Anatomy of the Respiratory System Includes Physiology Anatomy


















- Slides: 60
Anatomy of the Respiratory System Includes Physiology Anatomy & Physiology: Honors Turner College & Career High School 2018
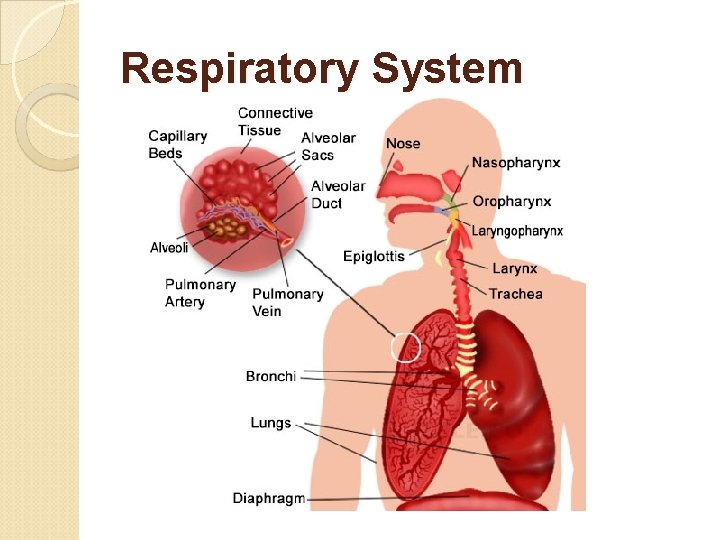
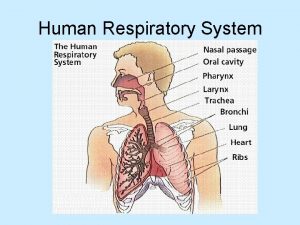
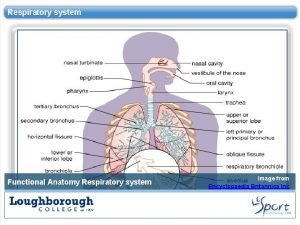
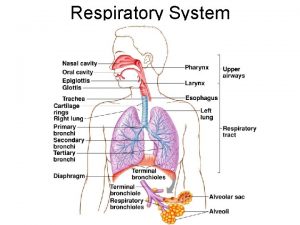
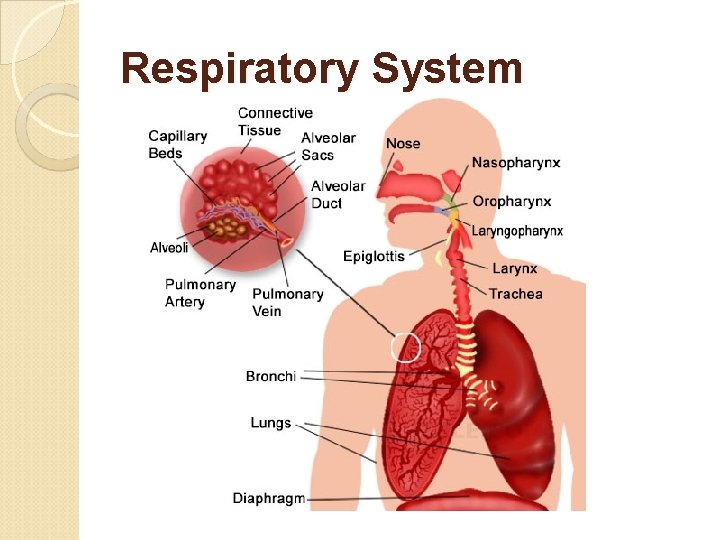
Respiratory System
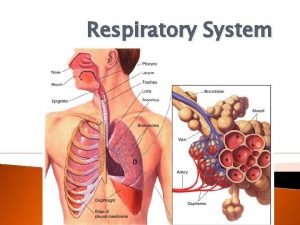
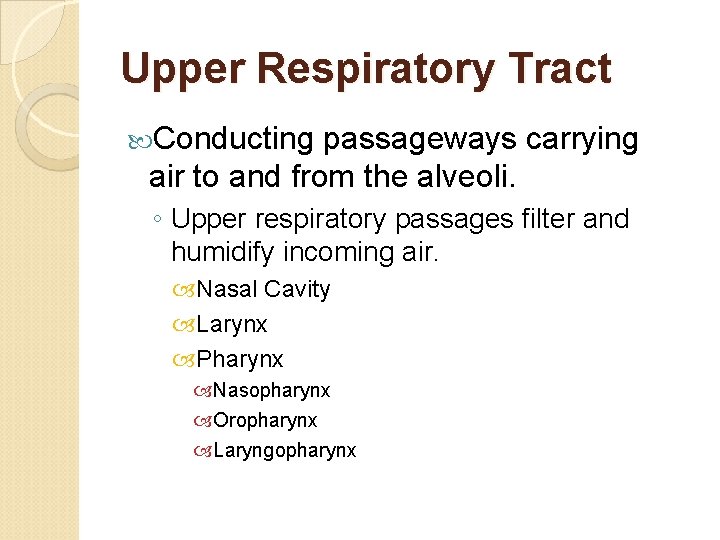
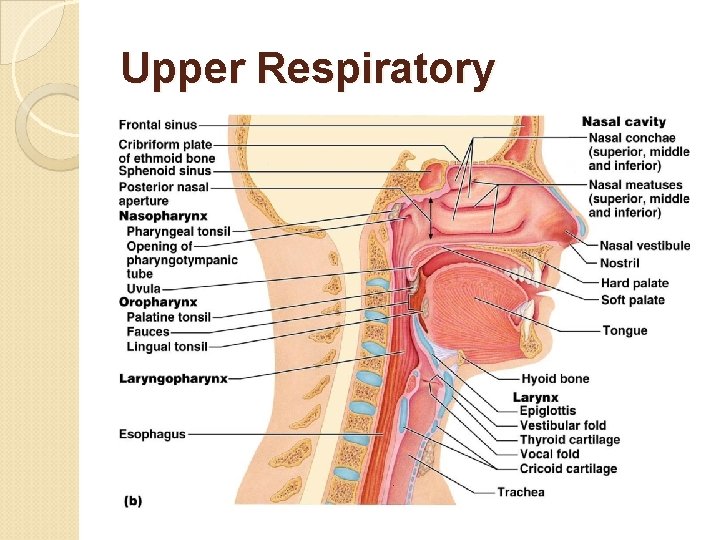
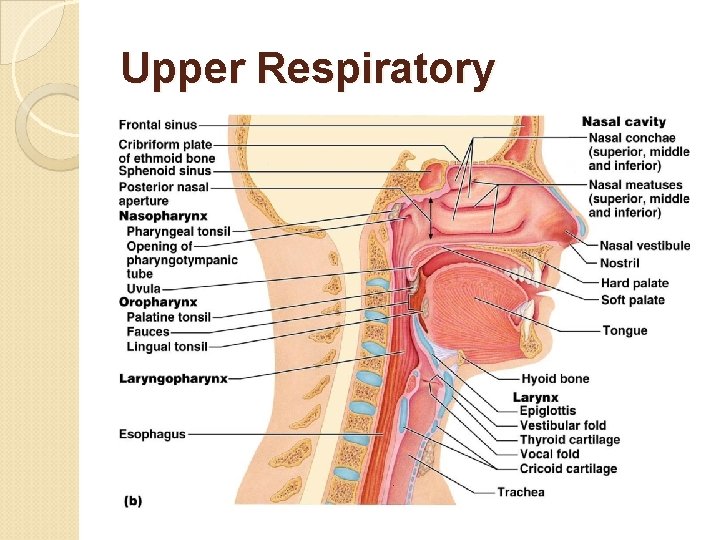
Upper Respiratory Tract Conducting passageways carrying air to and from the alveoli. ◦ Upper respiratory passages filter and humidify incoming air. Nasal Cavity Larynx Pharynx Nasopharynx Oropharynx Laryngopharynx
Lower Respiratory Tract Conducting passageways carrying air to and from the alveoli. ◦ Lower passageways include delicate conduction passages and alveolar exchange surfaces. Trachea Lungs Bronchioles Alveoli Diaphragm

Respiratory System Pathway Nasal Cavity (or oral cavity) Pharynx Trachea Primary bronchi (left or right) Secondary bronchi Tertiary bronchi Bronchioles Alveoli
Nasal Cavity Functions Provides an airway for respiration. Moistens and warms entering air. Filters and cleans inspired air. Resonating Detects chamber for speech. odors in the airstream.
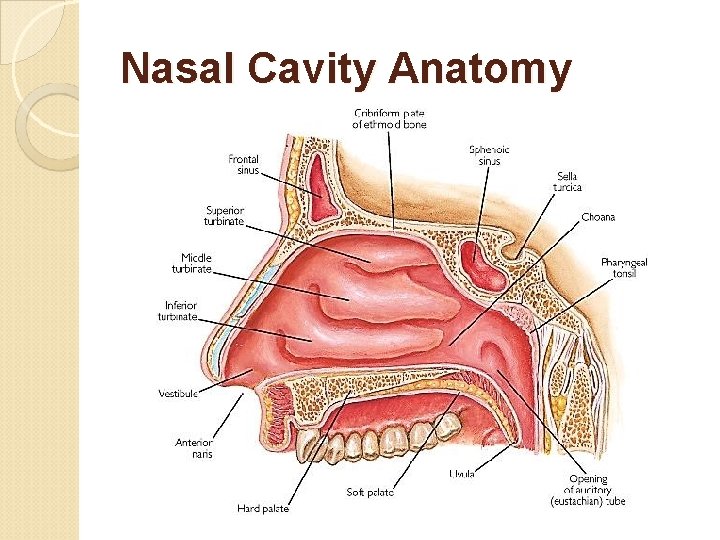
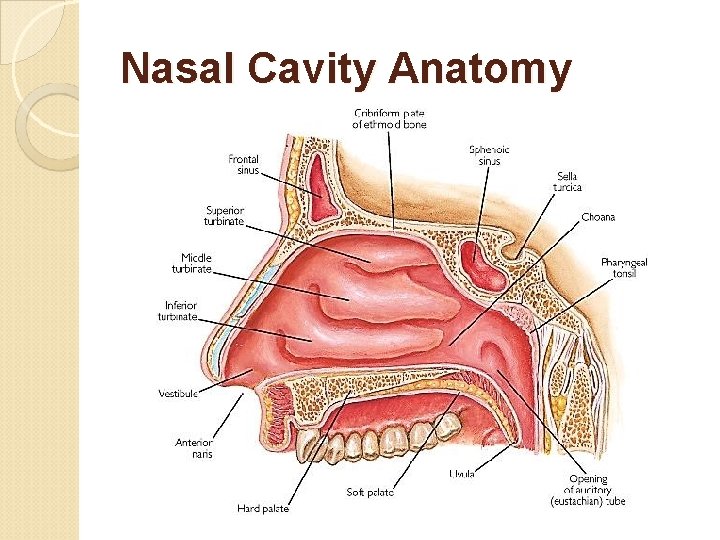
Nasal Cavity Anatomy
Nasal Cavity Anatomy Vibrissae (guard hairs) – stiff hairs that filter large particles from the air. Nasal cilia – hair-like projections that propel trapped particles towards the throat for digestion by digestive enzymes. Rich supply of capillaries warm the inspired air Nasal conchae – folds in the mucous membrane that increase air turbulence and ensures that most air contacts the mucous membranes.

