Essentials of Human Anatomy Physiology Chapter 16 The

- Slides: 62
Essentials of Human Anatomy & Physiology Chapter 16 The Reproductive System
The Reproductive System Function: Gamete production; transport; maintenance; production of sex hormones Meiosis Information contained in DNA Process of nuclear division Body cells contain 46 chromosomes Gametes contain 23 chromosomes 2 phases Meiosis I & Meiosis II Result is 4 gametes with 23 chromosomes Spermatogenesis 4 sperm Oogenesis 1 Ovum; 3 polar bodies
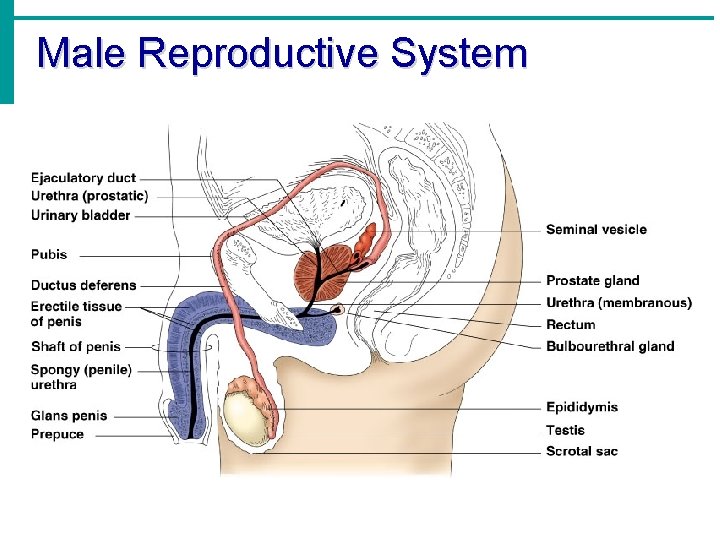
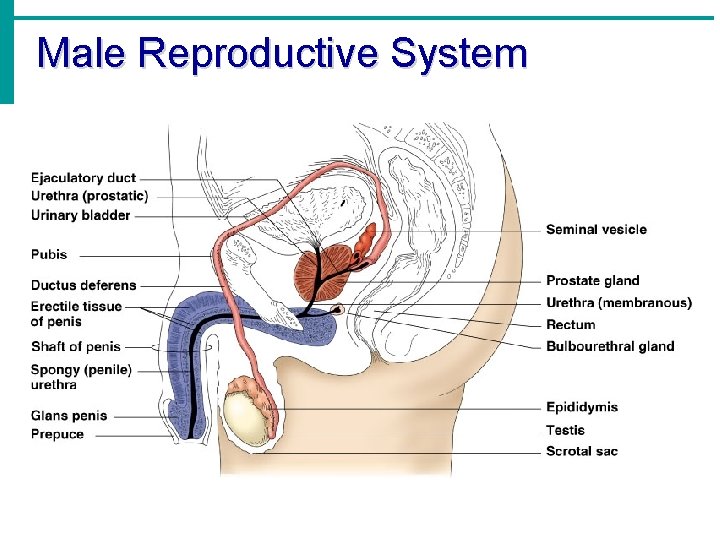
Male Reproductive System
Male Reproductive System Organs produce and maintain sperm; transport sperm and supporting fluids; secrete male sex hormones Testes (2), primary sex organ Exocrine function: produce sperm Endocrine function: produce testosterone Duct system, Epididymis, Ductus deferens, Urethra Accessory organs Seminal vesicle, Prostate gland, Bulbourethral gland External genitalia Penis, Scrotum
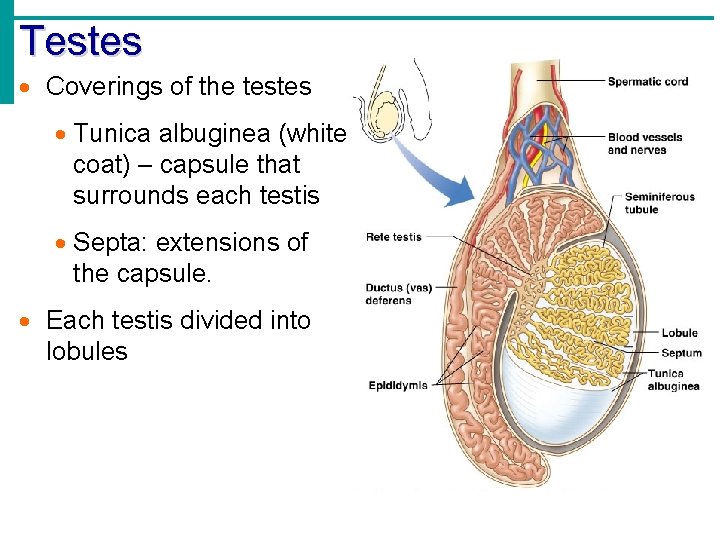
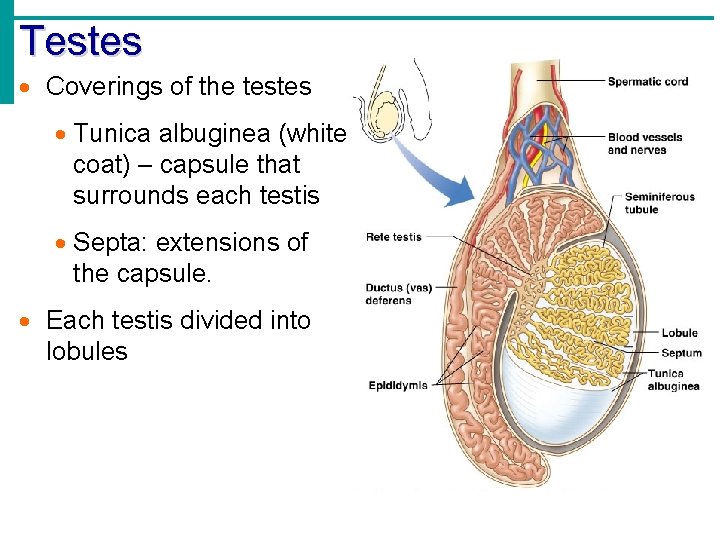
Testes Coverings of the testes Tunica albuginea (white coat) – capsule that surrounds each testis Septa: extensions of the capsule. Each testis divided into lobules
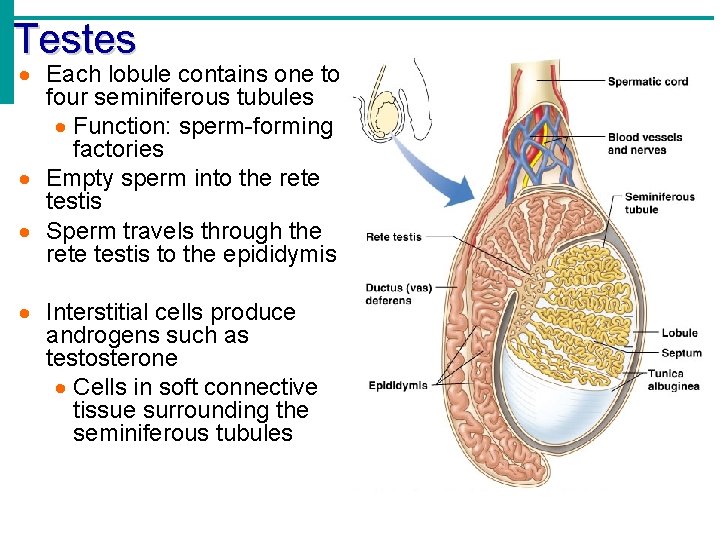
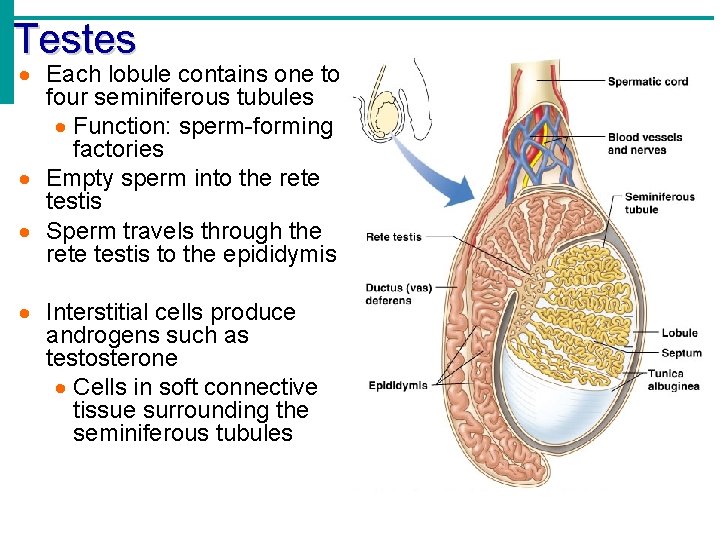
Testes Each lobule contains one to four seminiferous tubules Function: sperm-forming factories Empty sperm into the rete testis Sperm travels through the rete testis to the epididymis Interstitial cells produce androgens such as testosterone Cells in soft connective tissue surrounding the seminiferous tubules
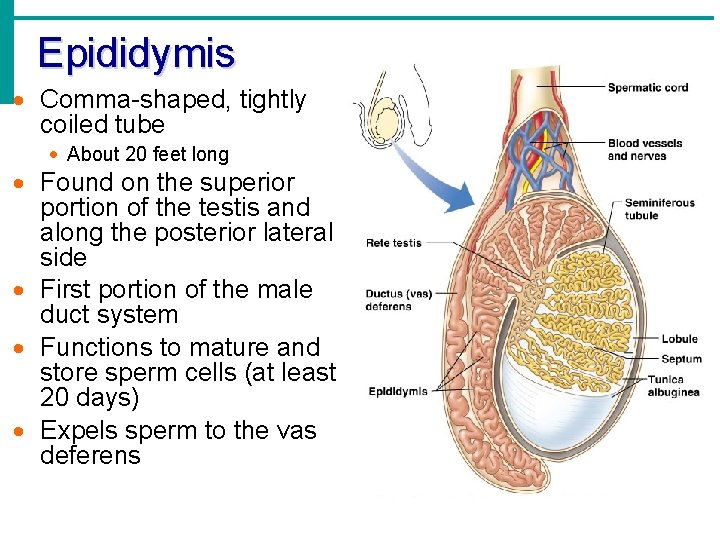
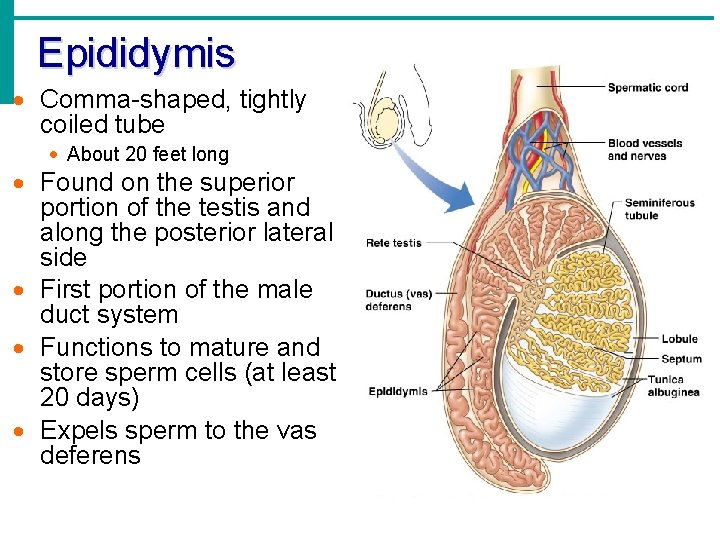
Epididymis Comma-shaped, tightly coiled tube About 20 feet long Found on the superior portion of the testis and along the posterior lateral side First portion of the male duct system Functions to mature and store sperm cells (at least 20 days) Expels sperm to the vas deferens
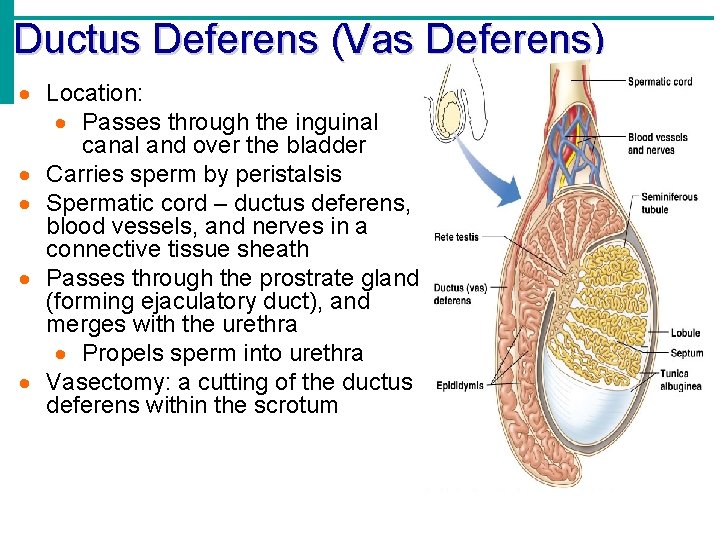
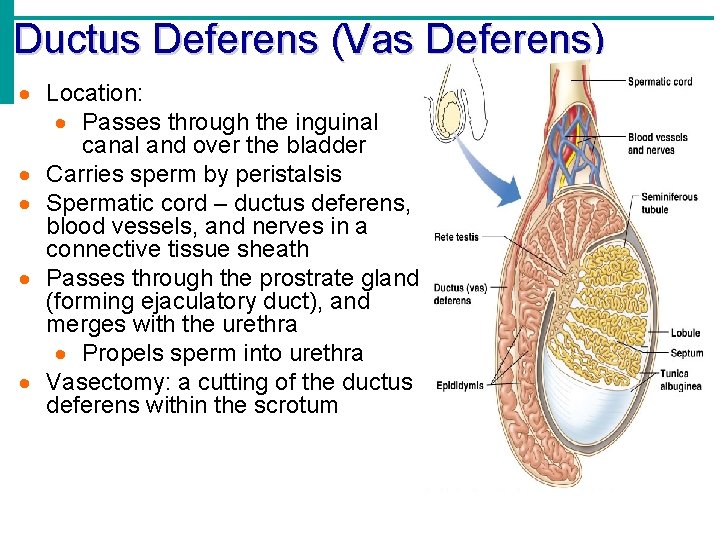
Ductus Deferens (Vas Deferens) Location: Passes through the inguinal canal and over the bladder Carries sperm by peristalsis Spermatic cord – ductus deferens, blood vessels, and nerves in a connective tissue sheath Passes through the prostrate gland (forming ejaculatory duct), and merges with the urethra Propels sperm into urethra Vasectomy: a cutting of the ductus deferens within the scrotum
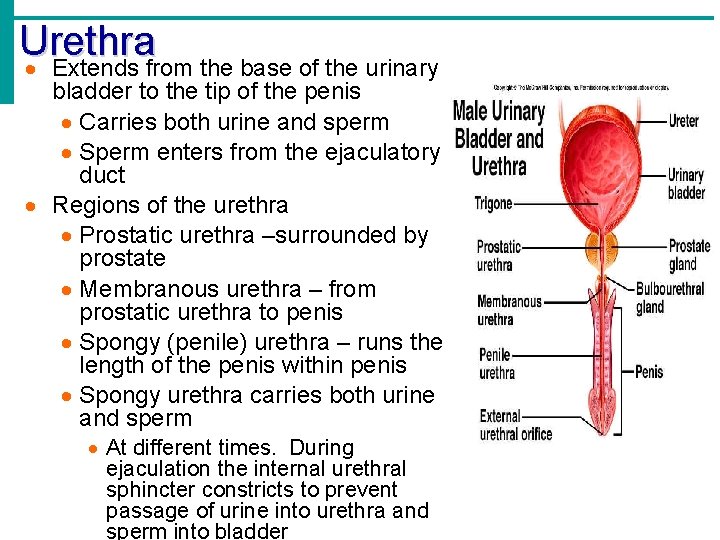
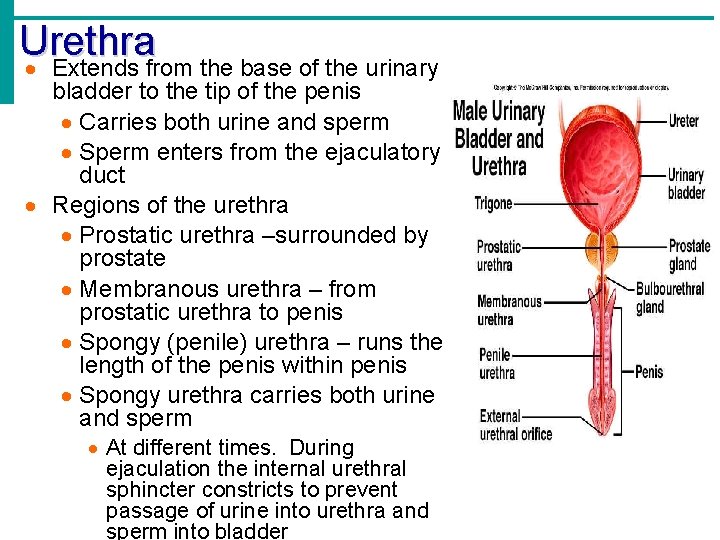
