A costeffectiveness study of enteral immune modulating nutrition



- Slides: 43
A cost-effectiveness study of enteral immune modulating nutrition in intensive care patients Elizabeth Coates Clare Hibbert Medical Economics and Research Centre, Sheffield (MERCS) CIMC 2001
What is immunonutrition? The term given to describe special enteral feeds containing: – Arginine – Omega-3 fatty acids – Nucleotides – (and sometimes, glutamine) Ref: Barbul A. Immunonutrition comes of age. Crit Care Med 2000; 28: 3: 884 -885 (editorial).
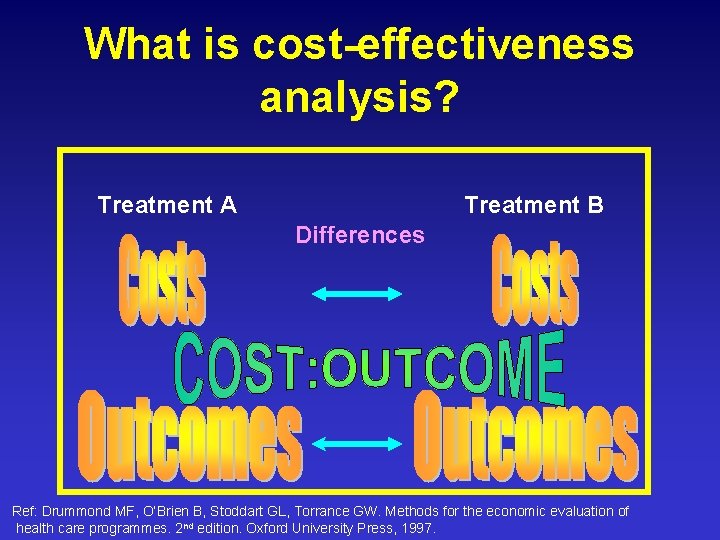
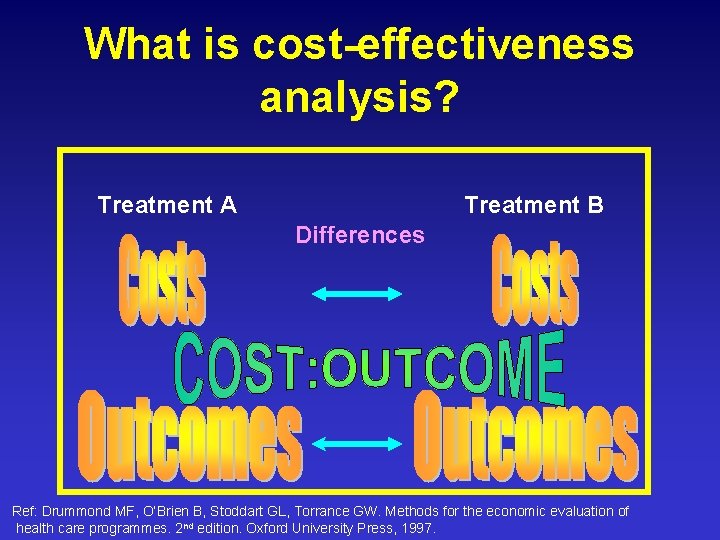
What is cost-effectiveness analysis? Treatment A Treatment B Differences Ref: Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 2 nd edition. Oxford University Press, 1997.
Rationale
1. The nature of critically ill patients’ conditions –Malnutrition –Compromise of immune system –Infection
All these increase: • Length of ICU and hospital stay • Morbidity • Mortality • Resource consumption • Costs of care

2. Growing evidence on the benefits of immunonutrition…
3. Despite these findings, and the increasing pressure to curtail expenditure The cost-effectiveness issue has rarely been explored…
Aim of the study To estimate the cost-effectiveness of immunonutrition (IMN) in reducing infection rates in critically ill adult patients when compared with standard enteral nutrition.
Outcome measure A reduction in the duration of days of infection in ICU patients with sepsis (from NHS perspective)
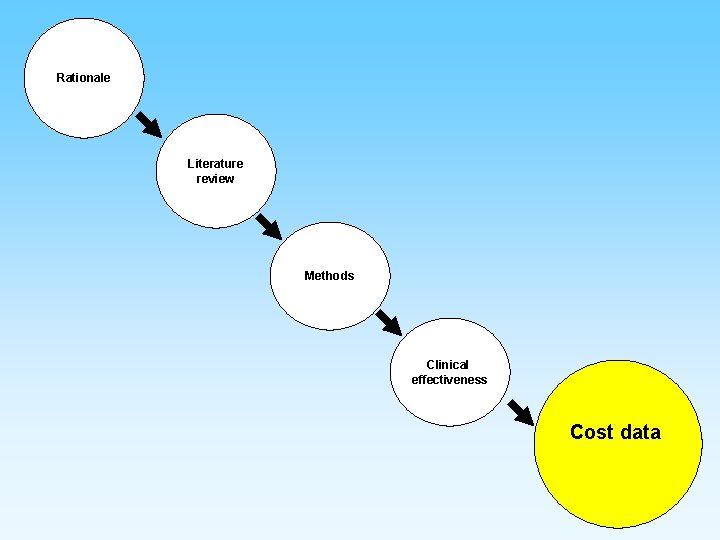
Rationale Literature review
Literature search Databases • • • Med. Line Embase CINAHL Search terms • • Review of the literature… Immunonutriton Nutrition Enteral feed Intensive care Critical care Costs Cost-effectiveness (analysis)
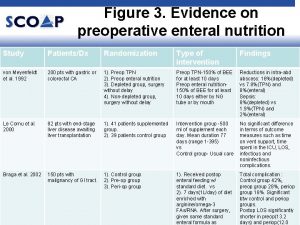
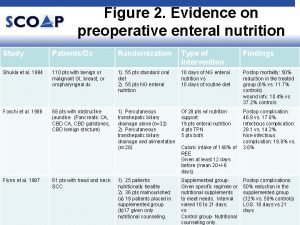
Studies of IMN • Atkinson (1998) reduced ICU & hospital LOS and duration of ventilation • Bower (1995) reduction in acquired infections and hospital LOS • Galban (2000) reduction in infection rate and lower mortality rate
Key paper Beale et al. Immunonutrition in the critically ill: A systematic review of clinical outcome. Critical Care Medicine 1999; 27: 12: 2799 -2805.
