Antipsychotic drugs Phenothiazines Aliphatic side chain Chlorpromazine Triflupromazine

- Slides: 41
Antipsychotic drugs
Phenothiazines Aliphatic side chain: -Chlorpromazine -Triflupromazine Piperidine side chain: -Thioridazine Piperazine side chain: -Trifluoperazine -Fluphenazine
Butyrophenones -Haloperidol -Trifluperidol -Penfluridol Thioxanthenes -Flupenthixol Other heterocyclics -Pimozide, Loxapine
• Atypical antipsychotics -Clozapine -Risperidone -Olanzapine -Quetiapine -Aripiprazole -Ziprasidone
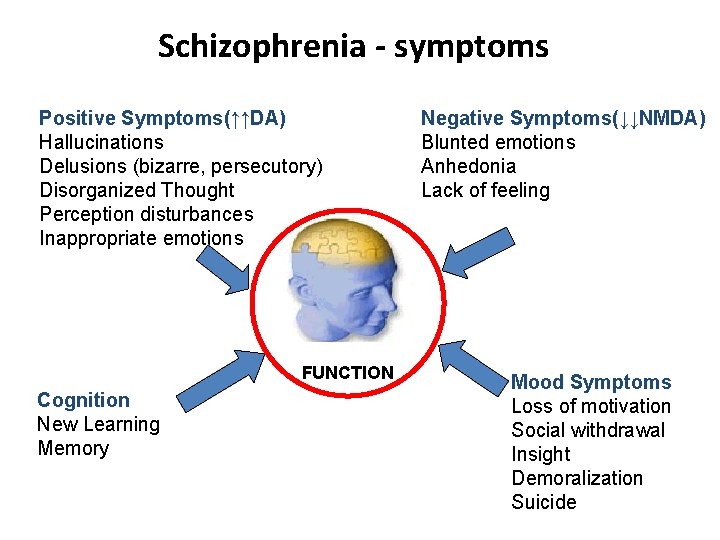
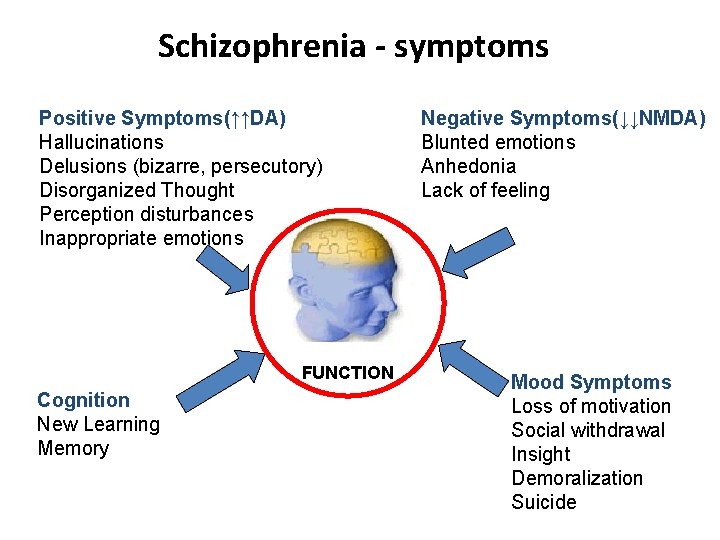
Schizophrenia - symptoms Positive Symptoms(↑↑DA) Hallucinations Delusions (bizarre, persecutory) Disorganized Thought Perception disturbances Inappropriate emotions FUNCTION Cognition New Learning Memory Negative Symptoms(↓↓NMDA) Blunted emotions Anhedonia Lack of feeling Mood Symptoms Loss of motivation Social withdrawal Insight Demoralization Suicide
• Positive/active symptoms include thought disturbances, delusions, hallucinations • Negative/passive symptoms include social withdrawal, loss of drive, diminished affect, paucity of speech. impaired personal hygiene
Prognosis of Schizophrenia • 10% continuous hospitalization • < 30% recovery = symptom-free for 5 years • 60% continued problems in living/episodic periods
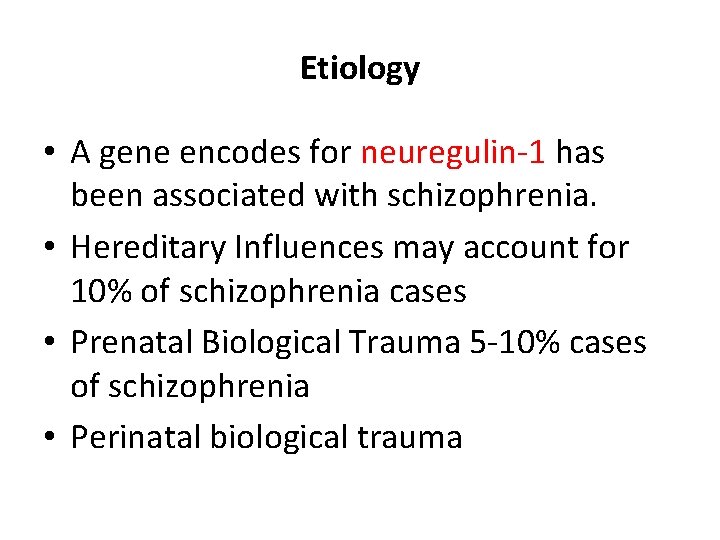
Etiology • A gene encodes for neuregulin-1 has been associated with schizophrenia. • Hereditary Influences may account for 10% of schizophrenia cases • Prenatal Biological Trauma 5 -10% cases of schizophrenia • Perinatal biological trauma
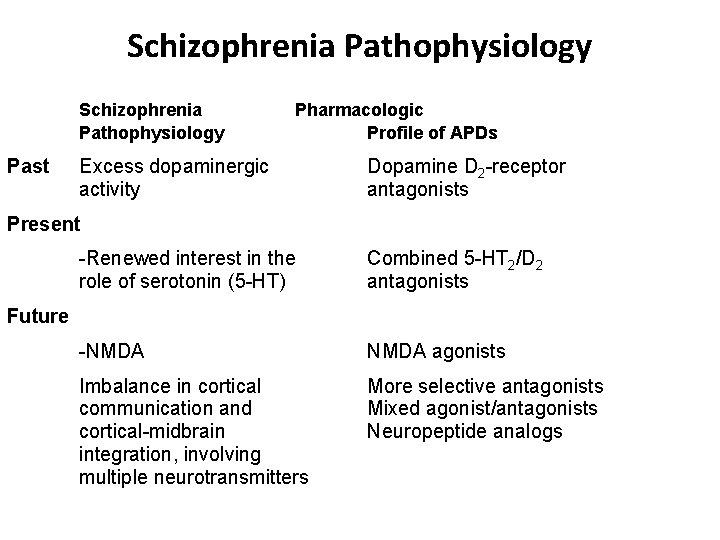
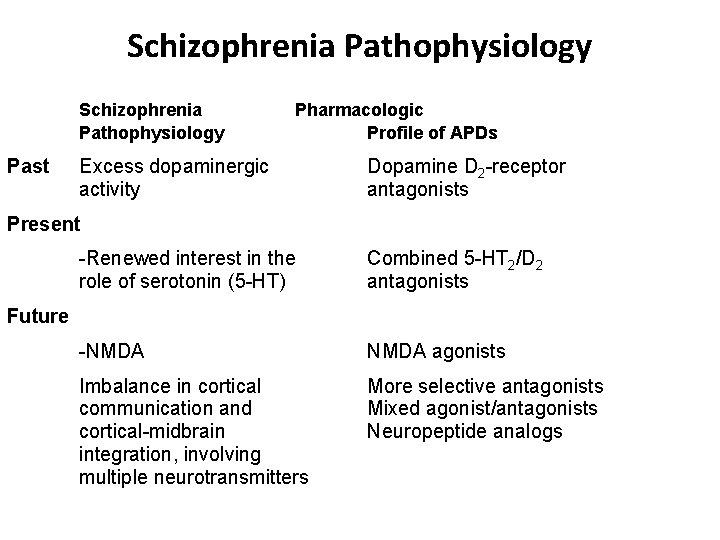
