ANAESTHETIC MANAGEMENT OF RENAL CELL CARCINOMA AND IVC



- Slides: 31
ANAESTHETIC MANAGEMENT OF RENAL CELL CARCINOMA AND IVC THROMBUS POSTED FOR LEFT SIDED RADICAL NEPHRECTOMY WITH THROMBECTOMY Presented by: Dr. Shreyank. P. Solanki (JRIII)
CASE HISTORY Ø 58 yr old male, R/O Alandi, Pune, farmer by occupation admitted on 14/8/2018. ØChief complaints: • Increase frequency of micturition and burning sensation x 1 month , • Generalized body weakness x 1 month , • Loss of appetite x 1 month, • Loss of weight.
HISTORY OF PRESENT ILLNESS ØMy patient was apparently asymptomatic 1 month back when he developed pain in abdomen with increased frequency of micturition. ØThis was sudden in onset and progressive in nature, not associated with any episode of vomiting or loose stools. ØHe also experienced loss of appetite and he lost approximately 7 kg weight in past one month.
PAST HISTORY ØHistory of pain abdomen since 1 month. ØUSG abdomen & pelvis done: enlarged prostate and enlarged kidney with ill defined lesion was found. ØMRI abdomen & pelvis done: neoplastic lesion s/o renal cell carcinoma and tumour thrombus extending into infrahepatic IVC. ØNo history of HTN/DM/TB/ASTHMA/SEIZURE DISORDER ØNo complaints of chest pain/ breathlessness/ palpitation. ØNo Complaint of cough/cold/fever.
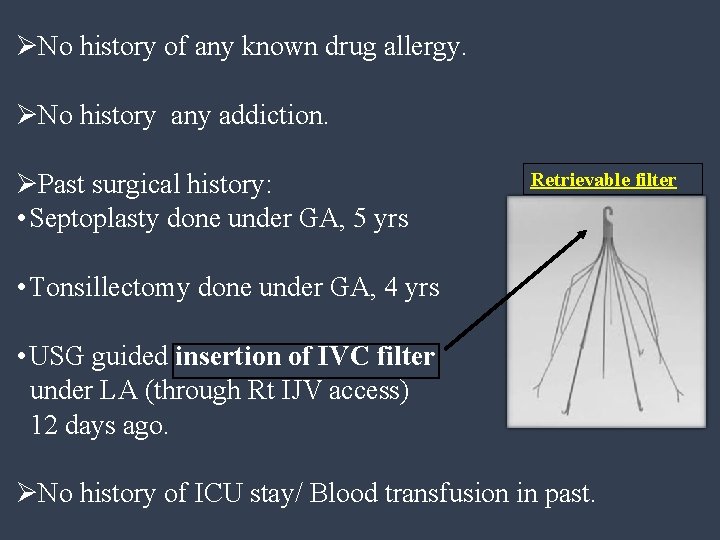
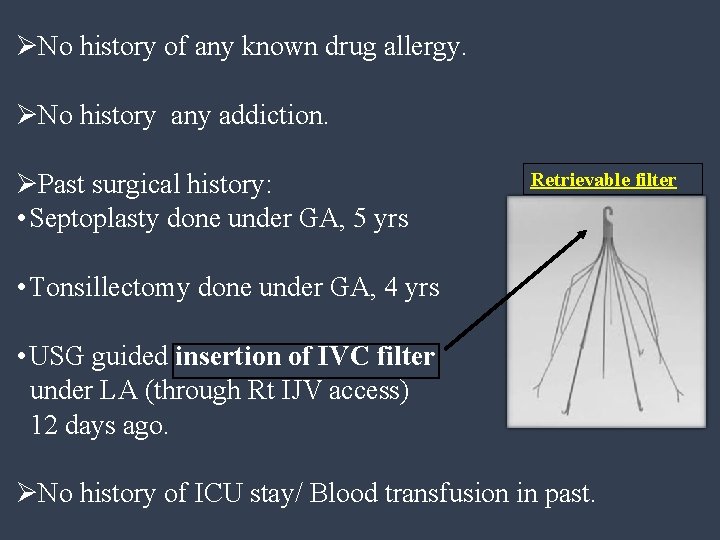
ØNo history of any known drug allergy. ØNo history any addiction. ØPast surgical history: • Septoplasty done under GA, 5 yrs Retrievable filter • Tonsillectomy done under GA, 4 yrs • USG guided insertion of IVC filter under LA (through Rt IJV access) 12 days ago. ØNo history of ICU stay/ Blood transfusion in past.
