CARCINOMA OF RECTUM Carcinoma Rectum Colorectal ca 3




- Slides: 19
CARCINOMA OF RECTUM
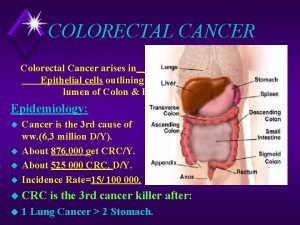
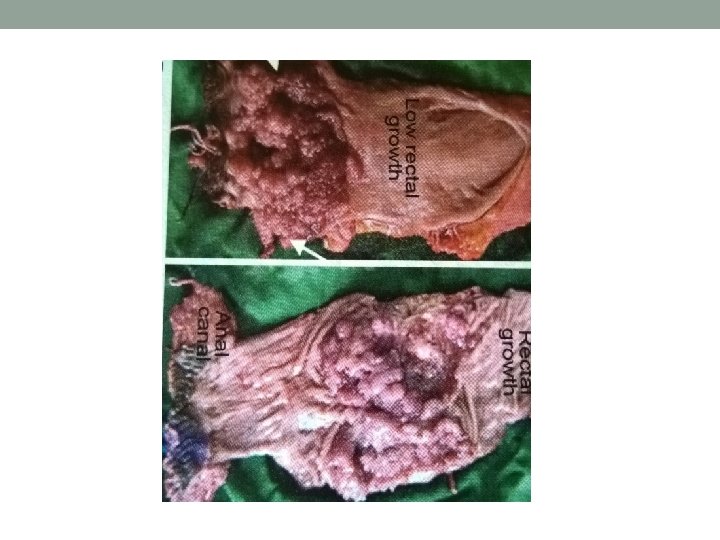
Carcinoma Rectum • Colorectal ca 3 rd commonest in men and 4 th commonest among women • Pathology- normal epi> adenoma with mild dysplasia> intermediate> severe> ca in situ> invasive ca • Well, moderately, poorly differentiated or anaplastic ca • Ulcerative/ proliferative • Columnar cell, colloid ca
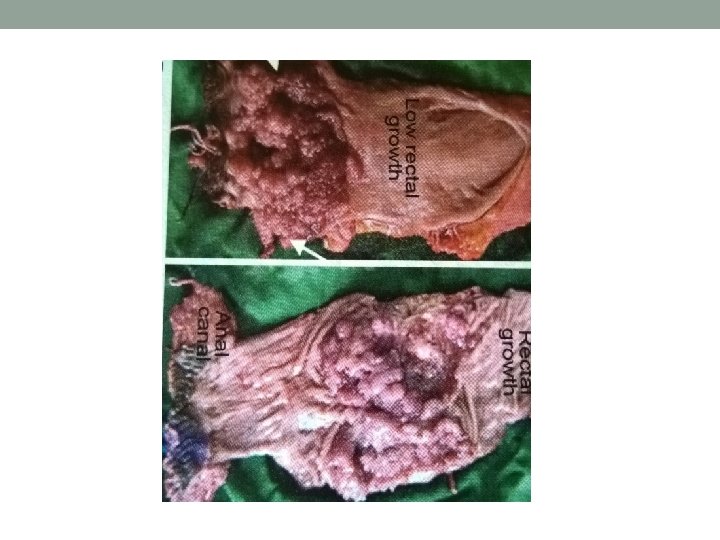
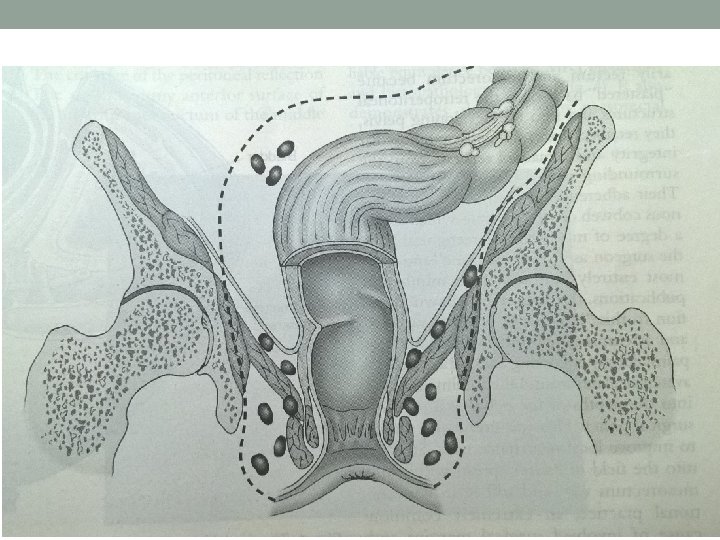
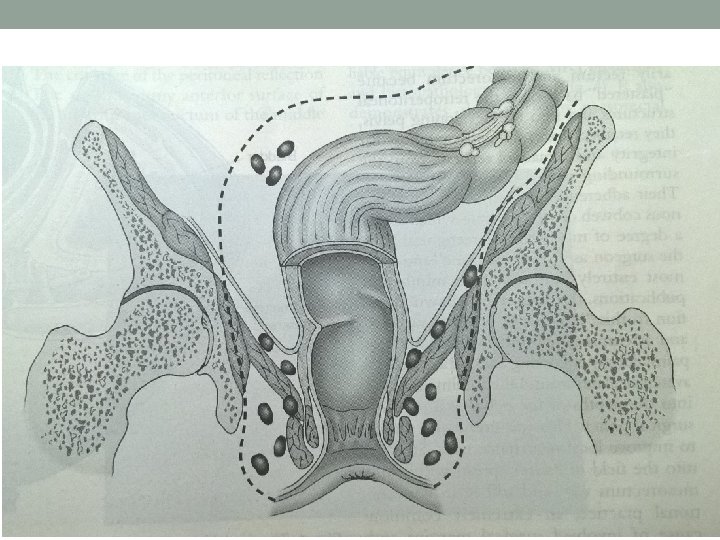
Spread • Local- circumferential: 6 months for ¼ circumference. Deeper: mesorectum, ureters, prostate, seminal vesicles, bladder, vagina, uterus, sacrum, sacral plexus • lymphatic- upto 1 -2 cm from anal verge, upwards to pararectal LN of Gerota. Atypical- widespread lymphatic permeation in Anaplastic ca
• Venous- late. Liver, lung, adrenals, brain • Peritoneal- upper rectal growth
