Enteral Nutrition A Clinical Case Study using the


- Slides: 38
Enteral Nutrition: A Clinical Case Study using the Nutrition Care Process By Yingying Yip February 25, 2015
Outline Introduction of enteral nutrition � Feeding tubes � Nutrition Assessment � Types of formula � Nutrition Diagnosis � Indications of EN � Nutrition Intervention � Complications Clinical Case Study � Nutrition Monitoring & Evaluation Dysphagia and Aspiration � Nutrition Follow-Up Outcomes and Lessons
Enteral Nutrition Provides nutrients into the GI tract using a tube The tube is usually placed into the stomach, duodenum or jejunum via either the nose, mouth or the direct percutaneous route Can be used in combination with oral and/or parenteral nutrition
Feeding Tubes q Nasogastric/Orogastric/Nasojejunal (NG/OG/NJ) q q Gastrostomy (GT) q q q Temporary, <30 days Long term Done in the OR, more invasive via laparotomy Percutaneous endoscopic gastrostomy or jejunostomy (PEG/PEJ) q q Long term Endoscopically using transillumination to make incision
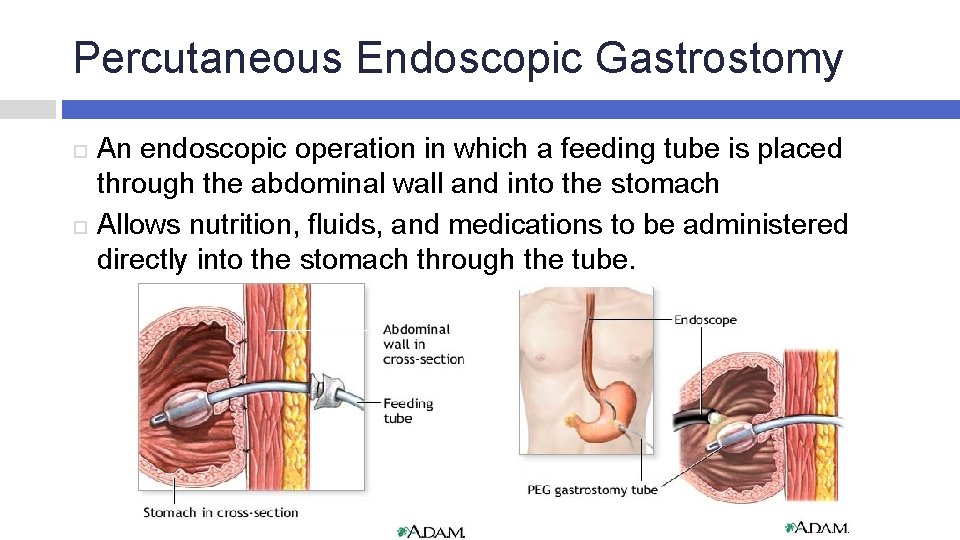
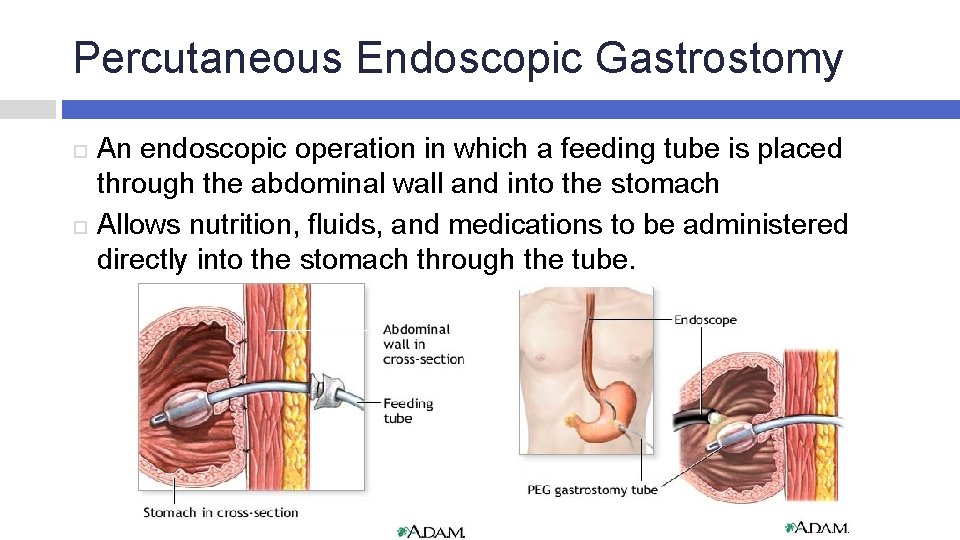
Percutaneous Endoscopic Gastrostomy An endoscopic operation in which a feeding tube is placed through the abdominal wall and into the stomach Allows nutrition, fluids, and medications to be administered directly into the stomach through the tube.
