Pelvic pain Prof Dr Rachana Saha Pain is




- Slides: 35
Pelvic pain Prof. Dr. Rachana Saha
• Pain is unpleasant sensory and emotional experience associated with actual or potential tissue damage. • Actually a protective mechanism • Two types: - 1. Acute 2. Chronic
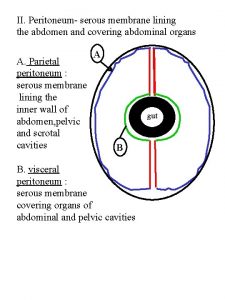
Neurophysiology of pain 1. somatic(somatic nervous system) 2. viscera(autonomic nervous system)
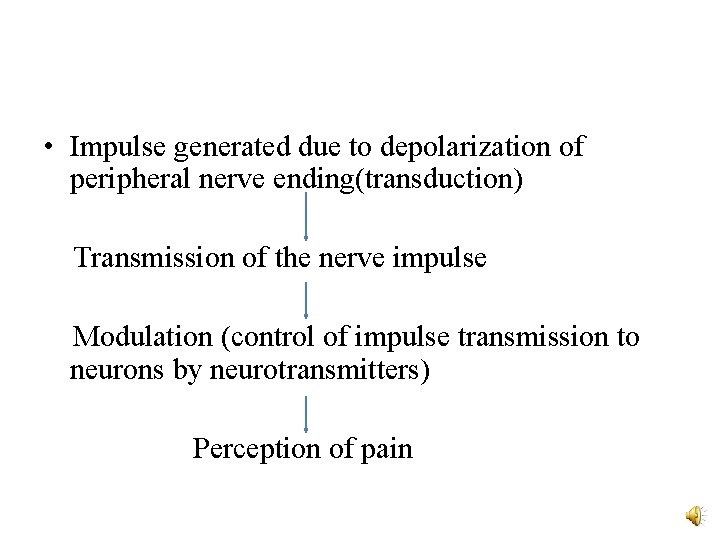
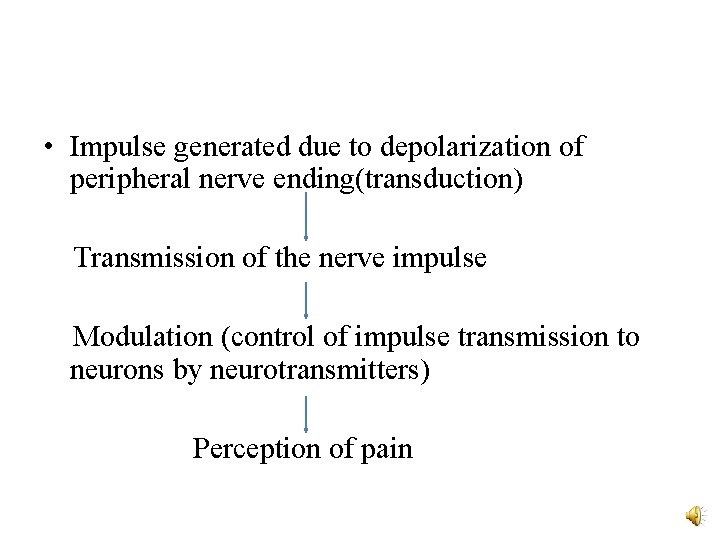
• Impulse generated due to depolarization of peripheral nerve ending(transduction) Transmission of the nerve impulse Modulation (control of impulse transmission to neurons by neurotransmitters) Perception of pain

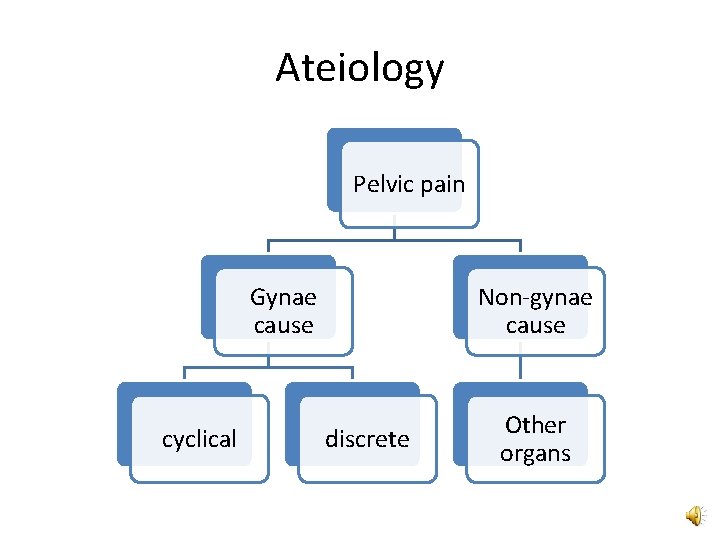
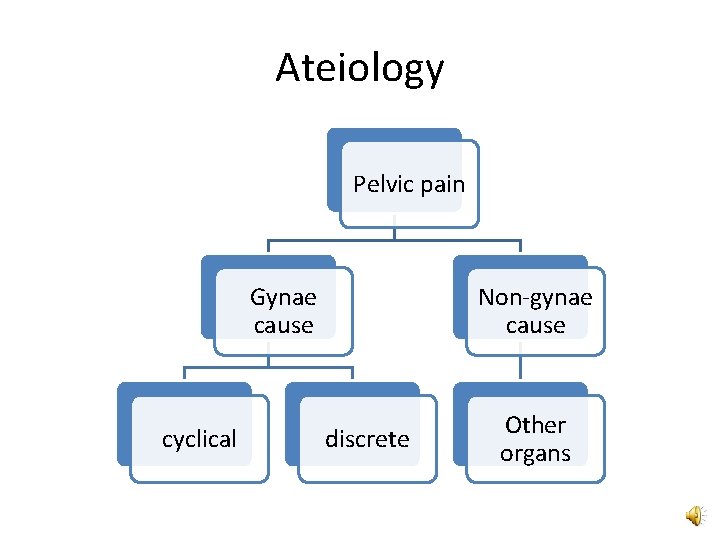
Ateiology Pelvic pain Gynae cause cyclical Non-gynae cause discrete Other organs
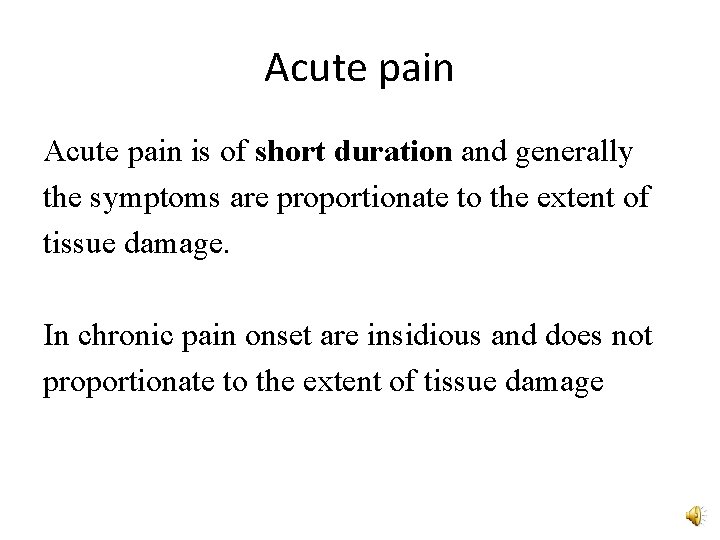
