Ascites The Aim Is To Approach The Patient





- Slides: 38
Ascites The Aim Is To Approach The Patient With Ascites In Terms Of : DEFINITION ; CAUSES ; CLINICAL FEATURES ; INVESTIGATIONS ; MANAGEMENT ; COMPLICATIONS ; MCQs.
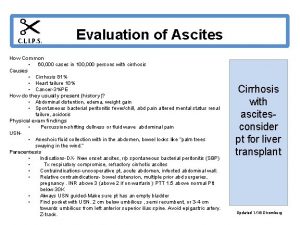
ASCITES IT IS THE CONDITION OF PATHOLOGICAL ACCUMULATION OF FLUID IN ABDOMINAL CAVITY
CAUSES Can Be Broadly Classified On The Basis Of : Normal peritoneum Diseased peritoneum
CAUSES NORMAL PERITONEUM Portal hypertension Congestive Heart Failure Constrictive Pericarditis Tricuspid Insufficiency Budd-Chiari Syndrome Liver Cirrhosis Alcoholic Hepatitis Fulminant Hepatic Failure Massive Hepatic Metastases
CAUSES NORMAL PERITONEUM Hypoalbuminemia Nephrotic Syndrome Protein-losing Enteropathy Severe Malnutrition with Anasarca
CAUSES NORMAL PERITONEUM Miscellaneous conditions Chylous ascites Pancreatic ascites Nephrogenic ascites Meig’s syndrome
CAUSES DISEASED PERITONEUM Infections Tuberculous Peritonitis Bacterial Peritonitis Fungal Peritonitis HIV associated peritonitis
CAUSES DISEASED PERITONEUM Malignant conditions Peritoneum Carcinomatosis Hepatocellula Carcinoma Primary Mesothelioma Pseudomyxoma Peritonei
CAUSES DISEASED PERITONEUM Other rare conditions Granulomatous Peritonitis Vasculitis
CLINICAL FEATURES PRESENTING COMPLAINTS Abdominal Distension Diffuse Abdominal Pain Bloated Feeling of Abdomen Dyspnoea and Orthopnea (due to elevation of daipharagm) Indigestion and Heart burn (due to inc intra abdominal pressure)