Schizophrenia Pathophysiology Past Pharmacologic Profile of APDs Excess dopaminergic activity Dopamine D 2 -receptor antagonists Present -Renewed interest in the role of serotonin (5 -HT) Combined 5 -HT 2/D 2 antagonists -NMDA agonists Imbalance in cortical communication and cortical-midbrain integration, involving multiple neurotransmitters More selective antagonists Mixed agonist/antagonists Neuropeptide analogs Future
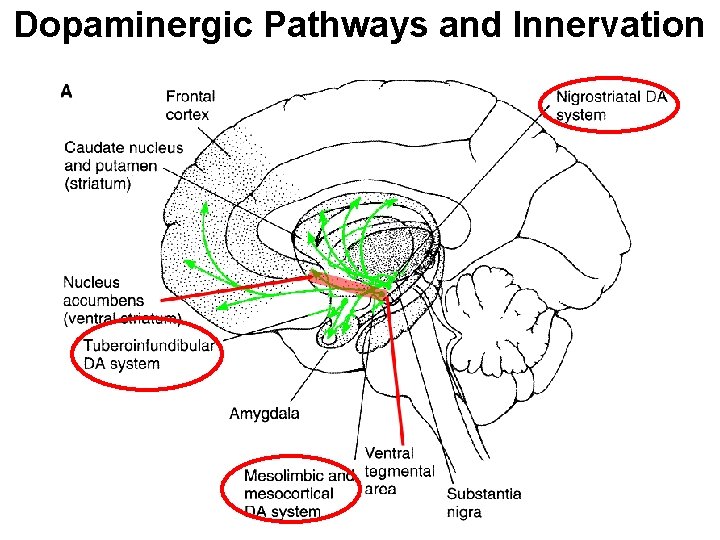
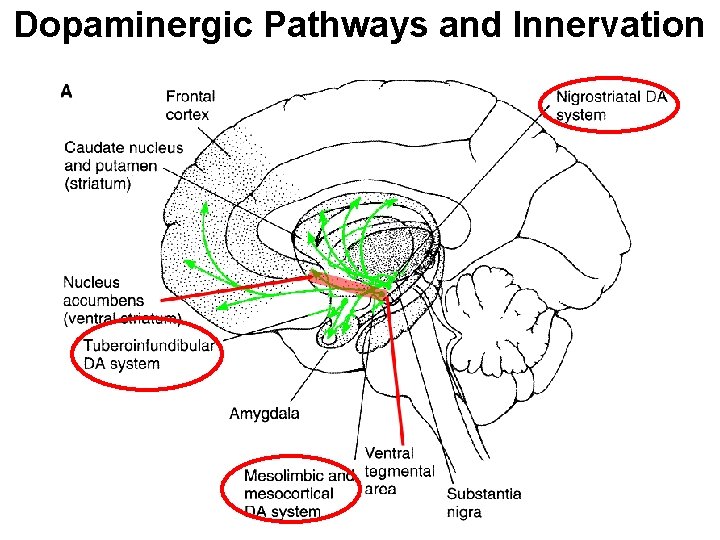
Dopaminergic Pathways and Innervation

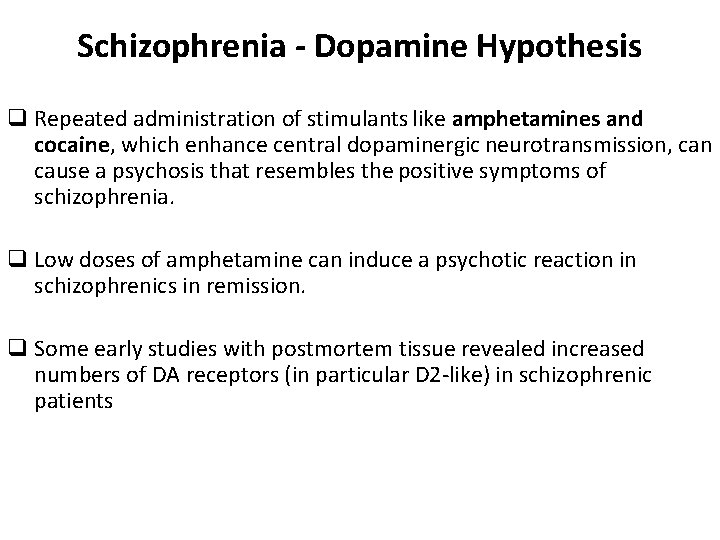
Schizophrenia - Dopamine Hypothesis q Repeated administration of stimulants like amphetamines and cocaine, which enhance central dopaminergic neurotransmission, can cause a psychosis that resembles the positive symptoms of schizophrenia. q Low doses of amphetamine can induce a psychotic reaction in schizophrenics in remission. q Some early studies with postmortem tissue revealed increased numbers of DA receptors (in particular D 2 -like) in schizophrenic patients
Serotonin Hypothesis of Schizophrenia • Hallucinogens such as LSD (lysergic acid diethylamide) and mescaline are serotonin (5 -HT) agonists • 5 -HT 2 A-receptor blockade is a key factor in the mechanism of action of the main class of atypical antipsychotic drugs such as clozapine and quetiapine. • 5 -HT 2 A-receptor modulate the release of dopamine in the cortex, limbic region, and striatum.
Schizophrenia - Glutamate Hypothesis • Preclinical as well as clinical studies provide evidence of hypofunction of NMDA receptors as a primary, or at least, a contributory process in the pathophysiology of schizophrenia • Several clinical trials with agents that act at the glycine modulatory site on the NMDA receptor have revealed consistent reductions in negative symptoms and variable effects of cognitive and positive symptoms • These studies also provide evidence that suggests the effects of clozapine on negative symptoms and cognition may be through activation of the glycine modulatory site on the NMDA receptor.
