Chapter 28 Wound Care Copyright 2013 Wolters Kluwer
- Slides: 35
Chapter 28 Wound Care Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following statement true or false? Macrophages are types of white blood cells. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer True. Macrophages are types of white blood cells. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wounds • Wound: damaged skin or soft tissue resulting from trauma – Open wounds: mucous membrane is no longer intact – Closed wounds: no open mucous membrane Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
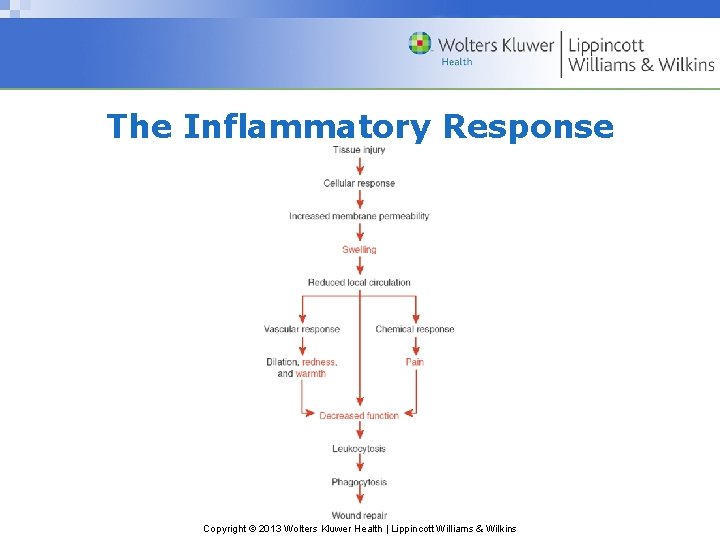
Wound Repair • Inflammation: physiologic defense occurring immediately after tissue injury, lasting 2 to 5 days – Purpose: limit local damage, remove injured cells/debris, prepare wound for healing – Signs and symptoms of inflammation: swelling, redness, warmth, pain, and decreased function Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Repair (cont’d) • Proliferation: period during which new cells fill and seal a wound; it occurs 2 days to 3 weeks after inflammatory phase – The integrity of skin and damaged tissue is restored by resolution, regeneration, and scar formation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Repair (cont’d) • Remodeling: period during which the wound undergoes changes and maturation – Lasts 6 months to 2 years – During remodeling, the wound contracts and the scar shrinks Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
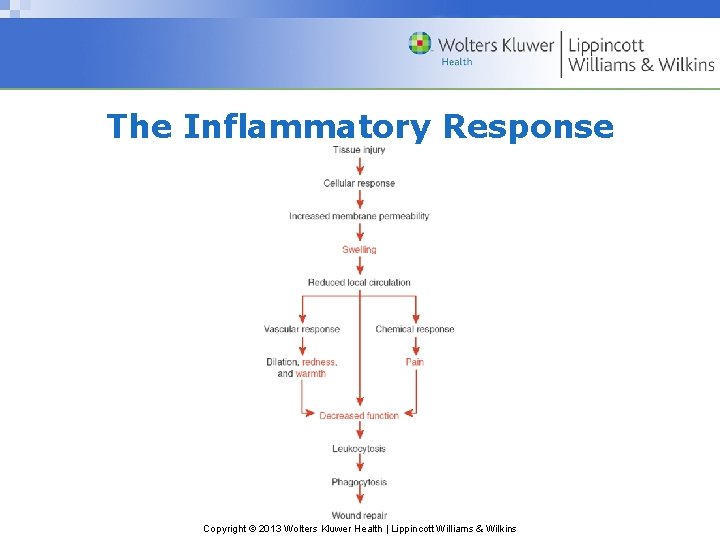
The Inflammatory Response Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
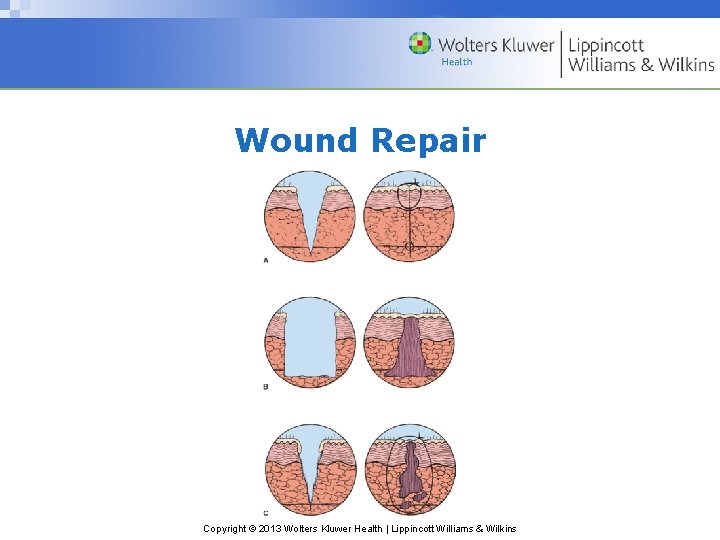
Wound Healing • First-intention healing: reparative process in which wound edges are directly next to each other • Second-intention healing: wound edges are widely separated; time-consuming, complex reparative process • Third-intention healing: deep wound edges brought together with some type of closure material, resulting in a broad, deep scar Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Healing Factors • Type of wound injury • Expanse or depth of wound • Circulation quality • Amount of wound debris • Presence of infection • Client’s health status Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
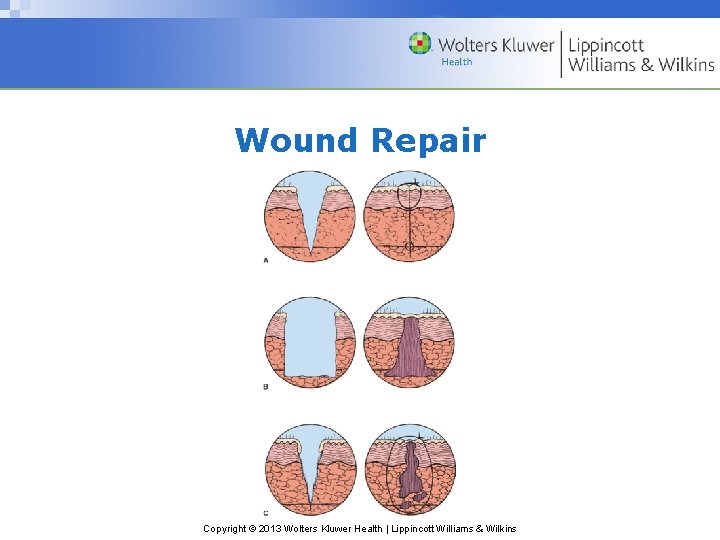
Wound Repair Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Healing Complications • Wound healing key: adequate blood flow to the injured tissue • Interfering factors may include: – Compromised circulation – Infection – Purulent, bloody, or serous fluid accumulation preventing skin and tissue approximation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Healing Complications (cont’d) • Potential surgical wound complications – Dehiscence: separation of wound edges – Evisceration: wound separation with protrusion of organs Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dressings • Dressing purposes: – Keeping wound clean – Absorbing drainage – Controlling bleeding – Protecting wound from further injury – Holding medication in place – Maintaining a moist environment Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dressings (cont’d) • Types of dressings: – Gauze dressings: ideal for covering fresh wounds that are likely to bleed, or wounds that exude drainage – Transparent dressings: used to cover peripheral and central IV insertion sites Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dressings (cont’d) • Types of dressings (cont’d) – Hydrocolloid dressings: keep wounds