Gastrostomy Caring for children in a community program
- Slides: 35
Gastrostomy Caring for children in a community program 2014 -02 -12
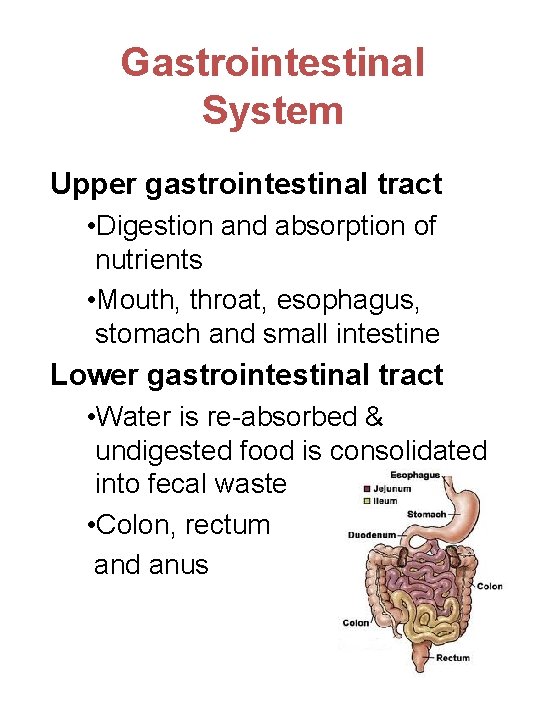
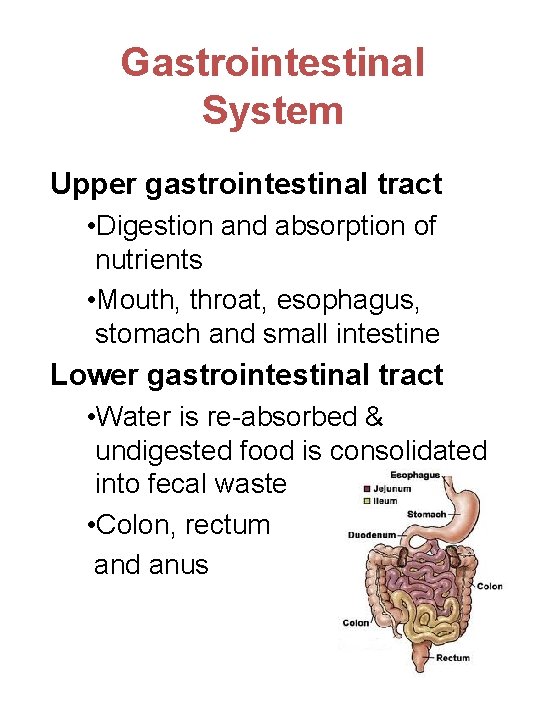
Gastrointestinal System Upper gastrointestinal tract • Digestion and absorption of nutrients • Mouth, throat, esophagus, stomach and small intestine Lower gastrointestinal tract • Water is re-absorbed & undigested food is consolidated into fecal waste • Colon, rectum and anus
Gastrostomy • Surgical opening (“stoma) into the stomach (“gastro") Gastrostomy tube • Small soft tube that goes into the body through the stoma and ends inside the stomach. • Rounded tips with holes on the end that is inside the stomach. • Ports on the end of the tube that is outside the body.