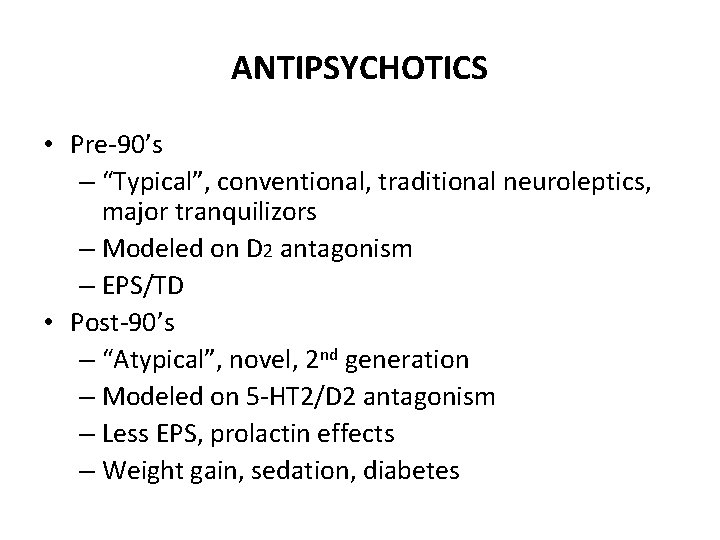
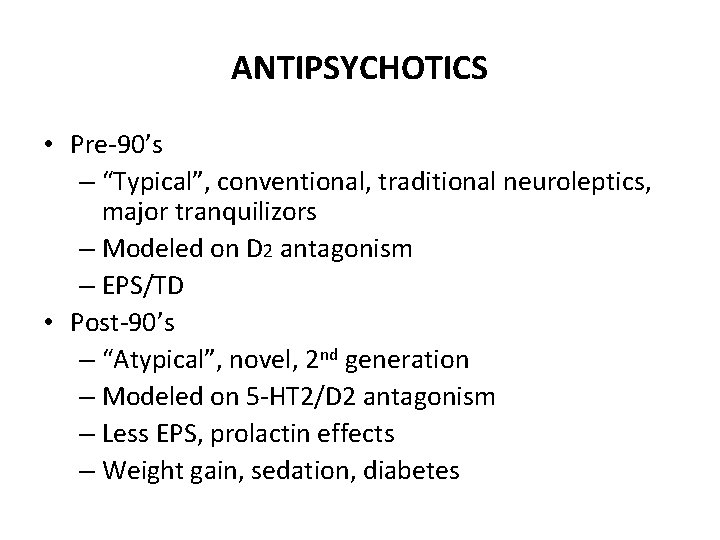
ANTIPSYCHOTICS • Pre-90’s – “Typical”, conventional, traditional neuroleptics, major tranquilizors – Modeled on D 2 antagonism – EPS/TD • Post-90’s – “Atypical”, novel, 2 nd generation – Modeled on 5 -HT 2/D 2 antagonism – Less EPS, prolactin effects – Weight gain, sedation, diabetes
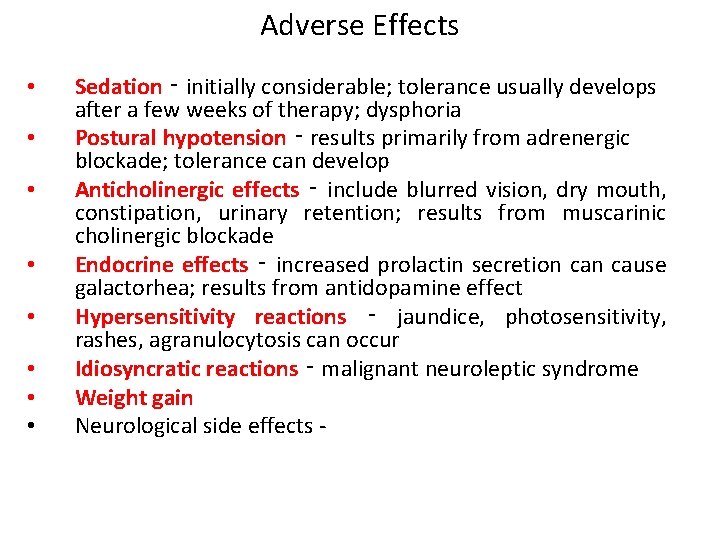
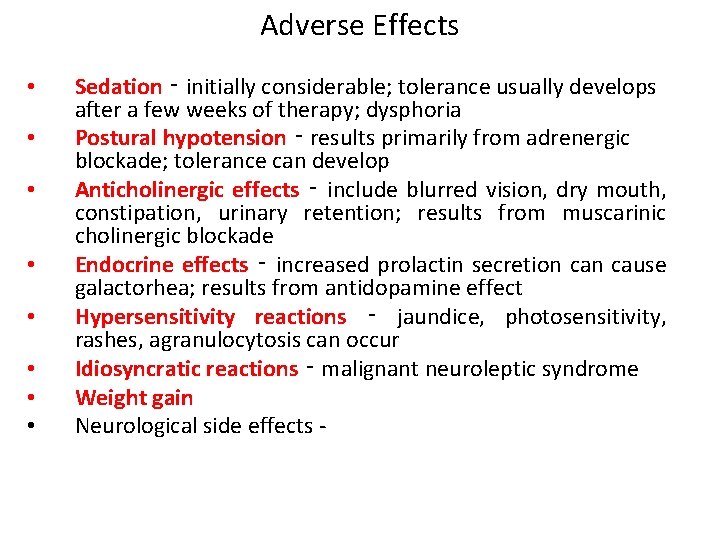
Adverse Effects • • Sedation ‑ initially considerable; tolerance usually develops after a few weeks of therapy; dysphoria Postural hypotension ‑ results primarily from adrenergic blockade; tolerance can develop Anticholinergic effects ‑ include blurred vision, dry mouth, constipation, urinary retention; results from muscarinic cholinergic blockade Endocrine effects ‑ increased prolactin secretion cause galactorhea; results from antidopamine effect Hypersensitivity reactions ‑ jaundice, photosensitivity, rashes, agranulocytosis can occur Idiosyncratic reactions ‑ malignant neuroleptic syndrome Weight gain Neurological side effects -
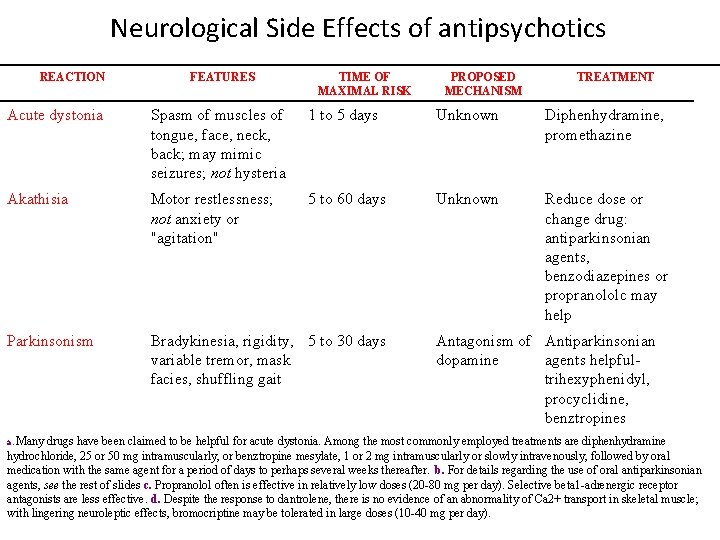
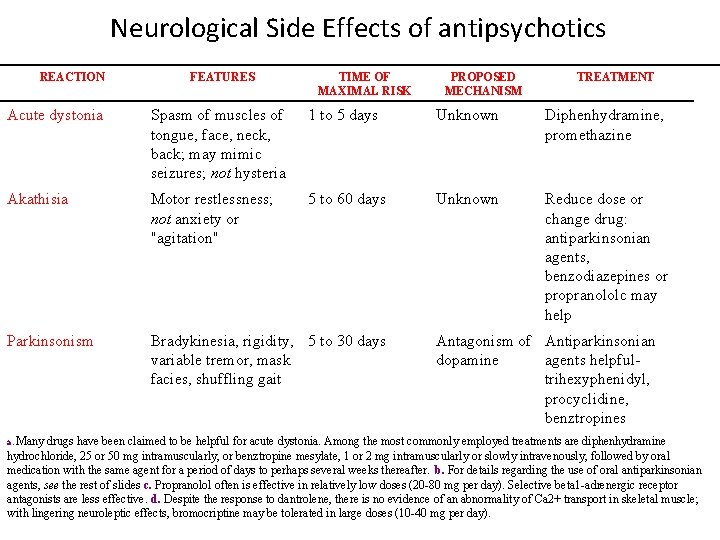
Neurological Side Effects of antipsychotics REACTION FEATURES TIME OF MAXIMAL RISK PROPOSED MECHANISM TREATMENT Acute dystonia Spasm of muscles of tongue, face, neck, back; may mimic seizures; not hysteria 1 to 5 days Unknown Diphenhydramine, promethazine Akathisia Motor restlessness; not anxiety or "agitation" 5 to 60 days Unknown Reduce dose or change drug: antiparkinsonian agents, benzodiazepines or propranololc may help Parkinsonism Bradykinesia, rigidity, 5 to 30 days variable tremor, mask facies, shuffling gait a. Many Antagonism of Antiparkinsonian dopamine agents helpfultrihexyphenidyl, procyclidine, benztropines drugs have been claimed to be helpful for acute dystonia. Among the most commonly employed treatments are diphenhydramine hydrochloride, 25 or 50 mg intramuscularly, or benztropine mesylate, 1 or 2 mg intramuscularly or slowly intravenously, followed by oral medication with the same agent for a period of days to perhaps several weeks