Acute pain is of short duration and generally the symptoms are proportionate to the extent of tissue damage. In chronic pain onset are insidious and does not proportionate to the extent of tissue damage
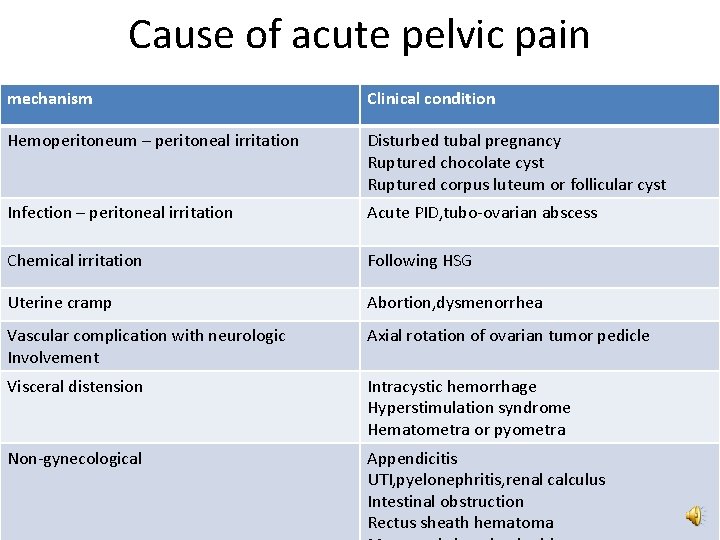
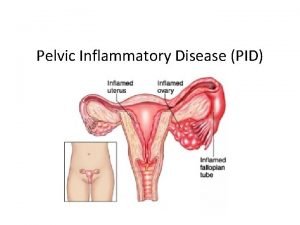
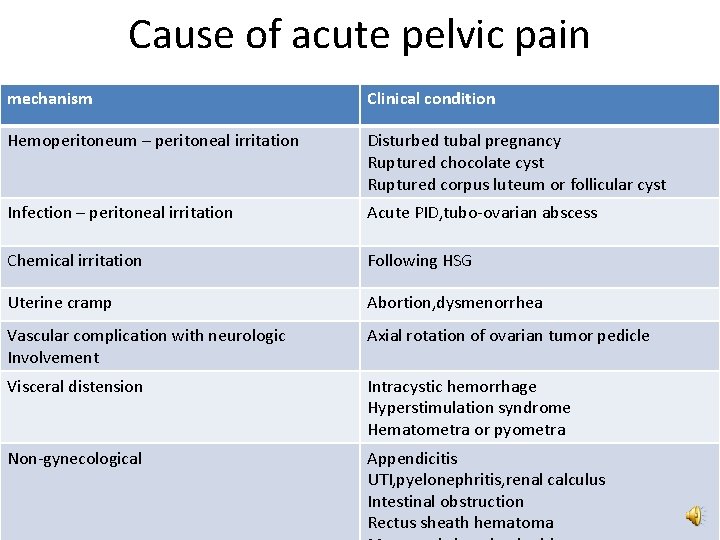
Cause of acute pelvic pain mechanism Clinical condition Hemoperitoneum – peritoneal irritation Disturbed tubal pregnancy Ruptured chocolate cyst Ruptured corpus luteum or follicular cyst Infection – peritoneal irritation Acute PID, tubo-ovarian abscess Chemical irritation Following HSG Uterine cramp Abortion, dysmenorrhea Vascular complication with neurologic Involvement Axial rotation of ovarian tumor pedicle Visceral distension Intracystic hemorrhage Hyperstimulation syndrome Hematometra or pyometra Non-gynecological Appendicitis UTI, pyelonephritis, renal calculus Intestinal obstruction Rectus sheath hematoma
Diagnosis • History taking and examination (systemic, abdominal and pelvic).
Guideline in clinical diagnosis: • Pain of gynecologic origin usually starts in lower abdomen and then spread to whole abdomen. • Pain preceded by amenorrhea is usually obstetrically related—disturbed ectopic pregnancy should be kept in mind. • Anorexia, nausea and vomiting are usually correlated well with gastrointestinal.
• Fever with chills and rigor is most often associated with acute pelvic inflammatory disease (PID). • Pain with syncopal attacks with collapse suggests intraperitoneal hemorrhage. • Abdominopelvic lump along with more or less stable vital signs points towards complicated pelvic tumor.
• Frequency of micturition, dysuria with or without fever point to the diagnosis of urinary tract infection. • Localized pain on anterior abdominal wall is often due to nerve entrapment or musculo fascial pain.
