Degenerative Spine Disorders Department of Neurosurgery Faculty of


- Slides: 56
Degenerative Spine Disorders Department of Neurosurgery Faculty of Medicine, Alexandria University
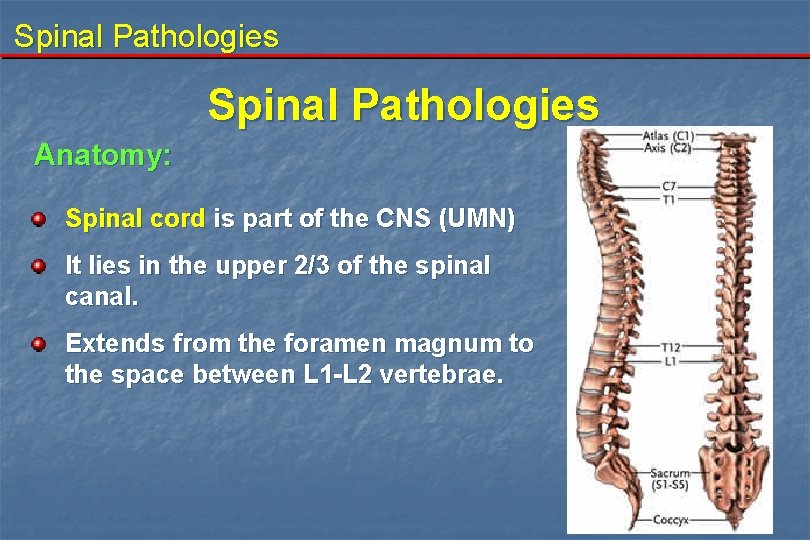
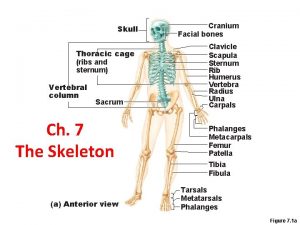
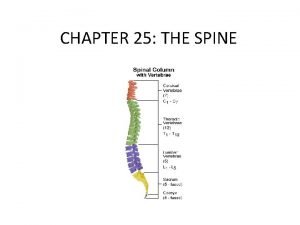
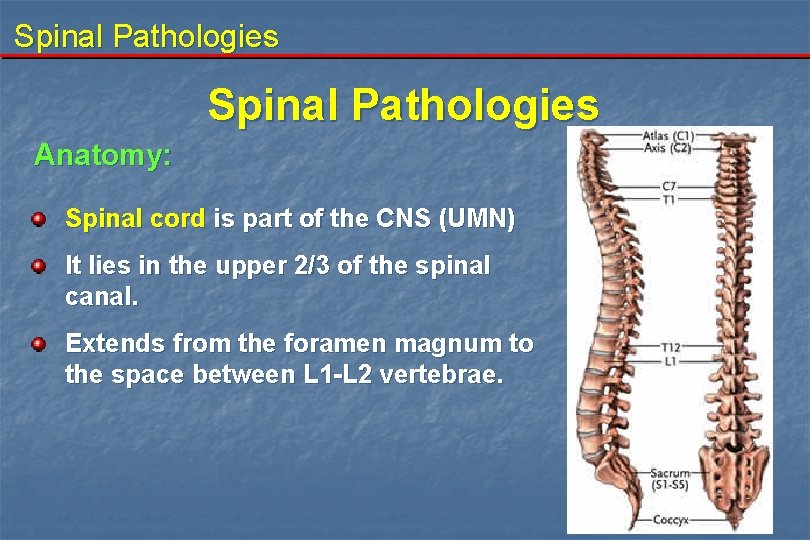
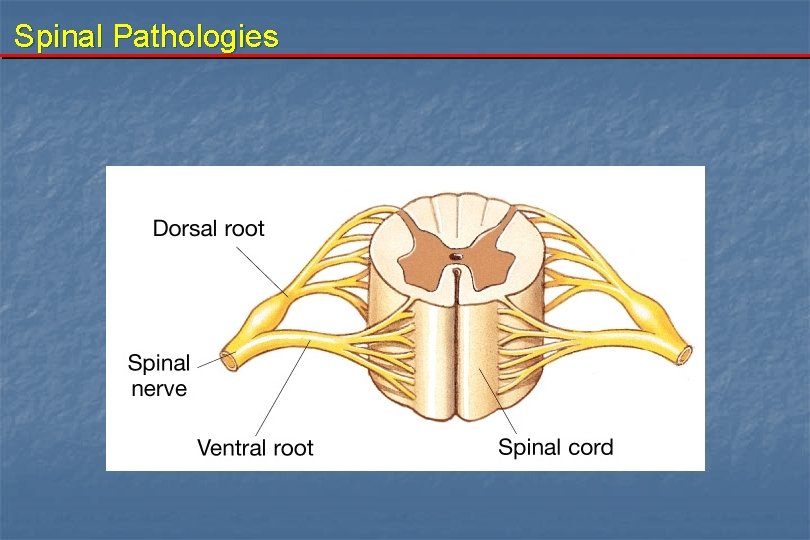
Spinal Pathologies Anatomy: Spinal cord is part of the CNS (UMN) It lies in the upper 2/3 of the spinal canal. Extends from the foramen magnum to the space between L 1 -L 2 vertebrae.
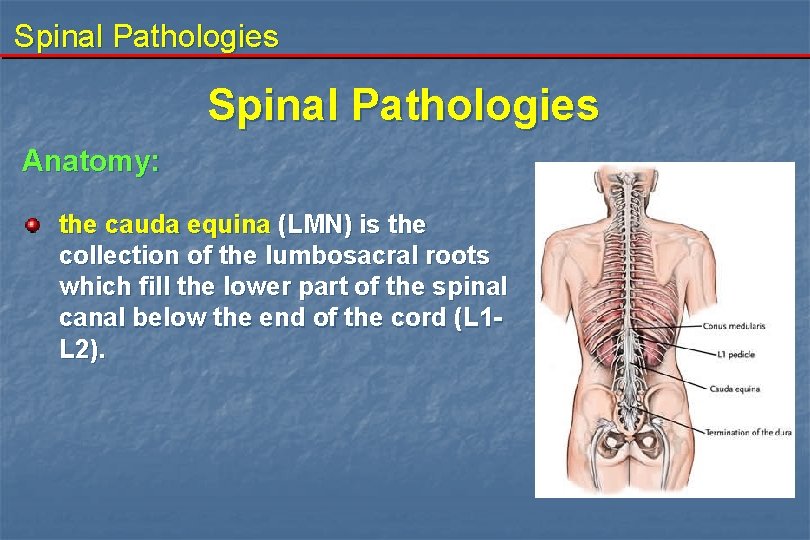
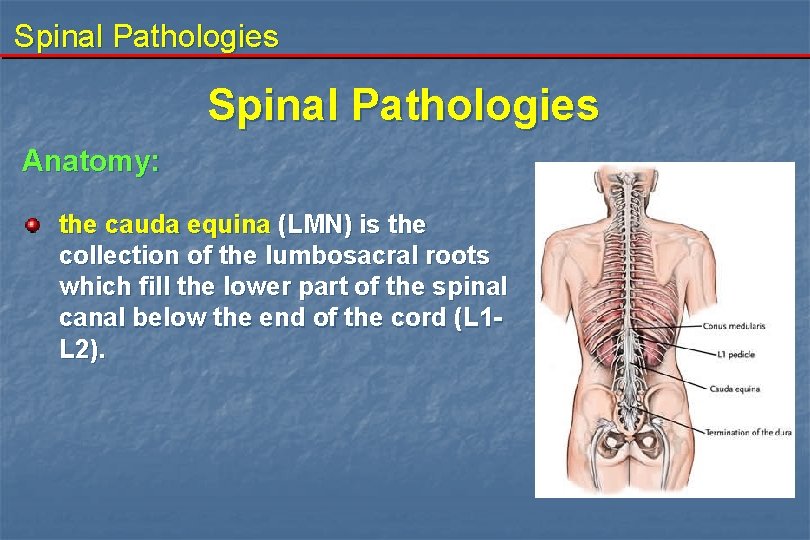
Spinal Pathologies Anatomy: the cauda equina (LMN) is the collection of the lumbosacral roots which fill the lower part of the spinal canal below the end of the cord (L 1 L 2).
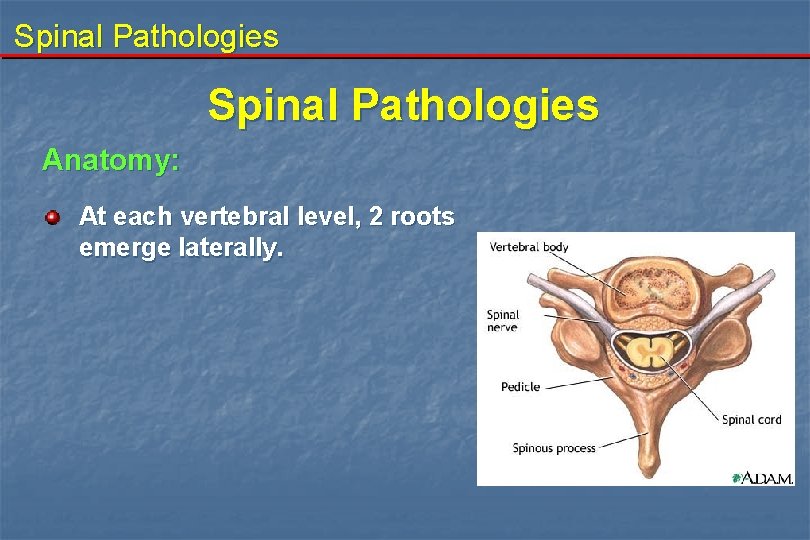
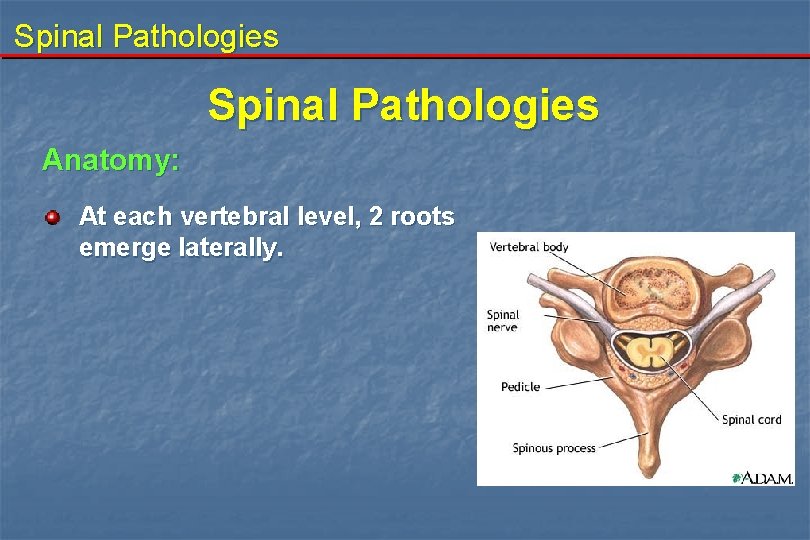
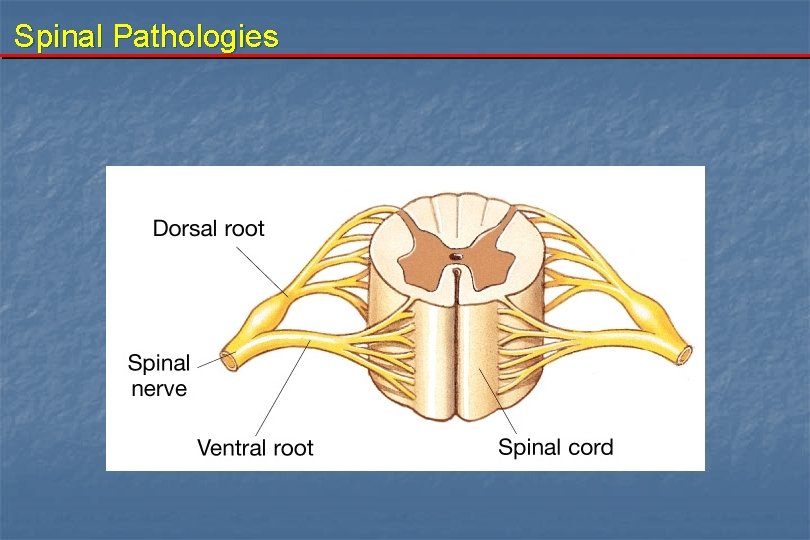
Spinal Pathologies Anatomy: At each vertebral level, 2 roots emerge laterally.