• Normal colonic mucosa>dysplastic aberrant crypt foci>early adenoma>intermediate adenoma>late adenoma>ca in situ>invasive ca • Tumour suppressor genes- APC gene, p 53 gene, STK 11 gene. • Mismatch Repair Gene, microsatellite instability. • Oncogenes- k ras.
Etiology • Diet- red meat, saturated fatty acid. • Alcohol and smoking • FAP, HNPCC, Adenoma. • Ulcerative colitis, Crohn’s disease. • Family history of rectal carcinoma.
Staging • Dukes: A- tumour confined to bowel wall B- spread beyond serosa to adjacent structures, no nodes C- Lymph nodes involved • TNM: Tx- primary cannot be assessed, T 0 - no evidence of primary, T 1 - tumour invades upto submucosa, T 2 - tumour upto muscularis propria, T 3 - invades upto subserosa or upto pericolic or pararectal tissue at unperitonealised area, T 4 invasion of adjacent organ or perforation

• N 0 - no regional nodes, N 1 - 1 to 3 nodes, N 2 - metastasis to 4 or more regional nodes • M 0 , M 1

Clinical Features • Usually > 55 years, rarely in younger- FAP • Bleeding – fresh • Tenesmus, spurious diarrhoea, bloody slime • Altered bowel habits, weight loss • Pain- colicky, due to obstruction, continuous due to deeper invasion • Intestinal obstruction, palpable liver, ascites • Rectal digital examination- 90% palpable
Investigations • Sigmoidoscopy, colonoscopy • Biopsy • Ba enema • USG, TRUS • CT abdomen • MRI

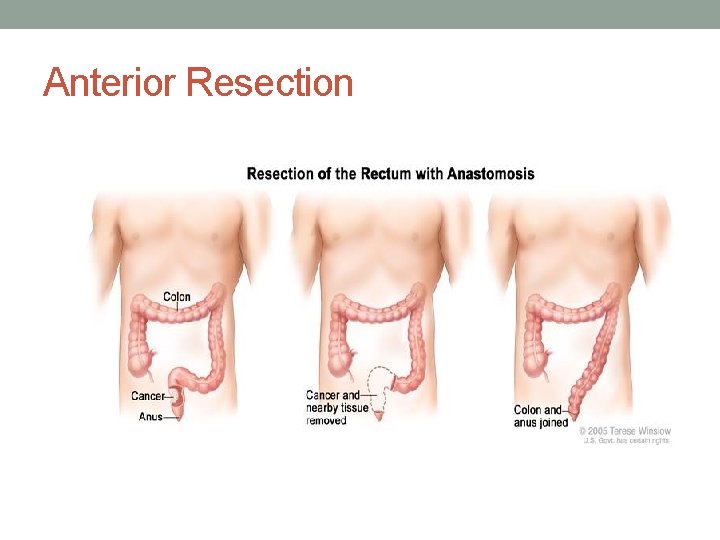
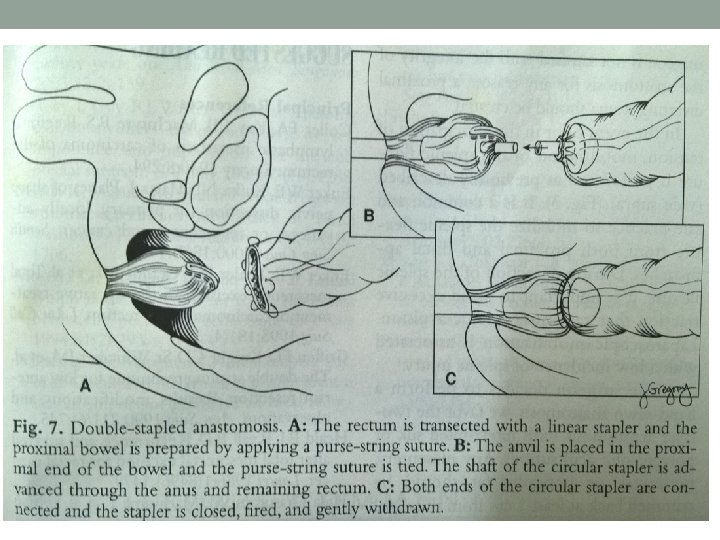
Treatment- Surgical • Principle- radical excision of rectum with mesorectum, involved LN(TME), localised liver metastasis if any. If advanced- palliative resection/ colostomy • Surgeries- Anterior resection, Abdominoperitoneal resection with colostomy, Transanal resection, Colostomy. • Open or laparoscopic approach, robotic surgery
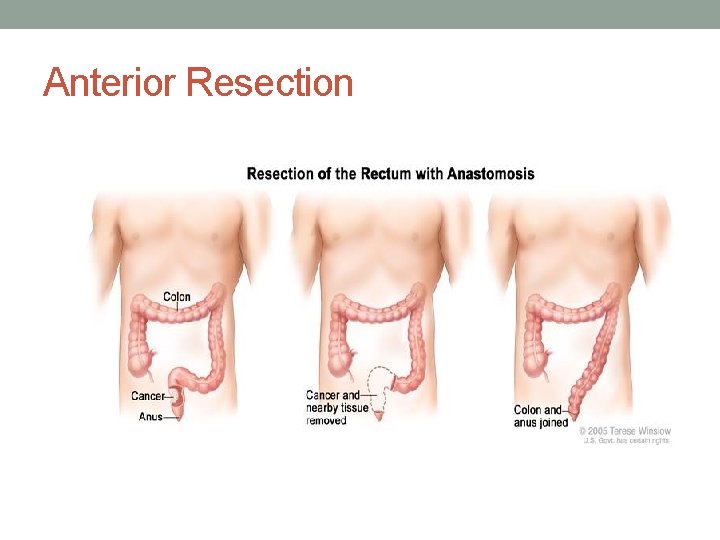
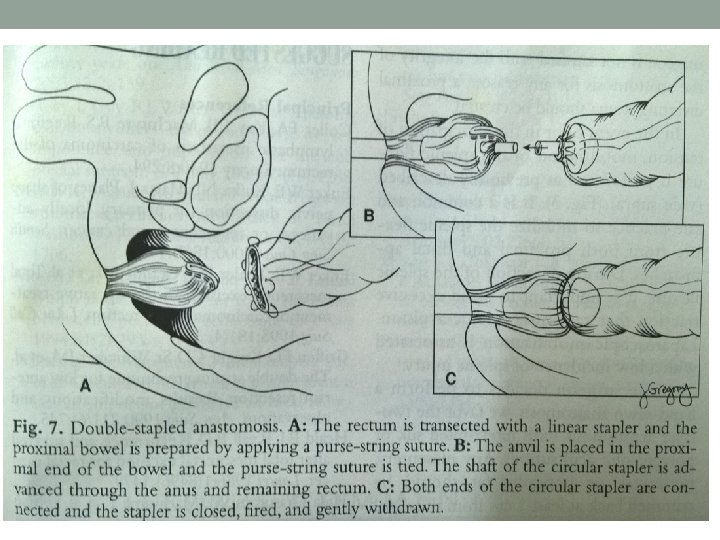
Anterior Resection

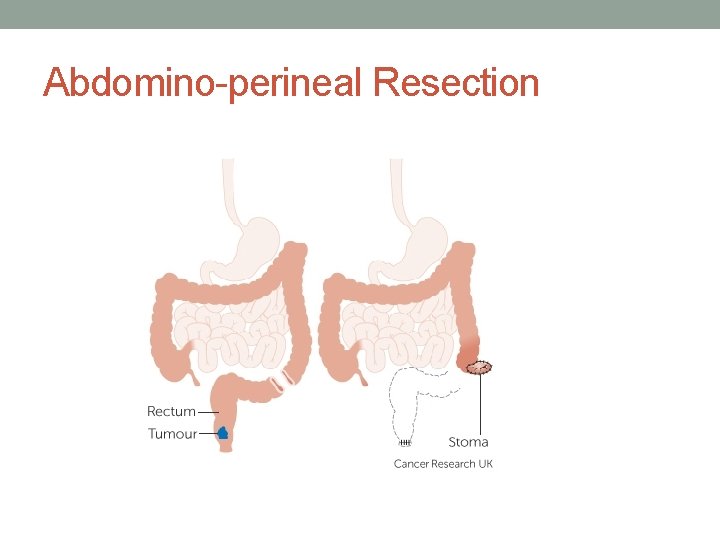
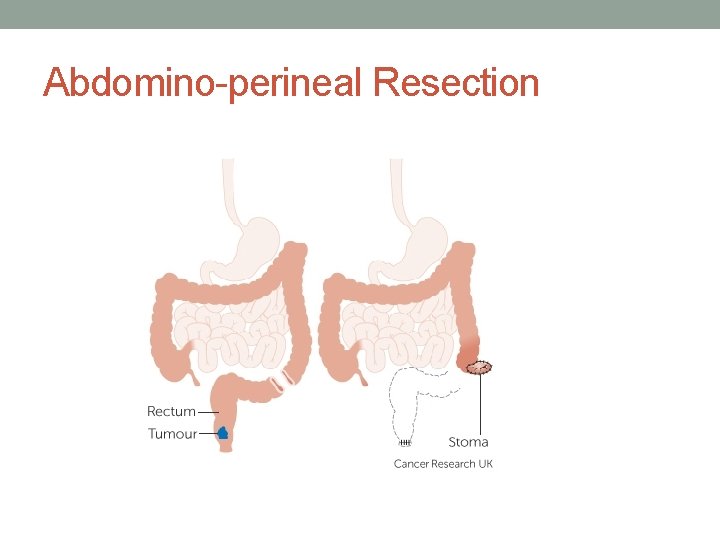
Abdomino-perineal Resection