Enteral Formulas Standard/polymeric � Contains intact nutrients: intact GI tract Elemental � Completely hydrolyzed nutrients: malabsorption Disease specific � For organ dysfunction or specific metabolic conditions: renal, trauma/burns
Indications for EN q q q “If the gut works, use it. ” Functional GI tract but oral intake may not be possible, adequate, or safe Malnourished or at risk of malnutrition Prolonged poor appetite Impaired swallowing function Conditions: anorexia, dysphagia, esophageal obstruction, esophageal dysmotility, reduced level of consciousness, short bowel syndrome(more than 100 cm of jejunum)
Complications Necrotizing fasciitis Intraperitoneal bleeding Bowel perforation Septicemia Aspiration pneumonia Buried bumper syndrome Skin abscess Cellulitis Tube blockages Tube falling out Leakage of gastric contents
Dysphagia Swallowing difficulty Pain while swallowing, unable to swallow liquids and foods safely Texture-modified diet and/or thickened liquids
Aspiration A condition when foods or fluids go into the lungs instead of the stomach Cough in order to clear the food or fluid out of their lungs aspiration pneumonia Eating becomes a big challenge for people with dysphagia and people who are at risk for aspiration
CLINICAL CASE STUDY
Methodology Data were collected from: �Patient’s medical record �Interview with patient Discussed nutrition plan of care with physician and nurse Initial nutrition assessment and follow-ups
