Endocrine Physiology and Disorders Endocrine Systems l Intercellular

- Slides: 51
Endocrine Physiology and Disorders
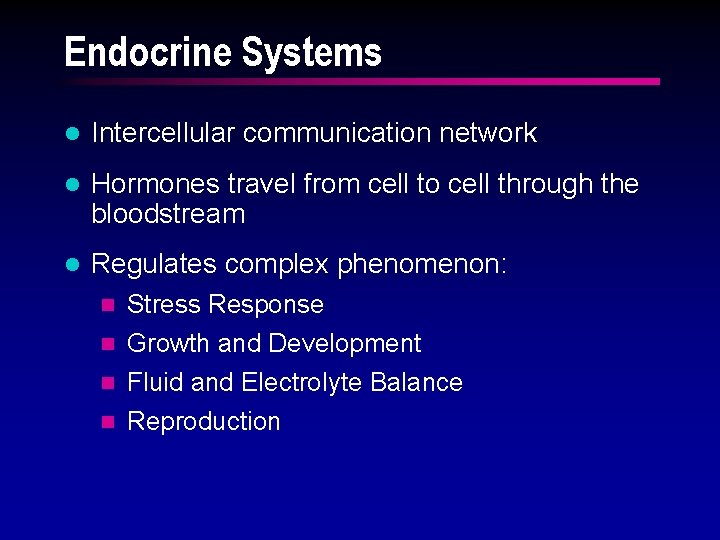
Endocrine Systems l Intercellular communication network l Hormones travel from cell to cell through the bloodstream l Regulates complex phenomenon: Stress Response n Growth and Development n Fluid and Electrolyte Balance n Reproduction n
Solubility of Hormones Determines Mechanism of Action l Lipid soluble hormones steroid n thyroid n l Water soluble hormones proteins and peptides n catecholamines n
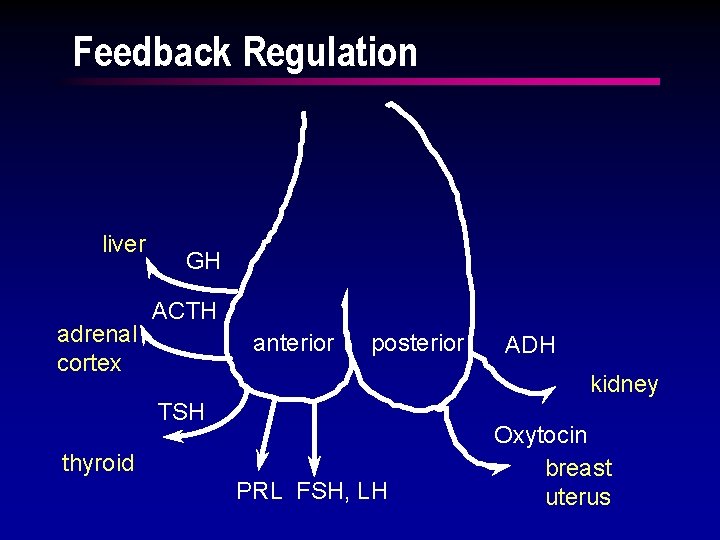
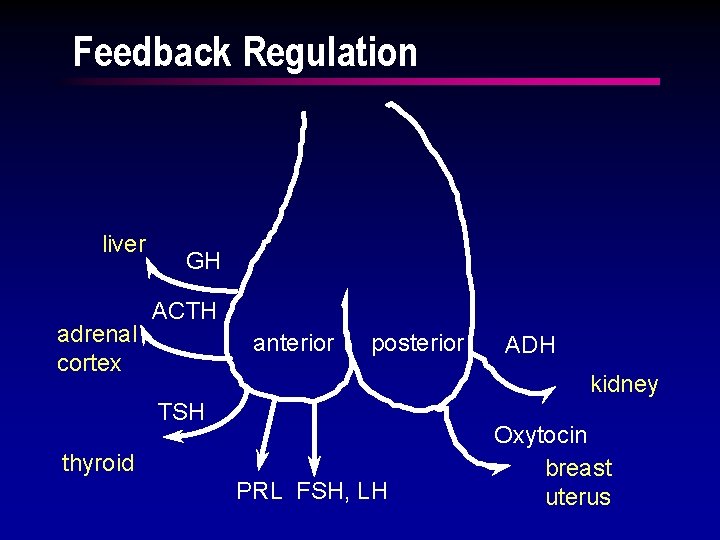
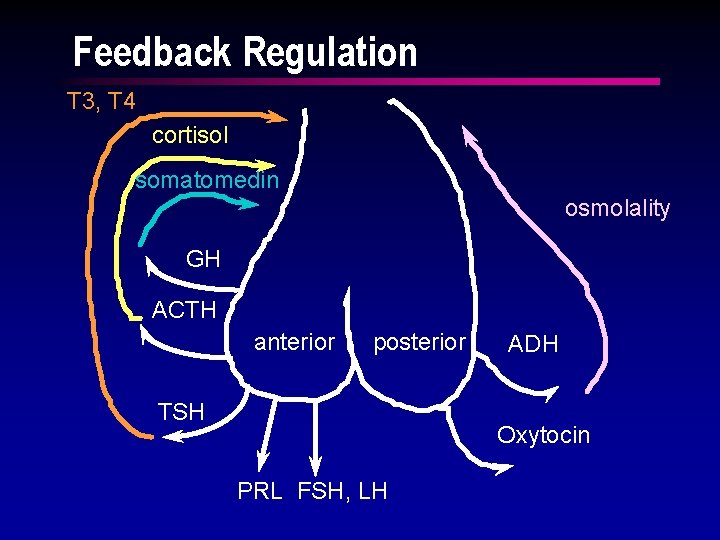
Feedback Regulation liver adrenal cortex GH ACTH anterior posterior ADH kidney TSH thyroid PRL FSH, LH Oxytocin breast uterus
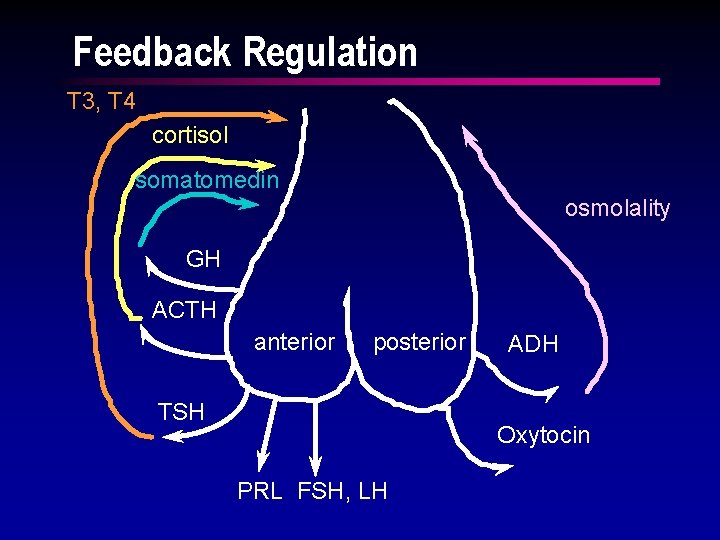
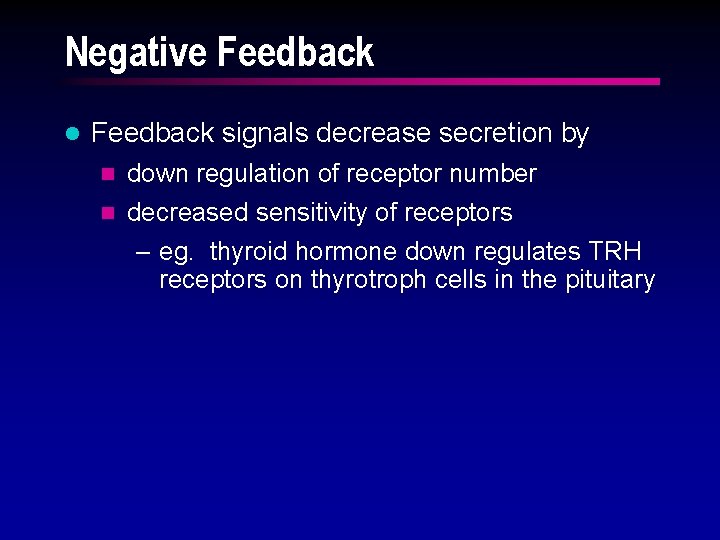
Feedback Regulation T 3, T 4 cortisol somatomedin osmolality GH ACTH anterior posterior TSH ADH Oxytocin PRL FSH, LH
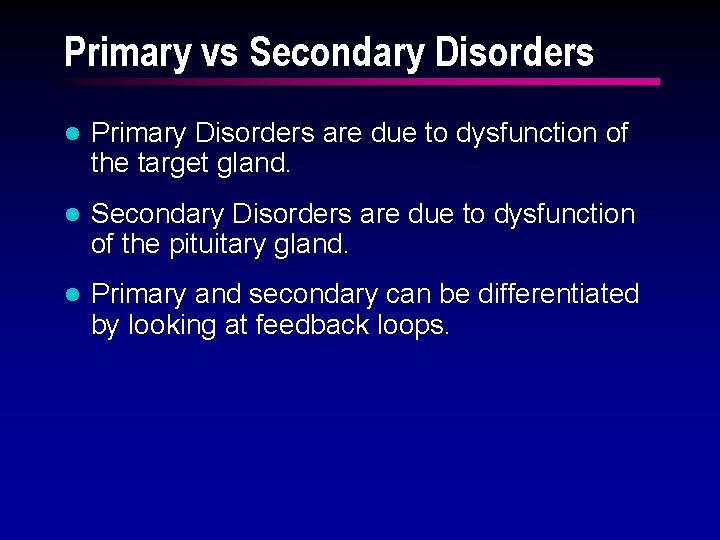
Negative Feedback l Feedback signals decrease secretion by n down regulation of receptor number n decreased sensitivity of receptors – eg. thyroid hormone down regulates TRH receptors on thyrotroph cells in the pituitary
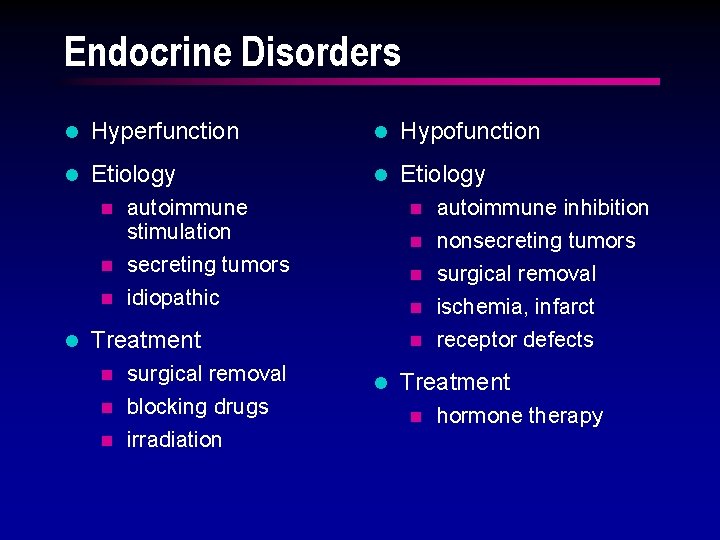
Primary vs Secondary Disorders l Primary Disorders are due to dysfunction of the target gland. l Secondary Disorders are due to dysfunction of the pituitary gland. l Primary and secondary can be differentiated by looking at feedback loops.
