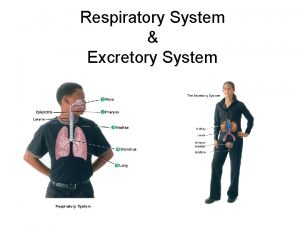
13 The Respiratory System Organs of the Respiratory






















- Slides: 101
13 The Respiratory System
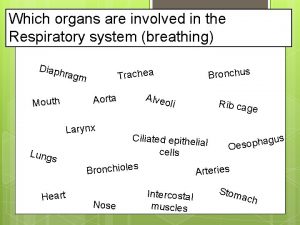
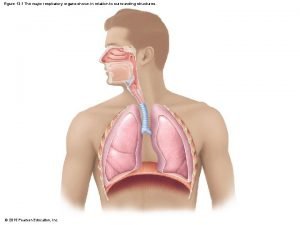
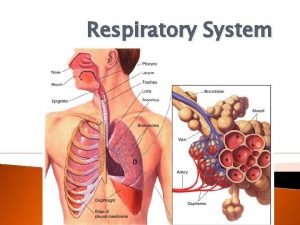
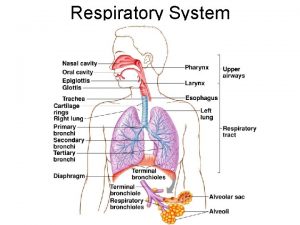
Organs of the Respiratory System 1. Nose 2. Pharynx 3. Larynx 4. Trachea 5. Bronchi 6. Lungs — alveoli

Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Right main (primary) bronchus Left lung Right lung Diaphragm Figure 13. 1
General Introduction https: //www. youtube. com/watch? v=NRT 1 h. Oqni. Z 0 https: //www. youtube. com/watch? v=o 2 Oc. Gg. Jbi. Uk Refer to PAL 3. 0 cadaver; anatomical and histological sites located in study area of Chapter 13.
Functions of the Respiratory System Gas exchanges between the blood and external environment Occurs in the alveoli of the lungs Passageways to the lungs purify, humidify, and warm the incoming air
1. The Nose Only externally visible part of the respiratory system Air enters the nose through the external nostrils (nares) nares Interior of the nose consists of a nasal cavity divided by a nasal septum
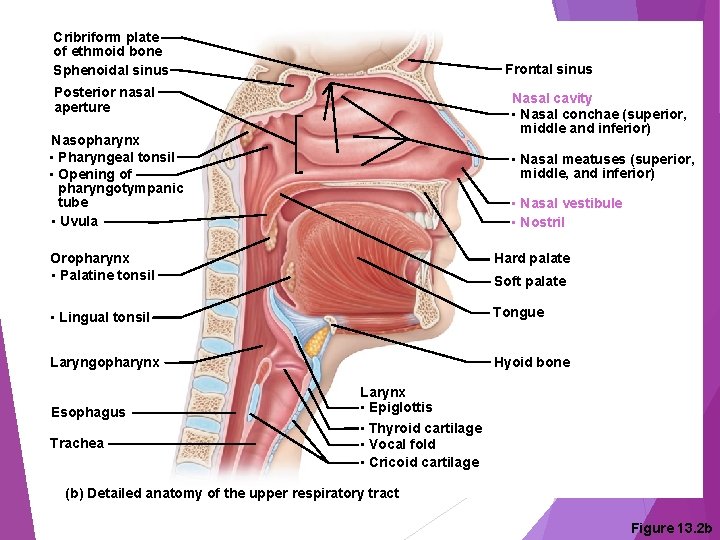
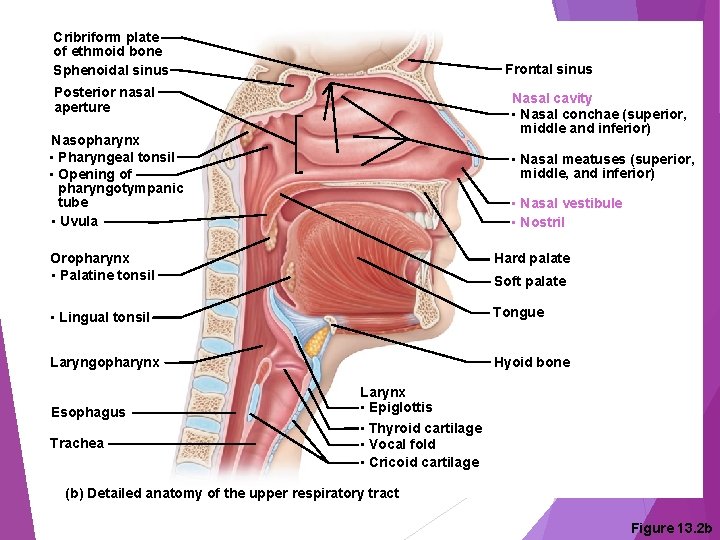
Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, middle and inferior) Nasopharynx • Pharyngeal tonsil • Opening of pharyngotympanic tube • Uvula • Nasal meatuses (superior, middle, and inferior) • Nasal vestibule • Nostril Oropharynx • Palatine tonsil Hard palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Esophagus Trachea Soft palate Larynx • Epiglottis • Thyroid cartilage • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract Figure 13. 2 b

Anatomy of the Nasal Cavity Olfactory receptors are located in the mucosa on the superior surface The rest of the cavity is lined with respiratory mucosa that Moisten air Trap incoming foreign particles

Anatomy of the Nasal Cavity Lateral walls have projections called conchae Increase surface area Increase air turbulence within the nasal cavity The nasal cavity is separated from the oral cavity by the palate Anterior hard palate (bone) Posterior soft palate (muscle)
Paranasal Sinuses Cavities within bones surrounding the nasal cavity are called sinuses Sinuses are located in the following bones Frontal bone Sphenoid bone Ethmoid bone Maxillary bone

Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, middle and inferior) Nasopharynx • Pharyngeal tonsil • Opening of pharyngotympanic tube • Uvula • Nasal meatuses (superior, middle, and inferior) • Nasal vestibule • Nostril Oropharynx • Palatine tonsil Hard palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Esophagus Trachea Soft palate Larynx • Epiglottis • Thyroid cartilage • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract Figure 13. 2 b
Paranasal Sinuses Function of the sinuses Lighten the skull Act as resonance chambers for speech Produce mucus that drains into the nasal cavity
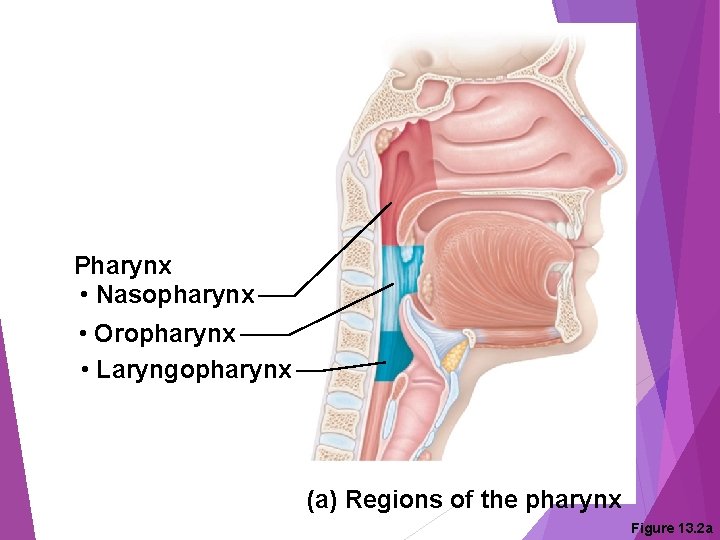
2. Pharynx (Throat) Muscular passage from nasal cavity to larynx Three regions of the pharynx Nasopharynx — superior region behind nasal cavity Oropharynx — middle region behind mouth Laryngopharynx — inferior region attached to larynx The oropharynx and laryngopharynx are common passageways for air and food
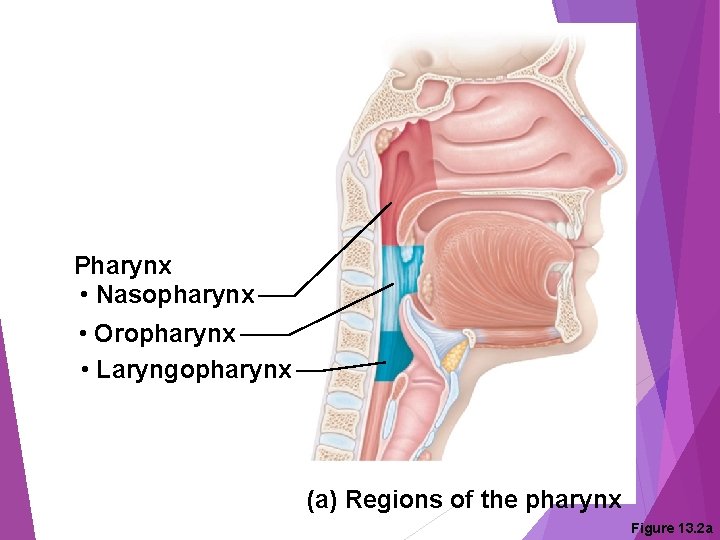
Pharynx • Nasopharynx • Oropharynx • Laryngopharynx (a) Regions of the pharynx Figure 13. 2 a

Structures of the Pharynx Pharyngotympanic tubes open into the nasopharynx Tonsils of the pharynx Pharyngeal tonsil (adenoid) is located in the nasopharynx Palatine tonsils are located in the oropharynx Lingual tonsils are found at the base of the tongue

Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, middle and inferior) Nasopharynx • Pharyngeal tonsil • Opening of pharyngotympanic tube • Uvula • Nasal meatuses (superior, middle, and inferior) • Nasal vestibule • Nostril Oropharynx • Palatine tonsil Hard palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Esophagus Trachea Soft palate Larynx • Epiglottis • Thyroid cartilage • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract Figure 13. 2 b

3. Larynx (Voice Box) Routes air and food into proper channels Plays a role in speech Made of eight rigid hyaline cartilages and a spoonshaped flap of elastic cartilage (epiglottis)
Structures of the Larynx Thyroid cartilage Largest of the hyaline cartilages Protrudes anteriorly (Adam’s apple) Epiglottis Protects the superior opening of the larynx Routes food to the esophagus and air toward the trachea When swallowing, the epiglottis rises and forms a lid over the opening of the larynx
Structures of the Larynx Vocal folds (true vocal cords) Vibrate with expelled air to create sound (speech) Glottis — opening between vocal cords

Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, middle and inferior) Nasopharynx • Pharyngeal tonsil • Opening of pharyngotympanic tube • Uvula • Nasal meatuses (superior, middle, and inferior) • Nasal vestibule • Nostril Oropharynx • Palatine tonsil Hard palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Esophagus Trachea Soft palate Larynx • Epiglottis • Thyroid cartilage • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract Figure 13. 2 b
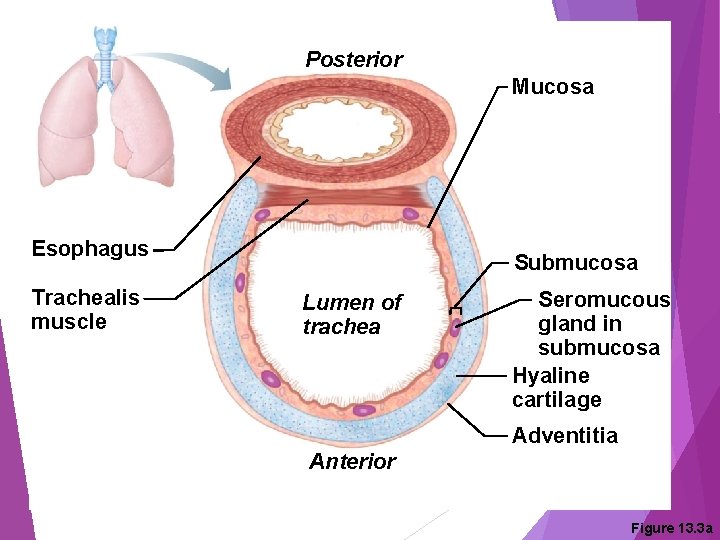
4. Trachea (Windpipe) Four-inch-long tube that connects larynx with bronchi Walls are reinforced with C-shaped hyaline cartilage Lined with ciliated mucosa Beat continuously in the opposite direction of incoming air Expel mucus loaded with dust and other debris away from lungs
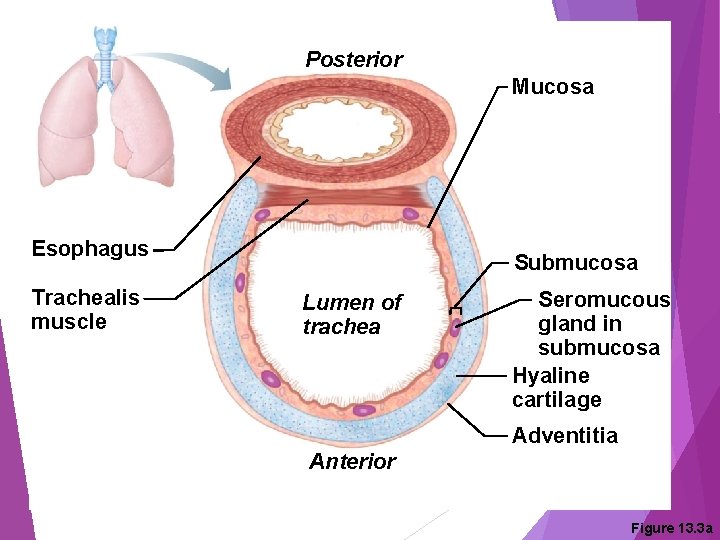
Posterior Mucosa Esophagus Trachealis muscle Submucosa Lumen of trachea Seromucous gland in submucosa Hyaline cartilage Adventitia Anterior Figure 13. 3 a
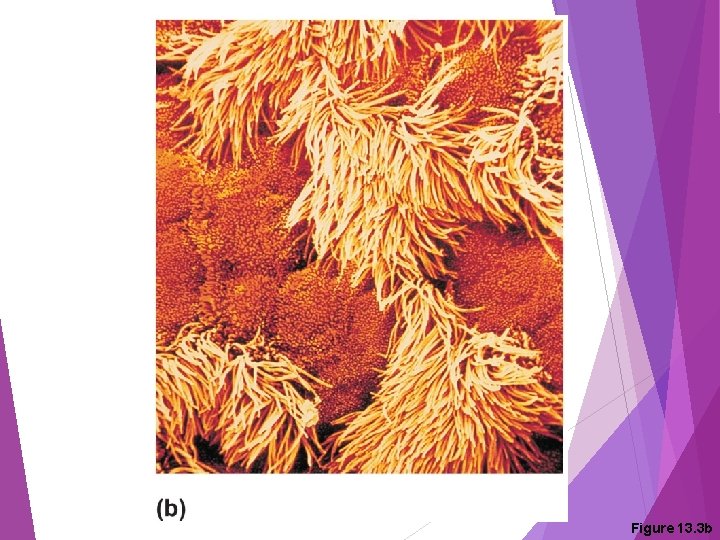
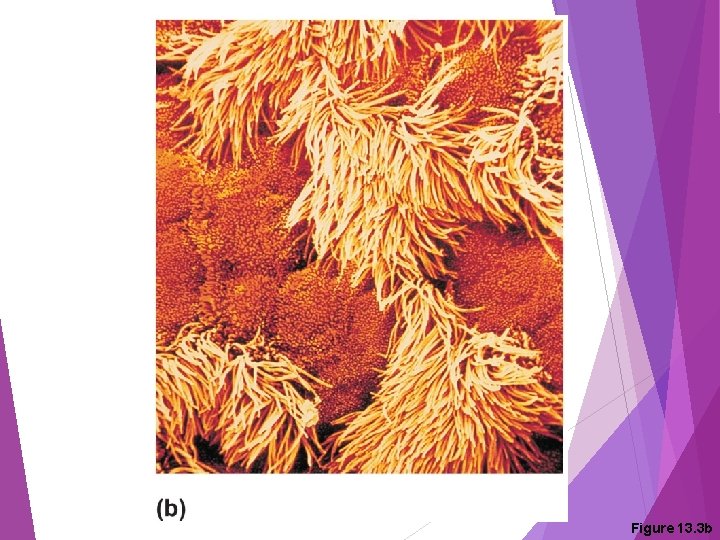
Figure 13. 3 b
5. Main (Primary) Bronchi Formed by division of the trachea Enters the lung at the hilum (medial depression) Right bronchus is wider, shorter, and straighter than left Bronchi subdivide into smaller and smaller branches
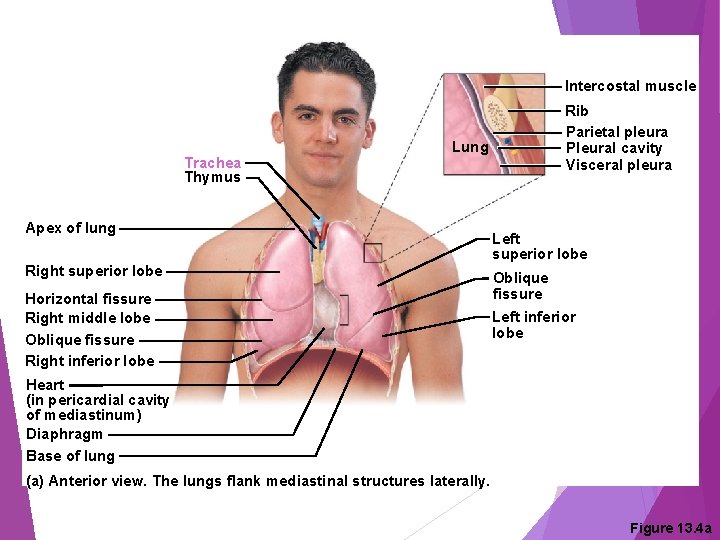
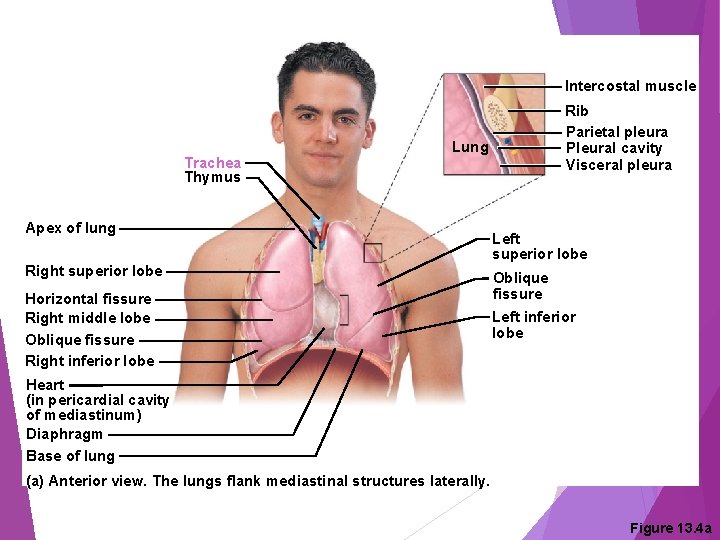
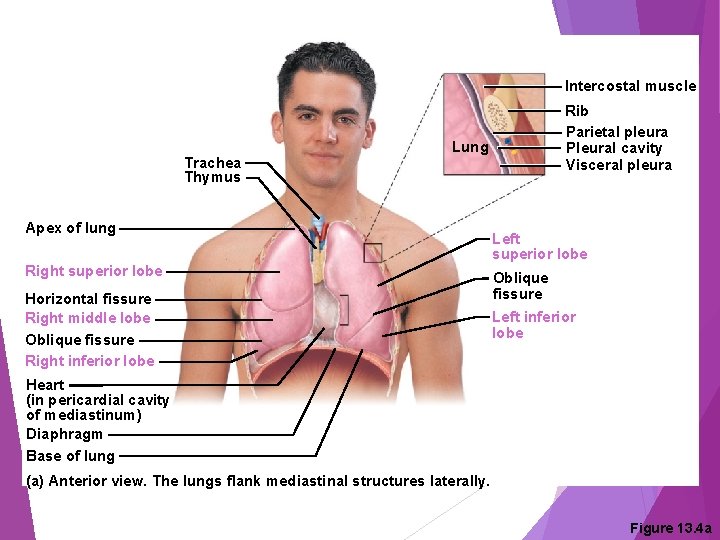
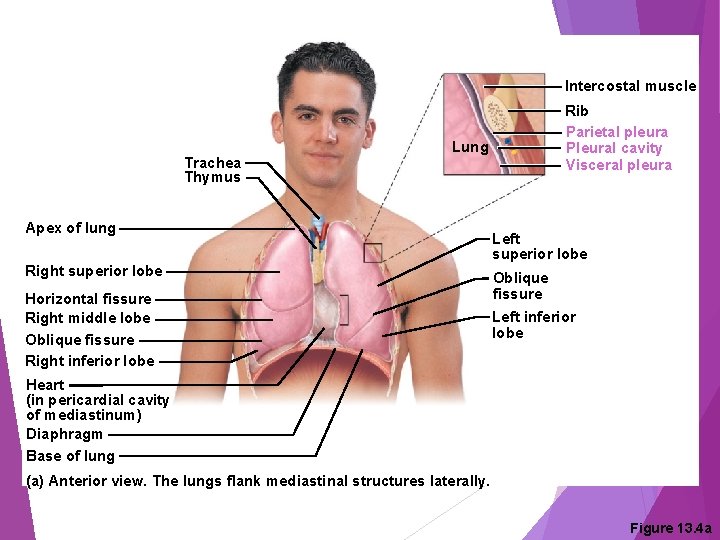
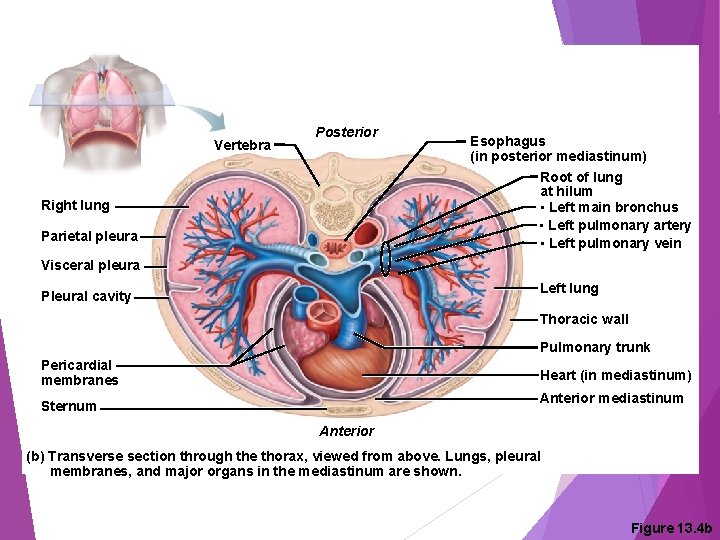
Intercostal muscle Trachea Thymus Rib Parietal pleura Pleural cavity Visceral pleura Lung Apex of lung Right superior lobe Horizontal fissure Right middle lobe Oblique fissure Right inferior lobe Left superior lobe Oblique fissure Left inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. Figure 13. 4 a
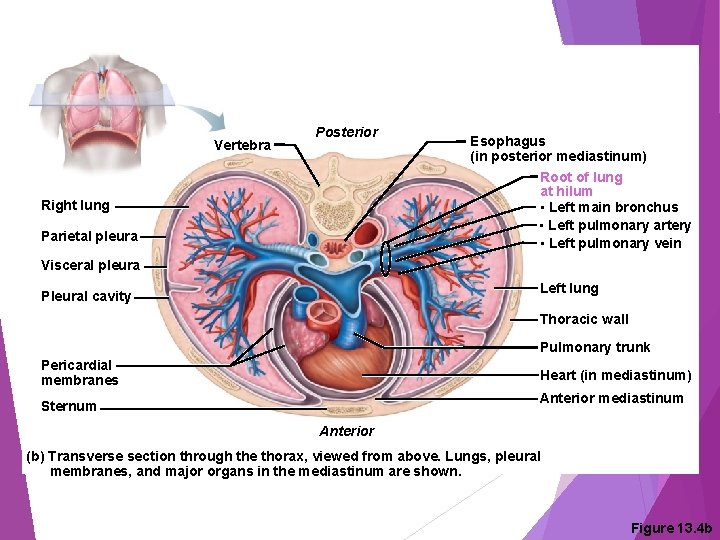
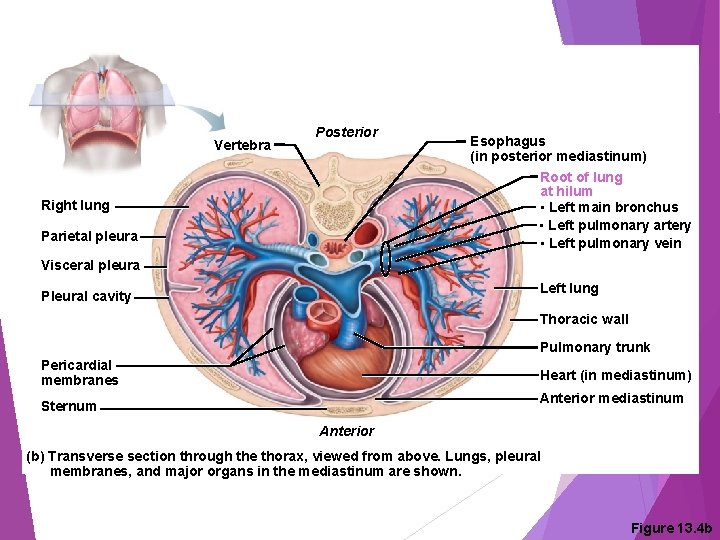
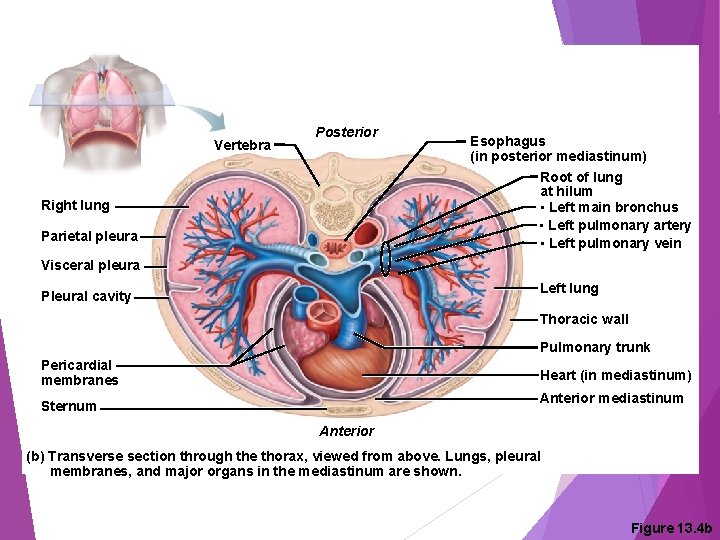
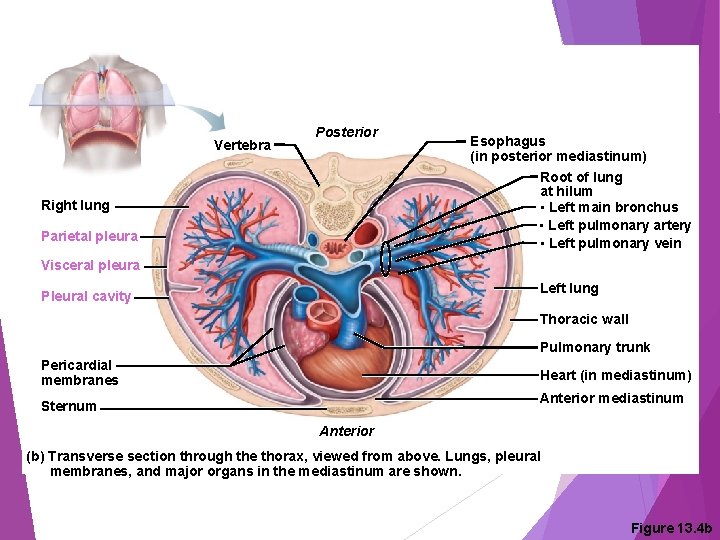
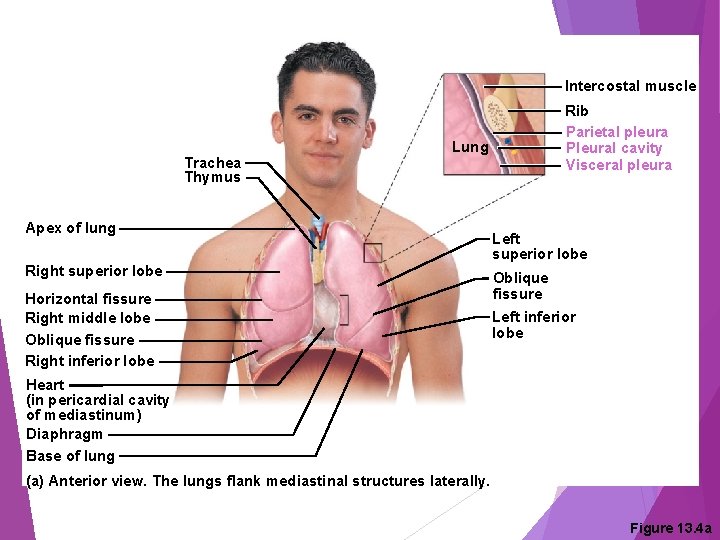
Vertebra Posterior Right lung Parietal pleura Esophagus (in posterior mediastinum) Root of lung at hilum • Left main bronchus • Left pulmonary artery • Left pulmonary vein Visceral pleura Left lung Pleural cavity Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Anterior mediastinum Sternum Anterior (b) Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. Figure 13. 4 b

