Hemodynamic Monitoring and Circulatory Assist Devices Chapter 66

- Slides: 83
Hemodynamic Monitoring and Circulatory Assist Devices Chapter 66 Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring • Measurement of pressure, flow, and oxygenation within the cardiovascular system • Assesses heart function, fluid balance, and effects of drugs on CO Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring • Invasive and noninvasive measurements • Systemic and pulmonary arterial pressures • Central venous pressure (CVP) • Pulmonary artery wedge pressure (PAWP) • Cardiac output (CO)/cardiac index (CI) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring • Invasive and noninvasive measurements • Stroke volume (SV)/stroke volume index (SVI) • Stroke volume variation (SVV) • O 2 saturation of arterial blood (Sa. O 2) • Mixed venous oxygenation saturation (Sv. O 2) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring Terminology • CO: volume of blood pumped by heart in 1 minute • CI: CO adjusted for body surface area (BSA) • SV: volume ejected with each heartbeat • SVI: SV adjusted for body size Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring Terminology • Systemic vascular resistance (SVR) and pulmonary vascular resistance (PVR) • Opposition to blood flow by systemic and pulmonary vasculature • Preload, afterload, and contractility determine SV Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring Terminology • Preload • Volume of blood within ventricle at end of diastole • PAWP: reflects left ventricular enddiastolic pressure • CVP: reflects right ventricular enddiastolic pressure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring Terminology • Afterload • Forces opposing ventricular ejection • SVR and arterial pressure indices of left ventricular afterload • PVR and pulmonary arterial pressure indices of right ventricular afterload Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hemodynamic Monitoring Terminology • Vascular resistance • Systemic and pulmonary • Reflect afterload • Contractility • Strength of ventricular contraction • No direct clinical measure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • A. J. , a 78 -year-old male, is admitted to the ICU in acute decompensated heart failure. • Health care provider decides to insert an arterial line and pulmonary artery catheter to facilitate treatment decisions. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • What equipment will you collect in preparation for insertion of these lines? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
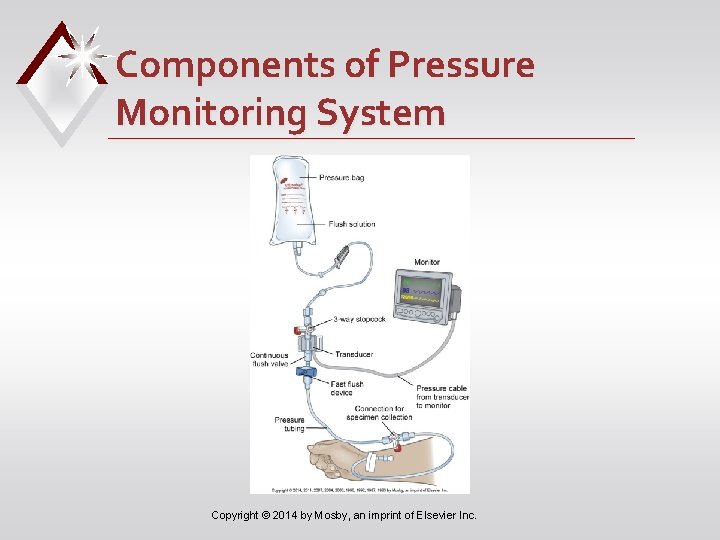
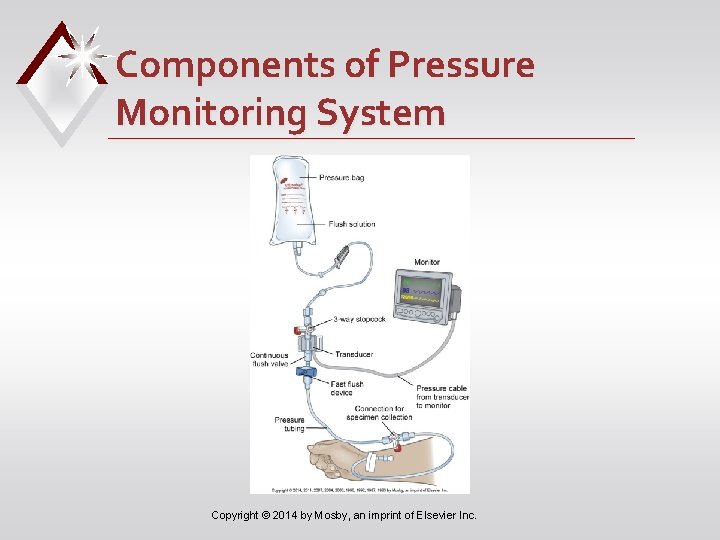
