COLON RECTUM ANUS DIAGNOSTIC EVALUATION Digital Rectal Examination



- Slides: 58
COLON , RECTUM & ANUS
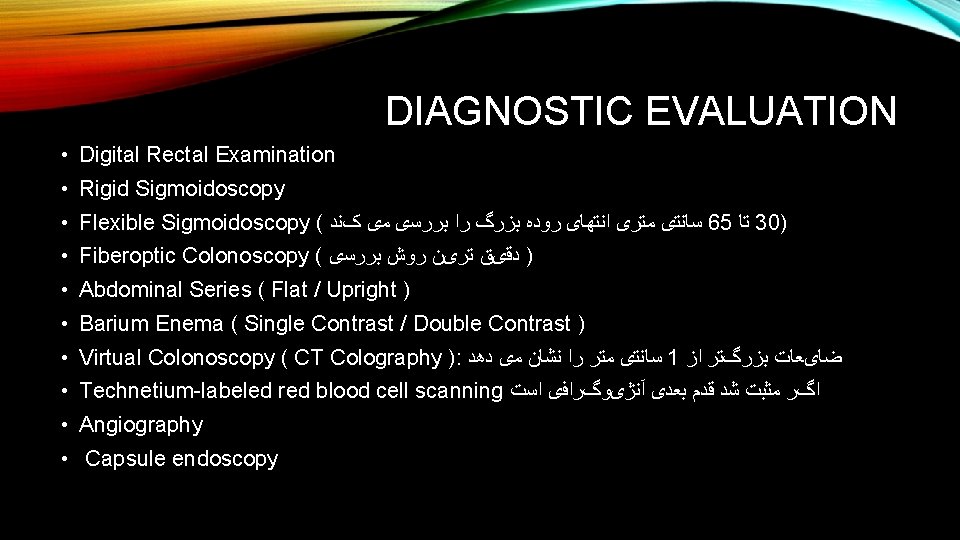
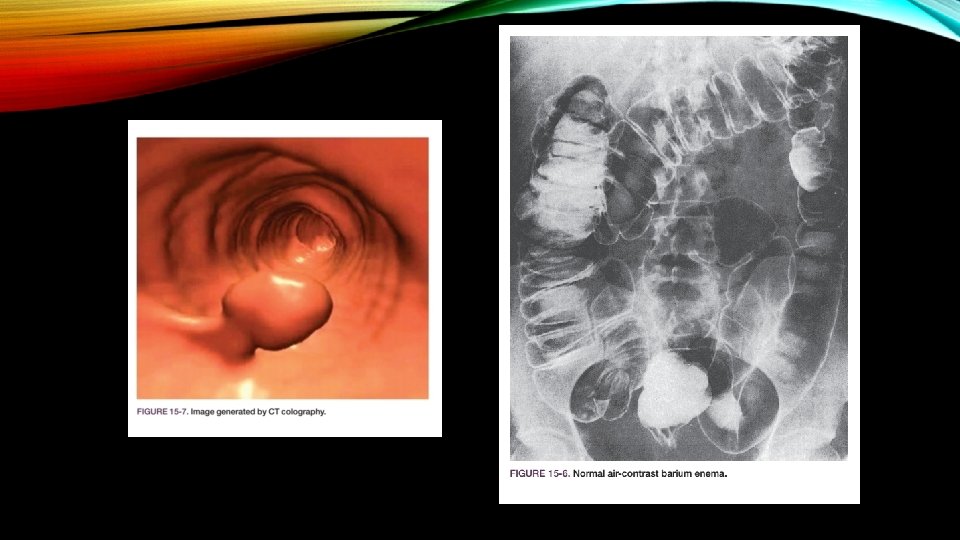
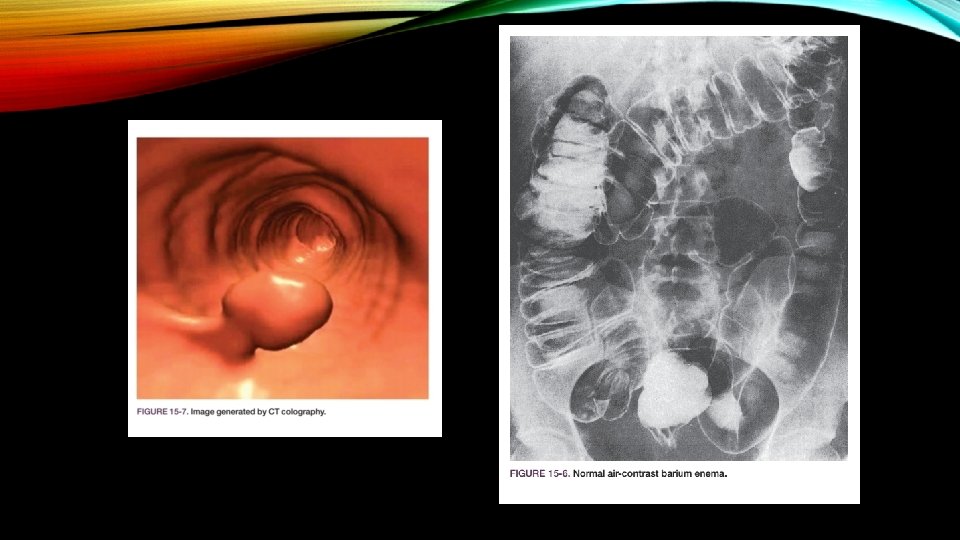
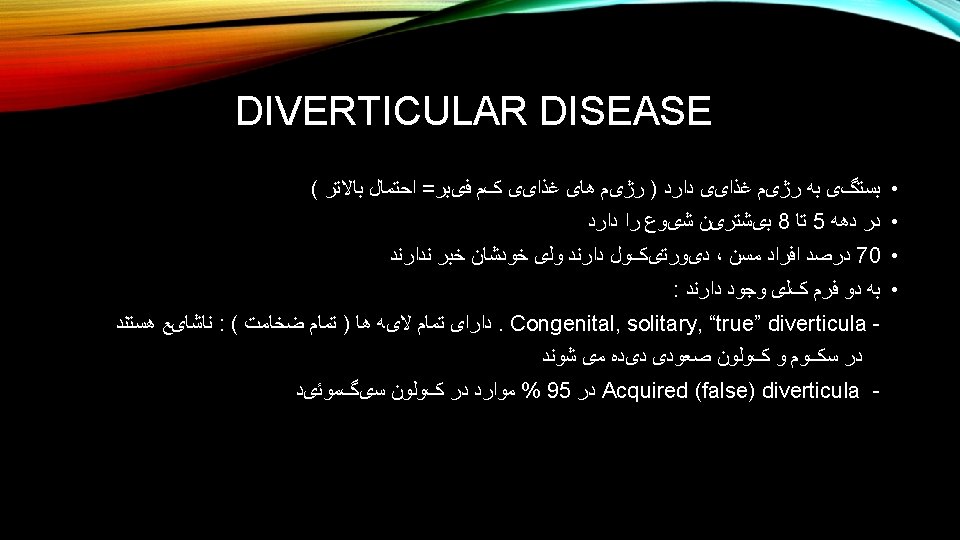
DIAGNOSTIC EVALUATION • Digital Rectal Examination • Rigid Sigmoidoscopy • Flexible Sigmoidoscopy ( ﺳﺎﻧﺘی ﻣﺘﺮی ﺍﻧﺘﻬﺎی ﺭﻭﺩﻩ ﺑﺰﺭگ ﺭﺍ ﺑﺮﺭﺳی ﻣی کﻨﺪ 65 ﺗﺎ 30) • Fiberoptic Colonoscopy ( ) ﺩﻗیﻖ ﺗﺮیﻦ ﺭﻭﺵ ﺑﺮﺭﺳی • Abdominal Series ( Flat / Upright ) • Barium Enema ( Single Contrast / Double Contrast ) • Virtual Colonoscopy ( CT Colography ): ﺳﺎﻧﺘی ﻣﺘﺮ ﺭﺍ ﻧﺸﺎﻥ ﻣی ﺩﻫﺪ 1 ﺿﺎیﻌﺎﺕ ﺑﺰﺭگﺘﺮ ﺍﺯ • Technetium-labeled red blood cell scanning ﺍگﺮ ﻣﺜﺒﺖ ﺷﺪ ﻗﺪﻡ ﺑﻌﺪی آﻨژیﻮگﺮﺍﻓی ﺍﺳﺖ • Angiography • Capsule endoscopy

TERMINOLOGY • Colostomy Loop Colostomy Hartmann’s procedure Mucous Fistula • Ileostomy • Proctocolectomy • Abdominoperineal Resection (APR) • Low Anterior Resection (LAR) ﺗﺎ ﺍﻭﺍﺳﻂ ﺭکﺘﻮﻡ ﺑﺮﺩﺍﺷﺘﻪ ﻣیﺸﻮﺩ

BENIGN COLONIC DISORDERS
DIVERTICULOSIS ● ● ● presence of multiple false diverticula in the colon ﻣﻮﺍﺭﺩ ﺑﺪﻭﻥ ﻋﻼﻣﺖ ﻫﺴﺘﻨﺪ % 80 ﺩﺭ ﻋﻼﺋﻢ : recurrent abdominal pain often localized to the LLQ functional changes in bowel habits, including bleeding, constipation, diarrhea, or alternating constipation and diarrhea ● ﻣﻌﺎیﻨﻪ : LLQ ﺍکﺜﺮﺍ ﻧکﺘﻪ ﻣﺜﺒﺘی ﻧﺪﺍﺭﻧﺪ یﺎ ﺩﺭ ﺣﺪ یک ﺗﻨﺪﺭﻧﺲ ﺧﻔیﻒ ﺩﺭ ● ﺩﺭﻣﺎﻥ : ﺗﻐییﺮ ﺭژیﻢ ﻏﺬﺍیی
DIVERTICULITIS • Diverticulitis describes a limited infection of one or more diverticula, including extension into adjacent tissue : • ﻋﻼﺋﻢ LLQ pain (subacute onset) Alteration in bowel habits (constipation or diarrhea) Occasionally a palpable mass Fever ﺩﺭ ﻣﻮﺍﺭﺩ ﺷﺪیﺪ Generalized Peritonitis ﺍﻧﻮﺍﻉ ﻓیﺴﺘﻮﻟﻬﺎ ﺍیﺠﺎﺩ ﻣیﺸﻮﺩ ، ﺩﺭ ﻣﻮﺍﺭﺩ ﻋﻮﺩ ﻫﺎی ﻣکﺮﺭ
DIAGNOSTIC EVALUATION abdominal radiographs are obtained to rule out pneumoperitoneum : • ﺩﺭ ﻣﻮﺍﺭﺩ ﺣﺎﺩ ( ﻫﻔﺘﻪ ﺑﻌﺪ ﺍﺯ ﻓﺎﺯ ﺣﺎﺩ ﻗﺎﺑﻞ ﺍﻧﺠﺎﻡ ﺍﺳﺖ 3 ﺍﻟی 2 ) کﻨﺘﺮﺍﻧﺪیکﻪ ﺍﺳﺖ ، ﺩﺭ ﻓﺎﺯ ﺣﺎﺩ ﺍﻧﺠﺎﻡ ﺑﺎﺭیﻢ ﺍﻧﻤﺎ : ﻧکﺘﻪ CT scan is the best diagnostic tool to confirm the diagnosis and determine if an abscess is present
