HAEMORRHOIDS Anatomy of Anal Canal Transverse Section Pathogenesis









- Slides: 36
HAEMORRHOIDS
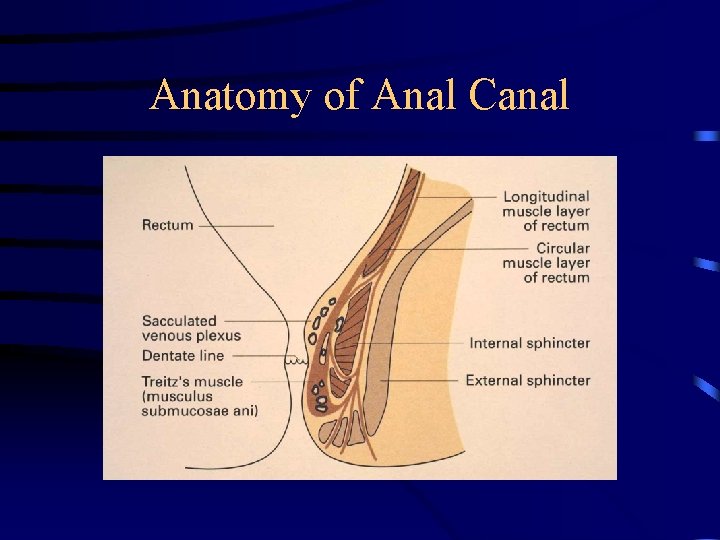
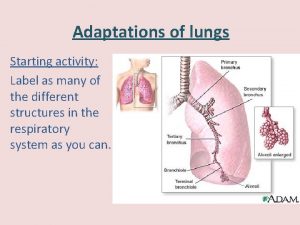
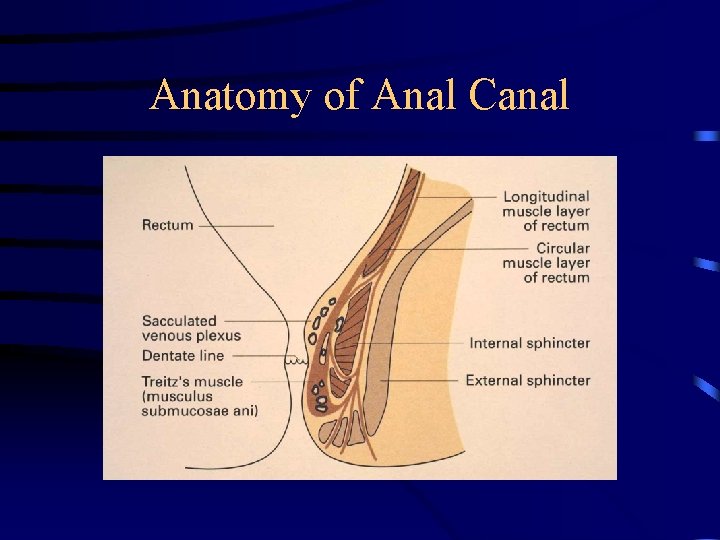
Anatomy of Anal Canal
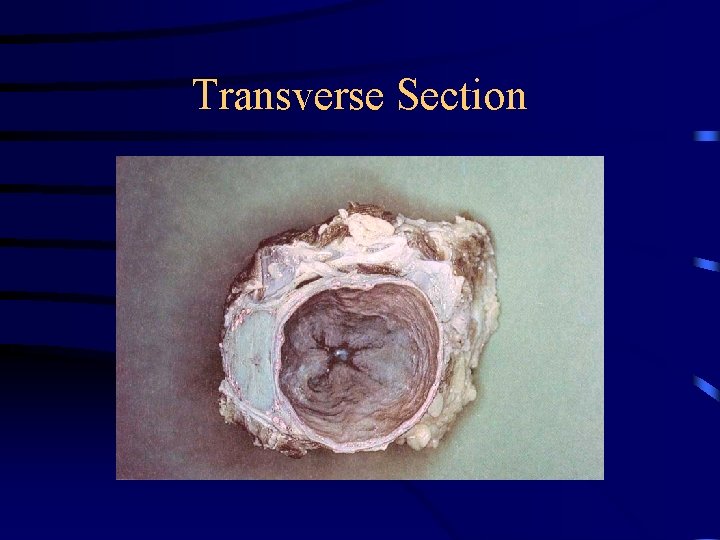
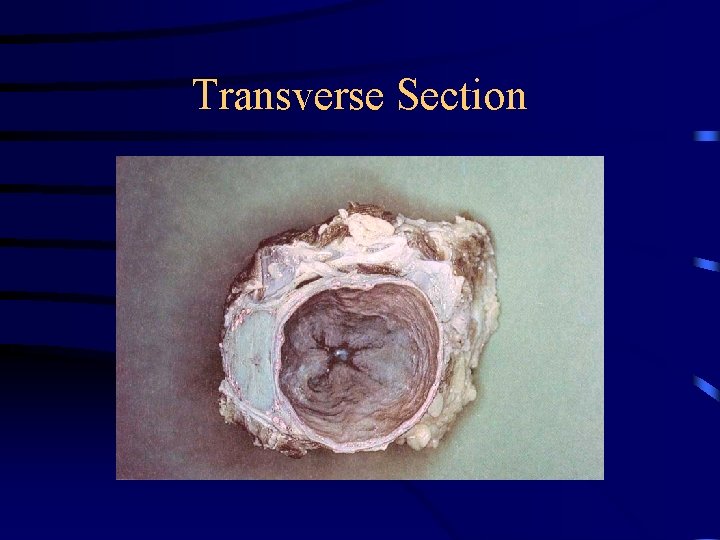
Transverse Section
Pathogenesis • Precise aetiology is unknown • Internal disruption and downward displacement of anal cushions by forces of defecation • Histological changes – Enlarged vascular spaces – Aggregation of connective tissue – Smooth muscle hypertrophy

Classification • First Degree - No Prolapse • Second Degree - Prolapse, spontaneously reduce • Third Degree - Prolapse, manually reducible • Fourth Degree - Irreducible
Presentation • Bleeding • Prolapse • • Pain Itching Anorectal Dysfunction Soiling


Management of Haemorrhoids Necessity for treatment is mostly determined by symptom severity Choice of treatment modality may be directed by grade of haemorrhoidal cushions
Conservative Management • Dietary manipulation to avoid hard stools • Increase fibre and fluid in diet • Stool-softeners • Advice re defecation habits • • Avoid excess straining at defecation Do not defer bowel motions Desist from reading in toilet Maintain good local hygiene • Topical Agents
Interventional Management for Low Grade Haemorrhoids • Principles – Reduction of bulk of anal cushions – Disruption of vascular supply leading to adhesion and scarring of remnants – Simple procedures – involving tissue above the dentate line (no anaesthesia) – Outpatient procedures

Interventional Management for Low Grade Haemorrhoids • Rubber band ligation • Sclerotherapy • Infra-red photo-coagulation / bipolar diathermy • Cryotherapy • Laser treatment
Rubber Band Ligation • • Simple Inexpensive Office-based procedure Low complication rate (<2%) Cure rate 60 -70% (single treatment) Patient satisfaction 80 -90% Recommended first-line treatment for first to third degree haemorrhoids • Most effective ambulant measure available