Components of Pressure Monitoring System Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • Why is it important to zero reference the transducer and perform a dynamic response test during initial setup of the equipment for A. J. ? • Where is the phlebostatic axis located? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Principles of Invasive Pressure Monitoring • Equipment must be referenced and zero balanced to environment and dynamic response characteristics optimized • Referencing: positioning transducer so zero reference point is at level of atria of heart or phlebostatic axis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
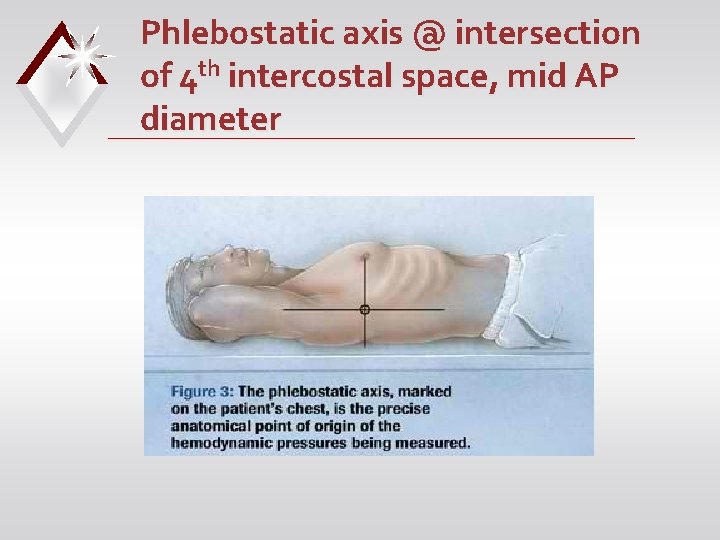
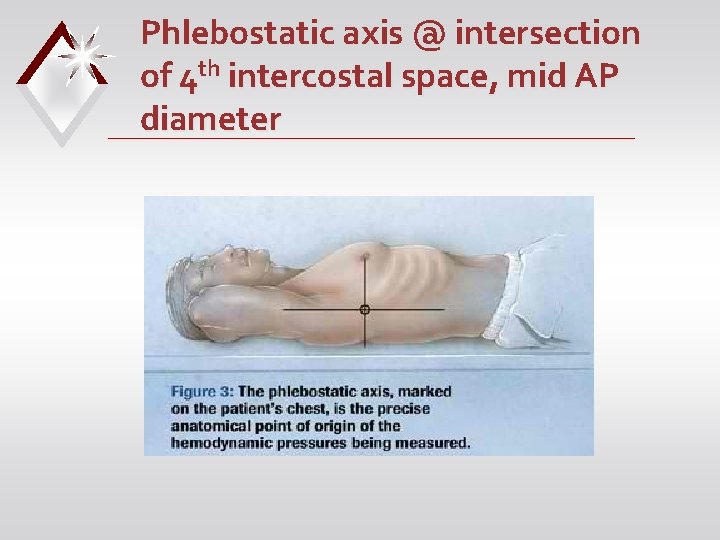
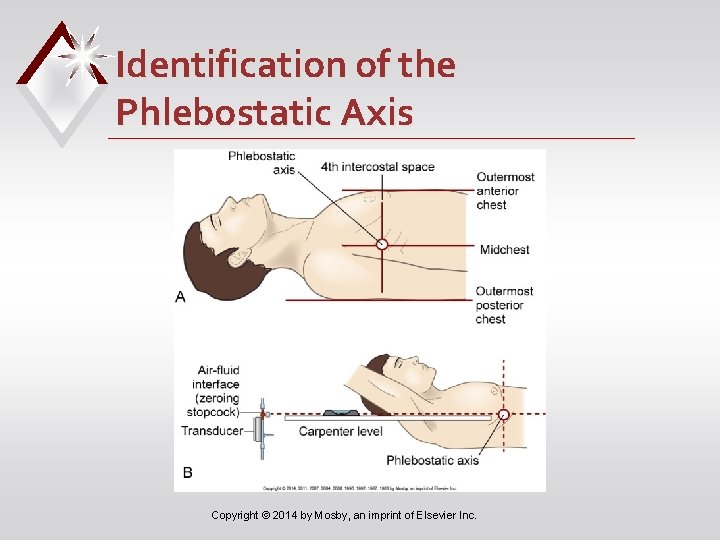
Phlebostatic axis @ intersection of 4 th intercostal space, mid AP diameter
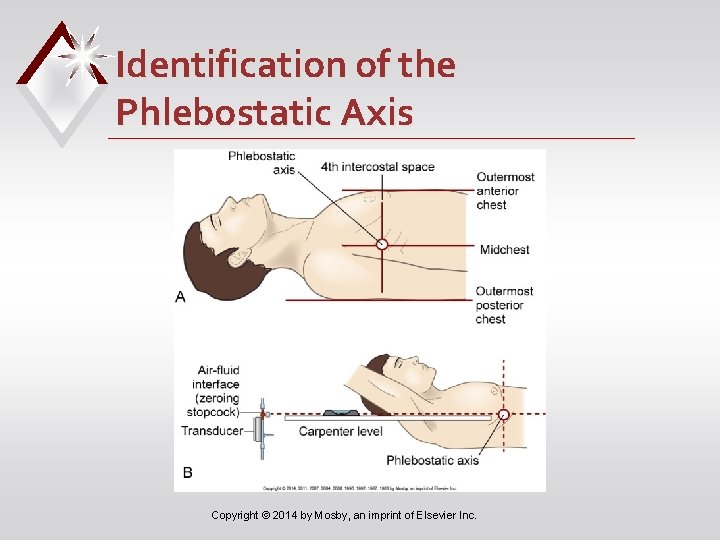
Identification of the Phlebostatic Axis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Principles of Invasive Pressure Monitoring • Zeroing: confirms that when pressure within system is zero, monitor reads zero • Done by opening reference stopcock to room air • With initial setup and periodically thereafter Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
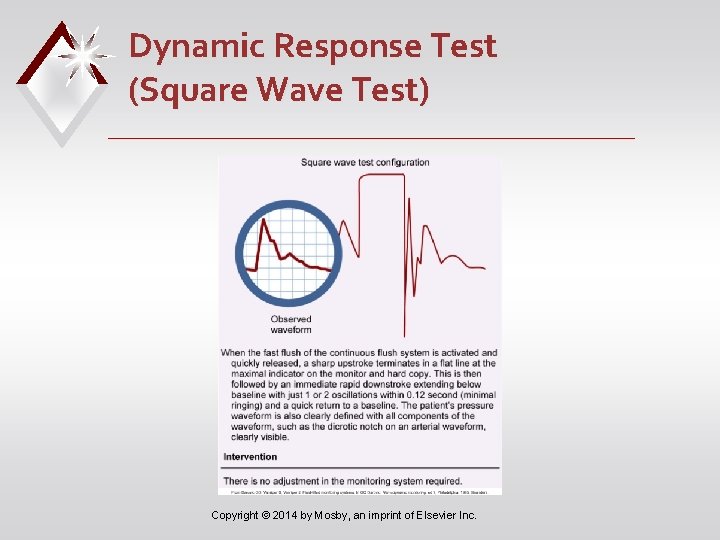
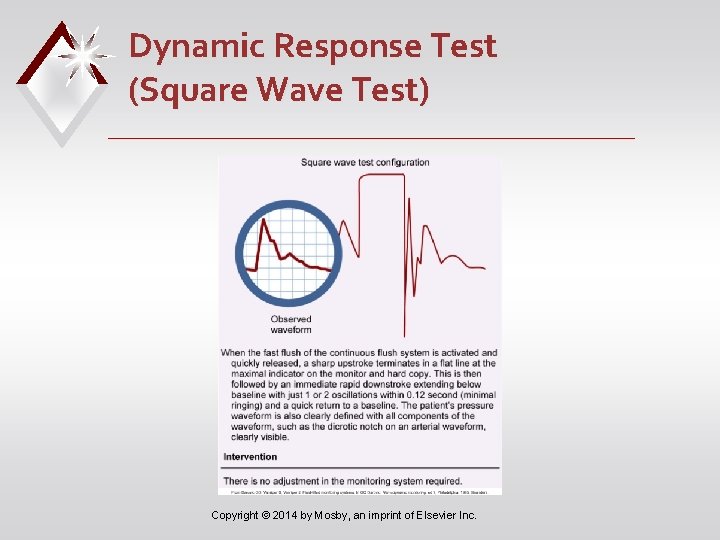
Dynamic Response Test (Square Wave Test) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Types of Invasive Pressure Monitoring • Arterial pressure monitoring • Various indications when continuous BP measurements useful • 20 -gauge, 2 -inch nontapered Teflon catheter into peripheral artery • Suture in place • Immobilize insertion site Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
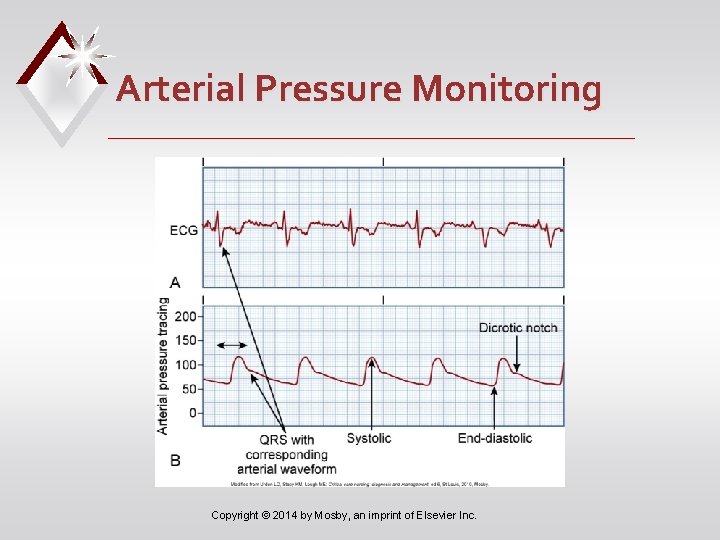
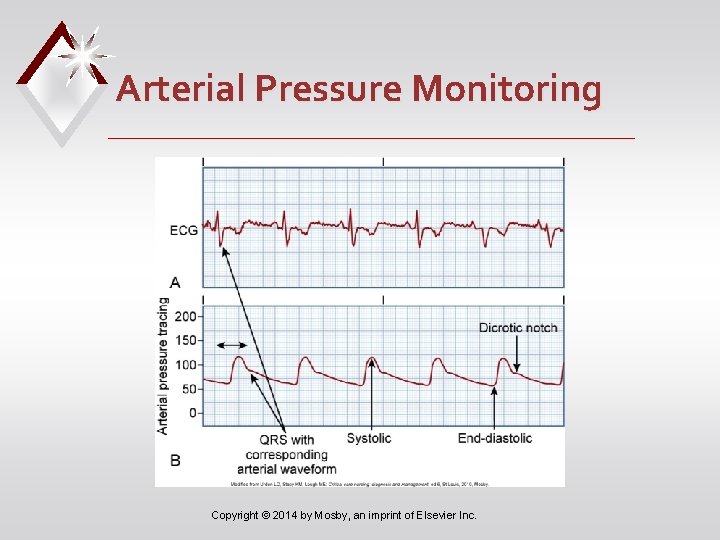
Arterial Pressure Monitoring Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • When planning care for A. J. , what nursing interventions will you perform to prevent complications related to his arterial line? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Arterial Pressure Monitoring • High- and low-pressure alarms • Risks/complications • Hemorrhage • Infection • Thrombus formation • Neurovascular impairment • Loss of limb Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Arterial Pressure Monitoring • Continuous flush irrigation system • Delivers 3– 6 m. L of saline/hour • Maintains line patency • Limits thrombus formation • Assess neurovascular status distal to arterial insertion site hourly Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
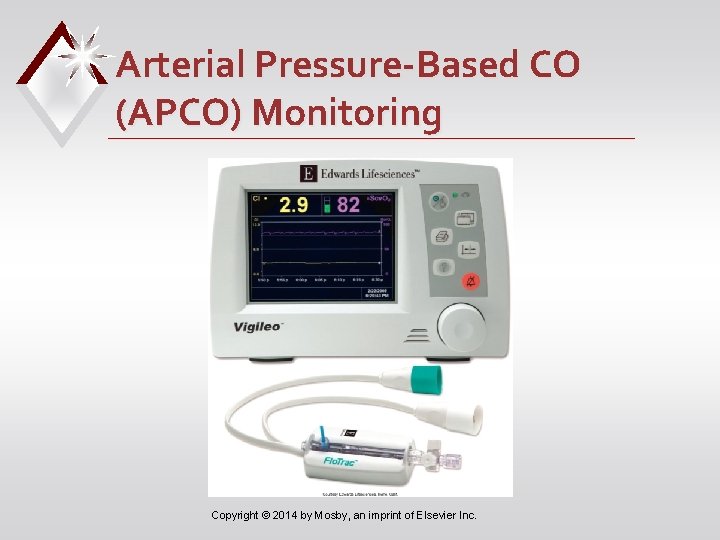
Arterial Pressure-Based CO (APCO) Monitoring • Calculates continuous CO and CI • Used to assess patient’s ability to respond to fluids • Uses arterial waveform characteristics and patient demographic data to calculate SVV, CCO/CCI, and SV/SVI every 20 seconds Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
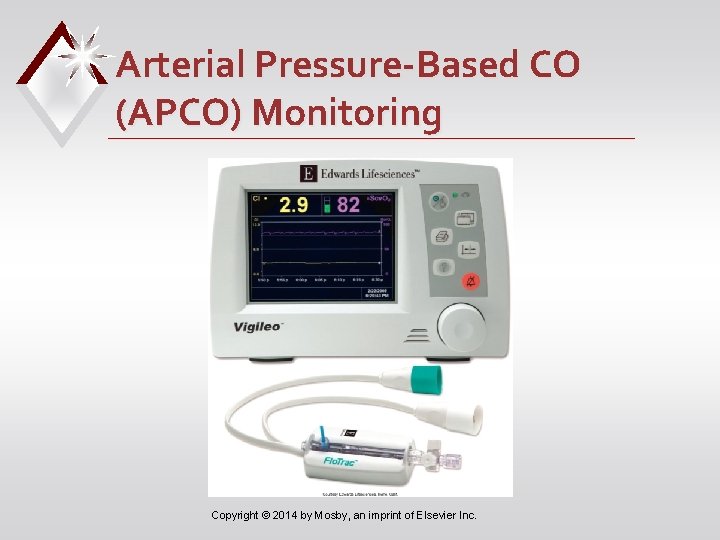
