Anatomy Physiology The Respiratory System Organs of the







- Slides: 43
Anatomy & Physiology The Respiratory System
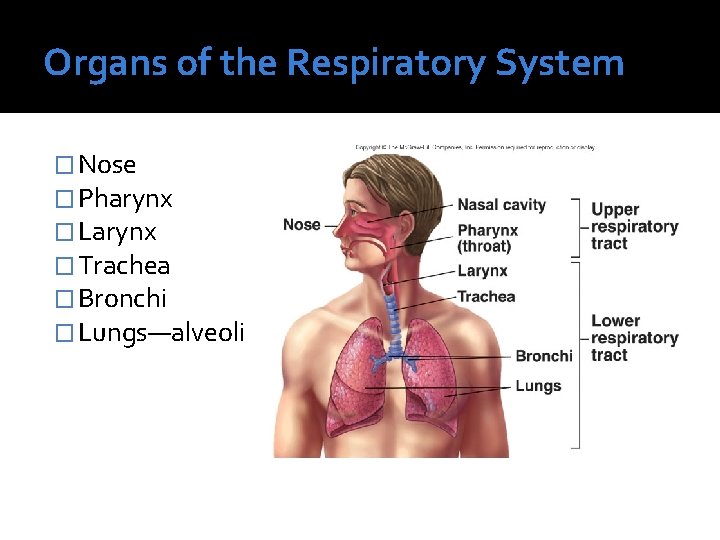
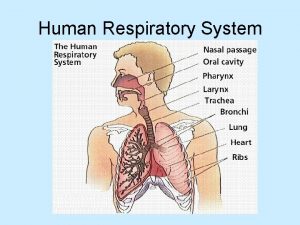
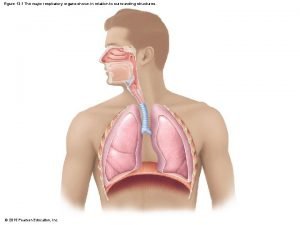
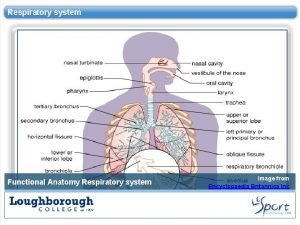
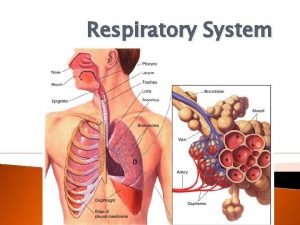
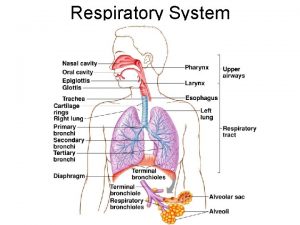
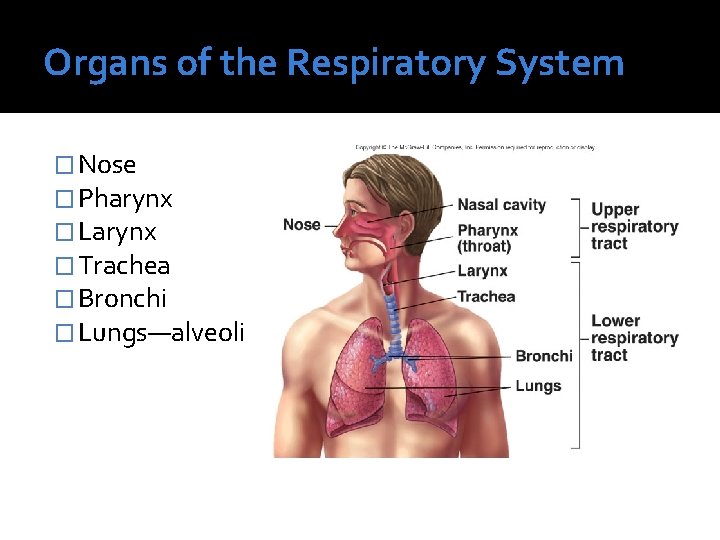
Organs of the Respiratory System � Nose � Pharynx � Larynx � Trachea � Bronchi � Lungs—alveoli
Functions of the Respiratory System �Creates gas exchanges within the blood in the alveoli (found in lungs) �Passageways leading to lungs function in: Purifying air Humidifies air Removes majority of irritants (i. e. dust/bacteria)
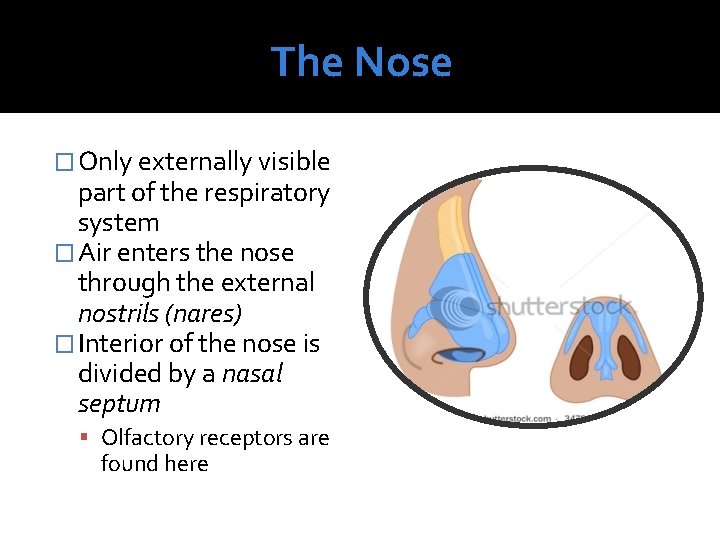
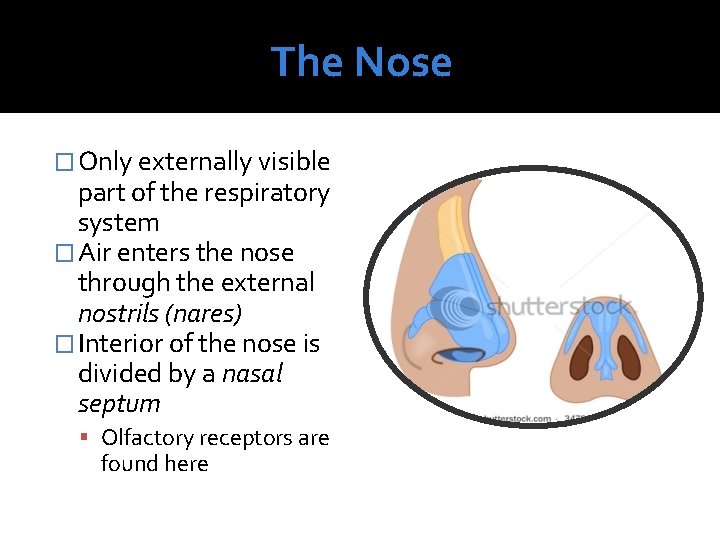
The Nose � Only externally visible part of the respiratory system � Air enters the nose through the external nostrils (nares) � Interior of the nose is divided by a nasal septum Olfactory receptors are found here
The Nose Cont’d �Sticky mucosa found in nose Traps bacteria/foreign pathogens ▪ Becomes destroyed by lysozymes Moistens air
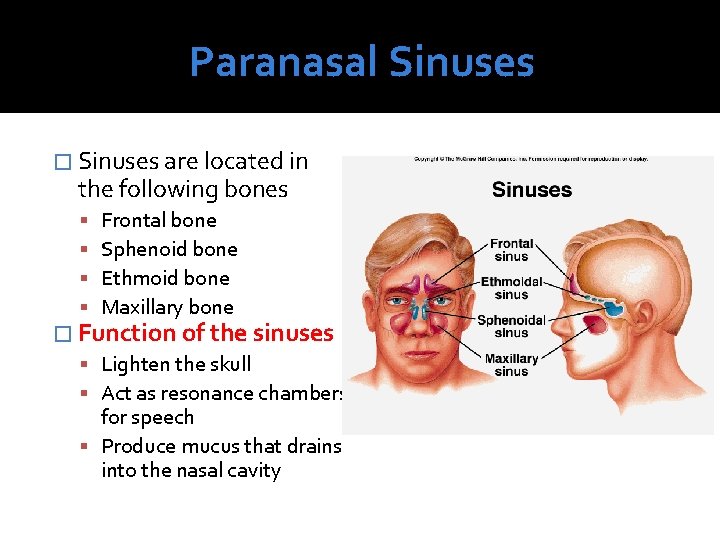
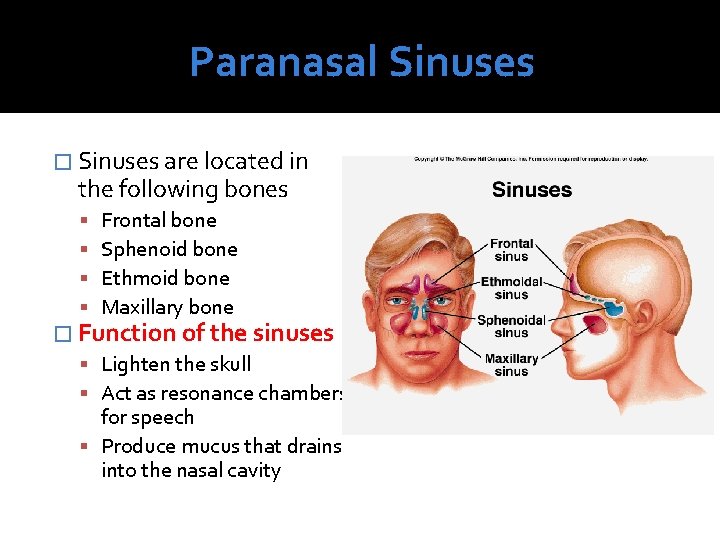
Paranasal Sinuses � Sinuses are located in the following bones Frontal bone Sphenoid bone Ethmoid bone Maxillary bone � Function of the sinuses Lighten the skull Act as resonance chambers for speech Produce mucus that drains into the nasal cavity
