VIRAL INFECTIONS Measles German measles Soumaya Hadhood Prof





- Slides: 39
VIRAL INFECTIONS (Measles & German measles) Soumaya Hadhood Prof. Of Pediatrics
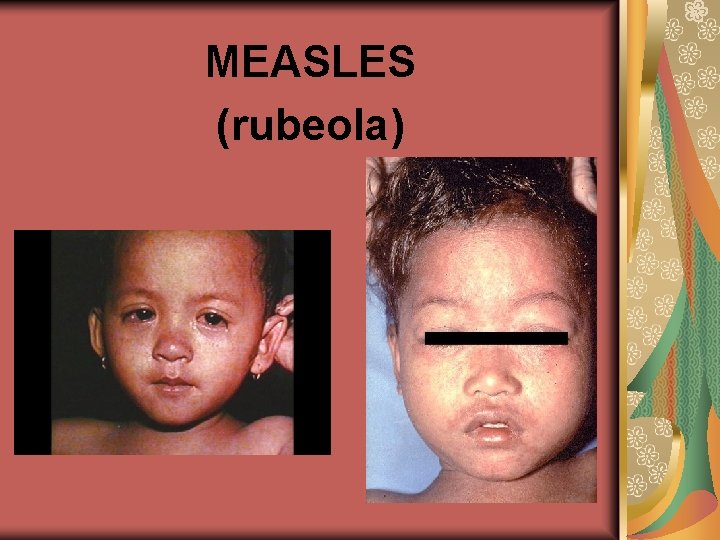
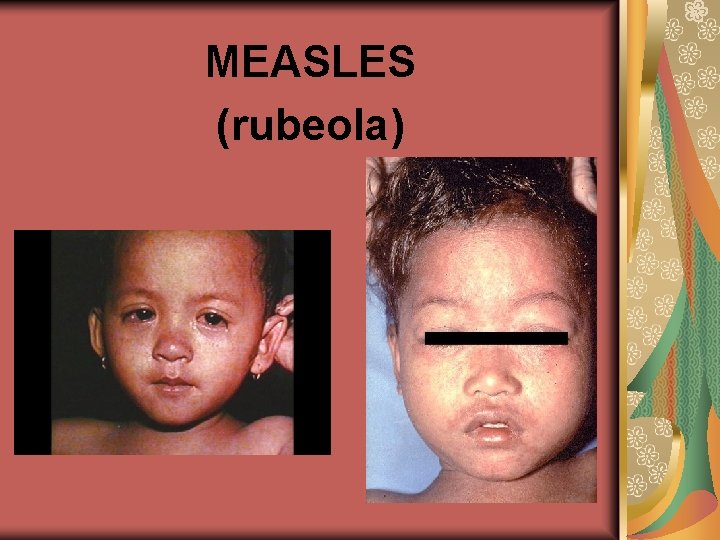
MEASLES (rubeola)
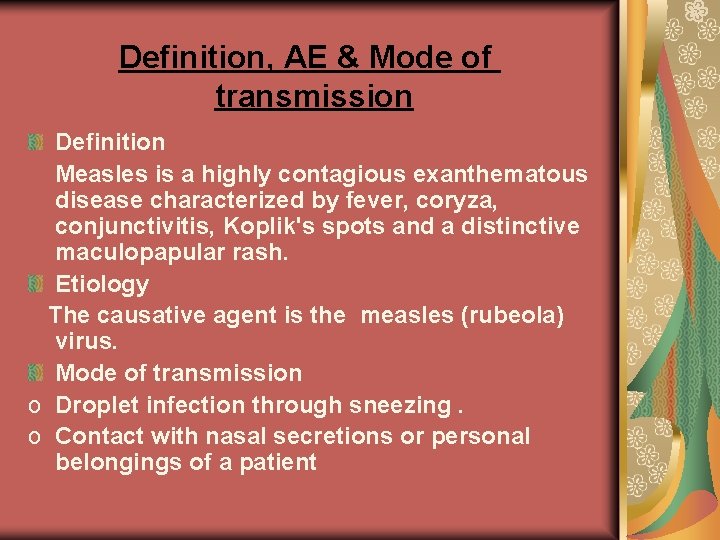
Definition, AE & Mode of transmission Definition Measles is a highly contagious exanthematous disease characterized by fever, coryza, conjunctivitis, Koplik's spots and a distinctive maculopapular rash. Etiology The causative agent is the measles (rubeola) virus. Mode of transmission o Droplet infection through sneezing. o Contact with nasal secretions or personal belongings of a patient
Incubation period & Infectivity Incubation period 7 -14 days (usually 10 days). Infectivity The period of infectivity is from the beginning of the prodromal stage until 5 days after the appearance of rash. The infant is protected for 4 -6 months after delivery if his mother had measles. Solid active immunity follows infection, so, it is very rare to have measles more than once
Clinical picture Highest incidence between 2 and 14 years. Prodromal (catarrhal) stage Acute onset of fever that tends to be highest just before the appearance of the rash. Generalized malaise. Irritating cough which becomes more frequent as the disease progresses. Sore throat , sneezing and mucopurulent nasal discharge. Lacrimation , photophobia, and nonpurulent conjunctivitis. Usually , lasts 4 -7 days
Enanthem and Koplik's spots Enanthem ( rash on mucous membranes ) appears 1 -2 days before the appearance of the rash as small red spots on the inflamed hard and soft palate. Koplik's spots are pathognomonic , appearing 1 day before the rash as rose - red spots with gray white dots in the center. They are first noted on the buccal mucosa opposite the molar teeth and usually disappear with the appearance of the skin rash


