Hyperthyroidism and Pregnancy Fereidoun Azizi Research Institute for




- Slides: 40

Hyperthyroidism and Pregnancy Fereidoun Azizi Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences Tehran, I. R. Iran
Objectives To review: �Changes in thyroid economy during pregnancy �Thyroid function tests in pregnancy �Hyperthyroidism and pregnancy
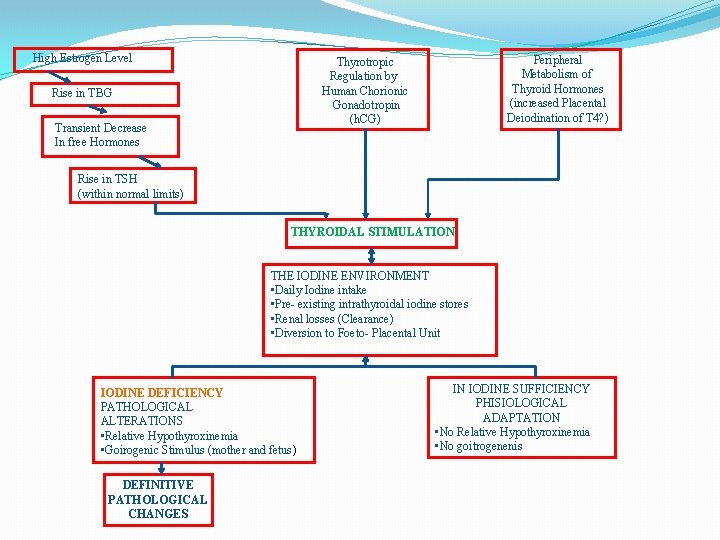
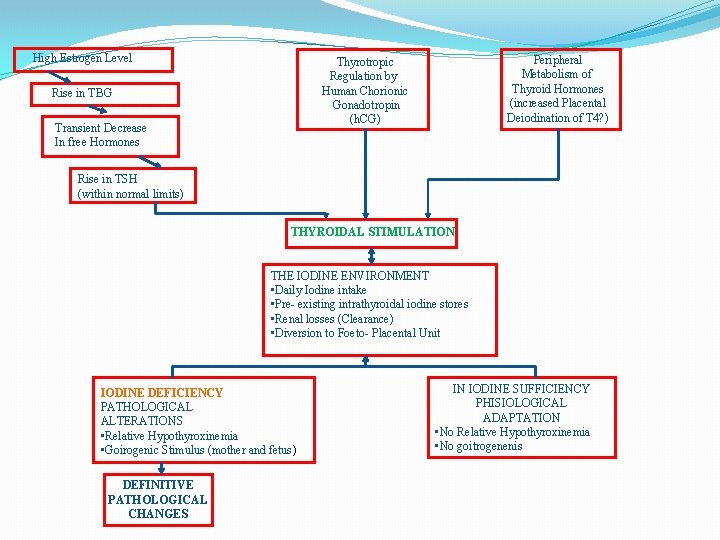
High Estrogen Level Peripheral Metabolism of Thyroid Hormones (increased Placental Deiodination of T 4? ) Thyrotropic Regulation by Human Chorionic Gonadotropin (h. CG) Rise in TBG Transient Decrease In free Hormones Rise in TSH (within normal limits) THYROIDAL STIMULATION THE IODINE ENVIRONMENT • Daily Iodine intake • Pre- existing intrathyroidal iodine stores • Renal losses (Clearance) • Diversion to Foeto- Placental Unit IODINE DEFICIENCY PATHOLOGICAL ALTERATIONS • Relative Hypothyroxinemia • Goirogenic Stimulus (mother and fetus) DEFINITIVE PATHOLOGICAL CHANGES IN IODINE SUFFICIENCY PHISIOLOGICAL ADAPTATION • No Relative Hypothyroxinemia • No goitrogenenis

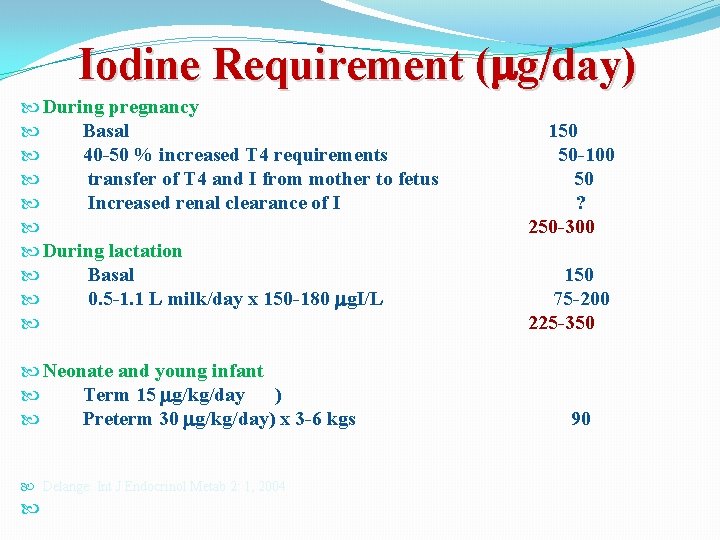
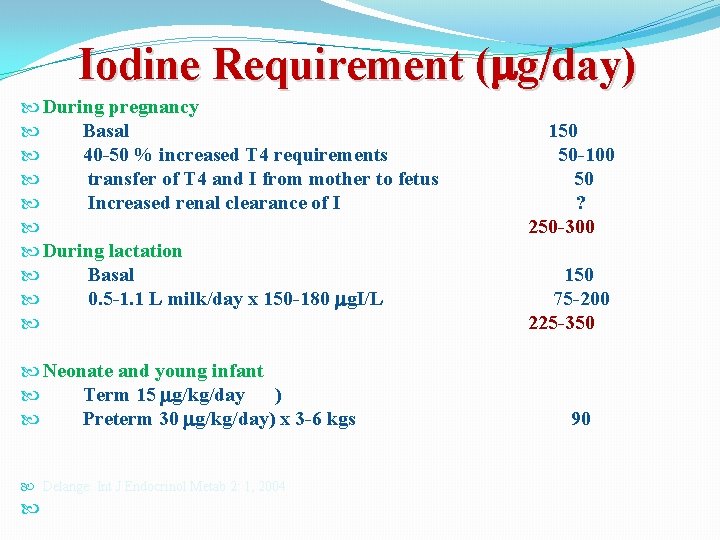
Iodine Requirement ( g/day) During pregnancy Basal 150 40 -50 % increased T 4 requirements 50 -100 transfer of T 4 and I from mother to fetus 50 Increased renal clearance of I ? 250 -300 During lactation Basal 150 0. 5 -1. 1 L milk/day x 150 -180 g. I/L 75 -200 225 -350 Neonate and young infant Term 15 g/kg/day ) Preterm 30 g/kg/day) x 3 -6 kgs 90 Delange: Int J Endocrinol Metab 2: 1, 2004
Thyroid Function Tests in Pregnancy
Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and Postpartum The American Thyroid Association Taskforce on Thyroid Disease During Pregnancy and Postpartum Alex Stagnaro-Green (Chair), Marcos Abalovich, Erik Alexander, Fereidoun Azizi, Jorge Mestman, Roberto Negro, Angelita Nixon, Elizabeth N. Pearce, Offie P. Soldin, Scott Sullivan and Wilmar Wiersinga 84 Questions 76 Recommendations Thyroid 2011; 21: 1081 -1125