Nasal Cavity Anatomy Olfactory mucosa – mucous membranes that contain smell receptors. Respiratory mucosa – pseudo-stratified ciliated columnar epithelium containing goblet cells that secrete mucus. ◦ Stickiness traps inhaled particles ◦ Lysozyme kills bacteria ◦ Lymphocytes & Ig. A antibodies protect against bacteria.
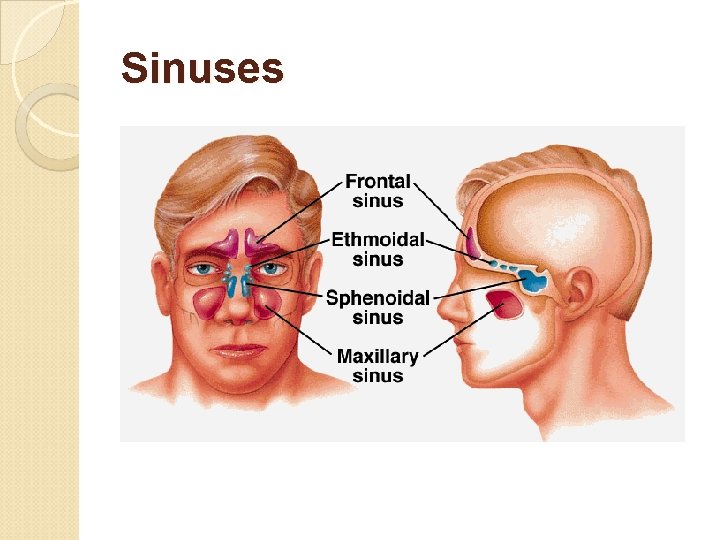
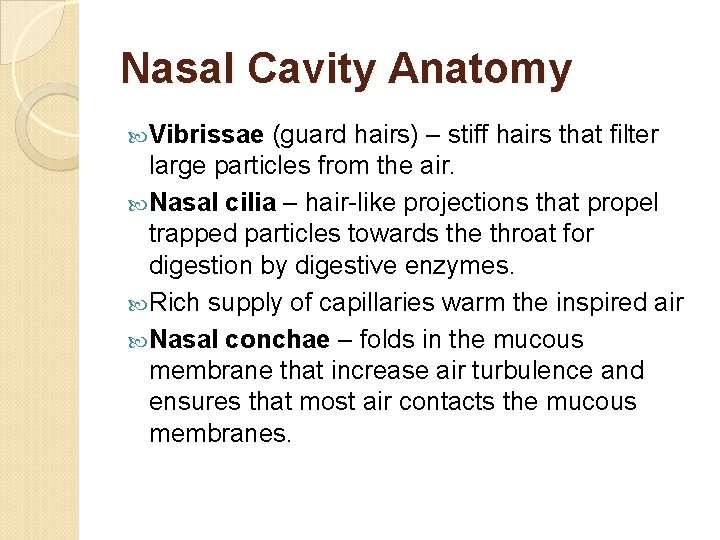
Sinuses

