Course Contents Section 1 Exercise and the cardiovascular

- Slides: 51
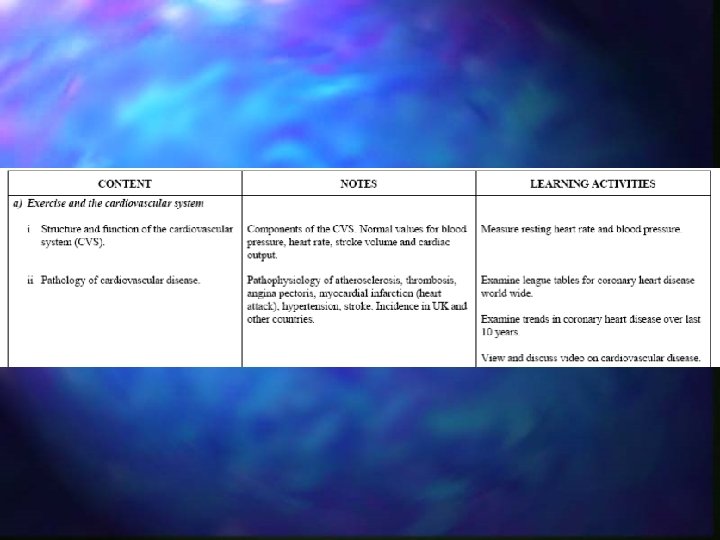
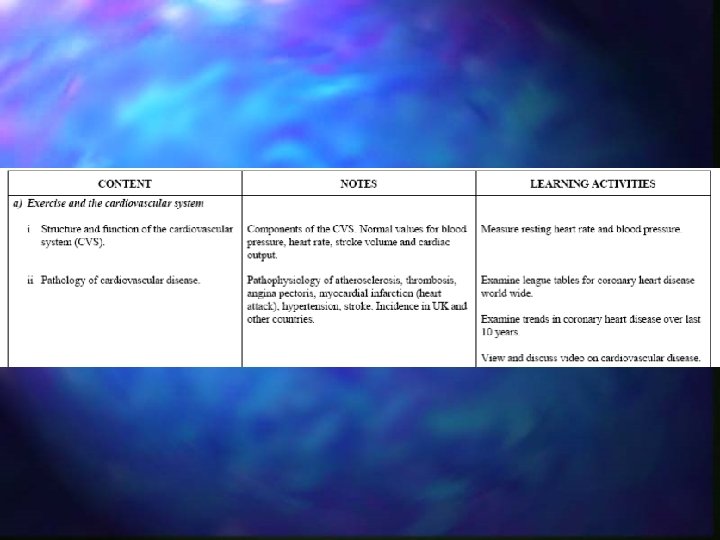
Course Contents Section 1 Exercise and the cardiovascular system 1. 1 Structure and function of the cardiovascular system 1. 2 Pathology of cardiovascular diseases (CVD) 1. 3 Role of exercise in prevention and treatment of CVD Section 2 Exercise and Metabolism 2. 1 Energy 2. 2 Body composition & Weight Control 2. 3 Diabetes Mellitus 2. 4 Osteoporosis
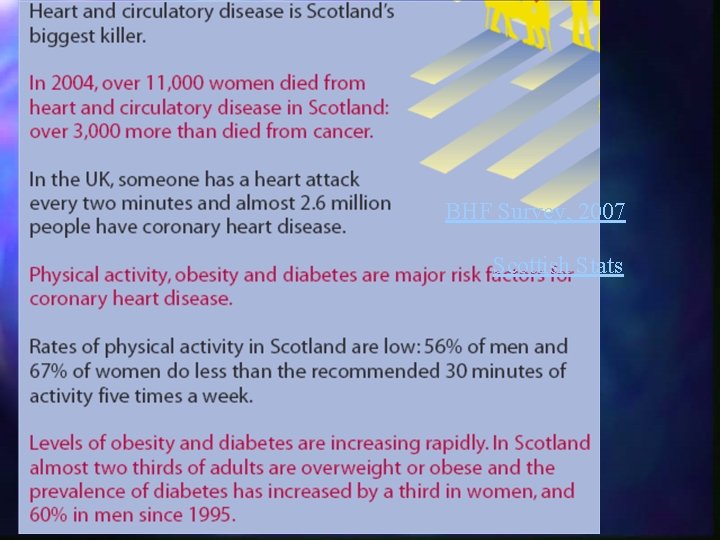
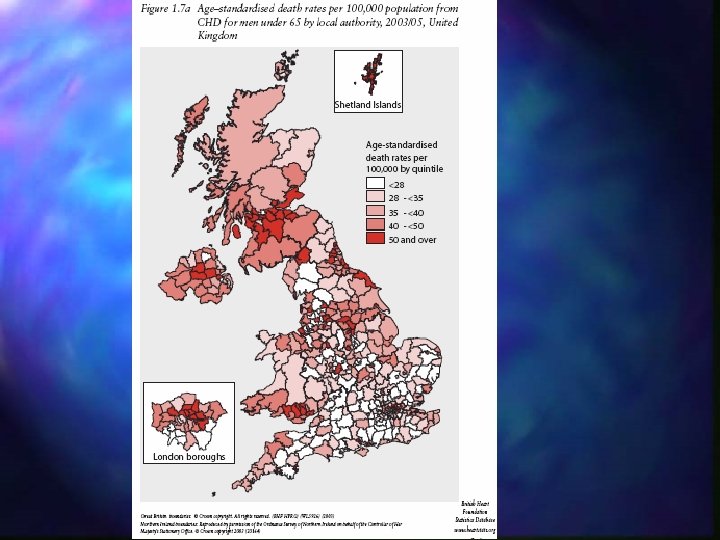
BHF Survey, 2007 Scottish Stats
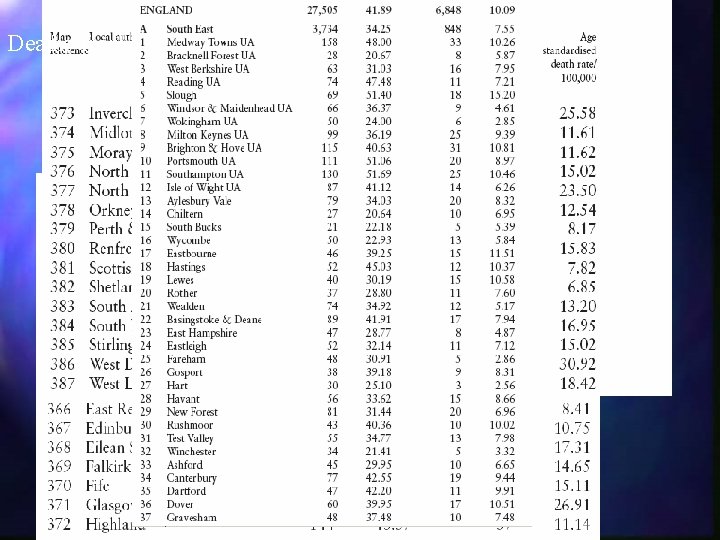
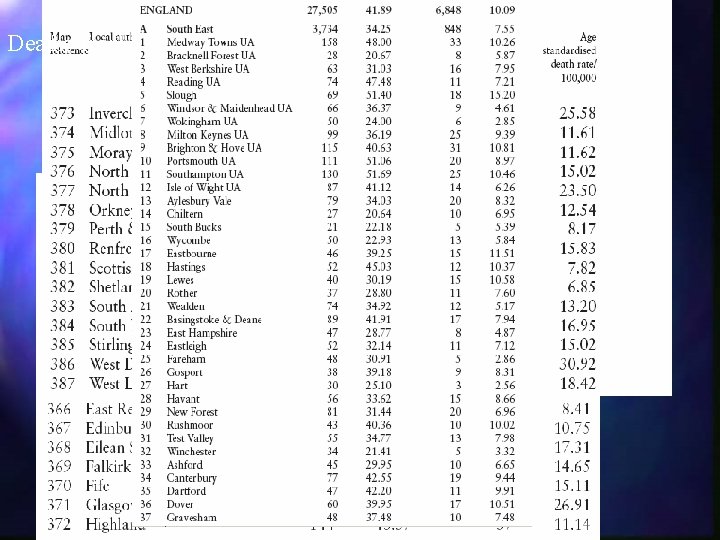
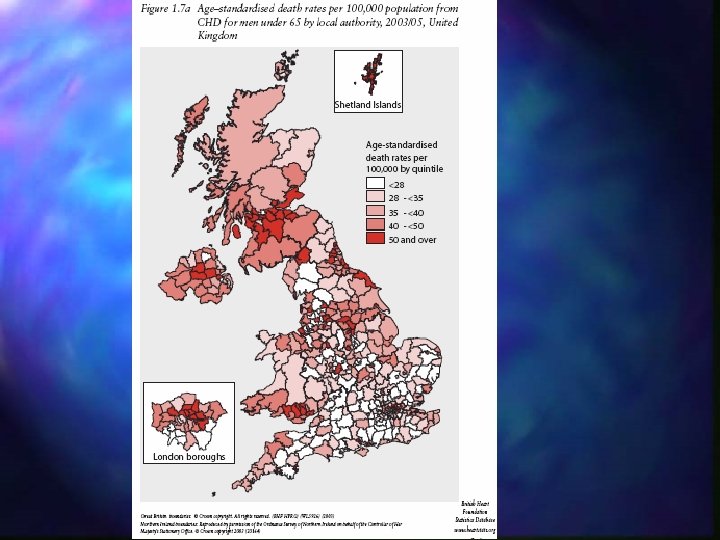
Deaths from CHD
The CVS is subject to disease processes e. g. Atherosclerosis & hypertension are disease processes that lead to the development of :
Structure/ Function of CVS n 2 parts: Pump n Vessels n
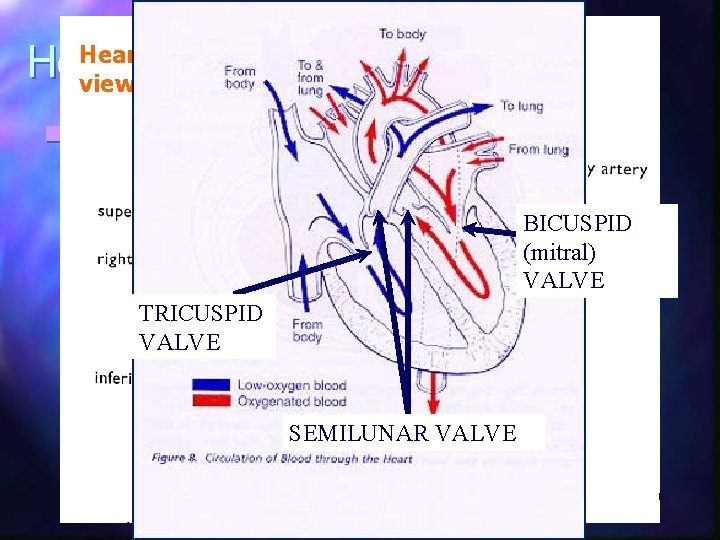
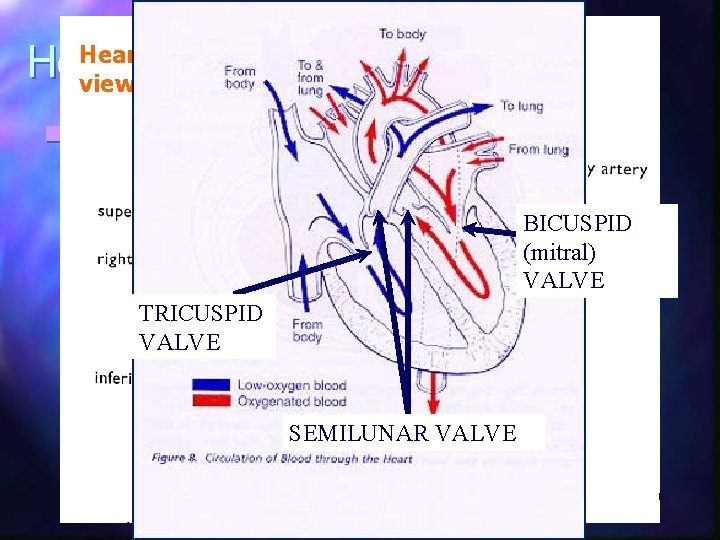
Heart external view n Double pump Right side – pumps to lungs (pulmonary circulation) BICUSPID n Left side – pumps to body (systemic (mitral) circulation VALVE n Left side > right side TRICUSPID VALVE n Heart Valves prevent backflow of blood n Coronary arteries supply heart muscle with blood (food & oxygen) n SEMILUNAR VALVE
