Hematuria Transient phenomenon of little significance Sign of














- Slides: 44

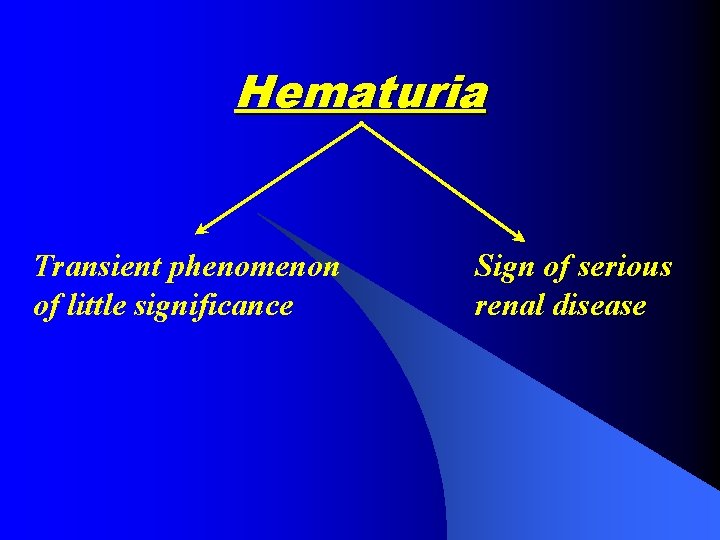
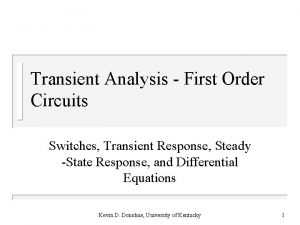
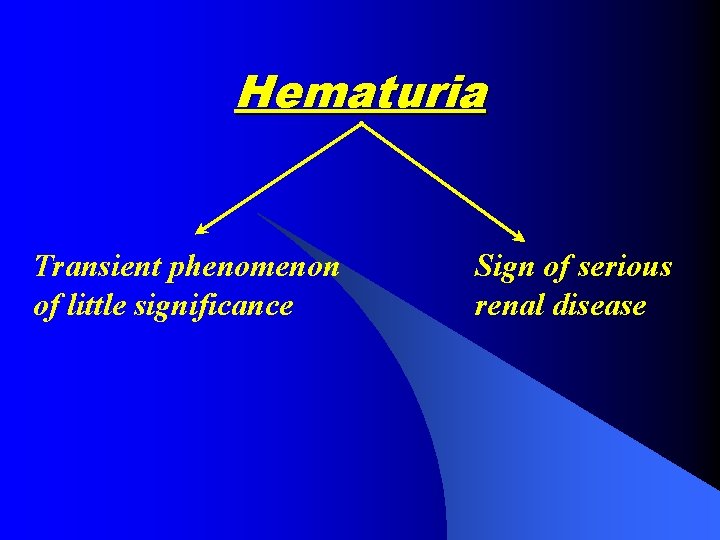
Hematuria Transient phenomenon of little significance Sign of serious renal disease
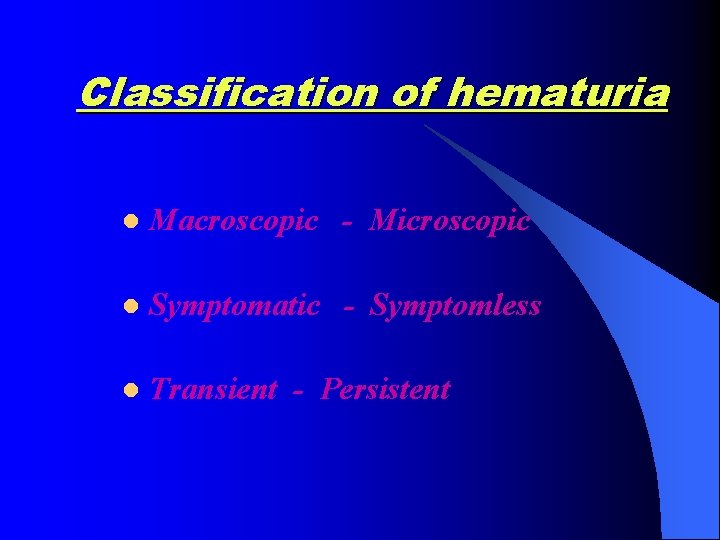
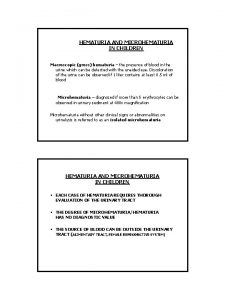
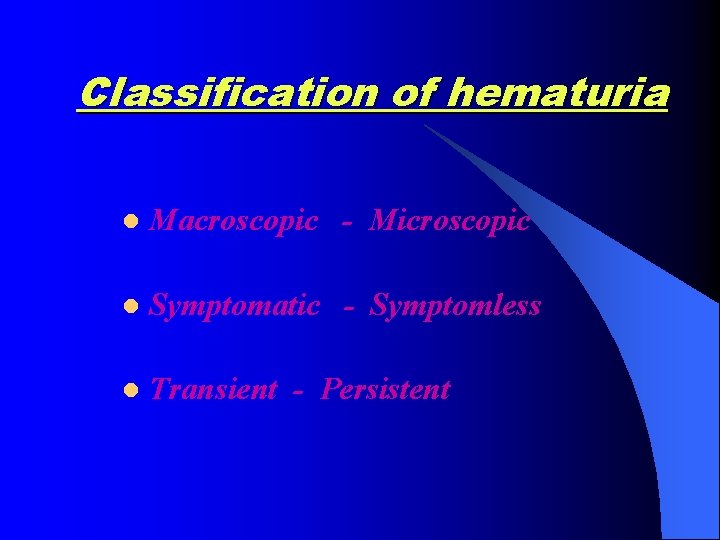
Classification of hematuria l Macroscopic - Microscopic l Symptomatic - Symptomless l Transient - Persistent

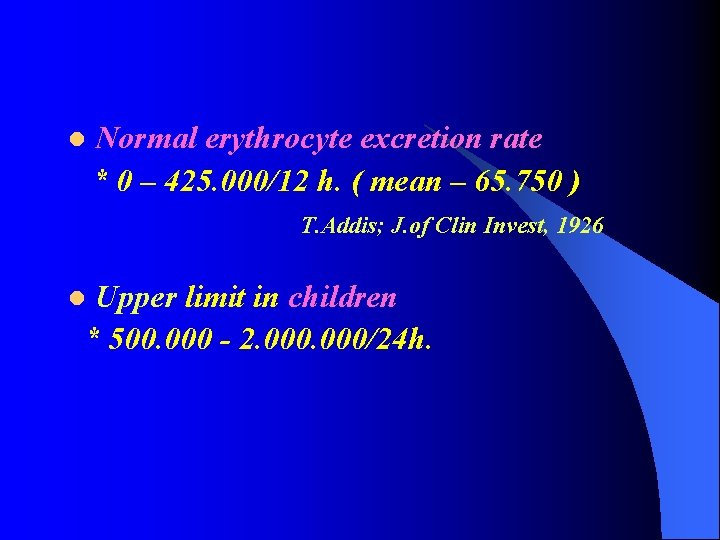
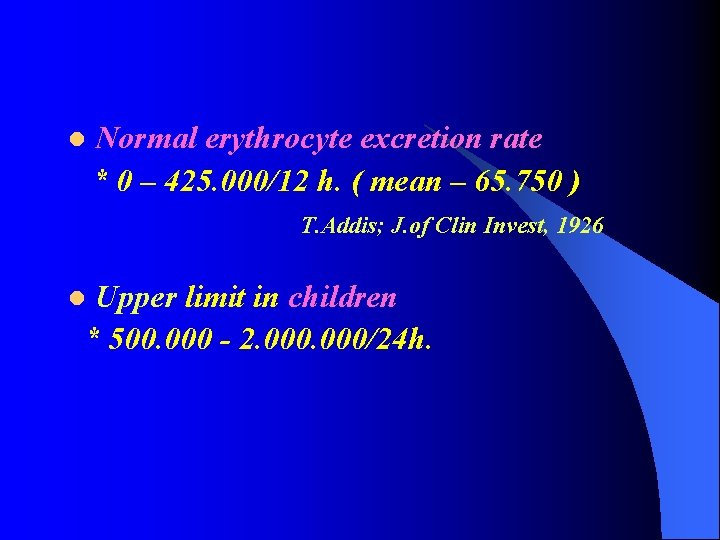
l Normal erythrocyte excretion rate * 0 – 425. 000/12 h. ( mean – 65. 750 ) T. Addis; J. of Clin Invest, 1926 Upper limit in children * 500. 000 - 2. 000/24 h. l
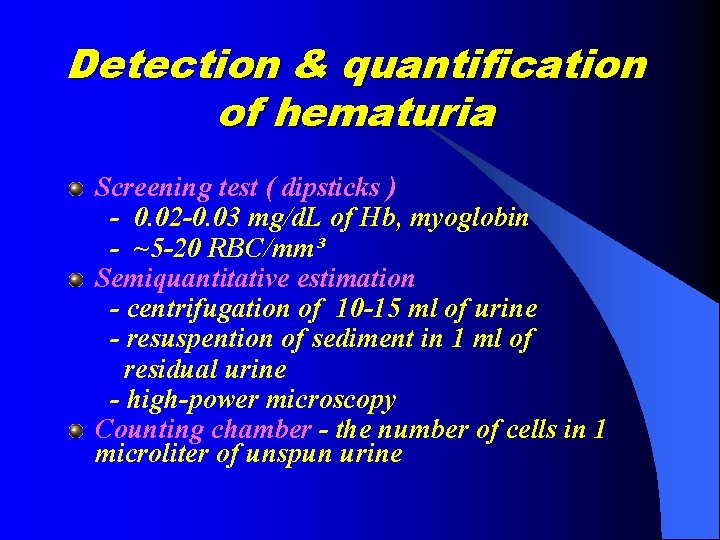
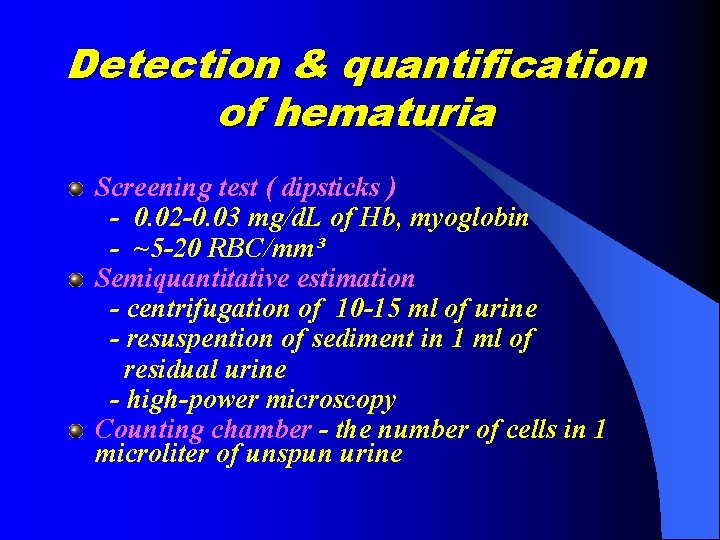
Detection & quantification of hematuria Screening test ( dipsticks ) - 0. 02 -0. 03 mg/d. L of Hb, myoglobin - ~5 -20 RBC/mm³ Semiquantitative estimation - centrifugation of 10 -15 ml of urine - resuspention of sediment in 1 ml of residual urine - high-power microscopy Counting chamber - the number of cells in 1 microliter of unspun urine
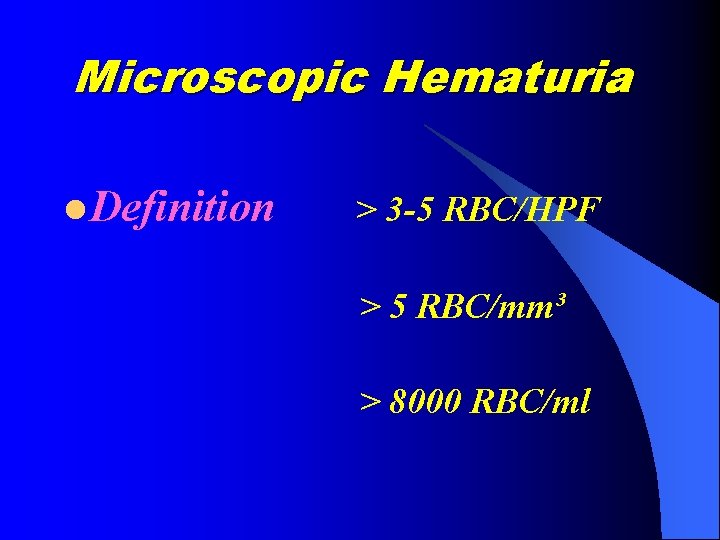
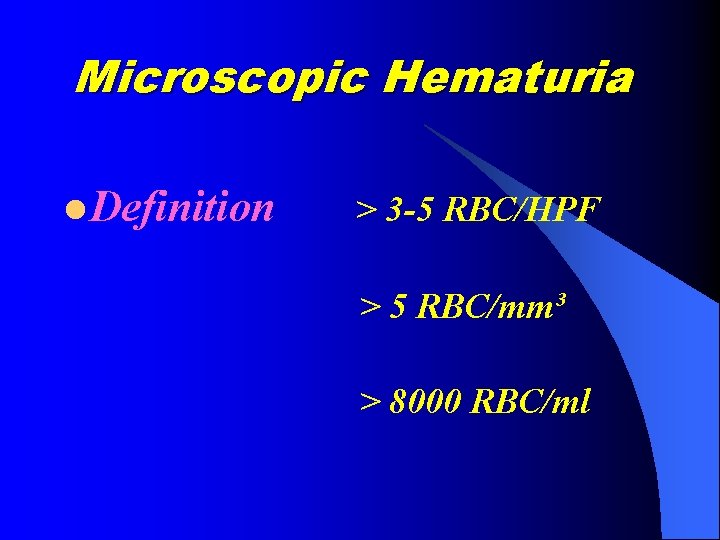