Urethra Extends from the base of the urinary bladder to the tip of the penis Carries both urine and sperm Sperm enters from the ejaculatory duct Regions of the urethra Prostatic urethra –surrounded by prostate Membranous urethra – from prostatic urethra to penis Spongy (penile) urethra – runs the length of the penis within penis Spongy urethra carries both urine and sperm At different times. During ejaculation the internal urethral sphincter constricts to prevent passage of urine into urethra and sperm into bladder
Seminal Vesicles Located at the base of the bladder Produces a thick, yellowish secretion (60% of semen) Fructose (sugar); ENERGY! Vitamin C Prostaglandins Other substances that nourish and activate sperm
Prostate Gland Encircles the urethra below bladder Secretes a milky fluid Helps to activate sperm; motility Enters the urethra through several small ducts Located anteriorly to rectum Bulbourethral Glands Pea-sized gland inferior to the prostate Produces a thick, clear mucus Cleanses the urethra of acidic urine; pre-ejaculate Serves as a lubricant during sexual intercourse Secreted into the penile urethra
Semen Mixture of sperm and accessory gland secretions Advantages of accessory gland secretions Fructose provides energy for sperm cells Alkalinity of semen helps neutralize the acidic environment of vagina Semen inhibits bacterial multiplication Elements of semen enhance sperm motility 50 -130 million sperm in each ml of semen Less that 20 million per ml makes fertilization improbable
External Genitalia Scrotum Divided sac of skin & subcutaneous tissue outside the abdomen enclosing testes; appears as single pouch, but house 2 testes Maintains testes at 3°C (~60 degrees F) lower than normal body temperature to protect sperm viability moved by cremaster muscle Penis Male excitatory organ Surrounds urethra Delivers sperm into the female reproductive tract Regions of the penis Shaft Glans penis (enlarged tip) Prepuce (foreskin) Folded cuff of skin around proximal end (Often removed by circumcision) Erection; emission; ejaculation; orgasm
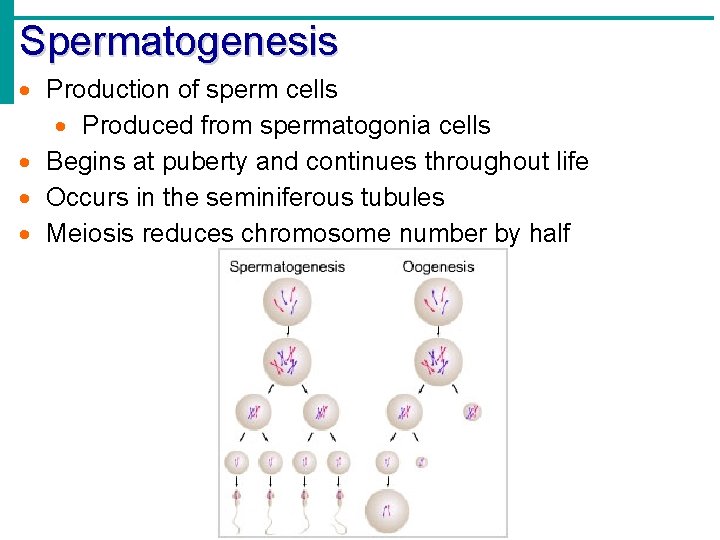
Spermatogenesis Production of sperm cells Produced from spermatogonia cells Begins at puberty and continues throughout life Occurs in the seminiferous tubules Meiosis reduces chromosome number by half
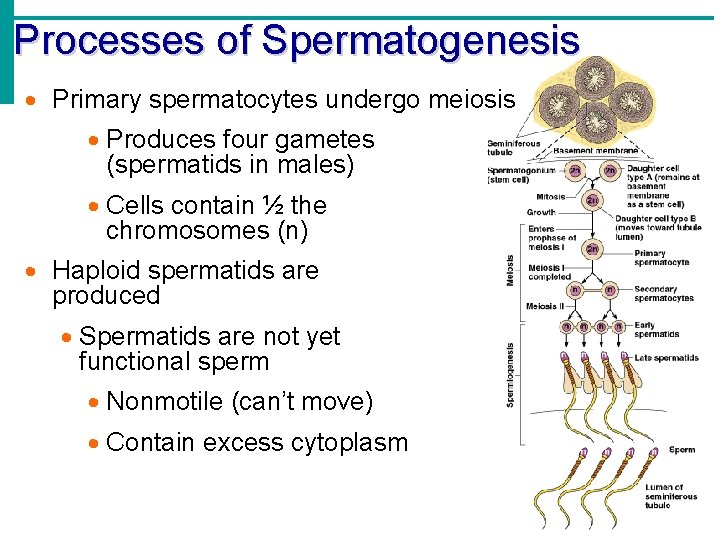
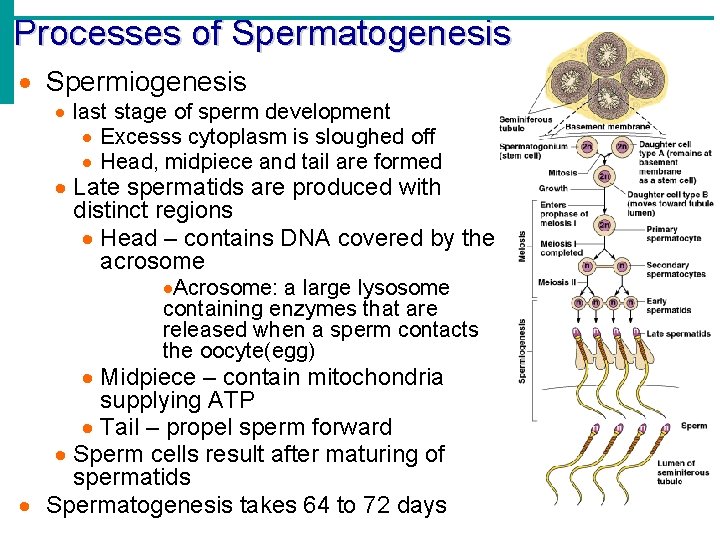
Processes of Spermatogenesis From birth to puberty: Spermatogonia (stem cells) undergo mitosis to produce stem cells before puberty During puberty and beyond: Follicle stimulating hormone (FSH) modifies spermatogonia division At each division now, two daughter cells are produced. We will call them daughter cell A and daughter cell B Type A daughter cell remains embedded in seminiferous tubule to maintain the stem cell population Type B daughter cell produced becomes a primary spermatocyte Travels toward the tubule lumen while undergoing meiosis