• Radiotherapy- Pre op if locally advanced. Post op. Palliative if inoperable/ painful local recurrence • Chemotherapy-Folinic acid, 5 FU, Oxaliplatin(FOLFOX) or Folinic acid, 5 FU, Irinotecan(FOLFIRI). Capecitabine • Monoclonal antibodies- Bevacizumab, cetuximab.
 Patho
Patho Colorectal cancer drug trial
Colorectal cancer drug trial Amsterdam criteria
Amsterdam criteria Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Colorectal cancer
Colorectal cancer Latus rectum
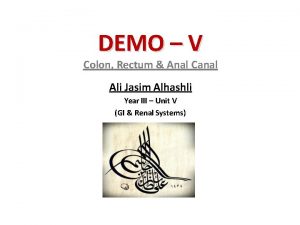
Latus rectum Rectum extraperitoneal
Rectum extraperitoneal Male rectum anatomy
Male rectum anatomy Proctitis adalah
Proctitis adalah Sims position
Sims position Sobia anal
Sobia anal What is encopresis
What is encopresis What is latus rectum
What is latus rectum Colon and rectum
Colon and rectum Cone-shaped projection hanging down from soft palate
Cone-shaped projection hanging down from soft palate Distensie
Distensie Squid order
Squid order Wikipedia commons
Wikipedia commons Breast papillary carcinoma
Breast papillary carcinoma Malignant neoplasm
Malignant neoplasm