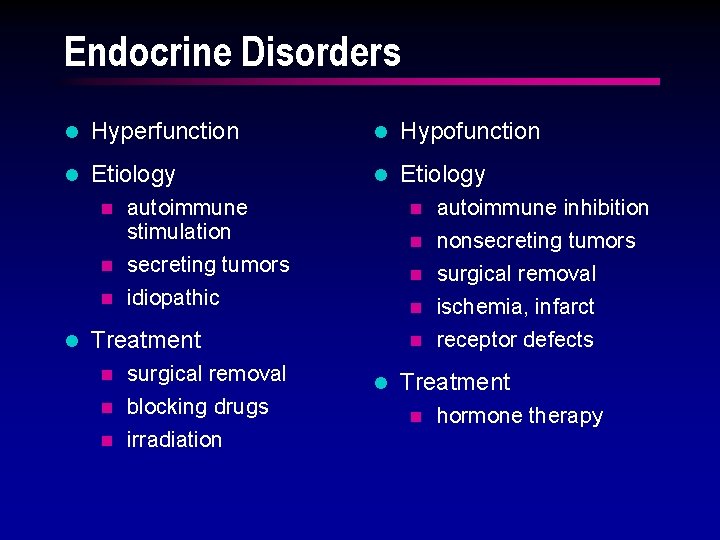
Endocrine Disorders l Hyperfunction l Hypofunction l Etiology autoimmune stimulation n secreting tumors n idiopathic autoimmune inhibition n nonsecreting tumors n l n surgical removal n ischemia, infarct n receptor defects n Treatment surgical removal n blocking drugs n irradiation n l Treatment n hormone therapy

Acromegaly l GH secreting pituitary adenoma n headache, visual disturbances hyperglycemia “diabetogenic” n increased lean body mass – bone and soft tissue n l Treatment hypophysectomy n irradiation n
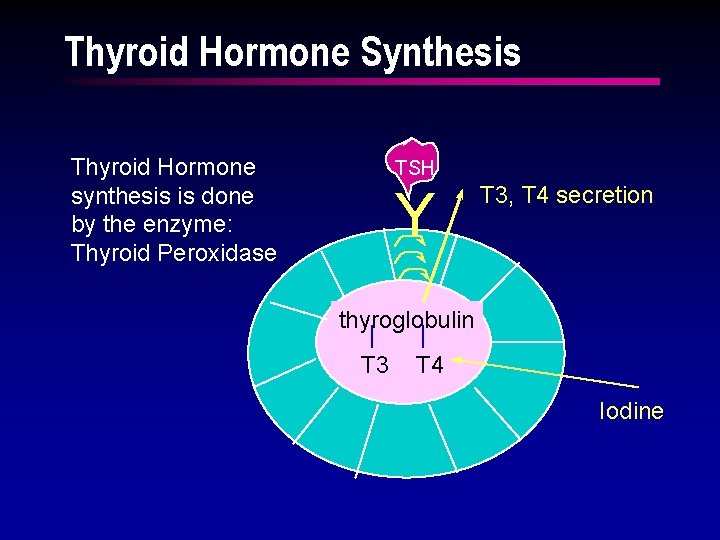
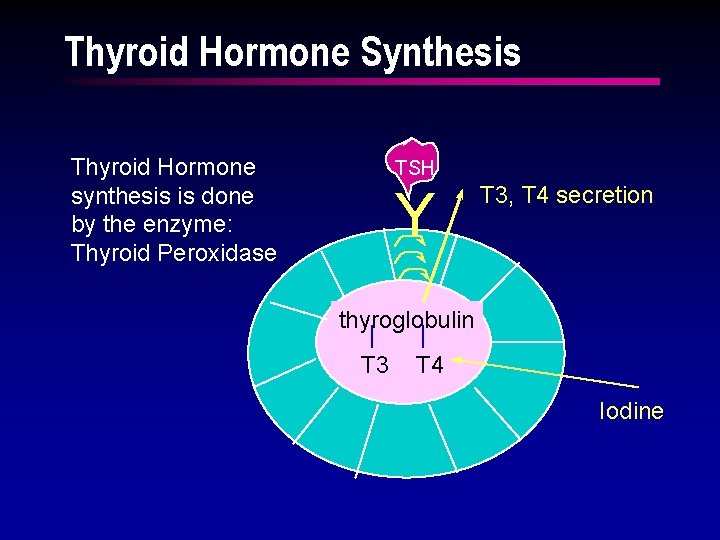
Thyroid Hormone Synthesis Thyroid Hormone synthesis is done by the enzyme: Thyroid Peroxidase TSH Y T 3, T 4 secretion thyroglobulin T 3 T 4 Iodine
Triiodothyronine and Thyroxine l About 90% is T 4 Most abundant l About 10% is T 3 Most biologically active
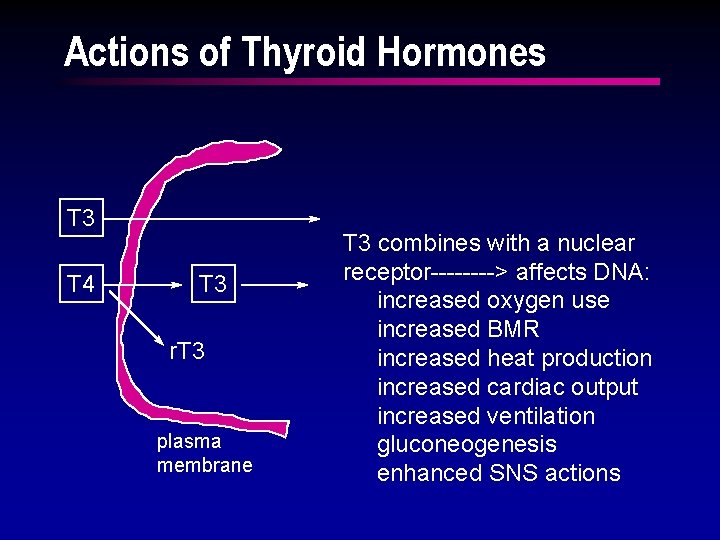
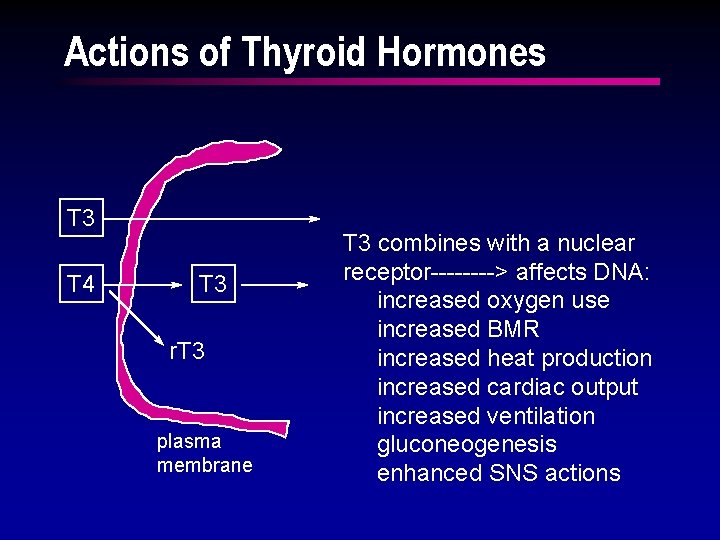
Actions of Thyroid Hormones T 3 T 4 T 3 r. T 3 plasma membrane T 3 combines with a nuclear receptor----> affects DNA: increased oxygen use increased BMR increased heat production increased cardiac output increased ventilation gluconeogenesis enhanced SNS actions
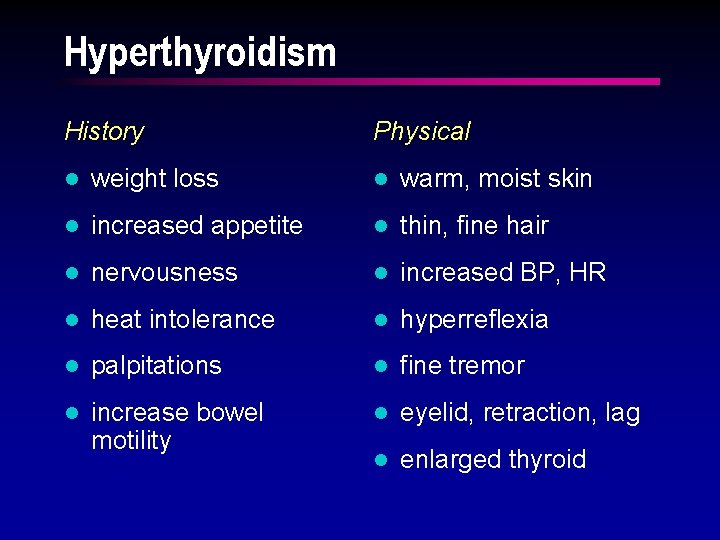
Hyperthyroidism History Physical l weight loss l warm, moist skin l increased appetite l thin, fine hair l nervousness l increased BP, HR l heat intolerance l hyperreflexia l palpitations l fine tremor l increase bowel motility l eyelid, retraction, lag l enlarged thyroid
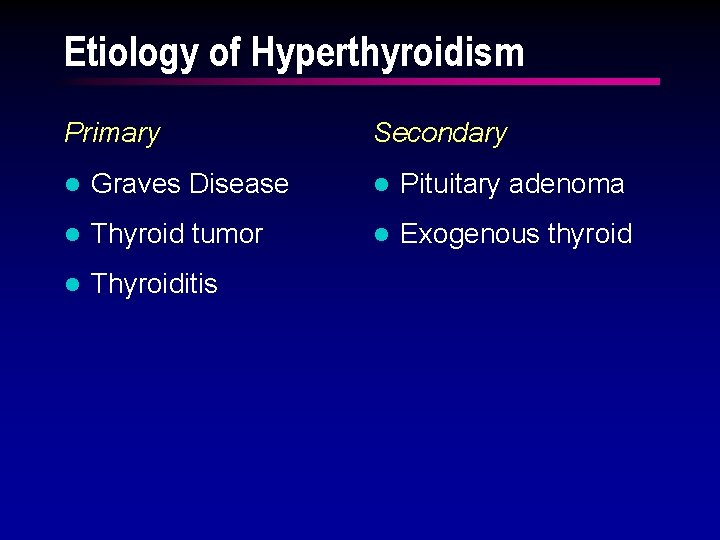
Etiology of Hyperthyroidism Primary Secondary l Graves Disease l Pituitary adenoma l Thyroid tumor l Exogenous thyroid l Thyroiditis
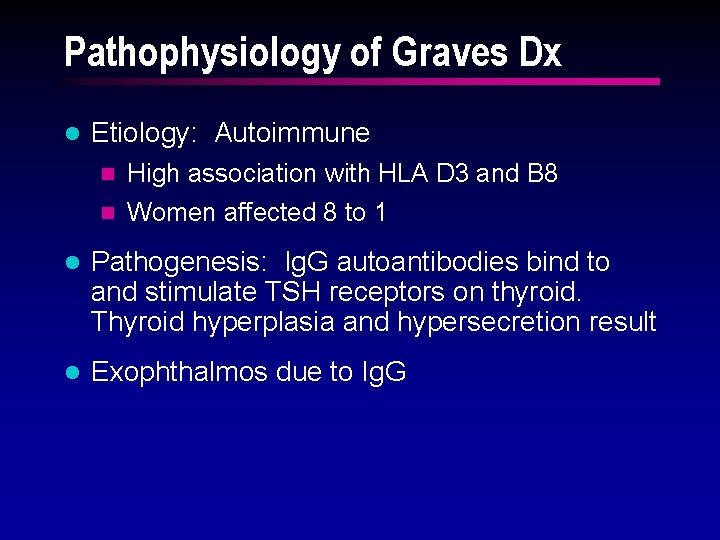
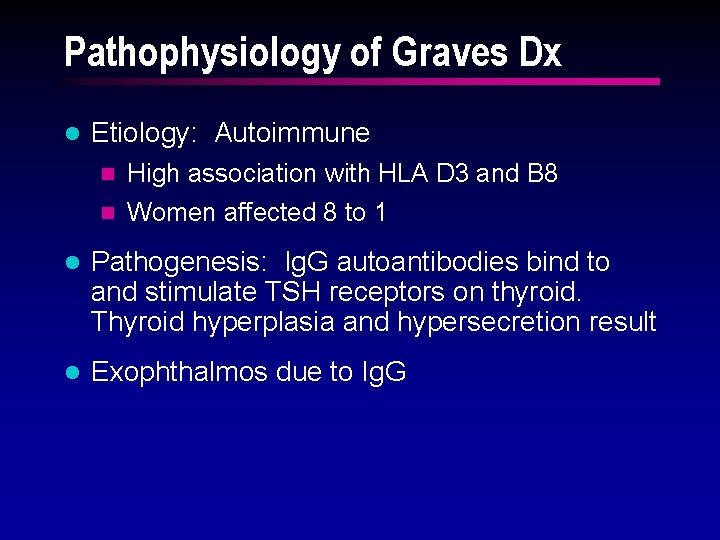