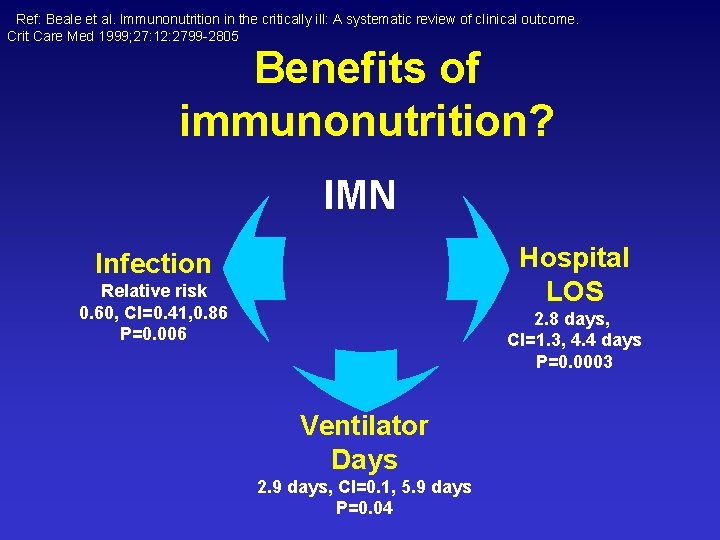
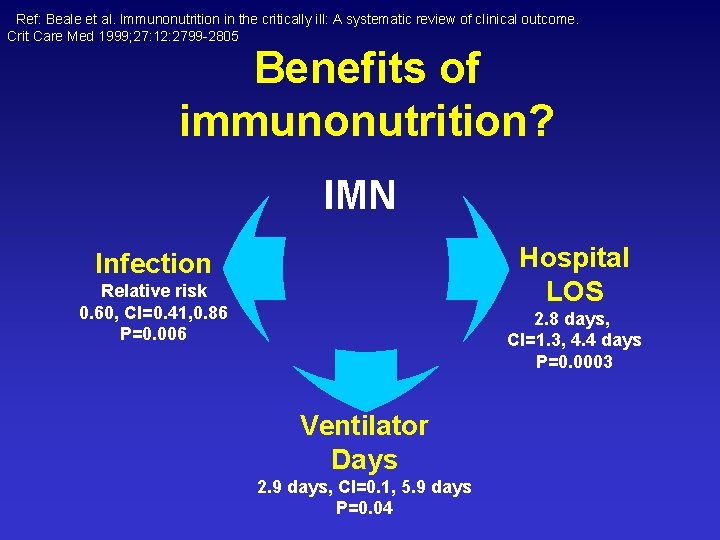
Ref: Beale et al. Immunonutrition in the critically ill: A systematic review of clinical outcome. Crit Care Med 1999; 27: 12: 2799 -2805 Benefits of immunonutrition? IMN Hospital LOS Infection Relative risk 0. 60, CI=0. 41, 0. 86 P=0. 006 2. 8 days, CI=1. 3, 4. 4 days P=0. 0003 Ventilator Days 2. 9 days, CI=0. 1, 5. 9 days P=0. 04
Rationale Literature review Methods
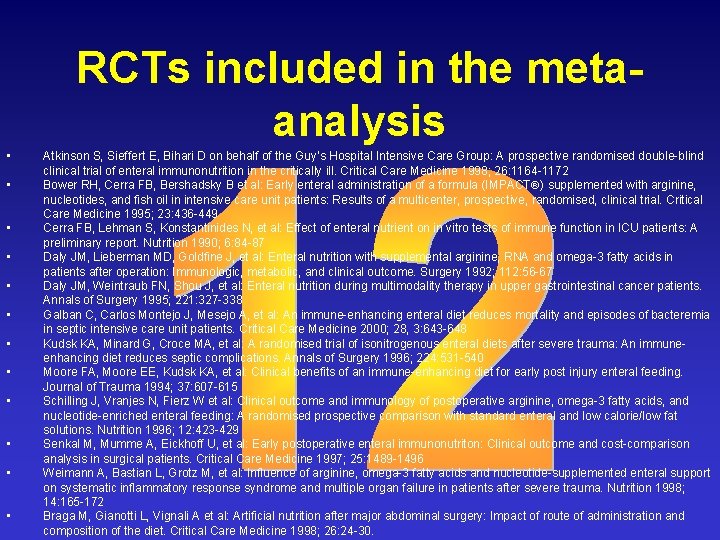
Methodology The evaluation of cost-effectiveness was based on two factors: 1. Evidence of effectiveness of IMN from the 12 RCTs included in the metaanalysis (1482 patients) 2. Retrospective cost data on individual ICU patients at the Royal Hallamshire Hospital
Rationale Literature review Methods Clinical effectiveness
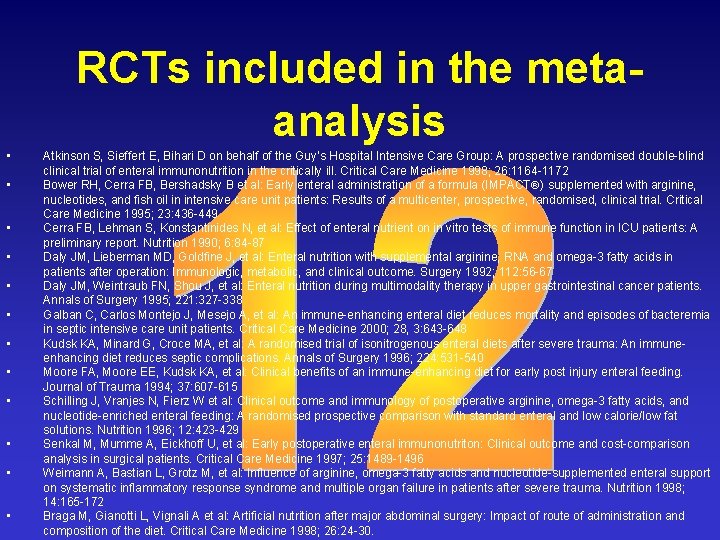
RCTs included in the metaanalysis • • • Atkinson S, Sieffert E, Bihari D on behalf of the Guy’s Hospital Intensive Care Group: A prospective randomised double-blind clinical trial of enteral immunonutrition in the critically ill. Critical Care Medicine 1998; 26: 1164 -1172 Bower RH, Cerra FB, Bershadsky B et al: Early enteral administration of a formula (IMPACT ) supplemented with arginine, nucleotides, and fish oil in intensive care unit patients: Results of a multicenter, prospective, randomised, clinical trial. Critical Care Medicine 1995; 23: 436 -449 Cerra FB, Lehman S, Konstantinides N, et al: Effect of enteral nutrient on in vitro tests of immune function in ICU patients: A preliminary report. Nutrition 1990; 6: 84 -87 Daly JM, Lieberman MD, Goldfine J, et al: Enteral nutrition with supplemental arginine, RNA and omega-3 fatty acids in patients after operation: Immunologic, metabolic, and clinical outcome. Surgery 1992; 112: 56 -67 Daly JM, Weintraub FN, Shou J, et al: Enteral nutrition during multimodality therapy in upper gastrointestinal cancer patients. Annals of Surgery 1995; 221: 327 -338 Galban C, Carlos Montejo J, Mesejo A, et al: An immune-enhancing enteral diet reduces mortality and episodes of bacteremia in septic intensive care unit patients. Critical Care Medicine 2000; 28, 3: 643 -648 Kudsk KA, Minard G, Croce MA, et al: A randomised trial of isonitrogenous enteral diets after severe trauma: An immuneenhancing diet reduces septic complications. Annals of Surgery 1996; 224: 531 -540 Moore FA, Moore EE, Kudsk KA, et al: Clinical benefits of an immune-enhancing diet for early post injury enteral feeding. Journal of Trauma 1994; 37: 607 -615 Schilling J, Vranjes N, Fierz W et al: Clinical outcome and immunology of postoperative arginine, omega-3 fatty acids, and nucleotide-enriched enteral feeding: A randomised prospective comparison with standard enteral and low calorie/low fat solutions. Nutrition 1996; 12: 423 -429 Senkal M, Mumme A, Eickhoff U, et al: Early postoperative enteral immunonutriton: Clinical outcome and cost-comparison analysis in surgical patients. Critical Care Medicine 1997; 25: 1489 -1496 Weimann A, Bastian L, Grotz M, et al: Influence of arginine, omega-3 fatty acids and nucleotide-supplemented enteral support on systematic inflammatory response syndrome and multiple organ failure in patients after severe trauma. Nutrition 1998; 14: 165 -172 Braga M, Gianotti L, Vignali A et al: Artificial nutrition after major abdominal surgery: Impact of route of administration and composition of the diet. Critical Care Medicine 1998; 26: 24 -30.
