Fluid Volume Electrolytes Causes ECF Volume deficit Hypovolemia
- Slides: 40
Fluid Volume Electrolytes
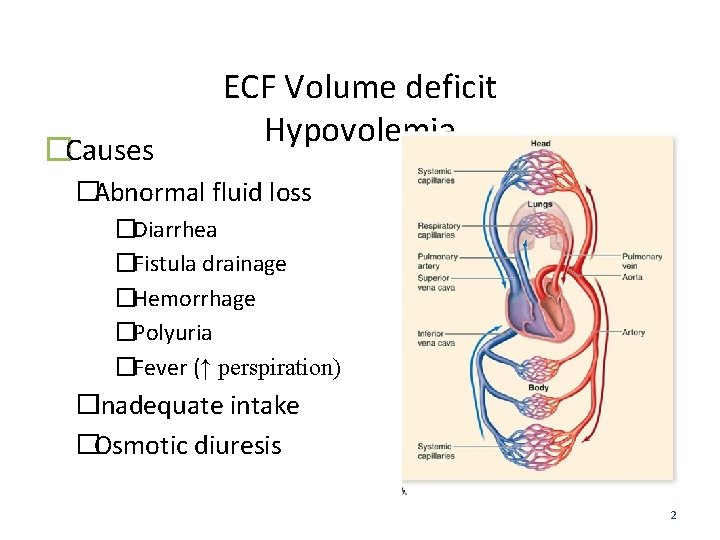
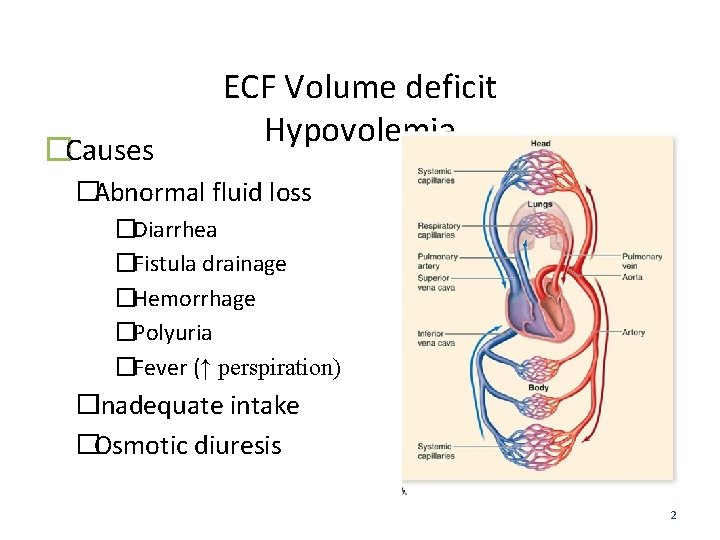
�Causes ECF Volume deficit Hypovolemia �Abnormal fluid loss �Diarrhea �Fistula drainage �Hemorrhage �Polyuria �Fever (↑ perspiration) �Inadequate intake �Osmotic diuresis 2
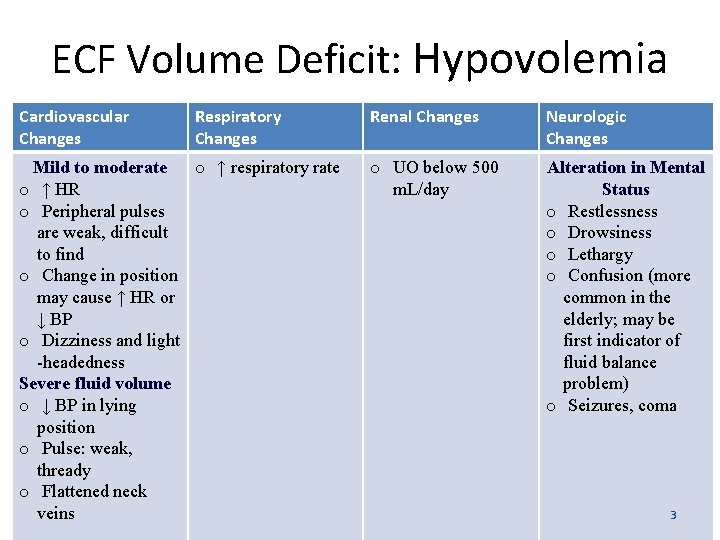
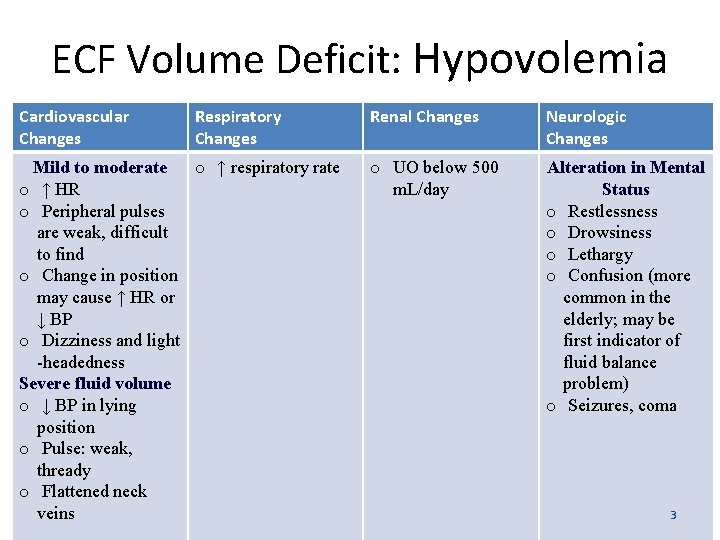
ECF Volume Deficit: Hypovolemia Cardiovascular Changes Respiratory Changes Mild to moderate o ↑ respiratory rate o ↑ HR o Peripheral pulses are weak, difficult to find o Change in position may cause ↑ HR or ↓ BP o Dizziness and light -headedness Severe fluid volume o ↓ BP in lying position o Pulse: weak, thready o Flattened neck veins Renal Changes Neurologic Changes o UO below 500 m. L/day Alteration in Mental Status o Restlessness o Drowsiness o Lethargy o Confusion (more common in the elderly; may be first indicator of fluid balance problem) o Seizures, coma 3
ECF Volume deficit Assessment Findings �Skin turgor is diminished �Skin may be warm and dry with mild deficit �Skin may be cool and moist with severe deficit �Skin may appear dry and wrinkled �Oral mucous membranes will be dry, sticky, pastelike coating and the tongue may be furrowed �Patient C/O thirst �Eyes: soft, sunken �Lab data: �↑ H & H; BUN; Josie King 4
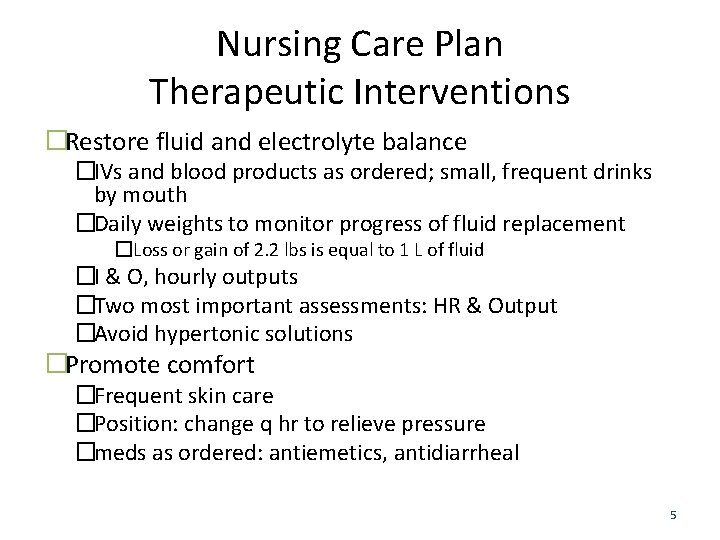
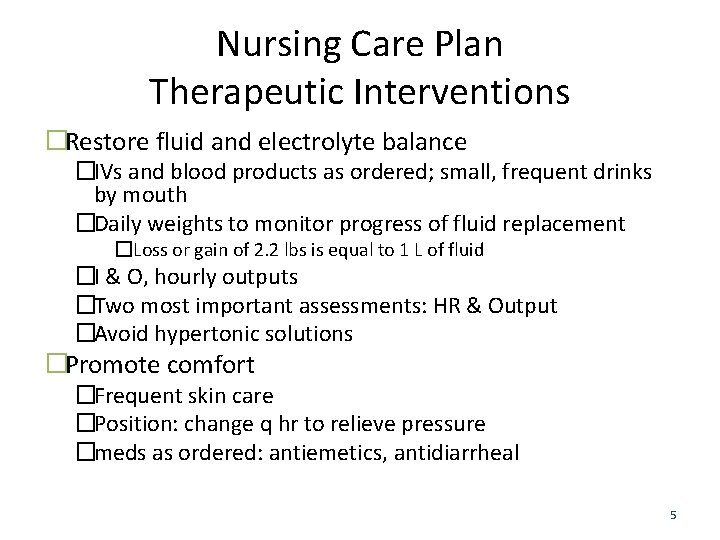