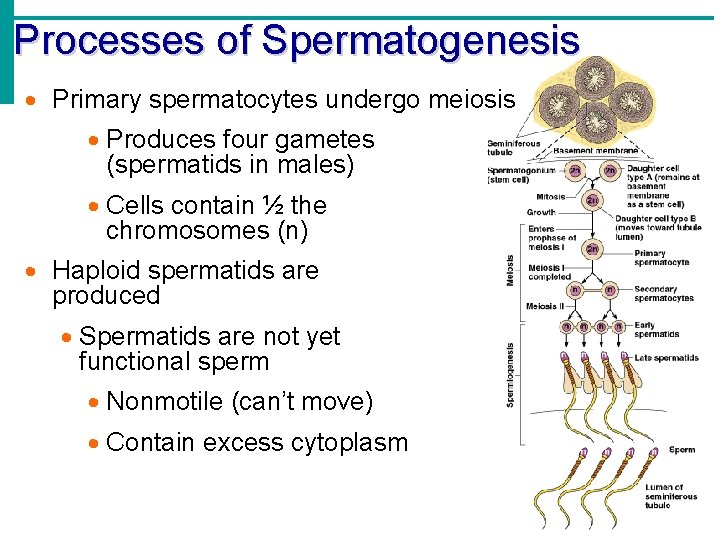
Processes of Spermatogenesis Primary spermatocytes undergo meiosis Produces four gametes (spermatids in males) Cells contain ½ the chromosomes (n) Haploid spermatids are produced Spermatids are not yet functional sperm Nonmotile (can’t move) Contain excess cytoplasm
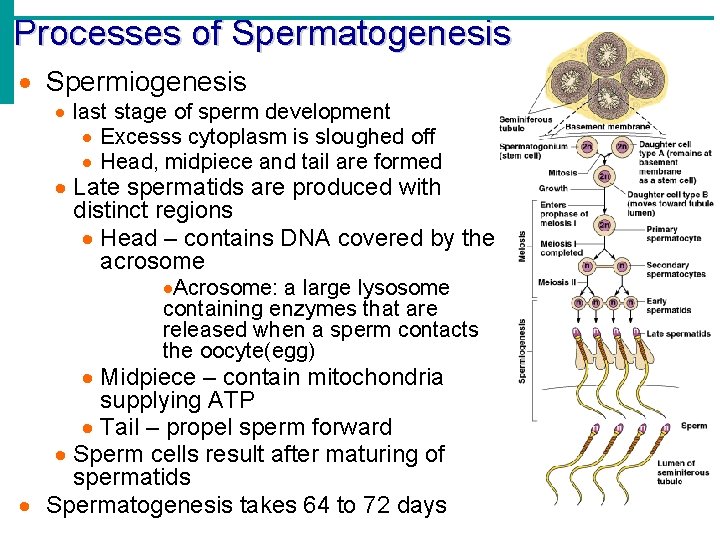
Processes of Spermatogenesis Spermiogenesis last stage of sperm development Excesss cytoplasm is sloughed off Head, midpiece and tail are formed Late spermatids are produced with distinct regions Head – contains DNA covered by the acrosome Acrosome: a large lysosome containing enzymes that are released when a sperm contacts the oocyte(egg) Midpiece – contain mitochondria supplying ATP Tail – propel sperm forward Sperm cells result after maturing of spermatids Spermatogenesis takes 64 to 72 days
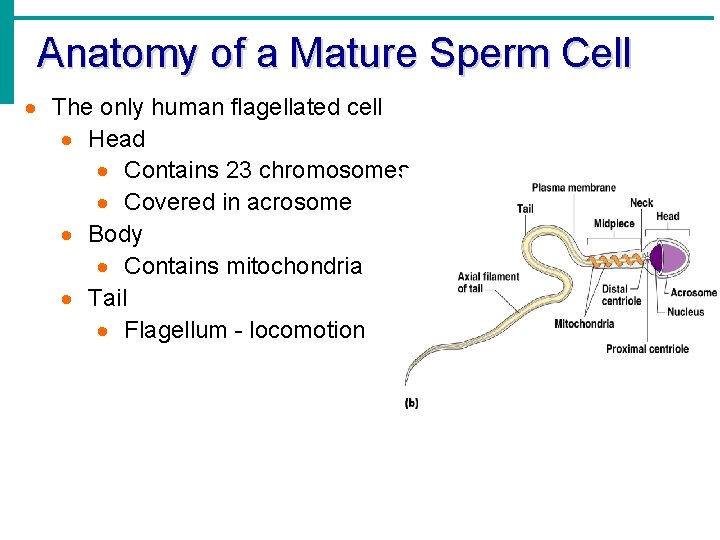
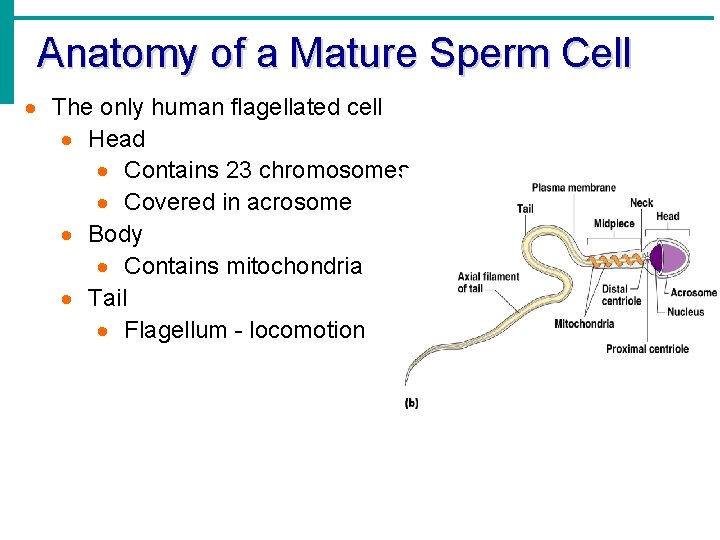
Anatomy of a Mature Sperm Cell The only human flagellated cell Head Contains 23 chromosomes Covered in acrosome Body Contains mitochondria Tail Flagellum - locomotion
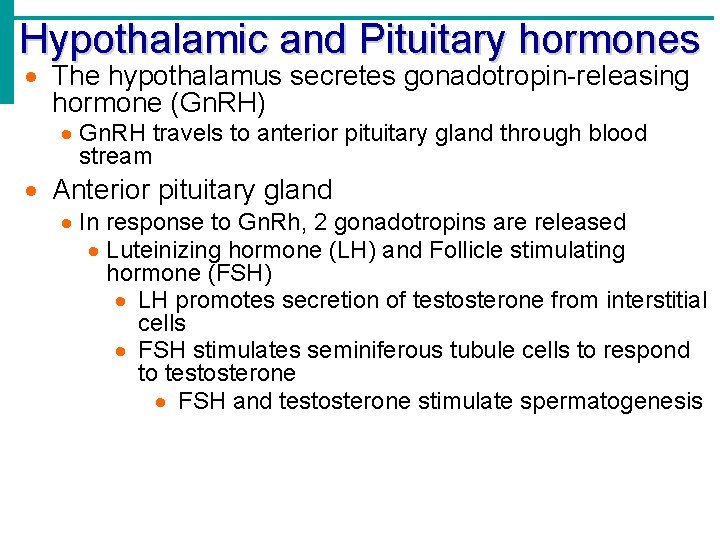
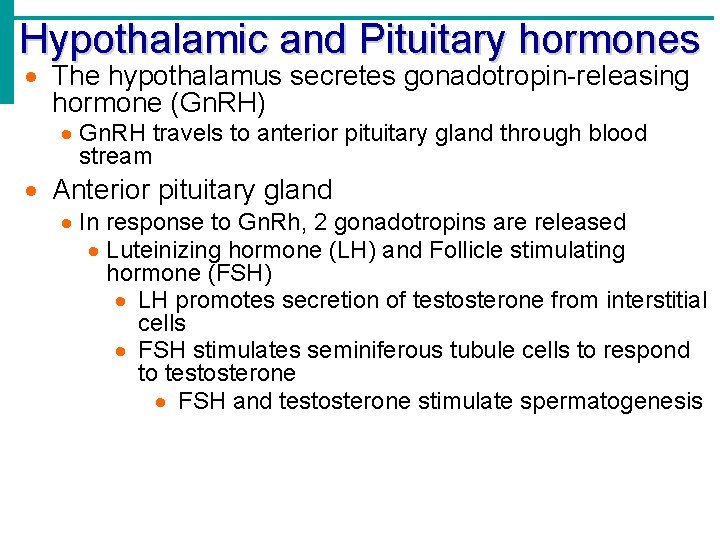
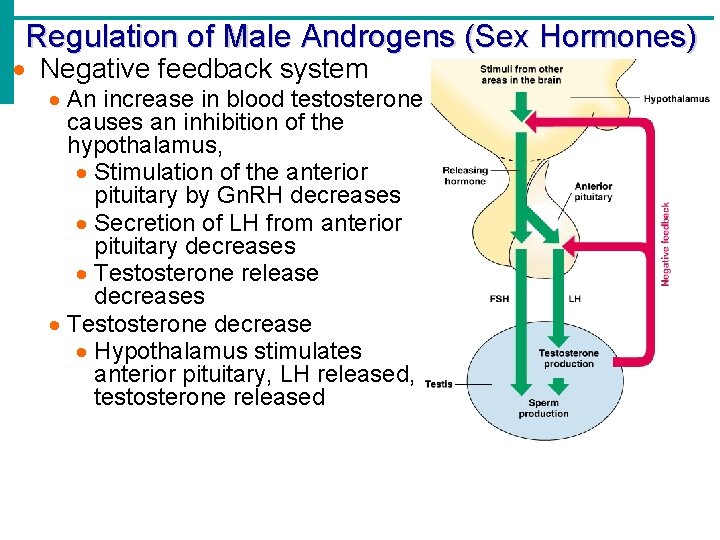
Hypothalamic and Pituitary hormones The hypothalamus secretes gonadotropin-releasing hormone (Gn. RH) Gn. RH travels to anterior pituitary gland through blood stream Anterior pituitary gland In response to Gn. Rh, 2 gonadotropins are released Luteinizing hormone (LH) and Follicle stimulating hormone (FSH) LH promotes secretion of testosterone from interstitial cells FSH stimulates seminiferous tubule cells to respond to testosterone FSH and testosterone stimulate spermatogenesis
Androgen (Testosterone) Production Testosterone: the most important hormone of the testes Testosterone produced continuously from puberty on within males Targets secondary sex organs Deepening of voice, Increased hair growth, Enlargement of skeletal muscles, Thickening of bones Functions of testosterone Stimulates reproductive organ development Underlies sex drive Sexual infantilism: the result of no testosterone production, the secondary sexual characteristics do not develop
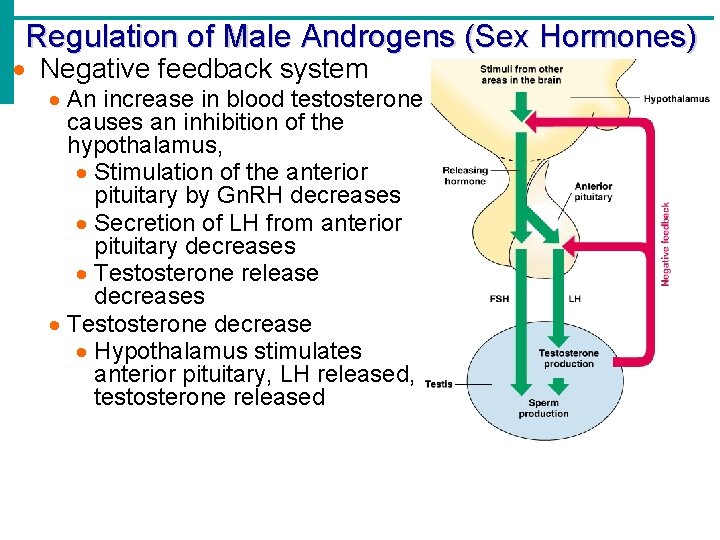
Regulation of Male Androgens (Sex Hormones) Negative feedback system An increase in blood testosterone causes an inhibition of the hypothalamus, Stimulation of the anterior pituitary by Gn. RH decreases Secretion of LH from anterior pituitary decreases Testosterone release decreases Testosterone decrease Hypothalamus stimulates anterior pituitary, LH released, testosterone released