6. Lungs Occupy most of the thoracic cavity Heart occupies central portion called mediastinum Apex is near the clavicle (superior portion) Base rests on the diaphragm (inferior portion) Each lung is divided into lobes by fissures Left lung — two lobes Right lung — three lobes [Why? ]
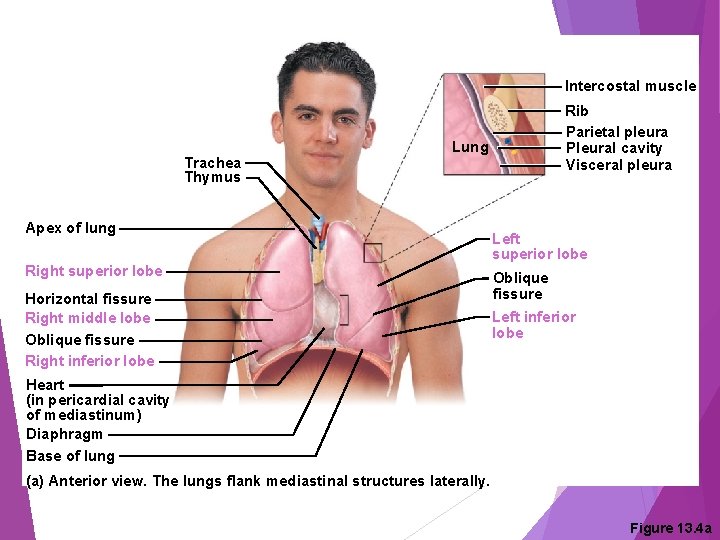
Intercostal muscle Trachea Thymus Rib Parietal pleura Pleural cavity Visceral pleura Lung Apex of lung Right superior lobe Horizontal fissure Right middle lobe Oblique fissure Right inferior lobe Left superior lobe Oblique fissure Left inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. Figure 13. 4 a
Vertebra Posterior Right lung Parietal pleura Esophagus (in posterior mediastinum) Root of lung at hilum • Left main bronchus • Left pulmonary artery • Left pulmonary vein Visceral pleura Left lung Pleural cavity Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Anterior mediastinum Sternum Anterior (b) Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. Figure 13. 4 b

Coverings of the Lungs Serosa covers the outer surface of the lungs Pulmonary (visceral) pleura covers the lung surface Parietal pleura lines the walls of the thoracic cavity Pleural fluid fills the area between layers of pleura to allow gliding These two pleural layers resist being pulled apart
Intercostal muscle Trachea Thymus Rib Parietal pleura Pleural cavity Visceral pleura Lung Apex of lung Right superior lobe Horizontal fissure Right middle lobe Oblique fissure Right inferior lobe Left superior lobe Oblique fissure Left inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. Figure 13. 4 a
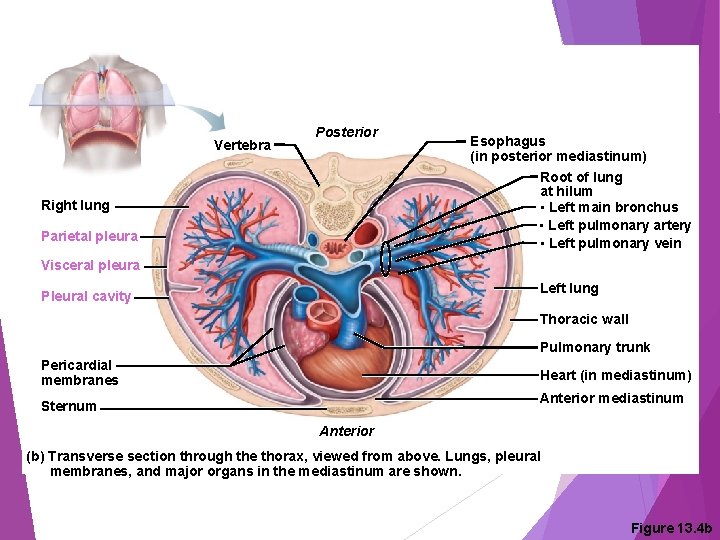
Vertebra Posterior Right lung Parietal pleura Esophagus (in posterior mediastinum) Root of lung at hilum • Left main bronchus • Left pulmonary artery • Left pulmonary vein Visceral pleura Left lung Pleural cavity Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Anterior mediastinum Sternum Anterior (b) Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. Figure 13. 4 b
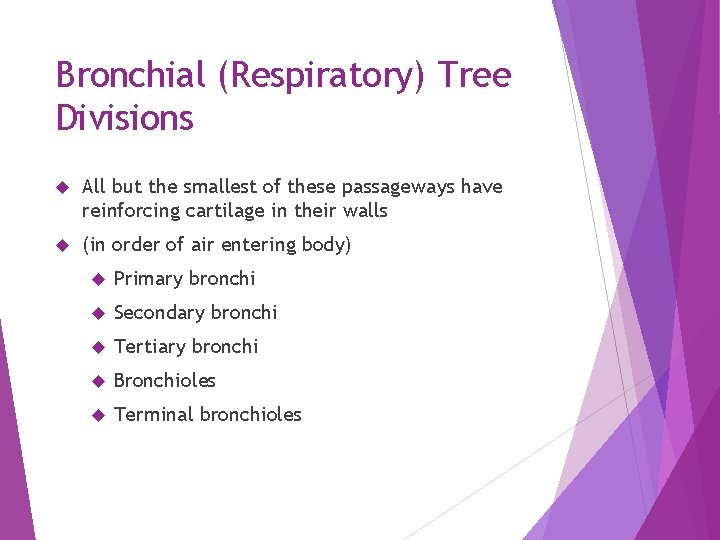
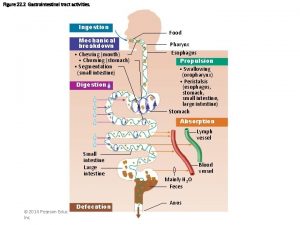
Bronchial (Respiratory) Tree Divisions All but the smallest of these passageways have reinforcing cartilage in their walls (in order of air entering body) Primary bronchi Secondary bronchi Tertiary bronchi Bronchioles Terminal bronchioles
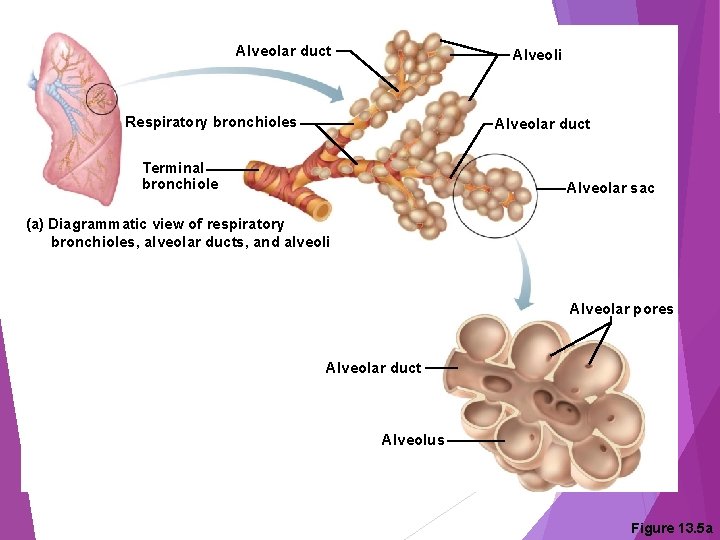
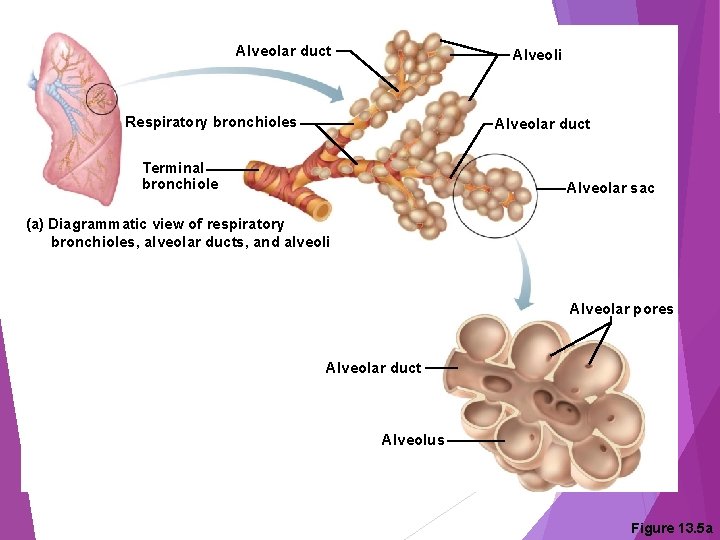
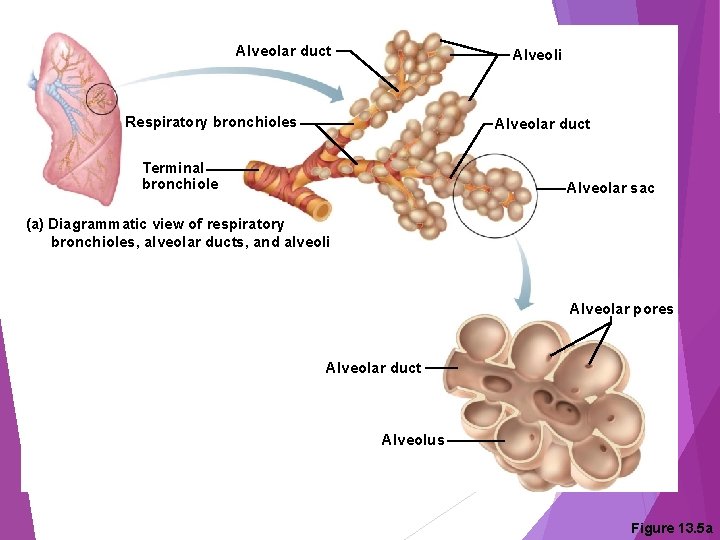
Alveolar duct Alveoli Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac (a) Diagrammatic view of respiratory bronchioles, alveolar ducts, and alveoli Alveolar pores Alveolar duct Alveolus Figure 13. 5 a
Respiratory Zone Structures Respiratory bronchioles Alveolar ducts Alveolar sacs Alveoli (air sacs) Site of gas exchange = alveoli only
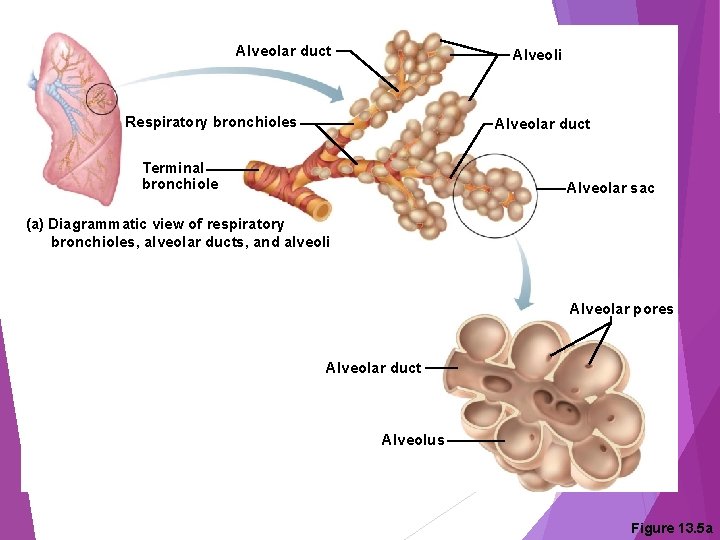
Alveolar duct Alveoli Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac (a) Diagrammatic view of respiratory bronchioles, alveolar ducts, and alveoli Alveolar pores Alveolar duct Alveolus Figure 13. 5 a
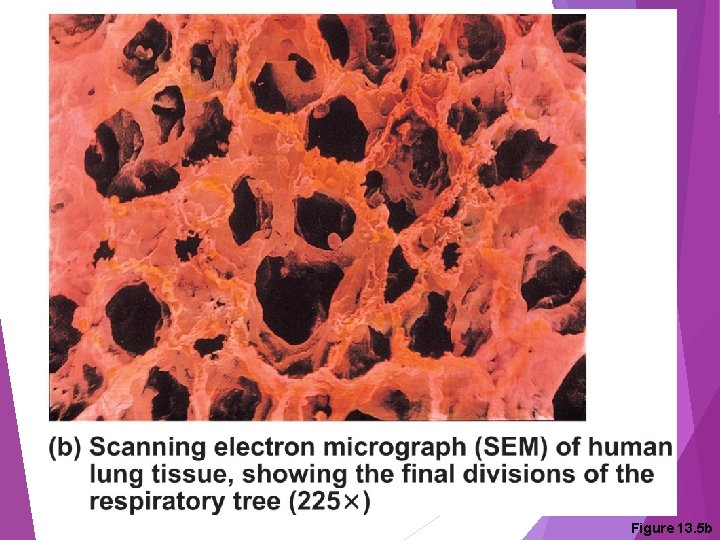
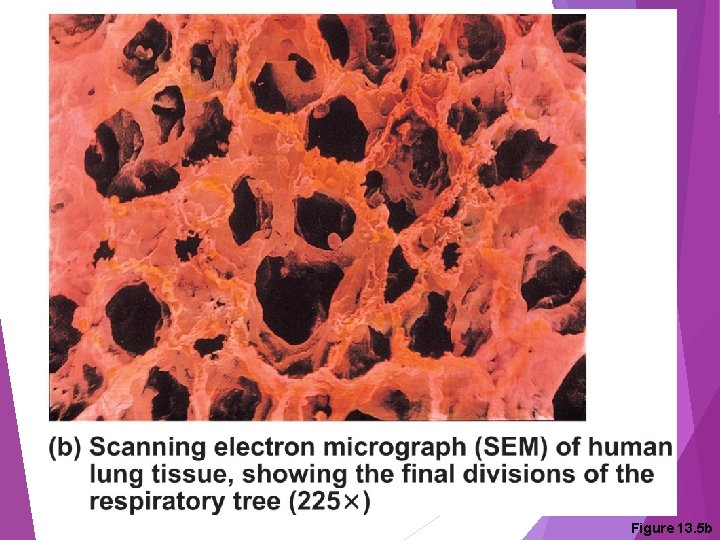
Figure 13. 5 b