Nutrition Assessment JB: 92 year old male admitted with inability to take adequate oral nutrition, aspiration pneumonia, and features of hypovolemia Underwent percutaneous endoscopic gastrostomy (PEG) tube placement and started tube feeding
PMH Venous insufficiency, peripheral neuropathy, osteoarthritis, GERD, hyperlipidemia, atrial fibrillation, CAD, DM, osteoporosis, HTN, BPH
Nutrition Assessment – Food/Nutrition History No known food allergies Coughed when he ate for the past six months and avoided the dining room Speech-language pathologist: allowed for small sips of water and possibly pureed diet for pleasure feeds post PEG placement
Nutrition Assessment - Physical Exam Alert and oriented x 3 Skin warm and dry Abdomen soft
Nutrition Assessment - Social and Family History JB - pharmacist, married Daughter-in law - ophthalmologist Son - rheumatologist Expressed concerns over the procedure, types of tube feeding formula, and new lifestyle adaptations Full resuscitation until conditions of advanced directives apply
Nutrition Assessment – Anthropometric measurement Height: 69 in / 175 cm Weight: 188. 5 lbs / 85. 7 kg BMI: 28 IBW: 172 lbs / 78. 2 kg
Nutrition Assessment – Nutrient Needs Estimated energy needs: 20 -25 kcal/kg (20 -25 kcal) * (85. 7 kg) = 1700 kcal - 2100 kcal Protein: 1 – 1. 2 g/kg 85 -100 g protein / day