moist; moist wounds heal more quickly; new cells grow more rapidly in a wet environment – Dressing changes: when a wound requires assessment or care Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Which dressing is ideal for covering fresh wounds that are likely to bleed? a. Gauze b. Transparent c. Hydrocolloid d. Dressing Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer a. Gauze dressing is used for covering fresh wounds. Transparent dressings are used to cover IV insertion sites. Hydrocolloid dressings keep wounds moist. Dressing changes are done when a wound requires assessment, care, or is saturated with drainage. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management • Drains – Open drains – Closed drains • Sutures; Staples Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following statement true or false? Steri-Strips can be used to close superficial lacerations instead of sutures or staples. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer True. Steri-Strips are also used to close superficial lacerations instead of sutures or staples. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management (cont’d) • Bandages and binders – Purpose: hold dressings in place, especially if tape cannot be used or dressing is very large – Support area around the wound or injury to reduce pain – Limit movement in wound area to promote healing Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management (cont’d) • Roller bandage application • Binder application – Different types of binders o Single T-binder o Double T-binder Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management (cont’d) • Debridement: removal of dead tissue – Sharp debridement: using sterile scissors, forceps, etc. – Enzymatic debridement: using chemical substances – Autolytic debridement: natural physiologic process Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management (cont’d) • Debridement (cont’d): – Mechanical debridement: physical removal of debris from a wound using wet-to-dry dressings, hydrotherapy, irrigation o Commonly irrigated structures include: § Wounds, eyes, ears, vagina Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Which type of debridement breaks down and liquefies wound debris? a. Autolytic b. Sharp c. Mechanical d. Enzymatic Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer d. Enzymatic debridement involves the use of topically applied chemical substances. Autolytic debridement allows the body’s enzymes to soften, liquefy, and release devitalized tissue. Sharp debridement is the removal of necrotic tissue with sterile scissors, forceps, or other instruments. Mechanical debridement involves physical removal of debris. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Wound Management (cont’d) • Heat and cold applications – Ice bag and ice collar – Chemical packs – Compresses – Aquathermia pad – Soaks and moist packs – Therapeutic baths Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pressure Ulcers • Also known as decubitus ulcers – Appear over bony prominences of the sacrum, hips, heals, and places where pressure is unrelieved • Risk factors include: − Inactivity, immobility, malnutrition, emaciation − Diaphoresis, incontinence, sedation − Vascular disease, localized edema, dehydration Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pressure Ulcers (cont’d) • Stages of pressure ulcers – Stage I: intact but reddened skin – Stage II: reddened skin accompanied by blistering or a skin tear – Stage III: shallow skin crater that