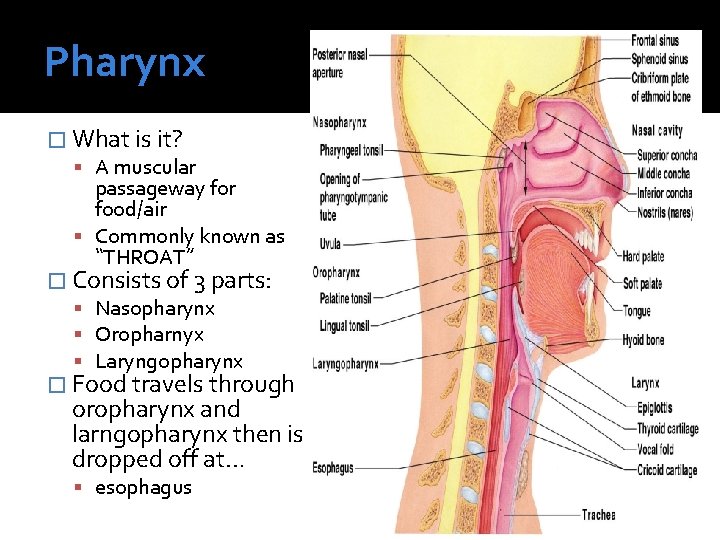
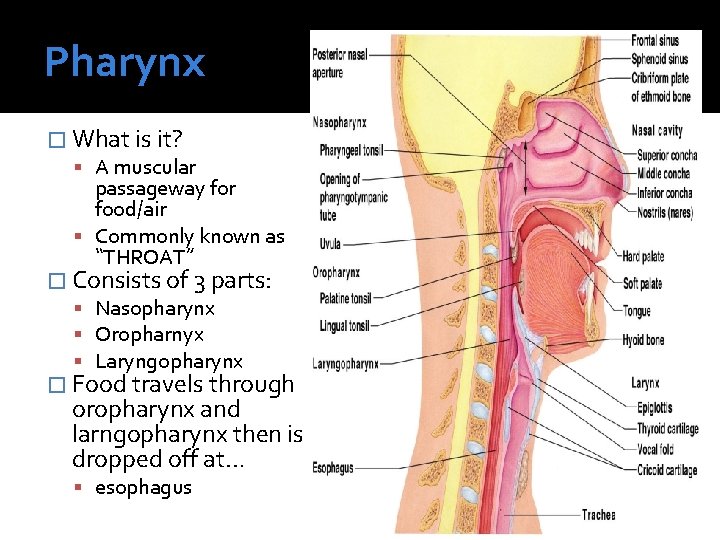
Pharynx � What is it? A muscular passageway for food/air Commonly known as “THROAT” � Consists of 3 parts: Nasopharynx Oropharnyx Laryngopharynx � Food travels through oropharynx and larngopharynx then is dropped off at… esophagus
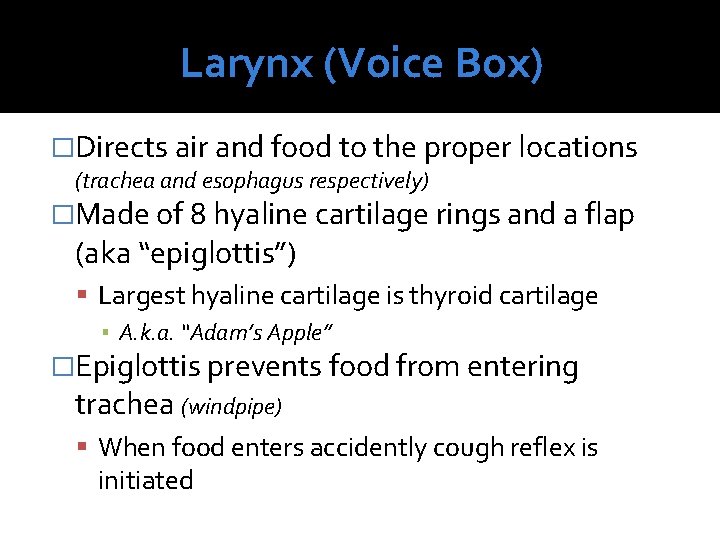
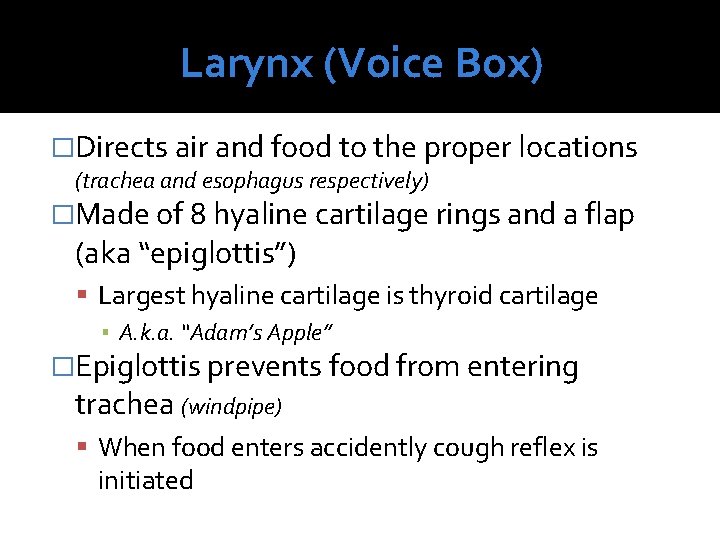
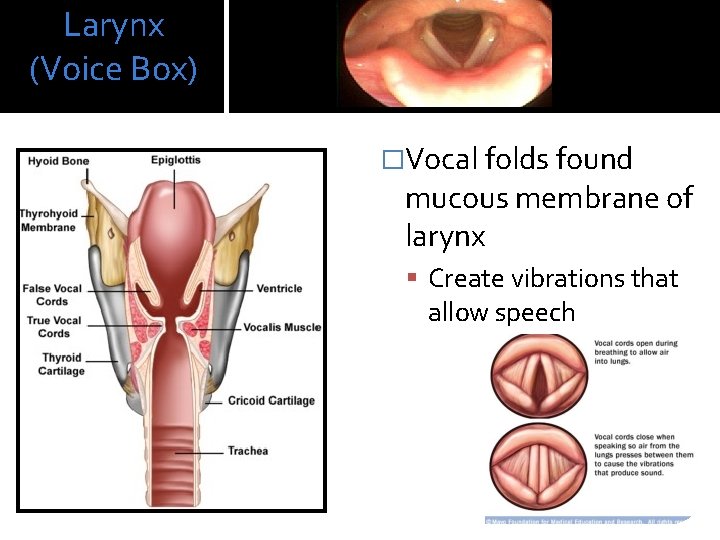
Larynx (Voice Box) �Directs air and food to the proper locations (trachea and esophagus respectively) �Made of 8 hyaline cartilage rings and a flap (aka “epiglottis”) Largest hyaline cartilage is thyroid cartilage ▪ A. k. a. “Adam’s Apple” �Epiglottis prevents food from entering trachea (windpipe) When food enters accidently cough reflex is initiated
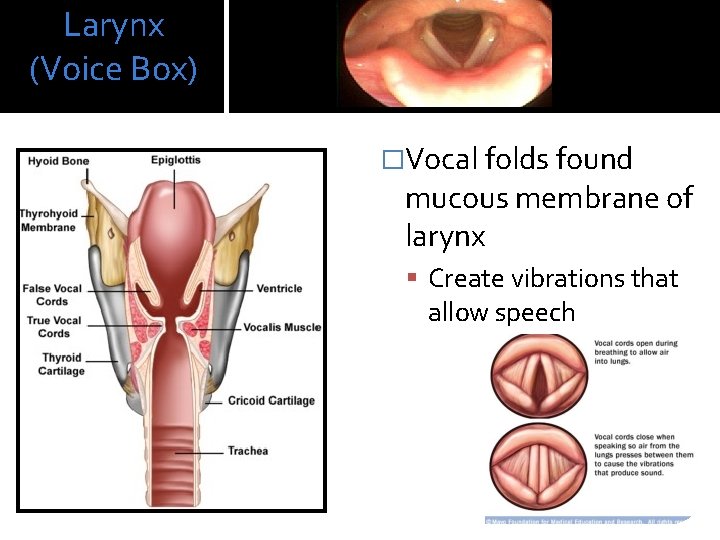
Larynx (Voice Box) �Vocal folds found mucous membrane of larynx Create vibrations that allow speech
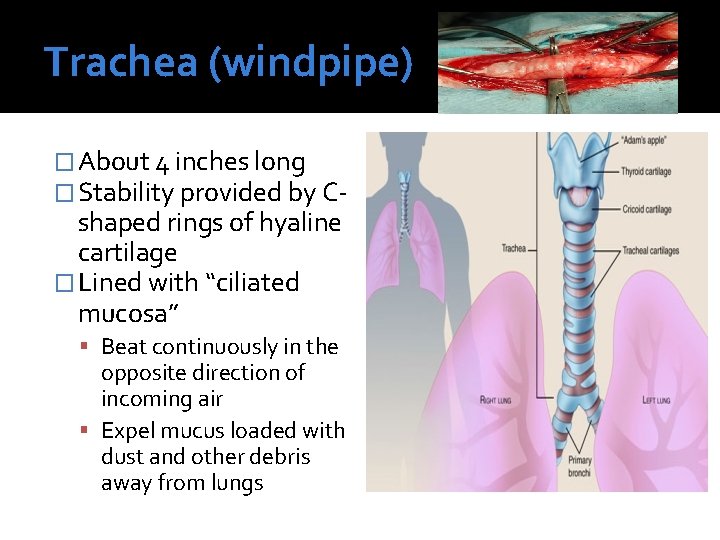
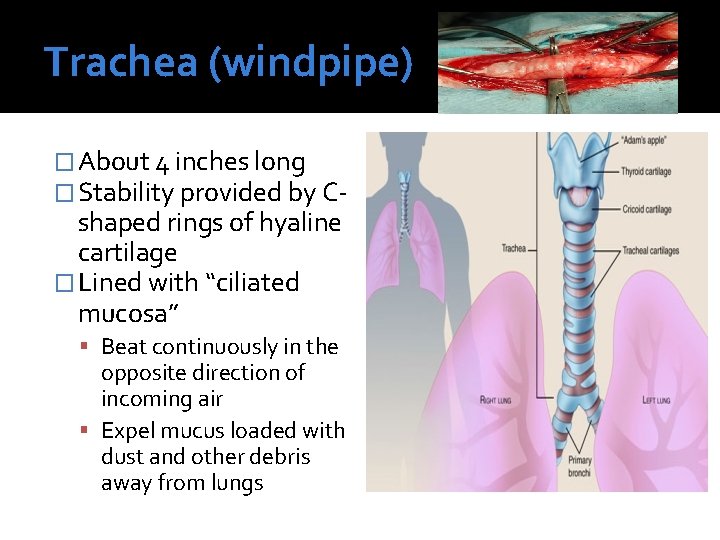
Trachea (windpipe) � About 4 inches long � Stability provided by C- shaped rings of hyaline cartilage � Lined with “ciliated mucosa” Beat continuously in the opposite direction of incoming air Expel mucus loaded with dust and other debris away from lungs

Main (Primary) Bronchi � Formed by division of the trachea � Right bronchus is wider, shorter, and straighter than left Common location for lodged objects � Bronchi subdivide into smaller and smaller branches within the lungs Known as “Bronchioles”