Arterial Pressure-Based CO (APCO) Monitoring Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Pulmonary Artery Pressure Monitoring • Guides management of patients with complicated cardiopulmonary problems • PA diastolic (PAD) pressure and PAWP → cardiac function and fluid volume status • Allows for precise manipulation of preload Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
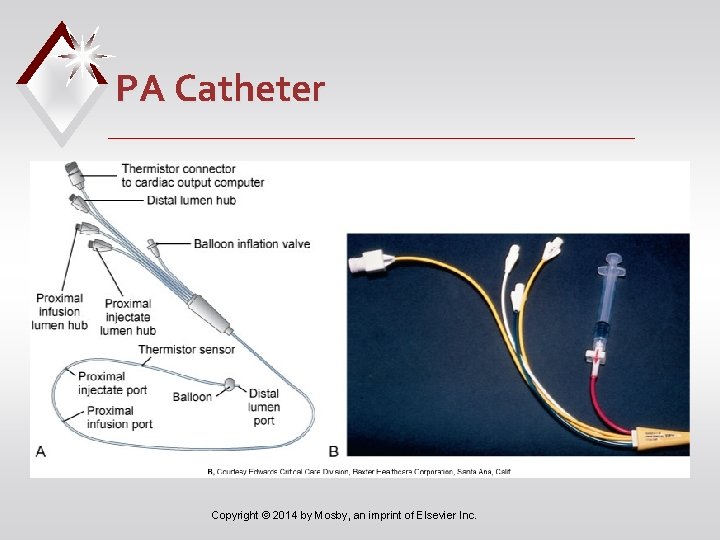
Pulmonary Artery Pressure Monitoring • PA flow-directed catheter (e. g. , Swan-Ganz) • Distal lumen port in PA • Balloon inflated to measure PAWP • Two proximal lumens to measure CVP, inject fluid for CO, draw blood, administer fluids or drugs • Thermistor port distally Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
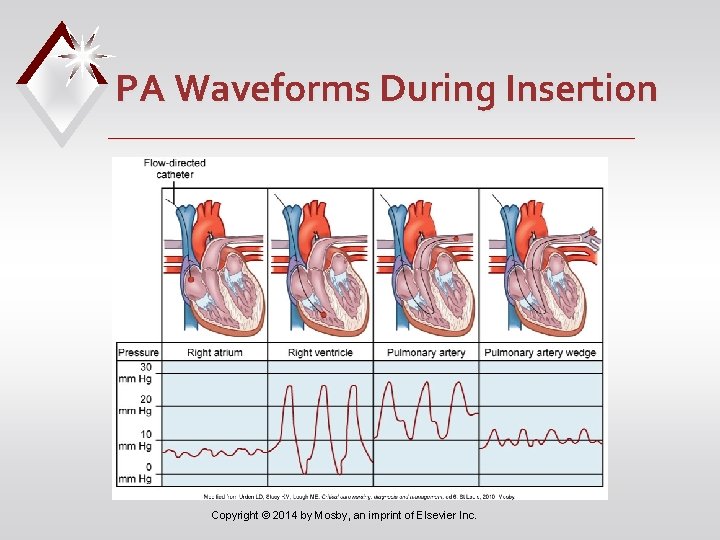
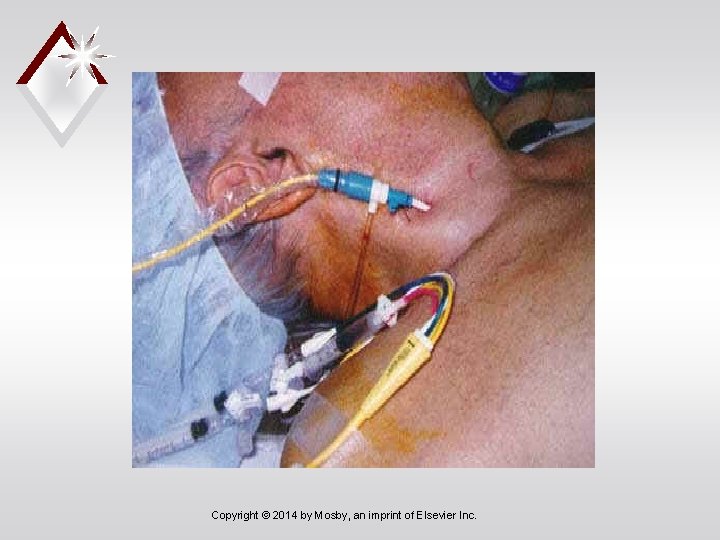
How do we measure Hemodynamics? • Pulmonary Artery Catheters (Swan Ganz) • Inserted via internal jugular vein • Line floated through right chambers of heart • End of catheter rests in proximal PA
Indications for PA Monitoring Diagnostics… -Shock (staging) -Pulmonary HTN, embolism, & edema, -Valvular disease -Cardiac Tamponade Evaluation of… -Volume status -Treatment modalities (i. e. gtt titration)
Contraindications for PA caths • Right side heart tumor or thrombus • Tricuspid or pulmonic valve prosthesis or endocarditis
PA Cath Insertion Risks • Dysrhythmias d/t RV irritation • PA rupture • Valve damage • Infection, Bleeding • Pneumo or hemothorax • Embolization • Catheter migration
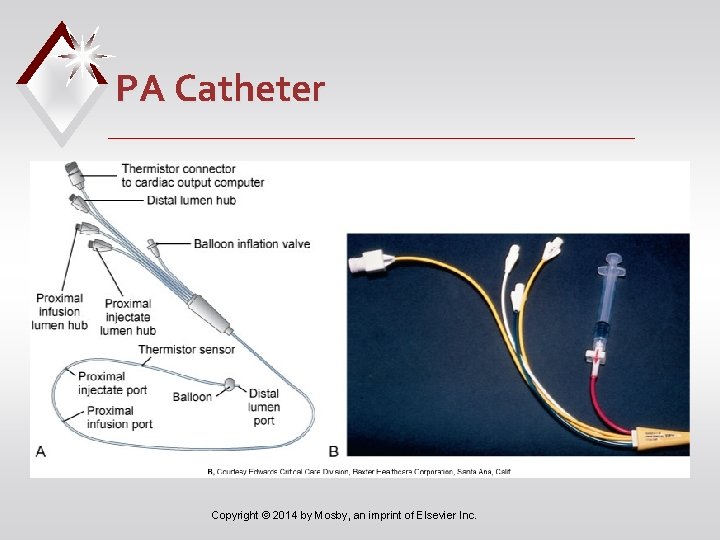
PA Catheter Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Pulmonary Artery Pressure Monitoring • Specialized features • Atrial electrode • Fiberoptic sensor for mixed venous O 2 saturation • Continuous measurement of right ventricular volume and EF • Continuous CO monitoring • Additional ports for IV access Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

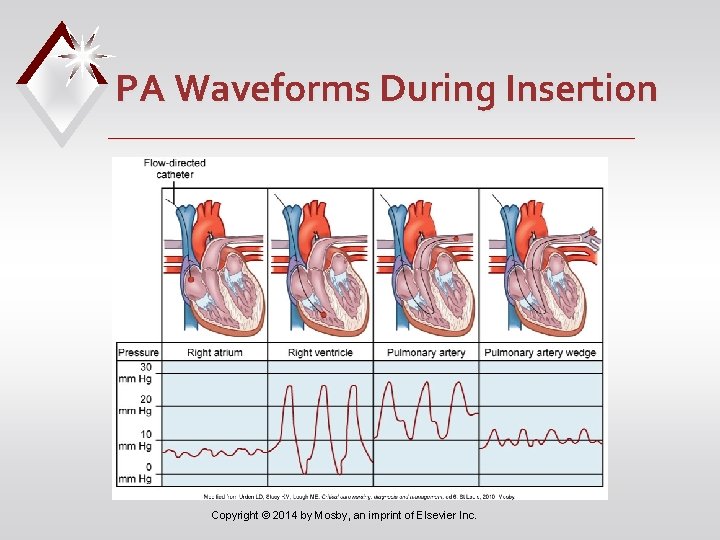
PA Waveforms During Insertion Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • After insertion of the PA line, the health care provider orders PAWP and CO measurement every 4 hours. • How will you obtain the PAWP measurement? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
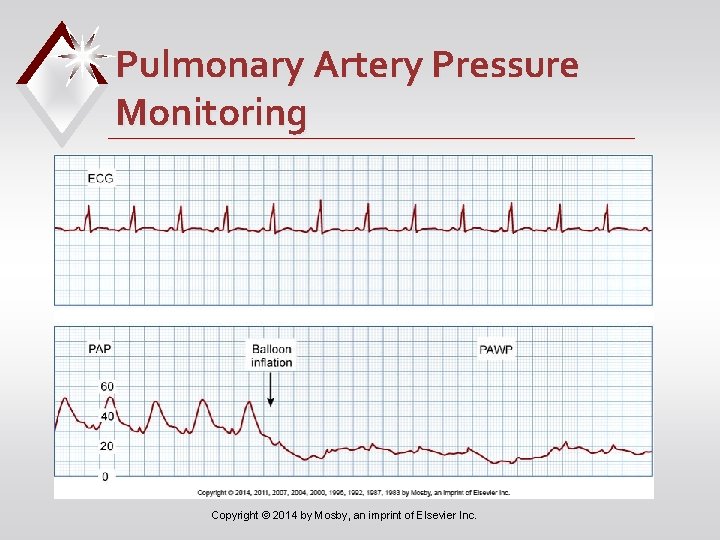
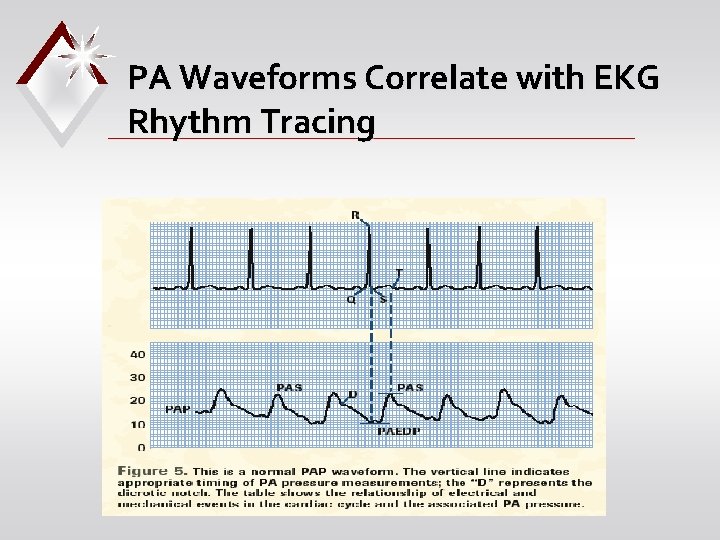
Pulmonary Artery Pressure Monitoring • When measurements are obtained: • PA: at end expiration • PAWP: slowly inflate balloon with air until PA waveform changes to PAWP waveform • Do not inflate for more than four respiratory cycles or 8– 15 seconds Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
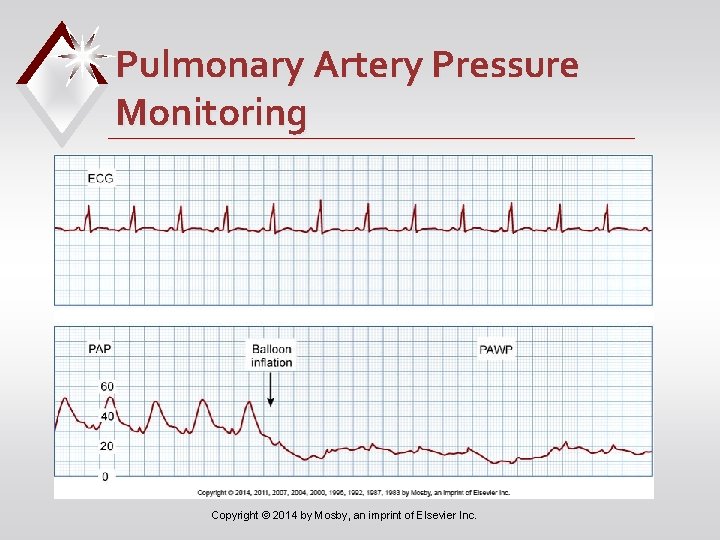
Pulmonary Artery Pressure Monitoring Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
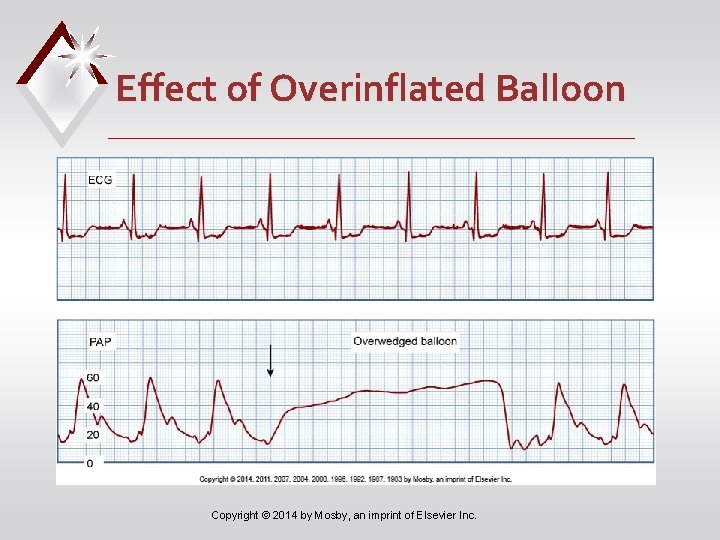
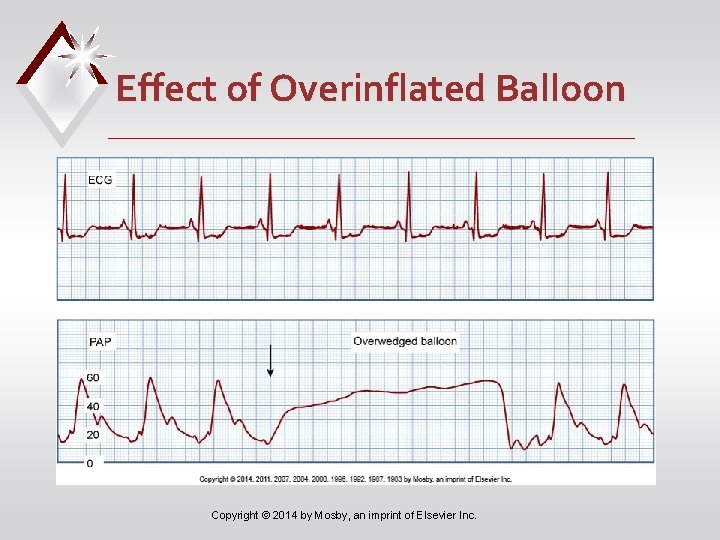
Effect of Overinflated Balloon Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
PA Catheter provides… • Continuous monitoring of… -CVP -PAP • Intermittent measure of… -PAWP