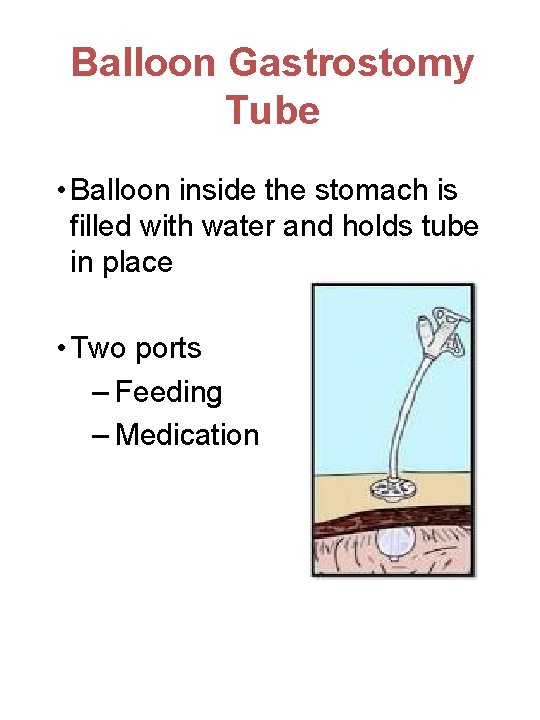
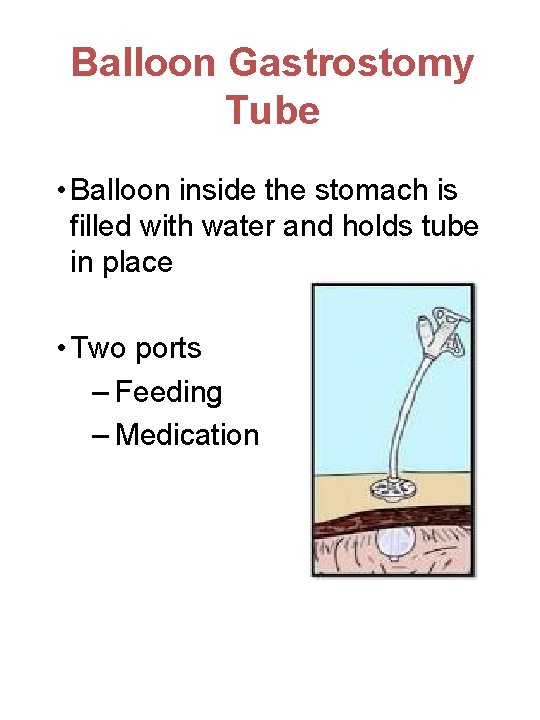
Balloon Gastrostomy Tube • Balloon inside the stomach is filled with water and holds tube in place • Two ports – Feeding – Medication
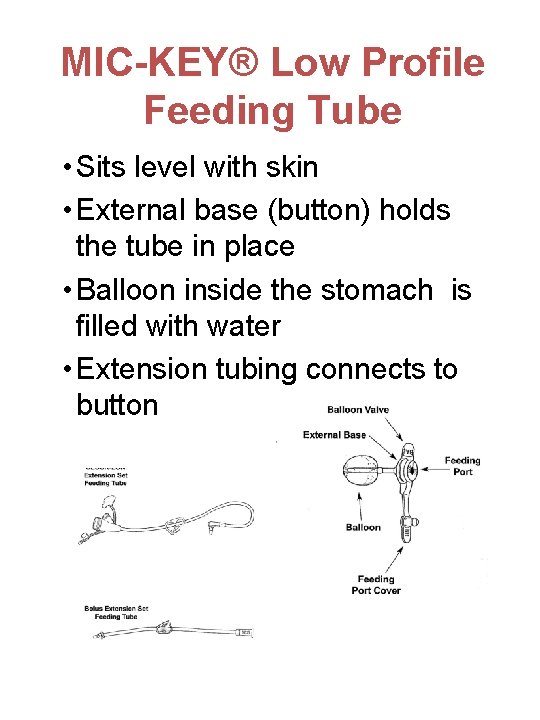
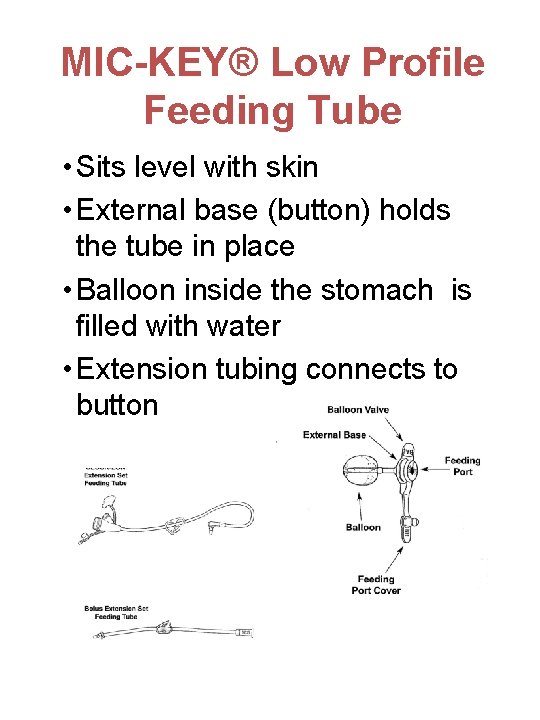
MIC-KEY® Low Profile Feeding Tube • Sits level with skin • External base (button) holds the tube in place • Balloon inside the stomach is filled with water • Extension tubing connects to button
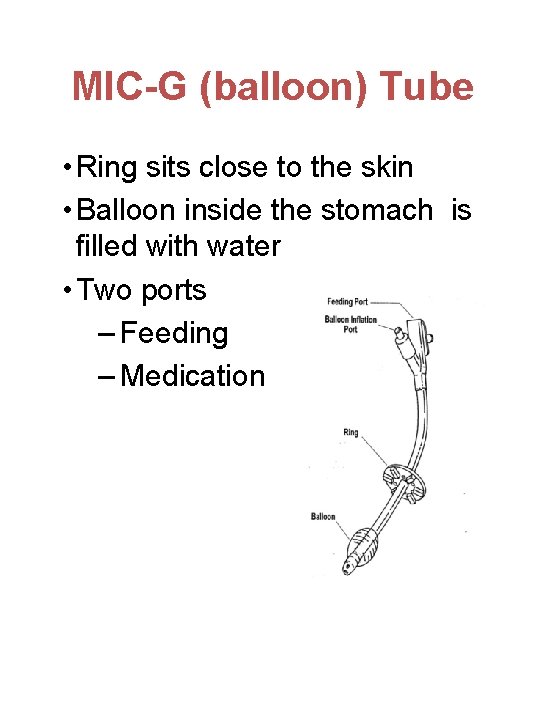
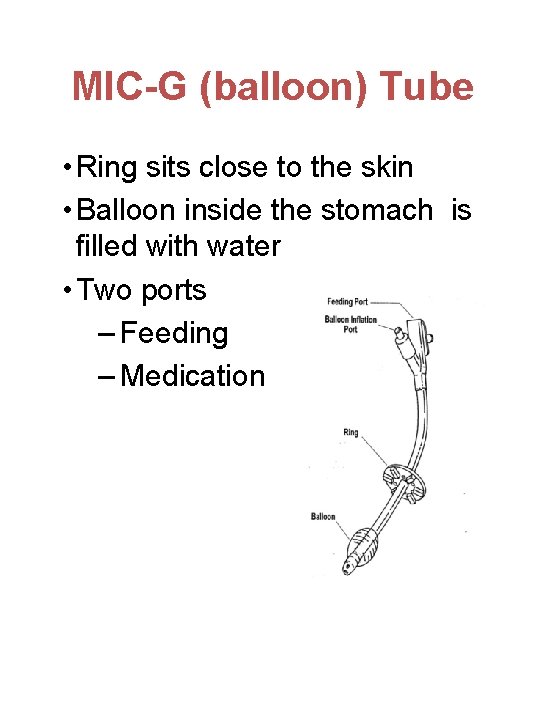
MIC-G (balloon) Tube • Ring sits close to the skin • Balloon inside the stomach is filled with water • Two ports – Feeding – Medication
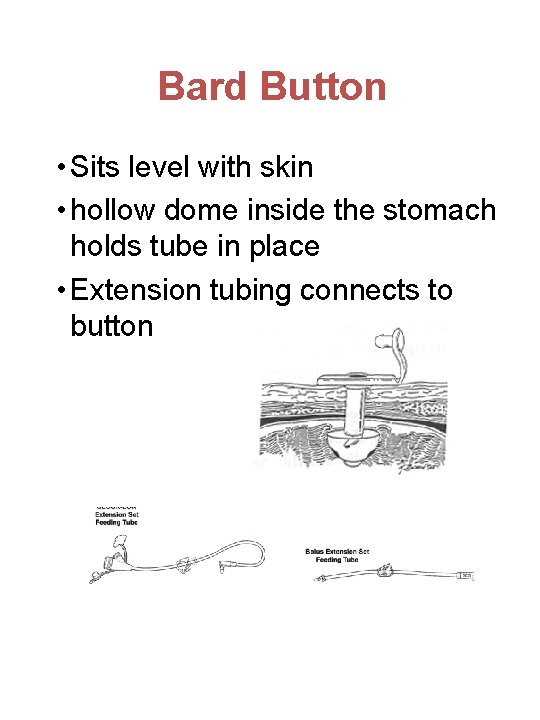
