Faculty of Medicine Introduction to Community Medicine Course




- Slides: 83

Faculty of Medicine Introduction to Community Medicine Course (31505201) Primary Health Care-PHC Maternal & Child Health- MCH By Hatim Jaber MD MPH JBCM Ph. D 1 - 11 - 2017 1
2
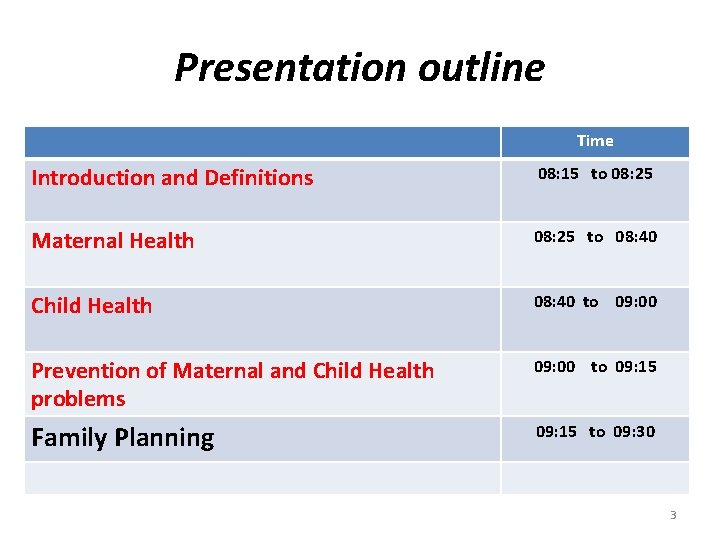
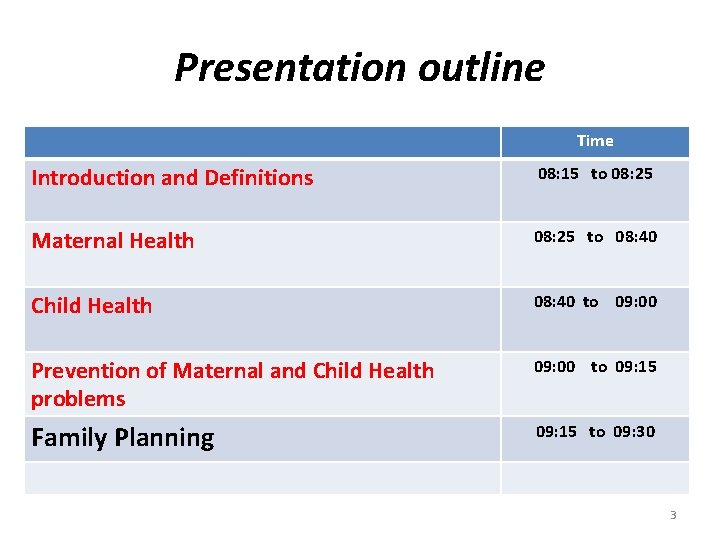
Presentation outline Time Introduction and Definitions 08: 15 to 08: 25 Maternal Health 08: 25 to 08: 40 Child Health 08: 40 to 09: 00 Prevention of Maternal and Child Health problems 09: 00 to 09: 15 Family Planning 09: 15 to 09: 30 3
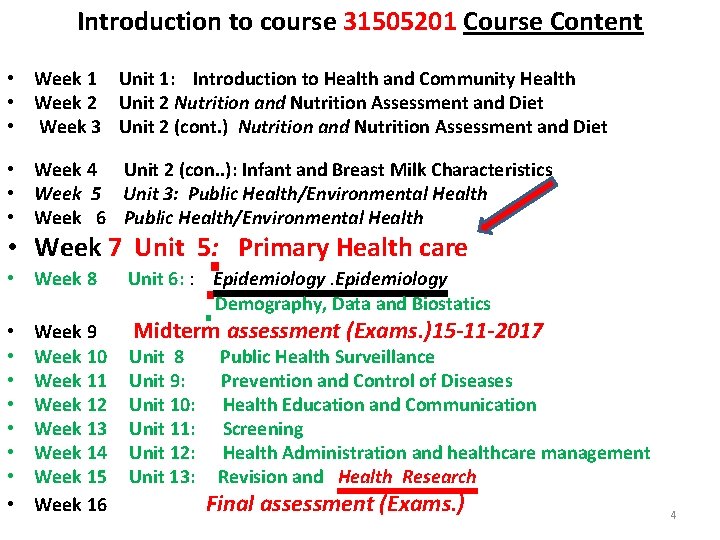
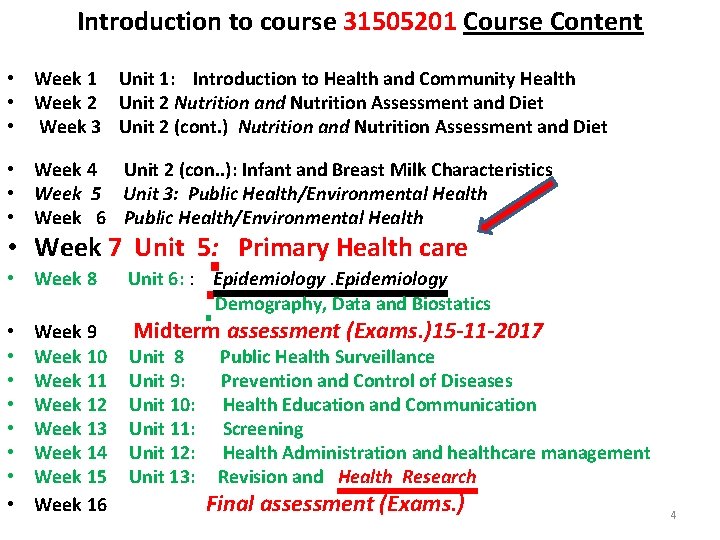
Introduction to course 31505201 Course Content • Week 1 Unit 1: Introduction to Health and Community Health • Week 2 Unit 2 Nutrition and Nutrition Assessment and Diet • Week 3 Unit 2 (cont. ) Nutrition and Nutrition Assessment and Diet • Week 4 Unit 2 (con. . ): Infant and Breast Milk Characteristics • Week 5 Unit 3: Public Health/Environmental Health • Week 6 Public Health/Environmental Health • Week 7 Unit 5: Primary Health care • Week 8 • • Week 9 Week 10 Week 11 Week 12 Week 13 Week 14 Week 15 Week 16 Unit 6: : Epidemiology Demography, Data and Biostatics Midterm assessment (Exams. )15 -11 -2017 Unit 8 Unit 9: Unit 10: Unit 11: Unit 12: Unit 13: Public Health Surveillance Prevention and Control of Diseases Health Education and Communication Screening Health Administration and healthcare management Revision and Health Research Final assessment (Exams. ) 4
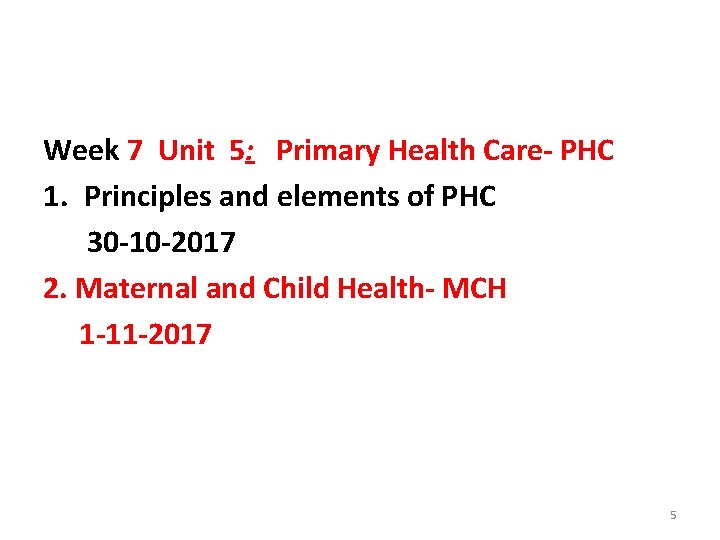
Week 7 Unit 5: Primary Health Care- PHC 1. Principles and elements of PHC 30 -10 -2017 2. Maternal and Child Health- MCH 1 -11 -2017 5
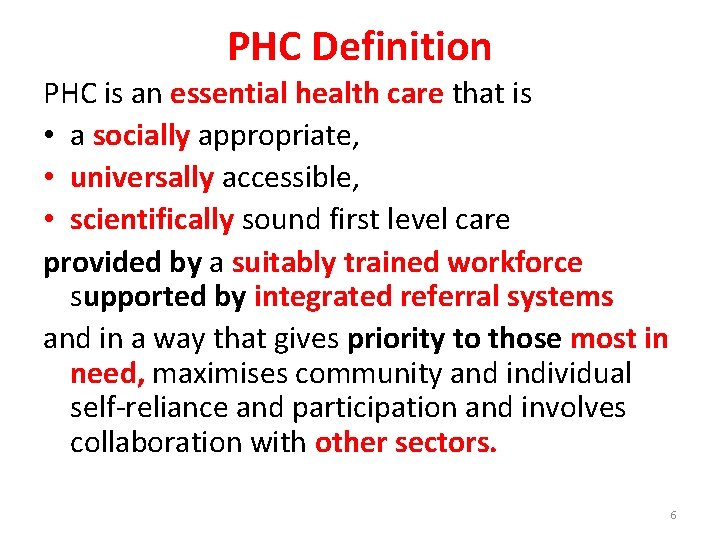
PHC Definition PHC is an essential health care that is • a socially appropriate, • universally accessible, • scientifically sound first level care provided by a suitably trained workforce supported by integrated referral systems and in a way that gives priority to those most in need, maximises community and individual self-reliance and participation and involves collaboration with other sectors. 6
Declaration of the Alma Ata • Released in 1978 and consisted of ten fundamental principles for effective comprehensive primary health care service delivery • Principles were in response to the broader community and social issues leading to poor population health 7
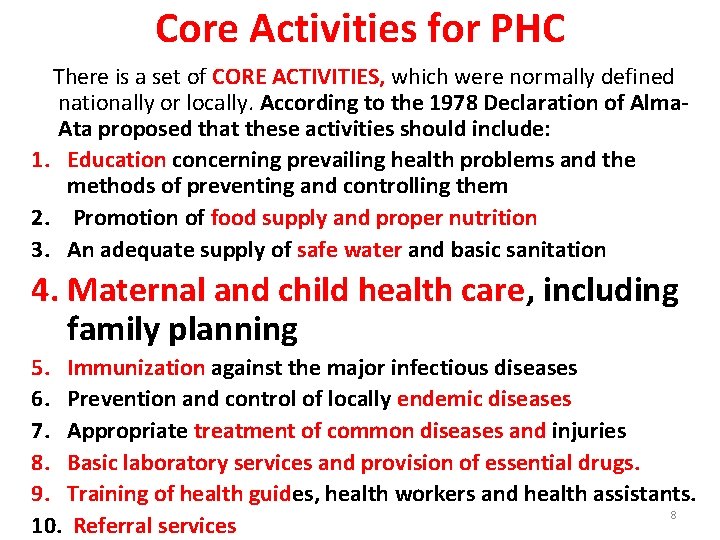
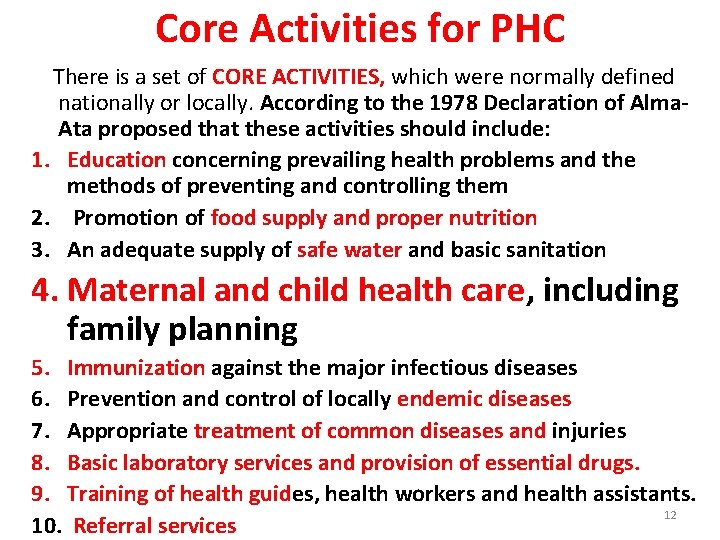
Core Activities for PHC There is a set of CORE ACTIVITIES, which were normally defined nationally or locally. According to the 1978 Declaration of Alma. Ata proposed that these activities should include: 1. Education concerning prevailing health problems and the methods of preventing and controlling them 2. Promotion of food supply and proper nutrition 3. An adequate supply of safe water and basic sanitation 4. Maternal and child health care, including family planning 5. Immunization against the major infectious diseases 6. Prevention and control of locally endemic diseases 7. Appropriate treatment of common diseases and injuries 8. Basic laboratory services and provision of essential drugs. 9. Training of health guides, health workers and health assistants. 8 10. Referral services
