Chapter 6 Respiratory System Copyright 2012 Wolters Kluwer
- Slides: 37
Chapter 6: Respiratory System Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Structure and Function of the Respiratory System • Structures – Nose/nostrils – Nasal cavity – Pharynx – Larynx – Trachea – Bronchioles – Alveoli Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
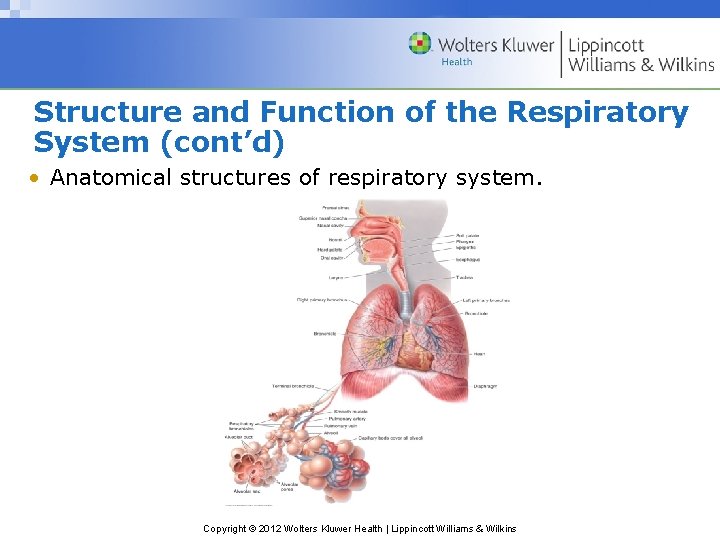
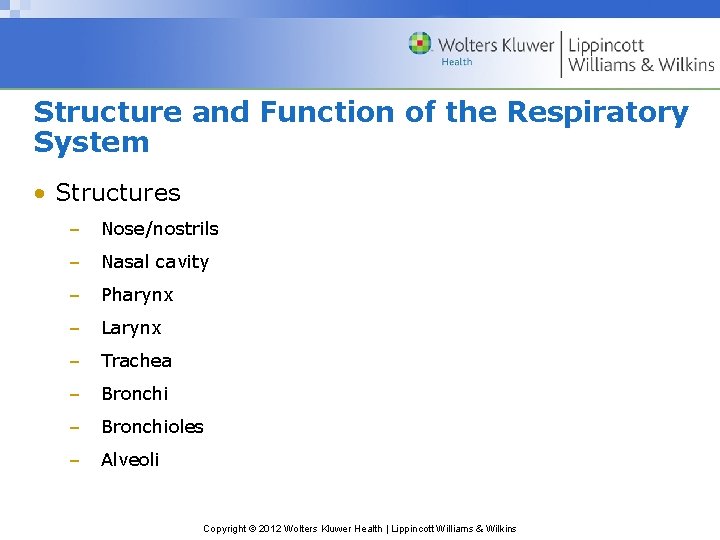
Structure and Function of the Respiratory System (cont’d) • Anatomical structures of respiratory system. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Structure and Function of the Respiratory System (cont’d) • Functions – Conducts air into & out of lungs – Exchanges gases between air & blood – Humidifies air: prevents damage to membranes due to drying out – Warms air: helps maintain body temperature – Filters air • Mucus traps airborne particles • Cilia move mucus toward oral cavity to be expelled Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Structure and Function of the Respiratory System (cont’d) • Alveoli – Saclike structures surrounded by capillaries in lungs – Attached to respiratory bronchioles – Site of exchange of oxygen & carbon dioxide – 300 million in lungs – Provide tremendous surface area where diffusion can take place – Respiratory membrane: 2 cell membranes that aid diffusion • Membrane of alveolar cells • Membrane of cells of capillary wall Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
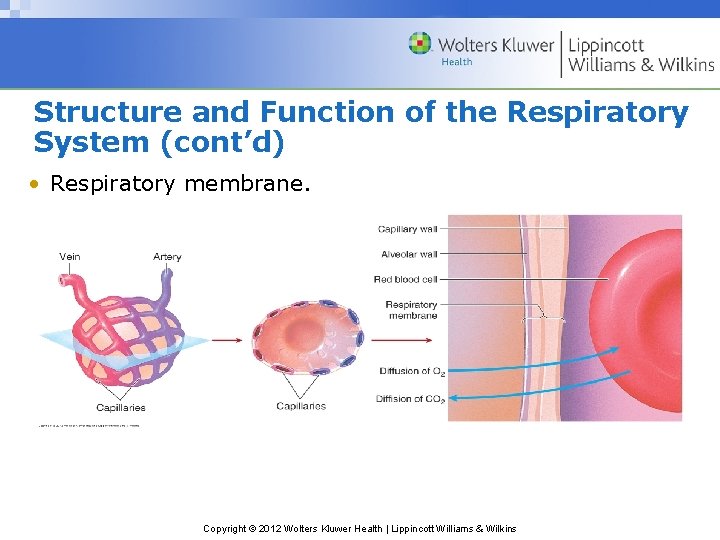
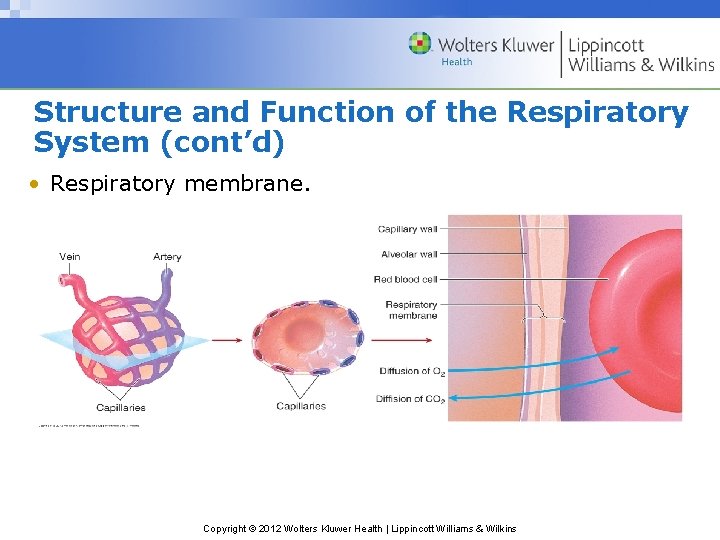