Pathophysiology of Graves Dx l Etiology: Autoimmune n High association with HLA D 3 and B 8 n Women affected 8 to 1 l Pathogenesis: Ig. G autoantibodies bind to and stimulate TSH receptors on thyroid. Thyroid hyperplasia and hypersecretion result l Exophthalmos due to Ig. G
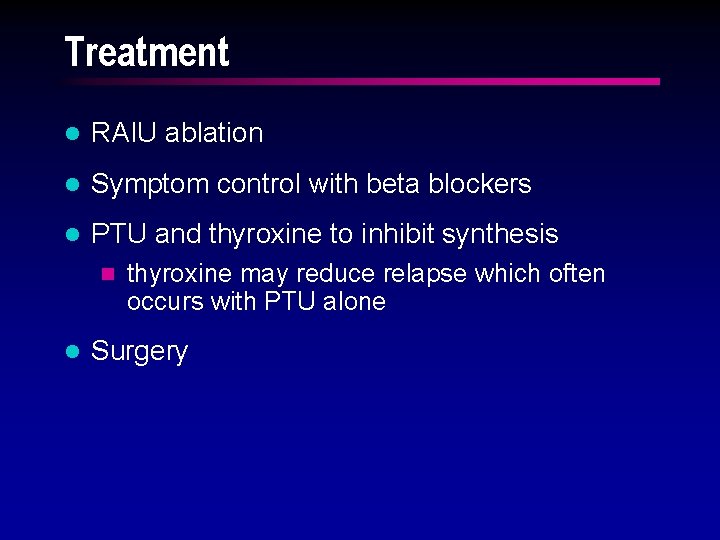
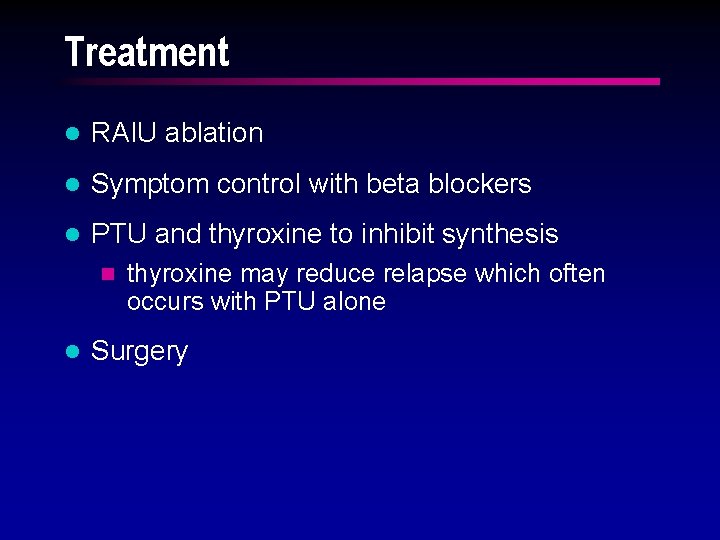
Treatment l RAIU ablation l Symptom control with beta blockers l PTU and thyroxine to inhibit synthesis n l thyroxine may reduce relapse which often occurs with PTU alone Surgery
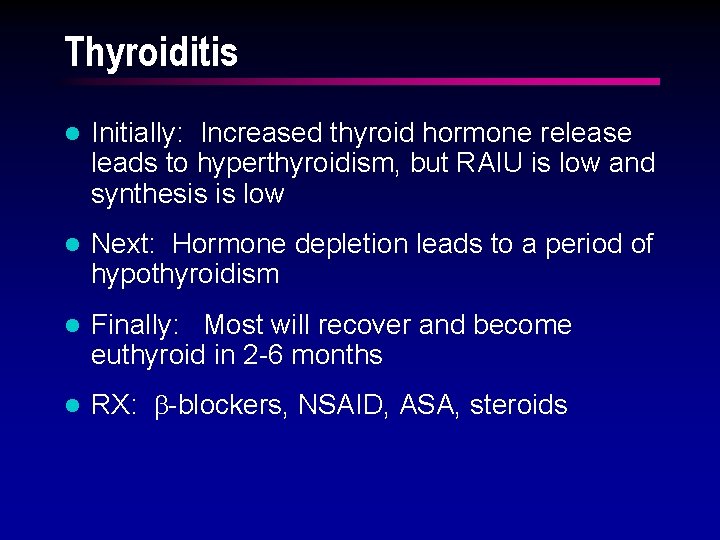
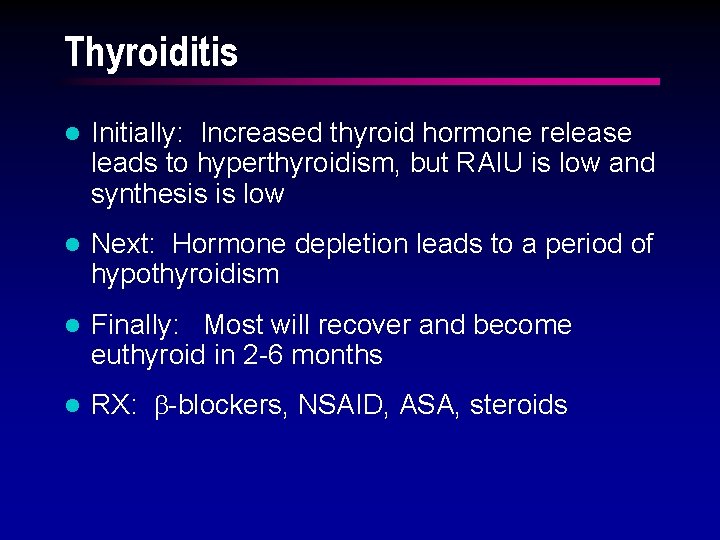
Thyroiditis l Initially: Increased thyroid hormone release leads to hyperthyroidism, but RAIU is low and synthesis is low l Next: Hormone depletion leads to a period of hypothyroidism l Finally: Most will recover and become euthyroid in 2 -6 months l RX: b-blockers, NSAID, ASA, steroids
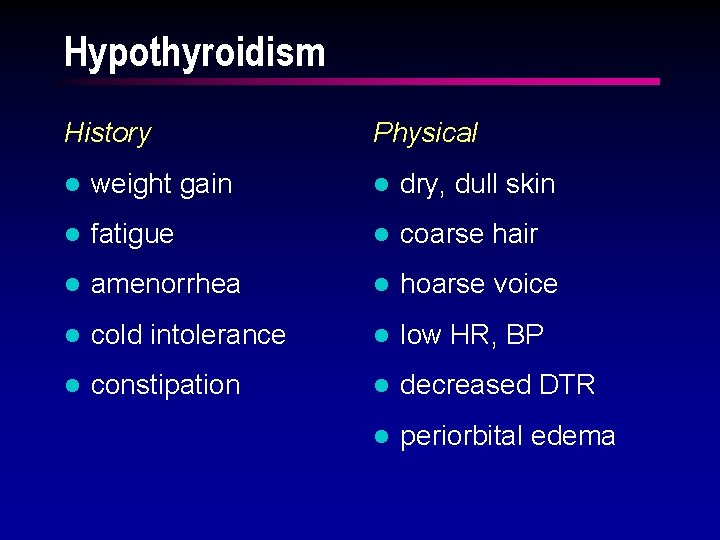
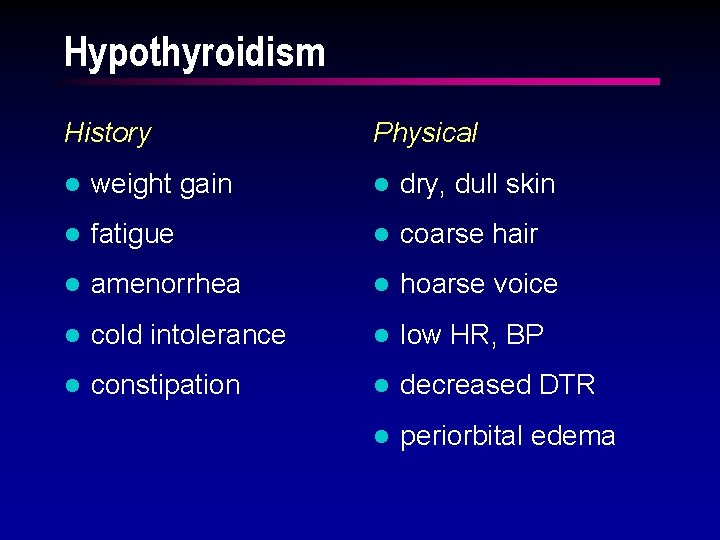
Hypothyroidism History Physical l weight gain l dry, dull skin l fatigue l coarse hair l amenorrhea l hoarse voice l cold intolerance l low HR, BP l constipation l decreased DTR l periorbital edema
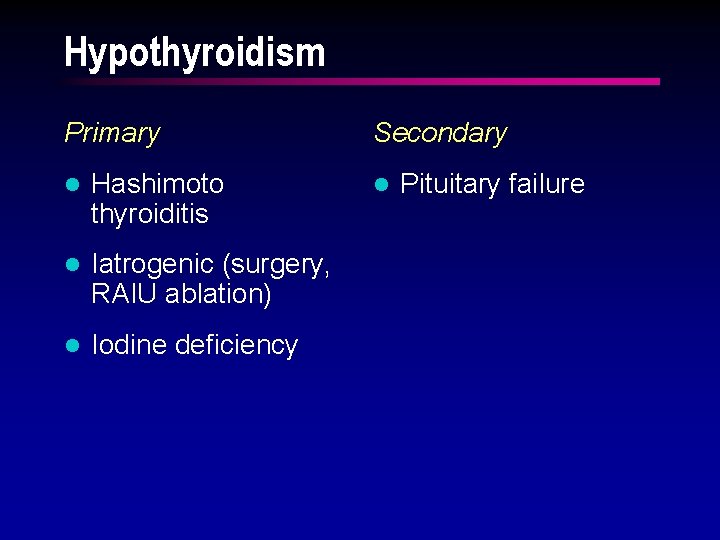
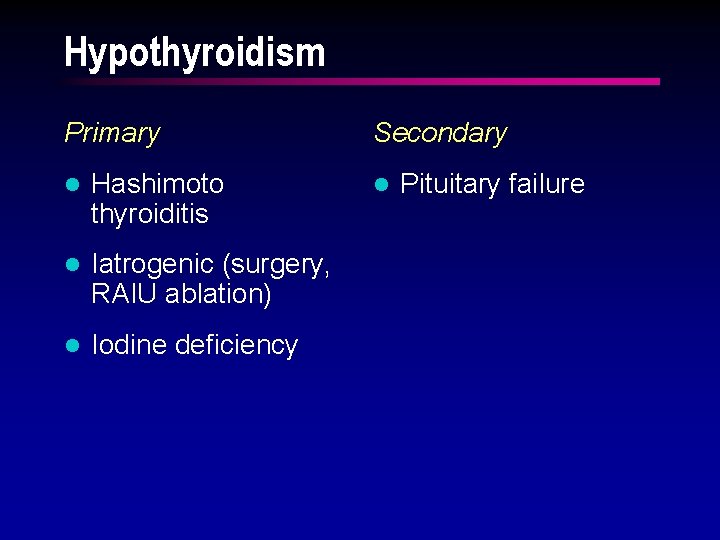
Hypothyroidism Primary l Hashimoto thyroiditis l Iatrogenic (surgery, RAIU ablation) l Iodine deficiency Secondary l Pituitary failure
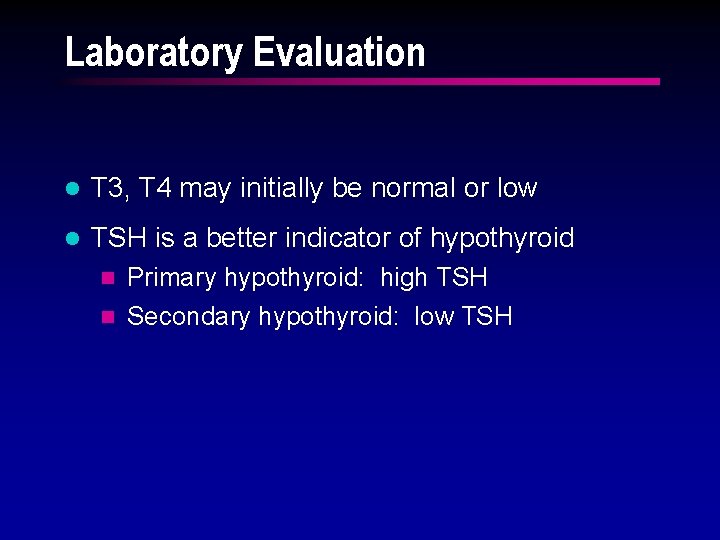
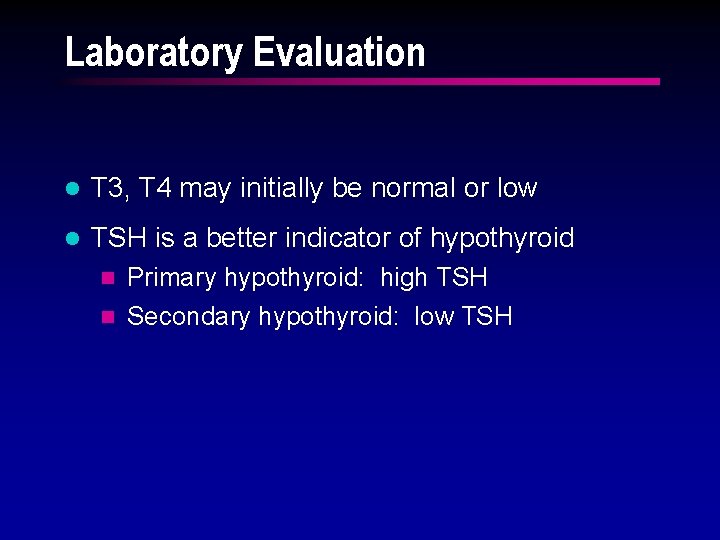
Laboratory Evaluation l T 3, T 4 may initially be normal or low l TSH is a better indicator of hypothyroid Primary hypothyroid: high TSH n Secondary hypothyroid: low TSH n
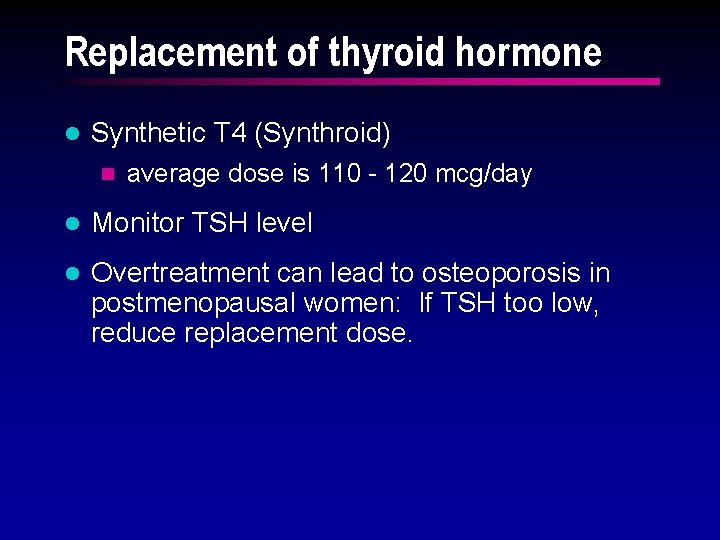
Replacement of thyroid hormone l Synthetic T 4 (Synthroid) n average dose is 110 - 120 mcg/day l Monitor TSH level l Overtreatment can lead to osteoporosis in postmenopausal women: If TSH too low, reduce replacement dose.
