Chapter 9 Hemodynamic Monitoring Copyright 2013 Wolters Kluwer
- Slides: 43
Chapter 9 Hemodynamic Monitoring Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Indications for Hemodynamic Monitoring • Assesses cardiac function and evaluates effectiveness of therapy – Cardiogenic shock – Severe heart failure – Sepsis or septic shock – Multiple organ system dysfunction (MODS) – Acute respiratory distress syndrome (ARDS) – Cardiac surgery Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
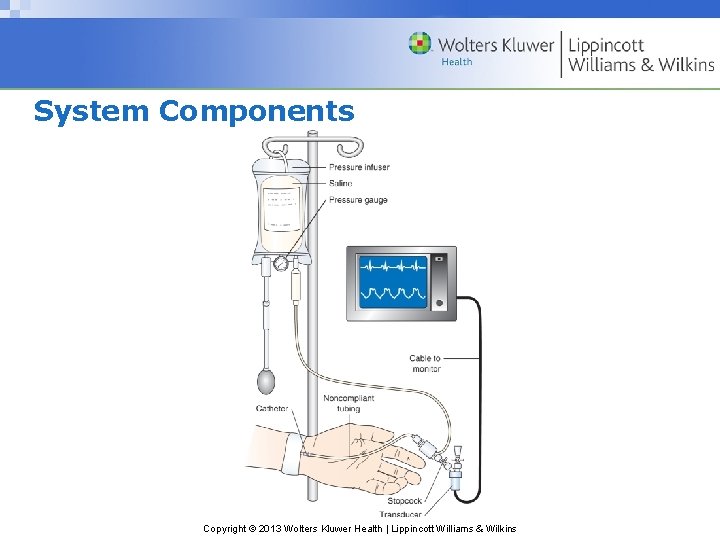
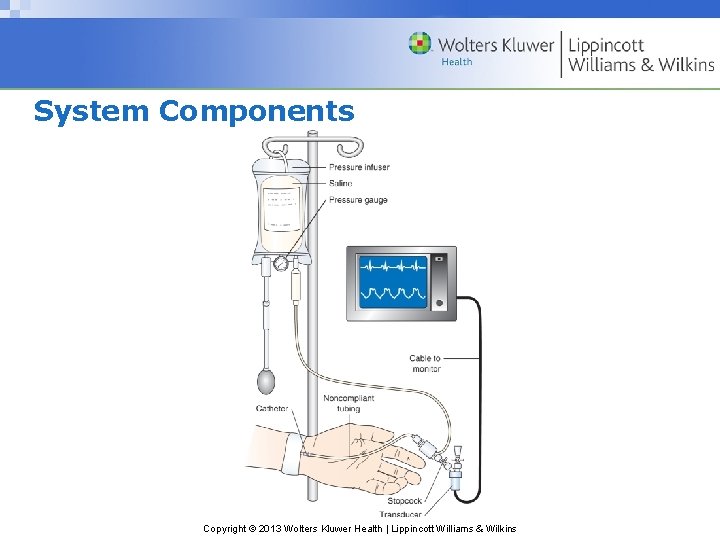
System Components Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
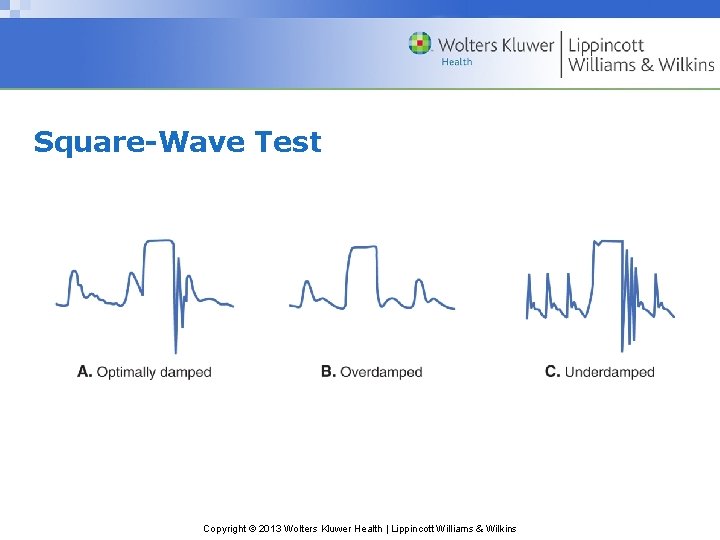
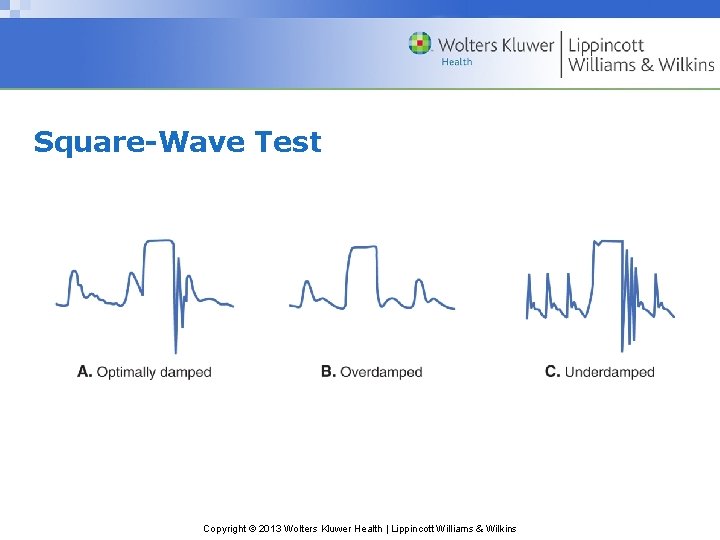
Square-Wave Test Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
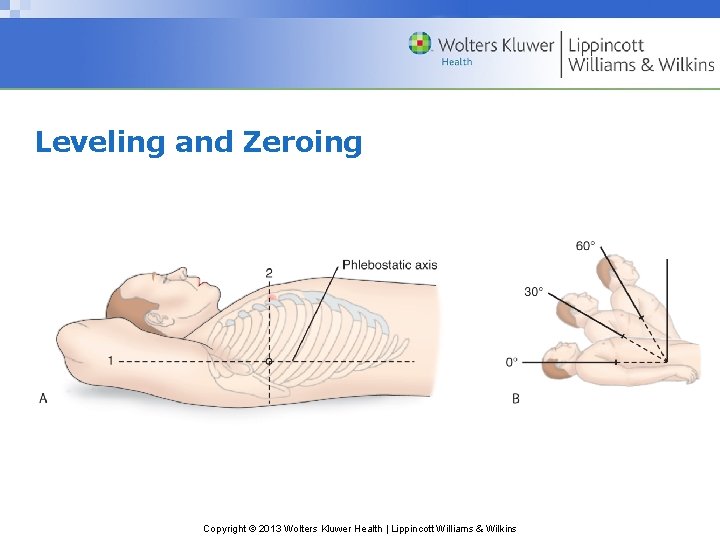
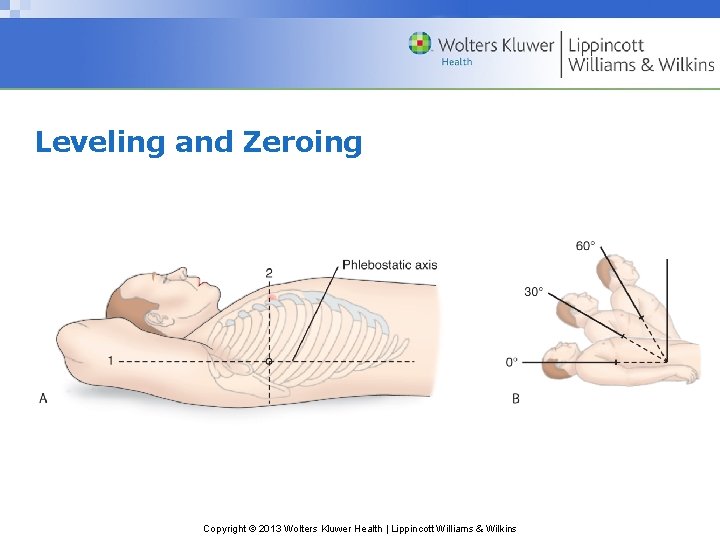
Leveling and Zeroing Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • To ensure accurate arterial pressures, the nurse must level the transducer to what landmark? – A. Nipple line – B. Phlebostatic axis – C. Sternal notch – D. Apical impulse Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • B. Phlebostatic axis • Rationale: The phlebostatic axis is between the fourth intercostal space and midaxillary line; this is the approximate location of the right atrium. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Arterial Pressure Monitoring • Continuous monitoring of arterial blood pressure • Vascular access for obtaining blood samples • Guides therapy Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Interventions for Arterial Lines • Ensure insertion site is visible at all times. • Ensure monitor alarms are visible and audible. • Set parameters according to the facility protocol. – Typically 10 to 20 mm Hg of the patient’s trended blood pressure • DO NOT infuse IV solution or medication through the arterial pressure monitoring system. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
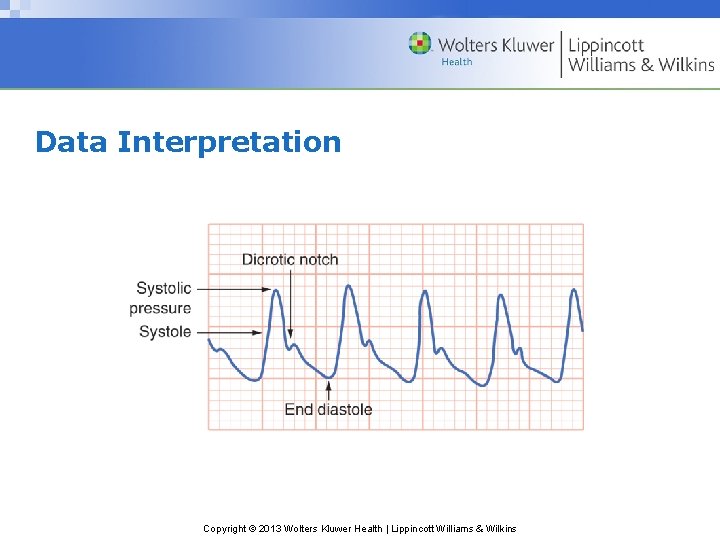
