Neoadjuvant therapy for Rectal cancer Rectal cancer Improvements

- Slides: 25

Neoadjuvant therapy for Rectal cancer
Rectal cancer • Improvements in management of rectal cancer in past decades • Preoperative accurate tumor staging • Good surgical technique (TME) • Neoadjuvant / adjuvant therapy • Improved pathological assessment identifying adequacy of resection
Preoperative Tumor Staging • All decisions on requirement for neoadjuvant • • • therapy are predicted on accurate tumor staging Local tumor staging of extent of tumor invasion (T) and nodal involvement (N) is important Clinical examination and contrast CT provides an estimate EUS & MRI are used for more accurate local tumor staging
EUS • Especially useful in assessment of early non-invasive T 1 • • disease Help to determine whether local excision is possible Disadvantages: – – Operator dependent Limited ability to assess stenotic / bulky tumors Cannot evaluate iliac, mesenteric or retroperitoneal LNs Cannot identify mesorectal fascia prediction of CRM not possible – Other prognostic factors cannot be assessed
MRI • High resolution MRI with rectal coil • Plane of mesorectal fascia can be seen on MRI which allows predicton of likelihood of a positive or close circumferential resection margin (CRM) • Other prognostic features including extramural venous invasion, nodal status and peritoneal infiltration
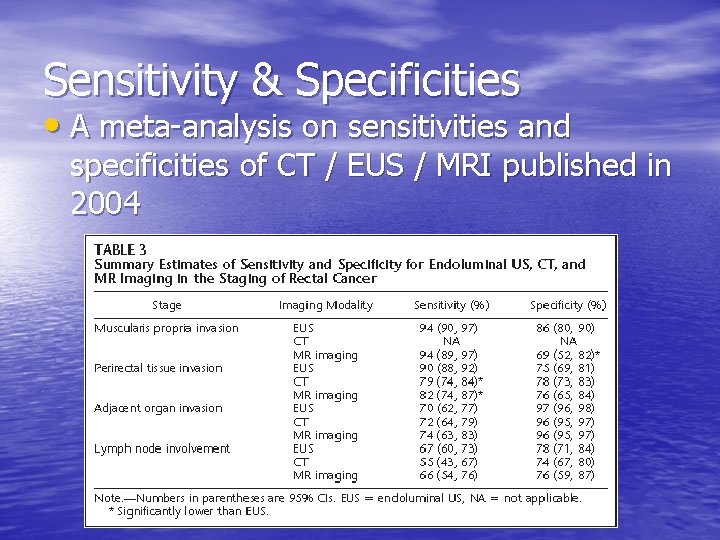
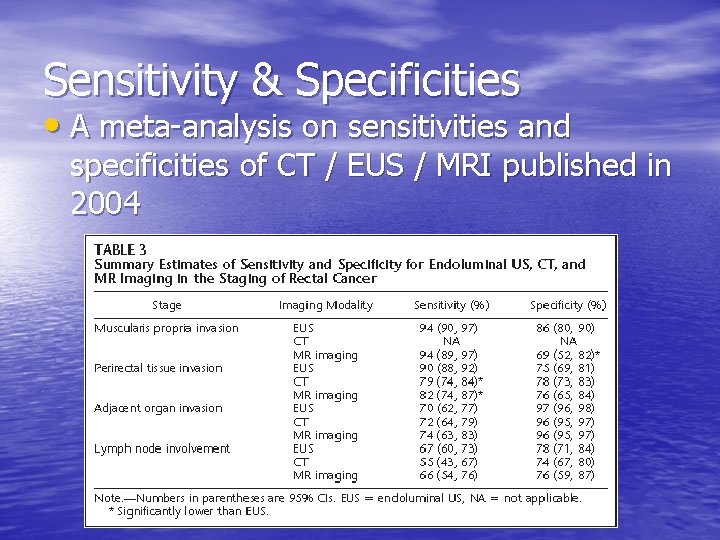
Sensitivity & Specificities • A meta-analysis on sensitivities and specificities of CT / EUS / MRI published in 2004
MRI prediction of CRM • A prospective observational study conducted by the • • • MERCURY Study Group published in 2006 tried to assess accuracy of MRI in predicting curative resection (clear CRM) Collected patients from 12 colorectal units in 4 European countries Using MRI with rectal coil and high resolution protocol Workshops to ensure standardization of scan techniques, image interpretation and reporting 92% specificity for a clear CRM (CI, 90 -95%) Reproducible in multicenter setting