Structure and Function of the Respiratory System (cont’d) • Respiratory membrane. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Mechanics of Ventilation • Pleural Sac – Double-layered membrane that encases each lung • Visceral (pulmonary) pleura: outer surface of lungs • Parietal pleura: inner surface of thoracic cavity & diaphragm • Pleural fluid: lubricating fluid between 2 membranes • Intrapleural pressure: pressure in pleural cavity between 2 membranes; less than atmospheric pressure Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
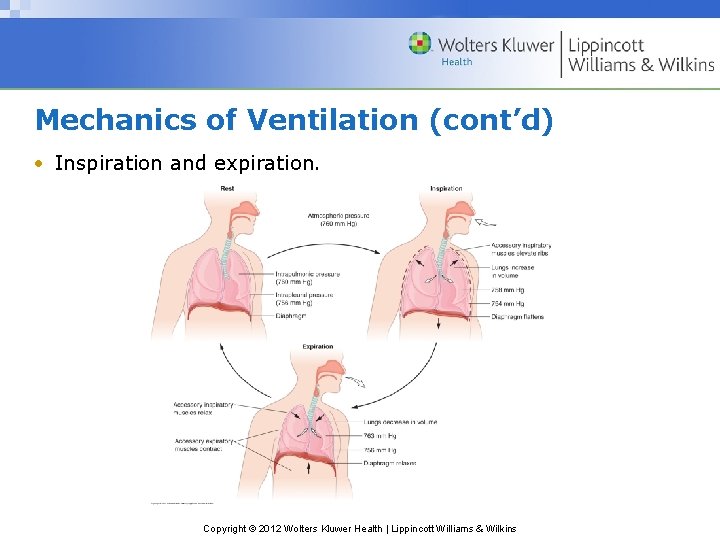
Mechanics of Ventilation (cont’d) • Pressure Changes During Ventilation – Increase in volume of intrathoracic cavity: • Increases lung volume • Decreases intrapulmonic pressure • Causes air to rush into lungs (inspiration) – Decrease in volume of intrathoracic cavity: • Decreases lung volume • Increases intrapulmonic pressure • Causes air to rush out of lungs (expiration) Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
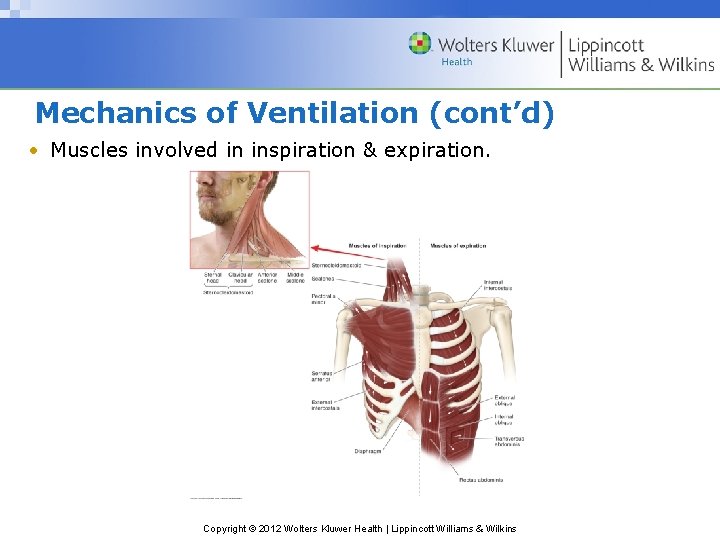
Mechanics of Ventilation (cont’d) • Inspiration – Inspiratory muscles increase intrathoracic cavity volume – Diaphragm: most important inspiratory muscle • Flattens as it contracts • Puts in motion pressure changes that cause inspiration • Contraction moves abdominal contents forward & downward – Muscles that elevate ribs: external intercostals, scalenes, sternocleidomastoid, pectoralis minor Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Mechanics of Ventilation (cont’d) • Expiration – No muscular effort needed at rest – Passive recoil of diaphragm & other muscles decreases intrathoracic cavity volume – During exercise or voluntary forced expiration, accessory muscles of expiration contract, pulling ribs downward: • Internal intercostals • Rectus abdominis • Internal oblique muscles of abdominal wall Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