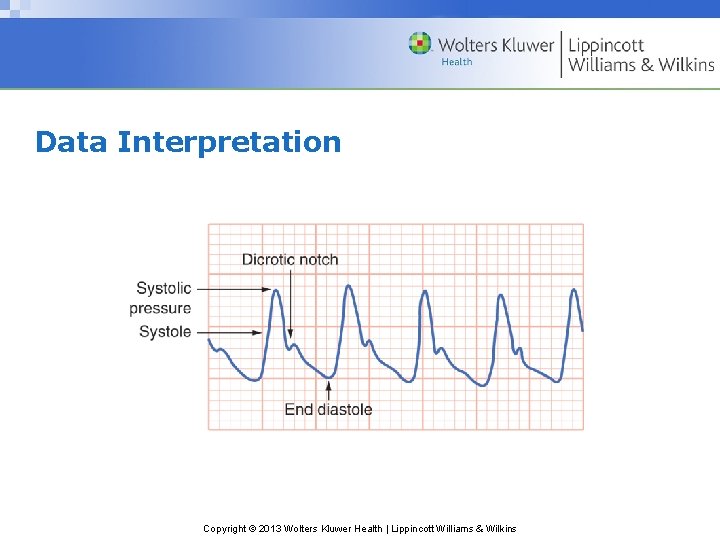
Data Interpretation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following question True or False? • It is acceptable to infuse medications via an arterial line. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • False • Rationale: An arterial pressure line is used for monitoring purposes only. NEVER infuse any medications or IV solutions via this line. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Arterial Lines • Accidental blood loss – Secure and tighten connections. – Immobilize extremity. – Expose extremity. • Infection – Observe a sterile technique. – Maintain a closed system. • Impaired circulation – Assess color, sensation, temperature, and movement of extremity. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Central Venous Pressure Monitoring • Normal values 2 to 8 mm Hg • Measures right atrial pressure • Left ventricular end-diastolic pressure • Reflects intravascular blood volume Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Central Venous Catheters • Infection – Assess the site. – Observe a sterile technique with any catheter manipulation. • Thrombosis – Monitor waveform, ability to flush, blood return. • Pneumothorax – CXR postinsertion • Air embolism – Ensure tight connections. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following statement True or False? • A central venous catheter measures right atrial pressure, left ventricular end-diastolic pressure, and intravascular blood volume. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • True • Rationale: Central venous catheter terminates in the superior vena cava near the right atrium; it measures right atrial pressures, left ventricular end-diastolic pressure, and intravascular blood volume. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pulmonary Artery Catheter • Four lumens – Distal lumen – Proximal lumen – Thermistor lumen – Balloon inflation lumen *Some PACs may have additional lumens. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Interventions for Pulmonary Artery Catheters • Assist with insertion. • Monitor waveform. • Observe for dysrhythmias. • Observe for accidental wedging of the catheter. • Maintain sterile dressing. *Central catheter placement must be confirmed by CXR before accessing the device. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Data Interpretation • Right atrial pressure 2 to 6 mm Hg – Measures pressure in the right ventricle during diastole, equals CVP • Right ventricular pressure 20 to 30 mm Hg – Equals the pulmonary artery systolic pressure Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Data Interpretation (cont. ) • Pulmonary artery pressure – Systolic pressure equals right ventricular systolic function 20 to 30 mm Hg. – Diastolic pressure equals the left ventricular enddiastolic pressure (LVEDP) 8 to 15 mm Hg. • Pulmonary artery wedge pressure 8 to 12 mm Hg – More accurate measure of LVEDP Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Pulmonary Artery Catheters • Ventricular dysrhythmias • Pulmonary artery rupture or perforation • Pulmonary infarction Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cardiac Output • Cardiac output (CO)—the amount of blood ejected from the heart per minute • Stroke volume (SV)—the milliliters of blood ejected from the ventricle with each contraction • HR x SV=CO • 4 to 8 L/minute at rest • Cardiac index (CI)—relates cardiac output to body size; normal is 2. 5 to 4 L/minute/m 2. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Stroke Volume • Preload – Amount of stretch on the myocardial muscle fibers at end diastole • Afterload – The resistance to ejection of blood from the ventricles • Contractility – Ability of the heart to contract independent of preload and afterload Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Methods of Evaluating Cardiac Output • Thermodilution • Arterial pressure and waveform-based methods • Electrical bioimpedance cardiography • Esophageal Doppler monitoring Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Determinants of stroke volume includes all of the following