Rubber Band Ligation • More painful than other outpatient modalities, but similar complication rates • Complications – – Bleeding Vaso-vagal Thrombosis in adjacent external haemorrhoid (1 -11%) Pelvic Sepsis (1/10000)
Mac. Rae H. M. , Mc. Leod R. S. Comparison of hemorroidal treatments: a meta-analysis. Dis Colon Rectum 1995 • A meta-analysis of all RCT’s assessing two or more treatment modalities for symptomatic hemorrhoids • 18 trials included, n=1952 • Outcome measures : response to therapy, need for furtherapy, complications and pain • Grade 4 haemorrhoids not evaluated in any of the studies
Mac. Rae H. M. , Mc. Leod R. S. Comparison of hemorroidal treatments: a meta-analysis. Dis Colon Rectum 1995 Summary of Results • Haemorrhoidectomy more effective than manual anal dilatation, with less need for furtherapy and no increased risk of complications but more pain post-op • Haemorrhoidectomy more effective than rubber band ligation (RBL), but greater risk of complications and pain • RBL more effective than sclerotherapy, with no significant difference in complication rate • RBL less likely to require furtherapy than sclerotherapy or infra-red photo-coagulation (IRC), but higher incidence of post-op pain • No difference found between sclerotherapy and IRC, for any of outcome measures
Operative Management Better chance of long-term cure Greater post-operative pain Longer recovery time
Haemorrhoidectomy • Indications – Large cutaneous/external componant – Ulceration – Gangrene – Extensive thrombosis – Failure of non-operative treatment
Haemorroidectomy • Can be done under LA & sedation • Rarely >overnight stay, possible day case • Techniques: – Open (Milligan-Morgan technique 1937) – Closed (Ferguson 1952) – Stapled (Peck, modified Longo 1998)
Open Haemorrhoidectomy • Involves dissection of venous saccules off internal sphincter, excision of mucosal, anodermal and cutaneous parts of haemorrhoid, ligation of vascular pedicle • May require extensive electro-cautery to achieve haemostasis • Wounds heal by secondary intention ( 10 days) • Excise symptomatic haemorrhoidal cushions • Must leave skin bridges • LA infiltration, light dressing • Post-op - stool-softeners, warm baths, analgesia, (Antibiotic cover not required)