DIVERTICULAR BLEEDING • Lower GI bleeding is the primary symptom in 5% to 10% of all patients with diverticular disease • Bleeding from diverticula is occasionally massive (diverticulosis is the most common cause of massive lower GI bleeding) and may be lethal • Of all patients with bleeding distal to the ligament of Treitz, approximately 70% have diverticulosis as the source of the bleeding. Approximately 25% of the time, the bleeding is massive.
TREATMENT • Most diverticular bleeding will stop without intervention • Mesenteric angiography is useful in detecting the source of moderate or rapid colonic bleeding, defi ned as a bleeding rate of 0. 5 m. L/minute or more => Vasopressin / transcatheter embolization • surgical resection of the involved segment of colon
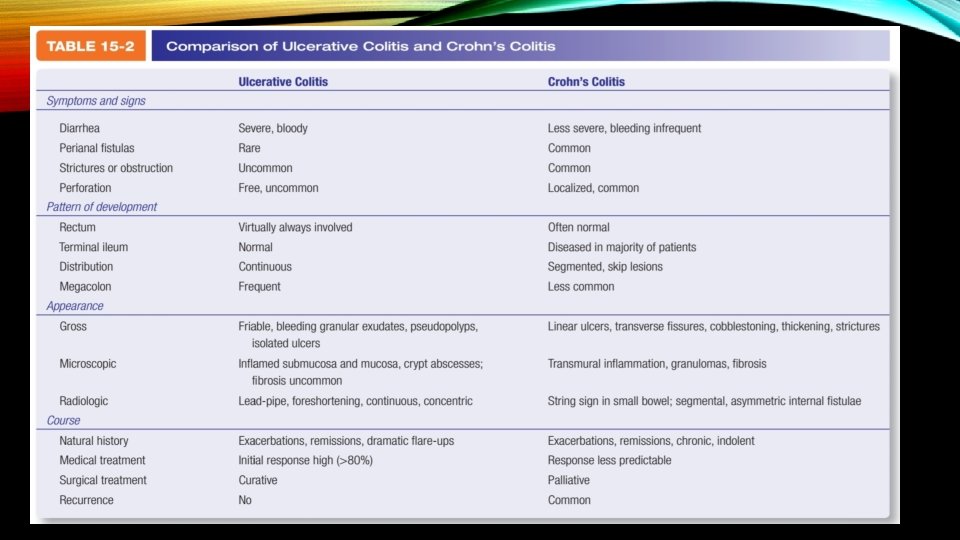
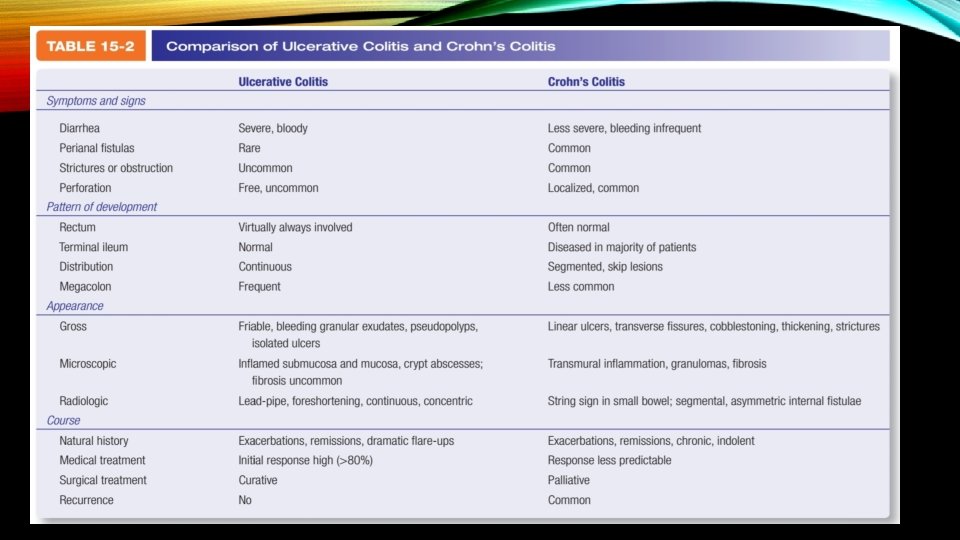
ULCERATIVE COLITIS AND CROHN’S DISEASE OF THE COLON
TREATMENT • Medical therapy is usually the initial treatment. It is successful in approximately 80% of cases / ﺣﺬﻑ ﺷیﺮ ﺍﺯ ﺭژیﻢ ﻏﺬﺍیی Mild Cases = Antidiarrheal agents that slow gut transit (e. g. , loperamide) bulking agents (psyllium seed products) and Moderate Cases = sulfasalazine or mesalamine-based preparations Sever Cases = Steroids / Anti-TNF / Monoclonal antibody (infliximab [Remicade])

SURGICAL THERAPY • Medical therapy fails • Surgically treatable complications ensue (e. g. , hemorrhage, perforation, obstruction, dysplasia, or carcinoma) • Because of the increased risk of carcinoma • Long-standing ulcerative colitis is also an indication for surgical intervention. (The risk increases 1% to 2% per year after the initial 10 years of disease) Total colectomy with proctectomy and ileoanal pull-through is now the operation of choice
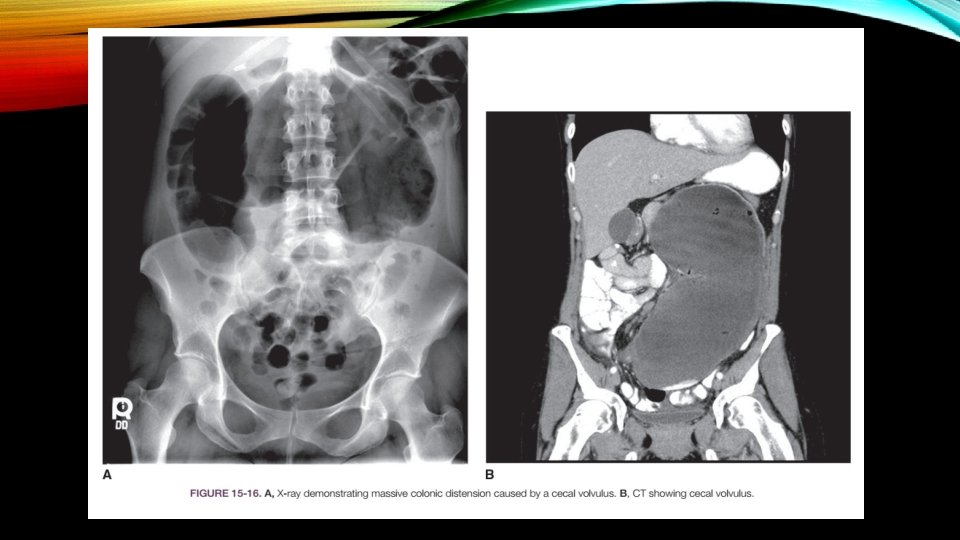