Microscopic Hematuria l Definition > 3 -5 RBC/HPF > 5 RBC/mm³ > 8000 RBC/ml



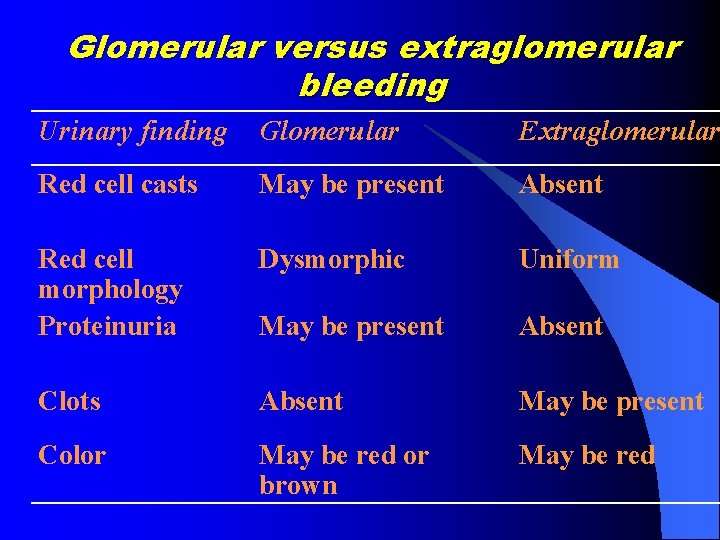
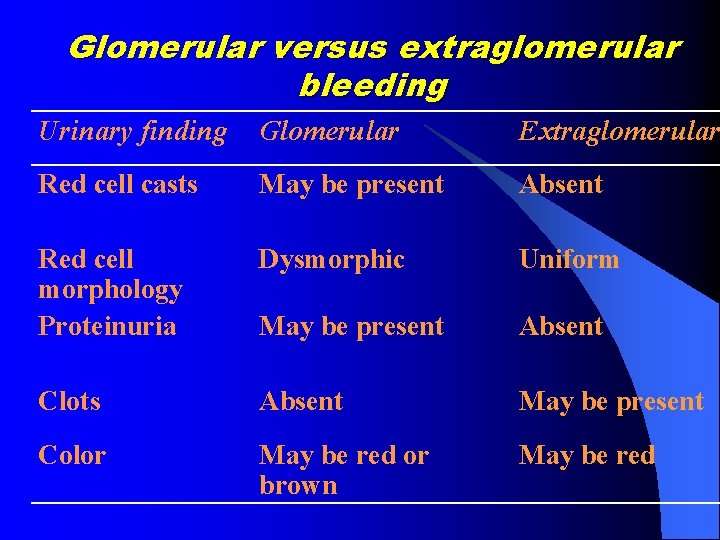
Glomerular versus extraglomerular bleeding Urinary finding Glomerular Extraglomerular Red cell casts May be present Absent Red cell morphology Proteinuria Dysmorphic Uniform May be present Absent Clots Absent May be present Color May be red or brown May be red




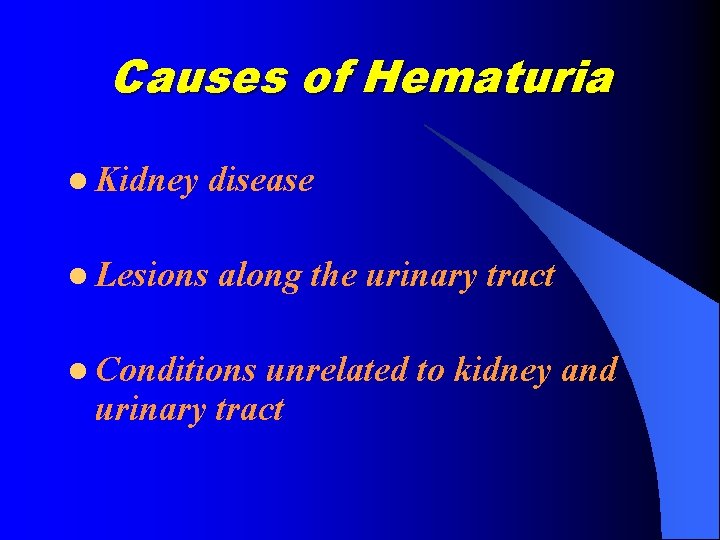
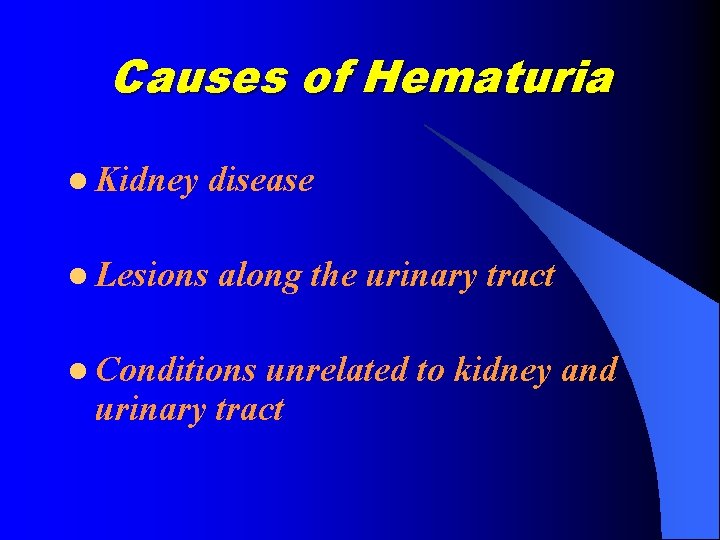
Causes of Hematuria l Kidney disease l Lesions along the urinary tract l Conditions unrelated to kidney and urinary tract
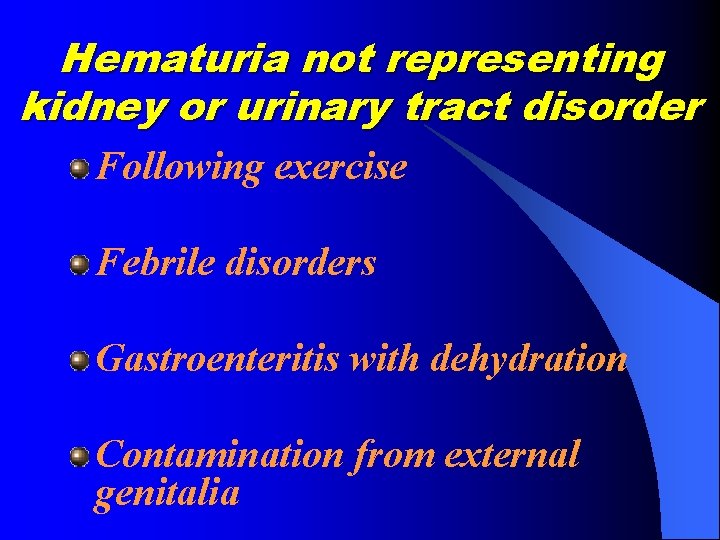
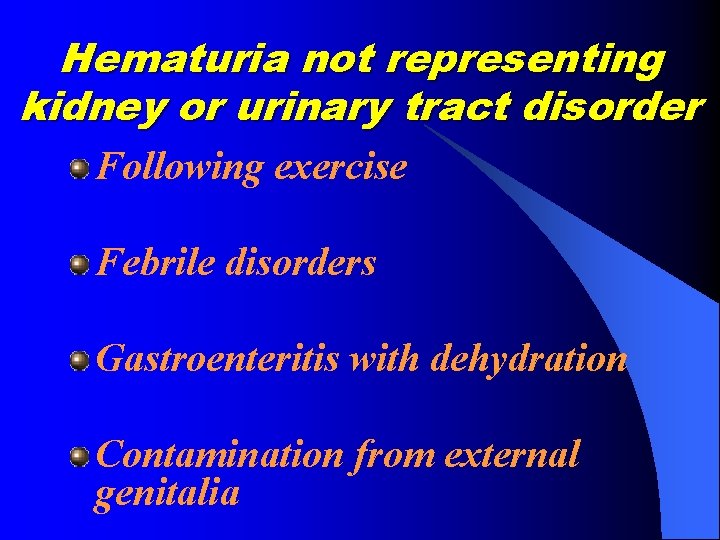
Hematuria not representing kidney or urinary tract disorder Following exercise Febrile disorders Gastroenteritis with dehydration Contamination from external genitalia


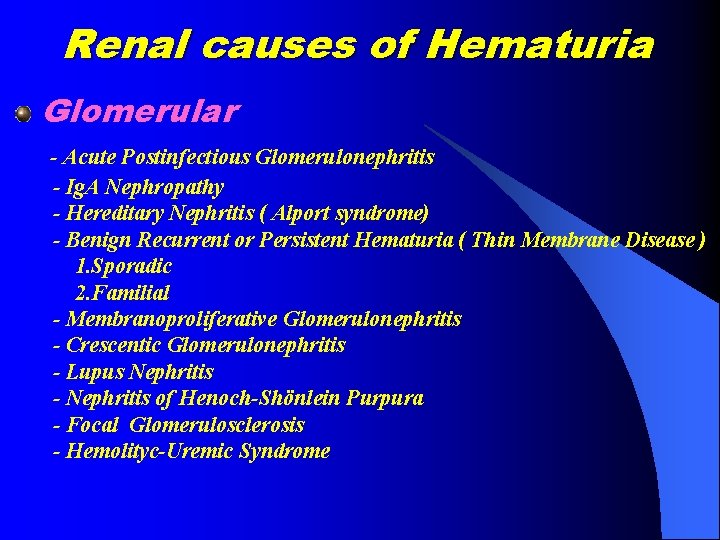
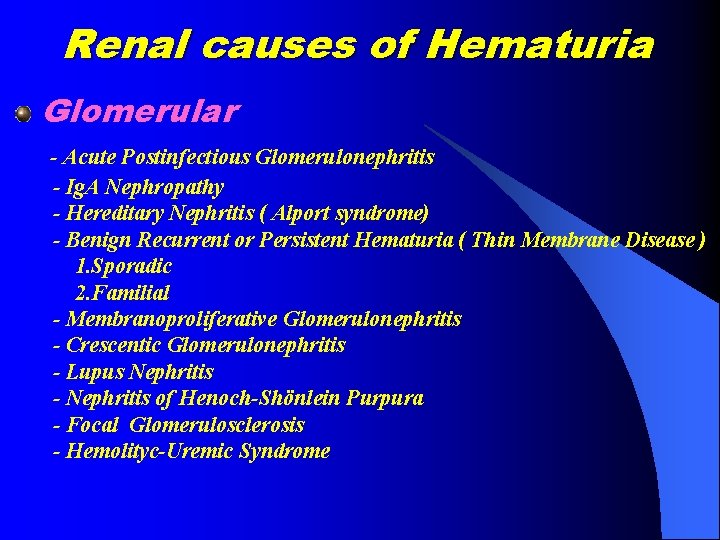
Renal causes of Hematuria Glomerular - Acute Postinfectious Glomerulonephritis - Ig. A Nephropathy - Hereditary Nephritis ( Alport syndrome) - Benign Recurrent or Persistent Hematuria ( Thin Membrane Disease ) 1. Sporadic 2. Familial - Membranoproliferative Glomerulonephritis - Crescentic Glomerulonephritis - Lupus Nephritis - Nephritis of Henoch-Shönlein Purpura - Focal Glomerulosclerosis - Hemolityc-Uremic Syndrome
