Liver Disease and Jaundice Kasia Lenz and Dr


- Slides: 69
Liver Disease and Jaundice Kasia Lenz and Dr. Andrea Boone February 2, 2012
Objectives • • Jaundice ALF – Etiology – Clinical presentation – Management – Disposition • Complications of Cirrhosis – SBP – encephalopathy

Jaundice
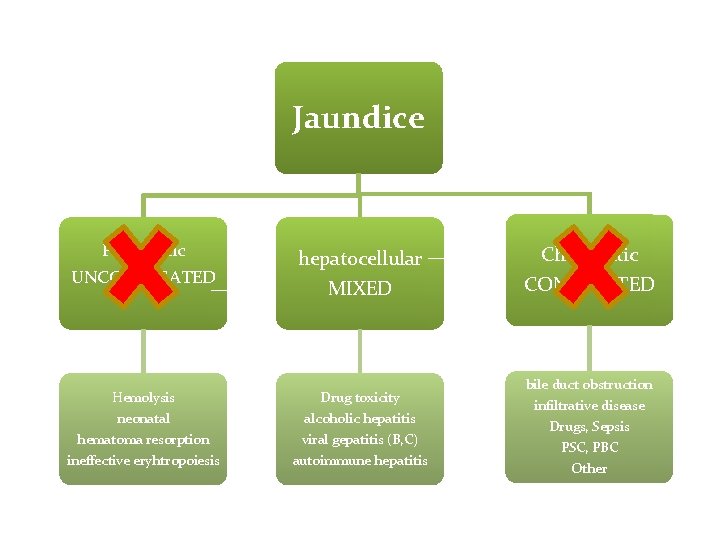
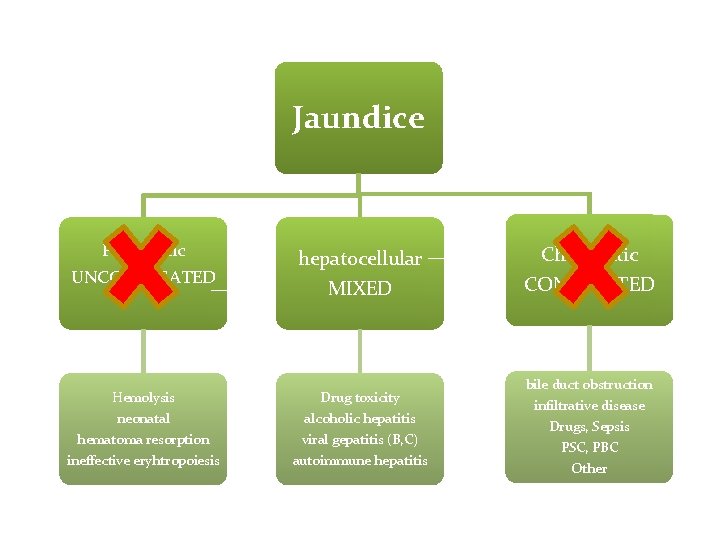
Jaundice Prehepatic UNCONJUGATED hepatocellular MIXED Hemolysis neonatal Drug toxicity alcoholic hepatitis hematoma resorption ineffective eryhtropoiesis viral gepatitis (B, C) autoimmune hepatitis Cholestatic CONJUGATED bile duct obstruction infiltrative disease Drugs, Sepsis PSC, PBC Other
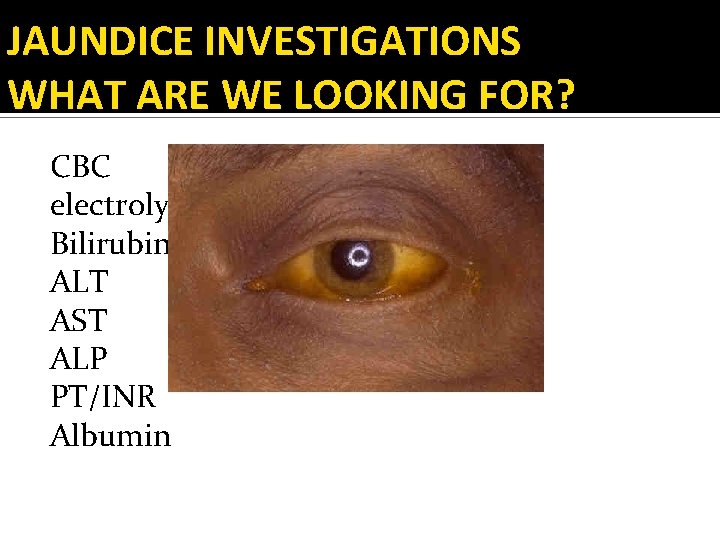
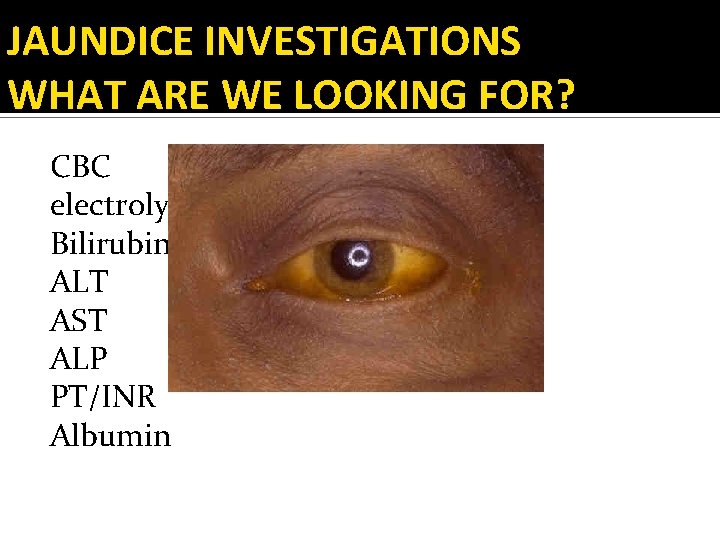
JAUNDICE INVESTIGATIONS WHAT ARE WE LOOKING FOR? CBC electrolytes Bilirubin (Direct/Indirect) ALT AST ALP PT/INR Albumin
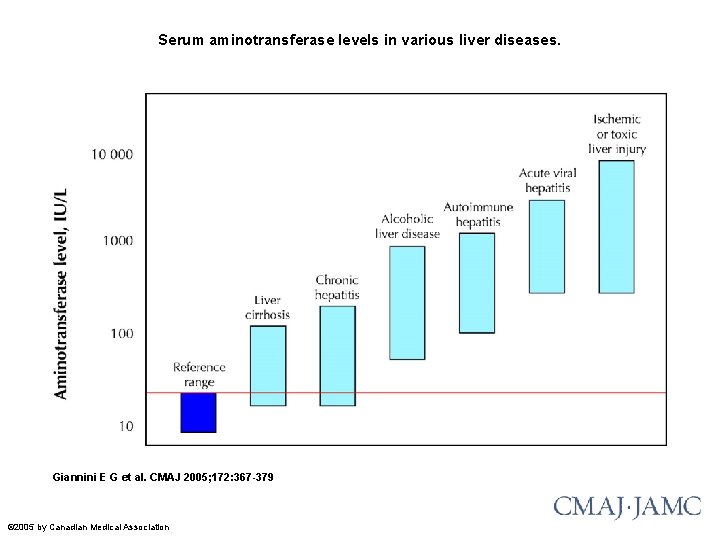
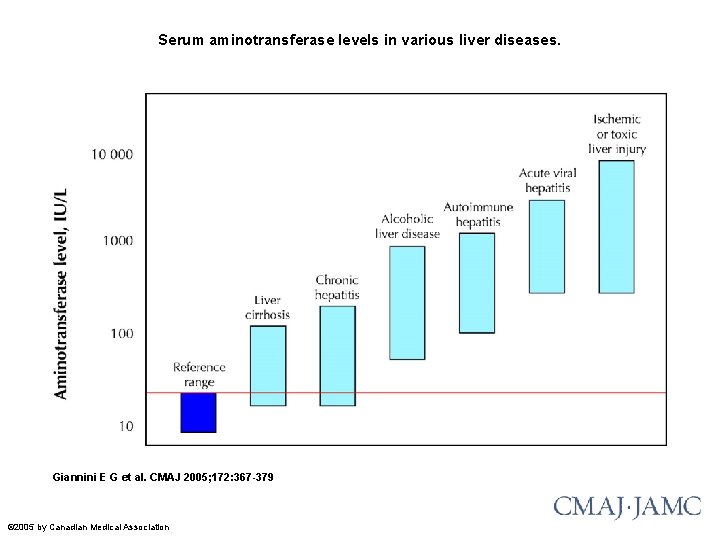
Serum aminotransferase levels in various liver diseases. Giannini E G et al. CMAJ 2005; 172: 367 -379 © 2005 by Canadian Medical Association
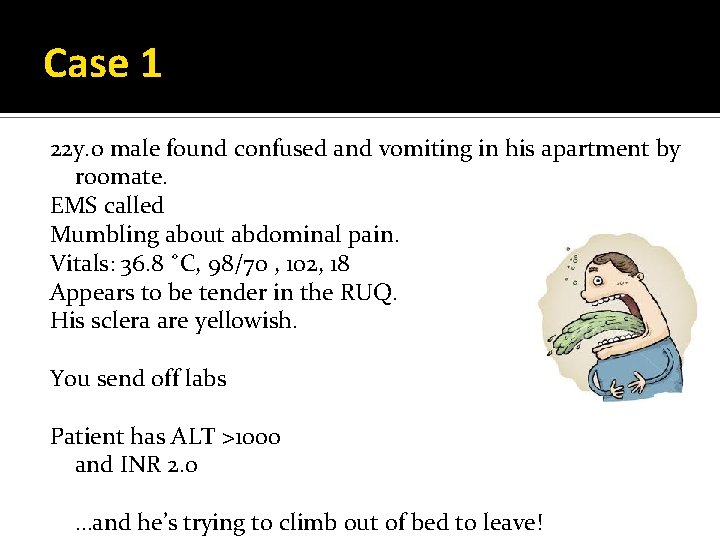
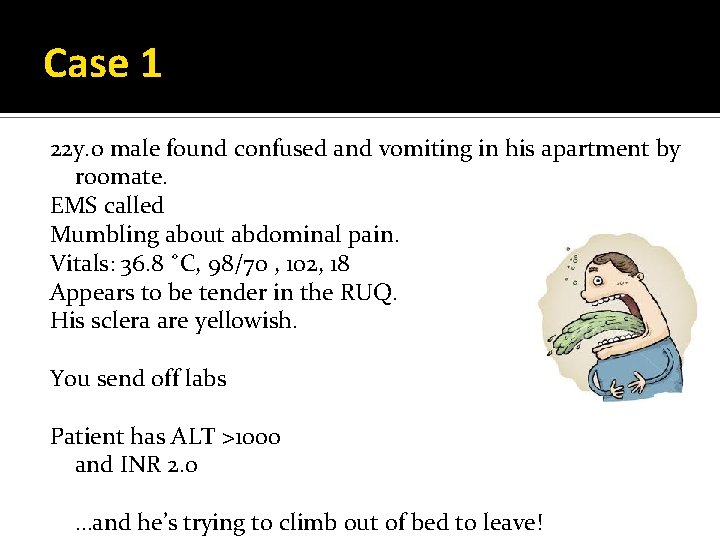
Case 1 22 y. o male found confused and vomiting in his apartment by roomate. EMS called Mumbling about abdominal pain. Vitals: 36. 8 ˚C, 98/70 , 102, 18 Appears to be tender in the RUQ. His sclera are yellowish. You send off labs Patient has ALT >1000 and INR 2. 0 …and he’s trying to climb out of bed to leave!