Workbook Page 256 #2
Workbook Page 258 #5
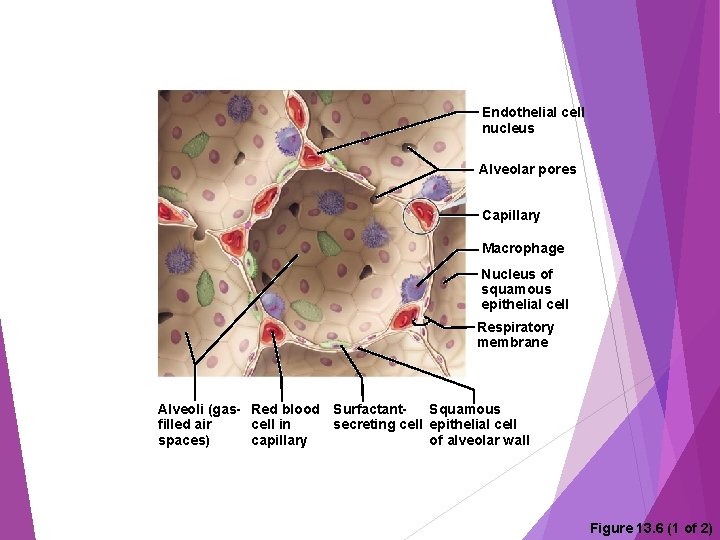
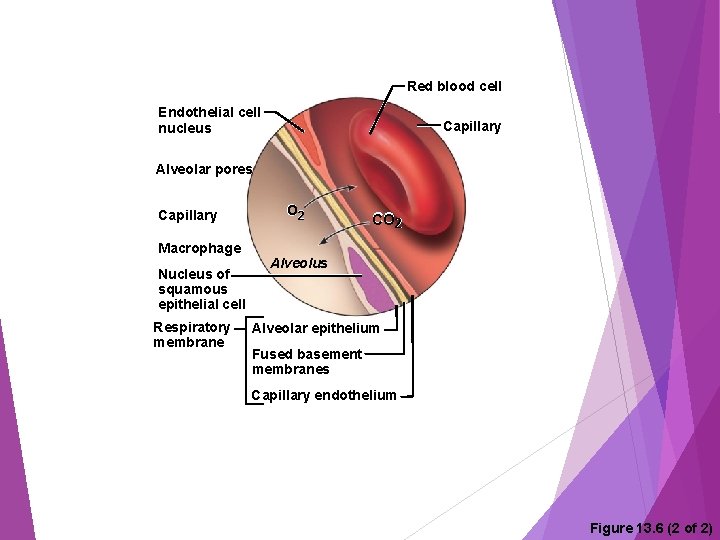
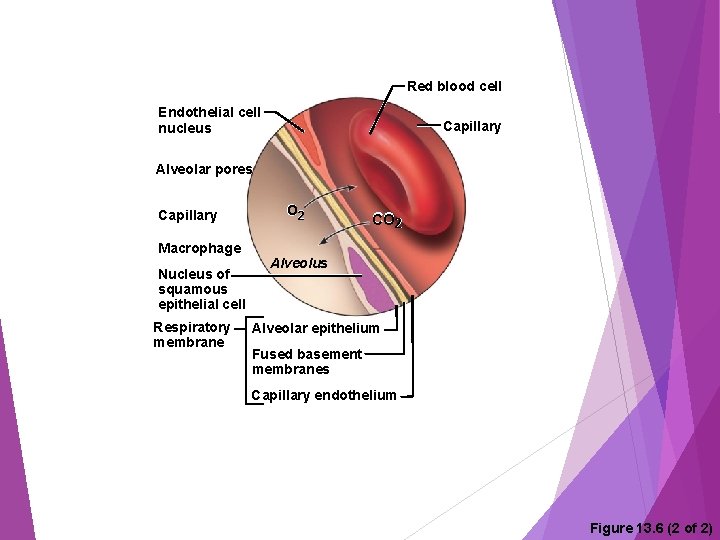
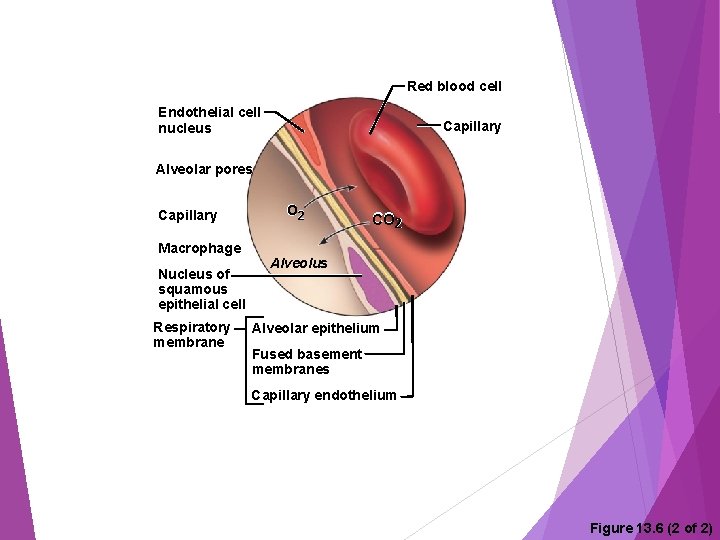
Respiratory Membrane (Air. Blood Barrier) Thin squamous epithelial layer lines alveolar walls Alveolar pores connect neighboring air sacs Pulmonary capillaries cover external surfaces of alveoli On one side of the membrane is air and on the other side is blood flowing past

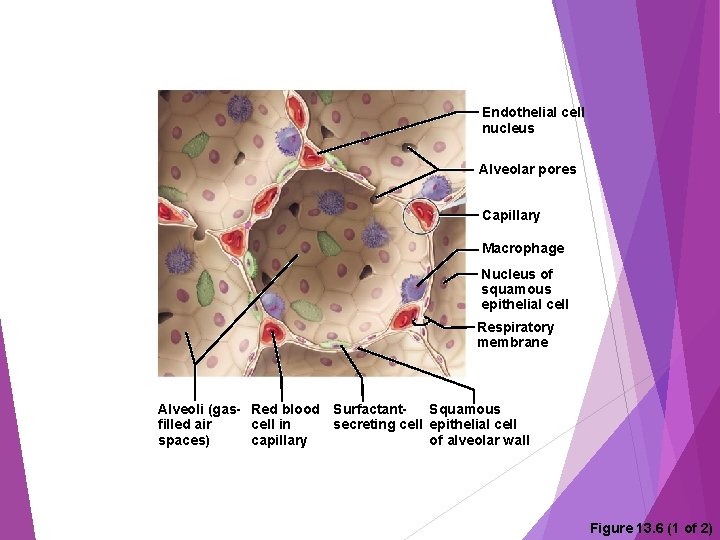
Endothelial cell nucleus Alveolar pores Capillary Macrophage Nucleus of squamous epithelial cell Respiratory membrane Alveoli (gas- Red blood Surfactant. Squamous secreting cell epithelial cell filled air cell in spaces) capillary of alveolar wall Figure 13. 6 (1 of 2)
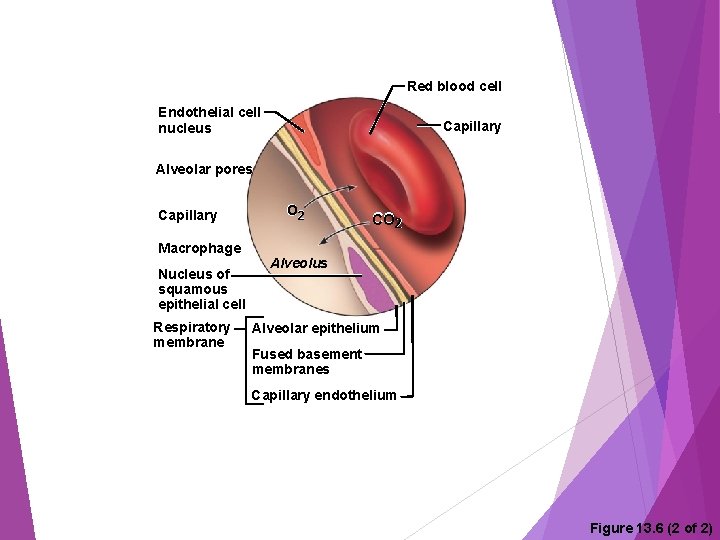
Red blood cell Endothelial cell nucleus Capillary Alveolar pores Capillary Macrophage Nucleus of squamous epithelial cell Respiratory membrane O 2 CO 2 Alveolus Alveolar epithelium Fused basement membranes Capillary endothelium Figure 13. 6 (2 of 2)

Gas Exchange Gas crosses the respiratory membrane by diffusion Oxygen enters the blood Carbon dioxide enters the alveoli Alveolar macrophages (“dust cells”) add protection by picking up bacteria, carbon particles, and other debris Surfactants (a lipid molecule) coat gas-exposed alveolar surfaces

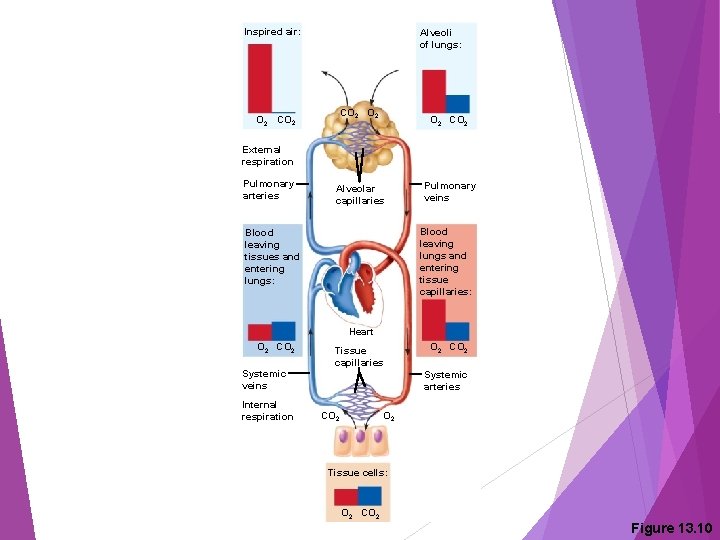
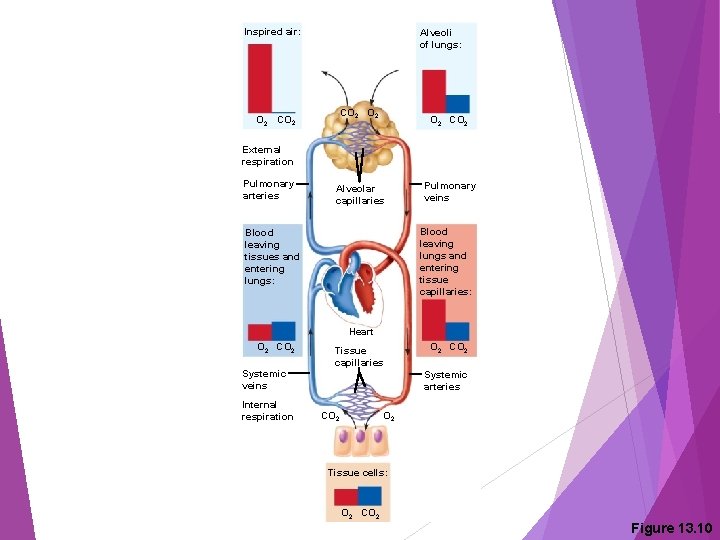
Four Events of Respiration (a) Pulmonary ventilation — moving air in and out of the lungs (commonly called breathing) (b) External respiration — gas exchange between pulmonary blood and alveoli Oxygen is loaded into the blood Carbon dioxide is unloaded from the blood
Red blood cell Endothelial cell nucleus Capillary Alveolar pores Capillary Macrophage Nucleus of squamous epithelial cell Respiratory membrane O 2 CO 2 Alveolus Alveolar epithelium Fused basement membranes Capillary endothelium Figure 13. 6 (2 of 2)
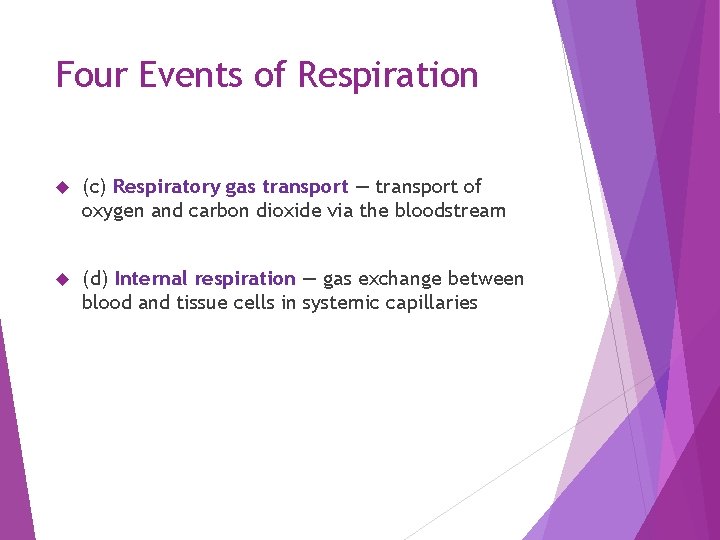
Four Events of Respiration (c) Respiratory gas transport — transport of oxygen and carbon dioxide via the bloodstream (d) Internal respiration — gas exchange between blood and tissue cells in systemic capillaries
Respiration & Gas Exchange https: //www. youtube. com/watch? v=Gjf. D 55 C 9 v 38 https: //www. youtube. com/watch? v=q. Dr. V 33 r. Zly. A
(a) Mechanics of Breathing (Pulmonary Ventilation) Completely mechanical process that depends on volume changes in the thoracic cavity Volume changes lead to pressure changes, which lead to the flow of gases to equalize pressure
Mechanics of Breathing (Pulmonary Ventilation) Two phases Inspiration = inhalation Flow of air into lungs Expiration = exhalation Air leaving lungs
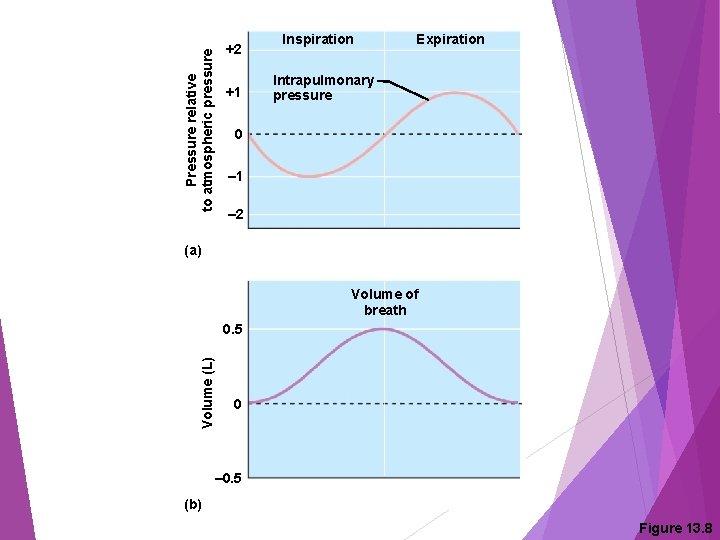
Inspiration Diaphragm and external intercostal muscles contract The size of the thoracic cavity increases External air is pulled into the lungs due to Increase in intrapulmonary volume Decrease in gas pressure

Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions Ribs elevated as external intercostals contract External intercostal muscles Full inspiration (External intercostals contract) Diaphragm moves inferiorly during contraction (a) Inspiration: Air (gases) flows into the lungs Figure 13. 7 a
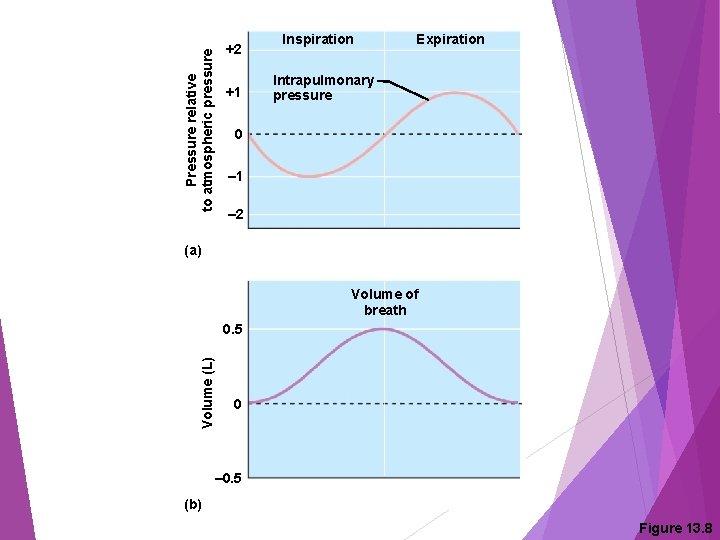
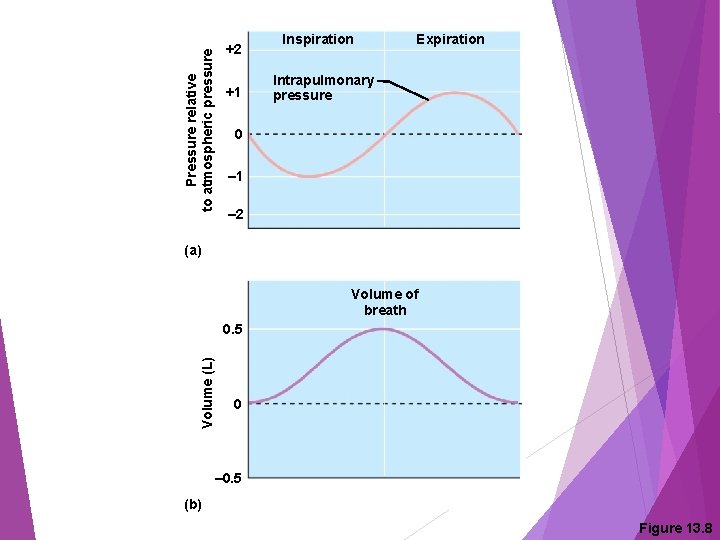
Pressure relative to atmospheric pressure +2 +1 Inspiration Expiration Intrapulmonary pressure 0 – 1 – 2 (a) Volume of breath Volume (L) 0. 5 0 – 0. 5 (b) Figure 13. 8