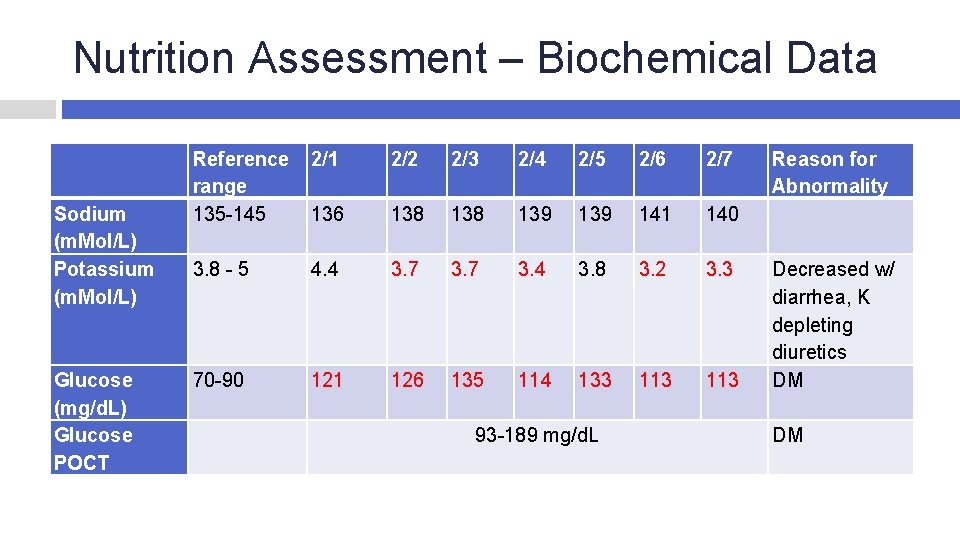
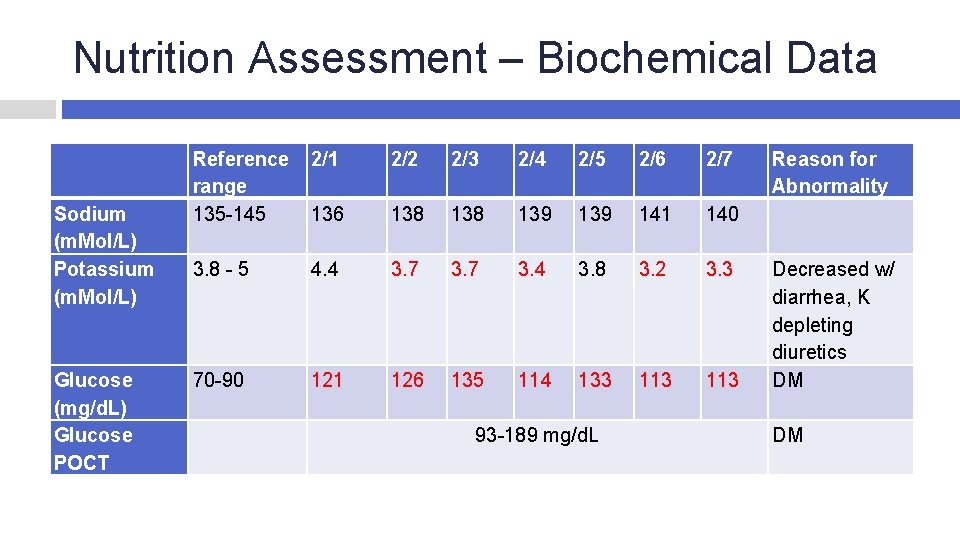
Nutrition Assessment – Biochemical Data Sodium (m. Mol/L) Potassium (m. Mol/L) Glucose (mg/d. L) Glucose POCT Reference 2/1 range 135 -145 136 2/2 2/3 2/4 2/5 2/6 2/7 138 139 141 140 3. 8 - 5 4. 4 3. 7 3. 4 3. 8 3. 2 3. 3 70 -90 121 126 135 114 133 113 93 -189 mg/d. L Reason for Abnormality Decreased w/ diarrhea, K depleting diuretics DM DM
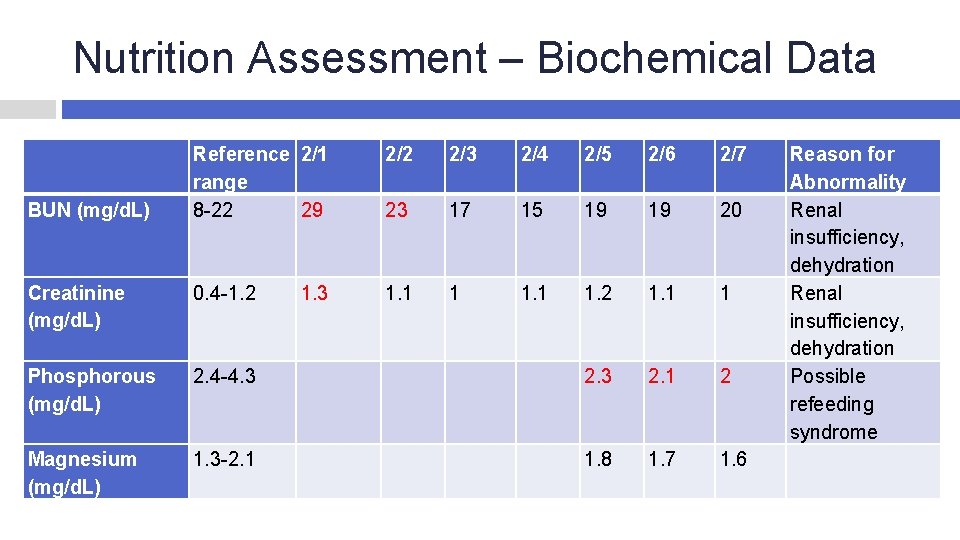
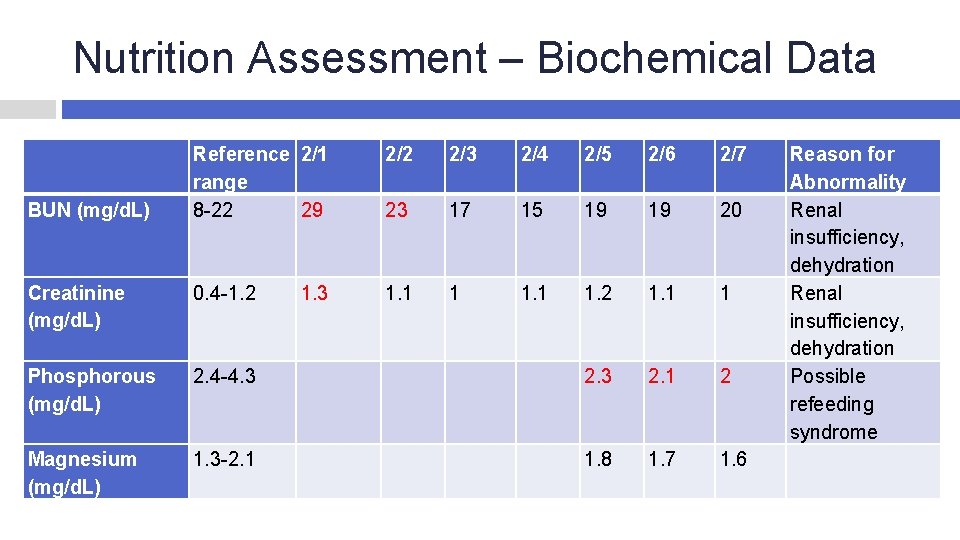
Nutrition Assessment – Biochemical Data Reference 2/1 range 8 -22 29 2/2 2/3 2/4 2/5 2/6 2/7 23 17 15 19 19 20 Creatinine (mg/d. L) 0. 4 -1. 2 1. 3 1. 1 1. 2 1. 1 1 Phosphorous (mg/d. L) 2. 4 -4. 3 2. 3 2. 1 2 Magnesium (mg/d. L) 1. 3 -2. 1 1. 8 1. 7 1. 6 BUN (mg/d. L) Reason for Abnormality Renal insufficiency, dehydration Possible refeeding syndrome

Medications Action Side Effect/Nutrition Implication Amlodipine antihypertensive Metoprolol Azithromycin SSI antihypertensive antibiotic antidiabetic Decrease Na may be recommended Dry mouth, diarrhea, N/V Diarrhea Hypoglycemia
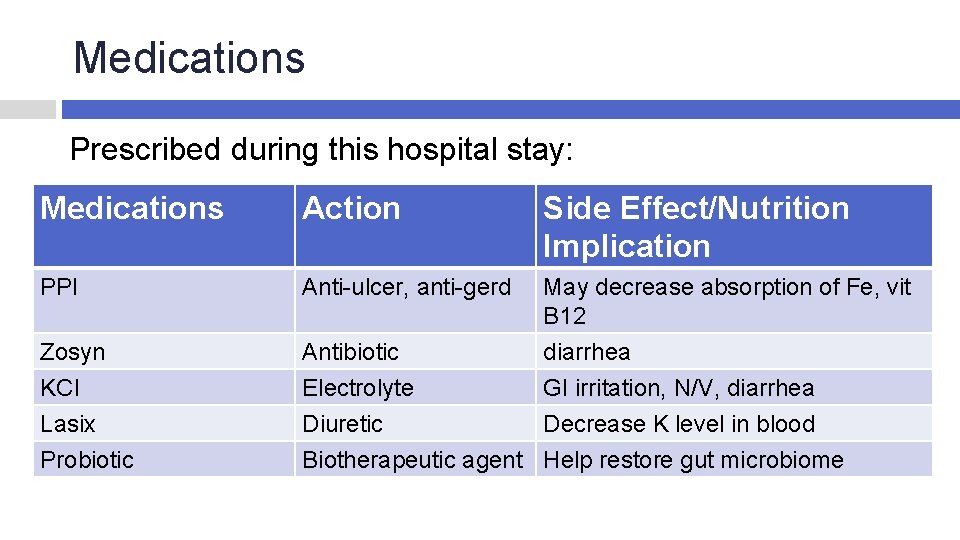
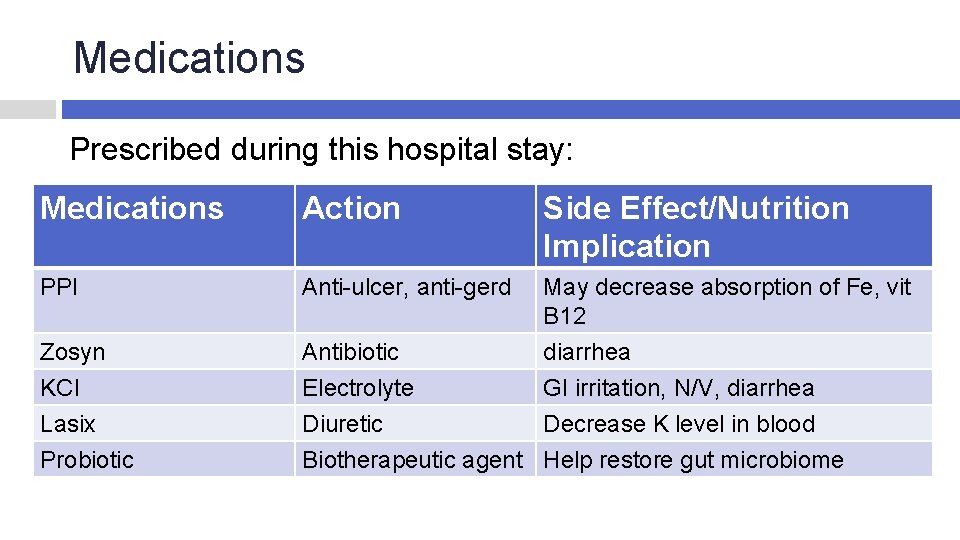
Medications Prescribed during this hospital stay: Medications Action Side Effect/Nutrition Implication PPI Anti-ulcer, anti-gerd May decrease absorption of Fe, vit B 12 Zosyn KCl Lasix Probiotic Antibiotic Electrolyte Diuretic Biotherapeutic agent diarrhea GI irritation, N/V, diarrhea Decrease K level in blood Help restore gut microbiome