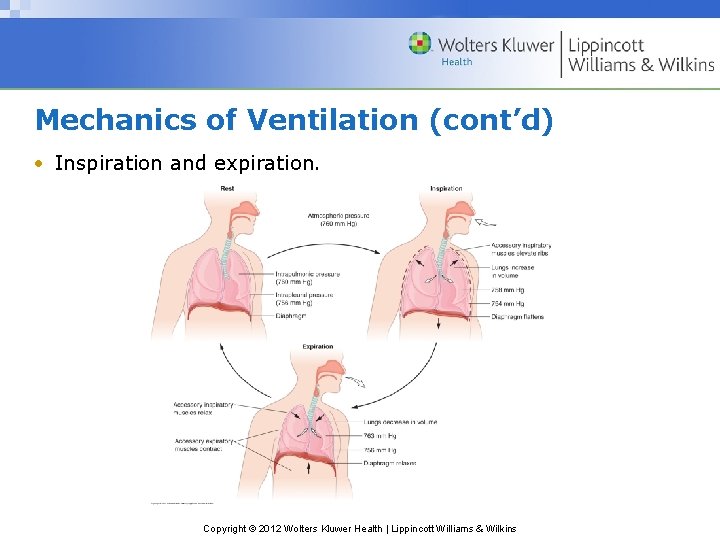
Mechanics of Ventilation (cont’d) • Inspiration and expiration. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
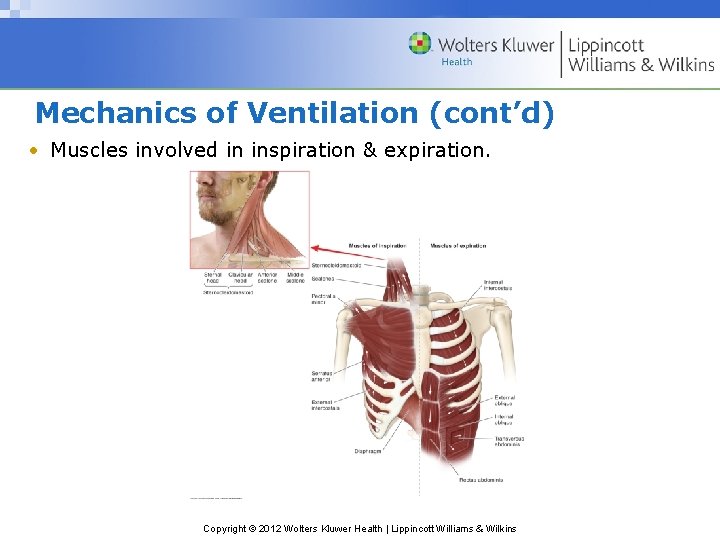
Mechanics of Ventilation (cont’d) • Muscles involved in inspiration & expiration. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Mechanics of Ventilation (cont’d) • Airflow Resistance – Airflow = P 1 − P 2/Resistance – Where P 1 − P 2 is pressure difference between 2 areas & Resistance is resistance to airflow between 2 areas – Thus, airflow can be increased by: • Amplifying pressure difference between 2 areas • Decreasing resistance to airflow – Diameter of airway is biggest factor affecting airflow at rest – In exercise, bronchodilation decreases resistance to airflow Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Mechanics of Ventilation (cont’d) • Pulmonary Ventilation – Amount of air moved in & out of lungs in given time period – Tidal volume: amount of air moved per breath – Volume of air moved per minute can be calculated as: • VE = VT × f • Where VE = volume of air expired per minute; VT = tidal volume; f = breathing frequency per minute – Greater in trained athletes – Pulmonary ventilation = anatomical dead space + alveolar ventilation Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
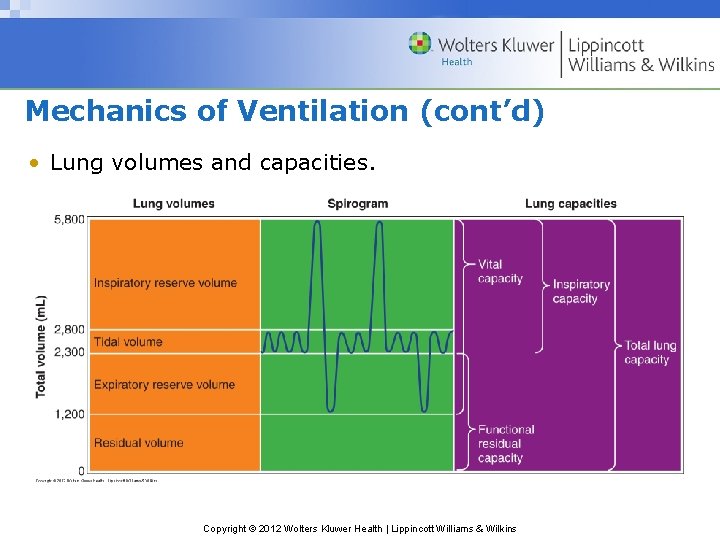