thereafter. b. For details regarding the use of oral antiparkinsonian agents, see the rest of slides c. Propranolol often is effective in relatively low doses (20 -80 mg per day). Selective beta 1 -adrenergic receptor antagonists are less effective. d. Despite the response to dantrolene, there is no evidence of an abnormality of Ca 2+ transport in skeletal muscle; with lingering neuroleptic effects, bromocriptine may be tolerated in large doses (10 -40 mg per day).
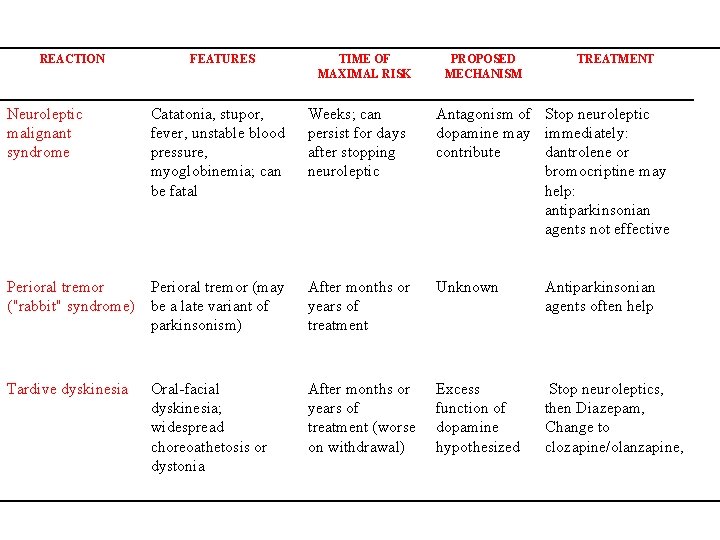
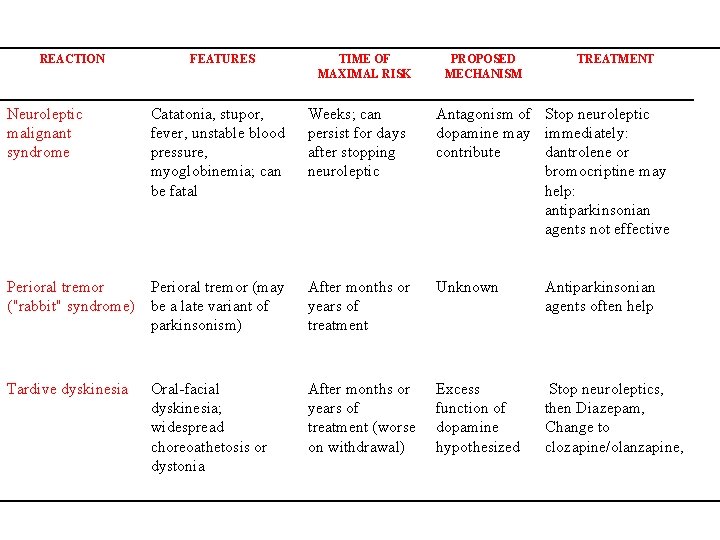
REACTION Neuroleptic malignant syndrome FEATURES TIME OF MAXIMAL RISK PROPOSED MECHANISM TREATMENT Catatonia, stupor, fever, unstable blood pressure, myoglobinemia; can be fatal Weeks; can persist for days after stopping neuroleptic Antagonism of Stop neuroleptic dopamine may immediately: contribute dantrolene or bromocriptine may help: antiparkinsonian agents not effective Perioral tremor (may ("rabbit" syndrome) be a late variant of parkinsonism) After months or years of treatment Unknown Antiparkinsonian agents often help Tardive dyskinesia After months or years of treatment (worse on withdrawal) Excess function of dopamine hypothesized Stop neuroleptics, then Diazepam, Change to clozapine/olanzapine, Oral-facial dyskinesia; widespread choreoathetosis or dystonia
Adverse Effects - EPS Details on two main extrapyramidal disturbances (EPS): • Parkinson-like symptoms – tremor, rigidity – direct consequence of block of nigrostriatal DA 2 R – reversible upon cessation of antipsychotics • Tardive dyskinesia • • involuntary movement of face and limbs less likely with atypical antipsychotics (AP) appears months or years after start of AP ? result of proliferation of DA R in striatum » presynaptic? • treatment is generally unsuccessful
Weight gain – 40% - weight gain now attributed to ratio of binding to D 2 and 5 -HT 2 receptors; possibly also histamine (for newer antipsychotics anyway) Sexual dysfunction • result from NE and SE blockade • erectile dysfunction in 23 -54% of men • retrograde ejaculation in • loss of libido and anorgasmia in men and women Seizures - <1% for generalized grand mal