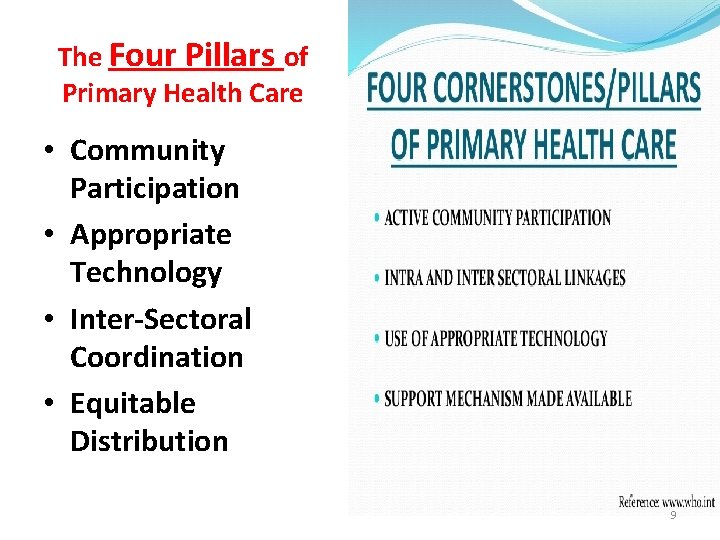
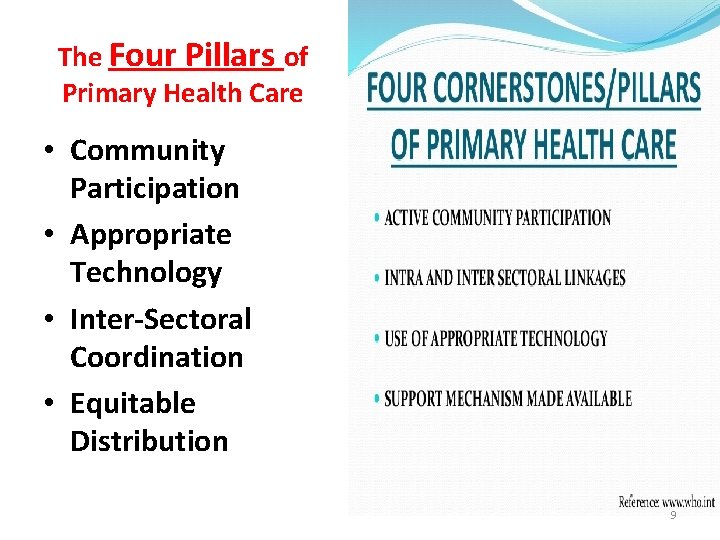
The Four Pillars of Primary Health Care • Community Participation • Appropriate Technology • Inter-Sectoral Coordination • Equitable Distribution 9
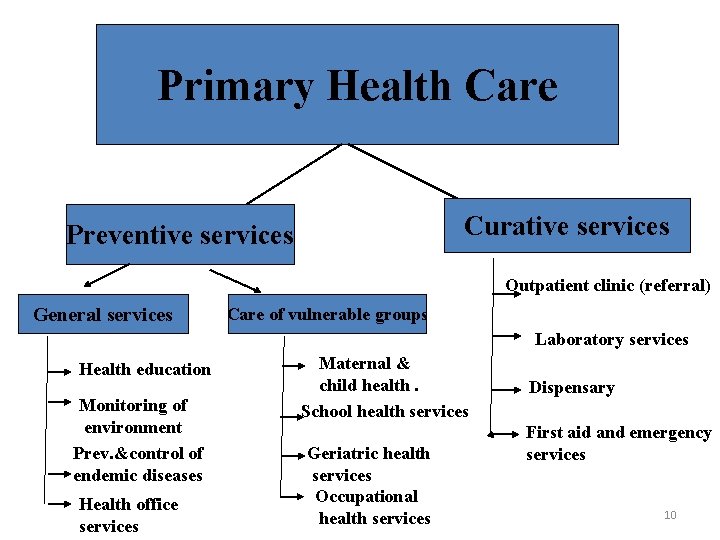
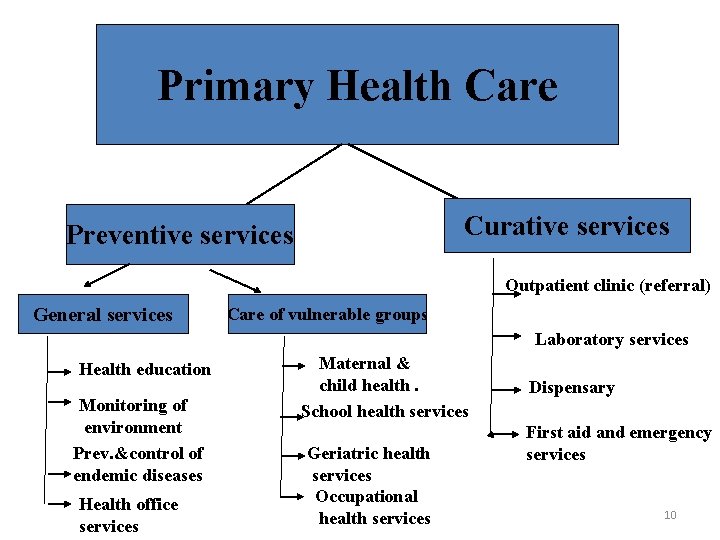
Primary Health Care Curative services Preventive services Outpatient clinic (referral) General services Care of vulnerable groups Laboratory services Health education Monitoring of environment Prev. &control of endemic diseases Health office services Maternal & child health. School health services Geriatric health services Occupational health services Dispensary First aid and emergency services 10
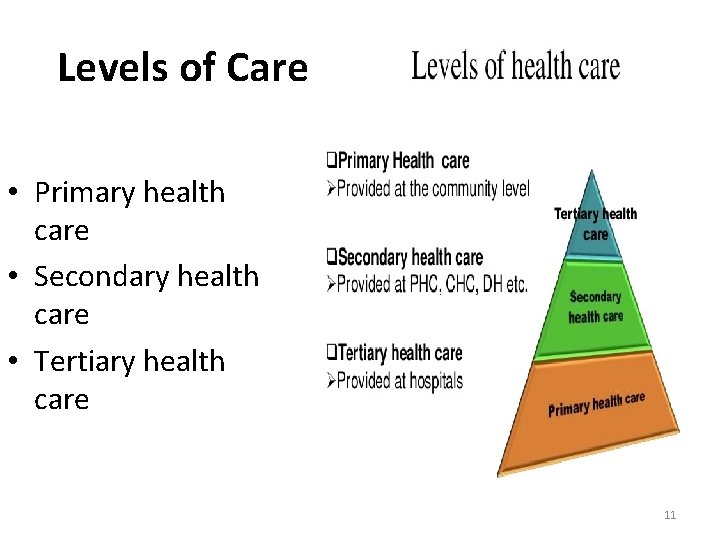
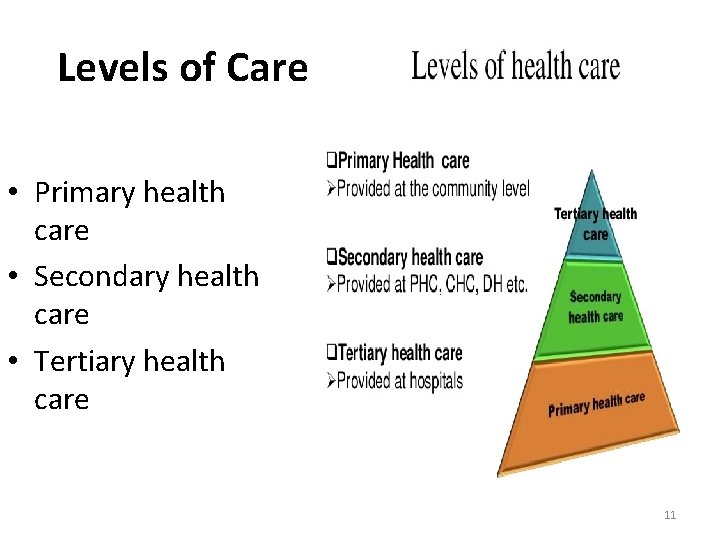
Levels of Care • Primary health care • Secondary health care • Tertiary health care 11
Core Activities for PHC There is a set of CORE ACTIVITIES, which were normally defined nationally or locally. According to the 1978 Declaration of Alma. Ata proposed that these activities should include: 1. Education concerning prevailing health problems and the methods of preventing and controlling them 2. Promotion of food supply and proper nutrition 3. An adequate supply of safe water and basic sanitation 4. Maternal and child health care, including family planning 5. Immunization against the major infectious diseases 6. Prevention and control of locally endemic diseases 7. Appropriate treatment of common diseases and injuries 8. Basic laboratory services and provision of essential drugs. 9. Training of health guides, health workers and health assistants. 12 10. Referral services
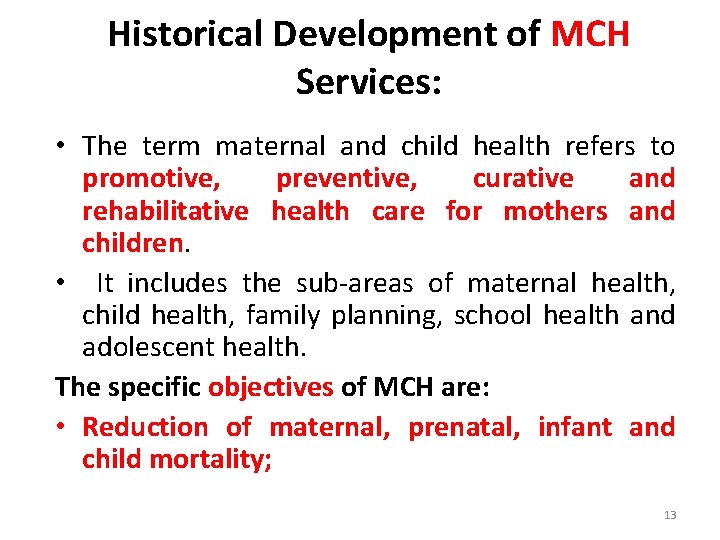
Historical Development of MCH Services: • The term maternal and child health refers to promotive, preventive, curative and rehabilitative health care for mothers and children. • It includes the sub-areas of maternal health, child health, family planning, school health and adolescent health. The specific objectives of MCH are: • Reduction of maternal, prenatal, infant and child mortality; 13
Objective of MCH • To improve the health status of the largest and most vulnerable sector of the population by providing the best health care available. 14
Major Targets of MCH Services – Women of reproductive age group (15 -49 yr) – Pregnant women – Children < 15 yr – Children <1 yr 15