Female Reproductive System
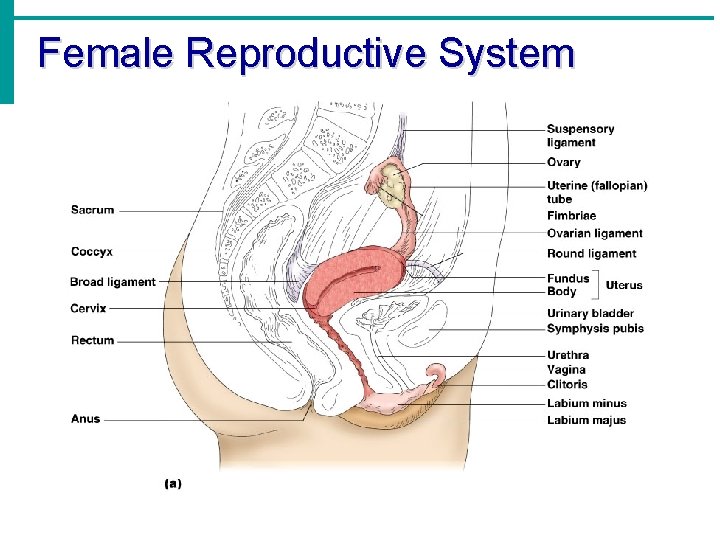
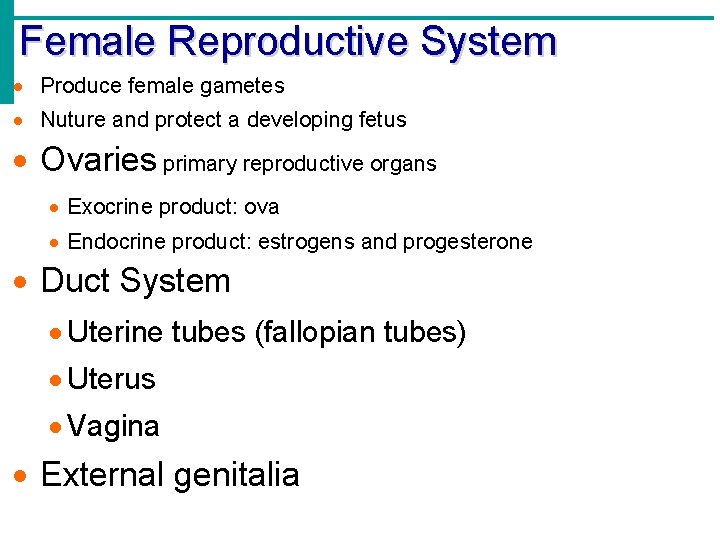
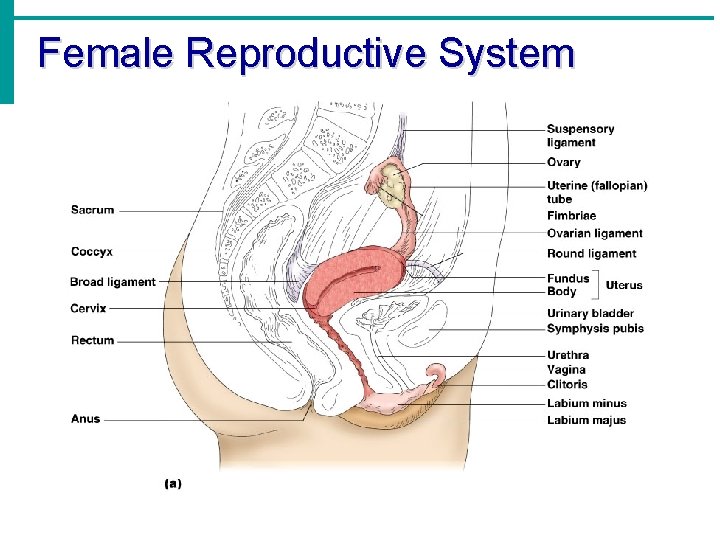
Female Reproductive System Produce female gametes Nuture and protect a developing fetus Ovaries primary reproductive organs Exocrine product: ova Endocrine product: estrogens and progesterone Duct System Uterine tubes (fallopian tubes) Uterus Vagina External genitalia
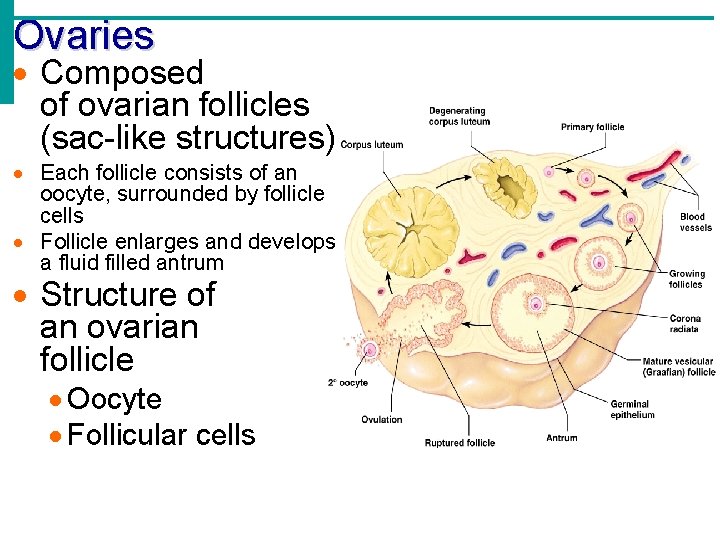
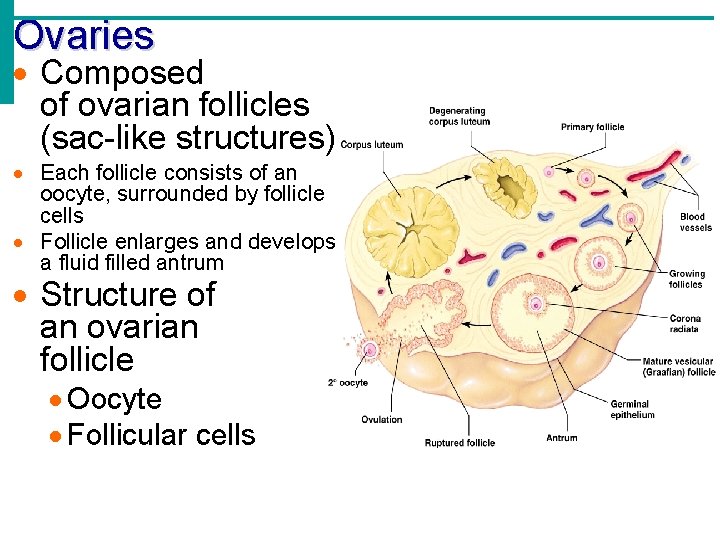
Ovaries Composed of ovarian follicles (sac-like structures) Each follicle consists of an oocyte, surrounded by follicle cells Follicle enlarges and develops a fluid filled antrum Structure of an ovarian follicle Oocyte Follicular cells
Ovarian Follicle Stages Primary follicle – contains an immature oocyte early stage Graafian (vesicular) follicle – growing follicle with a maturing oocyte later stage. The egg matures until ovulation Ovulation – when the egg is mature the follicle ruptures the oocyte is released from the ovary Occurs about every 28 days The ruptured follicle is transformed into a corpus luteum In older women the ovary surface is scarred and pitted
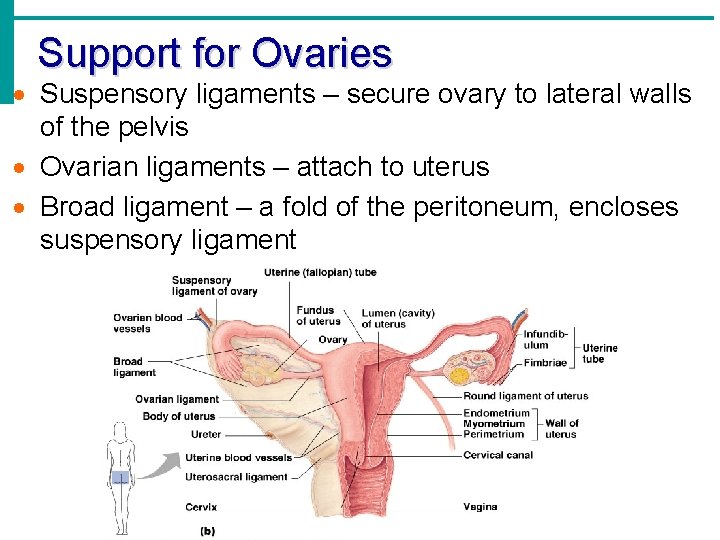
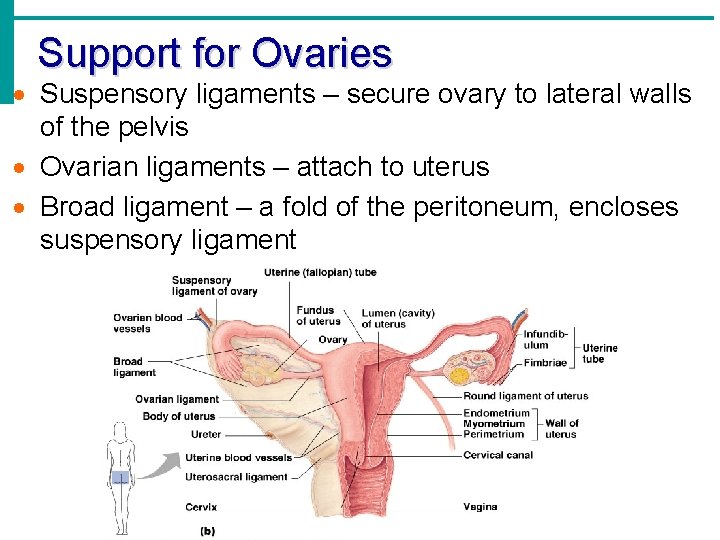
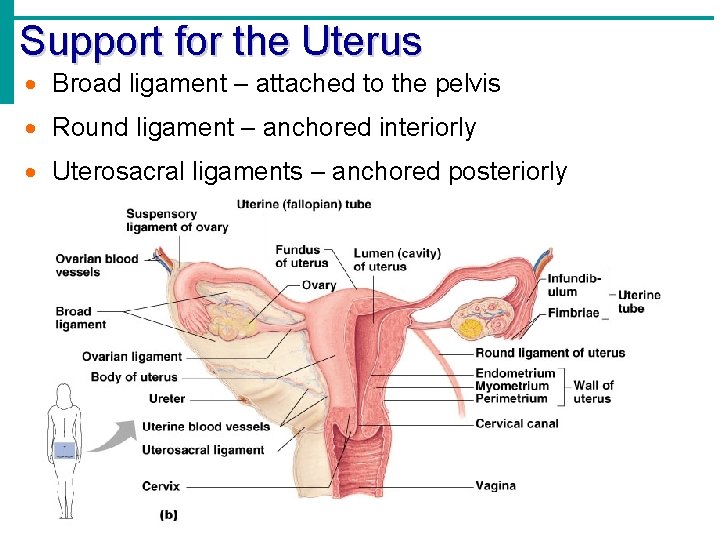
Support for Ovaries Suspensory ligaments – secure ovary to lateral walls of the pelvis Ovarian ligaments – attach to uterus Broad ligament – a fold of the peritoneum, encloses suspensory ligament
Uterine Tubes from ovaries to uterus (Begin duct system) 4 inches long Fimbriae – finger-like extentions at the distal end that receive the oocyte Provide a site for fertilization Does not physically attach to the ovary Supported by the broad ligament Attaches to the uterus Cilia inside the uterine tube slowly move the oocyte towards the uterus Fertilization occurs inside the uterine tube Oocyte is viable for 24 hours, journey takes 3 -4 days Many potential eggs are lost in the peritoneal cavity
Uterus Located between the urinary bladder and rectum Hollow, muscular organ Functions of the uterus Receives a fertilized egg Retains the fertilized egg Nourishes the fertilized egg Enlarges during pregnancy

Uterus Layers Endometrium Inner layer Allows for implantation of a fertilized egg Sloughs off if no pregnancy occurs (menses) Endometriosis = endometrial tissue in locations other than uterus; tissue bleeds, but does not shed, resulting in scars or adhesions; painful and possibly infertile condition Myometrium – middle layer of smooth muscle Serous layer – outer visceral peritoneum Lower 1/3 forms Cervix