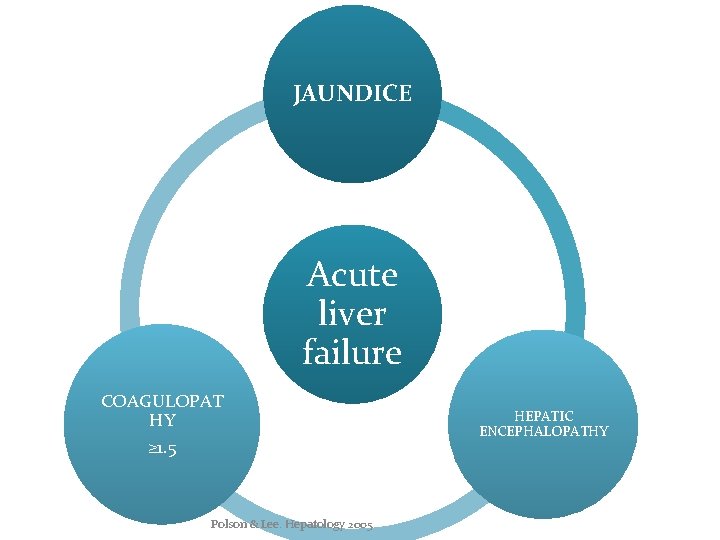
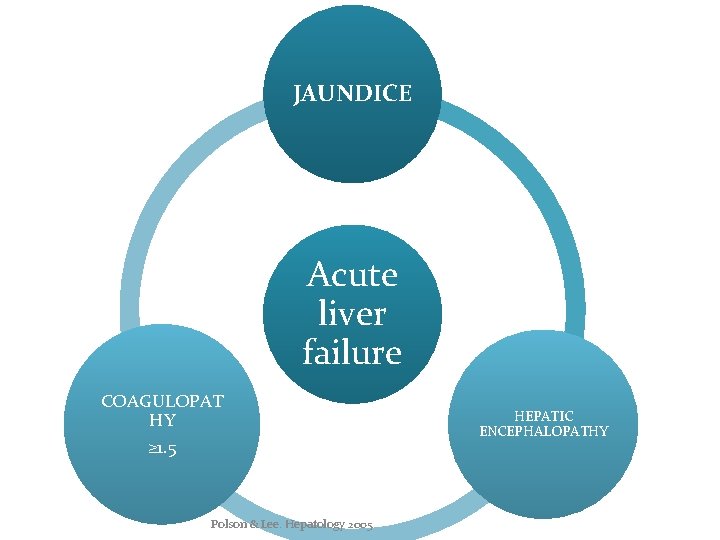
JAUNDICE Acute liver failure COAGULOPAT HY ≥ 1. 5 Polson & Lee. Hepatology 2005 HEPATIC ENCEPHALOPATHY
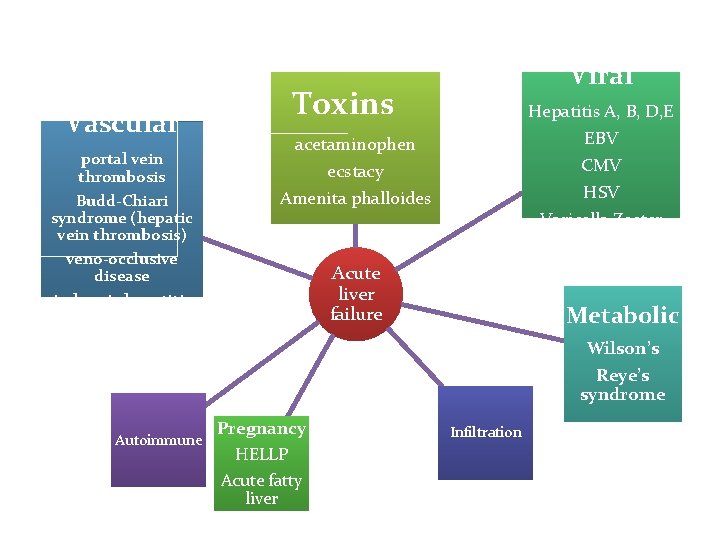
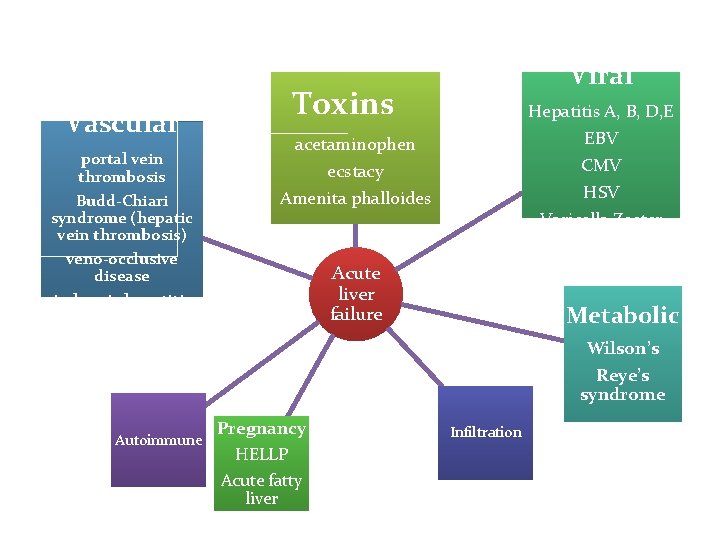
Vascular portal vein thrombosis Budd-Chiari syndrome (hepatic vein thrombosis) Viral Toxins Hepatitis A, B, D, E EBV CMV HSV Varicella Zoster acetaminophen ecstacy Amenita phalloides veno-occlusive disease ischemic hepatitis Acute liver failure Metabolic Wilson’s Reye’s syndrome Autoimmune Pregnancy HELLP Acute fatty liver Infiltration
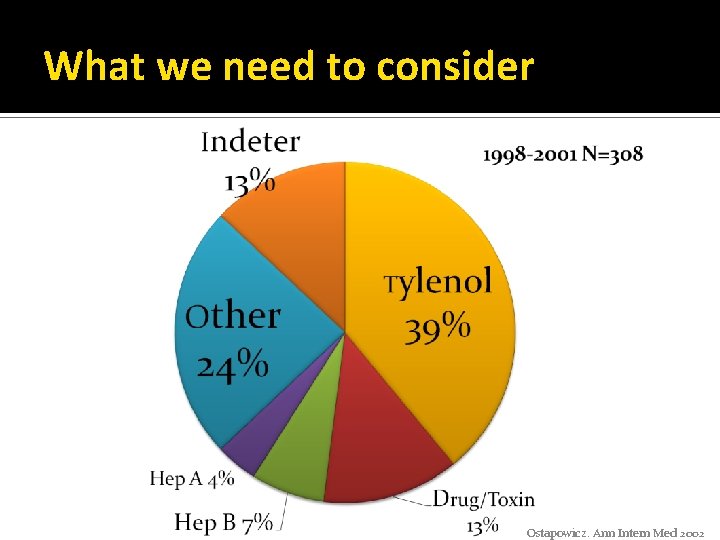
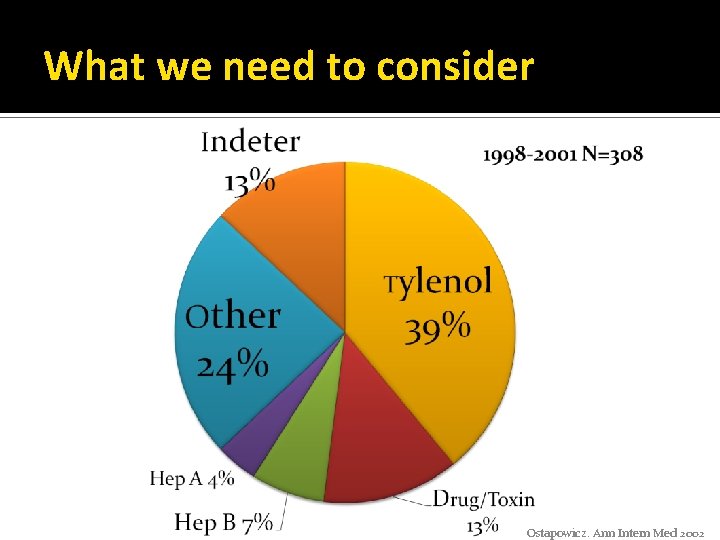
What we need to consider Ostapowicz. Ann Intern Med 2002
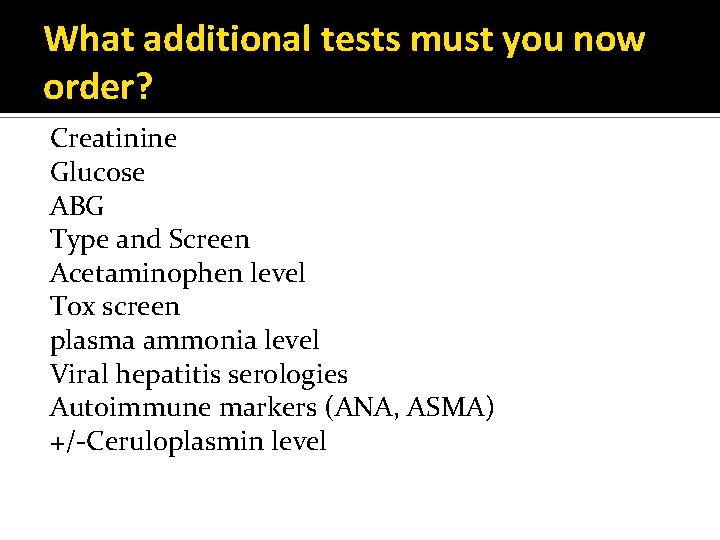
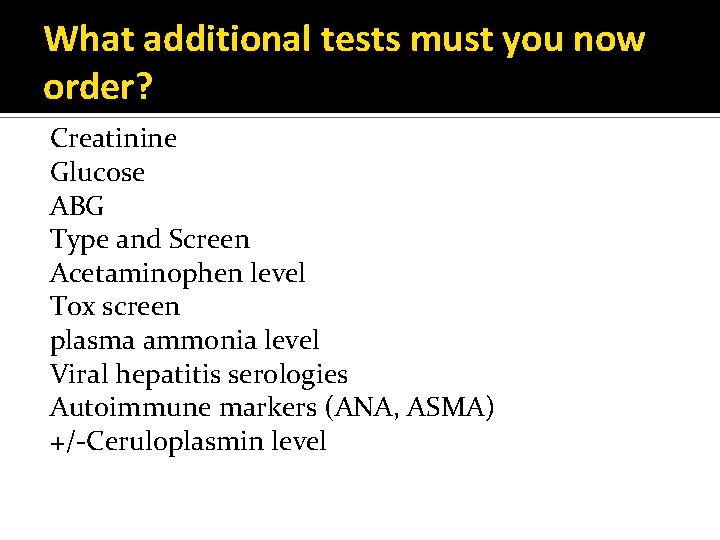
What additional tests must you now order? Creatinine Glucose ABG Type and Screen Acetaminophen level Tox screen plasma ammonia level Viral hepatitis serologies Autoimmune markers (ANA, ASMA) +/-Ceruloplasmin level
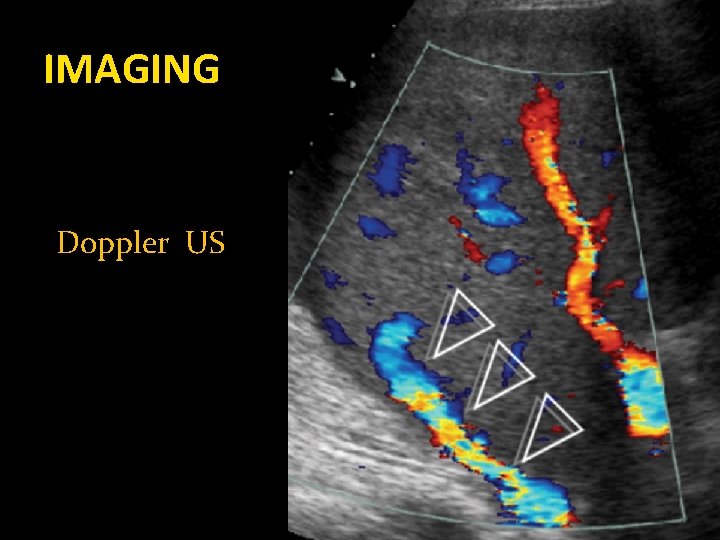
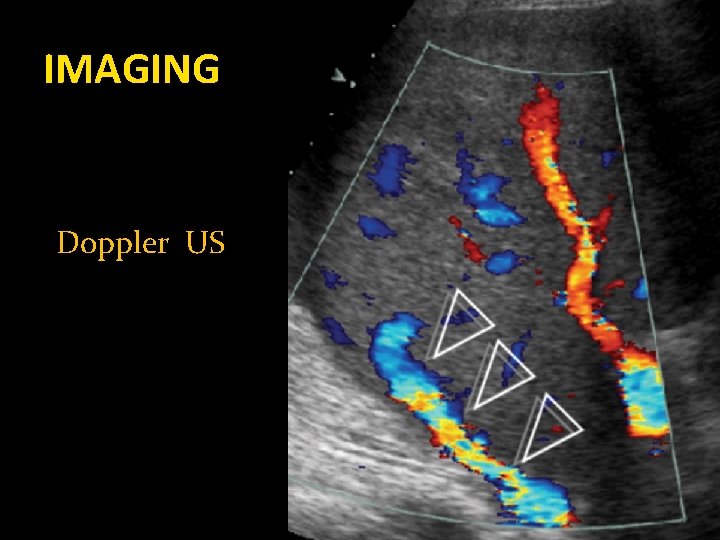
IMAGING Doppler US
NOW WHAT? What if he’s starting to crump?