Expiration Largely a passive process which depends on natural lung elasticity As muscles relax, air is pushed out of the lungs due to Decrease in intrapulmonary volume Increase in gas pressure Forced expiration can occur mostly by contracting internal intercostal muscles to depress the rib cage
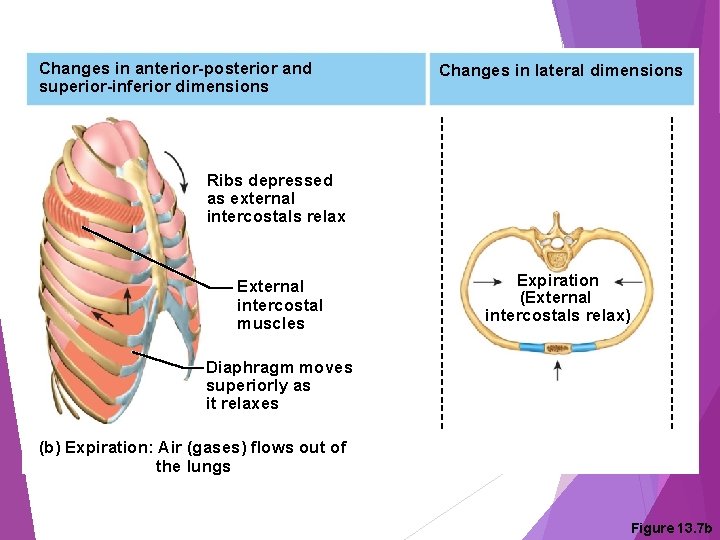
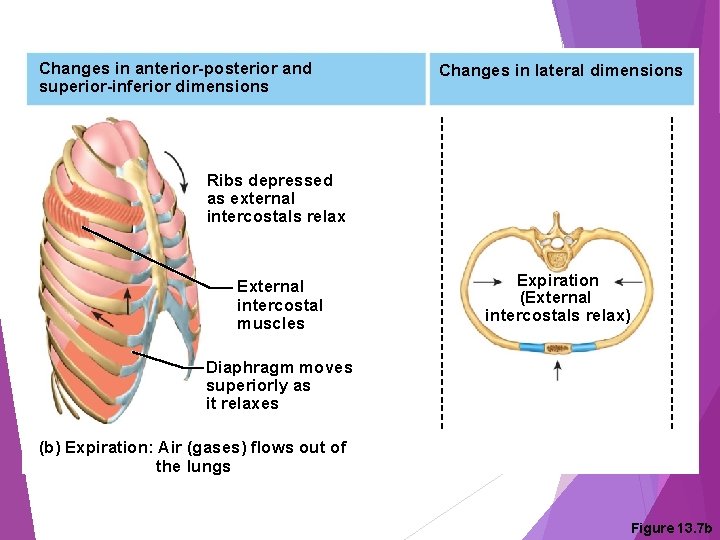
Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions Ribs depressed as external intercostals relax External intercostal muscles Expiration (External intercostals relax) Diaphragm moves superiorly as it relaxes (b) Expiration: Air (gases) flows out of the lungs Figure 13. 7 b
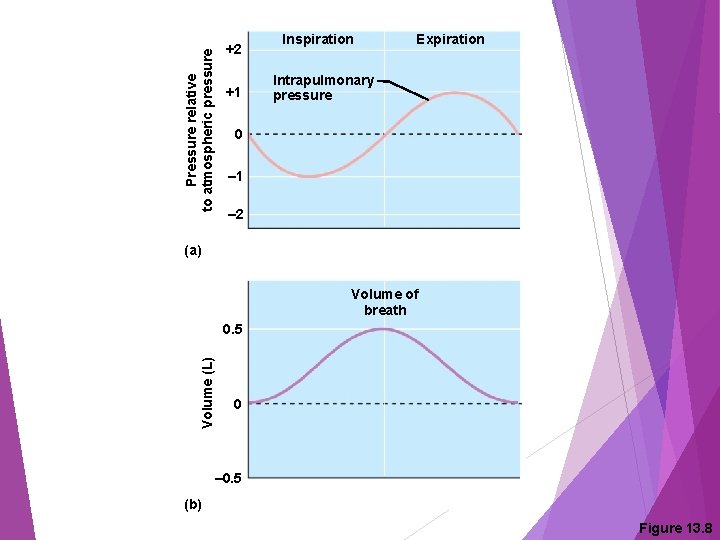
Pressure relative to atmospheric pressure +2 +1 Inspiration Expiration Intrapulmonary pressure 0 – 1 – 2 (a) Volume of breath Volume (L) 0. 5 0 – 0. 5 (b) Figure 13. 8

Workbook Page 264 #13
Pressure Differences in the Thoracic Cavity Normal pressure within the pleural space is always negative (intrapleural pressure) Differences in lung and pleural space pressures keep lungs from collapsing
Nonrespiratory Air (Gas) Movements Can be caused by reflexes or voluntary actions Examples: Cough and sneeze — clears lungs of debris Crying — emotionally induced mechanism Laughing — similar to crying Hiccup — sudden inspirations Yawn — very deep inspiration
Workbook Page 264 #15

TERMS THAT REQUIRE YOUR ATTENTION Tidal volume (TV) Inspiratory reserve volume (IRV) Expiratory reserve volume (ERV) Residual volume Vital capacity Dead space volume Functional volume
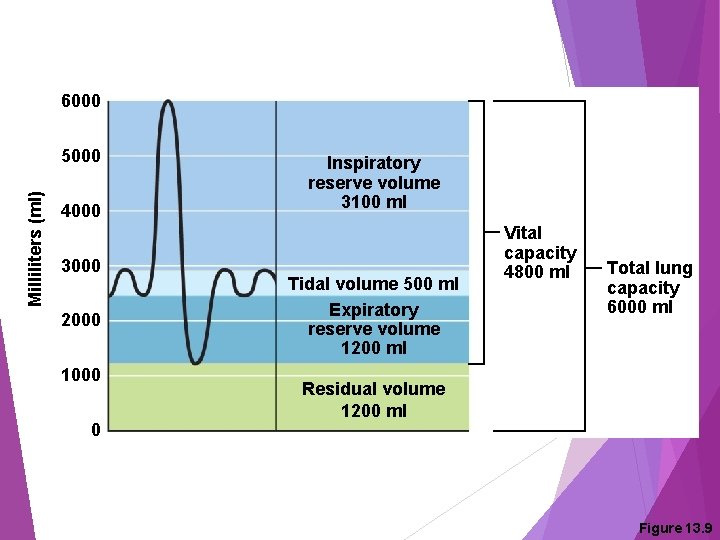
Respiratory Volumes and Capacities Normal breathing moves about 500 m. L of air with each breath This respiratory volume is tidal volume (TV) Many factors that affect respiratory capacity A person’s size Sex Age Physical condition
Respiratory Volumes and Capacities Inspiratory reserve volume (IRV) Amount of air that can be taken in forcibly over the tidal volume Usually around 3100 m. L Expiratory reserve volume (ERV) Amount of air that can be forcibly exhaled Approximately 1200 m. L
Respiratory Volumes and Capacities Residual volume Air remaining in lung after expiration About 1200 m. L
Respiratory Volumes and Capacities Vital capacity The total amount of exchangeable air Vital capacity = TV + IRV + ERV Dead space volume Air that remains in conducting zone and never reaches alveoli About 150 m. L
Respiratory Volumes and Capacities Functional volume Air that actually reaches the respiratory zone Usually about 350 m. L Respiratory capacities are measured with a spirometer
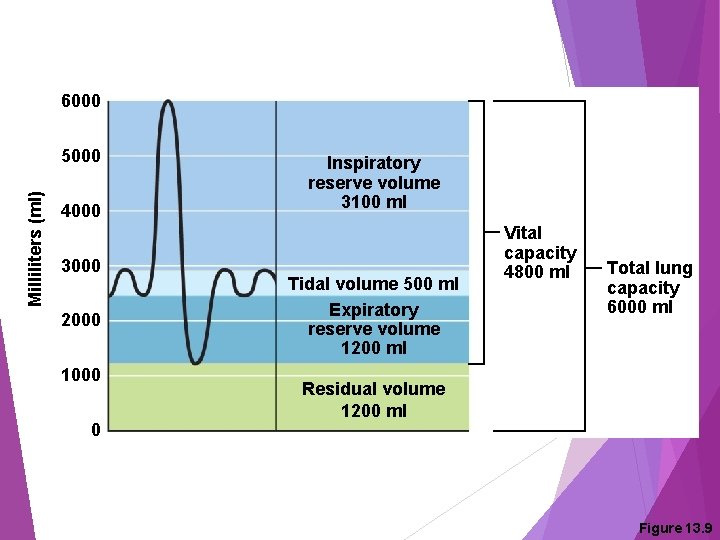
6000 Milliliters (ml) 5000 4000 3000 2000 1000 0 Inspiratory reserve volume 3100 ml Tidal volume 500 ml Expiratory reserve volume 1200 ml Vital capacity 4800 ml Total lung capacity 6000 ml Residual volume 1200 ml Figure 13. 9
Workbook Page 265 #16
Respiratory Sounds are monitored with a stethoscope Two recognizable sounds can be heard with a stethoscope (it takes practice) Bronchial sounds — produced by air rushing through large passageways such as the trachea and bronchi Vesicular breathing sounds — soft sounds of air filling alveoli
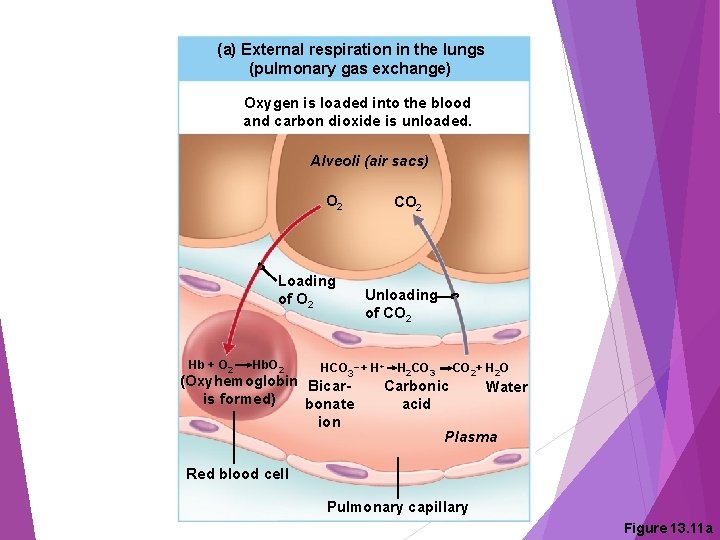
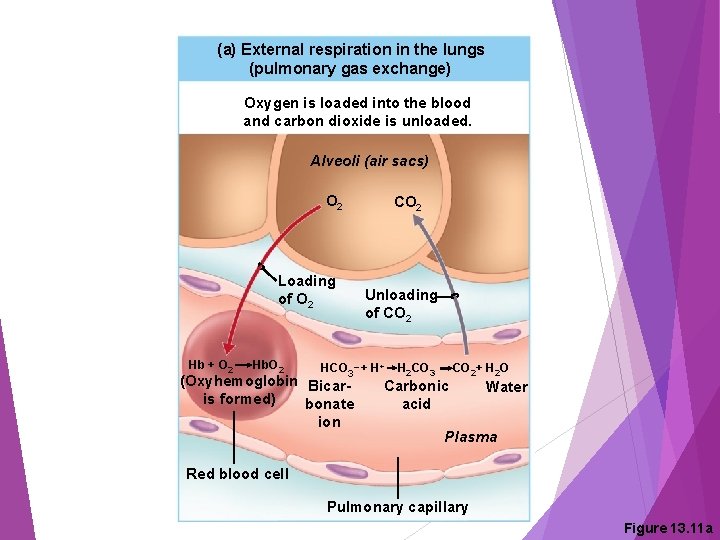
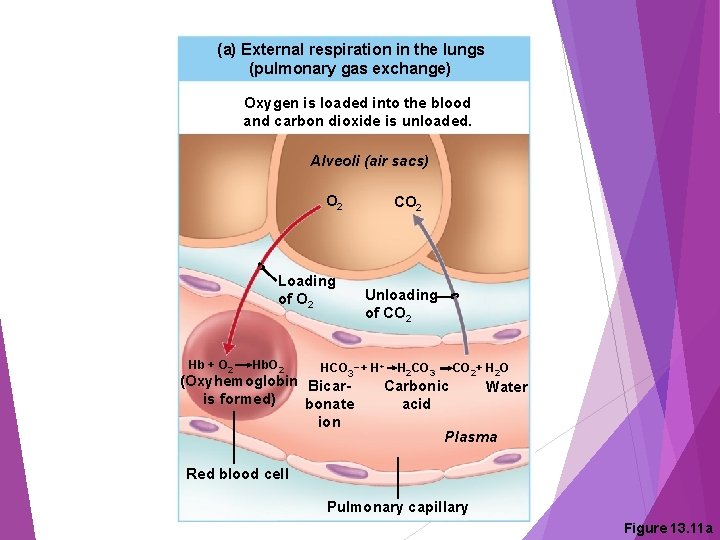
External Respiration Oxygen loaded into the blood The alveoli always have more oxygen than the blood Oxygen moves by diffusion towards the area of lower concentration Pulmonary capillary blood gains oxygen
External Respiration Carbon dioxide unloaded out of the blood Blood returning from tissues has higher concentrations of carbon dioxide than air in the alveoli Pulmonary capillary blood gives up carbon dioxide to be exhaled Blood leaving the lungs is oxygen-rich and carbon dioxide-poor
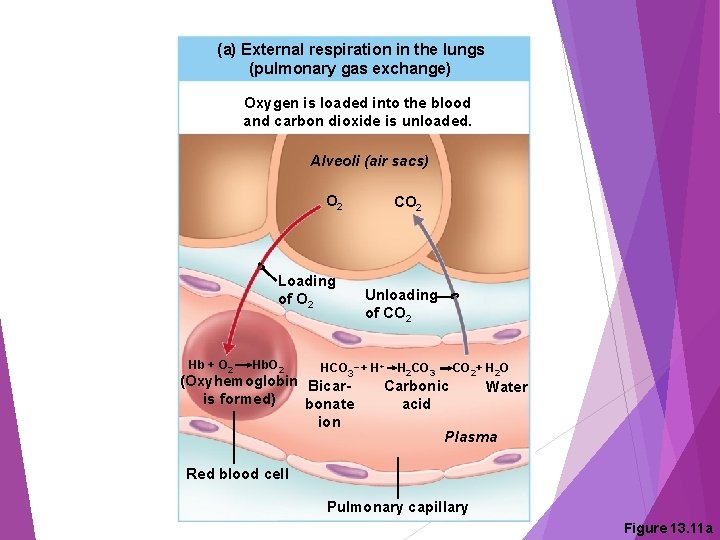
(a) External respiration in the lungs (pulmonary gas exchange) Oxygen is loaded into the blood and carbon dioxide is unloaded. Alveoli (air sacs) O 2 CO 2 Loading of O 2 Hb + O 2 Hb. O 2 Unloading of CO 2 _ HCO 3 + H+ (Oxyhemoglobin Bicaris formed) bonate ion H 2 CO 3 Carbonic acid CO 2+ H 2 O Water Plasma Red blood cell Pulmonary capillary Figure 13. 11 a
Gas Transport in the Blood Oxygen transport in the blood Most oxygen travels attached to hemoglobin and forms oxyhemoglobin (Hb. O 2) A small dissolved amount is carried in the plasma
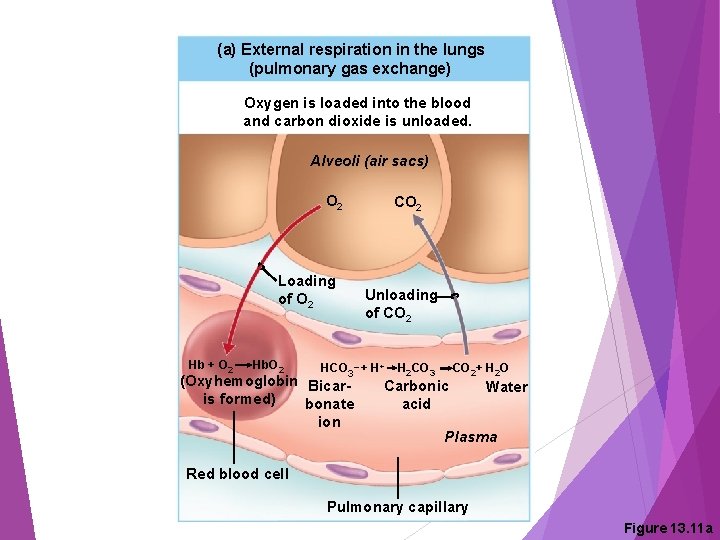
(a) External respiration in the lungs (pulmonary gas exchange) Oxygen is loaded into the blood and carbon dioxide is unloaded. Alveoli (air sacs) O 2 CO 2 Loading of O 2 Hb + O 2 Hb. O 2 Unloading of CO 2 _ HCO 3 + H+ (Oxyhemoglobin Bicaris formed) bonate ion H 2 CO 3 Carbonic acid CO 2+ H 2 O Water Plasma Red blood cell Pulmonary capillary Figure 13. 11 a
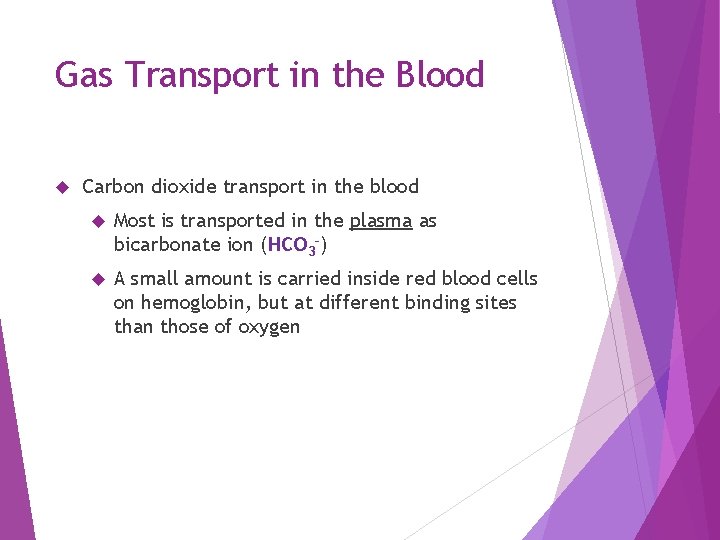
Gas Transport in the Blood Carbon dioxide transport in the blood Most is transported in the plasma as bicarbonate ion (HCO 3–) A small amount is carried inside red blood cells on hemoglobin, but at different binding sites than those of oxygen

