Venepuncture Peripheral IV Cannulation Study Day June 2009
- Slides: 36
Venepuncture & Peripheral IV Cannulation Study Day June 2009 20. 08. 09 1
Aim • Explore the legal and professional issues in the extended role • Discuss health and safety issues in venepuncture and cannulation • Describe infection control issues in venepuncture and cannulation • Explore practical aspects of venepuncture and cannulation 20. 08. 09 2
Venepuncture Procedure of entering a vein with a needle for the purpose of: • Obtaining a representative sample of blood for diagnostic purposes • Monitoring levels of blood components 20. 08. 09 3
Peripheral IV Cannulation • The procedure of puncturing a patient’s skin to allow insertion of a temporary plastic tube into a vein for the purpose of: • Bolus injection • Short term infusion • Blood transfusion • Rapid infusion of medication or fluid. (Jackson 2003) 20. 08. 09 4
Legal and professional • As a professional you are personally accountable for actions and omissions in your practice and must always be able to justify your decisions. • You must work within the limits of your competence • NMC 2008 20. 08. 09 5
NMC Code of Conduct • Consent • Keeping your knowledge and skills up to date • Keeping clear and accurate records 20. 08. 09 6
Consent • You must ensure that you gain consent before you begin any treatment or care • You must uphold peoples rights to be fully involved in decisions about their care • No adult can validly give consent for another adult unless legally authorised to do so Adults with Incapacity Act (2000) • It is not necessary to document consent to routine and low-risk procedures e. g. taking a blood sample. 20. 08. 09 7
Four Arenas of Accountability To the public To the patient To the employer To the profession 20. 08. 09 8
Health & Safety • • H&S applicable to venepuncture and cannulation includes: Sharps injury procedures Extended role training Policy for the disposal of sharps Prevention and protection from blood borne viruses. 20. 08. 09 9