ALF: CENTRAL NERVOUS SYSTEM Cerebral edema and intracranial hypertension MOST SERIOUS COMPLICATIONS
ALF: CENTRAL NERVOUS SYSTEM Goals: CPP> 50 -60 mm Hg ICP <20 -25 mm Hg Elevate the head of the bed to 30˚ Avoid stimulation (this includes intubation) 3. Mannitol if high ICP 0. 5 -1 g/kg repeat 1 -2 x PRN 1. 2. Polson & Lee. Hepatology 2005
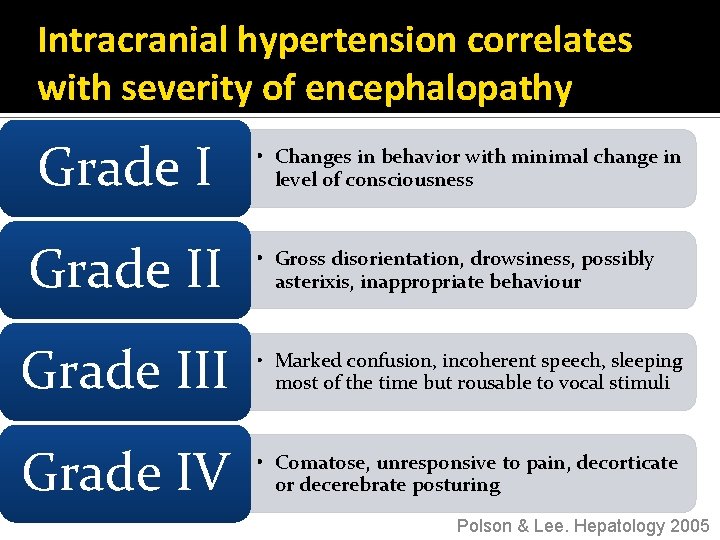
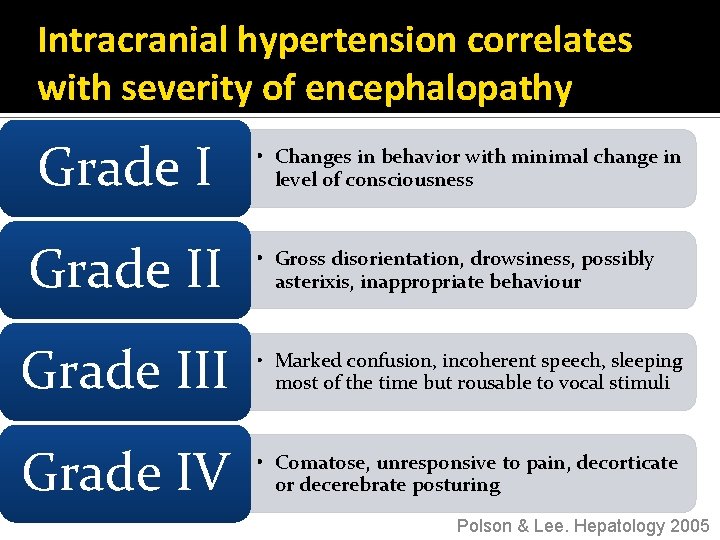
Intracranial hypertension correlates with severity of encephalopathy Grade II • Changes in behavior with minimal change in level of consciousness • Gross disorientation, drowsiness, possibly asterixis, inappropriate behaviour Grade III • Marked confusion, incoherent speech, sleeping most of the time but rousable to vocal stimuli Grade IV • Comatose, unresponsive to pain, decorticate or decerebrate posturing Polson & Lee. Hepatology 2005
Grade III/IV Ecephalopathy… INTUBATE Polson & Lee. Hepatology 2005
CIRCULATION Circulatory dysfunction mirrors sepsis keep MAP >65 early hemodynamic monitoring ▪ follow Early Goal Directed Therapy guidelines maintain normoglycemia and supplement electrolytes Polson & Lee. Hepatology 2005
Antibiotic Prophylaxis No routinely indicated BUT need to have routine surveillance AND low threshold for starting Polson & Lee. Hepatology 2005
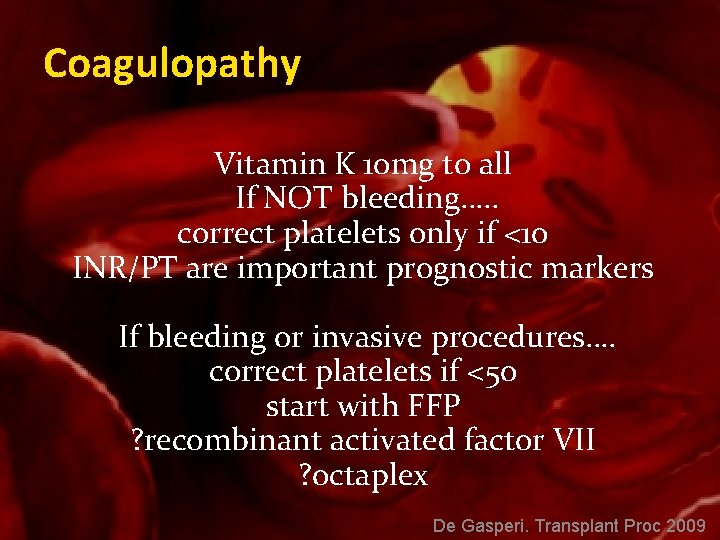
Coagulopathy Vitamin K 10 mg to all If NOT bleeding…. . correct platelets only if <10 INR/PT are important prognostic markers If bleeding or invasive procedures…. correct platelets if <50 start with FFP ? recombinant activated factor VII ? octaplex De Gasperi. Transplant Proc 2009
Agitation avoid sedation (if possible) small doses of short-acting benzos Polson & Lee. Hepatology 2005
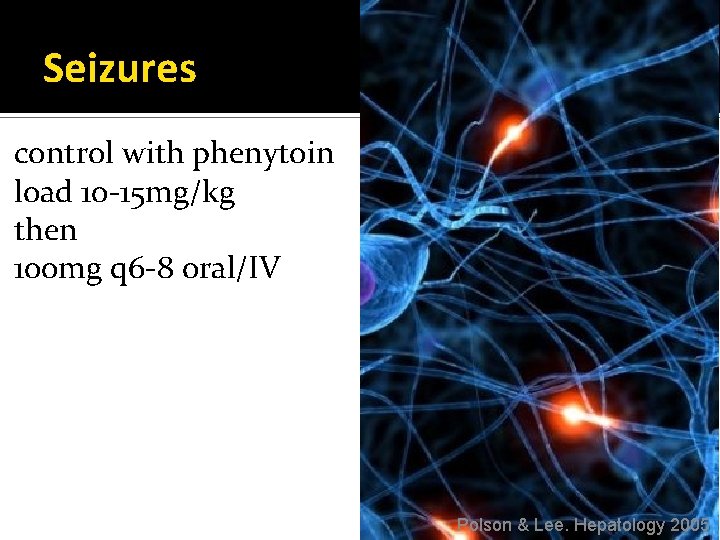
Seizures control with phenytoin load 10 -15 mg/kg then 100 mg q 6 -8 oral/IV Polson & Lee. Hepatology 2005
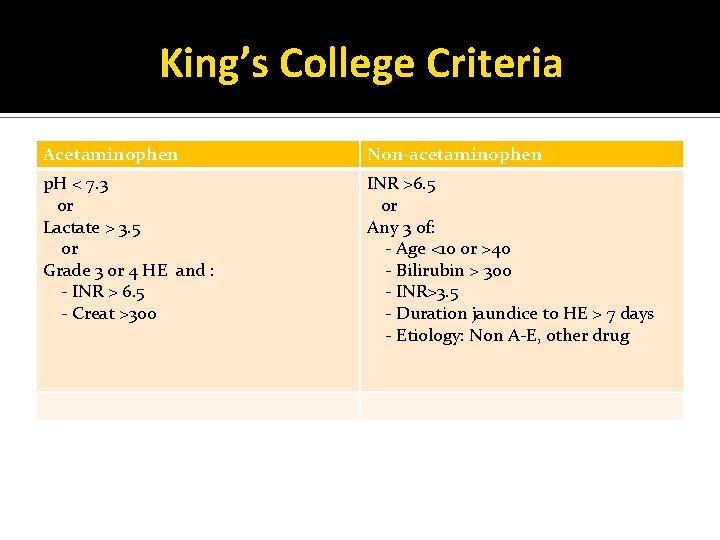
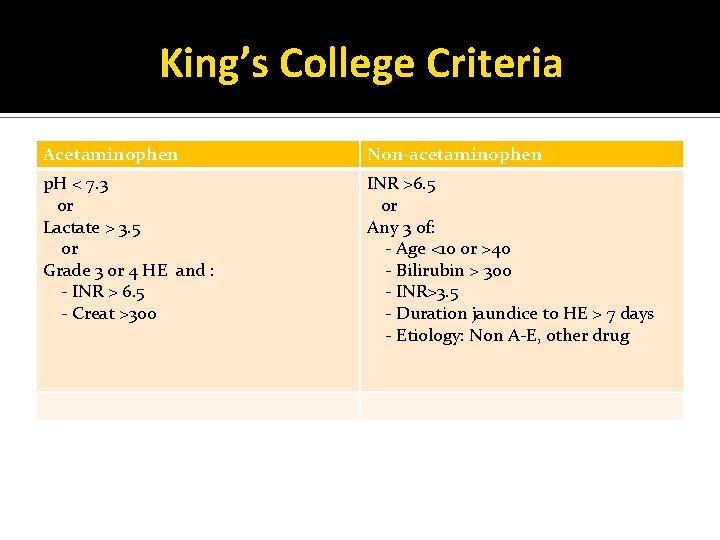
King’s College Criteria Acetaminophen Non-acetaminophen p. H < 7. 3 or Lactate > 3. 5 or Grade 3 or 4 HE and : - INR > 6. 5 - Creat >300 INR >6. 5 or Any 3 of: - Age <10 or >40 - Bilirubin > 300 - INR>3. 5 - Duration jaundice to HE > 7 days - Etiology: Non A-E, other drug
Acetaminophen Toxicity
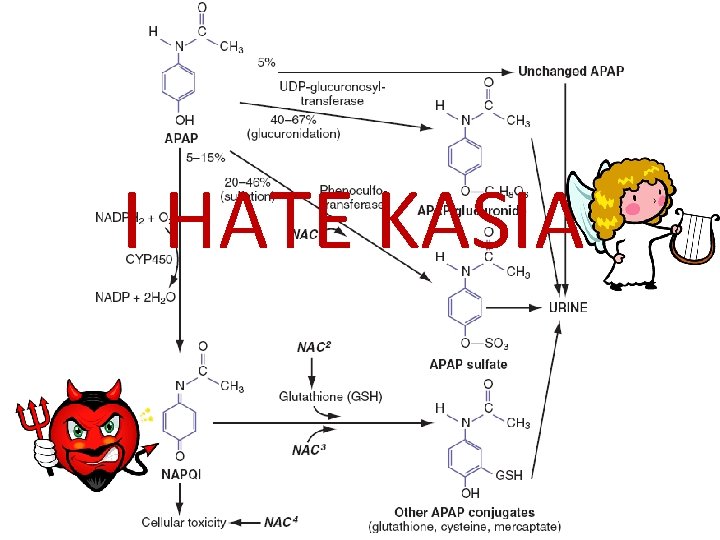
I HATE KASIA!
Acetaminophen Toxicity
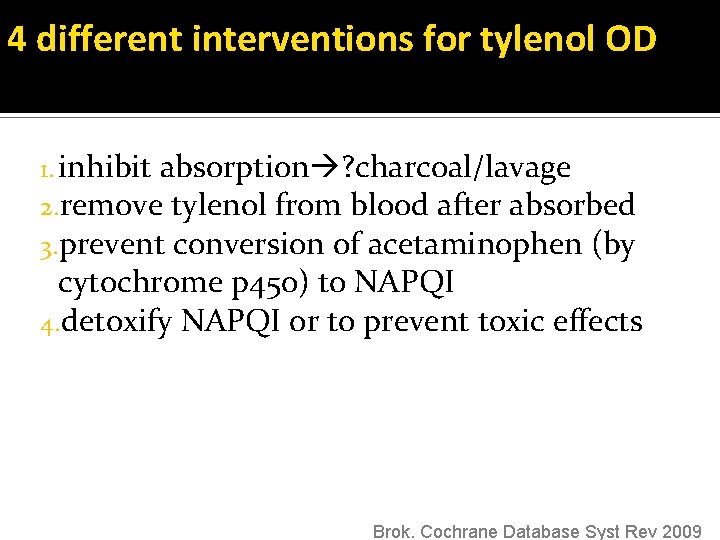
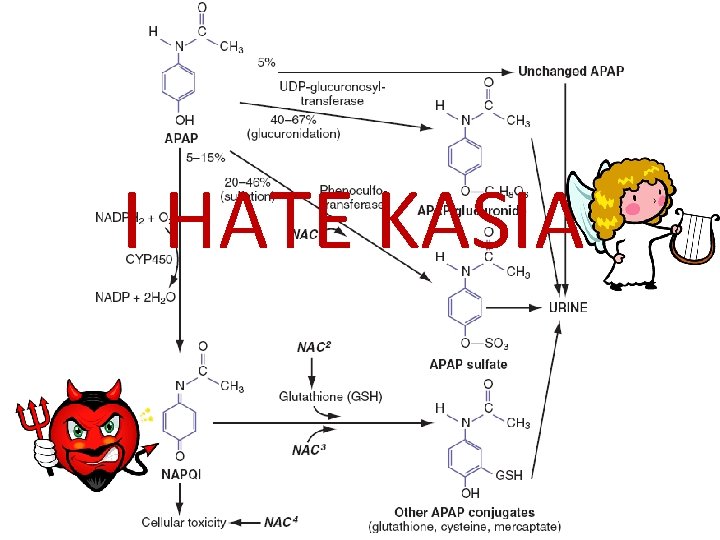
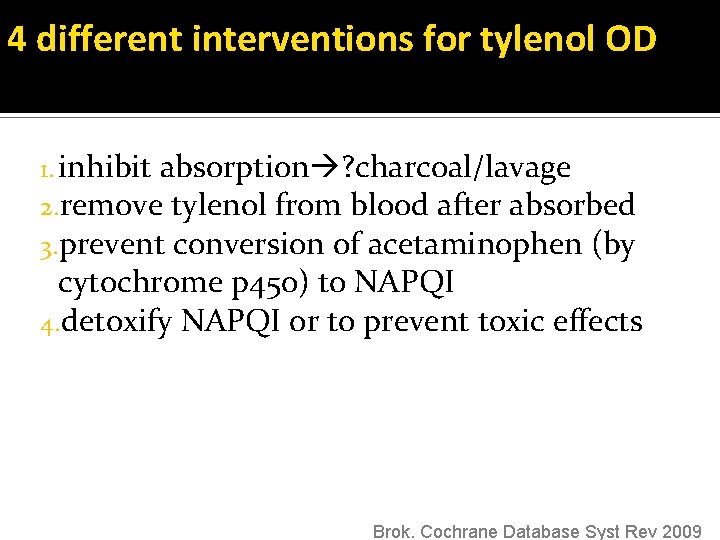
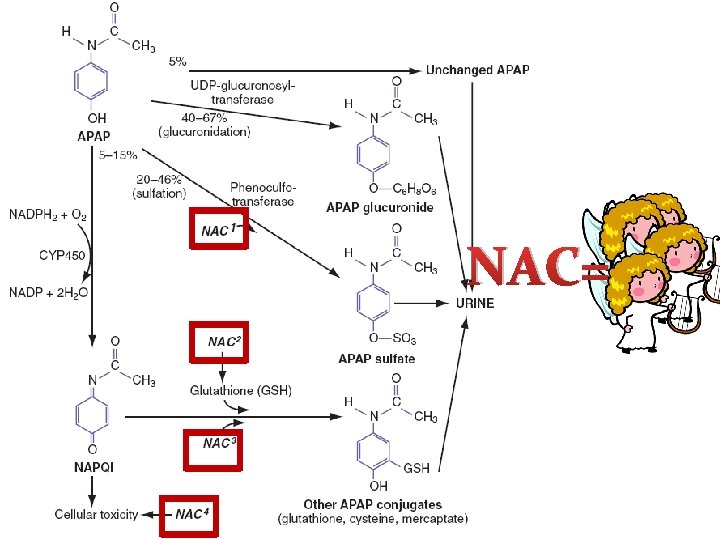
4 different interventions for tylenol OD 1. inhibit absorption ? charcoal/lavage 2. remove tylenol from blood after absorbed 3. prevent conversion of acetaminophen (by cytochrome p 450) to NAPQI 4. detoxify NAPQI or to prevent toxic effects Brok. Cochrane Database Syst Rev 2009
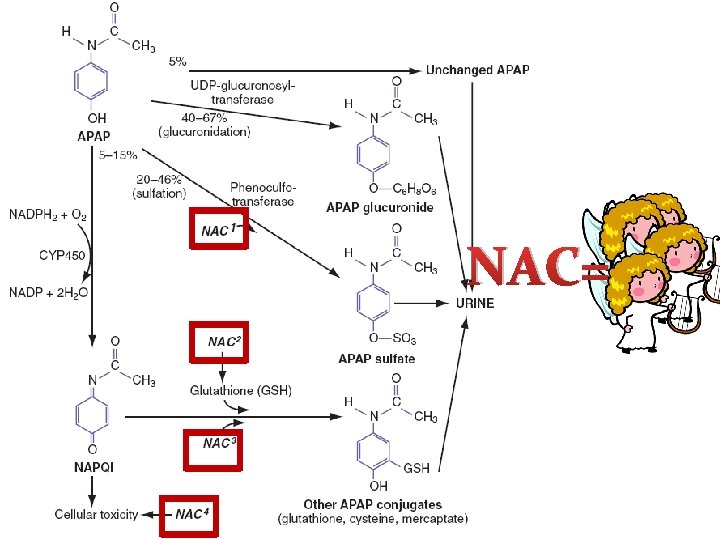
NAC=
NAC Free radical scavenger improves microcirculation and O 2 delivery antioxidant
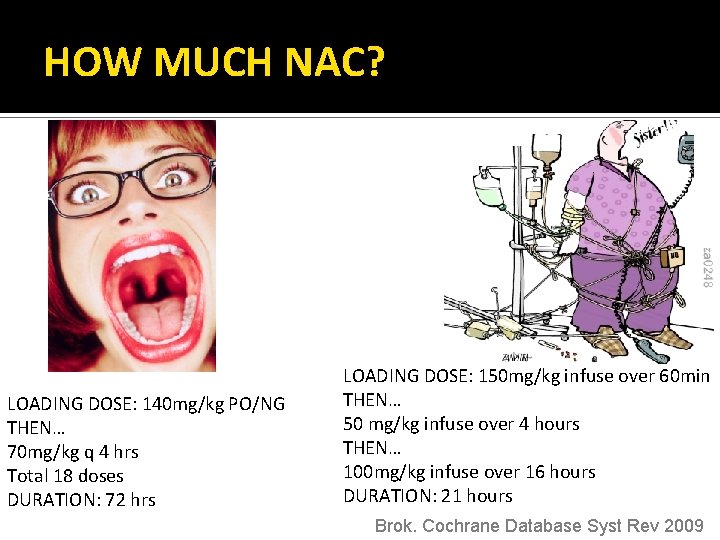
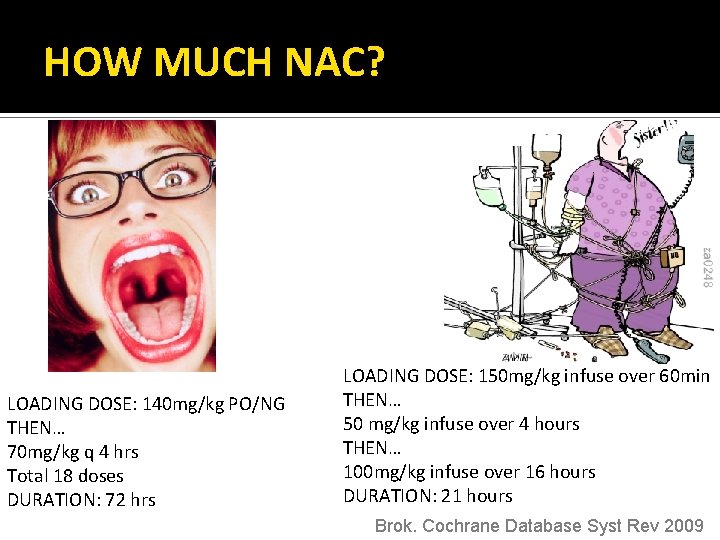