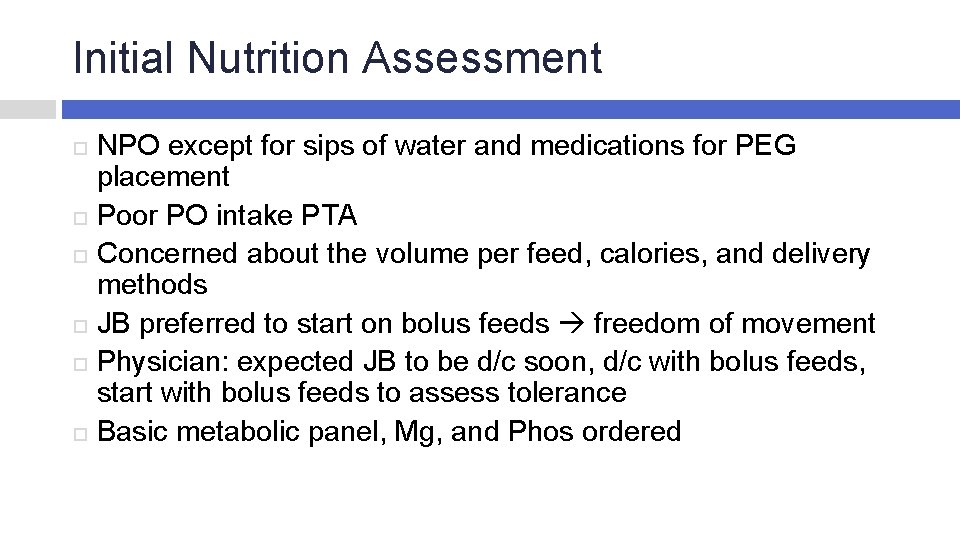
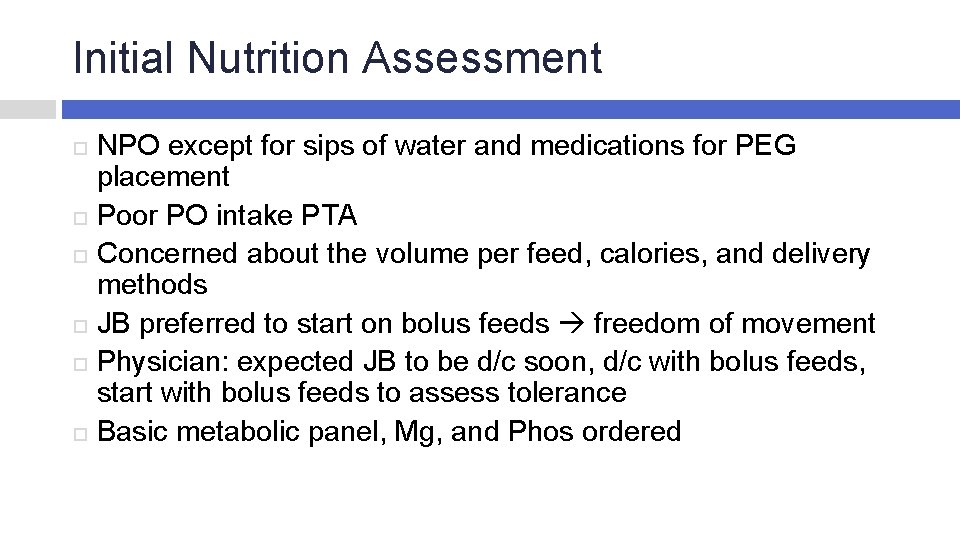
Initial Nutrition Assessment NPO except for sips of water and medications for PEG placement Poor PO intake PTA Concerned about the volume per feed, calories, and delivery methods JB preferred to start on bolus feeds freedom of movement Physician: expected JB to be d/c soon, d/c with bolus feeds, start with bolus feeds to assess tolerance Basic metabolic panel, Mg, and Phos ordered
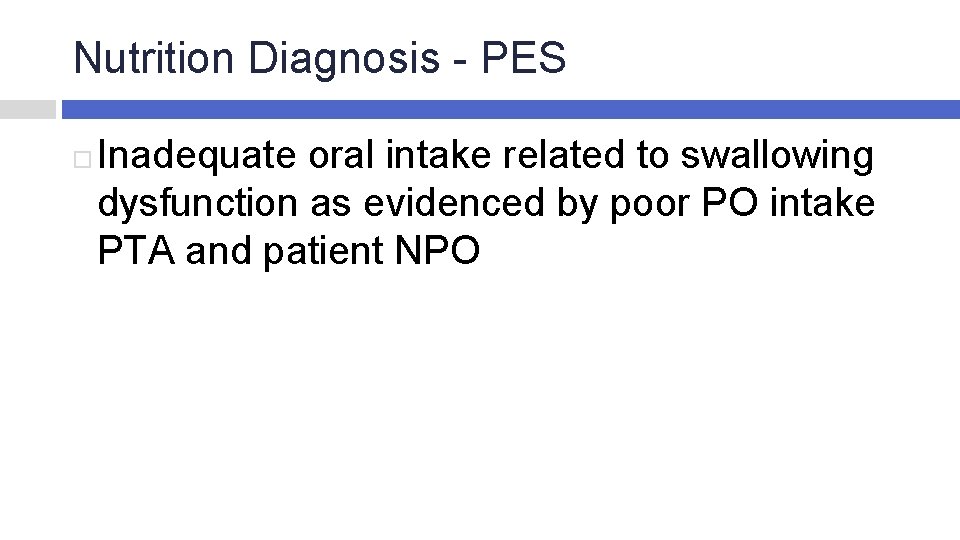
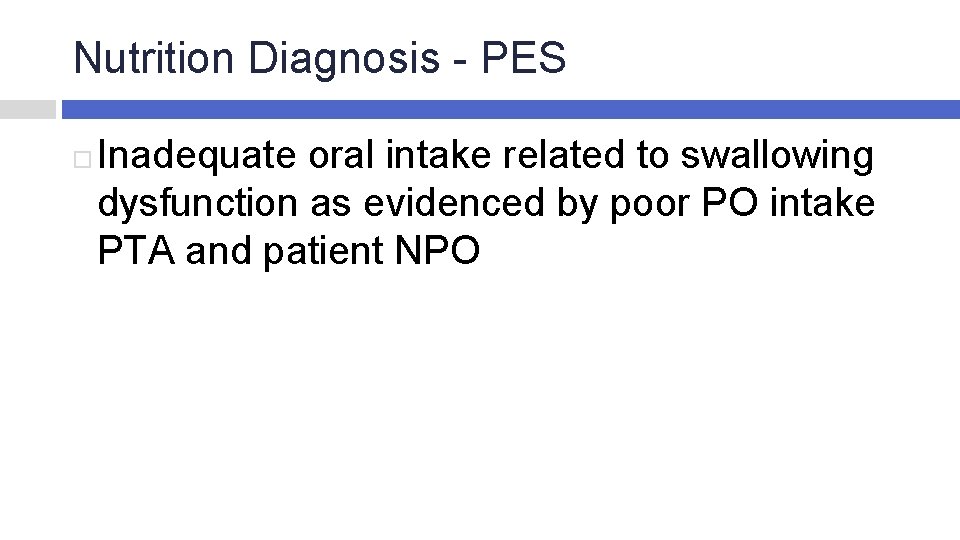
Nutrition Diagnosis - PES Inadequate oral intake related to swallowing dysfunction as evidenced by poor PO intake PTA and patient NPO
PES – Inadequate oral intake Goal: patient to meet nutritional needs via total enteral nutrition with tolerance Intervention: Jevity 1. 2 bolus feed via PEG: 2 cans at breakfast, 2 cans at lunch, 2 cans a dinner, 1 can 2 -3 hours after dinner feed (total 7 cans daily); 100 m. L free water flush before and after each feed (200 m. L per meal, total 800 m. L free water flushes) Total nutrition provided: 1995 kcal, 93 g protein, 2137 cc fluid
Nutrition Monitoring and Evaluation Indicator: Enteral nutrition Criteria: tolerate bolus feed at goal Indicator: Electrolytes and renal profile Criteria: WNL