Preparation for procedure • The patient – explanations, education re cannula care, assessment • Equipment – integrity of packaging and expiry dates • Environment – clean, clear, clutter free, good lighting • Cannula – smallest cannula to suit purpose • Veins – choose large veins for irritant drugs 20. 08. 09 10
Technique • Asepsis • Vein stabilised • Smooth accurate placement • Correct use of tourniquet • Correct vein assessment 20. 08. 09 • • For cannulation: Stylet never be re introduced Cannula flushed Connections secure Cannula secure 11
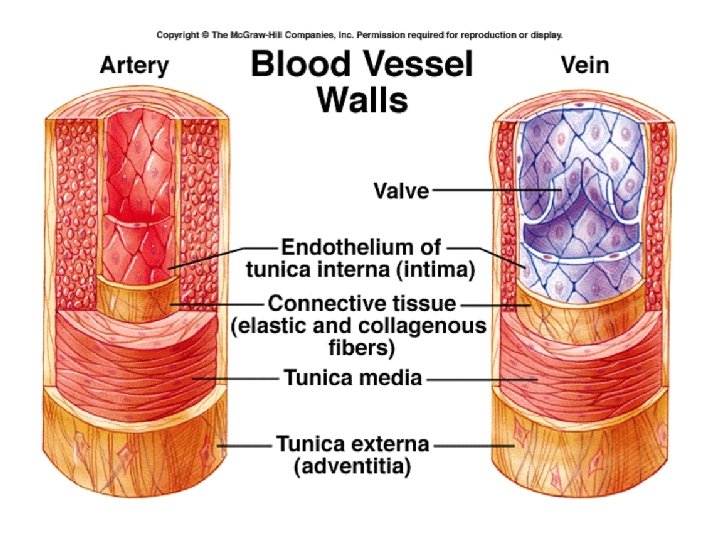
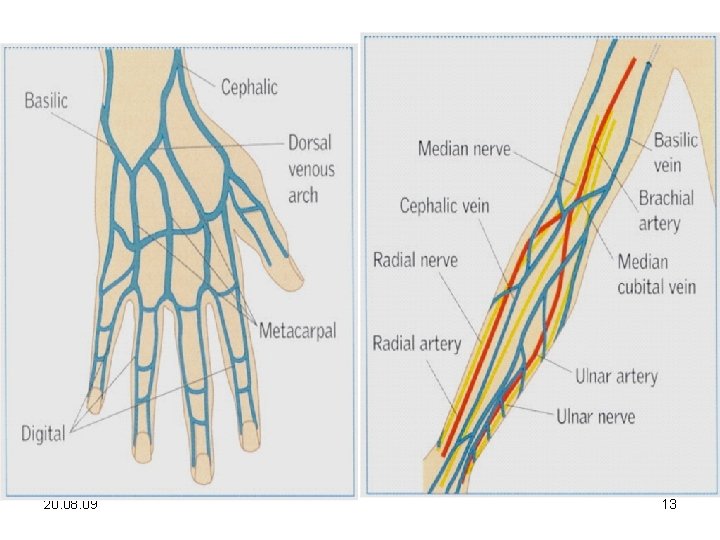
20. 08. 09 12
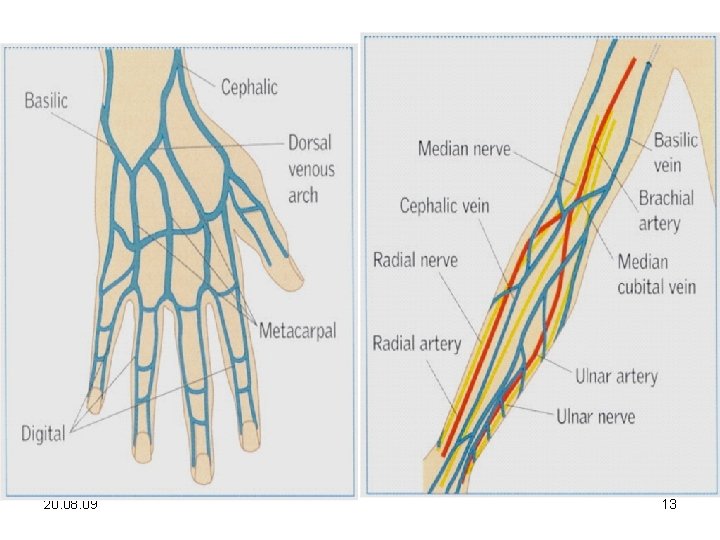
20. 08. 09 13
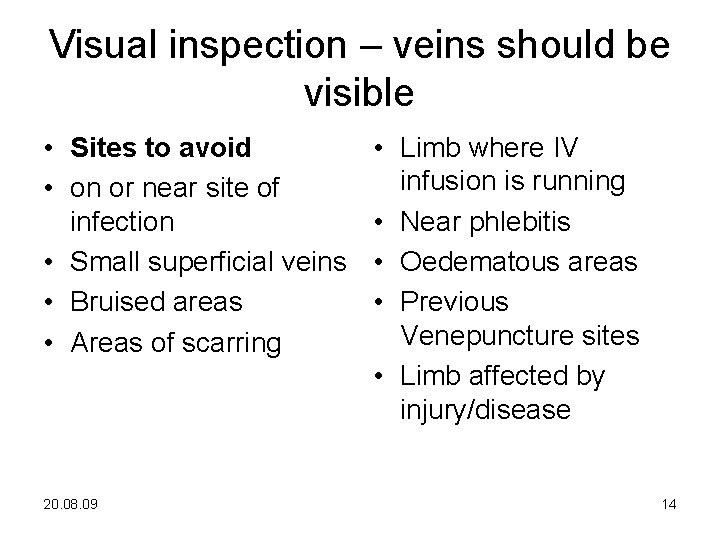
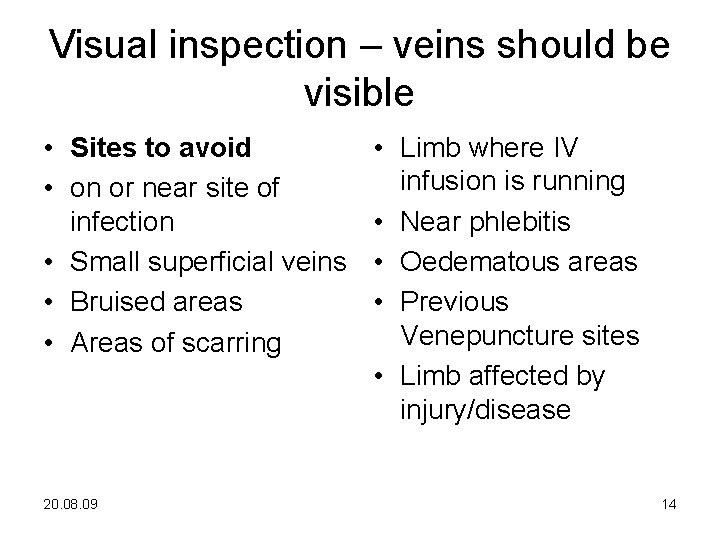