Nursing Care Plan Therapeutic Interventions �Restore fluid and electrolyte balance �IVs and blood products as ordered; small, frequent drinks by mouth �Daily weights to monitor progress of fluid replacement �Loss or gain of 2. 2 lbs is equal to 1 L of fluid �I & O, hourly outputs �Two most important assessments: HR & Output �Avoid hypertonic solutions �Promote comfort �Frequent skin care �Position: change q hr to relieve pressure �meds as ordered: antiemetics, antidiarrheal 5
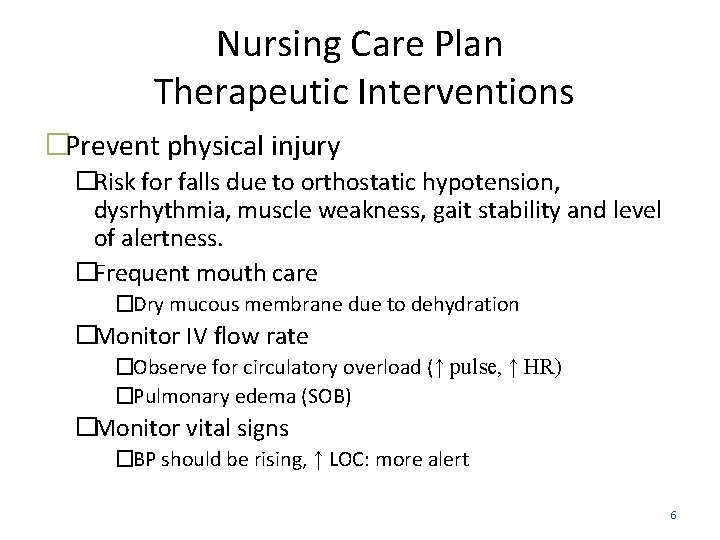
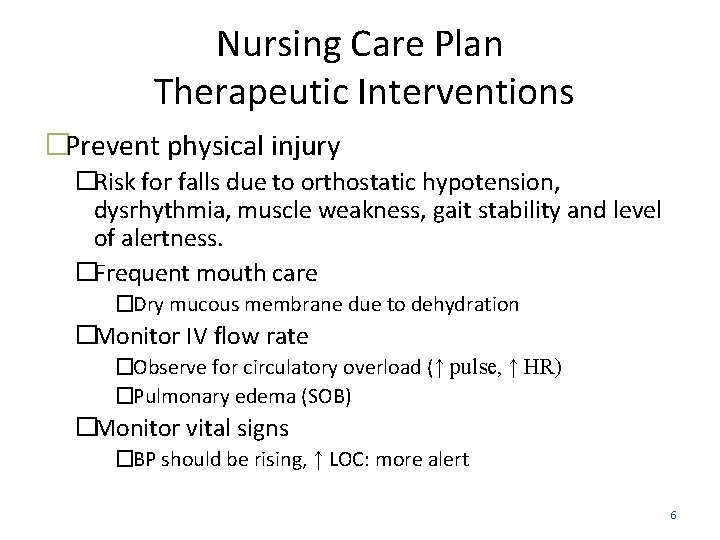
Nursing Care Plan Therapeutic Interventions �Prevent physical injury �Risk for falls due to orthostatic hypotension, dysrhythmia, muscle weakness, gait stability and level of alertness. �Frequent mouth care �Dry mucous membrane due to dehydration �Monitor IV flow rate �Observe for circulatory overload (↑ pulse, ↑ HR) �Pulmonary edema (SOB) �Monitor vital signs �BP should be rising, ↑ LOC: more alert 6
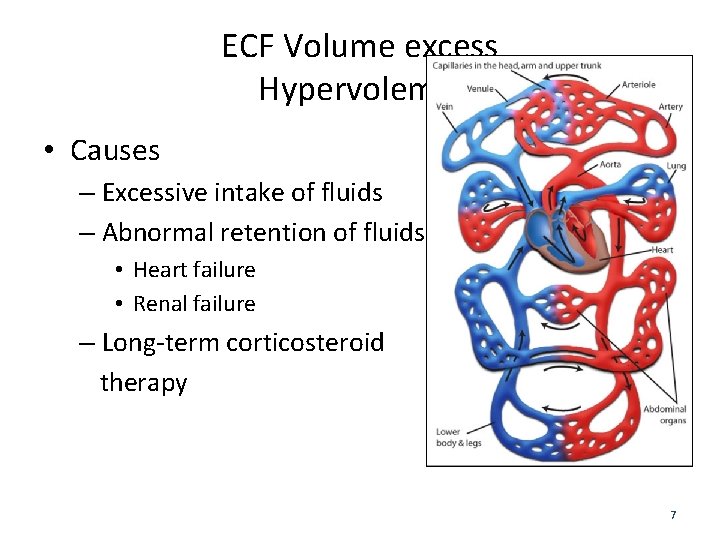
ECF Volume excess Hypervolemia • Causes – Excessive intake of fluids – Abnormal retention of fluids • Heart failure • Renal failure – Long-term corticosteroid therapy 7
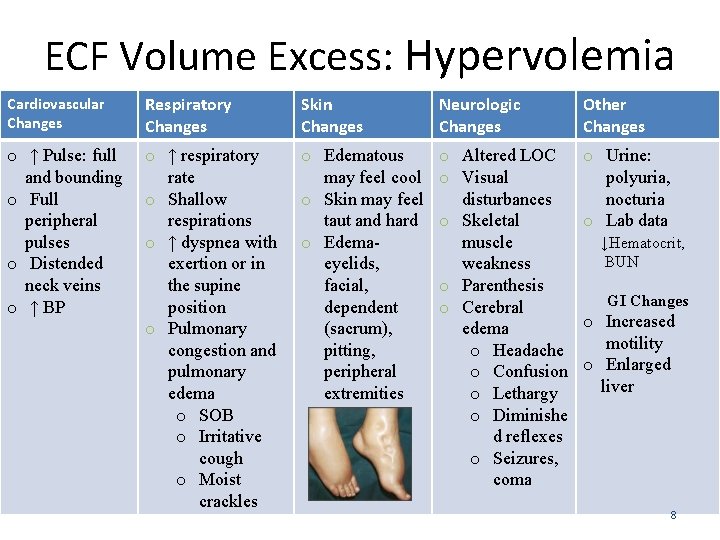
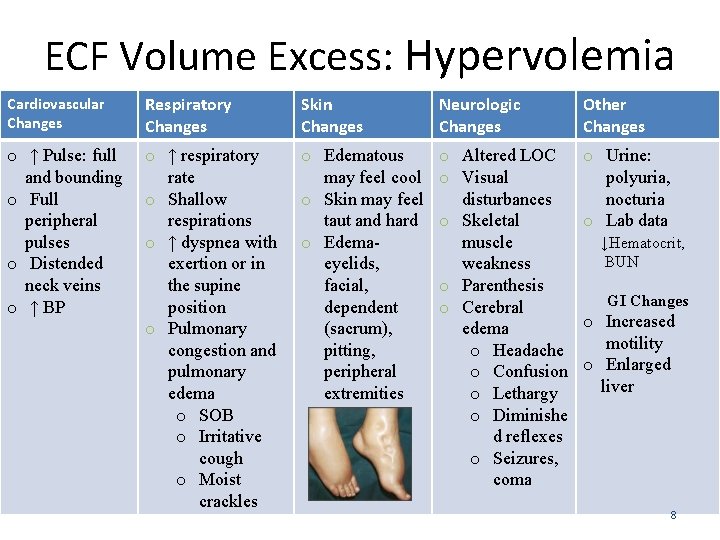
ECF Volume Excess: Hypervolemia Cardiovascular Changes Respiratory Changes Skin Changes Neurologic Changes Other Changes o ↑ Pulse: full and bounding o Full peripheral pulses o Distended neck veins o ↑ BP o ↑ respiratory rate o Shallow respirations o ↑ dyspnea with exertion or in the supine position o Pulmonary congestion and pulmonary edema o SOB o Irritative cough o Moist crackles o Edematous may feel cool o Skin may feel taut and hard o Edemaeyelids, facial, dependent (sacrum), pitting, peripheral extremities o Altered LOC o Visual disturbances o Skeletal muscle weakness o Parenthesis o Cerebral edema o Headache o Confusion o Lethargy o Diminishe d reflexes o Seizures, coma o Urine: polyuria, nocturia o Lab data ↓Hematocrit, BUN GI Changes o Increased motility o Enlarged liver 8
