ACCAHA 2007 Guidelines on Periop Cardiovascular Evaluation and

- Slides: 55
ACC/AHA 2007 Guidelines on Periop. Cardiovascular Evaluation and Care for Noncardiac Surgery Department of Anesthesiology and Pain Medicine Chungang University College of Medicine Yang So Young
Preamble � Consensus of expert opinion after a thorough review of the available, current scientific evidence � Reviewed annually by the ACC/AHA (Oct. 23 rd, 2007)
Purpose of These Guidelines �Preoperative intervention is rarely necessary to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context �Purpose of preop. testing is not to give medical clearance but rather to perform an evaluation of the patient’s current medical status �No test should be performed unless it is likely to influence patient treatment
General Approach � Preoperative tests are recommended only if the information obtained will result in a change in; ◦ Surgical procedure performed ◦ Medical therapy or monitoring ◦ Postponement of surgery until the cardiac condition can be stabilized
General Approach � History � Physical examination & routine lab. Tests � Multivariable indices to predict preop. cardiac morbidity � Clinical assessment
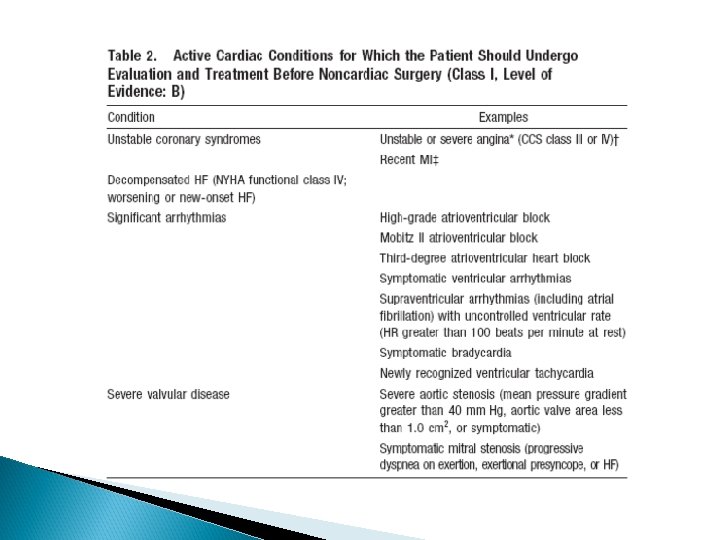
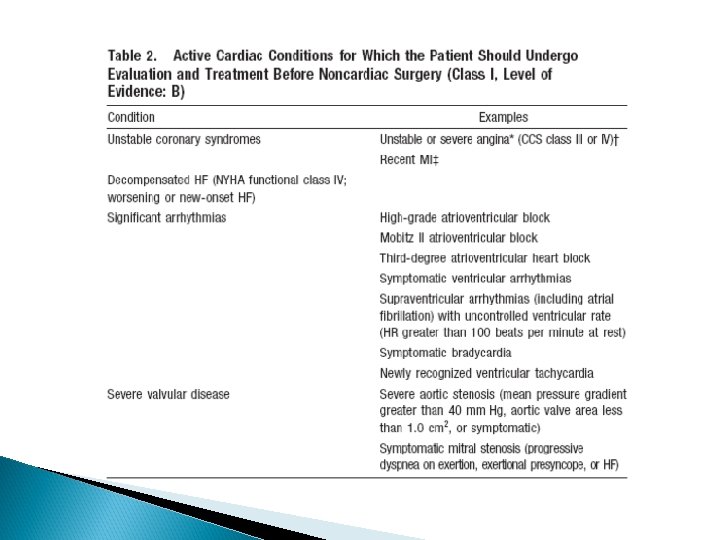
History �Crucial to the discovery of cardiac and/or comorbid disease �Should seek to identify serious cardiac conditions (Table 2) �Identify risk factors associated with increased periop. cardiovascular risk �In patients with established cardiac disease any recent changes in symptoms �Accurate recording of current medications