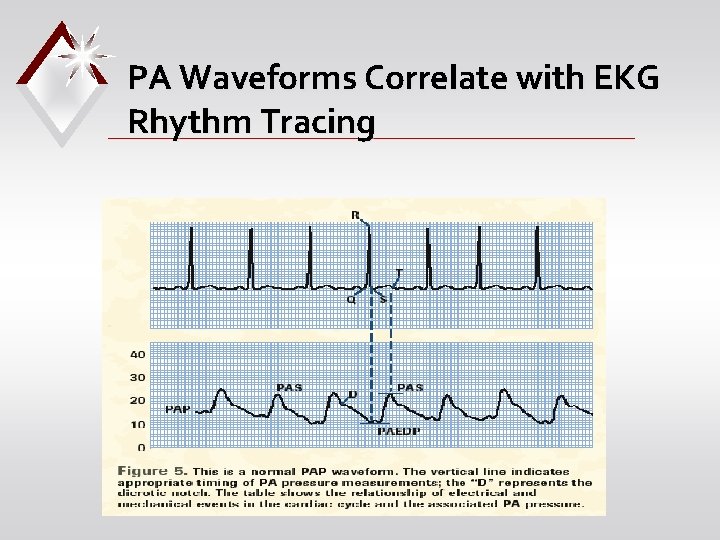
PA Waveforms Correlate with EKG Rhythm Tracing
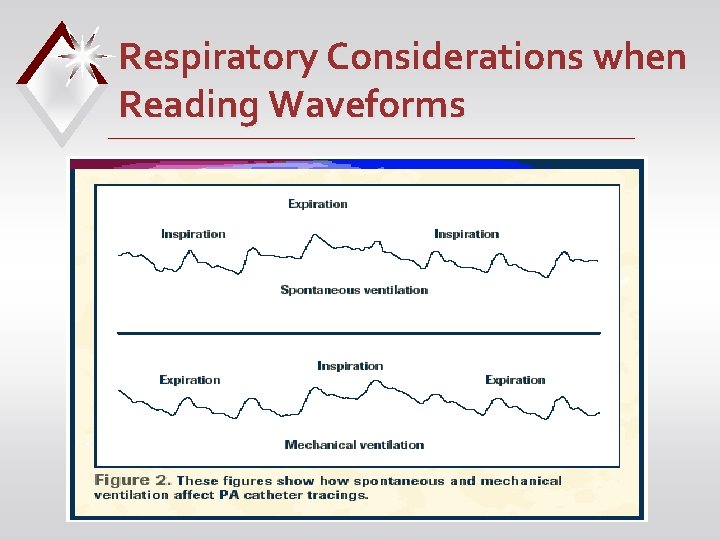
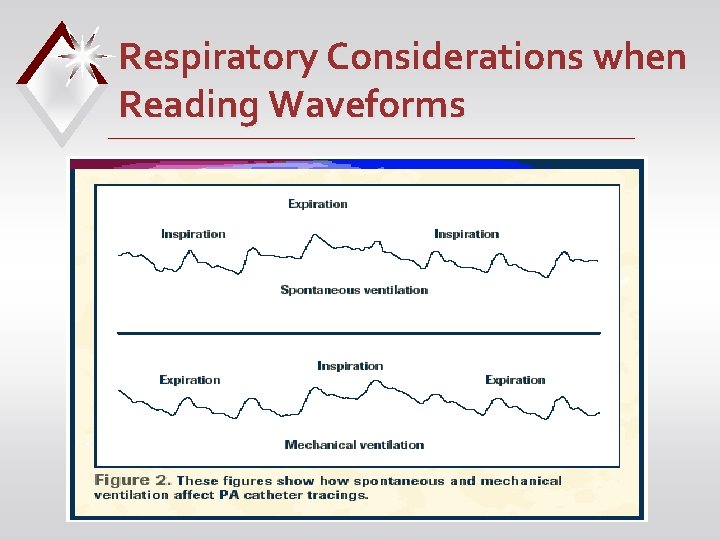
Respiratory Considerations when Reading Waveforms
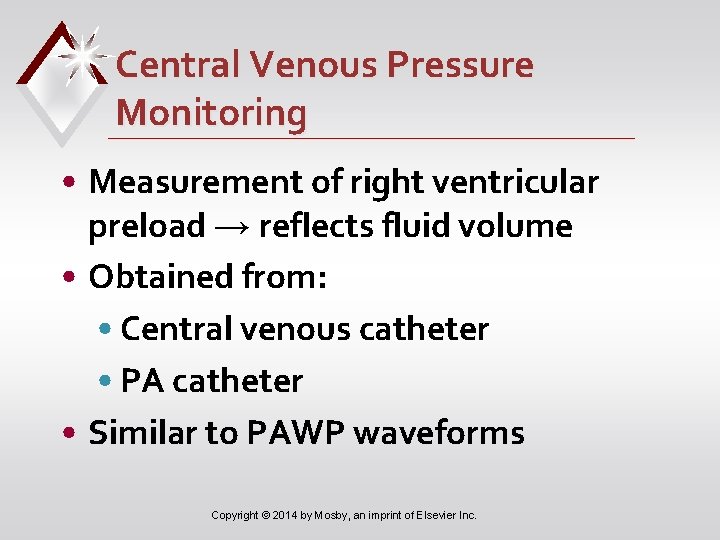
Central Venous Pressure Monitoring • Measurement of right ventricular preload → reflects fluid volume • Obtained from: • Central venous catheter • PA catheter • Similar to PAWP waveforms Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
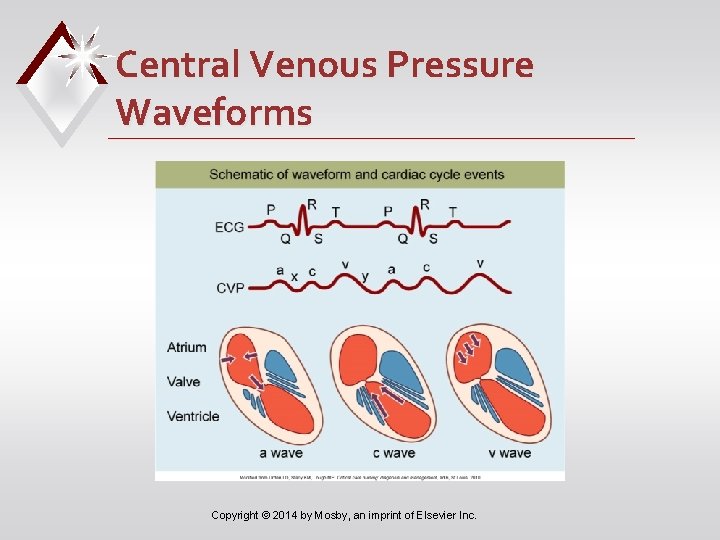
Central Venous Pressure Waveforms Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Measuring Cardiac Output • Continuous cardiac output (CCO) • PA catheter with thermal filament located in right atrium • Senses change in temperature of blood as it passes through right ventricle • Measures every 30– 60 seconds • Reflects average CO for past 3– 6 minutes Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • A. J. ’s pulmonary catheter does not have the capability to obtain continuous CO measurements. • How will you perform an intermittent bolus thermodilution CO assessment for A. J. ? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Measuring Cardiac Output • Intermittent bolus thermodilution (TDCO) • Inject saline or D 5 W into proximal lumen of PA catheter • Thermistor sensor detects differences in blood temperature and calculates CO • Uses average of three measurements Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
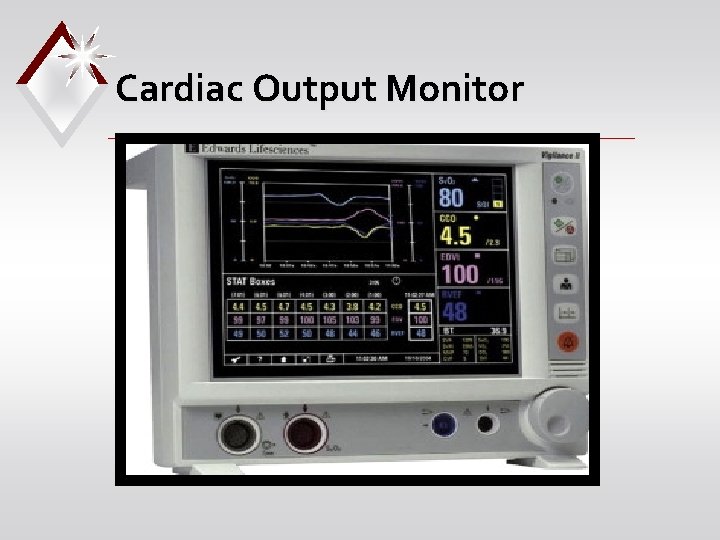
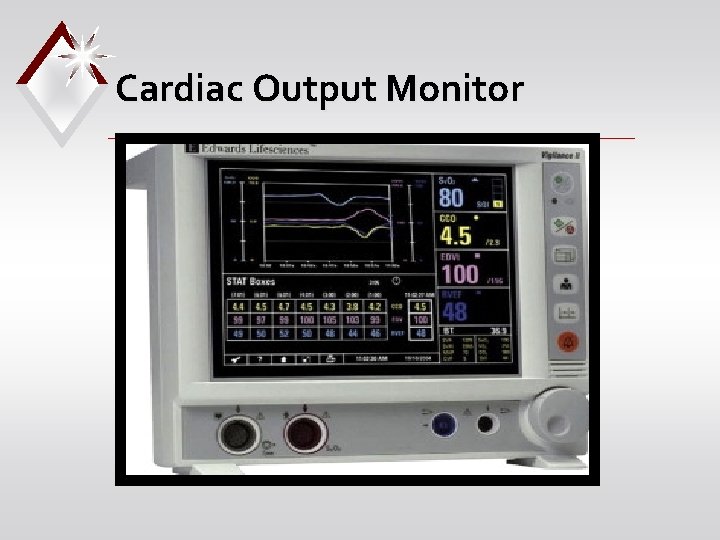
Cardiac Output Monitor
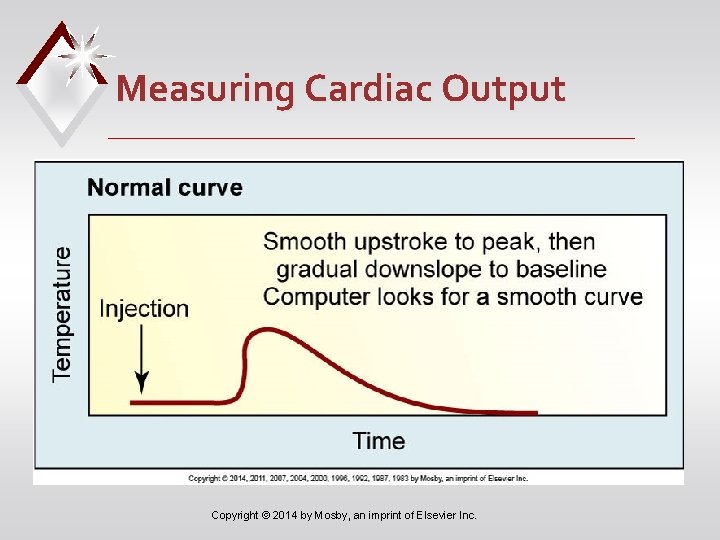
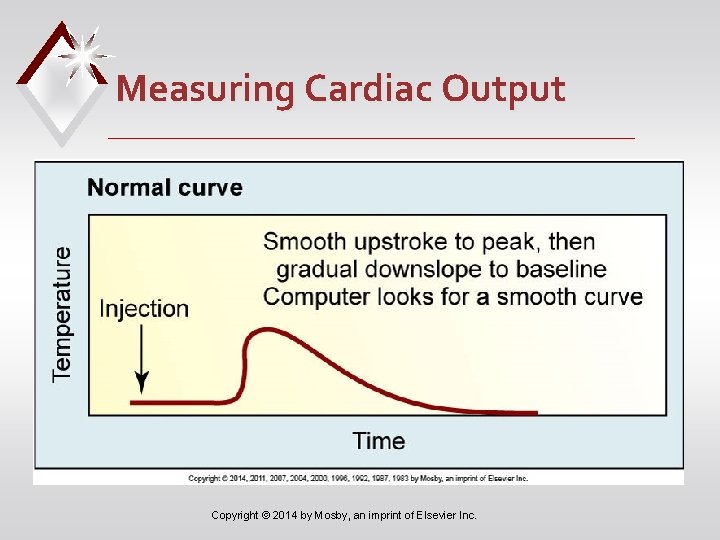
Measuring Cardiac Output Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Measuring Cardiac Output • SVR, SVRI, SV, and SVI calculated when CO is measured • ↑ SVR • Indicates vasoconstriction • ↓ SVR • Indicates vasodilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Venous Oxygen Saturation • PA and CVP catheters can be used • CVP measures central venous oxygen saturation (Scv. O 2) • PA measures mixed venous oxygen saturation (Sv. O 2) • Determines adequacy of tissue oxygenation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Venous Oxygen Saturation • Sv. O 2/Scv. O 2 reflect balance between oxygenation of arterial blood, tissue perfusion, and tissue oxygen consumption. • Assess hemodynamic status and response to treatment/activity • Normal 60%– 80% Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Venous Oxygen Saturation • ↓ In Sv. O 2/Scv. O 2 • ↓ Arterial oxygenation • Low CO • Low hemoglobin level • ↑ Oxygen consumption or extraction Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Venous Oxygen Saturation • ↑ In Sv. O 2/Scv. O 2 • May indicate clinical improvement (e. g. , improved arterial oxygen saturation) • Worsening clinical condition (e. g. , sepsis) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • What nursing interventions will you plan to prevent complications related to A. J. ’s pulmonary artery catheter? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications with PA Catheters • Infection and sepsis • Asepsis for insertion and maintenance • Change flush bag, pressure tubing, transducer, and stopcock every 96 hours • Air embolus (e. g. , disconnection) • Monitor for balloon integrity • Luer-Lok connections; alarms on Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications with PA Catheters • Pulmonary infarction or PA rupture • Do not inflate balloon with >1. 5 ml • Monitor waveforms continuously • Maintain continuous flush system • Ventricular dysrhythmias • Monitor during insertion and removal • Also for migration of PA catheter Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • A. J. ’s PA diastolic and PCWP are elevated. • What does this mean? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Noninvasive Arterial Oxygenation Monitoring • Pulse oximetry • Continuous method of determining arterial oxygenation (Sp. O 2) • Normal 95%– 100% • Accurate measurements may be difficult—consider forehead or earlobe • Used to evaluate effectiveness of O 2 therapy Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Noninvasive Hemodynamic Monitoring • Impedance cardiography (ICG) • Noninvasive method of obtaining CO and assessing thoracic fluid status • Based on concept of impedance • Uses four sets of external electrodes • Measures change in impedance in ascending aorta and left ventricle • Calculates CO, SV, and SVR Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management • Obtain baseline observational data • General appearance • Level of consciousness • Skin color/temperature • Vital signs • Peripheral pulses • Urine output Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management • Correlate baseline data with data obtained from biotechnology (e. g. , ECG; arterial, CVP, PA, and PAWP pressures; Sv. O 2/Scv. O 2) • Monitor trends Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Circulatory Assist Devices (CADs) • Decrease cardiac work and improve organ perfusion when drug therapy fails • Provide interim support when: • Recovering from acute injury • Stabilizing before surgical repair • Awaiting cardiac transplant Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • Despite aggressive medical care, A. J. ’s heart failure does not respond to medical treatment. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • The health care provider decides to insert an intraaortic balloon pump (IABP). • What is the purpose of the IABP? • How does it work? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
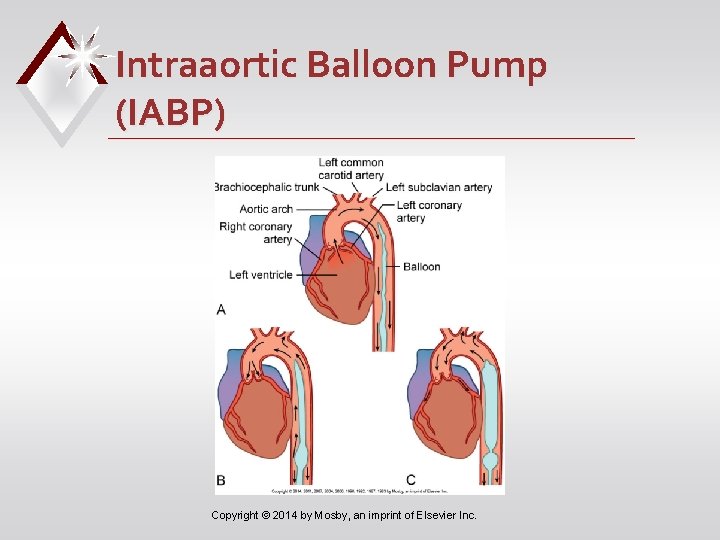