Mechanics of Ventilation (cont’d) • Lung Capacities and Volumes – Determined using spirometry equipment – Reserve of tidal volume at rest allows increase in tidal volume during maximal exercise – Residual volume: air left in lungs after max. exhalation • Frequency and Depth of Breathing – Increase in depth of breathing occurs first after onset of exercise – If increase in depth not sufficient, rate of breathing will increase Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
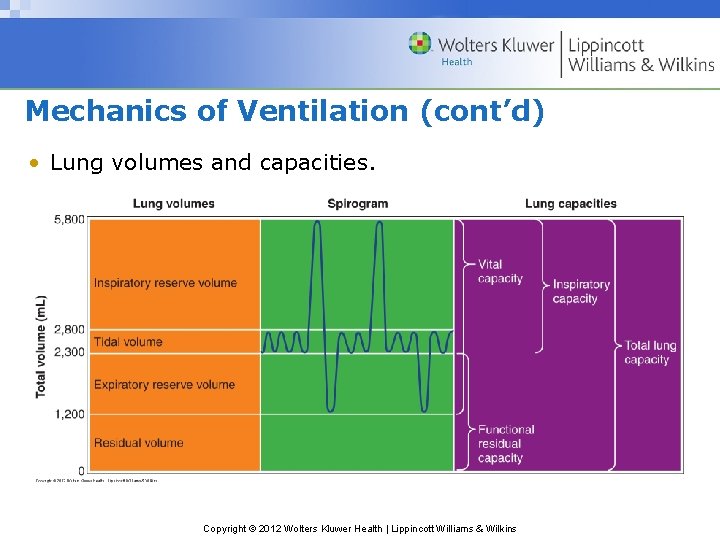
Mechanics of Ventilation (cont’d) • Lung volumes and capacities. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
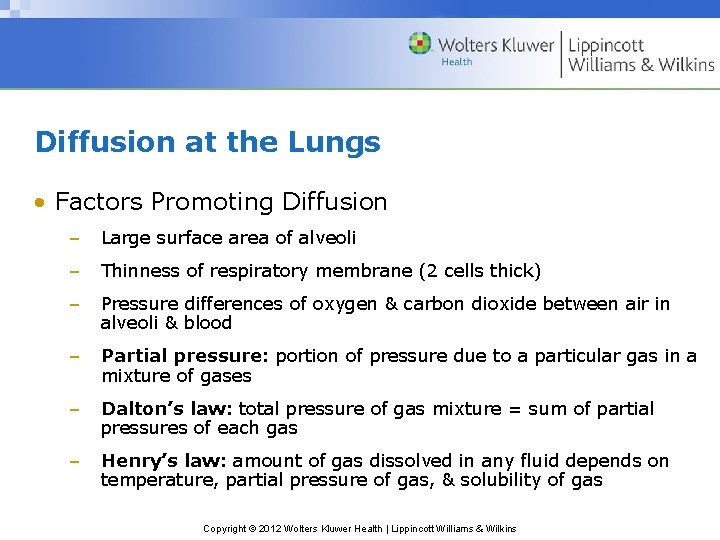
Diffusion at the Lungs • Factors Promoting Diffusion – Large surface area of alveoli – Thinness of respiratory membrane (2 cells thick) – Pressure differences of oxygen & carbon dioxide between air in alveoli & blood – Partial pressure: portion of pressure due to a particular gas in a mixture of gases – Dalton’s law: total pressure of gas mixture = sum of partial pressures of each gas – Henry’s law: amount of gas dissolved in any fluid depends on temperature, partial pressure of gas, & solubility of gas Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
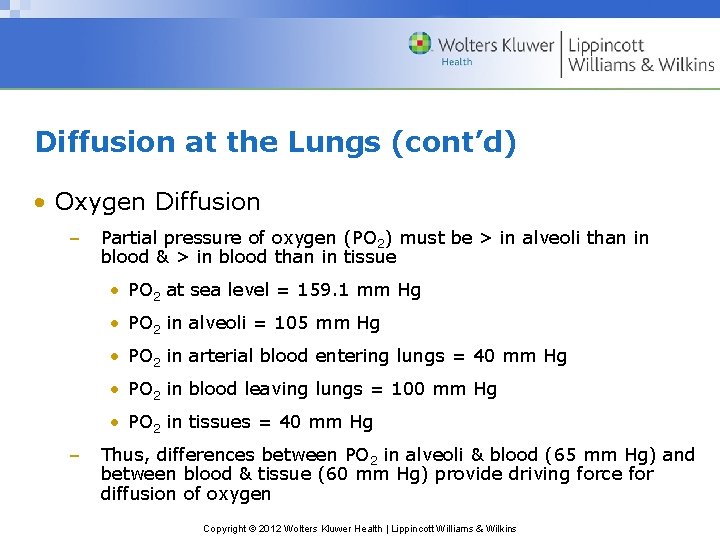
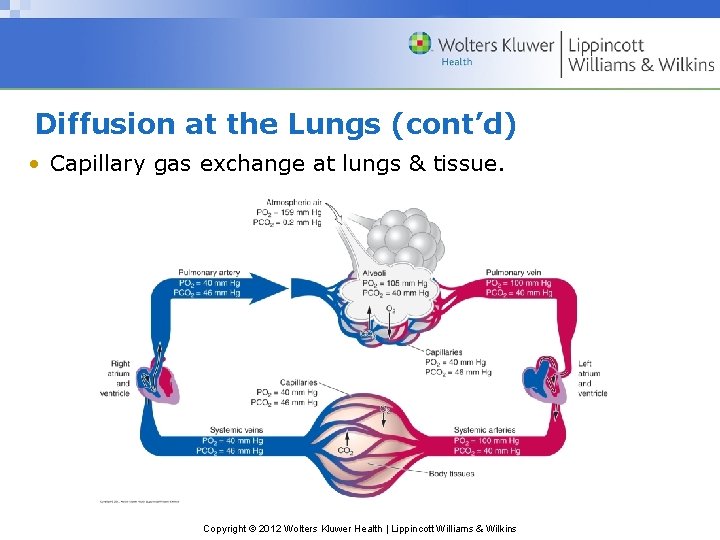
Diffusion at the Lungs (cont’d) • Oxygen Diffusion – Partial pressure of oxygen (PO 2) must be > in alveoli than in blood & > in blood than in tissue • PO 2 at sea level = 159. 1 mm Hg • PO 2 in alveoli = 105 mm Hg • PO 2 in arterial blood entering lungs = 40 mm Hg • PO 2 in blood leaving lungs = 100 mm Hg • PO 2 in tissues = 40 mm Hg – Thus, differences between PO 2 in alveoli & blood (65 mm Hg) and between blood & tissue (60 mm Hg) provide driving force for diffusion of oxygen Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