GENERAL PHYSICAL EXAMINATION ØAwake, conscious, oriented. ØAverage built, weight 80 kg. ØTemperature afebrile. ØPulse: 72 bpm regular, good volume. ØAll peripheral pulse felt. ØBP: 130/80 mm. Hg. ØRR: 14 breaths/min. ØNo pallor/icterus/clubbing/cyanosis. ØSpine: NAD
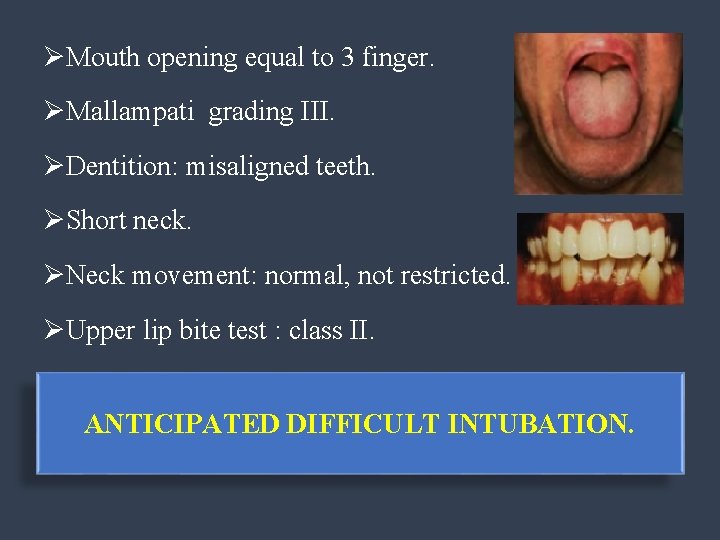
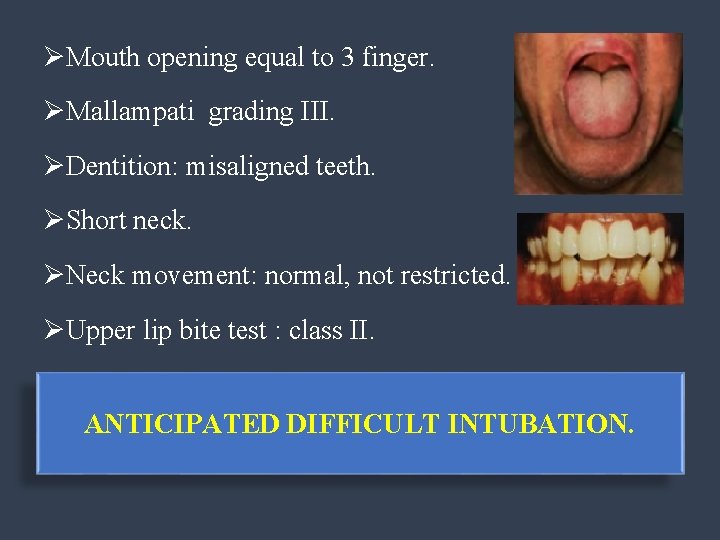
ØMouth opening equal to 3 finger. ØMallampati grading III. ØDentition: misaligned teeth. ØShort neck. ØNeck movement: normal, not restricted. ØUpper lip bite test : class II. ANTICIPATED DIFFICULT INTUBATION.
SYSTEMIC EXAMINATION 1. • • • RESPIRATORY: Chest movement bilaterally equal Air entry bilaterally equal No adventitous sounds. 2. CVS: Apical impulse palpable in left 5 th intercostal space just lateral to midclavicular line. S 1, S 2 + 3. CNS: conscious, alert and well oriented to time, place and person.