How much NAC? HOW MUCH NAC? LOADING DOSE: 140 mg/kg PO/NG THEN… 70 mg/kg q 4 hrs Total 18 doses DURATION: 72 hrs LOADING DOSE: 150 mg/kg infuse over 60 min THEN… 50 mg/kg infuse over 4 hours THEN… 100 mg/kg infuse over 16 hours DURATION: 21 hours Brok. Cochrane Database Syst Rev 2009
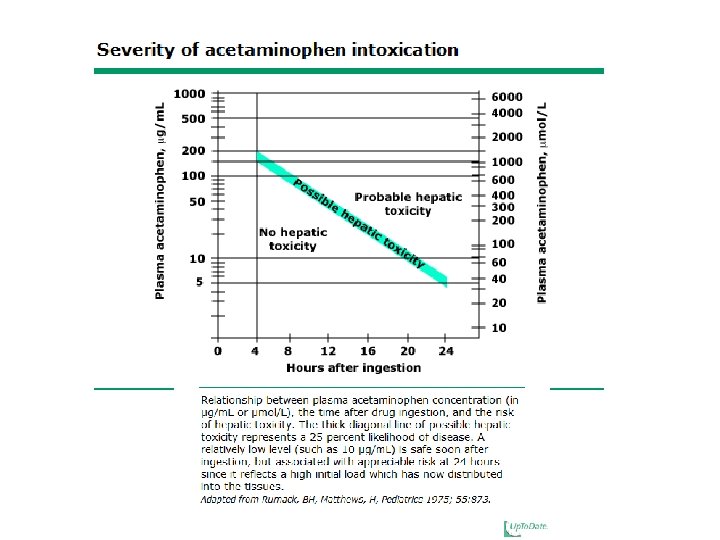
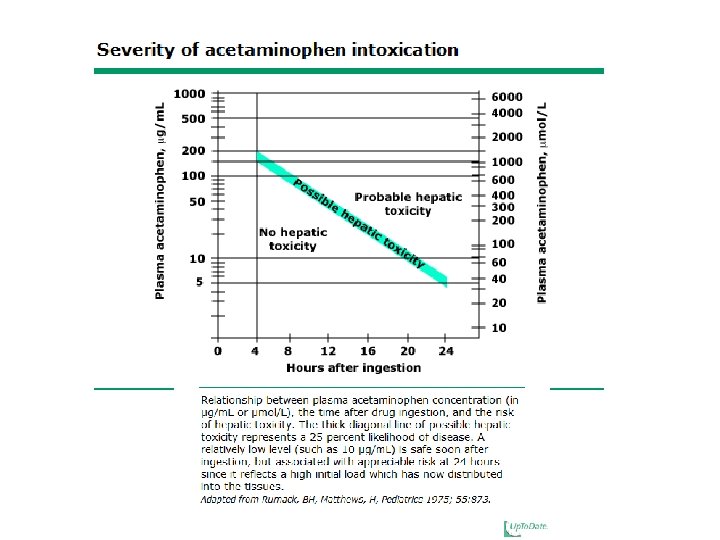
Acetaminophen: Summary 1. 2. 3. Can give activated charcoal if <2 hrs Treat if >150 ng/kg (>10 g) ingested Start NAC within 6 hrs
Case 2 34 y. o male presents to ED c/o feeling generally unwell with abdominal pain. His buddy noticed his eyes were yellow. He admits to drinking a 6 pack/night
Alcoholic Hepatitis Average >80 g/day x 5 years Not necessarily drinking now
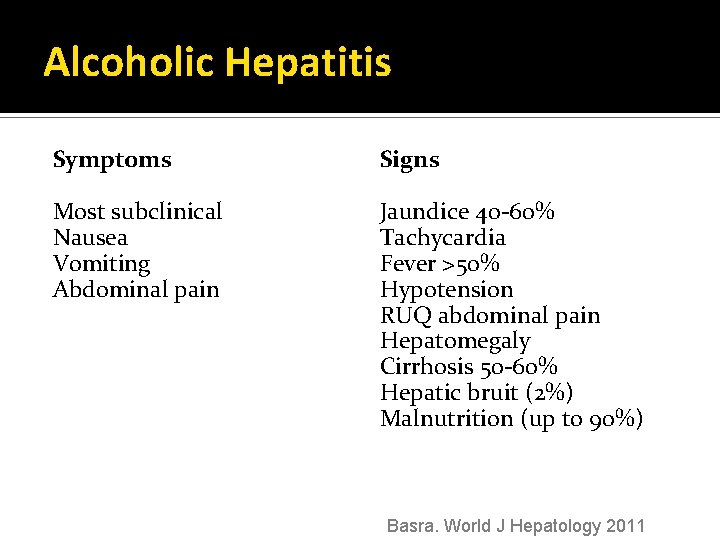
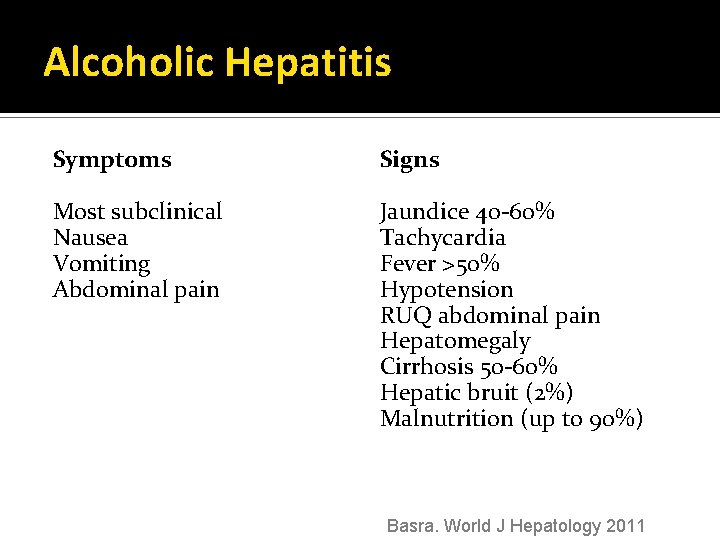
Alcoholic Hepatitis Symptoms Signs Most subclinical Nausea Vomiting Abdominal pain Jaundice 40 -60% Tachycardia Fever >50% Hypotension RUQ abdominal pain Hepatomegaly Cirrhosis 50 -60% Hepatic bruit (2%) Malnutrition (up to 90%) Basra. World J Hepatology 2011
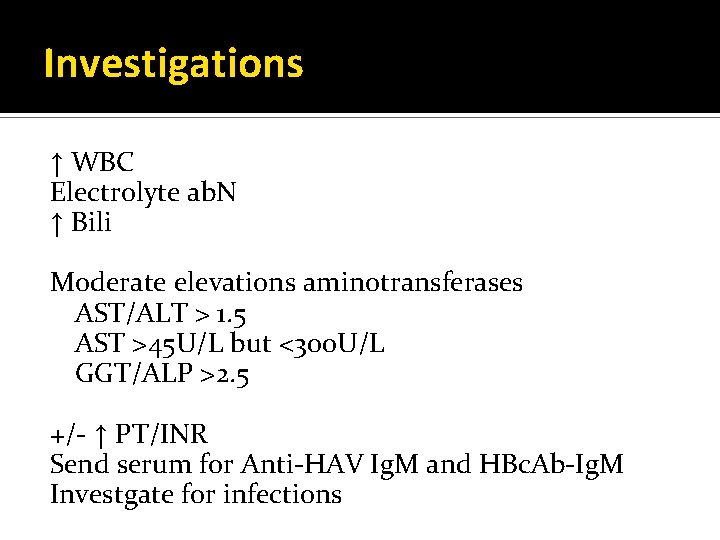
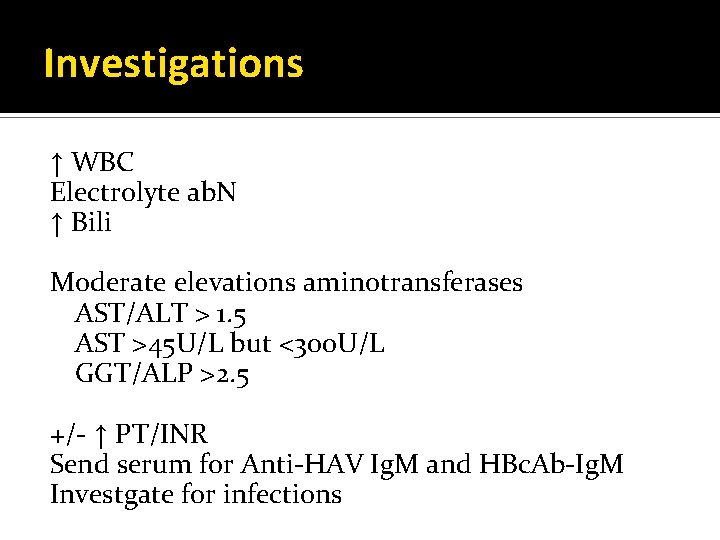
Investigations ↑ WBC Electrolyte ab. N ↑ Bili Moderate elevations aminotransferases AST/ALT > 1. 5 AST >45 U/L but <300 U/L GGT/ALP >2. 5 +/- ↑ PT/INR Send serum for Anti-HAV Ig. M and HBc. Ab-Ig. M Investgate for infections
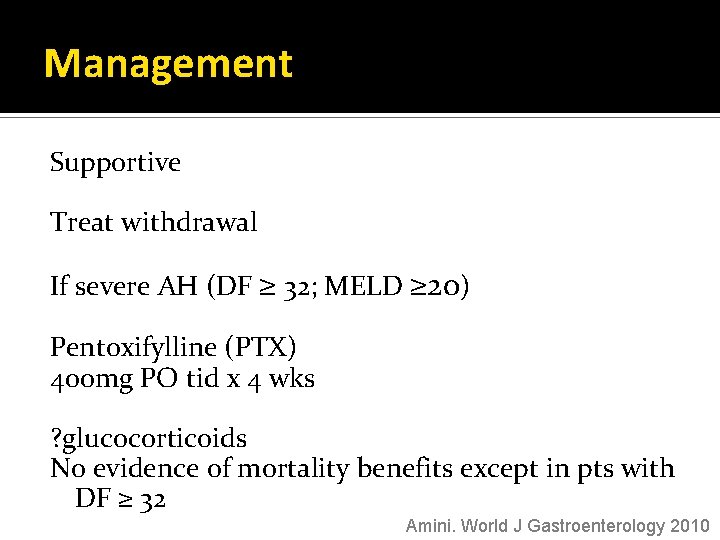
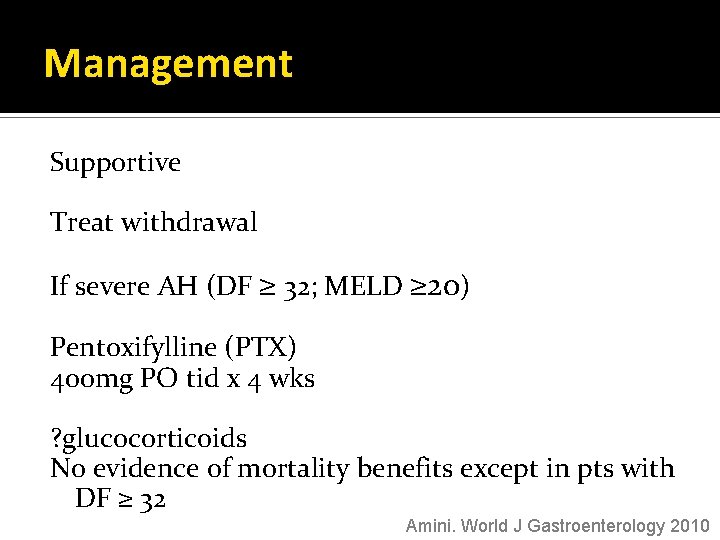
Management Supportive Treat withdrawal If severe AH (DF ≥ 32; MELD ≥ 20) Pentoxifylline (PTX) 400 mg PO tid x 4 wks ? glucocorticoids No evidence of mortality benefits except in pts with DF ≥ 32 Amini. World J Gastroenterology 2010
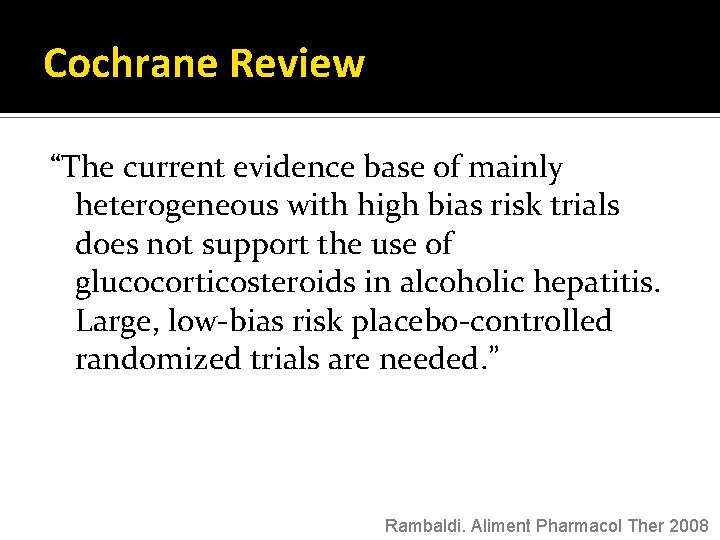
Cochrane Review “The current evidence base of mainly heterogeneous with high bias risk trials does not support the use of glucocorticosteroids in alcoholic hepatitis. Large, low-bias risk placebo-controlled randomized trials are needed. ” Rambaldi. Aliment Pharmacol Ther 2008
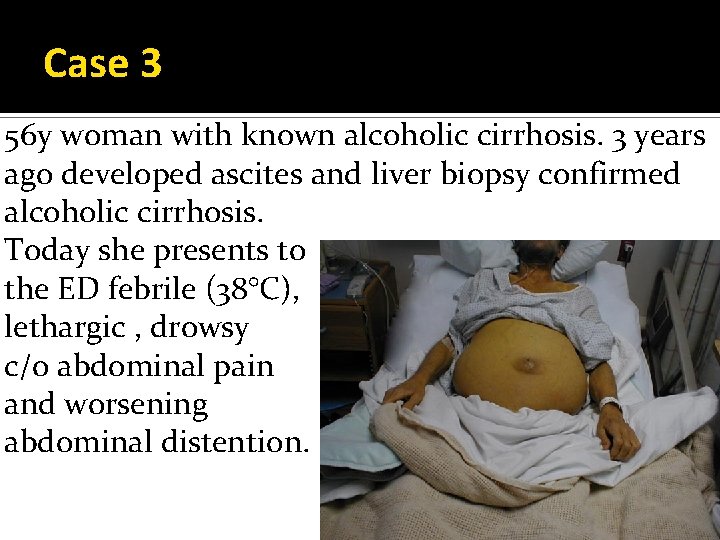
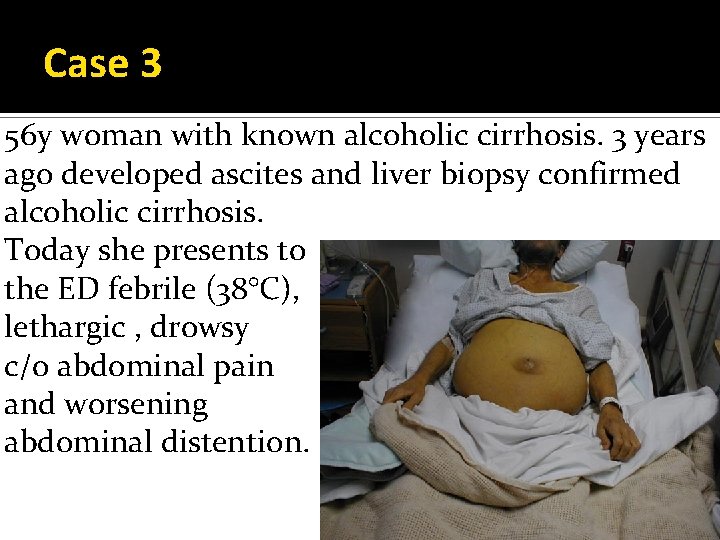
Case 3 56 y woman with known alcoholic cirrhosis. 3 years ago developed ascites and liver biopsy confirmed alcoholic cirrhosis. Today she presents to the ED febrile (38°C), lethargic , drowsy c/o abdominal pain and worsening abdominal distention.
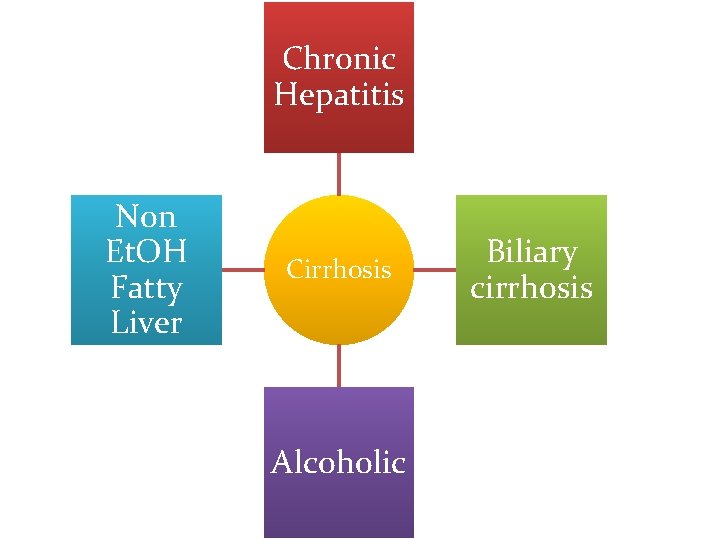
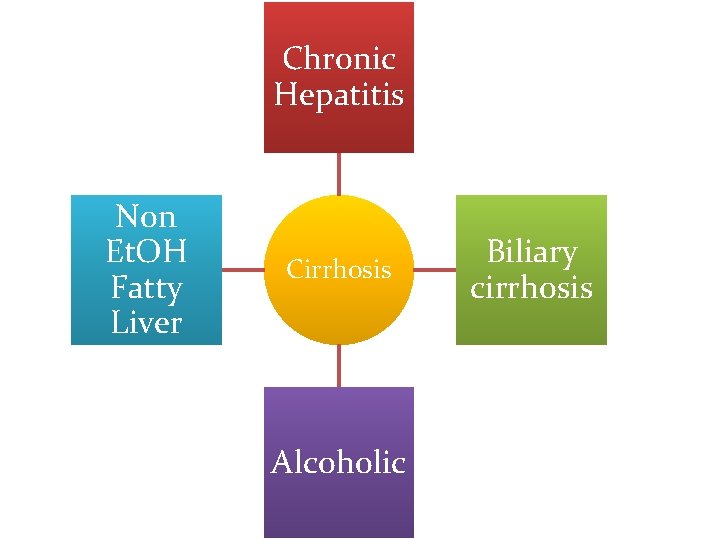
Chronic Hepatitis Non Et. OH Fatty Liver Cirrhosis Alcoholic Biliary cirrhosis
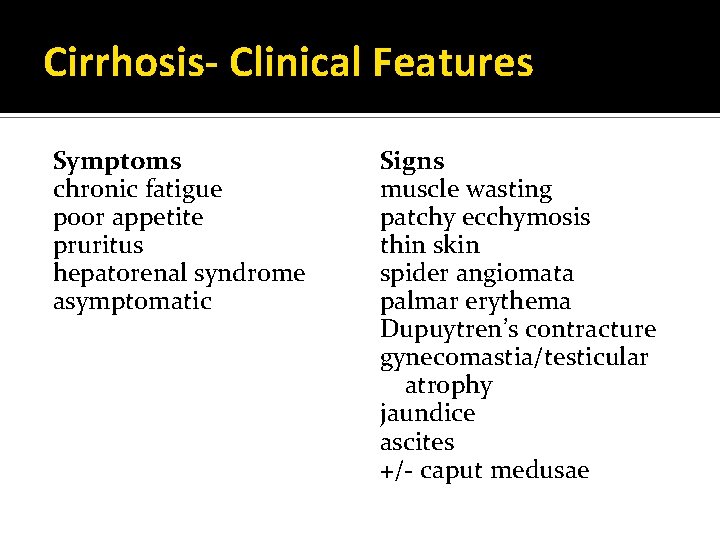
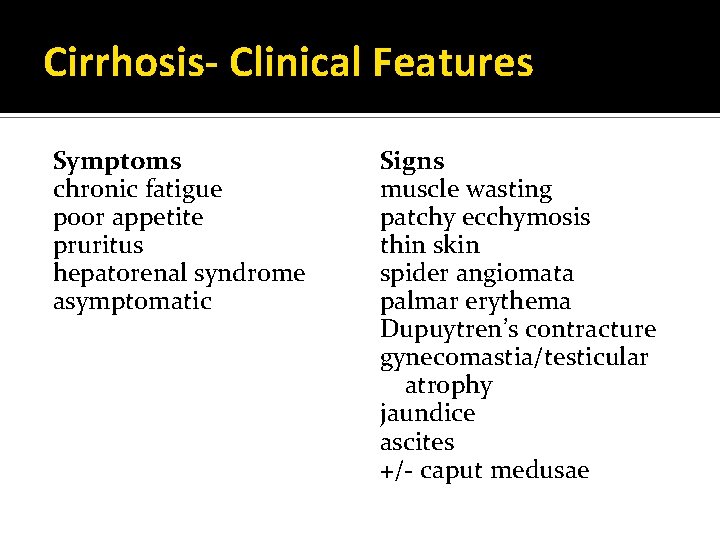
Cirrhosis- Clinical Features Symptoms chronic fatigue poor appetite pruritus hepatorenal syndrome asymptomatic Signs muscle wasting patchy ecchymosis thin skin spider angiomata palmar erythema Dupuytren’s contracture gynecomastia/testicular atrophy jaundice ascites +/- caput medusae
Cirrhosis: Management correct fluids/ lytes provide vitamins +/- paracentesis
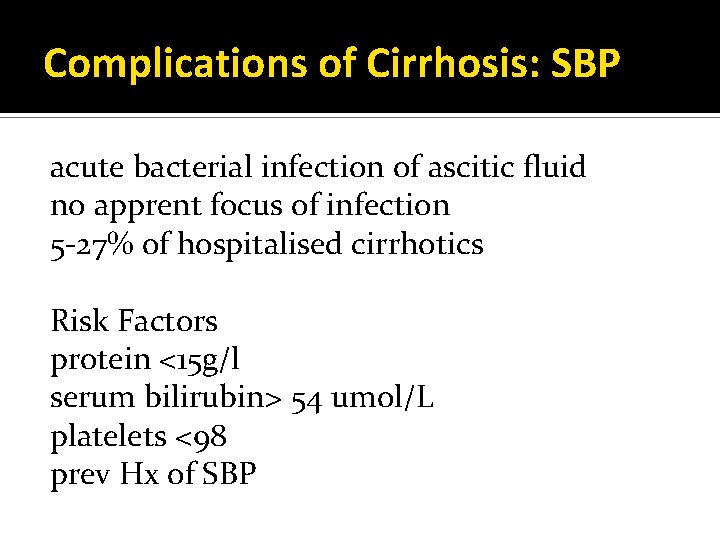
Complications of Cirrhosis: SBP acute bacterial infection of ascitic fluid no apprent focus of infection 5 -27% of hospitalised cirrhotics Risk Factors protein <15 g/l serum bilirubin> 54 umol/L platelets <98 prev Hx of SBP