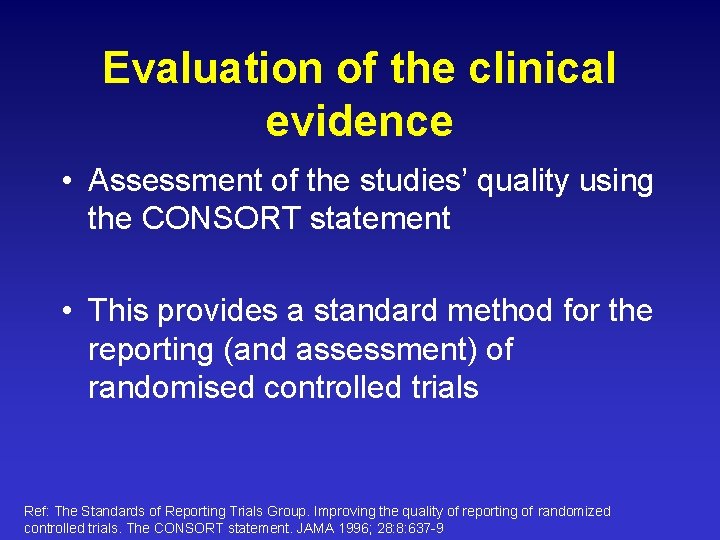
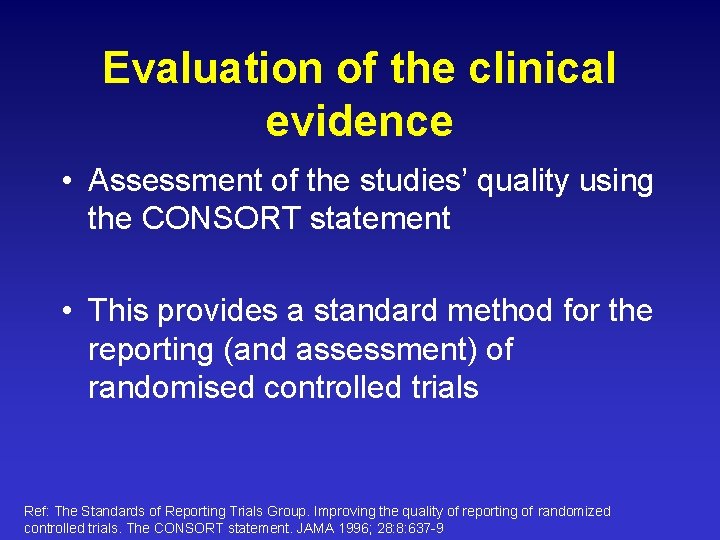
Evaluation of the clinical evidence • Assessment of the studies’ quality using the CONSORT statement • This provides a standard method for the reporting (and assessment) of randomised controlled trials Ref: The Standards of Reporting Trials Group. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 1996; 28: 8: 637 -9
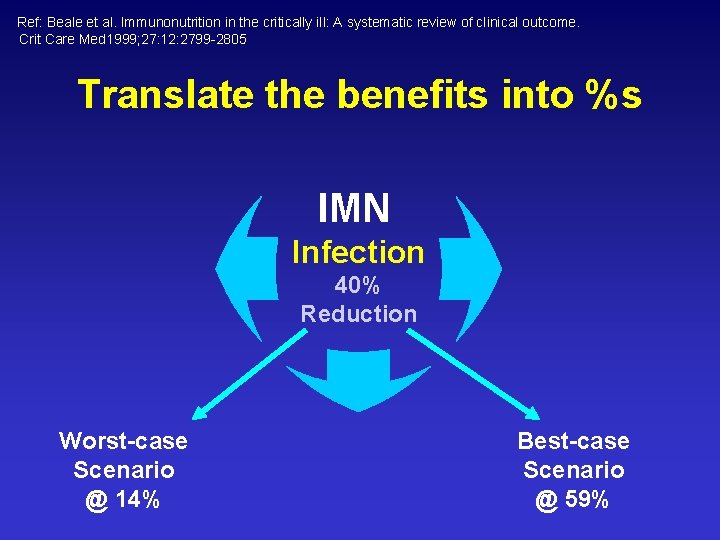
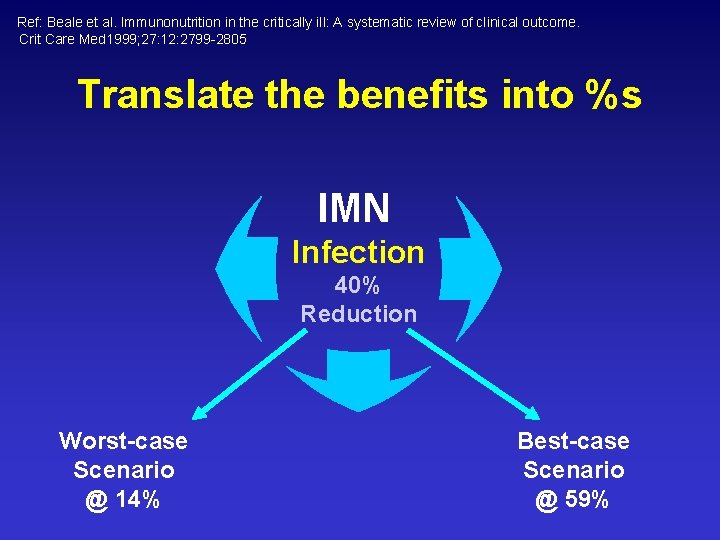
Ref: Beale et al. Immunonutrition in the critically ill: A systematic review of clinical outcome. Crit Care Med 1999; 27: 12: 2799 -2805 Translate the benefits into %s IMN Infection 40% Reduction Worst-case Scenario @ 14% Best-case Scenario @ 59%
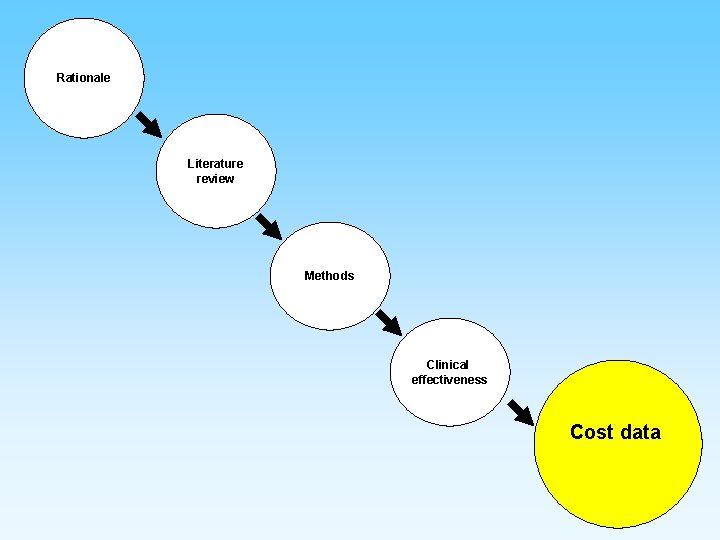
Rationale Literature review Methods Clinical effectiveness Cost data
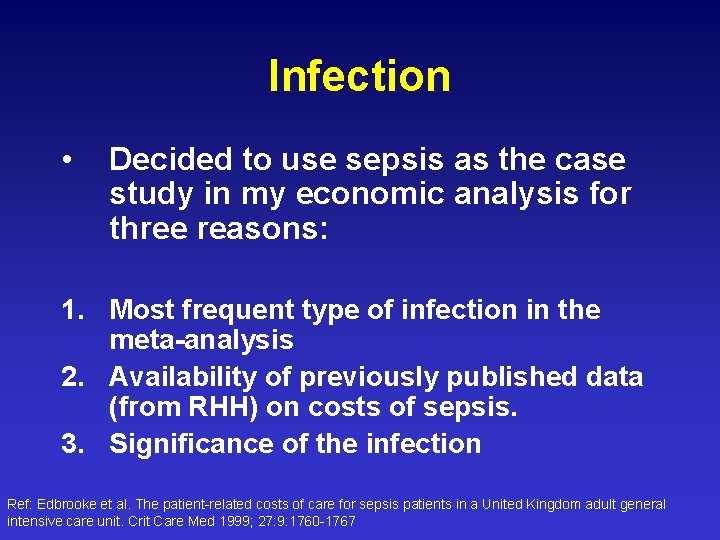
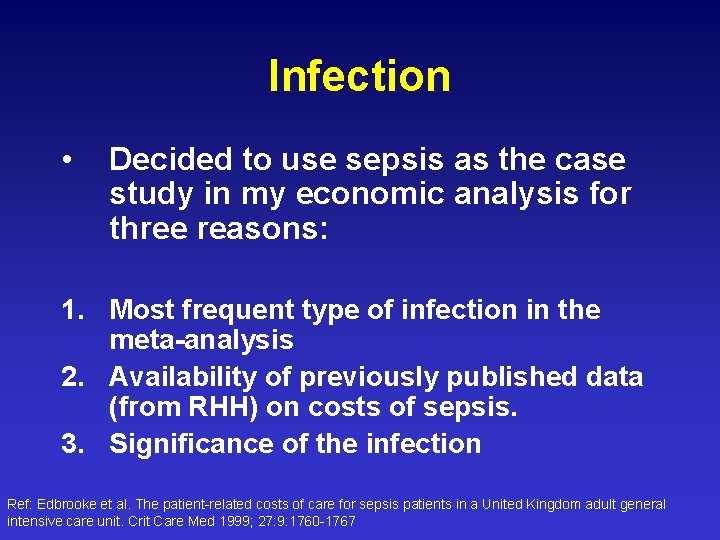
Infection • Decided to use sepsis as the case study in my economic analysis for three reasons: 1. Most frequent type of infection in the meta-analysis 2. Availability of previously published data (from RHH) on costs of sepsis. 3. Significance of the infection Ref: Edbrooke et al. The patient-related costs of care for sepsis patients in a United Kingdom adult general intensive care unit. Crit Care Med 1999; 27: 9: 1760 -1767
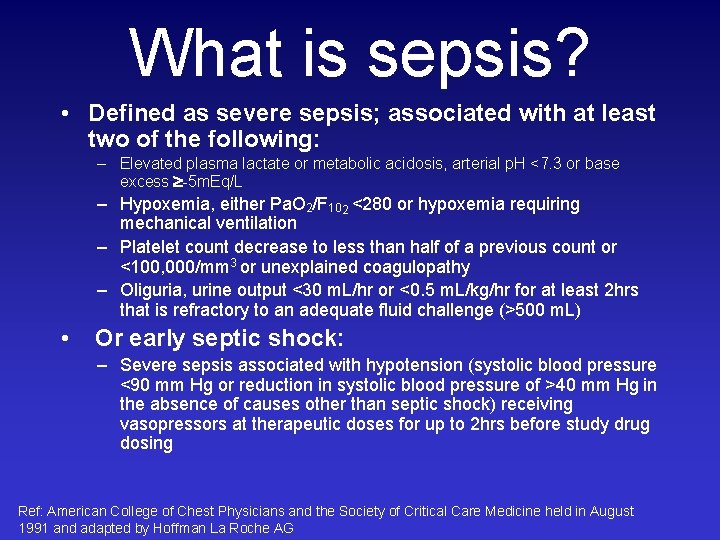
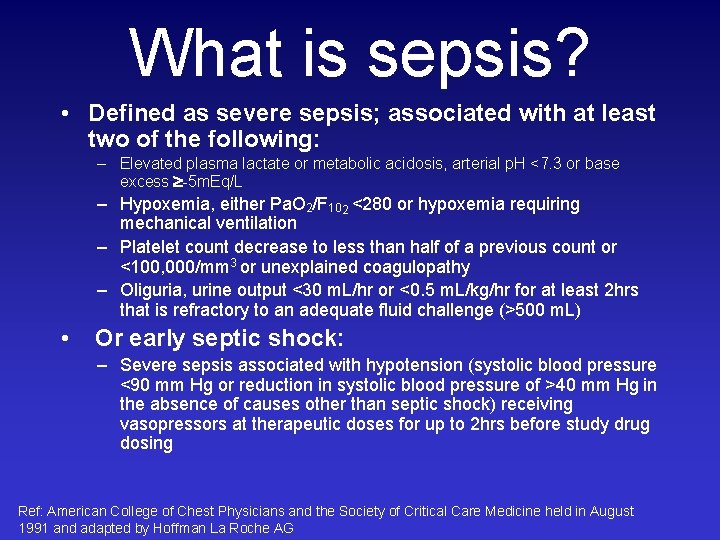