Adjuvant therapy: preop or postop? • Decades ago, standard management of locally • • advanced rectal cancer was surgery with adjuvant radiotherapy -In 1990, NIH recommended that postop chemoradiotherapy as standard for patients with locally advanced rectal cancer (stage II or III) However complications of RT were dose limiting, treatment-related complications and treatment tolerance were factors leading to trials comparing pre-op and post-op therapies
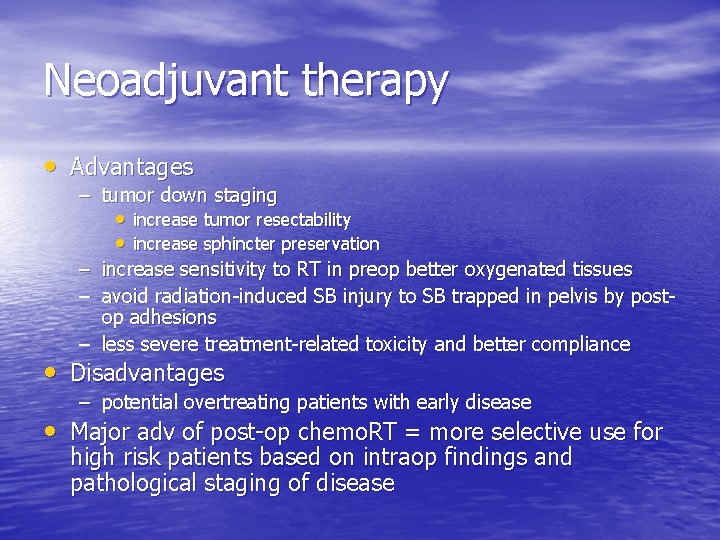
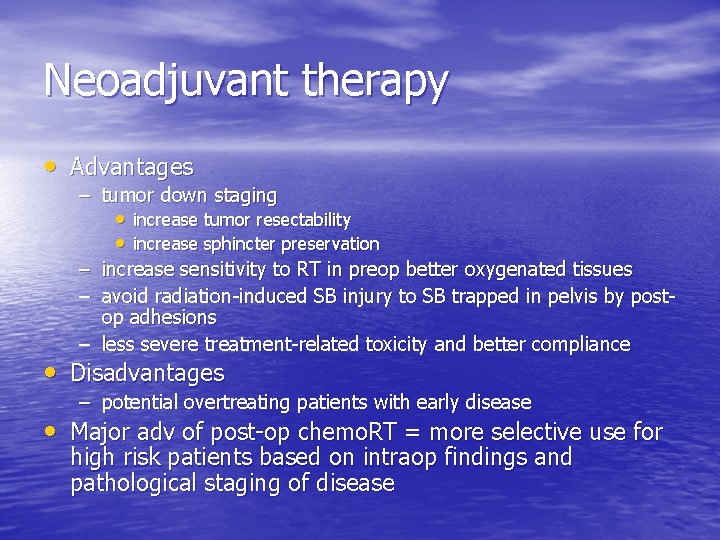
Neoadjuvant therapy • Advantages – tumor down staging • increase tumor resectability • increase sphincter preservation – increase sensitivity to RT in preop better oxygenated tissues – avoid radiation-induced SB injury to SB trapped in pelvis by postop adhesions – less severe treatment-related toxicity and better compliance • Disadvantages – potential overtreating patients with early disease • Major adv of post-op chemo. RT = more selective use for high risk patients based on intraop findings and pathological staging of disease
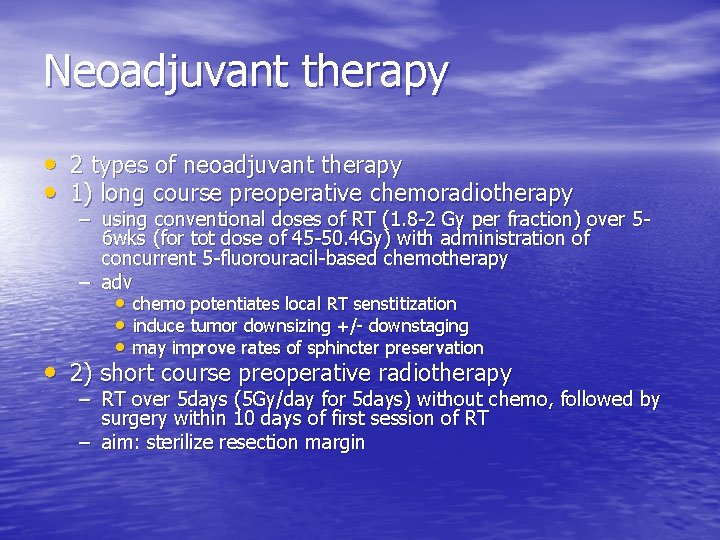
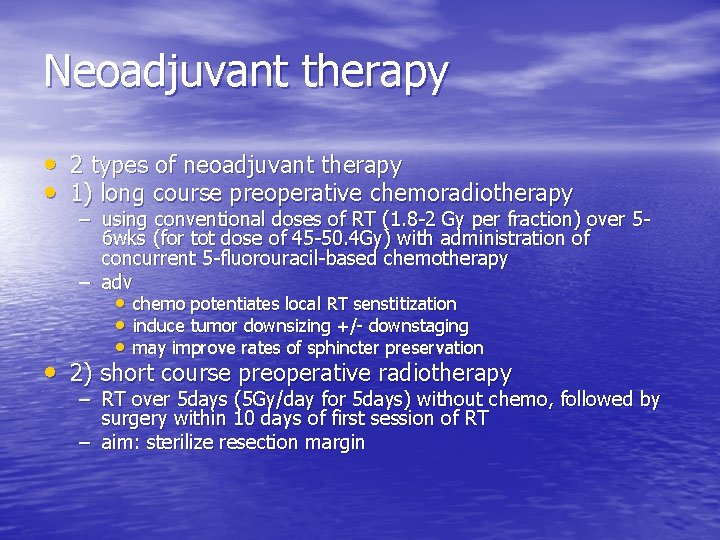
Neoadjuvant therapy • 2 types of neoadjuvant therapy • 1) long course preoperative chemoradiotherapy – using conventional doses of RT (1. 8 -2 Gy per fraction) over 56 wks (for tot dose of 45 -50. 4 Gy) with administration of concurrent 5 -fluorouracil-based chemotherapy – adv • chemo potentiates local RT senstitization • induce tumor downsizing +/- downstaging • may improve rates of sphincter preservation • 2) short course preoperative radiotherapy – RT over 5 days (5 Gy/day for 5 days) without chemo, followed by surgery within 10 days of first session of RT – aim: sterilize resection margin