NUTRITION FOLLOW-UPS
Nutrition Follow-up #1 JB w/ pleural effusion. Had diarrhea after each feed, refused feeding that morning. Formula changed to Osmolite 1. 2. Free water flush decreased. Nutrition dx: � 1) Inadequate oral intake --- regressing � 2) Altered GI function related to new PEG as evidenced by diarrhea after each feed Nutrition prescription: Osmolite 1. 2 bolus feed via PEG: 2 cans at breakfast, 2 cans at lunch, 2 cans a dinner, 1 can 3 hours after dinner feed (total 7 cans daily); 50 m. L free water flush before and after each feed (100 m. L per meal, total 400 m. L free water flushes) --- to provide 1995 kcal, 92 g protein, 1765 m. L free water
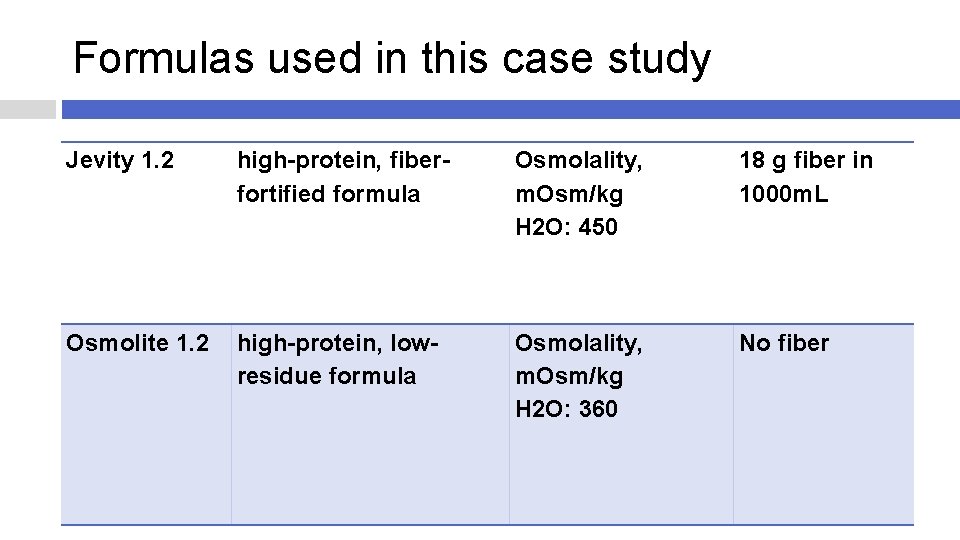
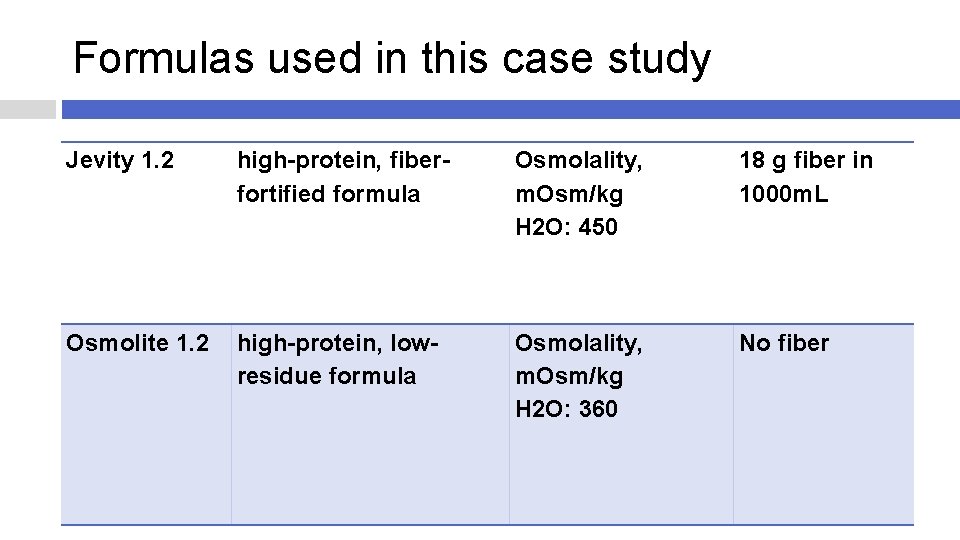
Formulas used in this case study Jevity 1. 2 high-protein, fiberfortified formula Osmolality, m. Osm/kg H 2 O: 450 18 g fiber in 1000 m. L Osmolite 1. 2 high-protein, lowresidue formula Osmolality, m. Osm/kg H 2 O: 360 No fiber
Nutrition Follow-up #2 Thoracentesis done and 1200 cc of fluid removed Still had diarrhea Space out the tube feed to improve tolerance Administer a probiotic to balance the antibiotics Decrease volume to 6 cans/day Nutrition prescription: Osmolite 1. 2 bolus feed via PEG: 1 can each on following schedule: 8 am, 9 am, 12 pm, 1 pm, 5 pm, 6 pm (total 6 cans/day); 75 m. L free water flush after each feed (75 m. L per feed, total 450 m. L Free water flush) --- to provide 1710 kcal, 80 g protein, 1620 m. L free water