Visual inspection – veins should be visible • Sites to avoid • on or near site of infection • Small superficial veins • Bruised areas • Areas of scarring 20. 08. 09 • Limb where IV infusion is running • Near phlebitis • Oedematous areas • Previous Venepuncture sites • Limb affected by injury/disease 14
Tourniquet • Know how to use it before approaching patient! • 10 cm above site (3 finger breadths) • 2 fingered gap • Apply tourniquet to the upper arm ensuring it does not obstruct arterial flow • Check patient is comfortable • A latex glove must 20. 08. 09 never be used 15
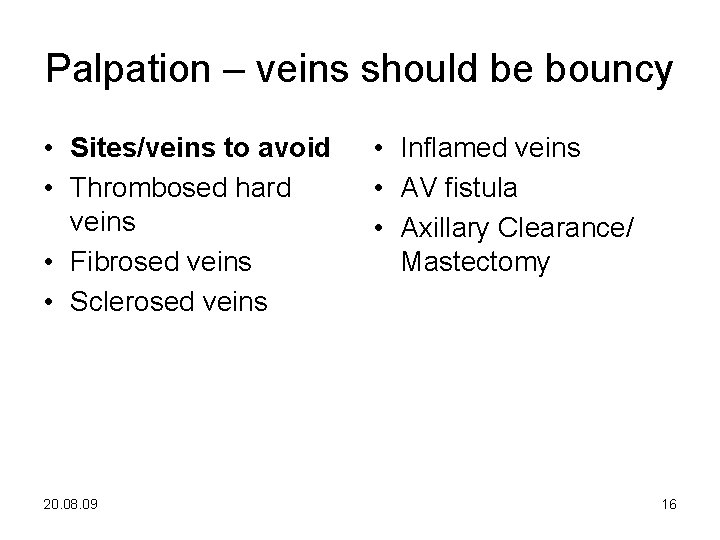
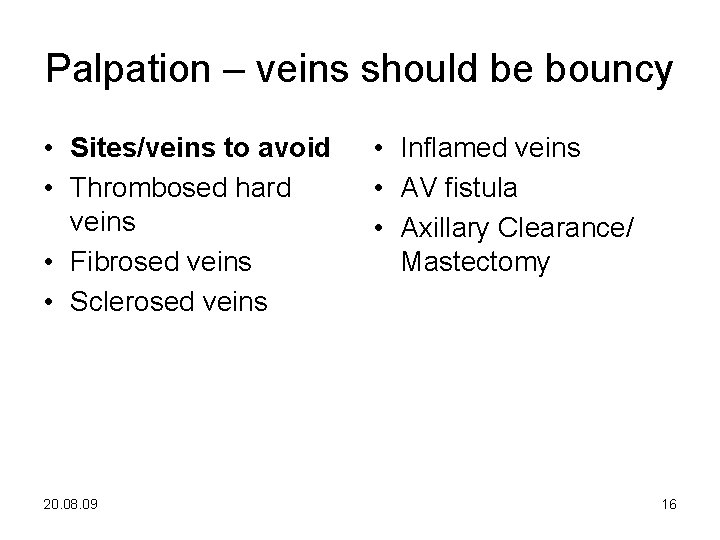
Palpation – veins should be bouncy • Sites/veins to avoid • Thrombosed hard veins • Fibrosed veins • Sclerosed veins 20. 08. 09 • Inflamed veins • AV fistula • Axillary Clearance/ Mastectomy 16
20. 08. 09 17
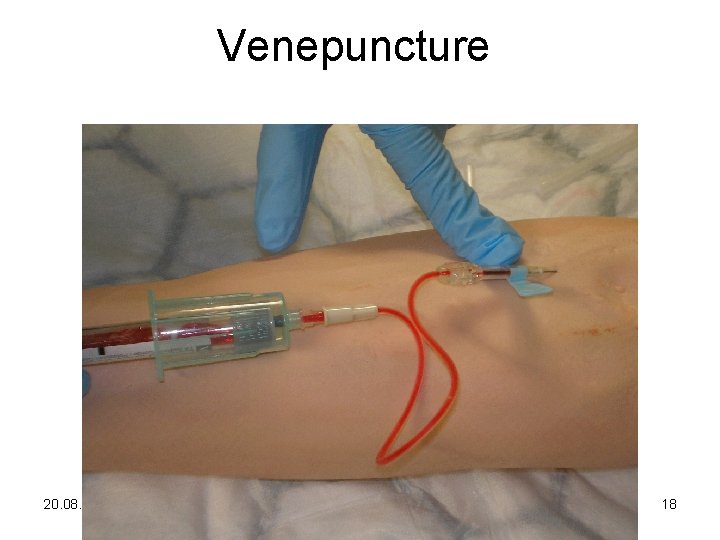
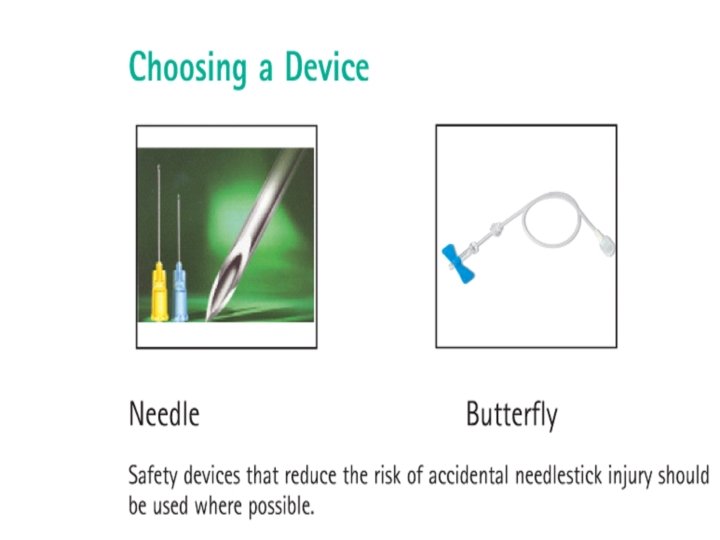
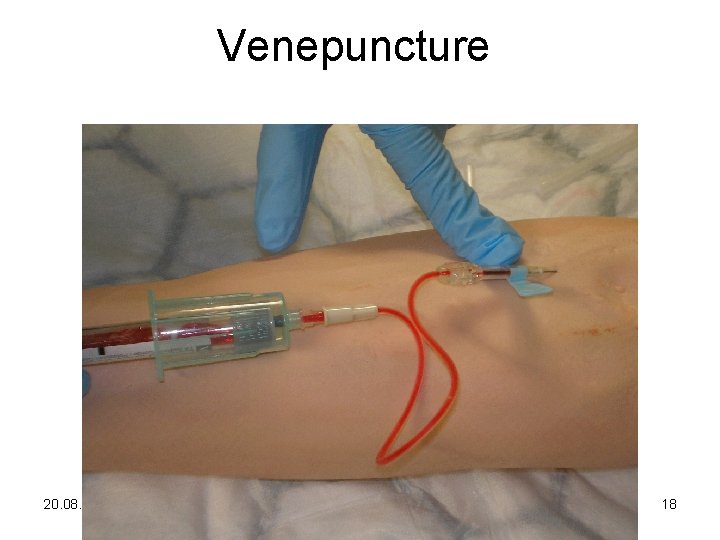
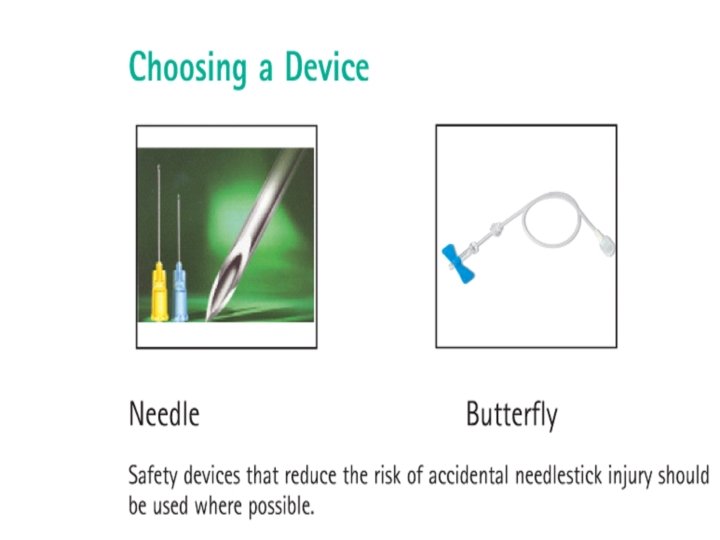
Venepuncture 20. 08. 09 18
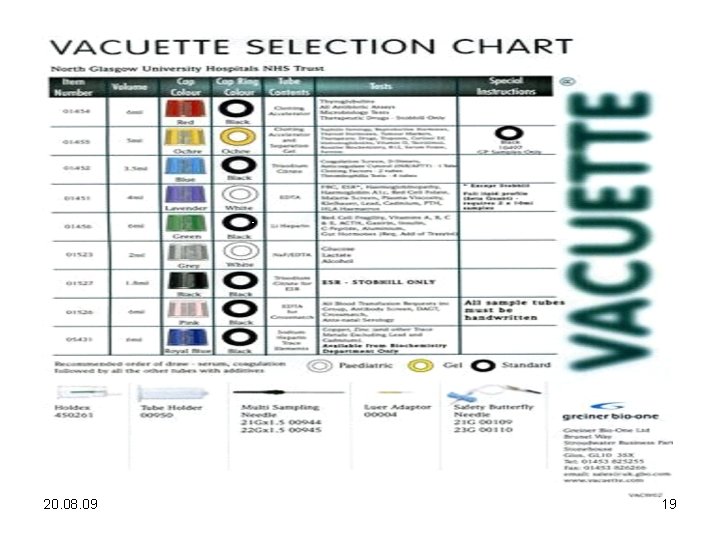