History � Determine patient’s functional capacity ◦ Correlate well with maximum oxygen uptake by treadmill testing
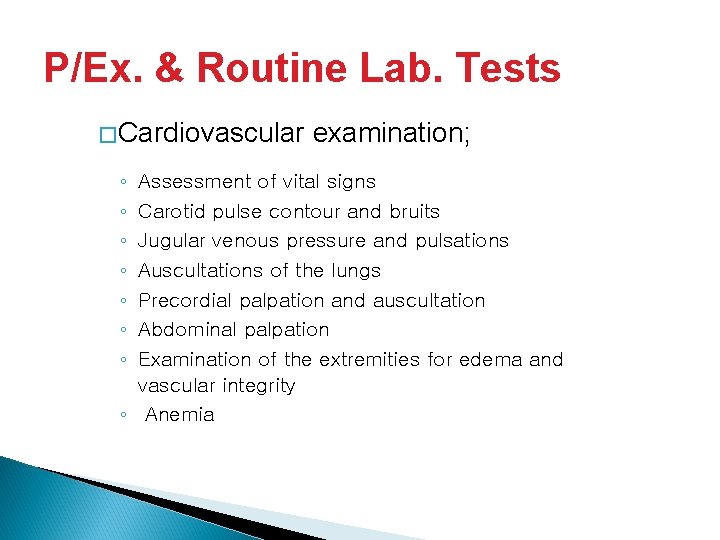
P/Ex. & Routine Lab. Tests �Cardiovascular ◦ ◦ ◦ ◦ examination; Assessment of vital signs Carotid pulse contour and bruits Jugular venous pressure and pulsations Auscultations of the lungs Precordial palpation and auscultation Abdominal palpation Examination of the extremities for edema and vascular integrity ◦ Anemia
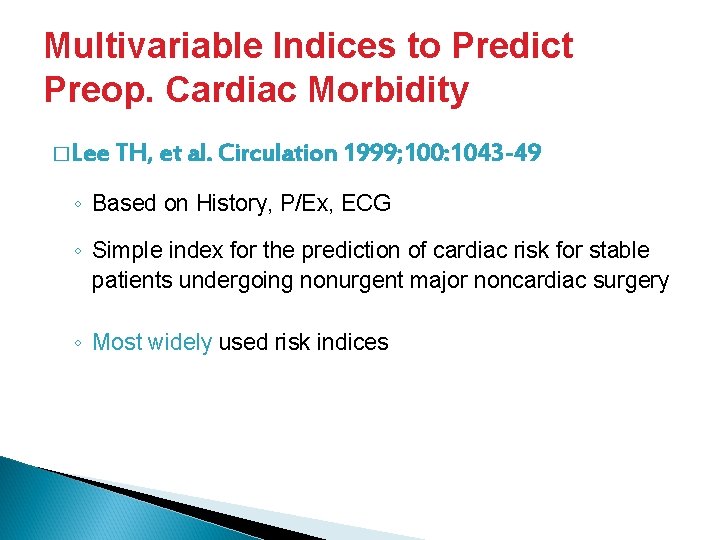
Multivariable Indices to Predict Preop. Cardiac Morbidity � Lee TH, et al. Circulation 1999; 100: 1043 -49 ◦ Based on History, P/Ex, ECG ◦ Simple index for the prediction of cardiac risk for stable patients undergoing nonurgent major noncardiac surgery ◦ Most widely used risk indices
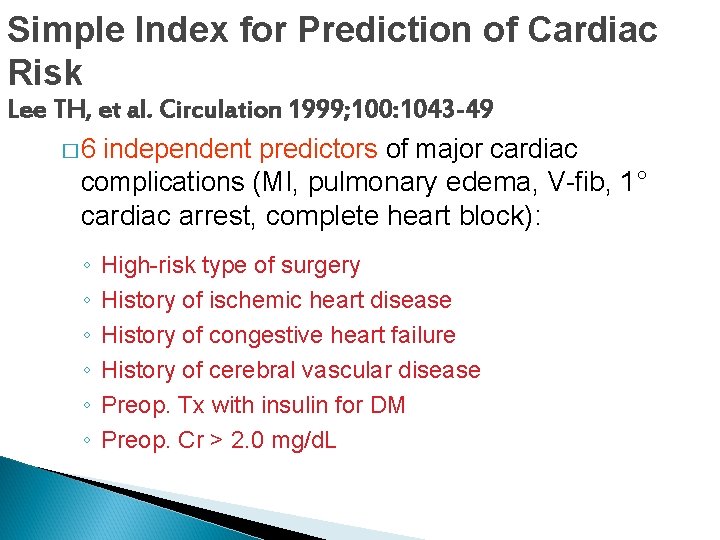
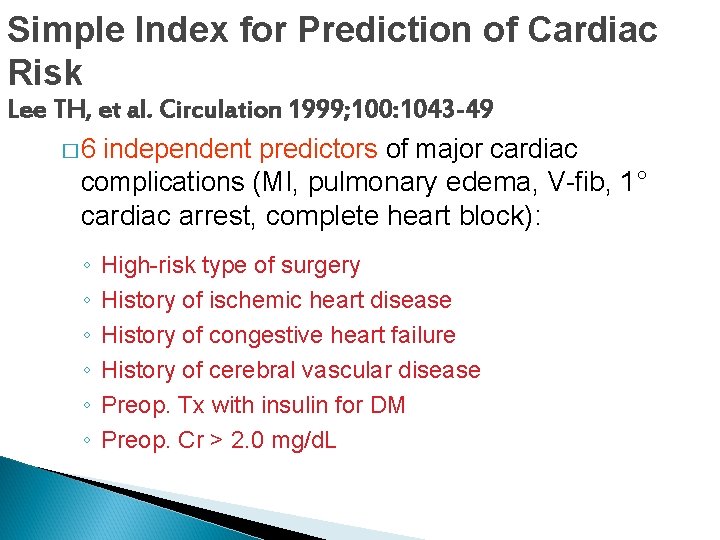
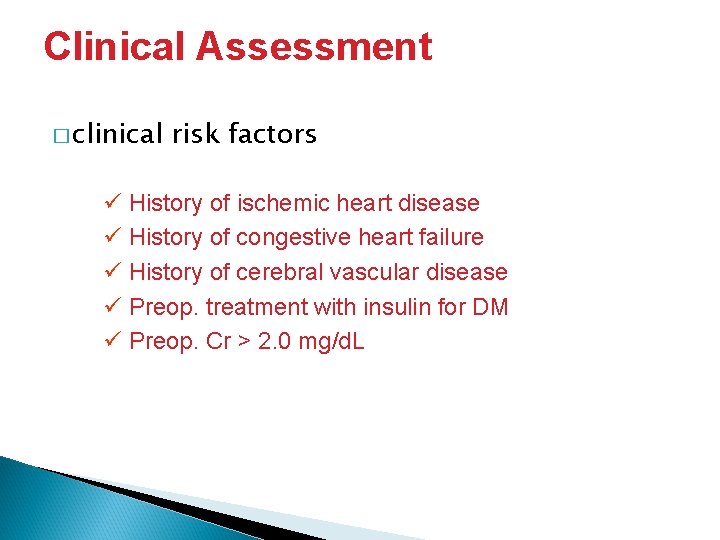
Simple Index for Prediction of Cardiac Risk Lee TH, et al. Circulation 1999; 100: 1043 -49 � 6 independent predictors of major cardiac complications (MI, pulmonary edema, V-fib, 1° cardiac arrest, complete heart block): ◦ ◦ ◦ High-risk type of surgery History of ischemic heart disease History of congestive heart failure History of cerebral vascular disease Preop. Tx with insulin for DM Preop. Cr > 2. 0 mg/d. L
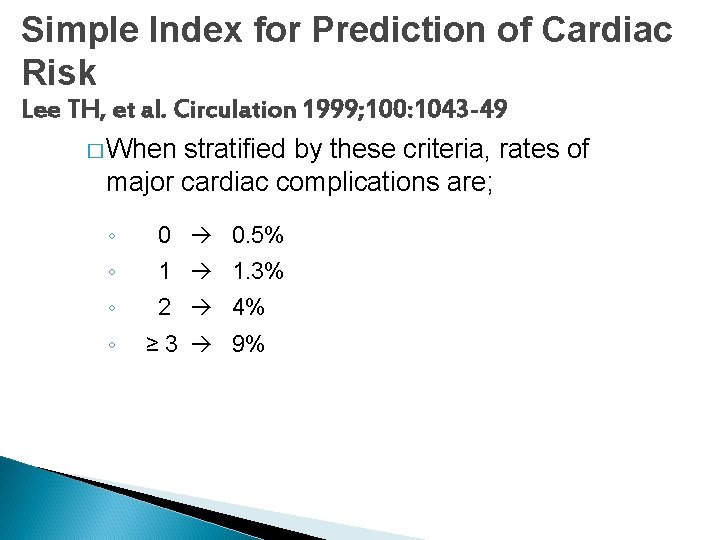
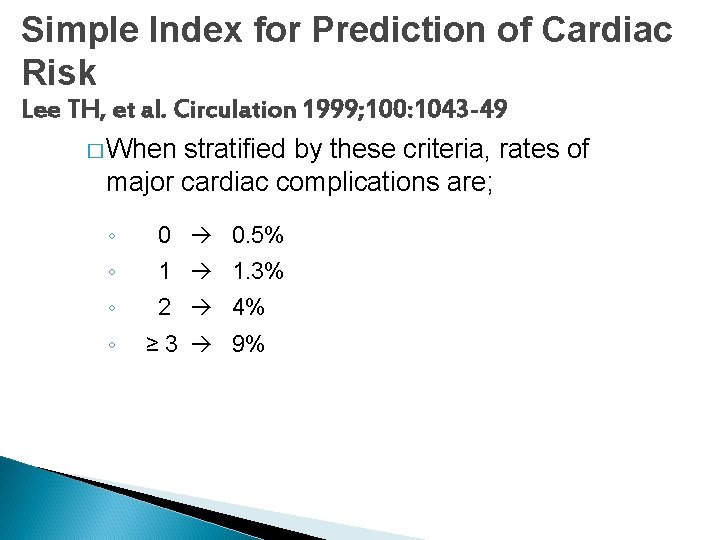
Simple Index for Prediction of Cardiac Risk Lee TH, et al. Circulation 1999; 100: 1043 -49 � When stratified by these criteria, rates of major cardiac complications are; ◦ 0 0. 5% ◦ 1 1. 3% ◦ 2 4% ◦ ≥ 3 9%
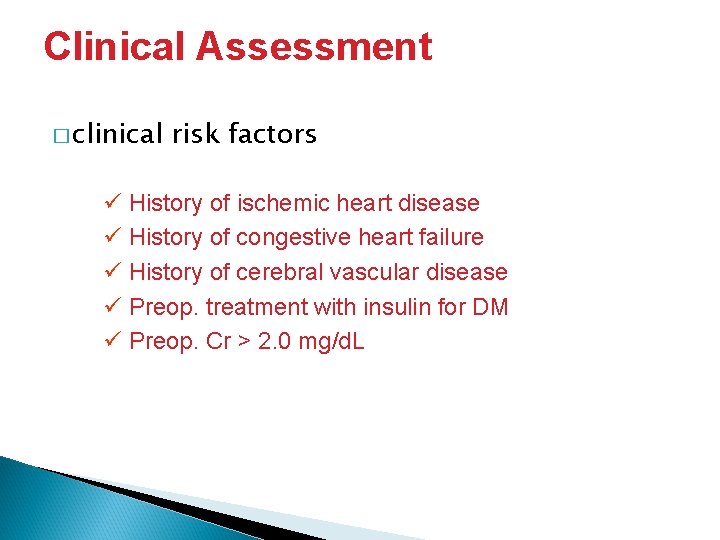