Intraaortic Balloon Pump (IABP) • Most common CAD • Benefits • ↓ventricular workload • ↑myocardial perfusion • Augment circulation • Temporary use only Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Intraaortic Balloon Pump (IABP) • Consists of: • Sausage-shaped balloon • Pump that inflates and deflates balloon • Control panel for synchronizing balloon inflation to cardiac cycle • Fail-safe features Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
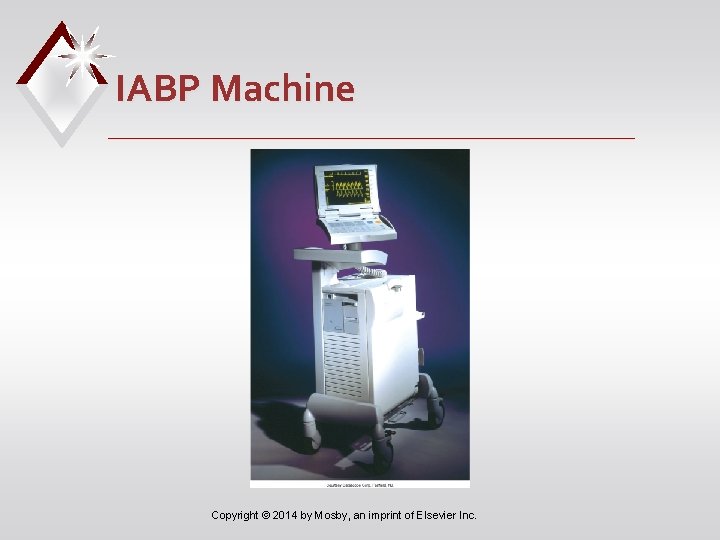
IABP Machine Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
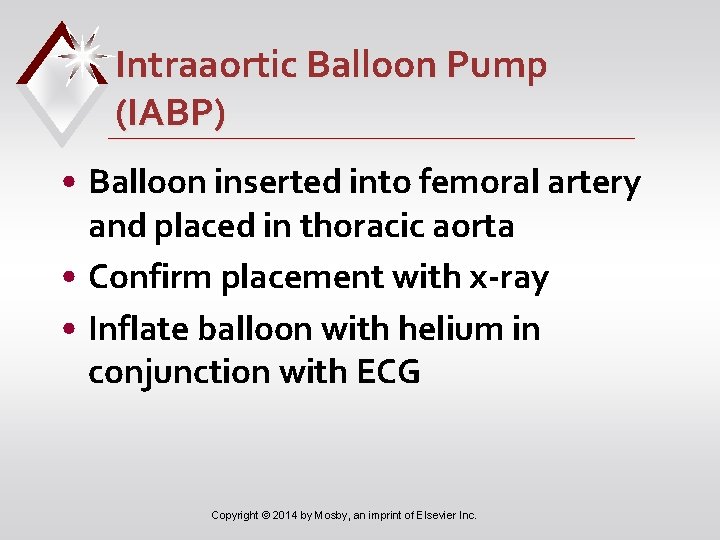
Intraaortic Balloon Pump (IABP) • Balloon inserted into femoral artery and placed in thoracic aorta • Confirm placement with x-ray • Inflate balloon with helium in conjunction with ECG Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
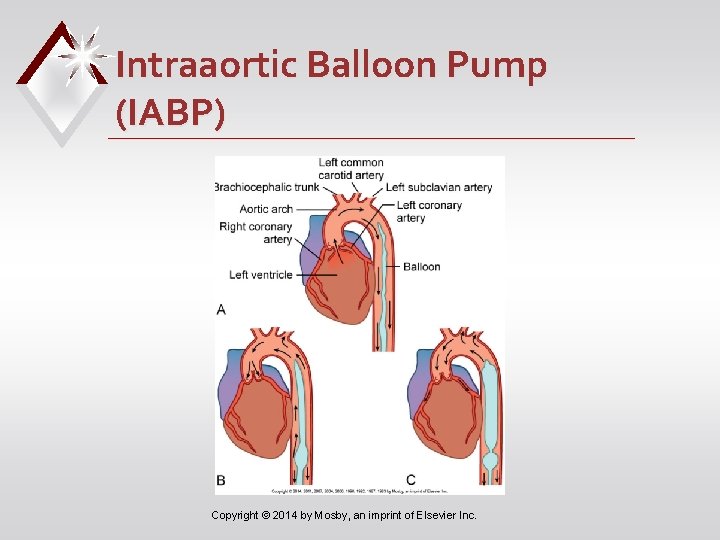
Intraaortic Balloon Pump (IABP) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
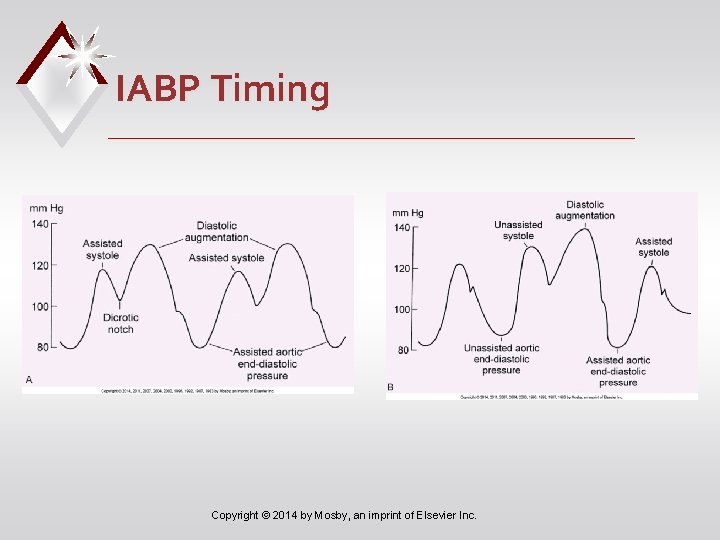
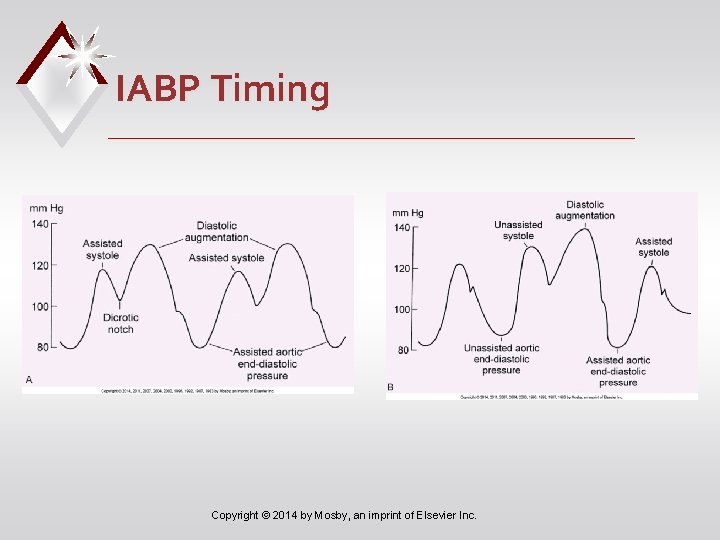
IABP Timing Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Intraaortic Balloon Pump (IABP) • Complications of IABP therapy • Vascular injuries • Thrombus and embolus formation • Thrombocytopenia • Peripheral nerve damage • Ischemia to periphery, kidneys, bowel • Infection Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Intraaortic Balloon Pump (IABP) • Complications of IABP • Mechanical complications • Improper timing of balloon inflation • Balloon leak • Malfunction of balloon or console Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • When updating the plan of care for A. J. , what interventions will you include related to the IABP? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Intraaortic Balloon Pump (IABP) • To decrease risks of IABP therapy • Frequent assessments • Keep patient immobile and limited to side-lying or supine positions with HOB <45 degrees • Wean from IABP by gradually reducing assist ratio Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
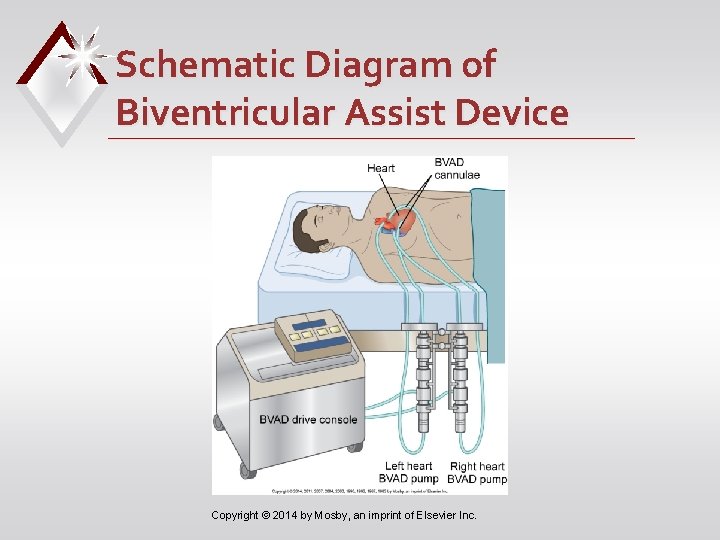
Ventricular Assist Devices (VADs) • Short- and long-term support • Allows more mobility than IABP • Inserted into path of flowing blood to augment or replace action of ventricle • Internal or external • Left, right, or biventricular Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Ventricular Assist Devices (VADs) • VADs can • Be implanted (e. g. , peritoneum) or positioned externally • Provide biventricular support Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
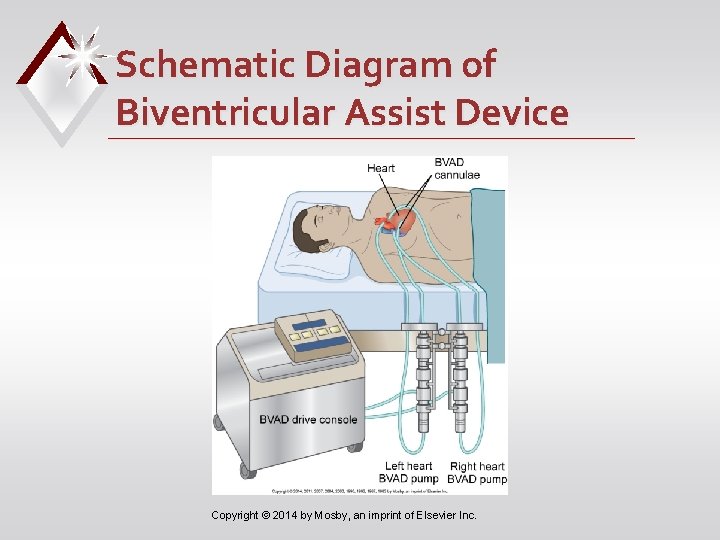
Schematic Diagram of Biventricular Assist Device Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Ventricular Assist Devices (VADs) • Indications for VAD therapy • Failure to wean from bypass • Failure after MI • Bridge while awaiting transplant • Cannula sites depend on type of device used Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Ventricular Assist Devices • Similar to care for patient with an IABP • Frequent assessments and observe for