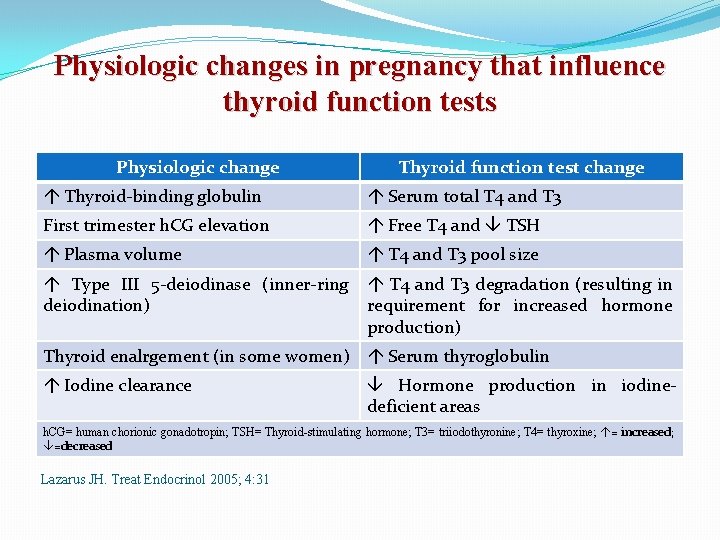
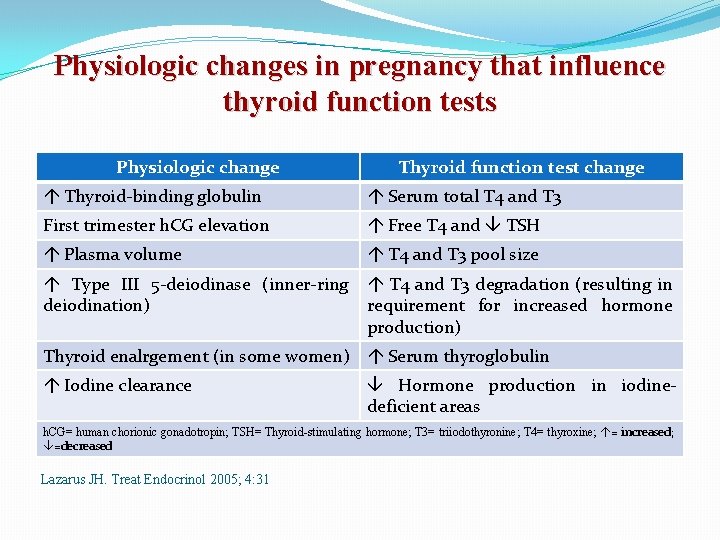
Physiologic changes in pregnancy that influence thyroid function tests Physiologic change Thyroid function test change Thyroid-binding globulin Serum total T 4 and T 3 First trimester h. CG elevation Free T 4 and TSH Plasma volume T 4 and T 3 pool size Type III 5 -deiodinase (inner-ring deiodination) T 4 and T 3 degradation (resulting in requirement for increased hormone production) Thyroid enalrgement (in some women) Serum thyroglobulin Iodine clearance Hormone production in iodinedeficient areas h. CG= human chorionic gonadotropin; TSH= Thyroid-stimulating hormone; T 3= triiodothyronine; T 4= thyroxine; = increased; =decreased Lazarus JH. Treat Endocrinol 2005; 4: 31
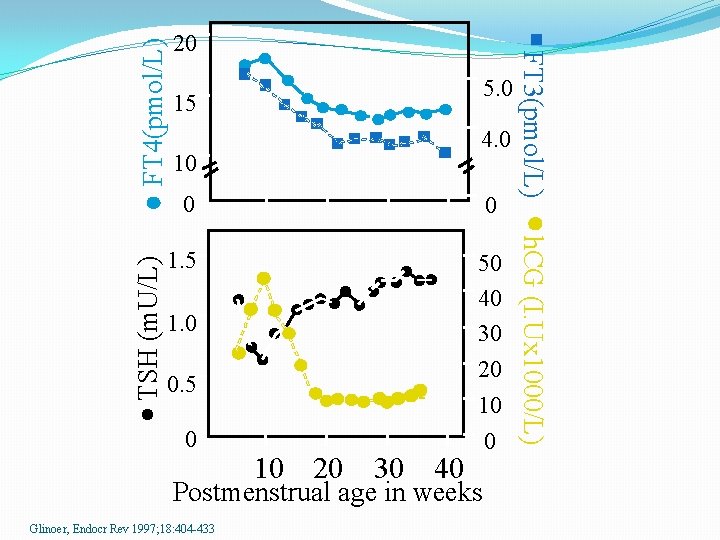
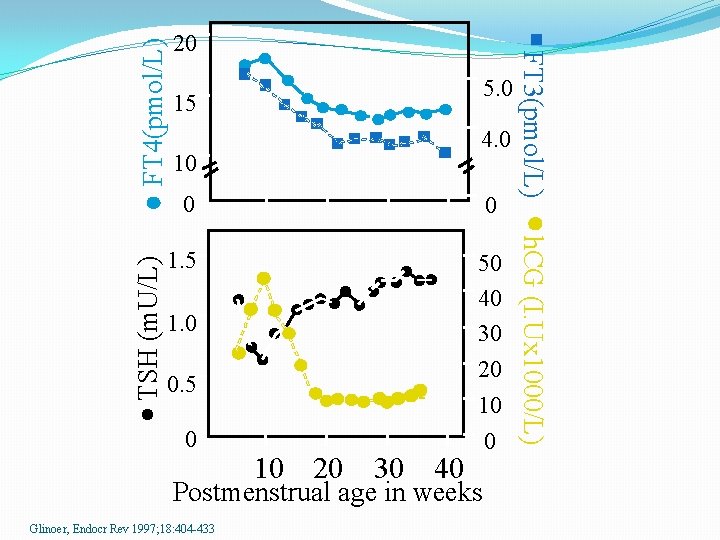
FT 4(pmol/L) 4. 0 10 0 0 1. 5 50 40 30 1. 0 20 0. 5 0 10 20 30 40 10 0 Postmenstrual age in weeks Glinoer, Endocr Rev 1997; 18: 404 -433 h. CG (I. Ux 1000/L) TSH (m. U/L) 5. 0 15 FT 3(pmol/L) 20
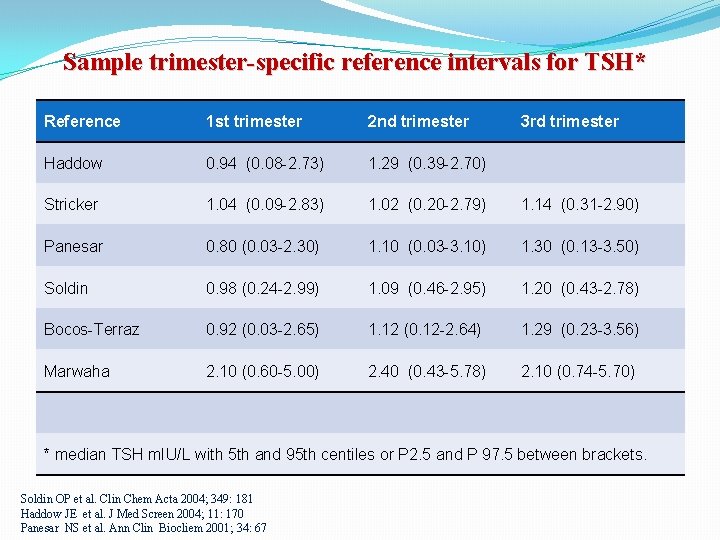
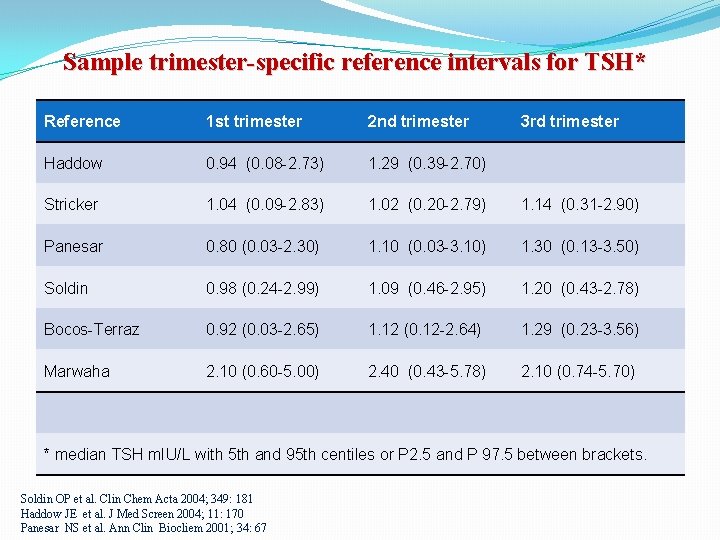
Sample trimester-specific reference intervals for TSH* Reference 1 st trimester 2 nd trimester 3 rd trimester Haddow 0. 94 (0. 08 -2. 73) 1. 29 (0. 39 -2. 70) Stricker 1. 04 (0. 09 -2. 83) 1. 02 (0. 20 -2. 79) 1. 14 (0. 31 -2. 90) Panesar 0. 80 (0. 03 -2. 30) 1. 10 (0. 03 -3. 10) 1. 30 (0. 13 -3. 50) Soldin 0. 98 (0. 24 -2. 99) 1. 09 (0. 46 -2. 95) 1. 20 (0. 43 -2. 78) Bocos-Terraz 0. 92 (0. 03 -2. 65) 1. 12 (0. 12 -2. 64) 1. 29 (0. 23 -3. 56) Marwaha 2. 10 (0. 60 -5. 00) 2. 40 (0. 43 -5. 78) 2. 10 (0. 74 -5. 70) * median TSH m. IU/L with 5 th and 95 th centiles or P 2. 5 and P 97. 5 between brackets. Soldin OP et al. Clin Chem Acta 2004; 349: 181 Haddow JE et al. J Med Screen 2004; 11: 170 Panesar NS et al. Ann Clin Biocliem 2001; 34: 67
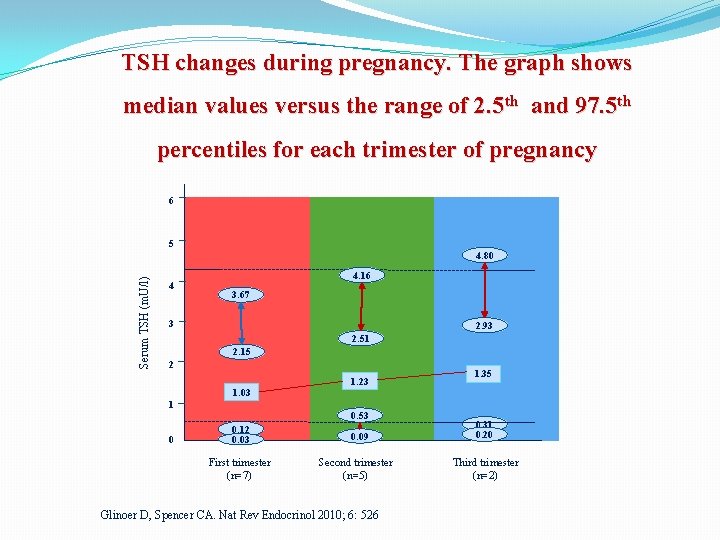
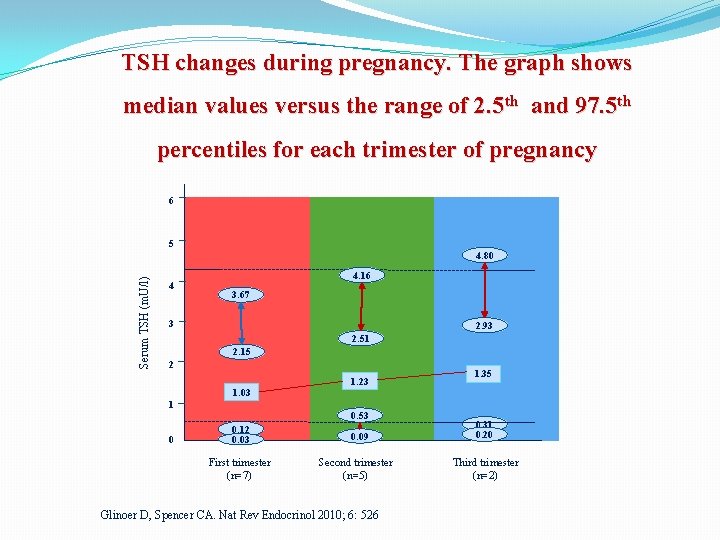