Nursing Care Plan Therapeutic Interventions �Maintain oxygen to all cells �Position: sim-Fowler’s or Fowler’s to facilitate improved gas exchange. �Vital signs; q 4 hrs and PRN �Tachycardia �↑ BP (overload) and ↓ BP (fluid deficit) �Fluid restriction: I & O �Promote excretion of excess fluid �Meds as ordered: diuretics �Monitor electrolytes, esp. Mg and K 9
Nursing Care Plan Therapeutic Interventions �Obtain/maintain fluid balance �Wt gain is the best indicator of fluid retention and overload �Weight daily; 2. 2 lbs = 1 Liter (1000 ml) �Measure: all edematous parts, abdominal girth, �I & O: fluid restriction �Limit fluids by mouth, IVs per doctors orders �Strict monitoring of IV fluids �Prevent tissue injury �Skin and mouth care as needed �Evaluate feet for edema and discoloration when client is OOB �Observe suture line on surgical clients (Potential for evisceration due to excess fluid retention) 10
Functions of Sodium • Regulates osmolality – ICF: 14 mmol/L & ECF: 135 -145 mmol/L • Helps maintain blood pressure by balancing the volume of water in the body • Works with other electrolytes to promote nerves, muscles and other body tissues to work properly. 11
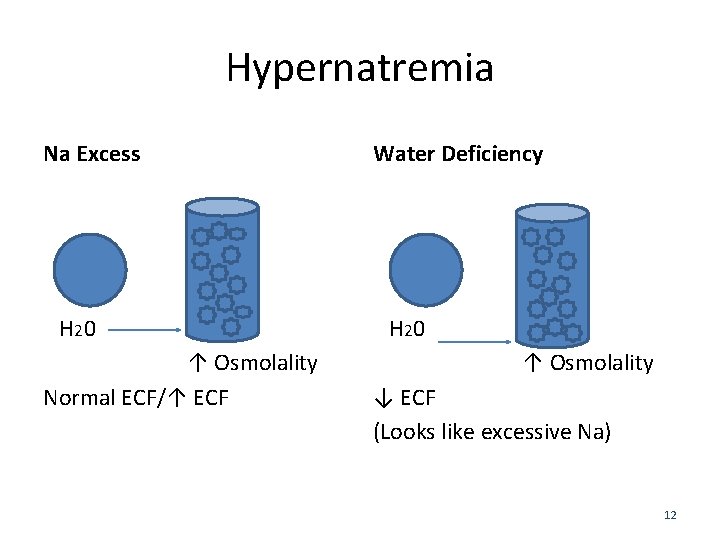
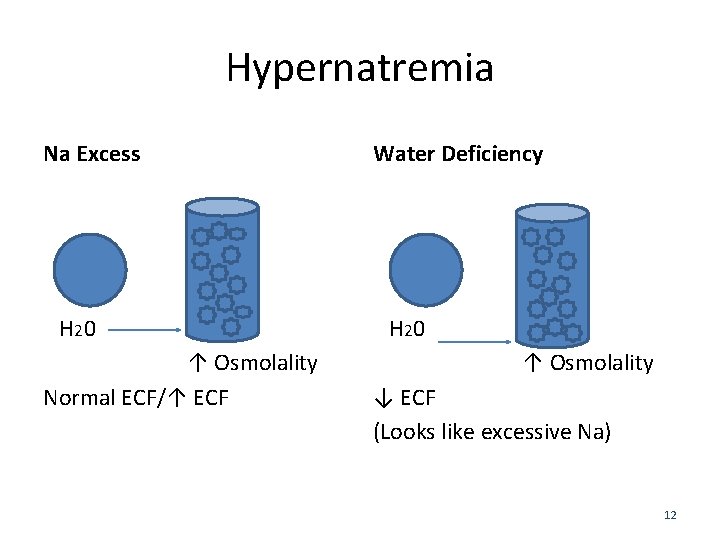
Hypernatremia Na Excess H 2 0 ↑ Osmolality Normal ECF/↑ ECF Water Deficiency H 2 0 ↑ Osmolality ↓ ECF (Looks like excessive Na) 12