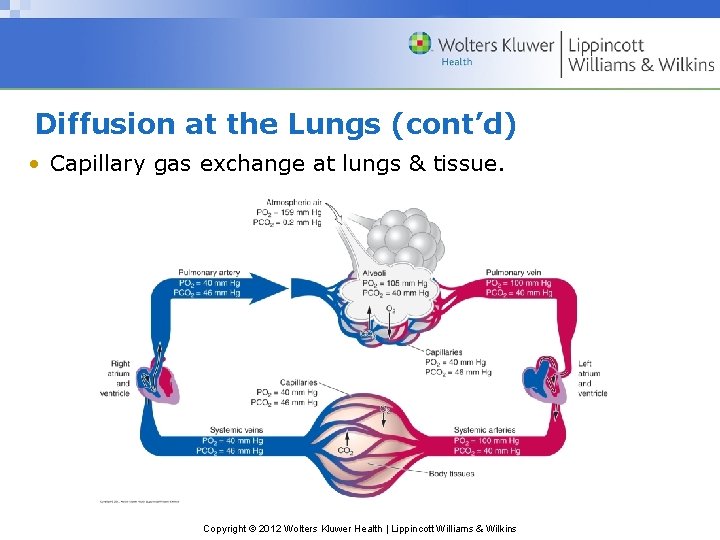
Diffusion at the Lungs (cont’d) • Capillary gas exchange at lungs & tissue. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Diffusion at the Lungs (cont’d) • Carbon Dioxide Diffusion – Partial pressure of carbon dioxide (PCO 2) must be > in blood than in alveoli & > in tissue than in blood • PCO 2 in atmospheric air = 0. 2 mm Hg • PCO 2 in alveoli = 40 mm Hg • PCO 2 in arterial blood entering lungs = 46 mm Hg • PCO 2 in blood leaving lungs = 40 mm Hg • PCO 2 in tissues = 46 mm Hg – Thus, differences between PCO 2 in alveoli & blood (6 mm Hg) and between blood & tissue (6 mm Hg) provide driving force for diffusion of carbon dioxide Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Diffusion at the Lungs (cont’d) • Lung Blood Flow – Determines velocity at which blood passes through pulmonary capillaries – Increased blood flow during exercise results in increased gas diffusion – Blood pressure in pulmonary circulation is low compared with systemic – Equilibration of oxygen between alveoli air & lung capillary blood takes 0. 25 seconds – As blood flow increases with exercise, less time is available for this equilibration – However, increased capillary blood volume slows blood flow Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Blood Gas Transport • Oxygen Transport – Only 9 to 15 m. L of oxygen can be dissolved in plasma, which is insufficient to meet needs of body – RBCs containing hemoglobin transport 98% of oxygen – Oxyhemoglobin: oxygen bound to hemoglobin – Deoxyhemoglobin: hemoglobin not bound to oxygen – Concentration of hemoglobin determines amount of oxygen that can be transported Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