Adrenocortical Hormones l Sugar: glucocorticoids (cortisol) l Salt: mineralocorticoids (aldosterone) l Sex: androgens, estrogens
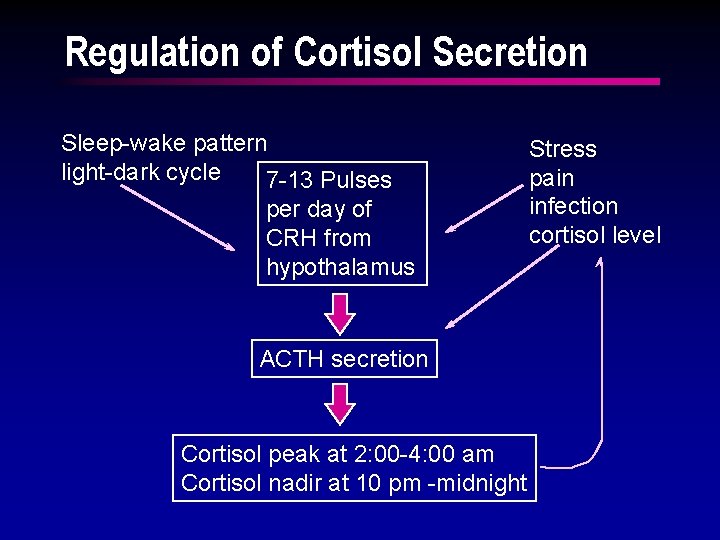
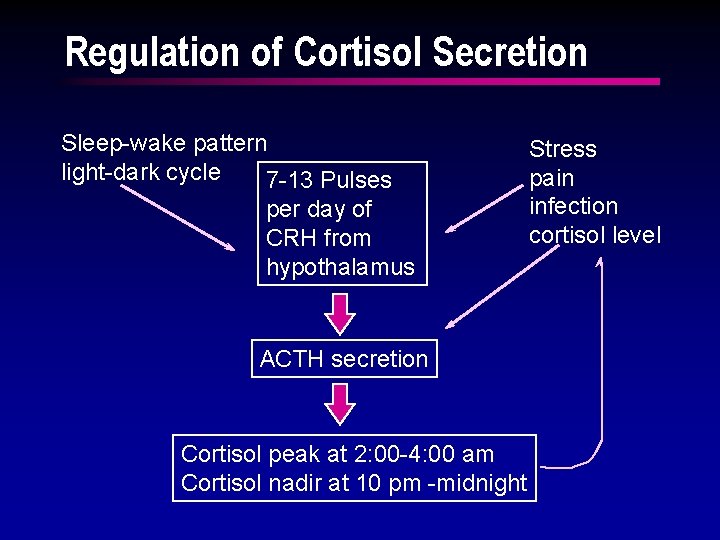
Regulation of Cortisol Secretion Sleep-wake pattern light-dark cycle 7 -13 Pulses per day of CRH from hypothalamus ACTH secretion Cortisol peak at 2: 00 -4: 00 am Cortisol nadir at 10 pm -midnight Stress pain infection cortisol level
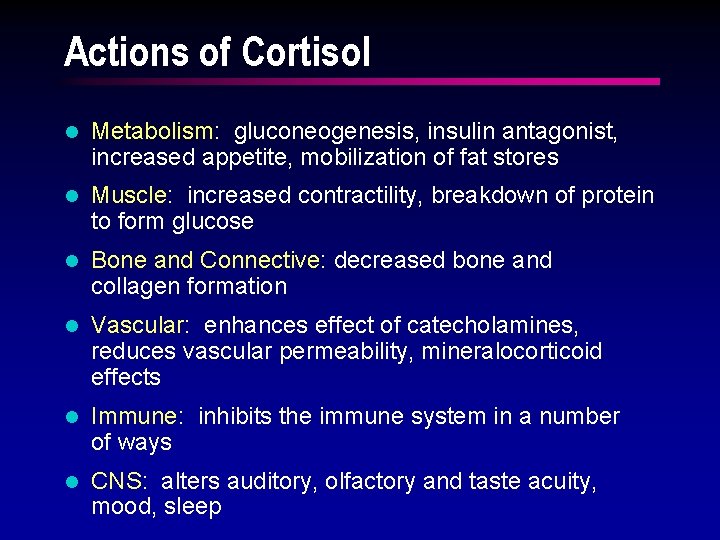
Actions of Cortisol l Metabolism: gluconeogenesis, insulin antagonist, increased appetite, mobilization of fat stores l Muscle: increased contractility, breakdown of protein to form glucose l Bone and Connective: decreased bone and collagen formation l Vascular: enhances effect of catecholamines, reduces vascular permeability, mineralocorticoid effects l Immune: inhibits the immune system in a number of ways l CNS: alters auditory, olfactory and taste acuity, mood, sleep
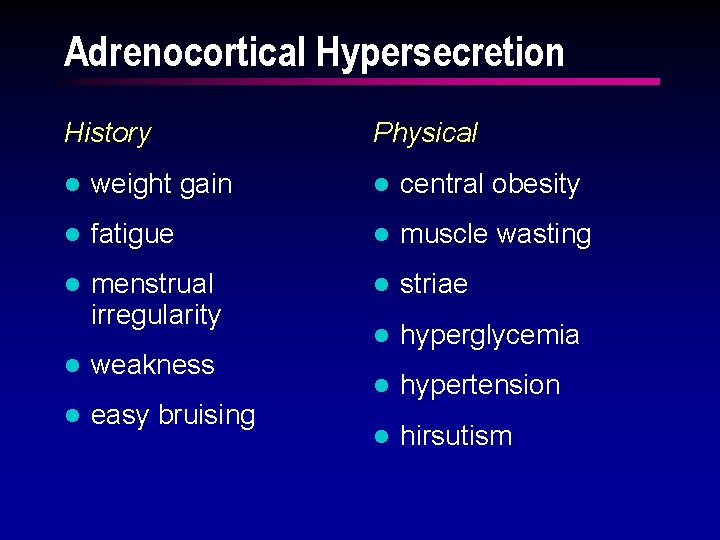
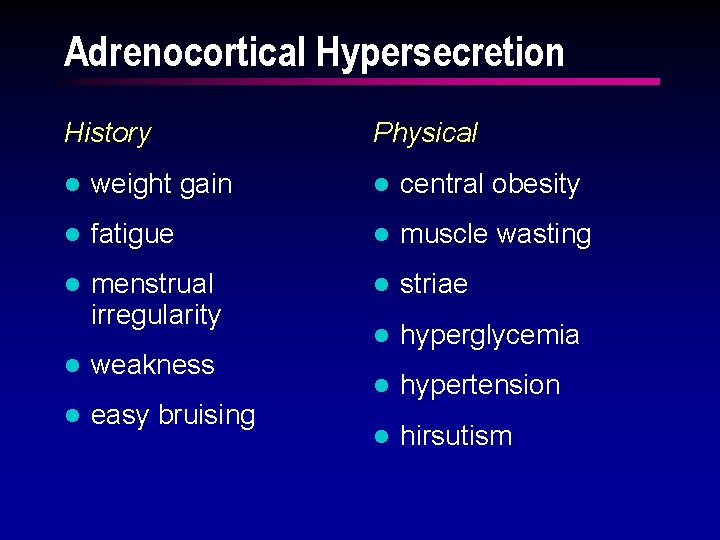
Adrenocortical Hypersecretion History Physical l weight gain l central obesity l fatigue l muscle wasting l menstrual irregularity l striae l hyperglycemia l hypertension l hirsutism l weakness l easy bruising
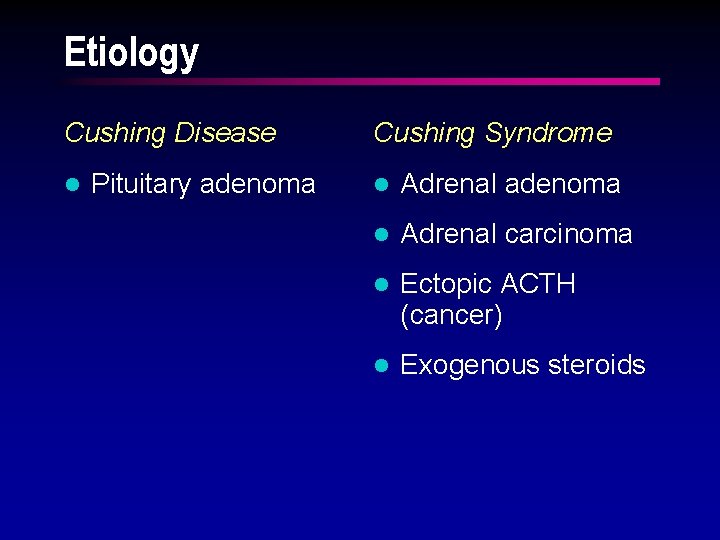
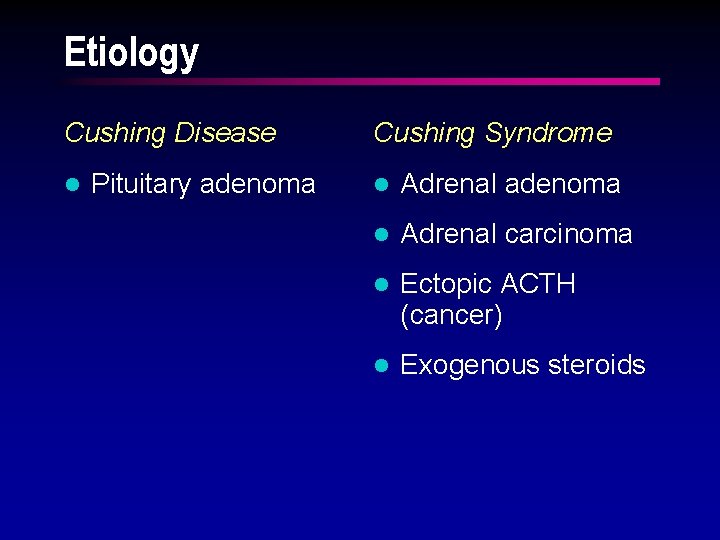
Etiology Cushing Disease l Pituitary adenoma Cushing Syndrome l Adrenal adenoma l Adrenal carcinoma l Ectopic ACTH (cancer) l Exogenous steroids
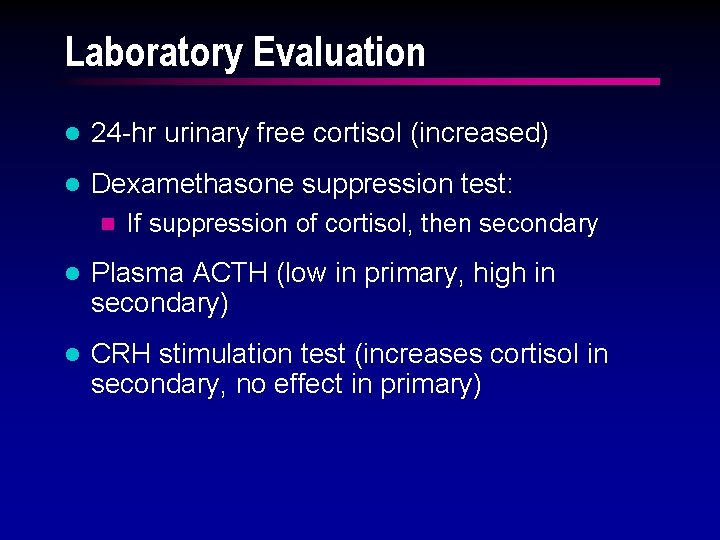
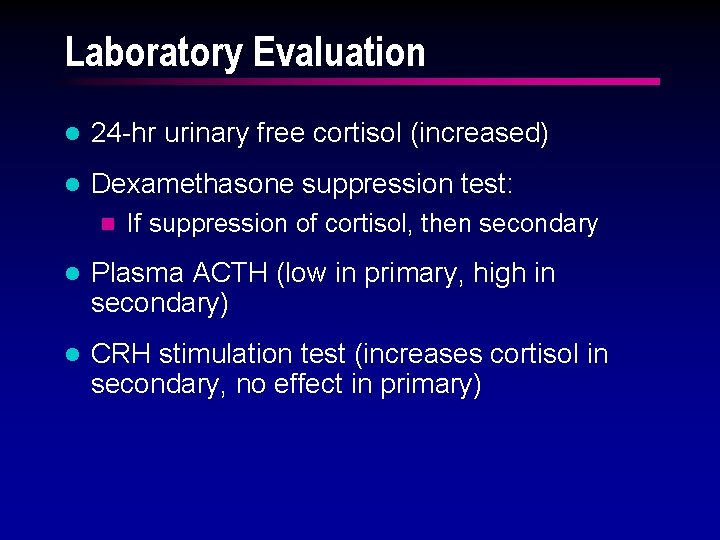
Laboratory Evaluation l 24 -hr urinary free cortisol (increased) l Dexamethasone suppression test: n If suppression of cortisol, then secondary l Plasma ACTH (low in primary, high in secondary) l CRH stimulation test (increases cortisol in secondary, no effect in primary)
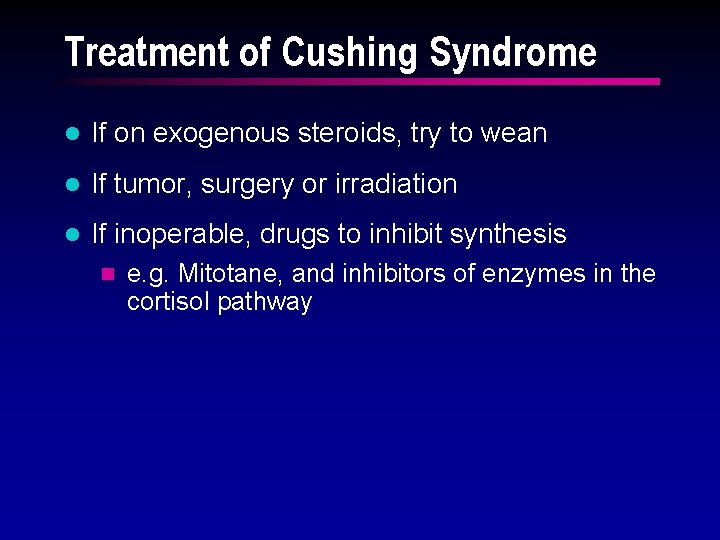
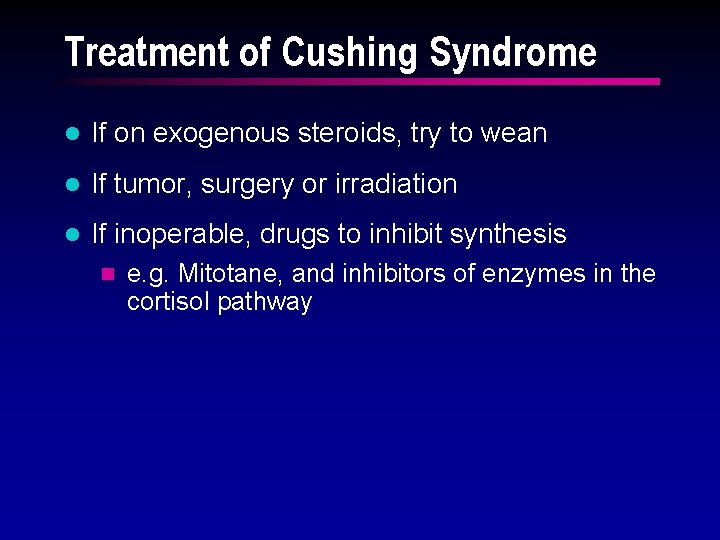
Treatment of Cushing Syndrome l If on exogenous steroids, try to wean l If tumor, surgery or irradiation l If inoperable, drugs to inhibit synthesis n e. g. Mitotane, and inhibitors of enzymes in the cortisol pathway
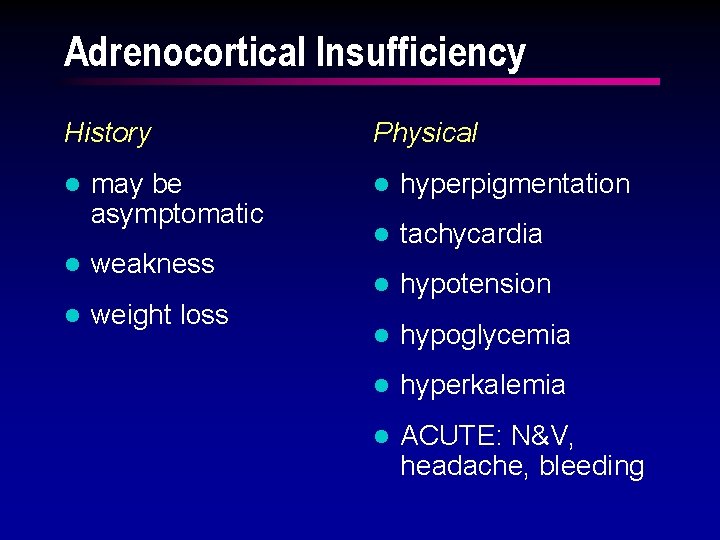
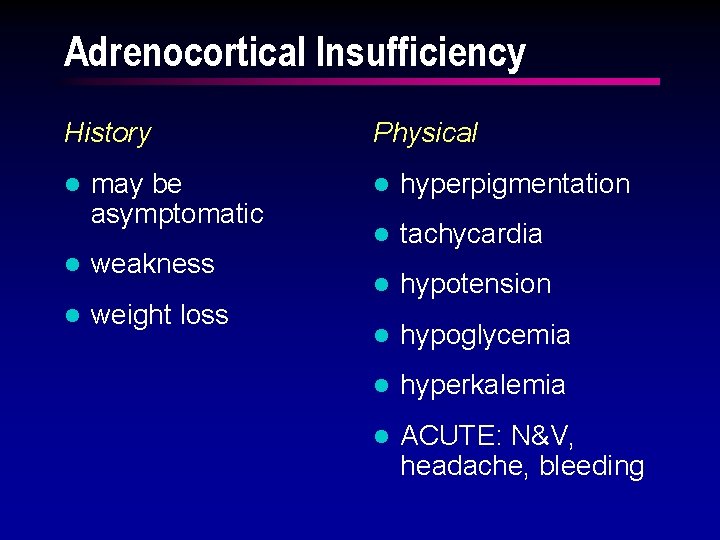
Adrenocortical Insufficiency History l may be asymptomatic l weakness l weight loss Physical l hyperpigmentation l tachycardia l hypotension l hypoglycemia l hyperkalemia l ACUTE: N&V, headache, bleeding
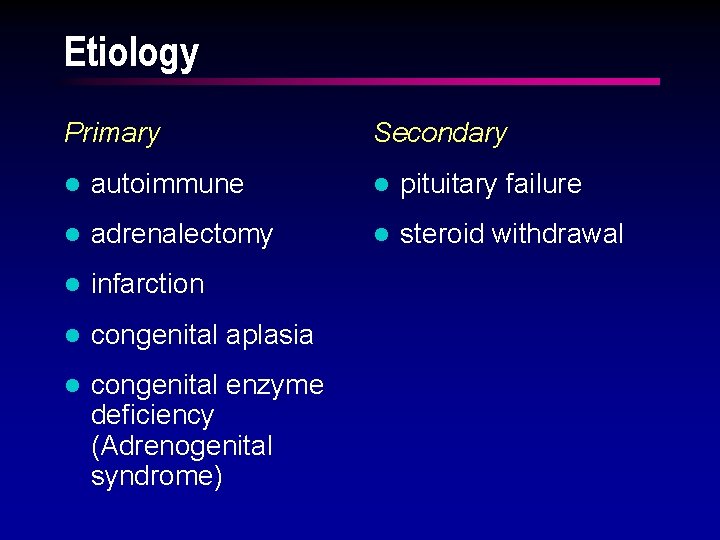
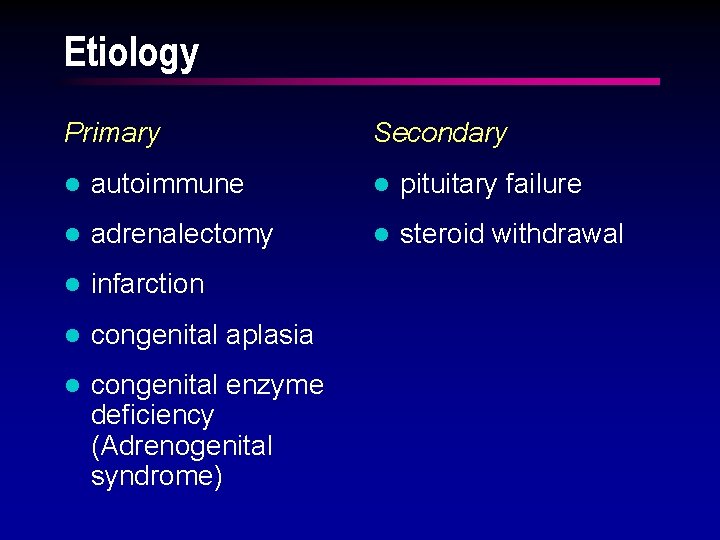
Etiology Primary Secondary l autoimmune l pituitary failure l adrenalectomy l steroid withdrawal l infarction l congenital aplasia l congenital enzyme deficiency (Adrenogenital syndrome)
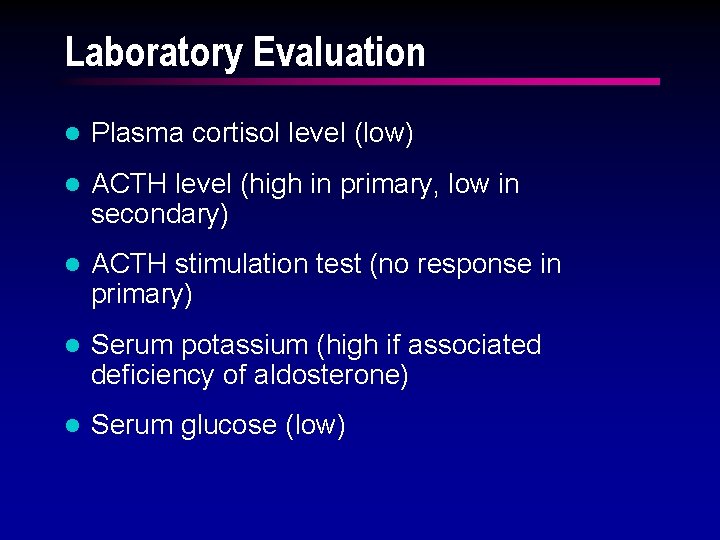
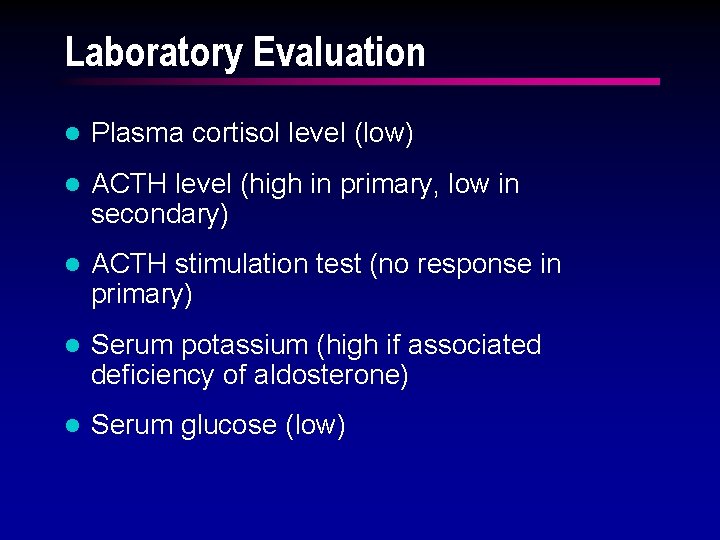
Laboratory Evaluation l Plasma cortisol level (low) l ACTH level (high in primary, low in secondary) l ACTH stimulation test (no response in primary) l Serum potassium (high if associated deficiency of aldosterone) l Serum glucose (low)
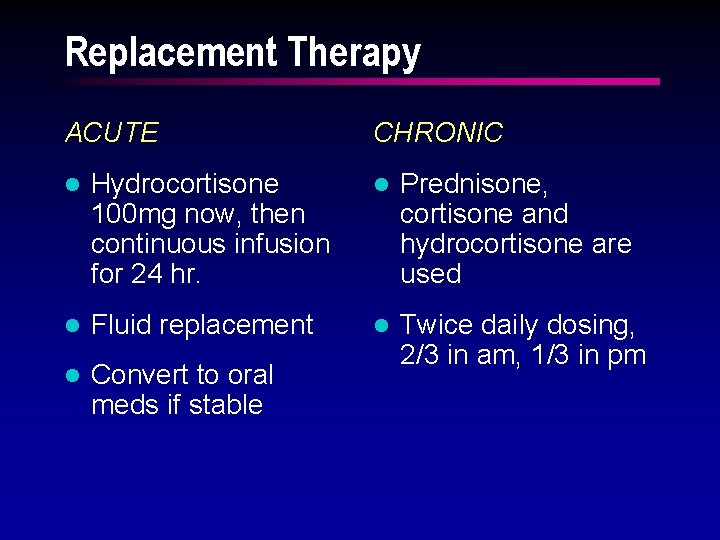
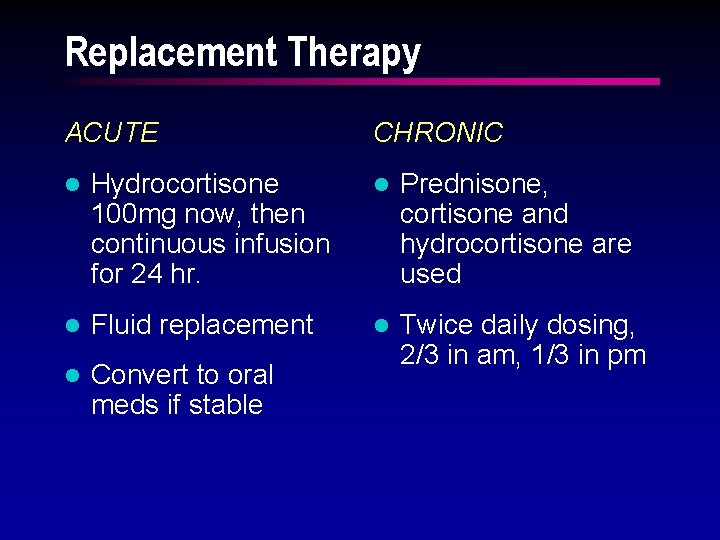