SBP: organisms Enteric Gram –ve E. coli Rarely polymicrobial, anaerobic
SBP: Clinical Features mild tenderness to acute onset severe abdo pain fever/chills hemodynamic instability or slow onset of abdo discomfort and low grade fever hepatic encephalopathy 20 -50% afebrile
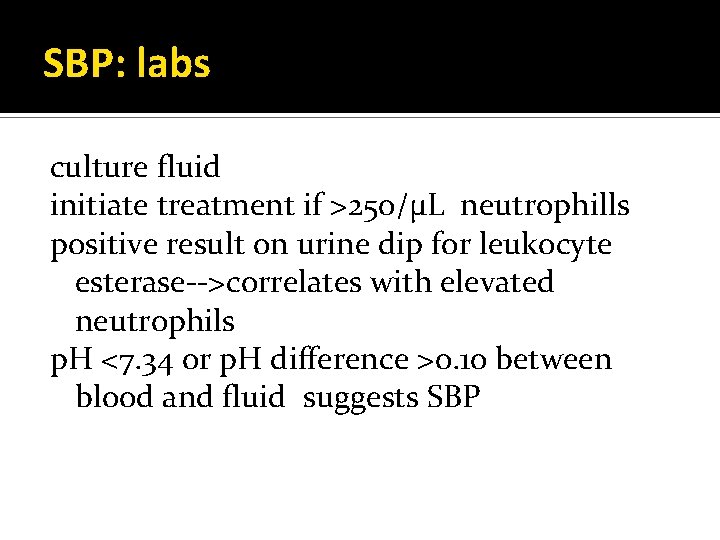
SBP: labs culture fluid initiate treatment if >250/µL neutrophills positive result on urine dip for leukocyte esterase-->correlates with elevated neutrophils p. H <7. 34 or p. H difference >0. 10 between blood and fluid suggests SBP
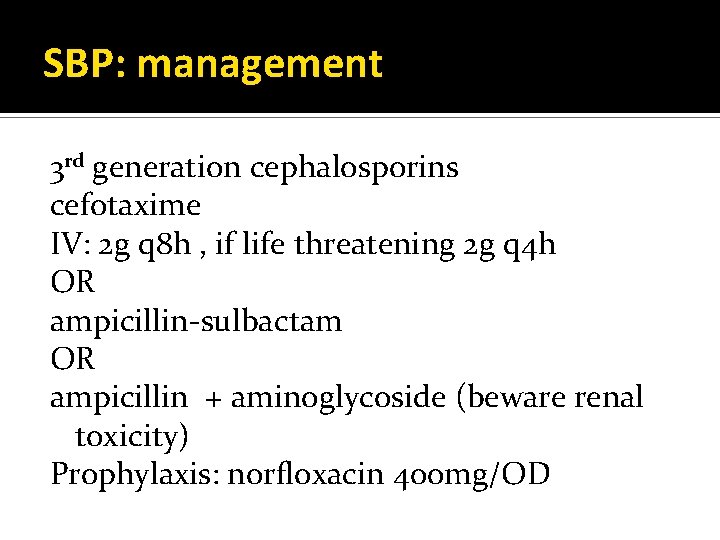
SBP: management 3 rd generation cephalosporins cefotaxime IV: 2 g q 8 h , if life threatening 2 g q 4 h OR ampicillin-sulbactam OR ampicillin + aminoglycoside (beware renal toxicity) Prophylaxis: norfloxacin 400 mg/OD
Complications of Cirrhosis: Encephalopathy acute/chronic liver disease mild cognitive dysfunction coma no correlation between [amonia] and severity Riggio World J Gastrointest Pharmacol Ther 2010
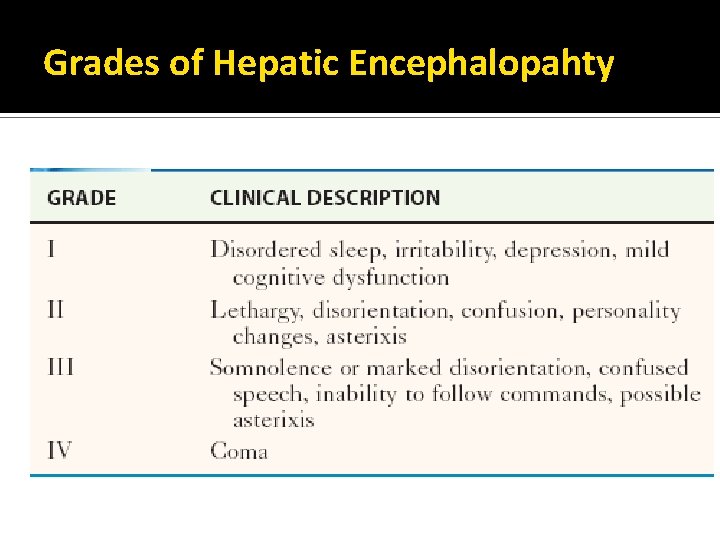
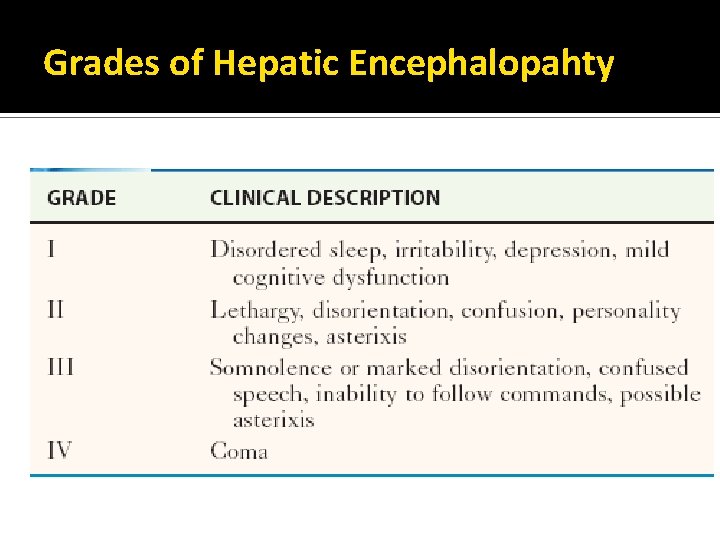
Grades of Hepatic Encephalopahty
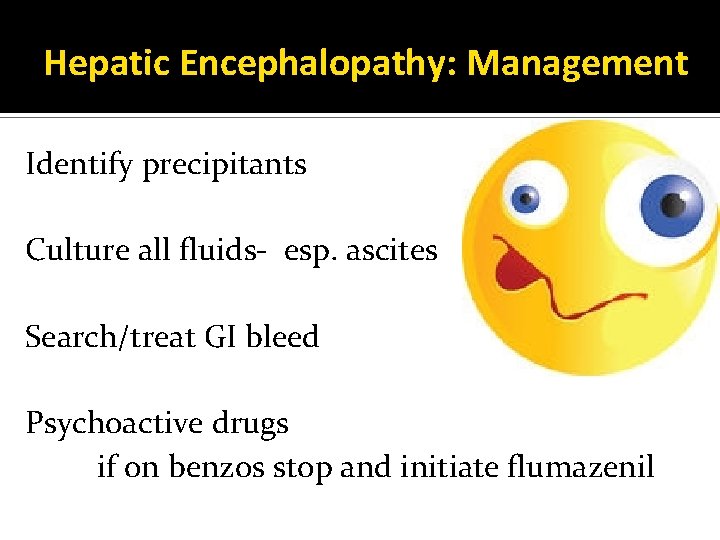
Hepatic Encephalopathy: Management Identify precipitants Culture all fluids- esp. ascites Search/treat GI bleed Psychoactive drugs if on benzos stop and initiate flumazenil
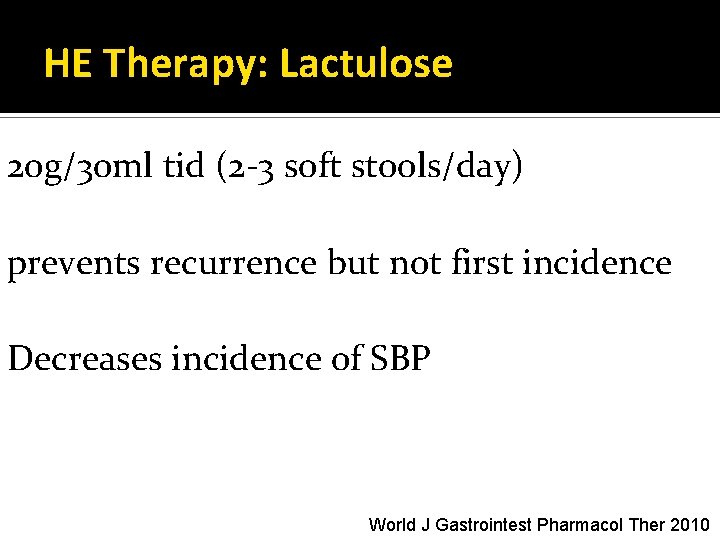
HE Therapy: Lactulose 20 g/30 ml tid (2 -3 soft stools/day) prevents recurrence but not first incidence Decreases incidence of SBP World J Gastrointest Pharmacol Ther 2010
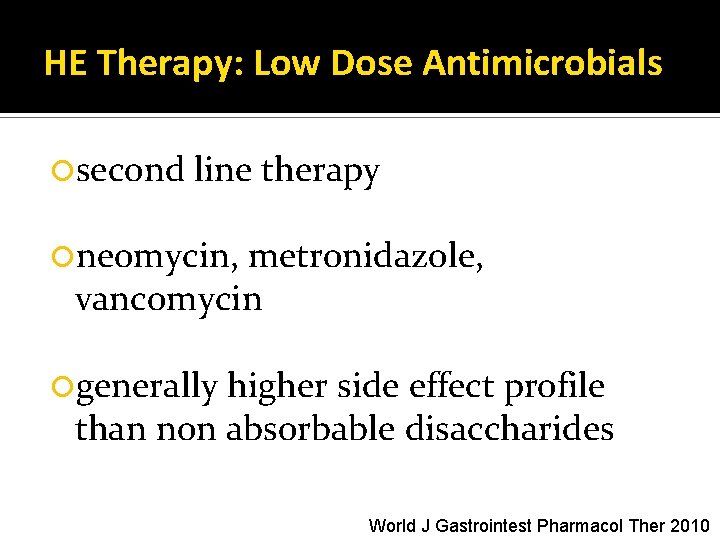
HE Therapy: Low Dose Antimicrobials second line therapy neomycin, metronidazole, vancomycin generally higher side effect profile than non absorbable disaccharides World J Gastrointest Pharmacol Ther 2010
HE Therapy: Rifaximin RCTs show at least as effective as lactulose, and low dose antimicrobials good side effect profile more RCTs still needed more expensive World J Gastrointest Pharmacol Ther 2010
HE Therapy: Flumazenil 27% improved vs 3% on placebo. Effective only in short term. 1 mg IV 6 RCTs show no difference in outcome of symptom improvement or mortality more studies needed World J Gastrointest Pharmacol Ther 2010
Thank you

References (1) Al-Khafaji A, Huang DT. Critical care management of patients with end-stage liver disease. Crit Care Med 2011 May; 39(5): 1157 -1166. (2) Amini M, Runyon BA. Alcoholic hepatitis 2010: a clinician's guide to diagnosis and therapy. World J Gastroenterol 2010 Oct 21; 16(39): 4905 -4912. (3) Arora R, Kathuria S, Jalandhara N. Acute renal dysfunction in patients with alcoholic hepatitis. World J Hepatol 2011 May 27; 3(5): 121 -124. (4) Basra G, Basra S, Parupudi S. Symptoms and signs of acute alcoholic hepatitis. World J Hepatol 2011 May 27; 3(5): 118 -120. (5) Bismuth M, Funakoshi N, Cadranel JF, Blanc P. Hepatic encephalopathy: from pathophysiology to therapeutic management. Eur J Gastroenterol Hepatol 2011 Jan; 23(1): 8 -22. (6) Brok J, Buckley N, Gluud C. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev 2009 Nov 08; (1)(1): CD 003328. (7) De Gasperi A, Corti A, Mazza E, Prosperi M, Amici O, Bettinelli L. Acute liver failure: managing coagulopathy and the bleeding diathesis. Transplant Proc 2009 May; 41(4): 1256 -1259. (8) Devictor D, Tissieres P, Afanetti M, Debray D. Acute liver failure in children. Clinics and Research in Hepatology and Gastroenterology 2011 6; 35(6– 7): 430 -437. (9) Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005 Feb 1; 172(3): 367 -379. (10) Hung OL, Kwon NS, Cole AE, Dacpano GR, Wu T, Chiang WK, et al. Evaluation of the physician's ability to recognize the presence or absence of anemia, fever, and jaundice. Acad Emerg Med 2000 Feb; 7(2): 146 -156. (11) Khashab M, Tector AJ, Kwo PY. Epidemiology of acute liver failure. Curr Gastroenterol Rep 2007 Mar; 9(1): 66 -73. (12) Li C, Martin BC. Trends in emergency department visits attributable to acetaminophen overdoses in the United States: 1993 -2007. Pharmacoepidemiol Drug Saf 2011 Aug; 20(8): 810 -818. (13) Ostapowicz G, Fontana RJ, Schiodt FV, Larson A, Davern TJ, Han SH, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002 Dec 17; 137(12): 947 -954. (14) Phongsamran PV, Kim JW, Cupo Abbott J, Rosenblatt A. Pharmacotherapy for hepatic encephalopathy. Drugs 2010 Jun 18; 70(9): 1131 -1148.
Refrences ( cont’d) (15) Polson J, Lee WM, American Association for the Study of Liver Disease. AASLD position paper: the management of acute liver failure. Hepatology 2005 May; 41(5): 1179 -1197. (16) Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: glucocorticosteroids for alcoholic hepatitis--a Cochrane Hepato-Biliary Group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther 2008 Jun; 27(12): 1167 -1178. (17) Riggio O, Ridola L, Pasquale C. Hepatic encephalopathy therapy: An overview. World J Gastrointest Pharmacol Ther 2010 Apr 6; 1(2): 54 -63. (18) Sheth M, Riggs M, Patel T. Utility of the Mayo End-Stage Liver Disease (MELD) score in assessing prognosis of patients with alcoholic hepatitis. BMC Gastroenterol 2002; 2: 2. (19) Singal AK, Duchini A. Liver transplantation in acute alcoholic hepatitis: Current status and future development. World J Hepatol 2011 Aug 27; 3(8): 215 -218. (20) Slack A, Wendon J. Acute liver failure. Clinical Medicine 2011 06; 11(3): 254 -258. (21) Srikureja W, Kyulo NL, Runyon BA, Hu KQ. MELD score is a better prognostic model than Child-Turcotte-Pugh score or Discriminant Function score in patients with alcoholic hepatitis. J Hepatol 2005 May; 42(5): 700 -706. (22) Sundaram V, Shaikh OS. Acute Liver Failure: Current Practice and Recent Advances. Gastroenterol Clin North Am 2011 9; 40(3): 523 -539. (23) Vaquero J, Blei AT. Etiology and management of fulminant hepatic failure. Curr Gastroenterol Rep 2003 Feb; 5(1): 39 -47. (24) Winger J, Michelfelder A. Diagnostic Approach to the Patient with Jaundice. Primary Care: Clinics in Office Practice 2011 9; 38(3): 469 -482.