What is sepsis? • Defined as severe sepsis; associated with at least two of the following: – Elevated plasma lactate or metabolic acidosis, arterial p. H <7. 3 or base excess -5 m. Eq/L – Hypoxemia, either Pa. O 2/F 102 <280 or hypoxemia requiring mechanical ventilation – Platelet count decrease to less than half of a previous count or <100, 000/mm 3 or unexplained coagulopathy – Oliguria, urine output <30 m. L/hr or <0. 5 m. L/kg/hr for at least 2 hrs that is refractory to an adequate fluid challenge (>500 m. L) • Or early septic shock: – Severe sepsis associated with hypotension (systolic blood pressure <90 mm Hg or reduction in systolic blood pressure of >40 mm Hg in the absence of causes other than septic shock) receiving vasopressors at therapeutic doses for up to 2 hrs before study drug dosing Ref: American College of Chest Physicians and the Society of Critical Care Medicine held in August 1991 and adapted by Hoffman La Roche AG
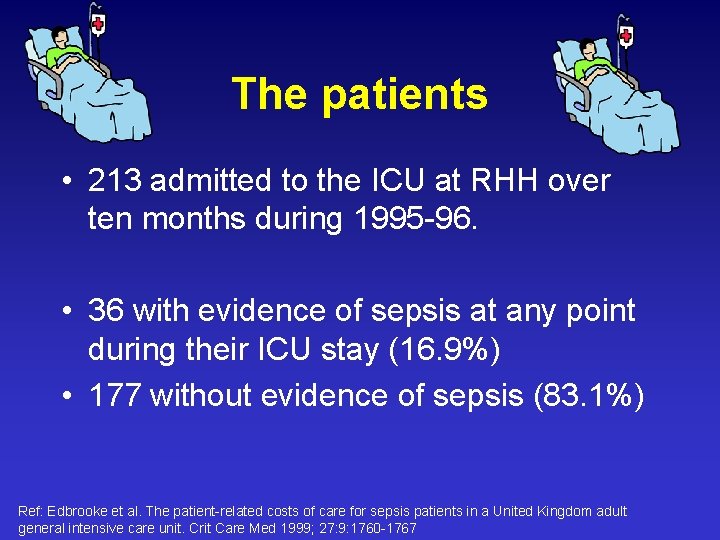
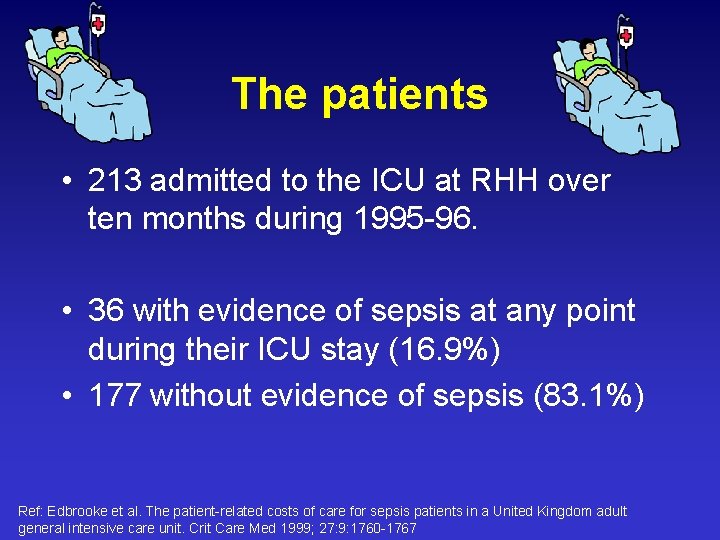
The patients • 213 admitted to the ICU at RHH over ten months during 1995 -96. • 36 with evidence of sepsis at any point during their ICU stay (16. 9%) • 177 without evidence of sepsis (83. 1%) Ref: Edbrooke et al. The patient-related costs of care for sepsis patients in a United Kingdom adult general intensive care unit. Crit Care Med 1999; 27: 9: 1760 -1767
Cost analysis Calculated total costs for each cost component: • Drugs • Fluids • Consumables • Medical Imaging