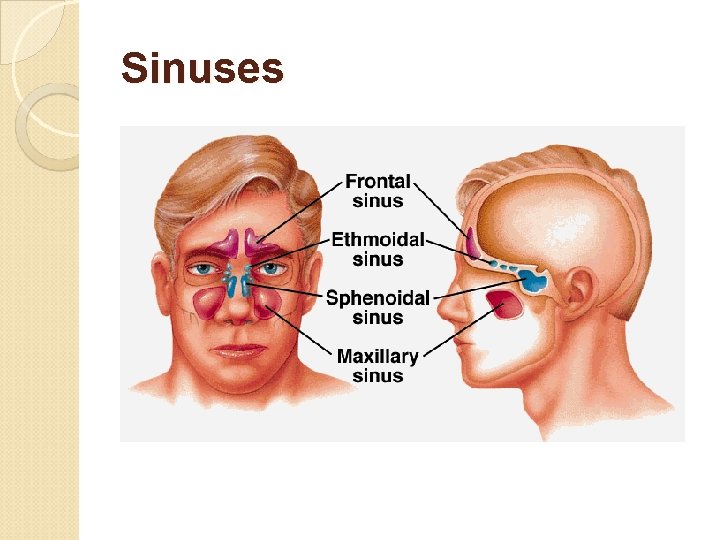
Upper Respiratory Three regions of the pharynx: • Nasopharynx – air passage (pseudostratified columnar epithelium). • Oropharynx – passageway for air, food, and drink (stratified squamous epithelium). • Laryngopharynx – passageway for air, food, and drink (stratified squamous epithelium).
Upper Respiratory
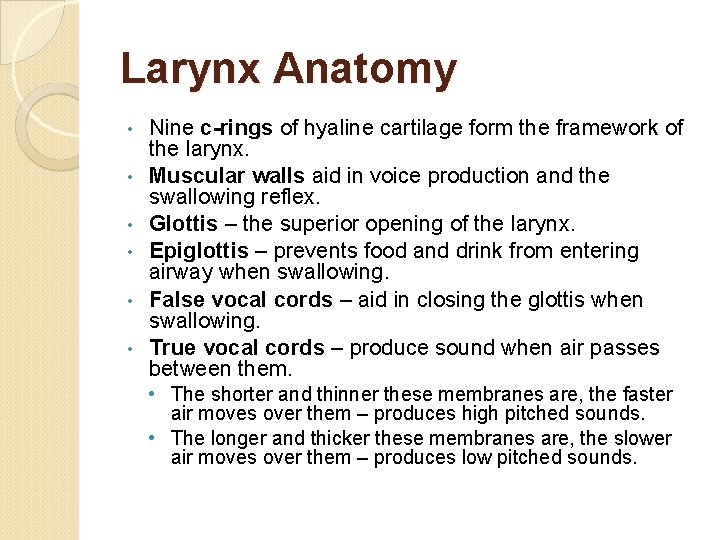
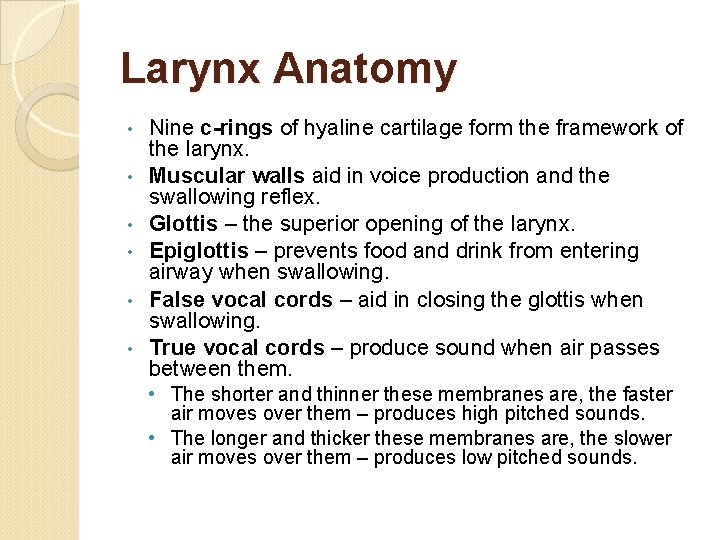
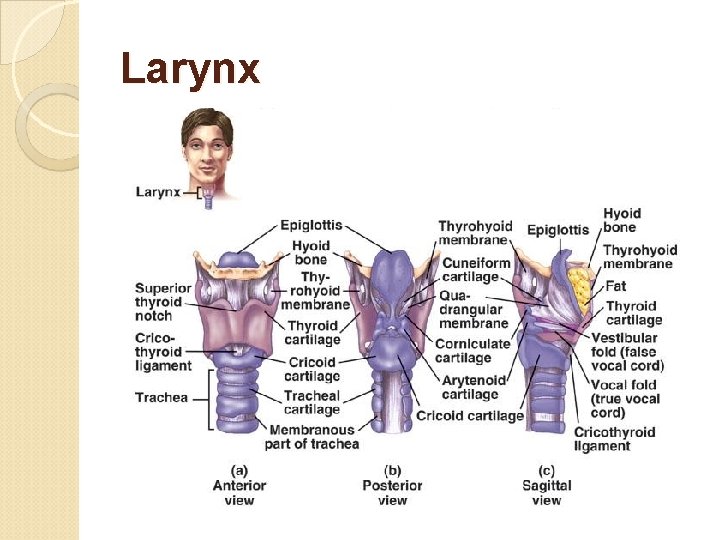
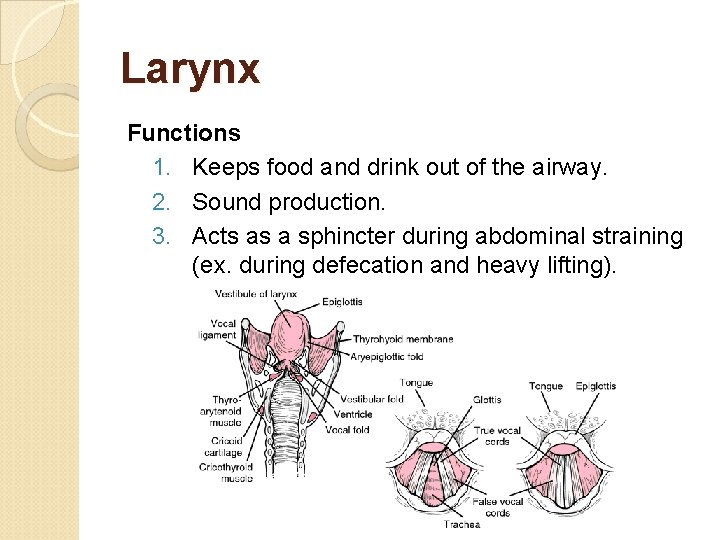
Larynx Anatomy • • • Nine c-rings of hyaline cartilage form the framework of the larynx. Muscular walls aid in voice production and the swallowing reflex. Glottis – the superior opening of the larynx. Epiglottis – prevents food and drink from entering airway when swallowing. False vocal cords – aid in closing the glottis when swallowing. True vocal cords – produce sound when air passes between them. • The shorter and thinner these membranes are, the faster air moves over them – produces high pitched sounds. • The longer and thicker these membranes are, the slower air moves over them – produces low pitched sounds.
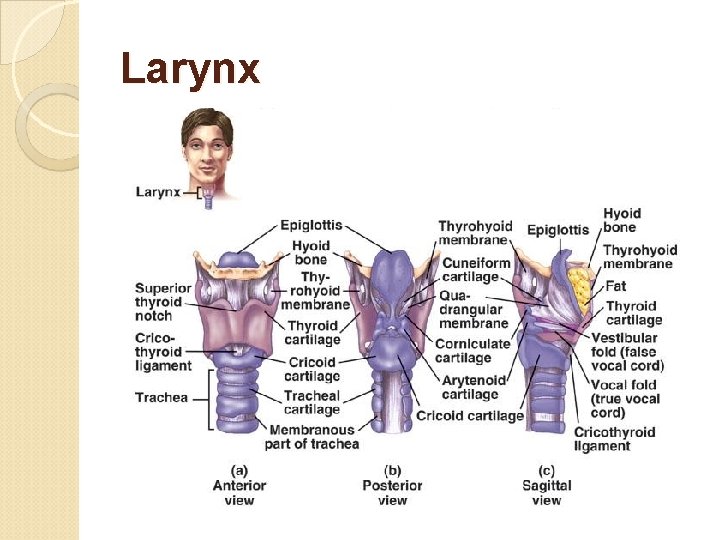
Larynx
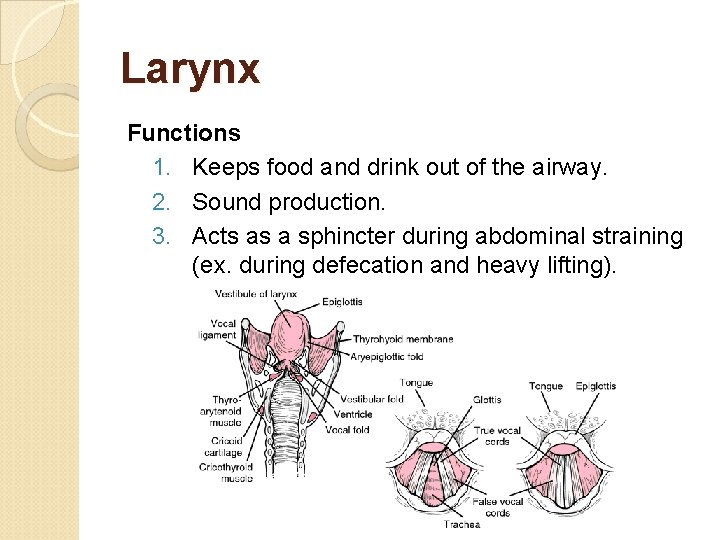
Larynx Functions 1. Keeps food and drink out of the airway. 2. Sound production. 3. Acts as a sphincter during abdominal straining (ex. during defecation and heavy lifting).
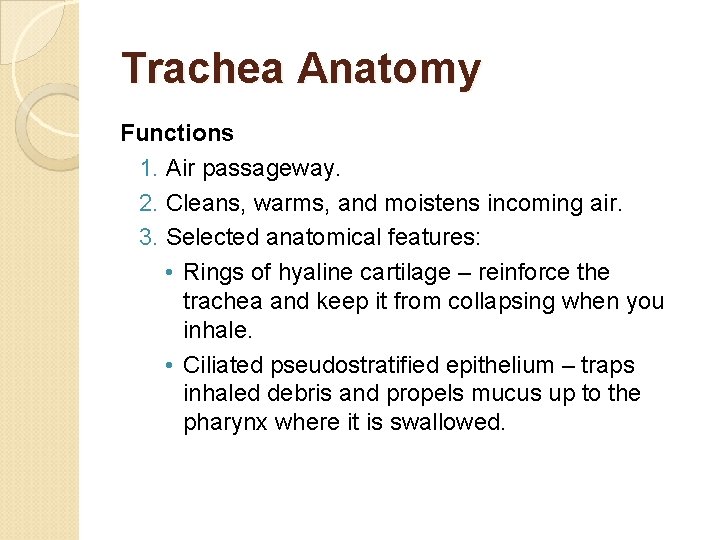
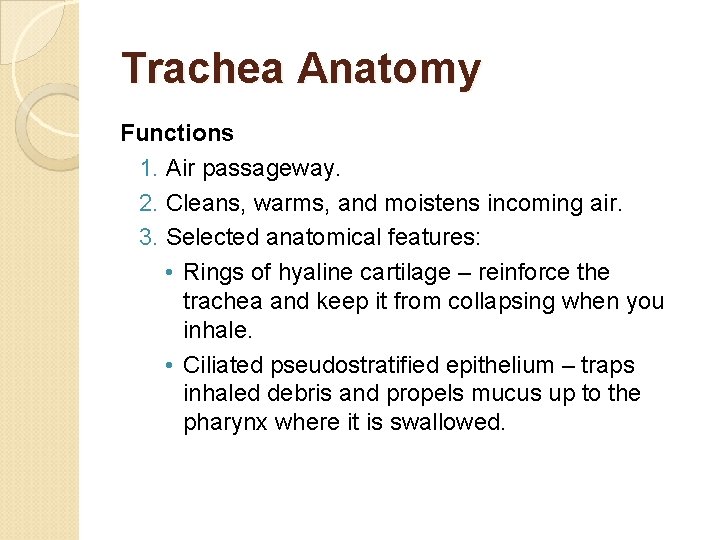
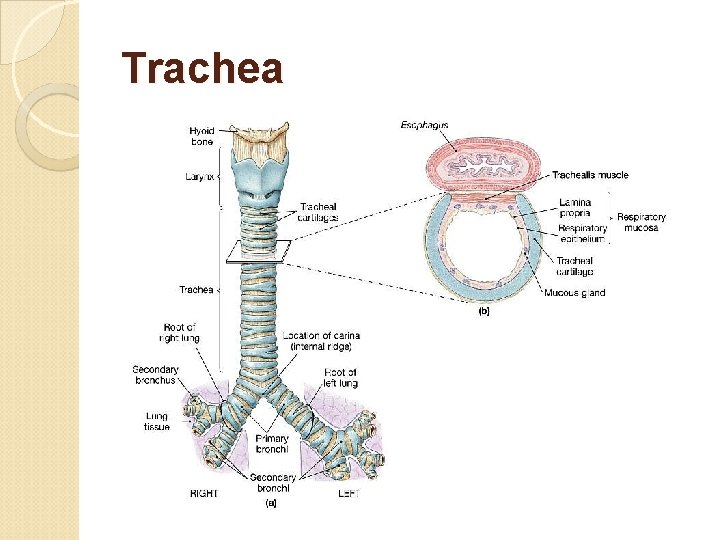
Trachea Anatomy Functions 1. Air passageway. 2. Cleans, warms, and moistens incoming air. 3. Selected anatomical features: • Rings of hyaline cartilage – reinforce the trachea and keep it from collapsing when you inhale. • Ciliated pseudostratified epithelium – traps inhaled debris and propels mucus up to the pharynx where it is swallowed.
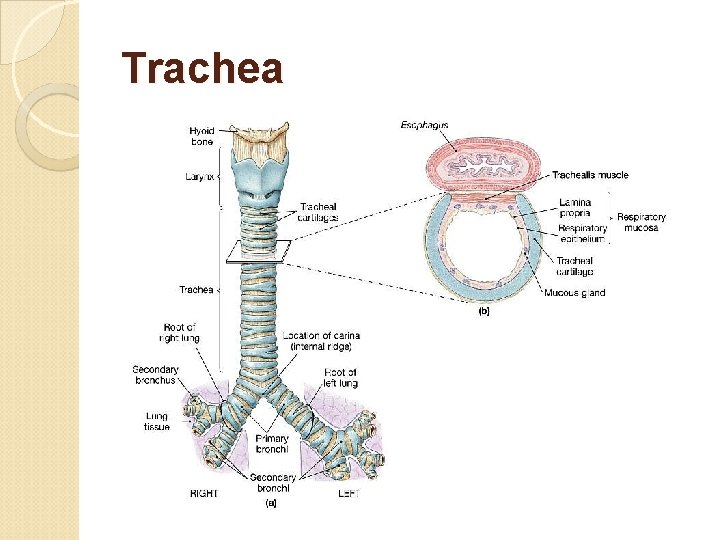
Trachea