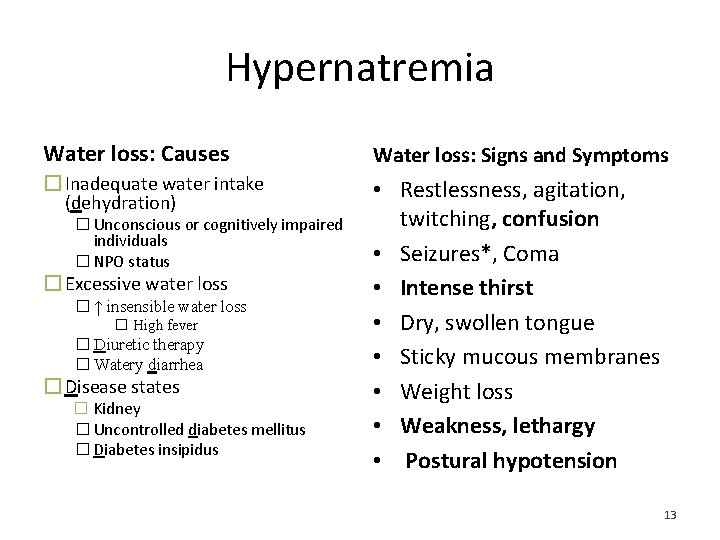
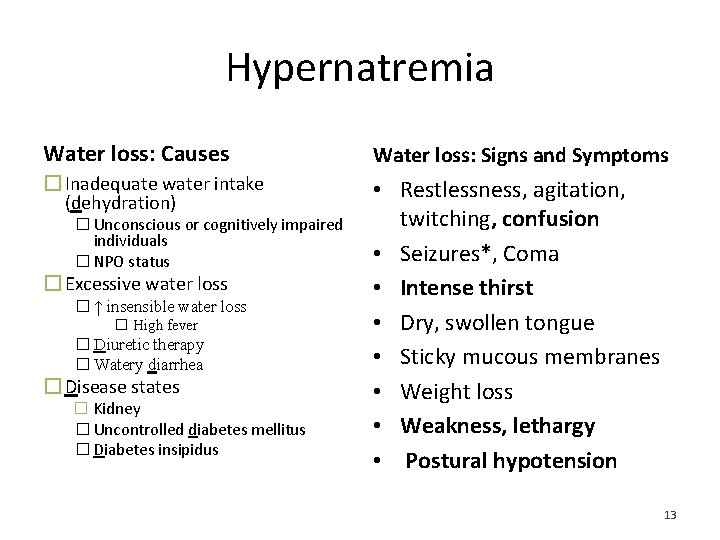
Hypernatremia Water loss: Causes Water loss: Signs and Symptoms � Inadequate water intake (dehydration) • Restlessness, agitation, twitching, confusion • Seizures*, Coma • Intense thirst • Dry, swollen tongue • Sticky mucous membranes • Weight loss • Weakness, lethargy • Postural hypotension � Unconscious or cognitively impaired individuals � NPO status � Excessive water loss � ↑ insensible water loss � High fever � Diuretic therapy � Watery diarrhea � Disease states � Kidney � Uncontrolled diabetes mellitus � Diabetes insipidus 13
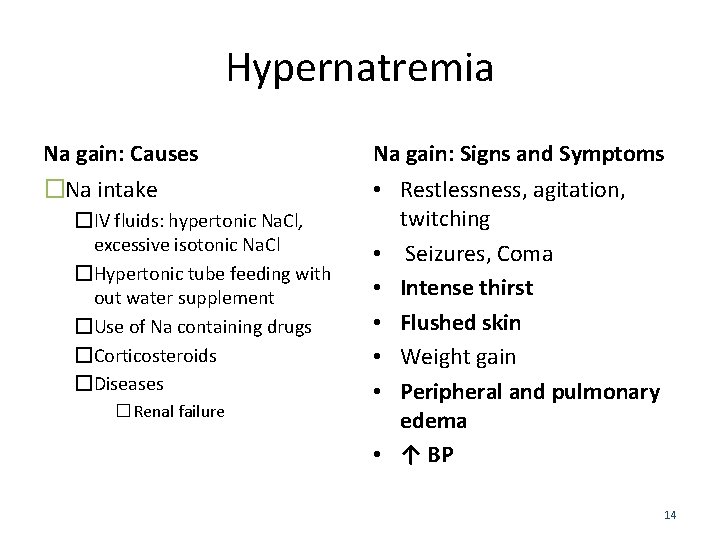
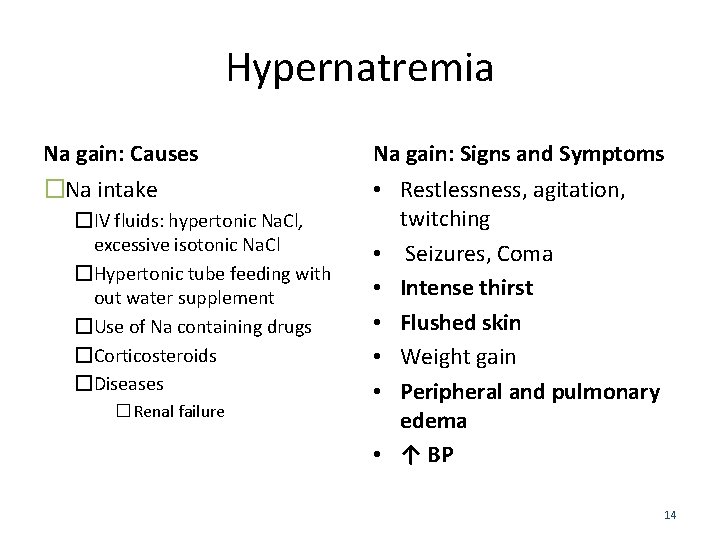
Hypernatremia Na gain: Causes Na gain: Signs and Symptoms �Na intake • Restlessness, agitation, twitching • Seizures, Coma • Intense thirst • Flushed skin • Weight gain • Peripheral and pulmonary edema • ↑ BP �IV fluids: hypertonic Na. Cl, excessive isotonic Na. Cl �Hypertonic tube feeding with out water supplement �Use of Na containing drugs �Corticosteroids �Diseases � Renal failure 14
Group learning • Discuss with your neighbor – Why in Hypernatremia (water deficit) and hypernatremia (gain of more salt) there is a difference in the BP (blood pressure). – List a Nursing Diagnosis for a patient with hypernatremia. 15
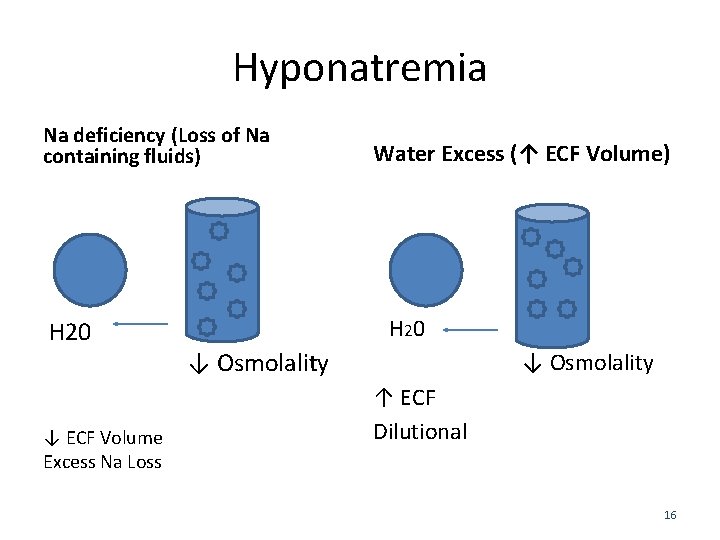
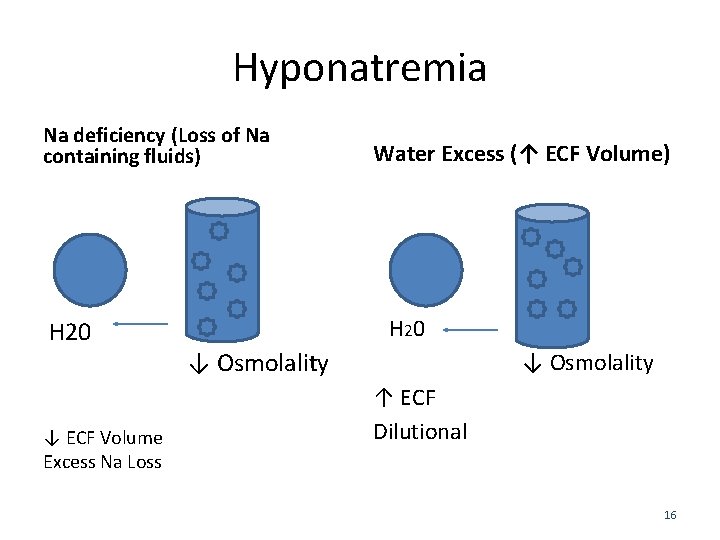
Hyponatremia Na deficiency (Loss of Na containing fluids) H 20 ↓ ECF Volume Excess Na Loss Water Excess (↑ ECF Volume) H 2 0 ↓ Osmolality ↑ ECF Dilutional 16
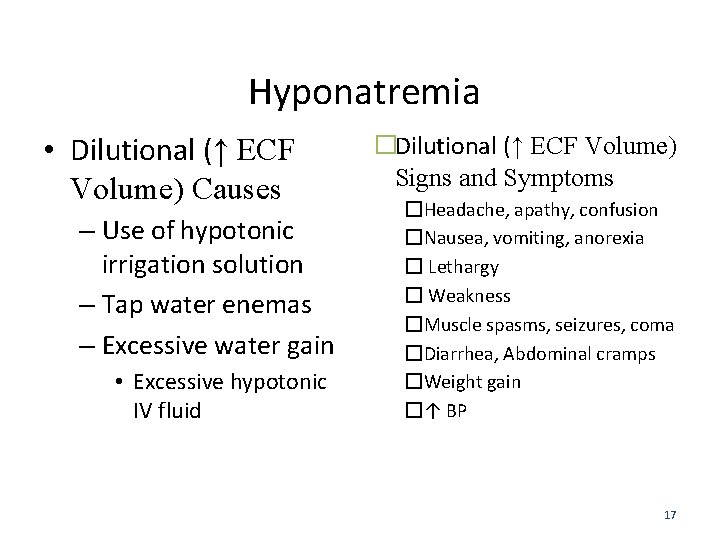
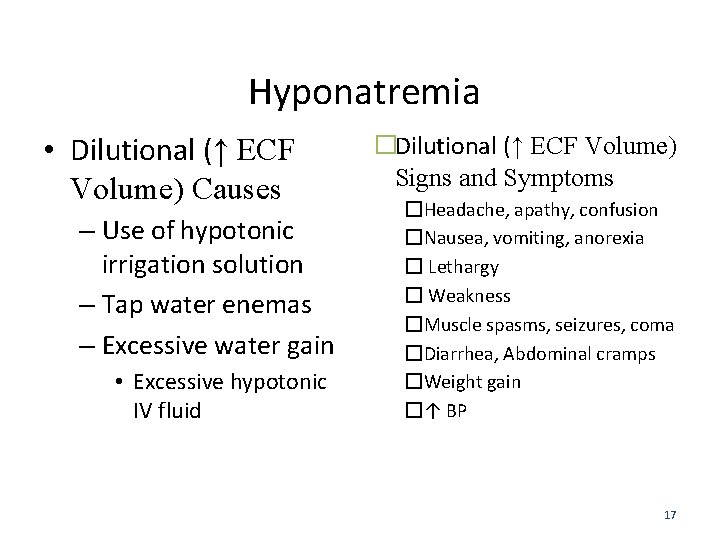