4. ABDOMEN: Scaphoid, soft, non tender, not distended.
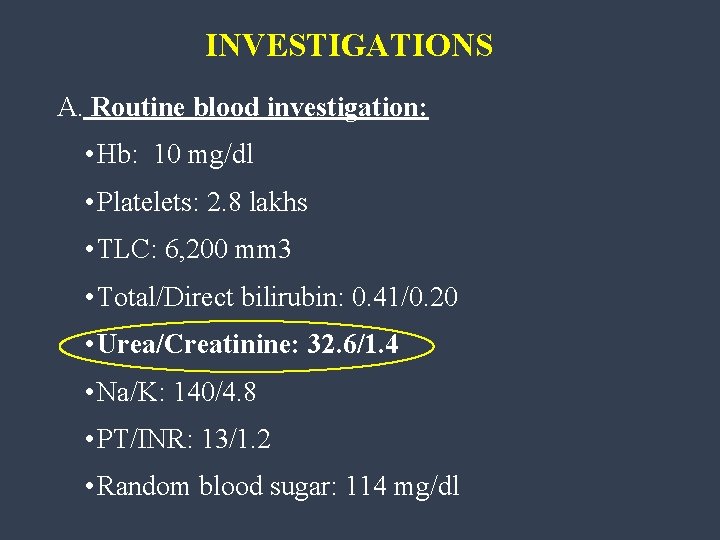
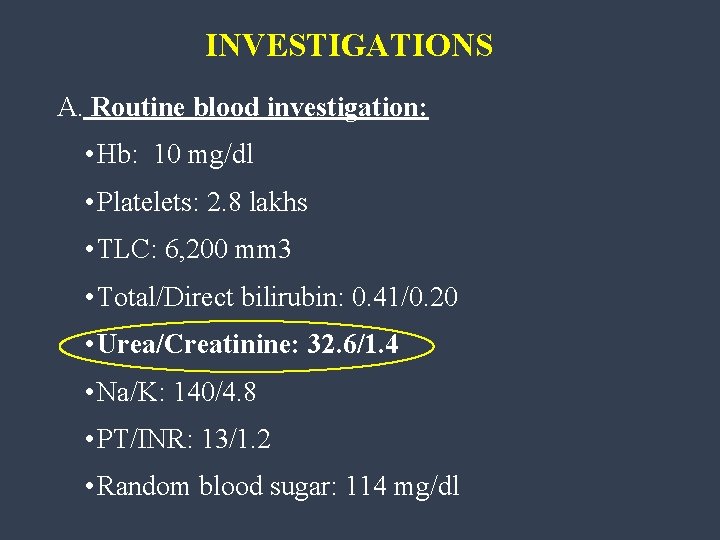
INVESTIGATIONS A. Routine blood investigation: • Hb: 10 mg/dl • Platelets: 2. 8 lakhs • TLC: 6, 200 mm 3 • Total/Direct bilirubin: 0. 41/0. 20 • Urea/Creatinine: 32. 6/1. 4 • Na/K: 140/4. 8 • PT/INR: 13/1. 2 • Random blood sugar: 114 mg/dl
B. Chest x-ray: NAD C. ECG: WNL D. 2 D ECHO: • LVEF: 60%. • Normal LV size and function. • Normal valves and normal RA/RV. • No RWMA. • Visible portion of pulmonary artery is free of clot.
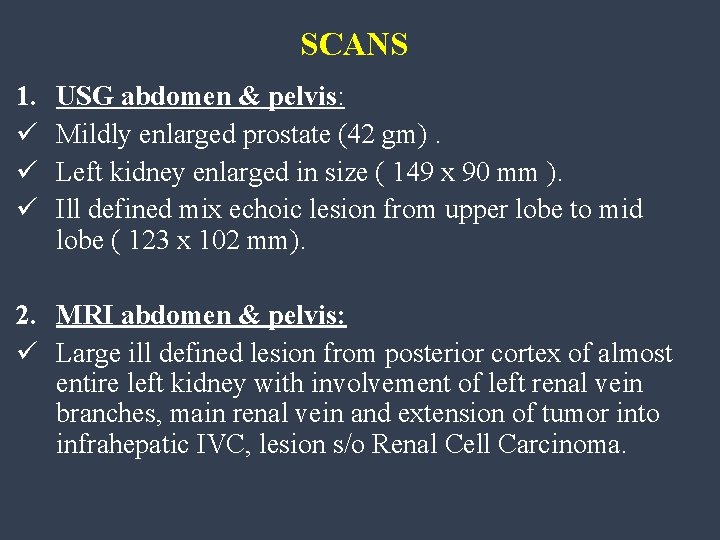
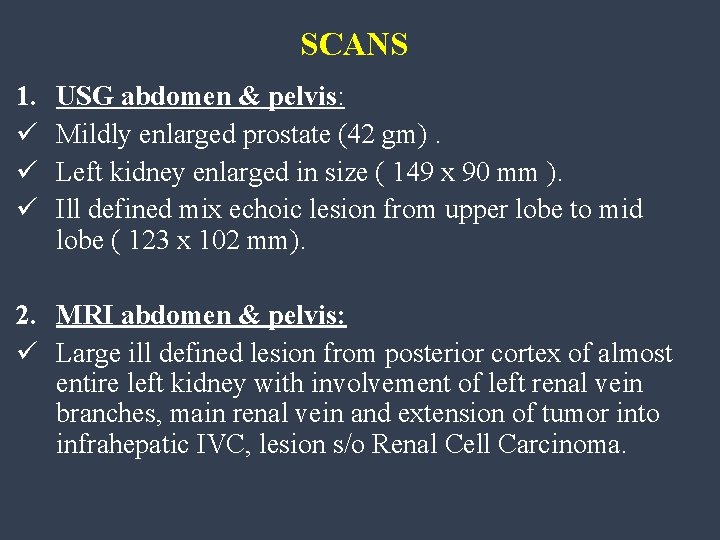
SCANS 1. ü ü ü USG abdomen & pelvis: Mildly enlarged prostate (42 gm). Left kidney enlarged in size ( 149 x 90 mm ). Ill defined mix echoic lesion from upper lobe to mid lobe ( 123 x 102 mm). 2. MRI abdomen & pelvis: ü Large ill defined lesion from posterior cortex of almost entire left kidney with involvement of left renal vein branches, main renal vein and extension of tumor into infrahepatic IVC, lesion s/o Renal Cell Carcinoma.
3. Histopathological report: Grade III renal cell carcinoma.