Exanthem (skin rash) It appears in the fifth day of illness. It begins as a maculopapular rash along the hair line on back of neck and behind the ears. It spreads rapidly to involve the whole body as it covers the trunk at the end of the second day and by the end of the third day , the whole body. . The fever remains high during the appearance of the rash. The rash is blotchy, irregular and coalesces into large red areas of varying sizes and shapes.
Rash …. . In the fourth day, the rash begins to fade in the same sequence (from the face downwards ) with brawny desquamation. The skin returns to normal or a light brown pigmentation is left that may persist for months.
Laboratory findings in measles Leucopenia with relative lymphocytosis. Leucocytosis occurs if secondary bacterial infection complicates the course of measles. Diagnostic rise in the specific antibody titer.
Differential Diagnosis of measles German measles It is not as severe as measles, no conjunctivitis , photophobia or Koplik’s spots and there is lymphadenopathy esp. of occipital and postauricular groups. Roseola infantum : It affects younger children and the rash appears after subsidence of the fever Scarlet fever: The rash is diffuse and blanchable with circumoral pallor. There is exudative tonsillitis , cervical lymphadenitis and Leucocytosis instead of leucopenia in measles. Drug rash
Complications Respiratory complications a. Pneumonia: Early interstitial pneumonia due to measles virus invasion. Late pneumonia caused by secondary bacterial infection. b. Otitis media : one of the most common complications. c. Sinusitis, mastoiditis, laryngitis (during the prodrome) and laryngotracheobronchitis. d. Activation of a dormant tuberculosis lesion
Neurological complications a. Encephalitis : Early viral encephalitis due to virus invasion. Late demyelinating encephalitis due to allergic reactions. Sub acute sclerosing panencephalitis which is a chronic progressive fatal encephalitis caused by persistent measles infection of the CNS. b. Aseptic meningitis. c. Guillain-Barré syndrome. d. Cerebellar ataxia.
Skin and mucous membranes Hemorrhagic rash ( black measles ) Purpura : thrombocytopenic and non-thrombocytopenic. Skin infections as impetigo, furunculosis and gangrenous stomatitis (cancrum oris).
GIT Complications Gastroenteritis. Ulcerative colitis. Protein energy malnutrition e. g. kwashiorkor.
Prophylaxis Active immunization: MMR vaccine (see vaccination) Passive immunization: a. by immune globulins injected deeply IM. b. given within 6 days of exposure to prevent or attenuate measles infection c. used in immune compromised children or young infants below 9 months if their mothers were not immune
General lines of ttt Isolation of the patient (for 5 -7 days from the onset of the rash). Rest until the patient becomes afebrile. Antipyretics for fever. Hygienic care of the eyes and mouth (saline sponges and irrigations). Diet is offered as tolerated by the child. Cough depressants only for the dry irritating cough (safe remedy). Treatment with oral vitamin A reduces the mortality and morbidity in children with severe measles and PEM. A single dose of 100 -200. 000 I. U is given, but in children with ophthalmologic complications , the dose is repeated in the 2 nd day and 4 weeks later.
Specific ttt & ttt of complications Specific No specific treatment. Treatment of complications Antibiotics for secondary bacterial infections. Symptomatic treatment for encephalitis as anticonvulsants. Correction of dehydration and electrolytes in diarrhea. Treatment with oral vitamin A reduces morbidity and mortality especially in children with measles and PEM in developing countries.
German measles (rubella) or (3 -days measles)