Hyponatremia • Dilutional (↑ ECF Volume) Causes – Use of hypotonic irrigation solution – Tap water enemas – Excessive water gain • Excessive hypotonic IV fluid �Dilutional (↑ ECF Volume) Signs and Symptoms �Headache, apathy, confusion �Nausea, vomiting, anorexia � Lethargy � Weakness �Muscle spasms, seizures, coma �Diarrhea, Abdominal cramps �Weight gain �↑ BP 17
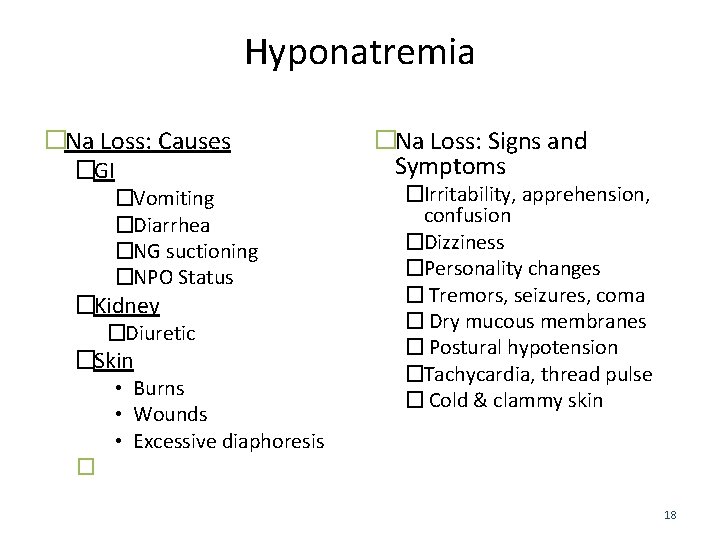
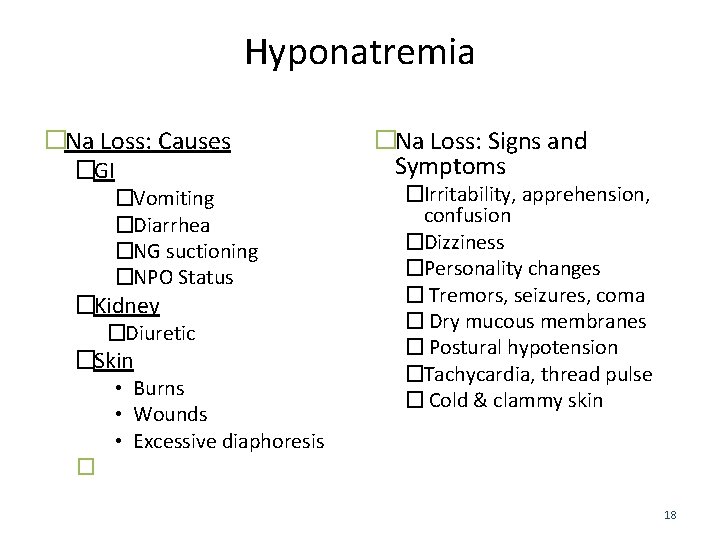
Hyponatremia �Na Loss: Causes �GI �Vomiting �Diarrhea �NG suctioning �NPO Status �Kidney �Diuretic �Skin • Burns • Wounds • Excessive diaphoresis �Na Loss: Signs and Symptoms �Irritability, apprehension, confusion �Dizziness �Personality changes � Tremors, seizures, coma � Dry mucous membranes � Postural hypotension �Tachycardia, thread pulse � Cold & clammy skin � 18
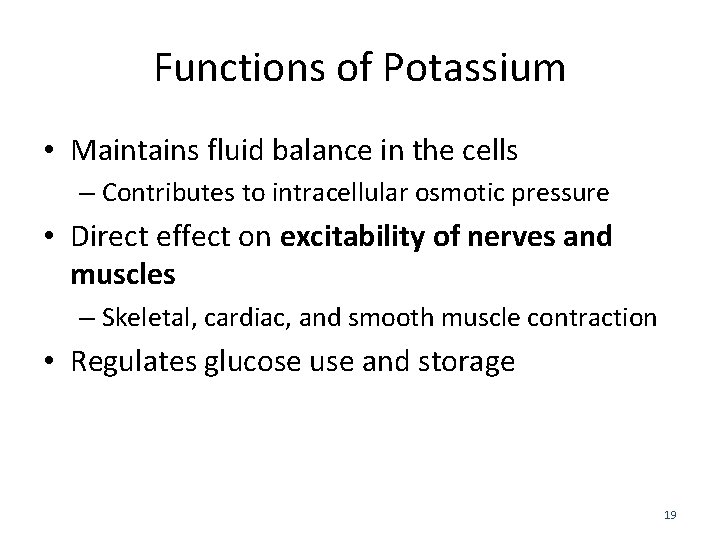
Functions of Potassium • Maintains fluid balance in the cells – Contributes to intracellular osmotic pressure • Direct effect on excitability of nerves and muscles – Skeletal, cardiac, and smooth muscle contraction • Regulates glucose use and storage 19
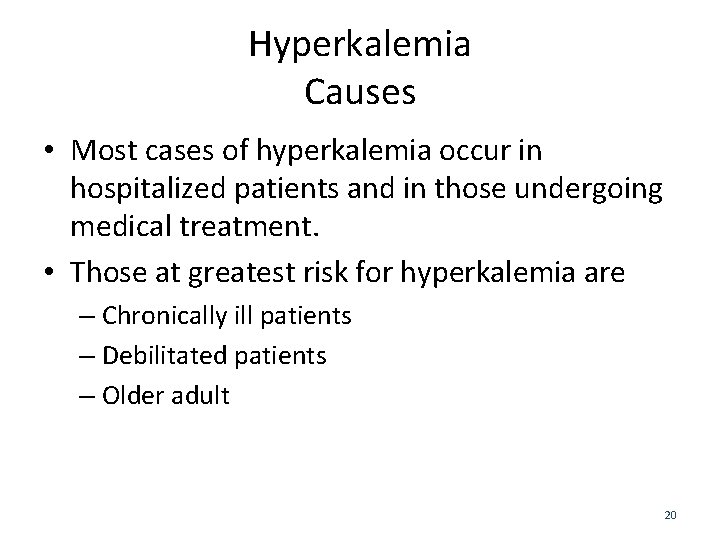
Hyperkalemia Causes • Most cases of hyperkalemia occur in hospitalized patients and in those undergoing medical treatment. • Those at greatest risk for hyperkalemia are – Chronically ill patients – Debilitated patients – Older adult 20
Hyperkalemia Causes Actual hyperkalemia Relative hyperkalemia • Excess potassium Intake • Shift of potassium Out of Cells – Excessive or rapid parenteral administration – Acidosis – Crushing injury – Tissue catabolism (fever, sepsis, burns) 21