Cost analysis Calculated total costs for each cost component: • Nurses • Doctors • Other staff (technical and admin)
Rationale Literature review Results Methods Clinical effectiveness Cost data
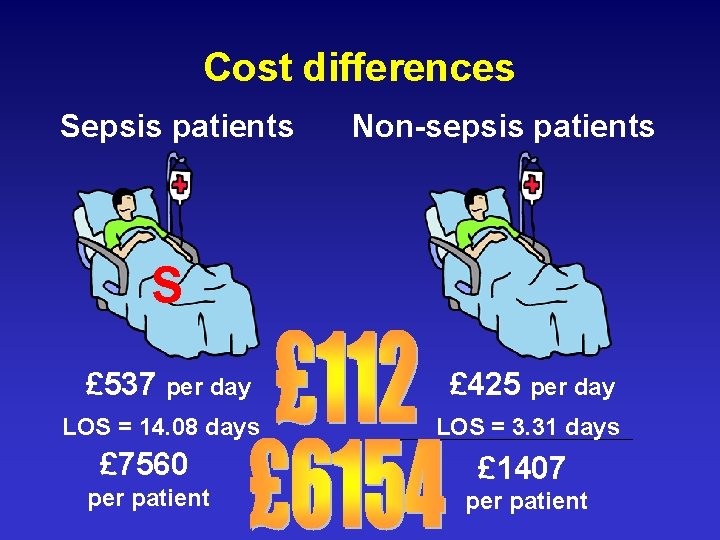
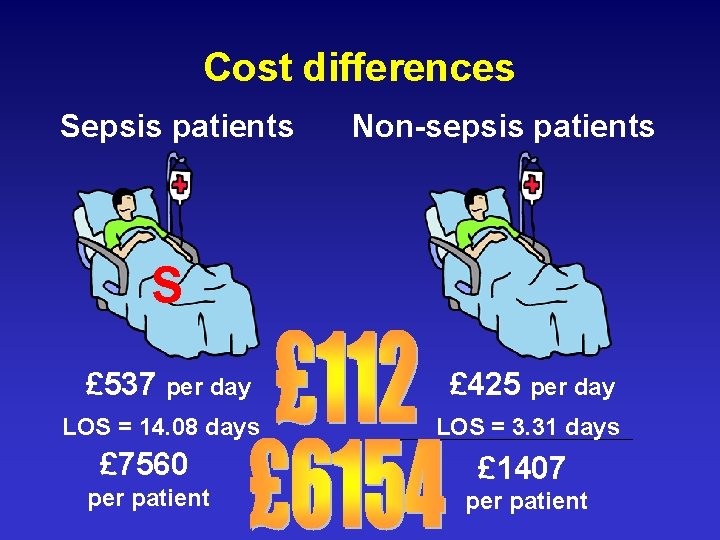
Cost differences Sepsis patients Non-sepsis patients S £ 537 per day LOS = 14. 08 days £ 7560 per patient £ 425 per day LOS = 3. 31 days £ 1407 per patient

Cost-effectiveness of IMN?
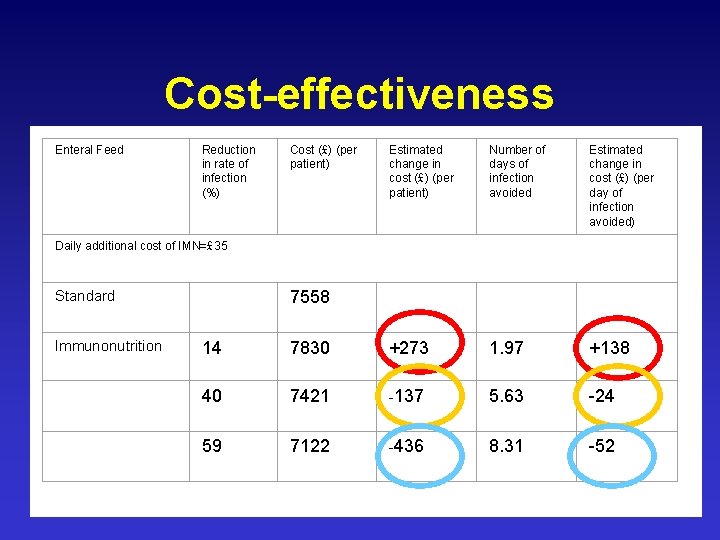
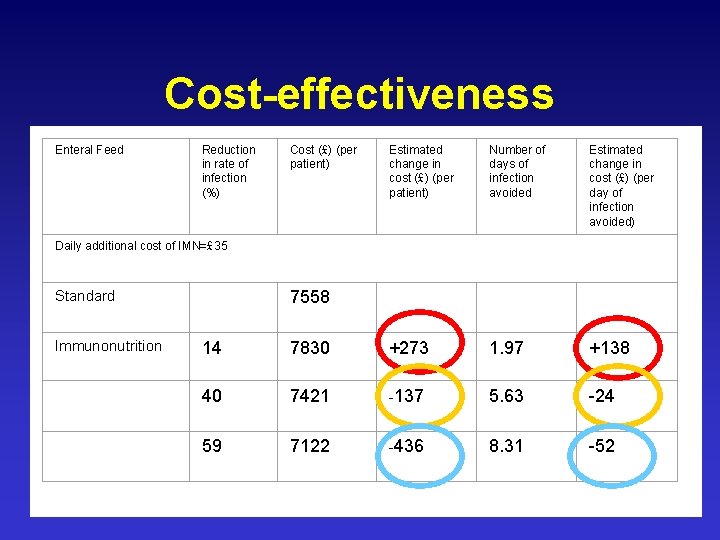
Cost-effectiveness Enteral Feed Reduction in rate of infection (%) Cost (£) (per patient) Estimated change in cost (£) (per patient) Number of days of infection avoided Estimated change in cost (£) (per day of infection avoided) Daily additional cost of IMN=£ 35 Standard Immunonutrition 7558 14 7830 +273 1. 97 +138 40 7421 -137 5. 63 -24 59 7122 -436 8. 31 -52
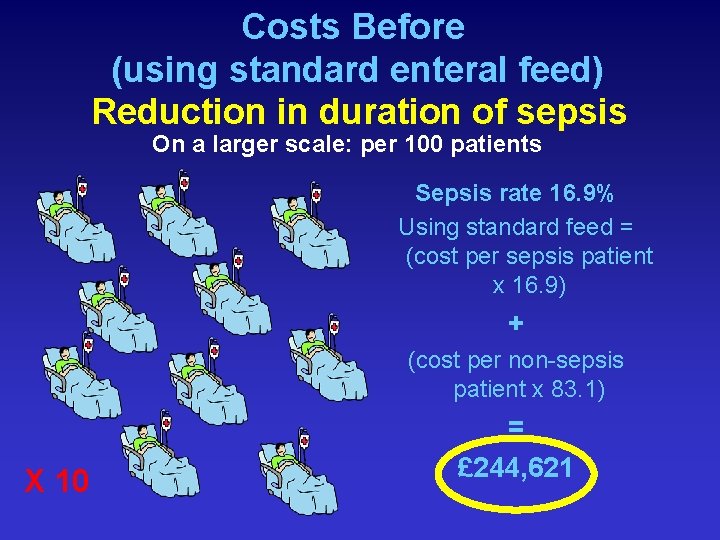
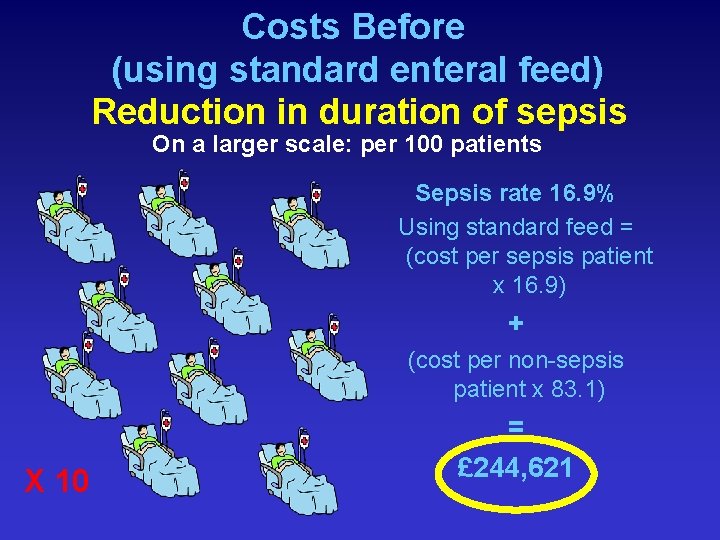
Costs Before (using standard enteral feed) Reduction in duration of sepsis On a larger scale: per 100 patients Sepsis rate 16. 9% Using standard feed = (cost per sepsis patient x 16. 9) + (cost per non-sepsis patient x 83. 1) X 10 = £ 244, 621
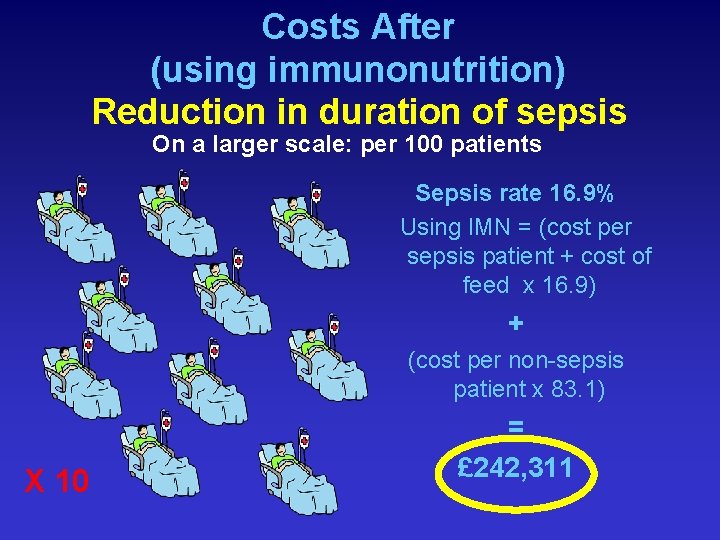
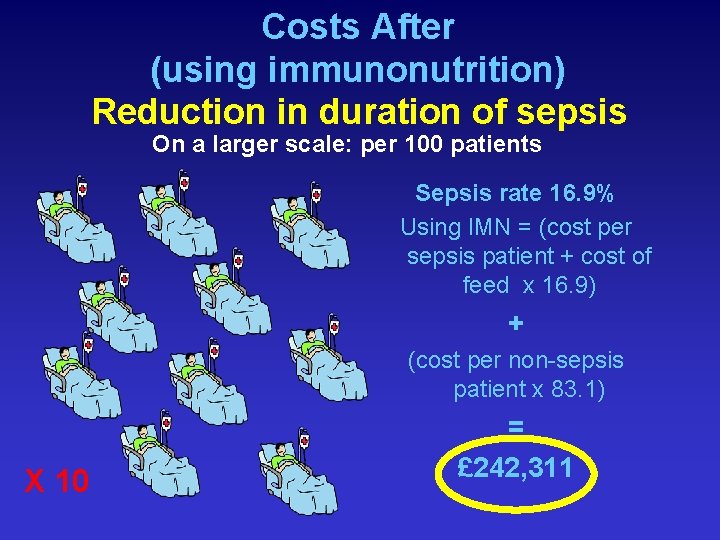
Costs After (using immunonutrition) Reduction in duration of sepsis On a larger scale: per 100 patients Sepsis rate 16. 9% Using IMN = (cost per sepsis patient + cost of feed x 16. 9) + (cost per non-sepsis patient x 83. 1) X 10 = £ 242, 311