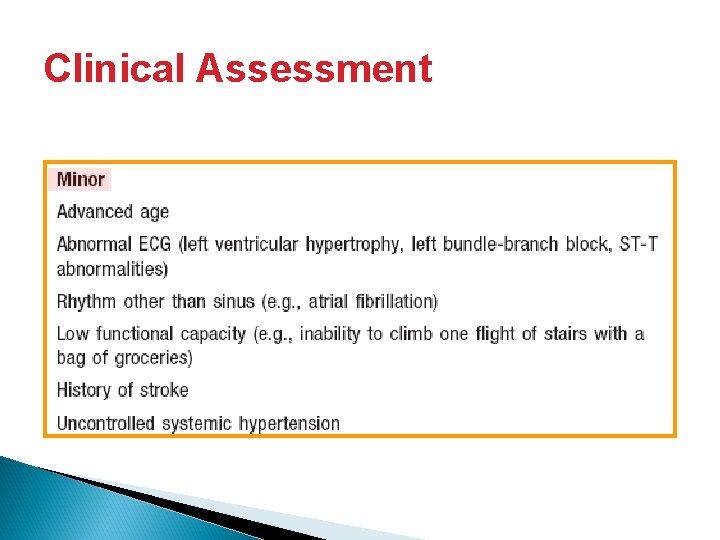
Clinical Assessment � clinical risk factors ü History of ischemic heart disease ü History of congestive heart failure ü History of cerebral vascular disease ü Preop. treatment with insulin for DM ü Preop. Cr > 2. 0 mg/d. L
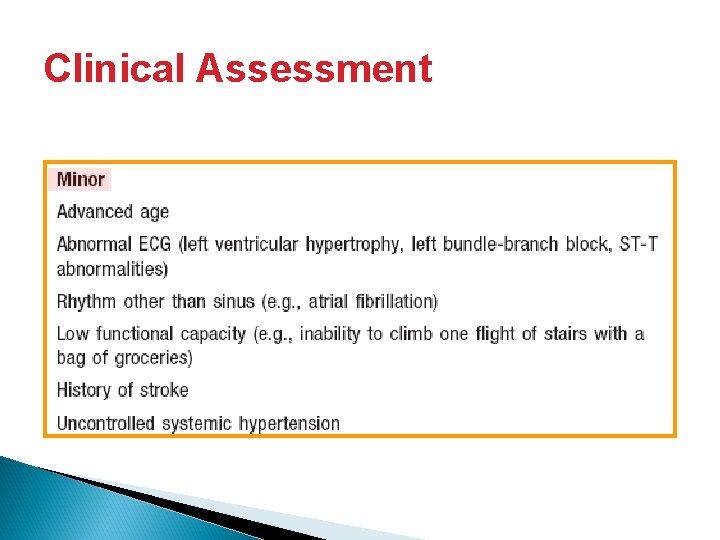
Clinical Assessment
2007 Guidelines
Disease Specific Approaches � Coronary artery disease � Hypertension � Valvular heart disease � Arrhythmias & conduction abnl
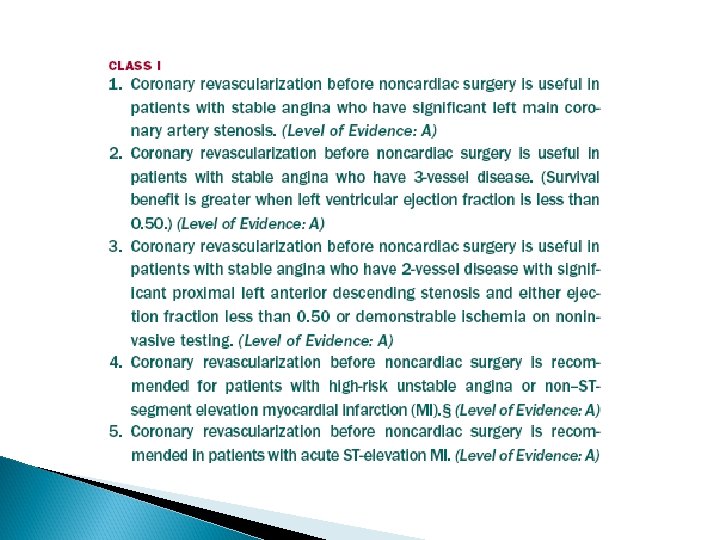
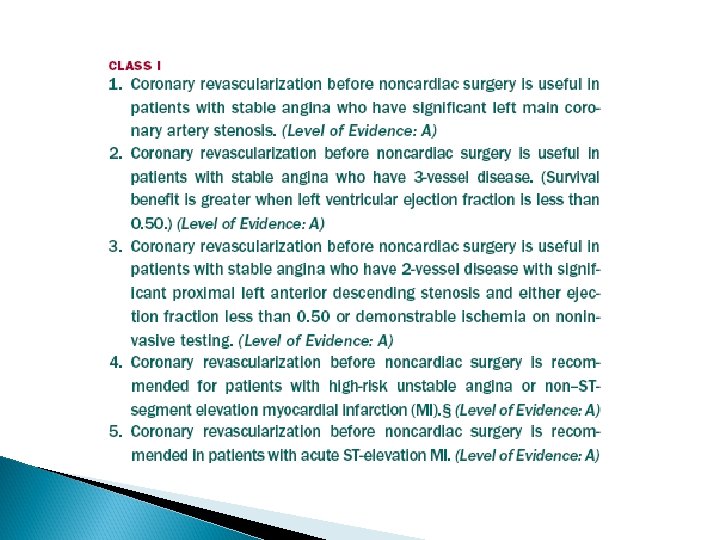
Coronary Artery Disease �Patients ◦ ◦ with known CAD What is the amount of myocardium in jeopardy? What is the ischemic threshold? What is the patient’s ventricular function? Is the patient on optimal medical regimen? �Limited value of coronary revascularization before noncardiac surgery ◦ Indication for preoperative testing is limited to patients in whom coronary revascularization may be beneficial independent of noncardiac surgery
Hypertension � SBP < 180 and DBP < 110 mm. Hg not an independent risk factor for CV complications 180 and DBP 110 mm. Hg consider risk/ benefit of delaying surgery � SBP ◦ One RCT: unable to demonstrate benefit of delaying surgery in patients without concomitant risk factors � If surgery is more urgent rapid-acting agents � Consider withholding ACEI, ARB on the morning of surgery restart only after the patient is euvolemic (renal dysfunction risk )