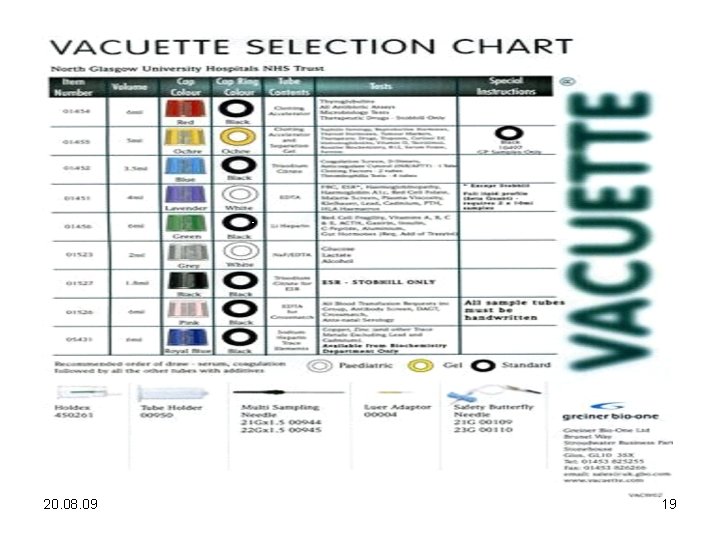
20. 08. 09 19
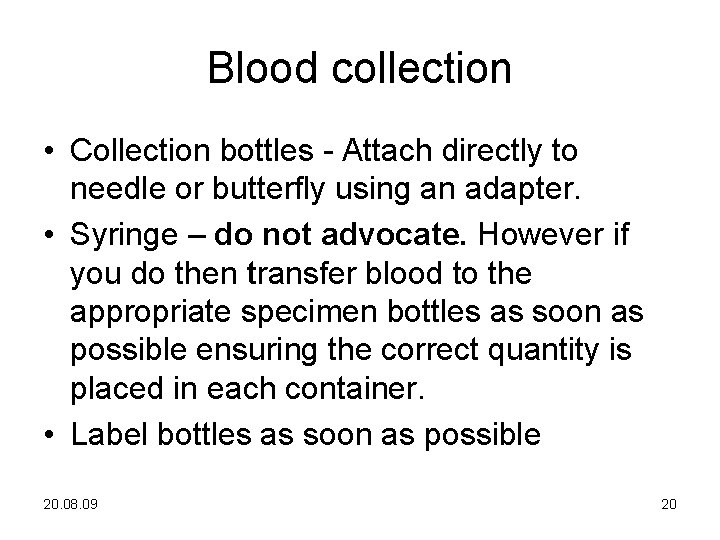
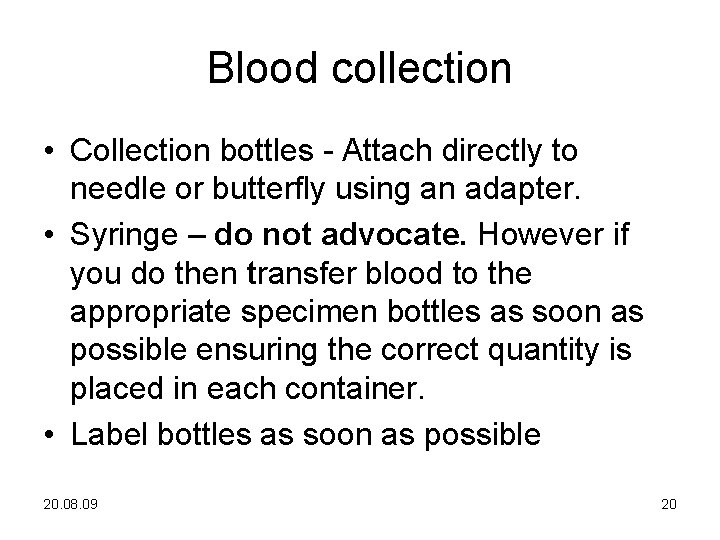
Blood collection • Collection bottles - Attach directly to needle or butterfly using an adapter. • Syringe – do not advocate. However if you do then transfer blood to the appropriate specimen bottles as soon as possible ensuring the correct quantity is placed in each container. • Label bottles as soon as possible 20. 08. 09 20
Via venous access device • Peripheral catheters should not be used for routine blood sampling • If necessary – do not use a prevacuumed system. • Use syringe 10 mls or less. 20. 08. 09 21
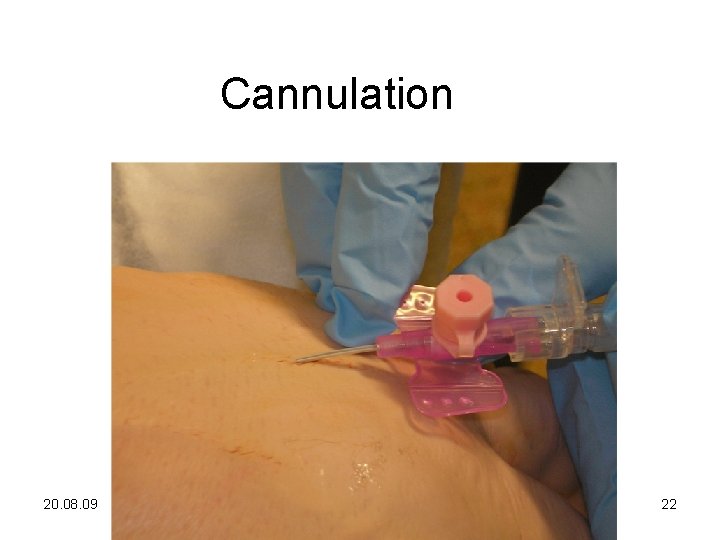
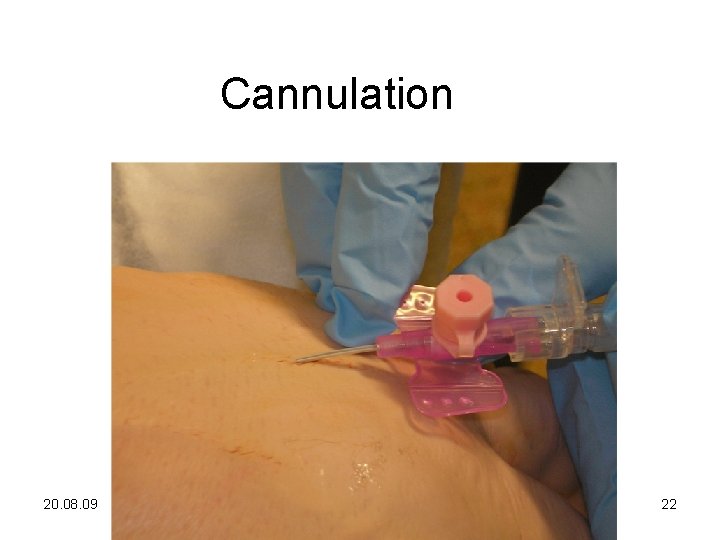
Cannulation 20. 08. 09 22
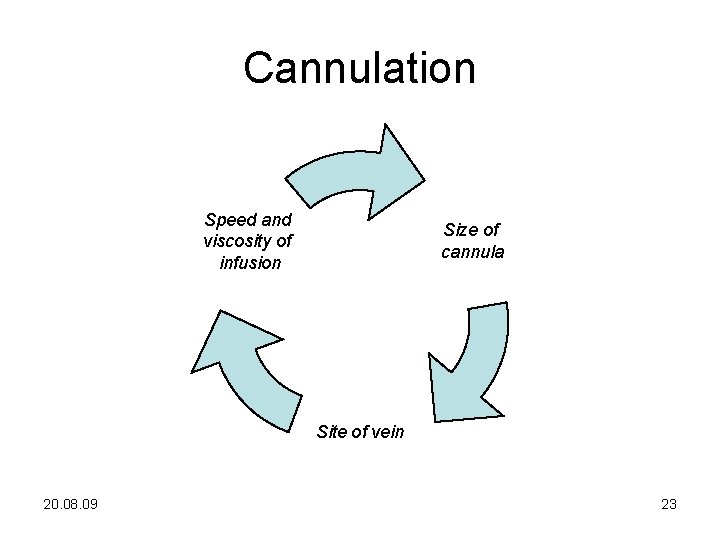
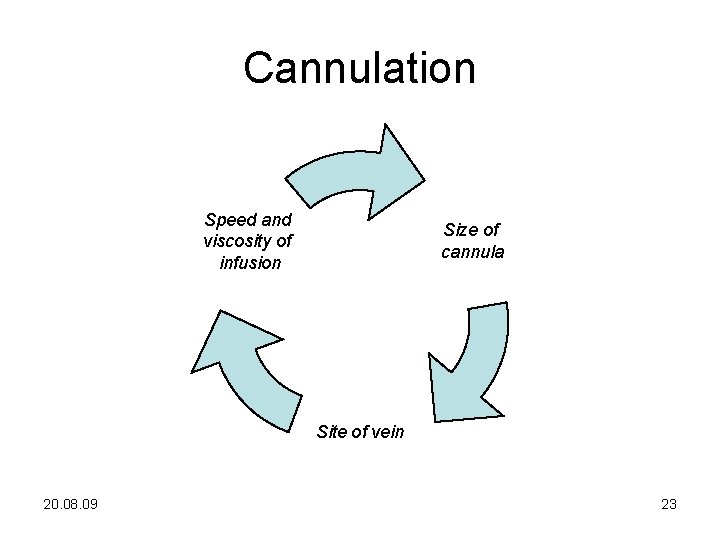
Cannulation Speed and viscosity of infusion Size of cannula Site of vein 20. 08. 09 23
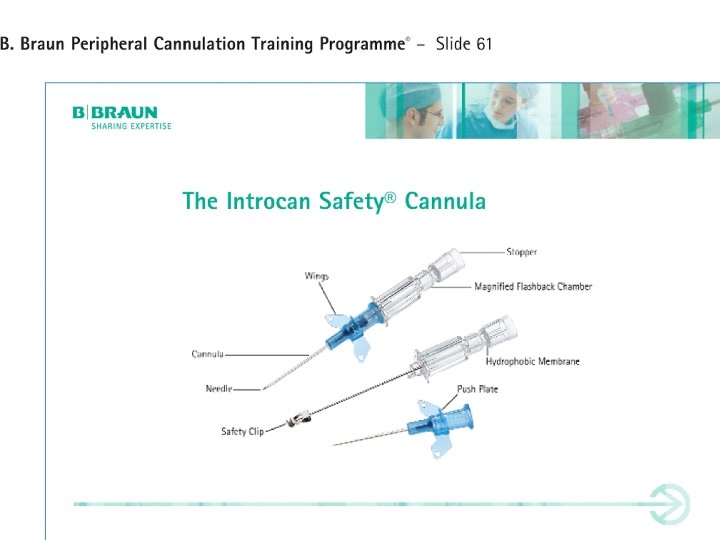
20. 08. 09 24