Lungs � Occupy most of the thoracic cavity Heart occupies central portion called mediastinum � Apex is near the clavicle (superior portion) � Base rests on the diaphragm (inferior portion) � Each lung is divided into lobes by fissures Left lung—two lobes Right lung—three lobes
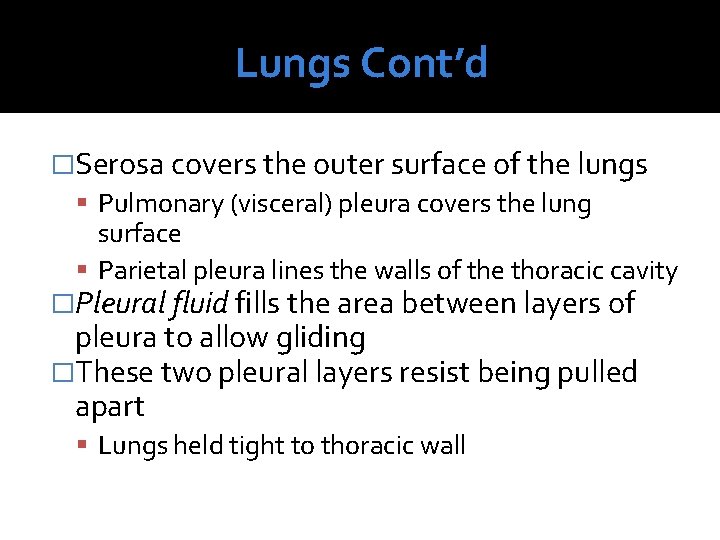
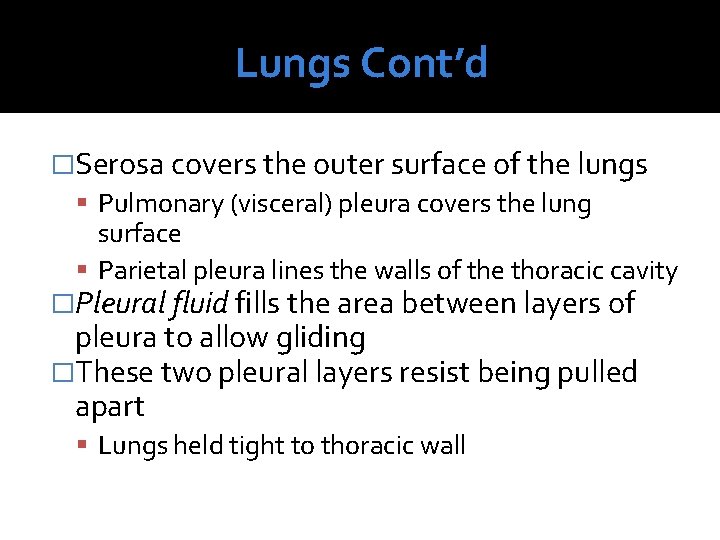
Lungs Cont’d �Serosa covers the outer surface of the lungs Pulmonary (visceral) pleura covers the lung surface Parietal pleura lines the walls of the thoracic cavity �Pleural fluid fills the area between layers of pleura to allow gliding �These two pleural layers resist being pulled apart Lungs held tight to thoracic wall
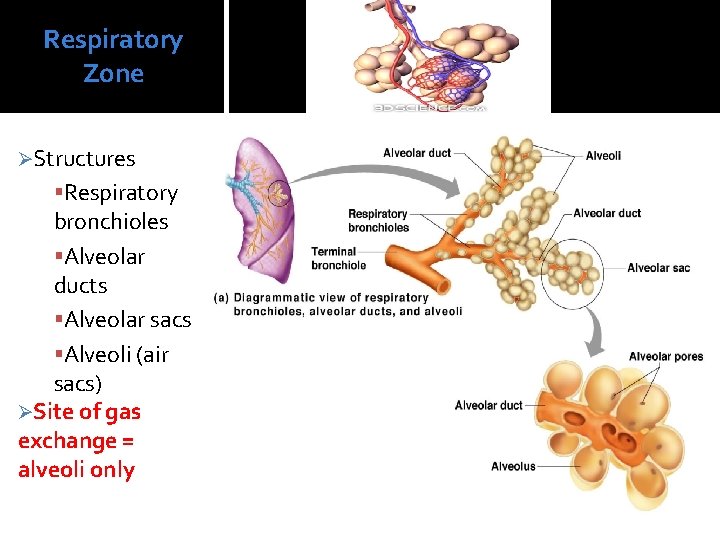
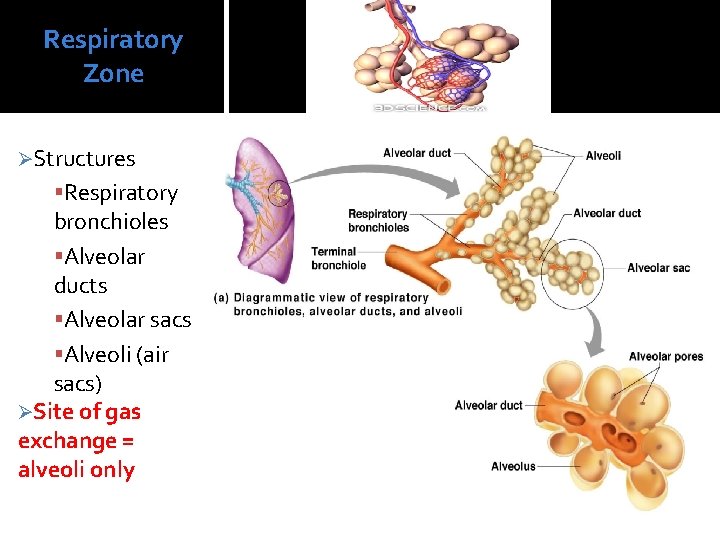
Respiratory Zone ØStructures Respiratory bronchioles Alveolar ducts Alveolar sacs Alveoli (air sacs) ØSite of gas exchange = alveoli only
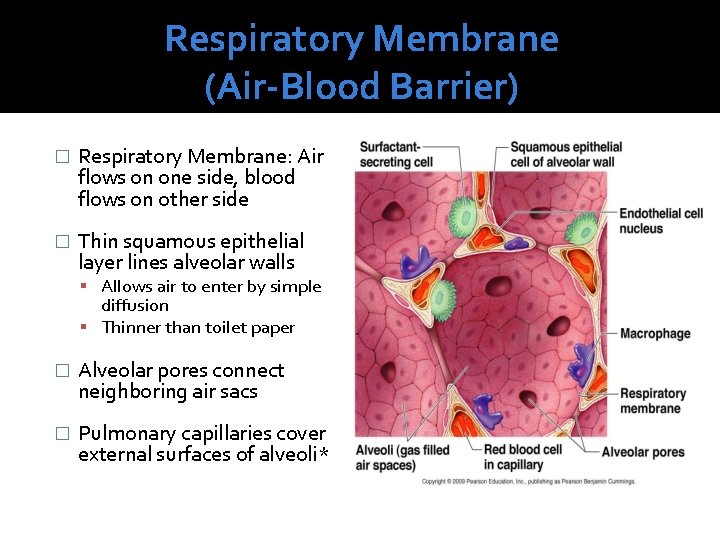
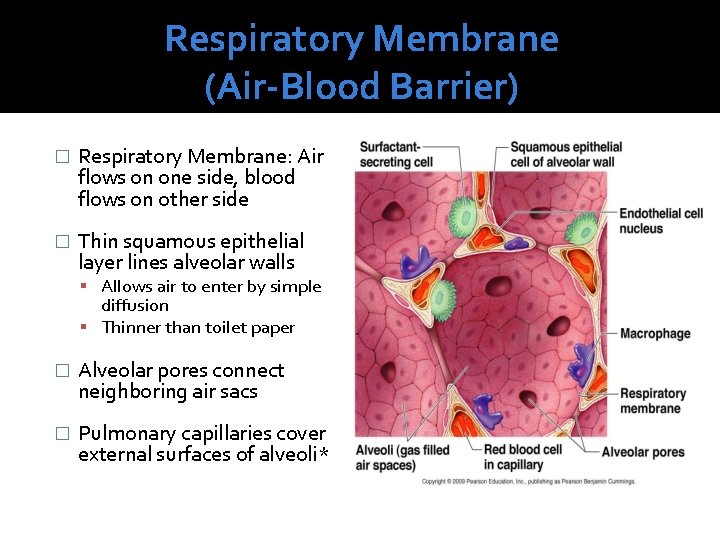
Respiratory Membrane (Air-Blood Barrier) � Respiratory Membrane: Air flows on one side, blood flows on other side � Thin squamous epithelial layer lines alveolar walls Allows air to enter by simple diffusion Thinner than toilet paper � Alveolar pores connect neighboring air sacs � Pulmonary capillaries cover external surfaces of alveoli*