Case 2 25 y. o. F returns from the Dominican Republic. Previously healthy. Feeling unwell x 1 wk with malaise N/V/D and now new onset jaundice
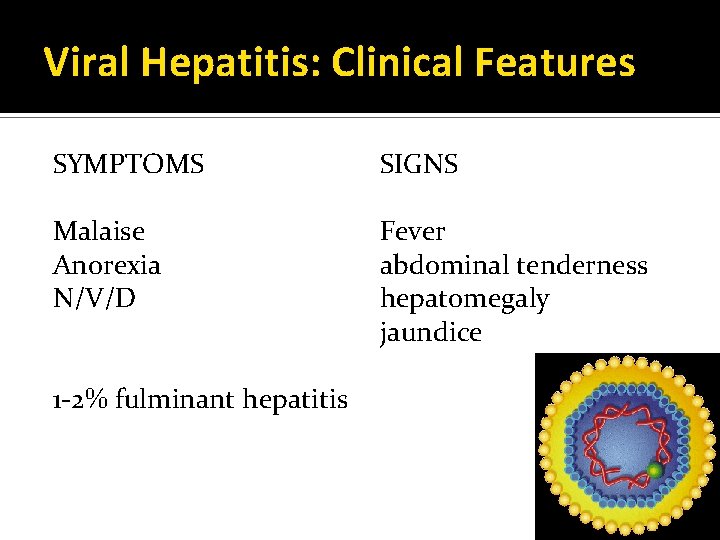
Viral Hepatitis: Clinical Features SYMPTOMS SIGNS Malaise Anorexia N/V/D Fever abdominal tenderness hepatomegaly jaundice 1 -2% fulminant hepatitis
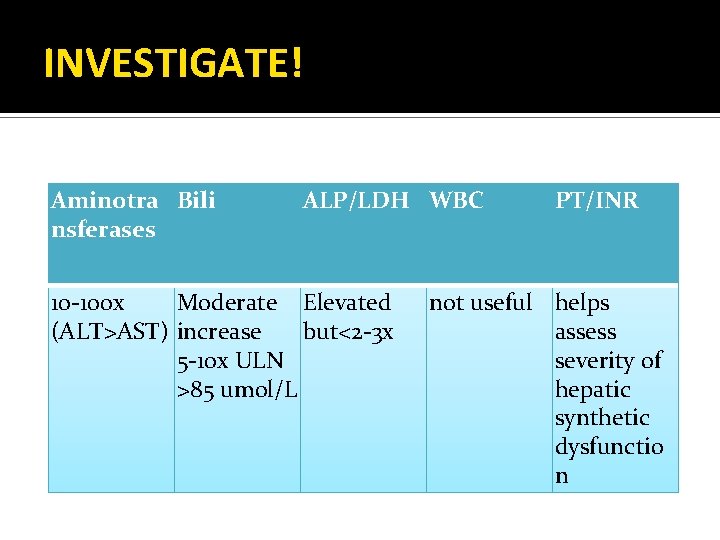
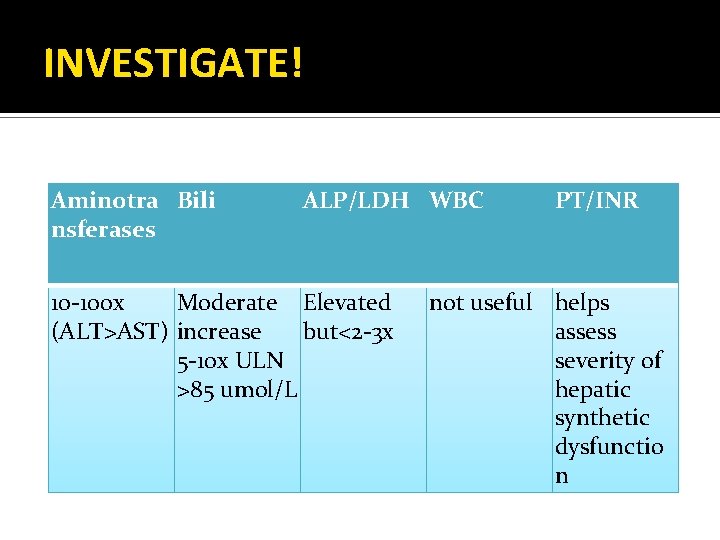
INVESTIGATE! Aminotra Bili nsferases ALP/LDH WBC 10 -100 x Moderate Elevated (ALT>AST) increase but<2 -3 x 5 -10 x ULN >85 umol/L PT/INR not useful helps assess severity of hepatic synthetic dysfunctio n
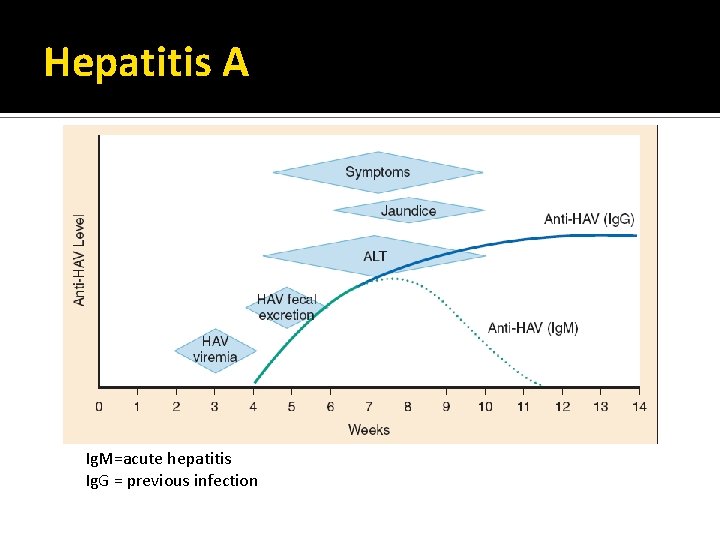
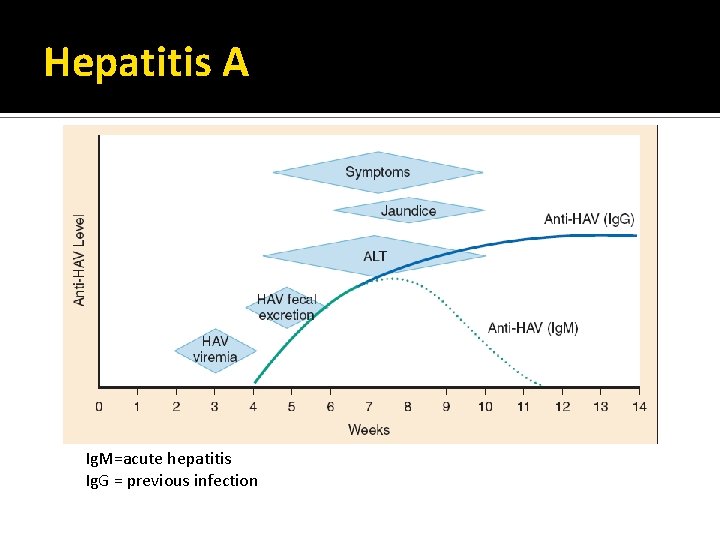
Hepatitis A Ig. M=acute hepatitis Ig. G = previous infection
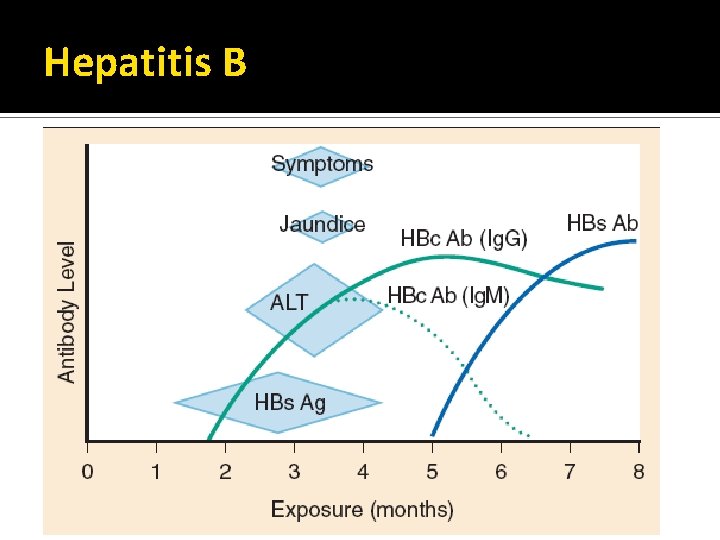
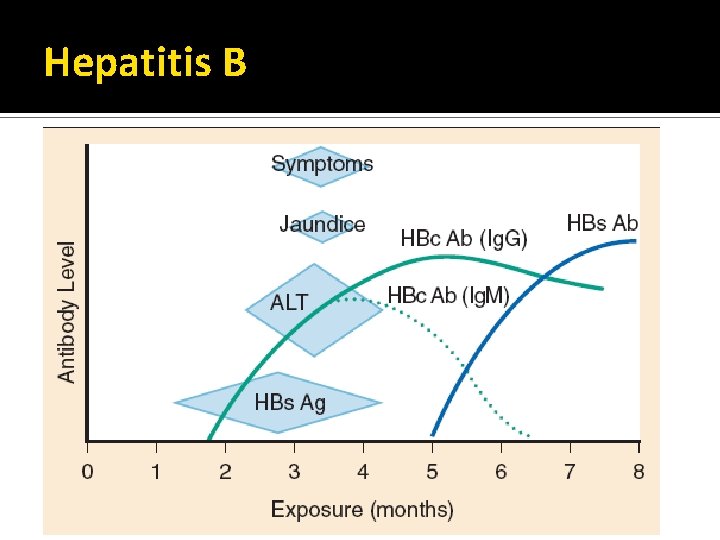
Hepatitis B
Hepatitis B Prodromal illness Arthralgia Arthritis (polyarticular) dermatitis
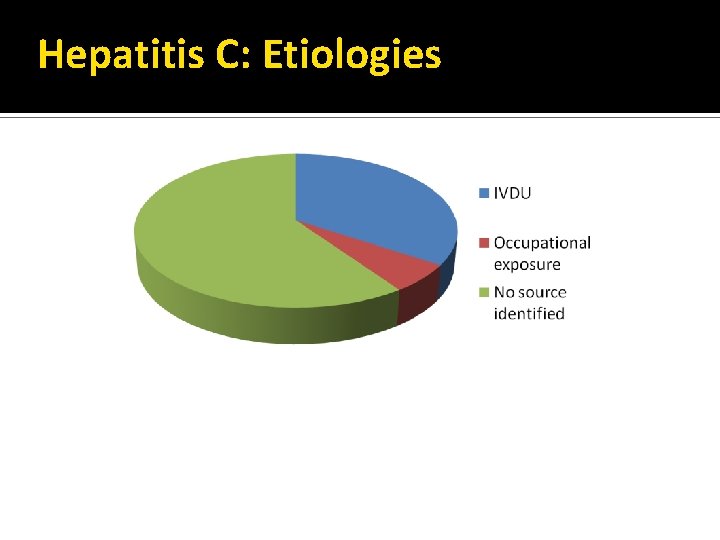
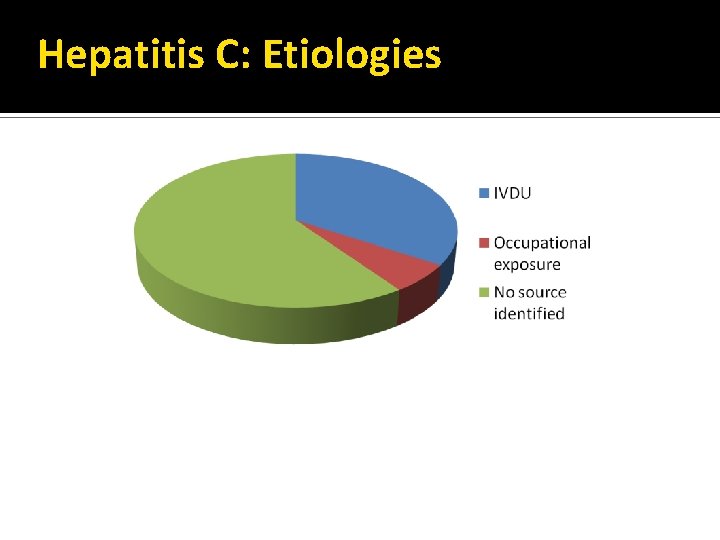
Hepatitis C: Etiologies
Viral Hepatitis-management Supportive correct fluids/lytes antiemetics Admit if supecting fulminant hepatitis Post Exposure Prophylaxis
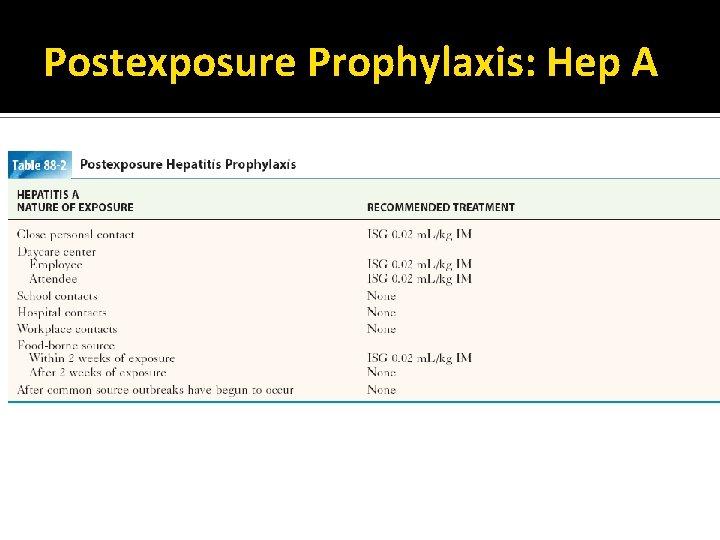
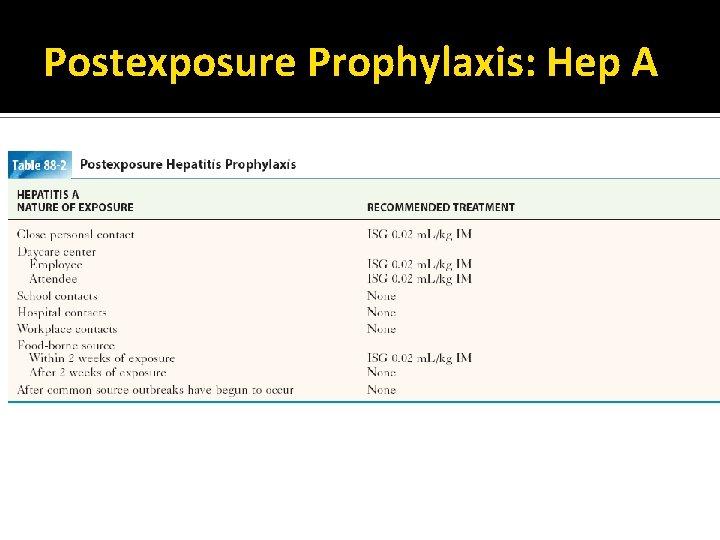
Postexposure Prophylaxis: Hep A
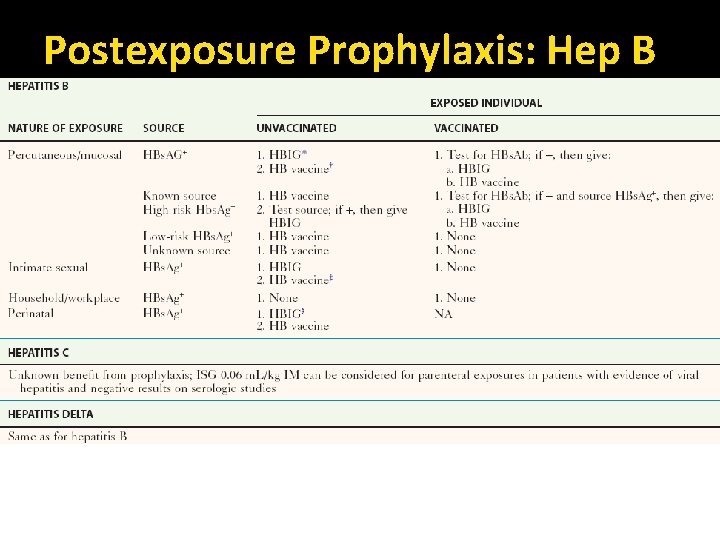
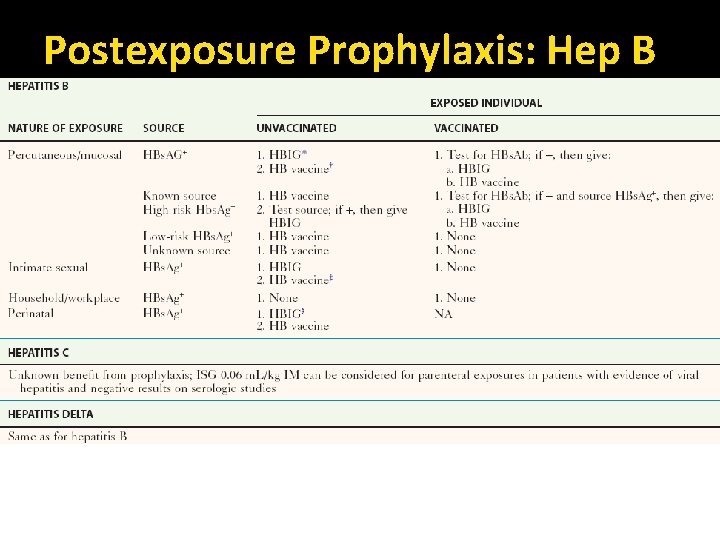
Postexposure Prophylaxis: Hep B
Viral Hepatitis: Reporting Hep A: confirmed and probable call Medical Officer of Health Hep B/C: confirmed acute and probable report to Communicable Disease Unit
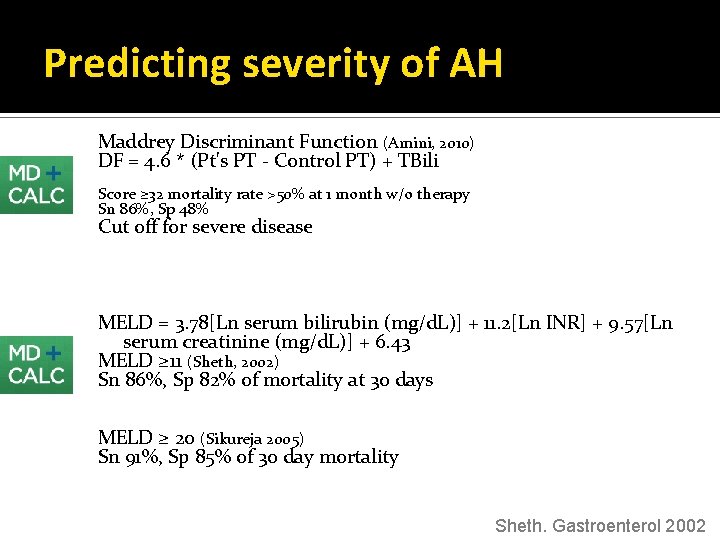
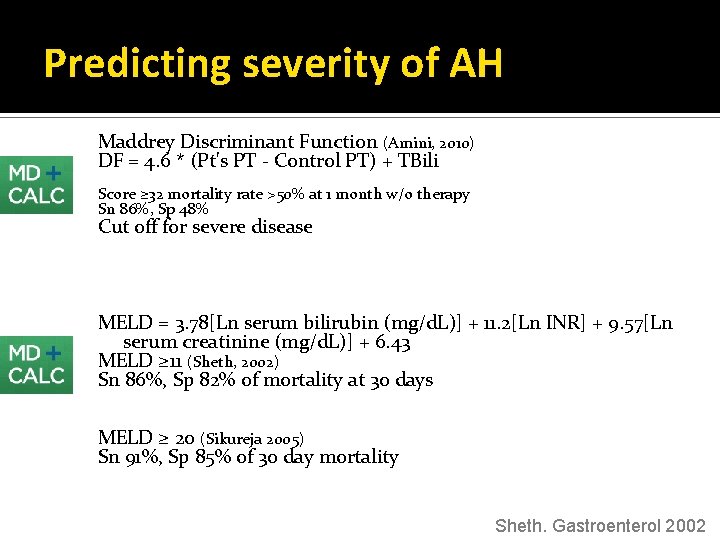
Predicting severity of AH Maddrey Discriminant Function (Amini, 2010) DF = 4. 6 * (Pt's PT - Control PT) + TBili Score ≥ 32 mortality rate >50% at 1 month w/o therapy Sn 86%, Sp 48% Cut off for severe disease MELD = 3. 78[Ln serum bilirubin (mg/d. L)] + 11. 2[Ln INR] + 9. 57[Ln serum creatinine (mg/d. L)] + 6. 43 MELD ≥ 11 (Sheth, 2002) Sn 86%, Sp 82% of mortality at 30 days MELD ≥ 20 (Sikureja 2005) Sn 91%, Sp 85% of 30 day mortality Sheth. Gastroenterol 2002
 Obstructive jaundice vs hemolytic jaundice
Obstructive jaundice vs hemolytic jaundice Alkaline phosphatase level in children
Alkaline phosphatase level in children Gastroenterology board review
Gastroenterology board review Stigmata of chronic liver disease
Stigmata of chronic liver disease Complications of cirrhosis
Complications of cirrhosis Elisabetta bugianesi
Elisabetta bugianesi Cld vs dcld
Cld vs dcld Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease How to diagnose liver disease
How to diagnose liver disease Stage 1 cirrhosis
Stage 1 cirrhosis Gennifer shafer liver disease
Gennifer shafer liver disease Alcoholic liver disease
Alcoholic liver disease Infiltrative liver disease
Infiltrative liver disease Suma wieku ani i oli wynosi 22 lata
Suma wieku ani i oli wynosi 22 lata Akt ślubowania nauczyciela mianowanego wzór
Akt ślubowania nauczyciela mianowanego wzór Kasia kamuda
Kasia kamuda Kasia muldner
Kasia muldner Pazdro
Pazdro Kasia kostun
Kasia kostun Kasia matysiak
Kasia matysiak Bharathi viswanathan
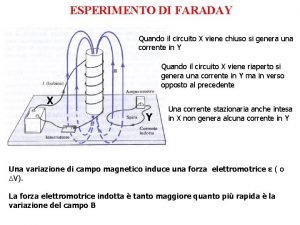
Bharathi viswanathan Legge di lenz spiegazione
Legge di lenz spiegazione State lenz law
State lenz law What is induction in physics
What is induction in physics Costante dielettrica
Costante dielettrica Ley de lenz
Ley de lenz Faraday's law vs lenz's law
Faraday's law vs lenz's law Magnetic field strength
Magnetic field strength Efectul electrochimic
Efectul electrochimic Lenz law
Lenz law Lenz rule
Lenz rule Indukci
Indukci Leyes de ohm, kirchoff, lenz, faraday y watt
Leyes de ohm, kirchoff, lenz, faraday y watt Irraggiamento
Irraggiamento Heinrich f.e. lenz
Heinrich f.e. lenz Lenz’s law
Lenz’s law Lenz law
Lenz law Lenz’s law
Lenz’s law Claus
Claus Regra do tapa fisica
Regra do tapa fisica Legge di faraday lenz
Legge di faraday lenz Ostern wenn der lenz erwacht
Ostern wenn der lenz erwacht Wet van lenz
Wet van lenz Michael faraday menyatakan bahwa
Michael faraday menyatakan bahwa Zeitraffung
Zeitraffung Intrahepatic jaundice
Intrahepatic jaundice Sonal pruthi
Sonal pruthi Types of jaundice
Types of jaundice Classification of jaundice
Classification of jaundice Obstructive jaundice differential diagnosis
Obstructive jaundice differential diagnosis Phototherapy unit
Phototherapy unit Jaundice classification
Jaundice classification Acholia causes
Acholia causes Benjamin classification of obstructive jaundice
Benjamin classification of obstructive jaundice Hyperbilirubinemia workup
Hyperbilirubinemia workup Differential diagnosis of jaundice in pediatrics
Differential diagnosis of jaundice in pediatrics Bhutani nomogram
Bhutani nomogram Pathologic jaundice
Pathologic jaundice Pathological jaundice workup
Pathological jaundice workup Jaundice graph
Jaundice graph Pathologic jaundice
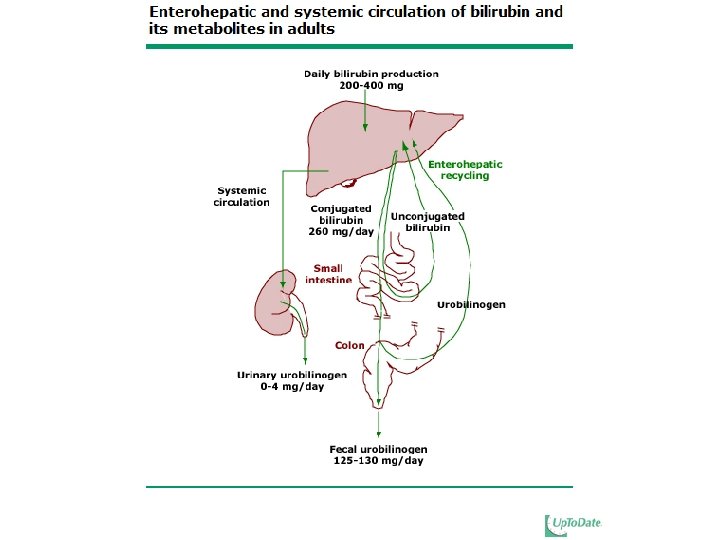
Pathologic jaundice Bilirubin production
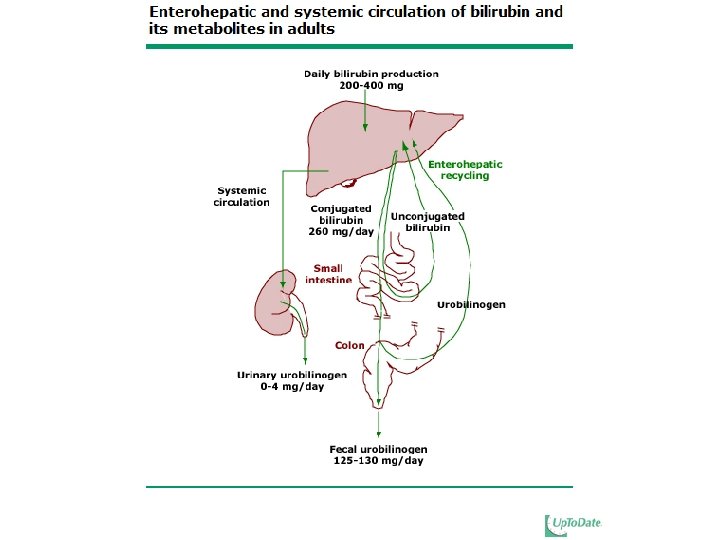
Bilirubin production Type of jaundice
Type of jaundice Intrahepatic jaundice
Intrahepatic jaundice Prehepatic jaundice
Prehepatic jaundice Pathologic jaundice
Pathologic jaundice Types of jaundice
Types of jaundice Post hepatic jaundice
Post hepatic jaundice Bilirubin pathway
Bilirubin pathway