Major component of MCH services Provision of quality ANC, delivery care, PNC, and FP services Prevention of STIs/HIV/AIDS Immunization Growth monitoring Well baby clinic Sick baby clinic Nutrition Rehabilitation Clinic (NRC) Nutrition counseling and health education School health education Adolescent health services 16
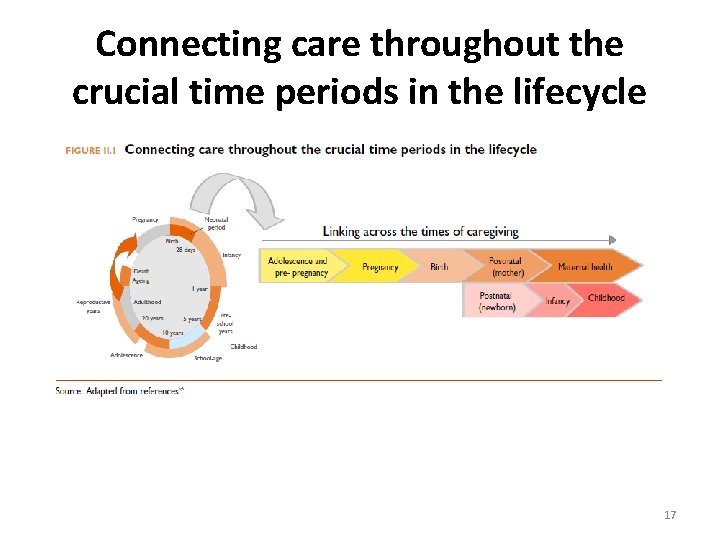
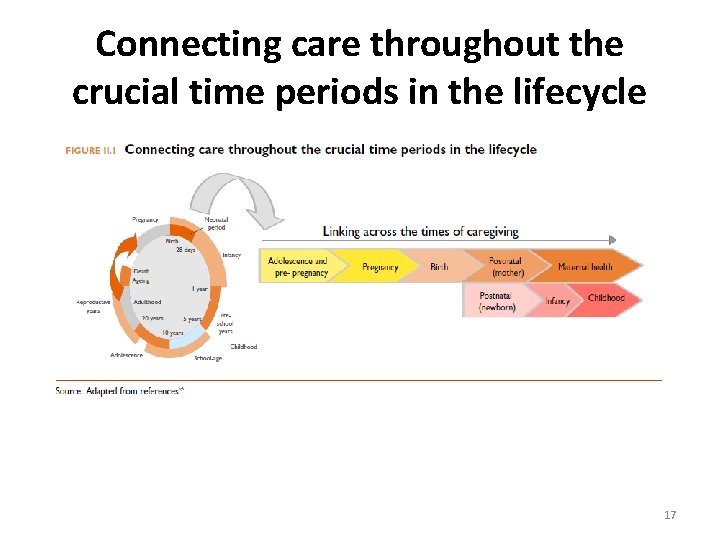
Connecting care throughout the crucial time periods in the lifecycle 17
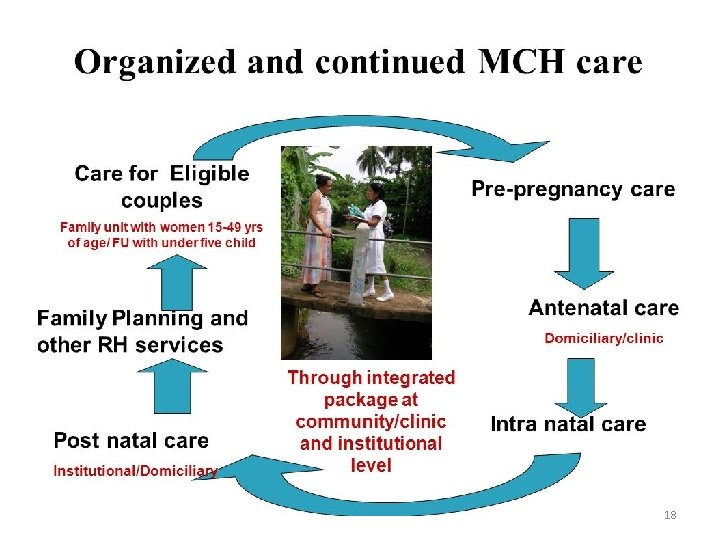
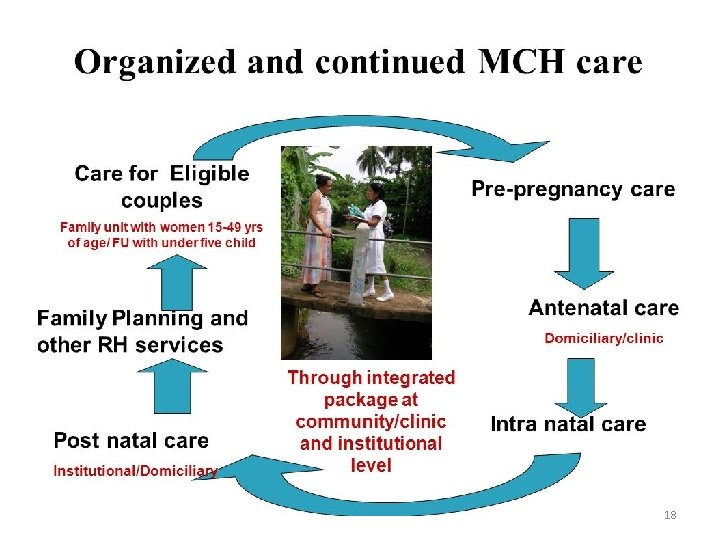
18
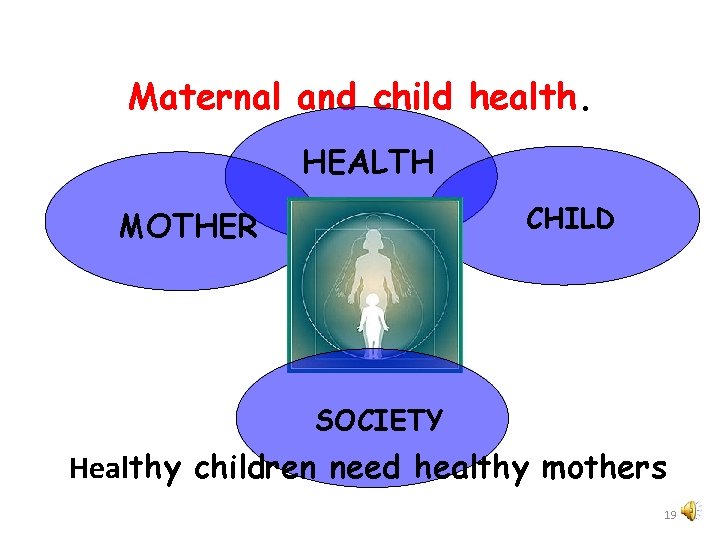
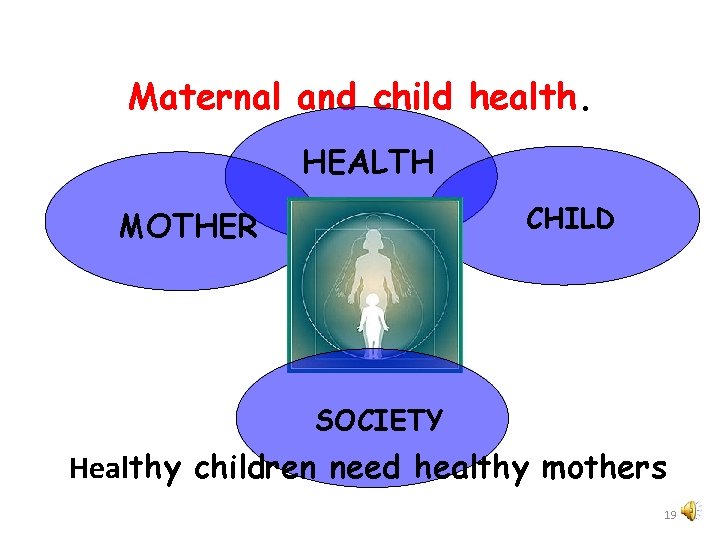
Maternal and child health. HEALTH CHILD MOTHER SOCIETY Healthy children need healthy mothers 19
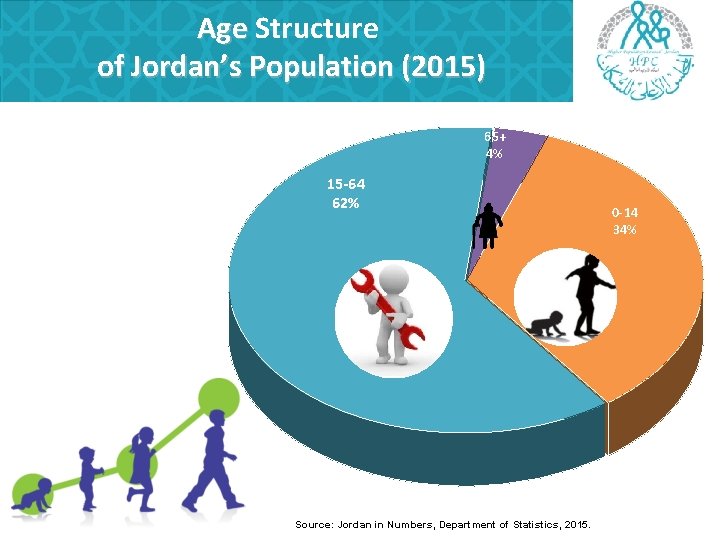
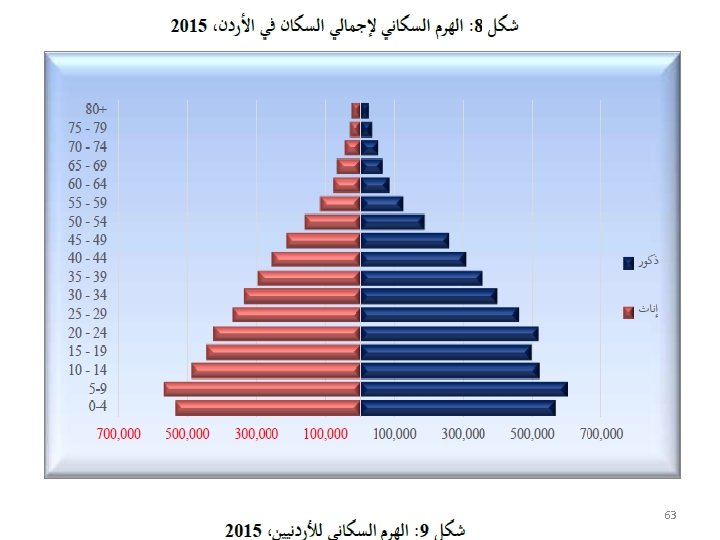
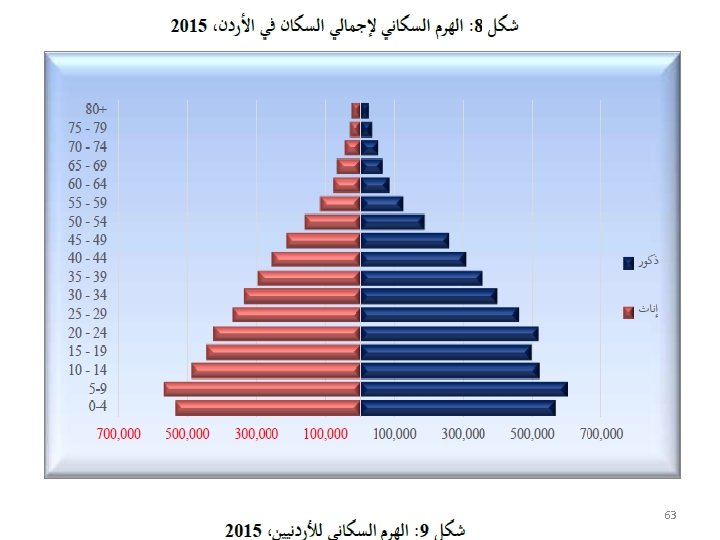
Maternal and Child Health • Mothers and children are both vulnerable groups of the community. • Women in the childbearing period (1549 years) constitute about 25% of the population. • Children on the other hand constitute about 40% to 45% of the population in developing countries. In Jordan ? ? ? • This group is characterized by relative high mortality and morbidity rates. 20
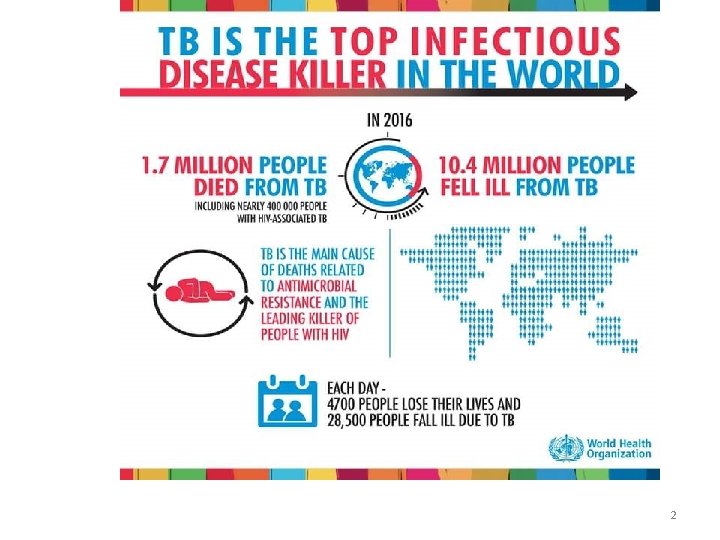
Maternal and child health and disease • Maternal and child health and disease has multi-factor origin and can exist of sequential and continuous form. • Bad maternal conditions account for the fourth leading cause of death for women after HIV/AIDS, malaria, and tuberculosis 21
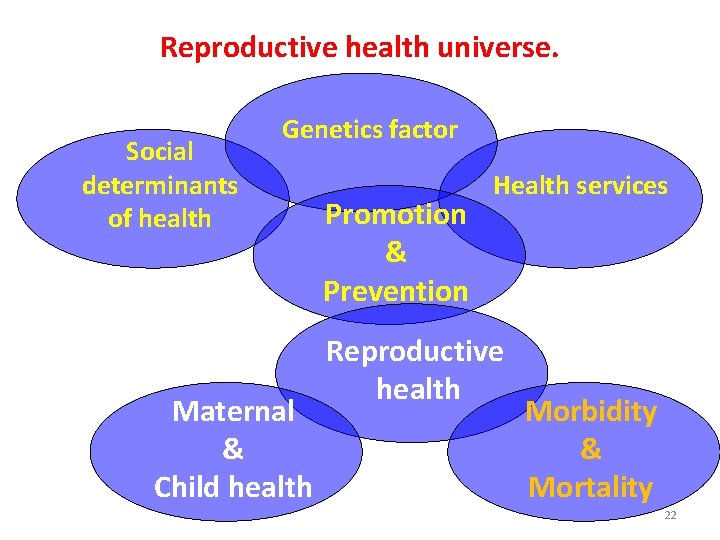
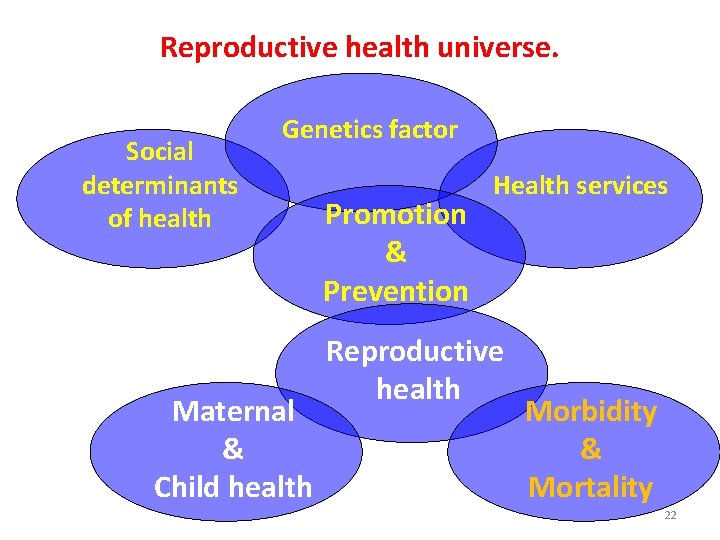
Reproductive health universe. Social determinants of health Genetics factor Maternal & Child health Promotion & Prevention Health services Reproductive health Morbidity & Mortality 22
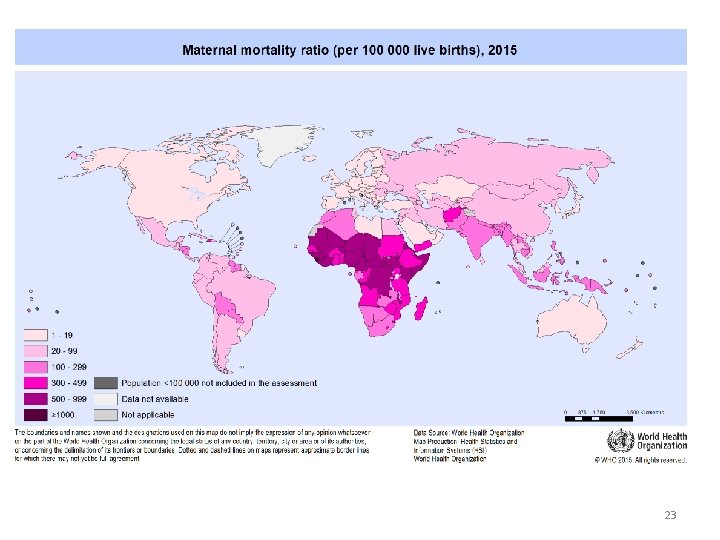
23
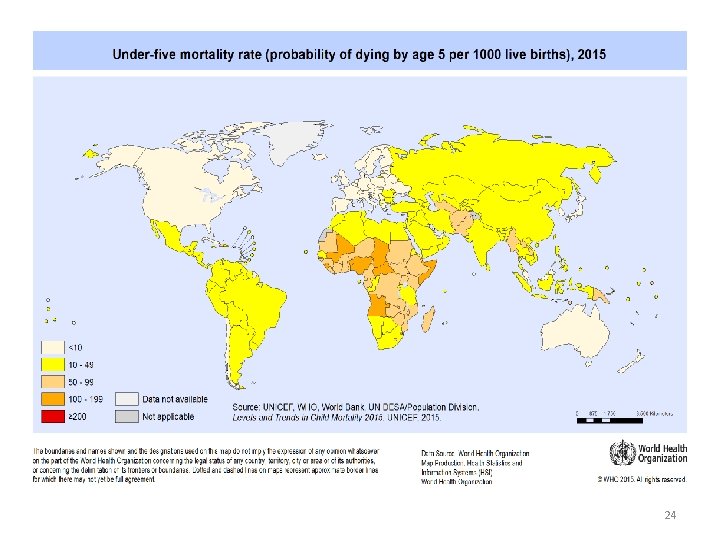
24
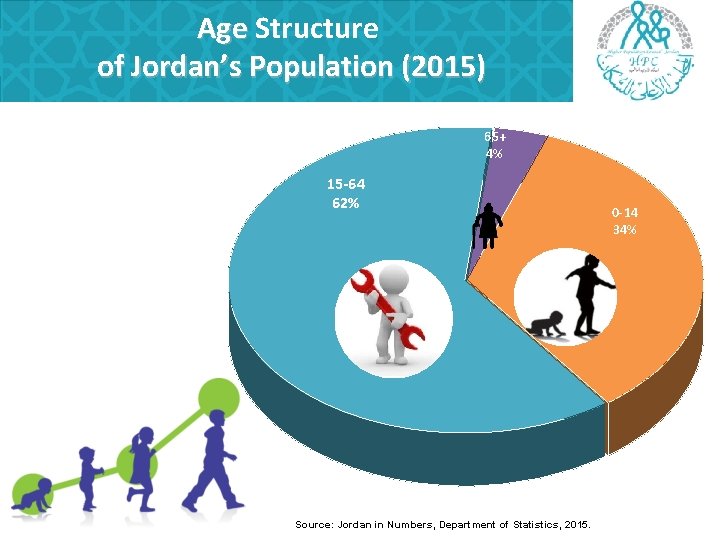
Age Structure of Jordan’s Population (2015) 65+ 4% 15 -64 62% Source: Jordan in Numbers, Department of Statistics, 2015. 0 -14 34%
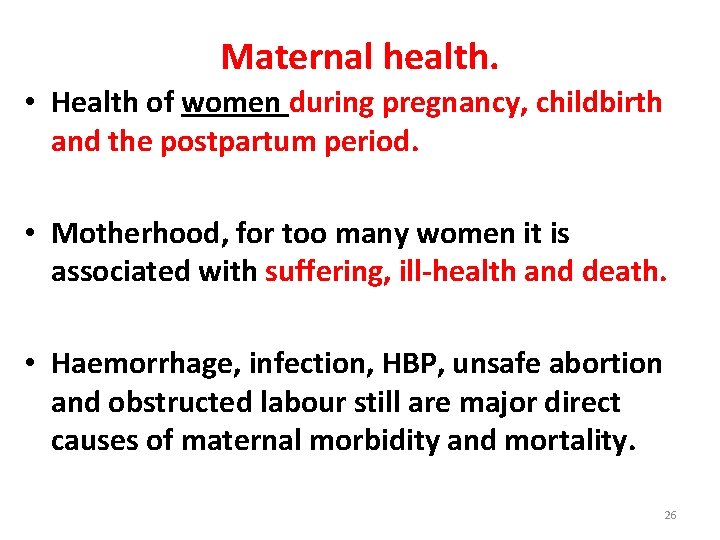
Maternal health. • Health of women during pregnancy, childbirth and the postpartum period. • Motherhood, for too many women it is associated with suffering, ill-health and death. • Haemorrhage, infection, HBP, unsafe abortion and obstructed labour still are major direct causes of maternal morbidity and mortality. 26
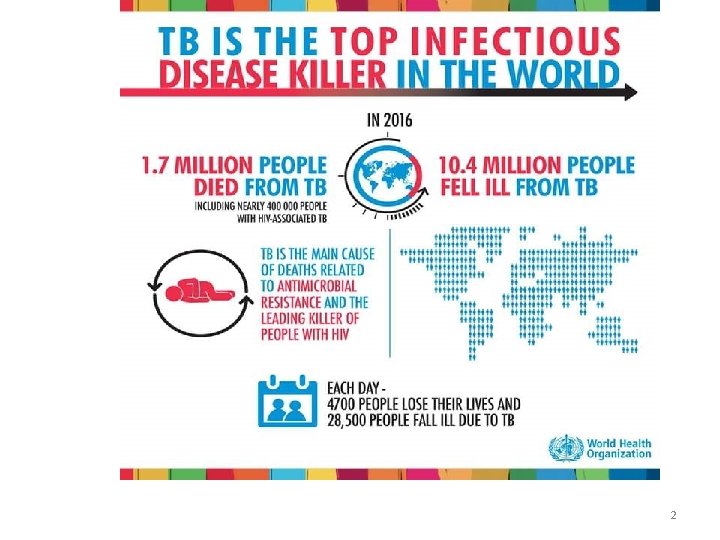
Some emerging and reemerging problems to M & Ch Health. • • HIV/AIDS and TB plus Multirresistant TB. Dengue. Others viral haemorragic fever. Old neglected diseases with new burden. Cholera outbreaks in Africa and Asia. Avian and swyne flu. Conflicts, war and infraestructure destruction. Bad governance and uneffective polices. 27
Maternal health care. • Is a concept that encompasses family planning, preconception, prenatal, and posnatal care. • Goals of preconception care can include providing education, health promotion, screening and interventions for women of reproductive age to reduce risk factors that might affect future pregnancies. 28