Events of Respiration 1) 1) Pulmonary ventilation— moving air in and out of the lungs (commonly called breathing) 3) External respiration—gas exchange between pulmonary blood and alveoli 4) Oxygen is loaded into the blood Carbon dioxide is unloaded from the blood Exchanges are made between blood and body exterior Respiratory gas transport of oxygen and carbon dioxide via the bloodstream to different areas in the body Internal respiration gas exchange between blood and tissue cells Gas exchange occurs inside the body
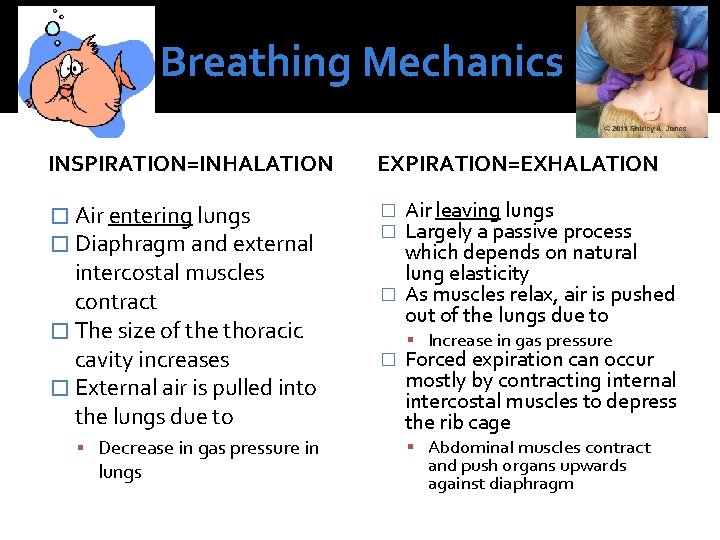
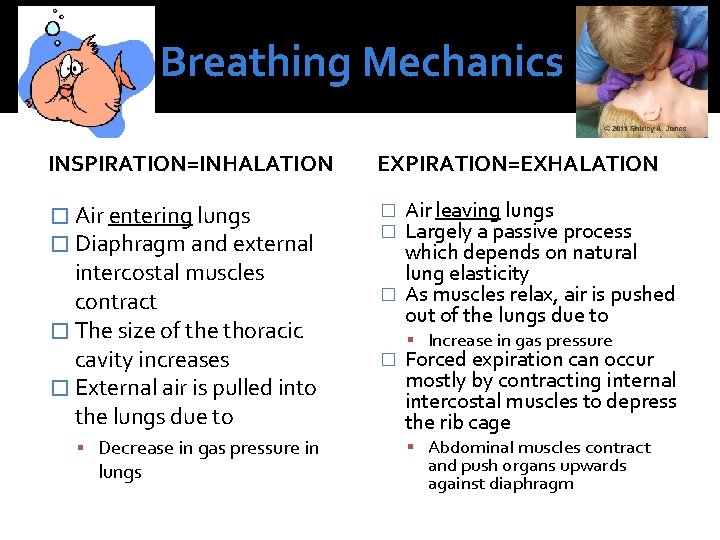
Breathing Mechanics INSPIRATION=INHALATION EXPIRATION=EXHALATION � Air entering lungs � Diaphragm and external � � intercostal muscles contract � The size of the thoracic cavity increases � External air is pulled into the lungs due to Decrease in gas pressure in lungs Air leaving lungs Largely a passive process which depends on natural lung elasticity � As muscles relax, air is pushed out of the lungs due to � Increase in gas pressure Forced expiration can occur mostly by contracting internal intercostal muscles to depress the rib cage Abdominal muscles contract and push organs upwards against diaphragm
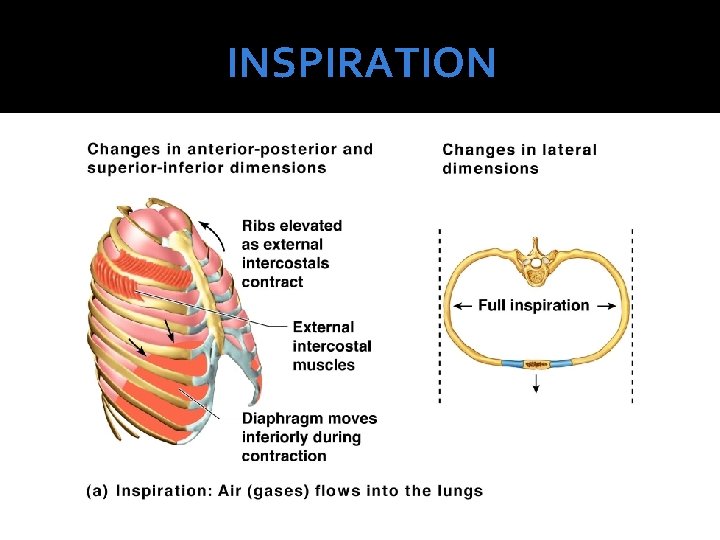
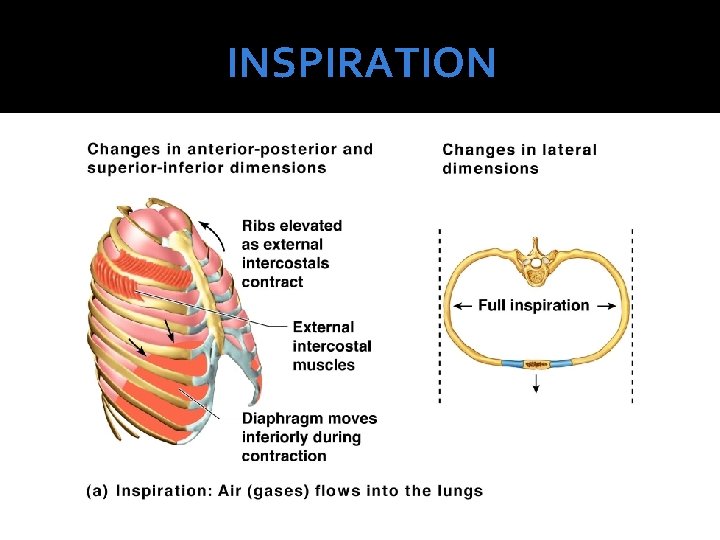
INSPIRATION

EXPIRATION
Nonrespiratory Air (Gas) Movements � Can be caused by reflexes or voluntary actions � Examples: Cough and sneeze—clears lungs of debris Crying—emotionally induced mechanism Laughing—similar to crying Hiccup—sudden inspirations Yawn—very deep inspiration