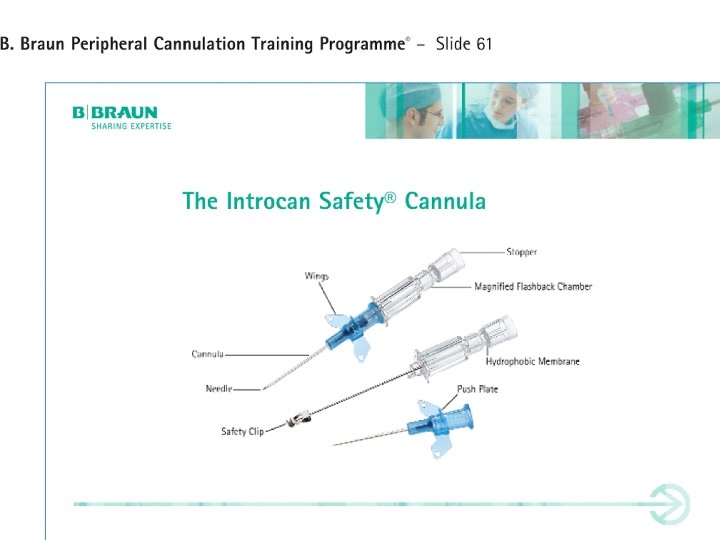
20. 08. 09 25
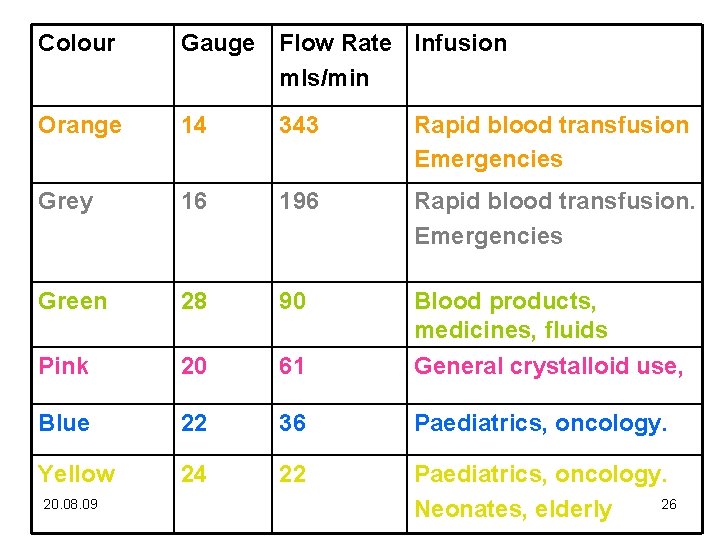
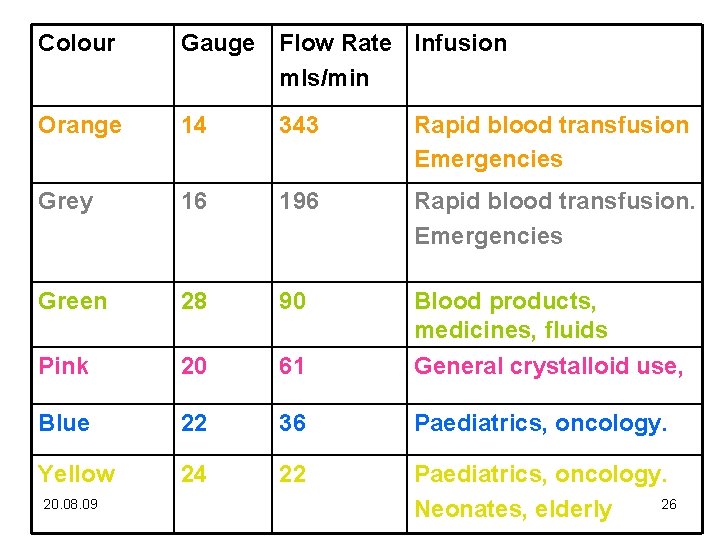
Colour Gauge Flow Rate Infusion mls/min Orange 14 343 Rapid blood transfusion Emergencies Grey 16 196 Rapid blood transfusion. Emergencies Green 28 90 Pink 20 61 Blood products, medicines, fluids General crystalloid use, Blue 22 36 Paediatrics, oncology. Yellow 24 22 Paediatrics, oncology. 26 Neonates, elderly 20. 08. 09
20. 08. 09 27
20. 08. 09 28
Complications Missed vein Haematoma Transfixation Phlebitis Blockage of cannula Needlestick injury Infection 20. 08. 09 Cannula embolism Pulmonary embolism Damage to surrounding nerves Arterial puncture Catheter fracture Thromboembolism 29
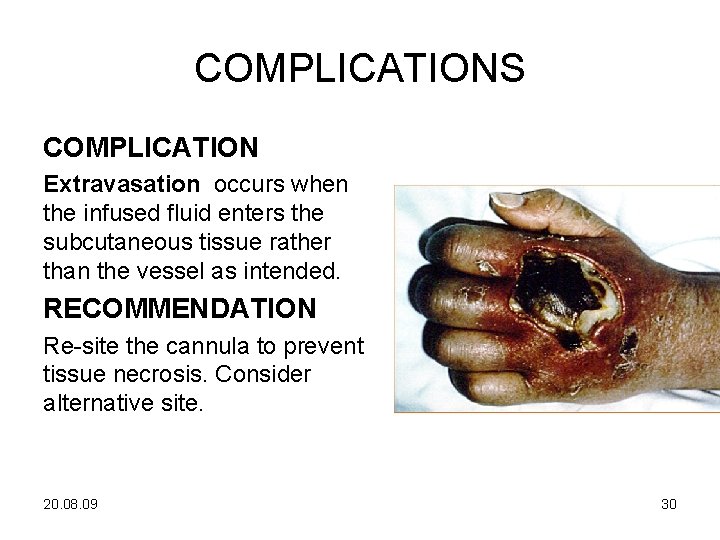
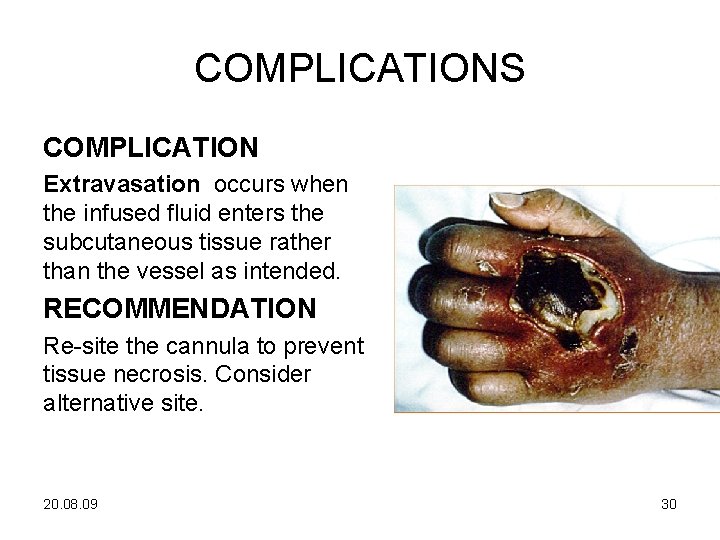
COMPLICATIONS COMPLICATION Extravasation occurs when the infused fluid enters the subcutaneous tissue rather than the vessel as intended. RECOMMENDATION Re-site the cannula to prevent tissue necrosis. Consider alternative site. 20. 08. 09 30