Valvular Heart Disease � Aortic stenosis ◦ Symptomatic AS delay elective noncardiac surgery (usually require AVR before elective surgery) ◦ Asymptomatic severe AS delay surgery if the valve has not been evaluated within the year ◦ Severe AS, who refuse or are not candidate for cardiac surgery noncardiac surgery can be performed with a mortality risk of ca. 10% �Percutaneous balloon aortic vavuloplasty as a bridge ◦ Presence of AS (severity not known) is associated with increased risk of MI (OR 1. 55) but not death
Valvular Heart Disease � Mitral stenosis ◦ Mild to moderate ensure control of heart rate ◦ Severe may benefit from balloon mitral valvuloplasty or open surgical repair before high risk surgery ◦ Significant MS increases the risk of heart failure however, preoperative MVR is not recommended, unless MVR is indicated unrelated to the noncardiac surgery
Valvular Heart Disease � Aortic, mitral regurgitation ◦ Provide appropriate medical therapy ◦ Volume control and afterload reduction ◦ Severe symptomatic MR or AR should be considered for further evaluation
Arrhythmias & Conduction Abnl � Careful evaluation for underlying cause: metabolic derangement, cardiopulmonary disease, drug toxicity, ongoing MI or infarction � Frequent PVCs and/or asymptomatic nonsustained V-tach are not associated with increased risk of nonfatal MI or cardiac death � High-grade conduction abnl increase operative risk, may necessitate pacing � Intraventricular conduction delays (+/- BBB) and no history of advanced heart block or symptoms rarely progress to complete heart block
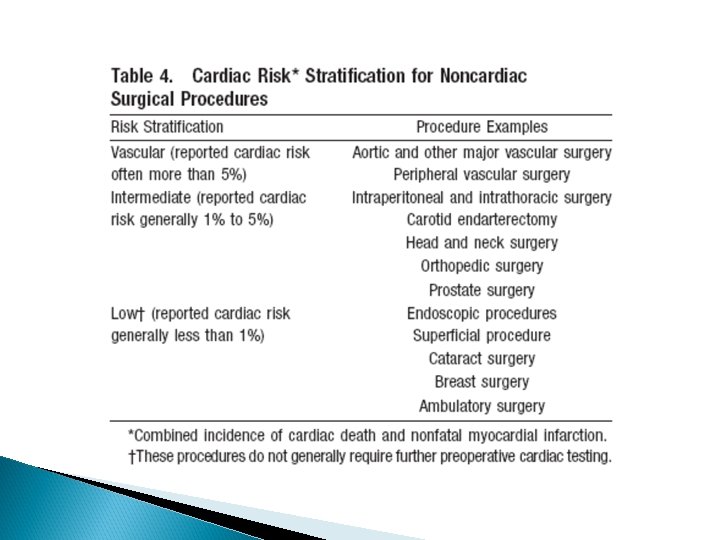
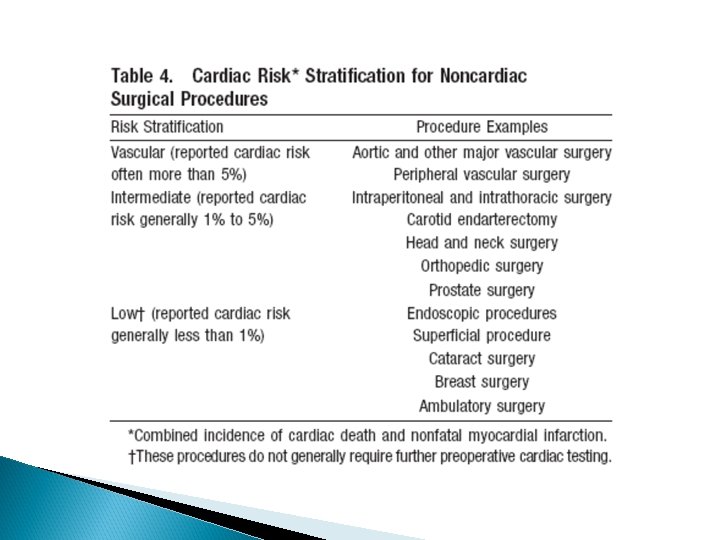
Surgery-Specific Issues �Major vascular procedures represent the highest-risk procedures ◦ Considered distinctly in the decision to perform further evaluation �Within the intermediate-risk category, morbidity and mortality vary depending on the surgical location and extent of the procedure