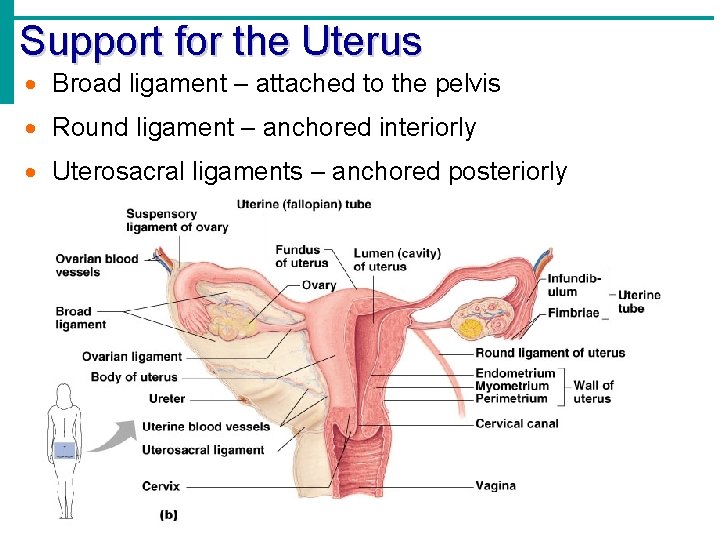
Support for the Uterus Broad ligament – attached to the pelvis Round ligament – anchored interiorly Uterosacral ligaments – anchored posteriorly
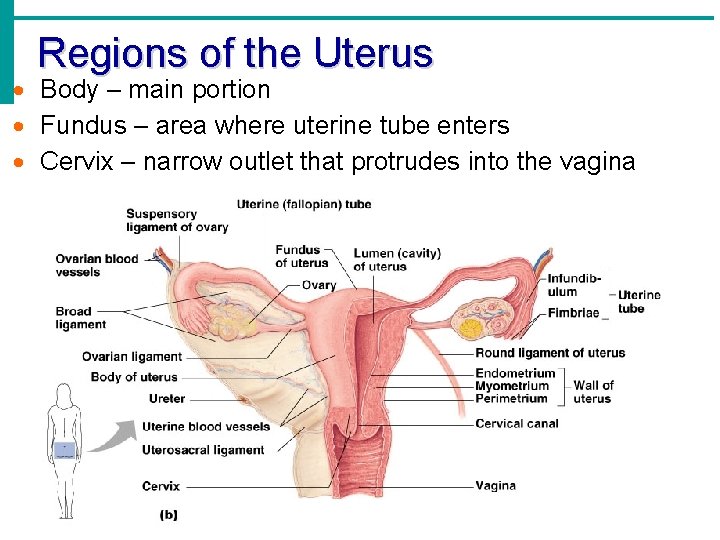
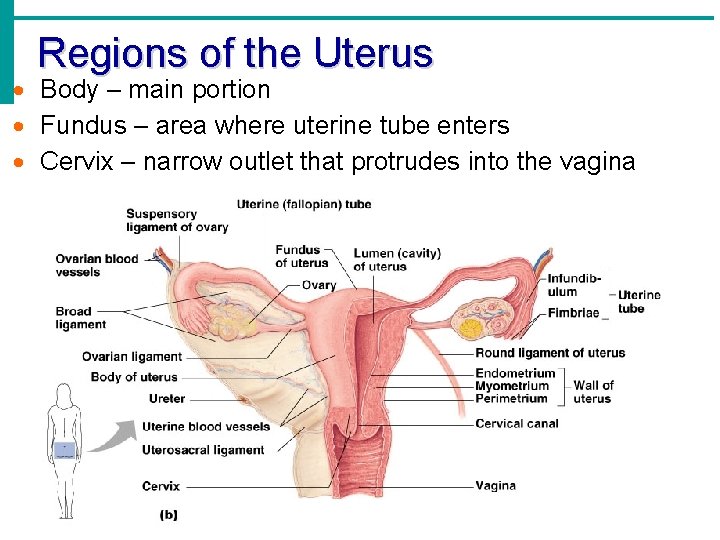
Regions of the Uterus Body – main portion Fundus – area where uterine tube enters Cervix – narrow outlet that protrudes into the vagina
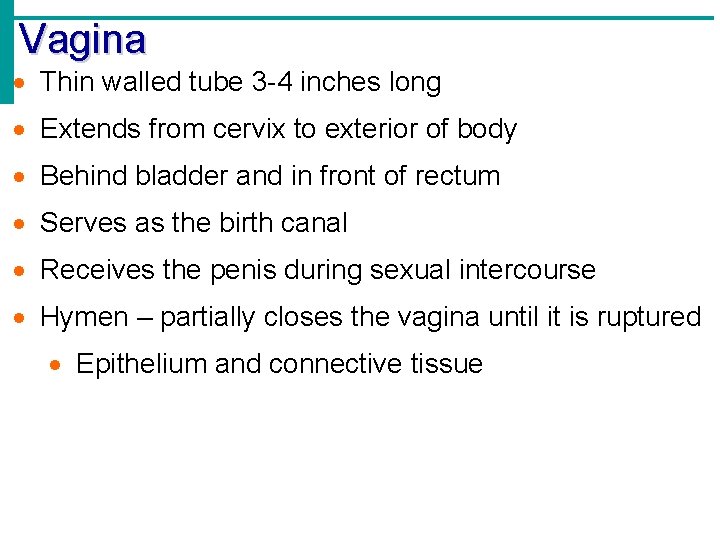
Vagina Thin walled tube 3 -4 inches long Extends from cervix to exterior of body Behind bladder and in front of rectum Serves as the birth canal Receives the penis during sexual intercourse Hymen – partially closes the vagina until it is ruptured Epithelium and connective tissue
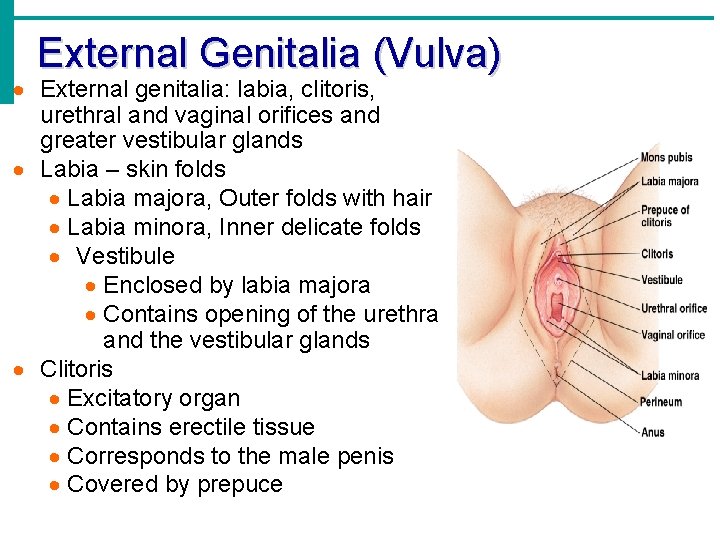
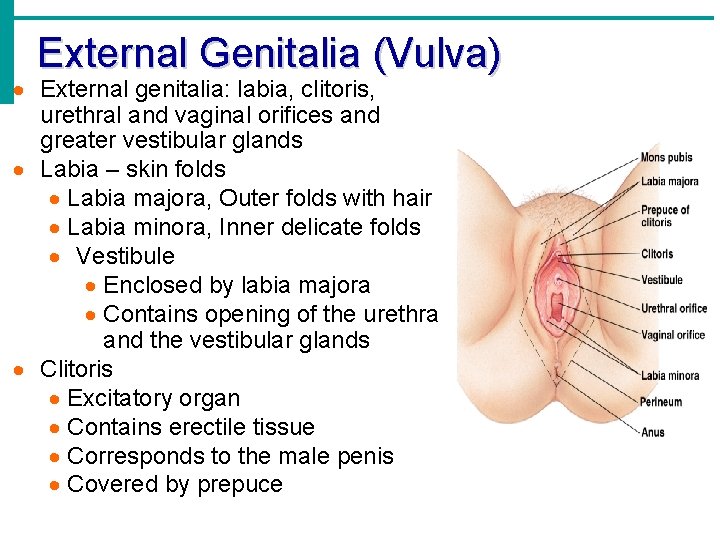
External Genitalia (Vulva) External genitalia: labia, clitoris, urethral and vaginal orifices and greater vestibular glands Labia – skin folds Labia majora, Outer folds with hair Labia minora, Inner delicate folds Vestibule Enclosed by labia majora Contains opening of the urethra and the vestibular glands Clitoris Excitatory organ Contains erectile tissue Corresponds to the male penis Covered by prepuce
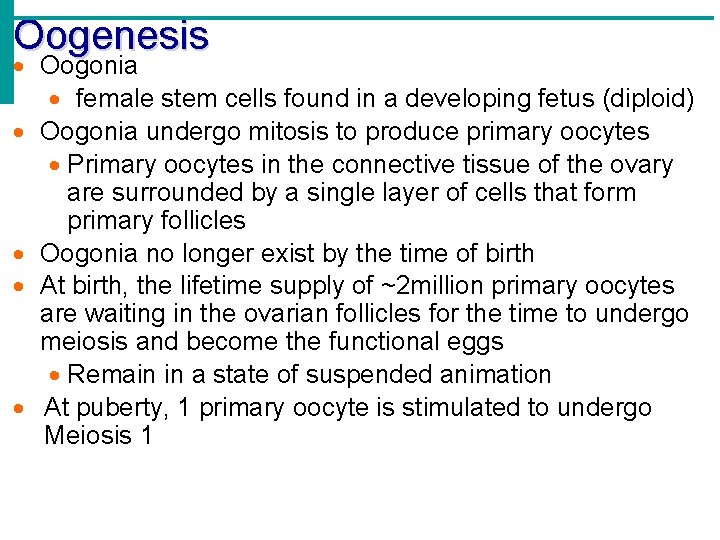
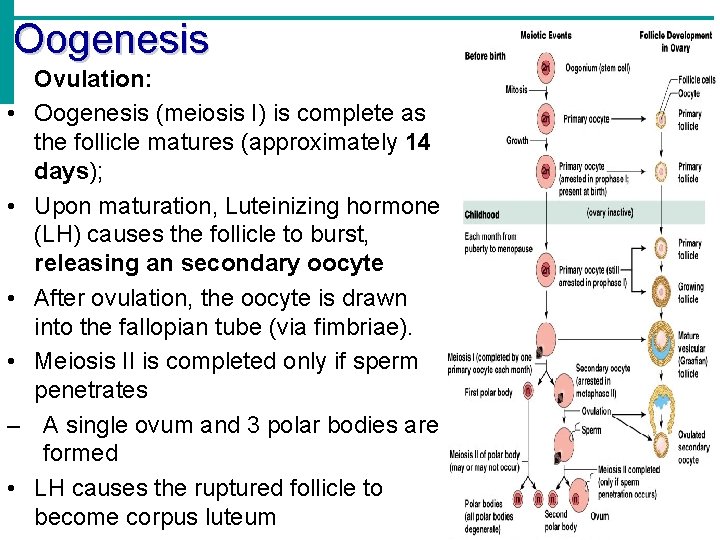
Oogenesis Oogonia female stem cells found in a developing fetus (diploid) Oogonia undergo mitosis to produce primary oocytes Primary oocytes in the connective tissue of the ovary are surrounded by a single layer of cells that form primary follicles Oogonia no longer exist by the time of birth At birth, the lifetime supply of ~2 million primary oocytes are waiting in the ovarian follicles for the time to undergo meiosis and become the functional eggs Remain in a state of suspended animation At puberty, 1 primary oocyte is stimulated to undergo Meiosis 1
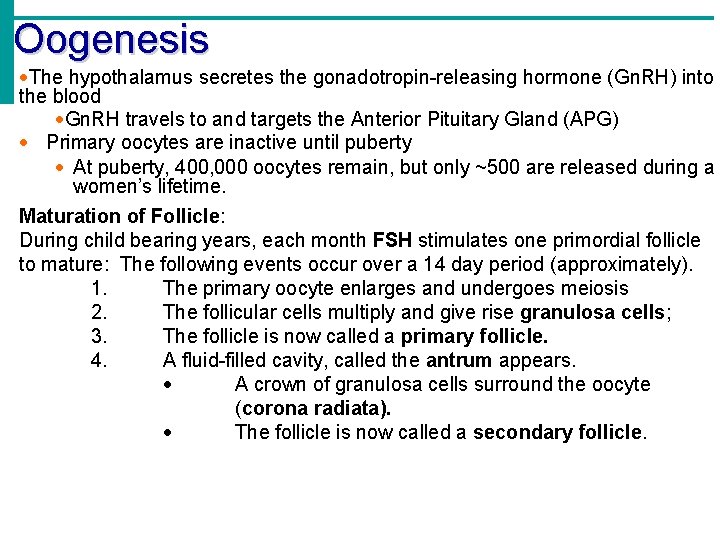
Oogenesis The hypothalamus secretes the gonadotropin-releasing hormone (Gn. RH) into the blood Gn. RH travels to and targets the Anterior Pituitary Gland (APG) Primary oocytes are inactive until puberty At puberty, 400, 000 oocytes remain, but only ~500 are released during a women’s lifetime. Maturation of Follicle: During child bearing years, each month FSH stimulates one primordial follicle to mature: The following events occur over a 14 day period (approximately). 1. The primary oocyte enlarges and undergoes meiosis 2. The follicular cells multiply and give rise granulosa cells; 3. The follicle is now called a primary follicle. 4. A fluid-filled cavity, called the antrum appears. A crown of granulosa cells surround the oocyte (corona radiata). The follicle is now called a secondary follicle.
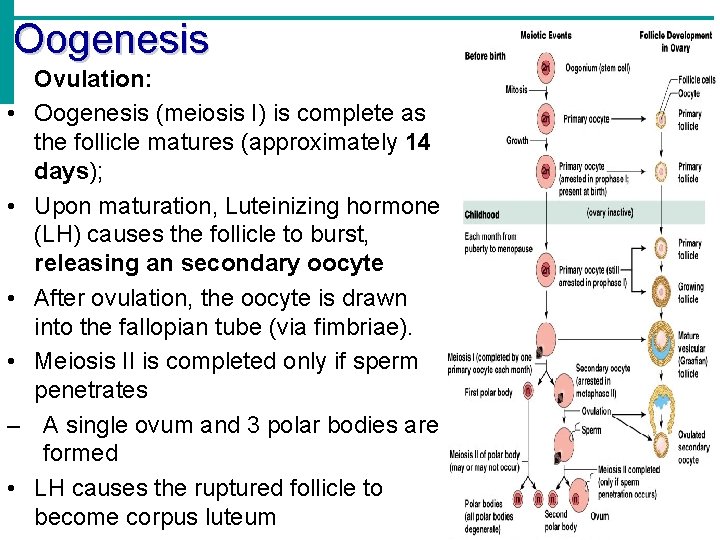
Oogenesis • Ovulation: • Oogenesis (meiosis I) is complete as the follicle matures (approximately 14 days); • Upon maturation, Luteinizing hormone (LH) causes the follicle to burst, releasing an secondary oocyte • After ovulation, the oocyte is drawn into the fallopian tube (via fimbriae). • Meiosis II is completed only if sperm penetrates – A single ovum and 3 polar bodies are formed • LH causes the ruptured follicle to become corpus luteum
Hormone Production by the Ovaries Estrogens Produced by maturing follicle cells (of ovary) Days 1 -14 Cause secondary sex characteristics Enlargement of accessory organs Development of breasts Appearance of pubic hair Increase in fat beneath the skin Widening and lightening of the pelvis Onset of menses Progesterone Produced by the corpus luteum Days 14 -24 Production continues until LH diminishes in the blood Prepares the uterus for zygote implantation • thickens the lining • promotes formation of glands and blood vessels
Menstrual (Uterine) Cycle ~28 days in length Cyclic changes of the endometrium mucosa of the uterus in response to hormone changes Regulated by cyclic production of estrogens and progesterone which are regulated by the anterior pituitary hormones =FSH and LH Stages of the menstrual cycle Menses – functional layer of the endometrium is sloughed days 1 -5 Proliferative stage – regeneration of functional layer days 6 -14 Secretory stage – endometrium increases in size and readies for implantation days 15 -28 Ovulation typically occurs on day 14
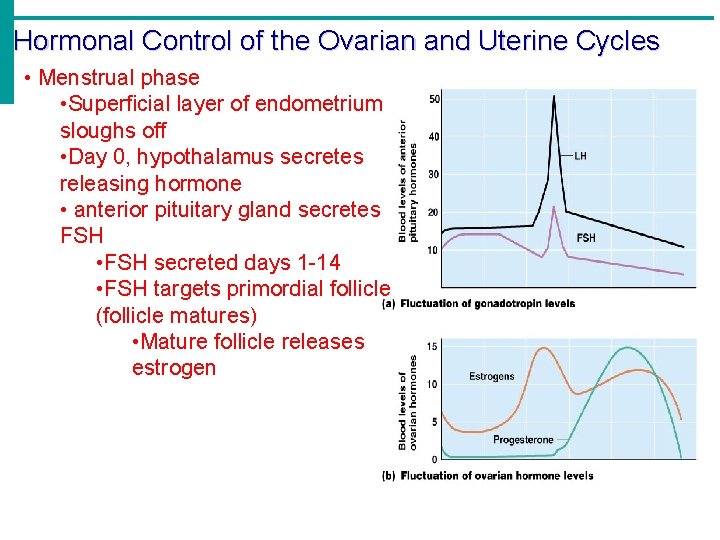
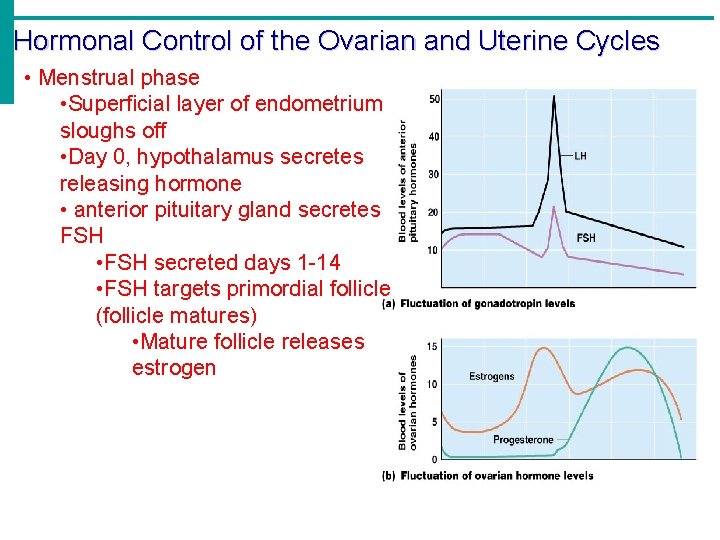
Hormonal Control of the Ovarian and Uterine Cycles • Menstrual phase • Superficial layer of endometrium sloughs off • Day 0, hypothalamus secretes releasing hormone • anterior pituitary gland secretes FSH • FSH secreted days 1 -14 • FSH targets primordial follicle (follicle matures) • Mature follicle releases estrogen
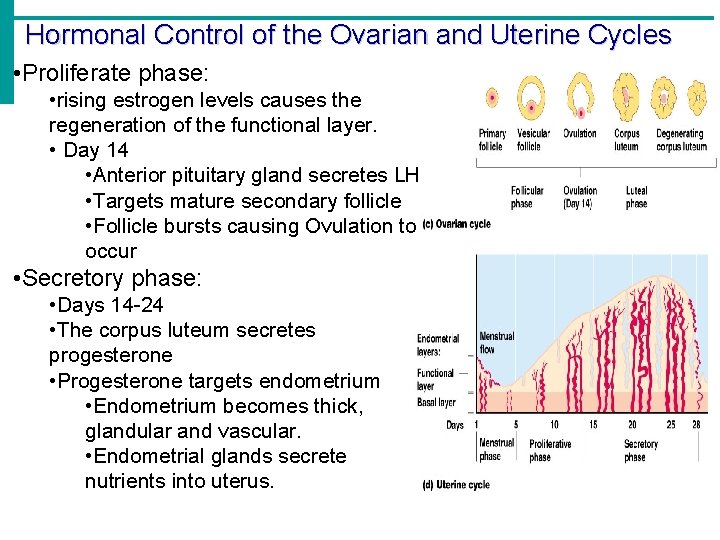
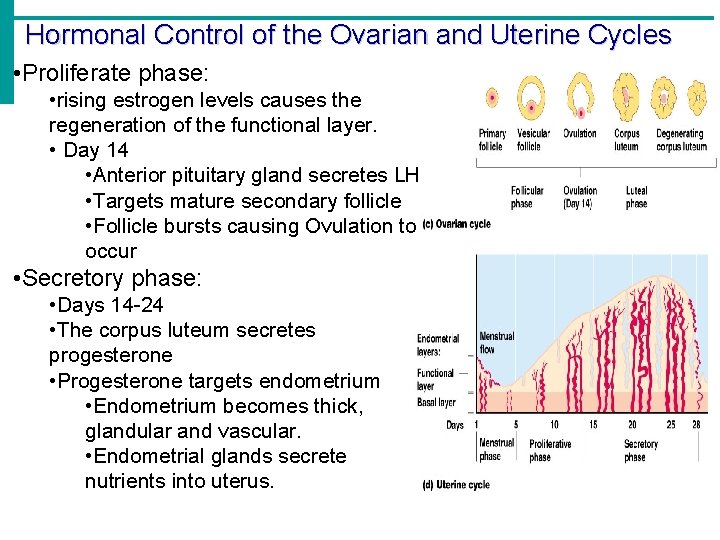
Hormonal Control of the Ovarian and Uterine Cycles • Proliferate phase: • rising estrogen levels causes the regeneration of the functional layer. • Day 14 • Anterior pituitary gland secretes LH • Targets mature secondary follicle • Follicle bursts causing Ovulation to occur • Secretory phase: • Days 14 -24 • The corpus luteum secretes progesterone • Progesterone targets endometrium • Endometrium becomes thick, glandular and vascular. • Endometrial glands secrete nutrients into uterus.
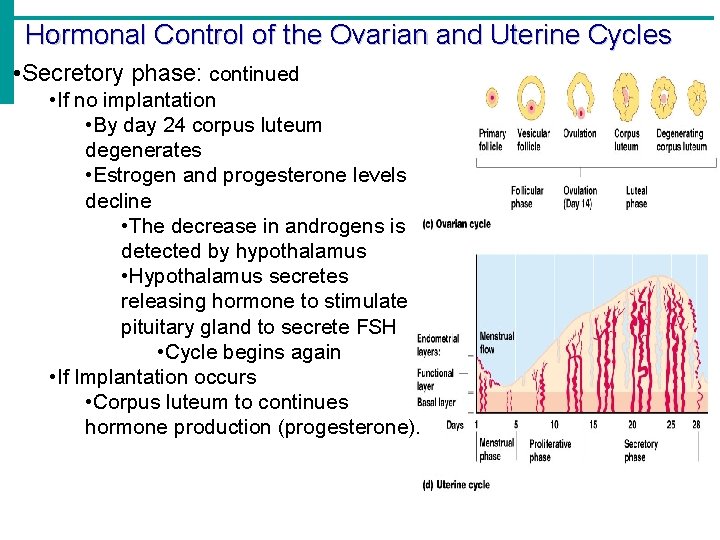
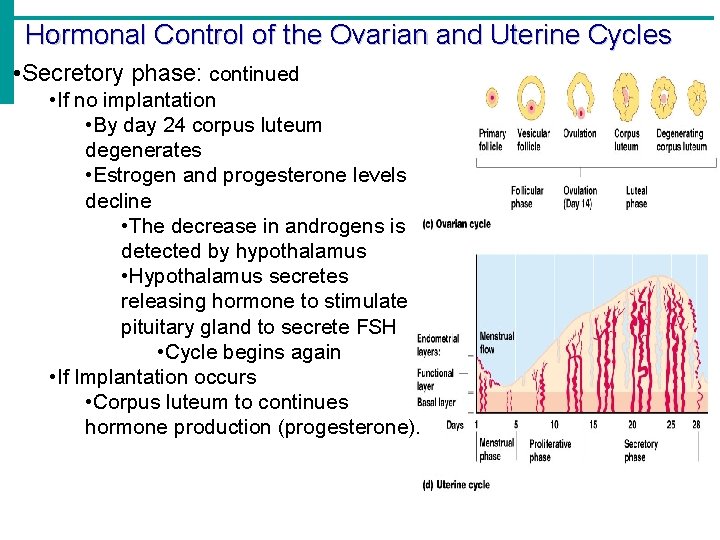
Hormonal Control of the Ovarian and Uterine Cycles • Secretory phase: continued • If no implantation • By day 24 corpus luteum degenerates • Estrogen and progesterone levels decline • The decrease in androgens is detected by hypothalamus • Hypothalamus secretes releasing hormone to stimulate pituitary gland to secrete FSH • Cycle begins again • If Implantation occurs • Corpus luteum to continues hormone production (progesterone).