COLONIC OBSTRUCTION AND VOLVULUS • The most common anatomic site of colonic obstruction is the sigmoid colon • • Adenocarcinoma (65%) Scarring associated with diverticulitis (20%) Volvulus (5%) Inflammatory disorders Benign tumors Foreign bodies Fecal impaction Obstructive adhesive bands
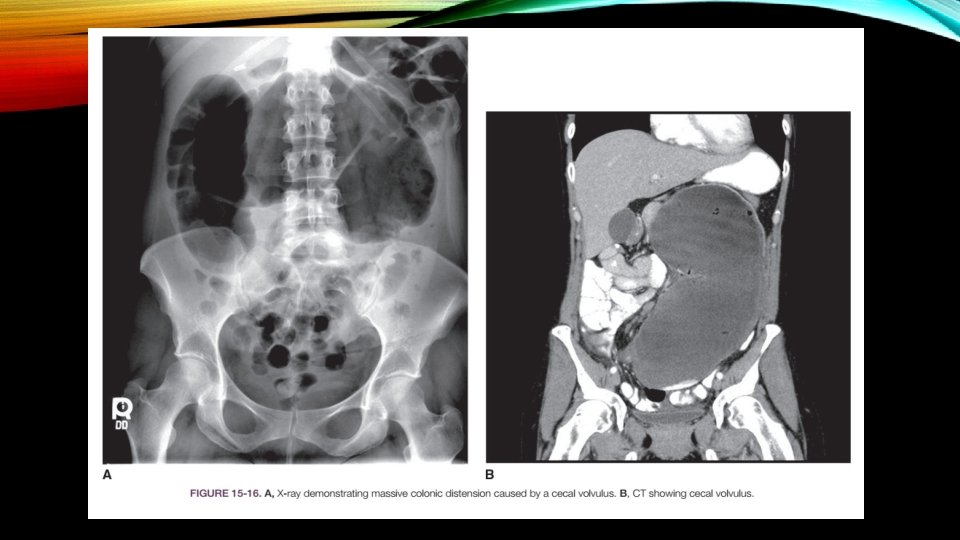
• Complete large bowel obstruction : ﺟﺮﺍﺣی ﻓﻮﺭی • Partial large bowel obstruction : ﻓﺮﺻﺖ ﺩﺍﺭیﻢ ﺗﺎ ﺑیﻤﺎﺭ پﺎیﺪﺍﺭ ﺷﻮﺩ ﻭ ﺑﺮﺭﺳی ﻫﺎی ﺑیﺸﺘﺮ ﺍﻧﺠﺎﻡ گیﺮﺩ Diagnosis : üPlain films of the abdomen : ﺳﺎﻧﺘی ﻣﺘﺮ ﺑﻮﺩ ﺟﺮﺍﺣی ﺑﺎیﺪ ﺻﻮﺭﺕ گیﺮﺩ 12 < ﺍگﺮ ﻗﻄﺮ ﺳکﻮﻡ ü Water-soluble contrast enema ü Colonoscopic examination plays a major role in Ogilvie’s syndrome (localized paralytic ileus of the colon without mechanical obstruction); otherwise, it is reserved for the occasional case of volvulus for decompression or those patients who may need colonic stent placement.
TREATMENT • IV fluids • NGT • Continuous observation until the diagnosis is established • Emergency laparotomy is undertaken for acute large bowel obstruction with cecal distension beyond 12 cm , severe tenderness , evidence of peritonitis, or generalized sepsis • Stent placement = large bowel obstruction due to cancer and without peritonitis
TREATMENT OF OGILVIE’S SYNDROME • IV Neostigmine • If unsuccessful, Fiberoptic Colonoscopy, with decompression and placement of a long rectal decompression tube • Cecostomy may be necessary in cases of recurrence.
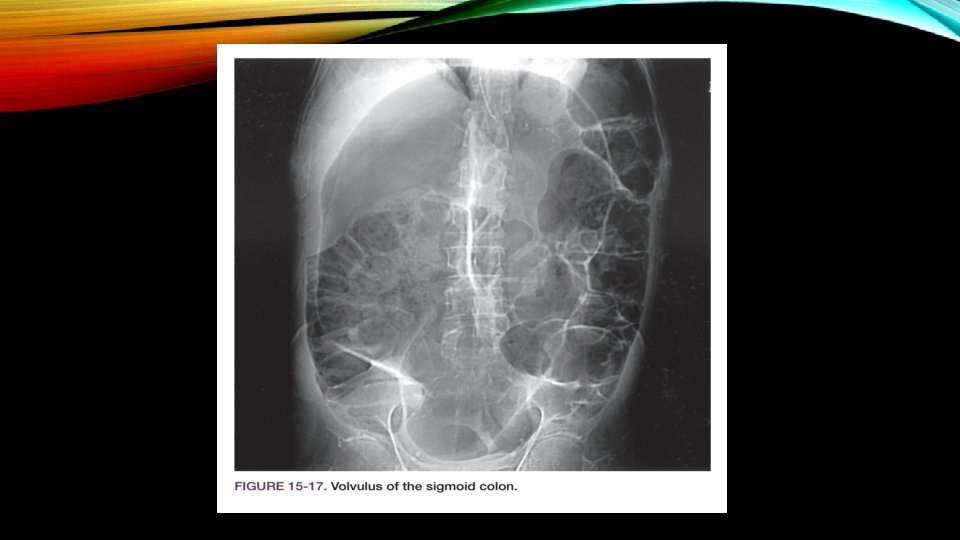
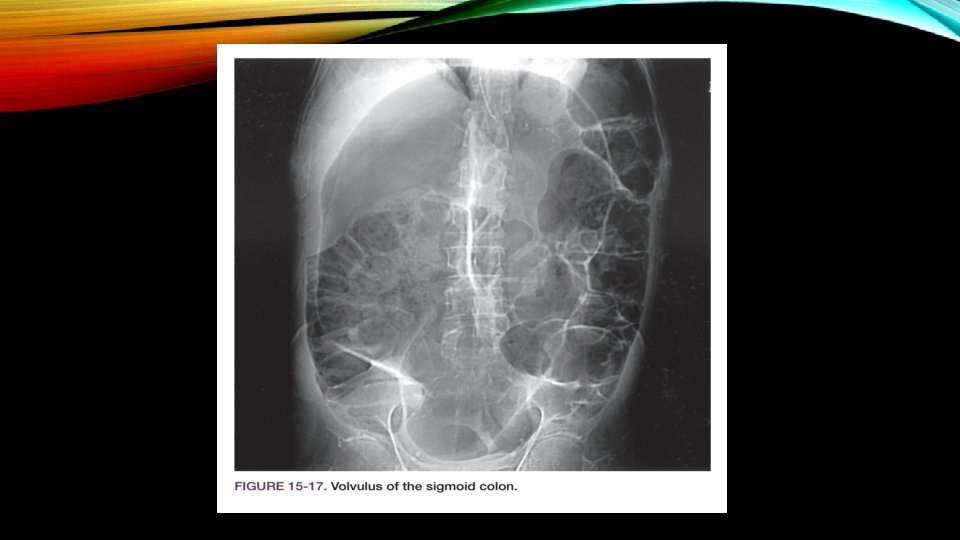
VOLVULUS OF THE LARGE INTESTINE • sigmoid (70%) • cecum (30%) • Volvulus accounts for 5% to 10% of cases of large bowel obstruction • second most common cause of complete colonic obstruction • Stretching and elongation of the sigmoid with age • patients who are confi ned to psychiatric institutions or nursing homes have an increased risk for this disease