TSH changes during pregnancy. The graph shows median values versus the range of 2. 5 th and 97. 5 th percentiles for each trimester of pregnancy 6 5 Serum TSH (m. U/l) 4. 80 4 4. 16 3. 67 3 2. 93 2. 51 2. 15 2 1. 03 1 0 1. 23 0. 53 0. 12 0. 03 First trimester (n=7) 0. 09 Second trimester (n=5) Glinoer D, Spencer CA. Nat Rev Endocrinol 2010; 6: 526 1. 35 0. 31 0. 20 Third trimester (n=2)
Trimester-specific reference ranges for TSH, as defined in populations with optimal iodine intake, should be applied. Haddow JE et al. J Med Screen 2004; 11: 170 Panesar NS et al. Ann Clin Biocliem 2001; 34: 67 The varaiah M et al. Malaysian J Pathol 2009; 31: 23
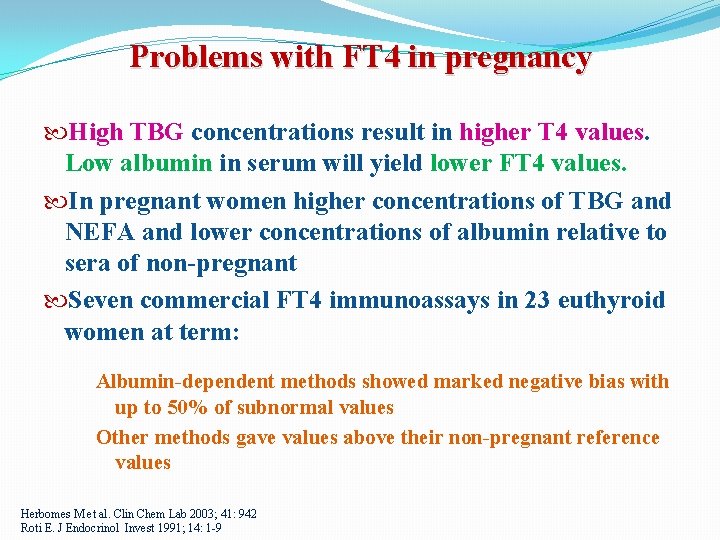
Problems with FT 4 in pregnancy High TBG concentrations result in higher T 4 values. Low albumin in serum will yield lower FT 4 values. In pregnant women higher concentrations of TBG and NEFA and lower concentrations of albumin relative to sera of non-pregnant Seven commercial FT 4 immunoassays in 23 euthyroid women at term: Albumin-dependent methods showed marked negative bias with up to 50% of subnormal values Other methods gave values above their non-pregnant reference values Herbomes M et al. Clin Chem Lab 2003; 41: 942 Roti E. J Endocrinol Invest 1991; 14: 1 -9
Accurate Measurement of FT 4 The latest development in the field of FT 4 analysis is to measure free thyroid hormones in the dialysate or ultrafiltrate using online solid phase extraction - liquid chromatography/tandem mass spectrometry. The 95% FT 4 reference intervals decreased gradually with advancing gestational age: from 1. 081. 82 ng/d. L in week 14 to 0. 86 -1. 53 ng/dl in week 20 Yue et al. Clin Chem 2008; 54: 642
WHAT IS THE OPTIMAL METHOD TO ASSESS FT 4 DURING PREGNANCY? To measure FT 4 in the presence of high concentrations of bound T 4 has proved to be challenging especially in abnormal binding-protein states such as pregnancy. The normal ranges for FT 4 index are calculated by TT 4 x T 3 uptake and TBG, but trimester-specific reference intervals for FT 4 index have not been established.