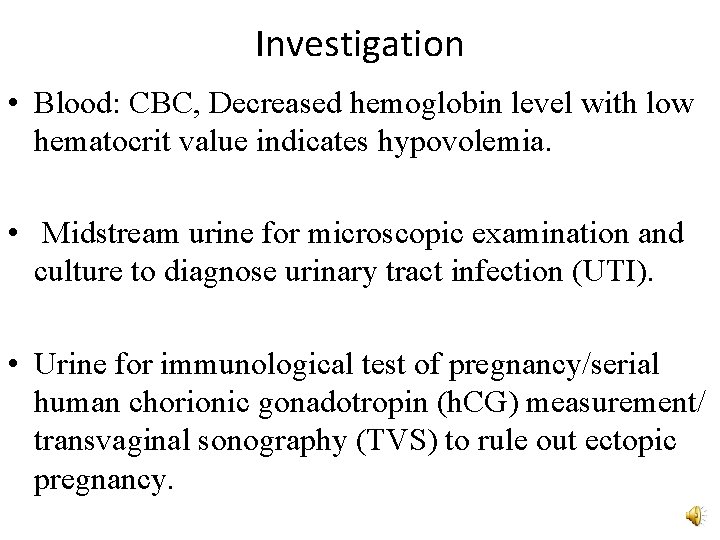
Investigation • Blood: CBC, Decreased hemoglobin level with low hematocrit value indicates hypovolemia. • Midstream urine for microscopic examination and culture to diagnose urinary tract infection (UTI). • Urine for immunological test of pregnancy/serial human chorionic gonadotropin (h. CG) measurement/ transvaginal sonography (TVS) to rule out ectopic pregnancy.
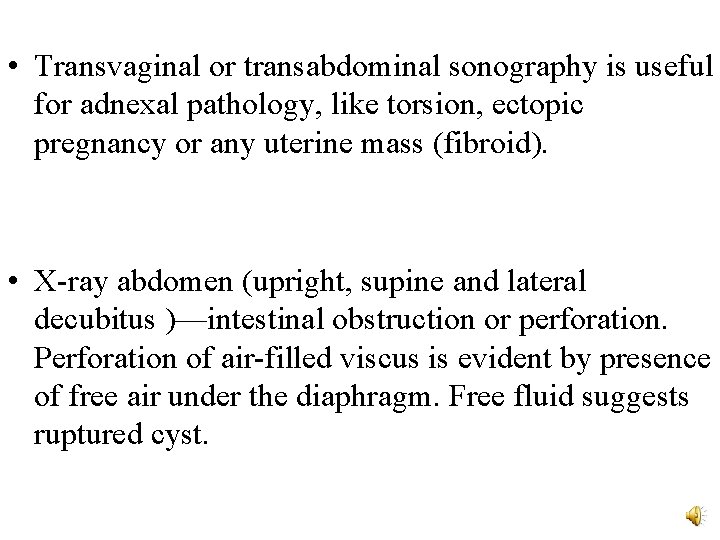
• Transvaginal or transabdominal sonography is useful for adnexal pathology, like torsion, ectopic pregnancy or any uterine mass (fibroid). • X-ray abdomen (upright, supine and lateral decubitus )—intestinal obstruction or perforation. Perforation of air-filled viscus is evident by presence of free air under the diaphragm. Free fluid suggests ruptured cyst.
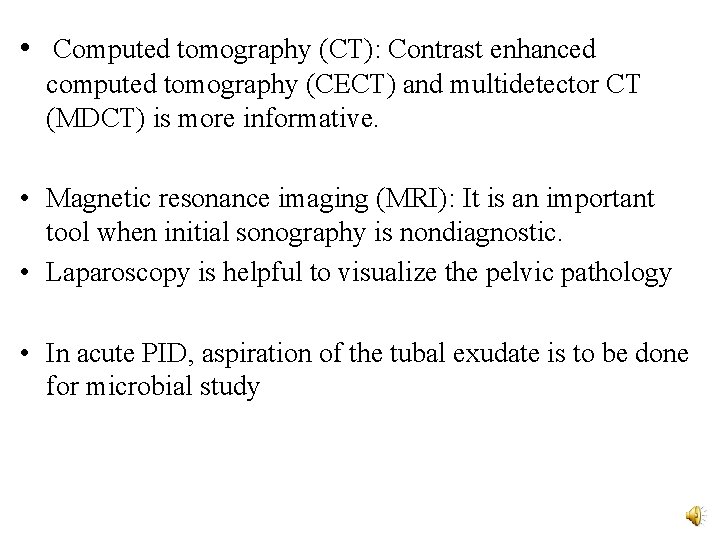
• Computed tomography (CT): Contrast enhanced computed tomography (CECT) and multidetector CT (MDCT) is more informative. • Magnetic resonance imaging (MRI): It is an important tool when initial sonography is nondiagnostic. • Laparoscopy is helpful to visualize the pelvic pathology • In acute PID, aspiration of the tubal exudate is to be done for microbial study
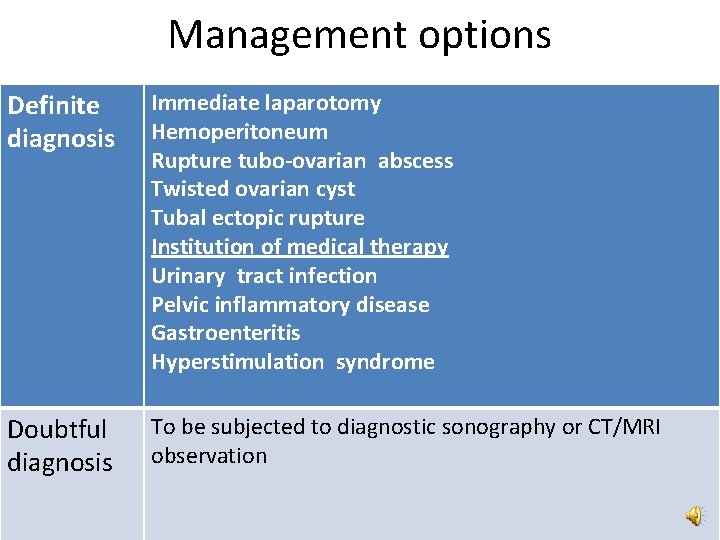
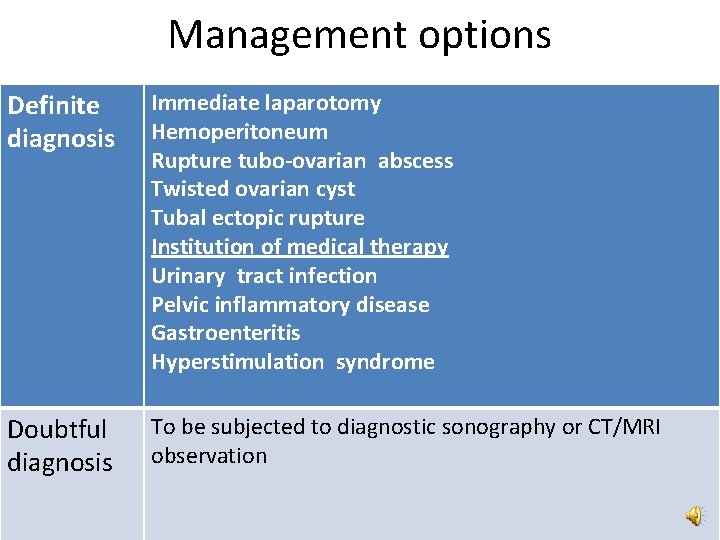
Management options Definite diagnosis Immediate laparotomy Hemoperitoneum Rupture tubo-ovarian abscess Twisted ovarian cyst Tubal ectopic rupture Institution of medical therapy Urinary tract infection Pelvic inflammatory disease Gastroenteritis Hyperstimulation syndrome Doubtful diagnosis To be subjected to diagnostic sonography or CT/MRI observation
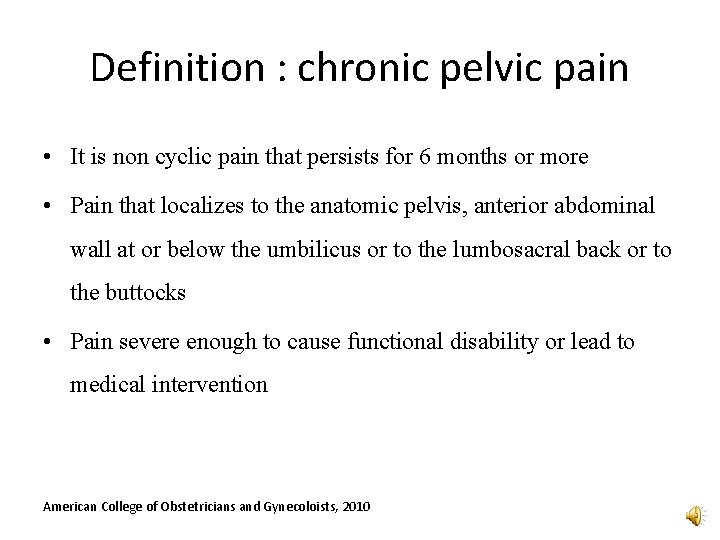
Definition : chronic pelvic pain • It is non cyclic pain that persists for 6 months or more • Pain that localizes to the anatomic pelvis, anterior abdominal wall at or below the umbilicus or to the lumbosacral back or to the buttocks • Pain severe enough to cause functional disability or lead to medical intervention American College of Obstetricians and Gynecoloists, 2010
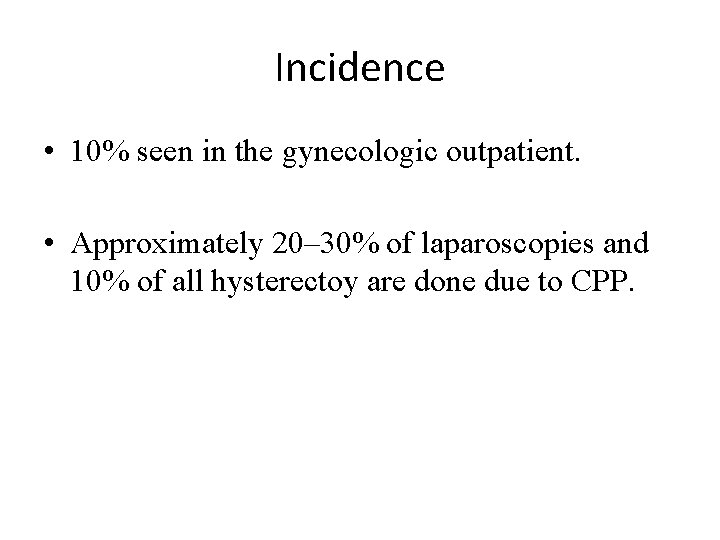
Incidence • 10% seen in the gynecologic outpatient. • Approximately 20– 30% of laparoscopies and 10% of all hysterectoy are done due to CPP.


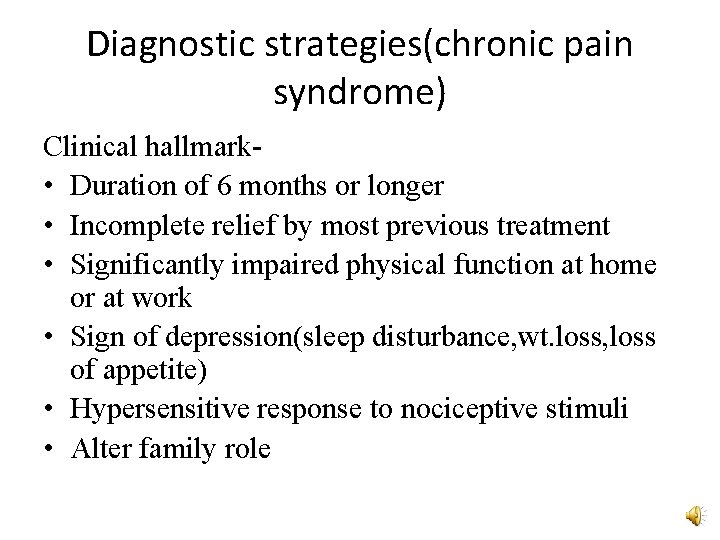
Diagnostic strategies(chronic pain syndrome) Clinical hallmark • Duration of 6 months or longer • Incomplete relief by most previous treatment • Significantly impaired physical function at home or at work • Sign of depression(sleep disturbance, wt. loss, loss of appetite) • Hypersensitive response to nociceptive stimuli • Alter family role