Heart & Blood Supply n Pulmonary artery – deoxygenated blood n Pulmonary vein – oxygenated N. B. Hepatic Portal Vein n Coronary arteries – supply heart does not return blood to heart. n Coronary veins – drain into the right atrium Supplies liver with products of digestion. n Aorta - blood to body (from Important in first pass metabolism L. ventricle) n Vena cava (sup. / inf. ) - drain body (into – allowing toxins to be broken down before systemic circulation R atrium)
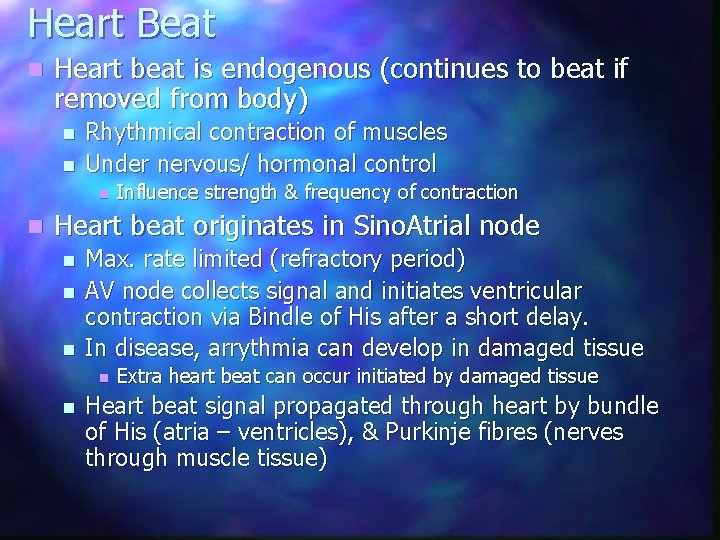
Heart Beat n Heart beat is endogenous (continues to beat if removed from body) n n Rhythmical contraction of muscles Under nervous/ hormonal control n n Influence strength & frequency of contraction Heart beat originates in Sino. Atrial node n n n Max. rate limited (refractory period) AV node collects signal and initiates ventricular contraction via Bindle of His after a short delay. In disease, arrythmia can develop in damaged tissue n n Extra heart beat can occur initiated by damaged tissue Heart beat signal propagated through heart by bundle of His (atria – ventricles), & Purkinje fibres (nerves through muscle tissue)
Heart Sounds n Stethoscope Listen to heart sounds n Lub dub (closing of valves) n Lub – closure of AV valves n Dub – closure of semilunar valves n n Diagnostic of valvular disease n Leaky – indistinct lub/ dub
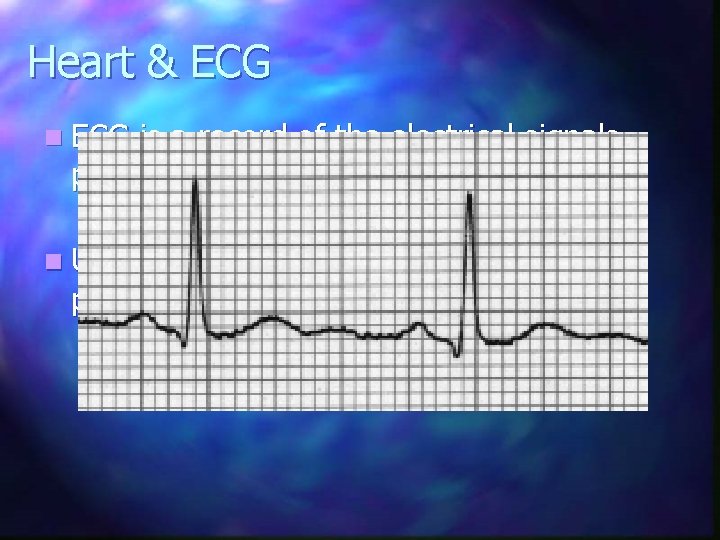
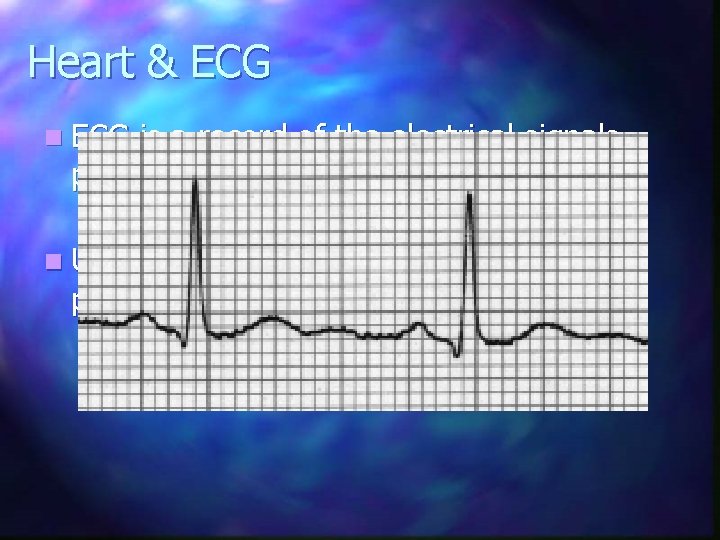