Neuroleptic malignant syndrome (1 -2% early in trt) • combination of motor rigidity, hyperthermia, and autonomic dysregulation of blood pressure and heart rate (both go up) • can be fatal in 5 -20% of cases if untreated • treatment – discontinue meds; give trts for fever and cardiac problems
Sensitivity to sun • some phenothiazines collect in skin (chlorpromazine) • sunlight causes pigmentation changes – grayishpurple (look bruised) • in eye, brown cornea, brownish cloud to vision and possibly permanent impairment Agranulocytosis - <1% (with clozapine) • reduced white blood cell count • lowered resistance to infection • can be fatal Jaundice – elevated bilirubin in liver - < ½%
Limitations Of Conventional Antipsychotics Approximately one-third of patients with schizophrenia fail to respond Limited efficacy against Negative symptoms Affective symptoms Cognitive deficits High proportion of patients relapse Side effects and compliance issues
Antipsychotic Drugs – New Generations “atypical” About 40 -60% do not respond to phenothiazines or cannot handle side effects • Questions remain about the efficacy of phenothiazines and haloperidole for negative symptoms • Drugs needed that are low in extrapyramidal side effects and at least equal in efficacy for positive symptoms, perhaps better for negative
Antipsychotic Drugs – New Generations “atypical” • • clozapine risperidone olanzapine sertindole Quetiapine Aripiprazole Ziprasidone
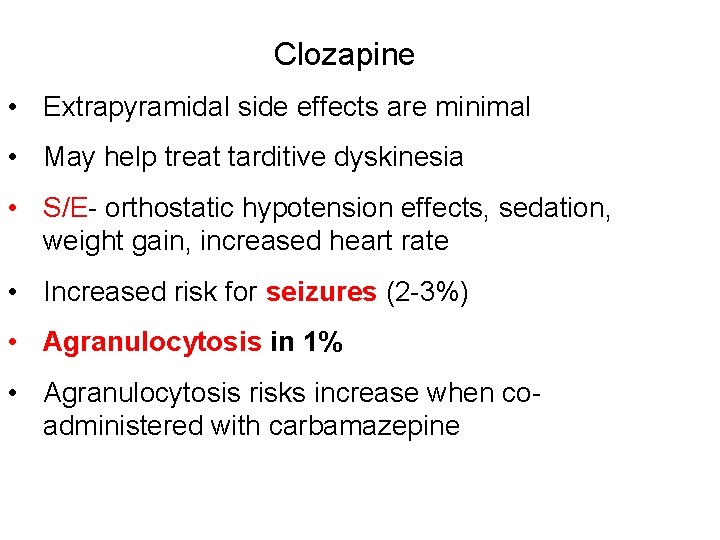
Clozapine (1989) • Selectively blocks dopamine D 2 receptors, avoiding nigrostriatal pathway • α-blockade • Also blocks H 1 • More strongly blocks 5 -HT 2 receptors in cortex which then acts to modulate some dopamine activity • Among non-responders to first generation meds or those who cannot tolerate side effects, about 30% do respond to Clozapine
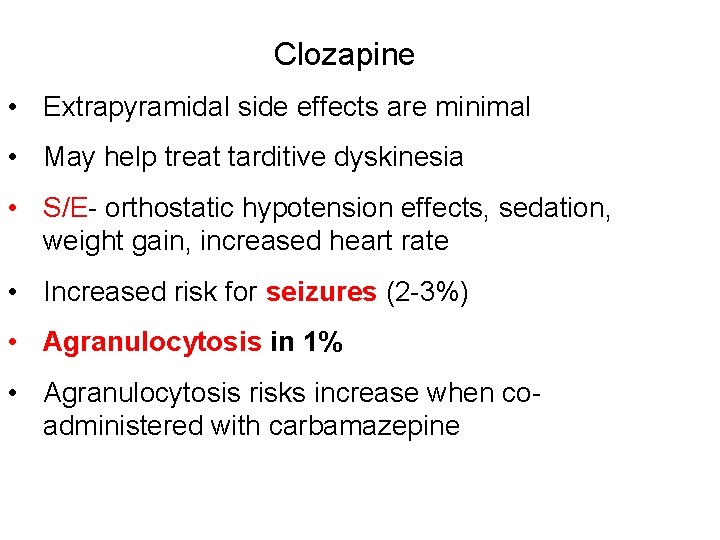
Clozapine • Extrapyramidal side effects are minimal • May help treat tarditive dyskinesia • S/E- orthostatic hypotension effects, sedation, weight gain, increased heart rate • Increased risk for seizures (2 -3%) • Agranulocytosis in 1% • Agranulocytosis risks increase when coadministered with carbamazepine