Perioperative Therapy � Preoperative coronary revascularization with CABG or PCI � Perioperative � Intraoperative medical therapy electromagnetic interference with implanted pacemakers and cardioverter defibrillators
Preoperative CABG � Several randomized trials assessing overall benefit of prophylactic CABG to lower operative risk ◦ CARP, DECREASE-II, DECREASE-V ◦ Lack of benefit of preoperative coronary revascularization in preventing death or MI � Should not be performed unless indicated unrelated to surgery
Preoperative PCI � Of no value in preventing perioperative cardiac events, except in those patients in whom PCI is independently indicated for an acute coronary syndrome
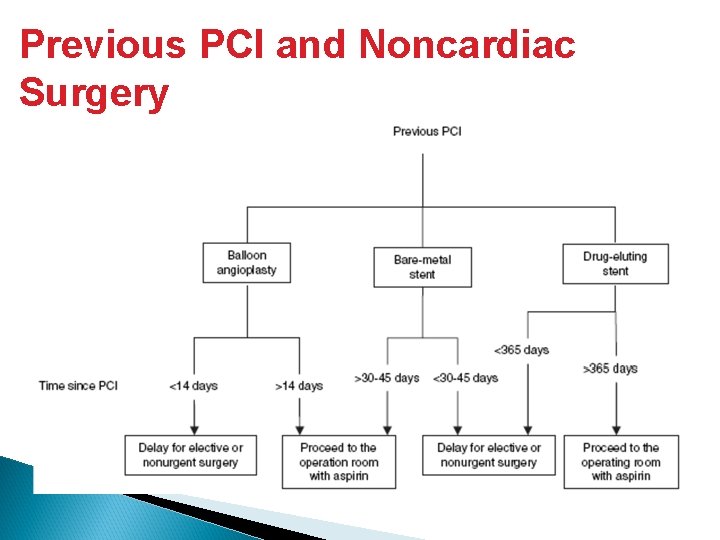
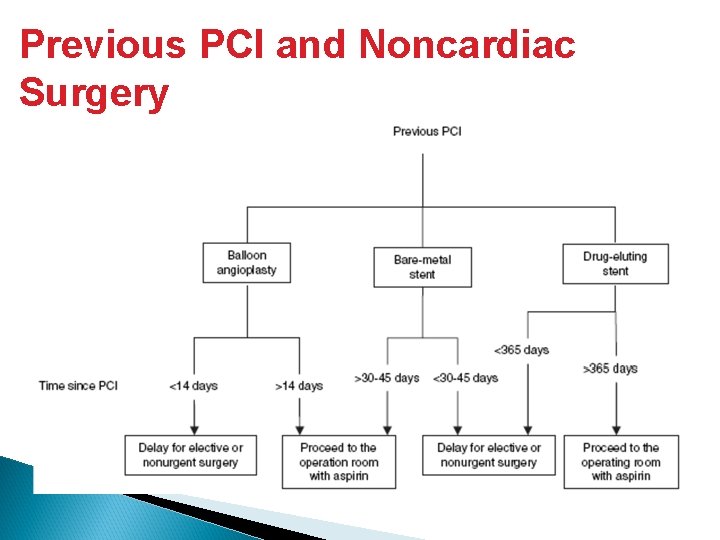
Previous PCI and Noncardiac Surgery
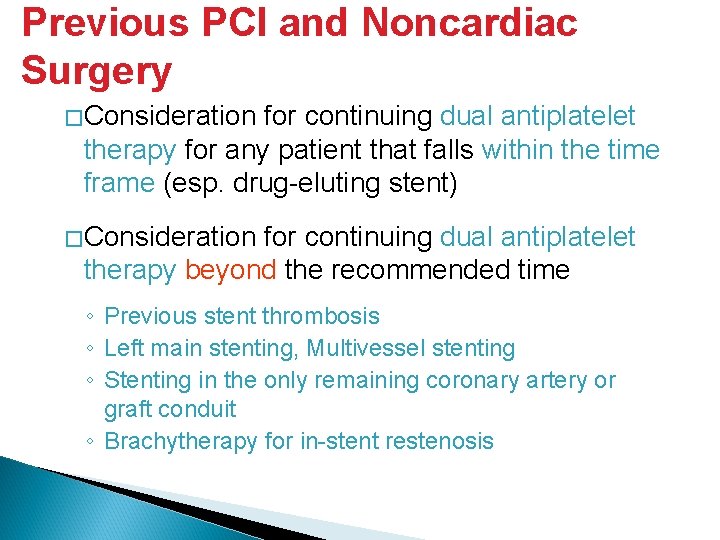
Previous PCI and Noncardiac Surgery �Consideration for continuing dual antiplatelet therapy for any patient that falls within the time frame (esp. drug-eluting stent) �Consideration for continuing dual antiplatelet therapy beyond the recommended time ◦ Previous stent thrombosis ◦ Left main stenting, Multivessel stenting ◦ Stenting in the only remaining coronary artery or graft conduit ◦ Brachytherapy for in-stent restenosis
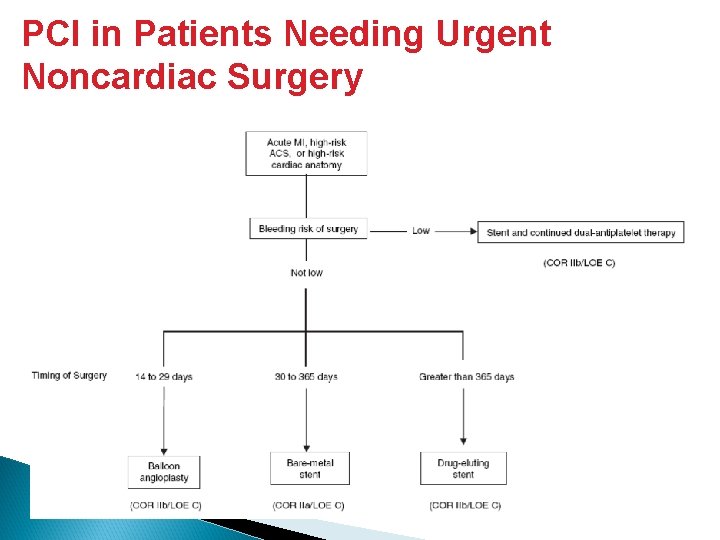
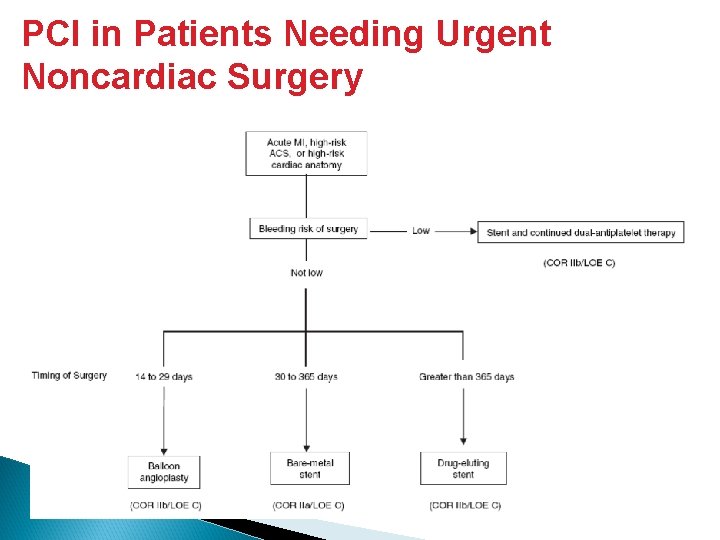
PCI in Patients Needing Urgent Noncardiac Surgery
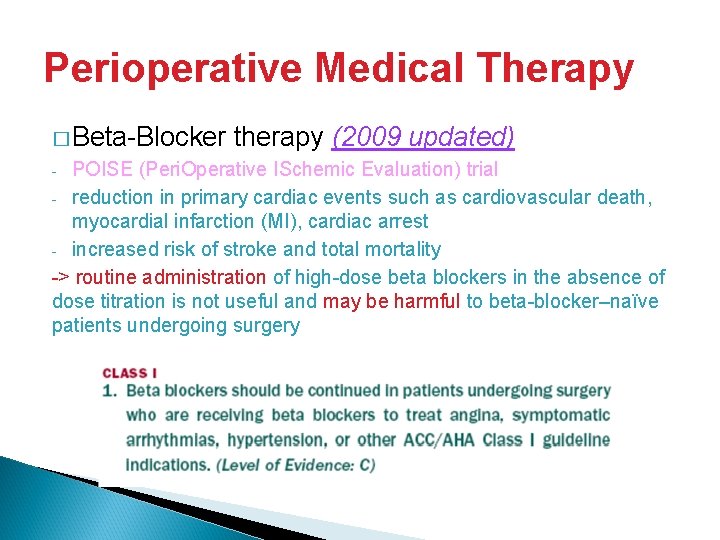
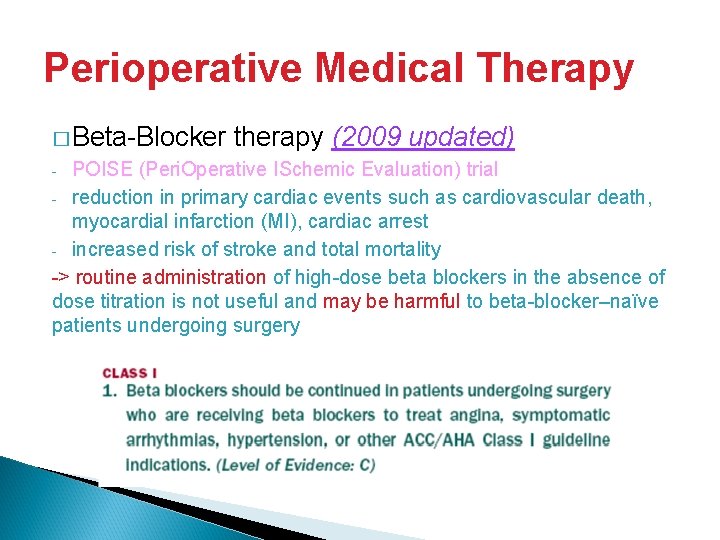