CLINICAL PRESENTATION AND EVALUATION • Abdominal distension • Vomiting • Abdominal pain • Obstipation • Tachypnea • Tympany • High-pitched tinkling sounds
DIAGNOSTIC STUDIES • Abdominal x-ray films (kidney bean appearance) • Watersoluble contrast enemas (funnel-like narrowing that often resembles a bird’s beak) • CT scan
TREATMENT • Sigmoidoscopy with rectal tube insertion • Strangulation or Perforation is suspected or if attempts to decompress the bowel are unsuccessful = Emergency operation • Cecal volvulus is always treated surgically, rarely with cecopexy (suturing the cecum to the parietal peritoneum) and most commonly with right hemicolectomy with ileotransverse colostomy
COLORECTAL POLYP • Approximately 5% of all barium enema and 5% to 10% of colonoscopic studies show polyps • Types of Polyps : üInfl ammatory polyps (pseudopolyps) are common in inflammatory bowel disease and have no malignant potential üHamartomas (juvenile polyps and polyps associated with Peutz-Jeghers syndrome) similarly have very low malignant potential and often spontaneously regress or autoamputate üAdenoma are clearly premalignant
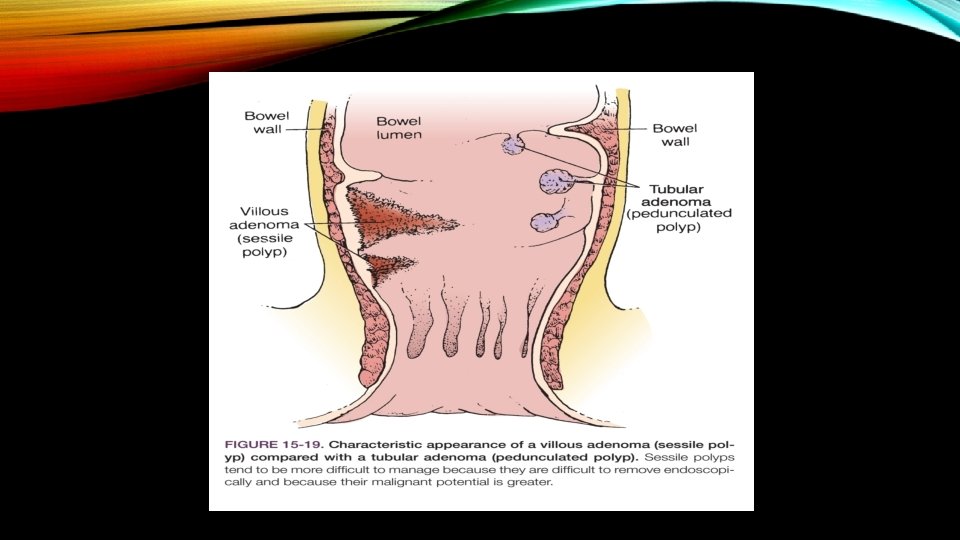
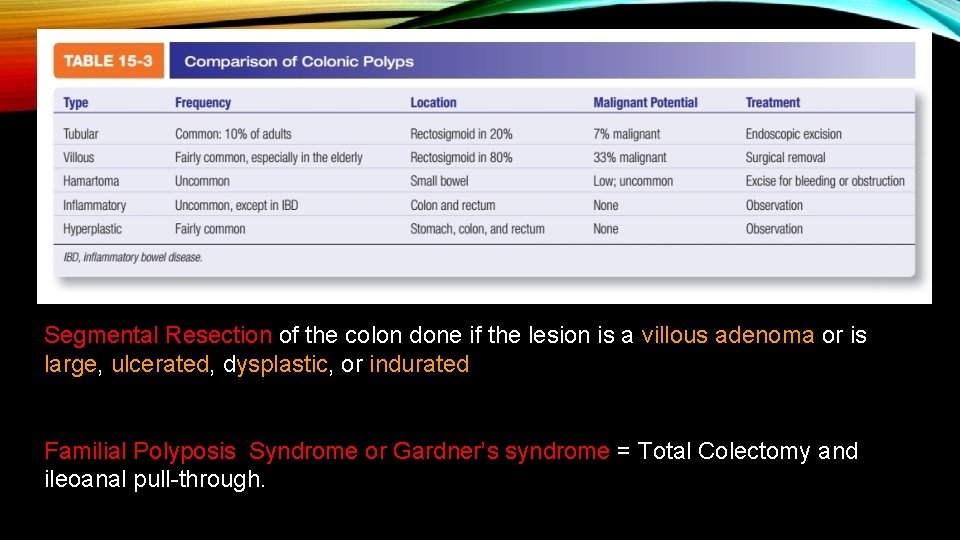
ADENOMAS 1. Tubular (%7 = )ﺍﺣﺘﻤﺎﻝ ﺗﺒﺪیﻞ ﺑﻪ ﺑﺪﺧیﻤی 2. Tubulovillous (% 20 = )ﺍﺣﺘﻤﺎﻝ ﺗﺒﺪیﻞ ﺑﻪ ﺑﺪﺧیﻤی 3. Villous (%33 = )ﺍﺣﺘﻤﺎﻝ ﺗﺒﺪیﻞ ﺑﻪ ﺑﺪﺧیﻤی ﺑﺎﺷﻨﺪ pedunculated یﺎ sessile ﻫﺮ کﺪﺍﻡ ﺍﺯ ﺍیﻦ ﺍﻧﻮﺍﻉ پﻮﻟیپ ﻫﺎ ﻣی ﺗﻮﺍﻧﻨﺪ Tubular and Tubulovillous adenomas are more commonly pedunculated, whereas Villous adenomas are more commonly sessile Villous adenomas >3 cm in diameter have a greater probability of malignancy.
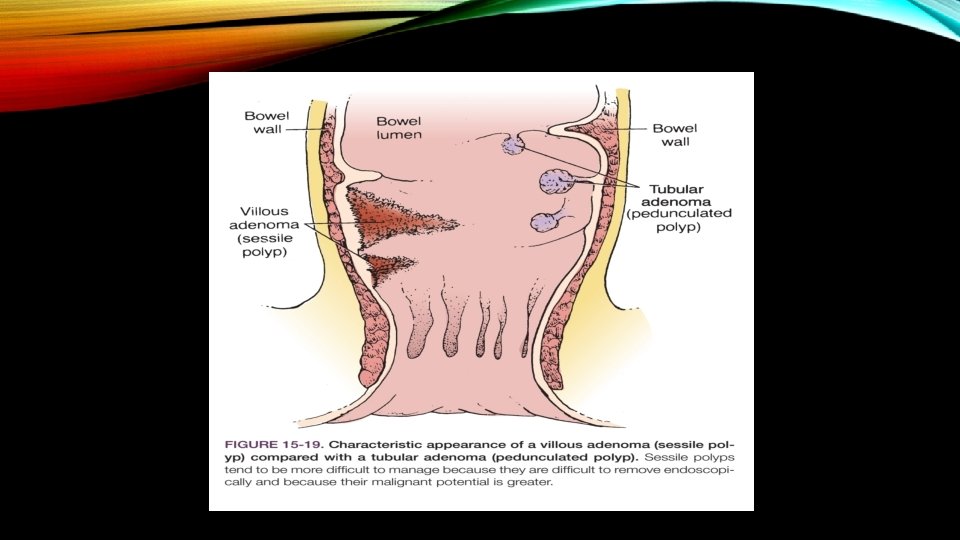
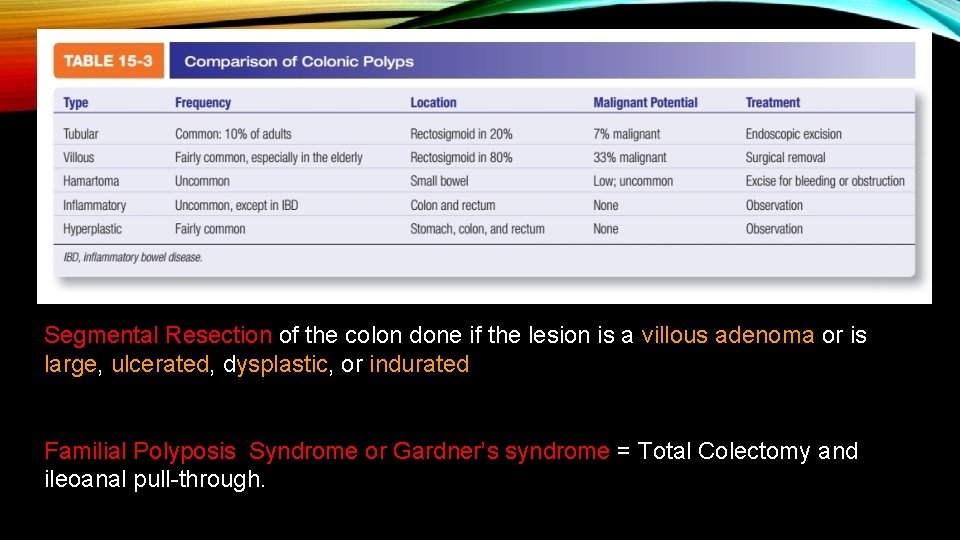
Segmental Resection of the colon done if the lesion is a villous adenoma or is large, ulcerated, dysplastic, or indurated Familial Polyposis Syndrome or Gardner’s syndrome = Total Colectomy and ileoanal pull-through.