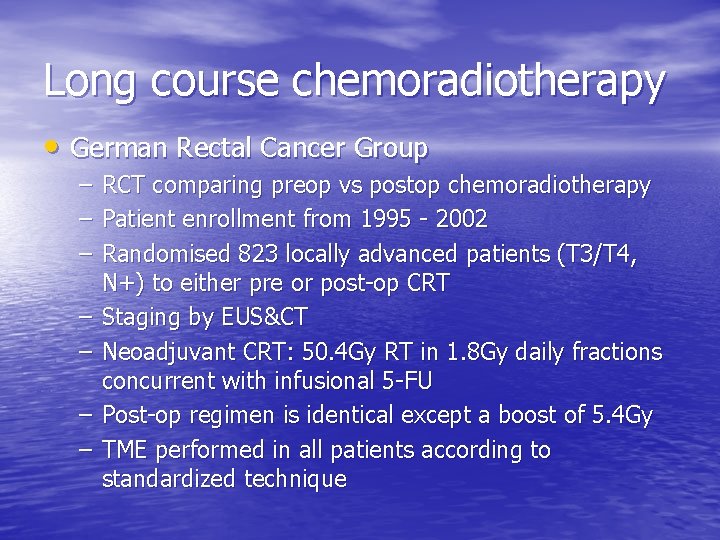
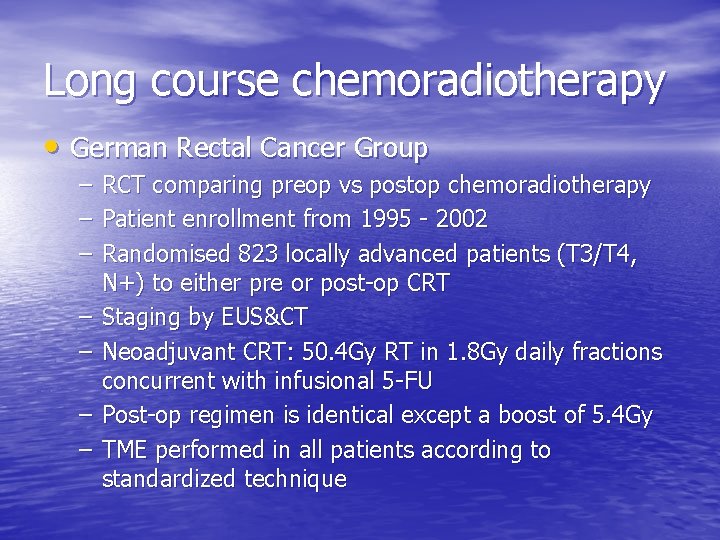
Long course chemoradiotherapy • German Rectal Cancer Group – – – – RCT comparing preop vs postop chemoradiotherapy Patient enrollment from 1995 - 2002 Randomised 823 locally advanced patients (T 3/T 4, N+) to either pre or post-op CRT Staging by EUS&CT Neoadjuvant CRT: 50. 4 Gy RT in 1. 8 Gy daily fractions concurrent with infusional 5 -FU Post-op regimen is identical except a boost of 5. 4 Gy TME performed in all patients according to standardized technique
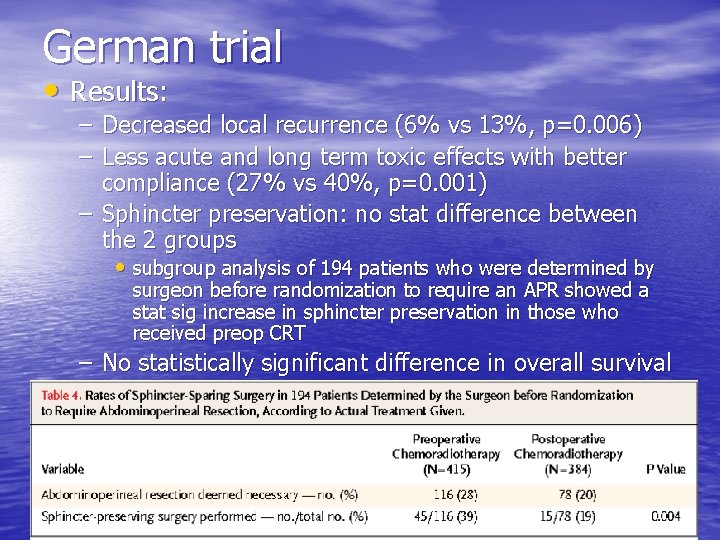
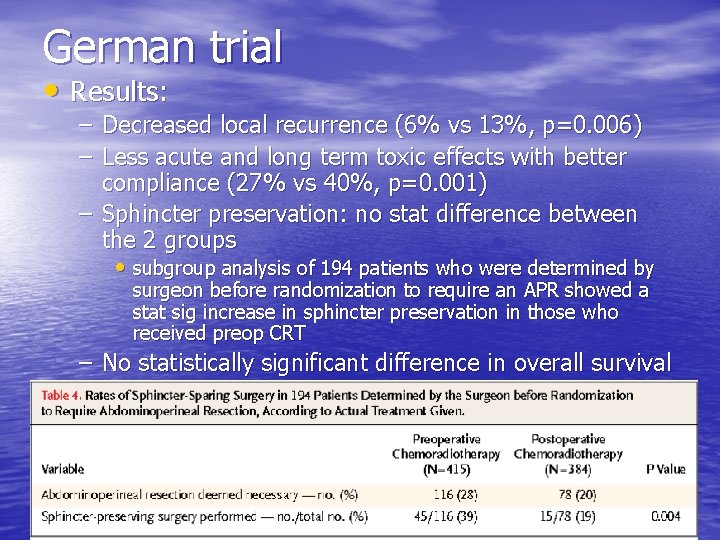
German trial • Results: – Decreased local recurrence (6% vs 13%, p=0. 006) – Less acute and long term toxic effects with better compliance (27% vs 40%, p=0. 001) – Sphincter preservation: no stat difference between the 2 groups • subgroup analysis of 194 patients who were determined by surgeon before randomization to require an APR showed a stat sig increase in sphincter preservation in those who received preop CRT – No statistically significant difference in overall survival
Short course preop radiotherapy • Several trials studied the effect of SCPRT vs surgery • alone but many of them are in the pre-TME era Swedish Rectal Cancer Trial – randomized 1168 patients in 1987 -1990 to either SCPRT then surgery or surgery alone – significant reduction in local recurrence (11% vs 27%, P<0. 001) and increase in 5 -yr survival (58% vs 48%, P=0. 002) – the only trial that showed improvement in survival – a follow up study at a median 13 yrs showed the local control and survival remained durable – the difference in local recurrence may account for the improved survival