Gas Transport in the Blood For carbon dioxide to diffuse out of blood into the alveoli, it must be released from its bicarbonate form: Bicarbonate ions enter RBC Combine with hydrogen ions Form carbonic acid (H 2 CO 3) Carbonic acid splits to form water + CO 2 Carbon dioxide diffuses from blood into alveoli
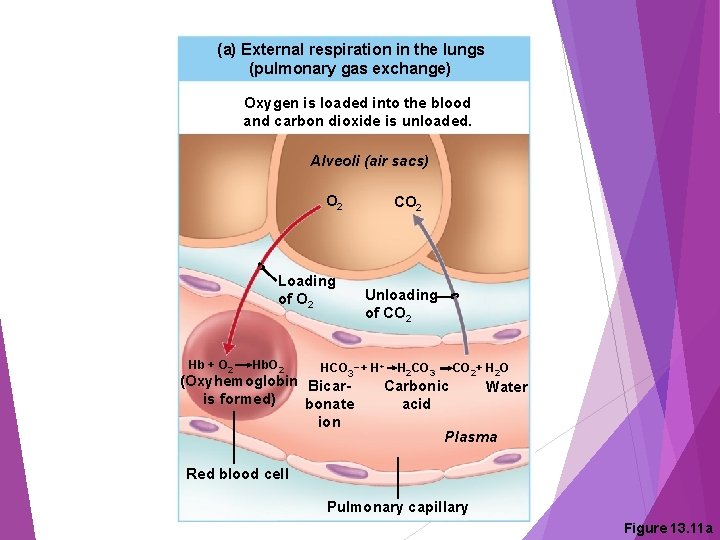
(a) External respiration in the lungs (pulmonary gas exchange) Oxygen is loaded into the blood and carbon dioxide is unloaded. Alveoli (air sacs) O 2 CO 2 Loading of O 2 Hb + O 2 Hb. O 2 Unloading of CO 2 _ HCO 3 + H+ (Oxyhemoglobin Bicaris formed) bonate ion H 2 CO 3 Carbonic acid CO 2+ H 2 O Water Plasma Red blood cell Pulmonary capillary Figure 13. 11 a

Internal Respiration Exchange of gases between blood and body cells An opposite reaction to what occurs in the lungs Carbon dioxide diffuses out of tissue to blood (called loading) Oxygen diffuses from blood into tissue (called unloading)

(b) Internal respiration in the body tissues (systemic capillary gas exchange) Oxygen is unloaded and carbon dioxide is loaded into the blood. Tissue cells CO 2 Loading of CO 2+ H 2 O H 2 CO 3 Unloading of O 2 H++ HCO 3_ Water Carbonic Bicaracid bonate Plasma ion Hb. O 2 Hb + O 2 Systemic capillary Red blood cell Figure 13. 11 b
Inspired air: Alveoli of lungs: CO 2 O 2 CO 2 External respiration Pulmonary arteries Alveolar capillaries Pulmonary veins Blood leaving lungs and entering tissue capillaries: Blood leaving tissues and entering lungs: Heart O 2 CO 2 Systemic veins Internal respiration Tissue capillaries O 2 CO 2 Systemic arteries CO 2 Tissue cells: O 2 CO 2 Figure 13. 10
Workbook Page 266 #18
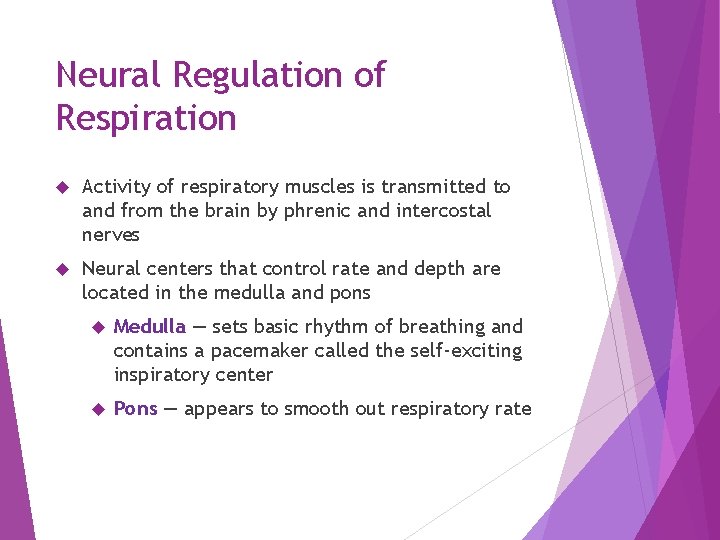
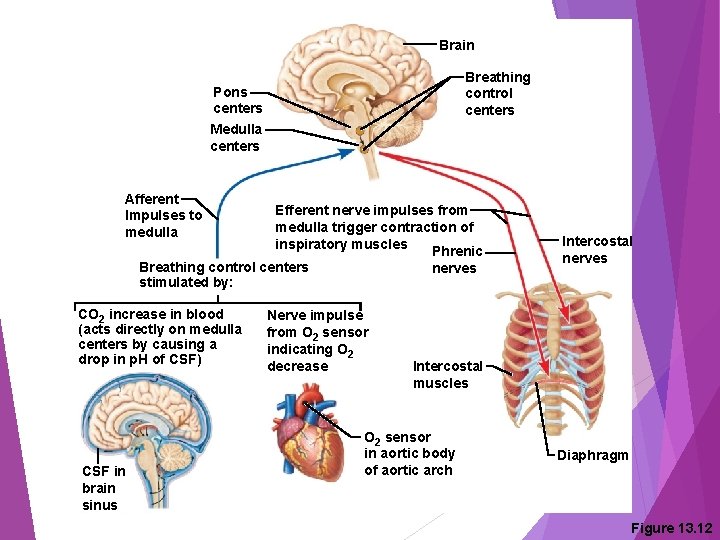
Neural Regulation of Respiration Activity of respiratory muscles is transmitted to and from the brain by phrenic and intercostal nerves Neural centers that control rate and depth are located in the medulla and pons Medulla — sets basic rhythm of breathing and contains a pacemaker called the self-exciting inspiratory center Pons — appears to smooth out respiratory rate
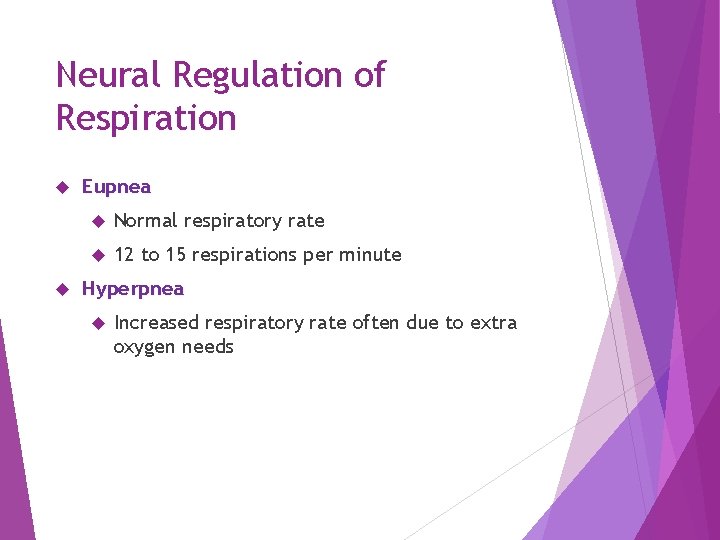
Neural Regulation of Respiration Eupnea Normal respiratory rate 12 to 15 respirations per minute Hyperpnea Increased respiratory rate often due to extra oxygen needs
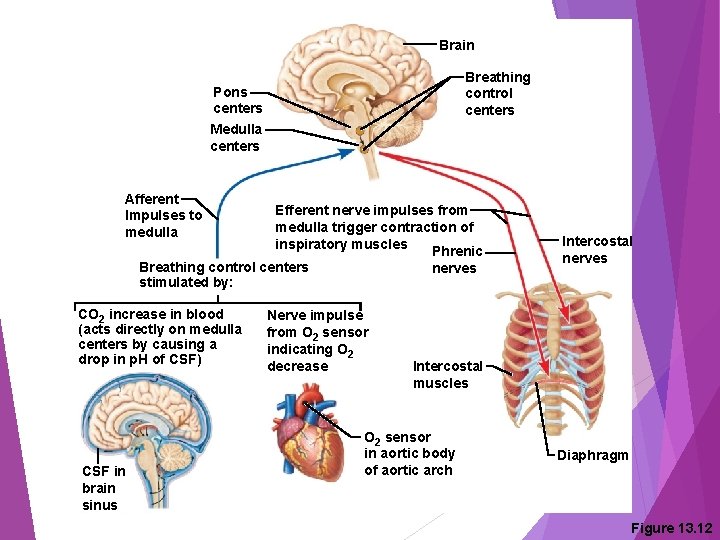
Brain Breathing control centers Pons centers Medulla centers Afferent Impulses to medulla Efferent nerve impulses from medulla trigger contraction of inspiratory muscles Phrenic Breathing control centers nerves stimulated by: CO 2 increase in blood (acts directly on medulla centers by causing a drop in p. H of CSF) CSF in brain sinus Nerve impulse from O 2 sensor indicating O 2 decrease Intercostal nerves Intercostal muscles O 2 sensor in aortic body of aortic arch Diaphragm Figure 13. 12
Non-Neural Factors Influencing Respiratory Rate and Depth (a) Physical factors Increased body temperature Exercise Talking Coughing (b) Volition (conscious control) (c) Emotional factors