PLANNING FOR ANAESTHESIA PREOPERATIVE: ØPatient was posted for left radical nephrectomy with thrombectomy under general anaesthesia. ØPatient was taken up for surgery under ASA III with written informed Consent for high risk, SICU and post ventilator support. ØCentral line was secured (left IJV) and post chest Xray done.
ØCVTS OT and Cardiopulmonary bypass was kept ready. ØAdequate blood and blood products were kept ready. ØPatient kept nill by mouth overnight. Anaesthesia planned: General anaesthesia + Epidural Anaesthesia ( for post operative pain management ).
ANAESTHETIC MANAGEMENT INTRAOPERATIVE ØAnaesthesia procedure was well explained to the patient. ØOT was prepared for surgery keeping in mind the anticipated and unanticipated problems. Ø 20 G IV line secured and i. v. crystalloid (RL) started. ØBasic monitors attached. ( Pulse oximetry, ECG, NIBP) ØBaseline vital parameters recorded (Pulse: 88 bpm BP: 130/80 mm. Hg, SPo 2: 100%) ØCVP transducer was attached to central line.
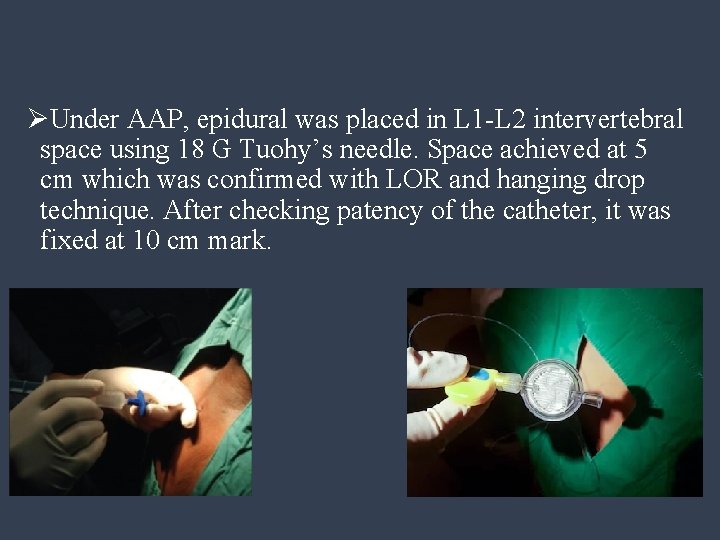
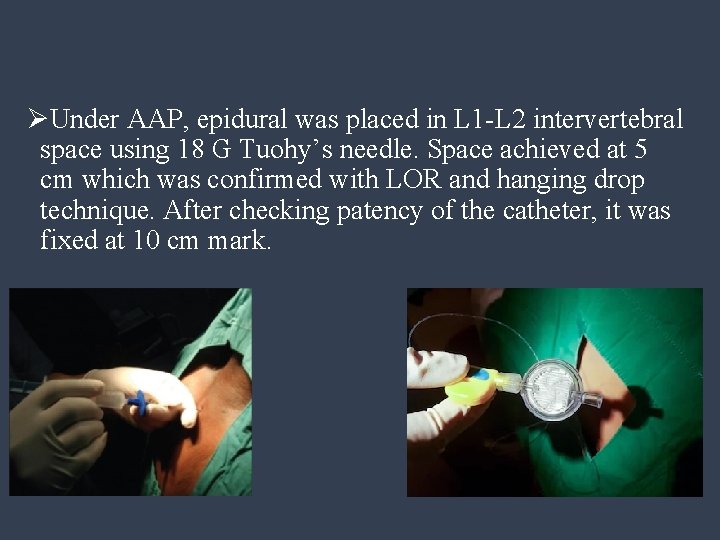
ØUnder AAP, epidural was placed in L 1 -L 2 intervertebral space using 18 G Tuohy’s needle. Space achieved at 5 cm which was confirmed with LOR and hanging drop technique. After checking patency of the catheter, it was fixed at 10 cm mark.