Thyrotoxicosis in pregnancy Occurs in 0. 2% of women Mostly caused by Graves’ disease
HOW CAN GESTATIONAL HYPERTHYROIDISM BE DIFFERENTIATED FROM GRAVES’ HYPERTHYROIDISM IN PREGNANCY? In the presence of a suppressed serum TSH in the first trimester, a history and physical exam is of the utmost importance. FT 4 I measurements should be obtained. Helpful lab: total T 3, presence of serum markers for autoimmune disease (TBII, TSI, or TPO antibody). Tan JY et al. BJOG 2002; 109: 683
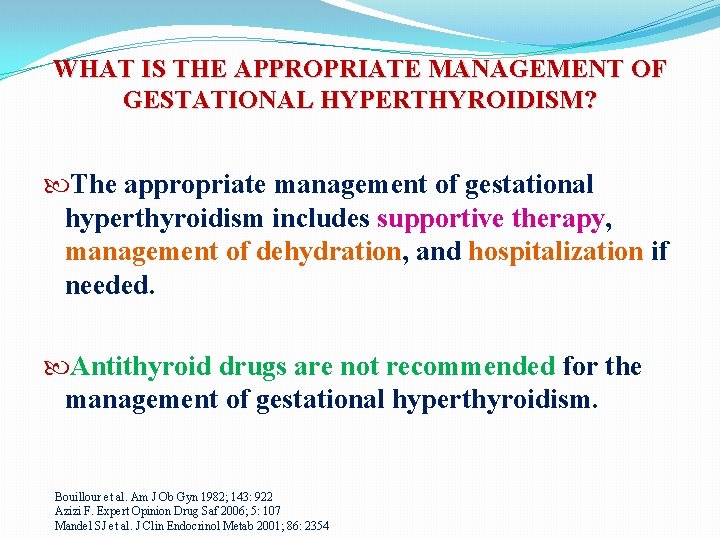
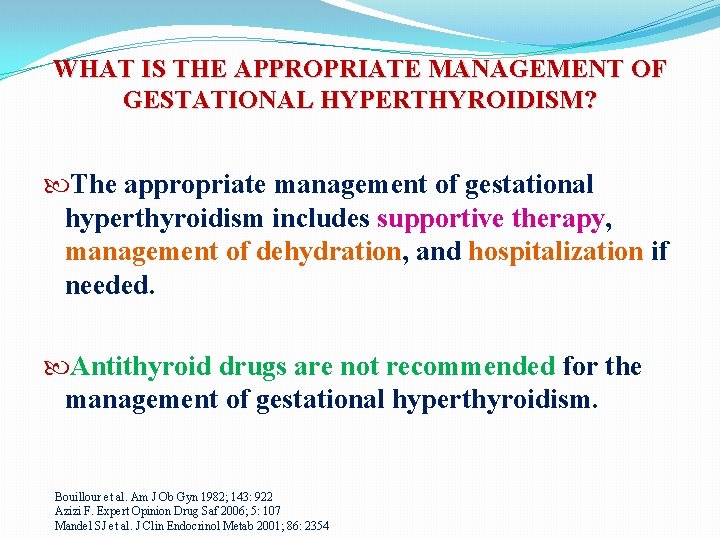
WHAT IS THE APPROPRIATE MANAGEMENT OF GESTATIONAL HYPERTHYROIDISM? The appropriate management of gestational hyperthyroidism includes supportive therapy, management of dehydration, and hospitalization if needed. Antithyroid drugs are not recommended for the management of gestational hyperthyroidism. Bouillour et al. Am J Ob Gyn 1982; 143: 922 Azizi F. Expert Opinion Drug Saf 2006; 5: 107 Mandel SJ et al. J Clin Endocrinol Metab 2001; 86: 2354
WHAT IS THE RECOMMENDED MANAGEMENT OF GRAVES’ HYPERTHYROIDISM IN PREGNANCY? Antithyroid drugs are the mainstay of therapy for hyperthyroidism during pregnancy Azizi F. Expert Opin Daug saf 2006; 5: 107 Mandel SJ et al. J Clin Endocrinol Metab 2001; 86: 2354

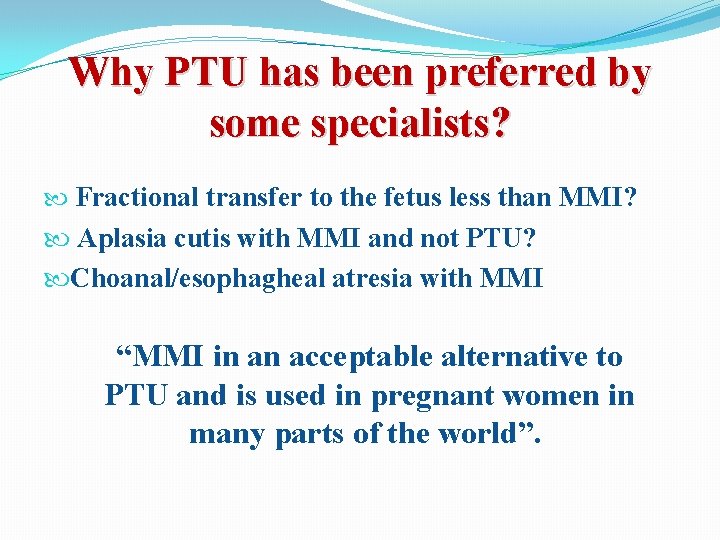
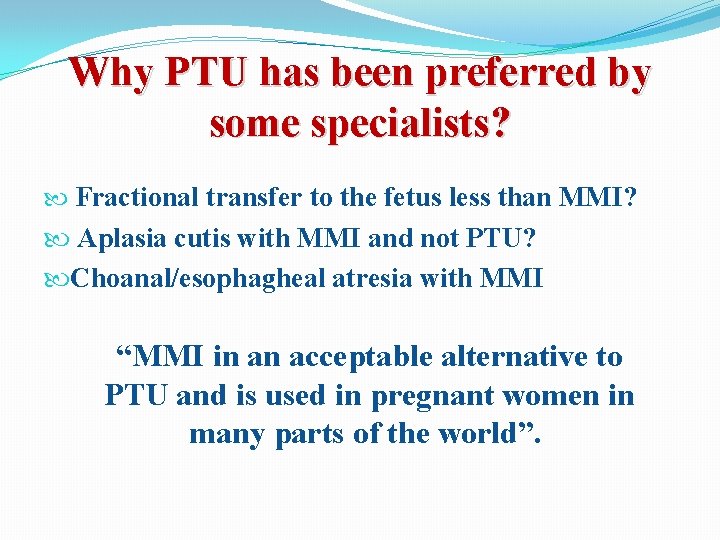
Why PTU has been preferred by some specialists? Fractional transfer to the fetus less than MMI? Aplasia cutis with MMI and not PTU? Choanal/esophagheal atresia with MMI “MMI in an acceptable alternative to PTU and is used in pregnant women in many parts of the world”.
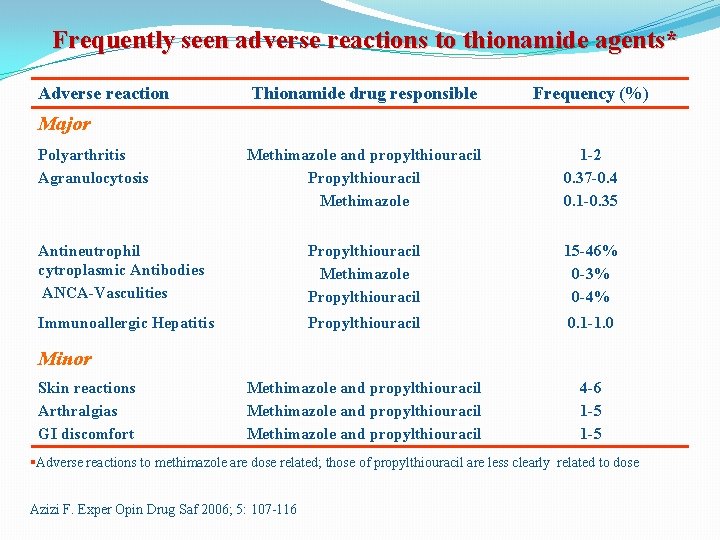
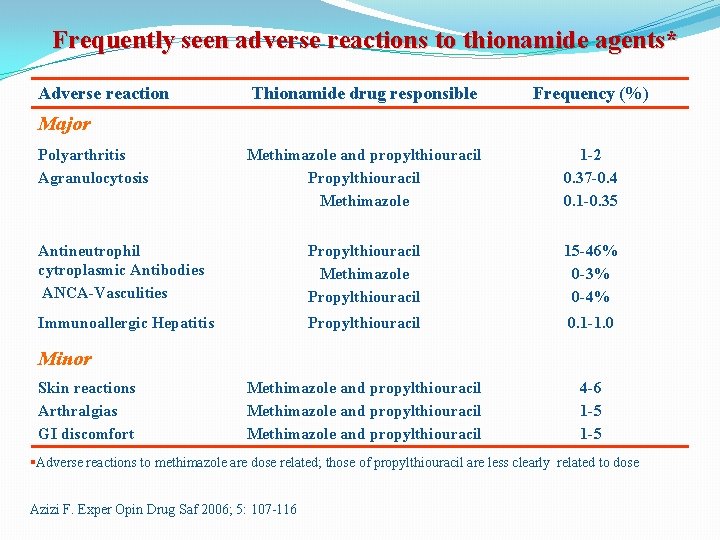
Frequently seen adverse reactions to thionamide agents* Adverse reaction Thionamide drug responsible Frequency (%) Methimazole and propylthiouracil Propylthiouracil Methimazole 1 -2 0. 37 -0. 4 0. 1 -0. 35 Antineutrophil cytroplasmic Antibodies ANCA-Vasculities Propylthiouracil Methimazole Propylthiouracil 15 -46% 0 -3% 0 -4% Immunoallergic Hepatitis Propylthiouracil 0. 