extends to the subcutaneous tissue – Stage IV: deeply ulcerated, extending to muscle and bone; life threatening Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pressure Ulcers (cont’d) • Prevention of pressure ulcers – Change client’s position frequently – Avoid using plastic-covered pillows – Use the lateral position for side-lying – Massage bony prominences – Use pressure-relieving devices – Provide a balanced diet and adequate fluid intake Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Implications • Potential nursing diagnoses: – Acute pain – Impaired skin and tissue integrity – Ineffective tissue perfusion – Risk for infection Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
General Gerontologic Considerations • Wound healing is delayed in older adults; regeneration of healthy skin takes twice as long for an 80 -year-old as it does for a 30 year-old • Age-related changes affecting wound healing include thinning dermal layer of skin; decreased subcutaneous tissue • Signs of inflammation may be more subtle in older adults Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
General Gerontologic Considerations (cont’d) • Diminished immune response from reduced T -lymphocyte cells predisposes older adults to wound infections • Conditions that interfere with circulation increase the older adult’s susceptibility to delayed wound healing and wound infections • Diminished mobility requires aggressive skin care to prevent pressure ulcers Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
General Gerontologic Considerations (cont’d) • Due to decreased blood supply to the skin, older adults may need position changes every 60 to 90 minutes, instead of every 20 minutes • Use special care when moving older adults; avoid friction on the skin • Depression, poor appetite, cognitive impairments, and physical/economic barriers interfering with adequate nutrition may impair wound healing Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
 Wolters kluwer health
Wolters kluwer health Lippincott
Lippincott Edgar lopategui corsino
Edgar lopategui corsino Wolters kluwer
Wolters kluwer Synaptic integration
Synaptic integration Wolters kluwer health
Wolters kluwer health Wolters kluwer health
Wolters kluwer health Exercise physiology for health, fitness, and performance
Exercise physiology for health, fitness, and performance Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer health
Wolters kluwer health Wolters kluwer
Wolters kluwer Wolters kluwer health
Wolters kluwer health Wolters kluwer health
Wolters kluwer health Virchow's triad
Virchow's triad Wolters kluwer pronunciation
Wolters kluwer pronunciation Wolters kluwer
Wolters kluwer Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer
Wolters kluwer Wolters kluwer ovid
Wolters kluwer ovid Wolters kluwer health lippincott williams & wilkins
Wolters kluwer health lippincott williams & wilkins Wolters kluwer culture
Wolters kluwer culture Wolters kluwer pronunciation
Wolters kluwer pronunciation Serosanguineous vs serous
Serosanguineous vs serous Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Copyright 2013
Copyright 2013 Ryb color code wound care
Ryb color code wound care Doylestown wound care center
Doylestown wound care center Shasta regional wound center
Shasta regional wound center Torrance memorial wound care center
Torrance memorial wound care center Code of conduct for healthcare support workers
Code of conduct for healthcare support workers Wound care pretest
Wound care pretest John boswick
John boswick