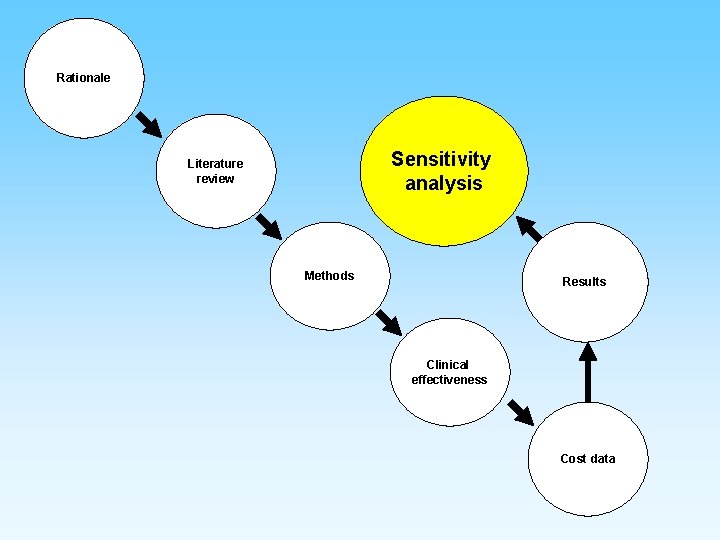
Rationale Sensitivity analysis Literature review Methods Results Clinical effectiveness Cost data
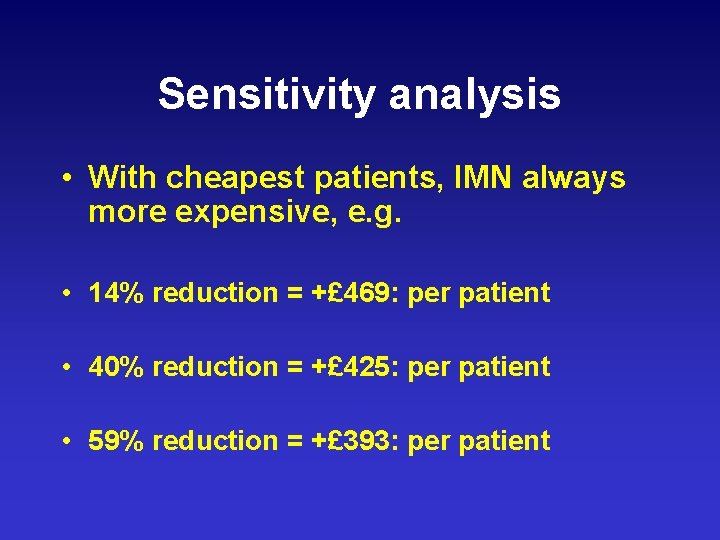
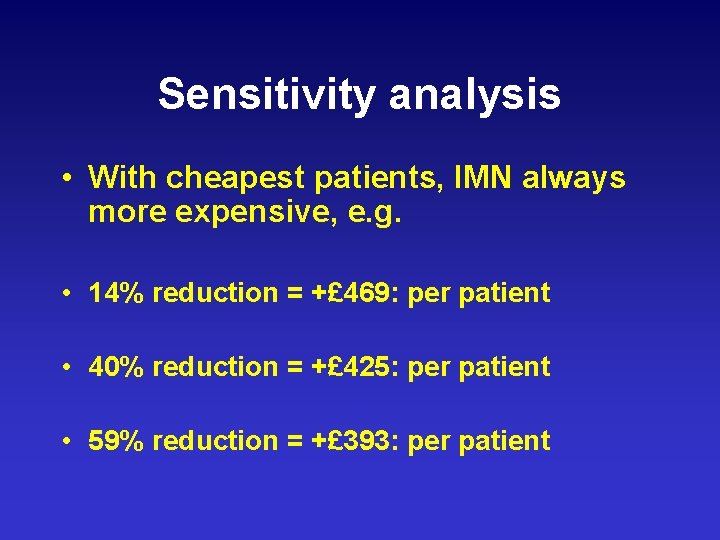
Sensitivity analysis • With cheapest patients, IMN always more expensive, e. g. • 14% reduction = +£ 469: per patient • 40% reduction = +£ 425: per patient • 59% reduction = +£ 393: per patient
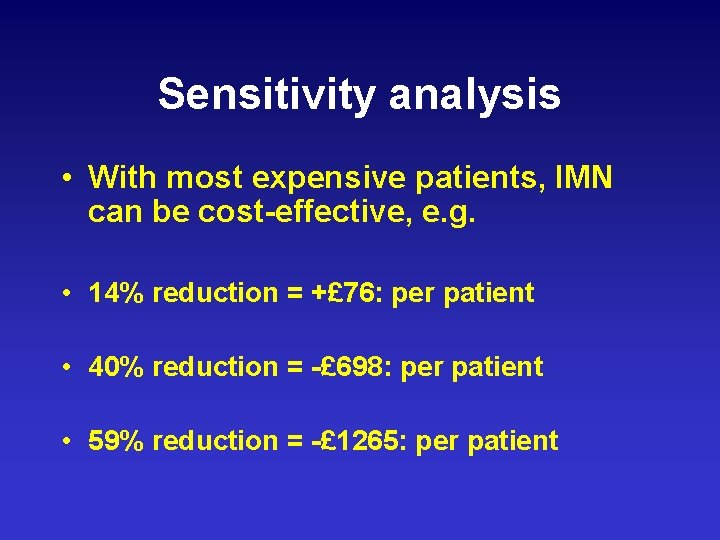
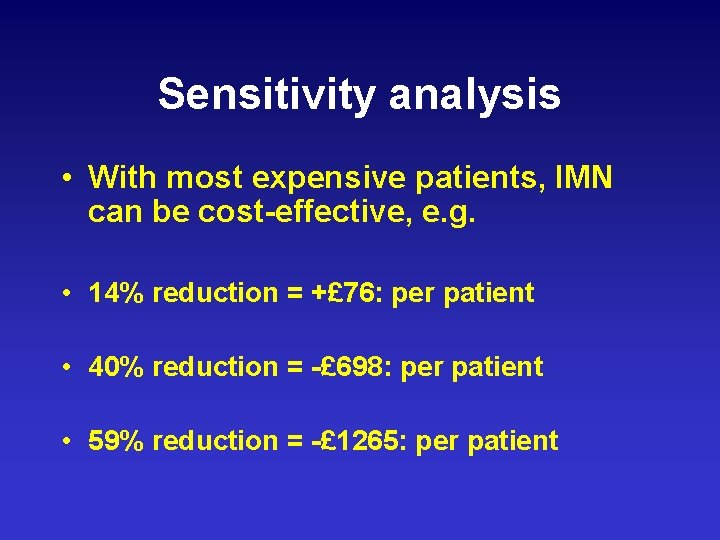
Sensitivity analysis • With most expensive patients, IMN can be cost-effective, e. g. • 14% reduction = +£ 76: per patient • 40% reduction = -£ 698: per patient • 59% reduction = -£ 1265: per patient
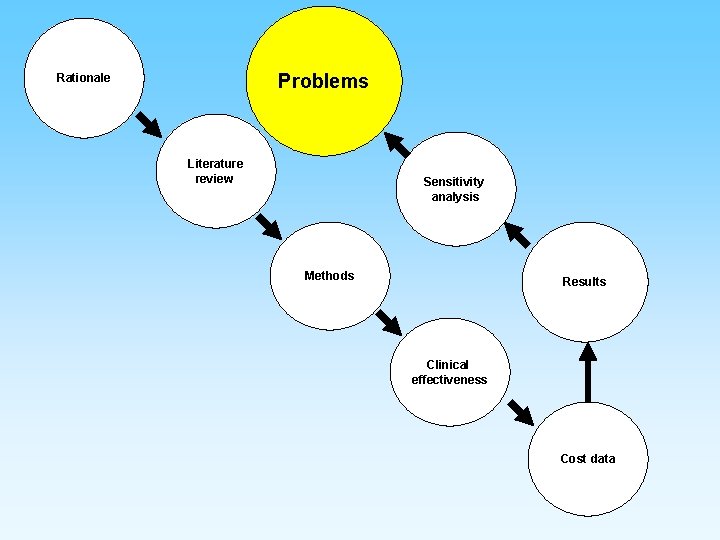
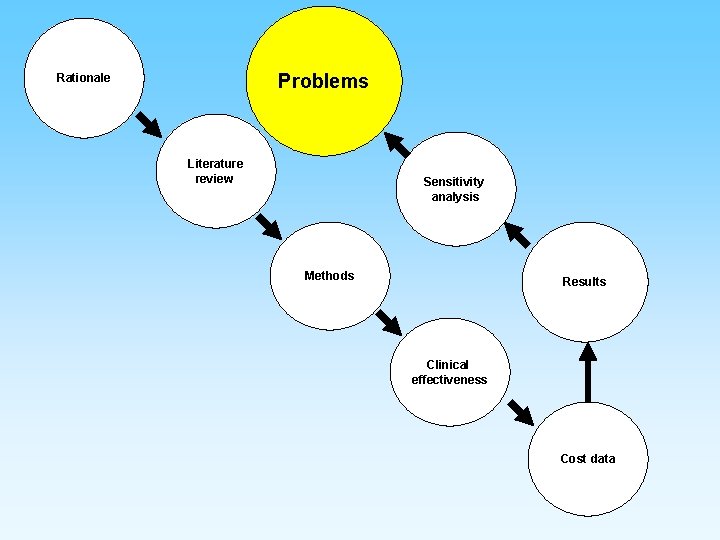
Problems Rationale Literature review Sensitivity analysis Methods Results Clinical effectiveness Cost data
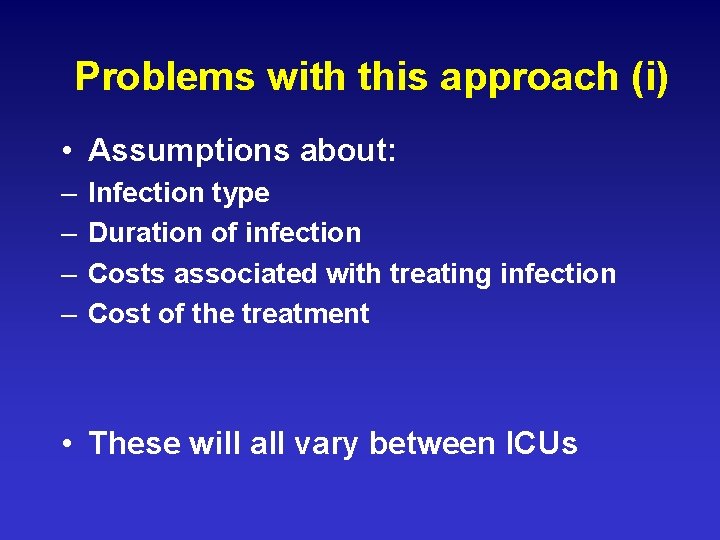
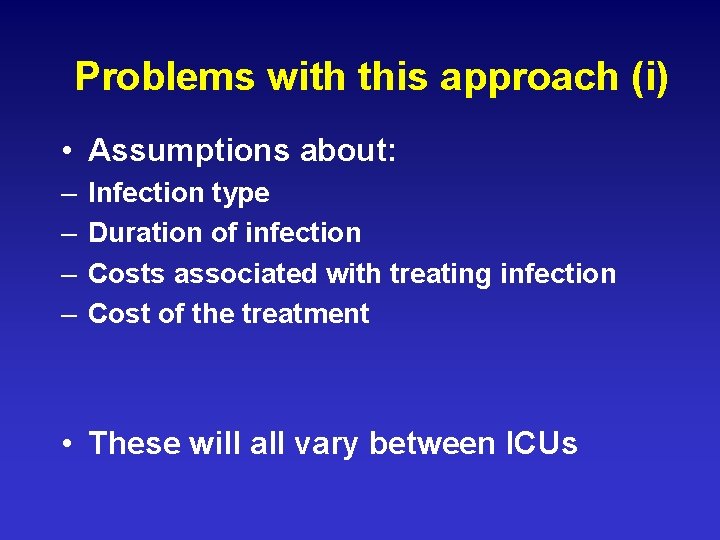
Problems with this approach (i) • Assumptions about: – – Infection type Duration of infection Costs associated with treating infection Cost of the treatment • These will all vary between ICUs
Problems with this approach (ii) • Ignores the potential length of stay reduction • Therefore, small cost savings • Doesn’t account for the recurrence of infection.
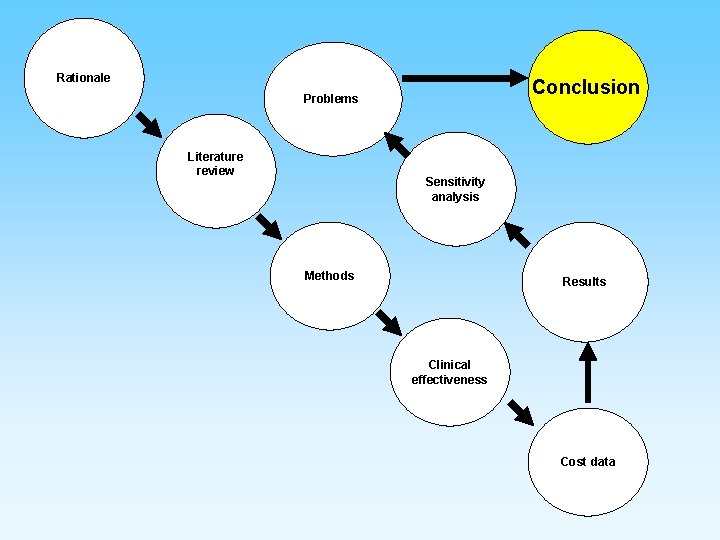