efinition & Etiology Definition It is a contagious disease characterized by typical eruption and lymph node enlargement. Etiology The causative agent is the German measles (rubella) virus
Modes of transmission Droplet infection. Direct contact. Transplacental congenital infection
Incubation period & Infectivity o o Incubation period 14 -21 days. Infectivity The period of infectivity is 5 -7 days prior to and 5 -7 days after appearance of the rash. Infant with congenital rubella is infectious for at least 10 -12 months. Infants are protected for about 6 months if their mothers were immune. Life long immunity develops after infection.
Clinical picture Age : highest incidence between 514 years. Prodromal stage: Shorter than that of measles (few hours up to one or two days). – May pass unnoticed. – It consists of mild fever, mild nasopharyngitis, no photophobia
Enanthem and lymph nodes enlargement The enanthem appears just before the rash in the form of small red spots on the soft palate and hard palate. Lymphadenopathy is evident 24 hours before the rash and may be present for a week or more. This is the most characteristic sign of the disease. The lymph nodes involved are postauricular, posterior cervical and posterior occipital. The lymph nodes are tender but the tenderness decreases as the rash appears. Mild splenomegaly and generalized lymphadenopathy may occur.
Exanthem (Skin rash ) It begins on the face and spreads quickly. On the first day the rash simulates that of measles (i. e. discrete maculopapular rash). On the second day, it resembles scarlet fever (finely papular diffuse erythema) called scarletiniform rash and On the third day, the rash fades with no desquamation or staining (hence the name 3 days measles). Evolution is so rapid that the rash may be fading on the face by the time it appears on the trunk.
Laboratory Findings Transient leucopenia may occur. Rubella Immunoglobulin M (Ig. M) antibodies are detectable in the first few days of illness
Differential Diagnosis : It should be differentiated from measles and other exanthematous diseases Complications not common. Encephalitis: may be fatal, but recovery is usual. Polyarthritis: sometimes occurs on the 2 nd /3 rd day of the rash affects mainly patients above the age of 16 years. several joints are involved with pain and ? effusion. Thrombocytopenic purpura: rare Congenital rubella syndrome : is the most serious complication (see below).
Prophylaxis of German measles Active immunization : by the MMR vaccine Passive immunization: a. immune serum globulin given within 7 days of exposure. b. it is given to non immune pregnant women on exposure
Treatment General : Avoid contact with pregnant females. Analgesics and antipyretics for arthralgia and fever Specific : No specific treatment. Treatment of Complications is Symptomatic

CONGENITAL RUBELLA SYNDROME
CONGENITAL RUBELLA SYNDROME If a pregnant female acquires rubella before the eighth week of gestation, between 50 -80% of fetuses become infected. If infection occurs by the second trimester no more than 10 -20% of infants become infected. If infection occurs during the third trimester, infection of the fetus is relatively uncommon. Infection of fetus may result in his death or congenital rubella syndrome.
Manifestations of congenital rubella syndrome : They range from subclinical to severe multi-systemic disease with multiple anomalies : Low birth weight or intrauterine growth retardation. – Bilateral congenital cataract, microphthalmia, retinal lesions and glaucoma. – Hearing loss which may be delayed in onset. If severe and present since birth it leads to deaf-mutism. –
–Congenital heart disease (PDA, pulmonary stenosis, VSD). – MR, microcephaly or hydrocephalus. –Viral interstitial pneumonia, hepatitis, thrombocytopenic purpura and anemia due to persistent viral infection
Management of a pregnant female exposed to or acquiring Rubella If a pregnant female of unknown immune status is exposed to rubella, a hemagglutination inhibition test measuring rubella antibodies is performed immediately. If she is immune, reassure her. If she is not immune and therapeutic abortion is not accepted, passive immunization with immunoglobulins is performed (however, effect is not predictable).
Other lines of management : If abortion is accepted, do not give immunoglobulins and follow her carefully for appearance of rubella manifestations and repeat the hemagglutination inhibition test If signs of rubella develops (particularly in first trimester) or if the level of antibodies rises, therapeutic abortion is performed.

THANK YOU
 Soumaya chaffar
Soumaya chaffar Soumaya el hassouni
Soumaya el hassouni Muse soumaya
Muse soumaya Low german vs high german
Low german vs high german Storch infections
Storch infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Classification of acute gingival infections
Classification of acute gingival infections Bone and joint infections
Bone and joint infections Opportunistic infections
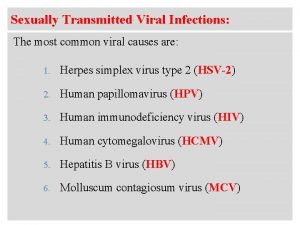
Opportunistic infections Genital infections
Genital infections Johnson and johnson botnet infections
Johnson and johnson botnet infections Infections opportunistes digestives
Infections opportunistes digestives Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Genital infections
Genital infections Storch infections
Storch infections Bacterial vaginosis
Bacterial vaginosis Opportunistic infections
Opportunistic infections Nosocomial infections
Nosocomial infections Phase of dengue fever
Phase of dengue fever Mrs measles
Mrs measles Pathophysiology of measles
Pathophysiology of measles Measles cdc
Measles cdc Sspe measles
Sspe measles Measles vs chicken pox
Measles vs chicken pox Ples phantom
Ples phantom Branny desquamation measles
Branny desquamation measles Mumps medicine
Mumps medicine Multiple choice questions on chicken pox
Multiple choice questions on chicken pox Measles cases
Measles cases Measles ppt 2020
Measles ppt 2020 Diff between measles and chickenpox
Diff between measles and chickenpox Measles cdc
Measles cdc Viral
Viral Itil wikipedia fr
Itil wikipedia fr Viral arthritis
Viral arthritis Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral
Viral Viral shedding
Viral shedding