Non-Neural Factors Influencing Respiratory Rate and Depth (d 1) Chemical factors: CO 2 levels The body’s need to rid itself of CO 2 is the most important stimulus Increased levels of carbon dioxide (and thus, a decreased or acidic p. H) in the blood increase the rate and depth of breathing Changes in carbon dioxide act directly on the medulla oblongata
Non-Neural Factors Influencing Respiratory Rate and Depth (d 2) Chemical factors: oxygen levels Changes in oxygen concentration in the blood are detected by chemoreceptors in the aorta and common carotid artery Information is sent to the medulla
Hyperventilation and Hypoventilation Hyperventilation Results from increased CO 2 in the blood (acidosis) Breathing becomes deeper and more rapid Blows off more CO 2 to restore normal blood p. H
Hyperventilation and Hypoventilation Results when blood becomes alkaline (alkalosis) Extremely slow or shallow breathing Allows CO 2 to accumulate in the blood
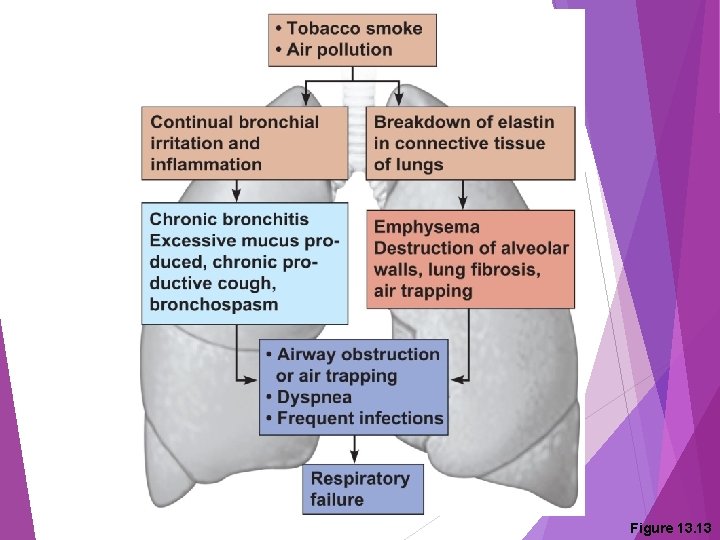
Respiratory Disorders: Chronic Obstructive Pulmonary Disease (COPD) Exemplified by chronic bronchitis and emphysema Major causes of death and disability in the United States
Respiratory Disorders: Chronic Obstructive Pulmonary Disease (COPD) Features of these diseases Patients almost always have a history of smoking Labored breathing (dyspnea) becomes progressively more severe Coughing and frequent pulmonary infections are common Most victims are hypoxic, retain carbon dioxide, and have respiratory acidosis Those infected will ultimately develop respiratory failure
Respiratory Disorders: Chronic Bronchitis xxxxxx Mucosa of the lower respiratory passages becomes severely inflamed Mucus production increases Pooled mucus impairs ventilation and gas exchange Risk of lung infection increases Pneumonia is common Called “blue bloaters” due to hypoxia and cyanosis
Respiratory Disorders: Emphysema Alveoli enlarge as adjacent chambers break through Chronic inflammation promotes lung fibrosis Airways collapse during expiration Patients use a large amount of energy to exhale Overinflation of the lungs leads to a permanently expanded barrel chest Cyanosis appears late in the disease; sufferers are often called “pink puffers”
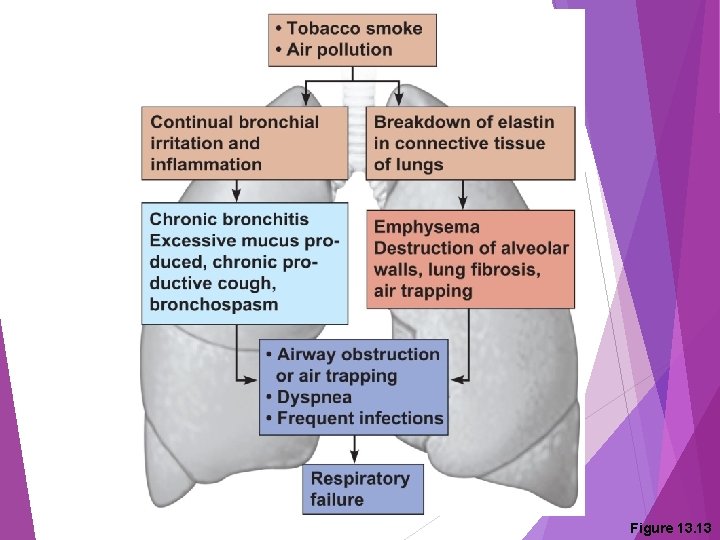
Figure 13. 13
Lung Cancer Accounts for one-third of all cancer deaths in the United States Increased incidence is associated with smoking Three common types Squamous cell carcinoma Adenocarcinoma Small cell carcinoma
Developmental Aspects of the Respiratory System Lungs are filled with fluid in the fetus Lungs are not fully inflated with air until two weeks after birth Surfactant is a fatty molecule made by alveolar cells Lowers alveolar surface tension so that lungs do not collapse between breaths Not present until late in fetal development and may not be present in premature babies Appears around 28 to 30 weeks of pregnancy
Developmental Aspects of the Respiratory System Homeostatic imbalance Infant respiratory distress syndrome (IRDS)— surfactant production is inadequate Cystic fibrosis—oversecretion of thick mucus clogs the respiratory system
Developmental Aspects of the Respiratory System Respiratory rate changes throughout life Newborns: 40 to 80 respirations per minute Infants: 30 respirations per minute Age 5: 25 respirations per minute Adults: 12 to 18 respirations per minute Rate often increases somewhat with old age
Developmental Aspects of the Respiratory System Sudden Infant Death Syndrome (SIDS) Apparently healthy infant stops breathing and dies during sleep Some cases are thought to be a problem of the neural respiratory control center One third of cases appear to be due to heart rhythm abnormalities Recent research shows a genetic component
Developmental Aspects of the Respiratory System Asthma Chronic inflamed hypersensitive bronchiole passages Response to irritants with dyspnea, coughing, and wheezing
Developmental Aspects of the Respiratory System Aging effects Elasticity of lungs decreases Vital capacity decreases Blood oxygen levels decrease Stimulating effects of carbon dioxide decrease Elderly are often hypoxic and exhibit sleep apnea More risks of respiratory tract infection
 Which organs are involved in respiratory system
Which organs are involved in respiratory system Respiratory system organs
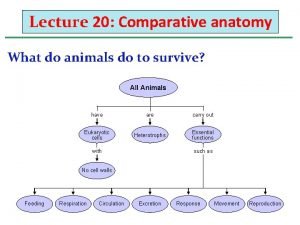
Respiratory system organs Invertebrate digestive system
Invertebrate digestive system Respiratory organs of invertebrates
Respiratory organs of invertebrates Organs forming the respiratory passageway
Organs forming the respiratory passageway Parts of the upper respiratory tract
Parts of the upper respiratory tract Figure 13-2 respiratory system
Figure 13-2 respiratory system Respiratory zone and conducting zone
Respiratory zone and conducting zone Site:slidetodoc.com
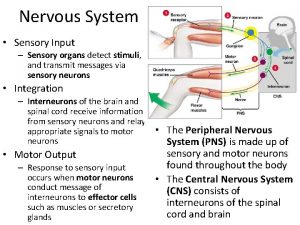
Site:slidetodoc.com Sensory system organs
Sensory system organs Major functions of the excretory system
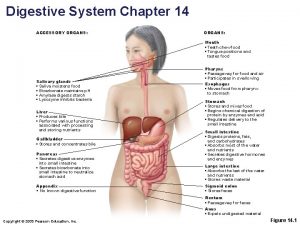
Major functions of the excretory system Accessory organ of the digestive system
Accessory organ of the digestive system Accessory organs of the digestive system
Accessory organs of the digestive system Major and accessory organs of the digestive system
Major and accessory organs of the digestive system Red and white blood cells difference
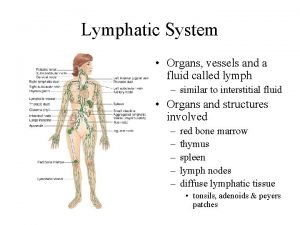
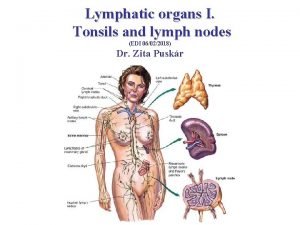
Red and white blood cells difference Lymphatic system organs
Lymphatic system organs Lymph nodules
Lymph nodules Lymphatic system organs and functions
Lymphatic system organs and functions Organs of the sensory system
Organs of the sensory system Chapter 16 matching question 6-10
Chapter 16 matching question 6-10 Tiny air sacs at the end of the bronchioles
Tiny air sacs at the end of the bronchioles Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Itpd
Itpd What are homologous analogous and vestigial structures
What are homologous analogous and vestigial structures The organs of articulation
The organs of articulation Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Infrahepatic space
Infrahepatic space Peritoneum serous membrane
Peritoneum serous membrane Greater sac lesser sac
Greater sac lesser sac Adh hormone produced by
Adh hormone produced by Bee organs
Bee organs Main excretory organs
Main excretory organs What organ
What organ Sense organs
Sense organs Organs homolegs ejemplos
Organs homolegs ejemplos Description of the larynx
Description of the larynx Major plant organs
Major plant organs Origin of phonetics
Origin of phonetics Articulatory organs
Articulatory organs Little organs
Little organs Protect bougainvillea from grazing animals.
Protect bougainvillea from grazing animals. Malt
Malt Nails integumentary system
Nails integumentary system Central lymphoid organs
Central lymphoid organs Articulatory organs
Articulatory organs Images of sense organs with names
Images of sense organs with names Quadrants of body and organs
Quadrants of body and organs External anatomy of frog parts and function
External anatomy of frog parts and function Urinary bladder with peritoneum
Urinary bladder with peritoneum Excreatory organ
Excreatory organ Vestigial organs
Vestigial organs Name the three organs of the government
Name the three organs of the government Regional anatomical terms
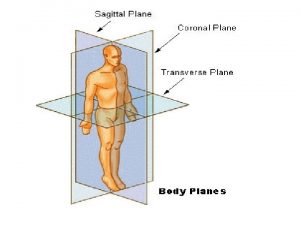
Regional anatomical terms Internal organs
Internal organs Ostium ileocaecalis
Ostium ileocaecalis Ts of liver
Ts of liver Little nicky (cat)
Little nicky (cat) Uterus perimetrium
Uterus perimetrium Plant organs
Plant organs Infindibulum
Infindibulum Yanylion
Yanylion Abdominopelvic organs
Abdominopelvic organs Right arm medical term
Right arm medical term Left lower quadrant organs female
Left lower quadrant organs female Body cavity quadrants
Body cavity quadrants Biomaterials artificial organs and tissue engineering
Biomaterials artificial organs and tissue engineering Git organs
Git organs Epiplon definicion
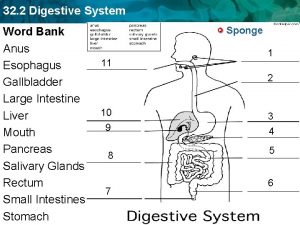
Epiplon definicion Digestive system word bank
Digestive system word bank Cephalic body region
Cephalic body region Reptiles organs for locomotion
Reptiles organs for locomotion Generative lymphoid organs
Generative lymphoid organs Six main organs of the united nations
Six main organs of the united nations Excretory organs in mammals
Excretory organs in mammals Male rat anatomy
Male rat anatomy Aphi sada u rat yaya
Aphi sada u rat yaya Organs xxx
Organs xxx Organs of speech diagram
Organs of speech diagram Stone cells in plants
Stone cells in plants Sense organs for class 1
Sense organs for class 1 What is a group of organs working together
What is a group of organs working together Frog testes
Frog testes Locomotion in fishes zoology notes
Locomotion in fishes zoology notes Main function of major organs
Main function of major organs Organs interns del cos huma
Organs interns del cos huma Rat internal organs
Rat internal organs Reptiles organs for locomotion
Reptiles organs for locomotion Reptiles organs for locomotion
Reptiles organs for locomotion Reptiles organs for locomotion
Reptiles organs for locomotion Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Plant tissue and organs
Plant tissue and organs Reproductive organs of the bull
Reproductive organs of the bull Duodemum
Duodemum Colonchyma
Colonchyma Internal organs of a fowel
Internal organs of a fowel Nine regions of the abdominopelvic cavity
Nine regions of the abdominopelvic cavity Soft paired cone shaped organs
Soft paired cone shaped organs What is gonad
What is gonad Organelles why are they important
Organelles why are they important Organs of extreme perfection
Organs of extreme perfection Gametophytes have gamete-producing organs called _____.
Gametophytes have gamete-producing organs called _____. Mesoperitoneal organs
Mesoperitoneal organs