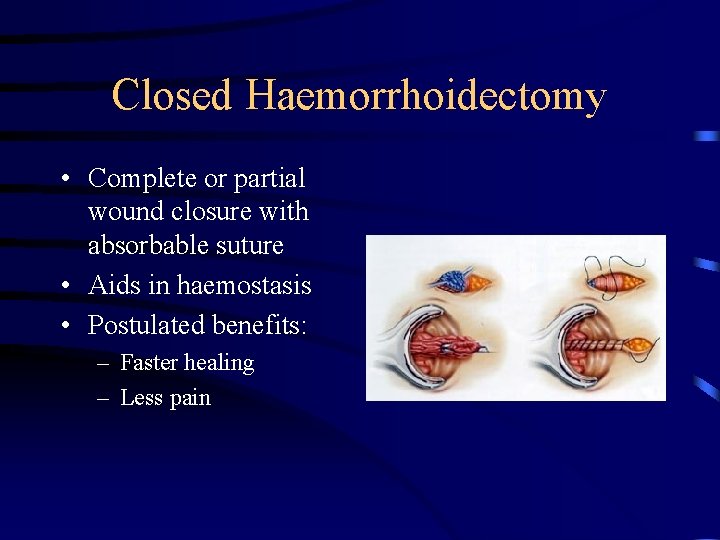
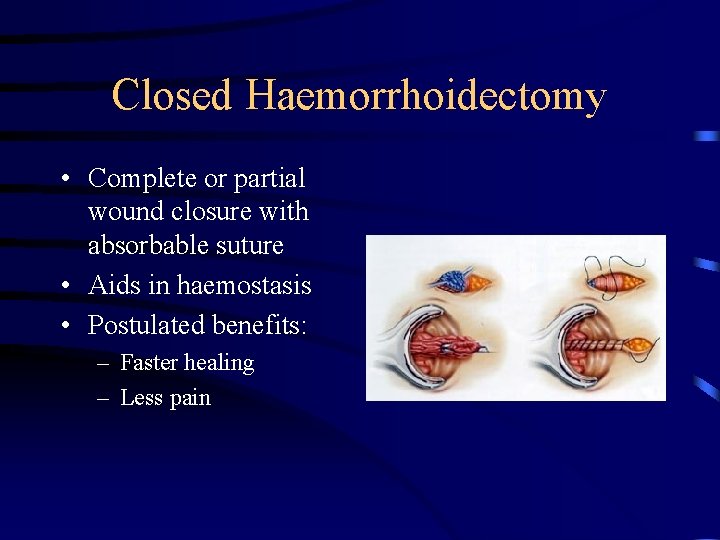
Closed Haemorrhoidectomy • Complete or partial wound closure with absorbable suture • Aids in haemostasis • Postulated benefits: – Faster healing – Less pain

Complications • • Pain Bleeding – primary and secondary Urinary retention Impaired continence Anal stenosis Residual skin tags Infection
Stapled Haemorrhoidectomy • Circular stapling device excises annulus of rectal mucosa above the pathological rectal mucosa (haemorrhoid) • Interruption of blood supply leads to reduction in size of vascular cushions • Reduction of available rectal mucosa for potential prolapse




A Systematic Review of Stapled Hemorrhoidectomy, Sutherland et al. Archives of Surgery, Dec 2002 • Summary of data obtained for ASERNIP-S • RCT’s, full peer reviewed, comparing stapled to conventional haemorrhoidectomy • 7 studies met inclusion criteria • Objective to assess: – Safety - complications, inc. bleeding, thrombosis, urinary retention, anal stenosis, sphincter damage – Efficacy - post-op pain, analgesia requirements, discharge, healing time, prolapse, skin tags, readmission rate, anal resting & squeeze volumes
Results • reasonably clear evidence for decreased incidence of bleeding at 2 weeks and length of hospital stay. • Favourable trends related to – – – – – pain bleeding anal discharge wound healing tenderness to per rectal examination incontinence scores earlier return of bowel function analgesic requirement resumption of normal activities
Issues Raised • one trial showed prolapse occurred at significantly higher rates in the stapled hemorrhoidectomy group, up to 19 months after surgery ? treatment failure. Case reports of major complications Rectal perforation Pelvic sepsis Recto-vaginal fistula Instrument failure Cost?
Limitations • small sample size • short follow-up times • significant lack of comparability - wide variation in patient characteristics, stapling equipment used, surgical protocol, postoperative care regimen and assessment, and methods of outcome measures
Conclusions Safety - at least as safe as conventional hemorrhoidal surgery techniques Efficacy - could not be determined Further studies needed
Post-operative Pain • Local anaesthesia - bupivocaine, ropivacaine • Caudal/lumbar extradural injections bupivocaine, morphine +/- lignocaine • low-dose narcotic spinal • transdermal fentanyl • corticosteroid injection • ischio-rectal fossa block
• Topical nitroglycerin – trend towards reduced analgesic use – significant morbidity • oral metronidazole post-op • internal sphincterotomy / anal stretch – no reduction in pain – risk of incontinence • Transcutaneous electrical nerve stimulation • local injection of ketorolac • subcutaneous morphine pump
Outpatient Haemorrhoidectomy • Commonly practiced in USA and Europe • many published series showing – around 80% success – good patient tolerance and acceptance – no significant increase in complications or recurrence – economic benefit – mainly limited by post-op pain
 Eco endoanal
Eco endoanal Anus diagram
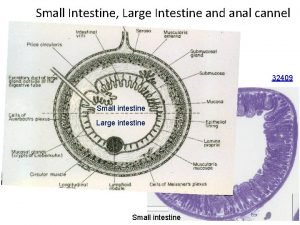
Anus diagram Lymphoid nodule colon
Lymphoid nodule colon Anal canal
Anal canal Perineum
Perineum Aparato digestivo embriologia
Aparato digestivo embriologia Lymphoid nodule colon
Lymphoid nodule colon Ligament of stomach
Ligament of stomach Equivalencia pulgadas mm tuberías polietileno
Equivalencia pulgadas mm tuberías polietileno Coronal axial sagittal
Coronal axial sagittal Standing position meaning
Standing position meaning Pathogenesis of pleomorphic adenoma
Pathogenesis of pleomorphic adenoma Uremia pathogenesis
Uremia pathogenesis Cholecystitis pathophysiology
Cholecystitis pathophysiology Acute cholecystitis clinical features
Acute cholecystitis clinical features Bacterial pathogenesis
Bacterial pathogenesis Cholecystitis pathogenesis
Cholecystitis pathogenesis Bacterial pathogenesis
Bacterial pathogenesis Nursing management of neonatal tetanus
Nursing management of neonatal tetanus Jaundice pathogenesis
Jaundice pathogenesis Pathogenesis dengue fever
Pathogenesis dengue fever Rabies pathogenesis
Rabies pathogenesis Appressorium diagram
Appressorium diagram Pathogenesis game
Pathogenesis game Pathogenesis of copd
Pathogenesis of copd Primary biliary cholangitis skin
Primary biliary cholangitis skin Histoplasma capsulatum pathogenesis
Histoplasma capsulatum pathogenesis Nursing management of pyelonephritis
Nursing management of pyelonephritis Pathophysiology of anemia
Pathophysiology of anemia Mechanism of ischemic stroke
Mechanism of ischemic stroke Pathogenesis of tuberculosis
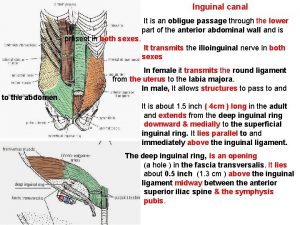
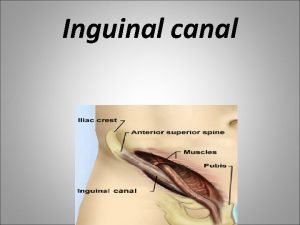
Pathogenesis of tuberculosis Inguinal canal anatomy diagram
Inguinal canal anatomy diagram Hesselbachs triangle
Hesselbachs triangle Goblet cell secretes
Goblet cell secretes Transverse incision c section
Transverse incision c section Orqa chiqaruv teshigi
Orqa chiqaruv teshigi Choque medular
Choque medular