Perioperative Medical Therapy � Beta-Blocker therapy (2009 updated) POISE (Peri. Operative ISchemic Evaluation) trial - reduction in primary cardiac events such as cardiovascular death, myocardial infarction (MI), cardiac arrest - increased risk of stroke and total mortality -> routine administration of high-dose beta blockers in the absence of dose titration is not useful and may be harmful to beta-blocker–naïve patients undergoing surgery -
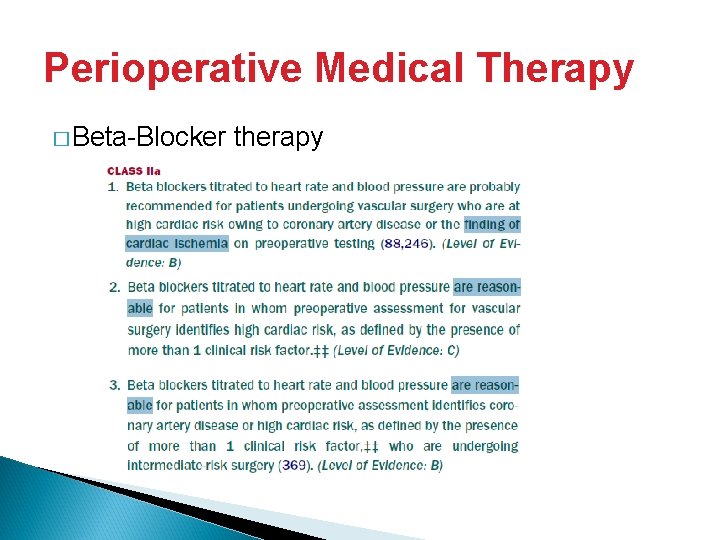
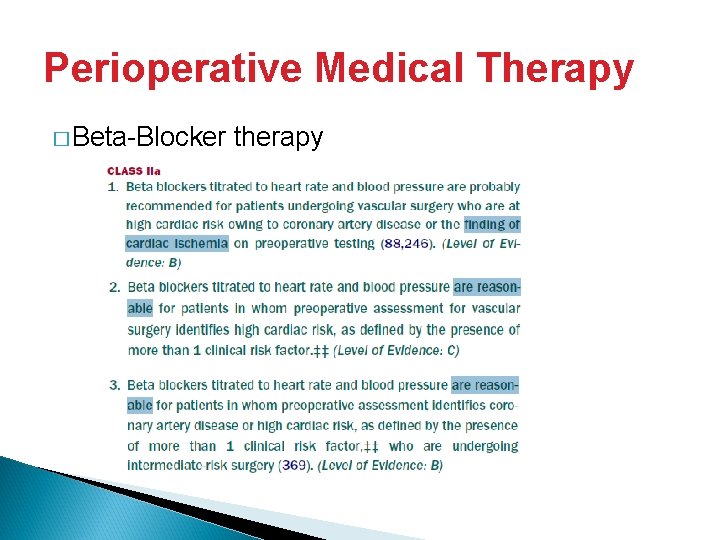
Perioperative Medical Therapy � Beta-Blocker therapy
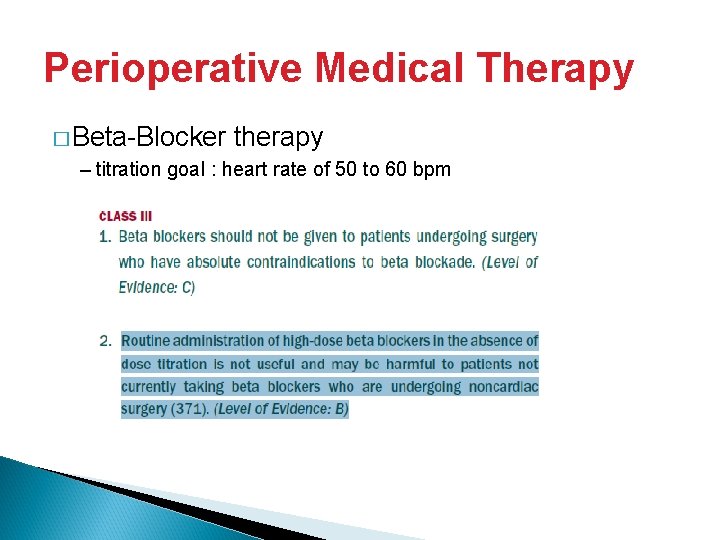
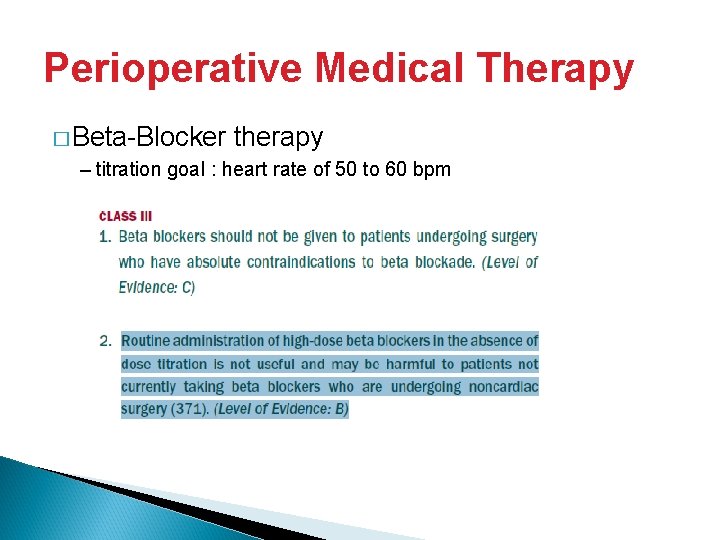
Perioperative Medical Therapy � Beta-Blocker therapy – titration goal : heart rate of 50 to 60 bpm
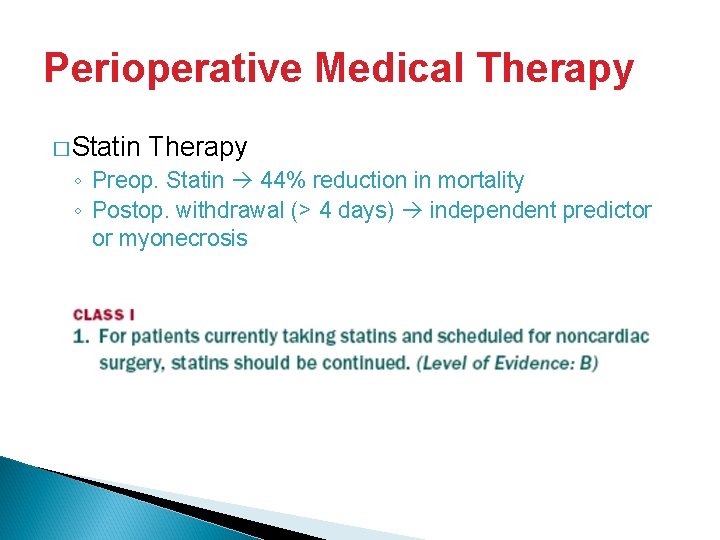
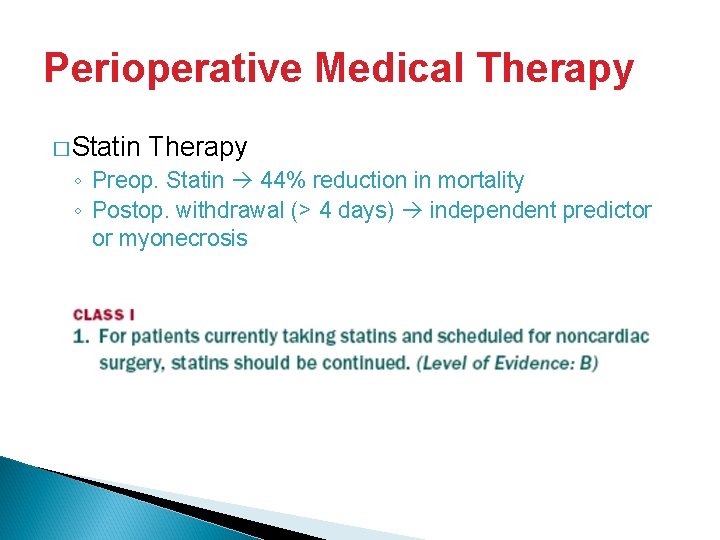
Perioperative Medical Therapy � Statin Therapy ◦ Preop. Statin 44% reduction in mortality ◦ Postop. withdrawal (> 4 days) independent predictor or myonecrosis
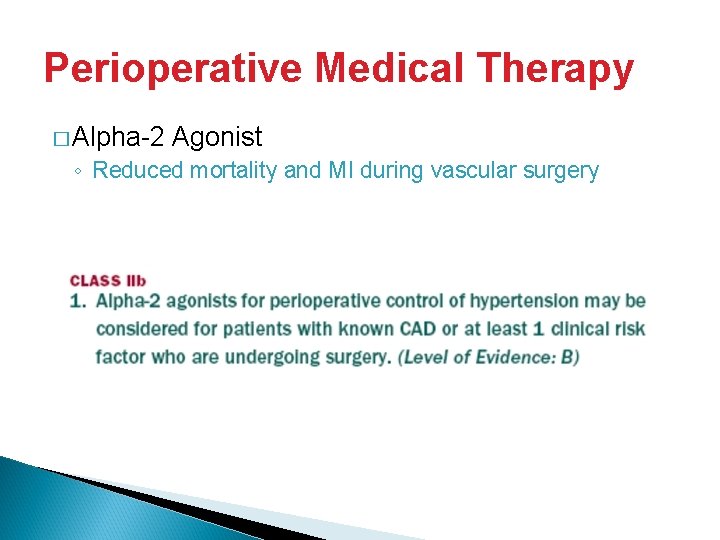
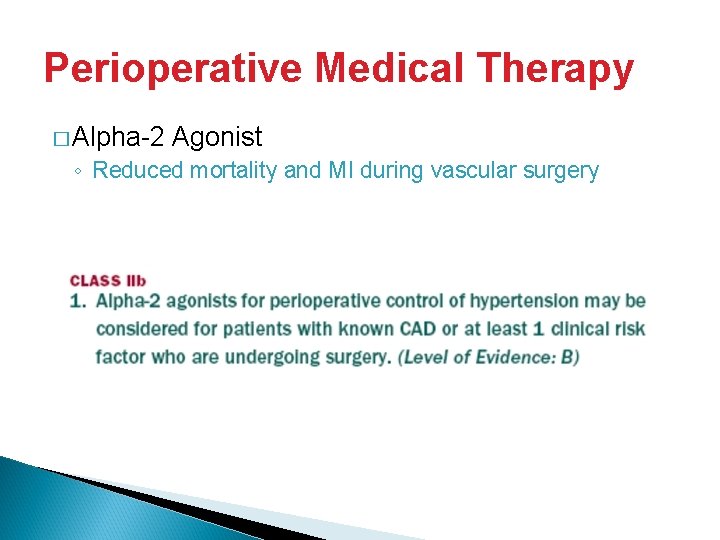
Perioperative Medical Therapy � Alpha-2 Agonist ◦ Reduced mortality and MI during vascular surgery
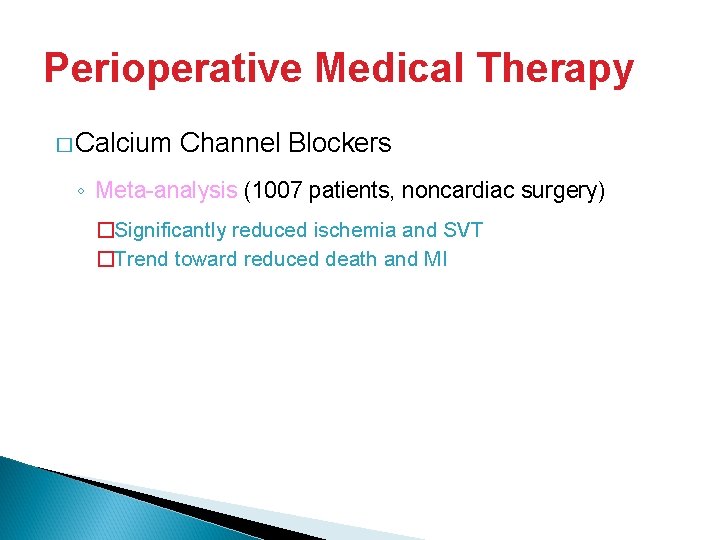
Perioperative Medical Therapy � Calcium Channel Blockers ◦ Meta-analysis (1007 patients, noncardiac surgery) �Significantly reduced ischemia and SVT �Trend toward reduced death and MI
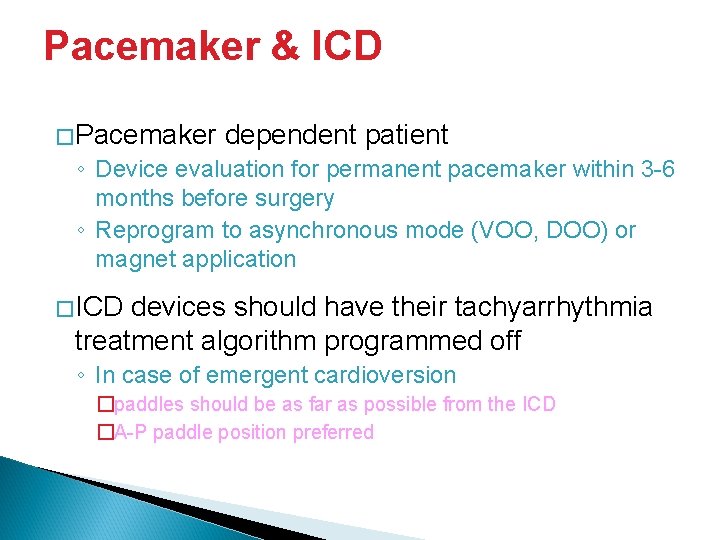
Pacemaker & ICD �Pacemaker dependent patient ◦ Device evaluation for permanent pacemaker within 3 -6 months before surgery ◦ Reprogram to asynchronous mode (VOO, DOO) or magnet application �ICD devices should have their tachyarrhythmia treatment algorithm programmed off ◦ In case of emergent cardioversion �paddles should be as far as possible from the ICD �A-P paddle position preferred