1 -1. 0 Methimazole and propylthiouracil 4 -6 1 -5 Major Polyarthritis Agranulocytosis Minor Skin reactions Arthralgias GI discomfort §Adverse reactions to methimazole are dose related; those of propylthiouracil are less clearly related to dose Azizi F. Exper Opin Drug Saf 2006; 5: 107 -116
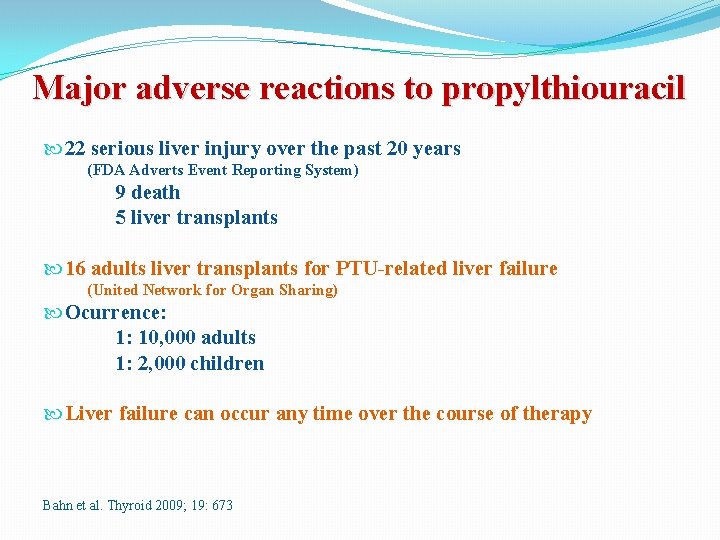
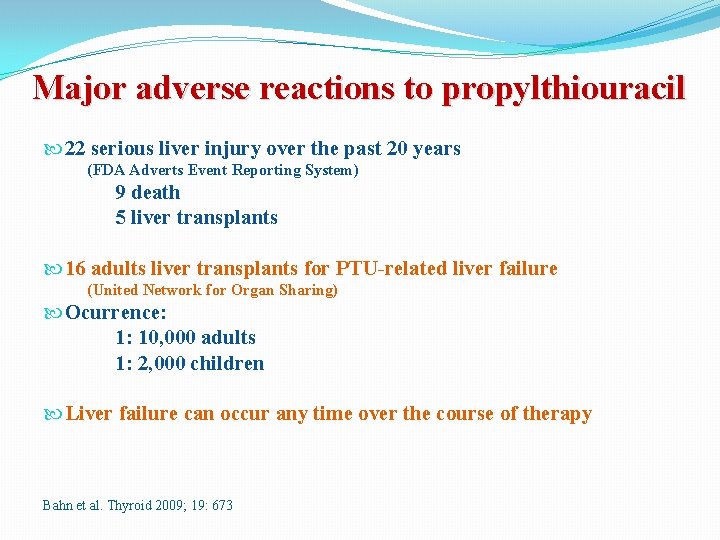
Major adverse reactions to propylthiouracil 22 serious liver injury over the past 20 years (FDA Adverts Event Reporting System) 9 death 5 liver transplants 16 adults liver transplants for PTU-related liver failure (United Network for Organ Sharing) Ocurrence: 1: 10, 000 adults 1: 2, 000 children Liver failure can occur any time over the course of therapy Bahn et al. Thyroid 2009; 19: 673
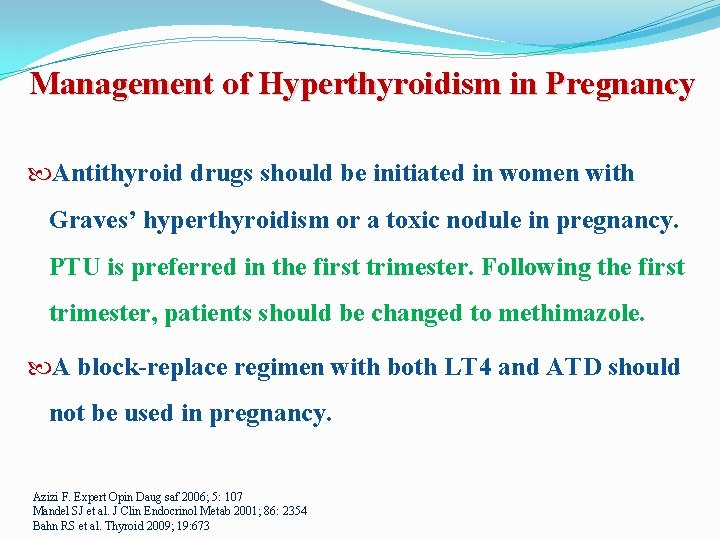
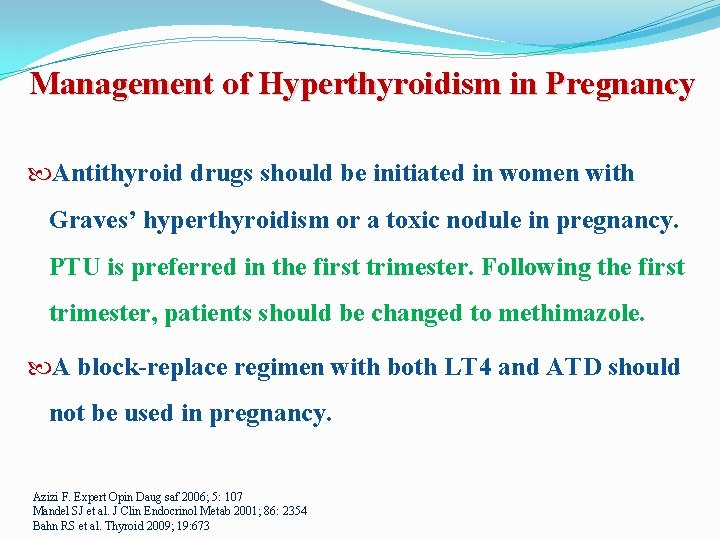
Management of Hyperthyroidism in Pregnancy Antithyroid drugs should be initiated in women with Graves’ hyperthyroidism or a toxic nodule in pregnancy. PTU is preferred in the first trimester. Following the first trimester, patients should be changed to methimazole. A block-replace regimen with both LT 4 and ATD should not be used in pregnancy. Azizi F. Expert Opin Daug saf 2006; 5: 107 Mandel SJ et al. J Clin Endocrinol Metab 2001; 86: 2354 Bahn RS et al. Thyroid 2009; 19: 673
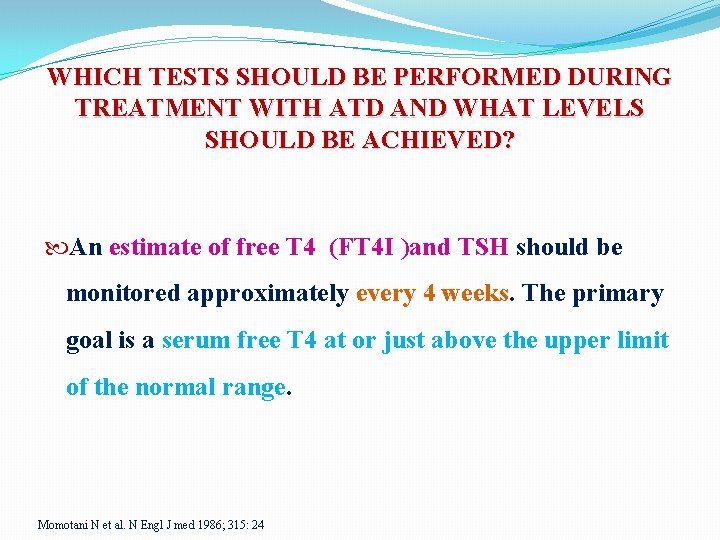
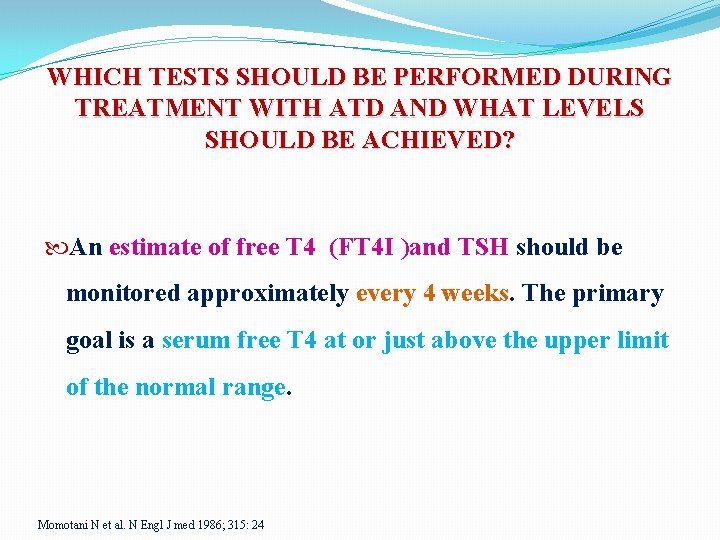
WHICH TESTS SHOULD BE PERFORMED DURING TREATMENT WITH ATD AND WHAT LEVELS SHOULD BE ACHIEVED? An estimate of free T 4 (FT 4 I )and TSH should be monitored approximately every 4 weeks. The primary goal is a serum free T 4 at or just above the upper limit of the normal range. Momotani N et al. N Engl J med 1986; 315: 24
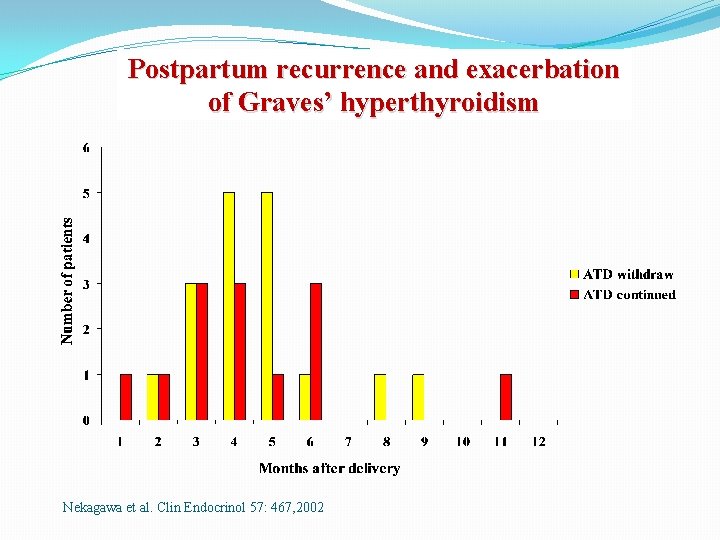
Should anithyroid drug therapy be discontinued in the last part of pregnancy? Can postpartum recurrence of Graves’ disease be prevented by the continuation of antithyroidis during pregnancy?