Spinal Pathologies
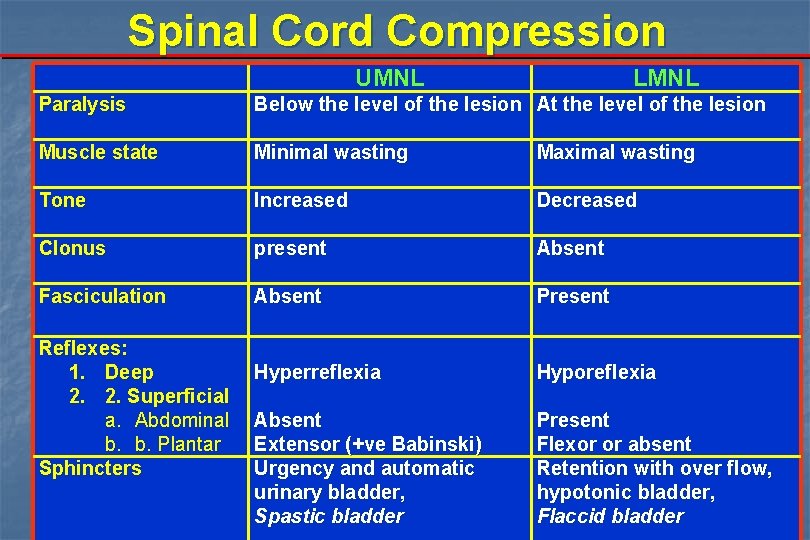
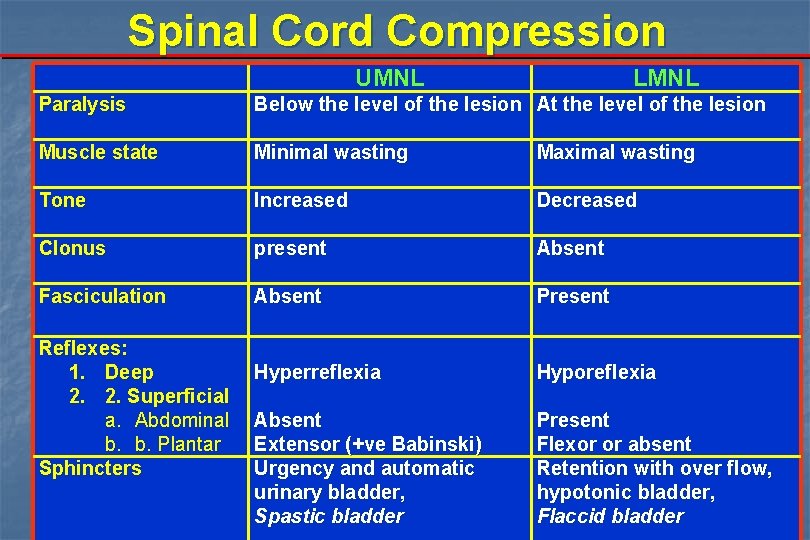
Spinal Cord Compression UMNL LMNL Paralysis Below the level of the lesion At the level of the lesion Muscle state Minimal wasting Maximal wasting Tone Increased Decreased Clonus present Absent Fasciculation Absent Present Hyperreflexia Hyporeflexia Absent Extensor (+ve Babinski) Urgency and automatic urinary bladder, Spastic bladder Present Flexor or absent Retention with over flow, hypotonic bladder, Flaccid bladder Reflexes: 1. Deep 2. 2. Superficial a. Abdominal b. b. Plantar Sphincters
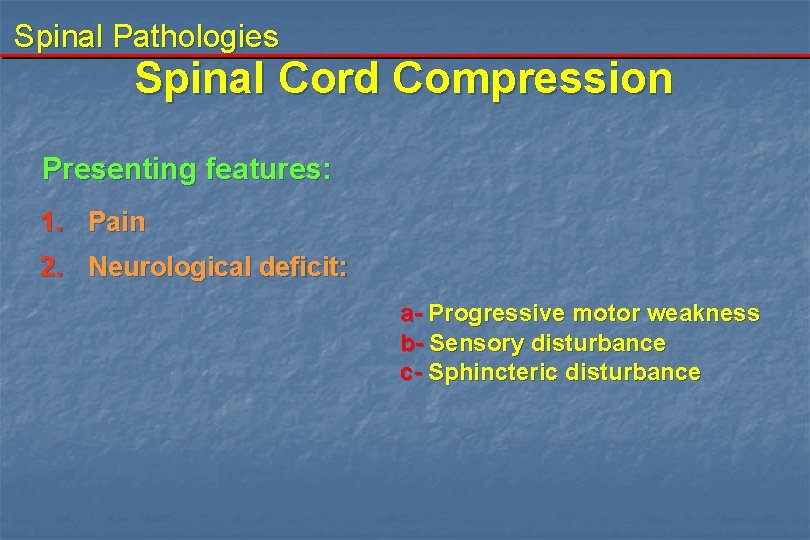
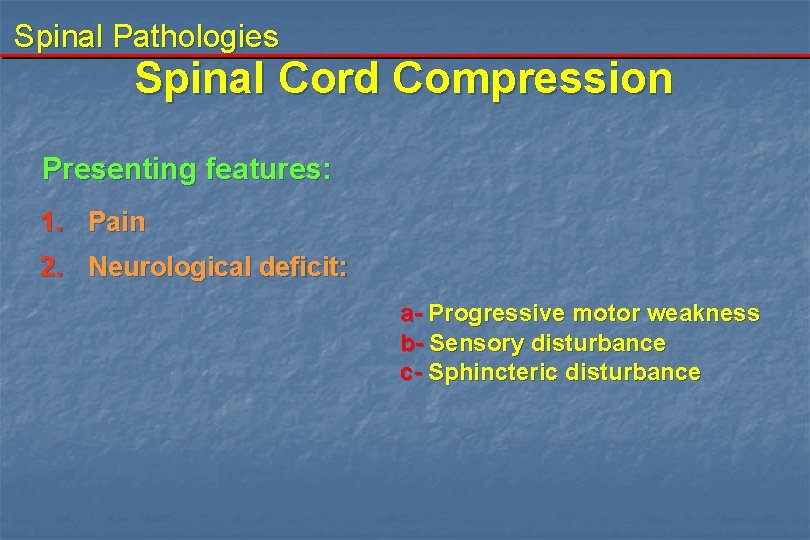
Spinal Pathologies Spinal Cord Compression Presenting features: 1. Pain 2. Neurological deficit: a- Progressive motor weakness b- Sensory disturbance c- Sphincteric disturbance
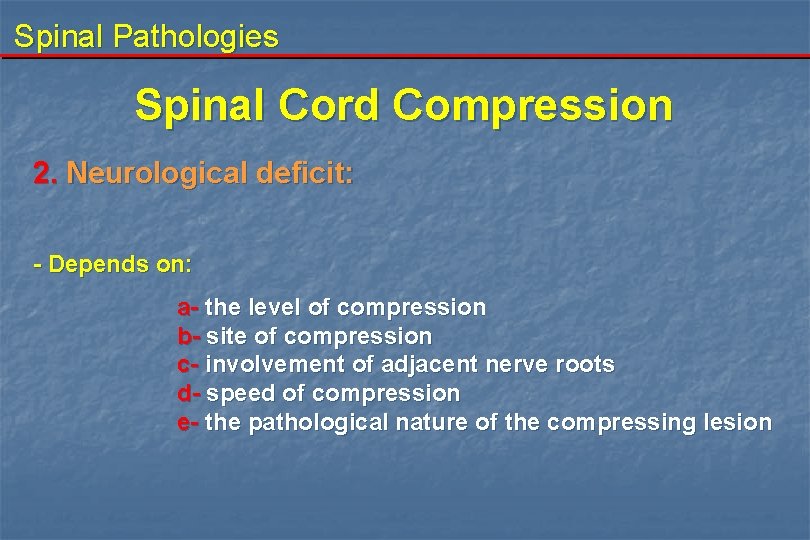
Spinal Pathologies Spinal Cord Compression 2. Neurological deficit: - Depends on: a- the level of compression b- site of compression c- involvement of adjacent nerve roots d- speed of compression e- the pathological nature of the compressing lesion
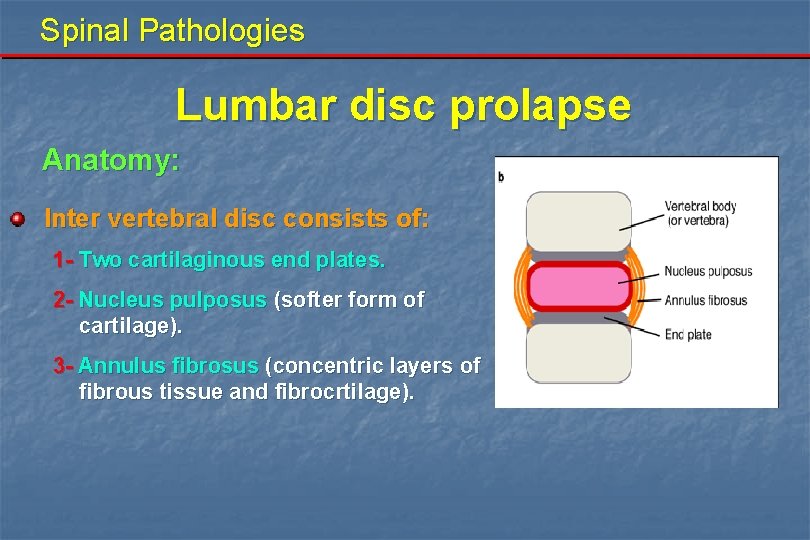
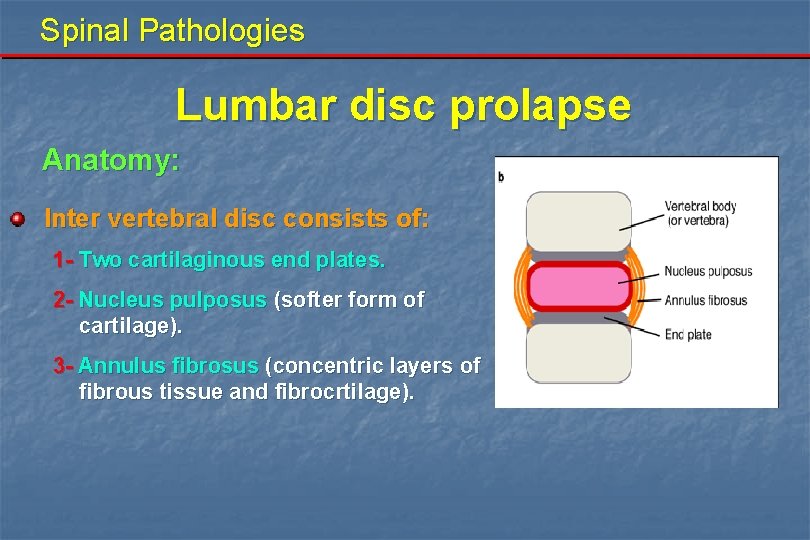
Spinal Pathologies Lumbar disc prolapse Anatomy: Inter vertebral disc consists of: 1 - Two cartilaginous end plates. 2 - Nucleus pulposus (softer form of cartilage). 3 - Annulus fibrosus (concentric layers of fibrous tissue and fibrocrtilage).
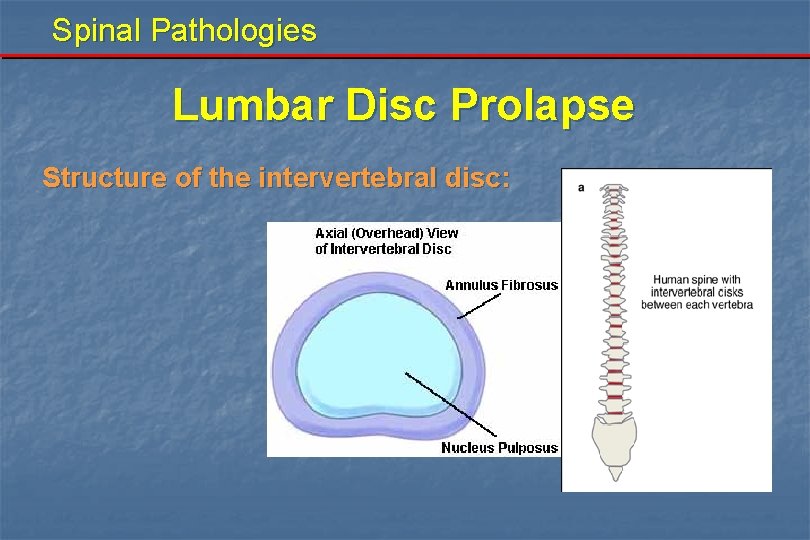
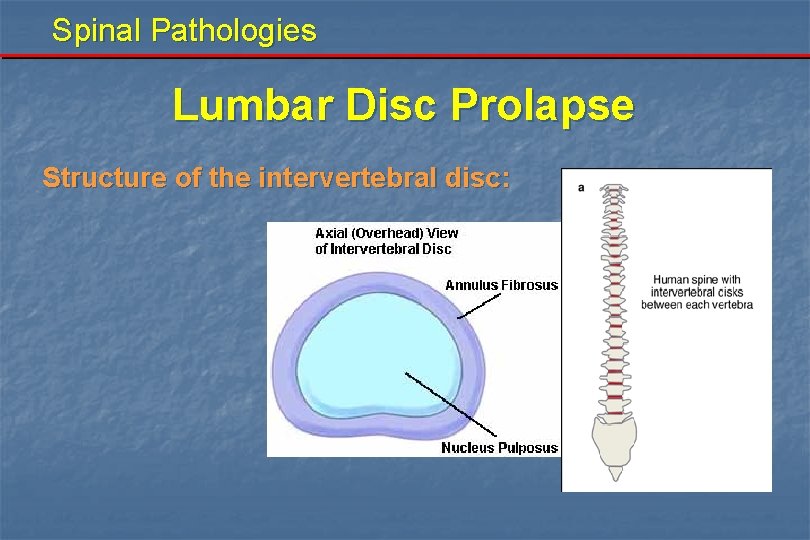
Spinal Pathologies Lumbar Disc Prolapse Structure of the intervertebral disc:
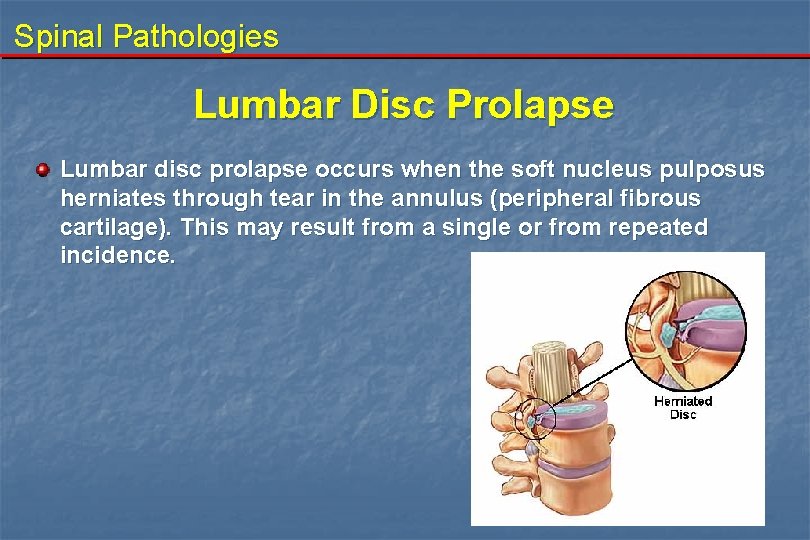
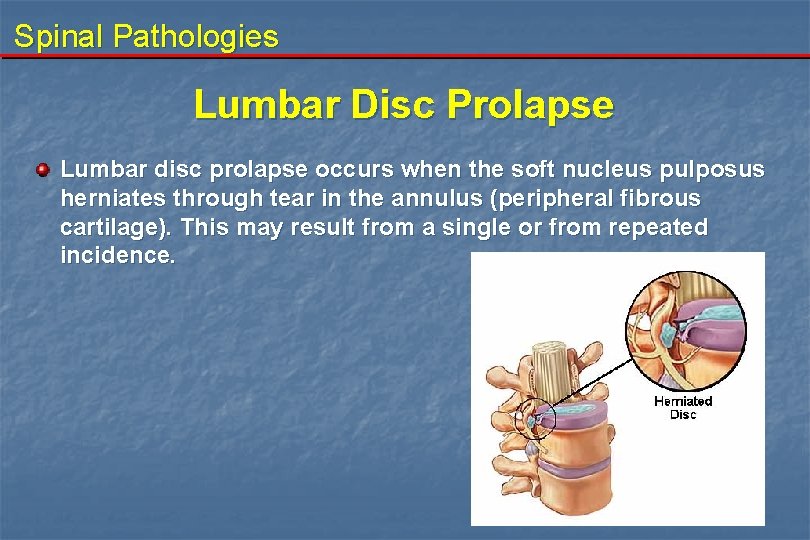
Spinal Pathologies Lumbar Disc Prolapse Lumbar disc prolapse occurs when the soft nucleus pulposus herniates through tear in the annulus (peripheral fibrous cartilage). This may result from a single or from repeated incidence.