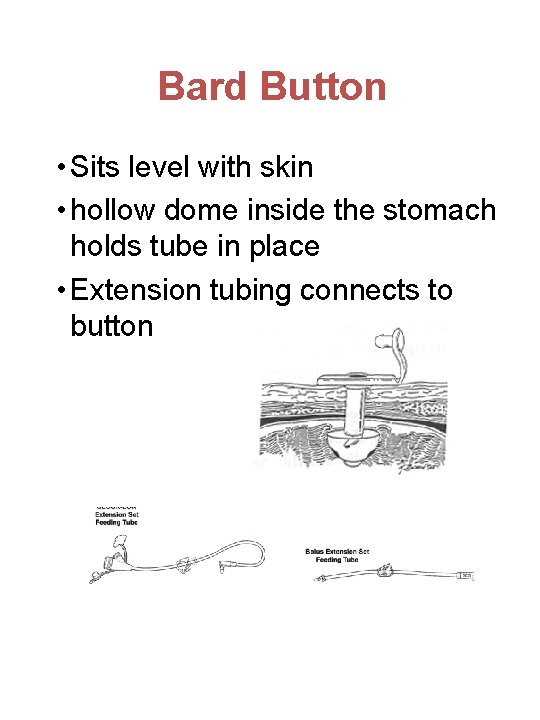
Bard Button • Sits level with skin • hollow dome inside the stomach holds tube in place • Extension tubing connects to button
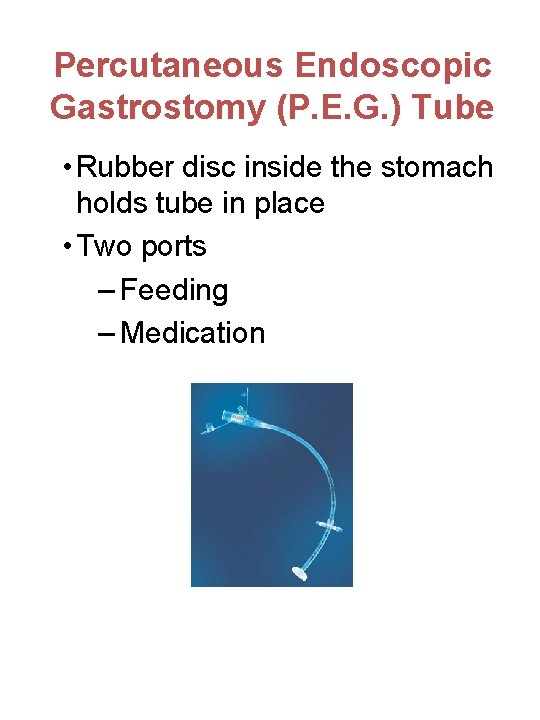
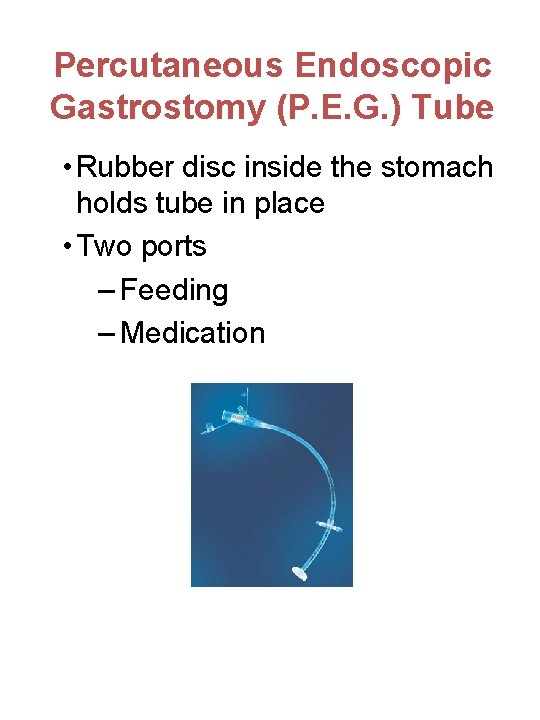
Percutaneous Endoscopic Gastrostomy (P. E. G. ) Tube • Rubber disc inside the stomach holds tube in place • Two ports – Feeding – Medication
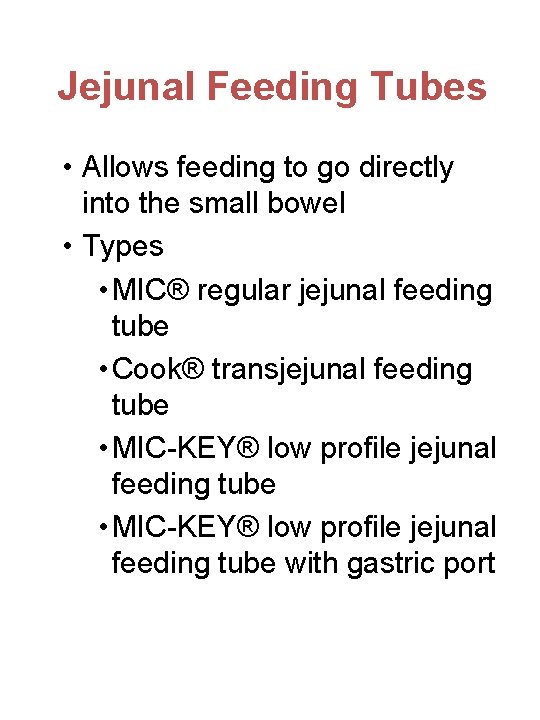
Jejunal Feeding Tubes • Allows feeding to go directly into the small bowel • Types • MIC® regular jejunal feeding tube • Cook® transjejunal feeding tube • MIC-KEY® low profile jejunal feeding tube with gastric port
Jejunal Feeding Tubes • Small bowel cannot handle a large feed like the stomach • Feeding is given continuously • Tube