Heart & ECG n ECG is a record of the electrical signals producing the heart beat n ECG= Electro. Cardio. Gram n Used diagnostically to show heart problems
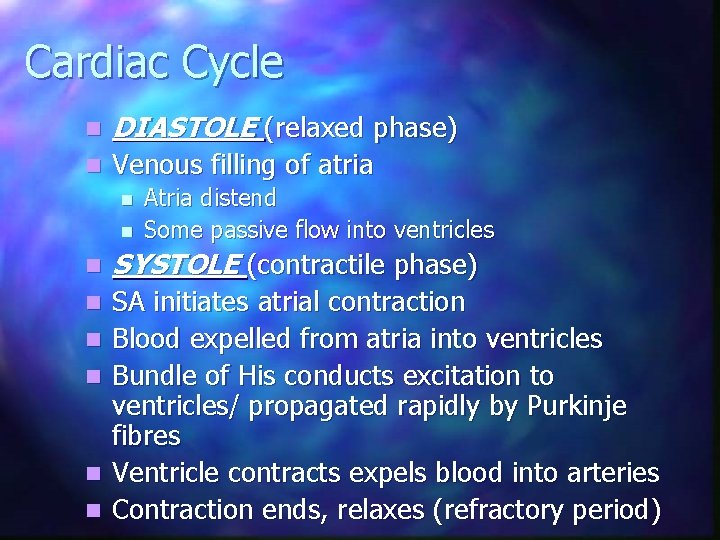
Cardiac Cycle n DIASTOLE (relaxed phase) n Venous filling of atria n n Atria distend Some passive flow into ventricles n SYSTOLE (contractile phase) n SA initiates atrial contraction Blood expelled from atria into ventricles Bundle of His conducts excitation to ventricles/ propagated rapidly by Purkinje fibres Ventricle contracts expels blood into arteries Contraction ends, relaxes (refractory period) n n
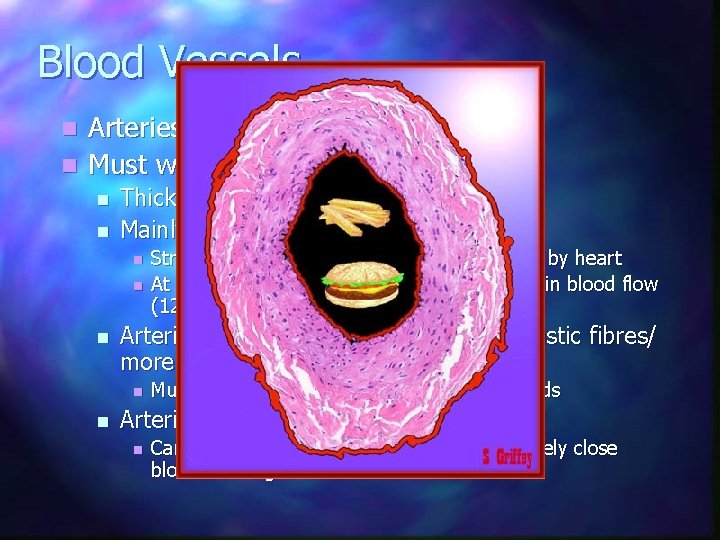
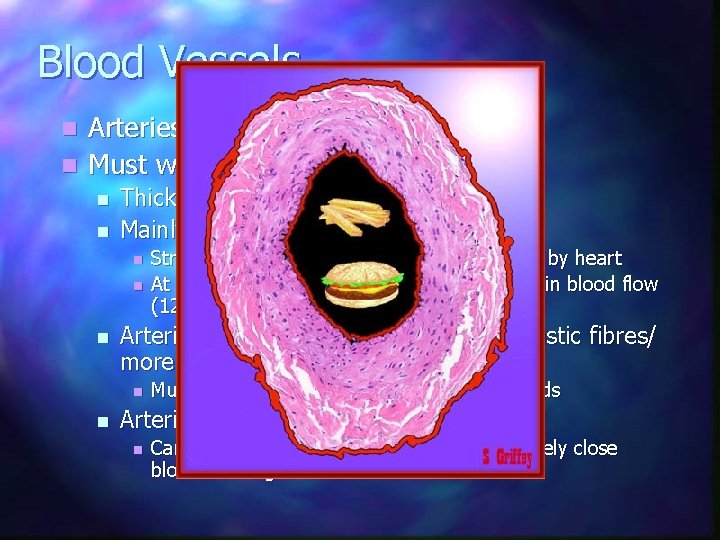
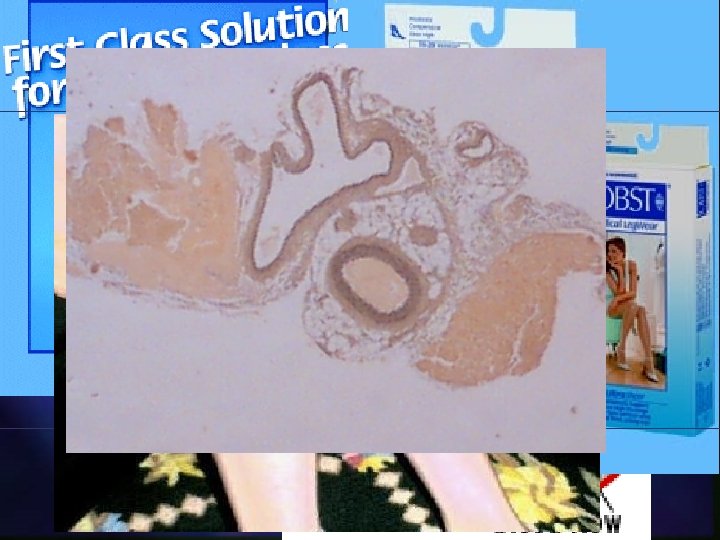
Blood Vessels Arteries n Must withstand high pressure n n n Thick walled Mainly elastic fibres near heart n n n Arteries more distant from heart less elastic fibres/ more muscle (under nervous control) n n Stretch to absorb pressure of blood expelled by heart At diastole stretched arteries relax so maintain blood flow (120/80 mm. Hg) Muscles regulate blood flow into capillary beds Arteries lead to arterioles n Can have pre-capillary sphincters to completely close blood flow e. g to skin in cold
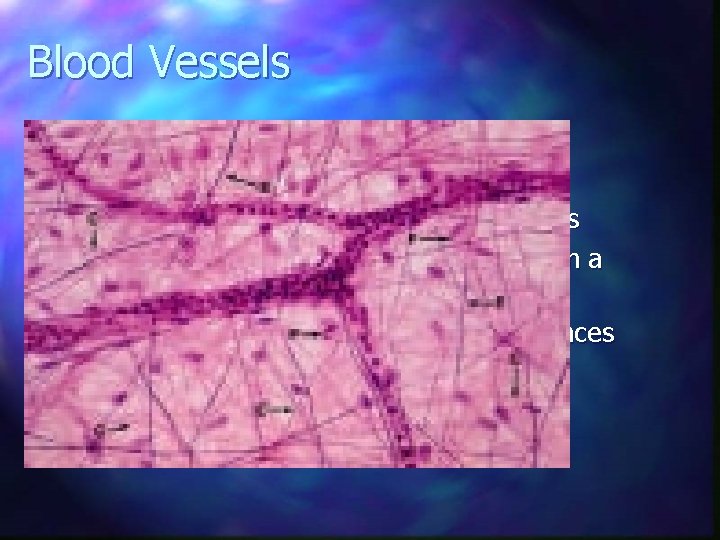
Blood Vessels n Capillaries Wall single cell thick n Allows exchange of soluble substances n No cell more than few cell widths from a capillary n Diffusion rapid over these short distances n