Evaluation : HISTORY TAKING 1. Gyneologic causes: abnormal vaginal bleeding , abnormal vaginal discharge, dysmenorrhea , dyspareunia , subfertility, sexual functioning 1. Urologic causes: urgency , frequency, nocturia, hesitancy, dysuria, hematuria, incontinence
3. Enterocolic Causes: constipation, diarrhea, flatuence, hematochezia, relationship of pain to times of altered bowel function or form and pain relief with bowel movement 4. Musculoskeletal/ neuropathic Causes : physical trauma – surgical (episiotomy, pfannensteil ) or injury , exacerbation with exercise or postural changes , weakness, numbness
5. Psychological causes : previous diagnosis , hospitalization, medications, current depression , anxiety, panic , suicidal ideation, past and current emotional , physical or sexual trauma
PHYSICAL EXAMINATION • Stance and gait • Presence of any mass , hernias • Carnett sign (increase tenderness when palpation done in abdomen wall flexion) to differentiated nerve entrapment pain which is may be due to entrapment of ilioinguinal, iliohypogastric or genitofemoral nerve. • Local examination to rule out vulval/ vestibular causes
• Single digit examination – pelvic floor muscles, anterior vaginal wall , cervical motion tenderness • Speculum examination • Bimanual examination – size , uniformity , mobility, adnexal tenderness or mass • Rectal examination , rectovaginal palapation