Hyperkalemia Causes • Failure to Eliminate Potassium – Renal disease – Potassium-sparing diuretics – ACE inhibitors 22
Hyperkalemia Signs and Symptoms Clinical Manifestations Electrocardiogram Changes �Irritability �Abdominal cramping, diarrhea �Weakness of lower extremities �Irregular pulse �Cardiac arrest if hyperkalemia sudden or severe • Ventricular fibrillation • Ventricular standstill 23
Hypokalemia Causes • Potassium Loss – GI losses: diarrhea, vomiting, fistulas, NG suction, NPO status – Renal losses: diuretics, – Skin losses: diaphoresis – Dialysis • Shift of Potassium into Cells – Alkalosis 24
Hypokalemia Causes • Lack of Potassium Intake – Starvation – Diet low in K – Failure to include K in parenteral fluids if NPO – TPN 25
Hypokalemia Signs and Symptoms Clinical Manifestations Electrocardiogram Changes �Fatigue �Muscle weakness, leg cramps �Nausea, vomiting, paralytic ileus �Soft, flabby muscles �Paresthesia, decreased reflexes �Weak, irregular pulse • Ventricular dysrhythmias (e. g. , PVCs) • Bradycardia 26
Hypokalemia Medical Management �Administration of KCl supplements �K may be given orally (K chloride, K gluconate, K citrate) or IV �KCl should be administered IV at a rate of 10 to 20 m. Eq/L over an hour. Rapid infusion could cause cardiac arrest �IV K solutions irritate veins and cause phlebitis. Check IV site q 2 hrs. Discontinue IV if infiltrate to prevent necrotic and slough of tissue 27
Functions of Calcium • Helps maintain muscle tone • Contributes to regulation of blood pressure by maintaining cardiac contractility • Necessary for nerve transmission and contraction of skeletal and cardiac muscle 28
Hypercalcemia Causes �Increased Total Calcium �Prolonged immobilization �Thiazide diuretics �Dehydration �Renal failure 29
Hypercalcemia Signs and Symptoms Clinical Manifestations Electrocardiogram Changes �Lethargy, weakness �Depressed reflexes (DTR) �Decreased memory �Confusion, personality changes, psychosis �Anorexia, nausea, vomiting, constipation �Bone pain, fractures • Ventricular dysrhythmias • Hypertension 30
Hypocalcemia Causes �Decreased Total Calcium �Chronic renal failure �Loop diuretics (e. g. , furosemide [Lasix]) �Chronic alcoholism �Diarrhea �Decreased Ionized Calcium �Excess administration of citrated blood 31
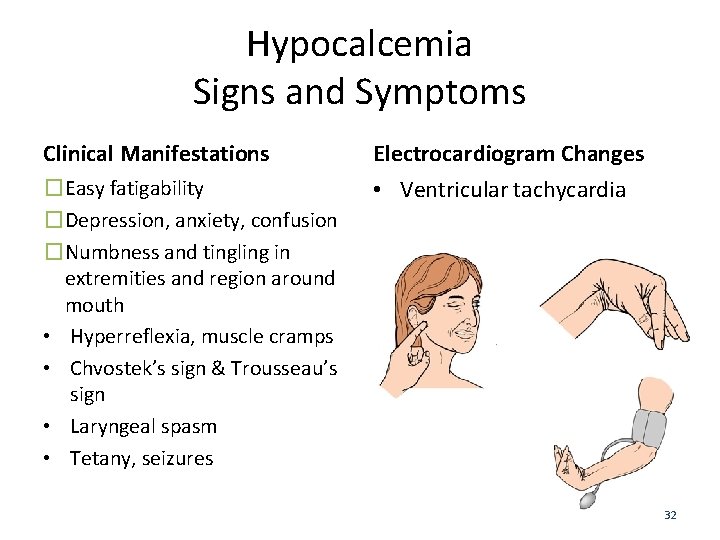
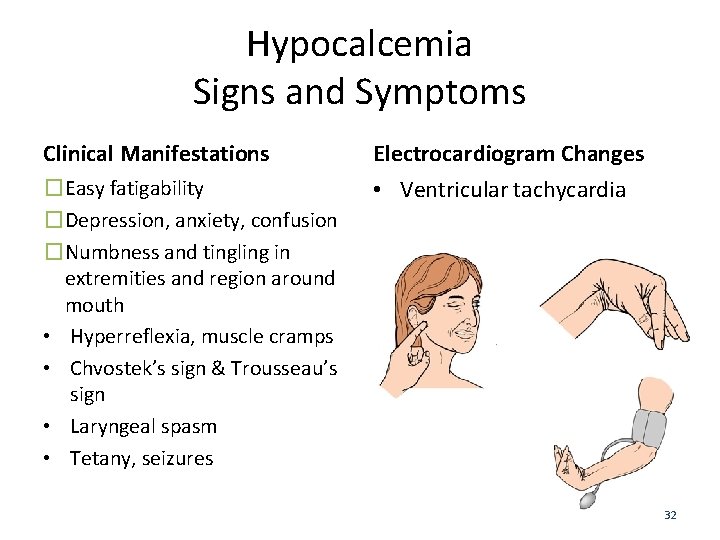
Hypocalcemia Signs and Symptoms Clinical Manifestations Electrocardiogram Changes �Easy fatigability �Depression, anxiety, confusion �Numbness and tingling in extremities and region around mouth • Hyperreflexia, muscle cramps • Chvostek’s sign & Trousseau’s sign • Laryngeal spasm • Tetany, seizures • Ventricular tachycardia 32
Functions of Magnesium • Cofactor in clotting cascade • Acts directly on myoneural junction, affecting muscular irritability and contractions • Maintains strong and healthy bones 33
Hypermagnesemia Causes �Renal failure �Diabetes Mellitus �Clients who ingest large amounts of Mgcontaining antacids such as Tums, Maalox, Mylanta, or laxatives such as MOM are also in ↑ risk for developing hypermagnesemia 34
Hypermagnesemia Signs and Symptoms – Bradycardia and hypotension – Severe hypermagnesemia: cardiac arrest – Drowsy or lethargic – Coma – Deep tendon reflexes are reduced or absent – Skeletal muscle contractions become progressively weaker and finally stop 35