must be flushed well • Observe child for abdominal bloating, pain, vomiting or diarrhea. • Length of the tube outside of the stomach should be measured every time • Do not spin the tube in the stoma • Do not pull back on a syringe to empty the tube
Gastrostomy Feeds Gravity feed • Bag • Syringe Push method • Syringe Pump • Kangaroo Joey • Kangaroo 924
Gastrostomy Feeds • Wash hands • Tube must be in correct position • Child should be sit upright during the feeding • Tube should be flushed with water after a tube feed or medication
Giving Medication • Do not mix medications • Give medication before feed • Do not add medication to formula or feeding bag • Pills must be crushed and mixed with water • Tube is flushed before, between and after medications
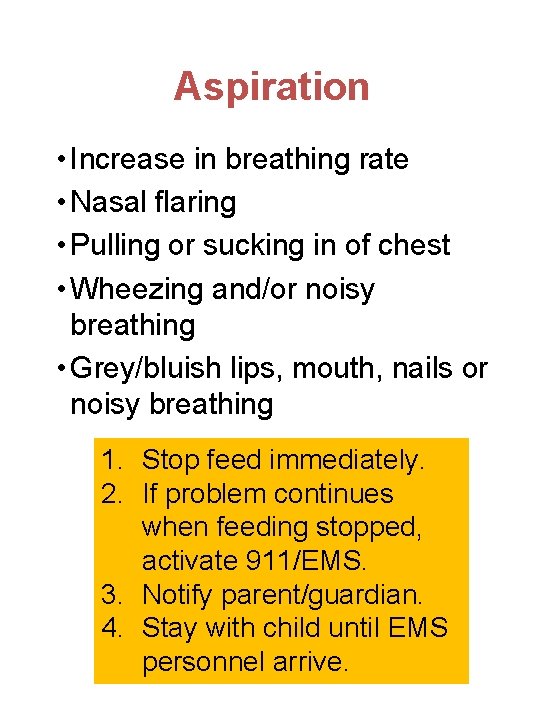
Aspiration • Increase in breathing rate • Nasal flaring • Pulling or sucking in of chest • Wheezing and/or noisy breathing • Grey/bluish lips, mouth, nails or noisy breathing 1. 2. 3. 4. Stop feed immediately. If problem continues when feeding stopped, activate 911/EMS. Notify parent/guardian. Stay with child until EMS personnel arrive.
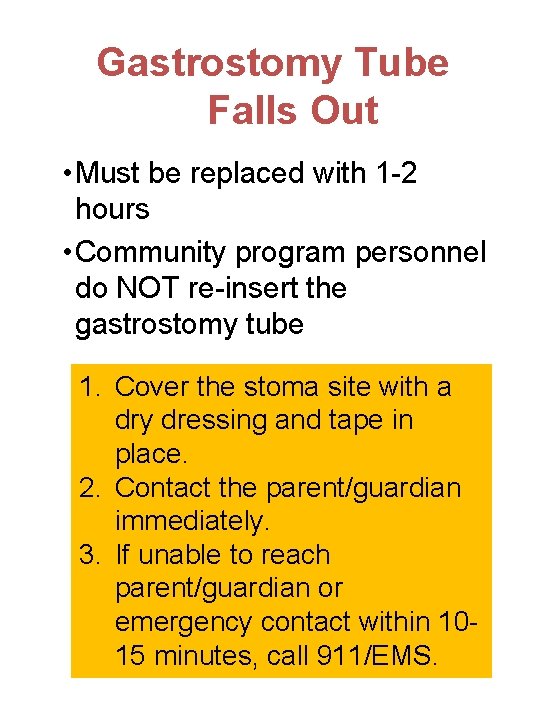
Gastrostomy Tube Falls Out • Must be replaced with 1 -2 hours • Community program personnel do NOT re-insert the gastrostomy tube 1. Cover the stoma site with a dry dressing and tape in place. 2. Contact the parent/guardian immediately. 3. If unable to reach parent/guardian or emergency contact within 1015 minutes, call 911/EMS.
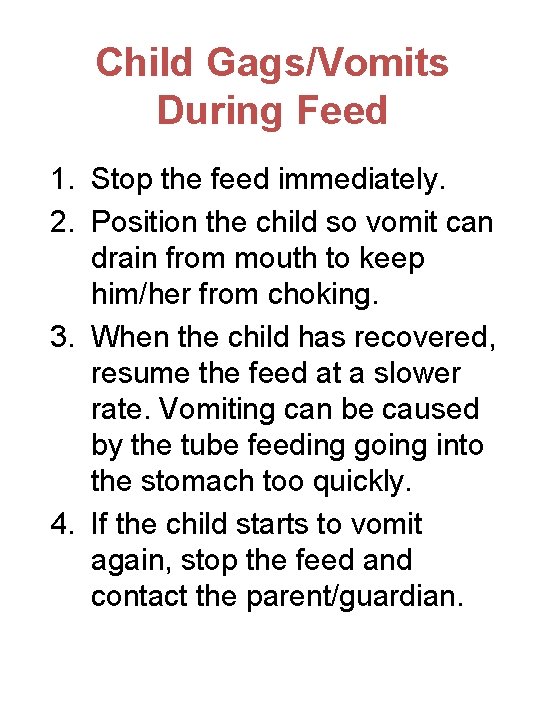
Child Gags/Vomits During Feed 1. Stop the feed immediately. 2. Position the child so vomit can drain from mouth to keep him/her from choking. 3. When the child has recovered, resume the feed at a slower rate. Vomiting can be caused by the tube feeding going into the stomach too quickly. 4. If the child starts to vomit again, stop the feed and contact the parent/guardian.
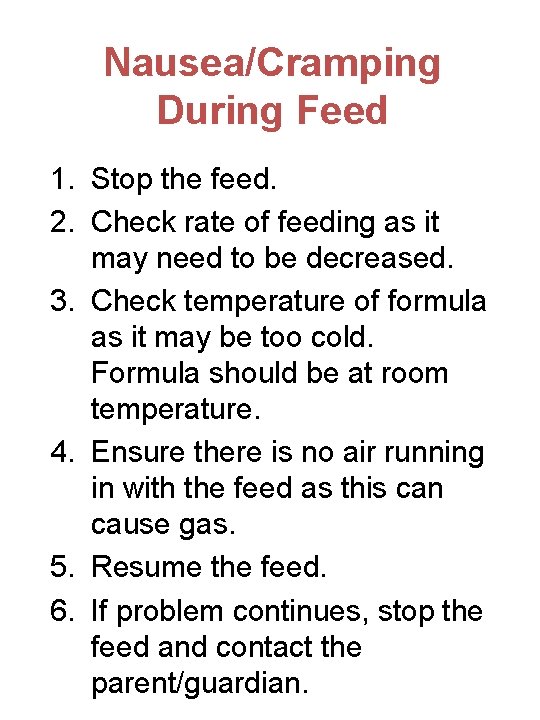
Nausea/Cramping During Feed 1. Stop the feed. 2. Check rate of feeding as it may need to be decreased. 3. Check temperature of formula as it may be too cold. Formula should be at room temperature. 4. Ensure there is no air running in with the feed as this can cause gas. 5. Resume the feed. 6. If problem continues, stop the feed and contact the parent/guardian.
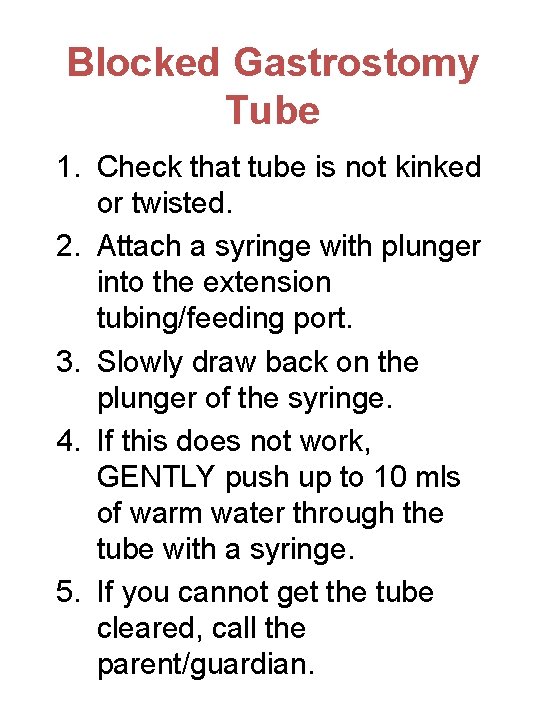
Blocked Gastrostomy Tube 1. Check that tube is not kinked or twisted. 2. Attach a syringe with plunger into the extension tubing/feeding port. 3. Slowly draw back on the plunger of the syringe. 4. If this does not work, GENTLY push up to 10 mls of warm water through the tube with a syringe. 5. If you cannot get the tube cleared, call the parent/guardian.
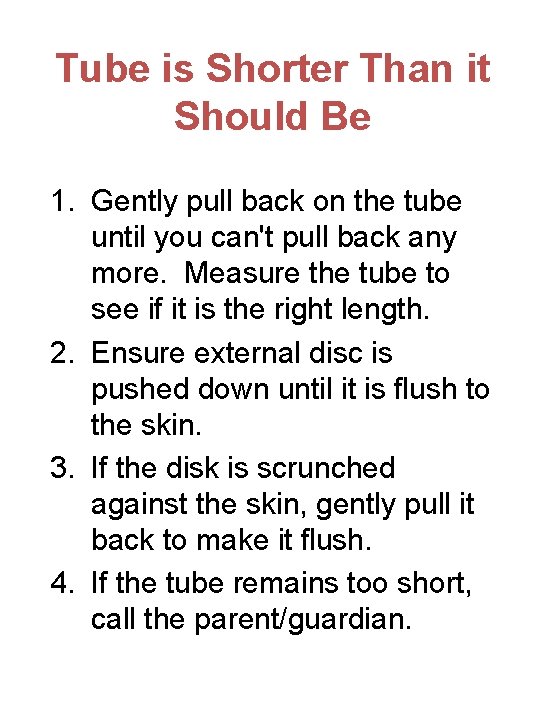
Tube is Shorter Than it Should Be 1. Gently pull back on the tube until you can't pull back any more. Measure the tube to see if it is the right length. 2. Ensure external disc is pushed down until it is flush to the skin. 3. If the disk is scrunched against the skin, gently pull it back to make it flush. 4. If the tube remains too short, call the parent/guardian.
Tube is Longer Than it Should Be Call the parent/guardian. Do NOT give feed or medication.
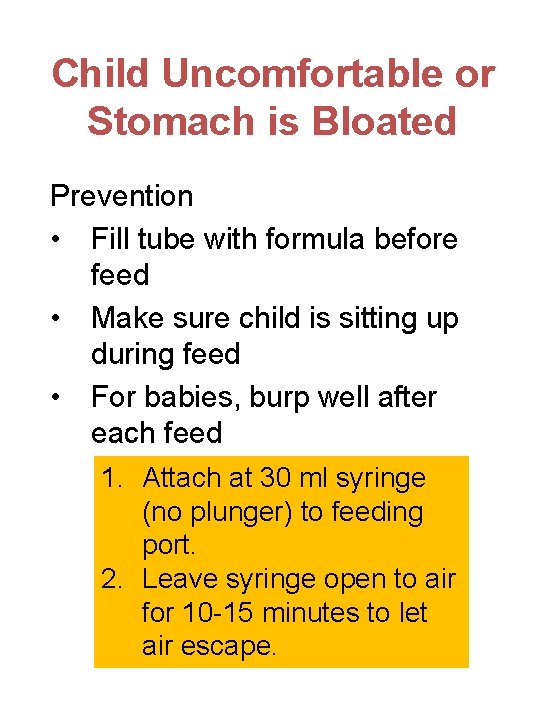
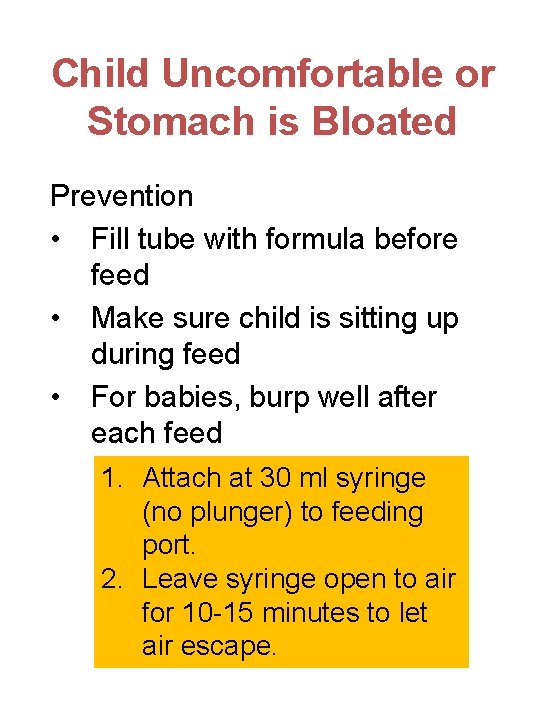
Child Uncomfortable or Stomach is Bloated Prevention • Fill tube with formula before feed • Make sure child is sitting up during feed • For babies, burp well after each feed 1. Attach at 30 ml syringe (no plunger) to feeding port. 2. Leave syringe open to air for 10 -15 minutes to let air escape.
Fever, Nausea, Vomiting, Diarrhea Notify the parent/guardian.
Redness, swelling change in color or odor at stoma site 1. Ensure the skin around the stoma site is clean and dry. 2. Notify the parent/guardian.
Feeding is leaking around gastrostomy tube 1. Stop the feed if child is experiencing pain or discomfort. 2. Ensure the skin around the stoma is clean and dry. 3. Notify the parent/guardian.
Bleeding or drainage around stoma 1. Ensure the skin around the stoma is clean and dry. 2. If there is a lot of oozing around the tube, cut a small gauze in a "Y" formation and place around tube. 3. Notify the parent/guardian.
Stoma Care 1. Wash hands and put on gloves. 2. Gather supplies and place on a clean surface. 3. Wash skin around stoma and tube/button with warm soapy water. 4. Rinse the skin and tube/button well with clear water. 5. Dry the skin.
Replacing Supplies • Feeding bag - weekly • Extension tube - monthly • Syringe - monthly or when plunger begin to sticks • Catheter tip adapter – re-use continuously • If the equipment does not appear clean after washing and rinsing thoroughly, replace it.
Cleaning Supplies 1. Ensure sink is clean. 2. Separate equipment. 3. Wash with warm water and mild dish soap. 4. Rinse equipment well. 5. Clear water from tubing as much as possible. 6. Air dry on a clean towel. Store in a clean and labeled container in fridge.
Formula • Check expiry date. Do not use formula after the expiry date • Wipe outside of can before opening • Shake well • Use formula within 4 hours after pouring it • Store unused formula in fridge. Use within 24 hours • Serve at room temperature • Do NOT use the microwave to warm up
Mouth Care • Daily • Use toothbrush, soft cloth, toothette or piece of gauze soaked in water • Fluoride toothpaste not recommended unless child can spit it out • Lip moisturizer may help with dry lips
Oral Stimulation • Some children are able to take small amounts of food • Oral motor stimulation can be nutritive or non-nutritive • Incorporate into regular play times and during tube feeds
Hand Washing • Before and after contact with body fluids • Iimmediately if in contact with blood or body fluids • After removal of gloves • Before and after contact with child • Before taking breaks • Use soap and water • Wash hands for at least 30 seconds
Wearing Gloves • Possible contact with blood or body fluids • Cleaning up spills of blood or body fluids • Handling items soiled with blood or body fluids • Contact with open wounds or sores • Performing mouth care • Assisting child with toileting/diapering • Caregiver has broken skin on the hands
Removing Gloves 1. Grasp cuff of one glove using the other gloved hand 2. Pull glove off the hand, allowing it to turn inside out 3. Grasp and contain the removed glove within the palm of the gloved hand 4. Place thumb of the ungloved hand underneath the cuff of the gloved hand, and remove it by pulling it inside out, over the first
Clean Up • Double bag items contaminated with blood or body fluids in separate container • Cleaning contaminated surfaces • Use absorbent disposable paper towel to clean up spills • Wash surfaces with water and detergent and then household bleach • Air dry cleaned surfaces