CLINICAL FEATURES PHYSICAL EXAMINATION Abdominal Distension Fullness of Flanks Umbilicus Flat and Everted Diverticulation of Recti Muscles Distended Abdominal Veins Shifting dullness (esp. when >1000 ml of fluid) Fluid Thrill Puddle Sign
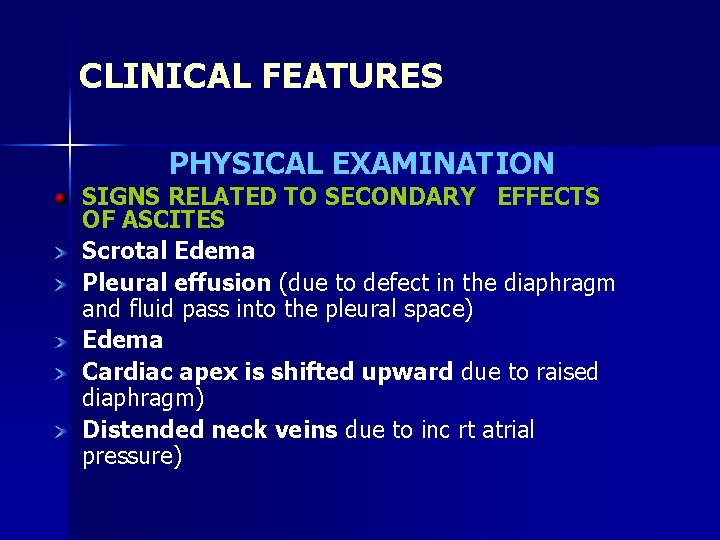
CLINICAL FEATURES PHYSICAL EXAMINATION SIGNS RELATED TO SECONDARY EFFECTS OF ASCITES Scrotal Edema Pleural effusion (due to defect in the diaphragm and fluid pass into the pleural space) Edema Cardiac apex is shifted upward due to raised diaphragm) Distended neck veins due to inc rt atrial pressure)
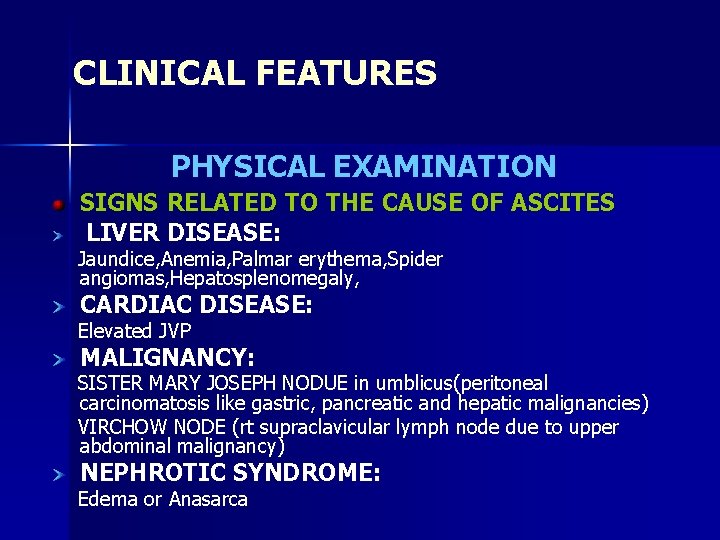
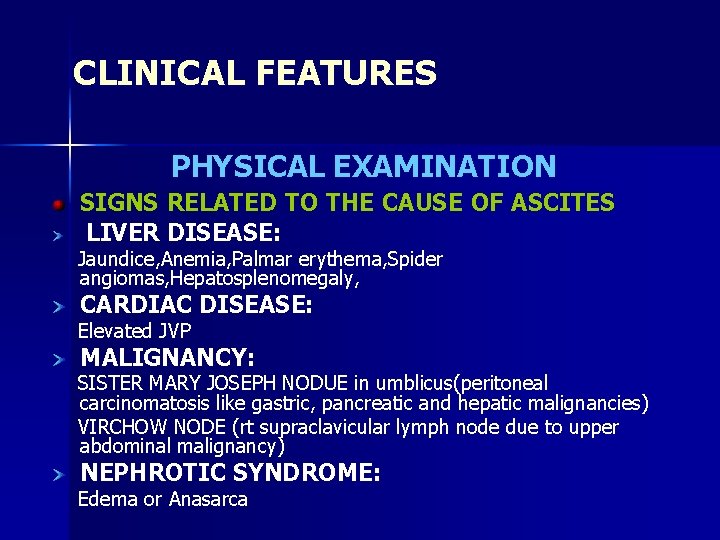
CLINICAL FEATURES PHYSICAL EXAMINATION SIGNS RELATED TO THE CAUSE OF ASCITES LIVER DISEASE: Jaundice, Anemia, Palmar erythema, Spider angiomas, Hepatosplenomegaly, CARDIAC DISEASE: Elevated JVP MALIGNANCY: SISTER MARY JOSEPH NODUE in umblicus(peritoneal carcinomatosis like gastric, pancreatic and hepatic malignancies) VIRCHOW NODE (rt supraclavicular lymph node due to upper abdominal malignancy) NEPHROTIC SYNDROME: Edema or Anasarca
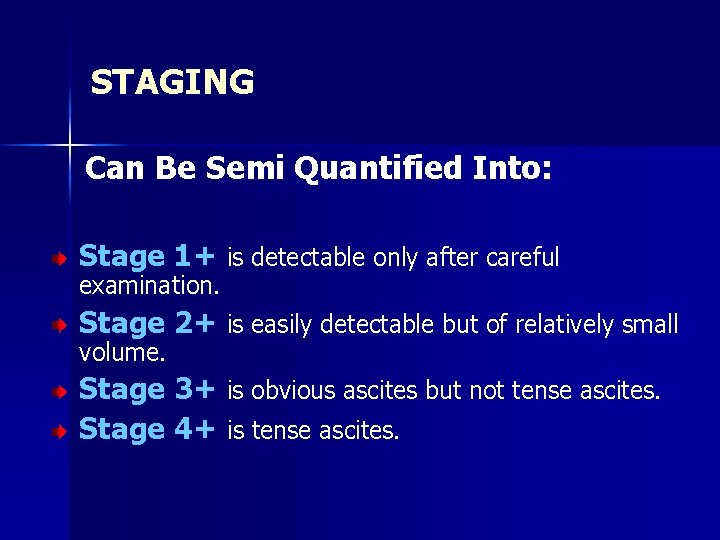
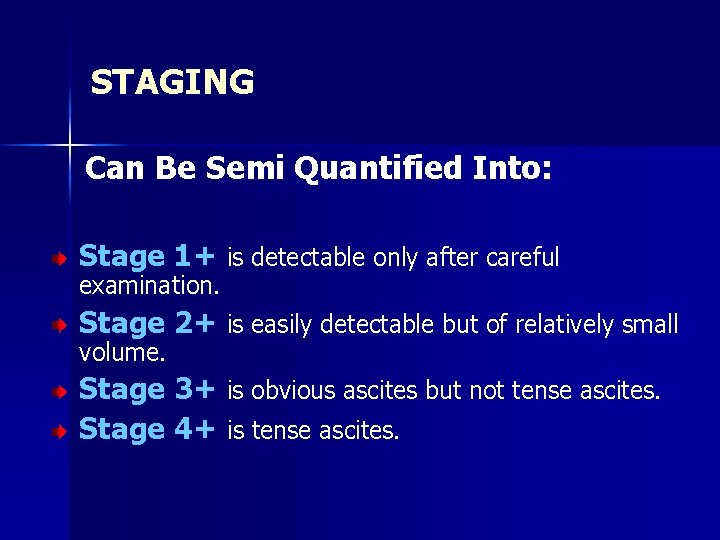
STAGING Can Be Semi Quantified Into: Stage 1+ is detectable only after careful examination. Stage 2+ is easily detectable but of relatively small volume. Stage 3+ is obvious ascites but not tense ascites. Stage 4+ is tense ascites.