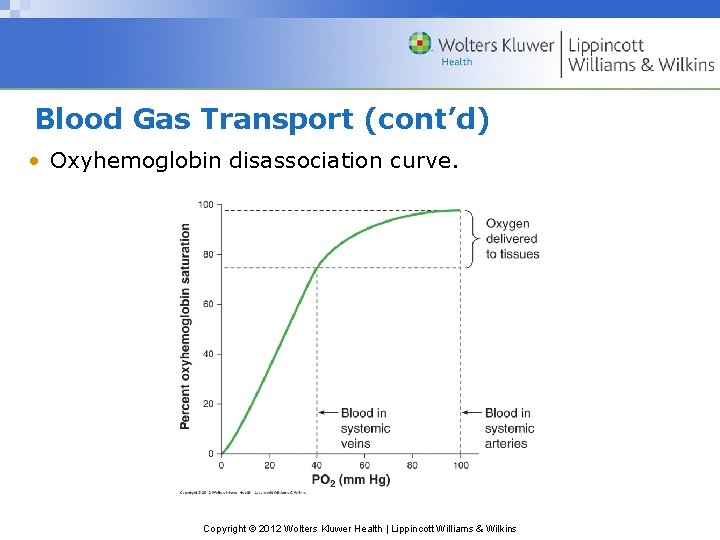
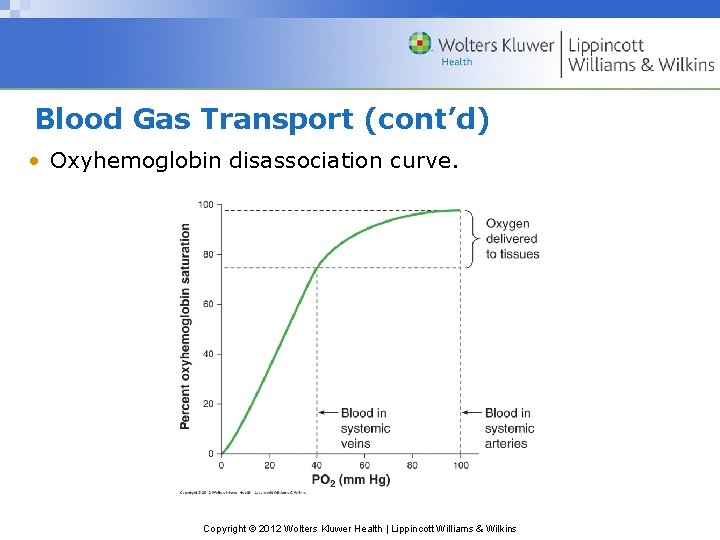
Blood Gas Transport (cont’d) • Oxyhemoglobin disassociation curve. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
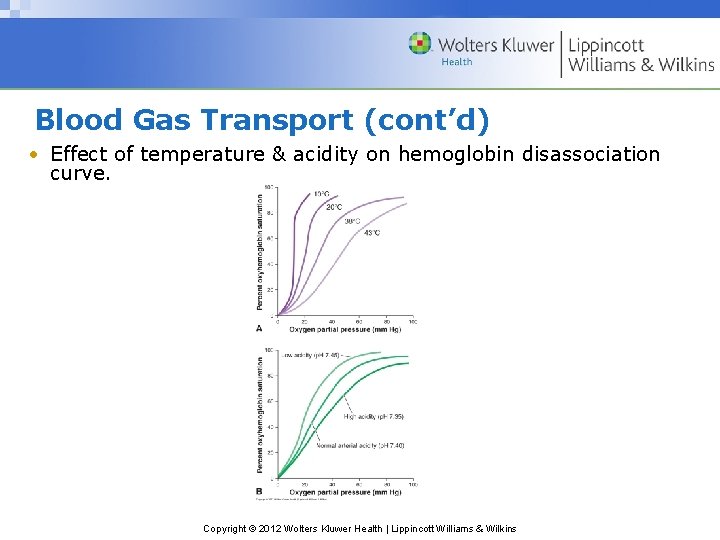
Blood Gas Transport (cont’d) • Oxyhemoglobin Disassociation Curve – Temperature effect • Increase in temp. • Shifts curve to right • Decreases affinity of hemoglobin for oxygen • Decrease in temp. • Shifts curve to left • Increases affinity of hemoglobin for oxygen Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
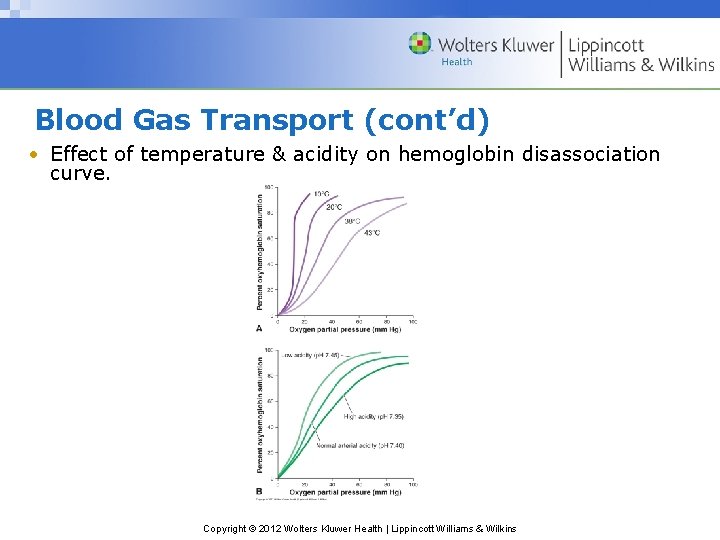
Blood Gas Transport (cont’d) • Effect of temperature & acidity on hemoglobin disassociation curve. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Blood Gas Transport (cont’d) • Oxyhemoglobin Disassociation Curve (cont’d) – p. H effect (Bohr effect) • Increase in acidity • Shifts curve to right • Decreases affinity of hemoglobin for oxygen • Decrease in acidity • Shifts curve to left • Increases affinity of hemoglobin for oxygen Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Blood Gas Transport (cont’d) • Oxyhemoglobin Disassociation Curve (cont’d) – 2, 3 -Diphosphoglycerate (2, 3 DPG) effect • Increase in 2, 3 DPG • Shifts curve to right • Decreases affinity of hemoglobin for oxygen • Decrease in 2, 3 DPG • Shifts curve to left • Increases affinity of hemoglobin for oxygen Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
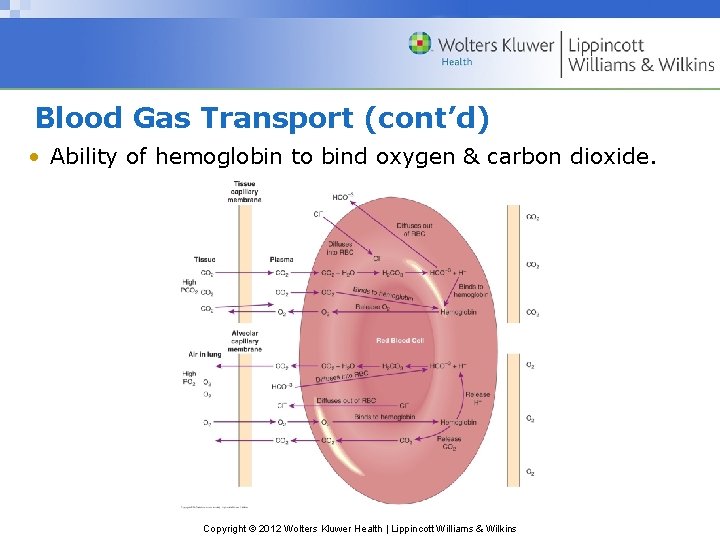
Blood Gas Transport (cont’d) • Carbon Dioxide Transport – 3 methods • 7% to 10% is dissolved in plasma • 20% is bound to hemoglobin • 70% is transported as bicarbonate Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