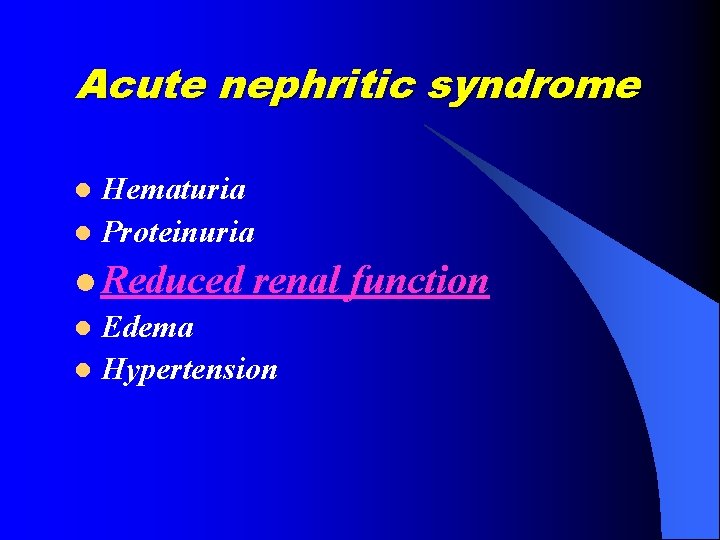
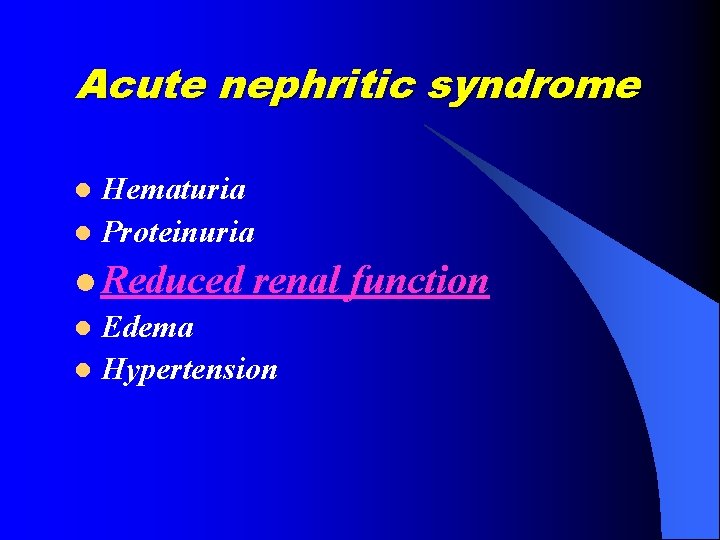
Acute nephritic syndrome Hematuria l Proteinuria l l Reduced renal l Edema l Hypertension function
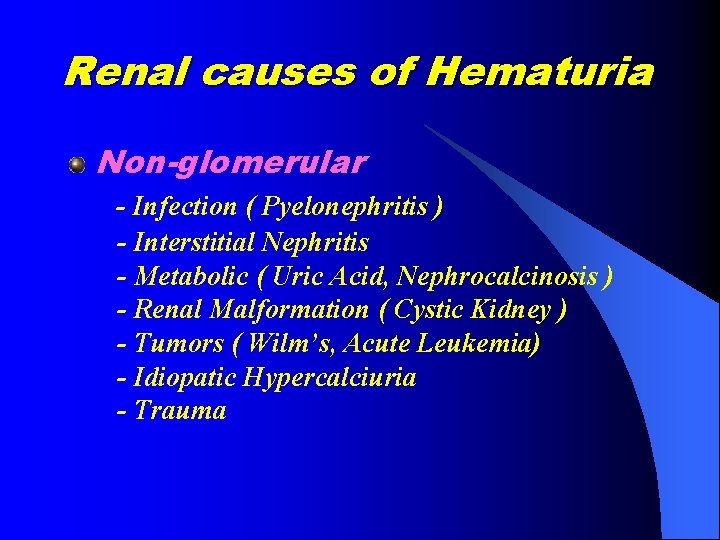
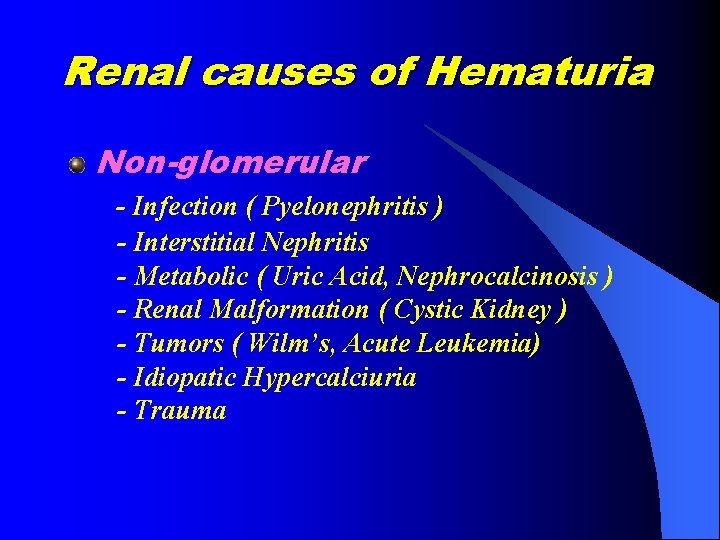
Renal causes of Hematuria Non-glomerular - Infection ( Pyelonephritis ) - Interstitial Nephritis - Metabolic ( Uric Acid, Nephrocalcinosis ) - Renal Malformation ( Cystic Kidney ) - Tumors ( Wilm’s, Acute Leukemia) - Idiopatic Hypercalciuria - Trauma
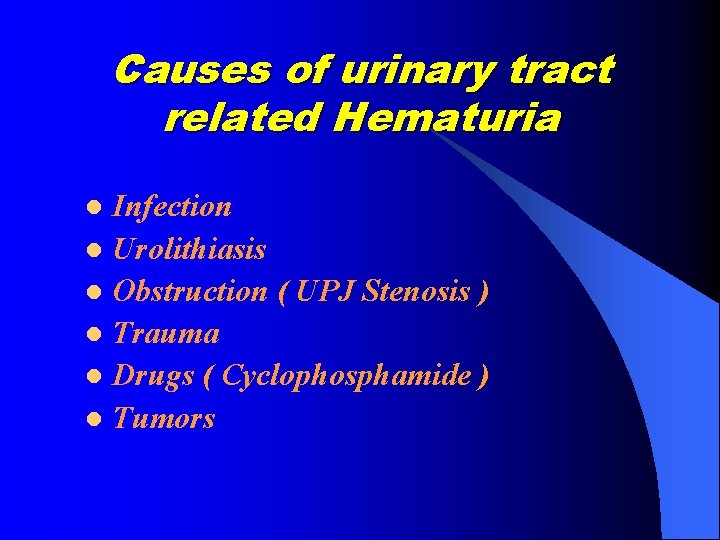
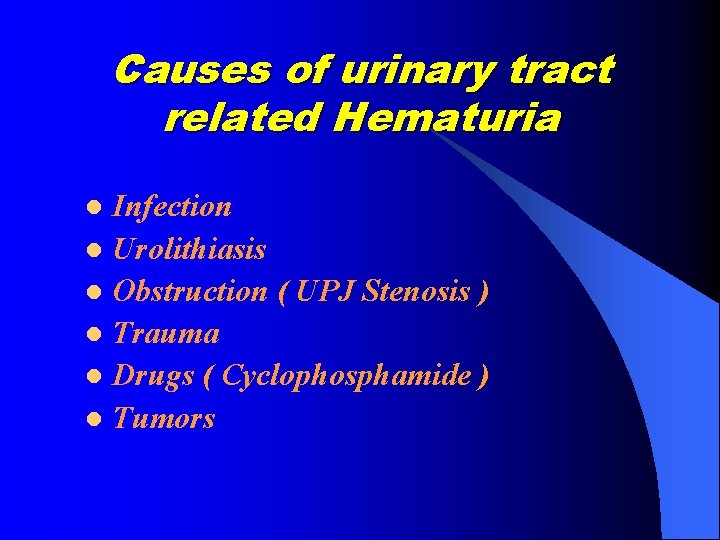
Causes of urinary tract related Hematuria Infection l Urolithiasis l Obstruction ( UPJ Stenosis ) l Trauma l Drugs ( Cyclophosphamide ) l Tumors l
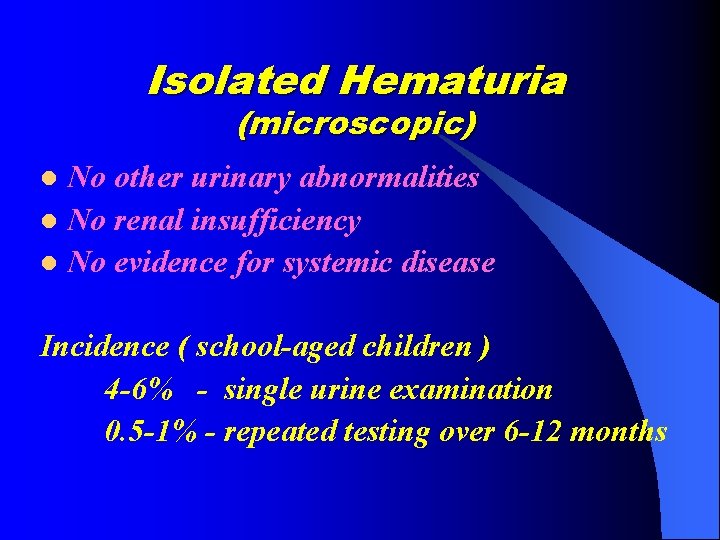
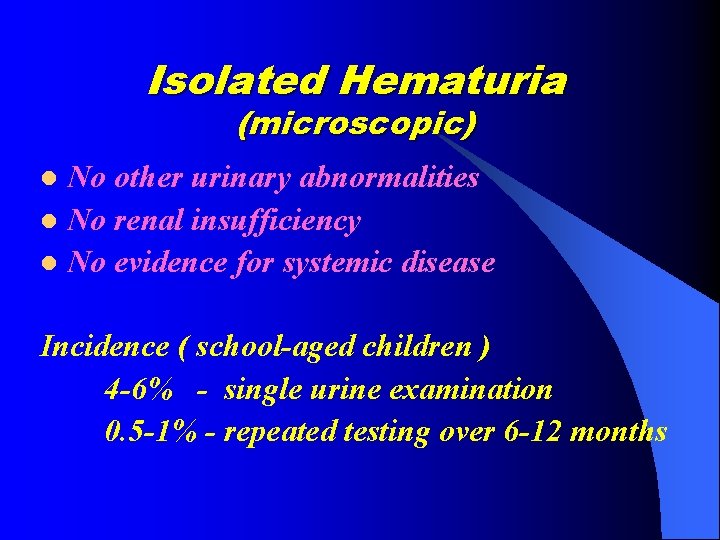
Isolated Hematuria (microscopic) No other urinary abnormalities l No renal insufficiency l No evidence for systemic disease l Incidence ( school-aged children ) 4 -6% - single urine examination 0. 5 -1% - repeated testing over 6 -12 months
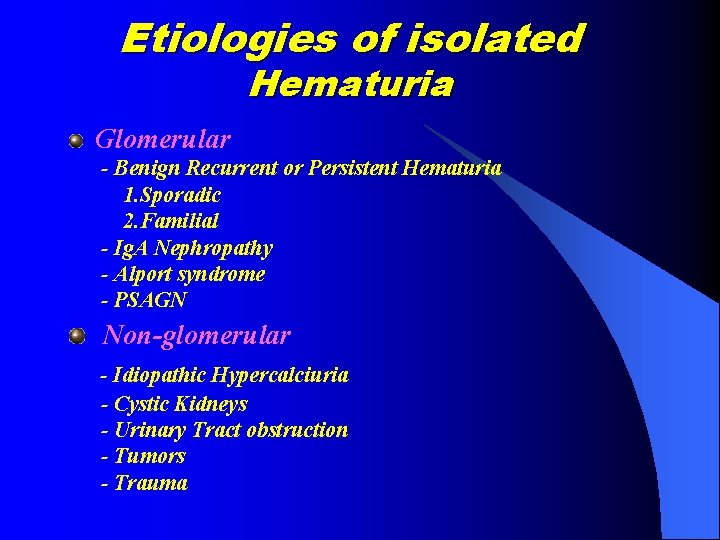
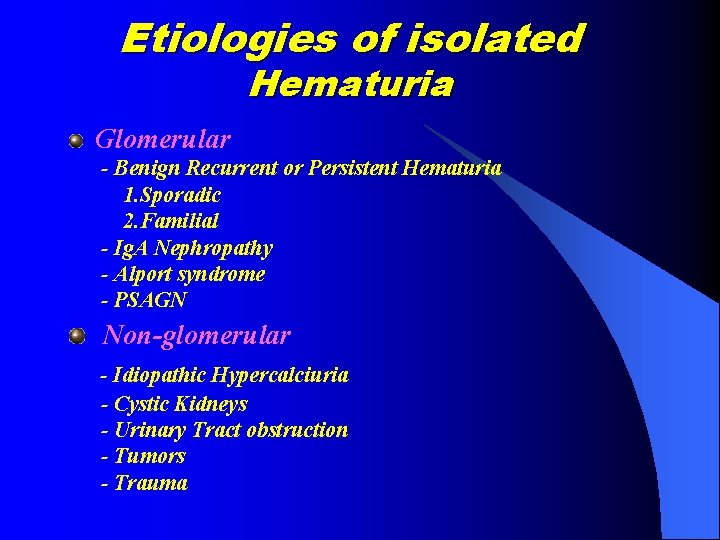