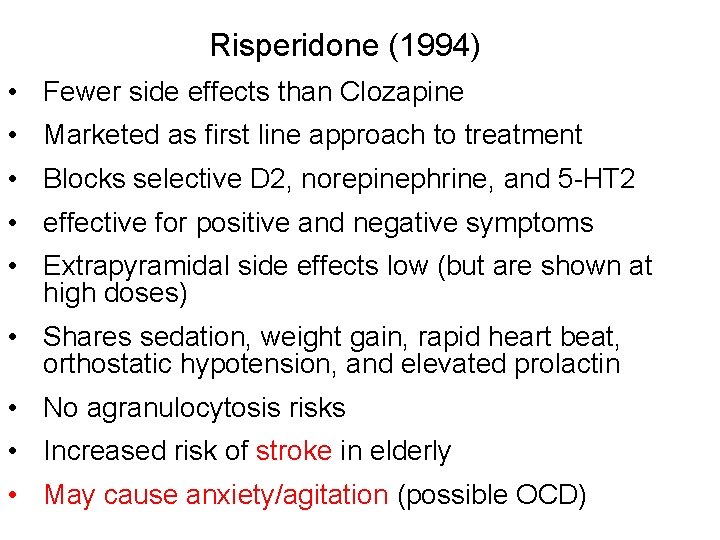
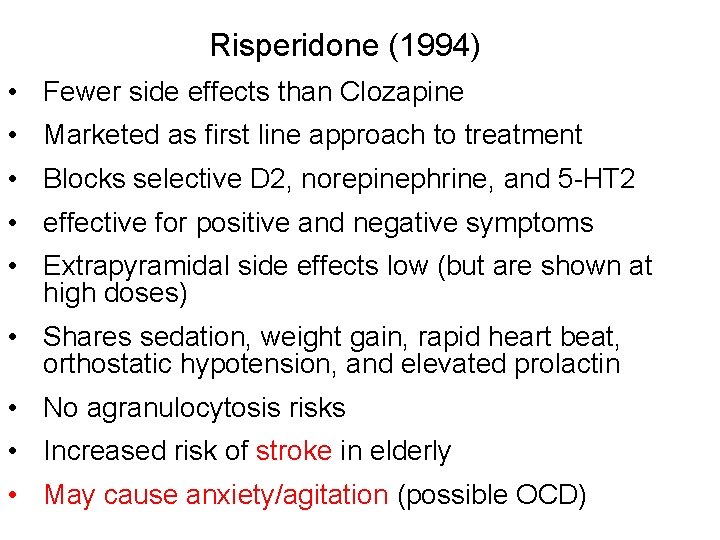
Risperidone (1994) • Fewer side effects than Clozapine • Marketed as first line approach to treatment • Blocks selective D 2, norepinephrine, and 5 -HT 2 • effective for positive and negative symptoms • Extrapyramidal side effects low (but are shown at high doses) • Shares sedation, weight gain, rapid heart beat, orthostatic hypotension, and elevated prolactin • No agranulocytosis risks • Increased risk of stroke in elderly • May cause anxiety/agitation (possible OCD)
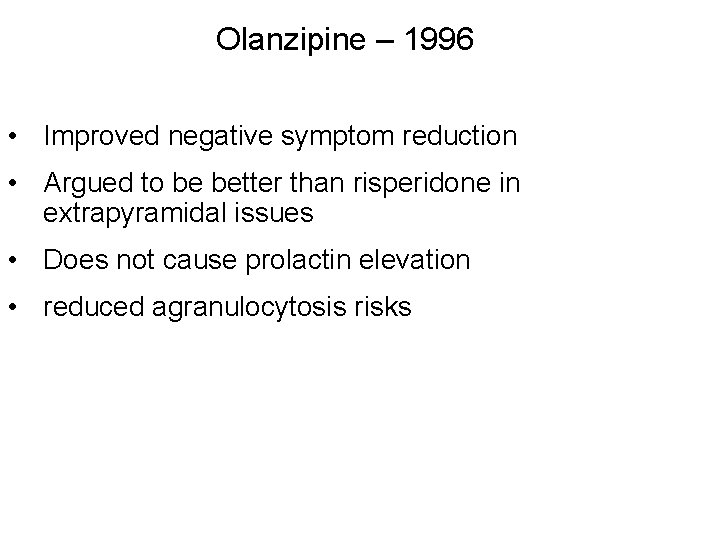
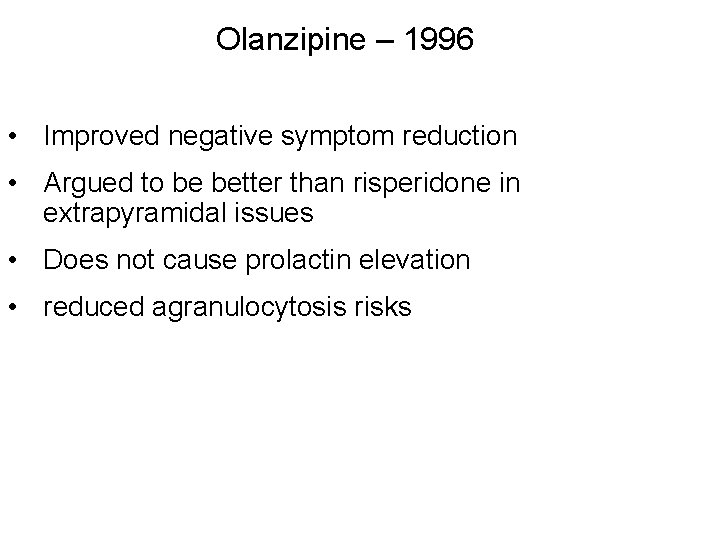
Olanzipine – 1996 • Improved negative symptom reduction • Argued to be better than risperidone in extrapyramidal issues • Does not cause prolactin elevation • reduced agranulocytosis risks
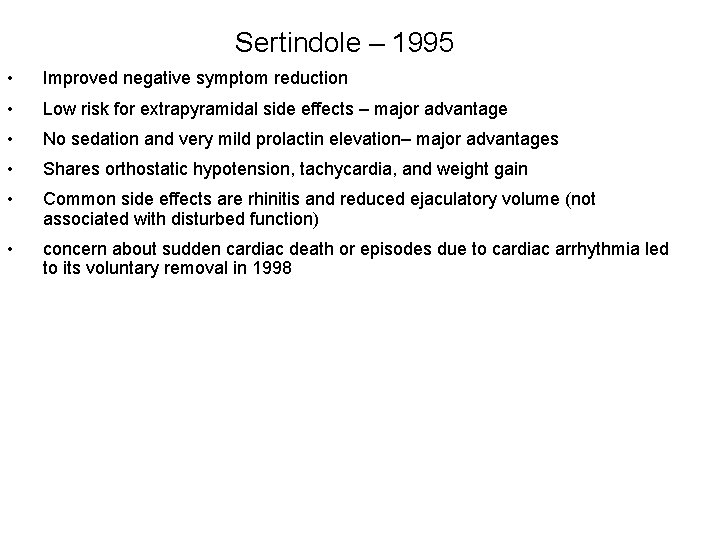
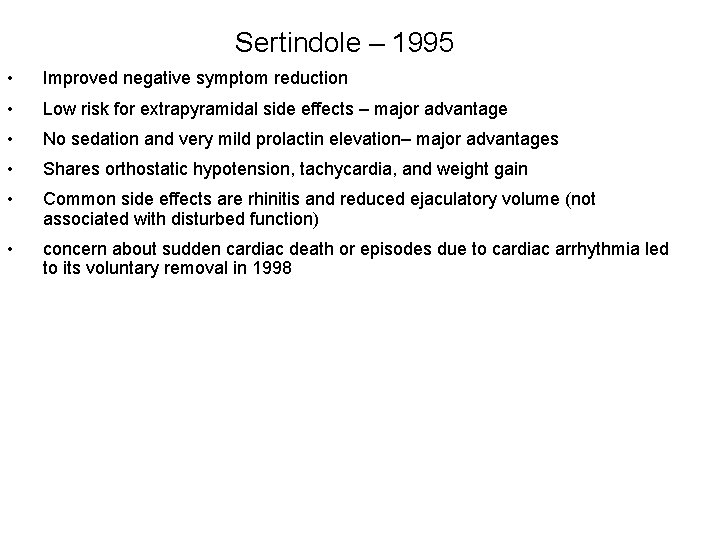
Sertindole – 1995 • Improved negative symptom reduction • Low risk for extrapyramidal side effects – major advantage • No sedation and very mild prolactin elevation– major advantages • Shares orthostatic hypotension, tachycardia, and weight gain • Common side effects are rhinitis and reduced ejaculatory volume (not associated with disturbed function) • concern about sudden cardiac death or episodes due to cardiac arrhythmia led to its voluntary removal in 1998
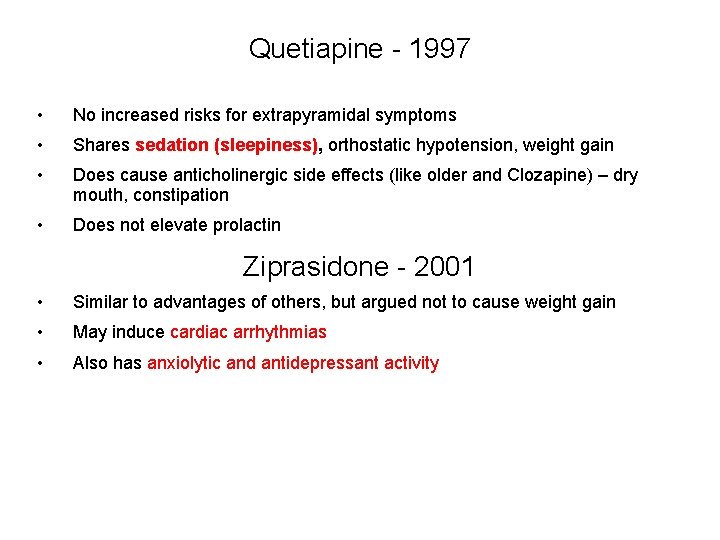
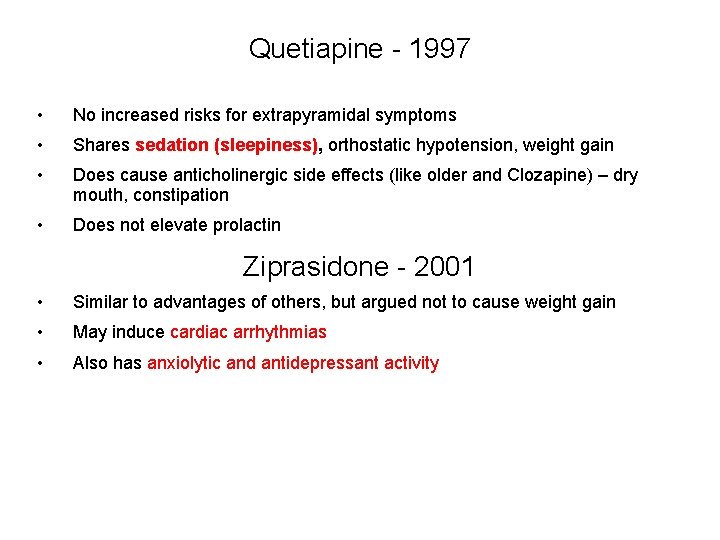
Quetiapine - 1997 • No increased risks for extrapyramidal symptoms • Shares sedation (sleepiness), orthostatic hypotension, weight gain • Does cause anticholinergic side effects (like older and Clozapine) – dry mouth, constipation • Does not elevate prolactin Ziprasidone - 2001 • Similar to advantages of others, but argued not to cause weight gain • May induce cardiac arrhythmias • Also has anxiolytic and antidepressant activity
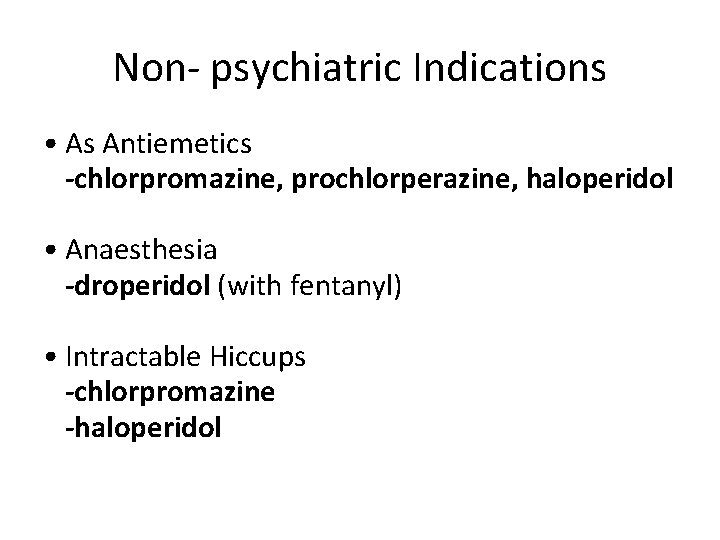
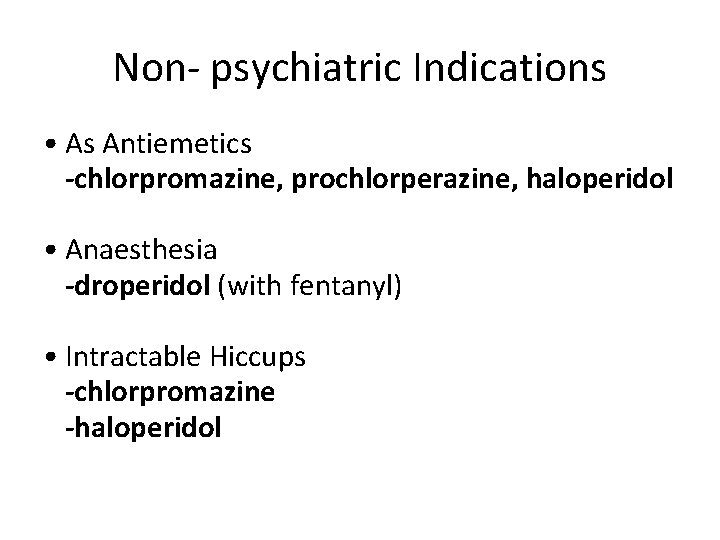
Non- psychiatric Indications • As Antiemetics -chlorpromazine, prochlorperazine, haloperidol • Anaesthesia -droperidol (with fentanyl) • Intractable Hiccups -chlorpromazine -haloperidol
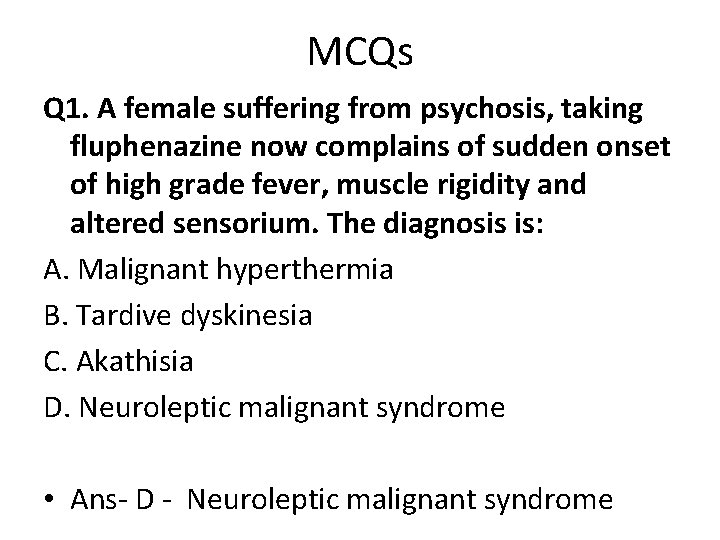
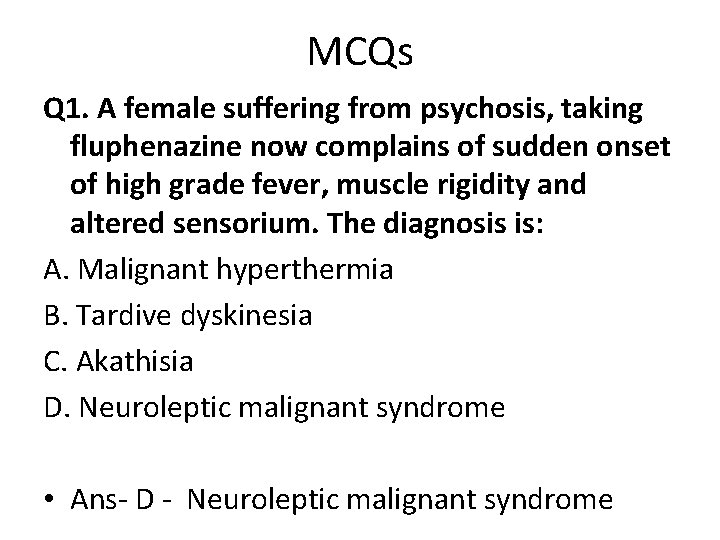
MCQs Q 1. A female suffering from psychosis, taking fluphenazine now complains of sudden onset of high grade fever, muscle rigidity and altered sensorium. The diagnosis is: A. Malignant hyperthermia B. Tardive dyskinesia C. Akathisia D. Neuroleptic malignant syndrome • Ans- D - Neuroleptic malignant syndrome
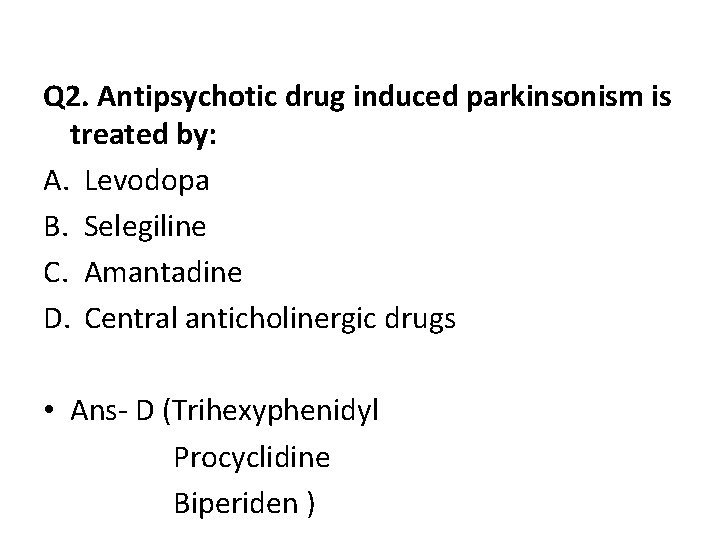
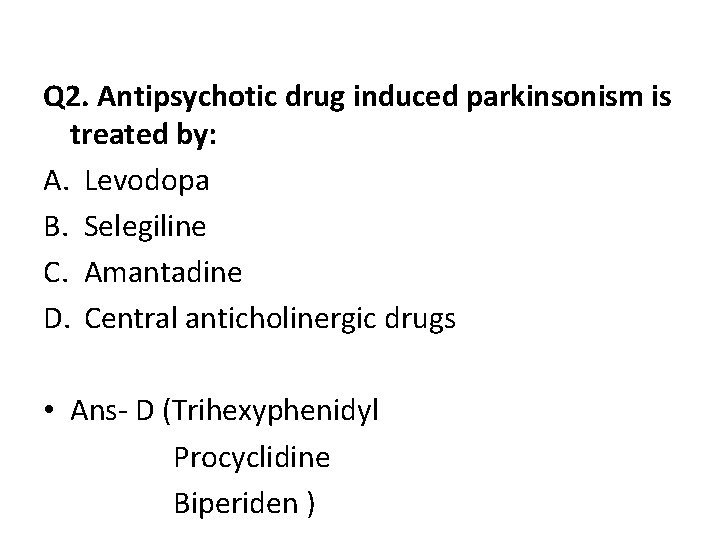
Q 2. Antipsychotic drug induced parkinsonism is treated by: A. Levodopa B. Selegiline C. Amantadine D. Central anticholinergic drugs • Ans- D (Trihexyphenidyl Procyclidine Biperiden )
Q 3. Least extrapyramidal side effects are seen with: A. Clozapine B. Haloperidol C. Trifluoperazine D. Chlorpromazine • Ans- A- Clozapine
Q 4. Risperidone is associated with the risk of: A. Cerebrovascular accidents B. Agranulocytosis C. Diabetes Insipidus D. Gout • Ans- A - Cerebrovascular accidents
Q 5. The antipsychotic drug that can also be used as antiemetics: A. chlorpromazine B. Clozapine C. Aripiprazole D. Loxapine • Ans- A - chlorpromazine
Q 6. The antipsychotics that can also be used as anaesthetic drug: A. Chlorpromazine B. Penfluridol C. Clozapine D. Droperidol • Ans- D - Droperidol
Q 7. The antipsychotic drug that can also be used to treat Intractable Hiccups: A. Clozapine B. Chlorpromazine C. Haloperidol D. Ziprasidone • Ans- B, C - Chlorpromazine, Haloperidol
Thank you
Bibliography • Essentials of Medical Pharmacology -7 th edition by KD Tripathi • Goodman & Gilman's the Pharmacological Basis of Therapeutics 12 th edition by Laurence Brunton (Editor) • Lippincott's Illustrated Reviews: Pharmacology - 6 th edition by Richard A. Harvey • Basic and Clinical pharmacology 11 th edition by Bertram G Katzung • Rang & Dale's Pharmacology -7 th edition by Humphrey P. Rang • Clinical Pharmacology 11 th edition By Bennett and Brown, Churchill Livingstone • Principles of Pharmacology 2 nd edition by HL Sharma and KK Sharma • Review of Pharmacology by Gobind Sparsh
 Antipsychotic drugs classification
Antipsychotic drugs classification Similar picture
Similar picture Sss similarity definition
Sss similarity definition Similarity theorems
Similarity theorems Ways to prove triangles similar
Ways to prove triangles similar Nama dagang chlorpromazine
Nama dagang chlorpromazine Chlorpromazine
Chlorpromazine Chlorpromazine
Chlorpromazine Acute dystonia
Acute dystonia Food chain food chain food chain
Food chain food chain food chain Aliphatic meaning chemistry
Aliphatic meaning chemistry Alifatik keton
Alifatik keton Aromatic amines structure
Aromatic amines structure Aliphatic vs aromatic
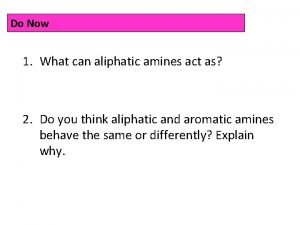
Aliphatic vs aromatic Primary aliphatic amines
Primary aliphatic amines Quaternary amine
Quaternary amine Aliphatic hydrocarbons
Aliphatic hydrocarbons Aliphatic amines and aromatic amines
Aliphatic amines and aromatic amines Classification of amines
Classification of amines Red side blue side
Red side blue side Two wheels roll side by side
Two wheels roll side by side Solclimatic
Solclimatic Server side scripting
Server side scripting Sell side vs buy side
Sell side vs buy side Full penetration welding
Full penetration welding Side by side stuff
Side by side stuff Sagittal plane border movement
Sagittal plane border movement Soda lime uses
Soda lime uses A regular pentagon of 30mm sides is resting on hp
A regular pentagon of 30mm sides is resting on hp Perfect competition side by side graphs
Perfect competition side by side graphs Videocon side by side refrigerator
Videocon side by side refrigerator Side angle side theorem
Side angle side theorem Tan geometry formula
Tan geometry formula Christensen phenomenon in complete denture
Christensen phenomenon in complete denture Tea side by side
Tea side by side Aromatic electrophilic substitution mechanism
Aromatic electrophilic substitution mechanism Carbohydrate side chain
Carbohydrate side chain Vender vs supplier
Vender vs supplier What is logistics management
What is logistics management Open kinetic chain exercises
Open kinetic chain exercises Dromotropy
Dromotropy Pharmacy jeopardy
Pharmacy jeopardy