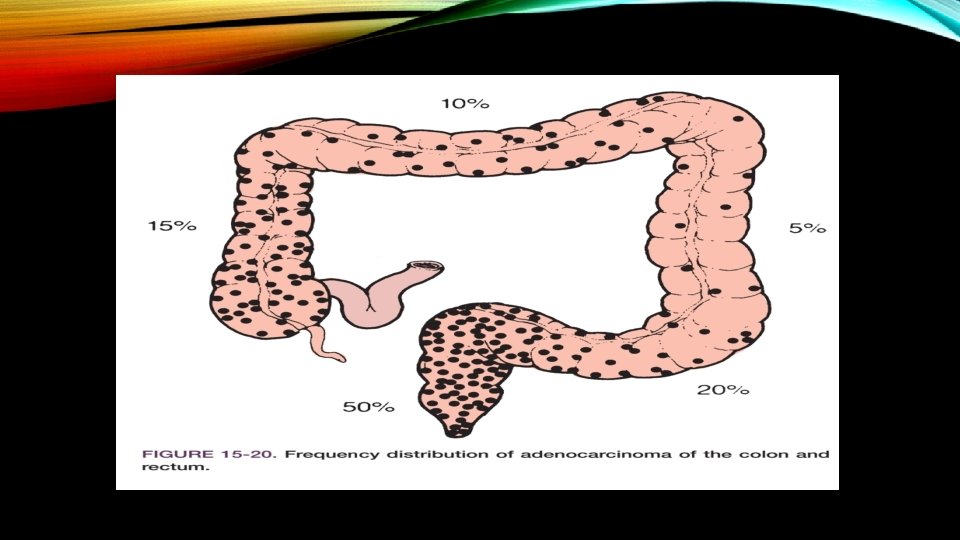
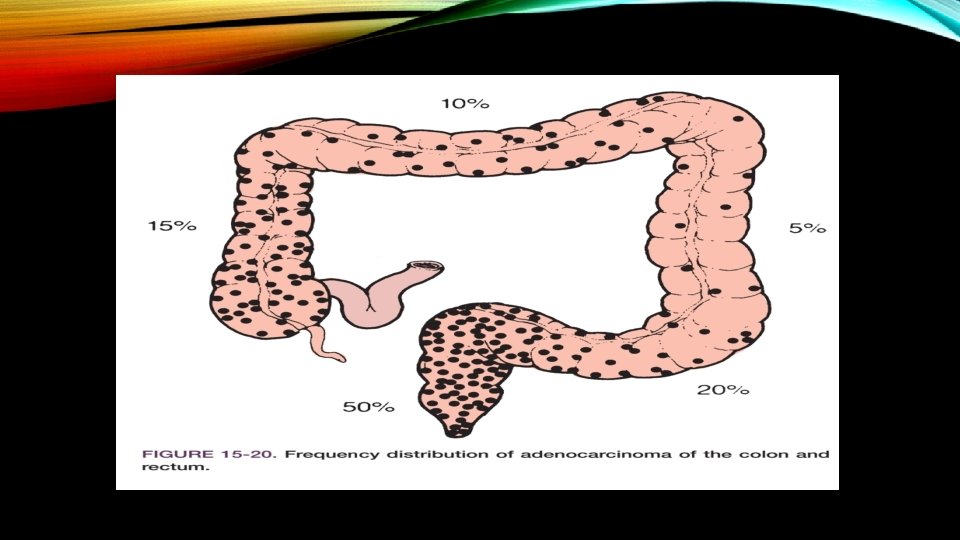
CARCINOMA OF THE COLON AND RECTUM Mild Risk Factors • Age • Diet • Physical Inactivity • Obesity • Smoking • Race • Alcohol
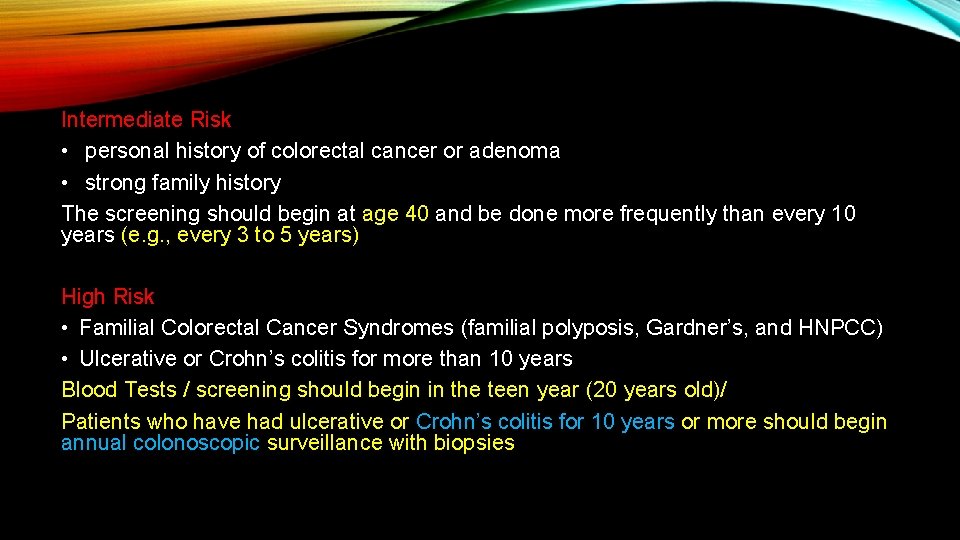
Intermediate Risk • personal history of colorectal cancer or adenoma • strong family history The screening should begin at age 40 and be done more frequently than every 10 years (e. g. , every 3 to 5 years) High Risk • Familial Colorectal Cancer Syndromes (familial polyposis, Gardner’s, and HNPCC) • Ulcerative or Crohn’s colitis for more than 10 years Blood Tests / screening should begin in the teen year (20 years old)/ Patients who have had ulcerative or Crohn’s colitis for 10 years or more should begin annual colonoscopic surveillance with biopsies
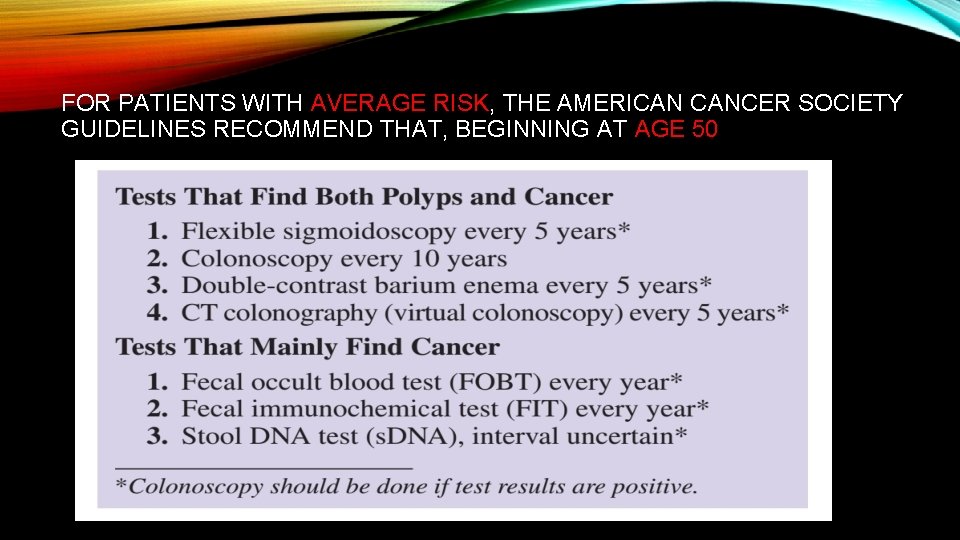
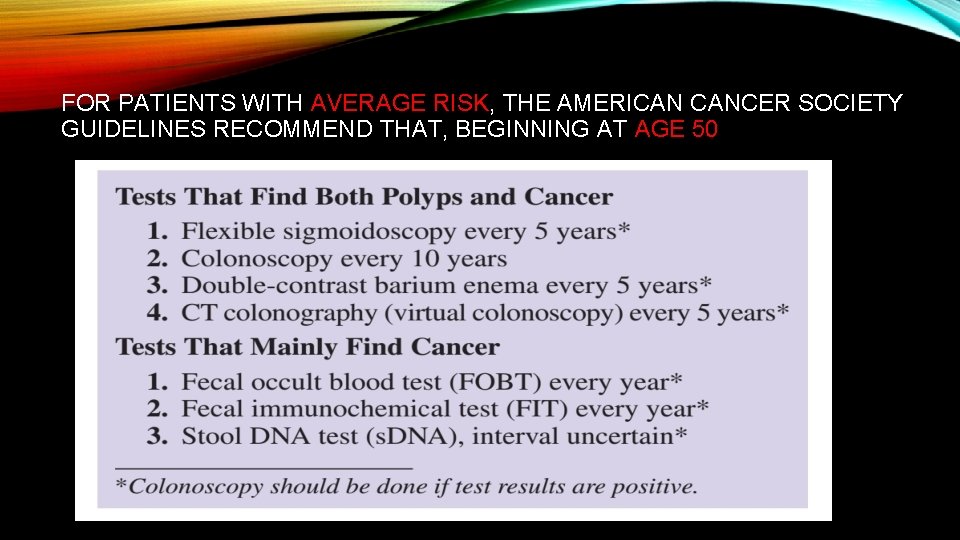
FOR PATIENTS WITH AVERAGE RISK, THE AMERICAN CANCER SOCIETY GUIDELINES RECOMMEND THAT, BEGINNING AT AGE 50
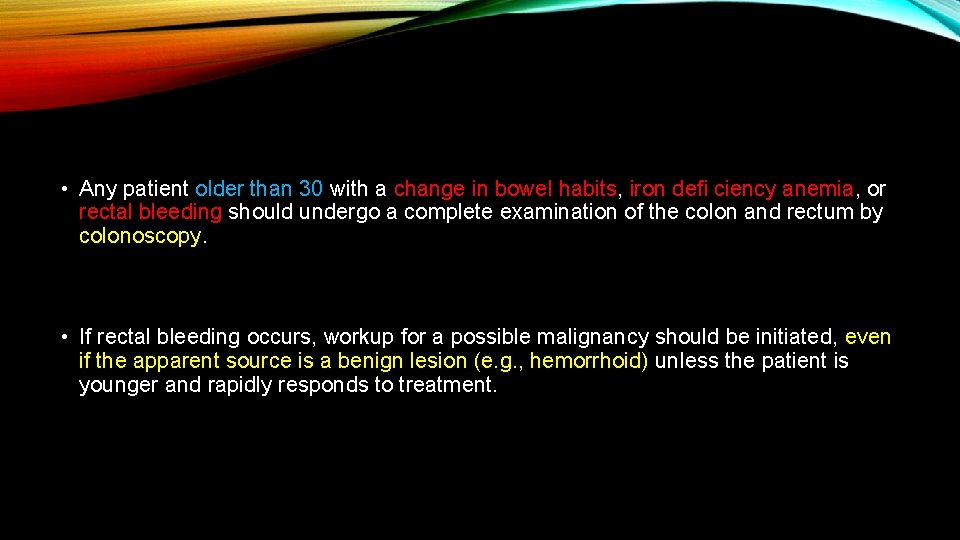
• Any patient older than 30 with a change in bowel habits, iron defi ciency anemia, or rectal bleeding should undergo a complete examination of the colon and rectum by colonoscopy. • If rectal bleeding occurs, workup for a possible malignancy should be initiated, even if the apparent source is a benign lesion (e. g. , hemorrhoid) unless the patient is younger and rapidly responds to treatment.