Etiologies of isolated Hematuria Glomerular - Benign Recurrent or Persistent Hematuria 1. Sporadic 2. Familial - Ig. A Nephropathy - Alport syndrome - PSAGN Non-glomerular - Idiopathic Hypercalciuria - Cystic Kidneys - Urinary Tract obstruction - Tumors - Trauma
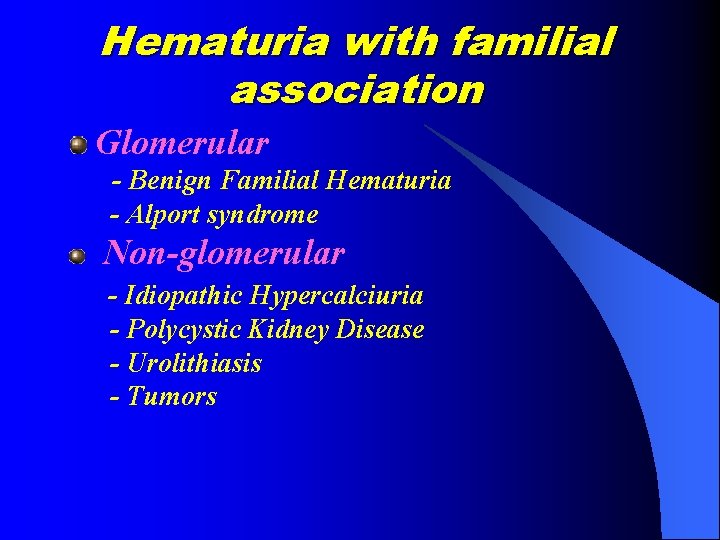
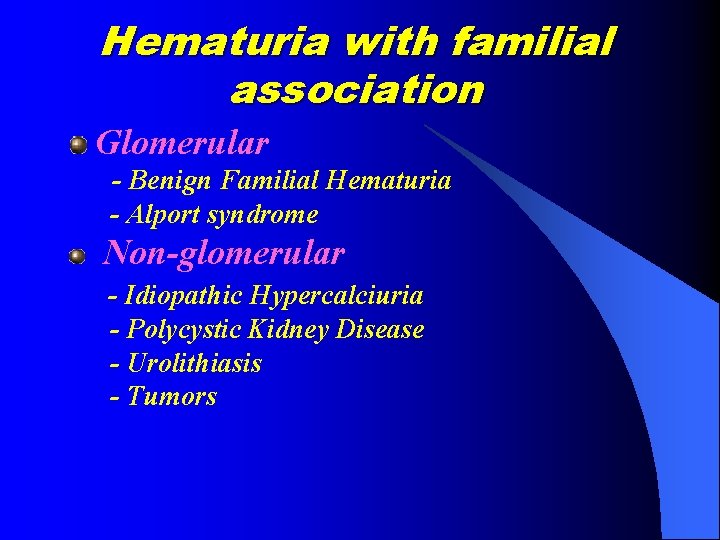
Hematuria with familial association Glomerular - Benign Familial Hematuria - Alport syndrome Non-glomerular - Idiopathic Hypercalciuria - Polycystic Kidney Disease - Urolithiasis - Tumors
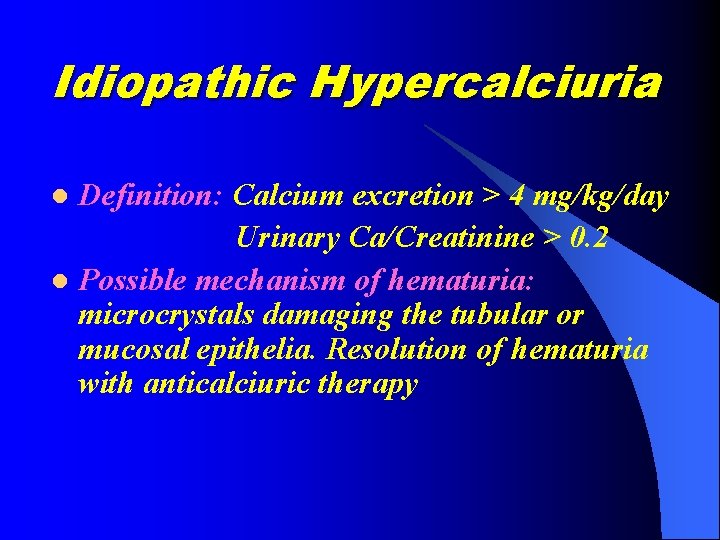
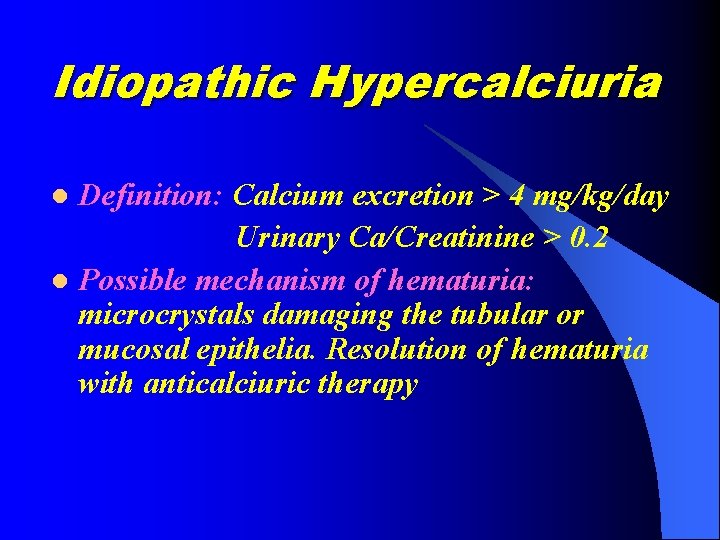
Idiopathic Hypercalciuria Definition: Calcium excretion > 4 mg/kg/day Urinary Ca/Creatinine > 0. 2 l Possible mechanism of hematuria: microcrystals damaging the tubular or mucosal epithelia. Resolution of hematuria with anticalciuric therapy l
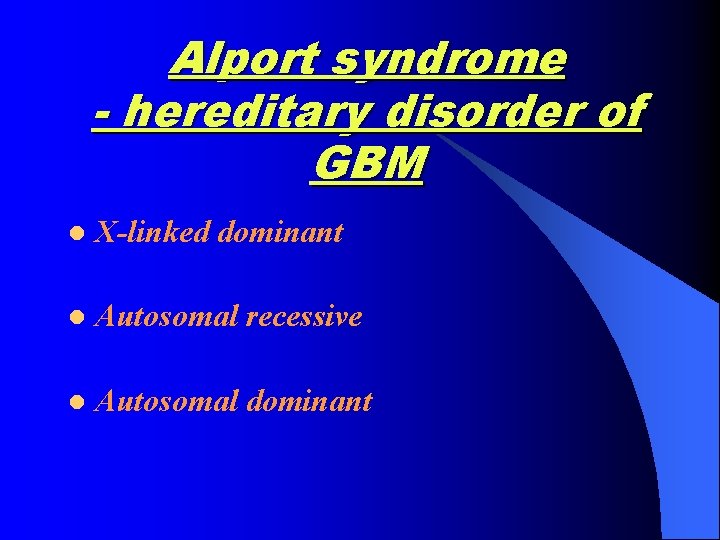
Alport syndrome - hereditary disorder of GBM l X-linked dominant l Autosomal recessive l Autosomal dominant
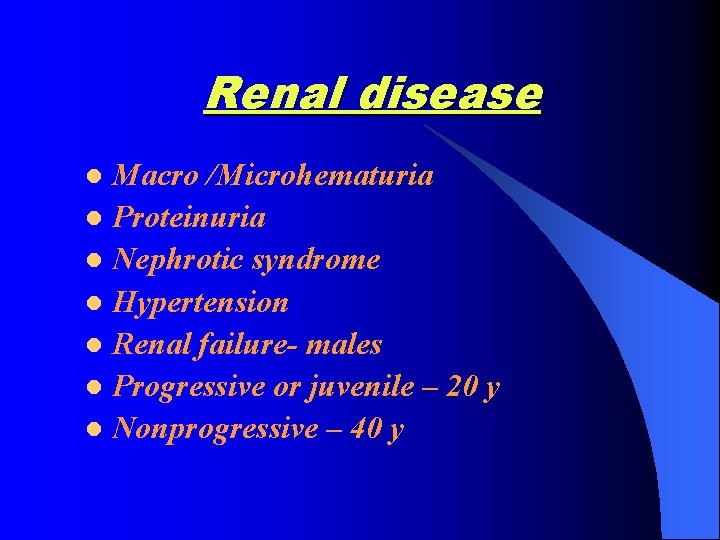
Renal disease Macro /Microhematuria l Proteinuria l Nephrotic syndrome l Hypertension l Renal failure- males l Progressive or juvenile – 20 y l Nonprogressive – 40 y l
Hearing defects Sensorineural bilateral Never congenital Boys- 85%. Girls – 18% < 15 y Progression of hearing loss parallels renal impairment
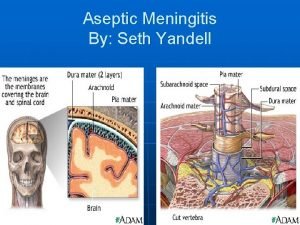