Dutch Colorectal Cancer Group Trial • First study to investigate benefit of preop RT in • • • combination with TME Randomized 1861 patients in 1996 -1999 with resectable rectal cancer to receive SCPRT or no SCPRT before standardized TME surgery Adjuvant therapy was only given to patients with intraoperative tumor spillage or positive margins at pathology Results: – preop RT further reduce local recurrence rate (2. 4% vs 8. 2% at 2 yrs)
Dutch TME trial: 12 yrs follow up • 12 yr follow up of Dutch TME trial – SCPRT decreases local recurrence rate compared to surgery alone (at 10 yrs, 5% vs 11%, p<0. 0001) – no effect on overall 10 -year survival (48% vs 49%, P=0. 86) – subgroup analysis: • 10 -yr survival was significantly improved in TNM stage III patients with negative CRM in the SCPRT + surgery group compared to surgery alone (5% vs 17%, P<0. 0001)
Medical Research Council CR 07 trial • Compare SCPRT vs surgery with selective postop • • chemoradiotherapy Multicentre RCT, recruited 1350 patients between 1998 to 2005 Randomized patients with resectable rectal cancer, assessed clinically or imaging (CT/MRI/EUS) to – either SCPRT – or initial surgery with selective postop chemoradiotherapy (CRM positive) • Primary outcome measure was local recurence • Results: – Absolute difference in 3 -yr local recurrence rate 6. 2% – Overall survival did not differ between the groups – Quality of surgery also examined, local recurrence rates 4% (good) vs 13% (poor) (P=0. 0039), 1% local recurrence rate at 3 yrs for those with SCPRT & achieved good mesorectal plane
Long course vs short course • Long-course chemoradiotherapy is therapy of choice for patients requiring preop downsizing / downstaging but its use is debatable for other patients • Few studies have directly compared the two
Polish Colorectal Study Group • Small RCT of 312 patients published in 2006 • Patients with T 3/4 rectal cancer, staged by clinically or • • EUS/MRT/CT All received TME surgery Results: – no sig diff in sphincter preservation rate (61. 2% vs 58% in CRT group, P=0. 57) – more acute toxicity in preop CRT than SCPRT gp (18. 2% vs 3. 2%, P<0. 001) – more positive CRM in SCPRT group (12. 9% vs 4. 4%, P=0. 017) – no difference in local recurrence (9% vs 14. 2% in CRT, P=0. 170) and overall 4 -yr survival rates (67. 2% vs 66. 2% in CRT, P=0. 820)