except what? – A. Preload – B. Cardiac output – C. Afterload – D. Contractility Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • B. Cardiac output • Rationale: Stroke volume is the volume of blood ejected from the ventricle with each contraction. Preload, afterload, and contractility determine stroke volume. Stroke volume X heart rate = cardiac output Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
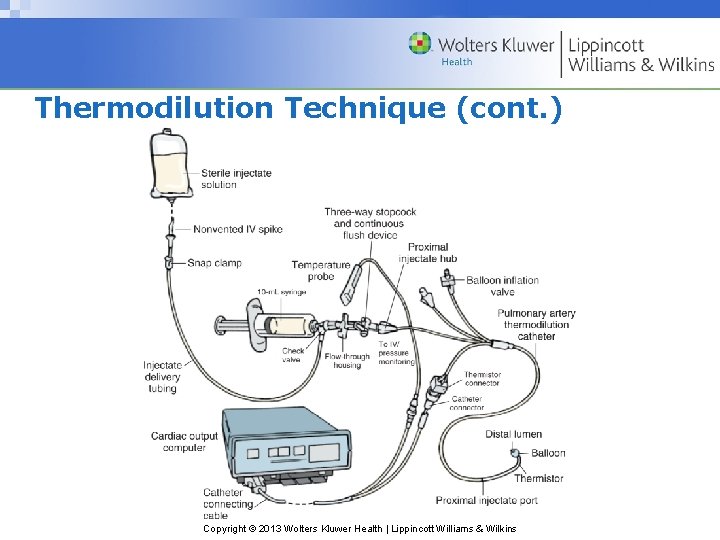
Thermodilution Technique • Gold standard for evaluating cardiac output – Intermittent • Measures change in blood temperature following injection of indicator solution – Continuous • Specialized PACs with thermal filaments Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
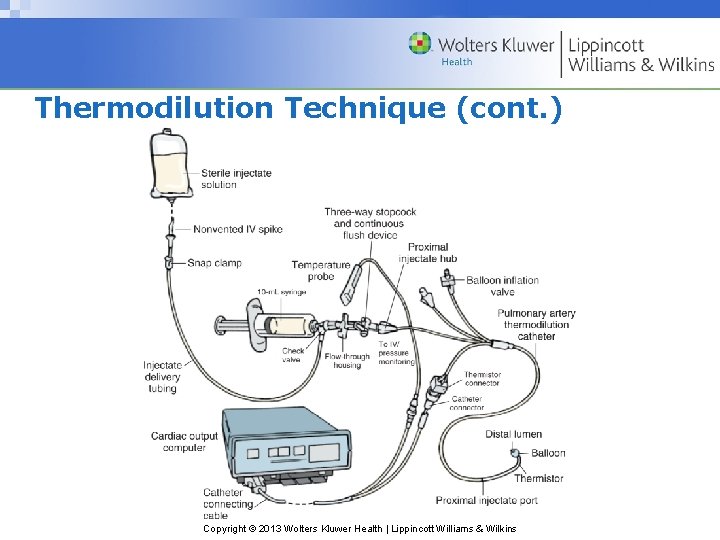
Thermodilution Technique (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
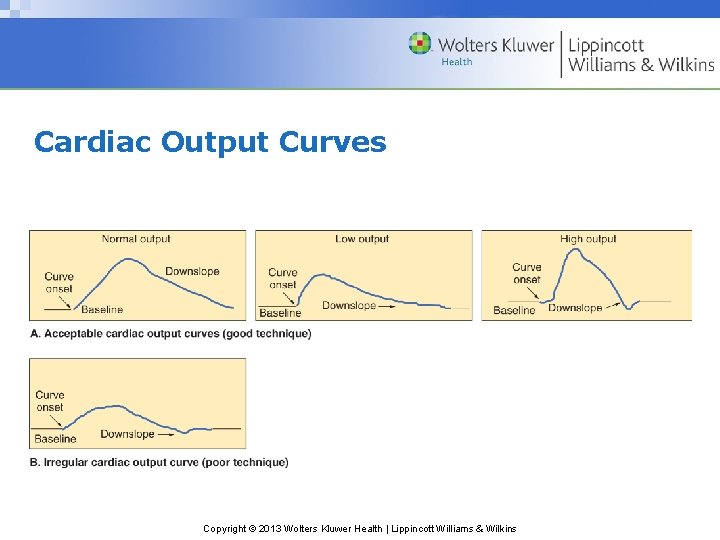
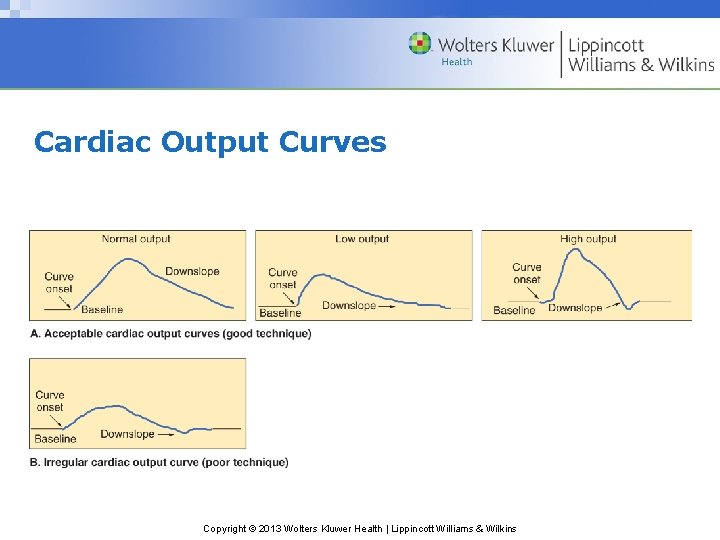
Cardiac Output Curves Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Thermodilution Technique (cont. ) • Ensure volume of injectate in the syringe is correct. • Inject the volume smoothly and rapidly, less than 4 seconds. • Wait approximately 1 minute between injections to allow the catheter thermistor to return to baseline. • Obtain three or more consecutive measurements. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Arterial Pressure and Waveform-Based Method • Proportional relationship between pulse pressure and stroke volume • Inverse relationship between pulse pressure and aortic compliance • Measures using an arterial line, special sensor, and a monitor that uses an algorithm for SV and CO Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Impedance Cardiography • Electrodes placed on the base of the neck and lower thorax • Measures impedance over time and is mathematically converted into SV and CO values using an algorithm Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Esophageal Doppler Monitoring • Doppler transducer in nasogastric tube • Placed in esophagus and monitors blood flow velocity through the descending aorta • Continuous CO and SV are calculated using an algorithm. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • What is the most widely used method to determine cardiac output? – A. Arterial pressure and waveform method – B. Impedance cardiography – C. Esophageal Doppler monitoring – D. Thermodilution Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • D. Thermodilution • Rationale: Thermodilution is the most common method used to measure cardiac output and is considered the clinical gold standard. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Oxygen Delivery and Demand Balance • Oxygen delivery (Da. O 2) – Amount of oxygen transported to tissues – Depends on cardiac output, hemoglobin levels, and arterial oxygen saturation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Balance Between Supply and Demand • Oxygen consumption—the amount of oxygen used by the cells of the body • Primary determinants: – Oxygen demand—the cells requirement for oxygen – Oxygen delivery—need adequate supply of oxygen to deliver to the cells – Oxygen extraction—the amount of oxygen removed from Hgb to be used by the cells Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Global Tissue Oxygenation Status • Metabolic indicators – Lactate levels, serum p. H, and base excess/base deficit • Venous oxygen saturation – Evaluates oxygen supply versus oxygen demand – Mixed venous oxygen saturation Sv. O 2 – Venous oxygen saturation Scv. O 2 Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following statement True or False? • Oxygen extraction is the amount of oxygen removed from Hgb to be used by the cells. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • True • Rationale: Oxygen extraction—the amount of oxygen removed from Hgb to be used by the cells; oxygen demand is the cells’ requirement for oxygen, oxygen delivery the need for adequate supply of oxygen to deliver to the cells. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
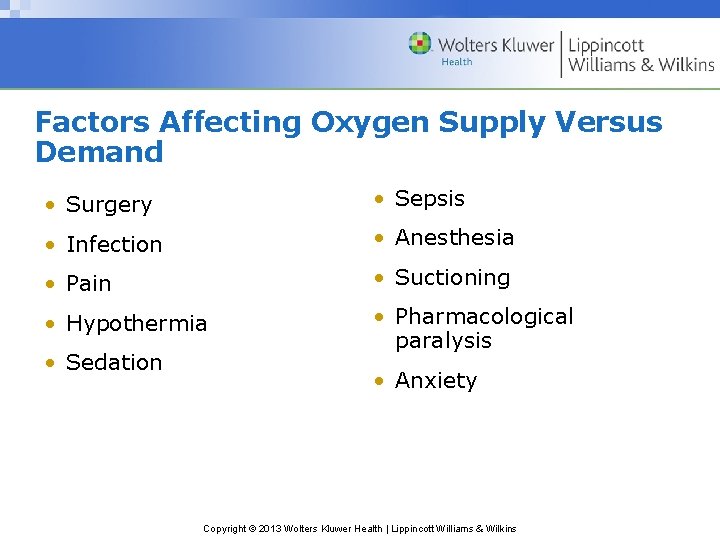