Diagnosis of Alport syndrome Hematuria with or without proteinuria l Hypertension l Renal failure l Ocular defects – anterior lenticonus l Familial hematuria l Sensorineural hearing loss l Progression to renal failure occurring in at least one affected subject l

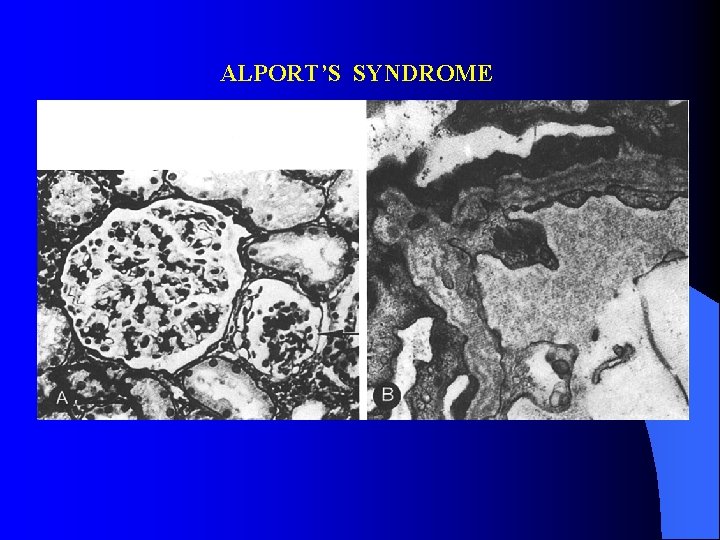
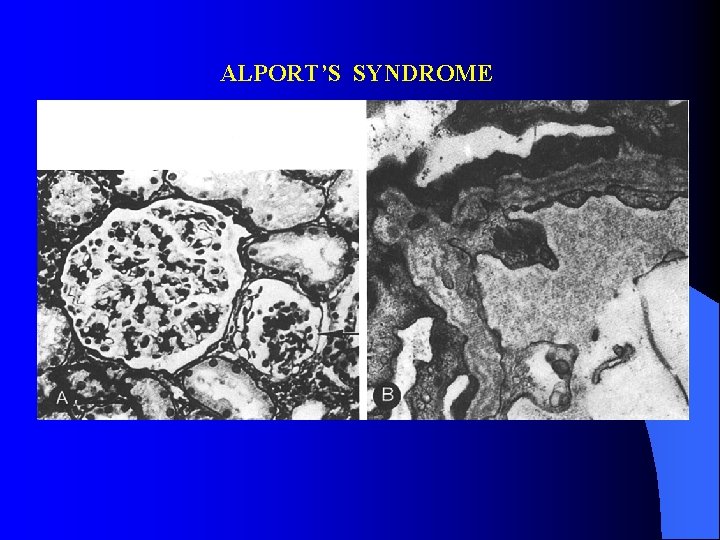
ALPORT’S SYNDROME
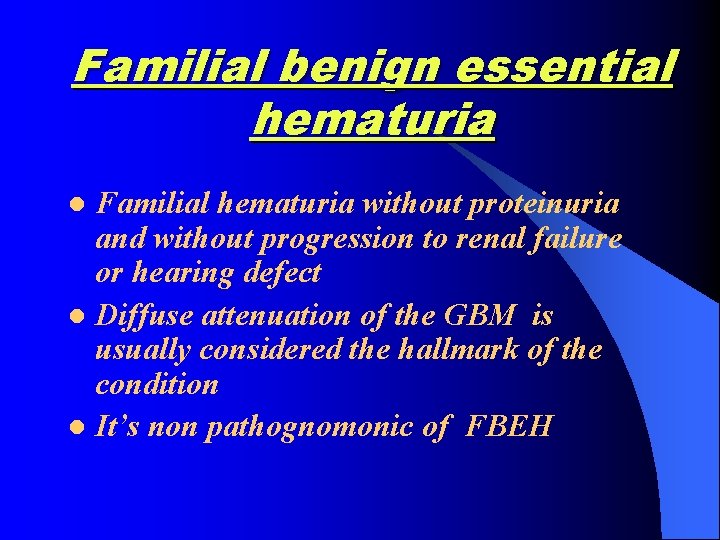
Familial benign essential hematuria Familial hematuria without proteinuria and without progression to renal failure or hearing defect l Diffuse attenuation of the GBM is usually considered the hallmark of the condition l It’s non pathognomonic of FBEH l
Continue l Autosomal dominant trait l Normal antigenicity of the GBM

Thin basement membrane nephropathy Hematuria l Proteinuria l Attenuation of the GBM l In children may be Alport l In adults m/p benign disorder l

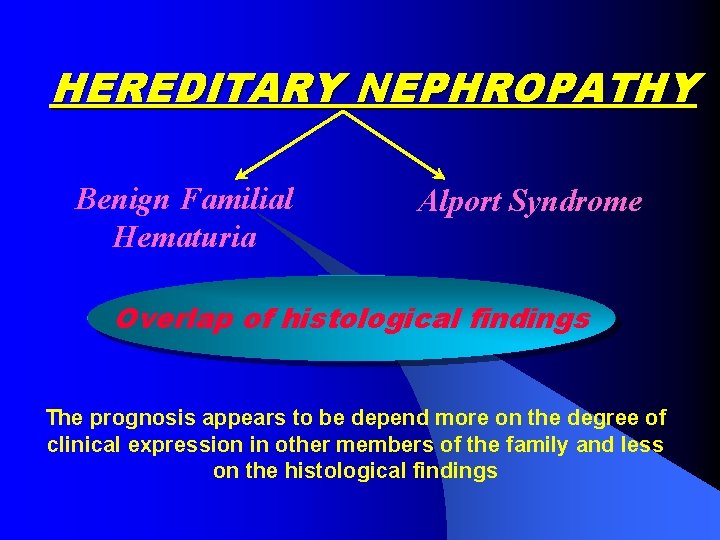
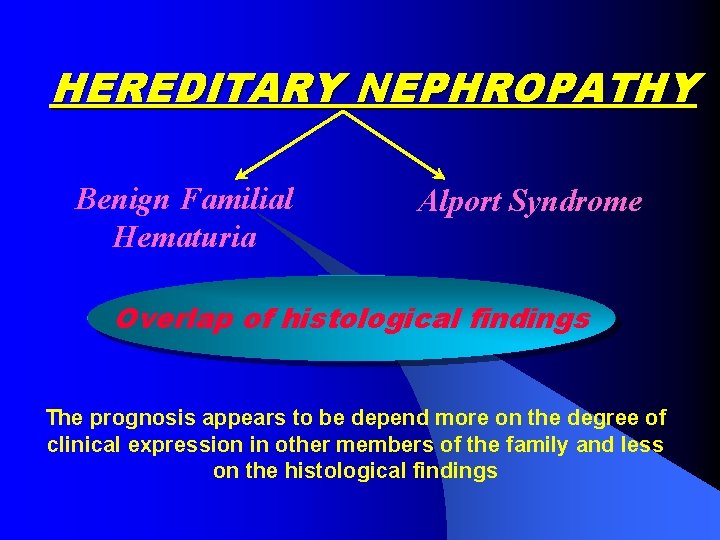
HEREDITARY NEPHROPATHY Benign Familial Hematuria Alport Syndrome Overlap of histological findings The prognosis appears to be depend more on the degree of clinical expression in other members of the family and less on the histological findings
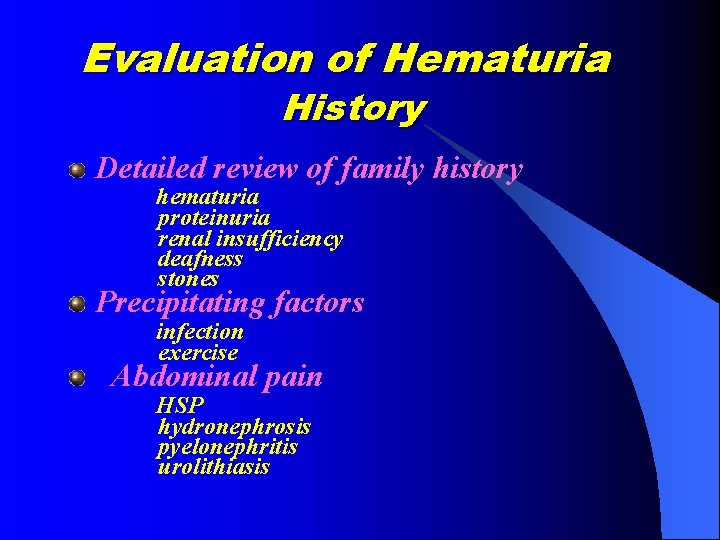
Evaluation of Hematuria History Detailed review of family history hematuria proteinuria renal insufficiency deafness stones Precipitating factors infection exercise Abdominal pain HSP hydronephrosis pyelonephritis urolithiasis