Australian / New Zealand trial • RCT of 326 patients published in 2010 • Recruited patients with T 3 Nany rectal cancer, • • staged by EUS / MRI All patients received post-op adjuvant chemotherapy Results: – no difference in 3 -yr local recurrence (7. 5% vs 4. 4% in CRT, P=0. 24) and 5 -yr overall survival rates (74% vs 70% in CRT, P=0. 56)
Adjuvant therapy after neoadjuvant • Since the introduction of neoadjuvant therapy, it had led to questions on need of further adjuvant tx • Support for use of adjuvant chemo came from extrapolation from colon cancer clinical trials suggest that approximately 6 months of FOLFOX is the optimal current strategy to improve survival
EORTC trial • Explored the impact of timing of chemo (preop / postop / both) on • • • outcome It is a four-arm RCT that randomised 1011 patients in 1993 -2003 with T 3/T 4 rectal cancer to receive preop RT +/- concurrent Chemo, followed by surgery with or without postop chemotherapy Staging of tumor by clinical, rigid proctoscopy and CT (EUS optional) Results: – significant decrease in local recurrence among patients who received chemotherapy (preop 8. 7%, postop 9. 6%, both 7. 6%) than RT alone (17. 1%) – no sig diff in survival between the groups that received chemo preop and those that received it postop – subgroup analysis revealed patients who responded to preop CRT (tumor downstaging to yp. T 0 -2) had a survival benefit from postop chemotherapy (5 yr disease free survival 76. 7% vs 65. 6%, P=0. 13)
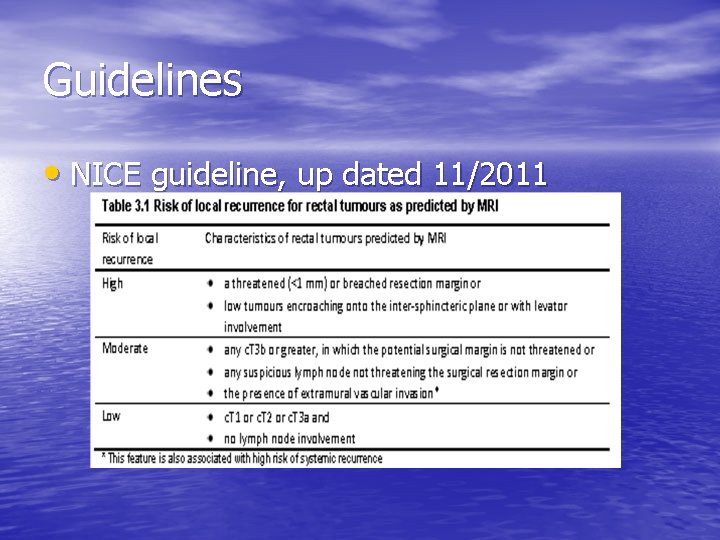
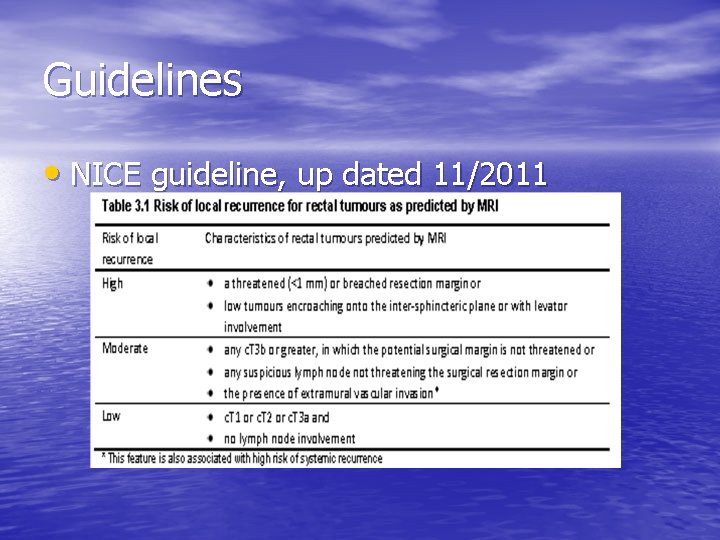
Guidelines • NICE guideline, up dated 11/2011