INVESTIGATIONS Includes: Imaging studies Lab studies Laparoscopy
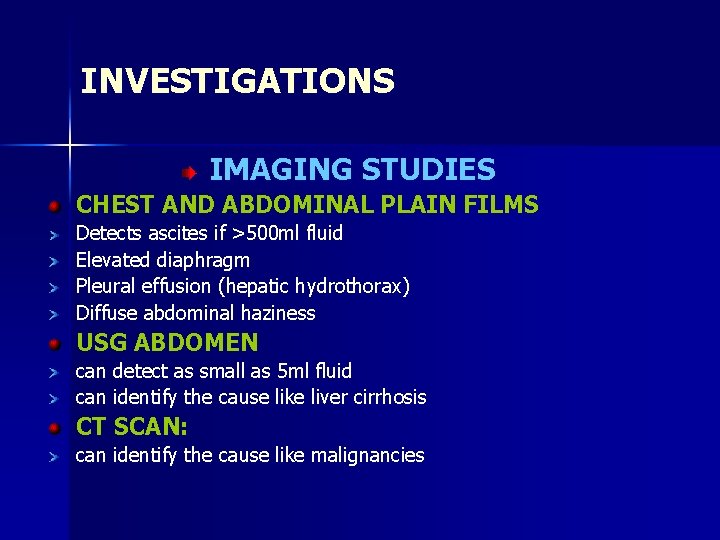
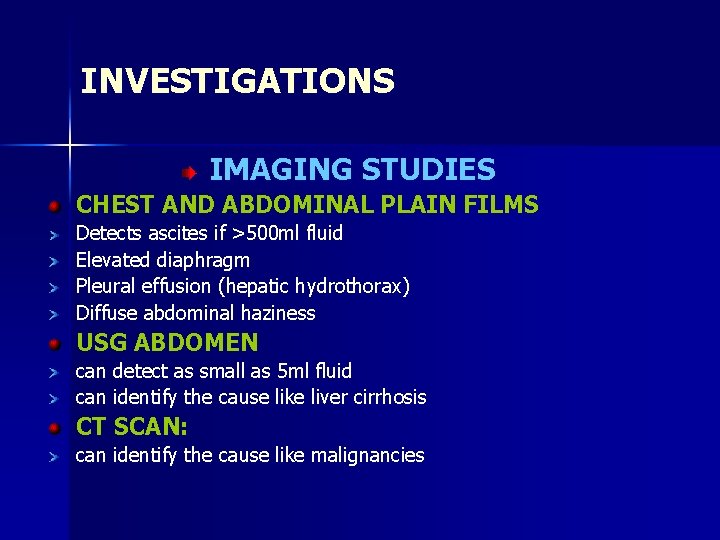
INVESTIGATIONS IMAGING STUDIES CHEST AND ABDOMINAL PLAIN FILMS Detects ascites if >500 ml fluid Elevated diaphragm Pleural effusion (hepatic hydrothorax) Diffuse abdominal haziness USG ABDOMEN can detect as small as 5 ml fluid can identify the cause like liver cirrhosis CT SCAN: can identify the cause like malignancies
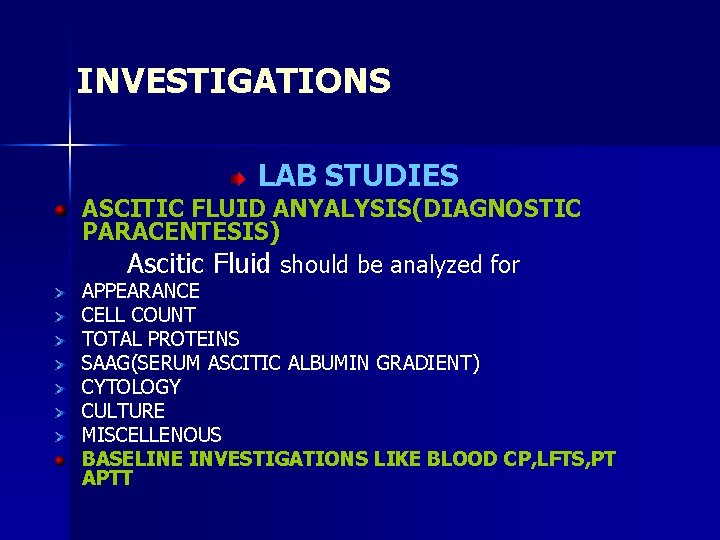
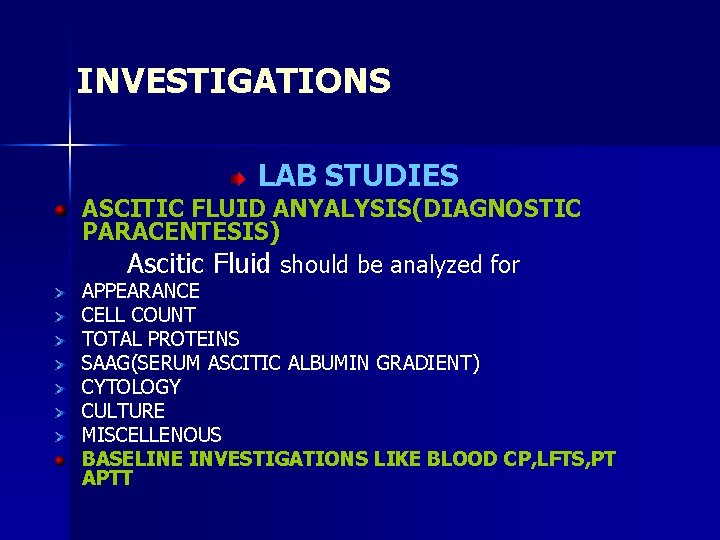
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) Ascitic Fluid should be analyzed for APPEARANCE CELL COUNT TOTAL PROTEINS SAAG(SERUM ASCITIC ALBUMIN GRADIENT) CYTOLOGY CULTURE MISCELLENOUS BASELINE INVESTIGATIONS LIKE BLOOD CP, LFTS, PT APTT