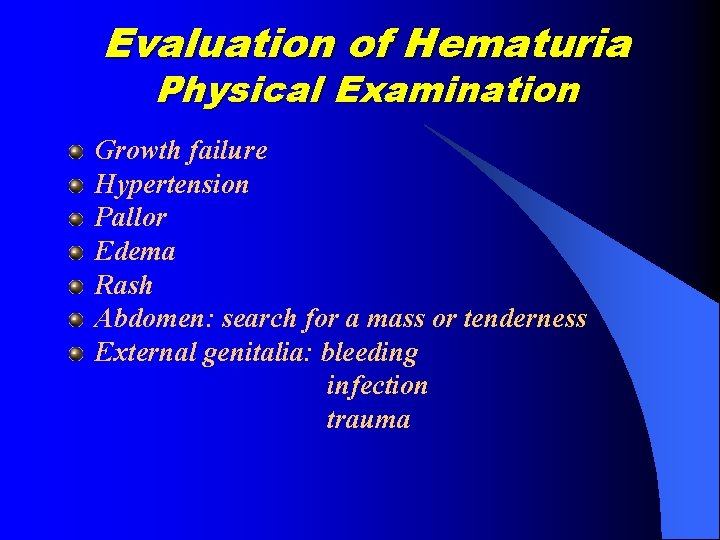
Evaluation of Hematuria Physical Examination Growth failure Hypertension Pallor Edema Rash Abdomen: search for a mass or tenderness External genitalia: bleeding infection trauma
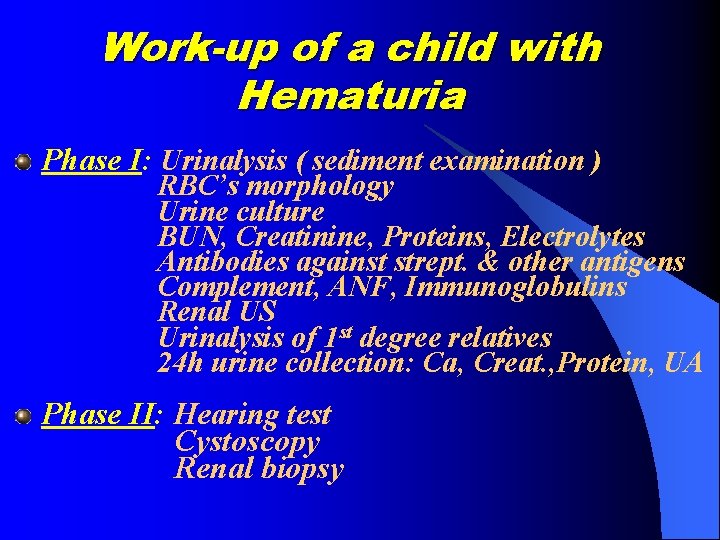
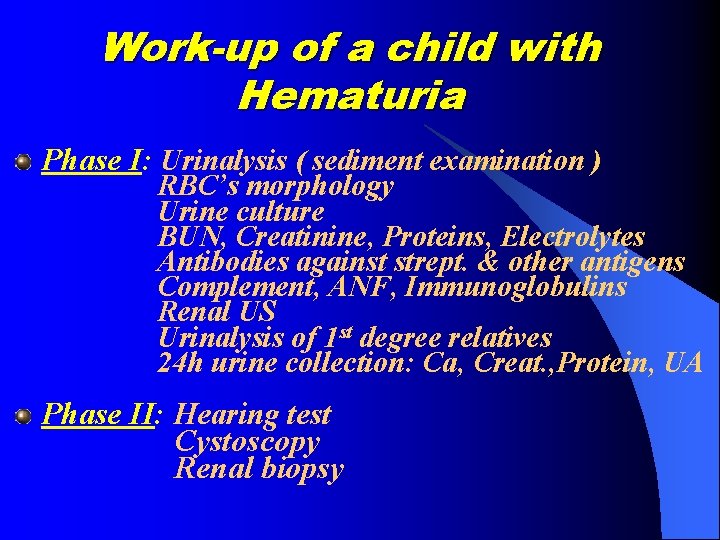
Work-up of a child with Hematuria Phase I: Urinalysis ( sediment examination ) RBC’s morphology Urine culture BUN, Creatinine, Proteins, Electrolytes Antibodies against strept. & other antigens Complement, ANF, Immunoglobulins Renal US Urinalysis of 1 st degree relatives 24 h urine collection: Ca, Creat. , Protein, UA Phase II: Hearing test Cystoscopy Renal biopsy
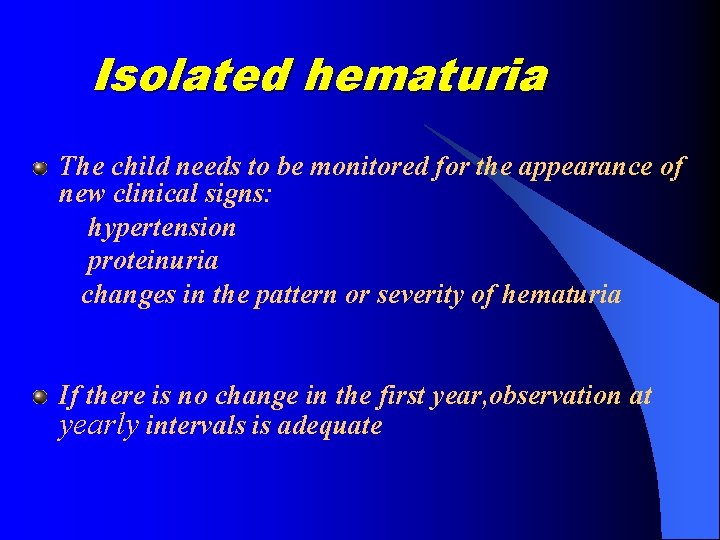
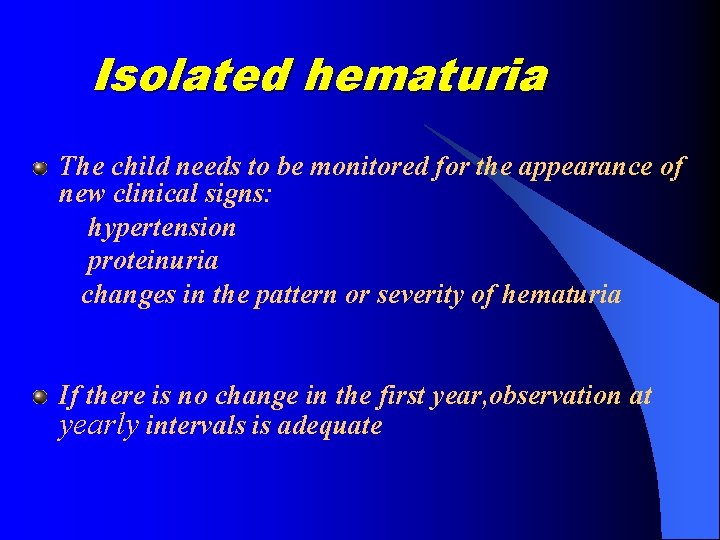
Isolated hematuria The child needs to be monitored for the appearance of new clinical signs: hypertension proteinuria changes in the pattern or severity of hematuria If there is no change in the first year, observation at yearly intervals is adequate
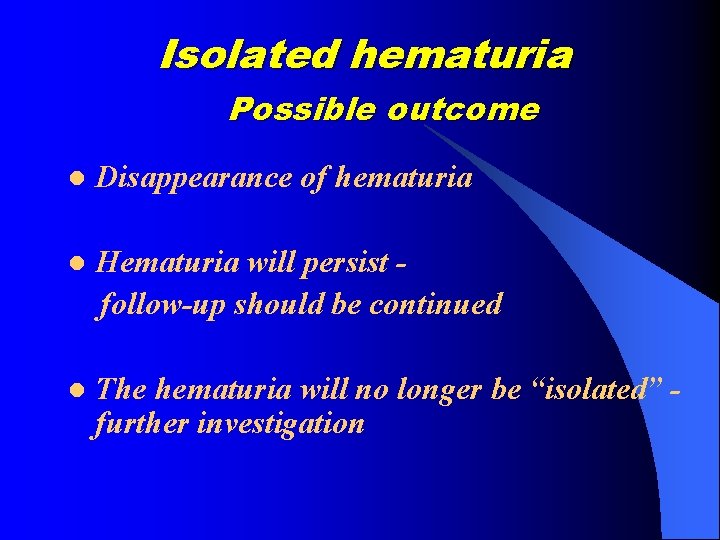
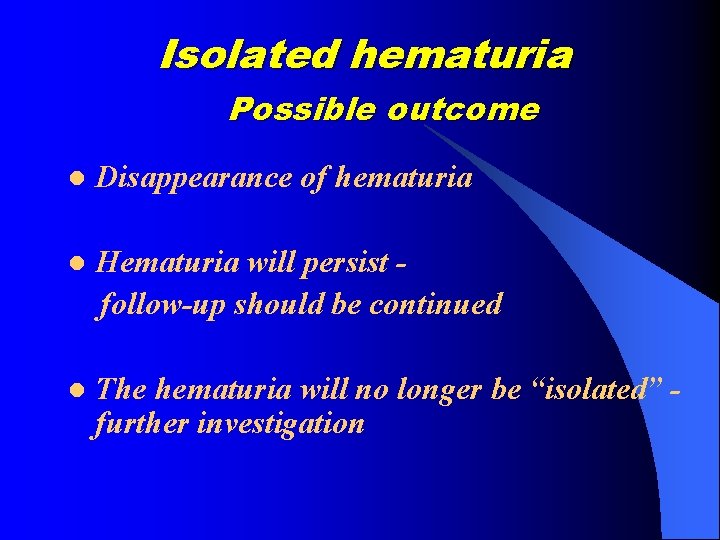
Isolated hematuria Possible outcome l Disappearance of hematuria l Hematuria will persist follow-up should be continued l The hematuria will no longer be “isolated” further investigation
Hematuria Transient phenomenon of little significance Sign of serious renal disease
 All traffic signs and meanings
All traffic signs and meanings Cristales de fosfato triple
Cristales de fosfato triple Macroscopic hematuria causes
Macroscopic hematuria causes Hematuria
Hematuria Hematuria ex vacuo
Hematuria ex vacuo Dr shezad tejani
Dr shezad tejani Hematuria causes
Hematuria causes Hematuria
Hematuria Eritrocitos isomorficos
Eritrocitos isomorficos Anuria disuria poliuria oliguria hematuria
Anuria disuria poliuria oliguria hematuria 10 mgd
10 mgd Hematuria
Hematuria 1 little 2 little 3 little indian
1 little 2 little 3 little indian Ten little indian boys poem
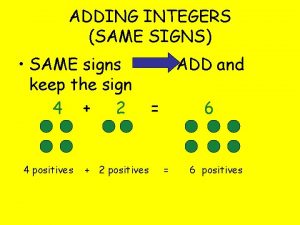
Ten little indian boys poem Adding integers with same sign
Adding integers with same sign Chvostek sign
Chvostek sign Trousseau sign hypocalcemia
Trousseau sign hypocalcemia Hypermagnesemia causes
Hypermagnesemia causes Kernig's sign
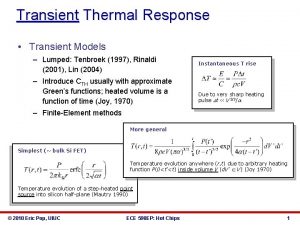
Kernig's sign Dc transient analysis
Dc transient analysis Alimam
Alimam Transient and steady state response analysis
Transient and steady state response analysis Transient line source technique
Transient line source technique Transient analysis thermodynamics