Respiratory Volumes and Capacities �Normal breathing moves about 500 m. L of air with each breath This respiratory volume is tidal volume (TV) �Many factors that affect respiratory capacity A person’s size Sex Age Physical condition
Respiratory Volumes and Capacities � Inspiratory reserve volume (IRV) Amount of air that can be taken in forcibly over the tidal volume Usually between 2100 and 3200 m. L � Expiratory reserve volume (ERV) Amount of air that can be forcibly exhaled Approximately 1200 m. L � Residual volume Air remaining in lung after expiration About 1200 ml Cannot leave lungs; needs to keep alveoli open � Vital capacity The total amount of exchangeable air Vital capacity = TV + IRV + ERV
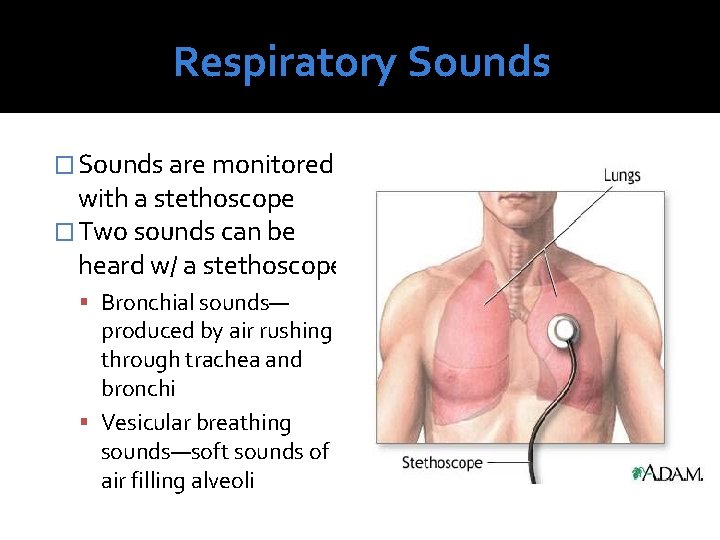
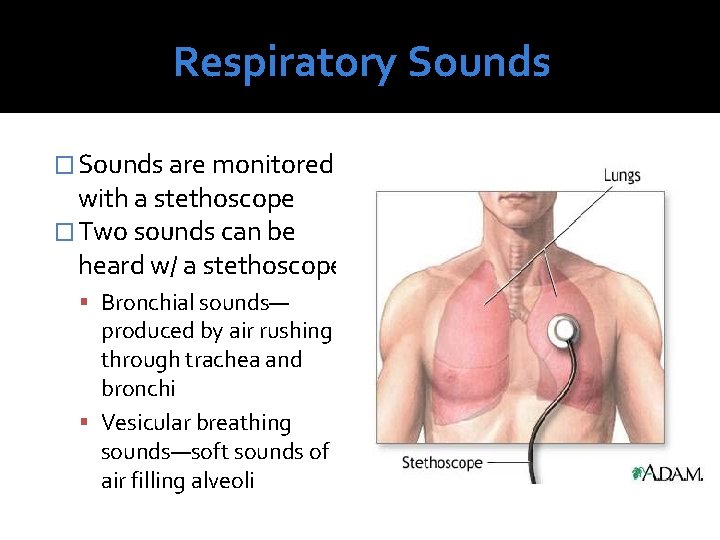
Respiratory Sounds � Sounds are monitored with a stethoscope � Two sounds can be heard w/ a stethoscope Bronchial sounds— produced by air rushing through trachea and bronchi Vesicular breathing sounds—soft sounds of air filling alveoli
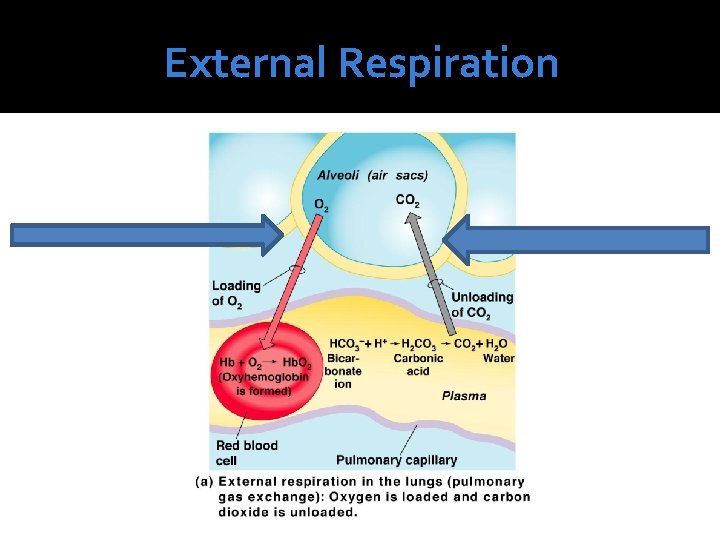
External Respiration � Gas exchange between alveoli (in lungs) and blood � Occurs through simple diffusion From higher concentration-lower concentration � Blood returning from tissues is CO 2 rich � Blood in pulmonary capillaries release CO 2 via exhalation � Blood leaving the alveoli in lungs is O 2 rich, CO 2 poor
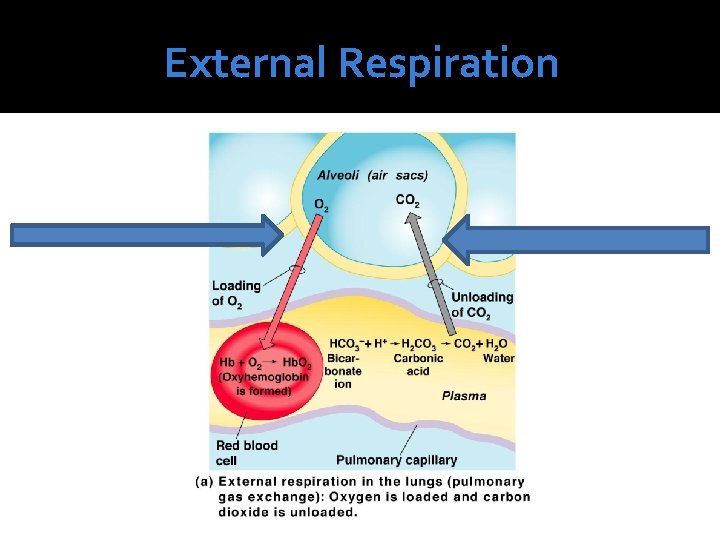
External Respiration
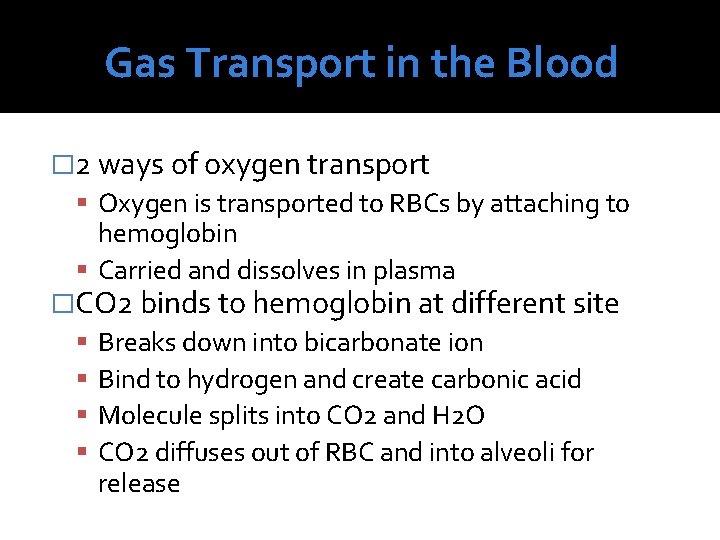