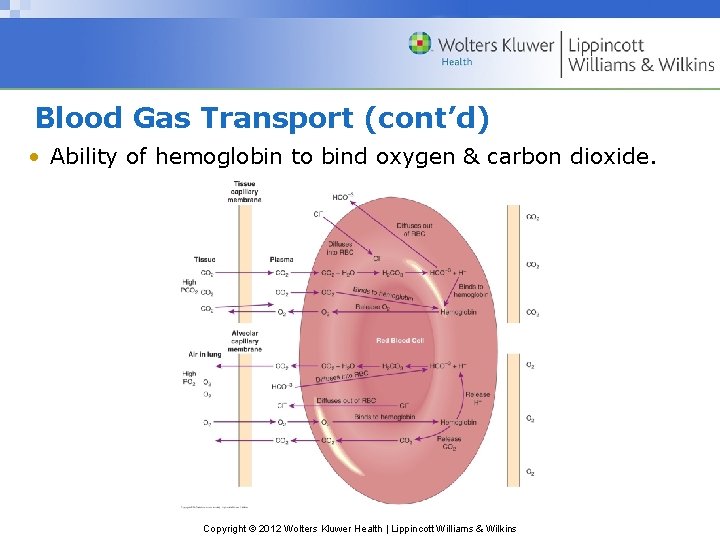
Blood Gas Transport (cont’d) • Ability of hemoglobin to bind oxygen & carbon dioxide. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Gas Exchange at the Muscle • Occurs due to partial pressure differences between oxygen & carbon dioxide between tissue & blood • Myoglobin – Oxygen transport molecule similar to hemoglobin – Found in skeletal & cardiac muscle – Reversibly binds with oxygen – Assists in passive diffusion of oxygen from cell membrane to mitochondria – Functions as oxygen reserve at start of exercise Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
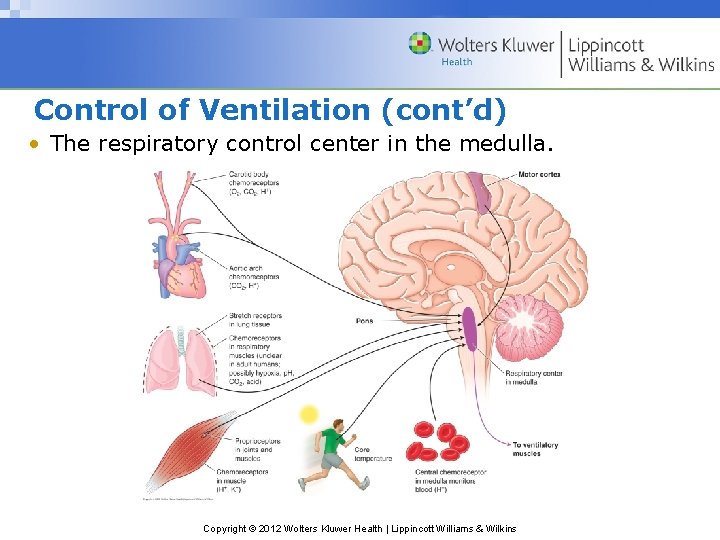
Control of Ventilation • Respiratory Control Center – Portion of medulla oblongata & pons – Serves as pacemaker, generating a rhythmical breathing pattern – Rate & depth of breathing can be modified by: • Higher brain centers • Chemoreceptors in medulla • Other peripheral inputs – Pulmonary ventilation is generally involuntary, but can changed voluntarily Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
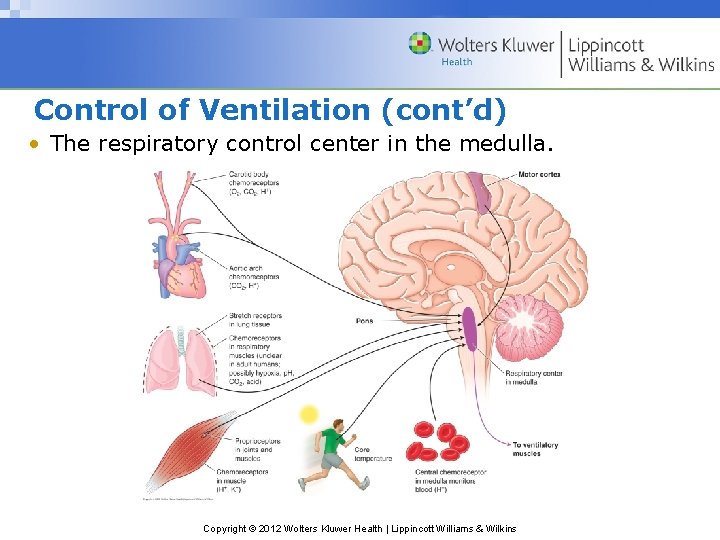
Control of Ventilation (cont’d) • The respiratory control center in the medulla. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
Control of Ventilation (cont’d) • Central Chemoreceptors – Located in medulla, separate from respiratory control center – Respond to changes within CSF, esp. in H+ concentration or p. H • Peripheral Chemoreceptors – Located in carotid arteries & aortic arch – Respond to changes in blood PCO 2 & H+ concentration • Other Neural Input – Stretch receptors in lungs & respiratory muscles – Proprioceptors & chemoreceptors in skeletal muscle & joints Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