Anesthetic Consideration � Intraoperative � Perioperative management pain management
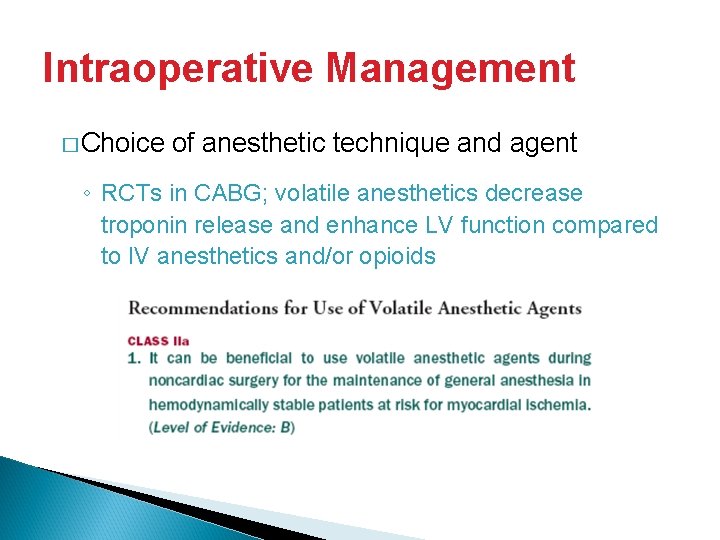
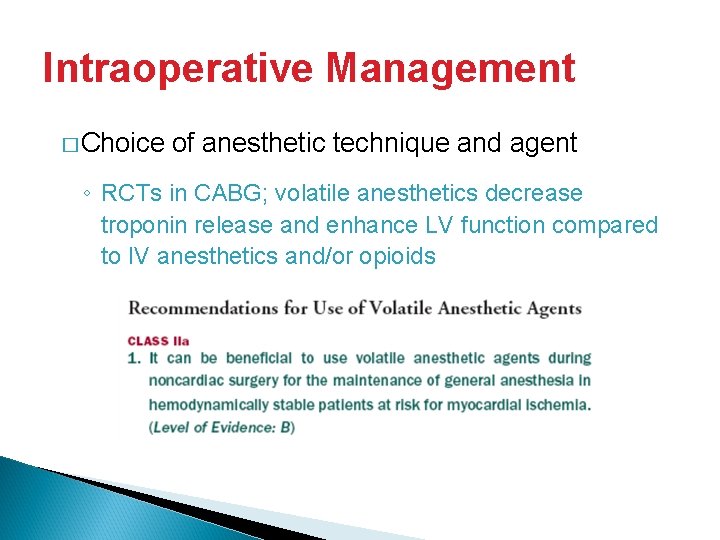
Intraoperative Management � Choice of anesthetic technique and agent ◦ RCTs in CABG; volatile anesthetics decrease troponin release and enhance LV function compared to IV anesthetics and/or opioids
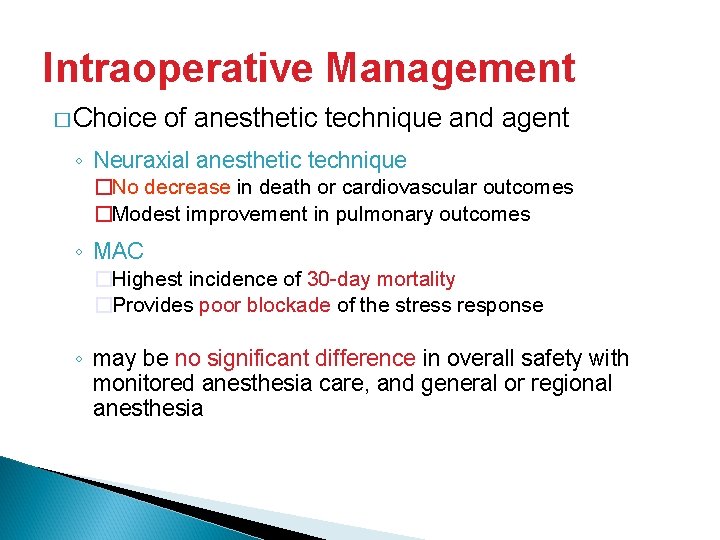
Intraoperative Management � Choice of anesthetic technique and agent ◦ Neuraxial anesthetic technique �No decrease in death or cardiovascular outcomes �Modest improvement in pulmonary outcomes ◦ MAC �Highest incidence of 30 -day mortality �Provides poor blockade of the stress response ◦ may be no significant difference in overall safety with monitored anesthesia care, and general or regional anesthesia
Intraoperative Management � Choice of anesthetic technique and agent ◦ no study demonstrated a change in outcome from routine use �PAC, ST-segment monitor, transesophageal echocardiography (TEE), intravenous nitroglycerin ◦ Best left to the discretion of the anesthesia care team
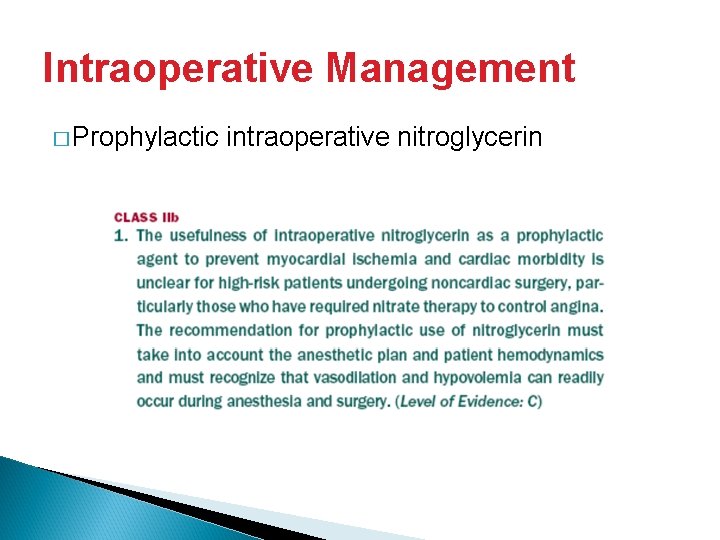
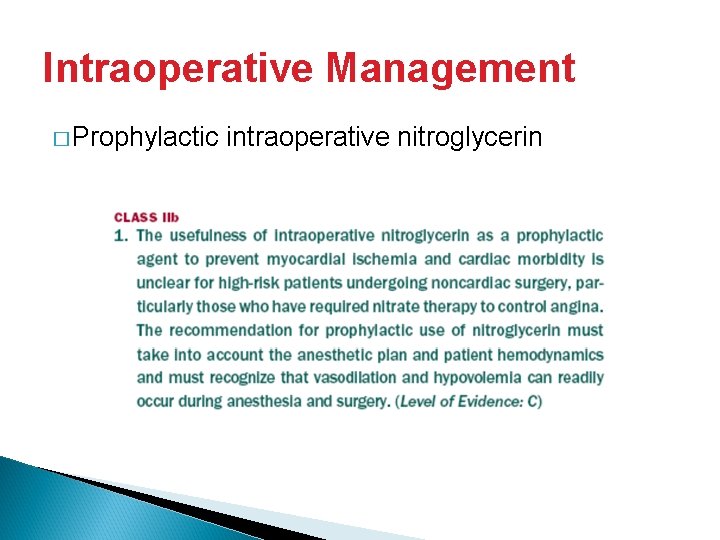
Intraoperative Management � Prophylactic intraoperative nitroglycerin
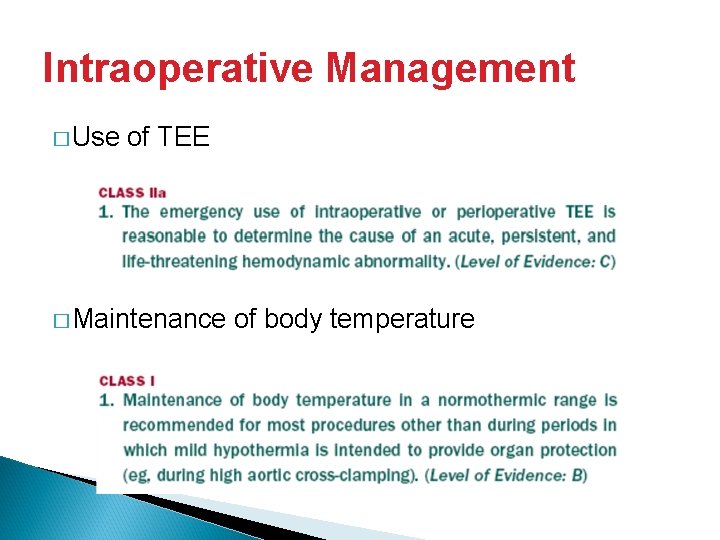
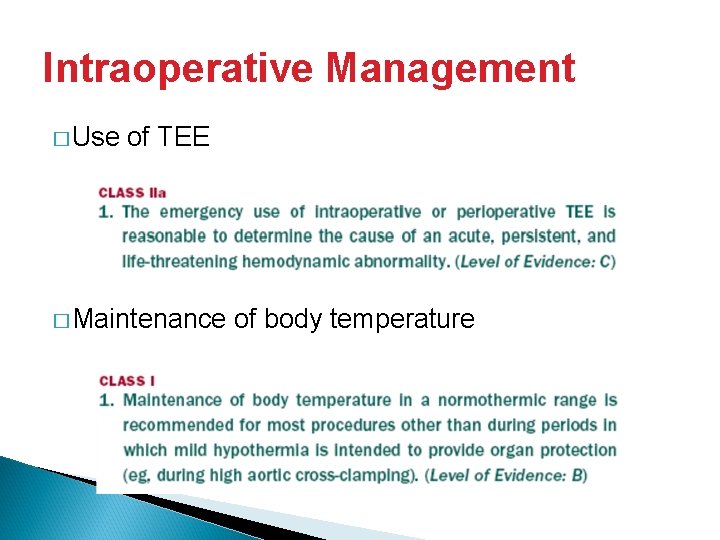
Intraoperative Management � Use of TEE � Maintenance of body temperature
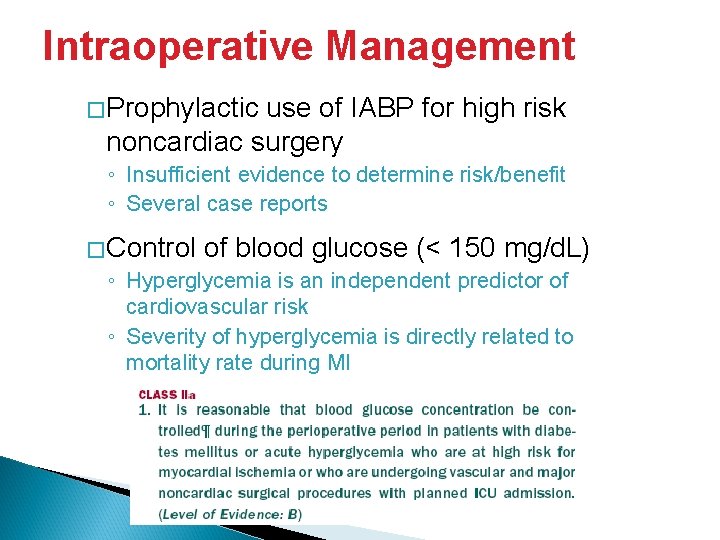
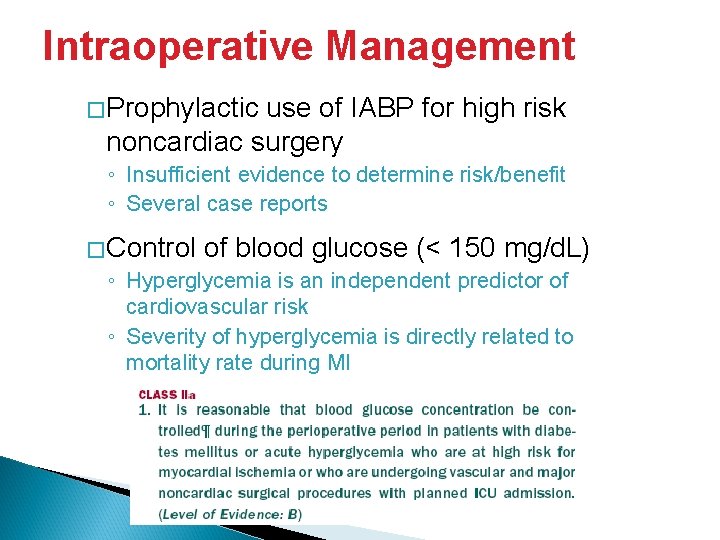