Factors Affecting Oxygen Supply Versus Demand • Surgery • Sepsis • Infection • Anesthesia • Pain • Suctioning • Hypothermia • Pharmacological paralysis • Sedation • Anxiety Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Regional Tissue Oxygenation Status • Gastric tonometry – Specialized nasogastric tube measures partial pressure of carbon dioxide (PCO 2) • Sublingual capnometry – Measures PCO 2 under the tongue Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
 Wolters kluwer health
Wolters kluwer health Wolters kluwer health
Wolters kluwer health Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer health
Wolters kluwer health Wolters kluwer
Wolters kluwer Exercise physiology for health, fitness, and performance
Exercise physiology for health, fitness, and performance Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer health
Wolters kluwer health Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer pronunciation
Wolters kluwer pronunciation Wolters kluwer
Wolters kluwer Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer ovid
Wolters kluwer ovid Wolters kluwer health lippincott williams & wilkins
Wolters kluwer health lippincott williams & wilkins Wolters kluwer culture
Wolters kluwer culture Wolters kluwer pronunciation
Wolters kluwer pronunciation Swan ganz catheter
Swan ganz catheter Pinsky hemodynamic monitoring
Pinsky hemodynamic monitoring Hemodynamic monitoring system
Hemodynamic monitoring system Gross features
Gross features Coagulation casecade
Coagulation casecade Hemodynamic disorders
Hemodynamic disorders Hemodynamic disorders
Hemodynamic disorders Body fluid
Body fluid Hemodynamic disorders
Hemodynamic disorders Hemodynamic disorders
Hemodynamic disorders Normal hemodynamic values
Normal hemodynamic values A line nursing
A line nursing Copyright 2013
Copyright 2013 Kluwer
Kluwer Hotel merken
Hotel merken Kse 2013
Kse 2013 Contoh cover dokumen 1 kurikulum 2013
Contoh cover dokumen 1 kurikulum 2013 Microsoft access 2013 tutorial
Microsoft access 2013 tutorial Quran in word 2013
Quran in word 2013