ØPt was made supine and was preoxygenated with 100% O 2 for 3 min with 4 no. anatomical face mask. ØPremedication: antistatic 4 Inj. Glycopyrrolate 0. 004 mg/kg, Inj. Midazolam 0. 02 mg/kg, Inj. Ondensetron 0. 1 mg/kg and Inj. Fentanyl 1. 5 mcg/kg was given i. v.
once induced, able to ventilate adequately. Inj. Succinylcholine 2 mg/kg given. oy C c M BOUGIE ØPatient induced with Inj propofol 2 mg/kg. Patient was intubated with 8. 0 mm cuffed ETT under vision, with the help of Mc. Ccoy laryngoscope blade no. 4 and bougie. ( Cormack Lehane Grade 3) AEBE, cuff inflated, Tube fixed, Et. Co 2 +.
ØLong acting muscle relaxant, Inj. Vecuronium 6 mg given i. v. and patient maintained on O 2: AIR: Sevoflurane: intermittent dose of relaxant. IPPV ØPost intubation vitals: P. R. : 90 bpm B. P. : 133/87 mm. Hg Sp. O 2: 100% Et. CO 2: 38 mm. Hg. CVP: 10 -12 cm. H 2 o
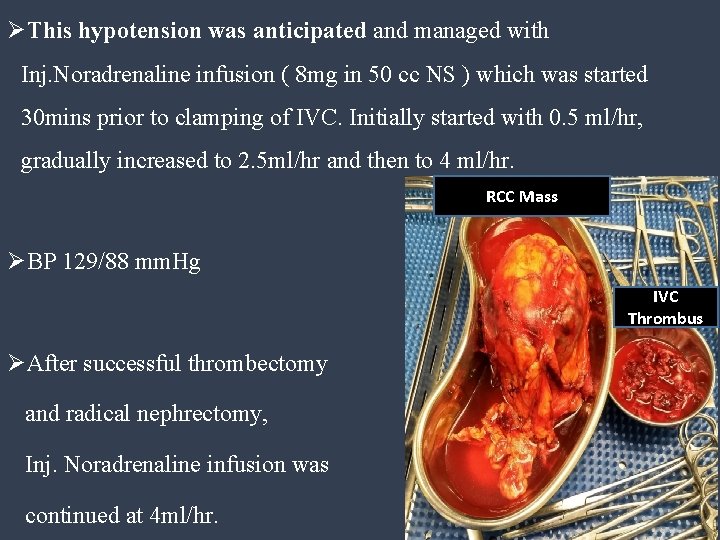
ØAfter proper padding and positioning intra arterial line secured under AAP on Rt hand & monitored (135/91 mm. Hg). ØIntra nasal temperature probe placed. ØAdequately padded the patient and warmer was placed. ØThe intraoperative course was hemodynamically stable, except there was an episode of hypotension when the IVC was clamped during thrombectomy. ØBP 89/60 mm. Hg.
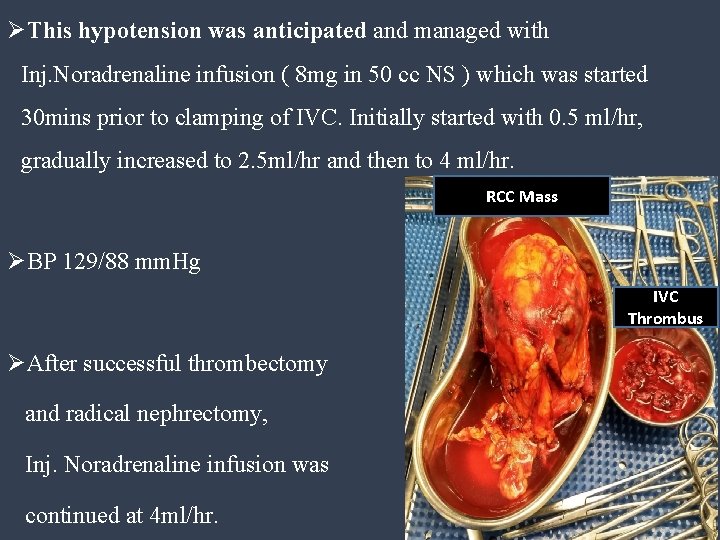
ØThis hypotension was anticipated and managed with Inj. Noradrenaline infusion ( 8 mg in 50 cc NS ) which was started 30 mins prior to clamping of IVC. Initially started with 0. 5 ml/hr, gradually increased to 2. 5 ml/hr and then to 4 ml/hr. RCC Mass ØBP 129/88 mm. Hg IVC Thrombus ØAfter successful thrombectomy and radical nephrectomy, Inj. Noradrenaline infusion was continued at 4 ml/hr.
ØThe intraoperative blood loss was around 3200 ml. ØThe loss was appropriately managed using Crystalloids (2000 ml) Colloid (500 ml) PCV ( 4 Units) FFP ( 2 Units) ØIntraoperatively, CVP was maintained between 8 -10 cm H 2 O. ØThe surgery lasted for 6 hours.
POSTOPERATIVE: Ø The patient was not extubated and placed on postoperative mechanical ventilation. Ø As the patient remained hemodynamically stable, he was extubated next morning after appropriate weaning trials. Ø Postop Analgesia was provided through epidural catheter with Inj. Bupivacaine 0. 125% + inj. Fentanyl 10 mcg 10 ml every 12 hourly. Ø DVT stocking, LMWH (inj. Clexane 0. 4 mg SC) and after that inj. Warfarin 5 mg was continued as venous thromboprophylaxis. Ø On post operative day 3, patient was discharged from the SICU and was shifted to general ward.

DISCUSSION
ØThe vast majority of solid renal masses are Renal cell carcinoma. It represents 2%- 3% of all the cancers. ØApproximately, 40 % of RCC are detected as an incidental finding on abdominal imaging. ØIt is a tumor with the distinct feature that it can invade through the renal vein into the inferior vena cava and can grow intravascularly, sometimes extending into right cardiac chambers. This extension is apparent in 4 - 10% of RCCs and can present with severe pulmonary congestion or embolism. ØSurgical management is preferred in these patients.
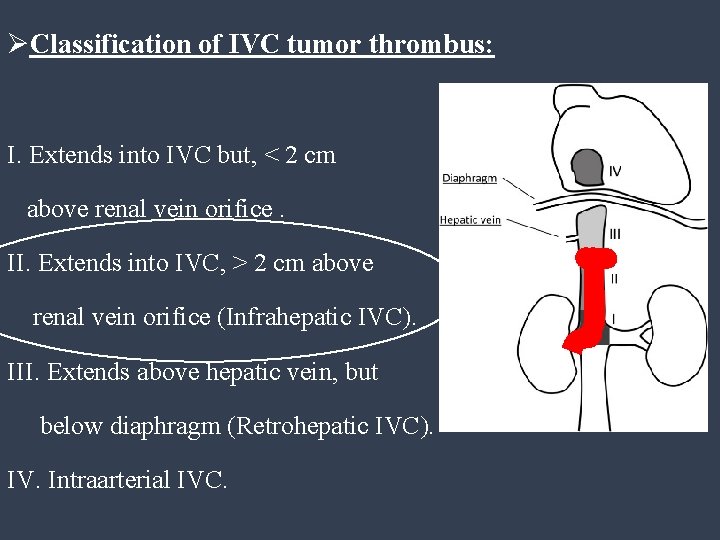
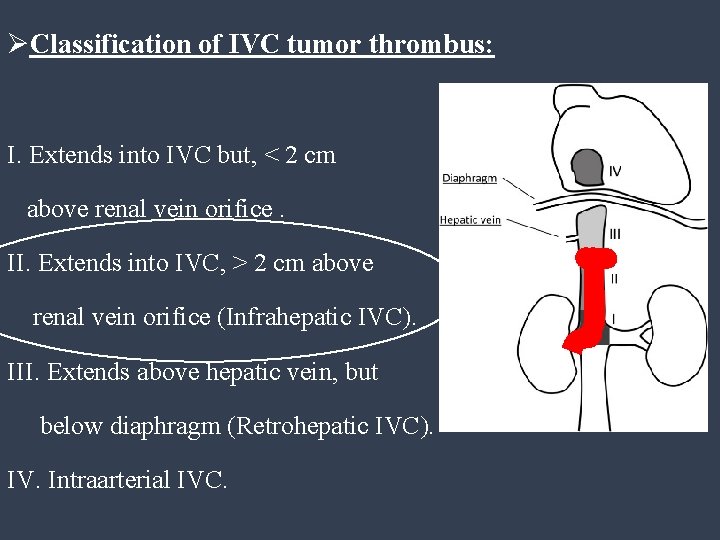
ØClassification of IVC tumor thrombus: I. Extends into IVC but, < 2 cm above renal vein orifice. II. Extends into IVC, > 2 cm above renal vein orifice (Infrahepatic IVC). III. Extends above hepatic vein, but below diaphragm (Retrohepatic IVC). IV. Intraarterial IVC.
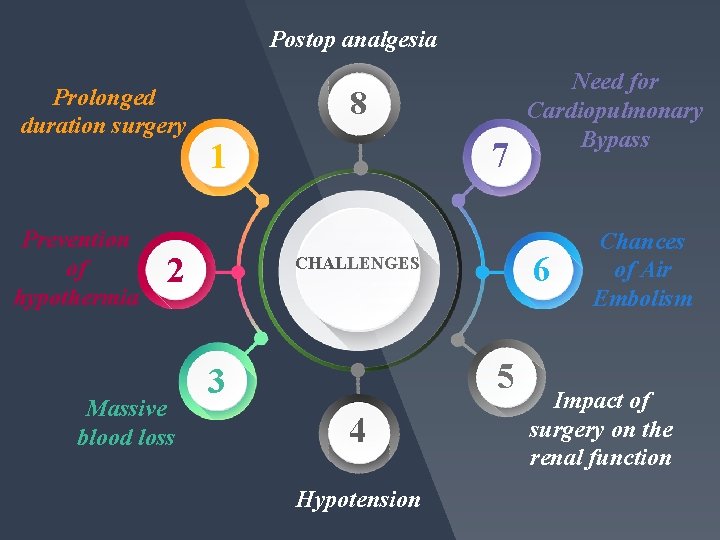
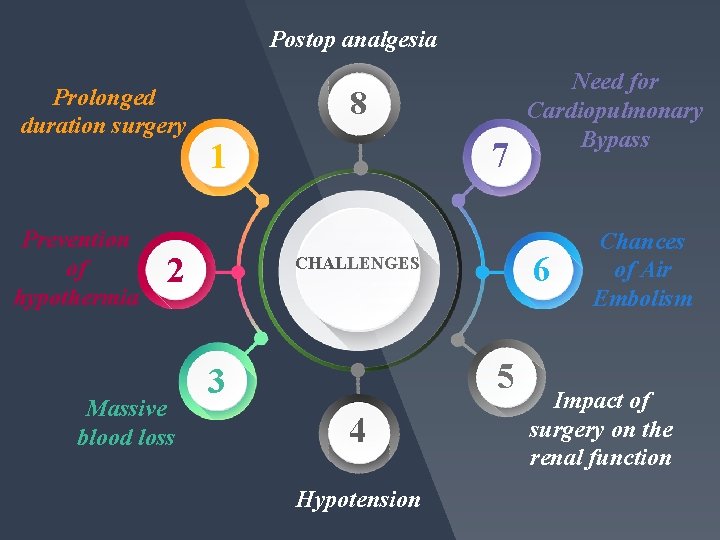
Postop analgesia Prolonged duration surgery Prevention of hypothermia 8 2 Massive blood loss 7 1 6 CHALLENGES 45 3 4 Hypotension Need for Cardiopulmonary Bypass Chances of Air Embolism Impact of surgery on the renal function

Positioning and padding Step 01 Cardiopulmonary bypass Active warming Step 02 Step 08 Step 03 Watchful of embolism consideration Step 07 Avoiding drugs dependant on metabolism Step 06 Step 04 Step 05 vasopressors Invasive monitoring Blood and blood products
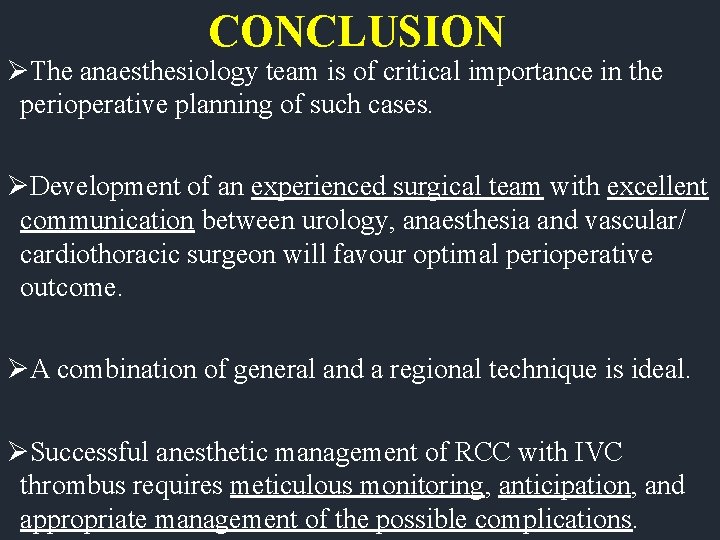
CONCLUSION ØThe anaesthesiology team is of critical importance in the perioperative planning of such cases. ØDevelopment of an experienced surgical team with excellent communication between urology, anaesthesia and vascular/ cardiothoracic surgeon will favour optimal perioperative outcome. ØA combination of general and a regional technique is ideal. ØSuccessful anesthetic management of RCC with IVC thrombus requires meticulous monitoring, anticipation, and appropriate management of the possible complications.

Their hands, our brains. Thank you !
 Res extra commercium
Res extra commercium Diagnostico etiologico
Diagnostico etiologico Naphthylamine
Naphthylamine Carcinoma renal de células claras fuhrman
Carcinoma renal de células claras fuhrman Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries Kode icd 10 basal cell carcinoma
Kode icd 10 basal cell carcinoma Squamous cell carcinoma louisiana
Squamous cell carcinoma louisiana Basal cell carcinoma
Basal cell carcinoma Squamous cell carcinoma
Squamous cell carcinoma Non neoplastic epithelial disorders
Non neoplastic epithelial disorders Bcc pathology
Bcc pathology Hedgehog urchin
Hedgehog urchin Papillary carcinoma
Papillary carcinoma Epithelial cells in urine images
Epithelial cells in urine images Ivc summer classes for high school students
Ivc summer classes for high school students Irvine valley college transcripts
Irvine valley college transcripts Ivc paralegal program
Ivc paralegal program Dmh 5-72-19
Dmh 5-72-19 Hepatic portal vein
Hepatic portal vein Ivc iniciacion a la vida cristiana
Ivc iniciacion a la vida cristiana Denali ivc filter mri
Denali ivc filter mri Ivc transfer center
Ivc transfer center Poloparazit
Poloparazit Ivc plethora definition
Ivc plethora definition Slidetodoc.com
Slidetodoc.com Neuro derm
Neuro derm Neoplasia
Neoplasia Invasive ductal carcinoma with medullary features
Invasive ductal carcinoma with medullary features Breast cancer staging chart
Breast cancer staging chart Carcinoma de mama
Carcinoma de mama Carcinoma in situ
Carcinoma in situ Lobular breast
Lobular breast