Intraoperative Management �Prophylactic use of IABP for high risk noncardiac surgery ◦ Insufficient evidence to determine risk/benefit ◦ Several case reports �Control of blood glucose (< 150 mg/d. L) ◦ Hyperglycemia is an independent predictor of cardiovascular risk ◦ Severity of hyperglycemia is directly related to mortality rate during MI
Perioperative pain management � Postoperative period ◦ Stress, adverse hemodynamics, hypercoagulable status ◦ majority of cardiac events occur � Effective analgesic regimen must be included in the perioperative plan
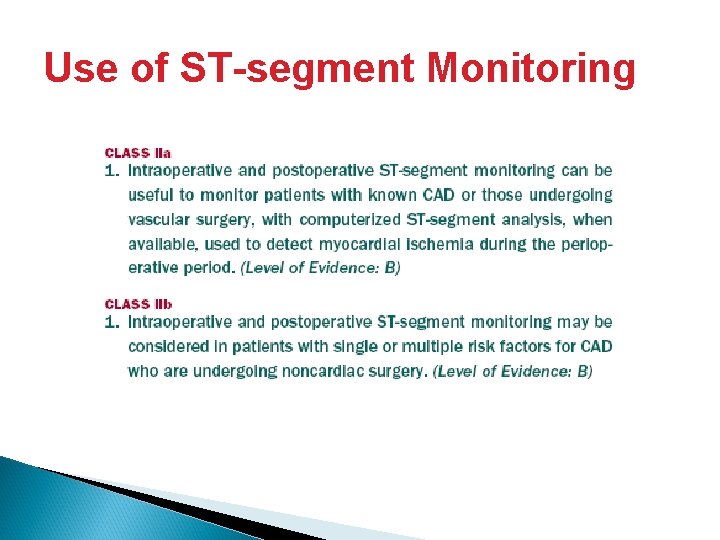
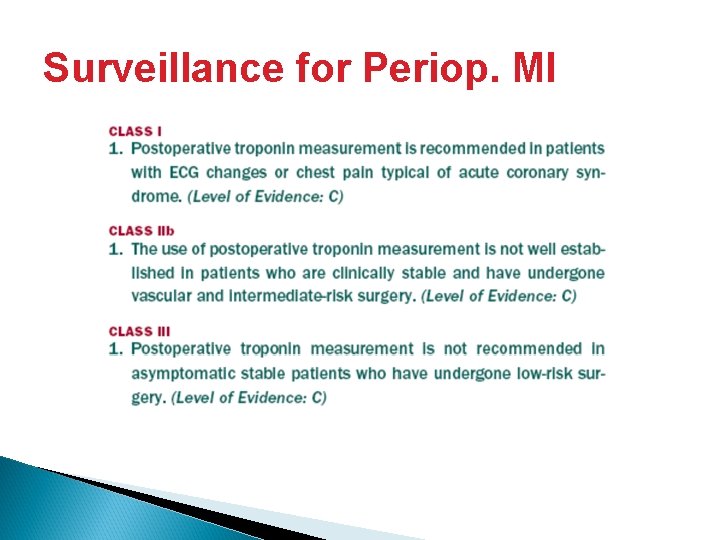
Perioperative Surveillance � Use of PACs � Use of ST-segment monitoring � Surveillance for periop. MI
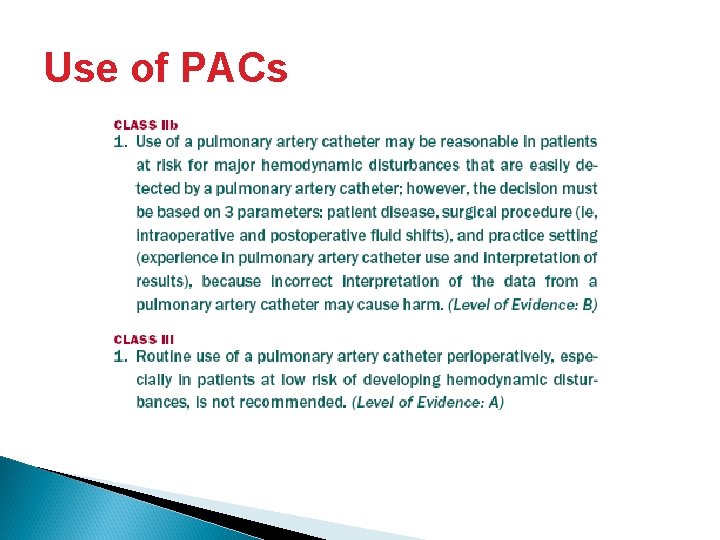
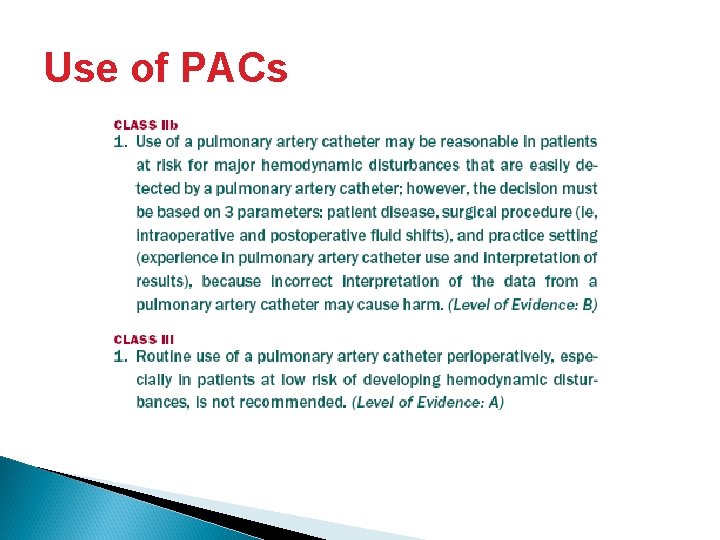
Use of PACs
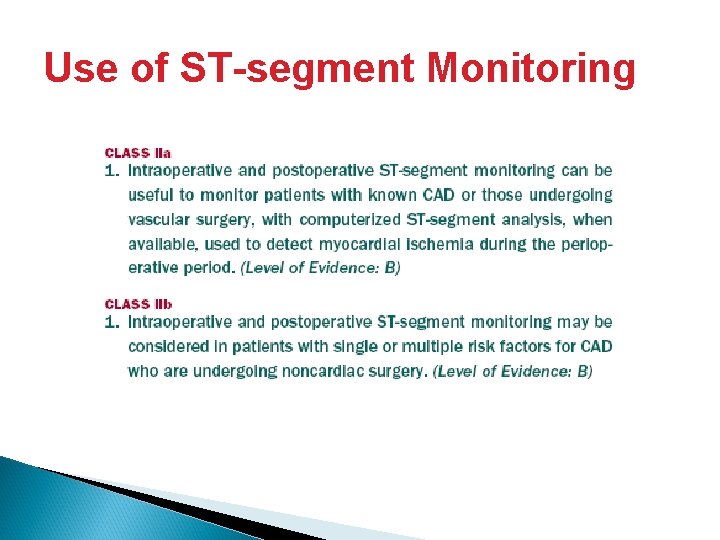
Use of ST-segment Monitoring
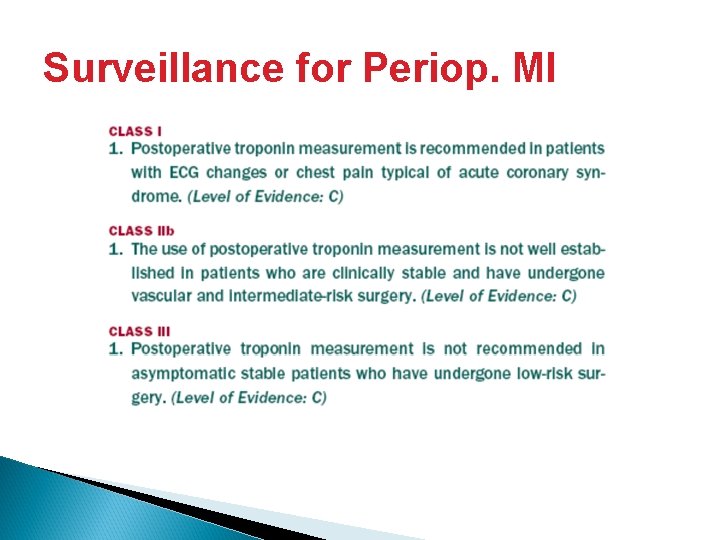
Surveillance for Periop. MI

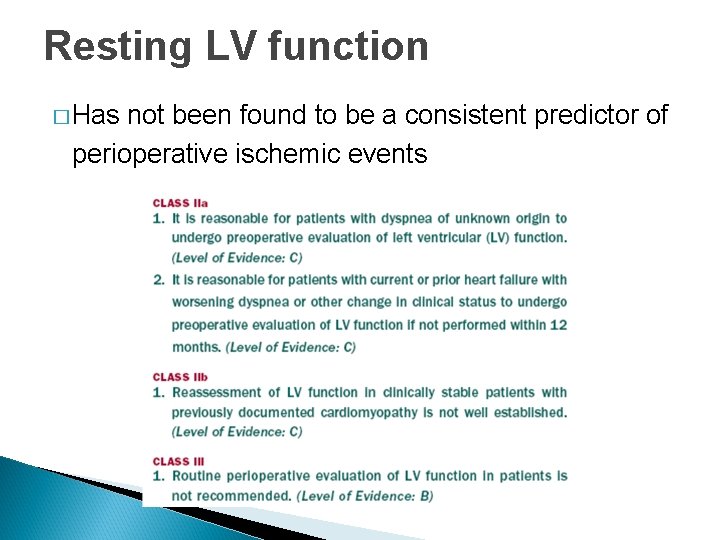
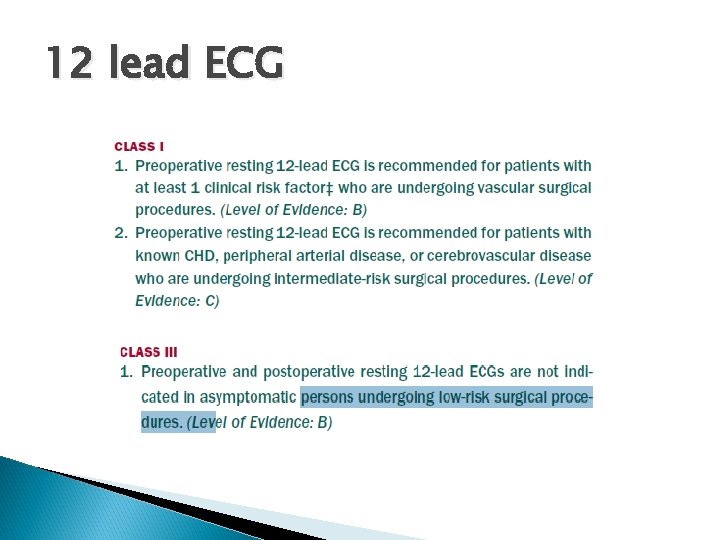
Supplemental Preoperative Evaluation
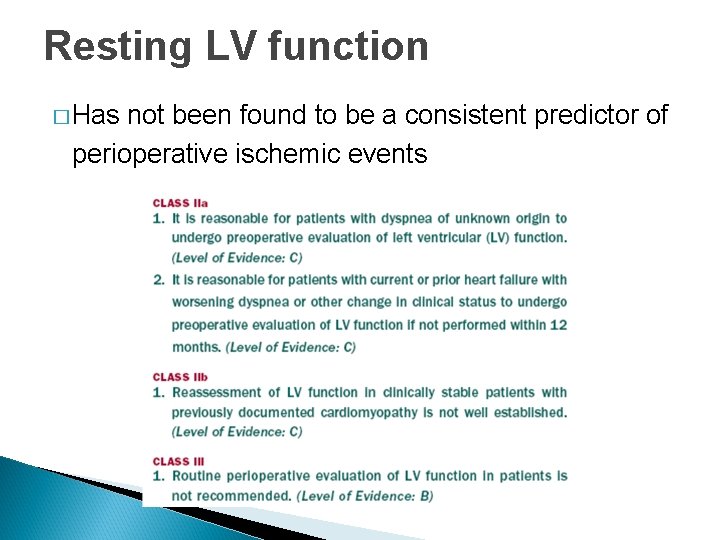
Resting LV function � Has not been found to be a consistent predictor of perioperative ischemic events
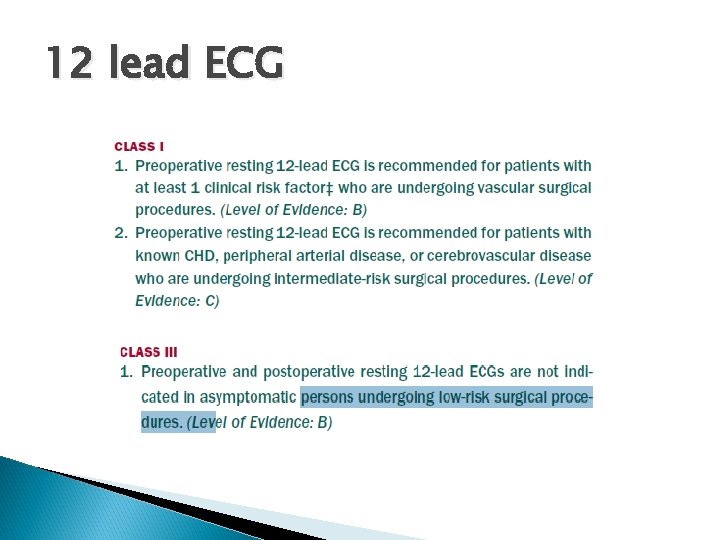
12 lead ECG
Exercise Stress Testing � Test of choice in most ambulatory patients � Provide � Detect an estimate of functional capacity myocardial ischemia
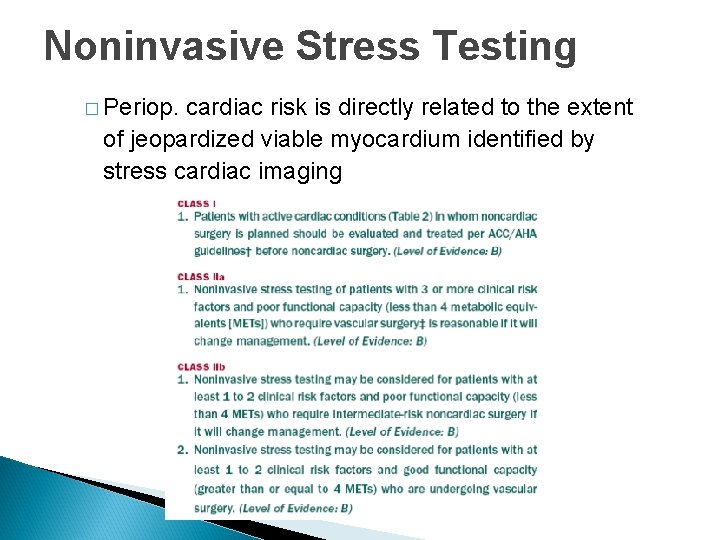
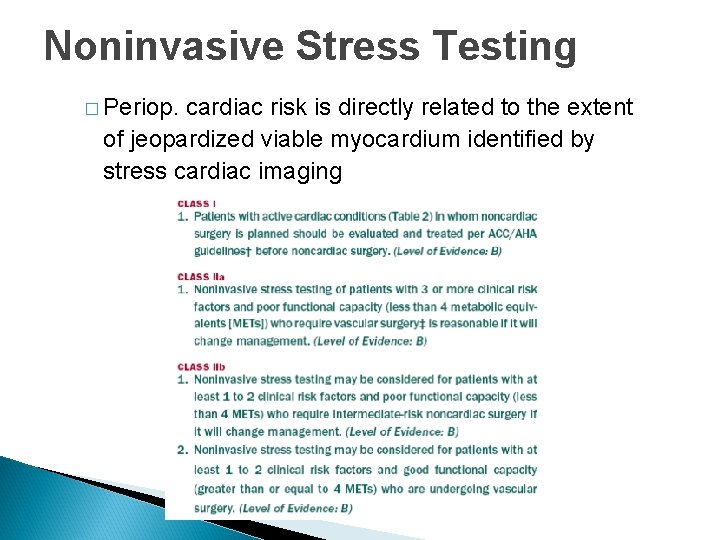
Noninvasive Stress Testing � Periop. cardiac risk is directly related to the extent of jeopardized viable myocardium identified by stress cardiac imaging