Replacement Therapy ACUTE CHRONIC l Hydrocortisone 100 mg now, then continuous infusion for 24 hr. l Prednisone, cortisone and hydrocortisone are used l Fluid replacement l l Convert to oral meds if stable Twice daily dosing, 2/3 in am, 1/3 in pm
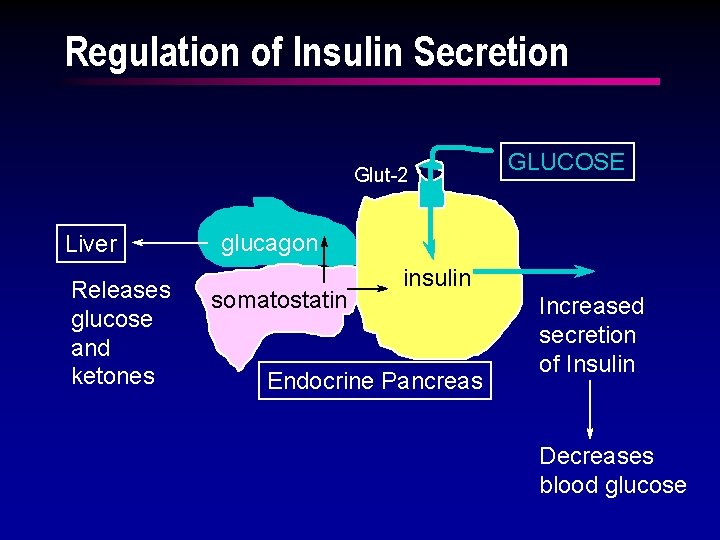
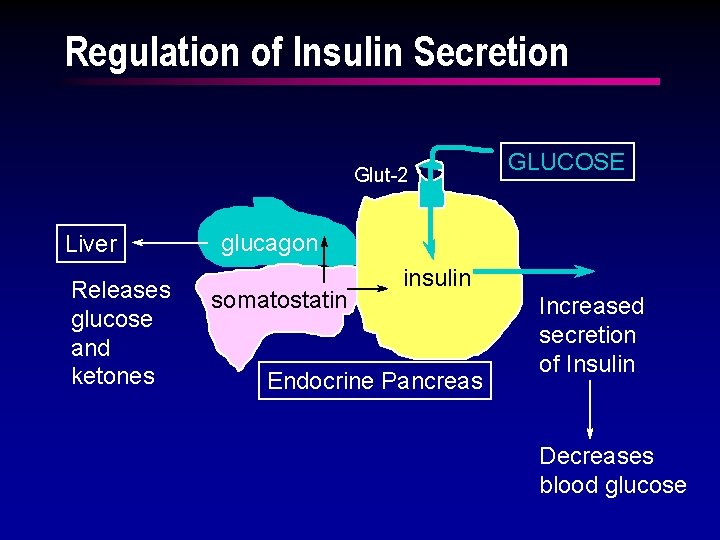
Regulation of Insulin Secretion Glut-2 Liver Releases glucose and ketones GLUCOSE glucagon somatostatin insulin Endocrine Pancreas Increased secretion of Insulin Decreases blood glucose
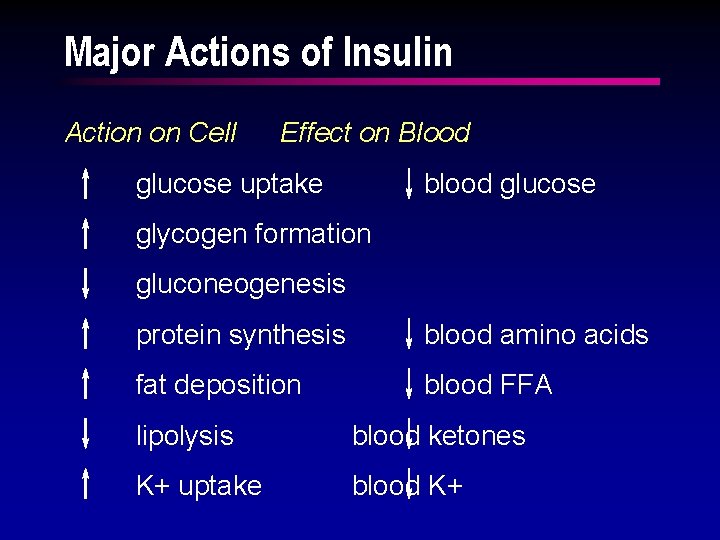
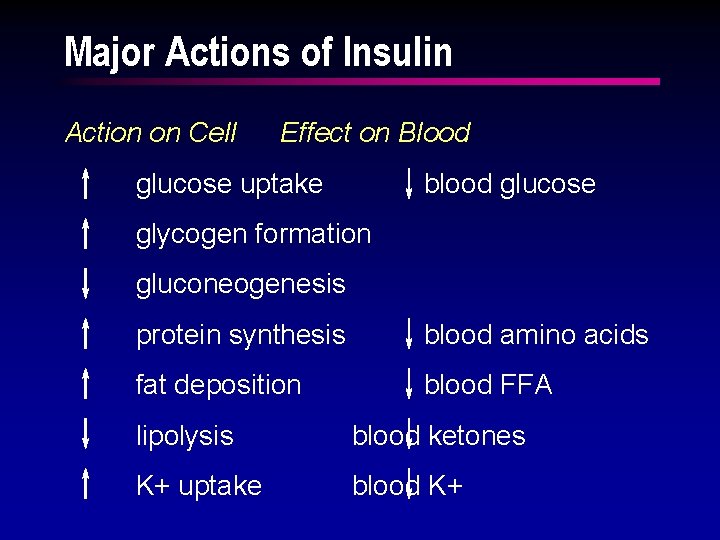
Major Actions of Insulin Action on Cell Effect on Blood glucose uptake blood glucose glycogen formation gluconeogenesis protein synthesis blood amino acids fat deposition blood FFA lipolysis blood ketones K+ uptake blood K+
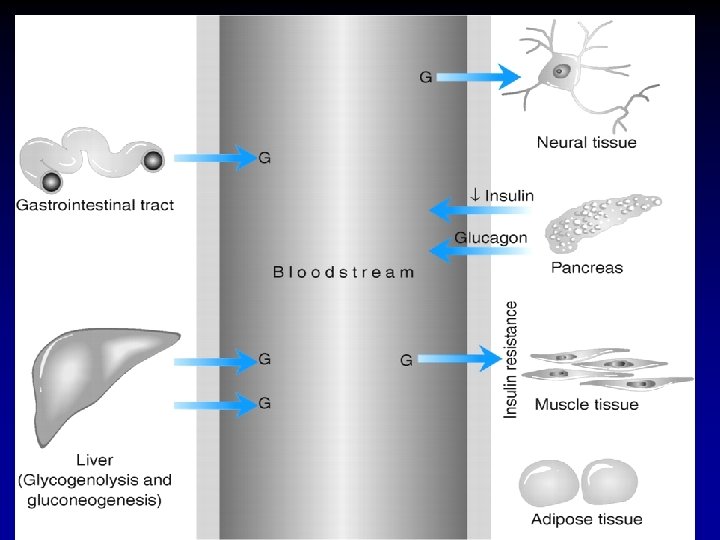
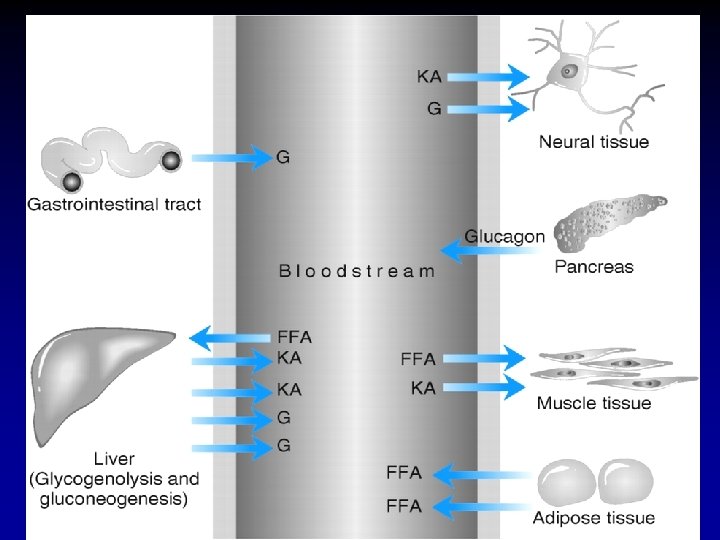
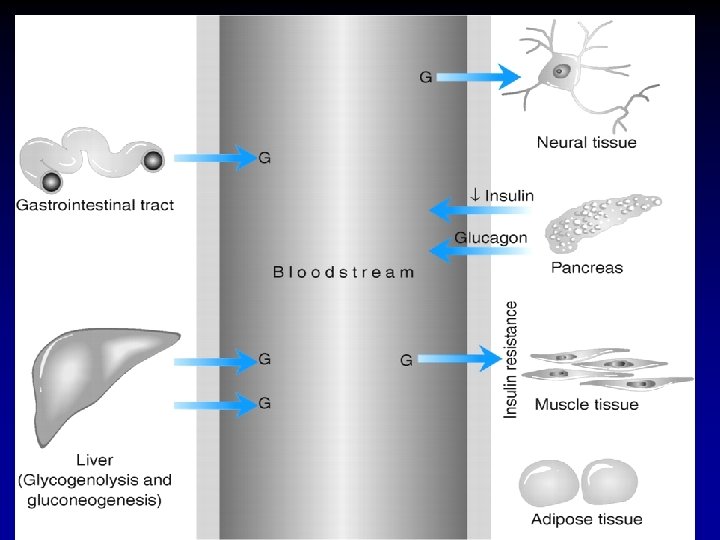
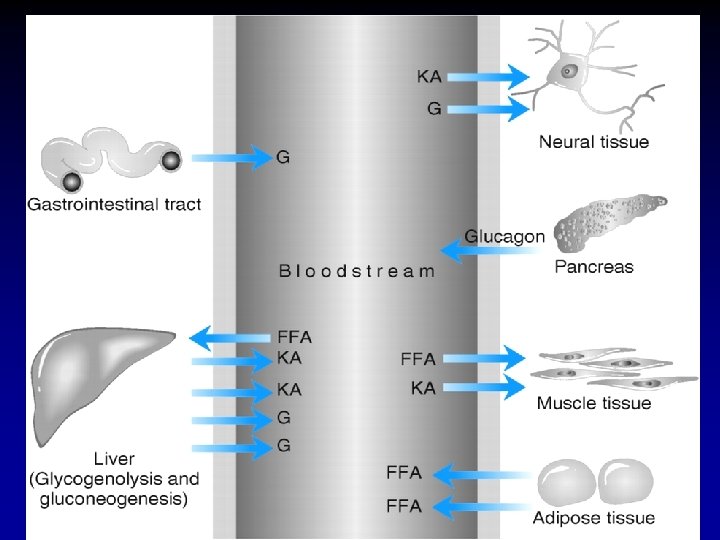
Figure: 41 -4 Metabolism in type 1 diabetes
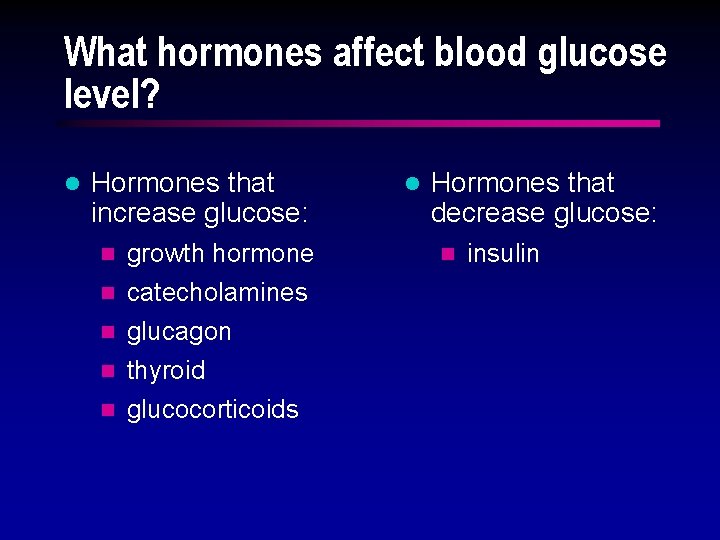
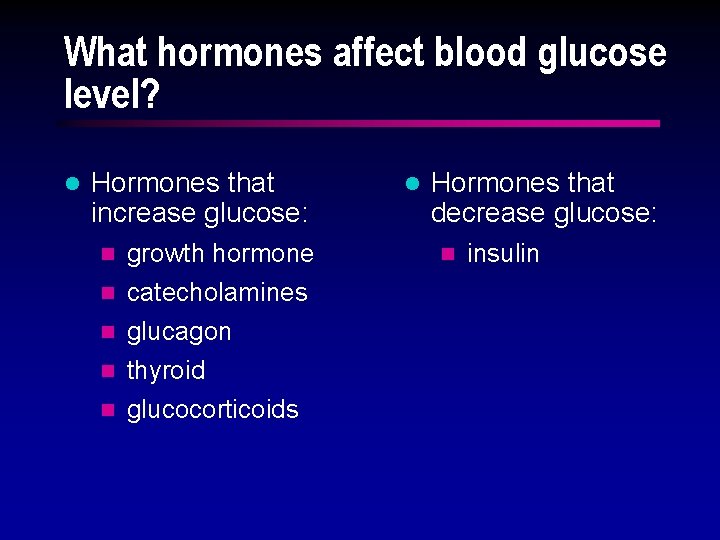
What hormones affect blood glucose level? l Hormones that increase glucose: n n n growth hormone catecholamines glucagon thyroid glucocorticoids l Hormones that decrease glucose: n insulin
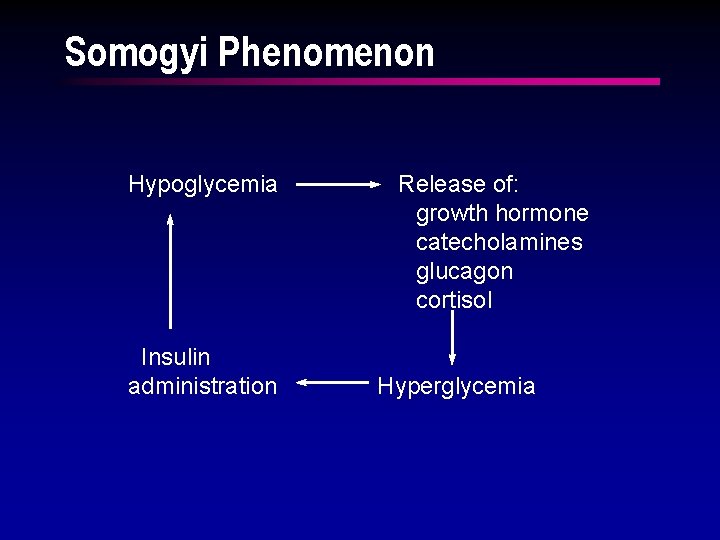
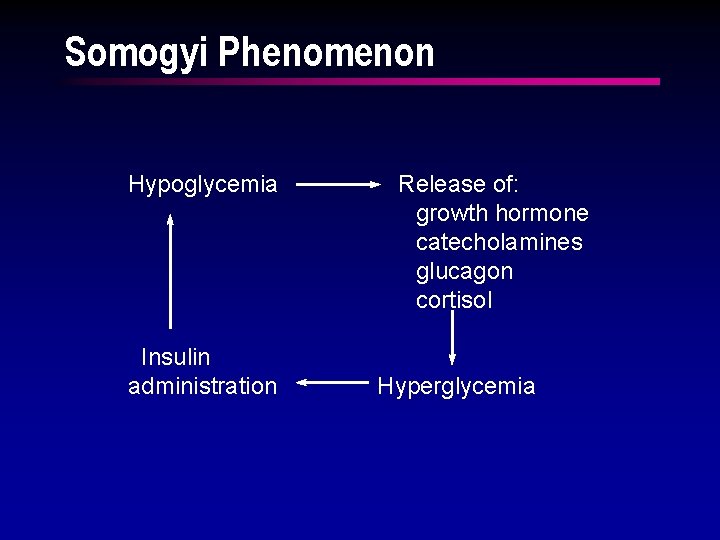
Somogyi Phenomenon Hypoglycemia Insulin administration Release of: growth hormone catecholamines glucagon cortisol Hyperglycemia
Diabetes Mellitus Insulin Dependent (Type 1) Non Insulin Dependent (Type 2)
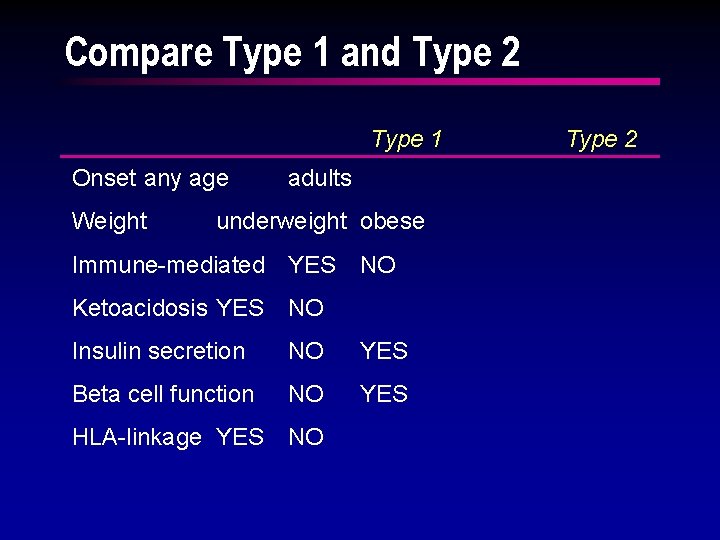