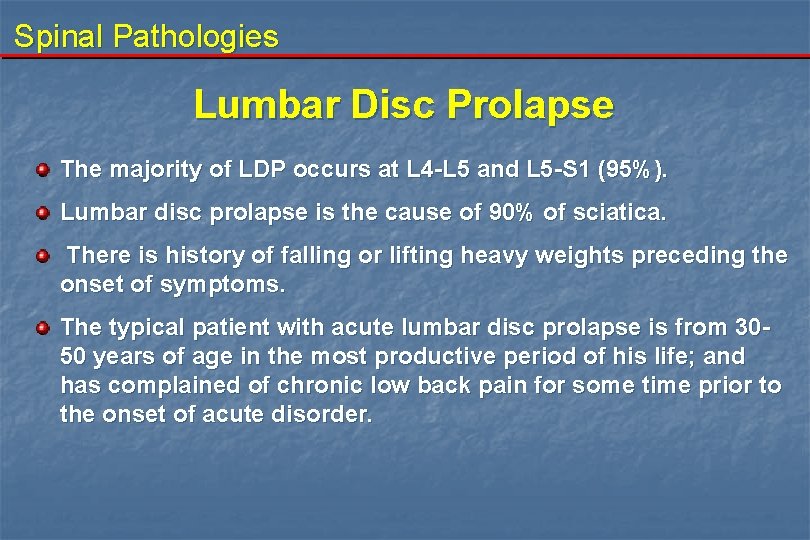
Spinal Pathologies Lumbar Disc Prolapse The majority of LDP occurs at L 4 -L 5 and L 5 -S 1 (95%). Lumbar disc prolapse is the cause of 90% of sciatica. There is history of falling or lifting heavy weights preceding the onset of symptoms. The typical patient with acute lumbar disc prolapse is from 3050 years of age in the most productive period of his life; and has complained of chronic low back pain for some time prior to the onset of acute disorder.
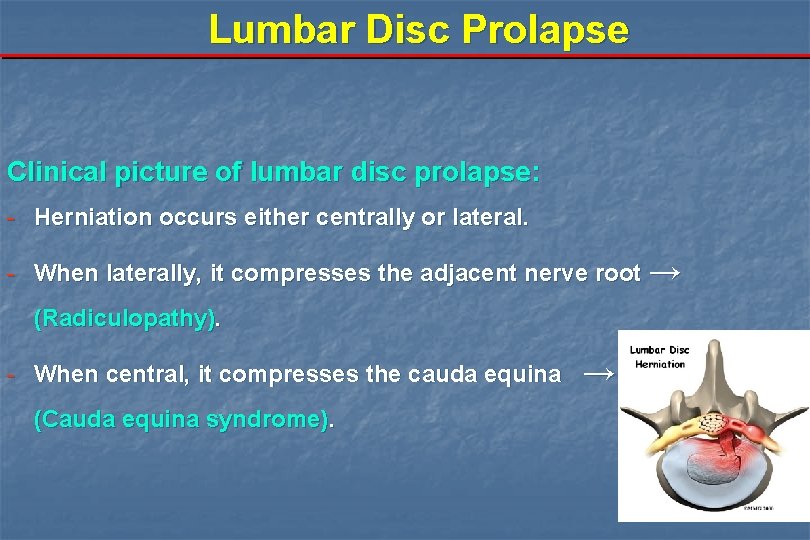
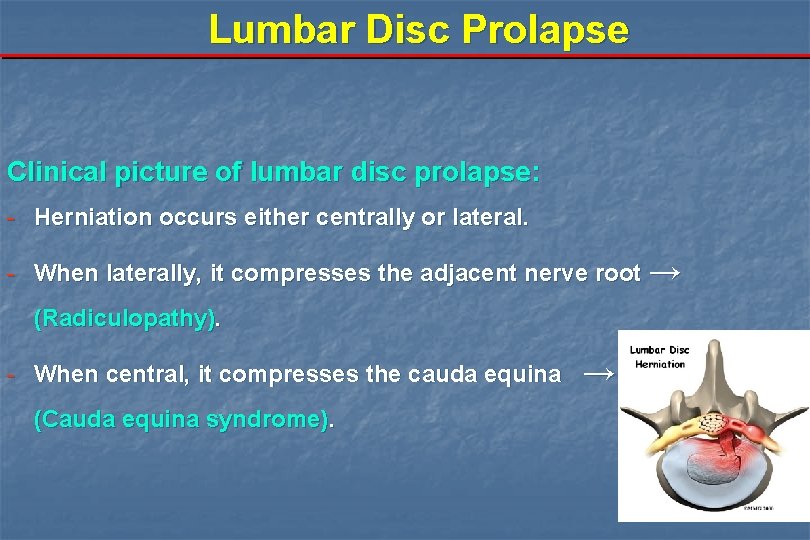
Lumbar Disc Prolapse Clinical picture of lumbar disc prolapse: - Herniation occurs either centrally or lateral. - When laterally, it compresses the adjacent nerve root → (Radiculopathy). - When central, it compresses the cauda equina (Cauda equina syndrome). →
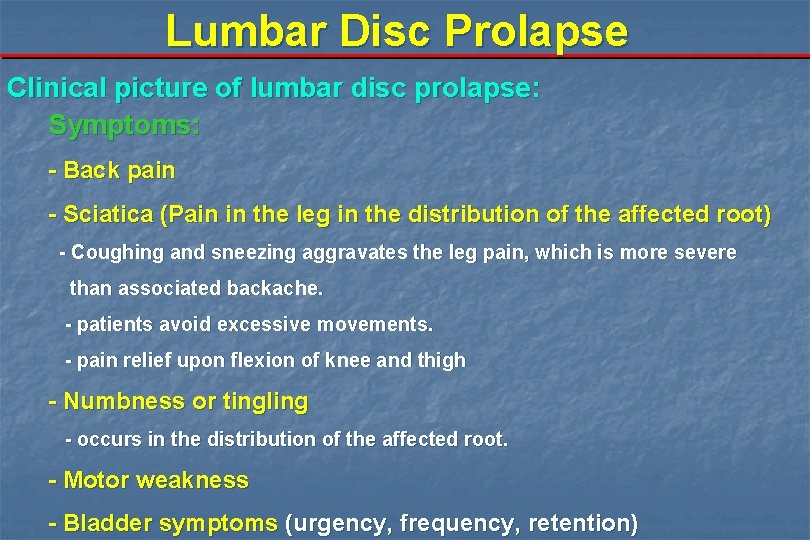
Lumbar Disc Prolapse Clinical picture of lumbar disc prolapse: Symptoms: - Back pain - Sciatica (Pain in the leg in the distribution of the affected root) - Coughing and sneezing aggravates the leg pain, which is more severe than associated backache. - patients avoid excessive movements. - pain relief upon flexion of knee and thigh - Numbness or tingling - occurs in the distribution of the affected root. - Motor weakness - Bladder symptoms (urgency, frequency, retention)
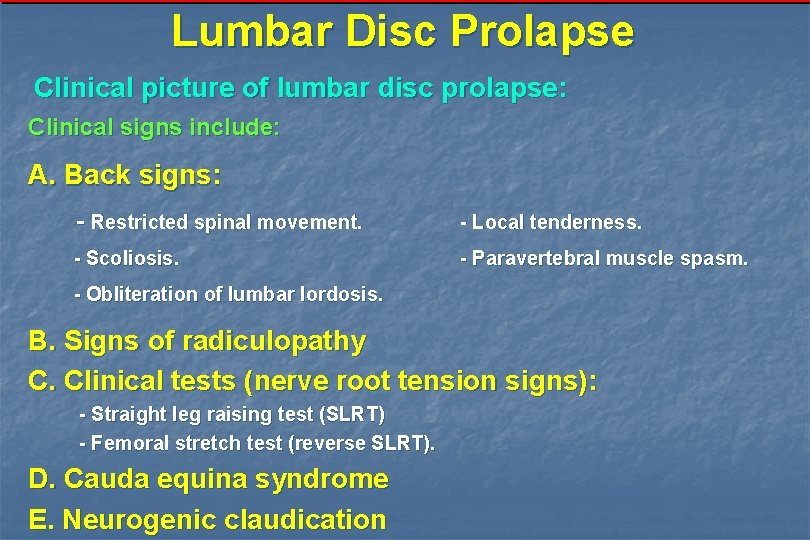
Lumbar Disc Prolapse Clinical picture of lumbar disc prolapse: Clinical signs include: A. Back signs: - Restricted spinal movement. - Local tenderness. - Scoliosis. - Paravertebral muscle spasm. - Obliteration of lumbar lordosis. B. Signs of radiculopathy C. Clinical tests (nerve root tension signs): - Straight leg raising test (SLRT) - Femoral stretch test (reverse SLRT). D. Cauda equina syndrome E. Neurogenic claudication
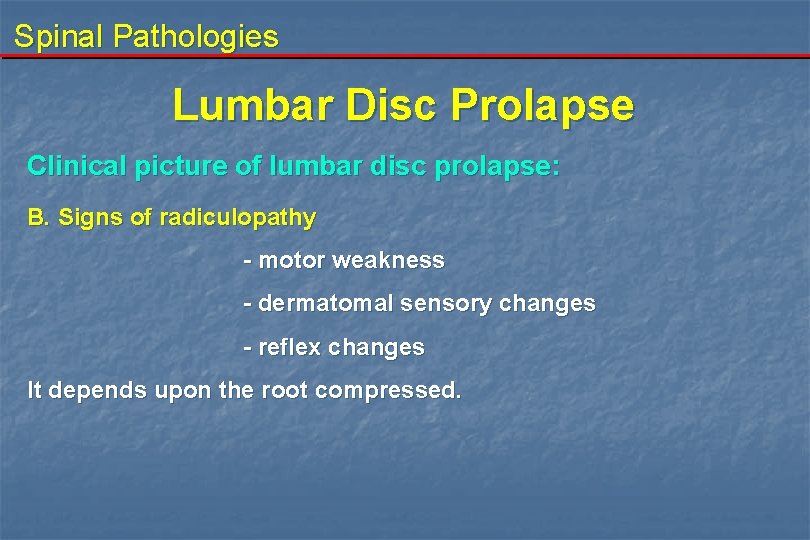
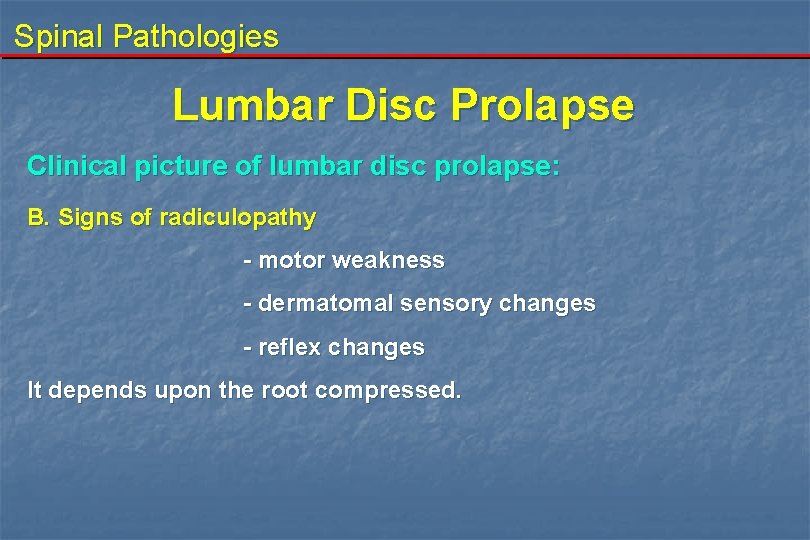
Spinal Pathologies Lumbar Disc Prolapse Clinical picture of lumbar disc prolapse: B. Signs of radiculopathy - motor weakness - dermatomal sensory changes - reflex changes It depends upon the root compressed.