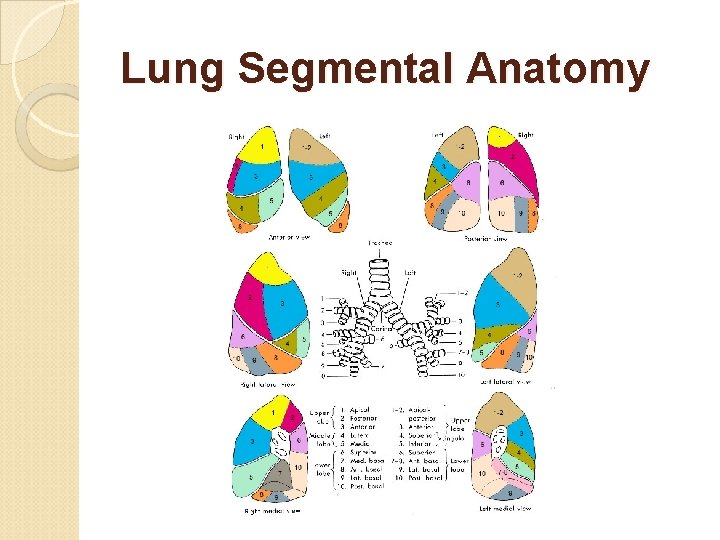
Lung Anatomy Function - Solely an air passageway.
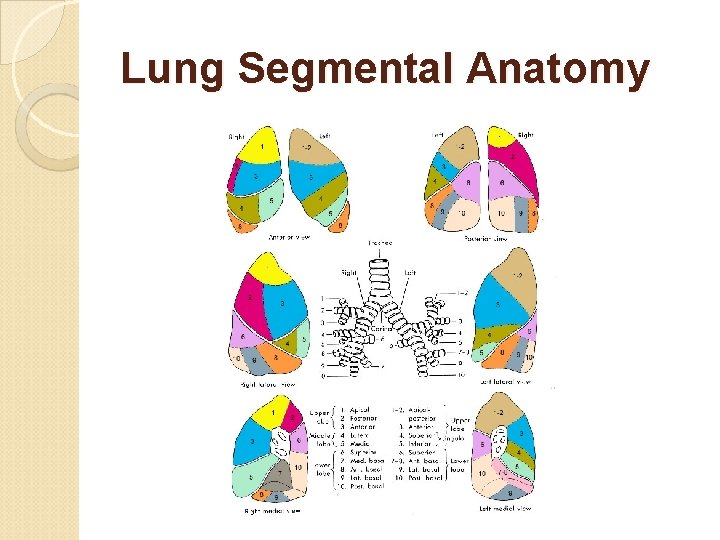
Lung Segmental Anatomy
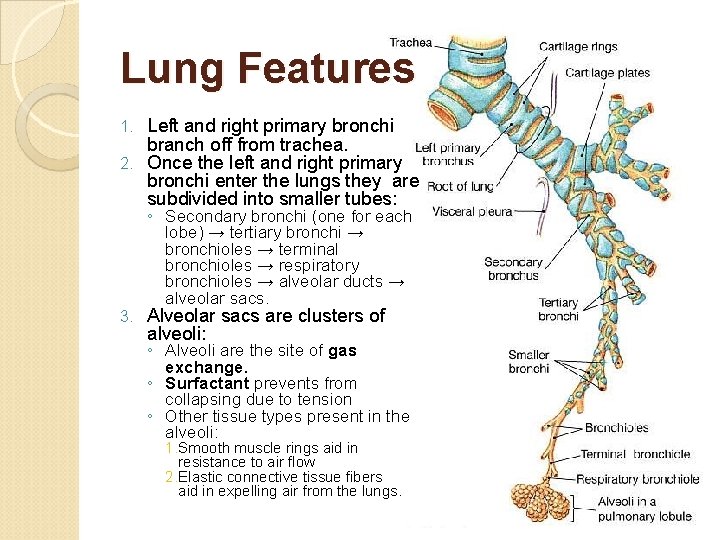
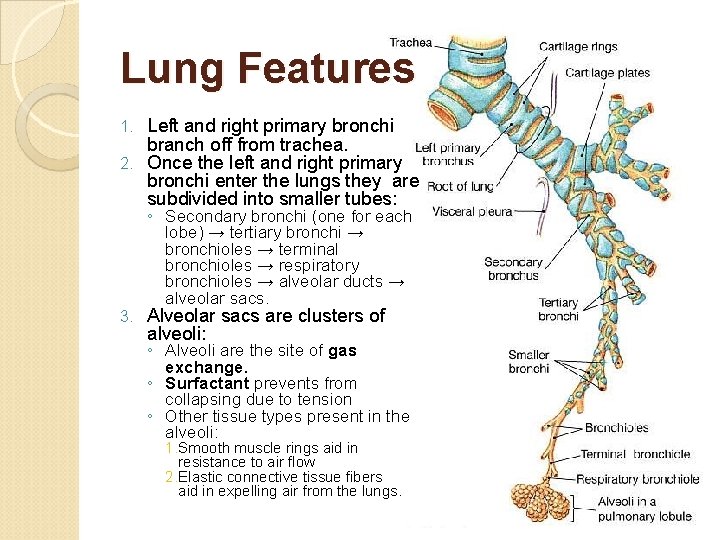
Lung Features Left and right primary bronchi branch off from trachea. 2. Once the left and right primary bronchi enter the lungs they are subdivided into smaller tubes: 1. ◦ Secondary bronchi (one for each lobe) → tertiary bronchi → bronchioles → terminal bronchioles → respiratory bronchioles → alveolar ducts → alveolar sacs. 3. Alveolar sacs are clusters of alveoli: ◦ Alveoli are the site of gas exchange. ◦ Surfactant prevents from collapsing due to tension ◦ Other tissue types present in the alveoli: 1. Smooth muscle rings aid in resistance to air flow 2. Elastic connective tissue fibers aid in expelling air from the lungs.



Normal Lungs
Cystic Fibrosis
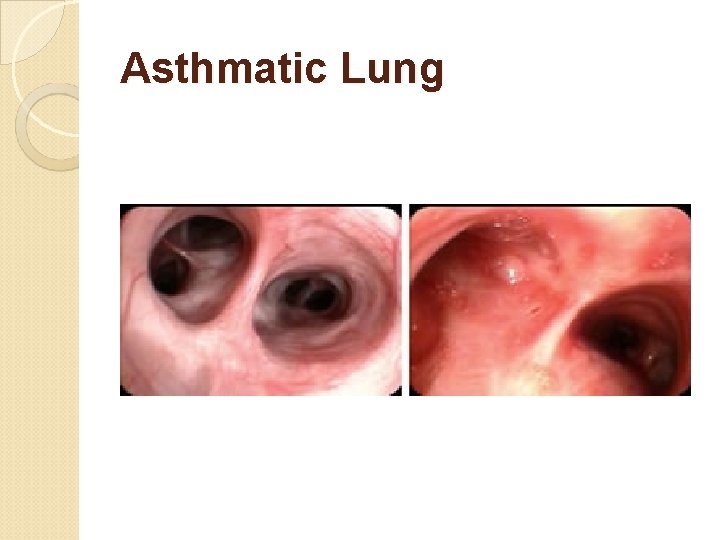
Asthmatic Lung
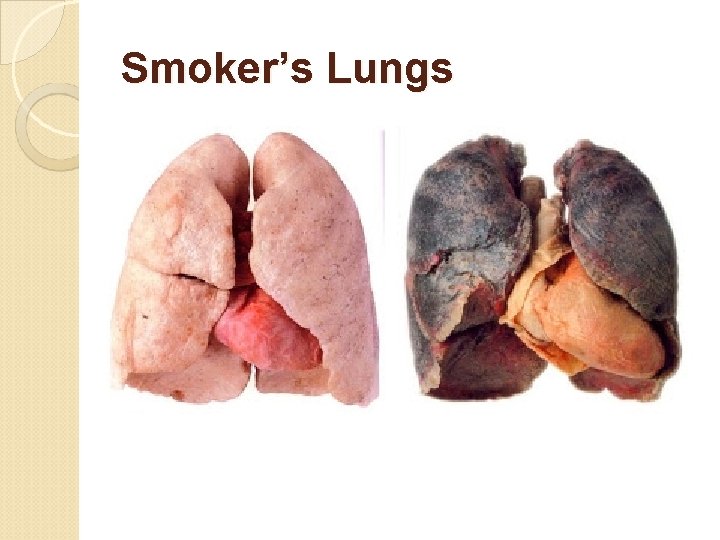
Smoker’s Lungs