Rationale Conclusion Problems Literature review Sensitivity analysis Methods Results Clinical effectiveness Cost data
Conclusion • IMN can be cost-effective • Need to ensure a certain level of clinical efficacy • Need to identify safe population who can demonstrate benefits worth the additional costs
Recommendation In an ideal situation, an economic evaluation would be completed alongside a multicentre RCT…
 Primary immune response and secondary immune response
Primary immune response and secondary immune response Coherent+
Coherent+ Enteral polimerik adalah
Enteral polimerik adalah Abbott enteral formulas
Abbott enteral formulas Flexiflo feeding tube
Flexiflo feeding tube Cyq
Cyq Immune effector cells
Immune effector cells Any substance capable of provoking an immune response
Any substance capable of provoking an immune response Primary immune response
Primary immune response Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Immune thrombocytopenic purpura
Immune thrombocytopenic purpura Passive vs active immunity
Passive vs active immunity Antigen defintion
Antigen defintion Chapter 35 immune system and disease
Chapter 35 immune system and disease Immune complex glomerulonephritis
Immune complex glomerulonephritis Lesson 12 blood and immune system
Lesson 12 blood and immune system 1what's the purpose of the body's immune system?
1what's the purpose of the body's immune system? Thalassemia autosomal recessive
Thalassemia autosomal recessive Primary and secondary immune response
Primary and secondary immune response Phagocitize
Phagocitize Hydrops fetalis
Hydrops fetalis Immune effector cells
Immune effector cells Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Tdmu
Tdmu Tonsil histology
Tonsil histology Immunity classification chart
Immunity classification chart Chapter 55 care of the patient with an immune disorder
Chapter 55 care of the patient with an immune disorder Phagocytic cells
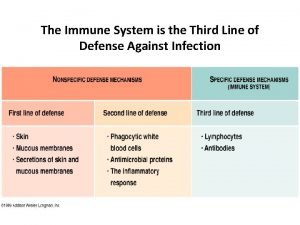
Phagocytic cells What is the third line of defense in the immune system
What is the third line of defense in the immune system Overreactions of the immune system
Overreactions of the immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Vaccinations help prepare the body to fight invasions of
Vaccinations help prepare the body to fight invasions of Cellular immune response
Cellular immune response Defination of tuberculosis
Defination of tuberculosis Difference between innate and learned behavior
Difference between innate and learned behavior Immune response controller crossword
Immune response controller crossword Oobean
Oobean Ap bio immune system
Ap bio immune system Hit heparin
Hit heparin Lymph diagram
Lymph diagram Immune reconstitution therapy
Immune reconstitution therapy Primary vs secondary immune response
Primary vs secondary immune response Adaptive immunity
Adaptive immunity Hangman flowchart
Hangman flowchart