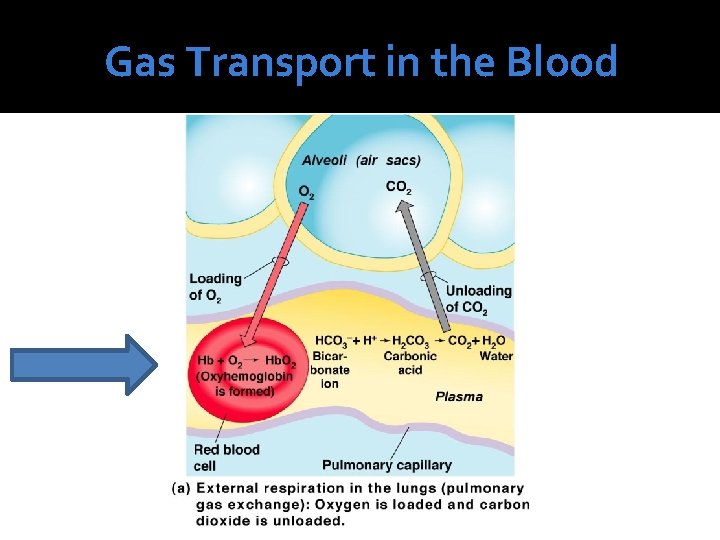
Gas Transport in the Blood � 2 ways of oxygen transport Oxygen is transported to RBCs by attaching to hemoglobin Carried and dissolves in plasma �CO 2 binds to hemoglobin at different site Breaks down into bicarbonate ion Bind to hydrogen and create carbonic acid Molecule splits into CO 2 and H 2 O CO 2 diffuses out of RBC and into alveoli for release
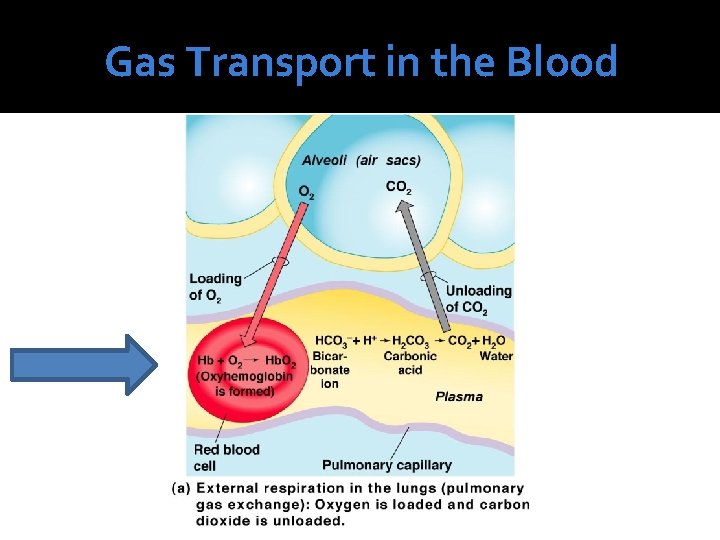
Gas Transport in the Blood
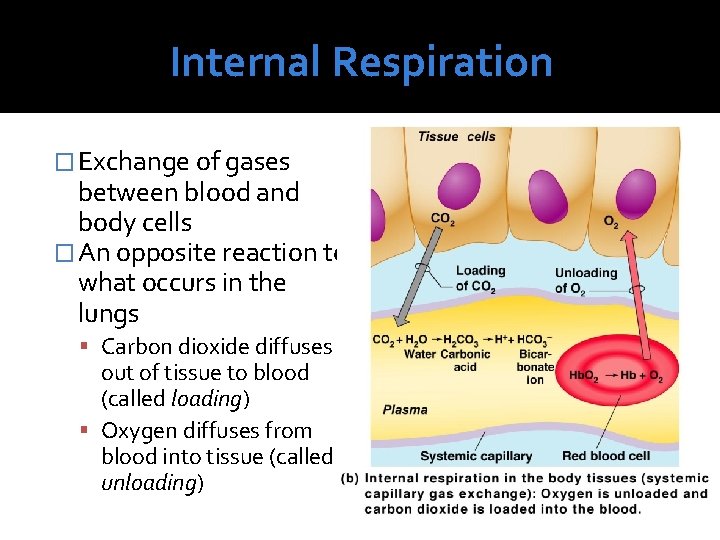
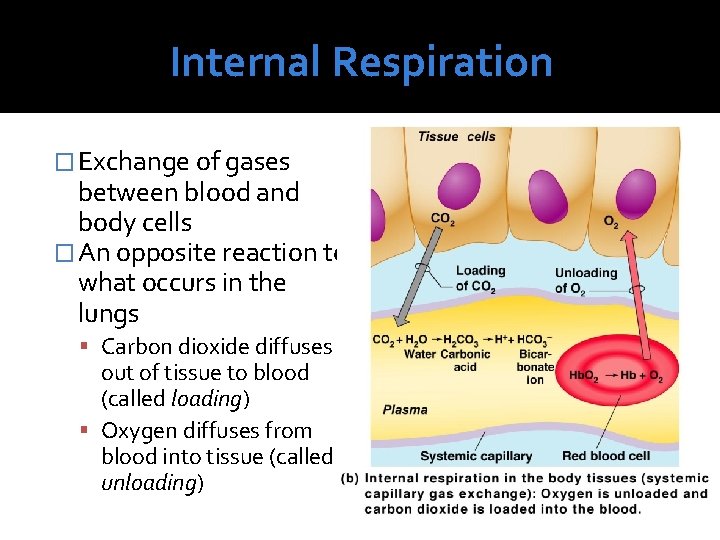
Internal Respiration � Exchange of gases between blood and body cells � An opposite reaction to what occurs in the lungs Carbon dioxide diffuses out of tissue to blood (called loading) Oxygen diffuses from blood into tissue (called unloading)
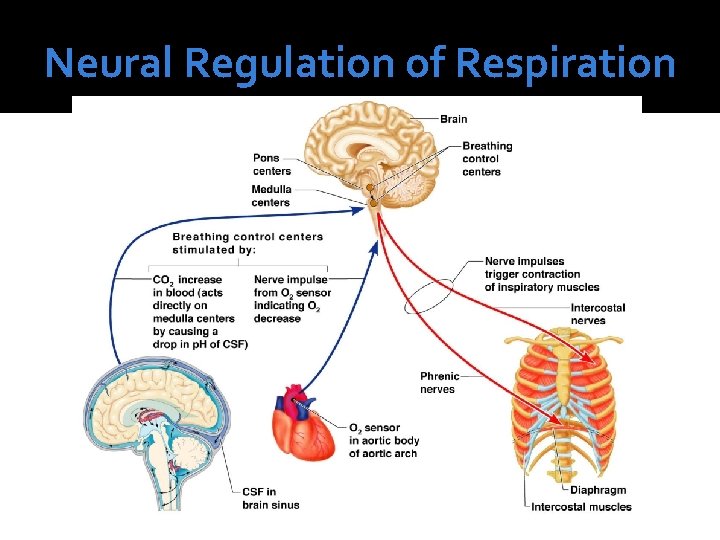
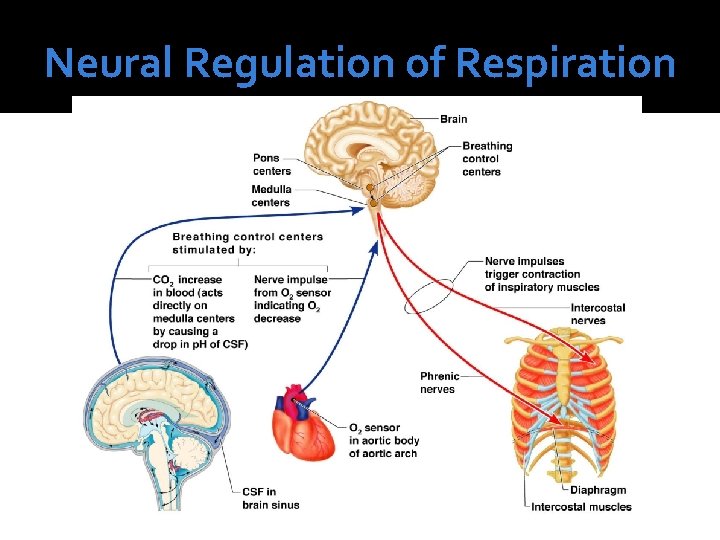
Neural Regulation of Respiration � Activity of respiratory muscles is transmitted to and from the brain by phrenic and intercostal nerves � Neural centers that control rate and depth are located in the medulla and pons Medulla—sets basic rhythm of breathing and contains a pacemaker called the self-exciting inspiratory center Pons—appears to smooth out respiratory rate
Neural Regulation of Respiration
Neural Regulation of Respiration �Normal respiratory rate (eupnea) 12– 15 respirations per minute �Hyperpnea Increased respiratory rate often due to extra oxygen needs ▪ Examples? ?