Blood vessels n Veins Less muscle/ elastic fibre than arteries n Floppy n Low pressure in vein – requires valves to stop backflow n Muscle pumping in calves helps venous return (Economy Class Syndrome) n
Blood Pressure n High arterial blood pressure (80 -120 mm. Hg (systolic/ diastolic) n Rapid fall in BP in arterioles/ capillaries n Very low BP in veins
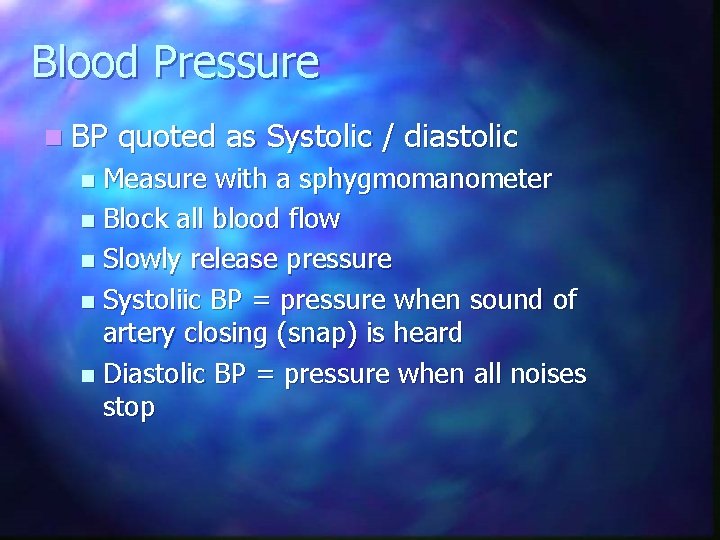
Blood Pressure n BP quoted as Systolic / diastolic Measure with a sphygmomanometer n Block all blood flow n Slowly release pressure n Systoliic BP = pressure when sound of artery closing (snap) is heard n Diastolic BP = pressure when all noises stop n
Summary of Structure
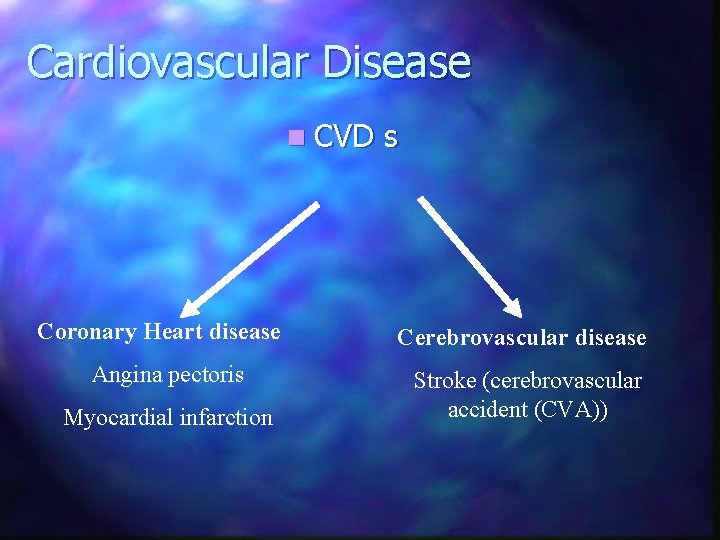
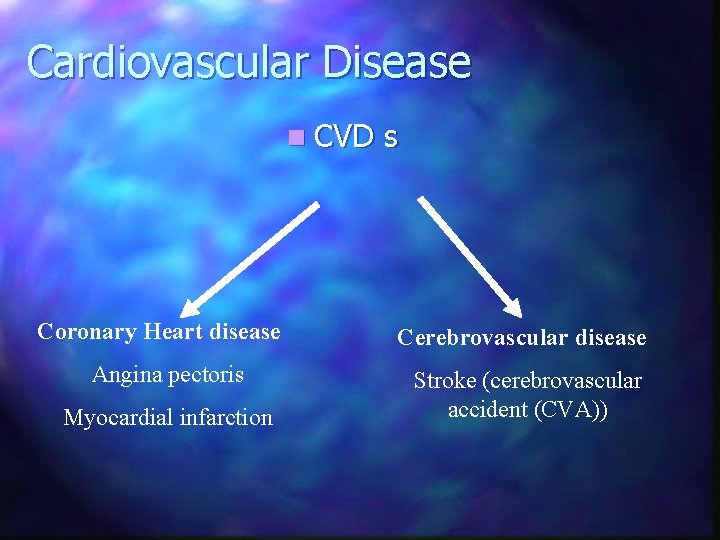
Cardiovascular Disease n CVD Coronary Heart disease Angina pectoris Myocardial infarction s Cerebrovascular disease Stroke (cerebrovascular accident (CVA))
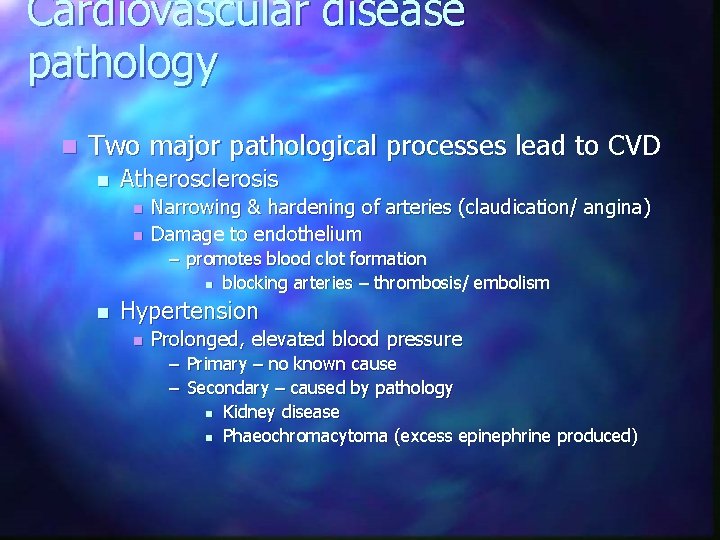
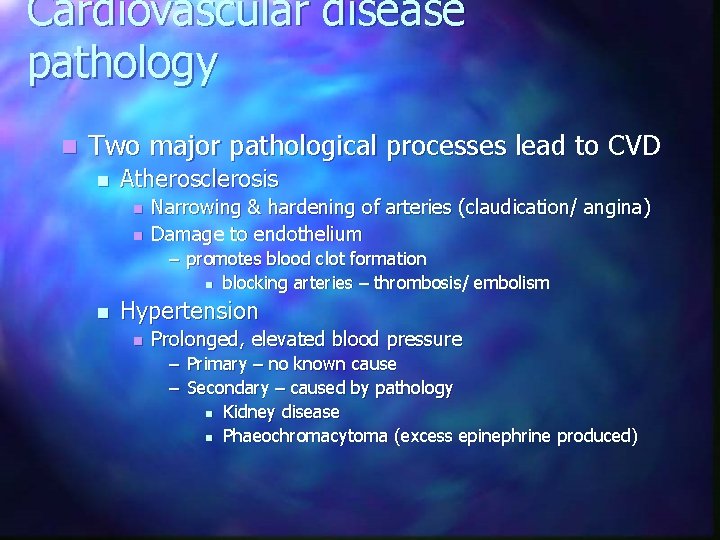
Cardiovascular disease pathology n Two major pathological processes lead to CVD n Atherosclerosis n n Narrowing & hardening of arteries (claudication/ angina) Damage to endothelium – promotes blood clot formation n blocking arteries – thrombosis/ embolism n Hypertension n Prolonged, elevated blood pressure – Primary – no known cause – Secondary – caused by pathology n Kidney disease n Phaeochromacytoma (excess epinephrine produced)