• Pessary test: In mobile retroverted uterus or slight degree of uterine descent. The pessary is inserted and kept for 3 months. If the symptoms are relieved, the diagnosis is certain and surgical correction is advisable. • Combined oral contraceptive pills: Functional ovarian cyst producing CPP are given cyclic oral contraceptive (OC) for 3 months.
• Transcutaneous electric nerve stimulation (TENS) : - Inhibit the transmissioin of nerve impulse via unmyelinated fibers. • Pain mapping is useful specially in assessment of adhesions. • Nongynecological disorders mostly related with disorders of bowel (spastic colon, irritable bowel syndrome). • Spasm or rigidity of muscles specially those of vertebral column suggests orthopedic, neurologic or rheumatic lesion.
• CPP without any organic lesion: usually in parous and perimenopausal, may be due to pelvic congestion, or may be due to psychosomatic disturbances. • Pelvic congestion syndrome (Taylor syndrome) is characterized by chronic pelvic pain, dyspareunia, abnormal uterine bleeding along with pelvic venous congestion.
INVESTIGATIONS 1. Urine routine and culture 2. Thryoid function (affects function of bowel and bladder) 3. Blood sugar levels (diabetic neuropathy), complete hemogram 4. Cervical and vaginal discharge(hanging drop preparation, gram stain and culture): - for diagnosis of PID. 5. Endometrial biopsy: -genital tuberculosis
6. Sonography of pelvic organs : endometriomas, leiomyomas, dilated veins , adnexal masses 7. Cystocopy 8. Colonosccopy, sigmoidoscopy 9. Laparascopy- (invaluable diagnostic tool and negative finding also have got value to assures the clinician that no abnormality exists. ) 10. X-rays of lumbosacral region and hip joints helps to detect orthopedic lesions 11. CT scan or MRI are less commonly used in the diagnosis of CPP except in malignant conditions.