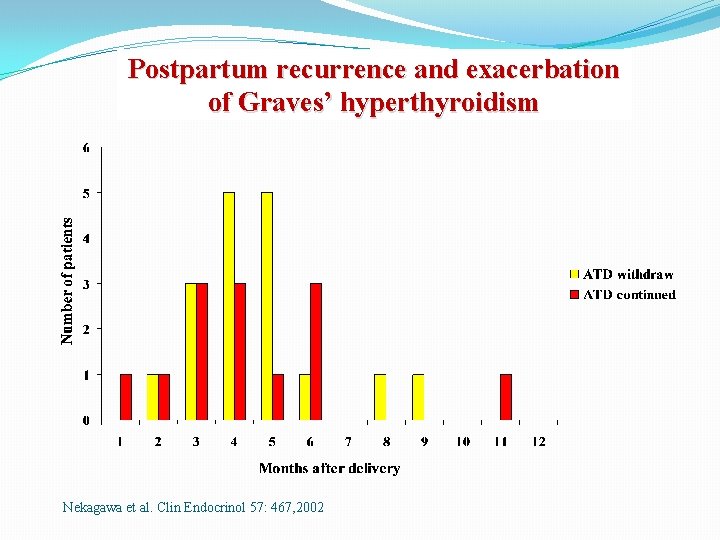
Postpartum recurrence and exacerbation of Graves’ hyperthyroidism Nekagawa et al. Clin Endocrinol 57: 467, 2002
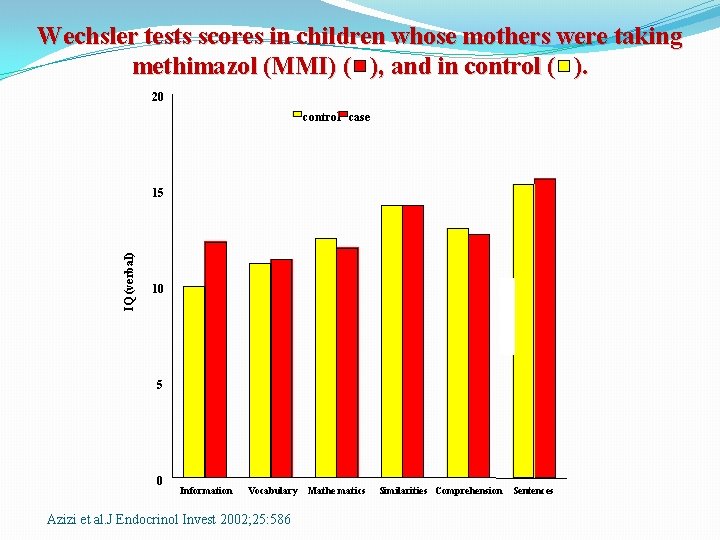
What are the long-term effects of antithyroid treatment in pregnancy on growth, intellectual development and thyroid function of the offspring?
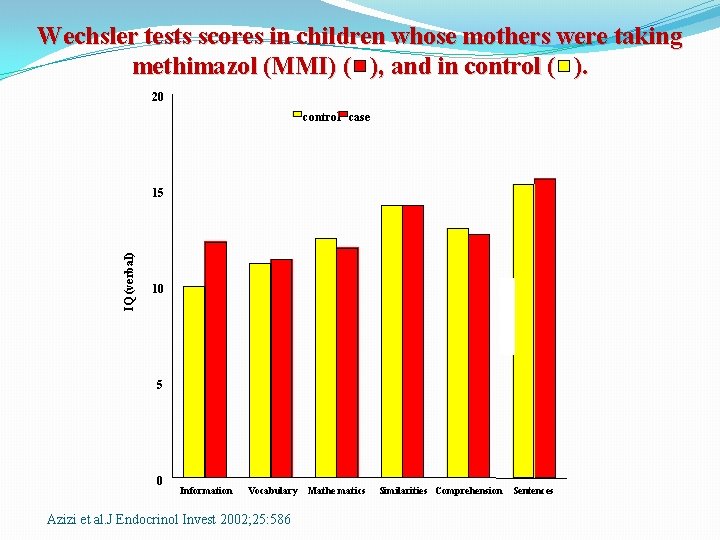
Wechsler tests scores in children whose mothers were taking methimazol (MMI) ( ), and in control ( ). 20 control case IQ (verbal) 15 10 5 0 Information Vocabulary Azizi et al. J Endocrinol Invest 2002; 25: 586 Mathe matics Similarities Comprehension Sentences
WHAT ARE THE INDICATIONS AND TIMING FOR THYROIDECTOMY IN THE MANAGEMENT OF GRAVES’ DISEASE IN HYPERTHYROIDISM? Thyroidectomy in pregnancy is rarely indicated. If required, the optimal time for thyroidectomy is in the second trimester.
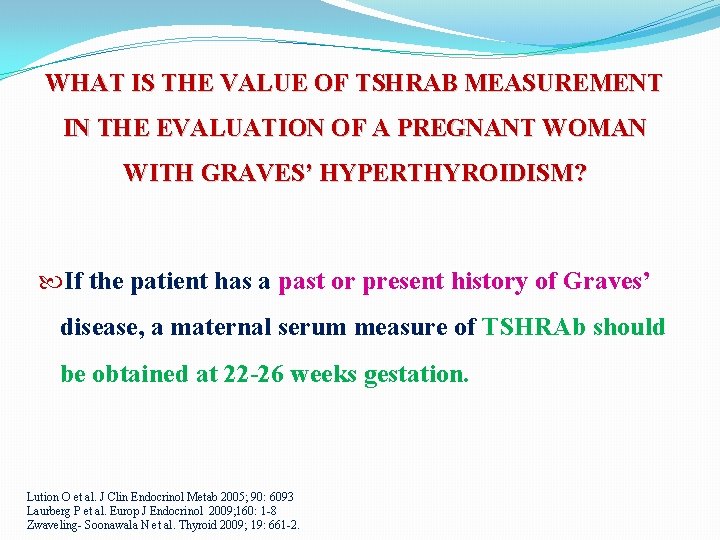
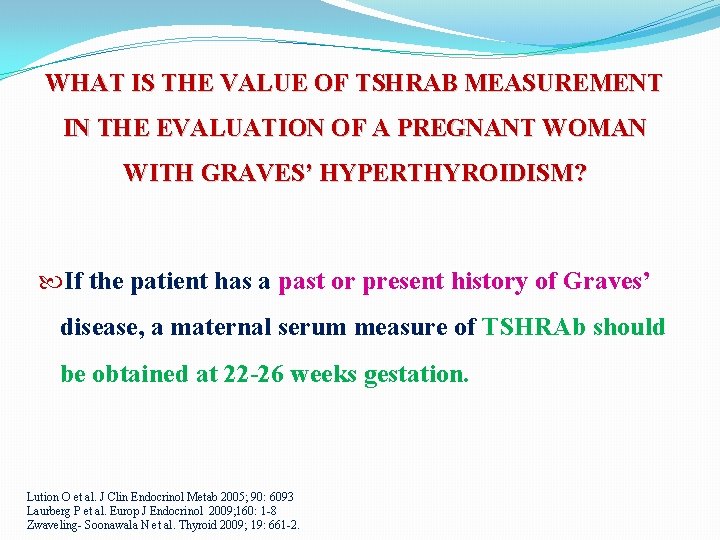
WHAT IS THE VALUE OF TSHRAB MEASUREMENT IN THE EVALUATION OF A PREGNANT WOMAN WITH GRAVES’ HYPERTHYROIDISM? If the patient has a past or present history of Graves’ disease, a maternal serum measure of TSHRAb should be obtained at 22 -26 weeks gestation. Lution O et al. J Clin Endocrinol Metab 2005; 90: 6093 Laurberg P et al. Europ J Endocrinol 2009; 160: 1 -8 Zwaveling- Soonawala N et al. Thyroid 2009; 19: 661 -2.