Infiltration / Extravasation • Infiltration occurs when - a non vesicant medication/solution leaks into the subcutaneous tissue. • Extravasation occurs when – a vesicant medication/solution leaks into the subcutaneous tissue. • NB – Vesicant – any substance that causes blistering or tissue necrosis and requires management to limit tissue damage 20. 08. 09 31
Managing extravasation • • • Stop infusion at once Withdraw drug Leave cannula insitu Elevate limb to reduce oedema Apply hot/cold pack Subsequent management depends upon drug involved and degree of damage. Maybe local extravasation policy i. e. use of antidote. 20. 08. 09 32
Preventing complications • • Ensure staff are trained and supervised Supervised practice and competence assessed Practice continually updated Ensure correct preparation of patient, equipment and environment • Aseptic non touch technique • Managed aftercare • Documentation 20. 08. 09 33
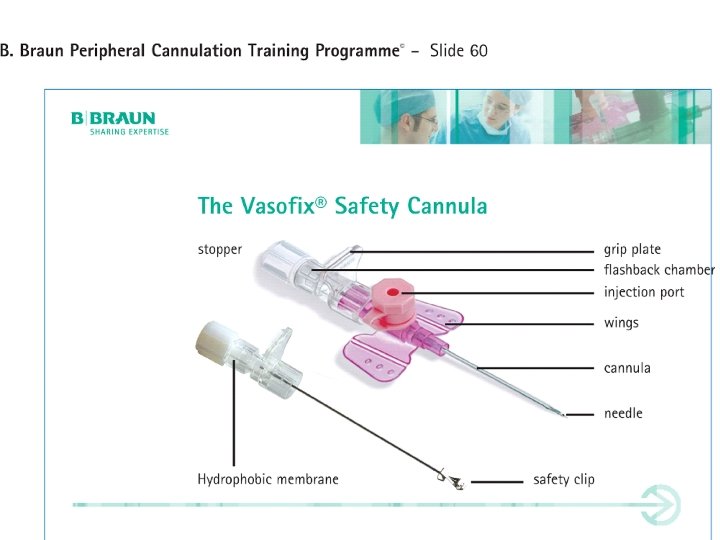
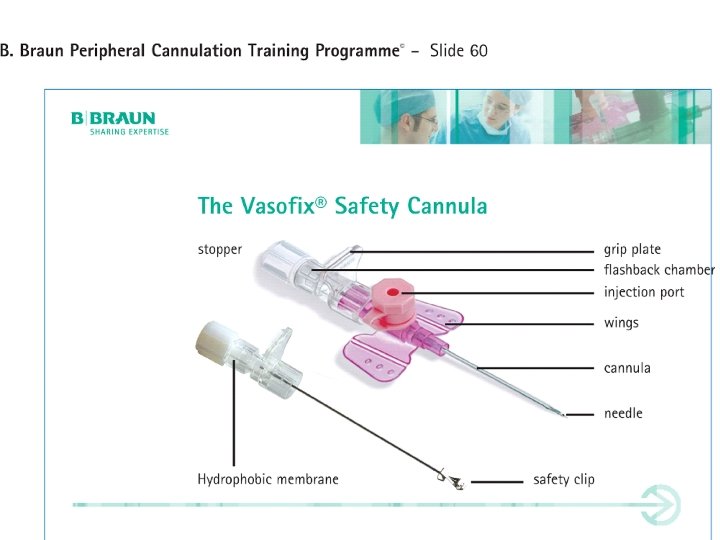
Documentation • • Venepuncture Which bloods taken Site Adverse events 20. 08. 09 • Cannulation • Type and gauge – Vasofix 22 g • Site – left hand • Date/time of insertion • Dressing must be labelled with date, time & initials • Number and location of attempts • Name of person inserting Cannula 34
Aftercare • Patient education • Asepsis for all cannula manipulations such as medicine administration and dressing changes. • Avoid over manipulation of cannula by using needle free devices. • Secure connections. • Regular monitoring and flushing • Planned removal of cannula 20. 08. 09 35
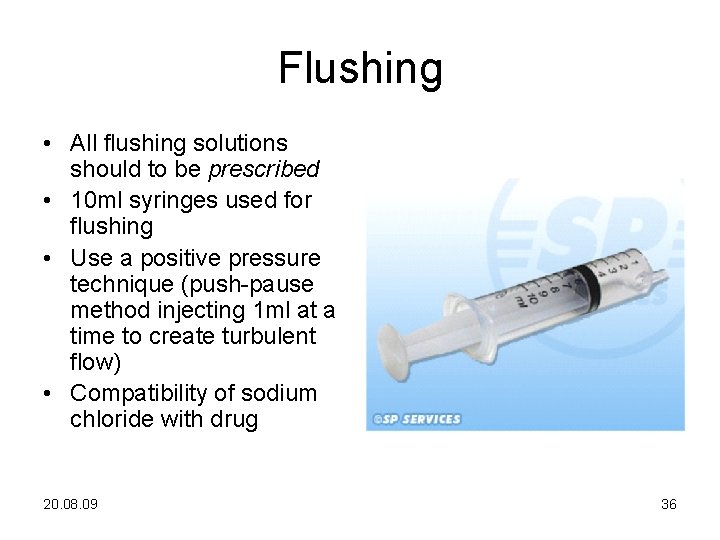
Flushing • All flushing solutions should to be prescribed • 10 ml syringes used for flushing • Use a positive pressure technique (push-pause method injecting 1 ml at a time to create turbulent flow) • Compatibility of sodium chloride with drug 20. 08. 09 36