Stages of Pregnancy and Development Fertilization Embryonic development Fetal development Childbirth
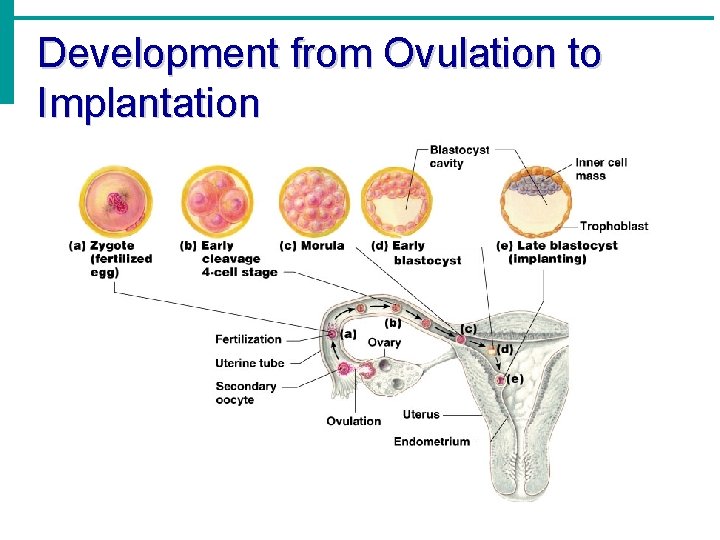
Fertilization Sperm become capacitated in female reproductive tract Secondary oocyte ovulated from ovary The oocyte is viable for 12 to 24 hours after ovulation Sperm are viable for 12 to 48 hours after ejaculation some super sperm are viable for 72 hours So intercourse must take place within 72 hours before to 24 hours after ovulation Sperm cells must make their way to the fallopian tube for fertilization to be possible Chemical messages released by the oocyte attract the sperm One sperm enters secondary oocyte The membrane of the oocyte does not permit a second sperm head to enter The oocyte then undergoes its second meiotic division Fertilization occurs when the genetic material of a sperm combines with that of an oocyte to form a zygote
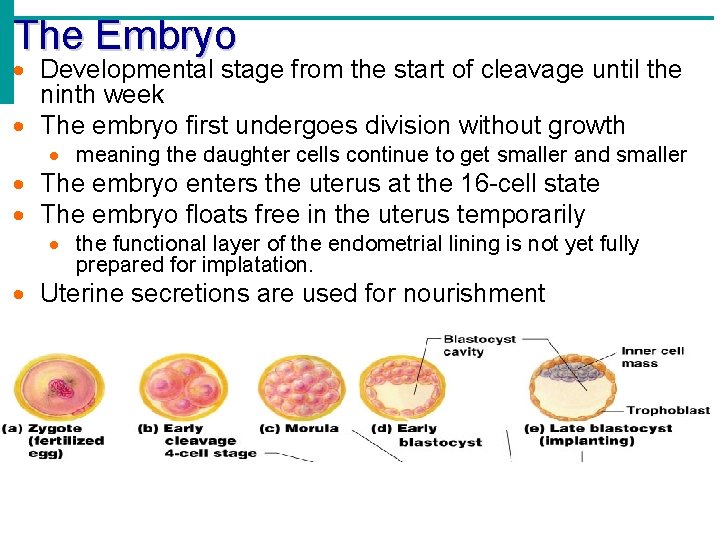
The Zygote First cell of a new individual The result of the fusion of DNA from sperm and egg The zygote begins rapid mitotic cell divisions The process is called cleavage. First division = 36 hours = 2 cells Second division = 48 hours = 4 cells Morula = solid ball of 32 cells = 96 hours The zygote stage is in the uterine tube, moving toward the uterus propelled by peristalsis and cilia Blastocyst = about 5 days A hollow ball of cells surrounding central cavity
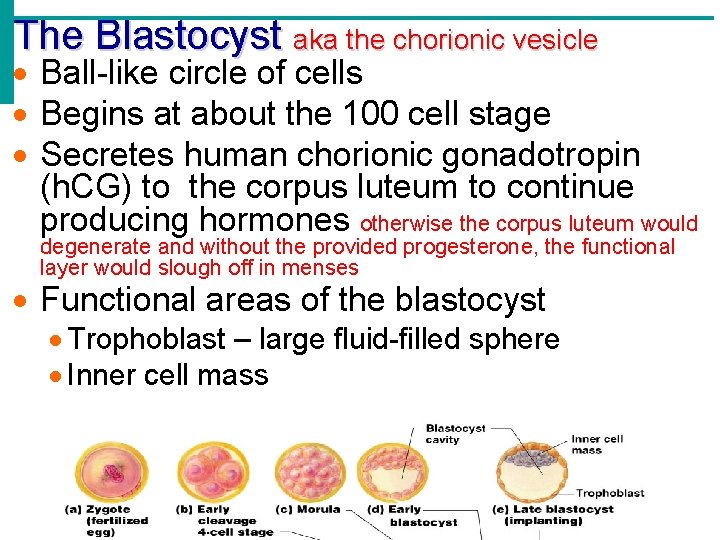
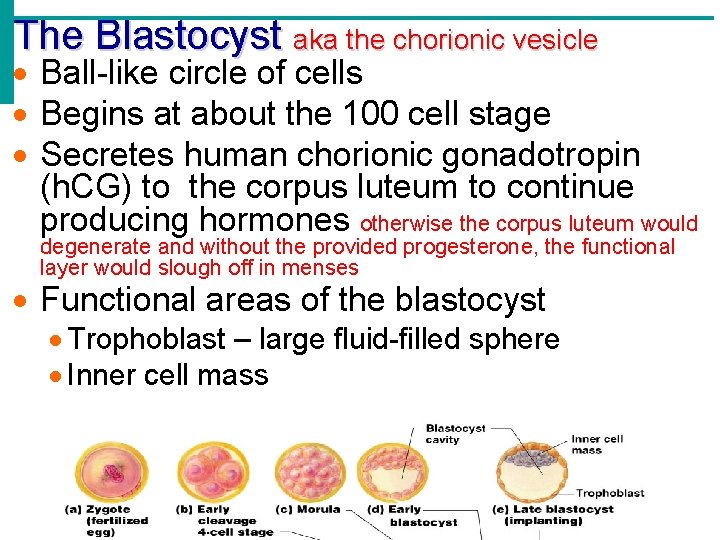
The Blastocyst aka the chorionic vesicle Ball-like circle of cells Begins at about the 100 cell stage Secretes human chorionic gonadotropin (h. CG) to the corpus luteum to continue producing hormones otherwise the corpus luteum would degenerate and without the provided progesterone, the functional layer would slough off in menses Functional areas of the blastocyst Trophoblast – large fluid-filled sphere Inner cell mass
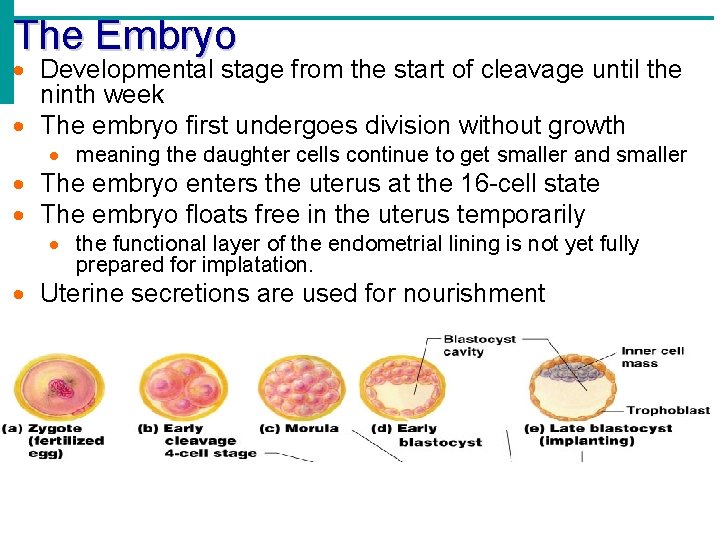
The Embryo Developmental stage from the start of cleavage until the ninth week The embryo first undergoes division without growth meaning the daughter cells continue to get smaller and smaller The embryo enters the uterus at the 16 -cell state The embryo floats free in the uterus temporarily the functional layer of the endometrial lining is not yet fully prepared for implatation. Uterine secretions are used for nourishment
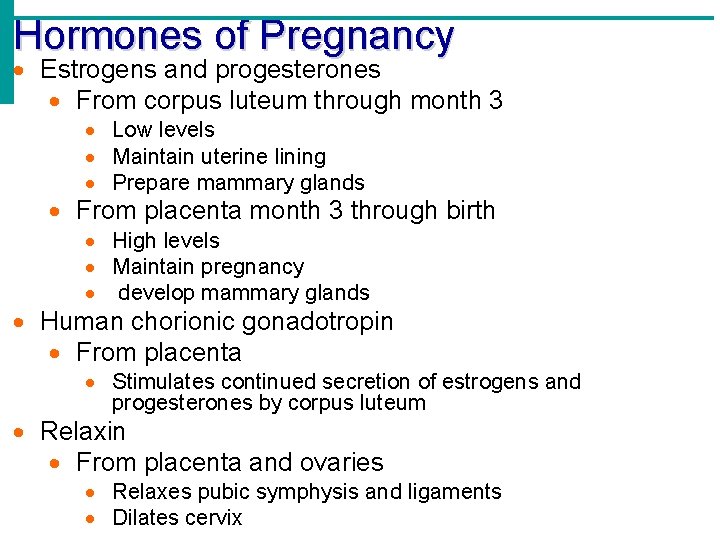
Hormones of Pregnancy Estrogens and progesterones From corpus luteum through month 3 Low levels Maintain uterine lining Prepare mammary glands From placenta month 3 through birth High levels Maintain pregnancy develop mammary glands Human chorionic gonadotropin From placenta Stimulates continued secretion of estrogens and progesterones by corpus luteum Relaxin From placenta and ovaries Relaxes pubic symphysis and ligaments Dilates cervix
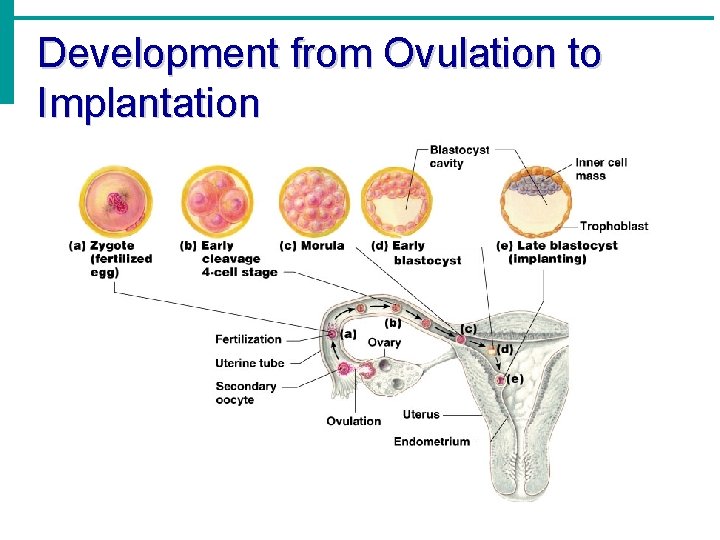
Development from Ovulation to Implantation
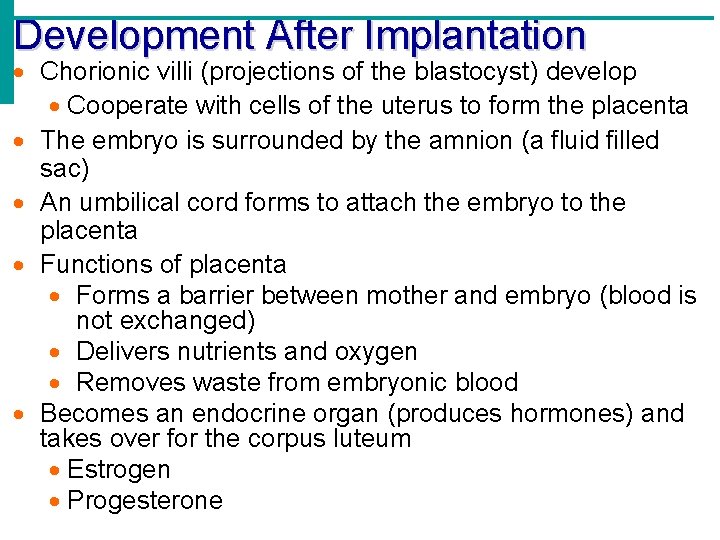
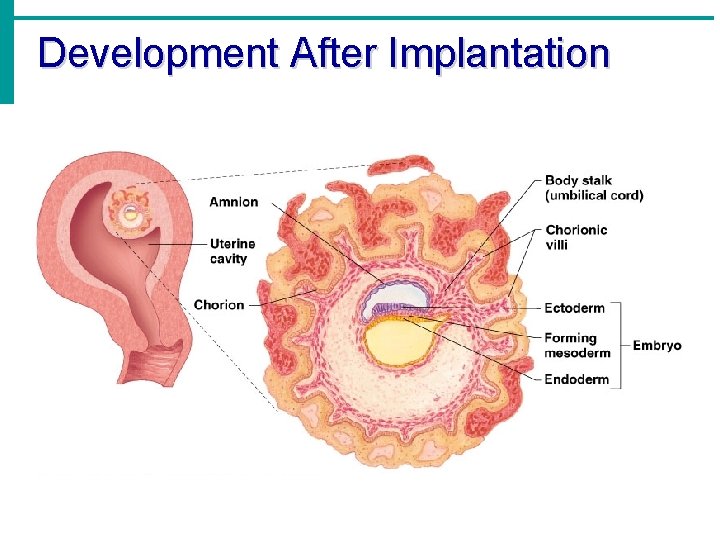
Development After Implantation Chorionic villi (projections of the blastocyst) develop Cooperate with cells of the uterus to form the placenta The embryo is surrounded by the amnion (a fluid filled sac) An umbilical cord forms to attach the embryo to the placenta Functions of placenta Forms a barrier between mother and embryo (blood is not exchanged) Delivers nutrients and oxygen Removes waste from embryonic blood Becomes an endocrine organ (produces hormones) and takes over for the corpus luteum Estrogen Progesterone