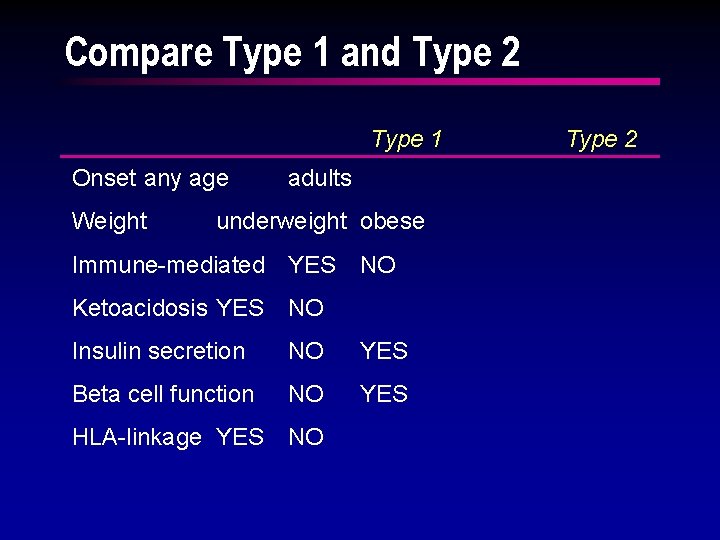
Compare Type 1 and Type 2 Type 1 Onset any age Weight adults underweight obese Immune-mediated YES NO Ketoacidosis YES NO Insulin secretion NO YES Beta cell function NO YES HLA-linkage YES NO Type 2
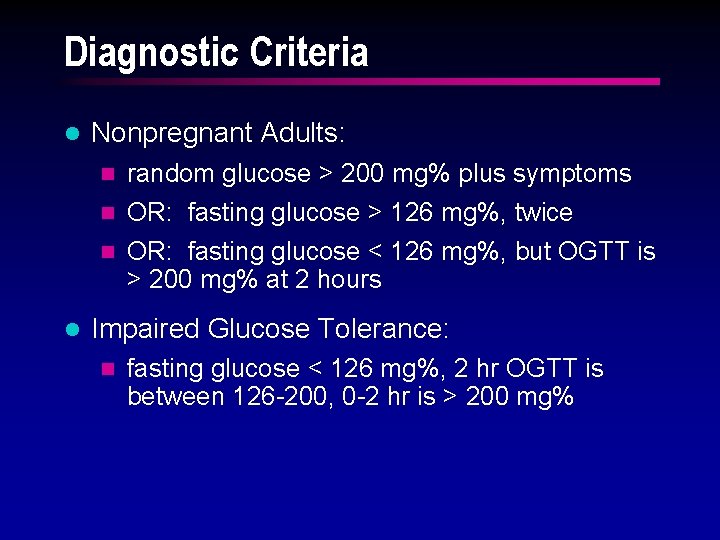
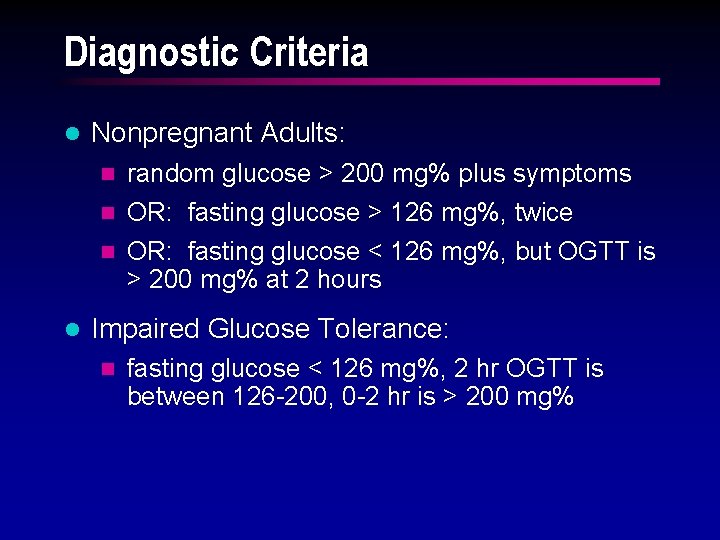
Diagnostic Criteria l Nonpregnant Adults: n random glucose > 200 mg% plus symptoms OR: fasting glucose > 126 mg%, twice n OR: fasting glucose < 126 mg%, but OGTT is > 200 mg% at 2 hours n l Impaired Glucose Tolerance: n fasting glucose < 126 mg%, 2 hr OGTT is between 126 -200, 0 -2 hr is > 200 mg%
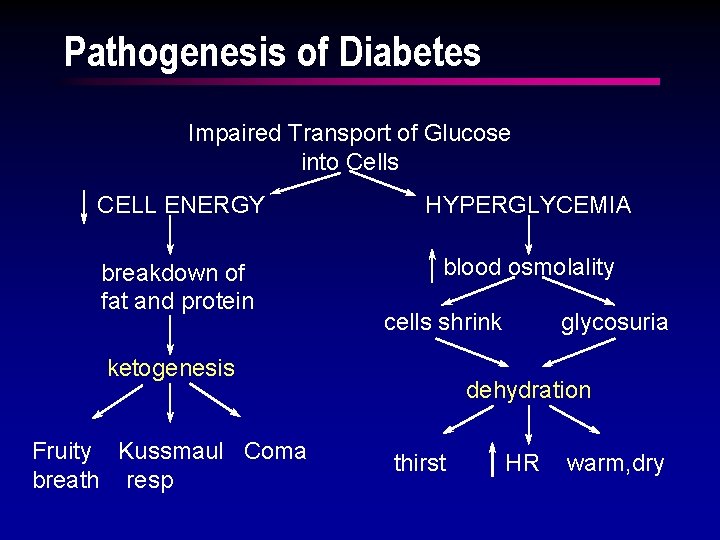
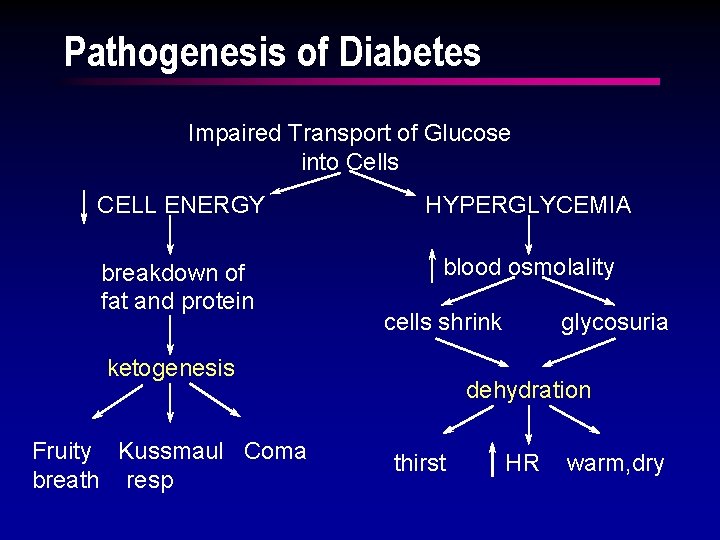
Pathogenesis of Diabetes Impaired Transport of Glucose into Cells CELL ENERGY HYPERGLYCEMIA breakdown of fat and protein blood osmolality cells shrink ketogenesis Fruity Kussmaul Coma breath resp glycosuria dehydration thirst HR warm, dry
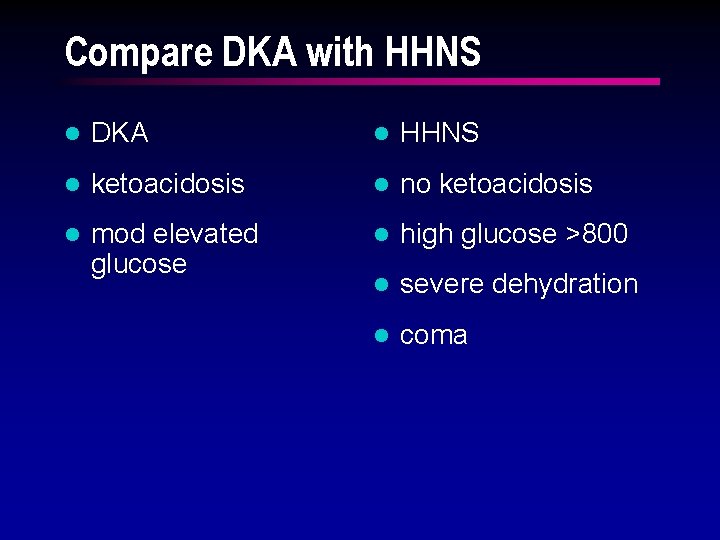
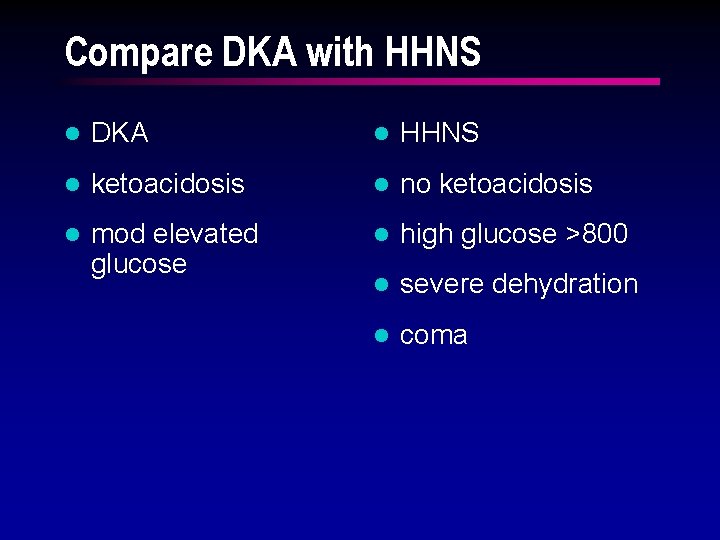
Compare DKA with HHNS l DKA l HHNS l ketoacidosis l no ketoacidosis l mod elevated glucose l high glucose >800 l severe dehydration l coma
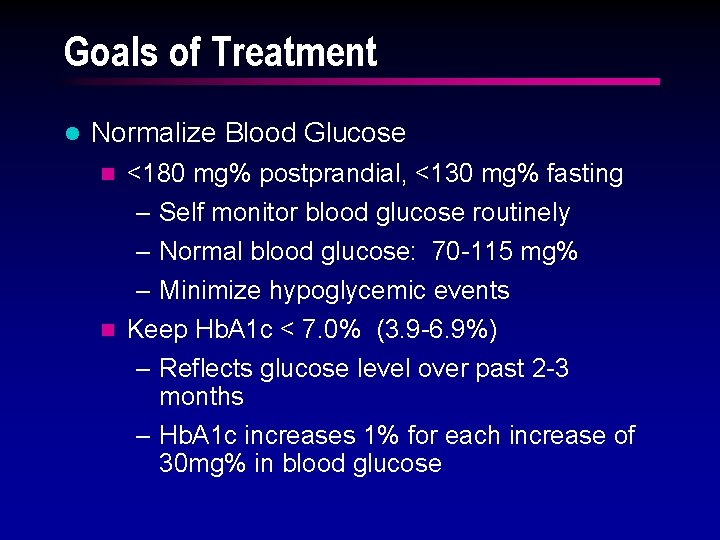
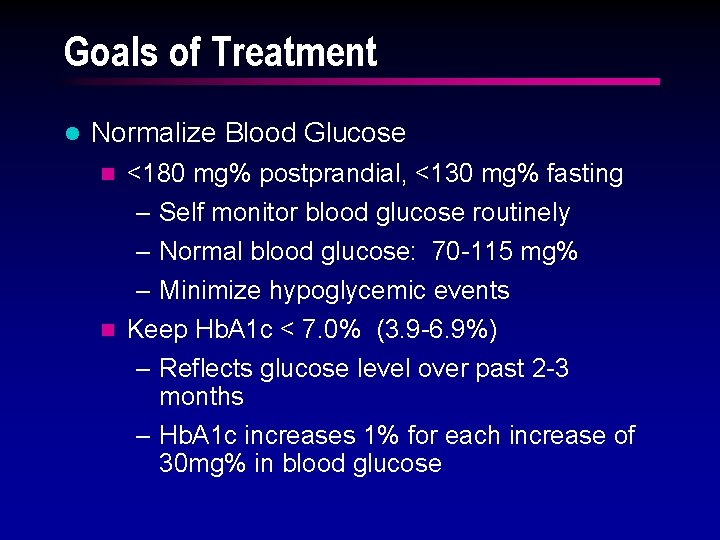
Goals of Treatment l Normalize Blood Glucose n <180 mg% postprandial, <130 mg% fasting – Self monitor blood glucose routinely – Normal blood glucose: 70 -115 mg% – Minimize hypoglycemic events n Keep Hb. A 1 c < 7. 0% (3. 9 -6. 9%) – Reflects glucose level over past 2 -3 months – Hb. A 1 c increases 1% for each increase of 30 mg% in blood glucose