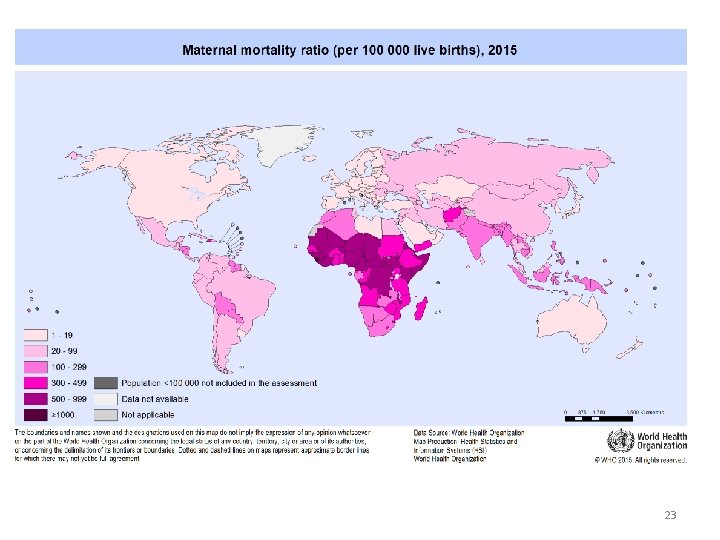
According to 2015 WHO estimations it was concluded that: • Maternal mortality is unacceptably high. About 830 women die from pregnancy- or childbirth-related complications around the world every day. • It was estimated that in 2015, roughly 303 000 women died during and following pregnancy and childbirth. • Almost all of these deaths occurred in lowresource settings, and most could have been prevented 29
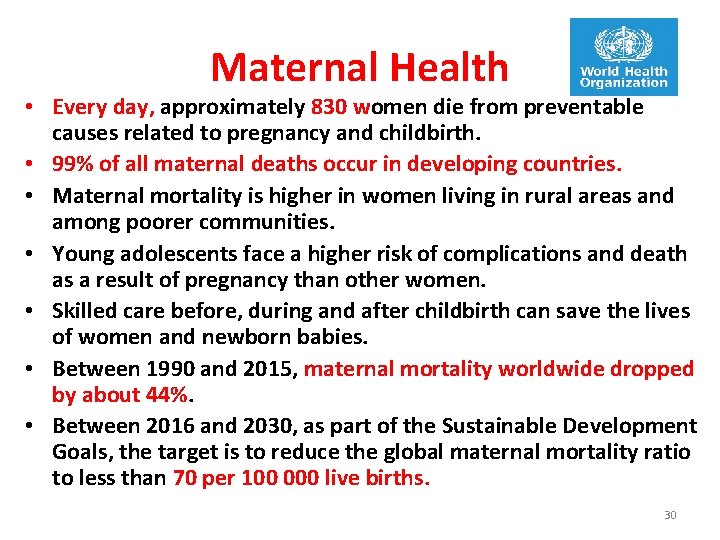
Maternal Health • Every day, approximately 830 women die from preventable causes related to pregnancy and childbirth. • 99% of all maternal deaths occur in developing countries. • Maternal mortality is higher in women living in rural areas and among poorer communities. • Young adolescents face a higher risk of complications and death as a result of pregnancy than other women. • Skilled care before, during and after childbirth can save the lives of women and newborn babies. • Between 1990 and 2015, maternal mortality worldwide dropped by about 44%. • Between 2016 and 2030, as part of the Sustainable Development Goals, the target is to reduce the global maternal mortality ratio to less than 70 per 100 000 live births. 30
The major cause of MM includes • Direct cause – are these disease or complications occur only during pregnancy and child birth e. g. , • Hemorrhage – 25% Sepsis – 15% • Unsafe abortion – 13% • Hypertensive disorder – 12% Obstructed labor – 8% • Other – 8% • Indirect cause – are these which are pre-existing disease but aggravated by pregnancy. 31
Ex- Anemia • Heart disease • - Essential HTN / 20% MM – DM – Kidney disease • Coincidental causes – are not related to pregnancy • Ex – Death from traffic accident 32
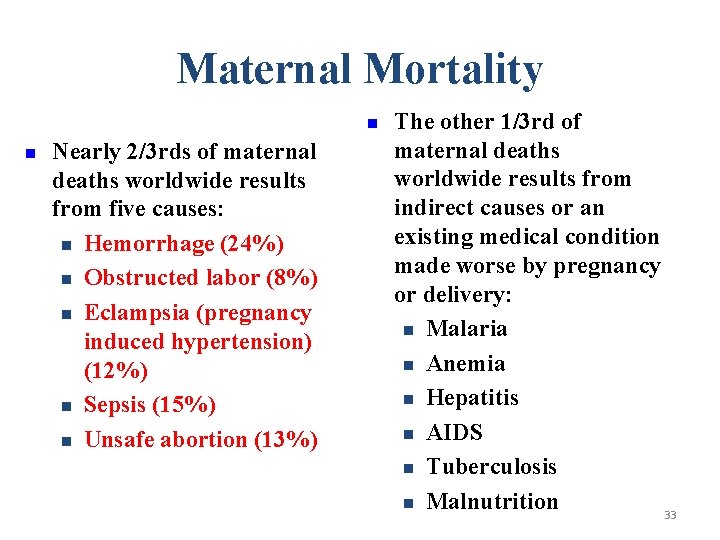
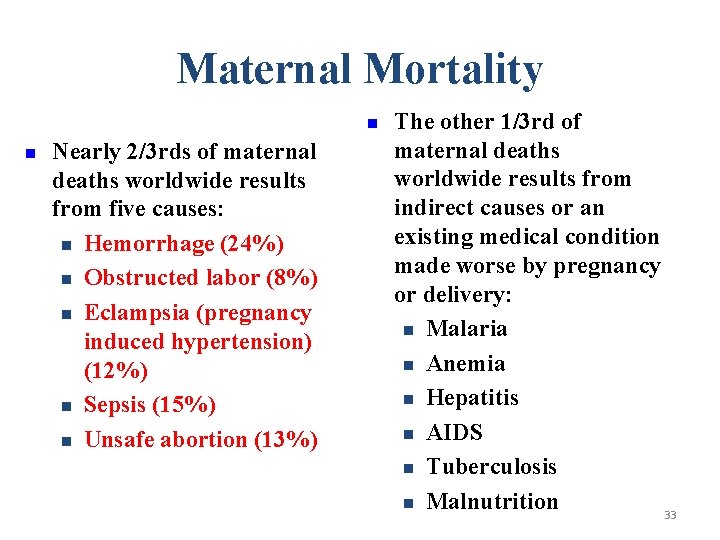
Maternal Mortality n n Nearly 2/3 rds of maternal deaths worldwide results from five causes: n Hemorrhage (24%) n Obstructed labor (8%) n Eclampsia (pregnancy induced hypertension) (12%) n Sepsis (15%) n Unsafe abortion (13%) The other 1/3 rd of maternal deaths worldwide results from indirect causes or an existing medical condition made worse by pregnancy or delivery: n Malaria n Anemia n Hepatitis n AIDS n Tuberculosis n Malnutrition 33
Why do women die? • Women die as a result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy and most are preventable or treatable. Other complications may exist before pregnancy but are worsened during pregnancy, especially if not managed as part of the woman’s care. The major complications that account for nearly 75% of all maternal deaths are: • severe bleeding (mostly bleeding after childbirth) • infections (usually after childbirth) • high blood pressure during pregnancy (pre-eclampsia and eclampsia) • complications from delivery 34 • unsafe abortion.
Some Factors that Contribute to Maternal Mortality and Morbidity • The 4 “too”s of pregnancy: – Too young – Too old – Too many – Too soon • In other words: young or old age of pregnancy, short intervals between pregnancies, and high parity. • Other factors include low socio-economic status and inadequate maternal care. 35
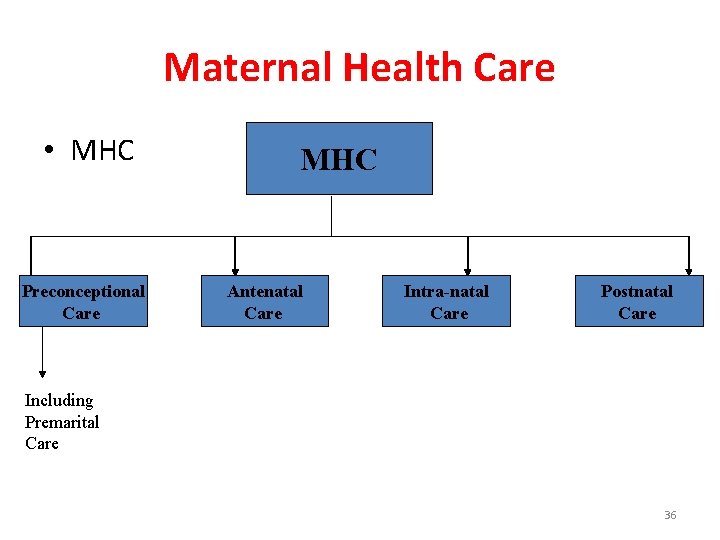
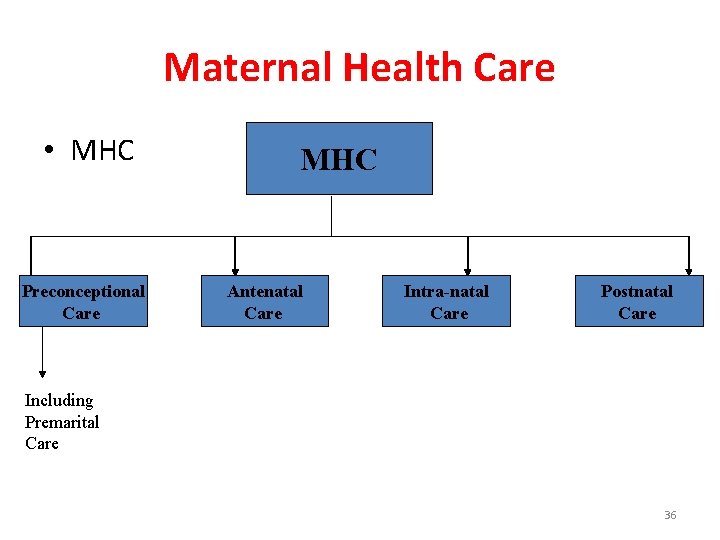
Maternal Health Care • MHC Preconceptional Care MHC Antenatal Care Intra-natal Care Postnatal Care Including Premarital Care 36
Preconception Care • It is a care of female before conception. • It is continued care from birth, through stages of growth and development, and until the time of conception and pregnancy, so as to prepare the female for normal child bearing and delivery in the future. 37
Components of Preconceptional Care: • Health promotion and prevention of health hazards specially those of particular risk to pregnancy. • Regular health appraisal for early case detection and management, and prevention of sequelae or complications. • Health education of young girls e. g. determinants and requirement of health, family planning…. . • Premarital care (for both partners). 38
Premarital Care It includes: • Premarital counseling • Premarital immunization • Premarital examination: • • History taking Genetic counseling Systemic medical examination Investigations 39
Antenatal (Prenatal) Care • General objective: • “ The general objective of antenatal (prenatal) care is to prepare the mother both physically and psychologically to give birth to a healthy newborn (favorable outcome of pregnancy) and to be able to care for it. ” 40
Components Antenatal (Prenatal) Care • Registration: During the booking visit, and record keeping • Medical examination and investigations; for both the booking visit and continuing visits. • Health education • Immunization • Supplementations • Clinical services • Social services (outreach services). 41
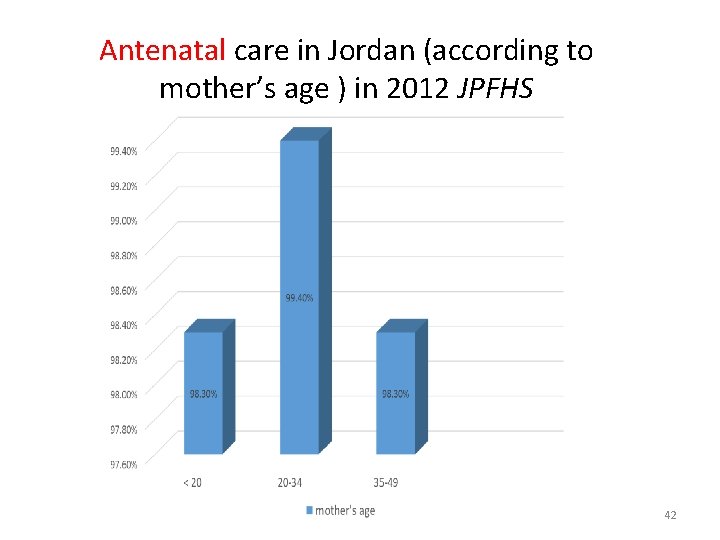
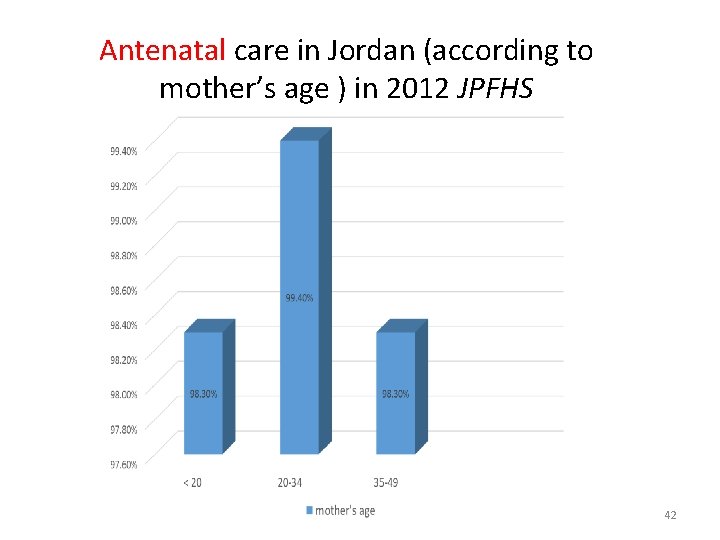
Antenatal care in Jordan (according to mother’s age ) in 2012 JPFHS 42
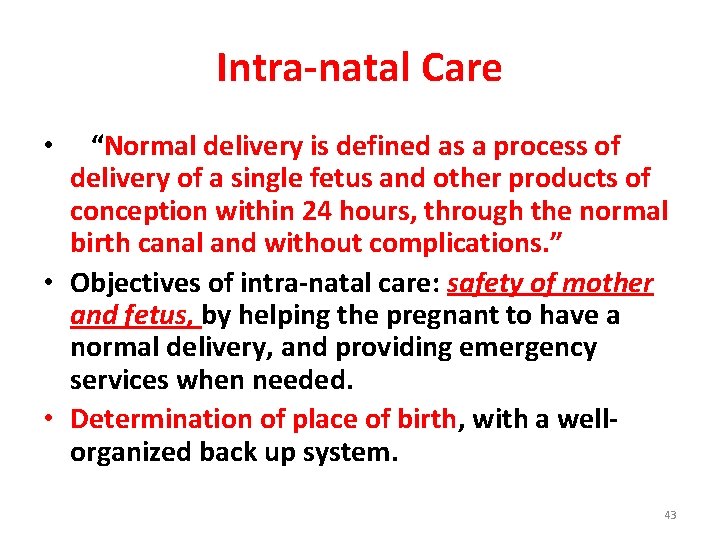
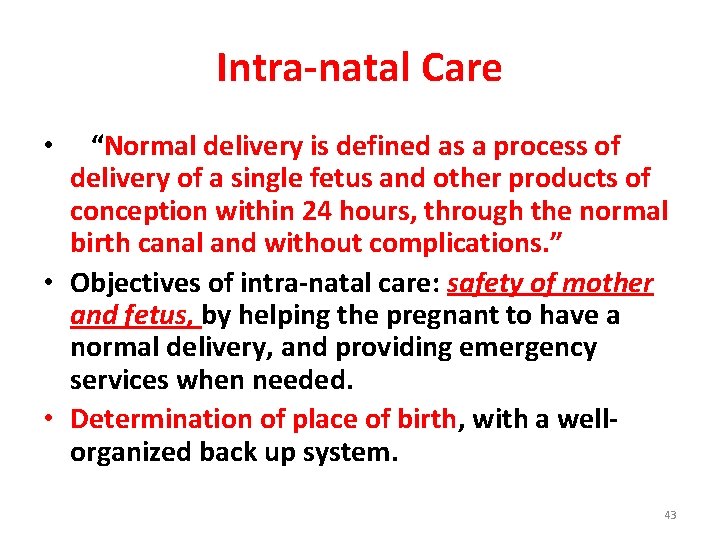
Intra-natal Care “Normal delivery is defined as a process of delivery of a single fetus and other products of conception within 24 hours, through the normal birth canal and without complications. ” • Objectives of intra-natal care: safety of mother and fetus, by helping the pregnant to have a normal delivery, and providing emergency services when needed. • Determination of place of birth, with a wellorganized back up system. • 43
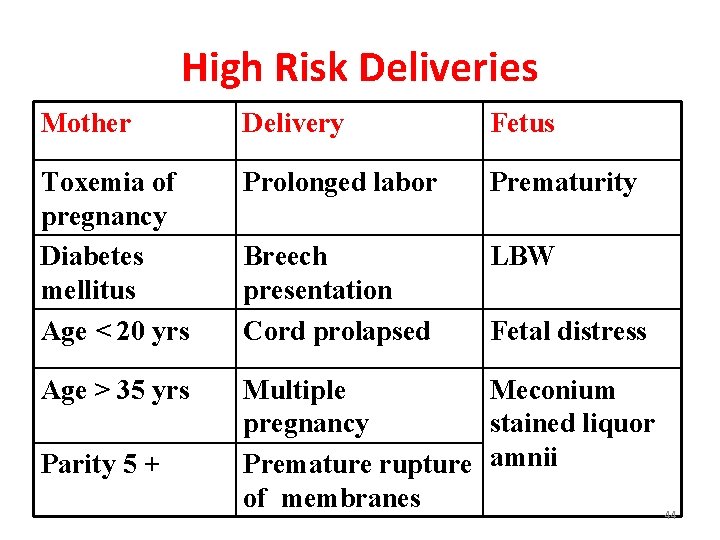
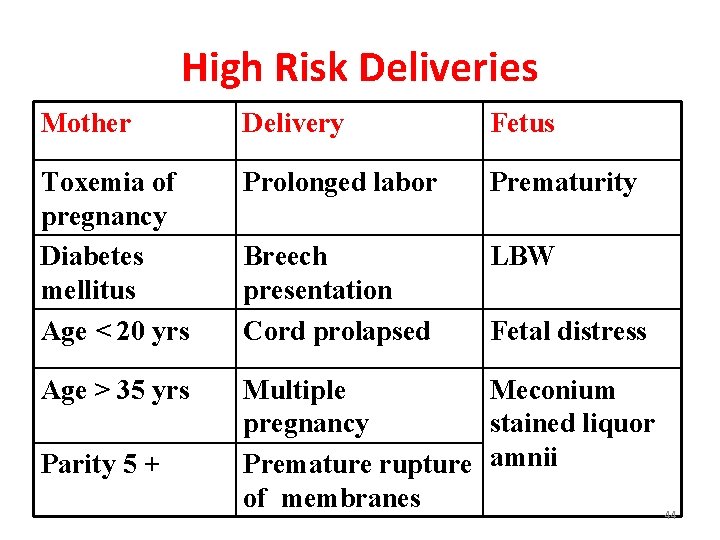
High Risk Deliveries Mother Delivery Fetus Toxemia of pregnancy Diabetes mellitus Age < 20 yrs Prolonged labor Prematurity Breech presentation Cord prolapsed LBW Age > 35 yrs Multiple Meconium pregnancy stained liquor Premature rupture amnii of membranes Parity 5 + Fetal distress 44
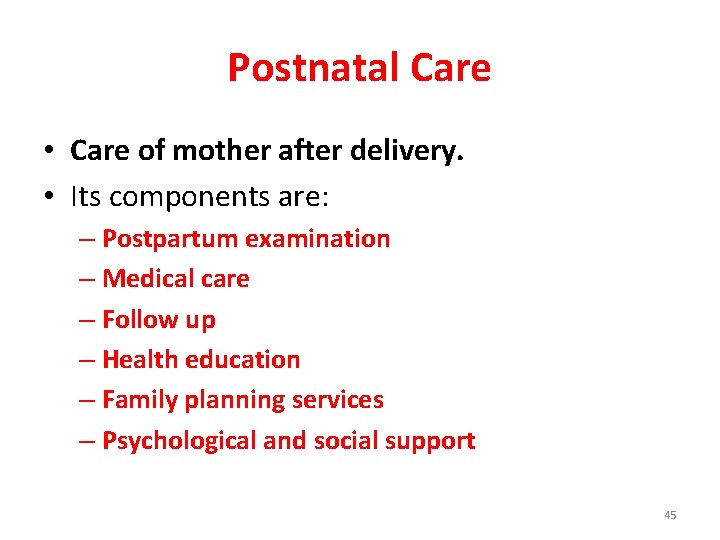
Postnatal Care • Care of mother after delivery. • Its components are: – Postpartum examination – Medical care – Follow up – Health education – Family planning services – Psychological and social support 45

46
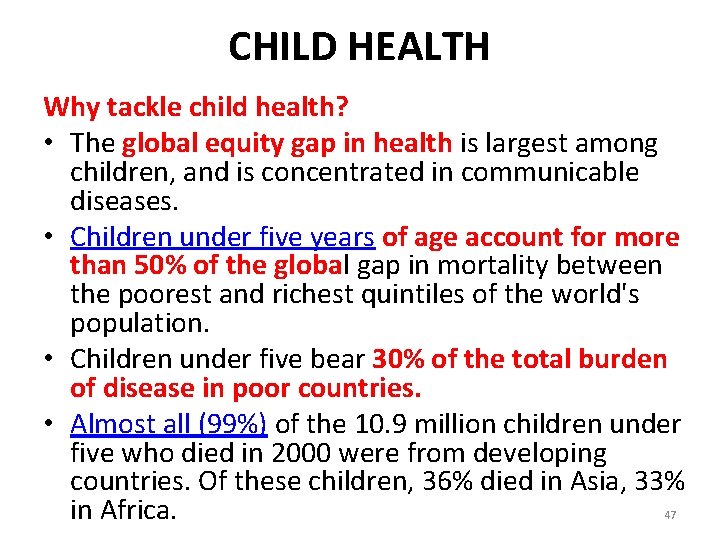
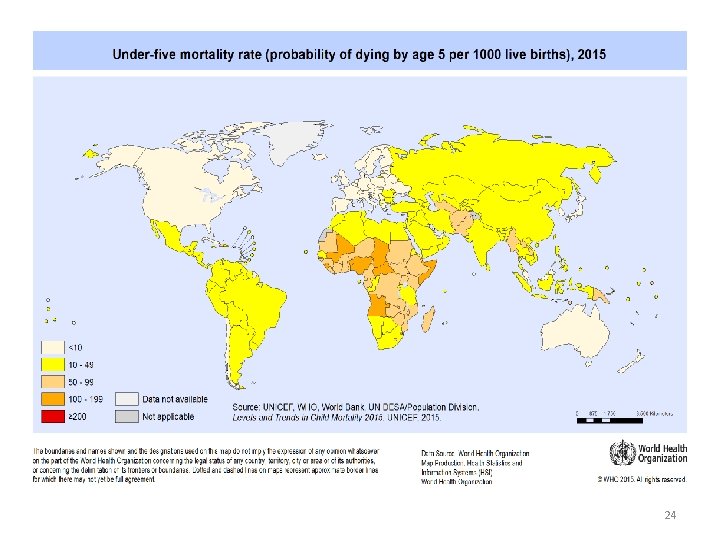
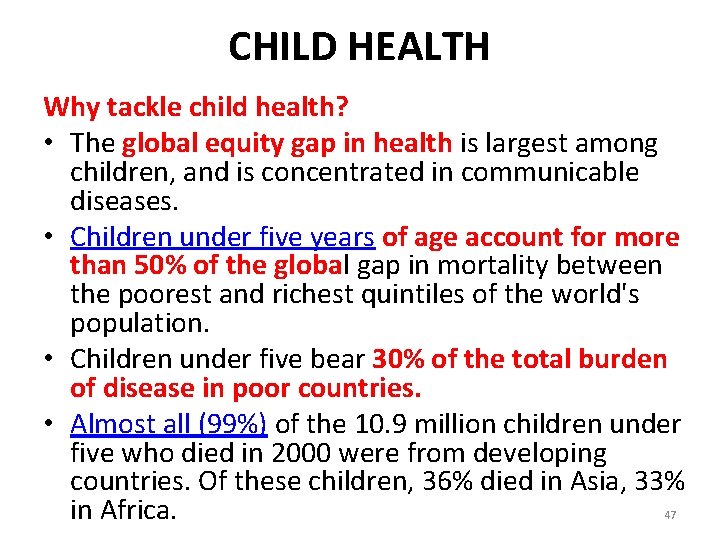
CHILD HEALTH Why tackle child health? • The global equity gap in health is largest among children, and is concentrated in communicable diseases. • Children under five years of age account for more than 50% of the global gap in mortality between the poorest and richest quintiles of the world's population. • Children under five bear 30% of the total burden of disease in poor countries. • Almost all (99%) of the 10. 9 million children under five who died in 2000 were from developing countries. Of these children, 36% died in Asia, 33% in Africa. 47
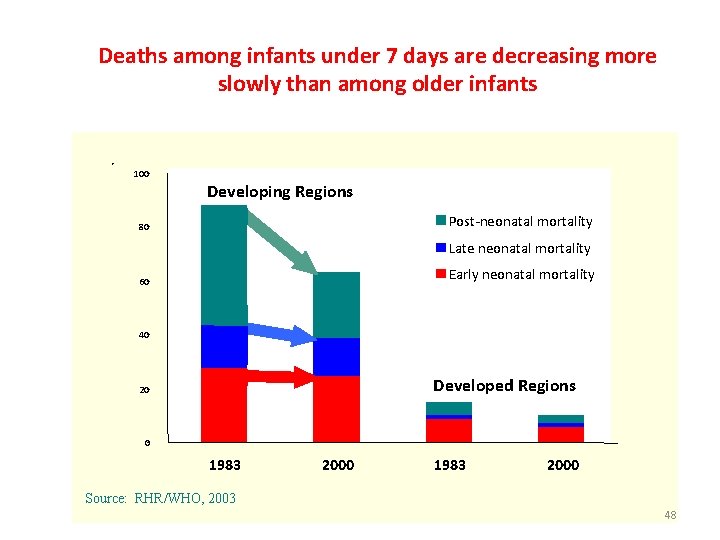
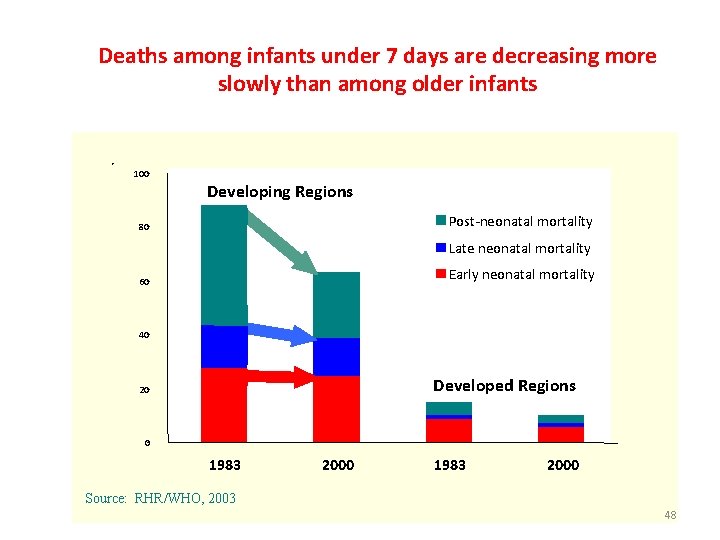
Deaths among infants under 7 days are decreasing more slowly than among older infants 100 Developing Regions Post-neonatal mortality 80 Late neonatal mortality Early neonatal mortality 60 40 Developed Regions 20 0 1983 2000 Source: RHR/WHO, 2003 48
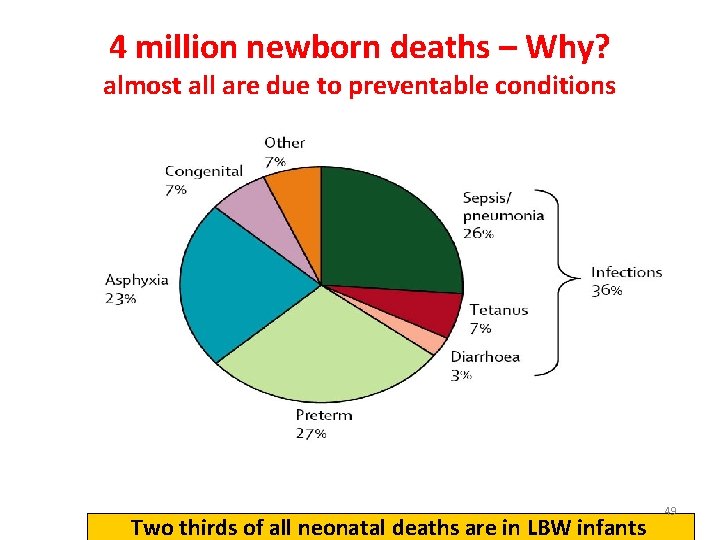
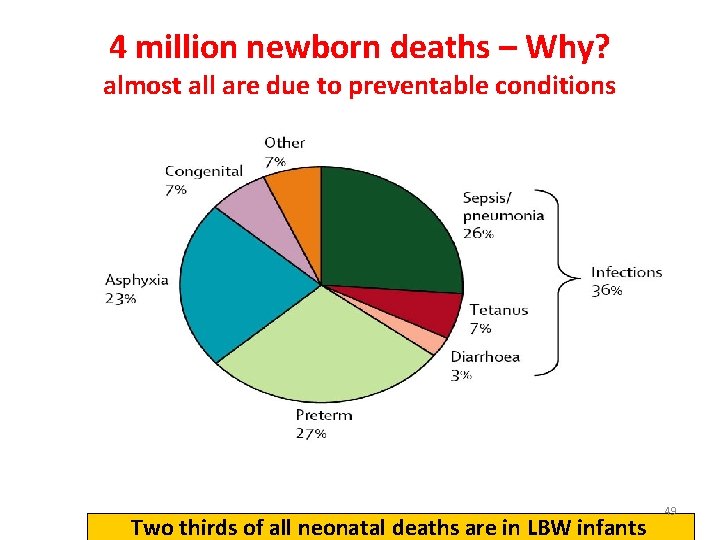
4 million newborn deaths – Why? almost all are due to preventable conditions Two thirds of all neonatal deaths are in LBW infants 49
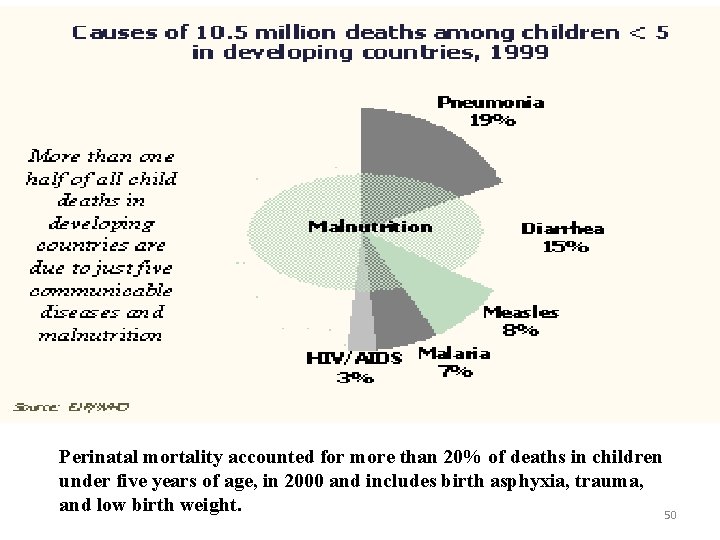
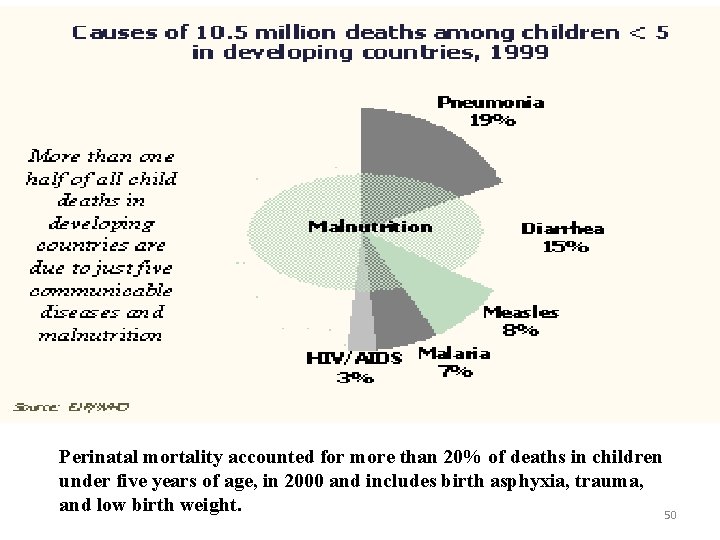
Perinatal mortality accounted for more than 20% of deaths in children under five years of age, in 2000 and includes birth asphyxia, trauma, and low birth weight. 50
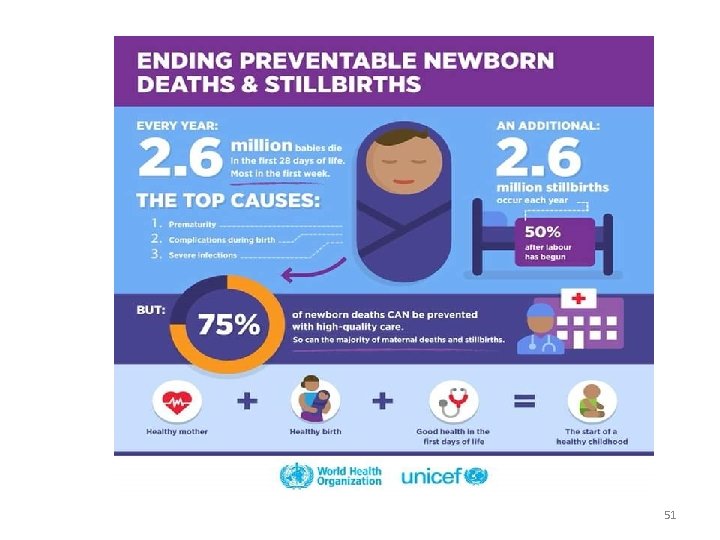
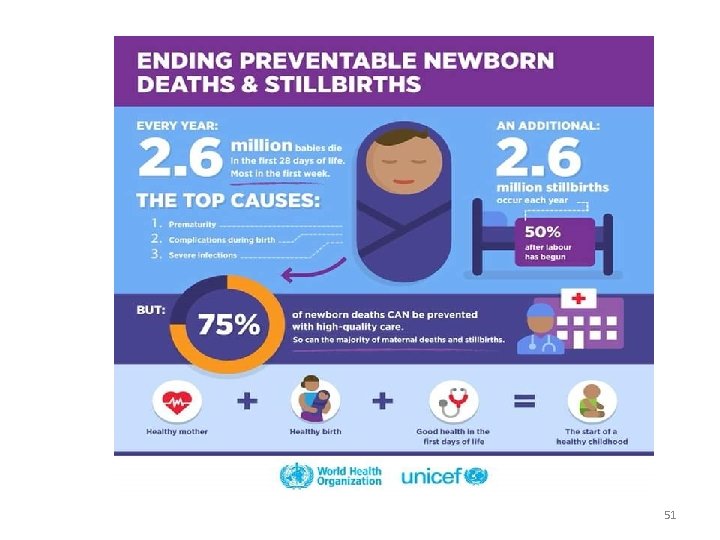
51

• What can be done to improve child health? 52
Infant and child priorities (UNICEF) • • Reduction of infant and under 5 mortality rate Reduction of moderate and severe malnutrition Universal access to safe drinking water Access to all couples to information and services to prevent pregnancies that are too early, too closely spaced, too late or too many. 53
Infant and child priorities (UNICEF) cont. • • Reduction of low birth weight babies Elimination of iodine deficiency Elimination of vitamin A deficiency Encouragement of women to breast feed their children exclusively Growth promotion and monitoring Eradication of poliomyelitis Elimination of neonatal tetanus Reduction of measles death 54
Infant and child priorities (UNICEF) cont. • Maintenance of a high level of immunization coverage. • Reduction of deaths due to diarrheal diseases • Reduction of deaths due to ARIs • Increased acquisition of knowledge, skills and values required for better living by all families. 55
The Integrated Management of Childhood Illness (IMCI) • IMCI is a broad strategy to improve child health outcomes developed by WHO and UNICEF. IMCI encompasses interventions at home, in the community and in the health system. • The aims are to reduce childhood deaths, illnesses, and disability and to improve children's growth and development, with a particular focus on the poorest and most disadvantaged children. IMCI has three main components: – Improve family and community practices related to child health and nutrition; – Improve the health system for effective management of childhood illness; – Improve health workers' skills. 56
Improve family and community practices related to child health and nutrition; • Counseling on child feeding including – exclusive breast feeding – Adequate amount of micronutrient or supplementation • Complete full course of immunization for children • Promote safe disposal of waste and hand washing before preparing meals and feeding children • Provide adequate care to sick children • Promote mental and social development by responding to children's needs for care, • Provide adequate prenatal care to every pregnant woman 57
Improve the health system for effective management of childhood illness; • Ensure drugs and supplies for treating major childhood illnesses are available in health facilities • Improve quality of care provided at health facilities and organization of work • Improve referral pathways • Identify and develop methods for sustainable financing and equity of access 58
Improve health workers' skills. • Develop and adapt case management guidelines and standards for major childhood illnesses in the country • Train health providers at first level health facilities and referral level in standard case management • Improve and maintain health workers' performance through follow-up after training and periodic supervision 59
• A combination of integrated curative and preventive interventions is required to address the immediate and underlying determinants of child health. Maternal determinants and risk factors associated with pregnancy and childbirth are especially important. • Simple, cost-effective interventions delivered at the community level can save most newborn and children lives in developing countries. 60
To summarize Optimum child health is achieved through: • Adequate maternal care • Periodic follow up of the “healthy child” • Breast feeding and proper child nutrition • Immunization • Early detection and proper management • A sanitary and safe environment • Health education of parents. 61

Family Planning In Jordan 62
63
Background • Family planning allows people to • attain their desired number of children • and determine the spacing of pregnancies. • It is achieved through use of contraceptive methods and the treatment of infertility 64
Background • An estimated 222 million women in developing countries would like to delay or stop childbearing but not using any contraception method • Reasons for this include: • limited choice of methods; limited access to contraception, particularly among young people, poorer segments of populations, or unmarried people • fear or experience of side-effects; • cultural or religious opposition; • poor quality of available services; • gender-based barriers. 65
Benefits of family planning Preventing pregnancy-related health risks in women • Family planning allows spacing of pregnancies and can delay pregnancies in young women at increased risk of health problems and death from early childbearing, and can prevent pregnancies among older women who also face increased risks. • Family planning enables women who wish to limit the size of their families to do so. Evidence suggests that women who have more than four children are at increased risk of maternal mortality. • By reducing rates of unintended pregnancies, family planning also reduces the need for unsafe abortion 66
Benefits of family planning Reducing infant mortality • Family planning can prevent closely spaced and ill-timed pregnancies and births, which contribute to some of the world’s highest infant mortality rates. Helping to prevent HIV/AIDS • Family planning reduces the risk of unintended pregnancies among women living with HIV, resulting in fewer infected babies and orphans. 67
Benefits of family planning Empowering people and enhancing education • Family planning enables people to make informed choices about their sexual and reproductive health. • Family planning represents an opportunity for women for enhanced education and participation in public life, including paid employment in non-family organizations. • Additionally, having smaller families allows parents to invest more in each child. Children with fewer siblings tend to stay in school longer than those with many siblings. 68
Benefits of family planning Reducing adolescent pregnancies • Pregnant adolescents are more likely to have preterm or low birth-weight babies. Babies born to adolescents have higher rates of neonatal mortality. Slowing population growth • Family planning is key to slowing unsustainable population growth and the resulting negative impacts on the economy, environment, and national and regional development efforts. 69
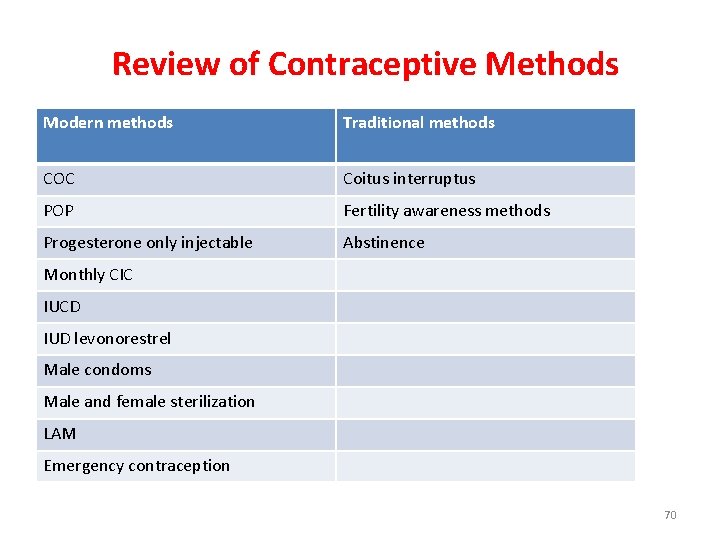
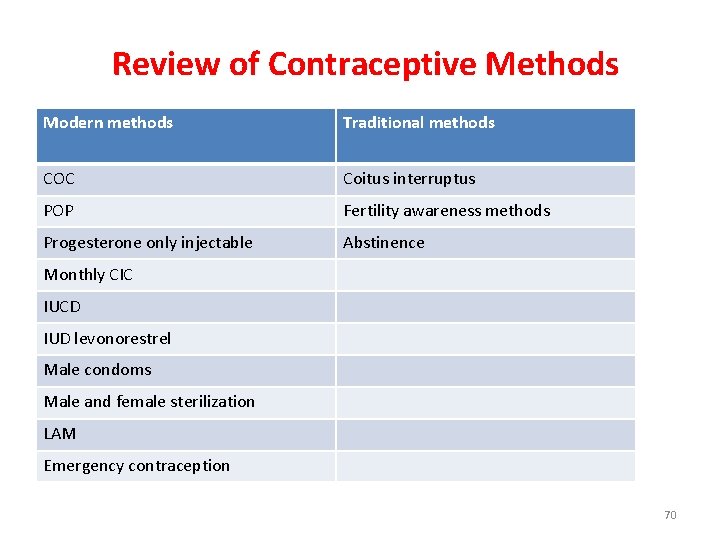
Review of Contraceptive Methods Modern methods Traditional methods COC Coitus interruptus POP Fertility awareness methods Progesterone only injectable Abstinence Monthly CIC IUCD IUD levonorestrel Male condoms Male and female sterilization LAM Emergency contraception 70
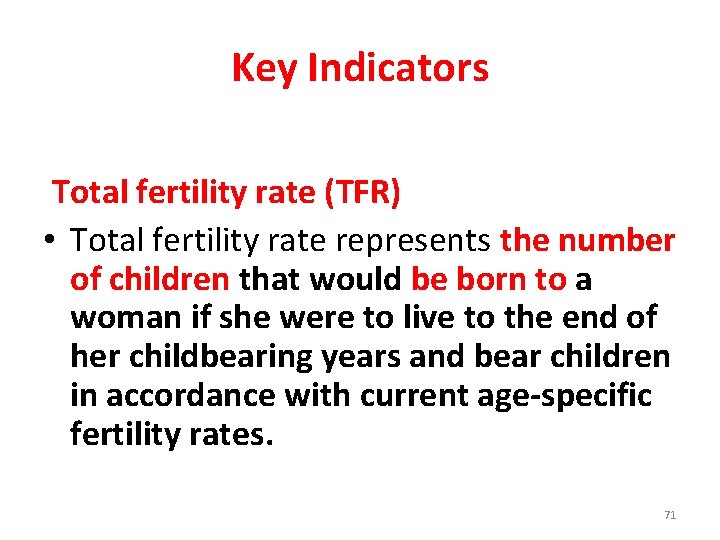
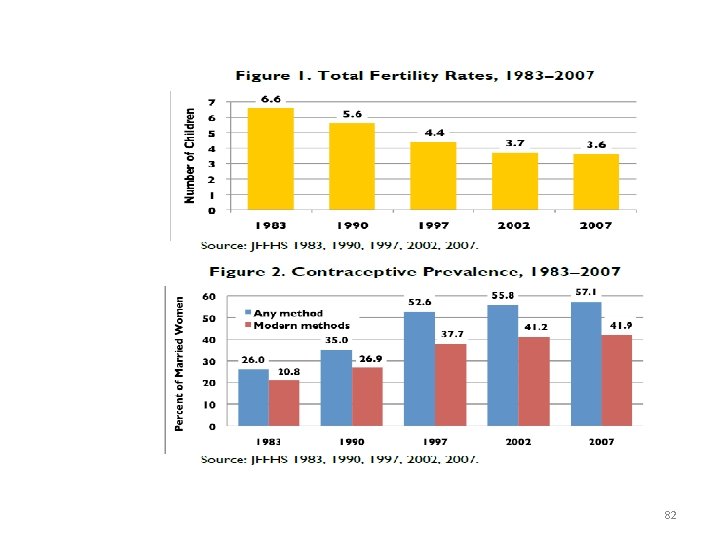
Key Indicators Total fertility rate (TFR) • Total fertility rate represents the number of children that would be born to a woman if she were to live to the end of her childbearing years and bear children in accordance with current age-specific fertility rates. 71
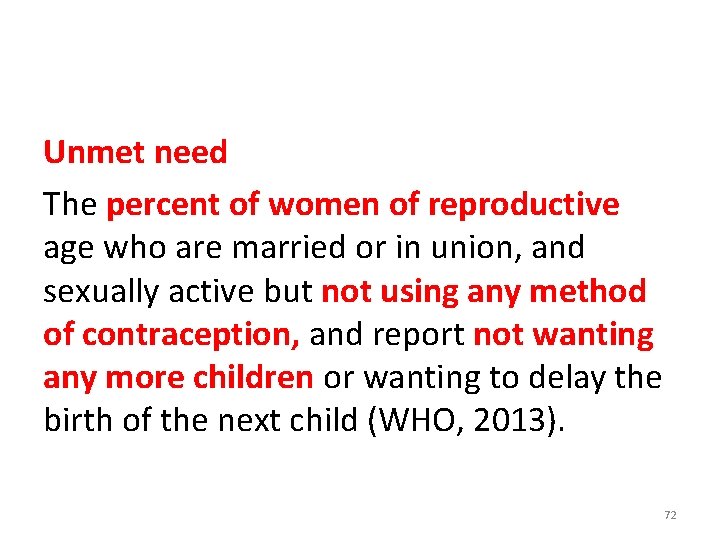
Unmet need The percent of women of reproductive age who are married or in union, and sexually active but not using any method of contraception, and report not wanting any more children or wanting to delay the birth of the next child (WHO, 2013). 72
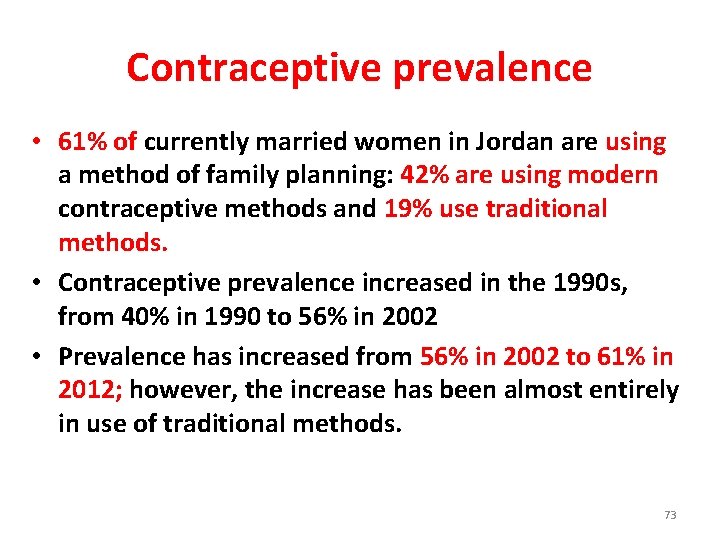
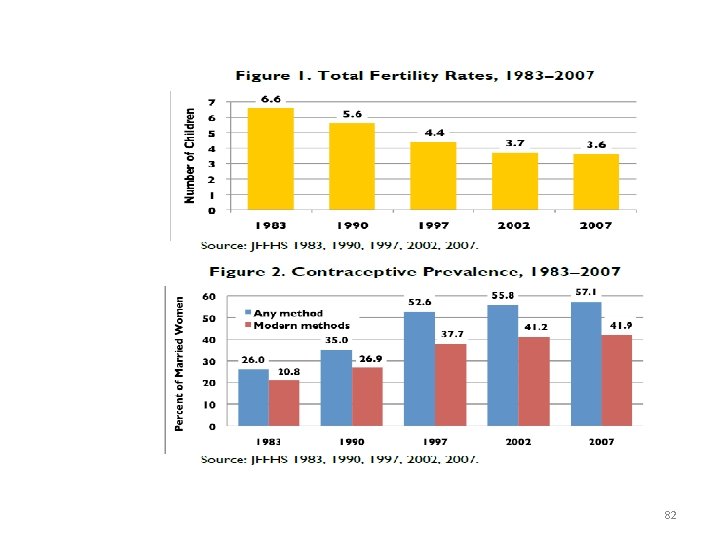
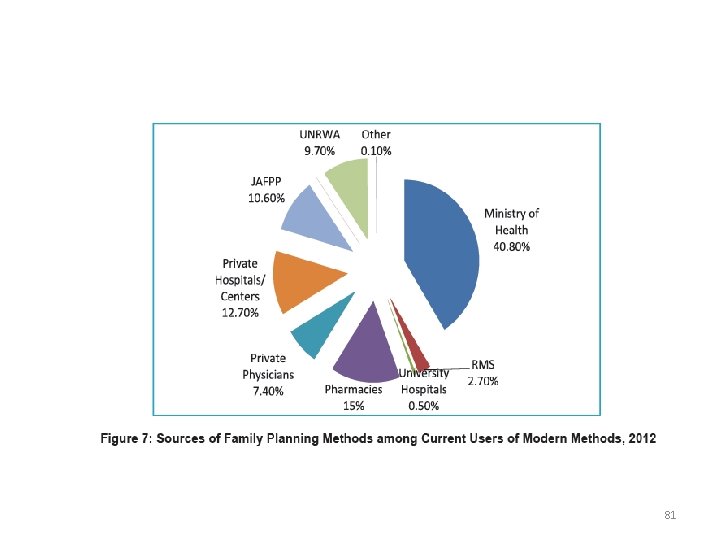
Contraceptive prevalence • 61% of currently married women in Jordan are using a method of family planning: 42% are using modern contraceptive methods and 19% use traditional methods. • Contraceptive prevalence increased in the 1990 s, from 40% in 1990 to 56% in 2002 • Prevalence has increased from 56% in 2002 to 61% in 2012; however, the increase has been almost entirely in use of traditional methods. 73
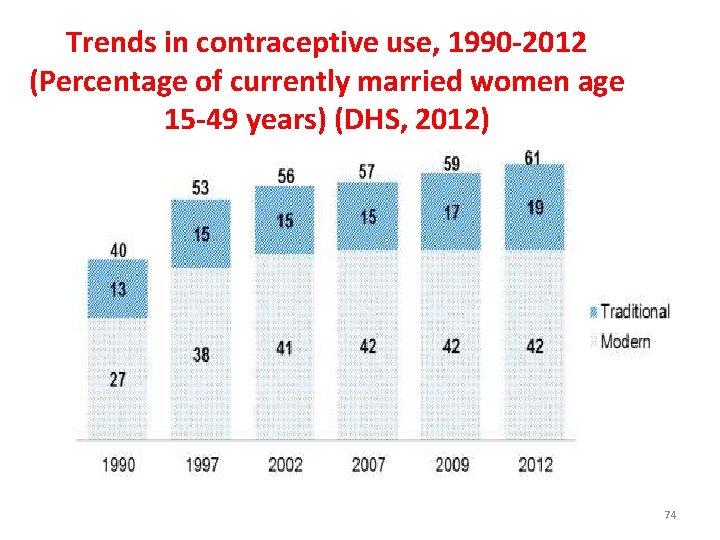
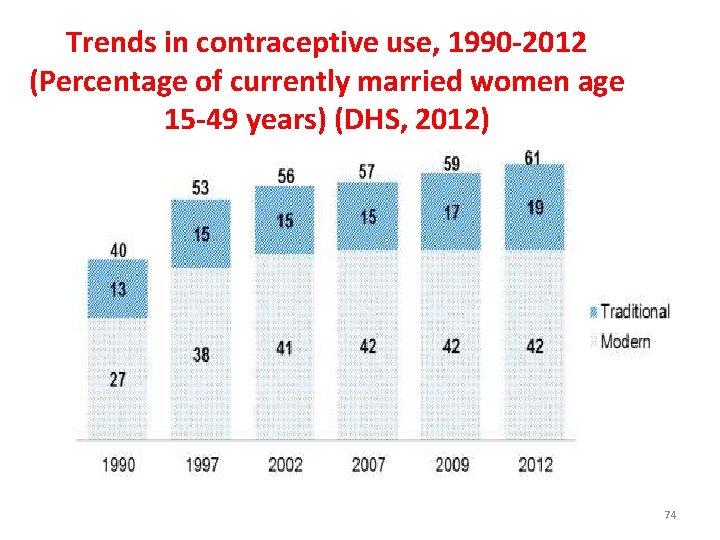
Trends in contraceptive use, 1990 -2012 (Percentage of currently married women age 15 -49 years) (DHS, 2012) 74
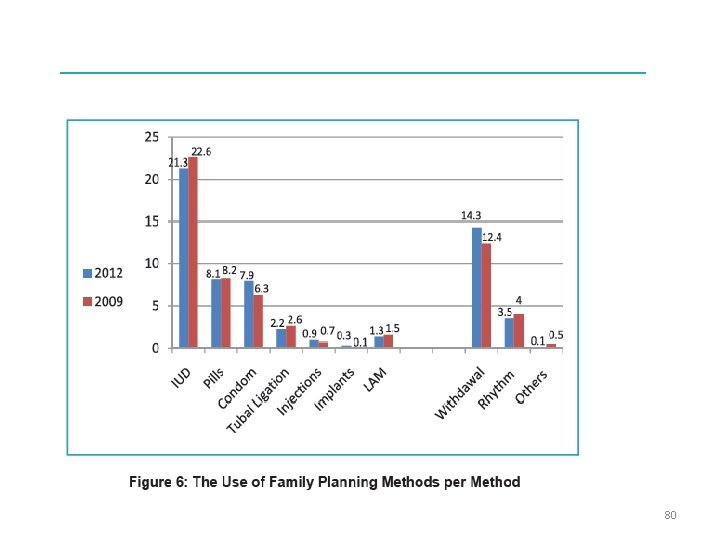
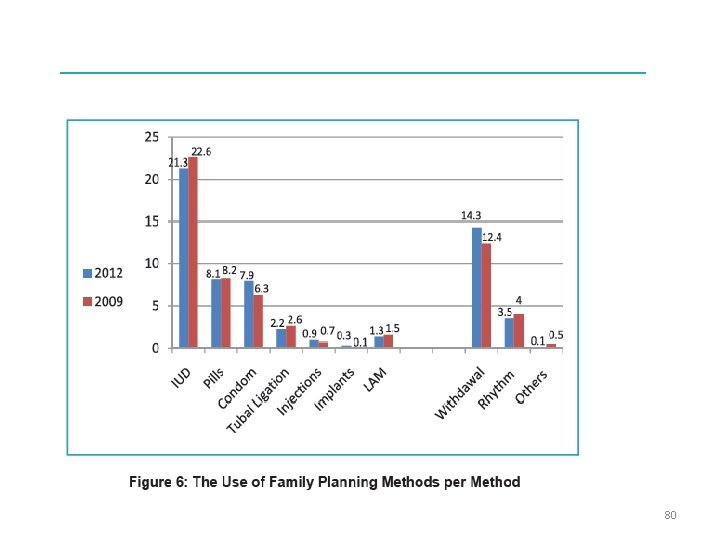
Contraceptive prevalence • The most popular modern method is the IUD, used by 21% of married women. • The next most popular modern methods are the pill (8%) and the condom (8%). Two percent of married women have been sterilized, while less than 1% are using injectable or implants. • As for traditional methods, withdrawal is used by 14 percent of currently married women and rhythm or periodic abstinence is used by about 4%. 75
How to get Family Planning in Jordan Public Sector • • • Government hospital Government health center Government MCH center University hospital/clinic Royal Medical Services 76
How to get Family Planning in Jordan Private Sector • • • Private hospital/clinic Private doctor Pharmacy JAFPP UNRWA clinic Other NGO 77
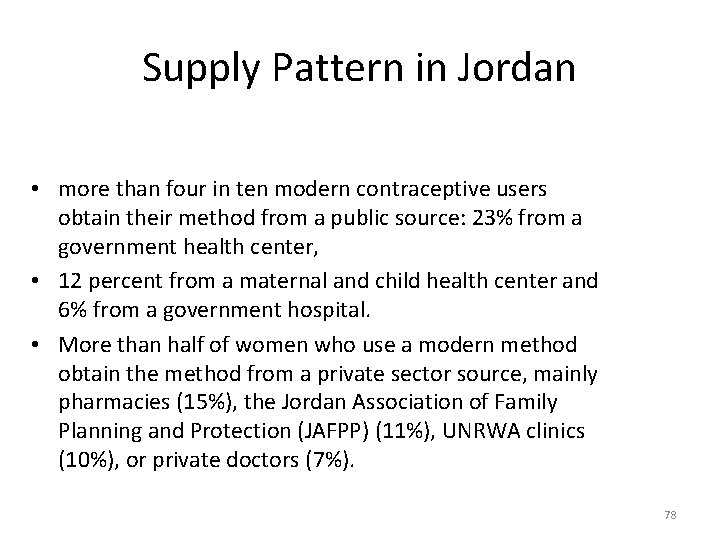
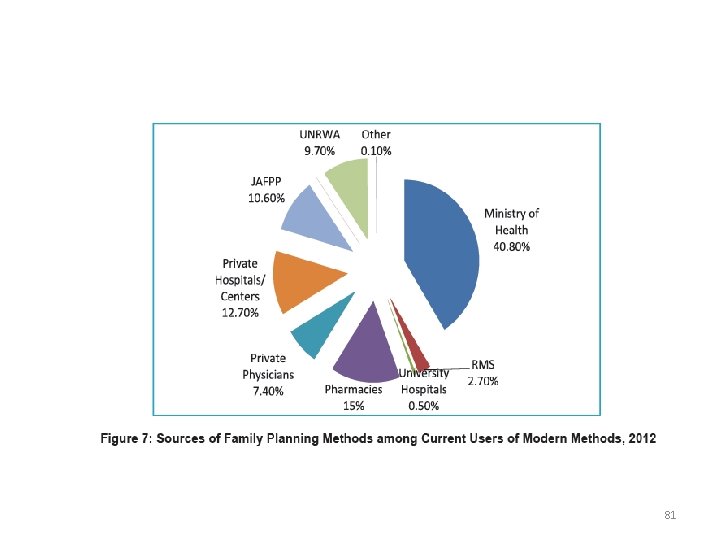
Supply Pattern in Jordan • more than four in ten modern contraceptive users obtain their method from a public source: 23% from a government health center, • 12 percent from a maternal and child health center and 6% from a government hospital. • More than half of women who use a modern method obtain the method from a private sector source, mainly pharmacies (15%), the Jordan Association of Family Planning and Protection (JAFPP) (11%), UNRWA clinics (10%), or private doctors (7%). 78
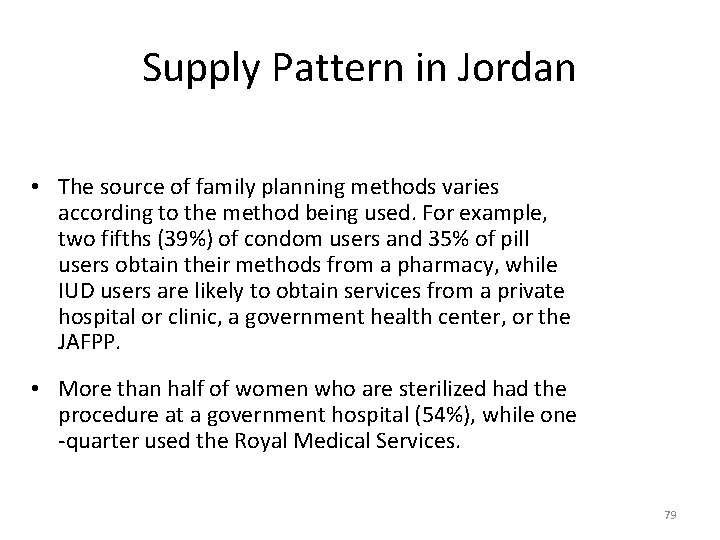
Supply Pattern in Jordan • The source of family planning methods varies according to the method being used. For example, two fifths (39%) of condom users and 35% of pill users obtain their methods from a pharmacy, while IUD users are likely to obtain services from a private hospital or clinic, a government health center, or the JAFPP. • More than half of women who are sterilized had the procedure at a government hospital (54%), while one -quarter used the Royal Medical Services. 79
80
81
82
Thank You THANK YOU 83
 Introduction to community medicine
Introduction to community medicine Concepts of health and disease