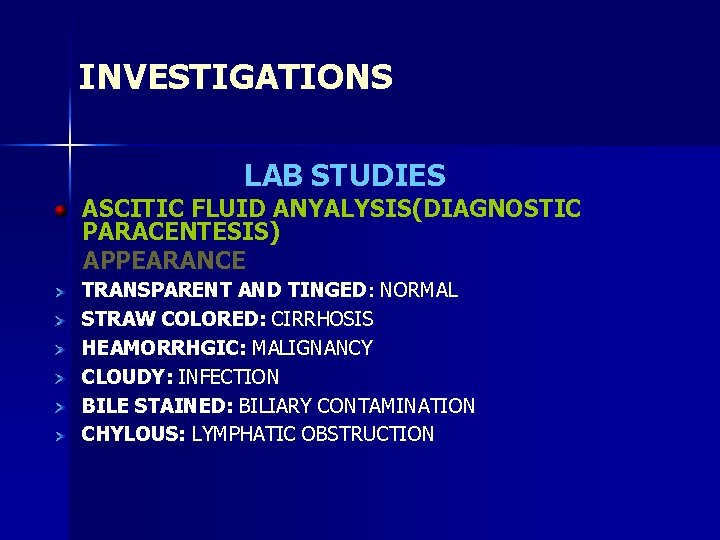
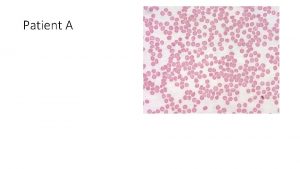
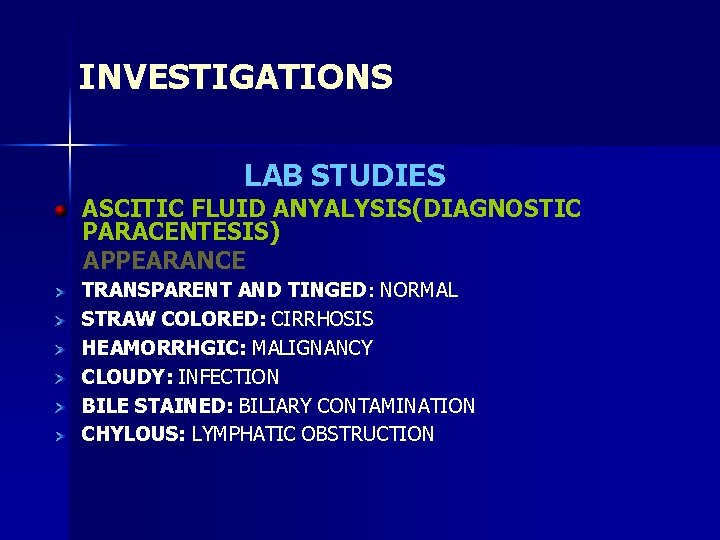
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) APPEARANCE TRANSPARENT AND TINGED: NORMAL STRAW COLORED: CIRRHOSIS HEAMORRHGIC: MALIGNANCY CLOUDY: INFECTION BILE STAINED: BILIARY CONTAMINATION CHYLOUS: LYMPHATIC OBSTRUCTION
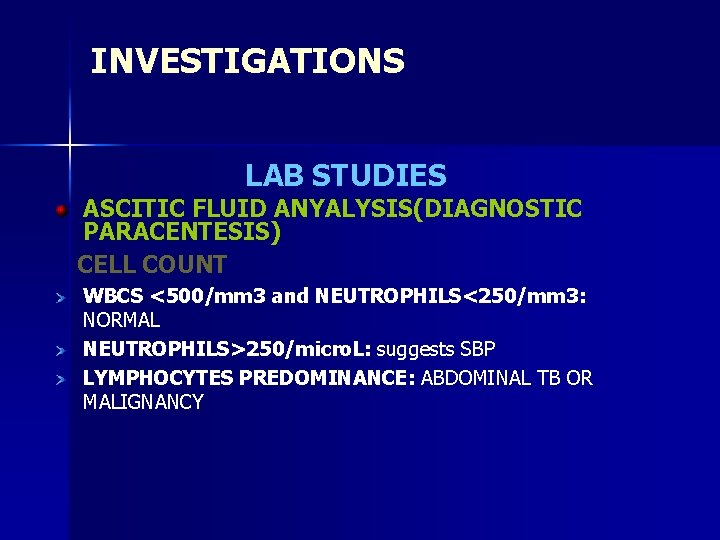
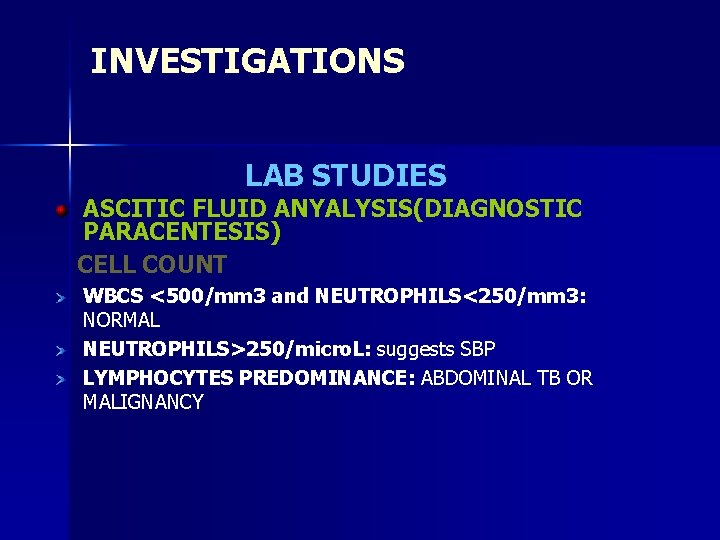
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) CELL COUNT WBCS <500/mm 3 and NEUTROPHILS<250/mm 3: NORMAL NEUTROPHILS>250/micro. L: suggests SBP LYMPHOCYTES PREDOMINANCE: ABDOMINAL TB OR MALIGNANCY
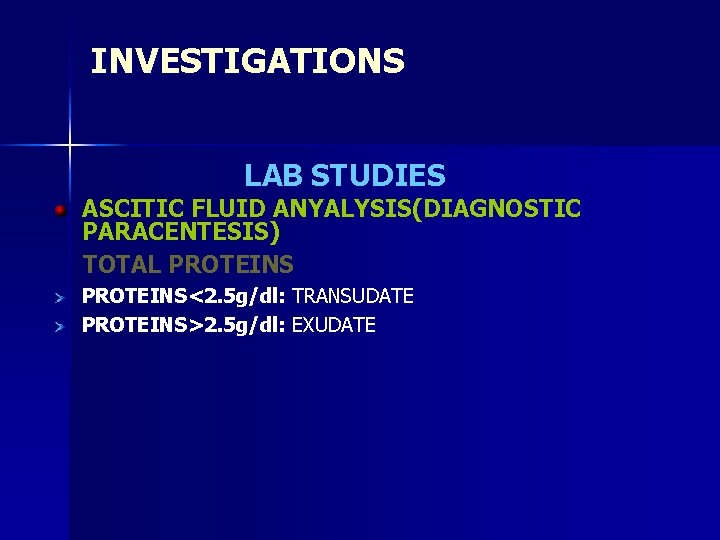
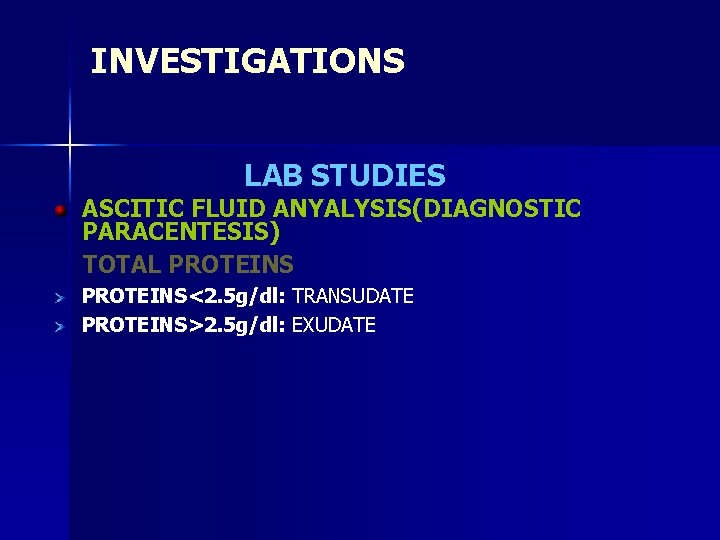
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) TOTAL PROTEINS<2. 5 g/dl: TRANSUDATE PROTEINS>2. 5 g/dl: EXUDATE
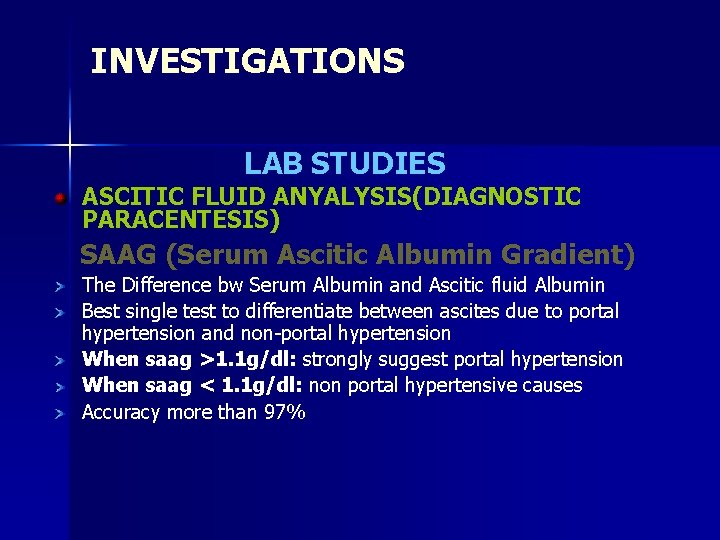
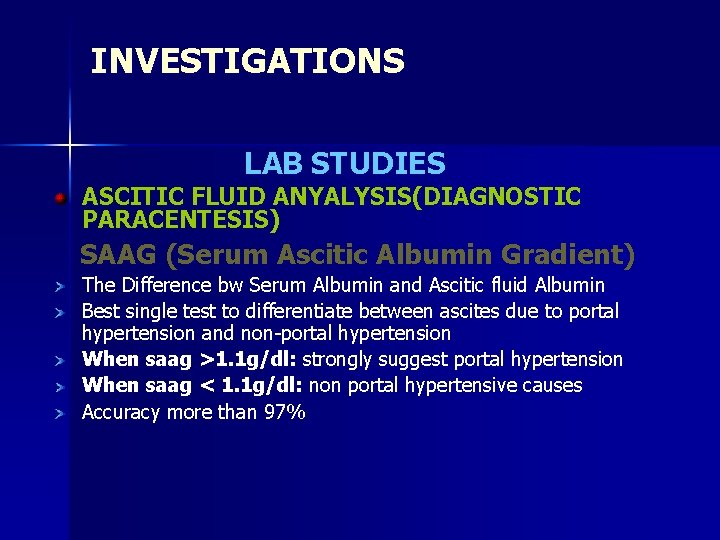
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) SAAG (Serum Ascitic Albumin Gradient) The Difference bw Serum Albumin and Ascitic fluid Albumin Best single test to differentiate between ascites due to portal hypertension and non-portal hypertension When saag >1. 1 g/dl: strongly suggest portal hypertension When saag < 1. 1 g/dl: non portal hypertensive causes Accuracy more than 97%
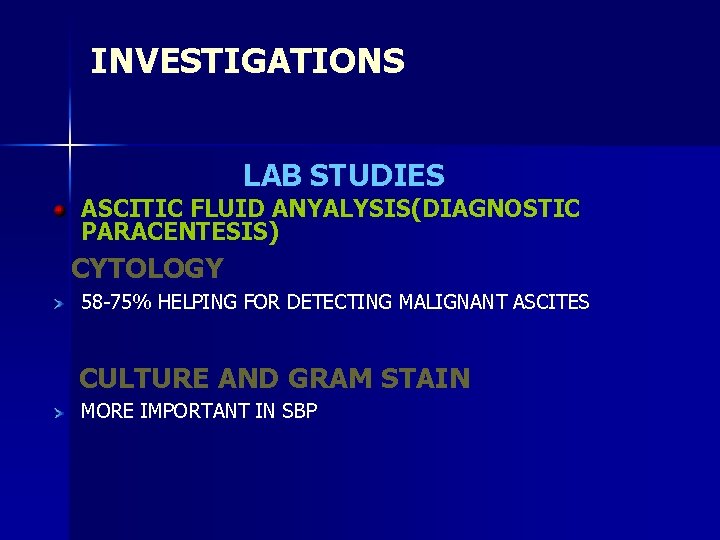
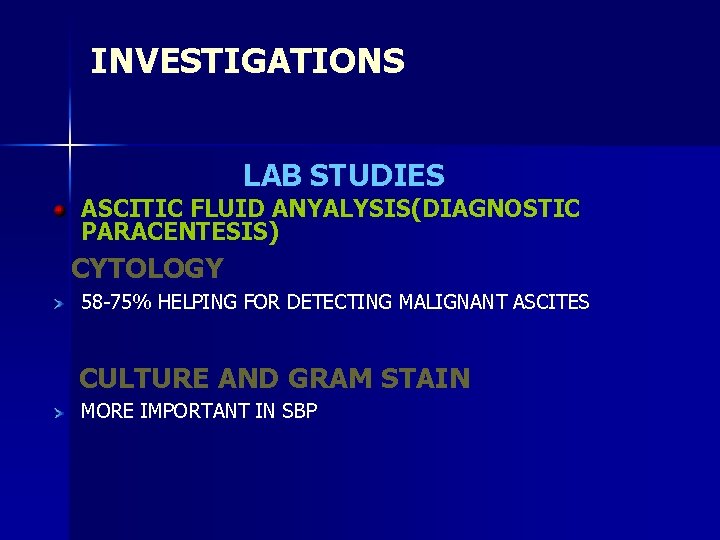
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) CYTOLOGY 58 -75% HELPING FOR DETECTING MALIGNANT ASCITES CULTURE AND GRAM STAIN MORE IMPORTANT IN SBP
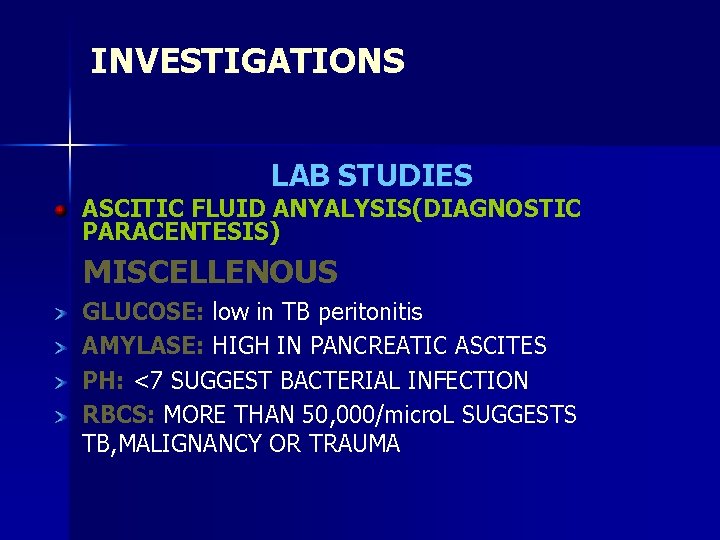
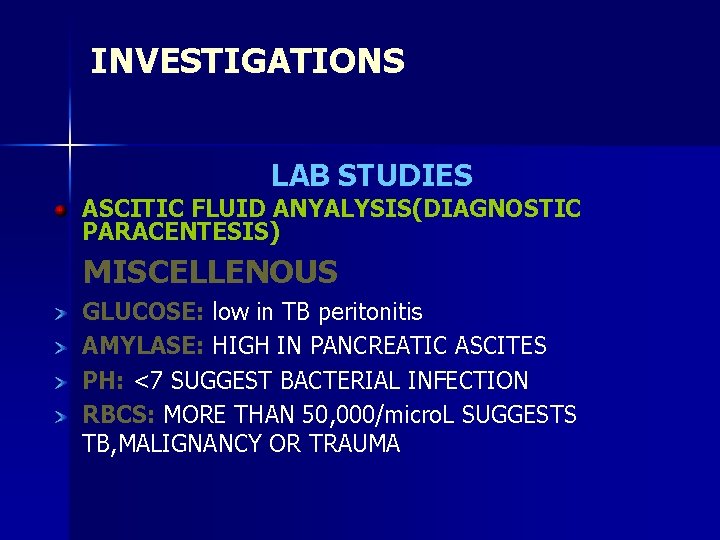
INVESTIGATIONS LAB STUDIES ASCITIC FLUID ANYALYSIS(DIAGNOSTIC PARACENTESIS) MISCELLENOUS GLUCOSE: low in TB peritonitis AMYLASE: HIGH IN PANCREATIC ASCITES PH: <7 SUGGEST BACTERIAL INFECTION RBCS: MORE THAN 50, 000/micro. L SUGGESTS TB, MALIGNANCY OR TRAUMA
INVESTIGATIONS LAPROSCOPY IN SOME PATIENTS FOR DIRCET VISUALIZATION TO TAKE BIOPSIES OF LIVER PERITONEUM INTRA ABDOMINAL LYMPHNODES

MANAGEMENT COMPRISES OF: General care Medical care Surgical care
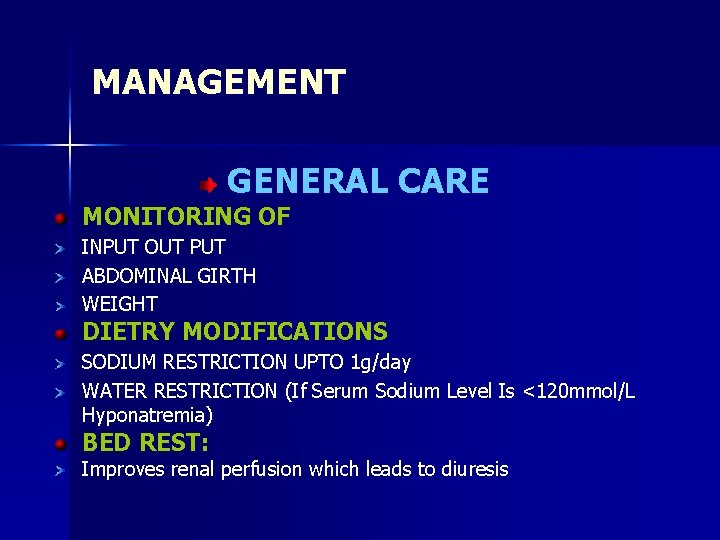
MANAGEMENT GENERAL CARE MONITORING OF INPUT OUT PUT ABDOMINAL GIRTH WEIGHT DIETRY MODIFICATIONS SODIUM RESTRICTION UPTO 1 g/day WATER RESTRICTION (If Serum Sodium Level Is <120 mmol/L Hyponatremia) BED REST: Improves renal perfusion which leads to diuresis