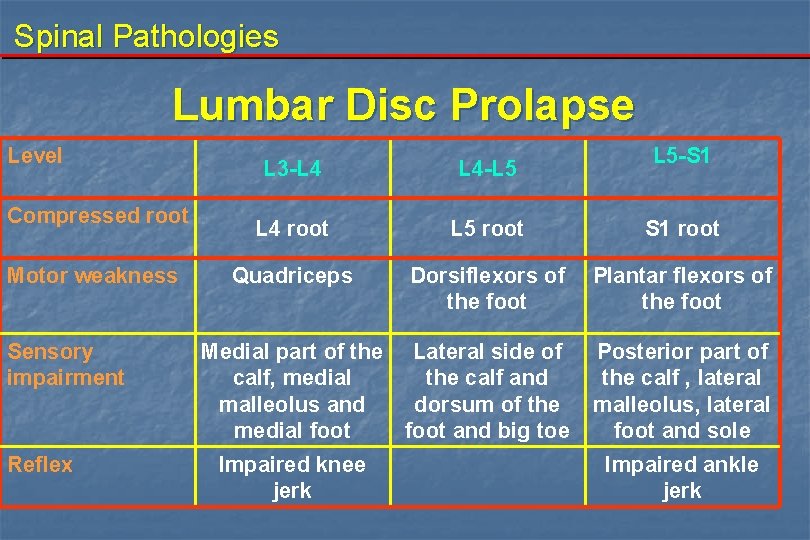
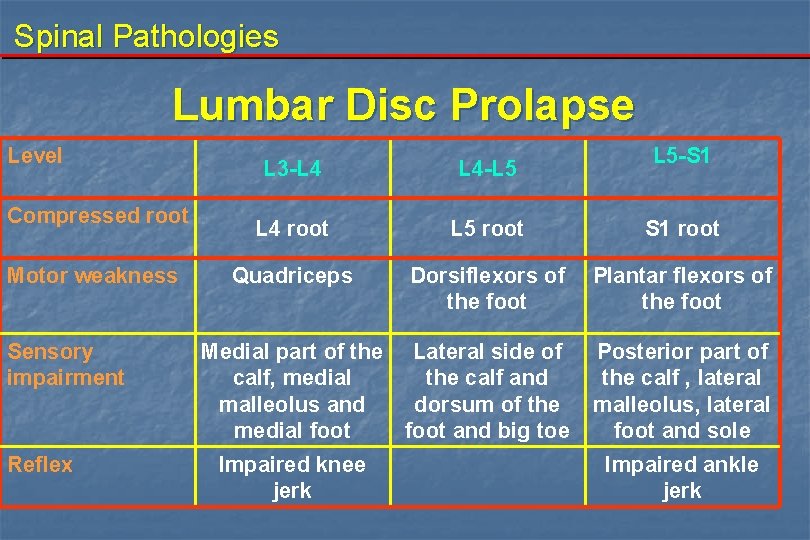
Spinal Pathologies Lumbar Disc Prolapse Level Compressed root Motor weakness Sensory impairment Reflex L 5 -S 1 L 3 -L 4 L 4 -L 5 L 4 root L 5 root S 1 root Quadriceps Dorsiflexors of the foot Plantar flexors of the foot Medial part of the Lateral side of calf, medial the calf and malleolus and dorsum of the medial foot and big toe Posterior part of the calf , lateral malleolus, lateral foot and sole Impaired knee jerk Impaired ankle jerk
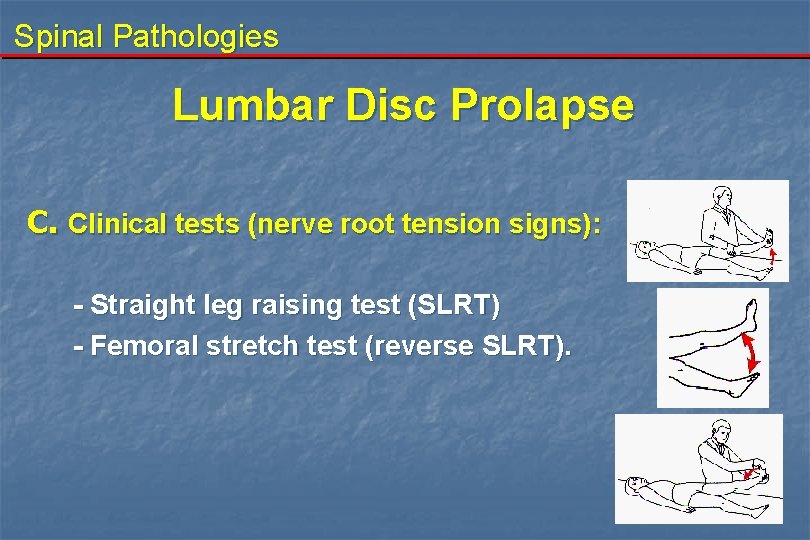
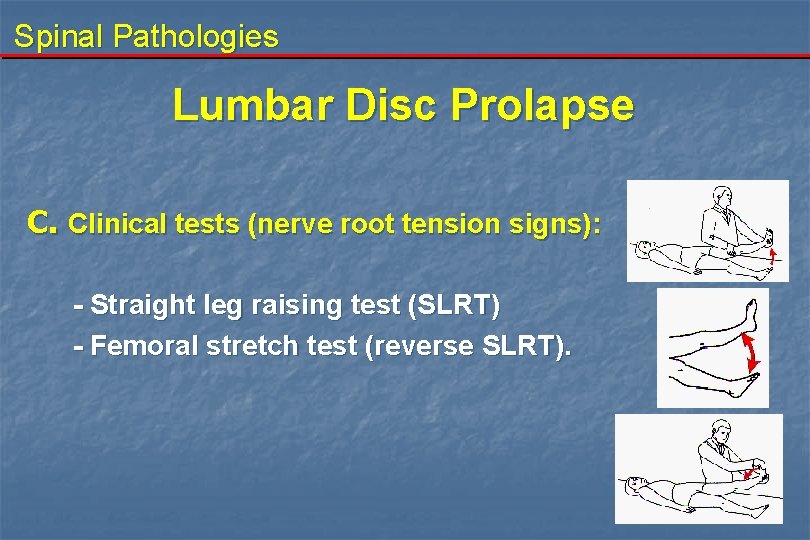
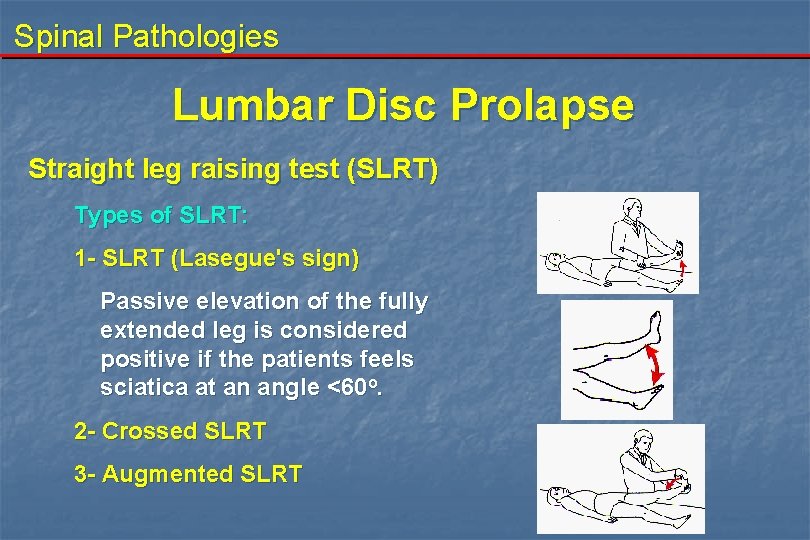
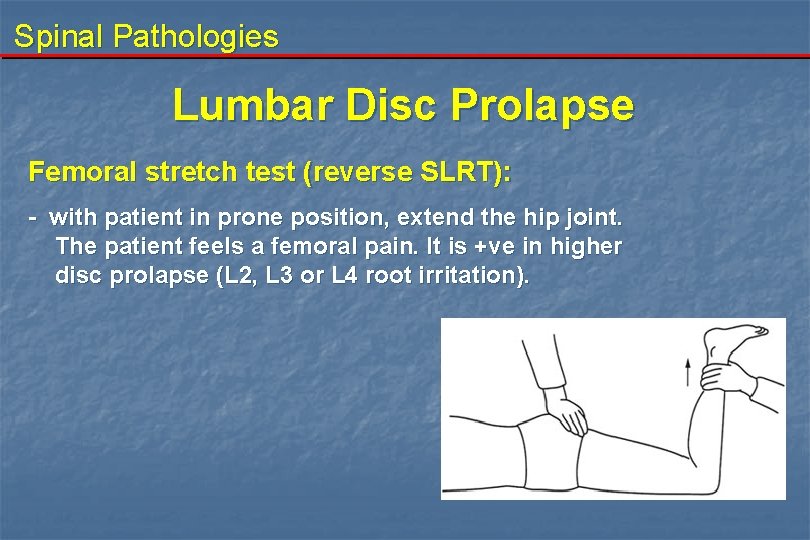
Spinal Pathologies Lumbar Disc Prolapse C. Clinical tests (nerve root tension signs): - Straight leg raising test (SLRT) - Femoral stretch test (reverse SLRT).
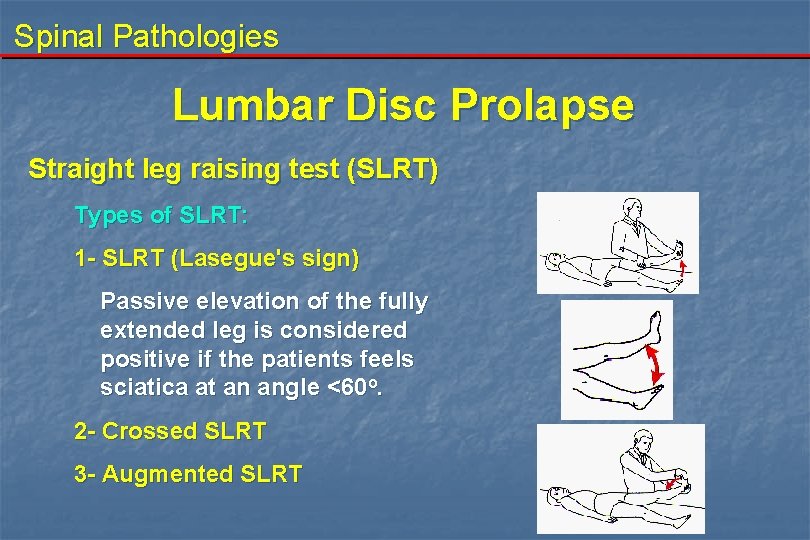
Spinal Pathologies Lumbar Disc Prolapse Straight leg raising test (SLRT) Types of SLRT: 1 - SLRT (Lasegue's sign) Passive elevation of the fully extended leg is considered positive if the patients feels sciatica at an angle <60 o. 2 - Crossed SLRT 3 - Augmented SLRT
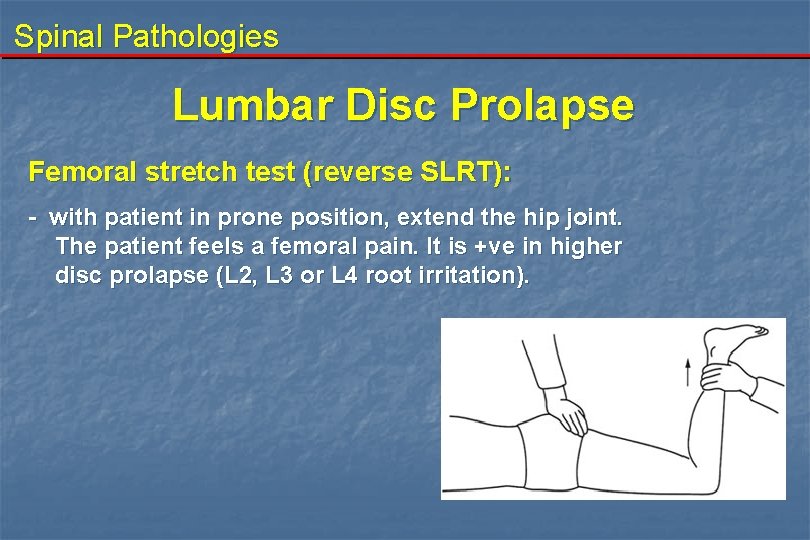
Spinal Pathologies Lumbar Disc Prolapse Femoral stretch test (reverse SLRT): - with patient in prone position, extend the hip joint. The patient feels a femoral pain. It is +ve in higher disc prolapse (L 2, L 3 or L 4 root irritation).
Spinal Pathologies Lumbar Disc Prolapse D. Cauda equina syndrome Presentation: - Low back pain and bilateral sciatica - Motor: bilateral weakness of dorsi and plantar flexion of the foot. Weakness of hip flexor and/or extensors and weakness of knee flexors and/or extensors may also occur. - Sensory: hyposthesia bilaterally according to the spinal roots affected and saddle shaped hyposthesia. - Reflexes: ankle reflex is lost bilaterally and also may be the knee reflex. - Sexual dysfunction (impotence) Sphincteric disturbance (retention or incontinence of urine, chronic constipation or incontinence of stools, diminished anal tone). - Clinical test: SLRT→positive bilaterally
Spinal Pathologies Lumbar Disc Prolapse E. Claudicating sciatica - It occurs in cases of lumbar canal stenosis which is either:
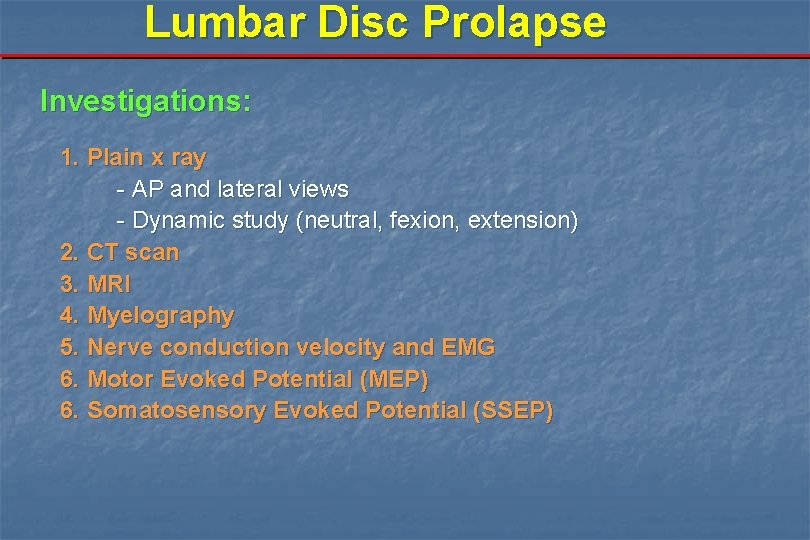
Lumbar Disc Prolapse Investigations: 1. Plain x ray - AP and lateral views - Dynamic study (neutral, fexion, extension) 2. CT scan 3. MRI 4. Myelography 5. Nerve conduction velocity and EMG 6. Motor Evoked Potential (MEP) 6. Somatosensory Evoked Potential (SSEP)
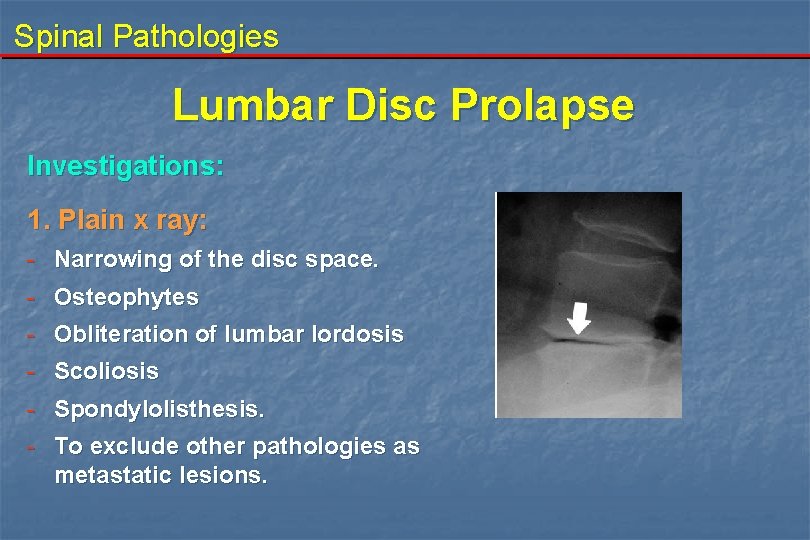
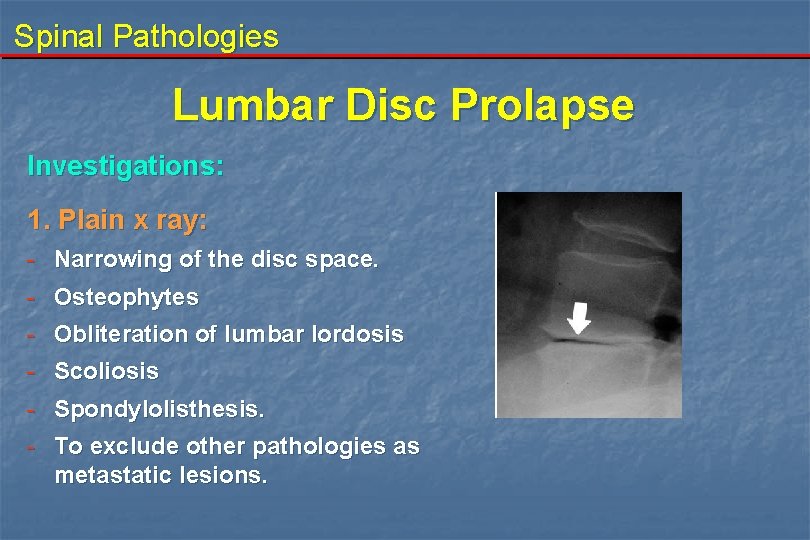
Spinal Pathologies Lumbar Disc Prolapse Investigations: 1. Plain x ray: - Narrowing of the disc space. - Osteophytes - Obliteration of lumbar lordosis - Scoliosis - Spondylolisthesis. - To exclude other pathologies as metastatic lesions.
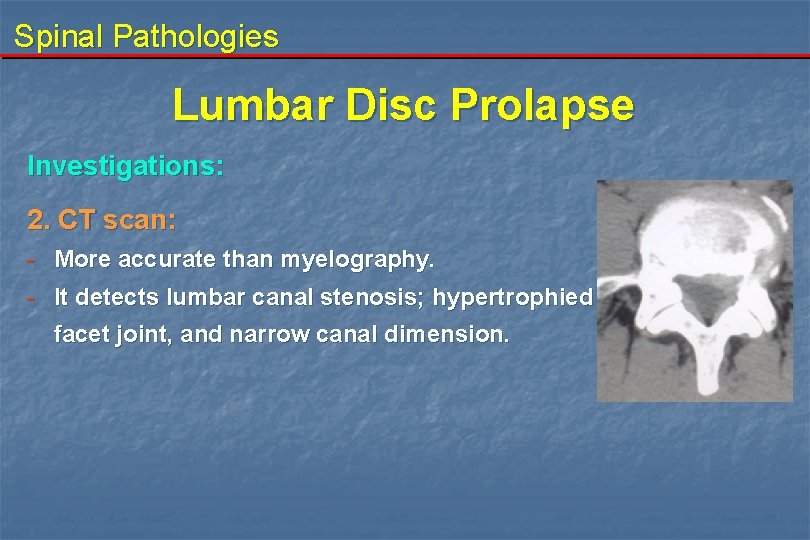
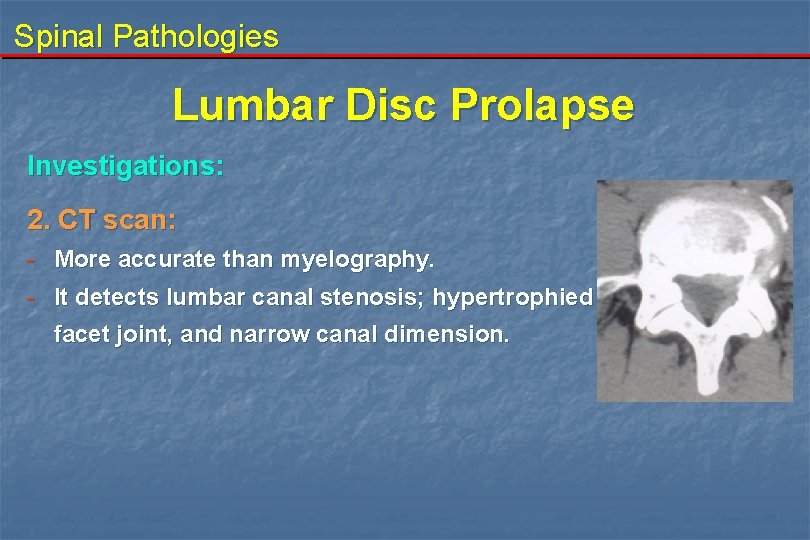
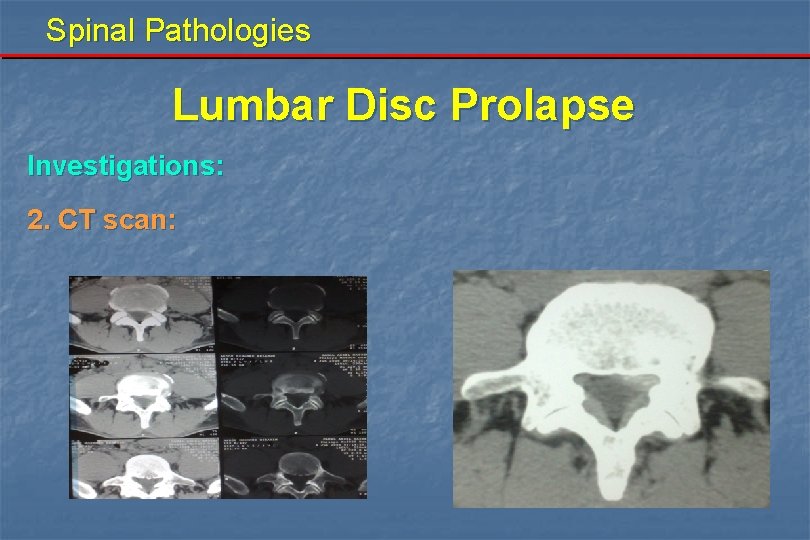
Spinal Pathologies Lumbar Disc Prolapse Investigations: 2. CT scan: - More accurate than myelography. - It detects lumbar canal stenosis; hypertrophied facet joint, and narrow canal dimension.
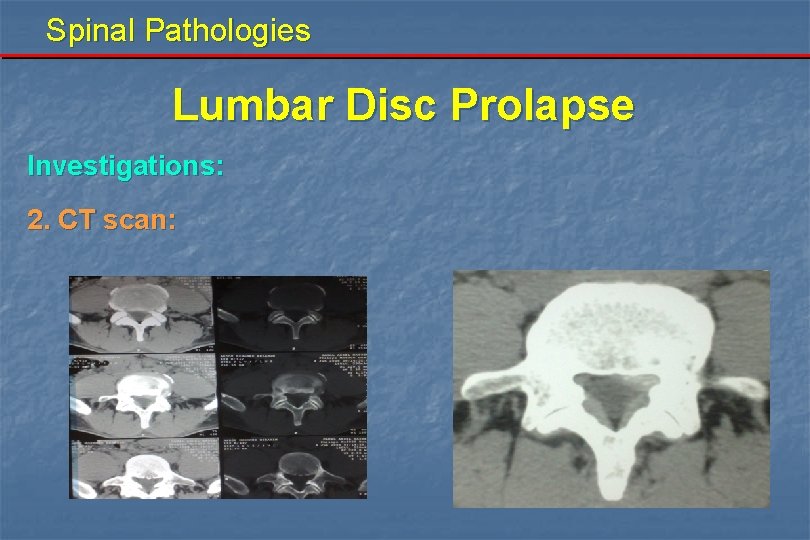
Spinal Pathologies Lumbar Disc Prolapse Investigations: 2. CT scan:
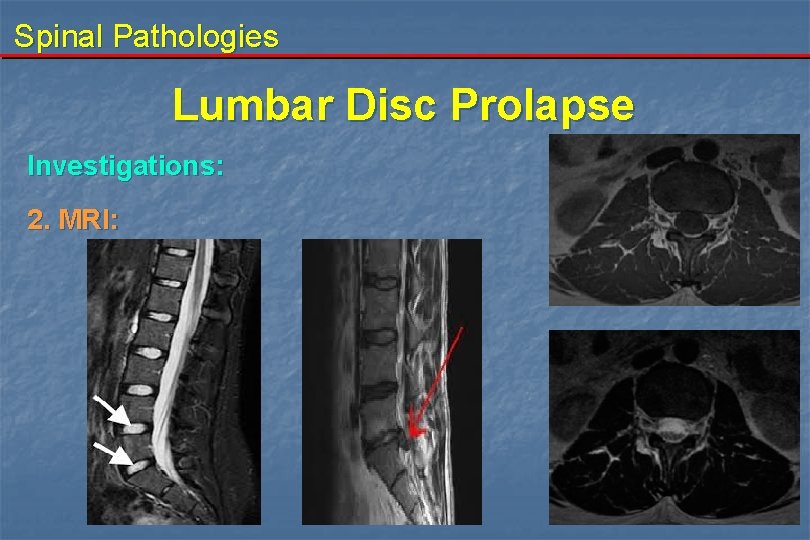
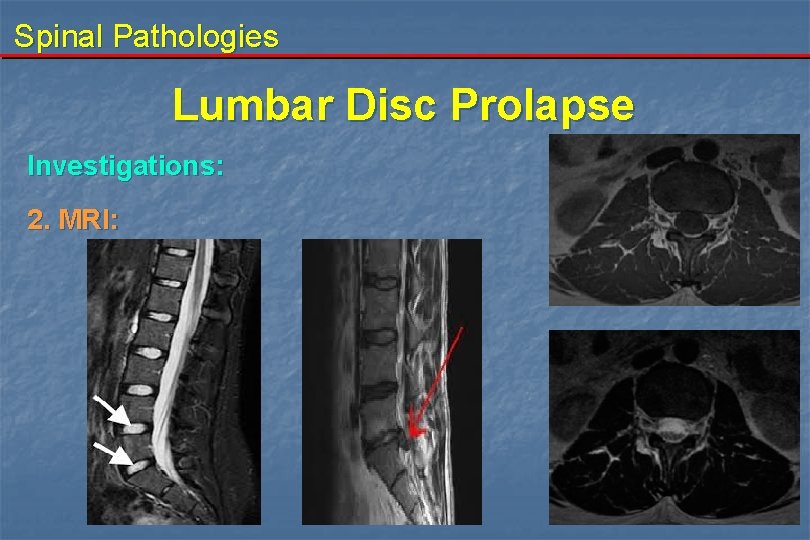
Spinal Pathologies Lumbar Disc Prolapse Investigations: 2. MRI:
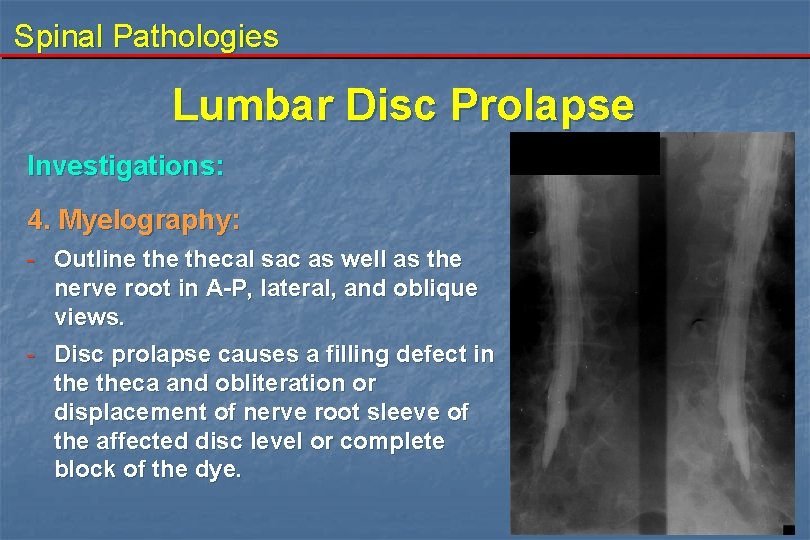
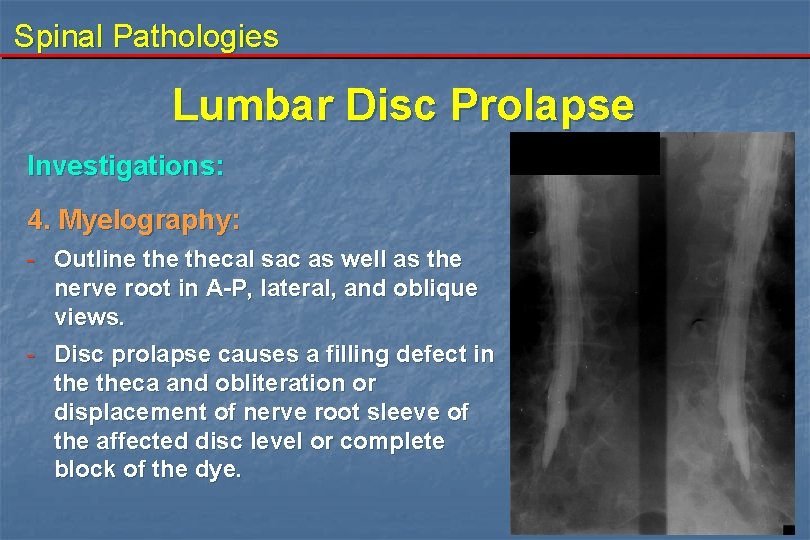
Spinal Pathologies Lumbar Disc Prolapse Investigations: 4. Myelography: - Outline thecal sac as well as the nerve root in A-P, lateral, and oblique views. - Disc prolapse causes a filling defect in theca and obliteration or displacement of nerve root sleeve of the affected disc level or complete block of the dye.
Spinal Pathologies Lumbar Disc Prolapse Investigations: 5. Nerve conduction velocity and EMG: - It will yield precise information on root lesion.

Spinal Pathologies Lumbar Disc Prolapse Treatment: a. Conservative treatment: 1 - Bed rest for 2 -4 days on hard board mattress. 2 - Activity modification and avoid lifting heavy weights. 3 - Exercise 4 - Analgesics 5 - Muscle relaxants 6 - Reduction of body weight 7 - Education
Spinal Pathologies Lumbar Disc Prolapse b. Surgical treatment: 1. Failure of non surgical treatment. 2. Patients who do not want to invest time in a trial of non surgical treatment. 3. Urgent surgery: - Cauda equina syndrome. - Severe, unremitting, leg pain which is not relieved by conservative measures. Progressive motor deficit.
Lumbar Disc Prolapse Surgical treatment: 1 - Transcanal approaches: a- Standard open laminectomy and discectomy b- Microdiscectomy c- Endoscopic discectomy 2 - Intradiscal procedures: a- Automated percutaneous lumbar discectomy (nucleotome) b- Percutaneous endoscopic discectomy c- Laser disc decompression d- Chemonucleolysis 3 - Artificial disc replacement
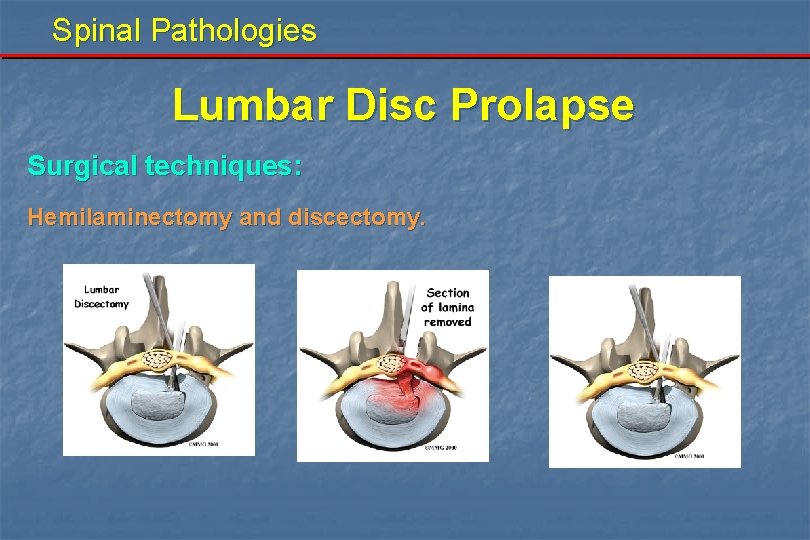
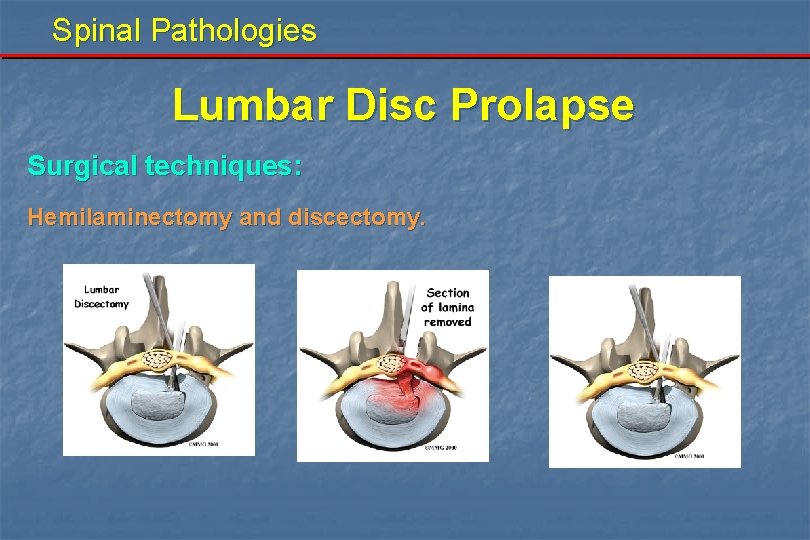
Spinal Pathologies Lumbar Disc Prolapse Surgical techniques: Hemilaminectomy and discectomy.
Spinal Pathologies Lumbar Disc Prolapse Surgical techniques: Endoscopic discectomy.
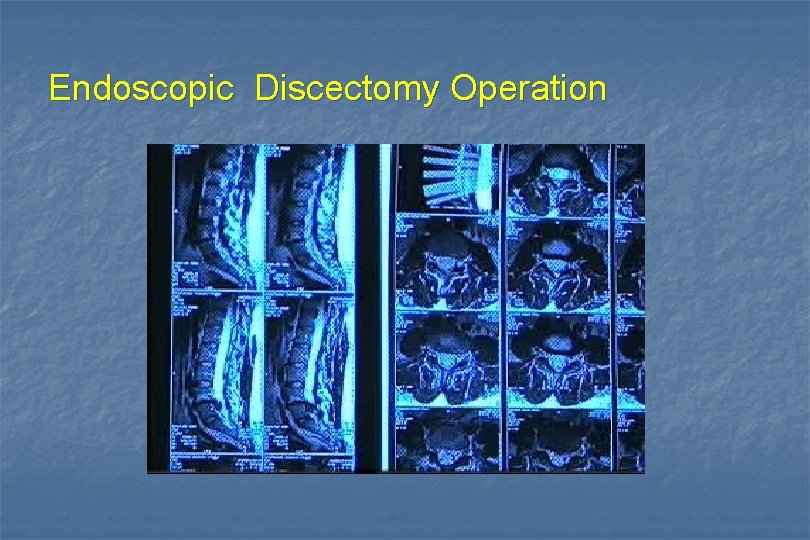
Endoscopic Discectomy Operation
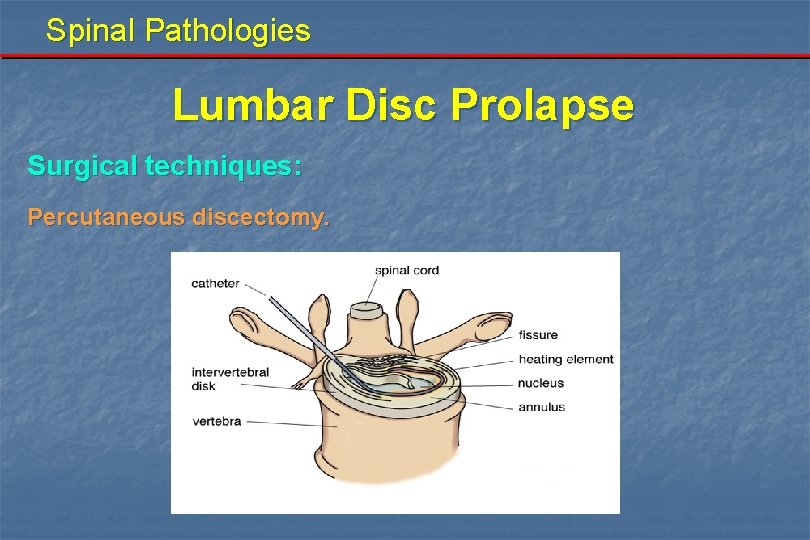
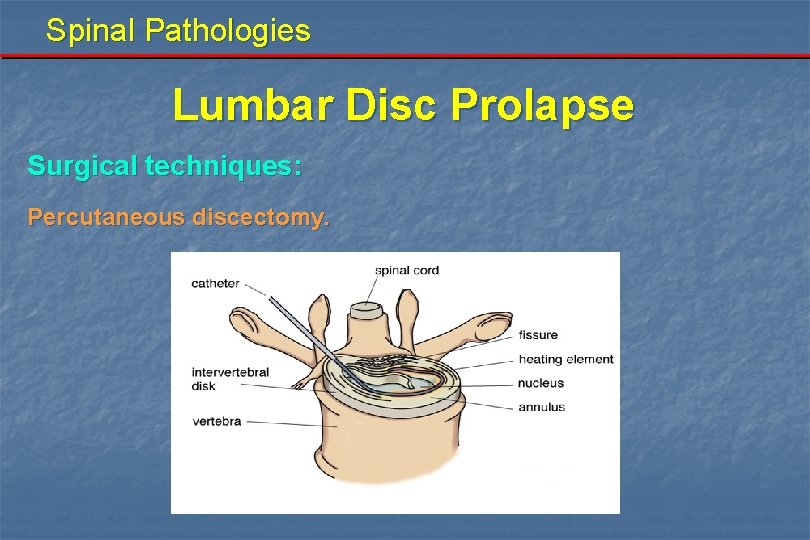
Spinal Pathologies Lumbar Disc Prolapse Surgical techniques: Percutaneous discectomy.
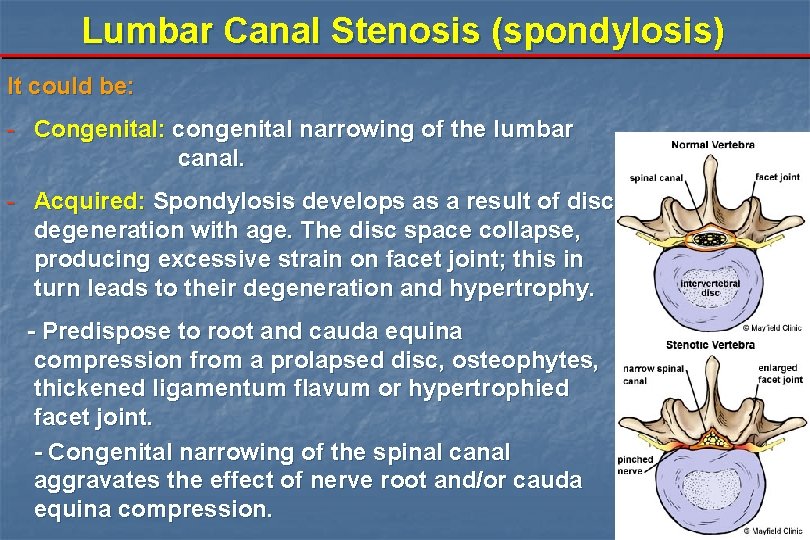
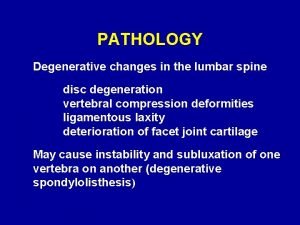
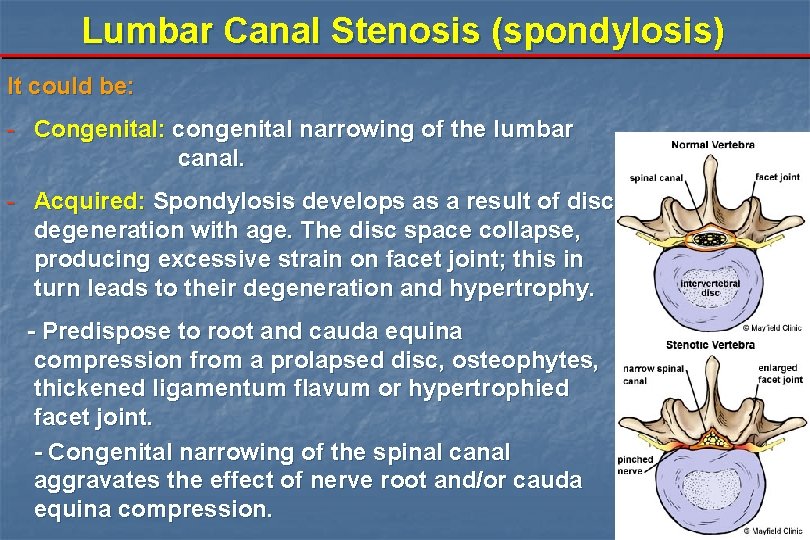
Lumbar Canal Stenosis (spondylosis) It could be: - Congenital: congenital narrowing of the lumbar canal. - Acquired: Spondylosis develops as a result of disc degeneration with age. The disc space collapse, producing excessive strain on facet joint; this in turn leads to their degeneration and hypertrophy. - Predispose to root and cauda equina compression from a prolapsed disc, osteophytes, thickened ligamentum flavum or hypertrophied facet joint. - Congenital narrowing of the spinal canal aggravates the effect of nerve root and/or cauda equina compression.
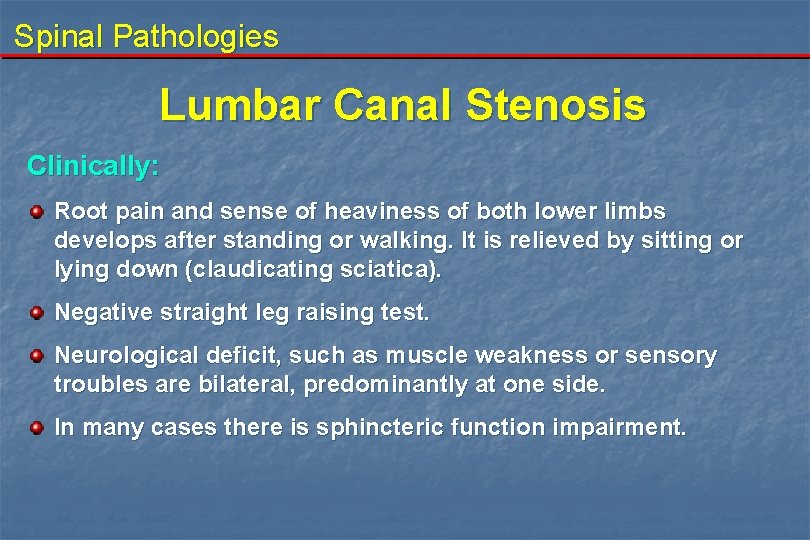
Spinal Pathologies Lumbar Canal Stenosis Clinically: Root pain and sense of heaviness of both lower limbs develops after standing or walking. It is relieved by sitting or lying down (claudicating sciatica). Negative straight leg raising test. Neurological deficit, such as muscle weakness or sensory troubles are bilateral, predominantly at one side. In many cases there is sphincteric function impairment.
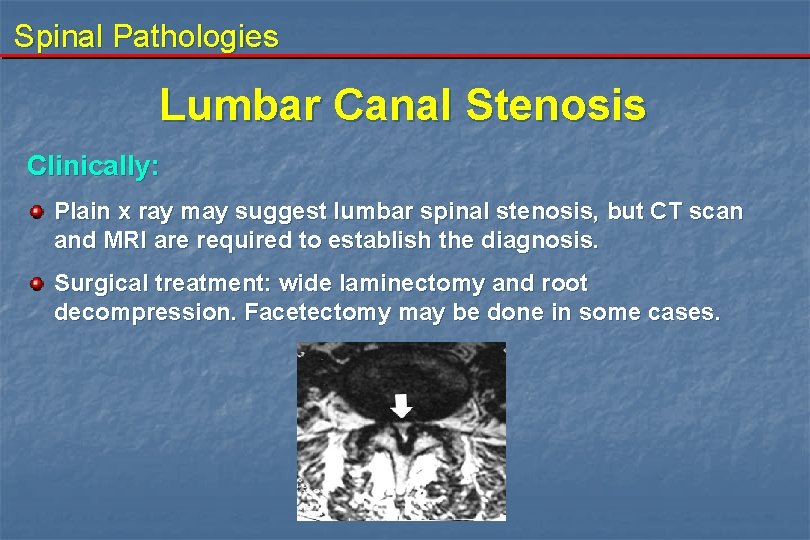
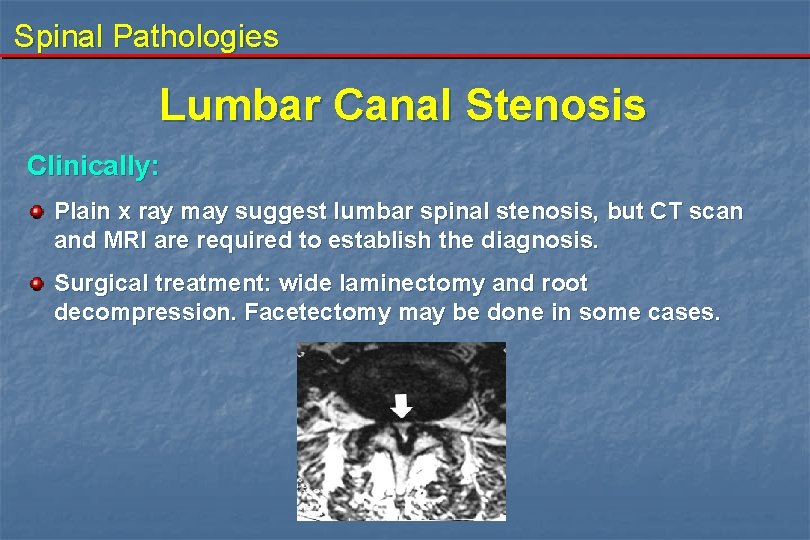
Spinal Pathologies Lumbar Canal Stenosis Clinically: Plain x ray may suggest lumbar spinal stenosis, but CT scan and MRI are required to establish the diagnosis. Surgical treatment: wide laminectomy and root decompression. Facetectomy may be done in some cases.
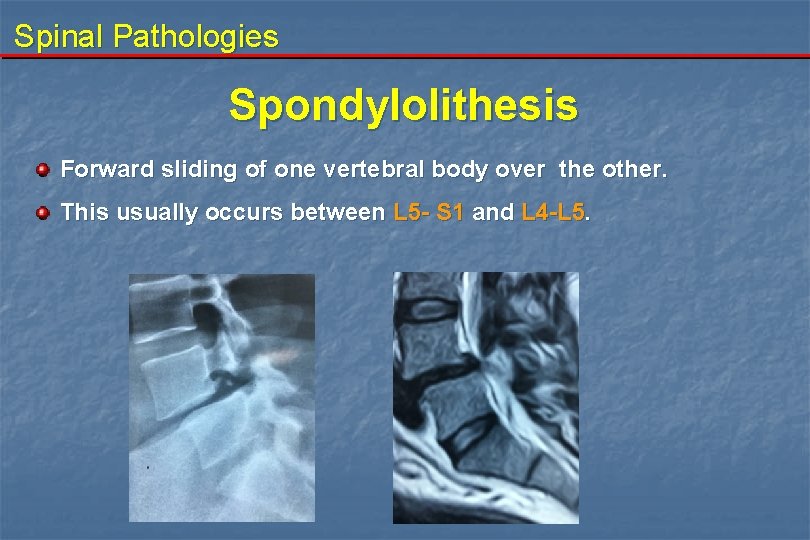
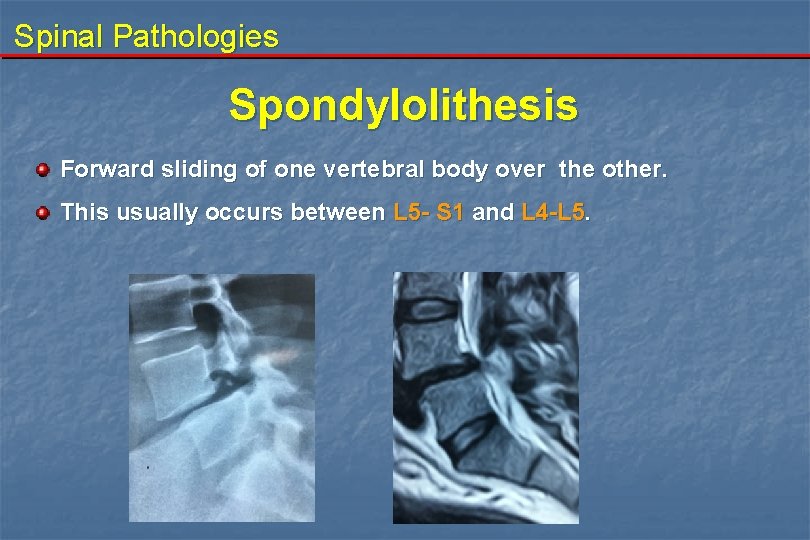
Spinal Pathologies Spondylolithesis Forward sliding of one vertebral body over the other. This usually occurs between L 5 - S 1 and L 4 -L 5.
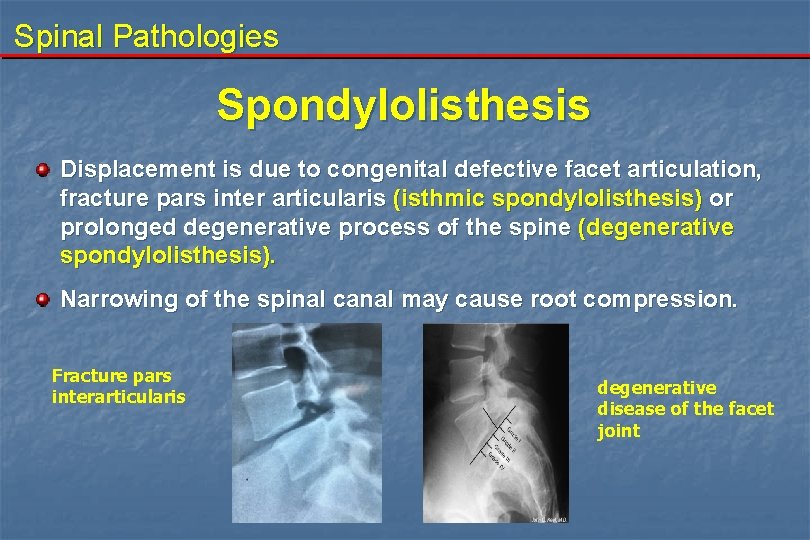
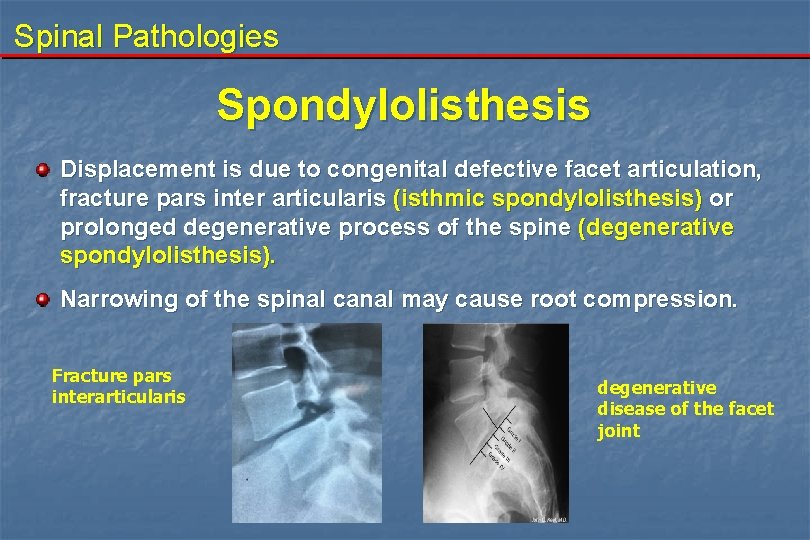
Spinal Pathologies Spondylolisthesis Displacement is due to congenital defective facet articulation, fracture pars inter articularis (isthmic spondylolisthesis) or prolonged degenerative process of the spine (degenerative spondylolisthesis). Narrowing of the spinal canal may cause root compression. Fracture pars interarticularis degenerative disease of the facet joint
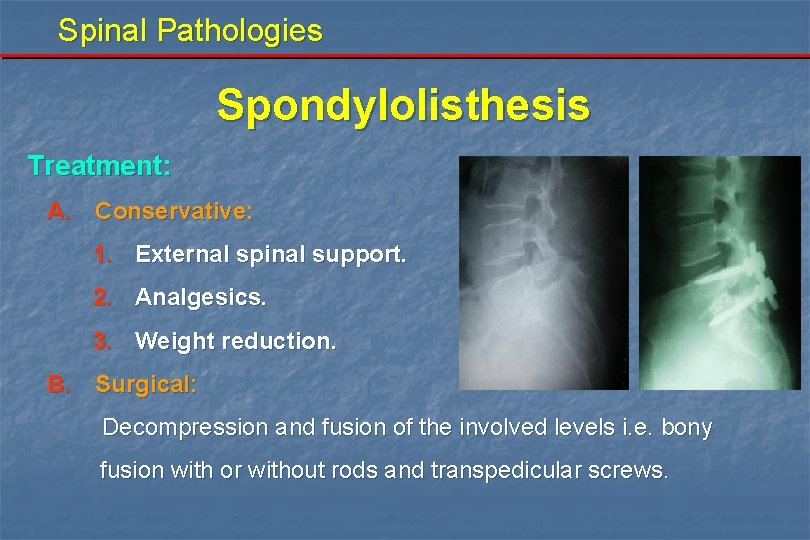
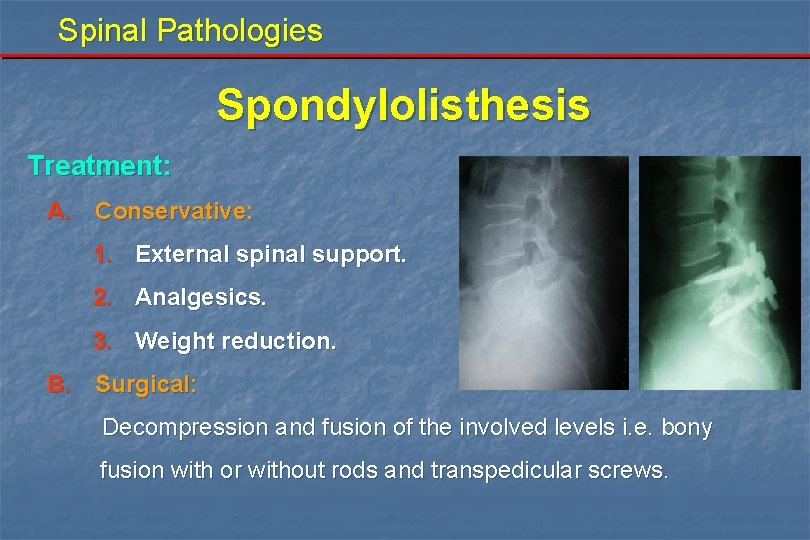
Spinal Pathologies Spondylolisthesis Treatment: A. Conservative: 1. External spinal support. 2. Analgesics. 3. Weight reduction. B. Surgical: Decompression and fusion of the involved levels i. e. bony fusion with or without rods and transpedicular screws.
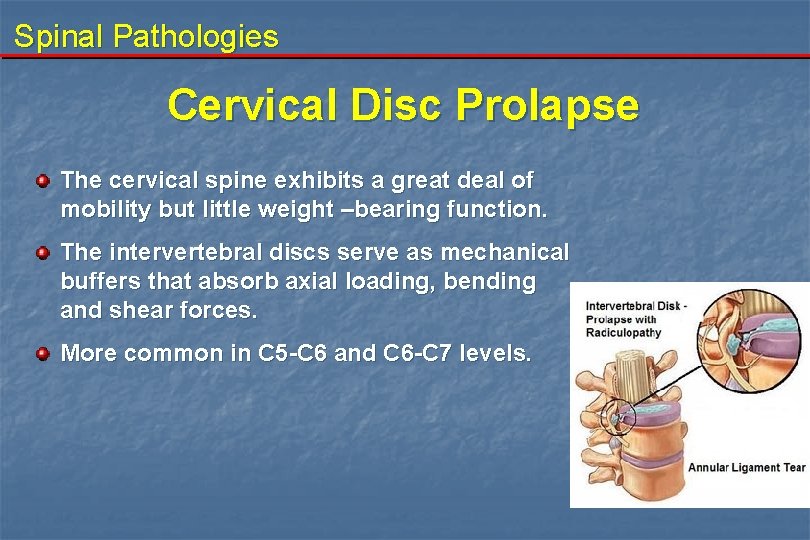
Spinal Pathologies Cervical Disc Prolapse The cervical spine exhibits a great deal of mobility but little weight –bearing function. The intervertebral discs serve as mechanical buffers that absorb axial loading, bending and shear forces. More common in C 5 -C 6 and C 6 -C 7 levels.
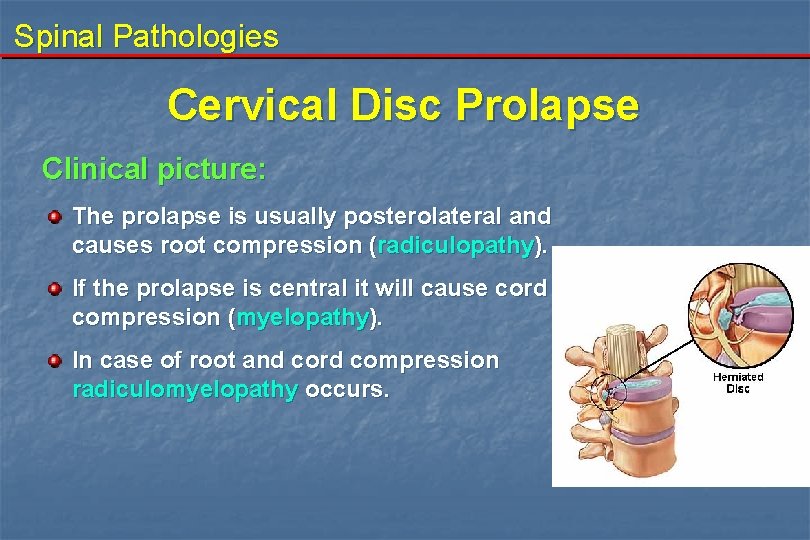
Spinal Pathologies Cervical Disc Prolapse Clinical picture: The prolapse is usually posterolateral and causes root compression (radiculopathy). If the prolapse is central it will cause cord compression (myelopathy). In case of root and cord compression radiculomyelopathy occurs.
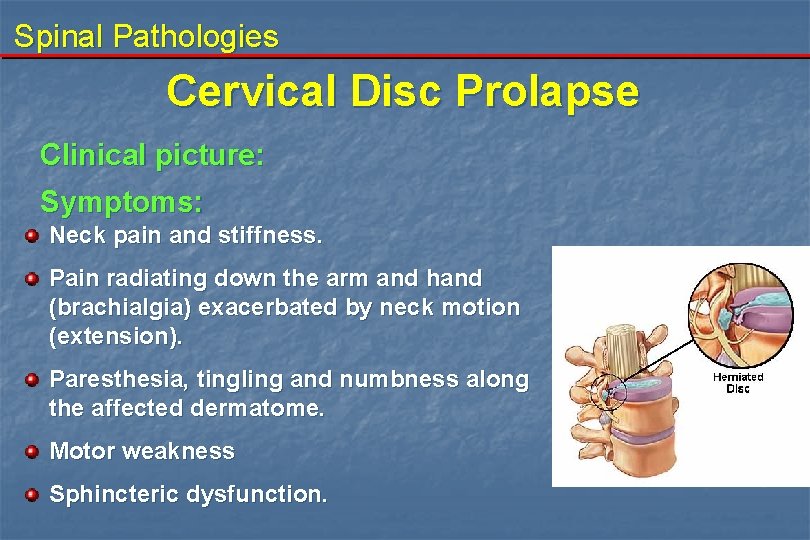
Spinal Pathologies Cervical Disc Prolapse Clinical picture: Symptoms: Neck pain and stiffness. Pain radiating down the arm and hand (brachialgia) exacerbated by neck motion (extension). Paresthesia, tingling and numbness along the affected dermatome. Motor weakness Sphincteric dysfunction.
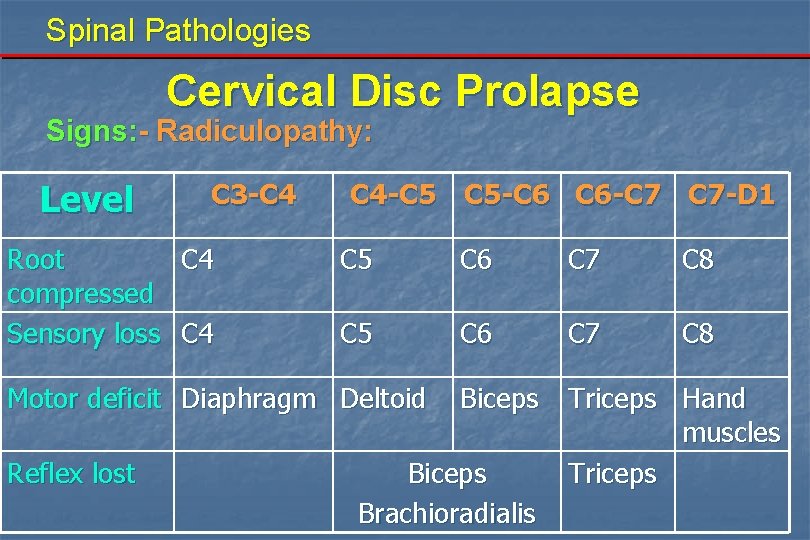
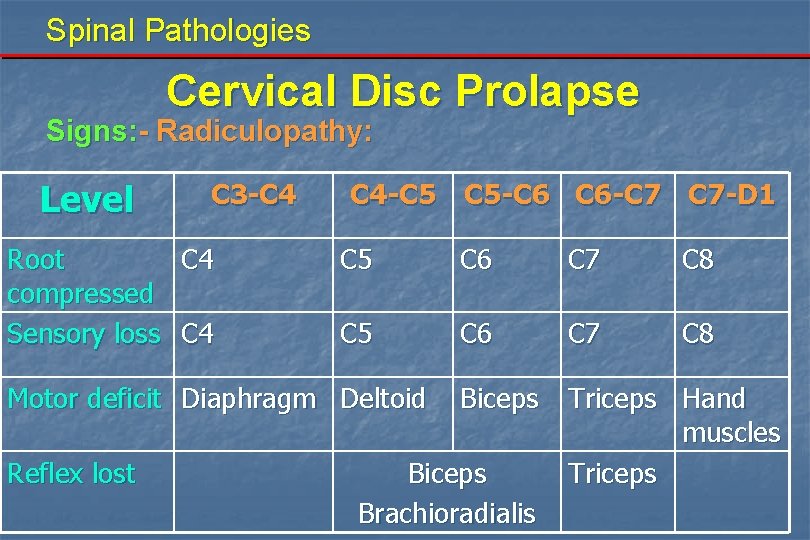
Spinal Pathologies Cervical Disc Prolapse Signs: - Radiculopathy: Level C 3 -C 4 Root C 4 compressed Sensory loss C 4 -C 5 C 5 -C 6 C 6 -C 7 C 7 -D 1 C 5 C 6 C 7 C 8 Biceps Triceps Hand muscles Triceps Motor deficit Diaphragm Deltoid Reflex lost Biceps Brachioradialis
Spinal Pathologies Cervical Disc Prolapse Signs: - Myelopathyhy: - Spastic quadriparesis - Hyperreflexia below the level of the compression - Clumsiness and ataxia of the extremities - Gait disturbance - Sphincteric disturbance.
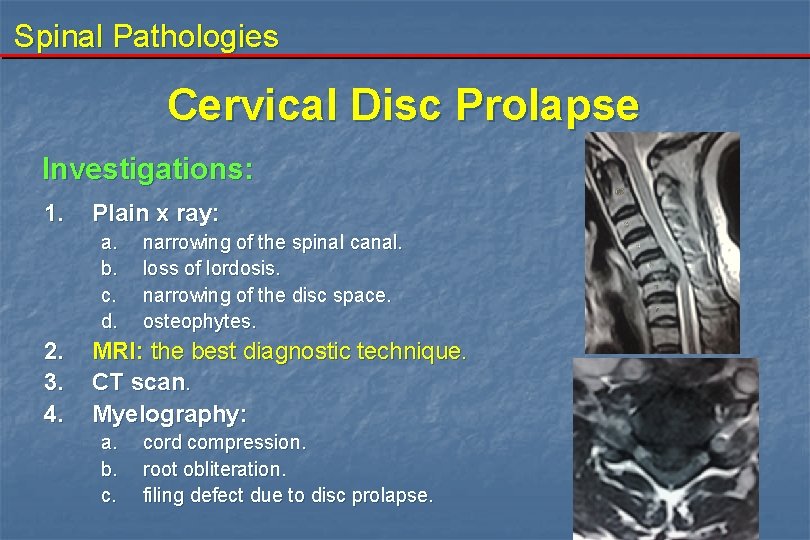
Spinal Pathologies Cervical Disc Prolapse Investigations: 1. Plain x ray: a. b. c. d. 2. 3. 4. narrowing of the spinal canal. loss of lordosis. narrowing of the disc space. osteophytes. MRI: the best diagnostic technique. CT scan. Myelography: a. b. c. cord compression. root obliteration. filing defect due to disc prolapse.
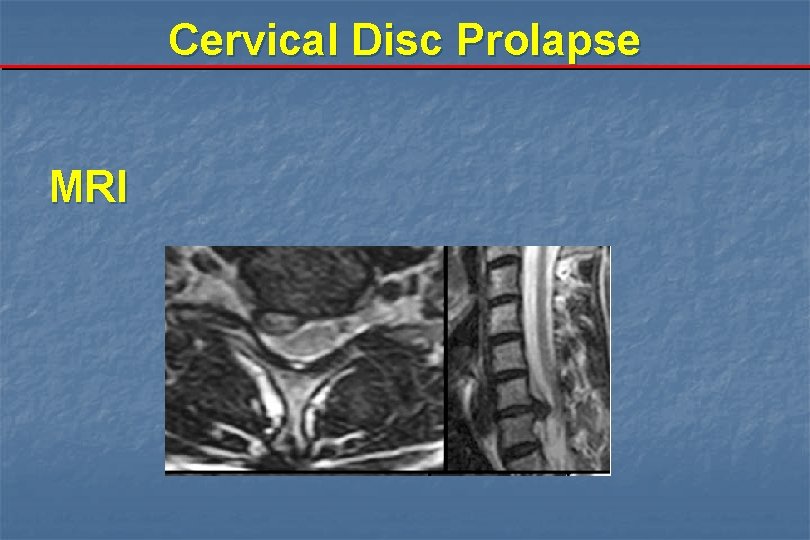
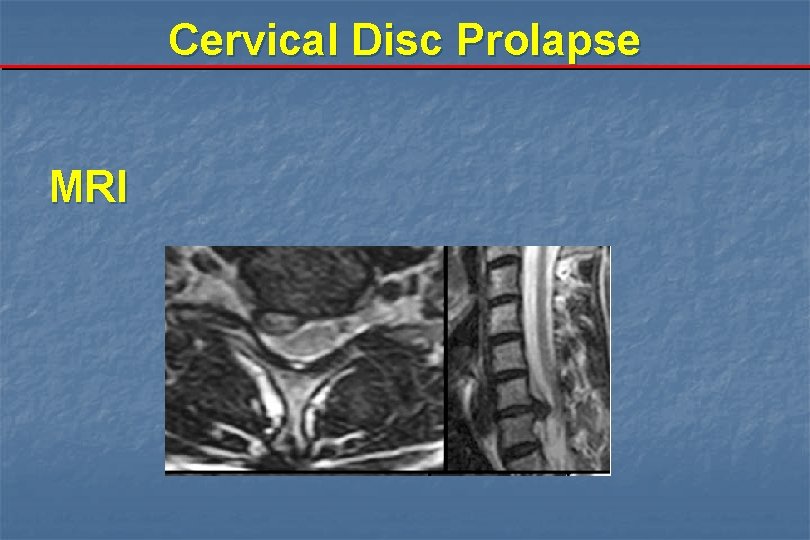
Cervical Disc Prolapse MRI
Cervical Disc Prolapse Management: either conservative or surgical a. Conservative Symptoms relevant to radiculopathy usually respond to conservative measures as: - bed rest - avoidance of heavy lifting - physical therapy - analgesics - muscle relaxant - neck collar b. Surgical
Cervical Disc Prolapse Management: b. Surgical - Indications for surgery: 1 - Brachialgia not responding to medical treatment. 2 - Progressive neurological deficit due to root compression. 3 - manifestations of cord compression i. e. myelopathy. Surgical procedures include: 1. Anterior cervical discectomy. 2. Posterior cervical laminectomy with or without forminotomy.
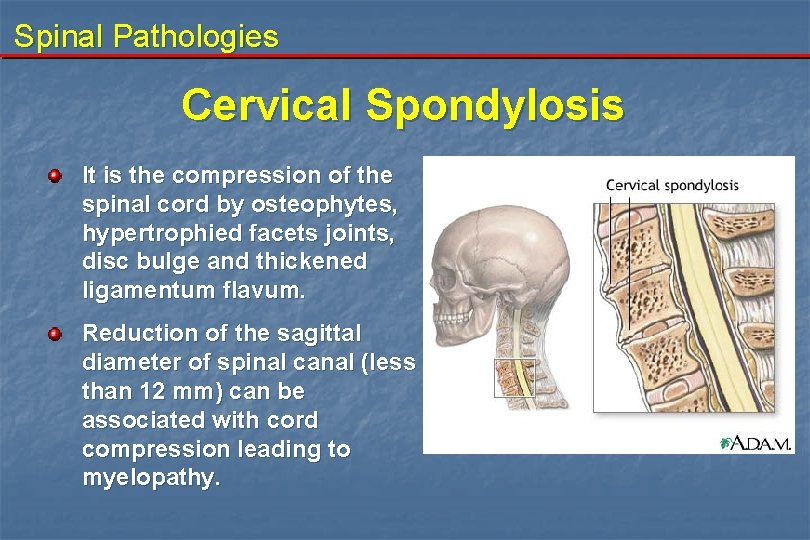
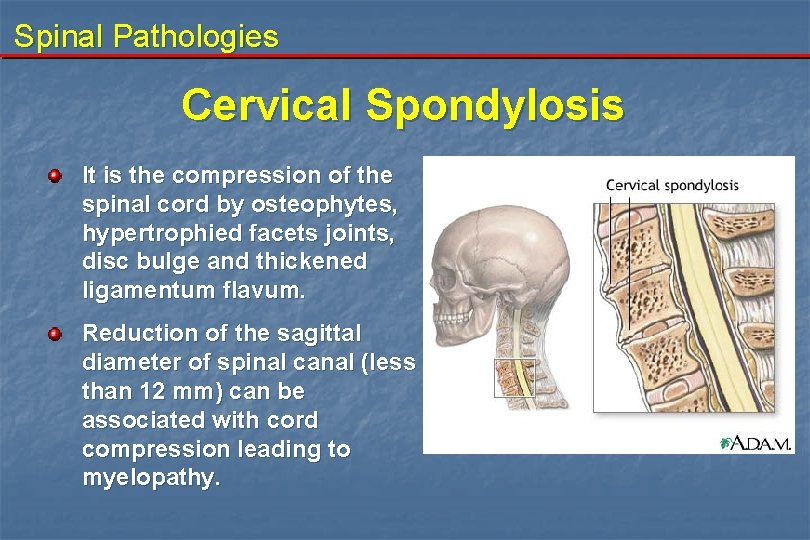
Spinal Pathologies Cervical Spondylosis It is the compression of the spinal cord by osteophytes, hypertrophied facets joints, disc bulge and thickened ligamentum flavum. Reduction of the sagittal diameter of spinal canal (less than 12 mm) can be associated with cord compression leading to myelopathy.
Spinal Pathologies Cervical Spondylosis Clinical picture: Insidious onset. Radiculopathy, myelopathy or radiculomyelopathy Spastic weakness of the lower limbs, with clonus, and + ve Babiniski sign. Weak hand grip and clumsiness. Hypoalgesia due to spinothalamic tract affection.
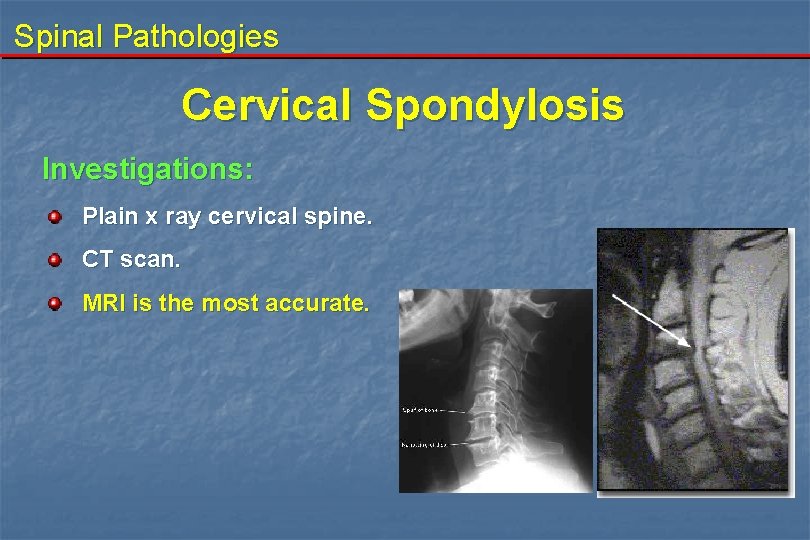
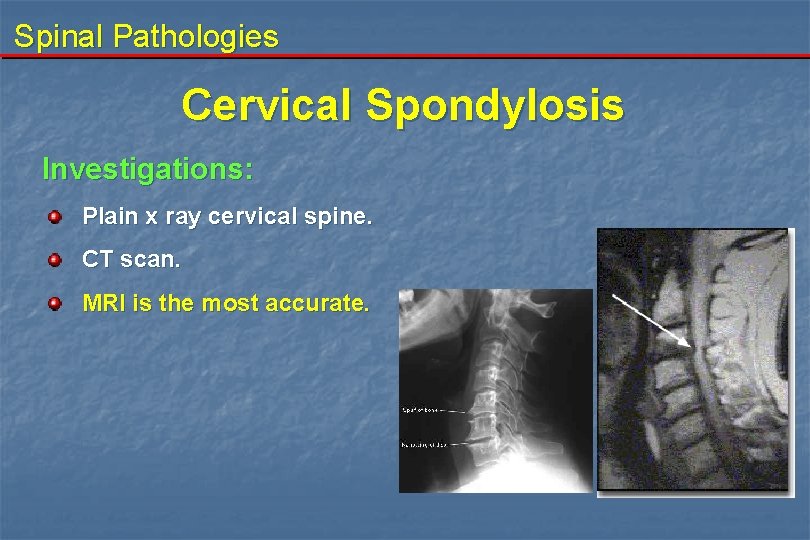
Spinal Pathologies Cervical Spondylosis Investigations: Plain x ray cervical spine. CT scan. MRI is the most accurate.
Spinal Pathologies Cervical Spondylosis Management: 1 - Conservative 2 - Surgical a. Posterior: - Laminectomy with or without foraminotomy - Laminoplasty b. Anterior: - Multilevel discectomy. - Removal of osteophytes. - Stabilization by interbody fusion.

 Penn state neurosurgery faculty
Penn state neurosurgery faculty Degenerative myelopathy wayne
Degenerative myelopathy wayne Faceta
Faceta Drug reaction treatment
Drug reaction treatment Walton centre for neurology
Walton centre for neurology Neurosurgery
Neurosurgery Alan cohen neurosurgery
Alan cohen neurosurgery Norse neurosurgery referral
Norse neurosurgery referral Uw neurological surgery
Uw neurological surgery Nit calicut chemistry department faculty
Nit calicut chemistry department faculty Nerve fibers
Nerve fibers Iliac crest level
Iliac crest level One leg is longer than the other
One leg is longer than the other Mental spine
Mental spine Clinical biomechanics of the spine
Clinical biomechanics of the spine Linear danger area hand signal
Linear danger area hand signal Mdcalc nexus c spine
Mdcalc nexus c spine Nexus rules c spine
Nexus rules c spine Spine technologies (i) pvt. ltd
Spine technologies (i) pvt. ltd Spine pathology
Spine pathology Spinal cord spasticity
Spinal cord spasticity Tubercle of rib
Tubercle of rib Reflexology tips
Reflexology tips Asia a b c d e
Asia a b c d e Chapter 28 head and spine injuries
Chapter 28 head and spine injuries Muscles of the pelvic girdle
Muscles of the pelvic girdle Position keeping
Position keeping Bid rent theory model
Bid rent theory model The story spine
The story spine Spine
Spine Uncovertebral joint
Uncovertebral joint Milwaukee brace
Milwaukee brace Short spine board digunakan untuk
Short spine board digunakan untuk Tata letak layout toko
Tata letak layout toko True vertebrae
True vertebrae C spine precautions
C spine precautions Thorcic spine
Thorcic spine Quartiere spine bianche matera
Quartiere spine bianche matera Noms score spine
Noms score spine Latissimus dorsi innervation
Latissimus dorsi innervation Forearm rom
Forearm rom Caudal medulla
Caudal medulla Anterior inferior iliac spine
Anterior inferior iliac spine Proximal tibia
Proximal tibia Split traction table
Split traction table Chapter 25 worksheet the spine
Chapter 25 worksheet the spine Shilla spine
Shilla spine Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Borrmann classification of gastric cancer
Borrmann classification of gastric cancer 3 inch binder spine template
3 inch binder spine template The story spine
The story spine Meracidium
Meracidium Who is in charge when spine boarding an athlete and why
Who is in charge when spine boarding an athlete and why Inferior glenohumeral ligament
Inferior glenohumeral ligament Thecal sac
Thecal sac Ganglion on spine
Ganglion on spine Spine vs thorn
Spine vs thorn