Lung Cancer

Part 2 Physiology of the Respiratory System Anatomy & Physiology: Honors Turner College & Career High School 2018
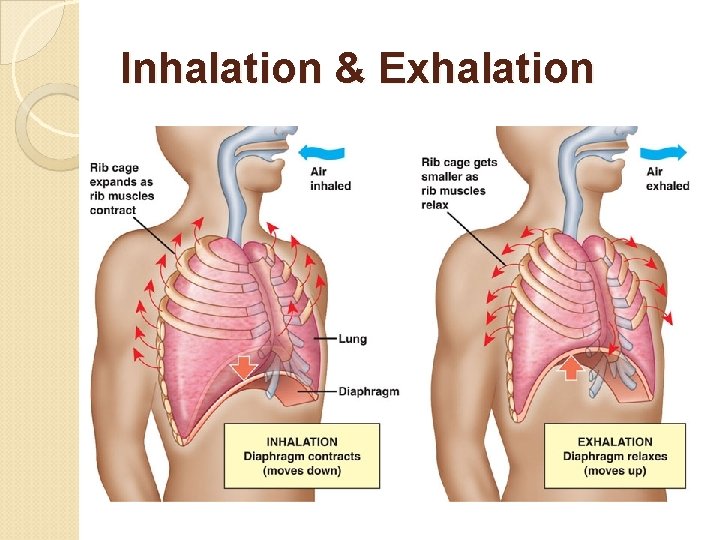
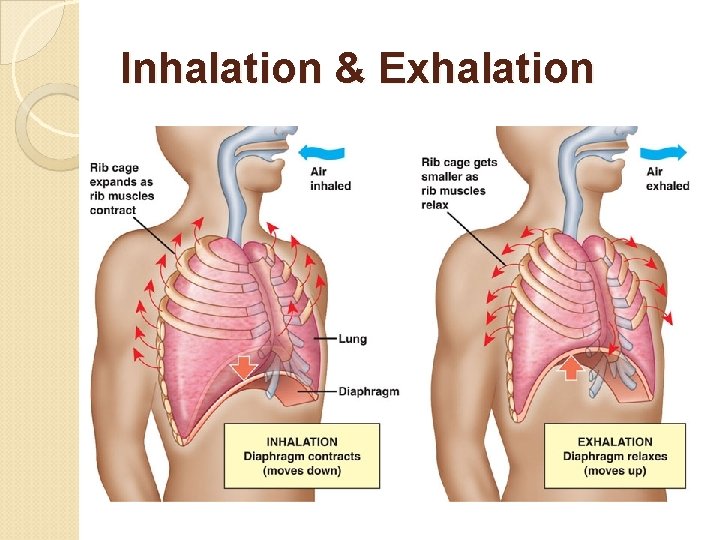
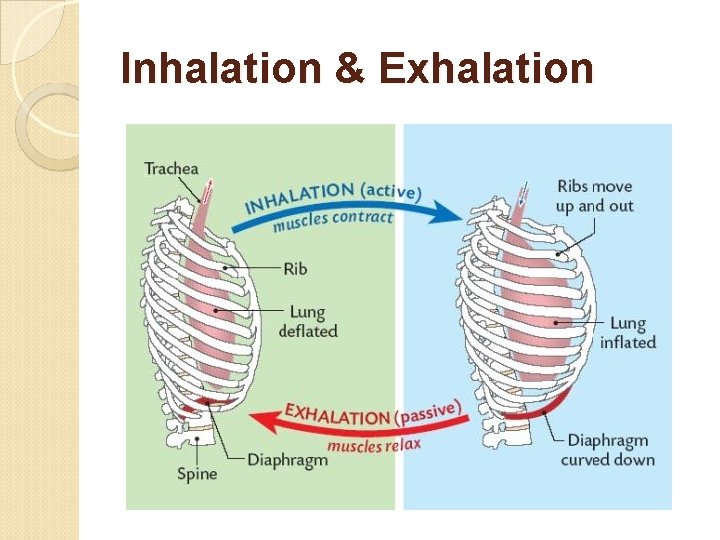
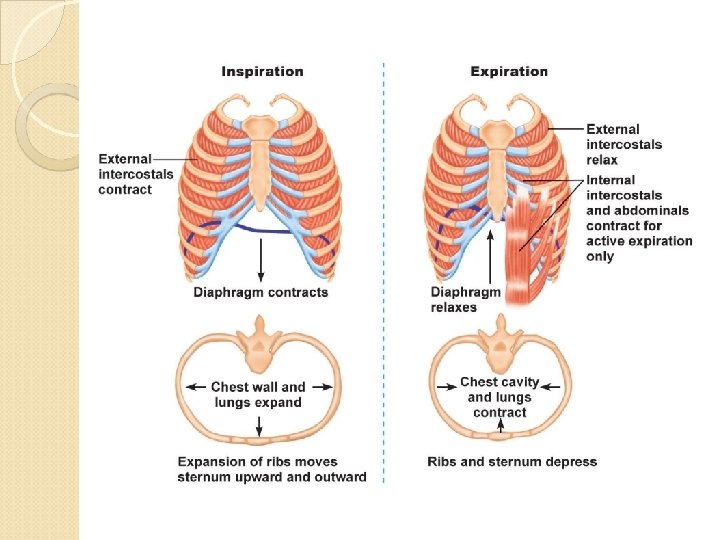
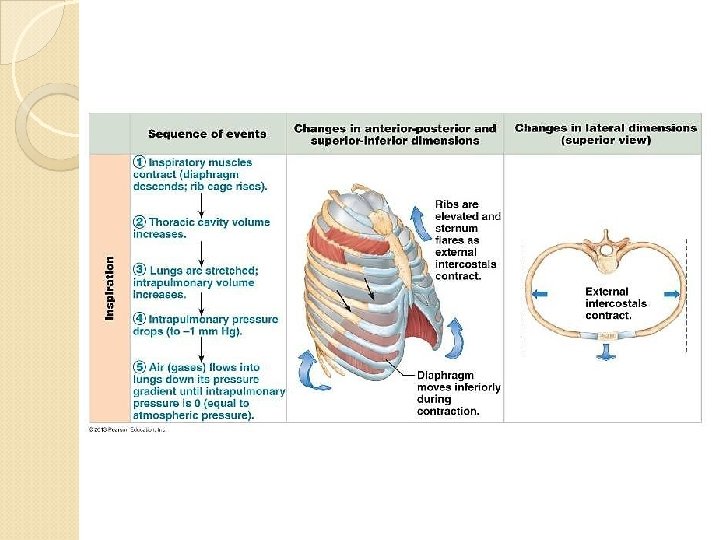
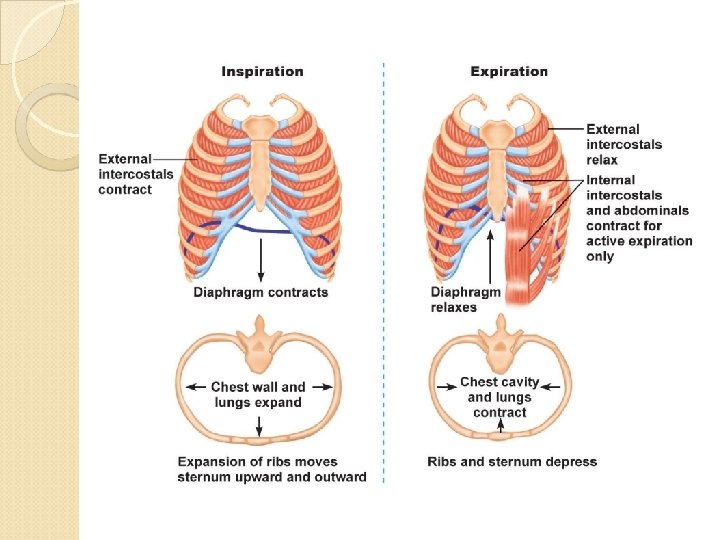
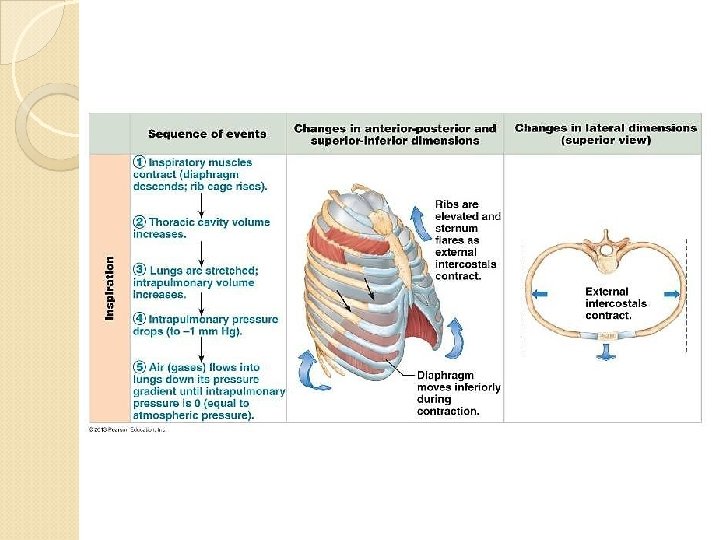
Inhalation & Exhalation
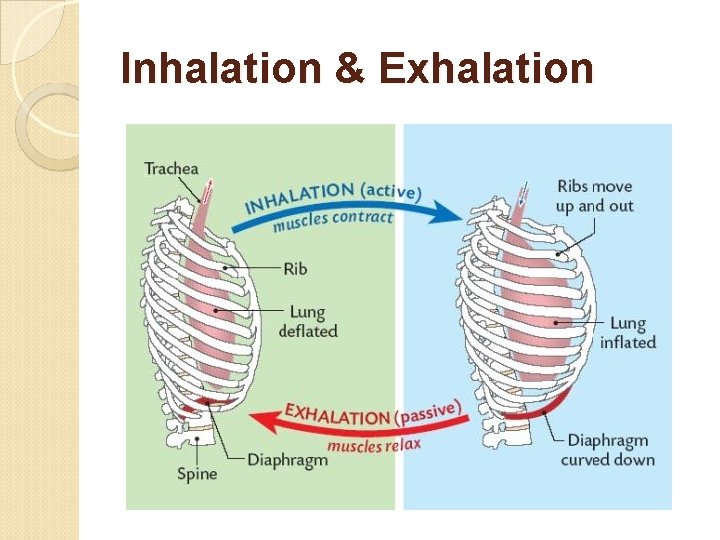
Inhalation & Exhalation
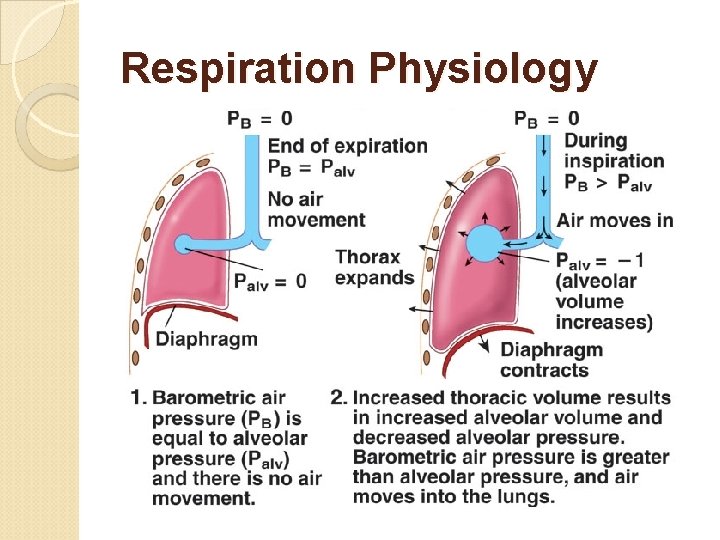
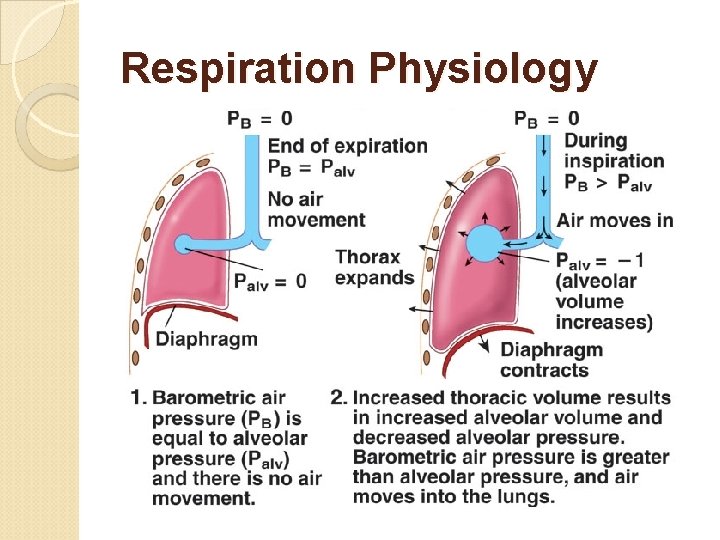
Respiration Physiology