Transient analysis thermodynamics Whats testimonial evidence
Whats testimonial evidence Wound care study days
Wound care study days Surface mount transient voltage suppressor
Surface mount transient voltage suppressor @transient in jpa
@transient in jpa Radial heat conduction
Radial heat conduction Transient evidence examples
Transient evidence examples Transient hypofrontality
Transient hypofrontality Conditional evidence example
Conditional evidence example Transient equilibrium equation
Transient equilibrium equation The developing person through childhood and adolescence
The developing person through childhood and adolescence Transient evidence examples
Transient evidence examples Forensic entomology does not include _____.
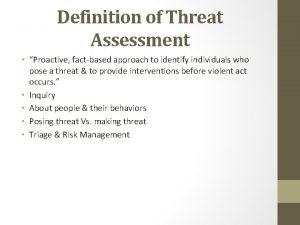
Forensic entomology does not include _____. Transient threat definition
Transient threat definition Transient solution differential equations
Transient solution differential equations Transient response in vlsi
Transient response in vlsi Dynamic response
Dynamic response Transient signal oscilloscope
Transient signal oscilloscope Ripple transient
Ripple transient Kutta
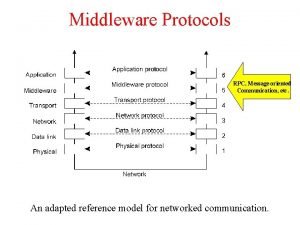
Kutta Message oriented communication
Message oriented communication Transient conduction means
Transient conduction means