Non-Neural Factors Influencing Respiratory Rate and Depth �Physical factors Increased body temperature Exercise Talking Coughing �Volition (conscious control) Temporary, body activates to initiate breathing again �Emotional factors
Non-Neural Factors Influencing Respiratory Rate and Depth �Chemical factors: CO 2 levels The body’s need to rid itself of CO 2 is the most important stimulus Increased levels of carbon dioxide (and thus, a decreased or acidic p. H) in the blood increase the rate and depth of breathing �Chemical factors: oxygen levels Changes in oxygen concentration in the blood are detected by chemoreceptors in the aorta and common carotid artery Information is sent to the medulla
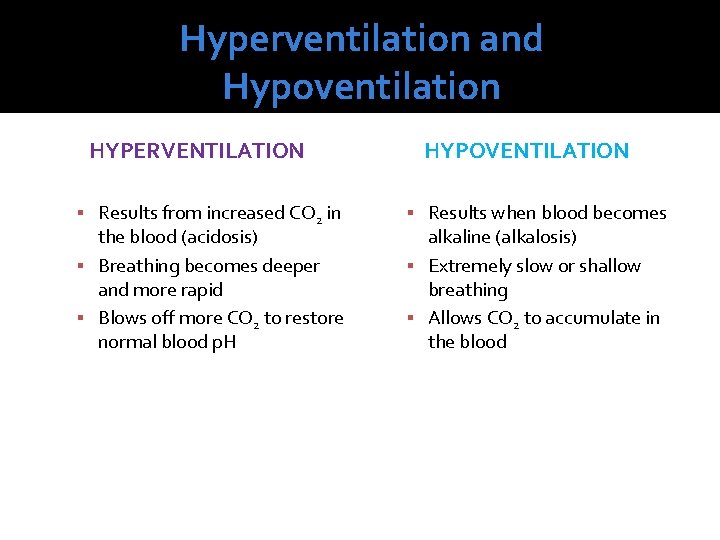
Hyperventilation and Hypoventilation HYPERVENTILATION Results from increased CO 2 in the blood (acidosis) Breathing becomes deeper and more rapid Blows off more CO 2 to restore normal blood p. H HYPOVENTILATION Results when blood becomes alkaline (alkalosis) Extremely slow or shallow breathing Allows CO 2 to accumulate in the blood
Homeostatic Imbalances �Chronic Obstructive Pulmonary Diseases (COPD) �Chronic Bronchitis �Emphysema �Lung Cancer �Sudden Infant Death Syndrome (SIDS) �Asthma
Chronic Obstructive Pulmonary Diseases (COPD) �Major cause of death in the U. S. �Signs/Symptoms: HX of smoking Dyspnea Coughing Frequent pulmonary infections Hypoxic and retain CO 2 Eventually leads to mortality

Chronic Bronchitis � Mucosa of respiratory passages becomes inflammed � Excess mucus is produced � Results in impaired breathing and gas exchange � Increases risk for pulmonary infection � “Blue Bloaters” Cyanotic due to CO 2 retention
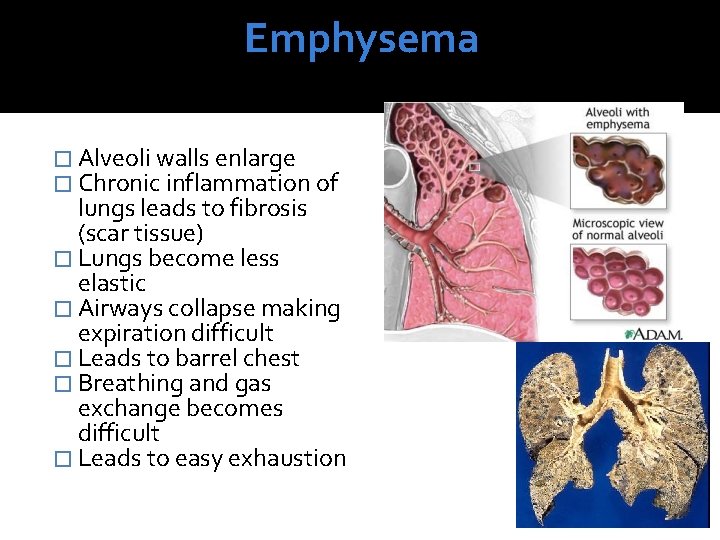
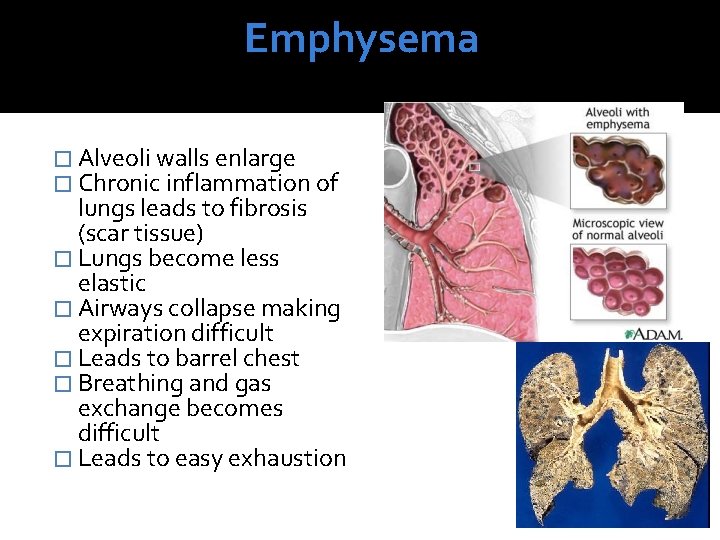
Emphysema � Alveoli walls enlarge � Chronic inflammation of lungs leads to fibrosis (scar tissue) � Lungs become less elastic � Airways collapse making expiration difficult � Leads to barrel chest � Breathing and gas exchange becomes difficult � Leads to easy exhaustion

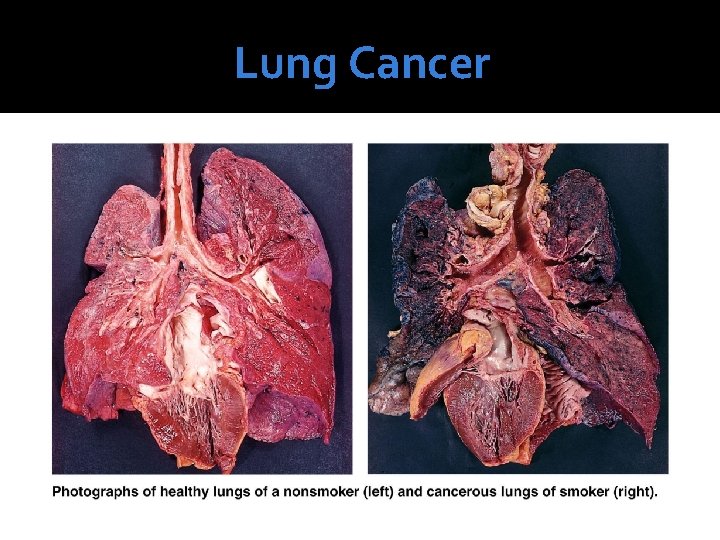
Lung Cancer �Accounts for one-third of all cancer deaths in the United States �Increased incidence is associated with smoking 90% if lung cancer patients are smokers �Leads to a series of other sides effects detrimental to health �Affected lobes are typically removed
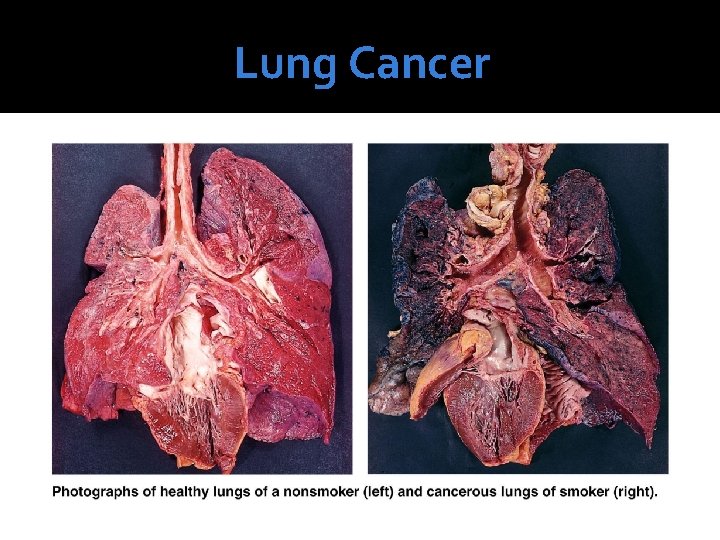
Lung Cancer
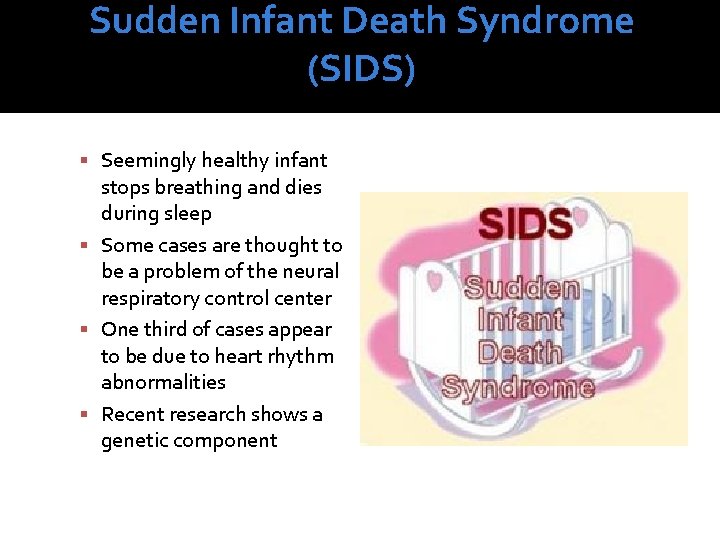
Sudden Infant Death Syndrome (SIDS) Seemingly healthy infant stops breathing and dies during sleep Some cases are thought to be a problem of the neural respiratory control center One third of cases appear to be due to heart rhythm abnormalities Recent research shows a genetic component