TREATMENT MEDICAL OPTIONS: 1. For pain relief NSAIDS( ibuprofen, naproxen, COX 2 inhibitors- celecoxib) Opioids: codeine, methadone Antidepressants (Neurolytic agents: - tricyclic agent: Amitriptyline, imipramine , SSRI: - sertraline, fluxetine, paroxentine Anticonvulsants: - gabapentine carbamazepine Cognitive behaviour therapy Acupuncture
2. For hormone suppression(young patients with minimal endometriosis, spasmodic dysmenorrhea or midmenstrual pain) progesterones Oral contraceptive pills gonadotrophin releasing hormone agonist
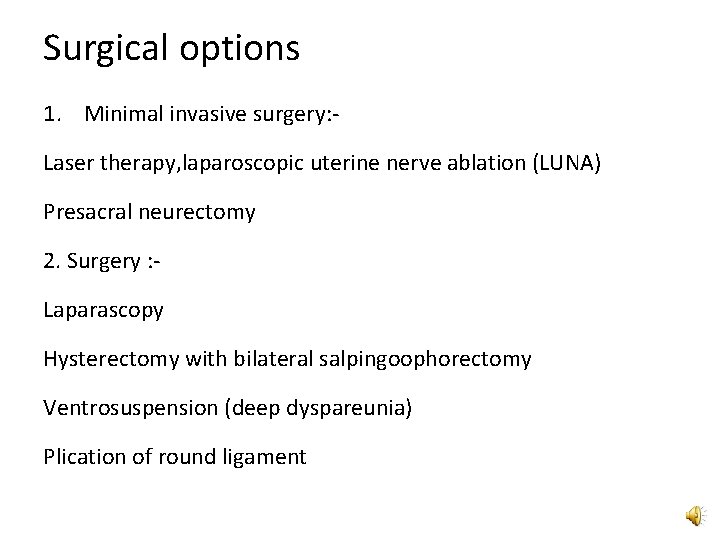
Surgical options 1. Minimal invasive surgery: Laser therapy, laparoscopic uterine nerve ablation (LUNA) Presacral neurectomy 2. Surgery : Laparascopy Hysterectomy with bilateral salpingoophorectomy Ventrosuspension (deep dyspareunia) Plication of round ligament

THANK YOU
 Uchicago globus
Uchicago globus Rachana balasubramanian
Rachana balasubramanian Pelvic inflammatory disease
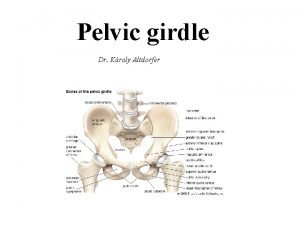
Pelvic inflammatory disease Pelvic girdle pain
Pelvic girdle pain Pelvic pain meaning
Pelvic pain meaning Scapular pain
Scapular pain Saha equation
Saha equation Scalede
Scalede Dr prantik saha
Dr prantik saha Saha gözlem ziyaretleri
Saha gözlem ziyaretleri Ece404 github
Ece404 github Tsg export sa
Tsg export sa Hentbol saha ölçüleri
Hentbol saha ölçüleri Riya saha shah
Riya saha shah Dr soma saha
Dr soma saha Beyzbol sahası ölçüleri
Beyzbol sahası ölçüleri Voleybol direk ölçüleri
Voleybol direk ölçüleri Voleybolda çift vuruş
Voleybolda çift vuruş Eskrim kaç metre uzunluğunda bir pistte oynanır?
Eskrim kaç metre uzunluğunda bir pistte oynanır? Saha chapter 1
Saha chapter 1 Suranjana saha
Suranjana saha Suranjana saha
Suranjana saha Absorption coefficient formula
Absorption coefficient formula Kalimah jeung nanyakeun tempat nyaeta
Kalimah jeung nanyakeun tempat nyaeta Am i getting my period or am i pregnant
Am i getting my period or am i pregnant Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Lewis mad pain and martian pain
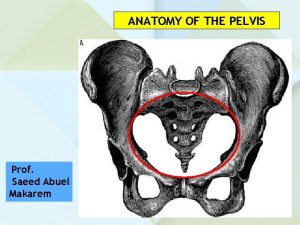
Lewis mad pain and martian pain Smallest anteroposterior diameter of the pelvic inlet
Smallest anteroposterior diameter of the pelvic inlet Pelvic mass pictures
Pelvic mass pictures Pelvis origin
Pelvis origin Pelvis minor and major
Pelvis minor and major What are pelvic fins
What are pelvic fins Dr mary bove
Dr mary bove Inlet outlet view
Inlet outlet view Pelvic wall
Pelvic wall Anal canal
Anal canal