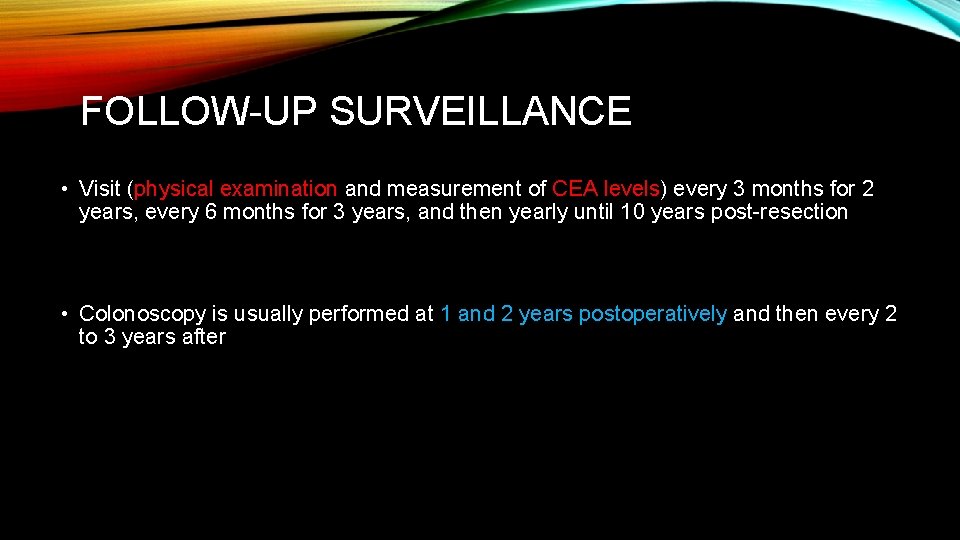
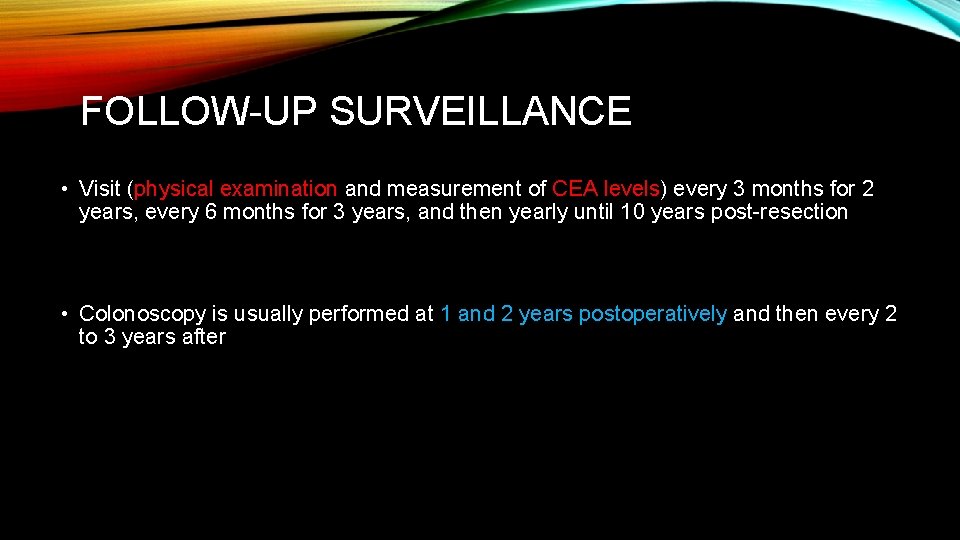
FOLLOW-UP SURVEILLANCE • Visit (physical examination and measurement of CEA levels) every 3 months for 2 years, every 6 months for 3 years, and then yearly until 10 years post-resection • Colonoscopy is usually performed at 1 and 2 years postoperatively and then every 2 to 3 years after
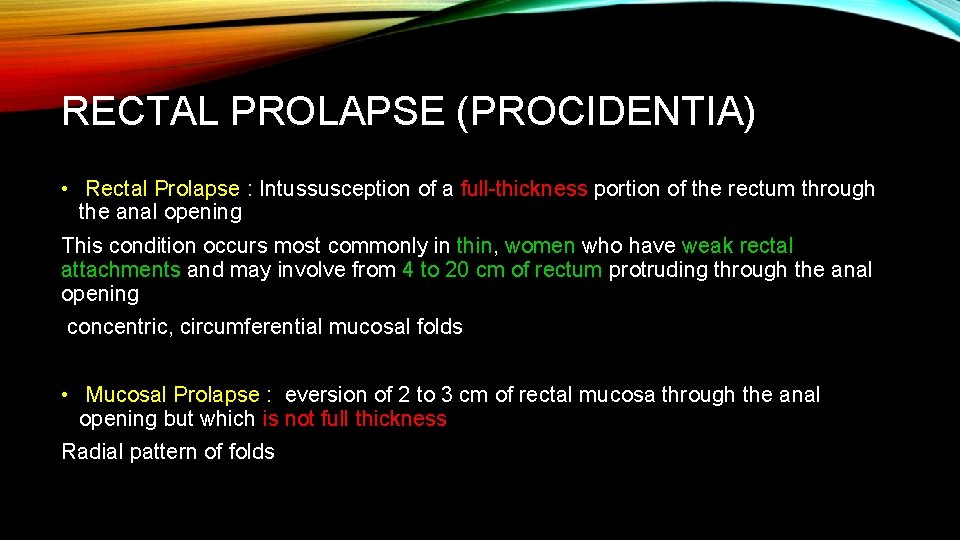
RECTAL PROLAPSE (PROCIDENTIA) • Rectal Prolapse : Intussusception of a full-thickness portion of the rectum through the anal opening This condition occurs most commonly in thin, women who have weak rectal attachments and may involve from 4 to 20 cm of rectum protruding through the anal opening concentric, circumferential mucosal folds • Mucosal Prolapse : eversion of 2 to 3 cm of rectal mucosa through the anal opening but which is not full thickness Radial pattern of folds
CLINICAL PRESENTATION AND EVALUATION • Rectal Pain or Pressure • Mild Bleeding • Incontinence • Mucous Discharge • Wet Anus • On rare occasions, the prolapse cannot be reduced and ischemia results
TREATMENT • Intra- abdominal procedure including sigmoid resection + Rectopexy ( % 5 > ) ﺍﺣﺘﻤﺎﻝ ﻋﻮﺩ • For high-risk patients : Transperineal ( )ﺍﺣﺘﻤﺎﻝ ﻋﻮﺩ ﺑیﺸﺘﺮ • Mucosal or Hemorrhoidal prolapse : Threecolumn hemorrhoidectomy.
HEMORRHOIDS • Constipation • Pregnancy • Increased Pelvic Pressure (Ascites, Tumors) • Portal Hypertension • Excessive Diarrhea • Hemorrhoids are usually found in three constant positions: left lateral, right anterior, and right posterior
• First-degree internal hemorrhoids : do not prolapse; the anoscope must be used to visualize them • Second-degree internal hemorrhoids : prolapse with defecation and return spontaneously to their anatomic position • Third-degree internal hemorrhoids : prolapse with defecation and require manual reduction • Fourthdegree hemorrhoids : are not reducible • There is no classification for external hemorrhoids; they are either present or absent
TREATMENT • Asymptomatic Hemorrhoids : are best left alone; cosmetic treatment is not indicated. Bulkforming agents (e. g. , psyllium derivatives) and avoidance of constipation are recommended • First-degree Internal Hemorrhoids : Small = Topical Agents or, if bleeding, with Injection / sclerotherapy or infrared coagulation Larger = Band Ligation • Second-degree internal hemorrhoids and some third-degree hemorrhoids : Band Ligation Formal surgical hemorrhoidectomy : is used for fourth-degree hemorrhoids, for mixed thirddegree hemorrhoids with a large external component, and in some emergency situations (e. g. , an acute hemorrhoidal attack with gangrene, severe ulceration)