Nutrition Follow-ups #3 � JB’s diarrhea had improved � MD ordered a test to rule out C. difficile infection #4 Day of Discharge � Tube feeding order was canceled accidentally � Jevity 1. 2 was sent and administered � Resent Osmolite 1. 2
Outcomes JB still had diarrhea at discharge but it had improved Tolerated Osmolite 1. 2 bolus feed, 6 cans per day with 75 m. L free water flush after each feed Provide 1710 kcal, 80 g protein, 1620 m. L water
Lessons Diabetes-specific enteral formula Tube feeding complications Continuous tube feed vs Bolus feed
References Bankhead, R. , Boullata, J. , Brantley, S. , Corkins, M. , Guenter, P. , Krenitsky, J. , et al. (2009). Enteral Nutrition Practice Recommendations. Journal of Parenteral and Enteral Nutrition. Botterill, I. , Miller, G. , Dexter, S. , & Martin, I. (1998). Deaths after delayed recognition of percutaneous endoscopic gastrostomy tube migration. British Medical Journal. Clearinghouse, N. I. (2010, October). Dysphagia. Retrieved from NIDCD: http: //www. nidcd. nih. gov/health/voice/pages/dysph. aspx Kirby, D. F. , & Delegge, M. H. (1995). American Gastroenterological Association Medical Position Statement: Guidelines for the Use of Enteral Nutrition. American Gastroenterological