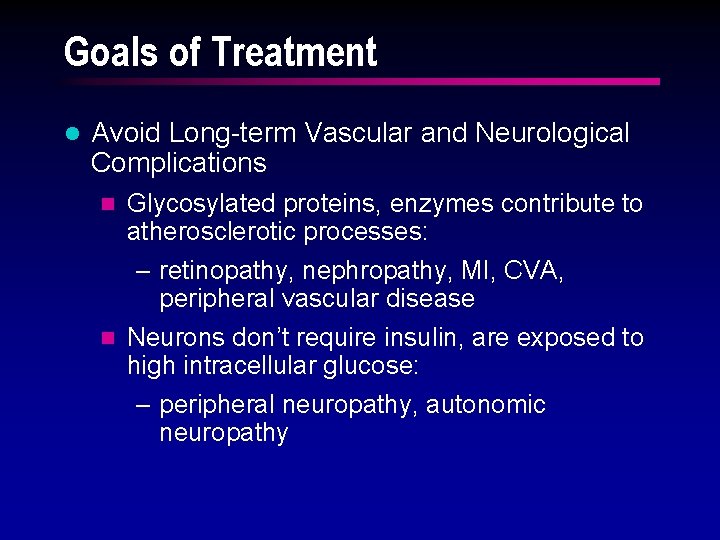
Goals of Treatment l Avoid Long-term Vascular and Neurological Complications Glycosylated proteins, enzymes contribute to atherosclerotic processes: – retinopathy, nephropathy, MI, CVA, peripheral vascular disease n Neurons don’t require insulin, are exposed to high intracellular glucose: – peripheral neuropathy, autonomic neuropathy n
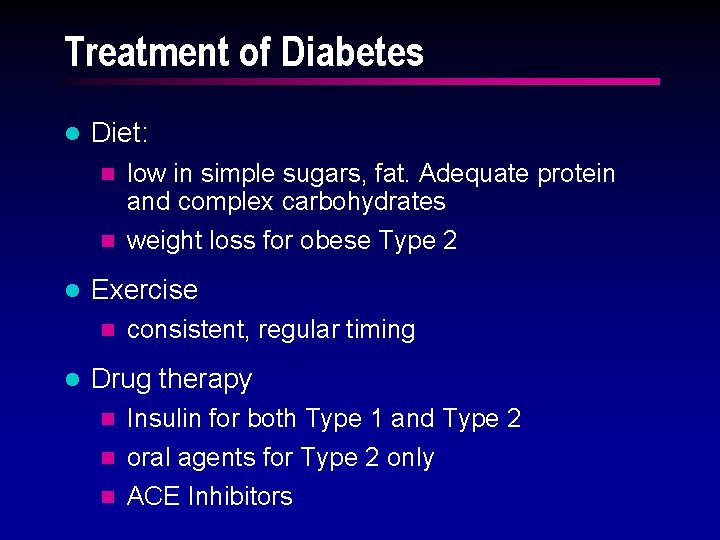
Treatment of Diabetes l Diet: low in simple sugars, fat. Adequate protein and complex carbohydrates n weight loss for obese Type 2 n l Exercise n l consistent, regular timing Drug therapy Insulin for both Type 1 and Type 2 n oral agents for Type 2 only n ACE Inhibitors n
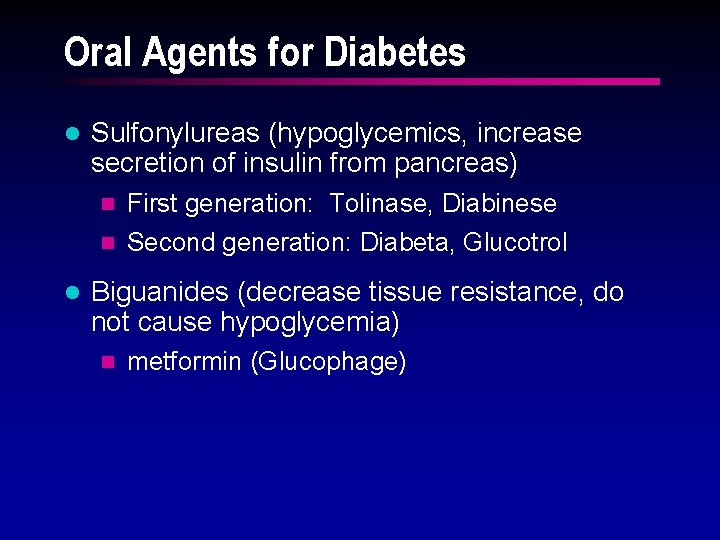
Oral Agents for Diabetes l Sulfonylureas (hypoglycemics, increase secretion of insulin from pancreas) First generation: Tolinase, Diabinese n Second generation: Diabeta, Glucotrol n l Biguanides (decrease tissue resistance, do not cause hypoglycemia) n metformin (Glucophage)
Teaching, Teaching l Blood glucose monitoring l Urine ketone monitoring l Drug onset, peak l Short and long term complications to monitor l When to call the provider, enter the hospital l Diet and Exercise plan
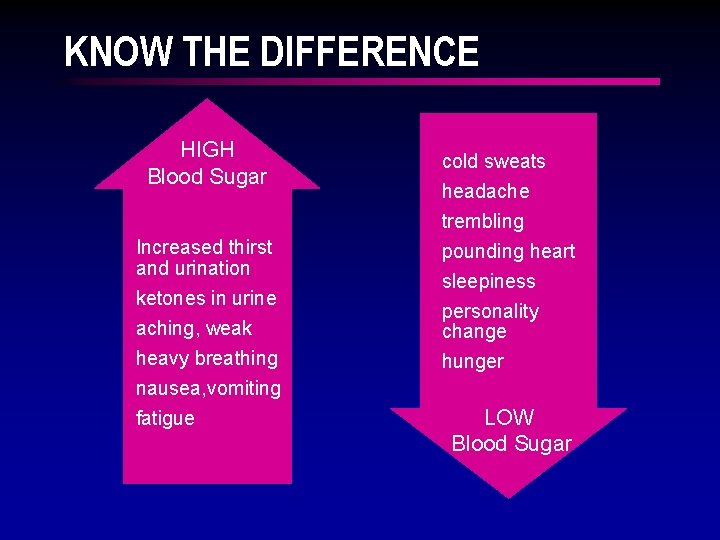
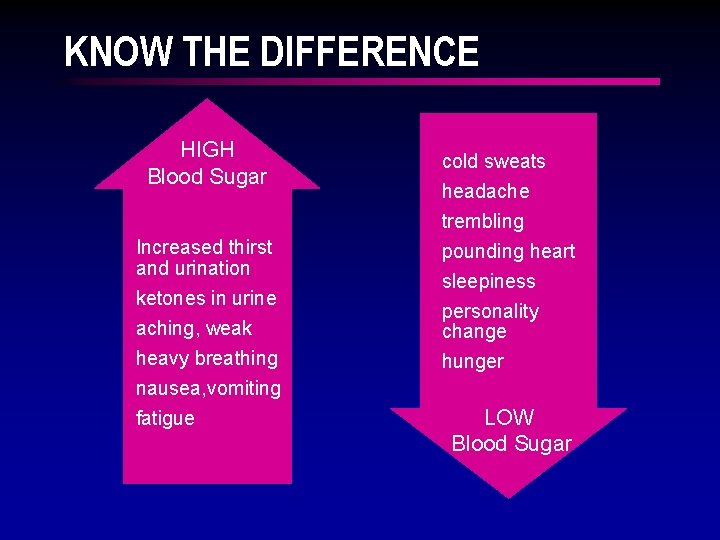
KNOW THE DIFFERENCE HIGH Blood Sugar Increased thirst and urination ketones in urine aching, weak heavy breathing cold sweats headache trembling pounding heart sleepiness personality change hunger nausea, vomiting fatigue LOW Blood Sugar
The End…