complications • Patient may be mobile and will require an activity plan • In-depth teaching if discharged to home Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Circulatory Assist Devices • Goal • Recovery through ventricular improvement • Heart transplantation • Artificial heart implantation • Many patients die or choose to terminate device, causing death • Emotional support for patient and caregiver essential Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Audience Response Question The nurse is caring for a patient with a pulmonary artery catheter. If the pulmonary artery waveform is blunted, the nurse will suspect which problem? a. The catheter balloon is overinflated. b. The catheter is occluded by a thrombus. c. The catheter is wedged in a pulmonary artery. d. The catheter has migrated to the right ventricle. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
 Central line types
Central line types Pinsky hemodynamic monitoring
Pinsky hemodynamic monitoring Hemodynamic monitoring system
Hemodynamic monitoring system Edema lesion
Edema lesion Mural thrombus
Mural thrombus Cerebral infarction
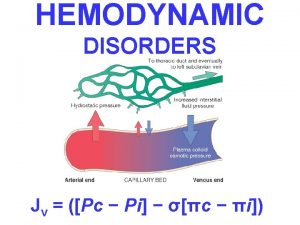
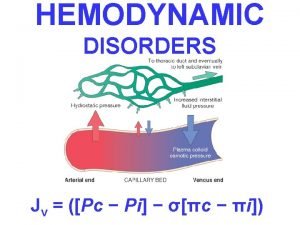
Cerebral infarction Hemodynamic disorders
Hemodynamic disorders Robbins
Robbins Difference between hyperemia and congestion
Difference between hyperemia and congestion Hemodynamic disorders
Hemodynamic disorders Dynapulse
Dynapulse Swan ganz catheter
Swan ganz catheter Chapter 33 circulatory and respiratory systems
Chapter 33 circulatory and respiratory systems One teach, one assist pros and cons
One teach, one assist pros and cons Hormonal stimulus
Hormonal stimulus Chapter 34 section 2 the respiratory system
Chapter 34 section 2 the respiratory system Chapter 19 the circulatory or cardiovascular system
Chapter 19 the circulatory or cardiovascular system Redcap choa
Redcap choa A coaching relationship focuses on providing marines
A coaching relationship focuses on providing marines Quality assist
Quality assist Leslie miller md
Leslie miller md Cisco smart assist
Cisco smart assist Peer assist adalah
Peer assist adalah Als assist
Als assist The whips assist the party leaders by
The whips assist the party leaders by Travel guard modify policy
Travel guard modify policy Pam assist contact number
Pam assist contact number Conclusion of brake system
Conclusion of brake system Intelligent assist device
Intelligent assist device A defective vacuum brake booster will cause a ________.
A defective vacuum brake booster will cause a ________. Assist user guide
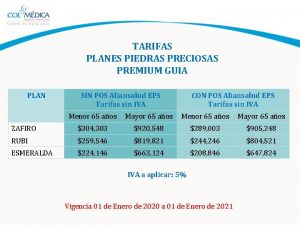
Assist user guide Esmeralda guia premium
Esmeralda guia premium Pbx call assist 2
Pbx call assist 2 School mental health assist
School mental health assist Mediassistindia login
Mediassistindia login Fire team column
Fire team column Business essentials smbs springchambers9to5mac
