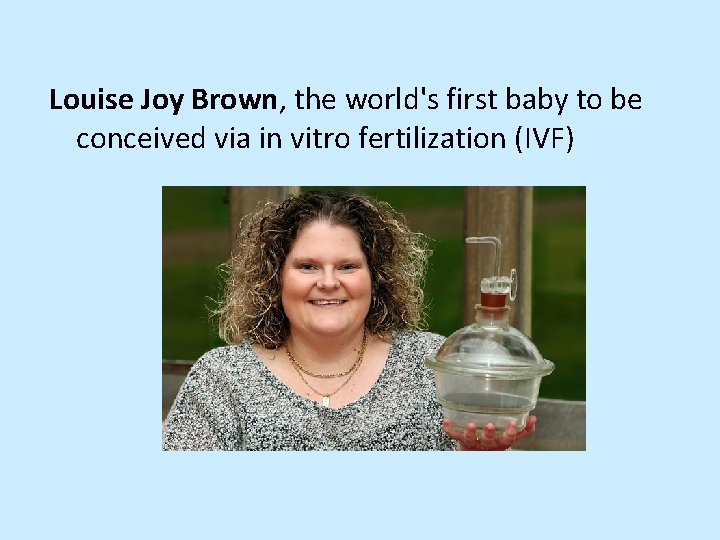
Louise Joy Brown, the world's first baby to be conceived via in vitro fertilization (IVF)
• On July 25, 1978, Louise Joy Brown, the world’s first baby conceived via in vitro fertilization (IVF) was born at Oldham and District General Hospital in Manchester, England, to parents Lesley and Peter Brown. The healthy baby was delivered shortly before midnight by caesarean section and weighed in at five pounds, 12 ounces.
• Before giving birth to Louise, Lesley Brown had suffered years of infertility due to blocked fallopian tubes • In November 1977, she underwent then-experimental IVF procedure • A mature egg was removed from one of her ovaries and combined in a laboratory dish with her husband’s sperm to form an embryo • The embryo then was implanted into her uterus a few days later • Her IVF doctors, British gynecologist Patrick Steptoe and scientist Robert Edwards, had begun their pioneering collaboration a decade earlier

• Dr. Subhash Mukhopadhyay created history when he became the first physician in India (and second in the world to perform the In vitro fertilization resulting in a test tube baby “Durga” (Kanupriya Agarwal) on October 3, 1978.

• Today, IVF is considered a mainstream medical treatment for infertility. Hundreds of thousands of children around the world have been conceived through the procedure, in some cases with donor eggs and sperm

• Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus • Previous tubal sterilization or removal. If one had tubal ligation and want to conceive, IVF may be an alternative to tubal ligation reversal • Endometriosis occurs when the uterine tissue implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes
• Uterine fibroids. Fibroids are benign tumors in the wall of the uterus and are common in women in their 30 s and 40 s. Fibroids can interfere with implantation of the fertilized egg • Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization • Premature ovarian failure is the loss of normal ovarian function before age 40. If your ovaries fail, they don't produce normal amounts of the hormone estrogen or have eggs to release regularly
• Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg • Unexplained infertility means no cause of infertility has been found despite evaluation for common causes
• A genetic disorder. If parents are at risk of passing on a genetic disorder to child, IVF is recommended for preimplantation genetic diagnosis. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found. Embryos that don't contain identified problems can be transferred to the uterus.

• Fertility preservation for cancer or other health conditions. If some one is about to start cancer treatment — such as radiation or chemotherapy — that could harm fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use
• Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman's eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier's uterus
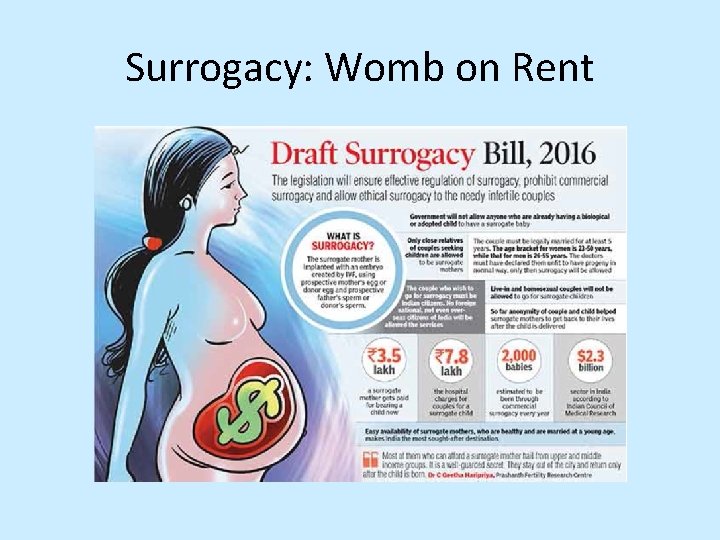
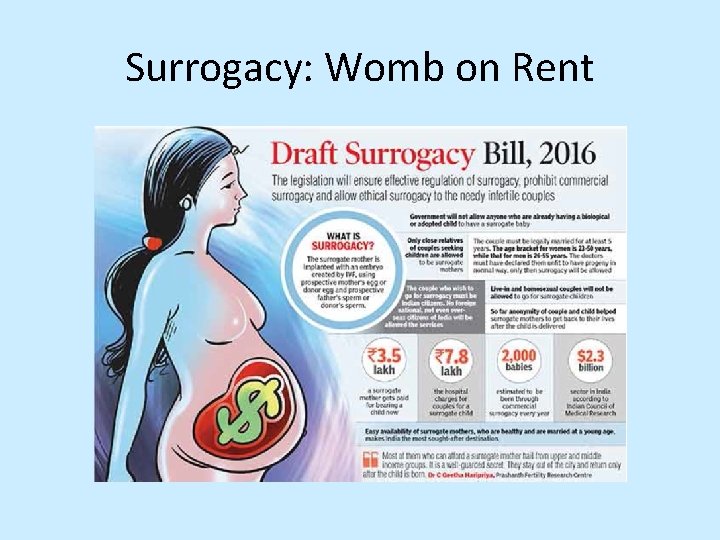
Surrogacy: Womb on Rent

• During IVF, mature eggs are collected (retrieved) from your ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs are implanted in uterus. One cycle of IVF takes about two weeks • IVF is the most effective form of assisted reproductive technology. The procedure can be done using own eggs and partner's sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — a woman who has an embryo implanted in her uterus — might be used


Hyperstimulation of the Ovaries • After pretreatment has taken place, the IVF patient will take multiple injections to stimulate the ovary in order to mature multiple eggs at the same time. Typically, the patient takes injectable FSH (follicle stimulating hormone) for 8 -11 days daily until her eggs mature. Taking injectable FSH causes several follicles to mature at a similar rate at the same time • Eggs (oocytes) are retrieved from patients approximately 36 hours after an injection of h. CG

Egg Retrieval • Egg retrieval is a minor surgical procedure that occurs under anesthesia at a sophisticated medical center once the follicles have reached maturity. The entire process only takes about 15 -20 minutes. During this time frame, an ultra-thin needle is used to extract the follicular fluid, which is then examined by an embryologist to find the mature eggs. At the same time semen sample of the male partner is collected

• Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into the vagina to identify follicles, and a needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device




• https: //www. youtube. com/watch? v=Of. GWx. G YFETo • Please watch this video

• Immediately after retrieval, each complex is identified under a microscope and then transferred to a special solution (“insemination media”) that is specially designed to provide all of the nutrients and other substances necessary to maximize the likelihood of successful fertilization of eggs by the sperm

• The dishes containing the eggs are then placed into an incubator, so that the environmental conditions surrounding the eggs can be tightly controlled with regard to light, oxygen and carbon dioxide concentrations, as well as the p. H and temperature. The cumulus cells are left attached to the oocyte for at least 4 hours postretrieval to allow the oocytes to complete their maturation. As different procedures regarding oocyte and embryonic development occur on specific days, we refer to the day of the oocyte retrieval as “Day zero
Fertilization • After the egg retrieval process is complete, they are combined in a laboratory with semen sample for natural fertilization • This usually takes place in a small medical dish with the aid of a nutrient fluid, which is then incubated overnight
Assessment of Fertilization • The assessment of fertilization takes place by evaluating each egg the day after the oocyte retrieval and looking for the presence of two pronuclei. One pronucleus contains the genetic material contributed by the egg; the other contains the genetic material contributed by the sperm • The presence of two pronuclei denotes normal fertilization. The pre-embryo at this one cell stage is referred to as a zygote, which is the first stage in embryo development. The presence of only one pronucleus generally means that the egg has been activated, but there is no sperm contribution
Fertilization • The presence of more than two pronuclei means either that more than one sperm has entered the oocyte or that the oocyte did not complete its final maturation process (which occurs after the sperm enters the egg). Consequently, there is too much maternal genetic material present for a normal embryo to develop. These zygotes that contain more or fewer than two pronuclei are chromosomally abnormal and, therefore, can never develop into a normal baby.
Embryo Transfer • The embryos are allowed to continue to grow in the lab and the selection of the best embryos is made on day 5 • If the transfer is on day 3, the embryos chosen for transfer are usually at the 6 -8 cell stage • By day 5, the embryos should be at the blastocyst stage at which time each embryo contains approximately 100 -120 cells. At this stage the embryo is beginning to differentiate. The cells destined to become the baby are identified as the “inner cell mass”. The cells around the periphery of the embryo are called the trophectoderm and become the placenta • The development of the trophectoderm and the inner cell mass is equally important for a healthy pregnancy to develop.
Embryo Transfer • Physician decides on the number of embryos to transfer according to strict guidelines developed based on an extensive review of the published literature in the hope of maximizing a couple’s chance for pregnancy while minimizing their risk of a multiple pregnancy • The number of embryos to transfer is determined by multiple factors such as age of the egg and the development of the embryos
Confirming IVF Implantation and Pregnancy • After the embryos are transferred to the patient, two follow-up tests are scheduled in order to confirm implantation • It is usually done within a few weeks after embryo transfer, and the second will occur one week after that. Once implantation is confirmed with two positive tests, the in vitro fertilization process is complete
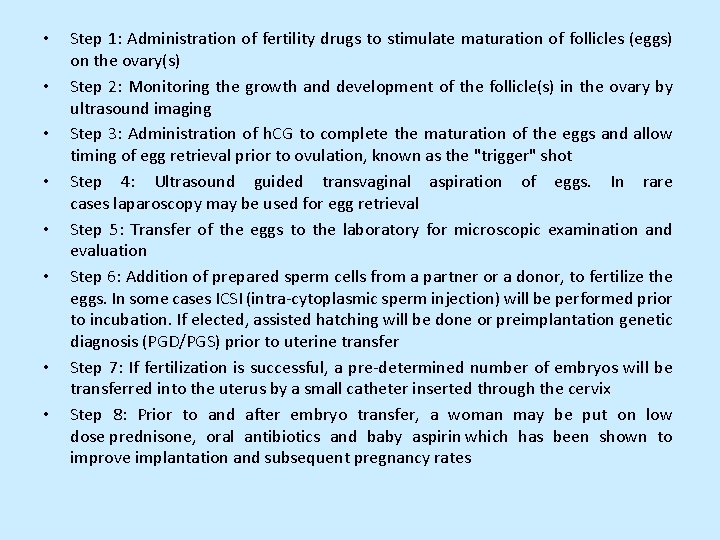
• • Step 1: Administration of fertility drugs to stimulate maturation of follicles (eggs) on the ovary(s) Step 2: Monitoring the growth and development of the follicle(s) in the ovary by ultrasound imaging Step 3: Administration of h. CG to complete the maturation of the eggs and allow timing of egg retrieval prior to ovulation, known as the "trigger" shot Step 4: Ultrasound guided transvaginal aspiration of eggs. In rare cases laparoscopy may be used for egg retrieval Step 5: Transfer of the eggs to the laboratory for microscopic examination and evaluation Step 6: Addition of prepared sperm cells from a partner or a donor, to fertilize the eggs. In some cases ICSI (intra-cytoplasmic sperm injection) will be performed prior to incubation. If elected, assisted hatching will be done or preimplantation genetic diagnosis (PGD/PGS) prior to uterine transfer Step 7: If fertilization is successful, a pre-determined number of embryos will be transferred into the uterus by a small catheter inserted through the cervix Step 8: Prior to and after embryo transfer, a woman may be put on low dose prednisone, oral antibiotics and baby aspirin which has been shown to improve implantation and subsequent pregnancy rates

Fates of Frozen Embryos • Store indefinitely. • Store and destroy after a set time. • Donate for embryonic stem cell derivation and research. • Thaw later for use by biological parents. • Thaw later for use by other parents. • Discard
Extra Embryos • In the United States, nearly half a million embryos derived from IVF sit in freezers; some have been there for years. • Most couples who donate embryos to others do so anonymously, with no intention of learning how their genetic offspring are raised.
Extra Embryos • In 2001, two of Glenda’s eighteen embryos were transferred to her uterus, and developed into twins Samantha and Mitchell • Through a website where couples chat about fertility issues, Scott and Glenda met and selected Bruce and Susan Lindeman to receive fourteen remaining embryos • This second couple had tried IVF three times, with no luck. The Lyonses frozen embryos were shipped cross-country to a clinic where two were implanted in Susan’s uterus. In July 2003, Chase and Jack Lindeman were born—genetic siblings of Samantha and Mitchell Lyones • But there were still embryos left. The Lyons allowed the Lindemans to send twelve embryos to a third couple, who used two to have twin daughters in August 2004. They are biological siblings of Samantha and Mitchell Lyons and Chase and Jack Lindeman.

Extra Embryos • Like the Lyonses a woman in California who had eight fertilized ova left over after using six to produce her six young children, also did not want to destroy them or continue to store them. Nadya Suleman was implanted with them, and in early 2009 gave birth to octuplets! • Donating fertilized ova and embryos for use in research is another alternative to disposing of them. The results of these experiments sometimes challenge long-held ideas, indicating that we still have much to learn about early human prenatal development
Preimplantation Genetic Diagnostics • Lisa and Jack Nash sought to have a child for a different reason. Their daughter Molly, born on July 4, 1994, had Fanconi anemia. This autosomal recessive condition would destroy her bone marrow and her immunity • An umbilical cord stem cell transplant from a sibling could likely cure her, but Molly had no siblings. Nor did her parents wish to have another child with a one in four chance of inheriting the disorder • In late 1999, researchers at the Reproductive Genetics Institute at Illinois Medical Center mixed Jack’s sperm with Lisa’s oocytes in a laboratory dish. After allowing fifteen of the fertilized ova to develop to the eight-cell stage, researchers separated and applied DNA probes to one cell from each embryo • A cell that had wild type Fanconi anemia alleles and that matched Molly’s human leukocyte antigen (HLA) type was identified and its seven-celled remainder implanted into Lisa’s uterus • Adam was born in late summer. A month later, physicians infused his umbilical cord stem cells into Molly, saving her life

Savior siblings
• However, an experimental ART called polar body biopsy may reduce this supply by increasing the success of IVF. Polar body biopsy is based on Mendel’s first law, the segregation of alleles. In the technique, if a polar body resulting from the first meiotic division in a woman who is a carrier of an X-linked disorder has the mutant allele, then the oocyte to which it clings lacks that allele. Oocytes that pass this test can be fertilized in vitro and the resulting embryo implanted. Polar body biopsy is possible because the polar body is attached to the much larger oocyte. A large pipette is used to hold the two cells in place, and a smaller pipette is used to separate the polar body. Then, DNA probes and FISH are used to look at genes and chromosomes in the polar body and infer the genotype of the oocyte. Polar body biopsy followed by PGD is quite effective in avoiding conceptions with chromosome abnormalities or certain single-gene disorders.

• A couple in search of an oocyte donor advertises in a college newspaper seeking an attractive young woman from an athletic family • A man paralyzed from the waist down has sperm removed and injected into his partner’s oocyte. He, too, becomes a parent when he thought he never would.
Postmortem Sperm Retrieval • Bruce and Gaby V. , in their early thirties, had delayed becoming parents, confident that their good health would make pregnancy possible later. But then Bruce suddenly died of an allergic reaction to a medication. Gaby knew how much Bruce had wanted to be a father, so she asked the medical examiner to collect Bruce’s sperm. The sample was sent to the California Cryobank, where it lay deeply frozen for more than a year. In the summer of 1978, Cappy Rothman, medical director of the sperm bank, defrosted the sperm and used it to fertilize one of Gaby’s oocytes. On March 17, Bruce and Gaby’s daughter was born. It was the first case of postmortem sperm retrieval in which the father did not actively participate in the decision.
• Postmortem sperm retrieval raises legal and ethical issues. A woman conceived twins with her husband’s consent 16 months after he died of leukemia at age 30. • The Social Security Administration refused to provide survivor benefits to their daughters, claiming that the husband was not a father, but a sperm donor. • The Massachusetts Superior Court reversed this decision. Like other assisted reproductive technologies, postmortem sperm retrieval is not regulated at the federal level in the United States. Bioethicists have identified situations to avoid: • Someone other than a spouse wishing to use the sperm • A too-hasty decision based on grief • Use of the sperm for monetary gain
Assisted Reproductive Disasters • A physician in California used his own sperm to perform intrauterine insemination on 15 patients, telling them that he had used sperm from anonymous donors • A plane crash killed the wealthy parents of two early embryos stored at − 320°F (− 195°C) in a hospital in Melbourne, Australia. Adult children of the couple were asked to share their estate with two 8 -celled siblings-to-be • 3. Several couples in Chicago planning to marry discovered that they were half-siblings. Their mothers had been inseminated with sperm from the same donor • 4. Two Rhode Island couples sued a fertility clinic for misplacing several embryos
Assisted Reproductive Disasters • Several couples in California sued a fertility clinic for implanting their oocytes or embryos in other women without donor consent. One woman requested partial custody of the resulting children if her oocytes were taken, and full custody if her embryos were used, even though the children were of school age and she had never met them. • A man sued his ex-wife for possession of their frozen fertilized ova. He won, and donated them for research. She had wanted to be pregnant. • The night before in vitro fertilized embryos were to be implanted in a 40 -year-old woman’s uterus after she and her husband had spent four years trying to conceive, the man changed his mind, and wanted the embryos destroyed. Their embryo custody battle is before the Supreme Court.
 Kamal kumar ips
Kamal kumar ips External fertilization birds
External fertilization birds Pyloric stenosis
Pyloric stenosis Dr pulin kumar gupta
Dr pulin kumar gupta Prof. dr. pradeep kumar gupta
Prof. dr. pradeep kumar gupta Wetboek familierecht
Wetboek familierecht Absorption intestinale
Absorption intestinale Tumacenje ige
Tumacenje ige Procedure for isolation of cell for in vitro culture
Procedure for isolation of cell for in vitro culture Iman siadat
Iman siadat Vitro data center
Vitro data center Felice shieh
Felice shieh Ahmad kamal
Ahmad kamal Dp
Dp Mukim tupai
Mukim tupai Big data analytics raj kamal
Big data analytics raj kamal Kamal shehadi
Kamal shehadi Kamal sarabandi
Kamal sarabandi Michael kamal
Michael kamal Kamal nasr
Kamal nasr Scott willenbrock
Scott willenbrock Herbalife mission and vision statement
Herbalife mission and vision statement Kamal field engineer
Kamal field engineer Kamal sarabandi
Kamal sarabandi Shirin kamal
Shirin kamal Moustapha kamal gueye
Moustapha kamal gueye Kamal ke saman nayan
Kamal ke saman nayan How to learn written english by mostafa kamal
How to learn written english by mostafa kamal Kamal benslama
Kamal benslama Mount litera zee school books solutions class 5
Mount litera zee school books solutions class 5 Kamal sarabandi
Kamal sarabandi Human fertilization
Human fertilization Tree fertilization saddle river nj
Tree fertilization saddle river nj Fertilization process in plants
Fertilization process in plants Cardinal ligament also known as
Cardinal ligament also known as Cnidaria
Cnidaria Lesson 15.4 ovulation fertilization and implantation
Lesson 15.4 ovulation fertilization and implantation Fertilization occurs
Fertilization occurs Parts of flower
Parts of flower Internal fertilization
Internal fertilization Double fertilization in angiosperms
Double fertilization in angiosperms Female part of a flower
Female part of a flower Angiosperms double fertilization
Angiosperms double fertilization Cilia 9+2 arrangement
Cilia 9+2 arrangement Sexual reproduction
Sexual reproduction Reproduction in pila
Reproduction in pila