Respiration Physiology


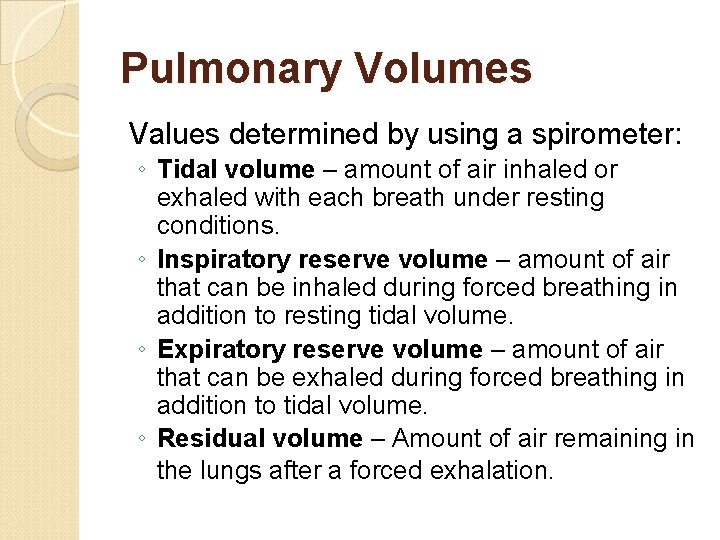
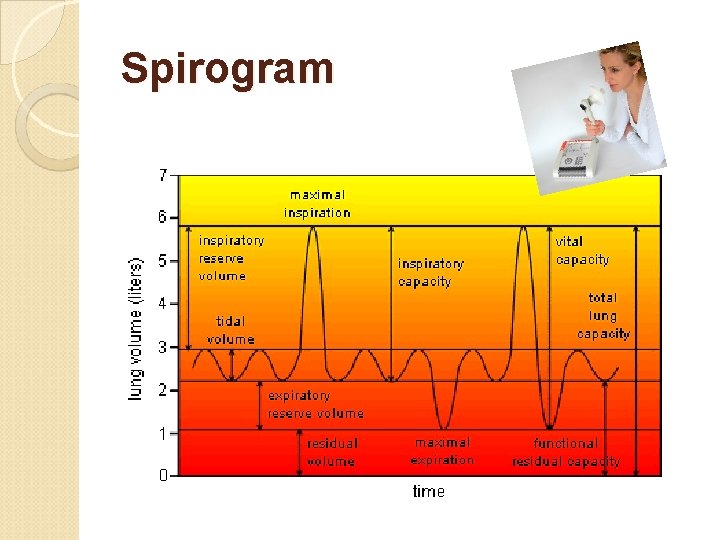
Pulmonary Volumes Values determined by using a spirometer: ◦ Tidal volume – amount of air inhaled or exhaled with each breath under resting conditions. ◦ Inspiratory reserve volume – amount of air that can be inhaled during forced breathing in addition to resting tidal volume. ◦ Expiratory reserve volume – amount of air that can be exhaled during forced breathing in addition to tidal volume. ◦ Residual volume – Amount of air remaining in the lungs after a forced exhalation.
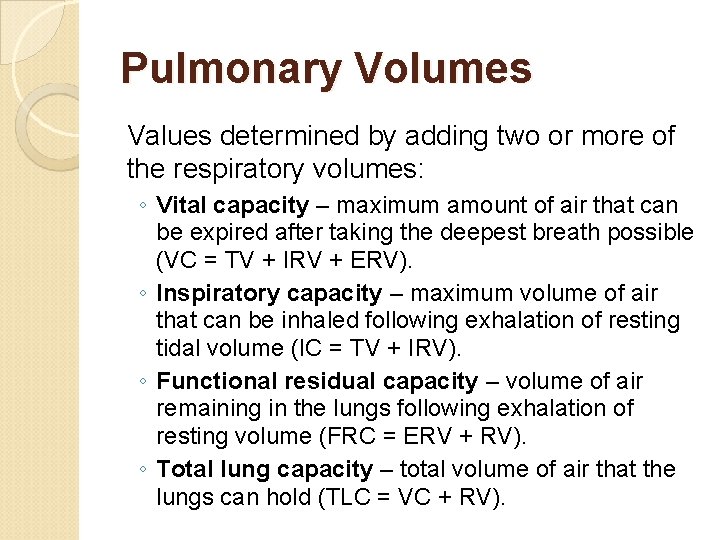
Pulmonary Volumes Values determined by adding two or more of the respiratory volumes: ◦ Vital capacity – maximum amount of air that can be expired after taking the deepest breath possible (VC = TV + IRV + ERV). ◦ Inspiratory capacity – maximum volume of air that can be inhaled following exhalation of resting tidal volume (IC = TV + IRV). ◦ Functional residual capacity – volume of air remaining in the lungs following exhalation of resting volume (FRC = ERV + RV). ◦ Total lung capacity – total volume of air that the lungs can hold (TLC = VC + RV).
Pulmonary Volumes Dead space: ◦ Anatomical dead space – areas of the conducting zone that contains air that never contributes to the gas exchange in the alveoli. ◦ Alveolar dead space – alveoli that are collapsed or obstructed and are not able to participate in gas exchange.
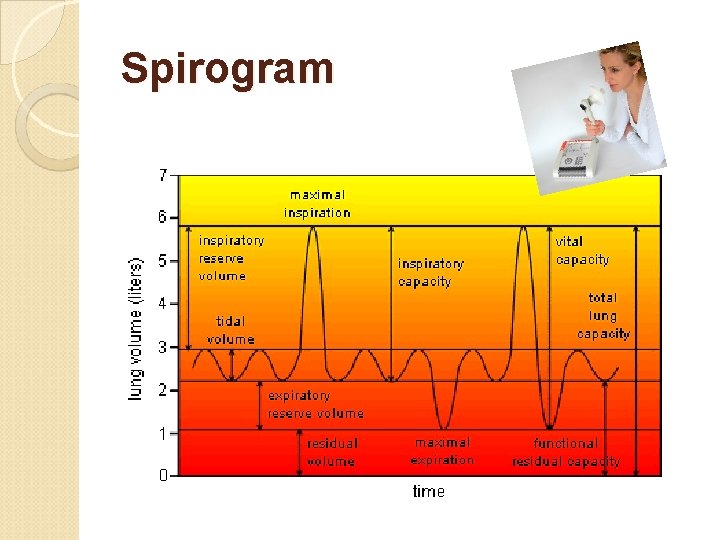
Spirogram
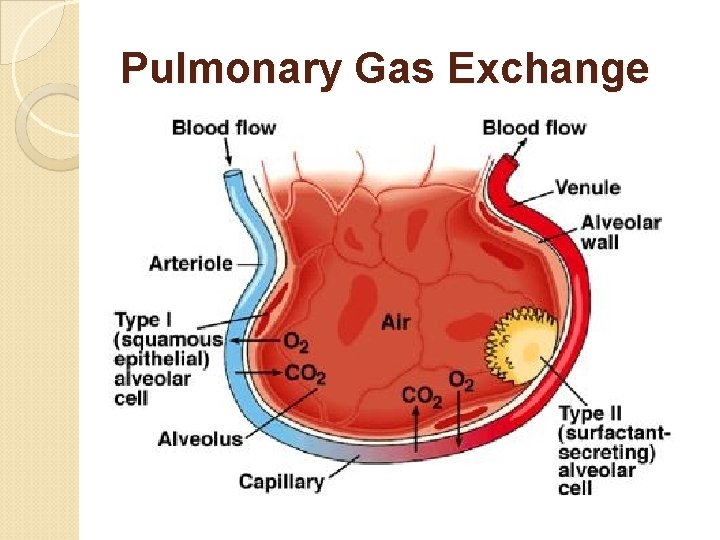
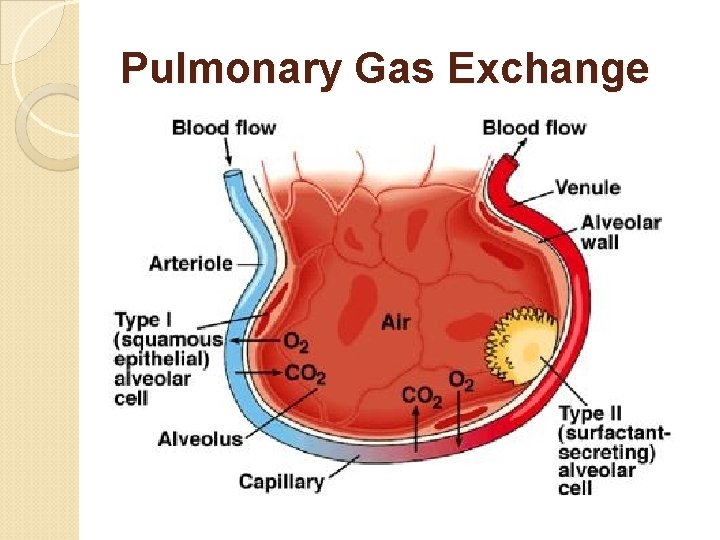
Pulmonary Gas Exchange

Pulmonary Gas Exchange
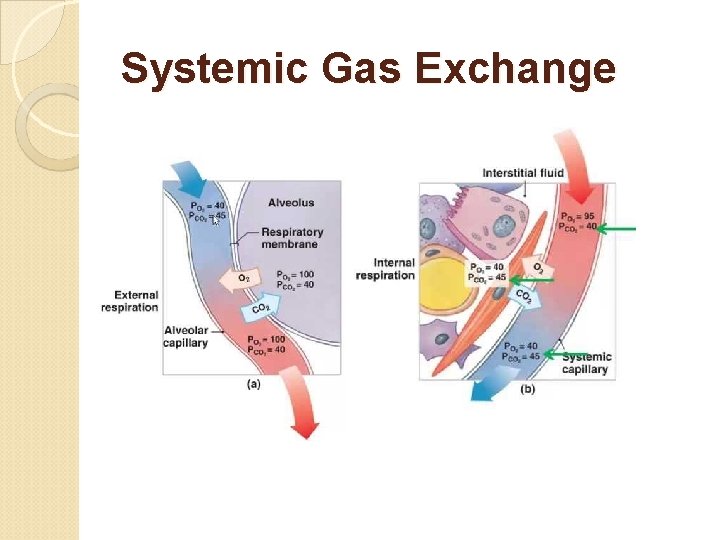
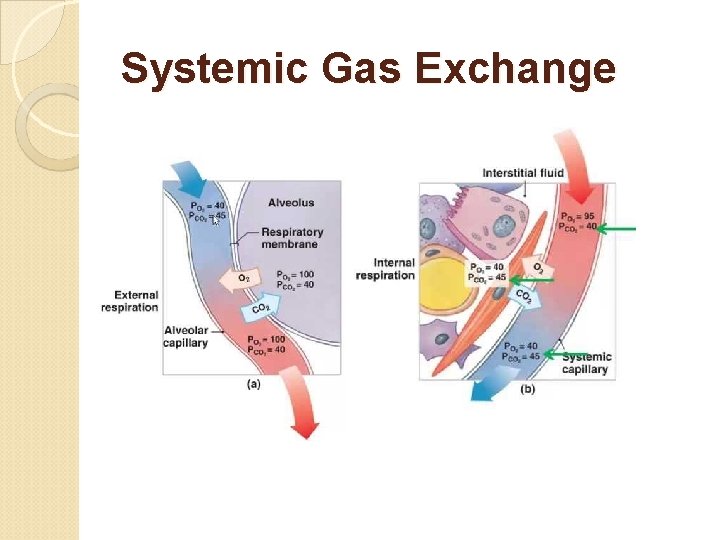
Systemic Gas Exchange

Hemoglobin Quaternary protein. • Fe centered heme groups. • O 2 binds to heme group. • CO 2 binds to amine groups. •
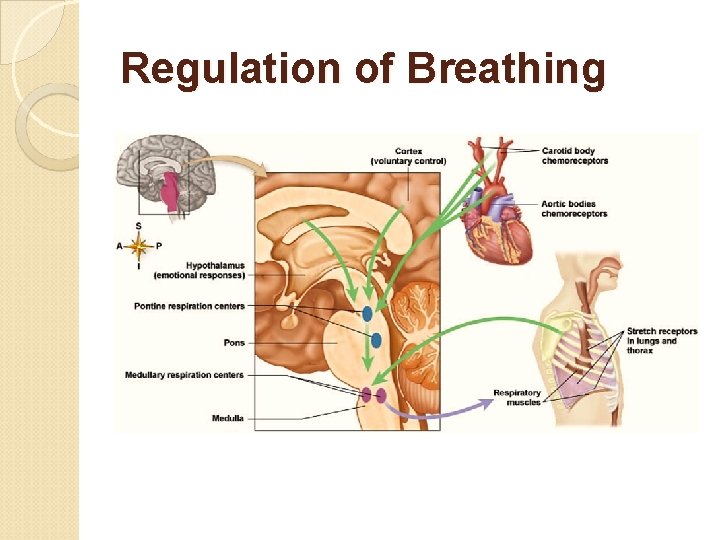
Regulation of Breathing Your respiratory rate changes. ◦ Active - your respiratory rate goes up. ◦ Less active, or sleeping - the rate goes down. Even though the respiratory muscles are voluntary, you can't consciously control them when you're sleeping. So, how is respiratory rate altered & how is respiration controlled when you're not consciously thinking about respiration?