Business essentials smbs springchambers9to5mac Cough assist als
Cough assist als Gx assist side effects
Gx assist side effects Park assist 2
Park assist 2 Mission assist
Mission assist Info assist
Info assist Assist electrical
Assist electrical What cognitive strategies assist our problem solving
What cognitive strategies assist our problem solving Traffic monitoring devices
Traffic monitoring devices What are the literary techniques
What are the literary techniques Output devices
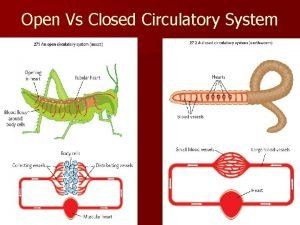
Output devices Difference between open and closed circulatory system
Difference between open and closed circulatory system Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Digestive system respiratory system and circulatory system
Digestive system respiratory system and circulatory system Circulatory and respiratory system working together
Circulatory and respiratory system working together Reptile circulatory system
Reptile circulatory system Coronary groove
Coronary groove Circulatory system steps in order
Circulatory system steps in order Superchp
Superchp Circulatory system of lungfish
Circulatory system of lungfish Clam circulatory system
Clam circulatory system Circulatory system of a cow
Circulatory system of a cow Carbon dioxide levels in the blood
Carbon dioxide levels in the blood Closed circulatory system
Closed circulatory system Jobs of the circulatory system
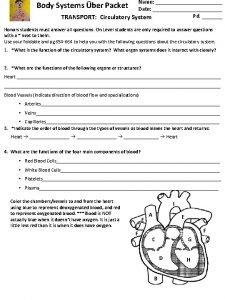
Jobs of the circulatory system 3 main parts of circulatory system
3 main parts of circulatory system Structure of blood cells
Structure of blood cells How respiratory system work with circulatory system
How respiratory system work with circulatory system Active animals
Active animals How circulatory system work
How circulatory system work What makes up the cardiovascular system
What makes up the cardiovascular system Gas exchange oxygen transport
Gas exchange oxygen transport Single circulation and double circulation
Single circulation and double circulation Subphylum
Subphylum Arthropoda
Arthropoda Single vs double circulatory system
Single vs double circulatory system Circulatory system foldable
Circulatory system foldable Invertebrate circulatory system
Invertebrate circulatory system Fetal pig circulatory system
Fetal pig circulatory system Unit 6:8 circulatory system
Unit 6:8 circulatory system Open circulatory system
Open circulatory system Invertebrate circulatory system
Invertebrate circulatory system Main function of the circulatory system
Main function of the circulatory system Two functions of the circulatory system
Two functions of the circulatory system Arthropods circulatory system
Arthropods circulatory system Circulatory system of amphibians
Circulatory system of amphibians Bombyx mori silkworm diagram
Bombyx mori silkworm diagram Function of the circulatory system
Function of the circulatory system