Concepts of health and disease Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis
Semmelweis Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Applied medical sciences
Applied medical sciences Agnes csaki semmelweis
Agnes csaki semmelweis Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Faculty of veterinary medicine - university of tehran
Faculty of veterinary medicine - university of tehran Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Faculty of medicine mcgill
Faculty of medicine mcgill Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Faculty of medicine dentistry and health sciences
Faculty of medicine dentistry and health sciences Emory anticoagulation clinic
Emory anticoagulation clinic Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Faculty introduction speech
Faculty introduction speech Stretcher bond t junction
Stretcher bond t junction Course title and course number
Course title and course number Course interne course externe
Course interne course externe Drinking water
Drinking water Lt lead time
Lt lead time Types of family in community medicine
Types of family in community medicine Concept of lead time
Concept of lead time 10 importance of health education
10 importance of health education Basic requirements for sound phc
Basic requirements for sound phc Cohort study community medicine
Cohort study community medicine Duke medicine grand rounds
Duke medicine grand rounds Seqs community medicine
Seqs community medicine Community action cycle for community mobilization
Community action cycle for community mobilization Introduction to banking course
Introduction to banking course Imbe introduction course v2
Imbe introduction course v2 Software engineering 1 course outline
Software engineering 1 course outline Ron had a course introduction
Ron had a course introduction Cleft sentences
Cleft sentences Awe aldermaston
Awe aldermaston Introduction to forensic medicine
Introduction to forensic medicine Introduction of community policing
Introduction of community policing Introduction to community pharmacy
Introduction to community pharmacy Introduction of community health nursing
Introduction of community health nursing An introduction to community asset mapping
An introduction to community asset mapping An introduction to community asset mapping
An introduction to community asset mapping Introduction to community pharmacy
Introduction to community pharmacy Herszon kherson maritime college of merchant marine fleet
Herszon kherson maritime college of merchant marine fleet Bridgeport engineering department
Bridgeport engineering department University of bridgeport computer engineering
University of bridgeport computer engineering Alamo colleges faculty salary schedule
Alamo colleges faculty salary schedule Hahnville high school powerschool
Hahnville high school powerschool Importance of faculty in higher education
Importance of faculty in higher education Faculty marshall usc advertising csv
Faculty marshall usc advertising csv Penn state neurosurgery
Penn state neurosurgery Mercy faculty forward
Mercy faculty forward Lee kong chian faculty of engineering and science
Lee kong chian faculty of engineering and science Carelli kutztown
Carelli kutztown Computer science fsu
Computer science fsu Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Umd electrical engineering
Umd electrical engineering Factors influencing faculty staff relationship
Factors influencing faculty staff relationship Nit calicut chemistry department
Nit calicut chemistry department Faculty of civil engineering ctu prague
Faculty of civil engineering ctu prague Ecu faculty manual
Ecu faculty manual Faculty of engineering shoubra
Faculty of engineering shoubra Singularity executive program
Singularity executive program Faculty of law maastricht
Faculty of law maastricht Medical faculty in novi sad dean
Medical faculty in novi sad dean Umn faculty dental clinic
Umn faculty dental clinic Sjsu faculty affairs
Sjsu faculty affairs Unlv faculty senate
Unlv faculty senate Ulm nursing faculty
Ulm nursing faculty Ucl computer science modules
Ucl computer science modules /scdl/bo 46
/scdl/bo 46 Faculty model of training
Faculty model of training Faculty washington edu chudler
Faculty washington edu chudler Kutztown parson
Kutztown parson Student faculty ratio for nba
Student faculty ratio for nba Kfupm clinic
Kfupm clinic Masaryk university medical faculty
Masaryk university medical faculty Faculty model of training
Faculty model of training Jeyakesavan veerasamy
Jeyakesavan veerasamy Fulbright faculty development program
Fulbright faculty development program Feup university of porto
Feup university of porto Faculty of organizational sciences
Faculty of organizational sciences Charles university faculty of humanities
Charles university faculty of humanities Electrotechnical faculty belgrade
Electrotechnical faculty belgrade