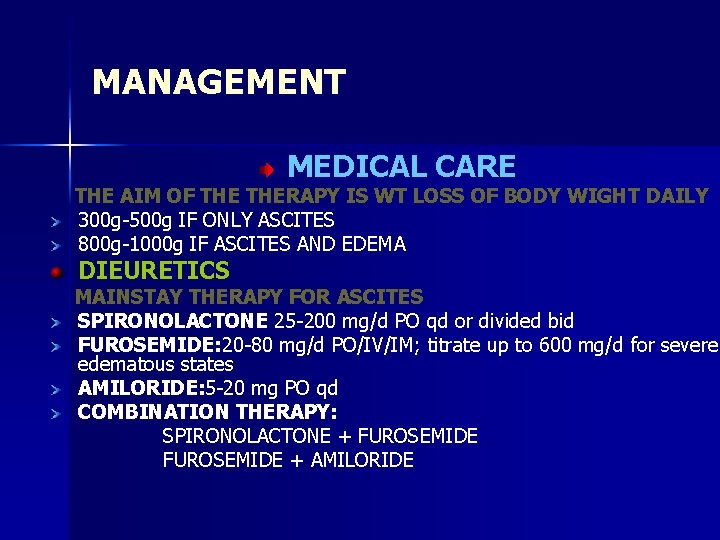
MANAGEMENT MEDICAL CARE THE AIM OF THERAPY IS WT LOSS OF BODY WIGHT DAILY 300 g-500 g IF ONLY ASCITES 800 g-1000 g IF ASCITES AND EDEMA DIEURETICS MAINSTAY THERAPY FOR ASCITES SPIRONOLACTONE 25 -200 mg/d PO qd or divided bid FUROSEMIDE: 20 -80 mg/d PO/IV/IM; titrate up to 600 mg/d for severe edematous states AMILORIDE: 5 -20 mg PO qd COMBINATION THERAPY: SPIRONOLACTONE + FUROSEMIDE + AMILORIDE
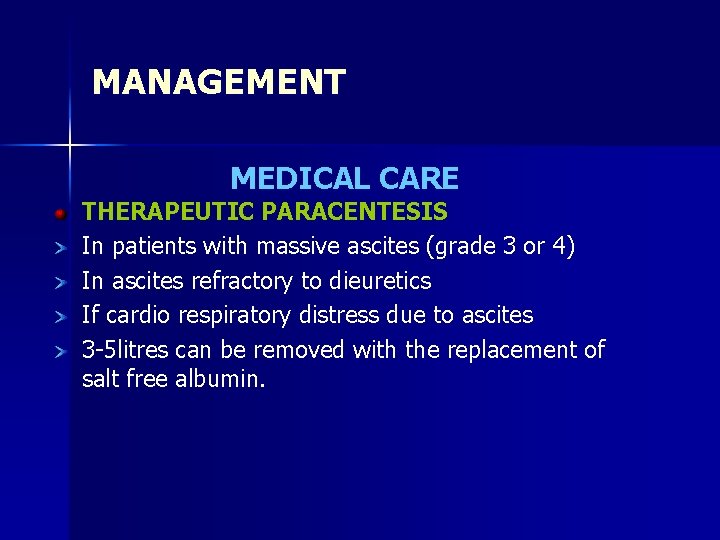
MANAGEMENT MEDICAL CARE THERAPEUTIC PARACENTESIS In patients with massive ascites (grade 3 or 4) In ascites refractory to dieuretics If cardio respiratory distress due to ascites 3 -5 litres can be removed with the replacement of salt free albumin.

MANAGEMENT MEDICAL CARE TIPS(TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT) Becoming standard of care in dieuretic resistant ascites
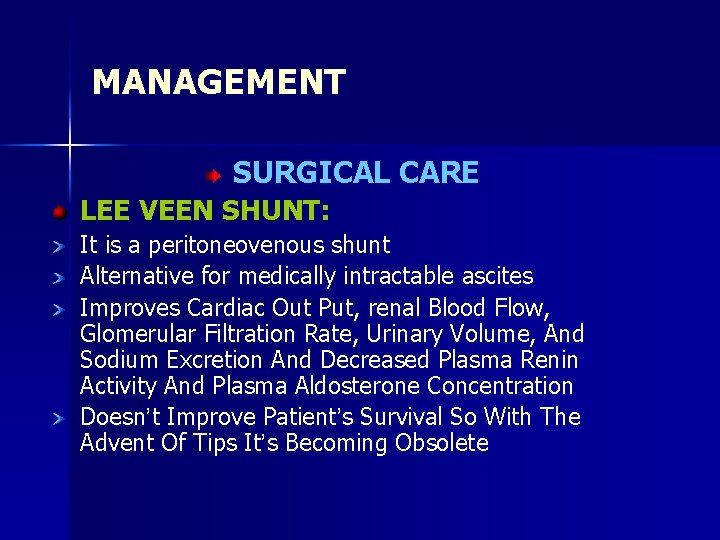
MANAGEMENT SURGICAL CARE LEE VEEN SHUNT: It is a peritoneovenous shunt Alternative for medically intractable ascites Improves Cardiac Out Put, renal Blood Flow, Glomerular Filtration Rate, Urinary Volume, And Sodium Excretion And Decreased Plasma Renin Activity And Plasma Aldosterone Concentration Doesn’t Improve Patient’s Survival So With The Advent Of Tips It’s Becoming Obsolete
COMPLICATIONS THE MOST COMMON COMPLICATION IS: SBP (Spontaneous Bacterial Peritonitis)
COMPLICATIONS SBP Most common bacteria is E. Coli. Bacteria are believed to gain access to peritoneum by hematogenous route. Low ascitic fluid albumin (<1 g/dl) predisposes SBP Abrupt onset of Fever, Chills, Generalizd Abdominal Pain, Rebound Tenderness. Ascitic Fluid analysis shows wbcs >500/mm 3 l and Eutrophil>250/mm 3 Third generation Cephalosporins 2 g tid started empirically for 5 days till c/s report is available. Recurrence is common. Ciprofloxacin 750 mg once weekly can be given prophylacticaly.

MCQs Q. No 1 IF SAAG IS >1. 1 THEN THE CAUSE WOULD BE ALL EXCEPT: PORTAL HYPERTENSION MYXEDEMA NEPHROTIC SYNDROME TUBERCULOUS PERITONITIS
MCQs Q. No 2 THE MOST EFFICACIOUS TREATMENT FOR REFRACTORY ASCITES IS MAXIMUM DOSE OF DIEURETICS THERAPEUTIC PARACENTESIS TIPS LEE VEEN SHUNT
MCQs Q. No 3 SBP IS MORE LIKELY WHEN WBCS >250/micro. L NEUTROPHILS>250/micro. L LYMPHOCYTES>500/micro. L ALL OF THE ABOVE

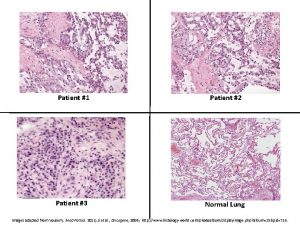
 Patient 2 patient
Patient 2 patient Ascites meaning
Ascites meaning Ascites
Ascites Ascites treatment
Ascites treatment Ascitic fluid neutrophil count
Ascitic fluid neutrophil count Saag gradient
Saag gradient Normal bowel sound
Normal bowel sound Rivalta próba
Rivalta próba How to palpate the spleen
How to palpate the spleen Ascites mnemonic
Ascites mnemonic Denver shunt for ascites
Denver shunt for ascites Neonatal liver failure
Neonatal liver failure Shifting dullness
Shifting dullness Psoas sign
Psoas sign Refractory ascites
Refractory ascites Pco wels
Pco wels Ascites vs belly fat
Ascites vs belly fat Abdominal
Abdominal Ascites punctio
Ascites punctio Overfill theory of ascites
Overfill theory of ascites Woman mild ascites pictures
Woman mild ascites pictures Positive castell's sign
Positive castell's sign Chylous ascites lymphoma
Chylous ascites lymphoma Sbp treatment guidelines
Sbp treatment guidelines Serous fluid
Serous fluid Saag ascites formula
Saag ascites formula Fluid thrill meaning
Fluid thrill meaning Peritoneal fluid analysis
Peritoneal fluid analysis Pbc vs psc
Pbc vs psc Dipping method of spleen palpation
Dipping method of spleen palpation Theoretical models of counseling
Theoretical models of counseling Research approach example
Research approach example Michael treacy and fred wiersema
Michael treacy and fred wiersema Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Multiple approach avoidance conflict
Multiple approach avoidance conflict Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Virtual circuit and datagram network
Virtual circuit and datagram network Bandura's reciprocal determinism
Bandura's reciprocal determinism Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi