Effects of acupuncture for chronic pelvic pain syndrome








































- Slides: 45



























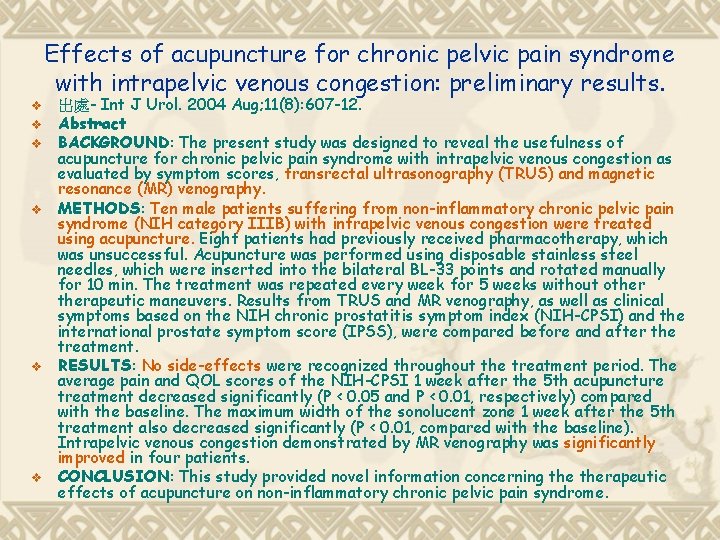
Effects of acupuncture for chronic pelvic pain syndrome with intrapelvic venous congestion: preliminary results. v v v 出處- Int J Urol. 2004 Aug; 11(8): 607 -12. Abstract BACKGROUND: The present study was designed to reveal the usefulness of acupuncture for chronic pelvic pain syndrome with intrapelvic venous congestion as evaluated by symptom scores, transrectal ultrasonography (TRUS) and magnetic resonance (MR) venography. METHODS: Ten male patients suffering from non-inflammatory chronic pelvic pain syndrome (NIH category IIIB) with intrapelvic venous congestion were treated using acupuncture. Eight patients had previously received pharmacotherapy, which was unsuccessful. Acupuncture was performed using disposable stainless steel needles, which were inserted into the bilateral BL-33 points and rotated manually for 10 min. The treatment was repeated every week for 5 weeks without otherapeutic maneuvers. Results from TRUS and MR venography, as well as clinical symptoms based on the NIH chronic prostatitis symptom index (NIH-CPSI) and the international prostate symptom score (IPSS), were compared before and after the treatment. RESULTS: No side-effects were recognized throughout the treatment period. The average pain and QOL scores of the NIH-CPSI 1 week after the 5 th acupuncture treatment decreased significantly (P < 0. 05 and P < 0. 01, respectively) compared with the baseline. The maximum width of the sonolucent zone 1 week after the 5 th treatment also decreased significantly (P < 0. 01, compared with the baseline). Intrapelvic venous congestion demonstrated by MR venography was significantly improved in four patients. CONCLUSION: This study provided novel information concerning therapeutic effects of acupuncture on non-inflammatory chronic pelvic pain syndrome.
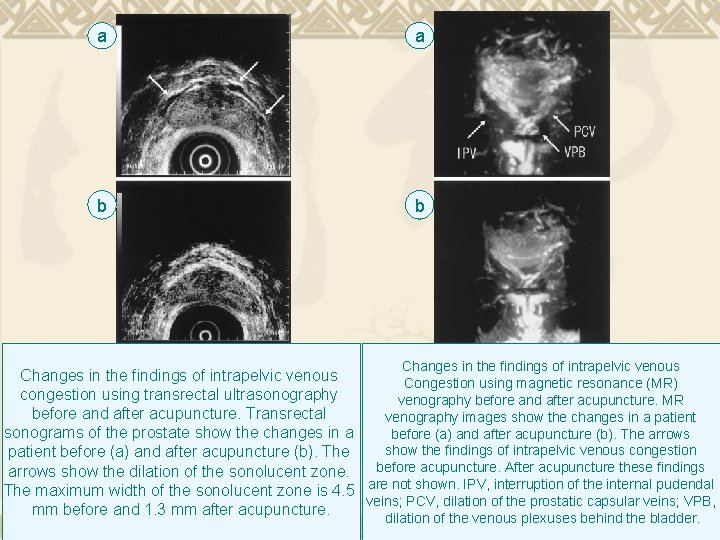
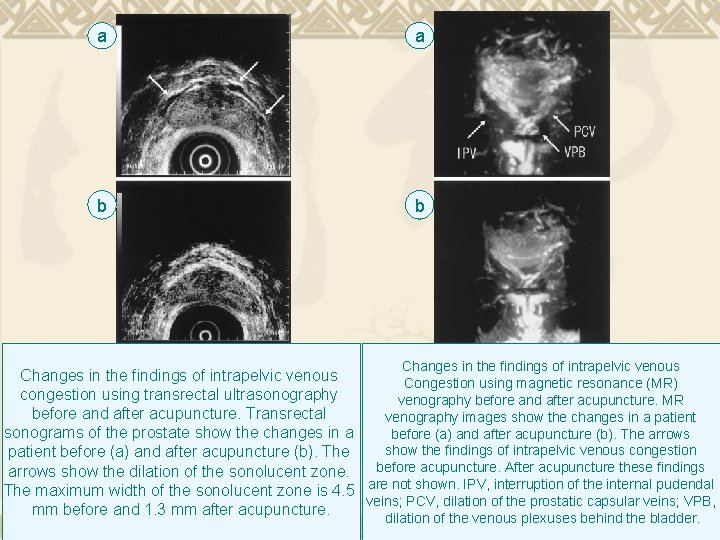
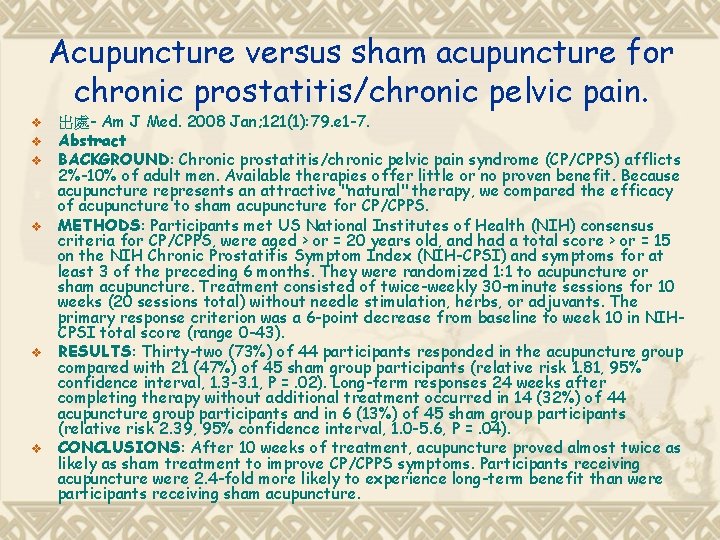
a a b b Changes in the findings of intrapelvic venous Congestion using magnetic resonance (MR) congestion using transrectal ultrasonography venography before and after acupuncture. MR before and after acupuncture. Transrectal venography images show the changes in a patient sonograms of the prostate show the changes in a before (a) and after acupuncture (b). The arrows show the findings of intrapelvic venous congestion patient before (a) and after acupuncture (b). The before acupuncture. After acupuncture these findings arrows show the dilation of the sonolucent zone. The maximum width of the sonolucent zone is 4. 5 are not shown. IPV, interruption of the internal pudendal veins; PCV, dilation of the prostatic capsular veins; VPB, mm before and 1. 3 mm after acupuncture. dilation of the venous plexuses behind the bladder.
Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. v v v 出處- Am J Med. 2008 Jan; 121(1): 79. e 1 -7. Abstract BACKGROUND: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) afflicts 2%-10% of adult men. Available therapies offer little or no proven benefit. Because acupuncture represents an attractive "natural" therapy, we compared the efficacy of acupuncture to sham acupuncture for CP/CPPS. METHODS: Participants met US National Institutes of Health (NIH) consensus criteria for CP/CPPS, were aged > or = 20 years old, and had a total score > or = 15 on the NIH Chronic Prostatitis Symptom Index (NIH-CPSI) and symptoms for at least 3 of the preceding 6 months. They were randomized 1: 1 to acupuncture or sham acupuncture. Treatment consisted of twice-weekly 30 -minute sessions for 10 weeks (20 sessions total) without needle stimulation, herbs, or adjuvants. The primary response criterion was a 6 -point decrease from baseline to week 10 in NIHCPSI total score (range 0 -43). RESULTS: Thirty-two (73%) of 44 participants responded in the acupuncture group compared with 21 (47%) of 45 sham group participants (relative risk 1. 81, 95% confidence interval, 1. 3 -3. 1, P =. 02). Long-term responses 24 weeks after completing therapy without additional treatment occurred in 14 (32%) of 44 acupuncture group participants and in 6 (13%) of 45 sham group participants (relative risk 2. 39, 95% confidence interval, 1. 0 -5. 6, P =. 04). CONCLUSIONS: After 10 weeks of treatment, acupuncture proved almost twice as likely as sham treatment to improve CP/CPPS symptoms. Participants receiving acupuncture were 2. 4 -fold more likely to experience long-term benefit than were participants receiving sham acupuncture.
Success of acupuncture in the treatment of painful bladder syndrome (interstitial cystitis) v v 出處- The Journal Of Urology Vol. 181, No. 4, Supplement, Saturday, April 25, 2009 Painful Bladder Syndrome (Interstitial Cystitis) (PBS/IC). Is an important clinical condition of unknown aetiology and affects between 0. 01% and 0. 5% of the female population. The goal of management is to ameliorate the associated pain and storage symptoms and improve quality of life. Available evidence on conservative and supportive therapy suggests limited efficacy for most therapies. Our objective was to determine how effective acupuncture is at reducing symptoms and improving quality of life in a group of individuals who had failed to respond to conventional conservative therapy.
Effectiveness of acupuncture in patients with category IIIB chronic pelvic pain syndrome: a report of 97 patients. v v v v v 出處- Pain Med. 2010 Apr; 11(4): 518 -23. Epub 2010 Jan 22. Abstract OBJECTIVE: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is of significant interest in urology and unfortunately, therapy modalities recommended are not fully effective. Therefore, we undertook a pilot study to determine whether acupuncture improves the pain, voiding symptoms, and quality of life in men with category IIIB CP/CPPS. DESIGN: Prospective, one-group trial, cohort study. SETTING: Outpatient urology clinic. PATIENTS AND INTERVENTIONS: Ninety-seven CP/CPPS patients received six sessions of acupuncture to the BL-33 acupoints once a week. The National Institute of Health Chronic Prostatitis Symptom Index (NIH-CPSI) was completed by each patient before and after the treatment and on 12 th and 24 th weeks following the treatment. OUTCOME MEASURES: Mean values of total CPSI score, pain subscore, urinary subscore, and quality of life subscore after the treatment and on follow-up after the treatment were compared with the baseline values. RESULTS: There was a statistically significant decrease in all of the subscores evaluated at all periods compared with the baseline. Eighty-six patients out of 93 (92. 47%) were NIH-CPSI responders (more than 50% decrease in total NIH-CPSI score from baseline) at the end of the treatment. CONCLUSIONS: The results of this study suggest that acupuncture appears to be a safe and potentially effective treatment in improving the symptoms and quality of life of men clinically diagnosed with CP/CPPS.













 Pelvic girdle pain
Pelvic girdle pain Pelvic pain meaning
Pelvic pain meaning Scapular pain
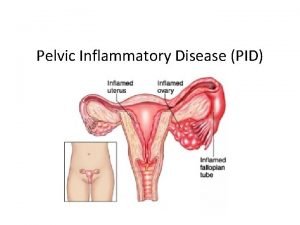
Scapular pain Pelvic inflammatory disease
Pelvic inflammatory disease Carmen bove
Carmen bove Thoracic facet joint pain referral patterns
Thoracic facet joint pain referral patterns Chronic pain definition
Chronic pain definition Chronic pain comorbidities
Chronic pain comorbidities Chronic coronary syndrome
Chronic coronary syndrome Pms symptoms
Pms symptoms Symptoms before period
Symptoms before period Lewis mad pain and martian pain
Lewis mad pain and martian pain Liao yuan
Liao yuan Liv3lo
Liv3lo Site:slidetodoc.com
Site:slidetodoc.com Acupuncture
Acupuncture Saam korean
Saam korean Kung fu panda acupuncture
Kung fu panda acupuncture Acupuncture for eating disorders
Acupuncture for eating disorders Al500 acupuncture laser
Al500 acupuncture laser What are pelvic fins
What are pelvic fins Pelvic inflammatory disease men
Pelvic inflammatory disease men Outlet of pelvis
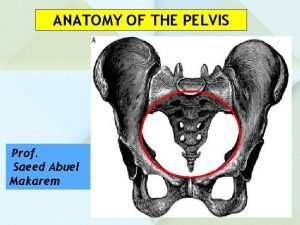
Outlet of pelvis Inlet outlet pelvis
Inlet outlet pelvis Ischiorectal fossa boundaries
Ischiorectal fossa boundaries Diameters of fetal skull
Diameters of fetal skull Pelvic traction weight calculation
Pelvic traction weight calculation Site:slidetodoc.com
Site:slidetodoc.com Internal iliac branches mnemonic
Internal iliac branches mnemonic Empty scrotum
Empty scrotum Bones of pelvic girdle
Bones of pelvic girdle Femoral triangle
Femoral triangle Fetal brow
Fetal brow Superior ramus of pubis
Superior ramus of pubis Muscles in the perineum
Muscles in the perineum Anterior view of right hand
Anterior view of right hand Pelvic splanchnic nerves
Pelvic splanchnic nerves Süleyman deniz sezer
Süleyman deniz sezer Concept map bones of the pelvic girdle
Concept map bones of the pelvic girdle What are the abnormal types of pelvis
What are the abnormal types of pelvis Submentovertical diameter of fetal skull
Submentovertical diameter of fetal skull Pelvis minor major
Pelvis minor major Pelvic exenteration surgery
Pelvic exenteration surgery Pelvic ultrasound
Pelvic ultrasound Leopold's maneuver
Leopold's maneuver Anterior thoracic tender points
Anterior thoracic tender points