Regulation of Breathing The rhythmicity center of the medulla: ◦ Controls automatic breathing. ◦ Consists of interacting neurons that fire either during inspiration (I neurons) or expiration (E neurons). I neurons - stimulate neurons that innervate respiratory muscles (to bring about inspiration) E neurons - inhibit I neurons (to 'shut down' the I neurons & bring about expiration). ◦ Apneustic center (located in the pons) stimulate I neurons to promote inspiration. ◦ Pneumotaxic center (located in the pons) inhibits apneustic center & inhibits inspiration (promotes expiration).
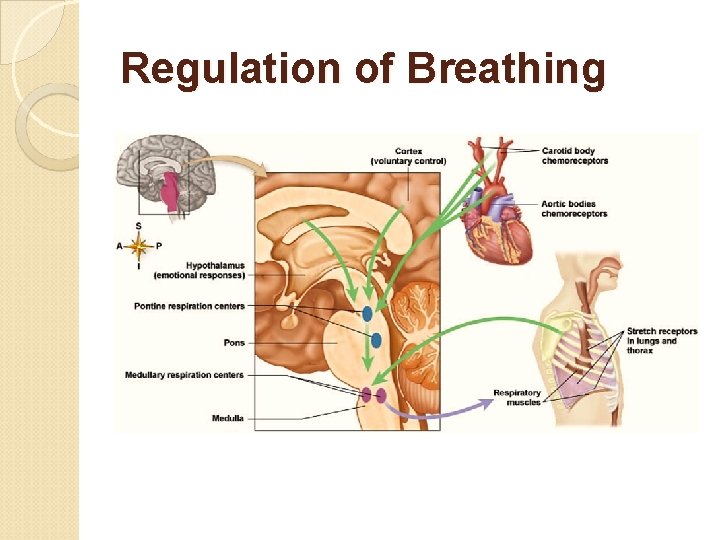
Regulation of Breathing
Patterns of Breathing Apnea – Temporary cessation of breathing (one or more skipped breaths). Dyspnea – Labored, gasping breathing; shortness of breath. Eupnea – Normal, relaxed, quiet breathing. Hyperpnea – Increased rate and depth of breathing in response to exercise, pain, or other conditions. Hyperventilation – Increased pulmonary ventilation in excess of metabolic demand. Hypoventilation – Reduced pulmonary ventilation. Orthopnea – Dyspnea that occurs when a person is lying down. Respiratory arrest – Permanent cessation of breathing.
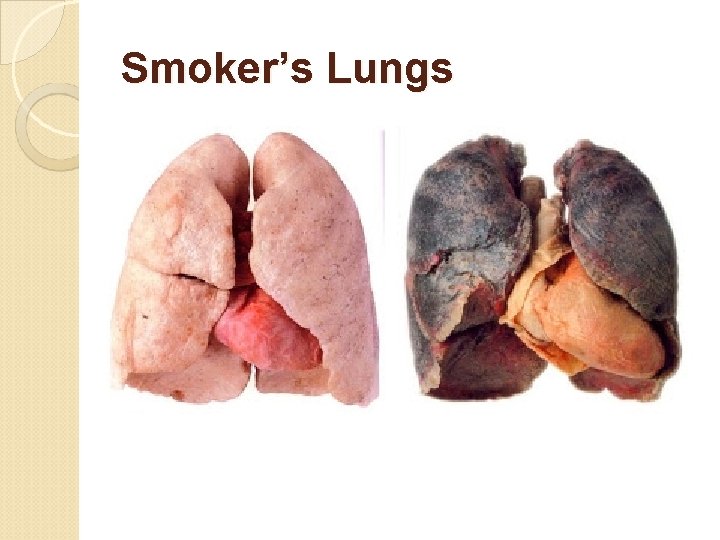
Clinical Disorders & Diseases Hypoxia – deficiency of oxygen in a tissue or the inability to use oxygen. Epistaxis – nosebleed. Oxygen toxicity – excess oxygen, causing the build up of peroxides and free radicals. Chronic obstructive pulmonary diseases (COPD) – long-term obstruction of airflow and a substantial reduction in pulmonary ventilation. ◦ Chronic bronchitis – cilia are immobilized and reduced in number; goblet cells increase their production of mucus → mucus clogs the airways and breeds infection. ◦ Emphysema – alveolar walls break down and the surface area of the lungs is reduced.
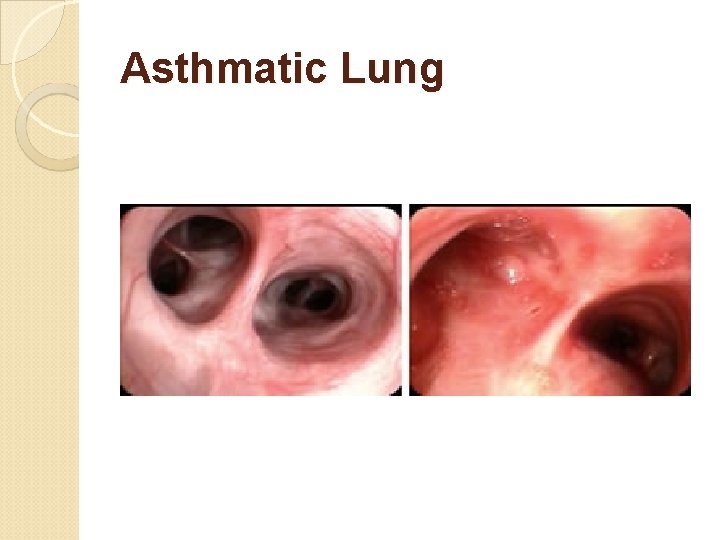
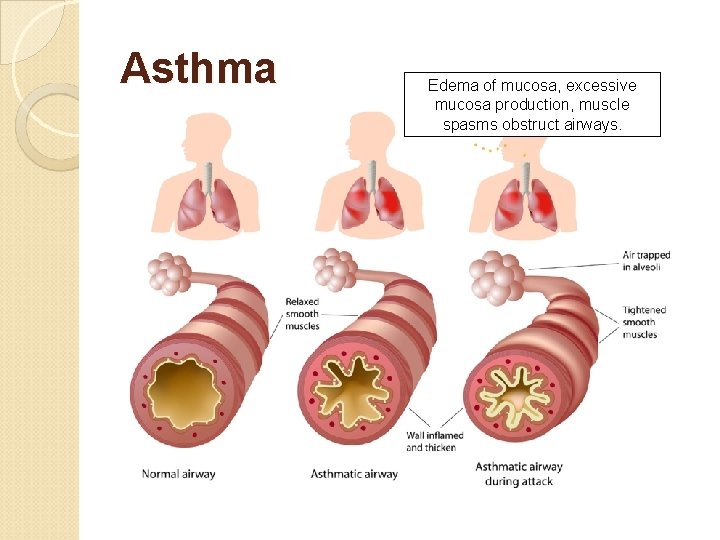
Clinical Disorders & Diseases Asthma – allergens trigger the release of histamine and other inflammatory chemicals that cause intense bronchoconstriction. ◦ In asthma, periodic constriction of the bronchi and bronchioles makes it more difficult to breathe in and, especially, out. ◦ The inflammation makes the airways swell. ◦ Asthma causes periods of wheezing, chest tightness, shortness of breath, and coughing. People who have asthma may experience symptoms that range from mild to severe and that may happen rarely or every day. ◦ Attacks of asthma can be triggered by airborne irritants such as chemical fumes and cigarette smoke or airborne particles to which the patient is allergic.
Clinical Disorders & Diseases Lung cancer –most common cancer and most common cause of cancer deaths in U. S. males. There are several forms of lung cancer, but the most common (and most rapidly increasing) types are those involving the epithelial cells lining the bronchi and bronchioles. ◦ The lining of these airways consists of two layers of cells. ◦ Chronic exposure to irritants causes the number of layers to increase. ◦ The ciliated and mucus-secreting cells disappear and are replaced by a disorganized mass of cells with abnormal nuclei. ◦ If the process continues, the growing mass penetrates the underlying basement membrane. ◦ Malignant cells can break away and be carried in lymph and blood to other parts of the body where they may lodge and continue to proliferate. It is this metastasis of the primary tumor that eventually kills the patient.
Clinical Disorders & Diseases Acute rhinitis – the common cold. Laryngitis – inflammation of the vocal folds. Pharyngitis – inflammation of the pharynx (sore throat). Pneumonia – lower respiratory infection of the alveoli that causes fluid build up in the lungs. It can be caused by many kinds of both bacteria (Streptococcus pneumoniae) and viruses. Tissue fluids accumulate in the alveoli reducing the surface area exposed to air. If enough alveoli are affected, the patient may need supplemental oxygen.
Clinical Disorders & Diseases Pleuritis – Inflammation of the pleura, producing more than the normal amount of fluid, causing a pleural effusion. The pain fibers of the lung are located in the pleura. When this tissue becomes inflamed, it results in a sharp pain in the chest that is worse with breathing in. Other symptoms of pleurisy can include cough, chest tenderness, and shortness of breath. Sleep apnea – Cessation of breathing for 10 seconds or longer during sleep.
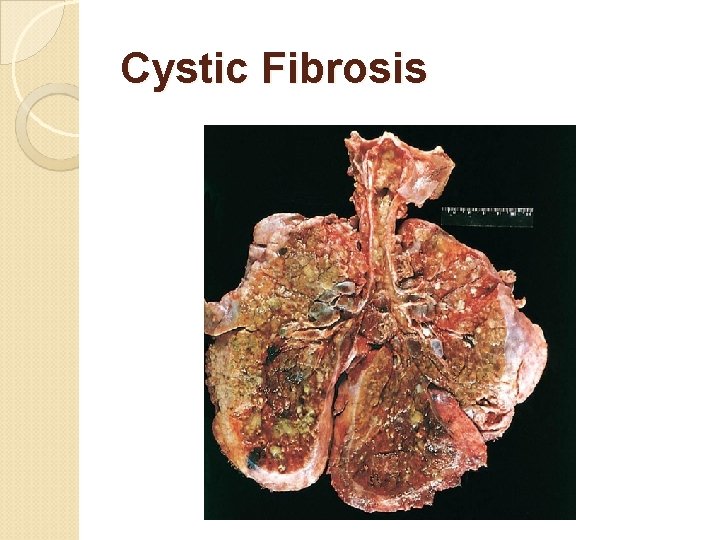
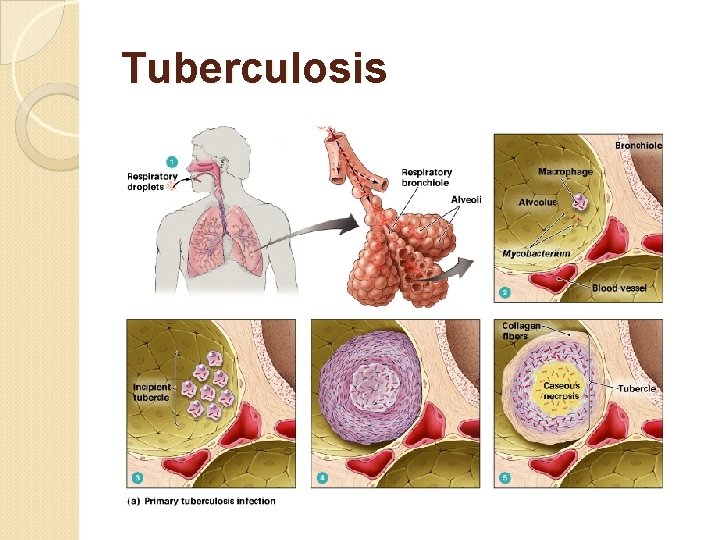
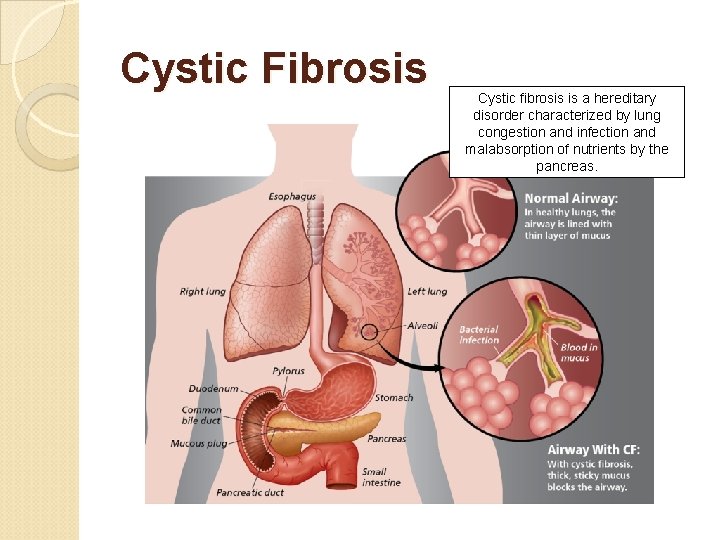
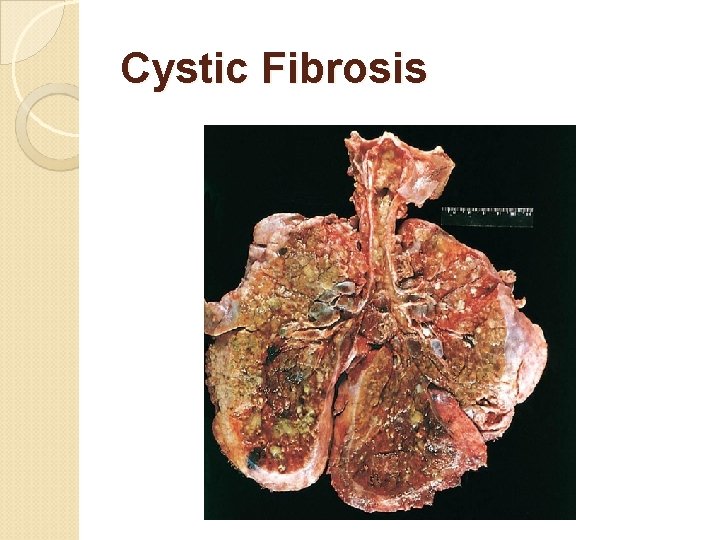
Clinical Disorders & Diseases Tuberculosis – pulmonary infection with Mycobacterium tuberculosis; reduces lung compliance. Cystic fibrosis – caused by inheriting two defective CFTR genes, a transmembrane protein needed for the transport of Cl− ions out of the epithelial cells of the lung thus enabling water to follow by osmosis. Diminished CFTR function reduces the water content of the fluid in the lungs making it more viscous and difficult for the ciliated cells to move it up out of the lungs. The accumulation of mucus plugs the airways interfering with breathing and causing a persistent cough. Cystic fibrosis is the most common inherited disease in the U. S. white population.