Atherosclerosis Typically starts in childhood, progresses in adulthood. n Damage to the arterial wall caused by e. g. n n n elevated levels of cholesterol and triglyceride in the blood high blood pressure. tobacco smoke diabetes
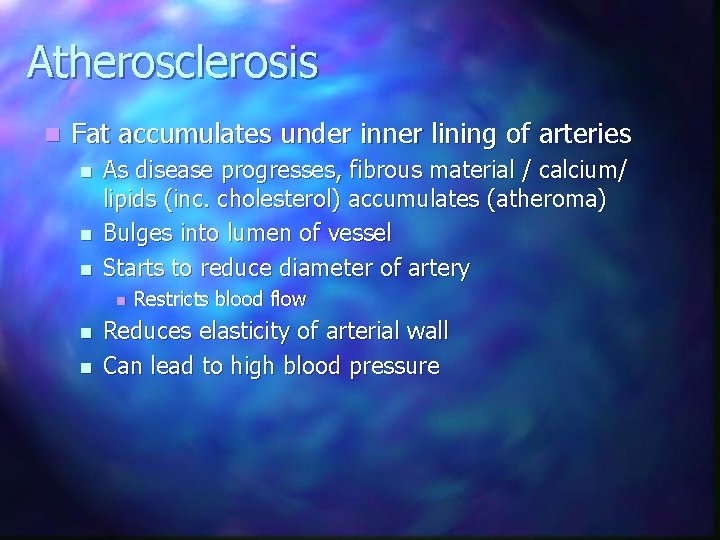
Atherosclerosis n Fat accumulates under inner lining of arteries n n n As disease progresses, fibrous material / calcium/ lipids (inc. cholesterol) accumulates (atheroma) Bulges into lumen of vessel Starts to reduce diameter of artery n n n Restricts blood flow Reduces elasticity of arterial wall Can lead to high blood pressure
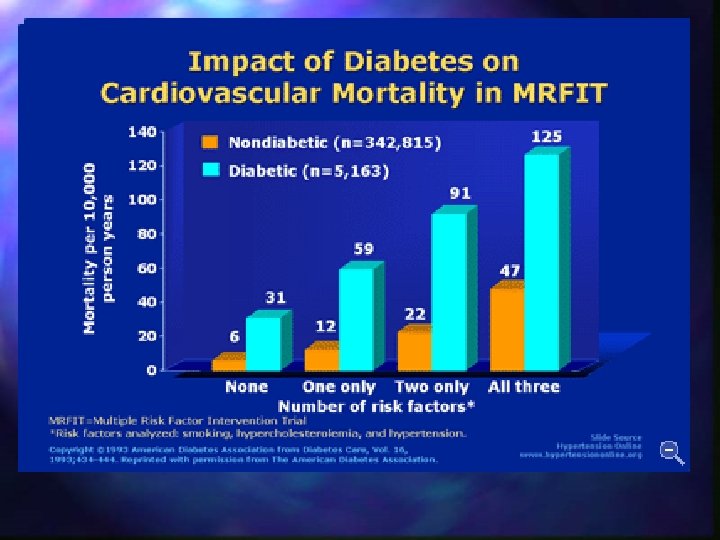
Atherosclerosis n Progression accelerated by: n n n High blood cholesterol (especially LDL or "bad" cholesterol over 100 mg/d. L) Cigarette smoking and exposure to tobacco smoke High blood pressure Diabetes mellitus Obesity Physical inactivity
Cholesterol & CVD n Cholesterol – steroid – Cell membranes, hormones, bile salts Most cholesterol in blood is synthesised by liver n Dietary cholesterol acts to suppress liver biosynthesis n n Dietary cholesterol NOT important risk factor for CVD (overall cholesterol should be less than 200 mg/dl) n Saturated fats (animal) are used by liver to produce cholesterol n High dietary saturated fat INCREASES blood cholesterol levels!!
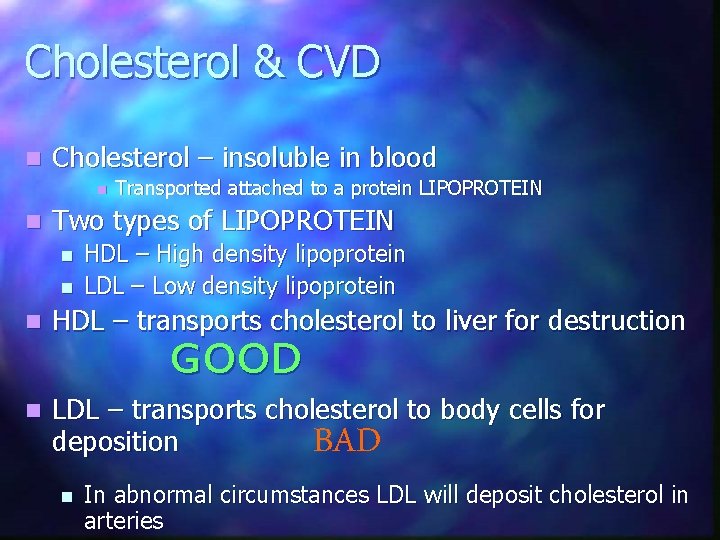
Cholesterol & CVD n Cholesterol – insoluble in blood n n Transported attached to a protein LIPOPROTEIN Two types of LIPOPROTEIN n n HDL – High density lipoprotein LDL – Low density lipoprotein n HDL – transports cholesterol to liver for destruction n LDL – transports cholesterol to body cells for deposition GOOD BAD n In abnormal circumstances LDL will deposit cholesterol in arteries
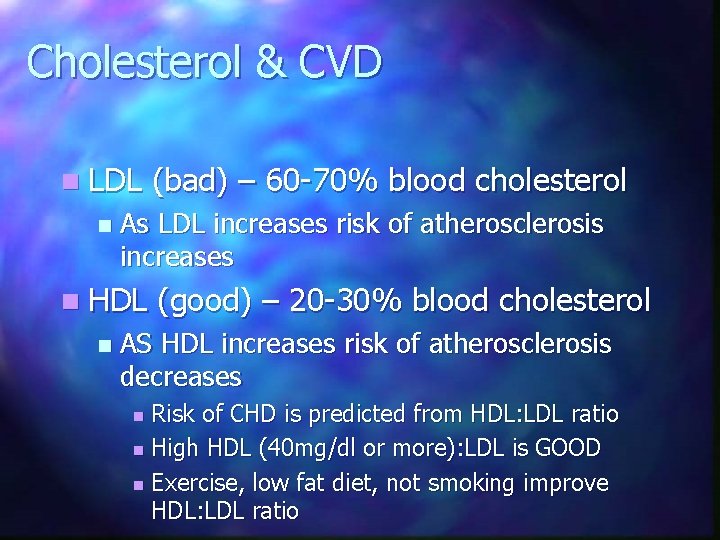
Cholesterol & CVD n LDL n As LDL increases risk of atherosclerosis increases n HDL n (bad) – 60 -70% blood cholesterol (good) – 20 -30% blood cholesterol AS HDL increases risk of atherosclerosis decreases Risk of CHD is predicted from HDL: LDL ratio n High HDL (40 mg/dl or more): LDL is GOOD n Exercise, low fat diet, not smoking improve HDL: LDL ratio n
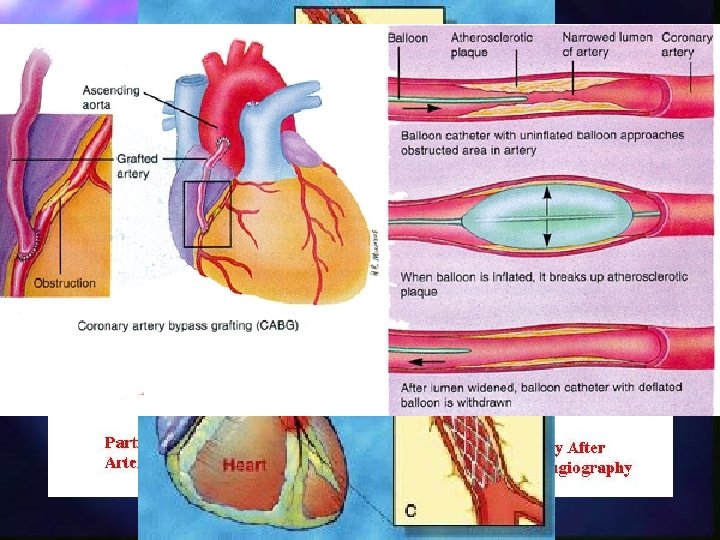
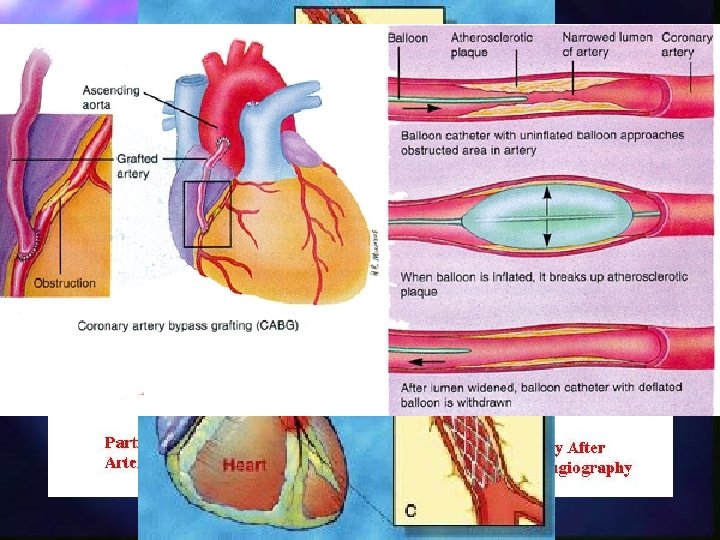
Atherosclerosis – Heart - AP n Narrowing of coronary arteries leads to ischaemia (inadequate blood flow) n n Pain - angina pectoris (AP) due to ischaemia in heart muscle AP only during exertion of heart (when O 2 needs are high) n n n Glycerol trinitrite tablets release Nitric oxide (dilates blood vessels) Angioplasty/ Stents Bypass surgery
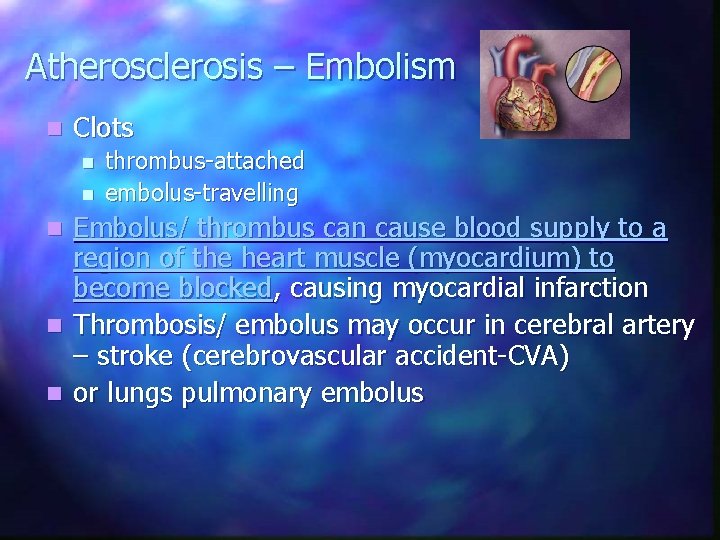
Atherosclerosis – Embolism n Clots n n thrombus-attached embolus-travelling Embolus/ thrombus can cause blood supply to a region of the heart muscle (myocardium) to become blocked, causing myocardial infarction n Thrombosis/ embolus may occur in cerebral artery – stroke (cerebrovascular accident-CVA) n or lungs pulmonary embolus n
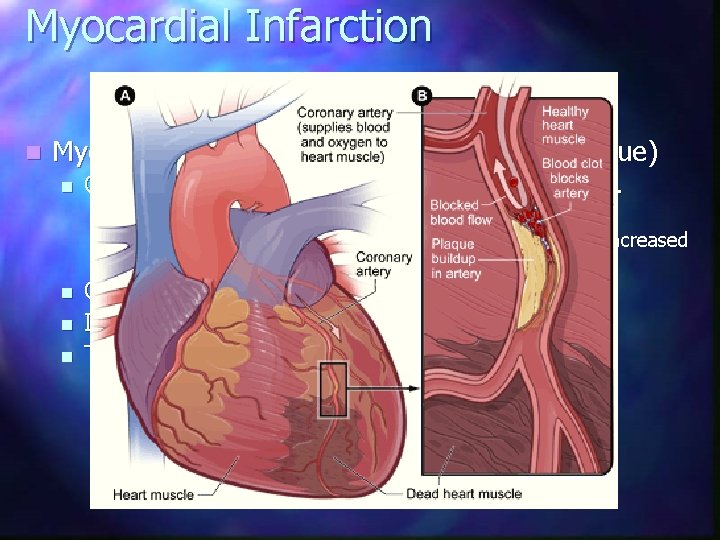
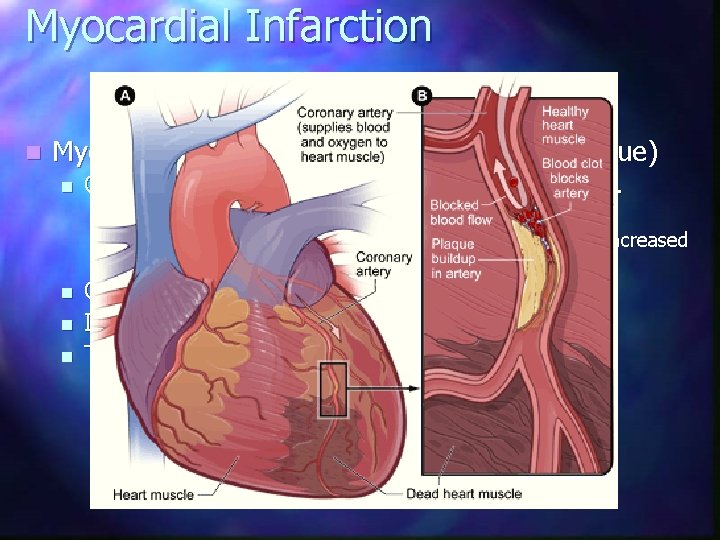
Myocardial Infarction n Myocardial infarction – MI (death of heart tissue) n Caused by a sudden blockage to a coronary artery. n n n Due thrombosis/ embolis Atherosclerosis (may cause angina symptoms) leads to increased likelihood that thombosis will occur. Causes pain (15 min) in arm, neck, jaw; nausea. If large artery blocked – collapse, sudden death Tissue dies forming a scar, can cause: n n n Heart failure (weak pumping action) Arrythmia, irregular contraction Cardiac arrest – ventricular fibrillation
Hypertension n Persistently high resting blood pressure e. g. diastolic >90 mm. Hg (normal 120/80; high 140/90) n Often caused by atherosclerosis leading to narrowing of arteries or loss of elasticity n Risk factor for majority of CVDs (incl. CHD)
Hypertension – risk factors n n n Diet (high salt (Na+), high fat) n Nicotine (vasoconstrictor) Smoking Obesity Genetic predisposition Stress
Risk Factors for CVD- SQA n Modifiable n Diet, Smoking, Activity, Obesity n Non n modifiable Age, Gender, Race, Heredity
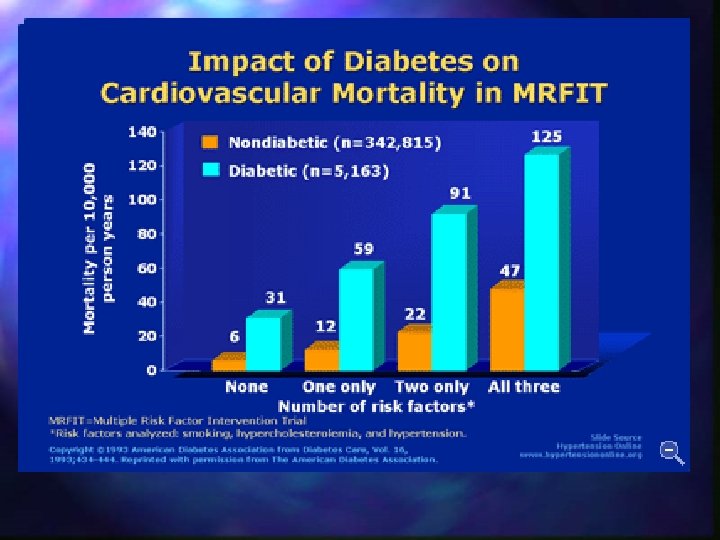
Risk factors Summary What other factors contribute to heart disease risk? • Diabetes • mellitus — The risk of heart disease in people who drink • Obesity and overweight — • Diabetes seriously increases your risk of developing moderate amounts of alcohol (an average of one drink cardiovascular disease. for women or two drinks for men per day) is lower than • People who have excess body fat — especially if a lot of it is at • risks are even greater if blood sugar is not well controlled. in nondrinkers. One drink is defined as 1 -1/2 fluid the waist — are more likely to develop heart disease and stroke Physical inactivity • About three-quarters of people with diabetes die of some form of ounces (fl oz) of 80 -proof spirits (such as bourbon, even if they have no other risk factors. Regular, moderate-to-vigorous physical activity helps prevent heart or blood vessel disease. Scotch, vodka, gin, etc. ), 1 fl oz of 100 -proof spirits, 4 fl High blood pressure High blood cholesterol and blood vessel disease. • Excess weight increases the heart's work. It also raises blood oz of wine or 12 fl oz of beer. It's not recommended High blood pressure increases the heart's workload, causing As blood cholesterol rises, so does risk of coronary heart The more vigorous the activity, the greater your benefits. pressure and blood cholesterol and triglyceride levels, and that nondrinkers start using alcohol or that drinkers the heart to thicken and become stiffer. disease. Physical activity can help control blood cholesterol, diabetes and lowers HDL ("good") cholesterol levels. increase the amount they drink. Tobacco smoke It also increases your risk of stroke, heart attack, kidney failure When other risk factors (such as high blood pressure and tobacco obesity, as well as help lower blood pressure in some people. • Smokers' risk of developing coronary heart disease is 2– 4 times that and congestive heart failure. • It can also make diabetes more likely to develop. Many obese smoke) are present, this risk increases even more. When high blood pressure exists with obesity, smoking, high of nonsmokers. and overweight people may have difficulty losing weight. But by A person's cholesterol level is also affected by age, sex, blood cholesterol levels or diabetes, the risk of heart attack or stroke • risk factor for sudden cardiac death: about twice the risk of losing even as few as 10 pounds, you can lower your heart heredity and diet. increases several times. nonsmokers. disease risk. • Exposure to other people's smoke increases the risk of heart disease even for nonsmokers.
Exercise & CVS n Cardiovascular system (CVS) delivers oxygen & nutrients to body tissues, removes wastes n n During exercises more O 2 & nutrients required by exercising tissues (muscles), wastes removed Exercise effects Cardiovascular system function n n Cardiac output increased Circulation redistributed to important tissues
Cardiac Output n Cardiac output (C. O. ) = volume of blood pumped per min. by the heart n Regulated by: – Heart rate (H. R. ) – Stroke volume (S. V. ) n C. O. = H. R. x S. V.
Exercise effects on Heart n Exercise causes HR & SV to increase i. e. CO n Meets needs of muscles
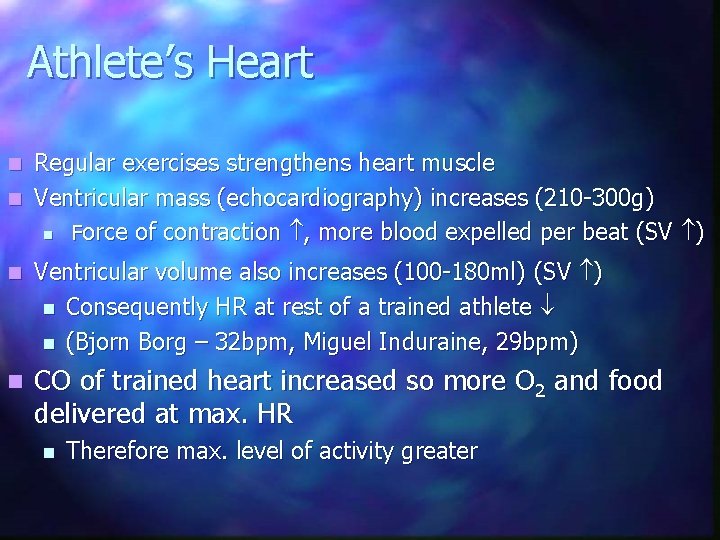
Athlete’s Heart Regular exercises strengthens heart muscle n Ventricular mass (echocardiography) increases (210 -300 g) n Force of contraction , more blood expelled per beat (SV ) n n Ventricular volume also increases (100 -180 ml) (SV ) n Consequently HR at rest of a trained athlete n (Bjorn Borg – 32 bpm, Miguel Induraine, 29 bpm) n CO of trained heart increased so more O 2 and food delivered at max. HR n Therefore max. level of activity greater
Redistribution of Blood flow n During exercise blood flow directed away from non-essential needs (gut, kidney) n Redirected to heart, muscles, skin (cooling) n Vasodilation/ vasoconstriction of supplies to these tissues.
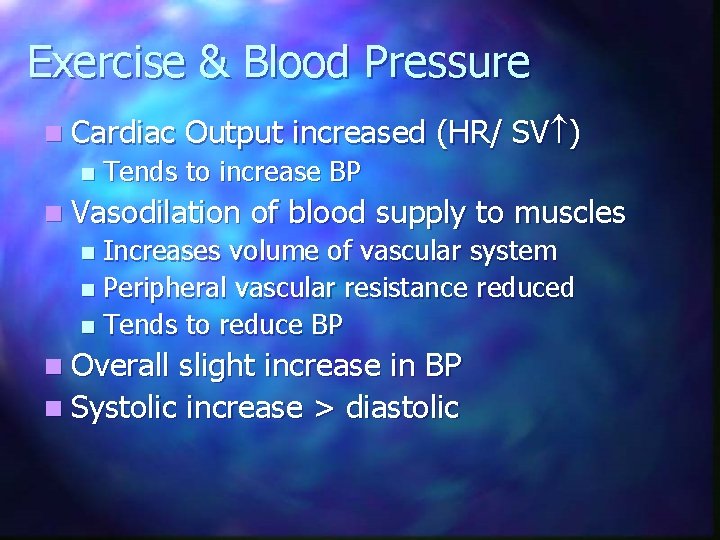
Exercise & Blood Pressure n Cardiac n Output increased (HR/ SV ) Tends to increase BP n Vasodilation of blood supply to muscles Increases volume of vascular system n Peripheral vascular resistance reduced n Tends to reduce BP n n Overall slight increase in BP n Systolic increase > diastolic
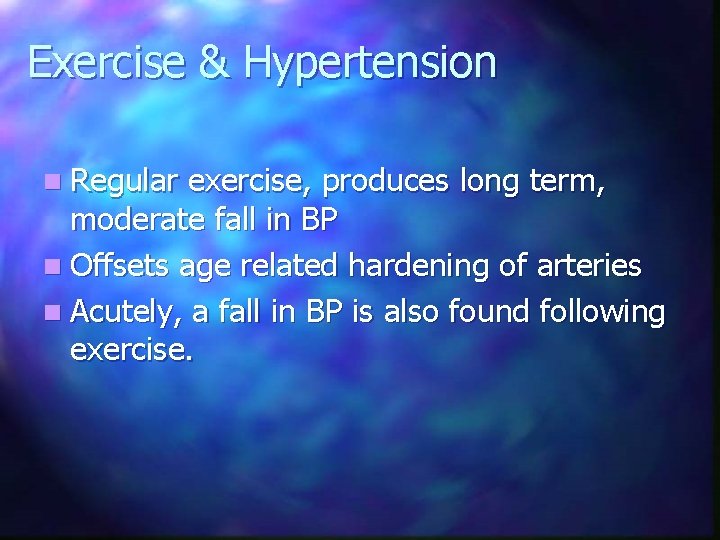
Exercise & Hypertension n Regular exercise, produces long term, moderate fall in BP n Offsets age related hardening of arteries n Acutely, a fall in BP is also found following exercise.
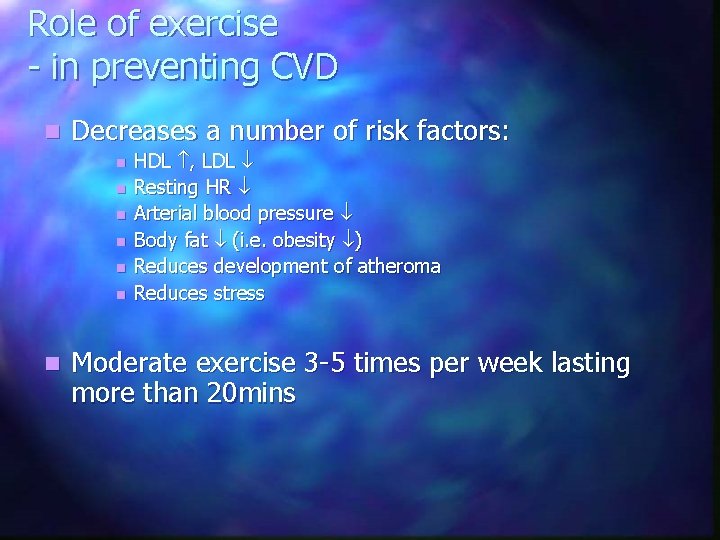
Role of exercise - in preventing CVD n Decreases a number of risk factors: n n n n HDL , LDL Resting HR Arterial blood pressure Body fat (i. e. obesity ) Reduces development of atheroma Reduces stress Moderate exercise 3 -5 times per week lasting more than 20 mins

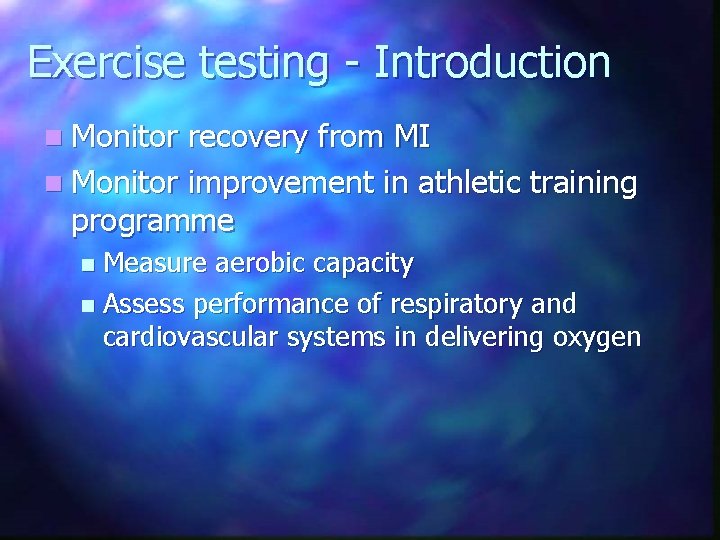
Exercise testing - Introduction n Monitor recovery from MI n Monitor improvement in athletic training programme Measure aerobic capacity n Assess performance of respiratory and cardiovascular systems in delivering oxygen n
Exercise testing - Principles Oxygen required by body to work n Maximum work rate – determined by body’s ability to deliver oxygen to body n n VO 2 max – maximal oxygen uptake Higher the VO 2 max, the greater the aerobic fitness Measure by exercising to exhaustion and directly measure O 2 uptake and CO 2 ouput
Exercise testing – Direct Method n Treadmill/ bicycle ergometer Using online gas analysis n Progressively increase workload until no further increase in O 2 consumption n i. e. exercise to exhaustion n Oxygen consumption at that point = VO 2 max n n Suitable for fit people
Exercise testing – Indirect Method n Shuttle test Run between two cones (20 m apart) n Rate determined by a tape (beep) n Subject continues until they can’t maintain pace n n Number of completed shuttles can be used to predict VO 2 max
Exercise Testing – Sub maximal n n n If exercise to exhaustion clinically contraindicated Submaximal testing used Patient O 2 consumption measured at various levels of work intensity (submaximal) Graph of O 2 consumption vs. HR plotted Theoretical max. HR calculated (220 -age) Graph extrapolated to estimate theoretical max. O 2 consumption
Exercise Testing – Sub maximal n Assumptions: n n Direct relation between HR and O 2 consumption and intensity of exercise Sources of error: n HR affected by other factors: – Emotion – Temperature – Anxiety n Predicted HR may be inaccurate for a given individual
Exercise Stress Testing n Used to diagnose heart abnormality only present under stressed conditions n Bruce Protocol Treadmill speed/gradient increased incrementally n Exercise to exhaustion n n ECG can be monitored to evaluate effect of exercise on heart