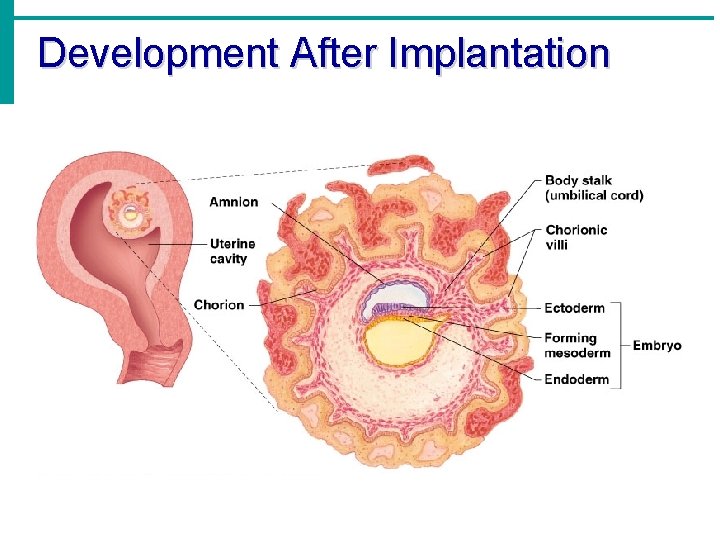
Development After Implantation
Gestation 266 days from fertilization All organ systems are formed by the end of the eighth week Anatomical changes Uterus occupies most of pelvic cavity by 3 rd month Most of abdominal cavity by end of pregnancy Abdominal organs pushed up Elevates diaphragm Widens thoracic cavity Ureters and bladder are compressed
Gestation Physiological changes General Weight gain Increase in storage of protiens, lipids and minerals Breast enlargement (lactation) Lower back pain (lordosis Cardiovascular SV and CO increase 30% HR increase 10 -15% Blood volume increase 30 -50% Edema due to compression of IVC Pulmonary changes TV & ERV increase 30 -40% Functional residual capacity decrease Oxygen consumption increases 10 -20%
Gestation Physiological changes GI changes Increased appetite More nausea, vomiting, heartburn Urinary changes Increase in frequency, urgency and incontinence Increased urine production Skin changes Increase in pigmentation
Mammary Glands Present in both sexes, but only function in females Modified sweat glands (apocrine) Function is to produce milk Stimulated by sex hormones (mostly estrogens) to increase in size Anatomy of mammary glands Areola – central pigmented area Nipple – protruding central area of areola Lobes – internal structures that radiate around nipple Composed of CT and alveoli Alveolar glands – clusters of milk producing glands within lobules Lactiferous ducts – connect alveolar glands to nipple
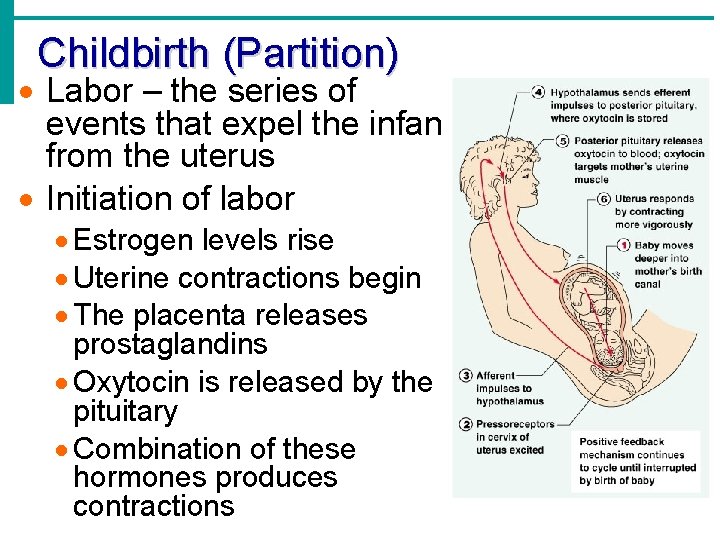
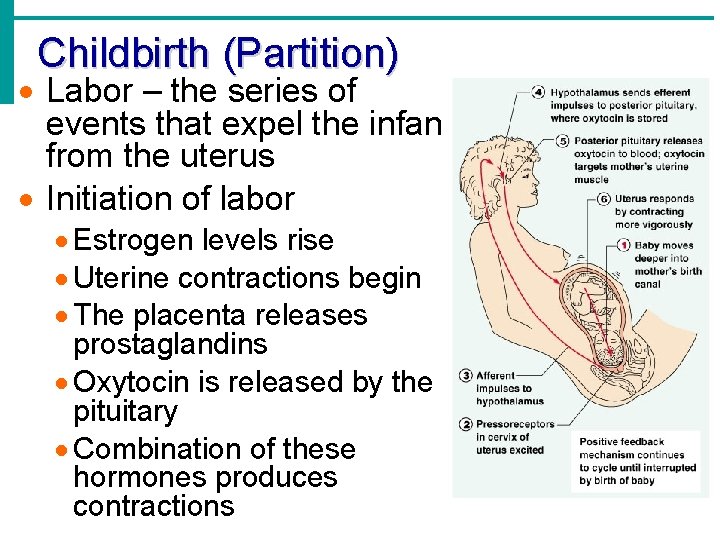
Childbirth (Partition) Labor – the series of events that expel the infant from the uterus Initiation of labor Estrogen levels rise Uterine contractions begin The placenta releases prostaglandins Oxytocin is released by the pituitary Combination of these hormones produces contractions
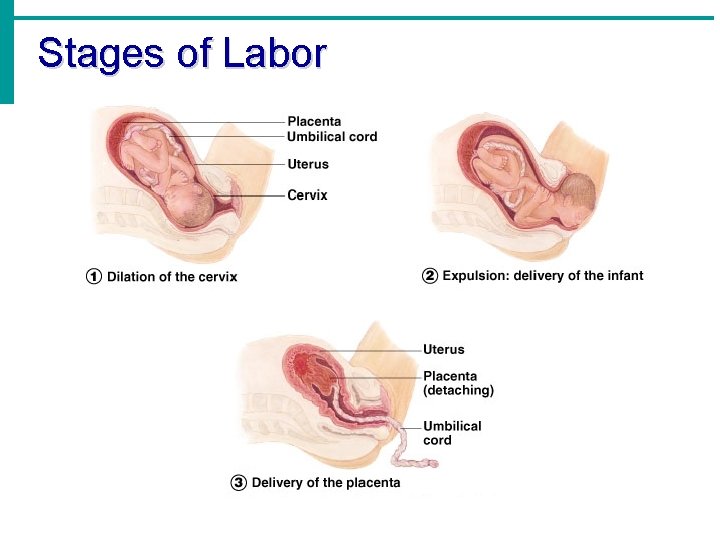
Stages of Labor Dilation Cervix becomes dilated Uterine contractions begin and increase The amnion ruptures Expulsion Infant passes through the cervix and vagina Normal delivery is head first Placental stage Delivery of the placenta
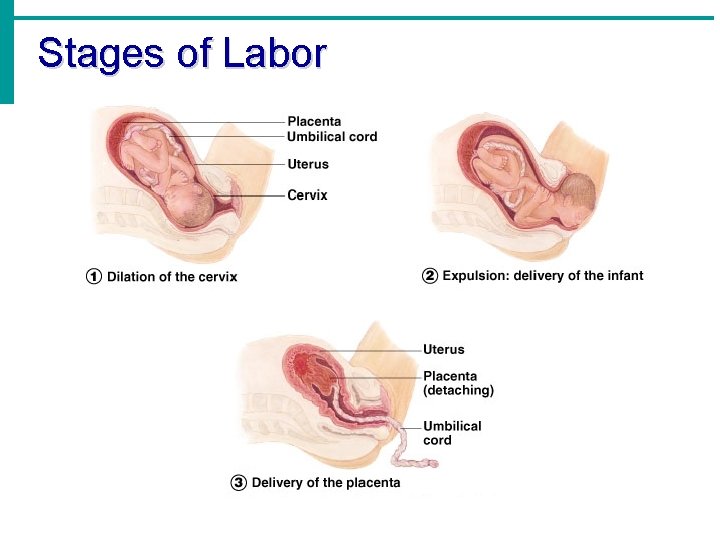
Stages of Labor
Developmental Aspects of the Reproductive System Gender is determined at fertilization Males have XY sex chromosomes Females have XX sex chromosomes Gonads do not begin to form until the eighth week
Developmental Aspects of the Reproductive System Testes form in the abdominal cavity and descend to the scrotum one month before birth The determining factor for gonad differentiation is testosterone
Developmental Aspects of the Reproductive System Reproductive system organs do not function until puberty Puberty usually begins between ages 10 and 15 The first menses usually occurs about two years after the start of puberty menarche Most women reach peak reproductive ability in their late 20 s
Developmental Aspects of the Reproductive System Menopause occurs when ovulation and menses cease entirely Ovaries stop functioning as endocrine organs There is a no equivalent of menopause in males, but there is a steady decline in testosterone
Sexually transmitted diseases AIDS Chlamidia Genital Herpes Genital Warts Gonorrhea Syphilis Hepatitis B