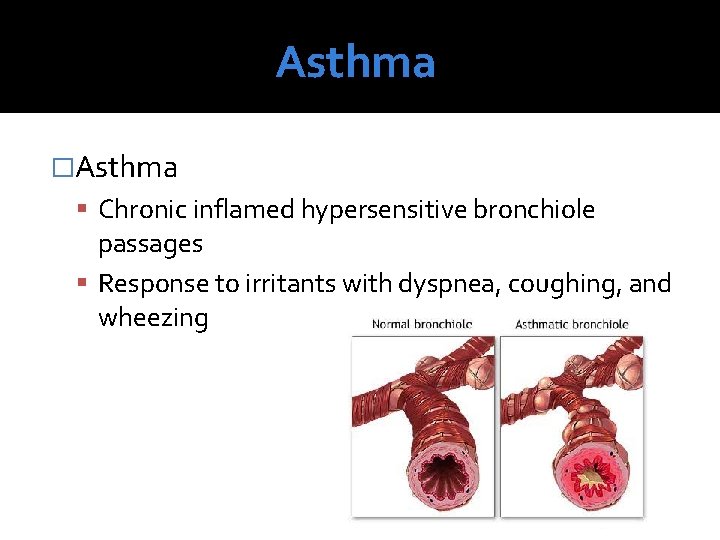
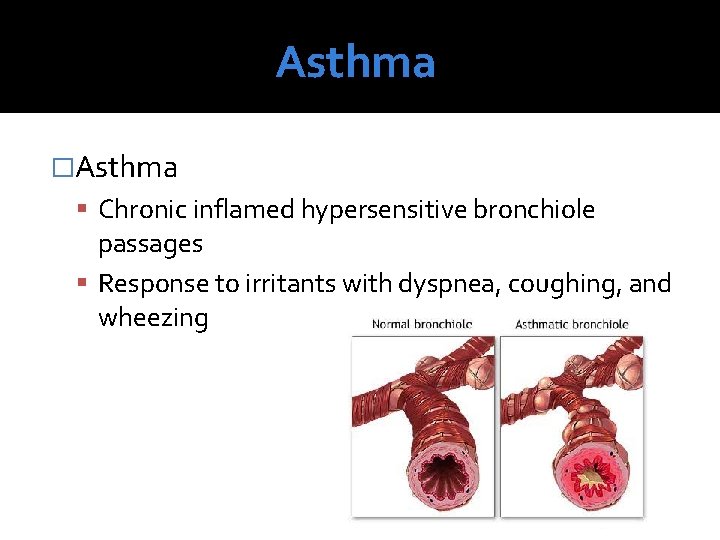
Asthma �Asthma Chronic inflamed hypersensitive bronchiole passages Response to irritants with dyspnea, coughing, and wheezing

Developmental Aspects of the Respiratory System �Aging effects Elasticity of lungs decreases Vital capacity decreases Blood oxygen levels decrease Stimulating effects of carbon dioxide decrease Elderly are often hypoxic and exhibit sleep apnea More risks of respiratory tract infection
 Types of respiration in human
Types of respiration in human Which organs are involved in respiratory system
Which organs are involved in respiratory system Respiratory system organs
Respiratory system organs Tidal volume
Tidal volume Respiratory zone and conducting zone
Respiratory zone and conducting zone Invertebrate respiratory system
Invertebrate respiratory system Respiratory organs of invertebrates
Respiratory organs of invertebrates Organs forming the respiratory passageway
Organs forming the respiratory passageway Upper and lower airway diagram
Upper and lower airway diagram Respiratory organs
Respiratory organs Anatomy and physiology unit 7 cardiovascular system
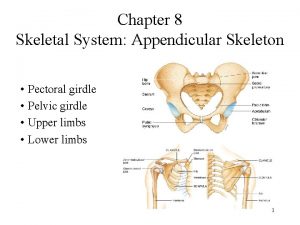
Anatomy and physiology unit 7 cardiovascular system Male vs female skeleton pelvis
Male vs female skeleton pelvis Trachea
Trachea Respiratory system
Respiratory system Respiratory system circulatory system digestive system
Respiratory system circulatory system digestive system Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Specialized stems examples
Specialized stems examples Bone anatomy and physiology
Bone anatomy and physiology Ulcer definition anatomy
Ulcer definition anatomy Sheep liver lobes
Sheep liver lobes Podbřišek
Podbřišek Epigastric vs hypogastric
Epigastric vs hypogastric Straw coloured fluid
Straw coloured fluid Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Endomysium
Endomysium Http://anatomy and physiology
Http://anatomy and physiology Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Anatomy and physiology of appendicitis
Anatomy and physiology of appendicitis Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Science olympiad forensics cheat sheet
Science olympiad forensics cheat sheet Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Stomach anatomy and physiology ppt
Stomach anatomy and physiology ppt Physiology
Physiology Anatomy and physiology chapter 7
Anatomy and physiology chapter 7 Anatomy and physiology coloring workbook figure 14-1
Anatomy and physiology coloring workbook figure 14-1 Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1