• Thrombosed External Hemorrhoid : If the patient is seen early in the course of the disease (the first 24 to 48 hours), or if it is ulcerated treatment consists of excision of the thrombosed hemorrhoid under local anesthesia If the patient is seen later in the course of the disease, spontaneous resolution is usually underway and conservative treatment is indicated
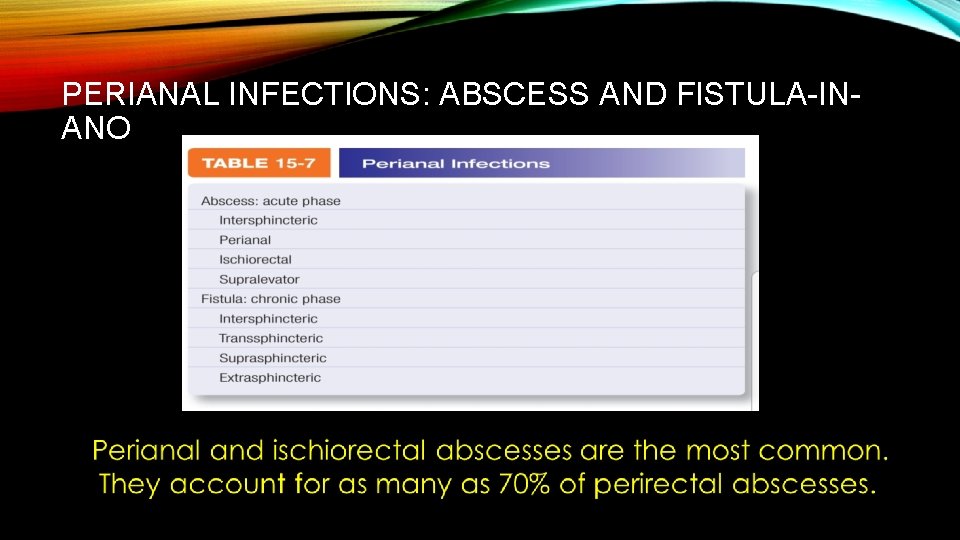
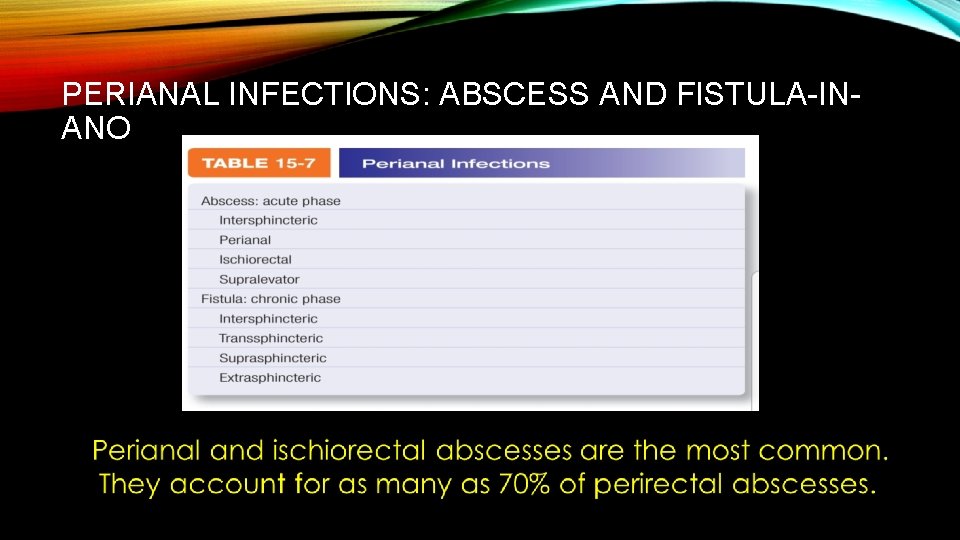
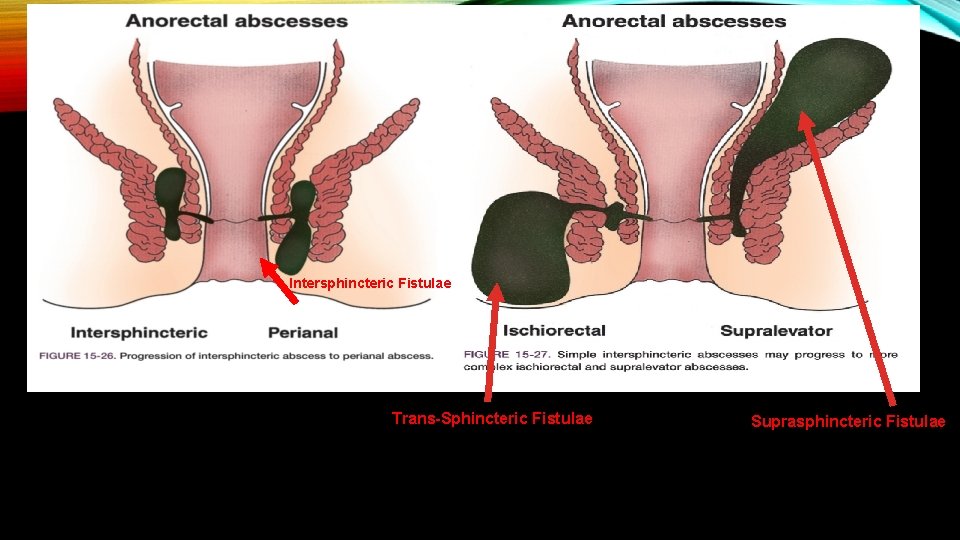
PERIANAL INFECTIONS: ABSCESS AND FISTULA-INANO
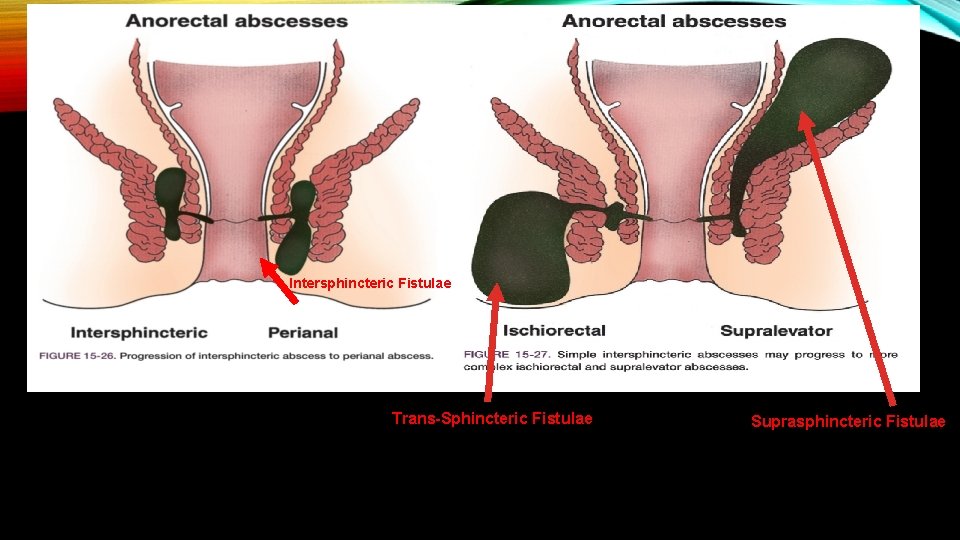
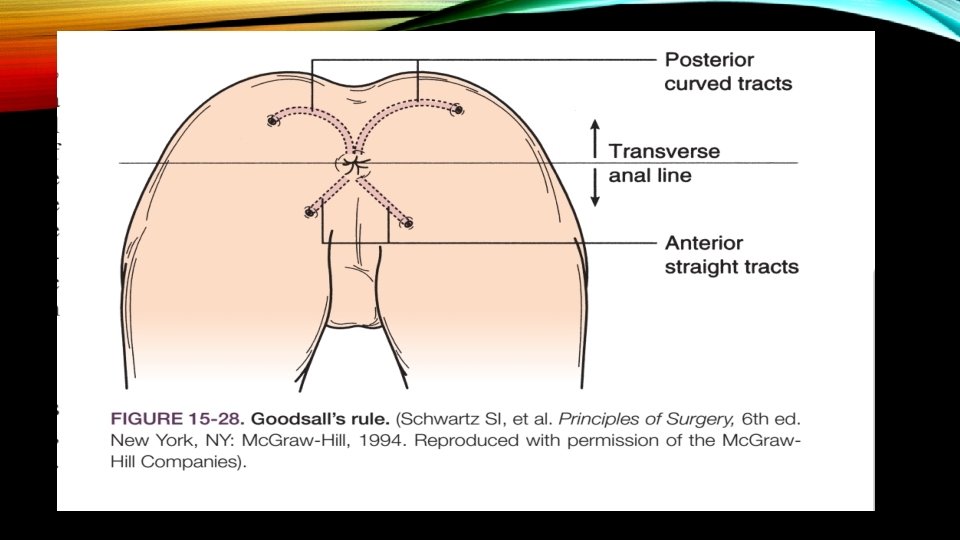
Intersphincteric Fistulae Trans-Sphincteric Fistulae Suprasphincteric Fistulae
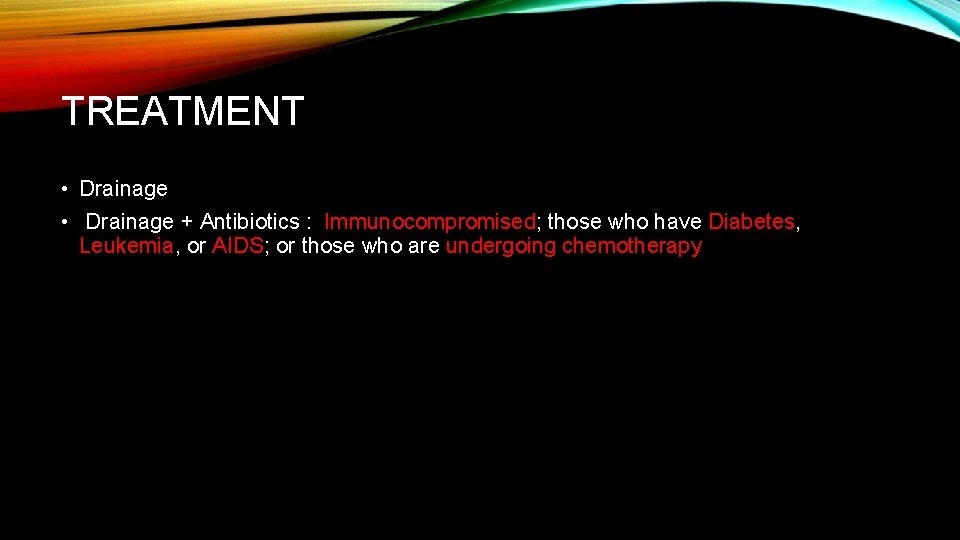
TREATMENT • Drainage + Antibiotics : Immunocompromised; those who have Diabetes, Leukemia, or AIDS; or those who are undergoing chemotherapy
TREATMENT • Fistulotomy / Fistulectomy • Seton Insertion • Fibrin Glue • Decellularized Collagen Plug
ANAL FISSURES • Ectopic lateral fi ssures suggest an unusual diagnosis (e. g. , Crohn’s disease, leukemia, sexually transmitted disease, malignancy). • Treatment : avoidance of diarrhea or constipation / bulk laxatives / mild nonnarcotic analgesic / Sitz baths / Topical agents (procainamide, nitroglycerin) / Botox injection / surgery )ﺩﺭ ( ﺻﻮﺭﺕ ﻋﺪﻡ پﺎﺳﺦ ﺑﻪ ﻣﻮﺍﺭﺩ ﻓﻮﻕ
ANAL MALIGNANCY 1. Epidermoid Carcinoma (squamous cell, basaloid, cloacogenic, mucoepidermoid, and transitional carcinomas) = Chemotherapy + Radiation ﺍگﺮ ﺗﻮﻣﻮﺭ ﺑﺎﻗی ﻣﺎﻧﺪ ﺟﺮﺍﺣی 2. Malignant Melanoma = APR