NCCN guideline • For T 3, N 0 or T any N 1 -2 lesions – should be treated by preop CRT unless medically contraindictated • Then undergo resection 5 -10 wks after completion of neoadjuvant therapy • Post-op adjuvant chemotherapy for 6 mo in total of pre & post op chemotherapy • No recommendation on SCPRT
Conclusion • Preop accurate staging in mandatory for • • • decisions for neoadjuvant therapy Increase widespread use of MRI for pre-op staging Neoadjuvant therapy will reduce local recurrence even in patients who undergo optimal surgery Preop CRT remains the standard for locally advanced rectal cancers that has to be downsized / downstaged before surgery
Questions
 Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Aktiv expektans
Aktiv expektans Proton therapy for breast cancer after mastectomy
Proton therapy for breast cancer after mastectomy Wireless oss
Wireless oss What improvements have been made to kevlar
What improvements have been made to kevlar Direct improvements
Direct improvements Svcfin com payment
Svcfin com payment Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Offsite improvements
Offsite improvements Tenant improvement and betterments
Tenant improvement and betterments Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Rectal temperature range
Rectal temperature range Posicion tacto rectal
Posicion tacto rectal Normolíneo
Normolíneo Syndrome rectal de bensaude
Syndrome rectal de bensaude Pararectal
Pararectal Rectal rocket compound
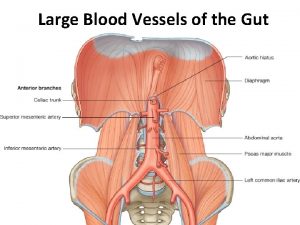
Rectal rocket compound Superior rectal artery is a branch of
Superior rectal artery is a branch of Colon rectal
Colon rectal Proctalgia fugax
Proctalgia fugax Valores normales de la temperatura oral axilar y rectal
Valores normales de la temperatura oral axilar y rectal Zonas de puncion
Zonas de puncion Flatus tube pdf
Flatus tube pdf Rubefacient mechanism of action
Rubefacient mechanism of action