Chronic Bronchitis Bronchi narrow due to swollen tissue and excessive mucus production.
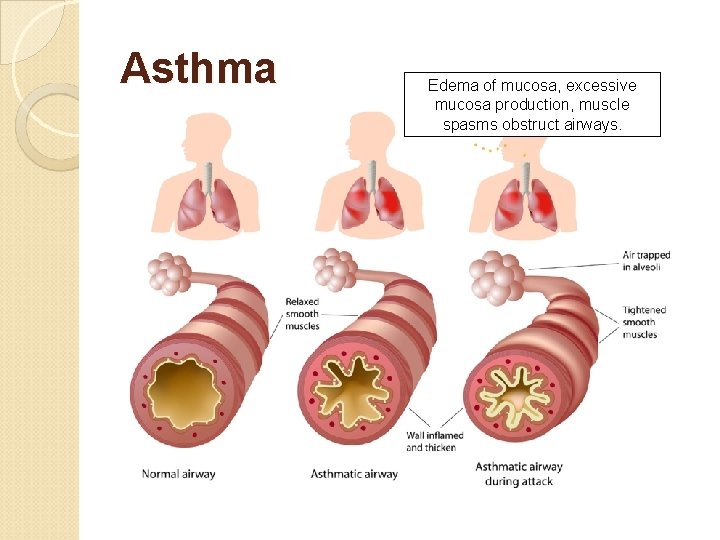
Asthma Edema of mucosa, excessive mucosa production, muscle spasms obstruct airways.

Emphysema Alveolar walls torn and can’t repair, alveoli fuse into large air spaces.
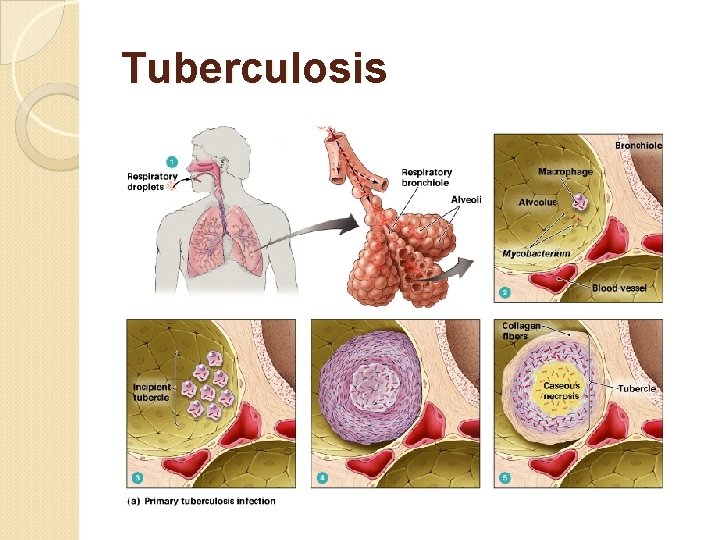
Tuberculosis

COPD Chronic obstructive pulmonary disease (COPD) refers to a group of lung diseases that block airflow and make breathing difficult.
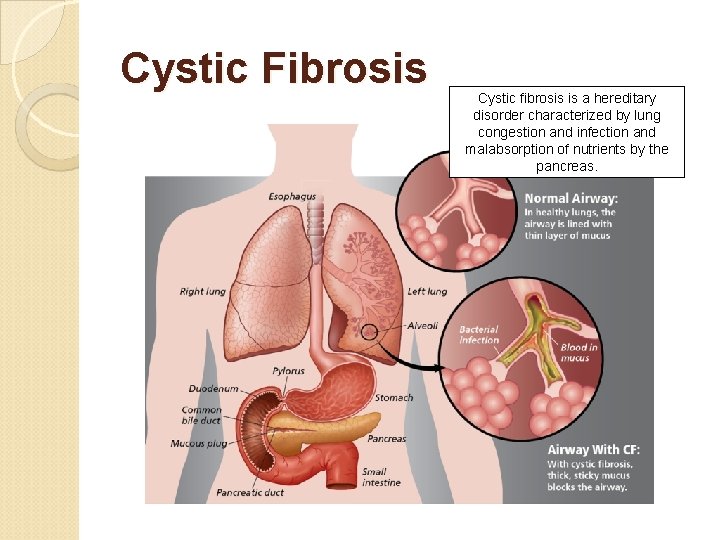
Cystic Fibrosis Cystic fibrosis is a hereditary disorder characterized by lung congestion and infection and malabsorption of nutrients by the pancreas.
 Types of respiration in human
Types of respiration in human Larynx and trachea
Larynx and trachea Respiratory zone
Respiratory zone Upper respiratory labeled
Upper respiratory labeled Respiratory digestive and circulatory system
Respiratory digestive and circulatory system Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Male vs female skeleton pelvis
Male vs female skeleton pelvis Respiratory system diagram
Respiratory system diagram Functional anatomy of the respiratory system
Functional anatomy of the respiratory system How respiratory system work with circulatory system
How respiratory system work with circulatory system Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Tattoo anatomy and physiology
Tattoo anatomy and physiology International anatomy olympiad
International anatomy olympiad Woody stem parts
Woody stem parts Anatomy and physiology bones
Anatomy and physiology bones Ulcer anatomy
Ulcer anatomy Liver anatomy
Liver anatomy Hypogastric region
Hypogastric region Hypogastric region
Hypogastric region Google
Google Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Http://anatomy and physiology
Http://anatomy and physiology Waistline
Waistline Appendicitis anatomy and physiology
Appendicitis anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Teks anatomy and physiology
Teks anatomy and physiology Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Stomach anatomy and physiology ppt
Stomach anatomy and physiology ppt Pancreas anatomy and physiology
Pancreas anatomy and physiology Chapter 7 anatomy and physiology
Chapter 7 anatomy and physiology Art labeling activity: figure 14.1 (3 of 3)
Art labeling activity: figure 14.1 (3 of 3) Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Necessary life functions anatomy and physiology
Necessary life functions anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Gi tract histology
Gi tract histology Anatomy and physiology
Anatomy and physiology Anterior posterior distal proximal
Anterior posterior distal proximal The speed at which the body consumes energy
The speed at which the body consumes energy Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anterior posterior ventral dorsal
Anterior posterior ventral dorsal Physiology exam 1
Physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Anatomy and physiology of the foot
Anatomy and physiology of the foot Anatomy and physiology of psoriasis
Anatomy and physiology of psoriasis Pse4u
Pse4u Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology