Acute Chronic Sinusitis Ephraim Eviatar Assaf Harofeh Medical







- Slides: 52
Acute & Chronic Sinusitis המשך לימודי Ephraim Eviatar Assaf Harofeh Medical Center

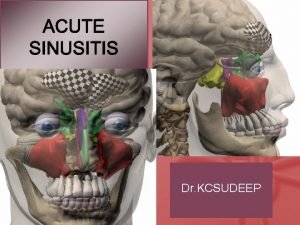
Rhinosinusitis Acute rhinosinusitis Subacute rhinosinusitis Chronic rhinosinusitis Recurrent ARS Acute rhinosinusitis superimposed on CRS
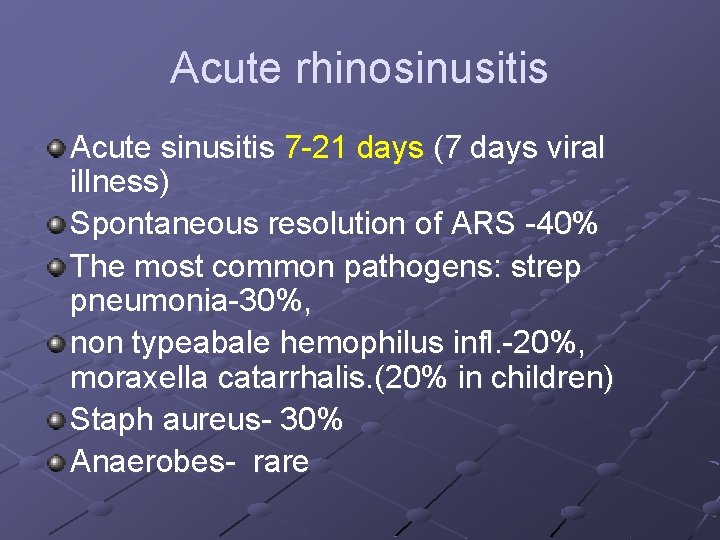
Acute rhinosinusitis Acute sinusitis 7 -21 days (7 days viral illness) Spontaneous resolution of ARS -40% The most common pathogens: strep pneumonia-30%, non typeabale hemophilus infl. -20%, moraxella catarrhalis. (20% in children) Staph aureus- 30% Anaerobes- rare
Recurrent ARS Episodes of bacterial infection of the paranasal sinuses, each lasting less than 30 days and separated by intervals of at least 10 days during which the patient is asymptomatic.
Subacute sinusitis Subacute RS: 3 W-3 months The same pathogens as in ARS
Chronic rhinosinusitis Beyond 3 months Bacteria are as in ARS, but More non-typeable H Influezae More staph aureus, anaerobic bacteria, gram- Negative, pseudomonase aeruginosa Polymicrobials with resistant organism Culture recommended
Acute bacterial sinusitis superimposed on chronic sinusitis Patients with residual respiratory symptoms develop new respiratory symptoms. When treated with antimicrobials, these new symptoms resolve, but the underlying residual symptoms do not.
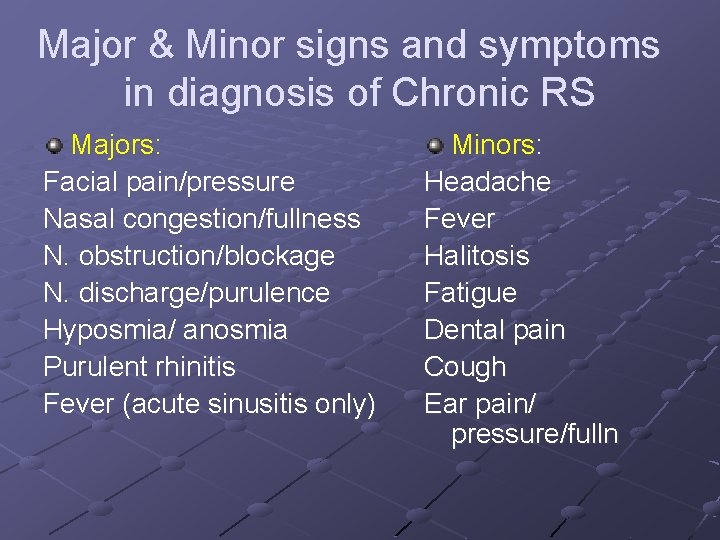
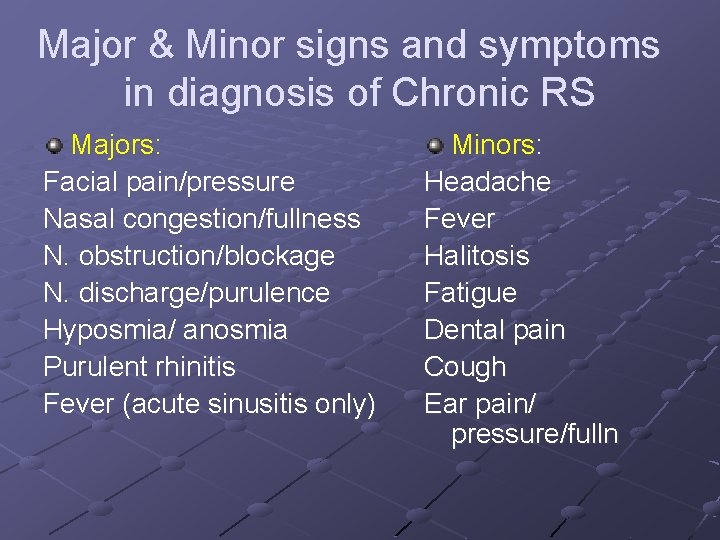
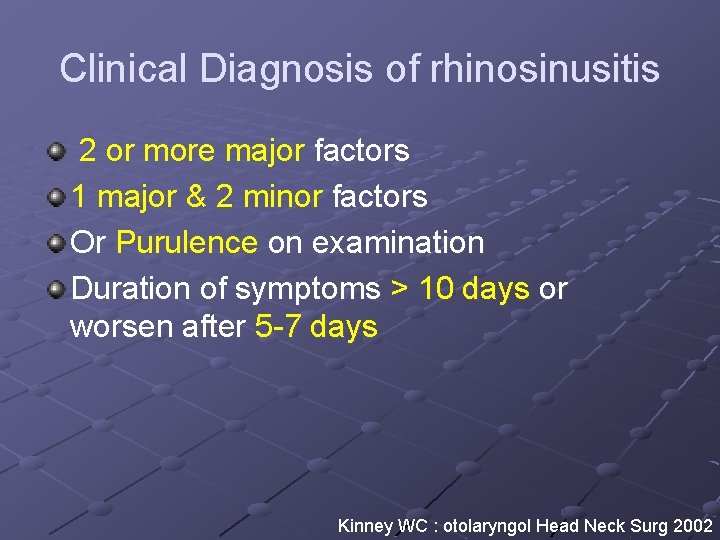
Major & Minor signs and symptoms in diagnosis of Chronic RS Majors: Facial pain/pressure Nasal congestion/fullness N. obstruction/blockage N. discharge/purulence Hyposmia/ anosmia Purulent rhinitis Fever (acute sinusitis only) Minors: Headache Fever Halitosis Fatigue Dental pain Cough Ear pain/ pressure/fulln
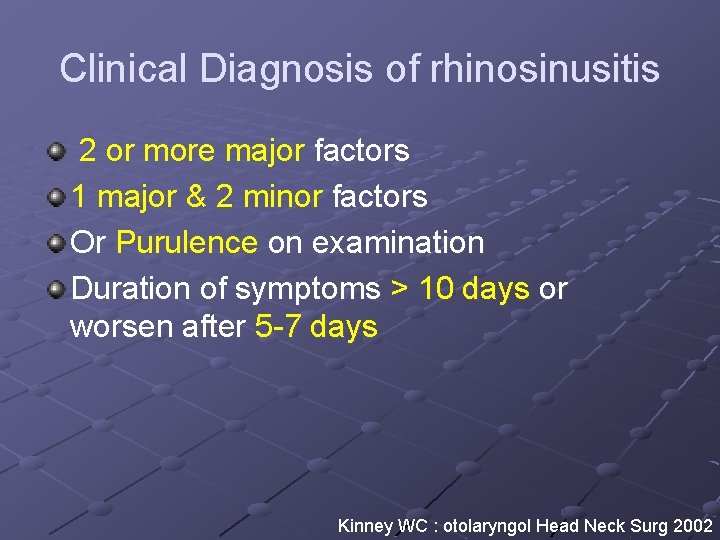
Clinical Diagnosis of rhinosinusitis 2 or more major factors 1 major & 2 minor factors Or Purulence on examination Duration of symptoms > 10 days or worsen after 5 -7 days Kinney WC : otolaryngol Head Neck Surg 2002
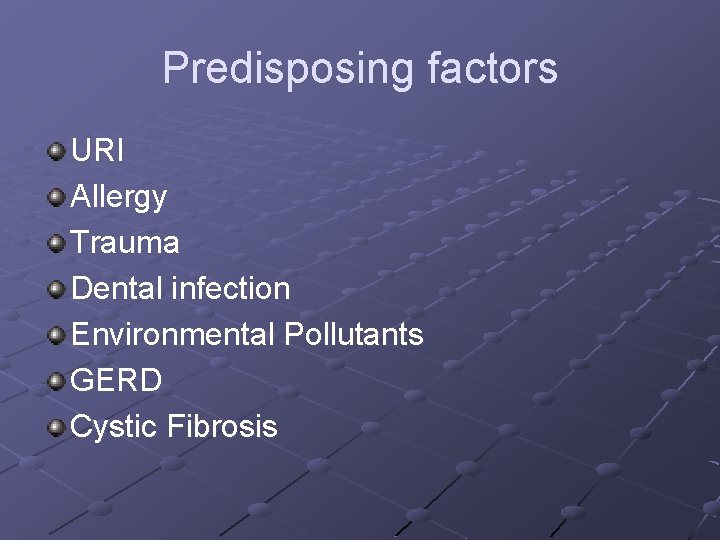
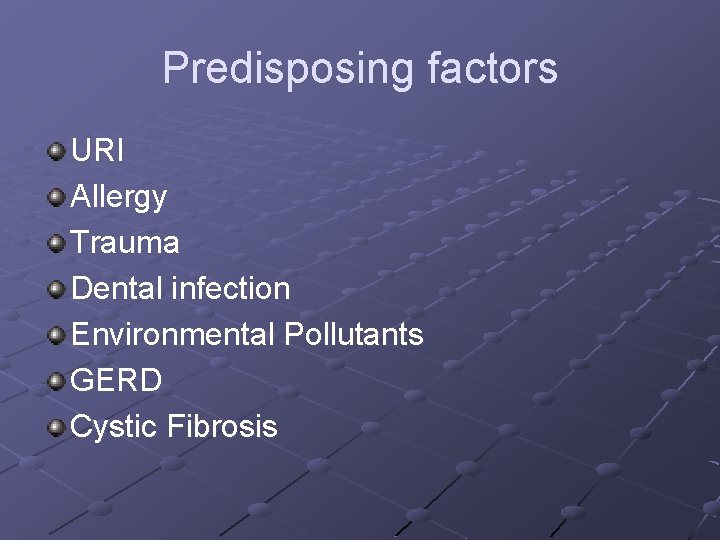
Predisposing factors URI Allergy Trauma Dental infection Environmental Pollutants GERD Cystic Fibrosis
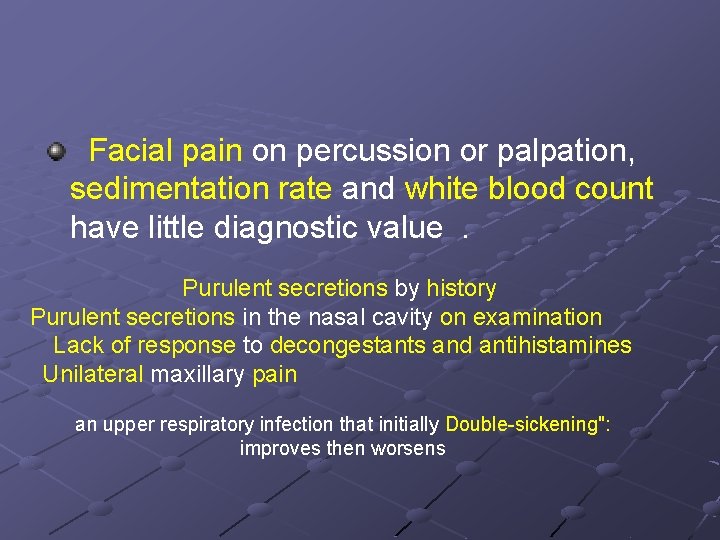
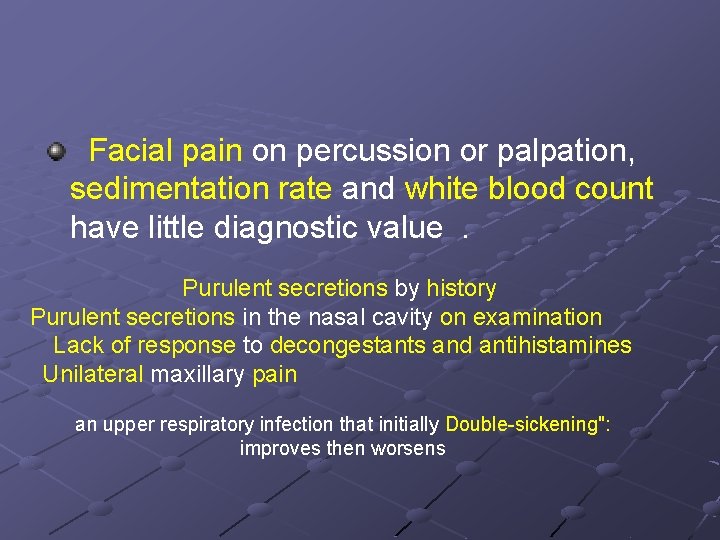
Facial pain on percussion or palpation, sedimentation rate and white blood count have little diagnostic value . Purulent secretions by history Purulent secretions in the nasal cavity on examination Lack of response to decongestants and antihistamines Unilateral maxillary pain an upper respiratory infection that initially Double-sickening": improves then worsens
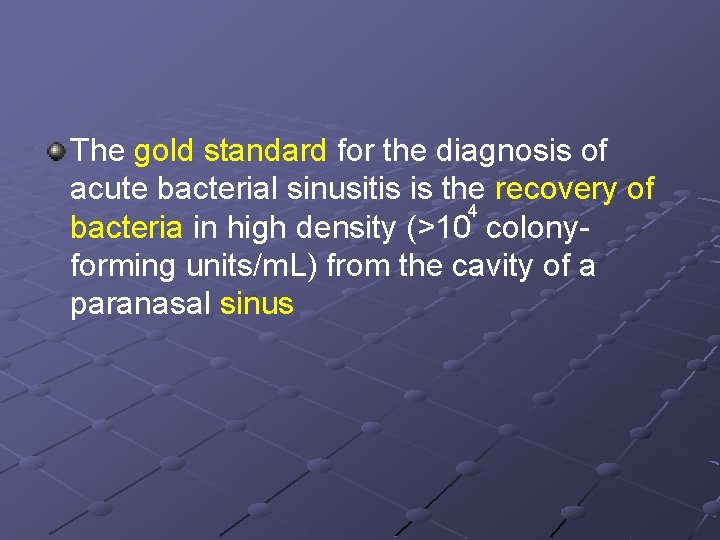
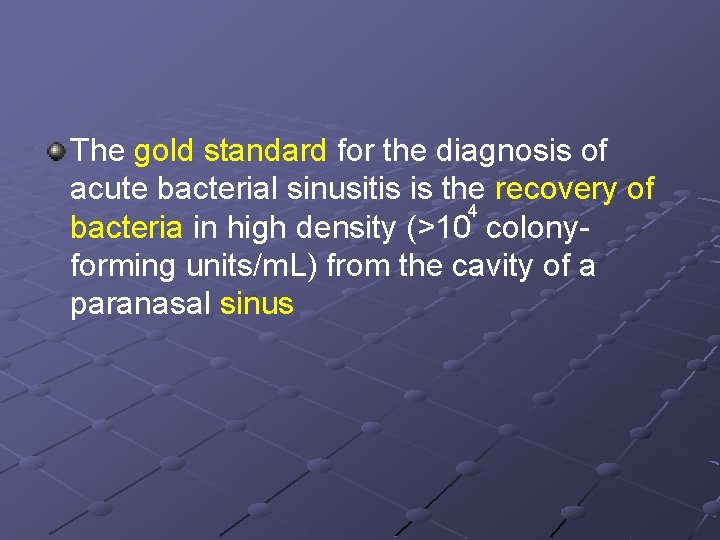
The gold standard for the diagnosis of acute bacterial sinusitis is the recovery of 4 bacteria in high density (>10 colonyforming units/m. L) from the cavity of a paranasal sinus
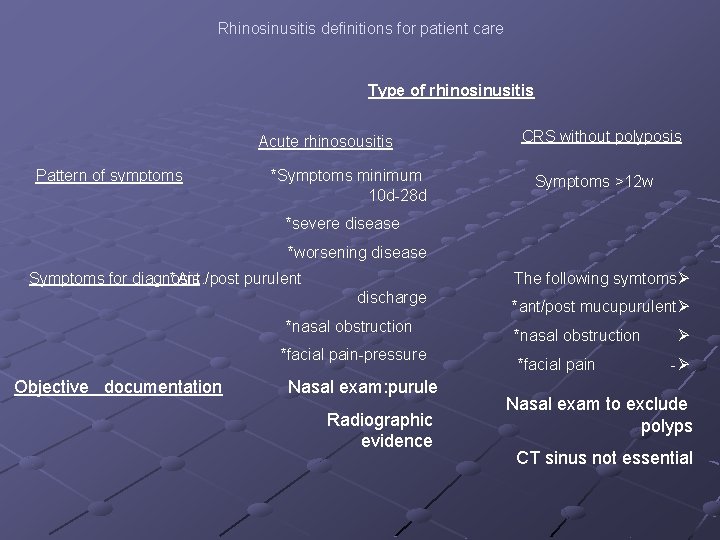
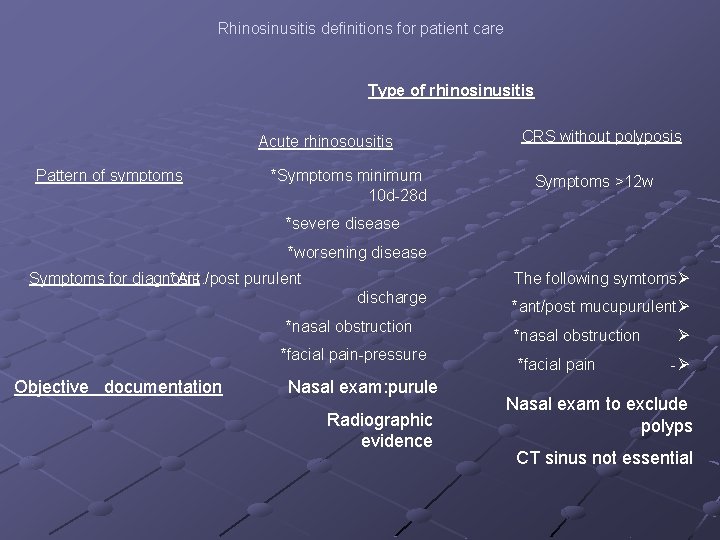
Rhinosinusitis definitions for patient care Type of rhinosinusitis Acute rhinosousitis Pattern of symptoms *Symptoms minimum 10 d-28 d CRS without polyposis Symptoms >12 w *severe disease *worsening disease Symptoms for diagnosis *Ant. /post purulent discharge *nasal obstruction *facial pain-pressure Objective documentation Nasal exam: purule Radiographic evidence The following symtomsØ *ant/post mucupurulentØ *nasal obstruction Ø *facial pain -Ø Nasal exam to exclude polyps CT sinus not essential
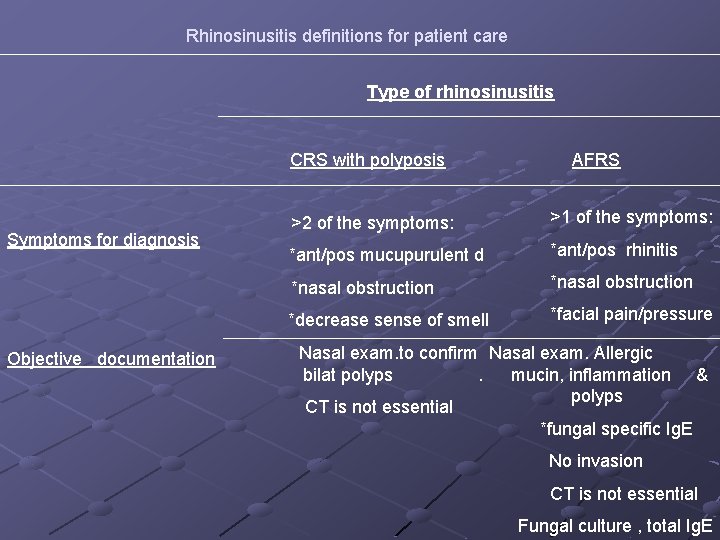
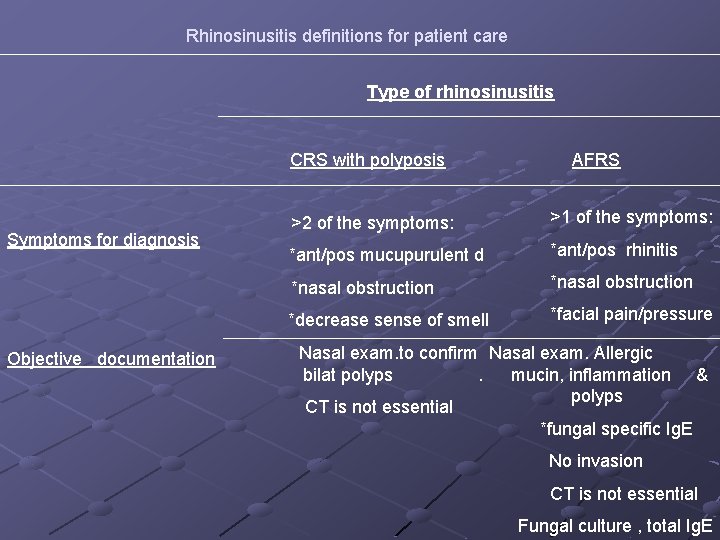
Rhinosinusitis definitions for patient care Type of rhinosinusitis CRS with polyposis Symptoms for diagnosis Objective documentation AFRS >2 of the symptoms: >1 of the symptoms: *ant/pos mucupurulent d *ant/pos rhinitis *nasal obstruction *decrease sense of smell *facial pain/pressure Nasal exam. to confirm Nasal exam. Allergic bilat polyps . mucin, inflammation & polyps CT is not essential *fungal specific Ig. E No invasion CT is not essential Fungal culture , total Ig. E
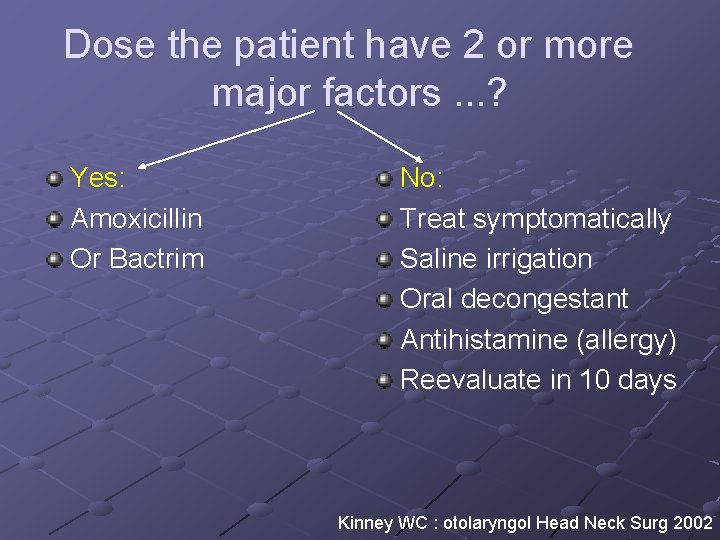
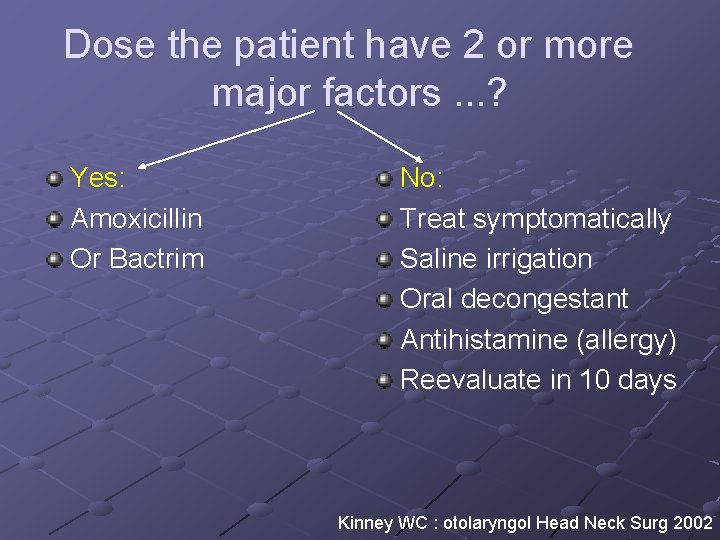
Dose the patient have 2 or more major factors. . . ? Yes: Amoxicillin Or Bactrim No: Treat symptomatically Saline irrigation Oral decongestant Antihistamine (allergy) Reevaluate in 10 days Kinney WC : otolaryngol Head Neck Surg 2002
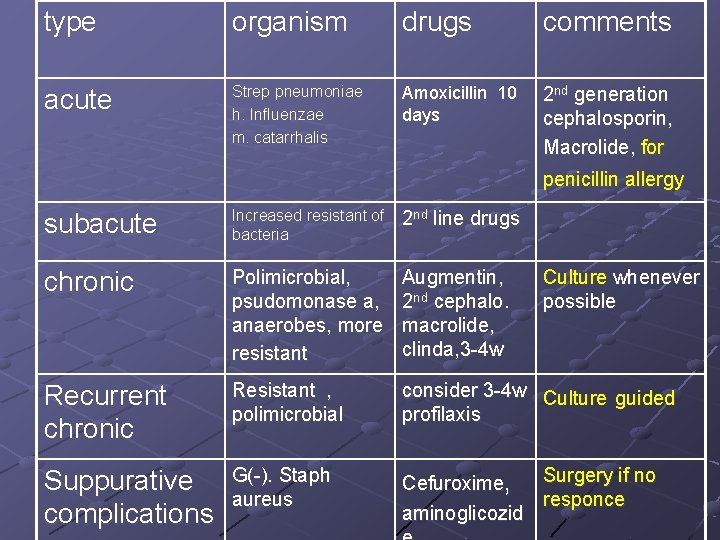
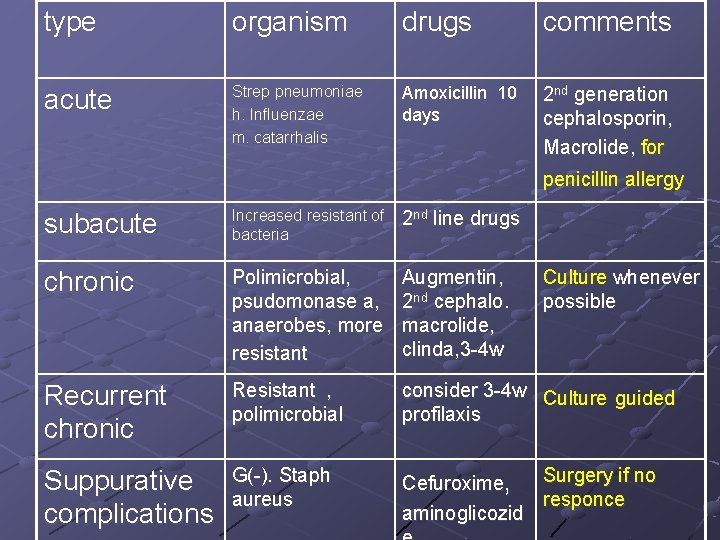
type organism drugs comments acute Strep pneumoniae h. Influenzae m. catarrhalis Amoxicillin 10 days 2 nd generation cephalosporin, Macrolide, for penicillin allergy subacute Increased resistant of bacteria 2 nd line drugs chronic Polimicrobial, psudomonase a, anaerobes, more resistant Augmentin, 2 nd cephalo. macrolide, clinda, 3 -4 w Recurrent chronic Resistant , polimicrobial consider 3 -4 w Culture guided profilaxis Suppurative complications G(-). Staph aureus Surgery if no Cefuroxime, responce aminoglicozid Culture whenever possible
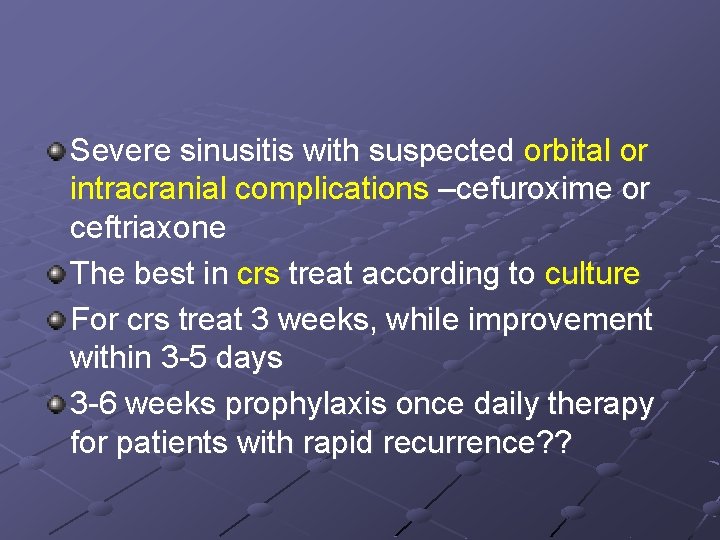
Severe sinusitis with suspected orbital or intracranial complications –cefuroxime or ceftriaxone The best in crs treat according to culture For crs treat 3 weeks, while improvement within 3 -5 days 3 -6 weeks prophylaxis once daily therapy for patients with rapid recurrence? ?
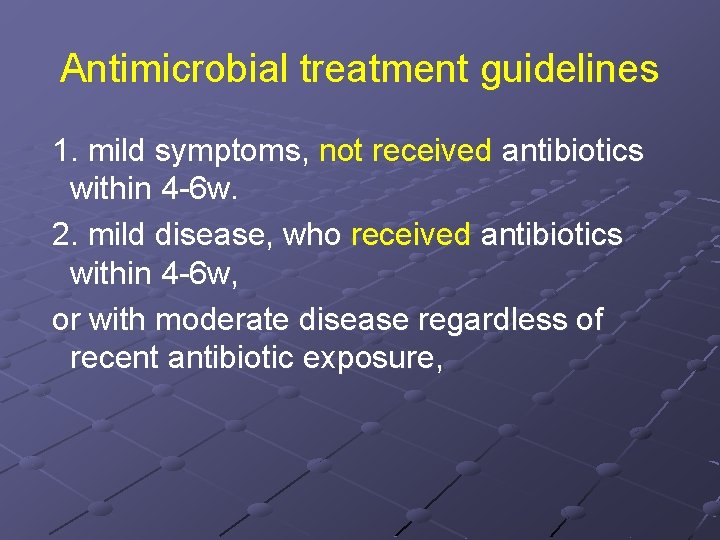
Antimicrobial treatment guidelines 1. mild symptoms, not received antibiotics within 4 -6 w. 2. mild disease, who received antibiotics within 4 -6 w, or with moderate disease regardless of recent antibiotic exposure,

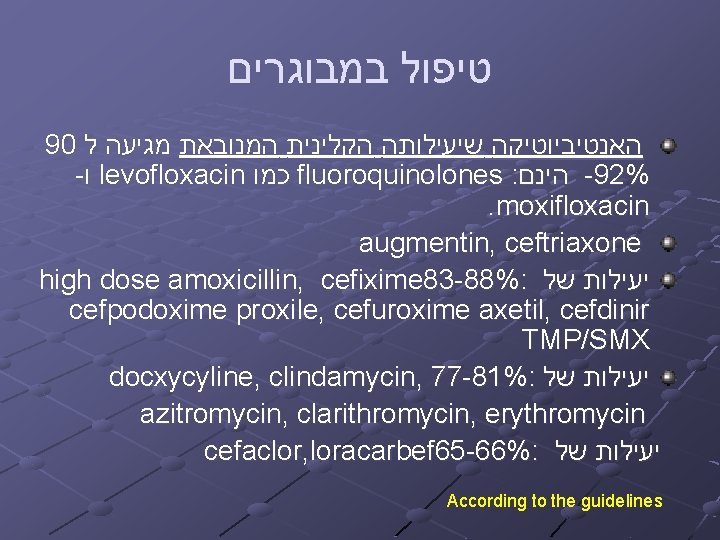
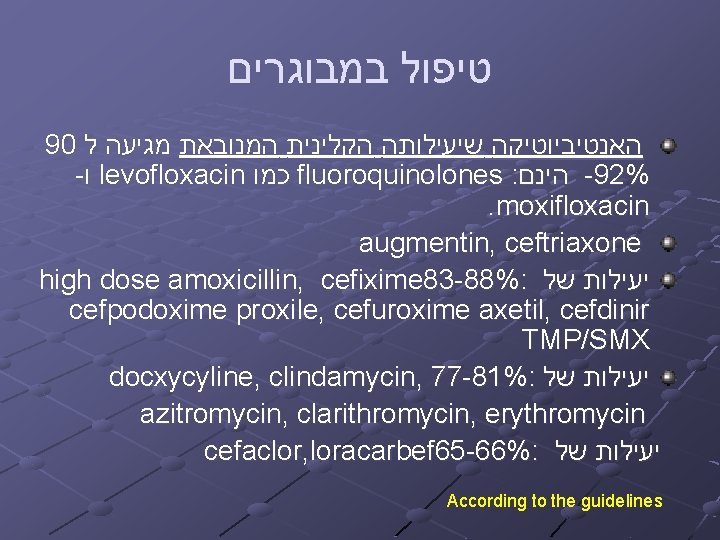
במבוגרים טיפול 90 ל מגיעה המנובאת הקלינית שיעילותה האנטיביוטיקה - ו levofloxacin כמו fluoroquinolones : הינם -92%. moxifloxacin augmentin, ceftriaxone high dose amoxicillin, cefixime 83 -88%: של יעילות cefpodoxime proxile, cefuroxime axetil, cefdinir TMP/SMX docxycyline, clindamycin, 77 -81%: של יעילות azitromycin, clarithromycin, erythromycin cefaclor, loracarbef 65 -66%: של יעילות According to the guidelines
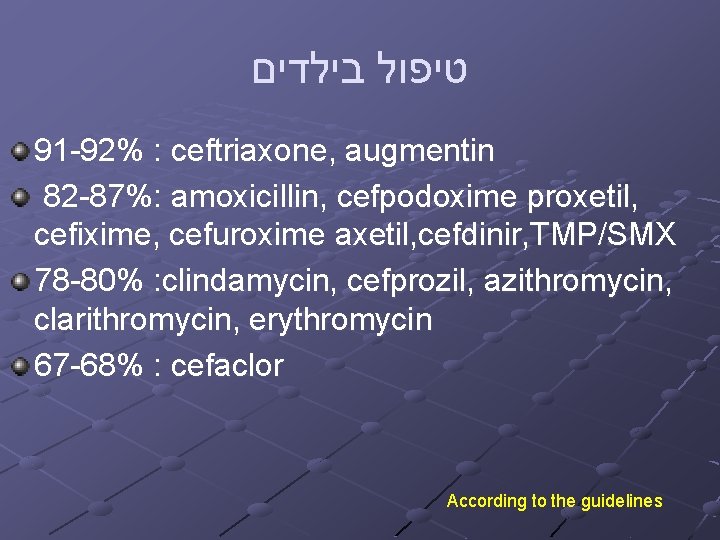
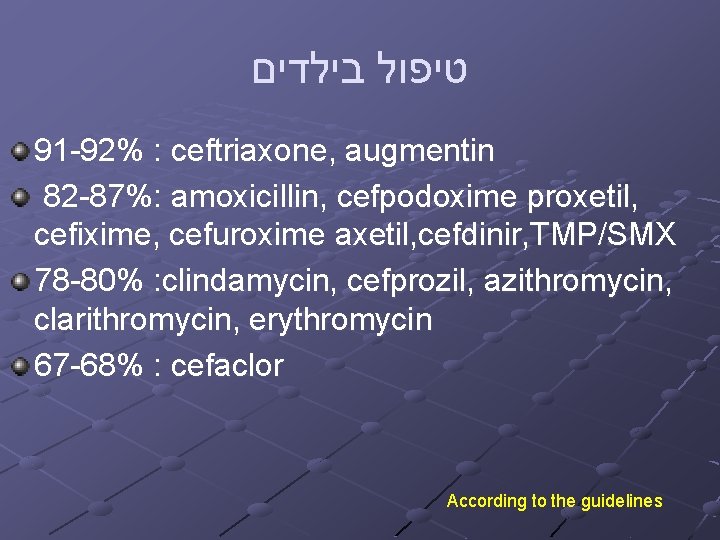
בילדים טיפול 91 -92% : ceftriaxone, augmentin 82 -87%: amoxicillin, cefpodoxime proxetil, cefixime, cefuroxime axetil, cefdinir, TMP/SMX 78 -80% : clindamycin, cefprozil, azithromycin, clarithromycin, erythromycin 67 -68% : cefaclor According to the guidelines
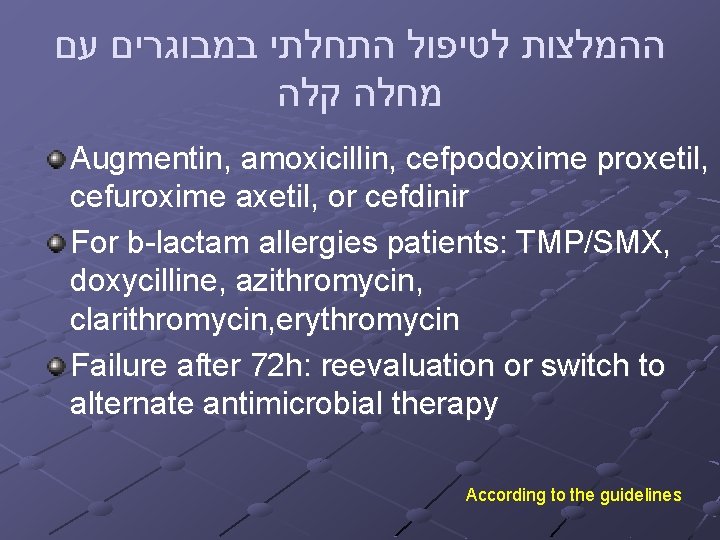
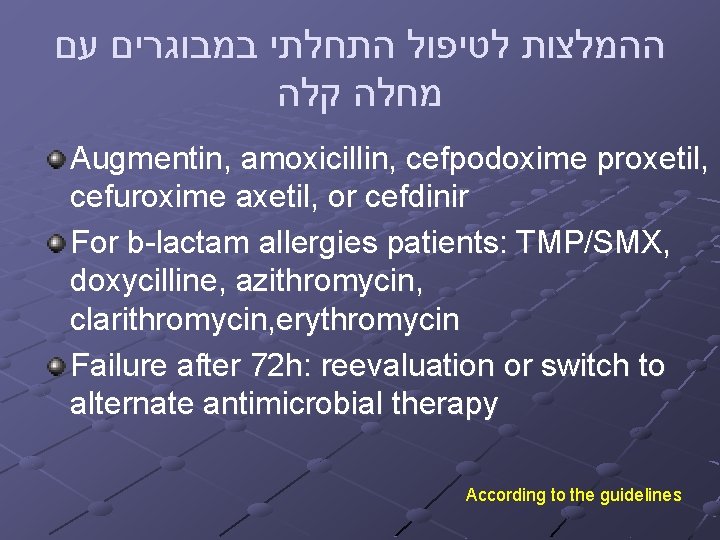
עם במבוגרים התחלתי לטיפול ההמלצות קלה מחלה Augmentin, amoxicillin, cefpodoxime proxetil, cefuroxime axetil, or cefdinir For b-lactam allergies patients: TMP/SMX, doxycilline, azithromycin, clarithromycin, erythromycin Failure after 72 h: reevaluation or switch to alternate antimicrobial therapy According to the guidelines
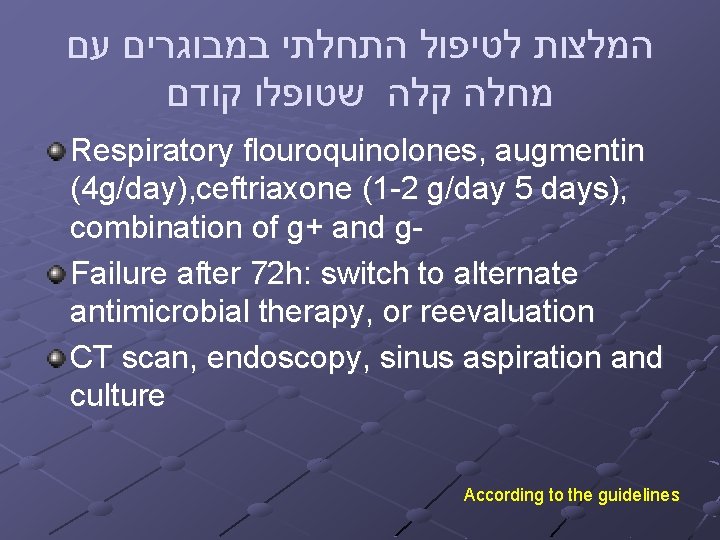
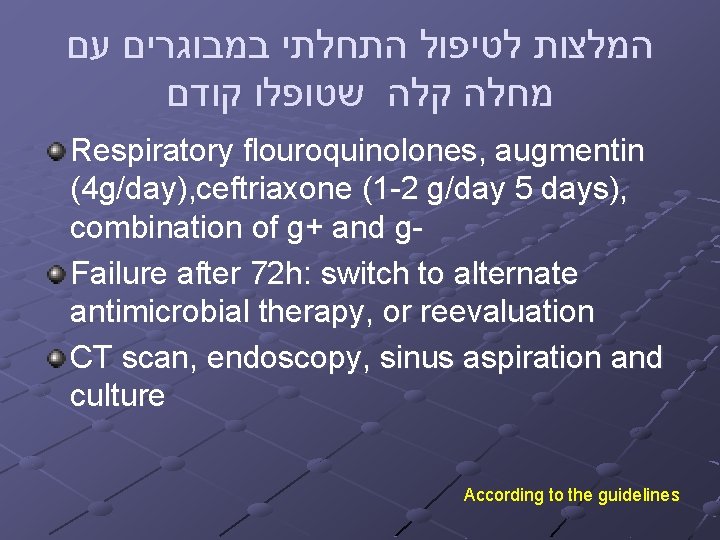
עם במבוגרים התחלתי לטיפול המלצות קודם שטופלו קלה מחלה Respiratory flouroquinolones, augmentin (4 g/day), ceftriaxone (1 -2 g/day 5 days), combination of g+ and g. Failure after 72 h: switch to alternate antimicrobial therapy, or reevaluation CT scan, endoscopy, sinus aspiration and culture According to the guidelines
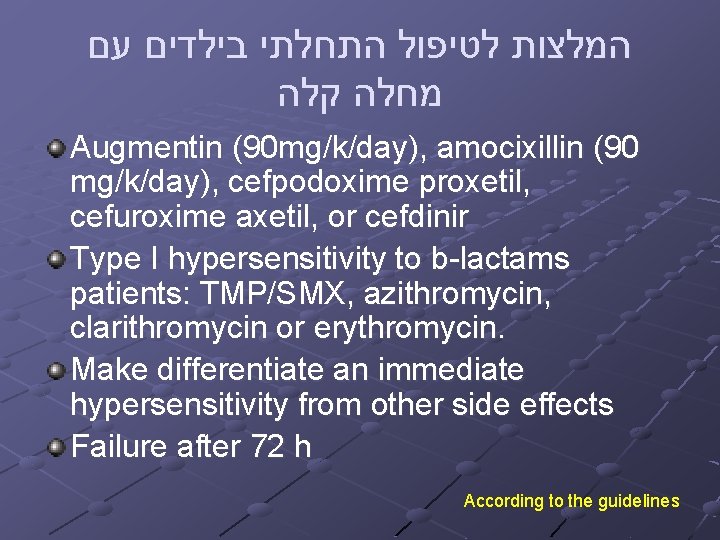
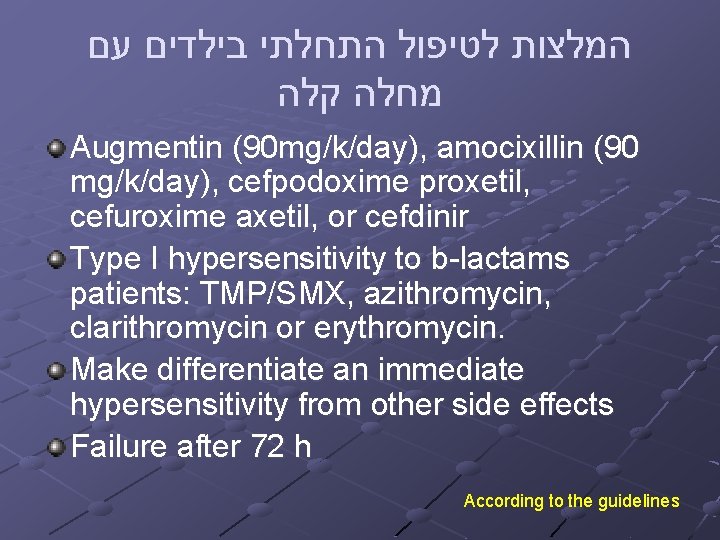
עם בילדים התחלתי לטיפול המלצות קלה מחלה Augmentin (90 mg/k/day), amocixillin (90 mg/k/day), cefpodoxime proxetil, cefuroxime axetil, or cefdinir Type I hypersensitivity to b-lactams patients: TMP/SMX, azithromycin, clarithromycin or erythromycin. Make differentiate an immediate hypersensitivity from other side effects Failure after 72 h According to the guidelines
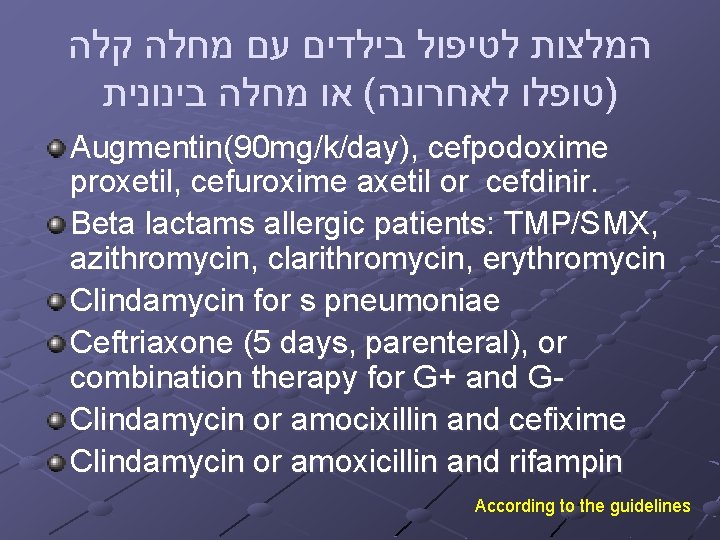
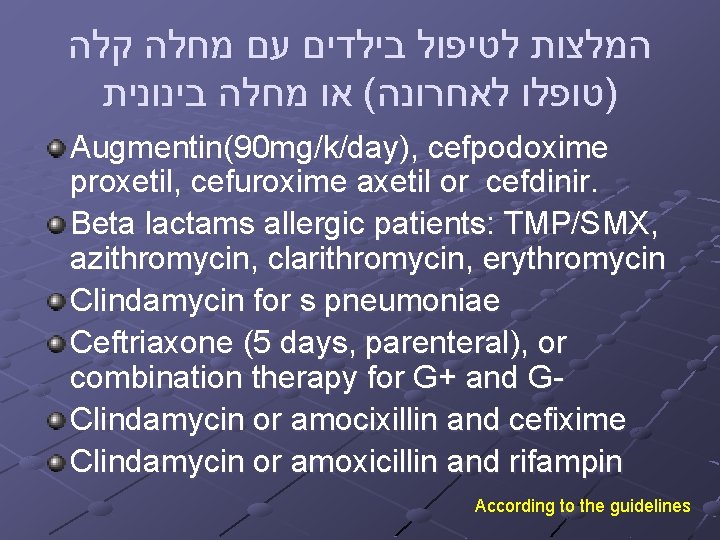
קלה מחלה עם בילדים לטיפול המלצות בינונית מחלה או ( לאחרונה )טופלו Augmentin(90 mg/k/day), cefpodoxime proxetil, cefuroxime axetil or cefdinir. Beta lactams allergic patients: TMP/SMX, azithromycin, clarithromycin, erythromycin Clindamycin for s pneumoniae Ceftriaxone (5 days, parenteral), or combination therapy for G+ and G- Clindamycin or amocixillin and cefixime Clindamycin or amoxicillin and rifampin According to the guidelines
New insights into the role of bacteria in CRS Bacterial superantigens-exotoxins that are able to activate T lymphocytes Pathogenesis of nasal polyposis- superantigens from S aureus
Biofilms-a artificial or damaged biologic surface that formed communicating organization of microorganisms surrounded by a glycocalys Biofilms is relatively impervious to antibiotics and is never eradicated Mechanical debridement- the only way to resolve biofilms
Osteitis: the role of the bone Osteomyelitis can be seen at a distance from the primary infection Inflammatory bone changes were noted on contralateral side in 52% of the animals Khalid et al. laryngoscope 2002 The changes in the involved bone can explain why CRS is relatively resistant to medical therapy.
Failed CRS To sinus surgery or systemic steroid/antibiotics Macrolid therapy (long term, low dose) effective Cervin A et al: Otolaryngol Head Neck Surg 2002
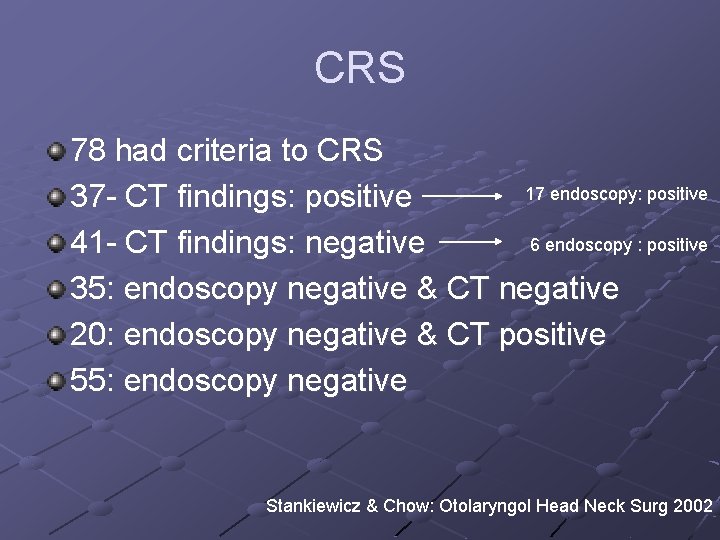
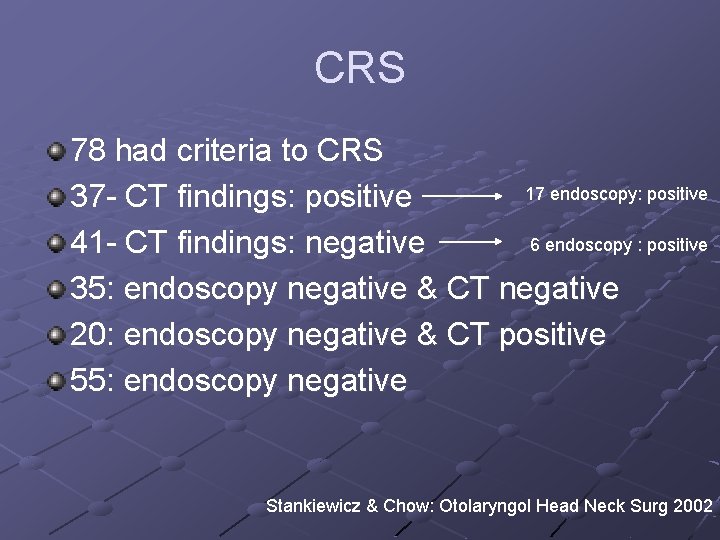
CRS 78 had criteria to CRS 17 endoscopy: positive 37 - CT findings: positive 6 endoscopy : positive 41 - CT findings: negative 35: endoscopy negative & CT negative 20: endoscopy negative & CT positive 55: endoscopy negative Stankiewicz & Chow: Otolaryngol Head Neck Surg 2002
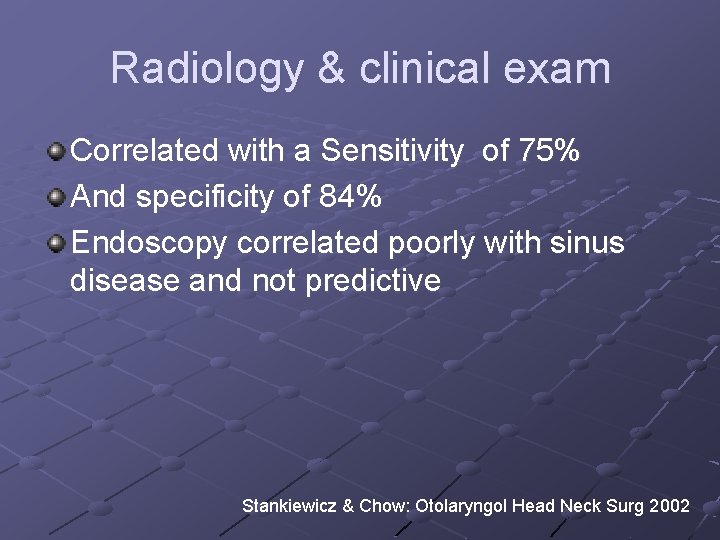
Radiology & clinical exam Correlated with a Sensitivity of 75% And specificity of 84% Endoscopy correlated poorly with sinus disease and not predictive Stankiewicz & Chow: Otolaryngol Head Neck Surg 2002

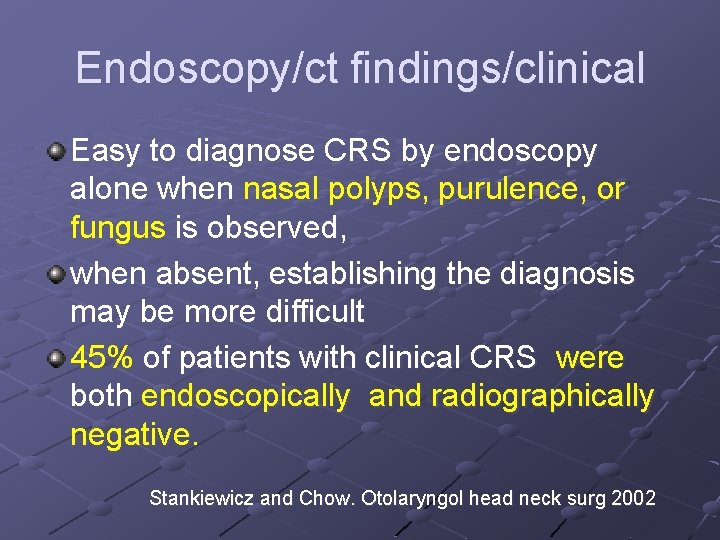
Endoscopy/ct findings/clinical Easy to diagnose CRS by endoscopy alone when nasal polyps, purulence, or fungus is observed, when absent, establishing the diagnosis may be more difficult 45% of patients with clinical CRS were both endoscopically and radiographically negative. Stankiewicz and Chow. Otolaryngol head neck surg 2002
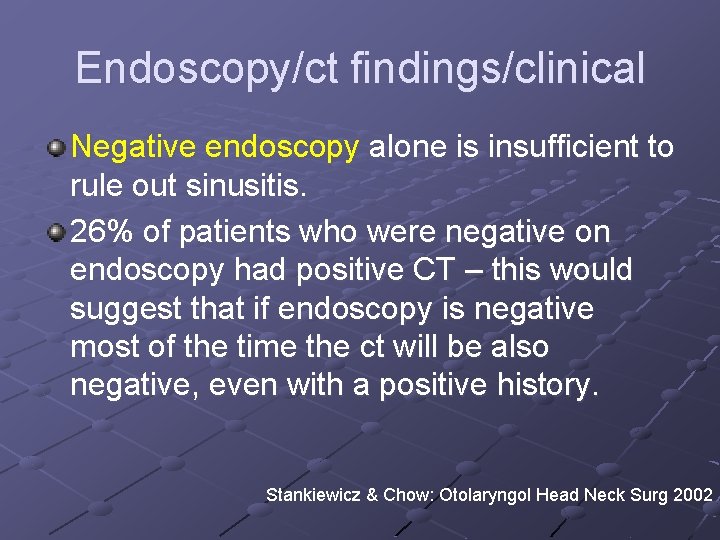
Endoscopy/ct findings/clinical Negative endoscopy alone is insufficient to rule out sinusitis. 26% of patients who were negative on endoscopy had positive CT – this would suggest that if endoscopy is negative most of the time the ct will be also negative, even with a positive history. Stankiewicz & Chow: Otolaryngol Head Neck Surg 2002
בילדים גדול יופיע (URI )בעקבות חיידקי שזיהום הסיכון ימים 10 מעל נמשכת המחלה אם יותר סימפטומים עם ומבוגרים בילדים תעשה אבחנה או ימים 10 אחרי השתפרו שלא VIRAL URI של . ימים 5 -7 אחרי הוחמרו The diagnosis of acute bacterial sinusitis is based on clinical criteria in children who present with upper respiratory symptoms that are either persistent or severe Guidelines of American Academy of Pediatrics
בילדים Persistent symptoms are those that last longer than 10 to 14, but less than 30, days. Such symptoms include nasal or postnasal discharge (of any quality), daytime cough (which may be worse at night), or both. Guidelines of American Academy of Pediatrics
בילדים Severe symptoms include a temperature of at least 102°F (39 o. C) and purulent nasal discharge present concurrently for at least 3 to 4 consecutive days in a child who seems ill. The child who seems toxic should be hospitalized and is not considered in this algorithm. Guidelines of American Academy of Pediatrics

ARS in children Diagnosis in children based on clinical criteria Radiology is only for complications, persistent or recurrent sinusitis For prevention there is no prophylactic antimicrobial treatment, ancillary therapies, complementary/alternative medicine Guidelines of American Academy of Pediatrics
Surgical management of crs in children 5 -8 events of colds/year 5%-13% will complicate by acute RS Most of children with RS respond to medical treatment Today surgery consist of sinus lavage, ESS, adenoidectomy
Goal of surgery Surgery is for control of symptoms, better quality of life and to prevent complications Indications to surgery are not uniform between OL and P “cure”-the goal for surgery, but is not the likely end point Reversible mucosal disease may be possible in the long run, but is unlikely to be realized in the short term

Maximal medical management Reflux Macrolids Antileukotriens Irrigations-nasal sprays Alternative medical approaches

Surgical management children Biomaterials Subperiosteal abscess
The surgical site in children There is strong evidence to support the fact that the OMC area is the primary site of involvement of inflammatory sinuses disease.

Surgical management in children Role of adenoidectomy: 1. reservoir for pathogenic bacteria 2. interfere with nasal mucociliary clearance 3. better drainage Overall success of adenoidectomy-50% Studies show reduction in the number of bacterial pathogens in the nasopharynx after adenoidectomy
? Fear of surgery Surgery may cause growth retardation of the midface Bothwell et al. showed no difference in facial growth of children with CRS who operated compare with children who refused surgery.
Surgery Children who fail medical therapy benefit from surgery Adenoidectomy recommended initially for children 6 years of age (no asthma, low CT score) ESS and adenoidectomy for children older than 6 (asthma and high CT score) Ramadan. Laryngoscope. 2004
Results of surgery children Older children do better than youngest Old children (>6 y/o)- successes rate is 89% , but younger children (<6 y/o)- successes rate is only 73% >3 y/o who were operated have 75% chance to be reoperate
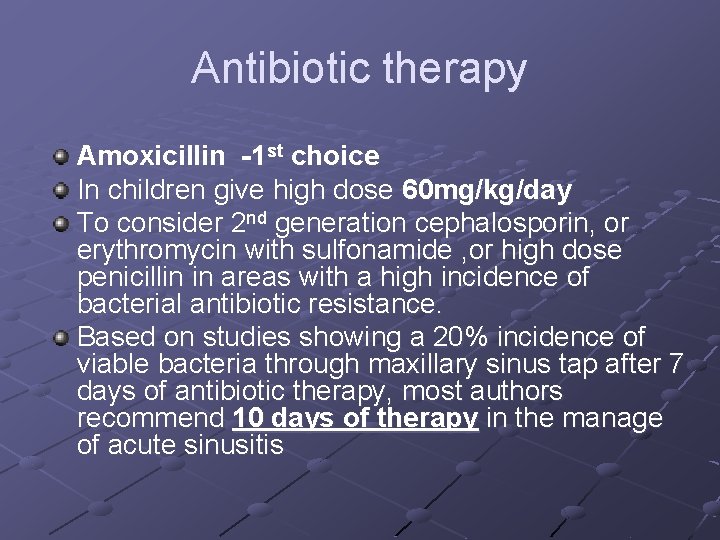
Antibiotic therapy Amoxicillin -1 st choice In children give high dose 60 mg/kg/day To consider 2 nd generation cephalosporin, or erythromycin with sulfonamide , or high dose penicillin in areas with a high incidence of bacterial antibiotic resistance. Based on studies showing a 20% incidence of viable bacteria through maxillary sinus tap after 7 days of antibiotic therapy, most authors recommend 10 days of therapy in the manage of acute sinusitis
 Chronic sinusitis
Chronic sinusitis Eviatar fields
Eviatar fields Morphological patterns of inflammation
Morphological patterns of inflammation Acute subacute chronic
Acute subacute chronic Acute vs chronic heart failure
Acute vs chronic heart failure Gallbladder
Gallbladder Leukemoid reaction
Leukemoid reaction Cardinal signs of inflammation
Cardinal signs of inflammation Chapter 18 common chronic and acute conditions
Chapter 18 common chronic and acute conditions Phoenix abscess
Phoenix abscess Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Ephraim mogale bursary
Ephraim mogale bursary Judges of israel
Judges of israel Ephraim mogale local municipality councillors
Ephraim mogale local municipality councillors Ephraim mogale local municipality councillors
Ephraim mogale local municipality councillors Ephraim temple
Ephraim temple Assaf natanzon
Assaf natanzon Assaf hamdani
Assaf hamdani Sqlshare
Sqlshare Eshrak assaf
Eshrak assaf Aare tool
Aare tool Allergic fungal sinusitis treatment
Allergic fungal sinusitis treatment Anillo de waldeyer
Anillo de waldeyer Frontonasoplaca
Frontonasoplaca Wikipedia
Wikipedia Rhinosinusite iness
Rhinosinusite iness Hiatus maxillaris
Hiatus maxillaris Criterios de centor
Criterios de centor Black mucus
Black mucus Sinusitis maxillaris chronica
Sinusitis maxillaris chronica Criterio de centor
Criterio de centor Clasificacion de sinusitis
Clasificacion de sinusitis Sinusitis
Sinusitis Pan sinusitis
Pan sinusitis Cartersville medical center medical records
Cartersville medical center medical records Greater baltimore medical center medical records
Greater baltimore medical center medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial medical center medical records
Torrance memorial medical center medical records Ptal california medical board
Ptal california medical board Multiple chronic conditions chartbook
Multiple chronic conditions chartbook Refifs
Refifs Scarred gallbladder
Scarred gallbladder Improving chronic illness care model
Improving chronic illness care model Cholecystitis nursing care plan
Cholecystitis nursing care plan Acute calculous cholecystitis
Acute calculous cholecystitis Hep b mode of transmission
Hep b mode of transmission Chronic rejection
Chronic rejection Chronic pain comorbidities
Chronic pain comorbidities Chronic amebiasis
Chronic amebiasis Chronic inflammation
Chronic inflammation Stigmata of chronic liver disease
Stigmata of chronic liver disease Wagner chronic care model 1998
Wagner chronic care model 1998 Dcld vs cld
Dcld vs cld