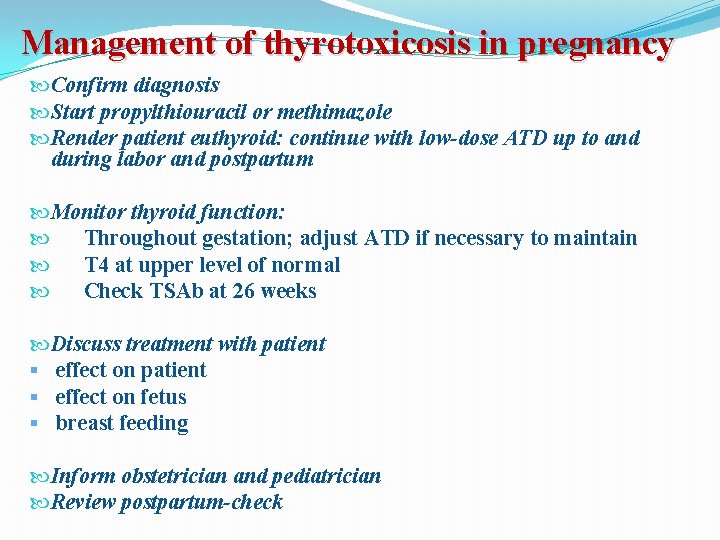
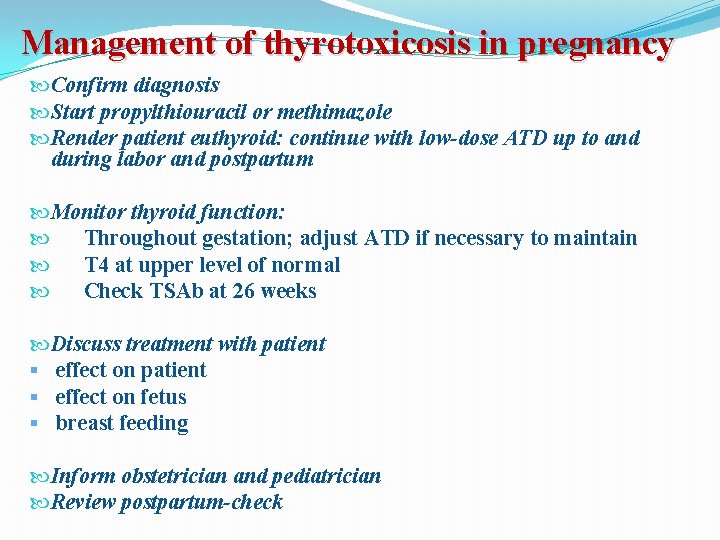
Management of thyrotoxicosis in pregnancy Confirm diagnosis Start propylthiouracil or methimazole Render patient euthyroid: continue with low-dose ATD up to and during labor and postpartum Monitor thyroid function: Throughout gestation; adjust ATD if necessary to maintain T 4 at upper level of normal Check TSAb at 26 weeks Discuss treatment with patient § effect on fetus § breast feeding Inform obstetrician and pediatrician Review postpartum-check
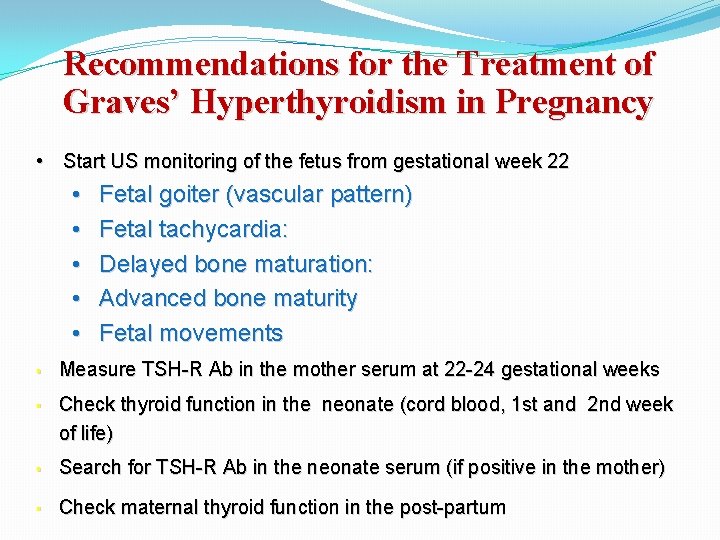
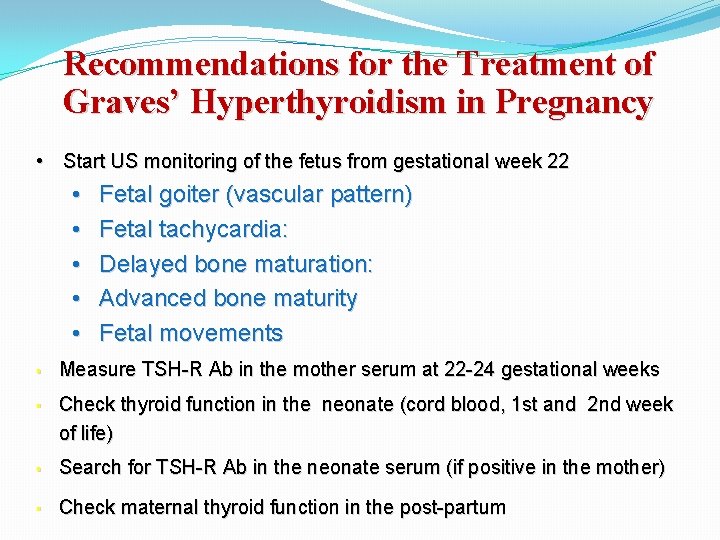
Recommendations for the Treatment of Graves’ Hyperthyroidism in Pregnancy • Start US monitoring of the fetus from gestational week 22 • • • § § Fetal goiter (vascular pattern) Fetal tachycardia: Delayed bone maturation: Advanced bone maturity Fetal movements Measure TSH-R Ab in the mother serum at 22 -24 gestational weeks Check thyroid function in the neonate (cord blood, 1 st and 2 nd week of life) § Search for TSH-R Ab in the neonate serum (if positive in the mother) § Check maternal thyroid function in the post-partum
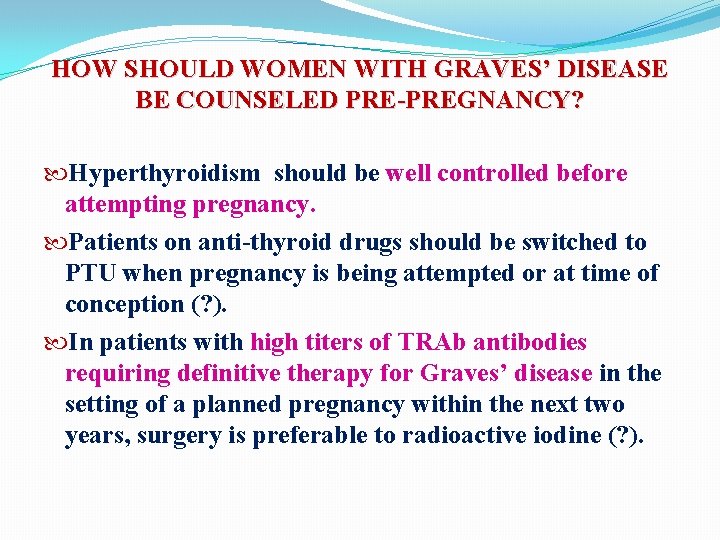
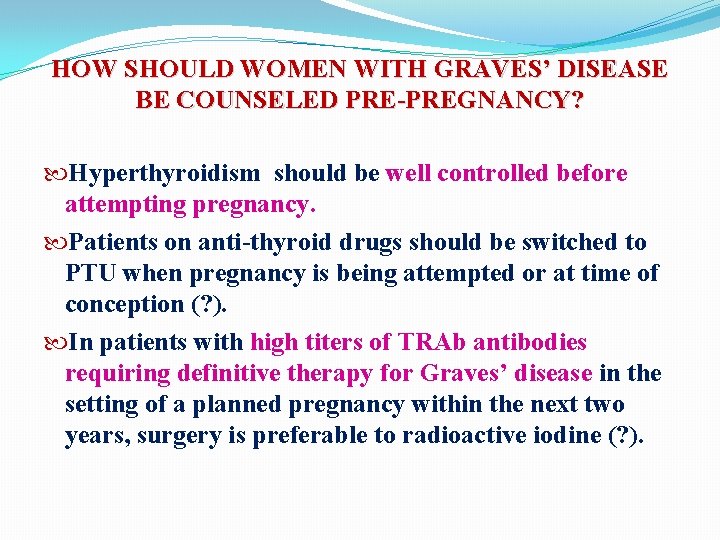
HOW SHOULD WOMEN WITH GRAVES’ DISEASE BE COUNSELED PRE-PREGNANCY? Hyperthyroidism should be well controlled before attempting pregnancy. Patients on anti-thyroid drugs should be switched to PTU when pregnancy is being attempted or at time of conception (? ). In patients with high titers of TRAb antibodies requiring definitive therapy for Graves’ disease in the setting of a planned pregnancy within the next two years, surgery is preferable to radioactive iodine (? ).