Association. Lloyd, D. , & Powell-Tuck, J. (2004). Artificial Nutrition: Principles and Practice of Enteral Feeding. Clin Colon Rectal Surg. Lo¨ser, C. , Aschl, G. , Hebuterne, X. , Mathus-Vliegen, E. , Muscaritoli, M. , Niv, Y. , et al. (2005). ESPEN guidelines on artificial enteral nutrition - Percutaneous endoscopic gastrostomy (PEG). Clinical Nutrition. Lynch, C. , & Fang, J. (2004). Prevention and Management of Complications of percutaneous Endoscopic Gastrostomy (PEG) Tubes. NUTRITION ISSUES IN GASTROENTEROLOGY. Mc. Mahon, M. , Nystrom, E. , Braunschweig, C. , Miles, J. , & Compher, C. (2012). A. S. P. E. N. Clinical Guidelines: Nutrition Support of Adult Patients With Hyperglycemia. Journal of Parenteral and Enteral Nutrition. Stroud, M. , Duncan, H. , & Nightingale, J. (2003). Guidelines for enteral feeding in adult hospital patients. Gut. http: //www. summitgastro. com/endoscopic-procedures/peg-placement
Thank You! Any Questions?
Delivery Methods Continuous � Uses a pump, low infusion rate � Ideal for inpatient, bedbound, high aspiration risk, acutely ill Bolus � Uses a syringe, administer 240 -480 ml in 5 -20 mins � Ideal for those living at home allows freedom of movement � Rapid infusion may cause GI intolerance
Complications Diarrhea/constipation/nausea/vomiting Distention/bloating/cramping Aspiration Dehydration/overhydration Malabsorption/maldigestion Hyperglycemia Refeeding syndrome