Hypomagnesaemia Causes • Malabsorption disorders – Inflammatory bowel disease (IBD) – Bowel resection – Bariatric population who undergoes gastric bypass surgery • Alcoholism • Prolonged diarrhea • Draining GI fistulas • Diuretics 36
Hypomagnesaemia Signs and Symptoms • Confusion • Hyperactive deep tendon reflexes • Tremors • Seizures • Neuromuscular changes – Hyperactive deep tendon reflexes – Numbness and tingling – Painful muscle contractions – Monitor for positive Chvostek’s and Trousseau’s signs (hypocalemia may 37
Group learning • Discuss with your neighbor – The questions the nurse asks to elicit risk factors for fluid and electrolyte imbalances – How recent surgery causes changes in F & E imbalances – How increased GI output can cause changes in F & E imbalances 38
Physical Assessment • Daily weights – Indicator of fluid status – Use same conditions. • Fluid intake and output (I&O) – 24 -hour I&O: compare intake versus output – Intake includes all liquids eaten, drunk, or received through IV. – Output = Urine, diarrhea, vomitus, gastric suction, wound drainage • Laboratory studies
Fluid and Electrolyte Assessment • Nutritional-Metabolic Pattern – What is your typical daily food intake? Describe a day’s meals, snacks, and vitamins. – How much salt do you typically add to your food? Do you use salt substitutes? – How is your appetite? – Do you have any difficulty chewing or swallowing? – What is your typical daily fluid intake? What types of fluids (water, juices, soft drinks, coffee, tea)? How much? 40