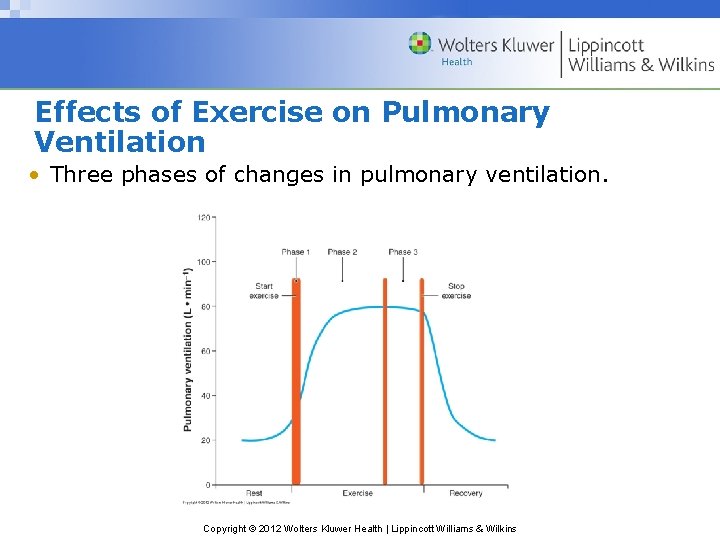
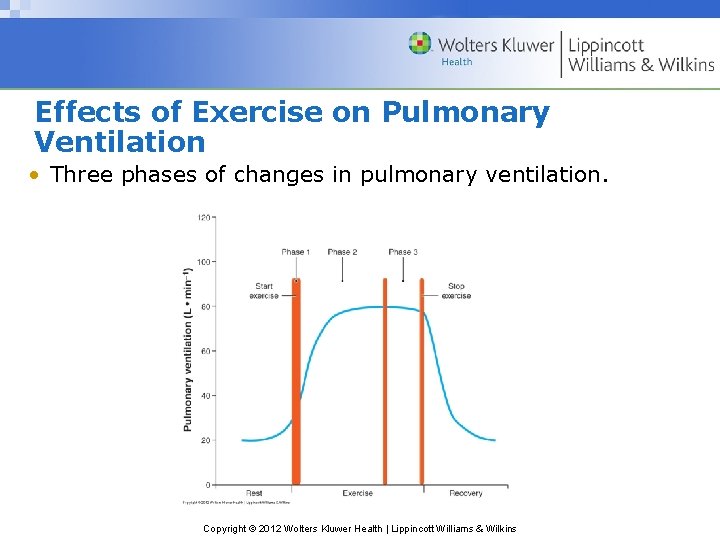
Effects of Exercise on Pulmonary Ventilation • Three phases of changes in pulmonary ventilation. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
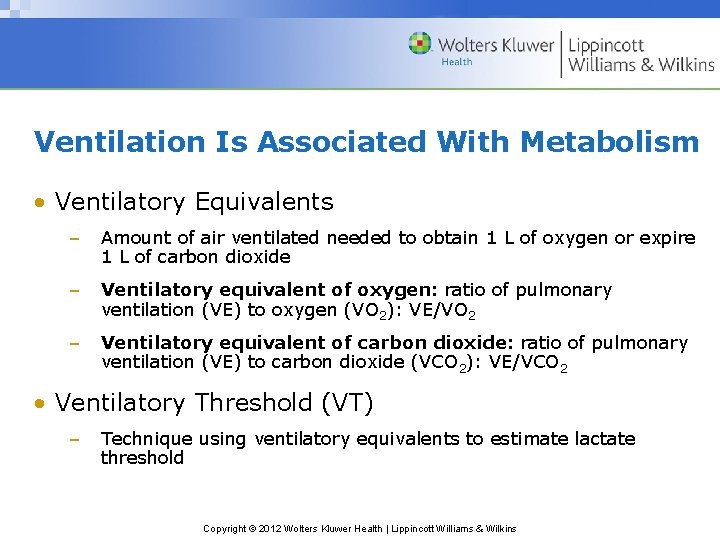
Ventilation Is Associated With Metabolism • Ventilatory Equivalents – Amount of air ventilated needed to obtain 1 L of oxygen or expire 1 L of carbon dioxide – Ventilatory equivalent of oxygen: ratio of pulmonary ventilation (VE) to oxygen (VO 2): VE/VO 2 – Ventilatory equivalent of carbon dioxide: ratio of pulmonary ventilation (VE) to carbon dioxide (VCO 2): VE/VCO 2 • Ventilatory Threshold (VT) – Technique using ventilatory equivalents to estimate lactate threshold Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
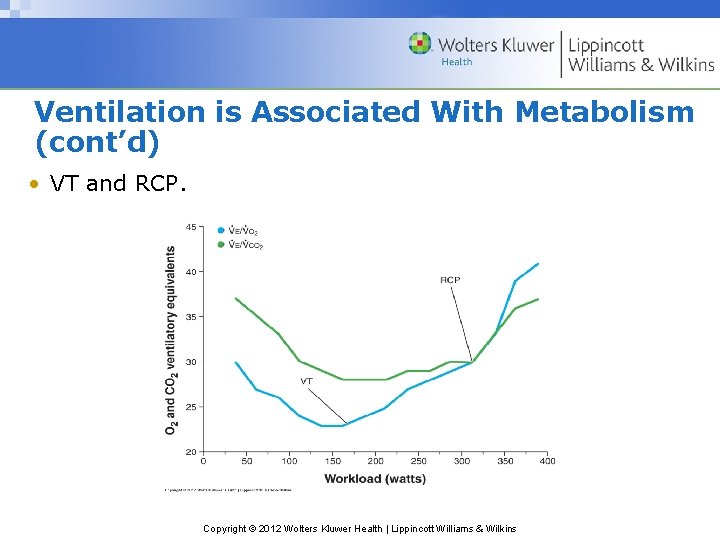
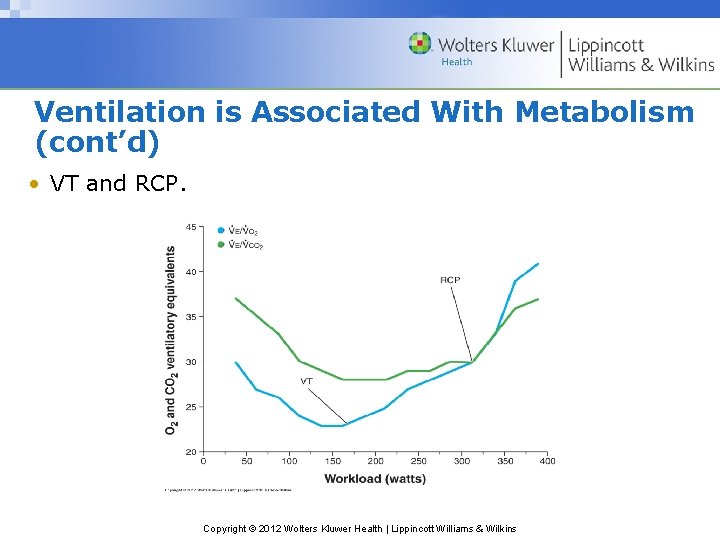
Ventilation is Associated With Metabolism (cont’d) • VT and RCP. Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins
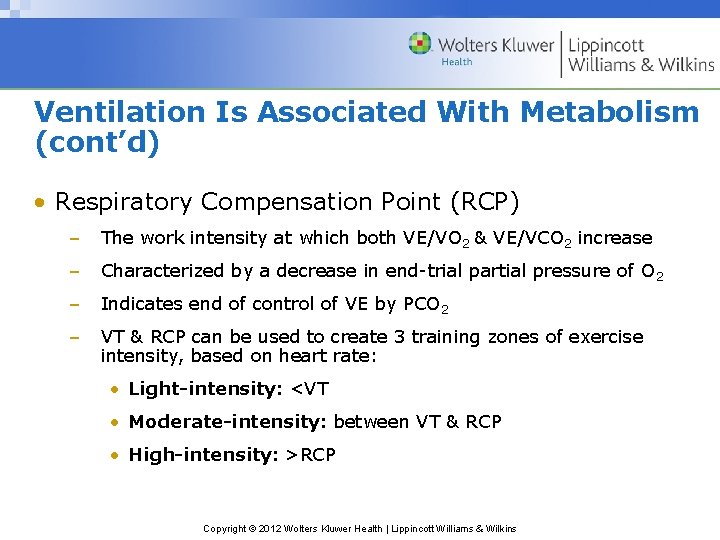
Ventilation Is Associated With Metabolism (cont’d) • Respiratory Compensation Point (RCP) – The work intensity at which both VE/VO 2 & VE/VCO 2 increase – Characterized by a decrease in end-trial partial pressure of O 2 – Indicates end of control of VE by PCO 2 – VT & RCP can be used to create 3 training zones of exercise intensity, based on heart rate: • Light-intensity: <VT • Moderate-intensity: between VT & RCP • High-intensity: >RCP Copyright © 2012 Wolters Kluwer Health | Lippincott Williams & Wilkins