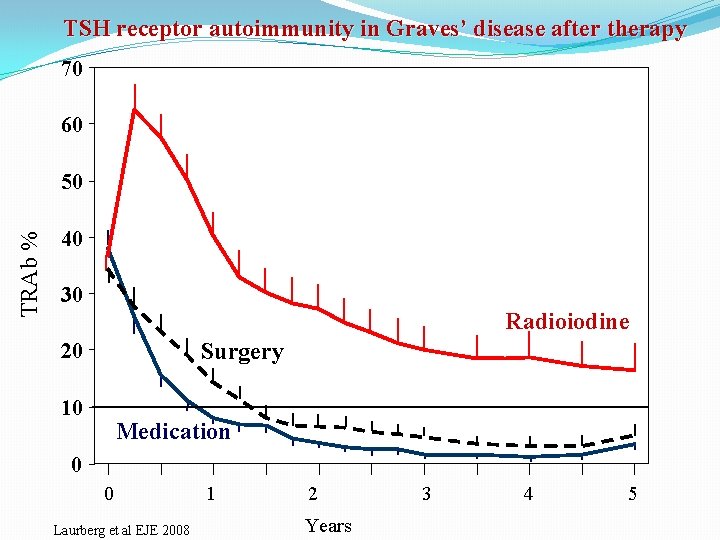
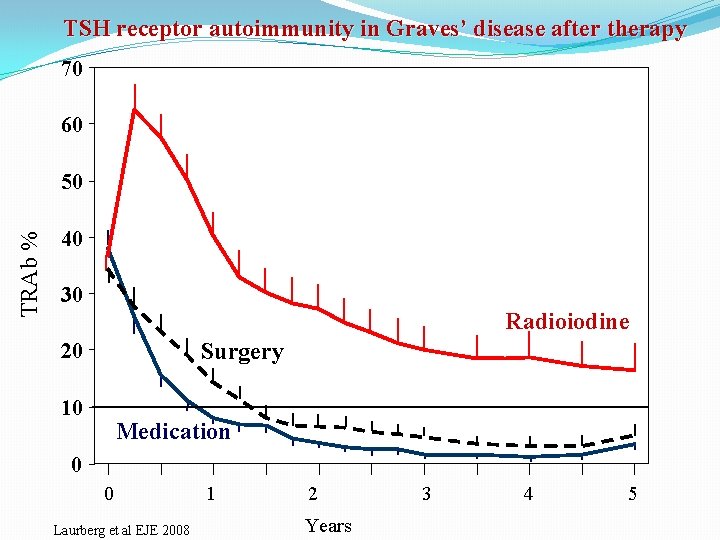
TSH receptor autoimmunity in Graves’ disease after therapy 70 60 TRAb % 50 40 30 Radioiodine Surgery 20 10 Medication 0 0 Laurberg et al EJE 2008 1 2 Years 3 4 5
HOW SHOULD GRAVES’ HYPERTHYROIDISM BE TREATED IN LACTATING WOMEN? Methimazole in doses up to 20 -30 mg daily is safe for lactating mothers and their infants. PTU is a second-line agent due to concerns about severe hepatotoxicity, but is safe for lactating mothers and their infants in doses up to 300 mg daily. Azizi F et al J Endocrinol Invest 2006; 29: 244 Azizi F et al. J Ped Endocrinol Metab 2003; 16: 1239 Azizi F et al. J Clin Endocrinol Metab 2000; 85: 3233
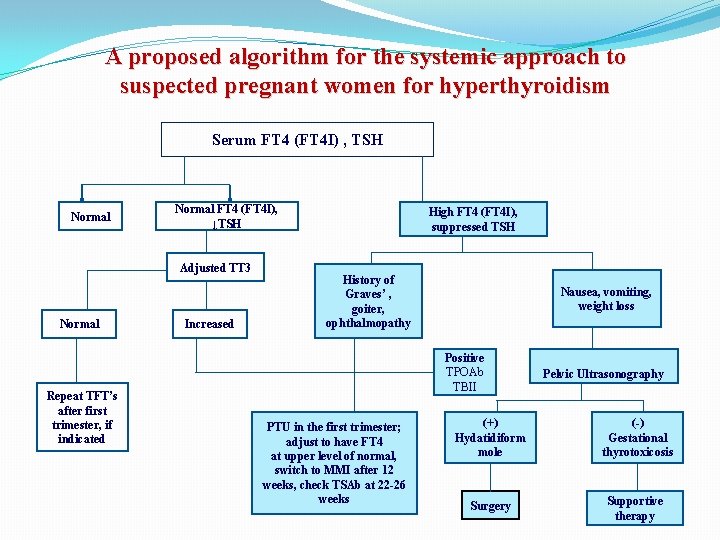
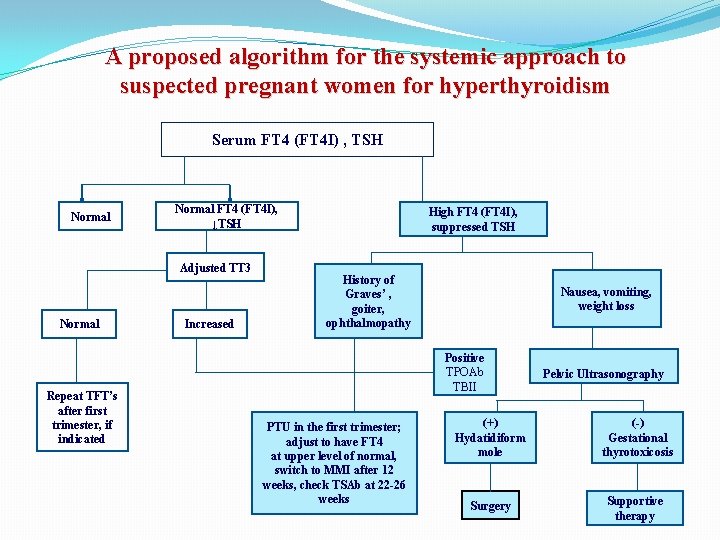
A proposed algorithm for the systemic approach to suspected pregnant women for hyperthyroidism Serum FT 4 (FT 4 I) , TSH Normal FT 4 (FT 4 I), ↓TSH Adjusted TT 3 Normal Repeat TFT’s after first trimester, if indicated Increased High FT 4 (FT 4 I), suppressed TSH History of Graves’ , goiter, ophthalmopathy Nausea, vomiting, weight loss Positive TPOAb TBII PTU in the first trimester; adjust to have FT 4 at upper level of normal, switch to MMI after 12 weeks, check TSAb at 22 -26 weeks Pelvic Ultrasonography (+) Hydatidiform mole (-) Gestational thyrotoxicosis Surgery Supportive therapy
Conclusion § Thyroid diseases, both clinical and subclinical, are common during pregnancy and postpartum and influence the health of mother, fetus and infant. § Effective evidence based strategies for both detection and management should be developed for the benefit of both mother and child. § Prompt and appropriate treatment of thyroid disease could dramatically improve the pregnancy outcome and ensure health promotion for mother and infant.

Thank You
 Fereidoun azizi
Fereidoun azizi Hypothyroidism treatment
Hypothyroidism treatment Definition of spotting during pregnancy
Definition of spotting during pregnancy Sadoon azizi
Sadoon azizi Sadoon azizi
Sadoon azizi Hypothyroidism complications
Hypothyroidism complications Hyperthyroidism primary and secondary
Hyperthyroidism primary and secondary Euthyriod
Euthyriod Sick euthyroid
Sick euthyroid Management of hyperthyroidism
Management of hyperthyroidism Subclinical hyperthyroidism
Subclinical hyperthyroidism Amiodarone thyroid toxicity
Amiodarone thyroid toxicity Management of hyperthyroidism
Management of hyperthyroidism Type of hyperthyroidism
Type of hyperthyroidism Thyroid scintigraphy
Thyroid scintigraphy Thyroxine function
Thyroxine function Hyperthyroidism in babies
Hyperthyroidism in babies Thyroid symptoms
Thyroid symptoms Hyperthyroidism treatment
Hyperthyroidism treatment Causes of hypothyroidism
Causes of hypothyroidism Lesson 6 employee health status
Lesson 6 employee health status Hijama for autoimmune disease
Hijama for autoimmune disease Sagar institute of research and technology
Sagar institute of research and technology Electronics and telecommunications research institute
Electronics and telecommunications research institute Target institute of medical education and research
Target institute of medical education and research Prof ram meghe institute of technology and research
Prof ram meghe institute of technology and research Swedish national road and transport research institute
Swedish national road and transport research institute Kirdi departments
Kirdi departments Picme2.0
Picme2.0 Iso 22301 utbildning
Iso 22301 utbildning Novell typiska drag
Novell typiska drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Returpilarna
Returpilarna Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Tidbok för yrkesförare
Tidbok för yrkesförare A gastrica
A gastrica Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild