Vasoactive drugs Ian Lyons Senior Clinical Fellow Critical
![Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-5.jpg)
![Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-6.jpg)
![Vasopressors DO 2 =CO{(1. 34 x [Hb] x Sp. O 2 ) + (Pa. Vasopressors DO 2 =CO{(1. 34 x [Hb] x Sp. O 2 ) + (Pa.](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-7.jpg)



![Distributive shock DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) + Distributive shock DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) +](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-39.jpg)

![Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-63.jpg)


- Slides: 107
Vasoactive drugs Ian Lyons, Senior Clinical Fellow, Critical Care October 2017
Overview � The science bit…. � Practicalities �A case
The science bit…. � Basic science � Systemic circulation ◦ Pressors ◦ Dilators ◦ Drugs affecting cardiac output � Pulmonary ◦ Dilators ◦ Hypoxia circulation
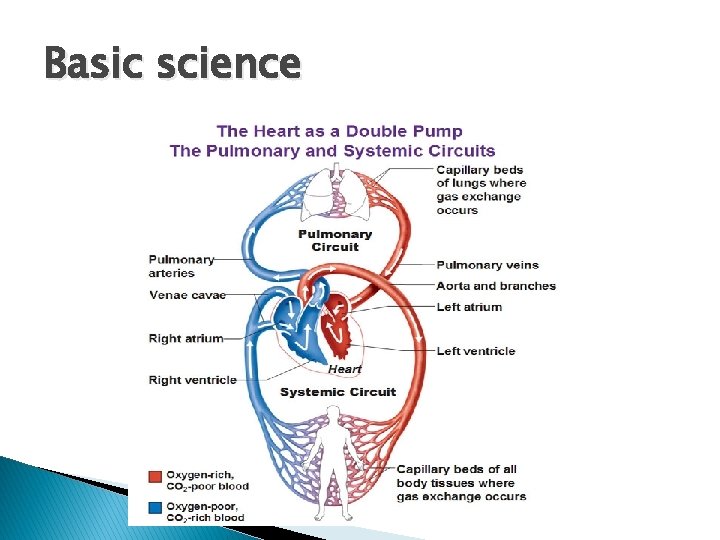
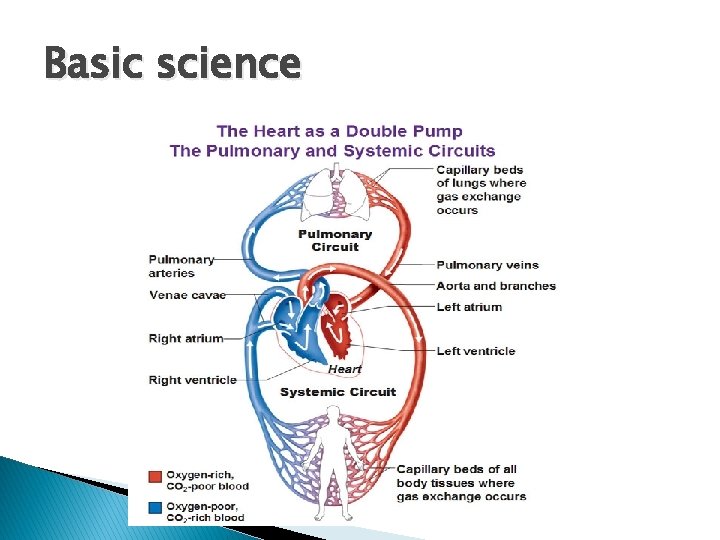
Basic science
![Maintaining delivery of oxygen DO 2 CO1 34 x Hb x Sp O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-5.jpg)
Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) + (Pa. O 2 x 0. 023)]
![Maintaining delivery of oxygen DO 2 CO1 34 x Hb x Sp O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-6.jpg)
Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) + (Pa. O 2 x 0. 023)] BP = CO x SVR
![Vasopressors DO 2 CO1 34 x Hb x Sp O 2 Pa Vasopressors DO 2 =CO{(1. 34 x [Hb] x Sp. O 2 ) + (Pa.](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-7.jpg)
Vasopressors DO 2 =CO{(1. 34 x [Hb] x Sp. O 2 ) + (Pa. O 2 x 0. 023)} BP = CO x SVR
‘Basically it modulates the intracellular calcium levels……’


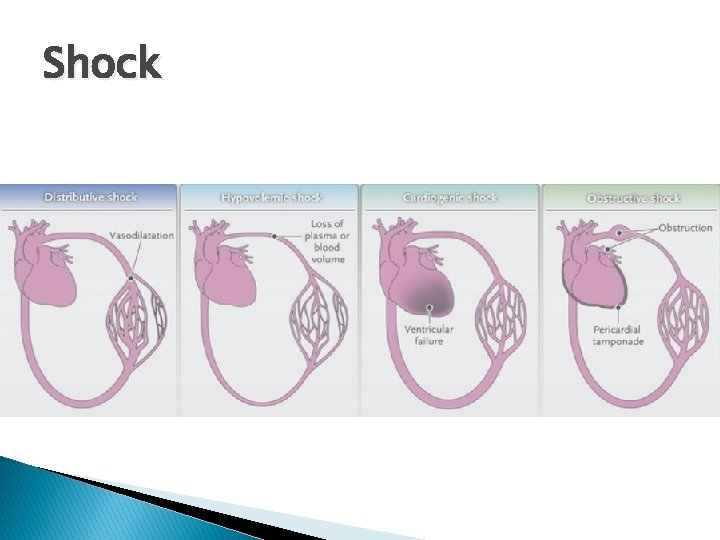
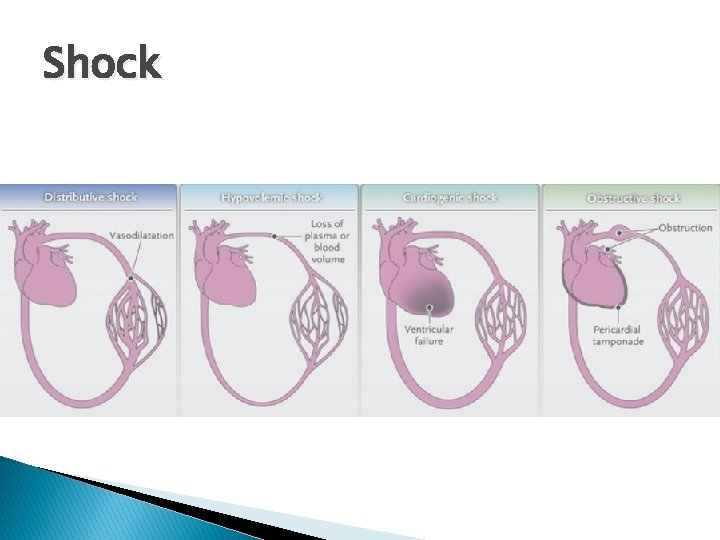
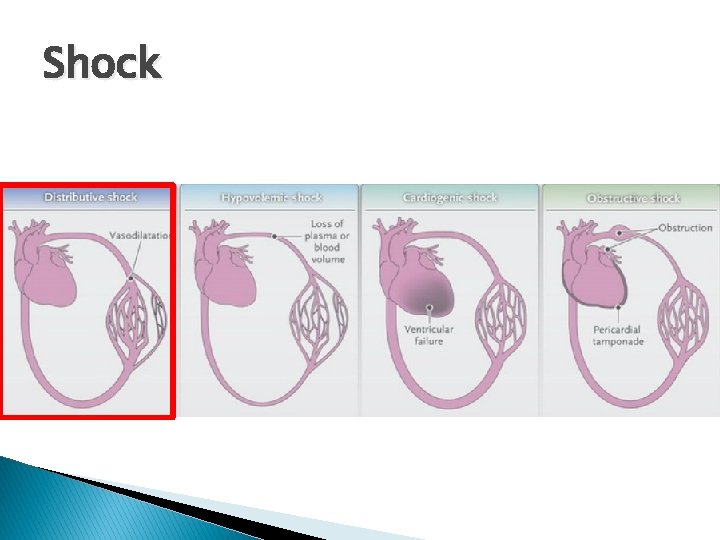
Shock
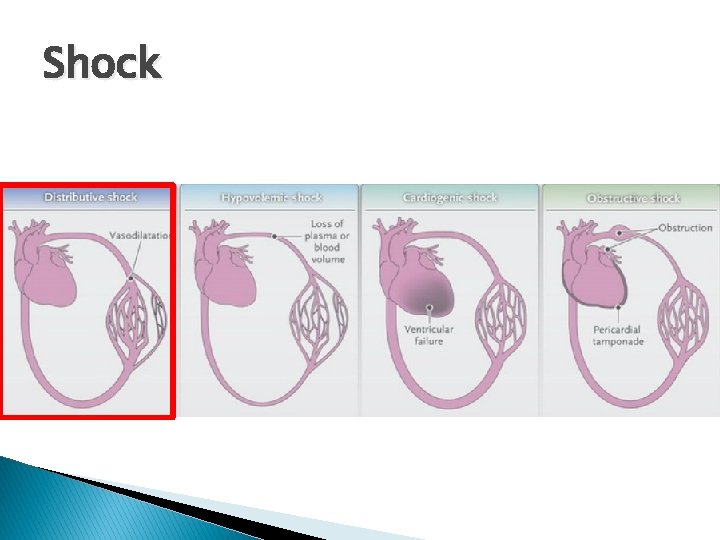
Shock
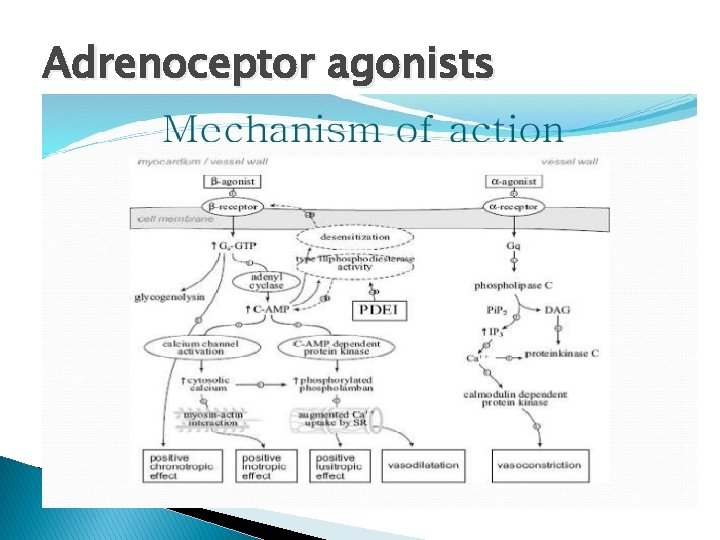
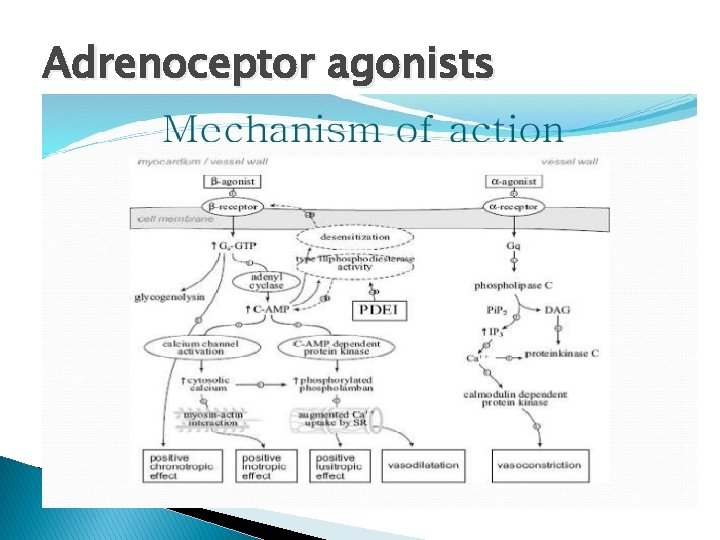
Adrenoceptor agonists
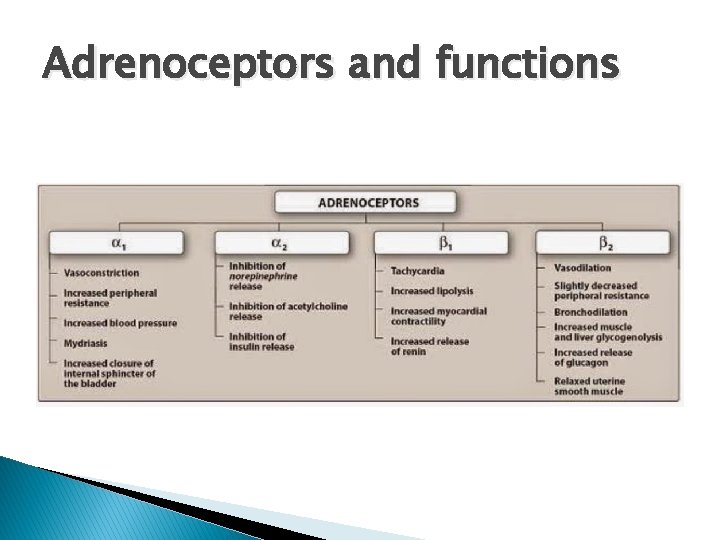
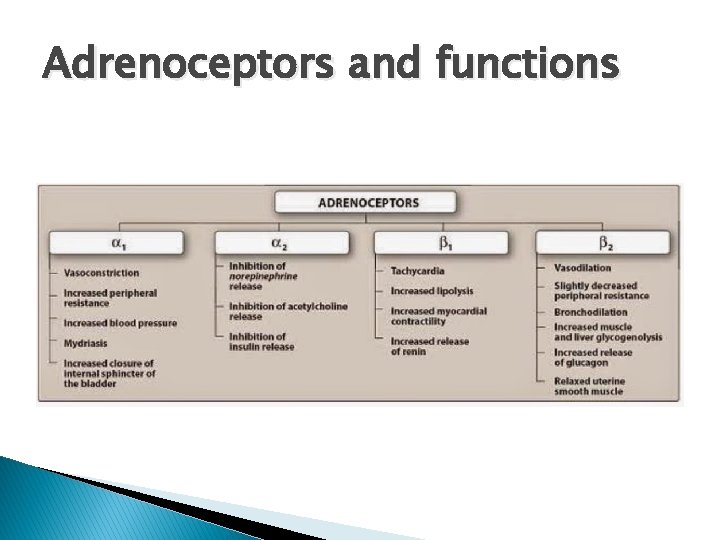
Adrenoceptors and functions
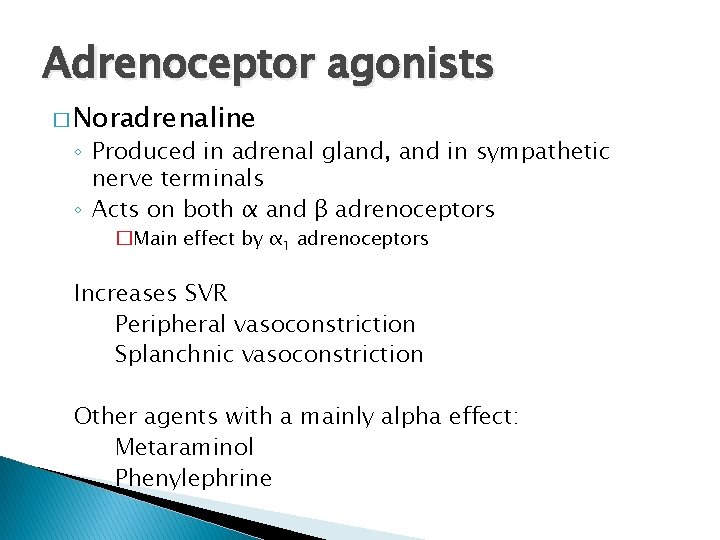
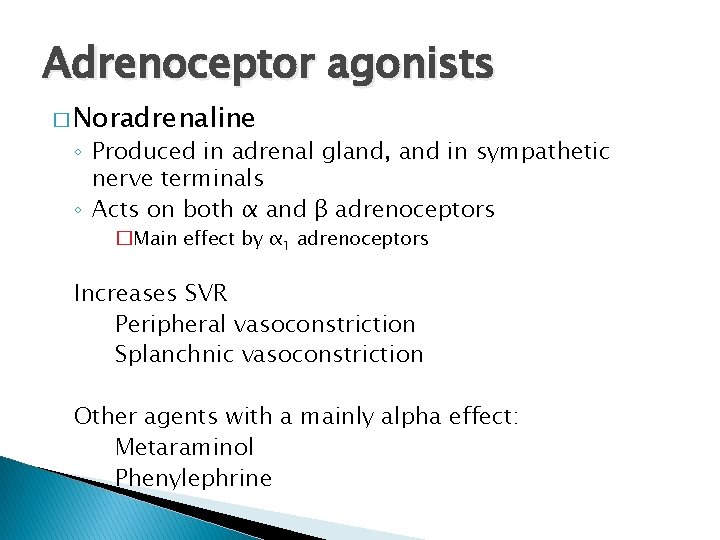
Adrenoceptor agonists � Noradrenaline ◦ Produced in adrenal gland, and in sympathetic nerve terminals ◦ Acts on both α and β adrenoceptors �Main effect by α 1 adrenoceptors Increases SVR Peripheral vasoconstriction Splanchnic vasoconstriction Other agents with a mainly alpha effect: Metaraminol Phenylephrine
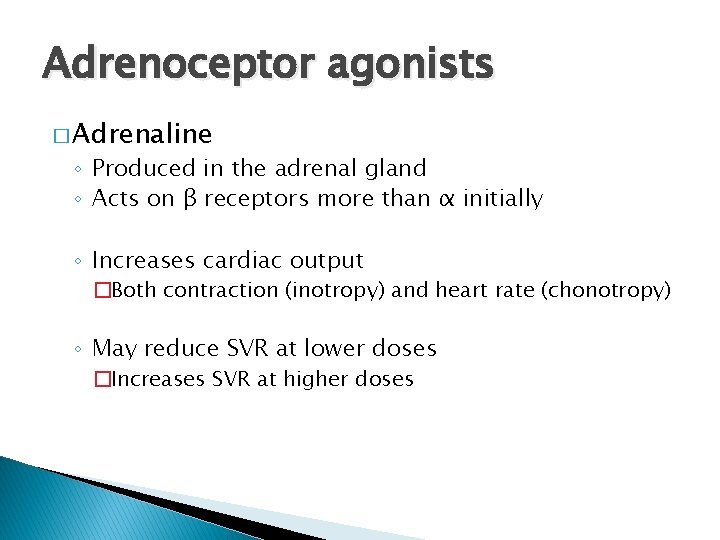
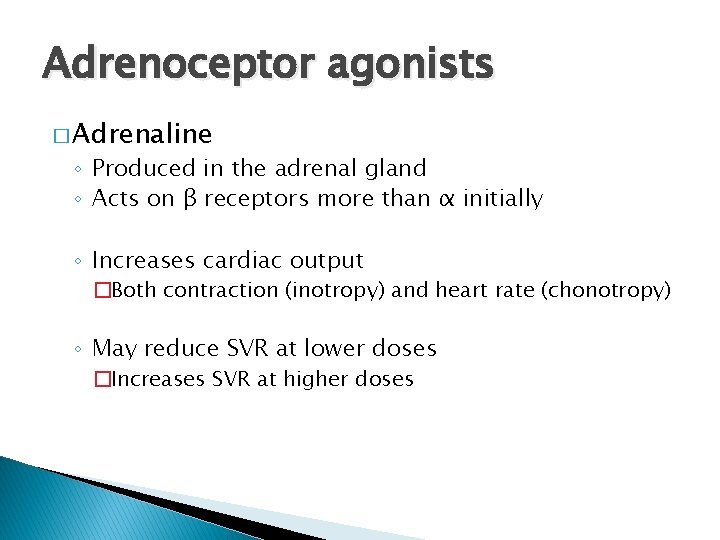
Adrenoceptor agonists � Adrenaline ◦ Produced in the adrenal gland ◦ Acts on β receptors more than α initially ◦ Increases cardiac output �Both contraction (inotropy) and heart rate (chonotropy) ◦ May reduce SVR at lower doses �Increases SVR at higher doses
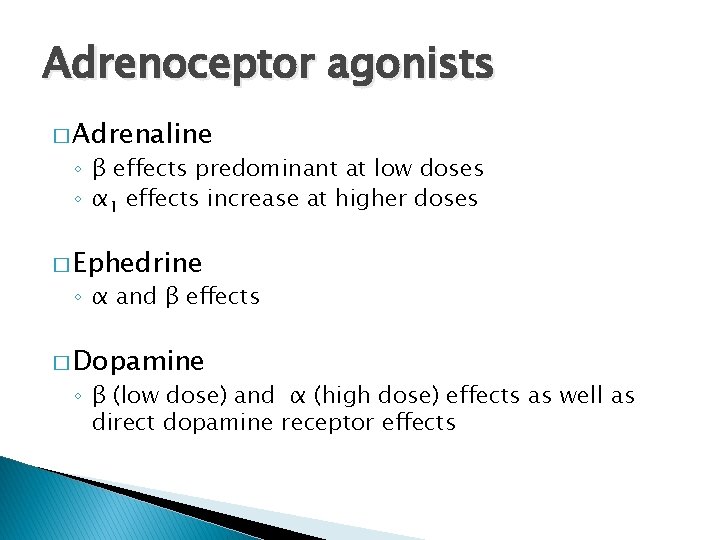
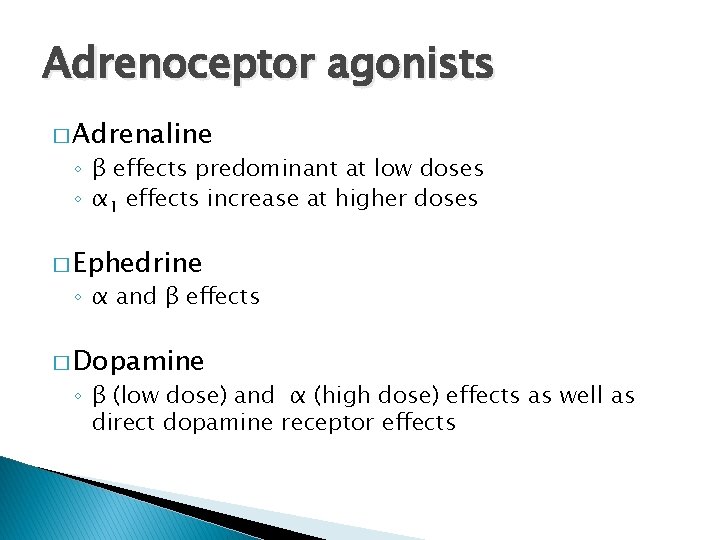
Adrenoceptor agonists � Adrenaline ◦ β effects predominant at low doses ◦ α 1 effects increase at higher doses � Ephedrine ◦ α and β effects � Dopamine ◦ β (low dose) and α (high dose) effects as well as direct dopamine receptor effects
Vasopressin � Antidiuretic � Potent hormone vasoconstrictor ◦ Doesn’t act on adrenoceptors � Can be effective when unresponsive to adrenoceptor agonists
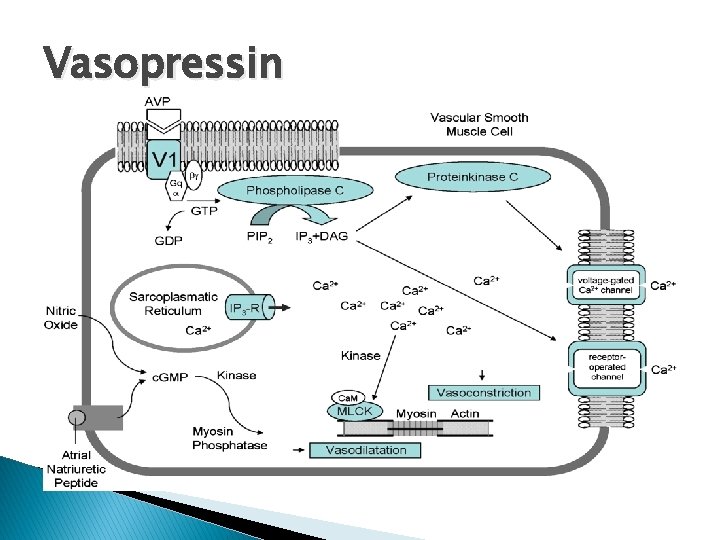
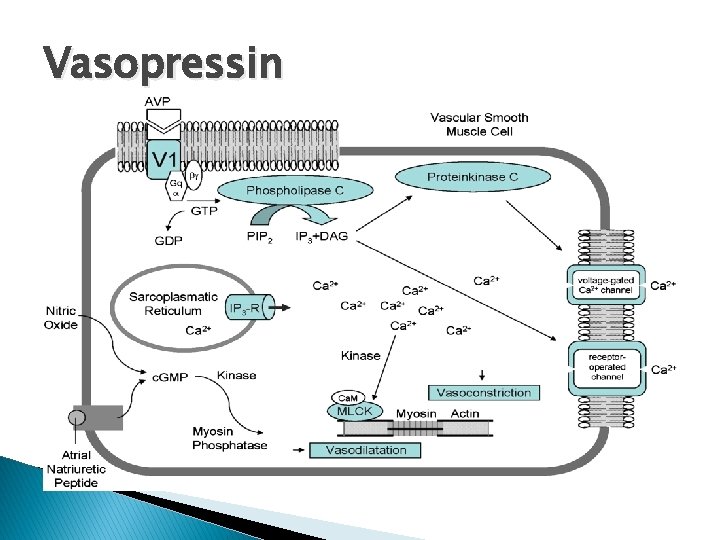
Vasopressin
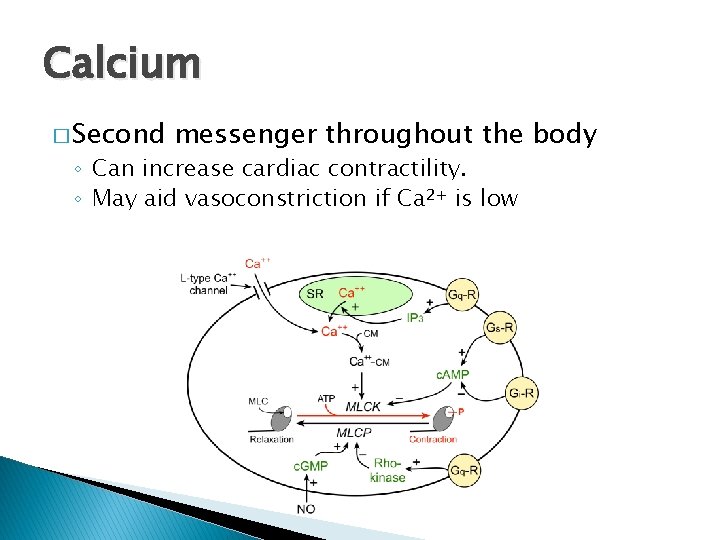
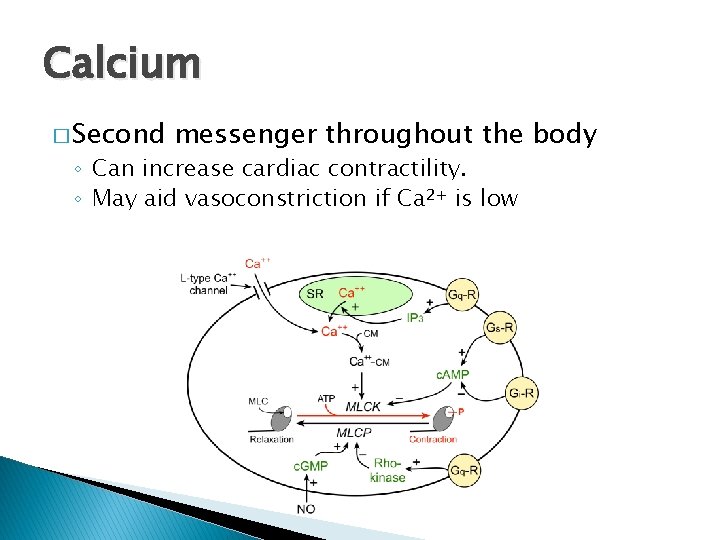
Calcium � Second messenger throughout the body ◦ Can increase cardiac contractility. ◦ May aid vasoconstriction if Ca 2+ is low
Vasodilators � Indications ◦ Hypertension ◦ Heart failure ◦ Angina ◦ Specific regions �Ischaemic limbs �Pulmonary hypertension
Vasodilators � Arterial � BP vs venous = CO x SVR
Anti-adrenergics �α blockers ◦ (e. g. Prazosin, Phentolamine, Phenoxybenzamine) BP = CO x SVR �β blockers (e. g. Labetalol, Bisoprolol, Esmolol)
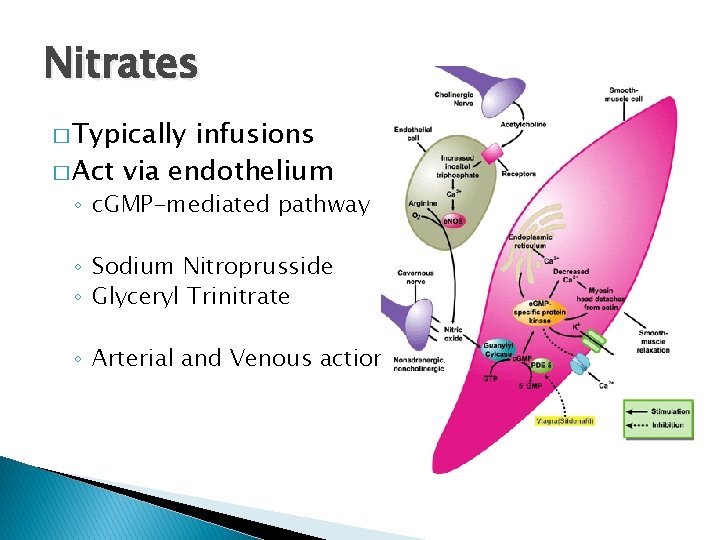
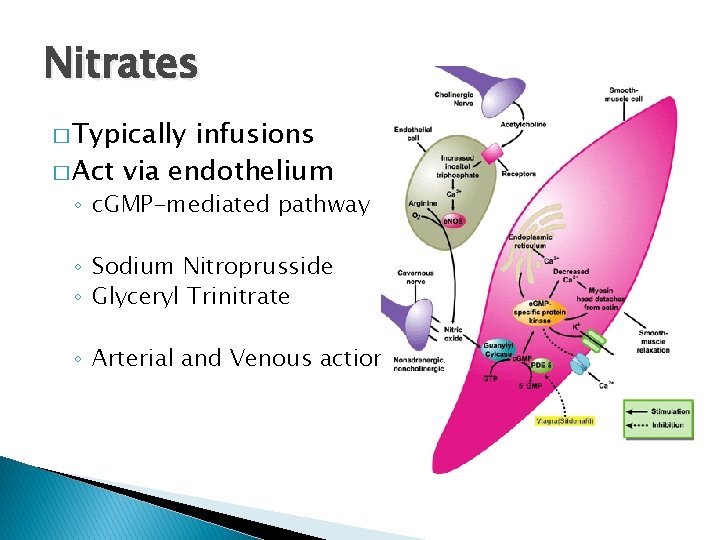
Nitrates � Typically infusions � Act via endothelium ◦ c. GMP-mediated pathway ◦ Sodium Nitroprusside ◦ Glyceryl Trinitrate ◦ Arterial and Venous action
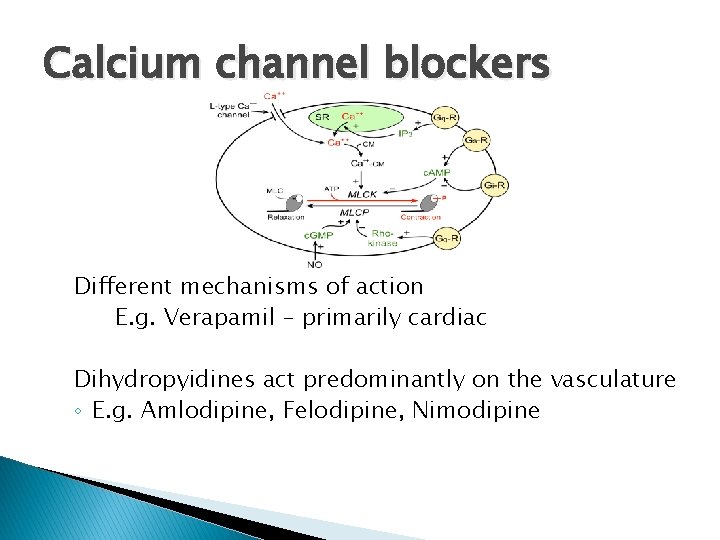
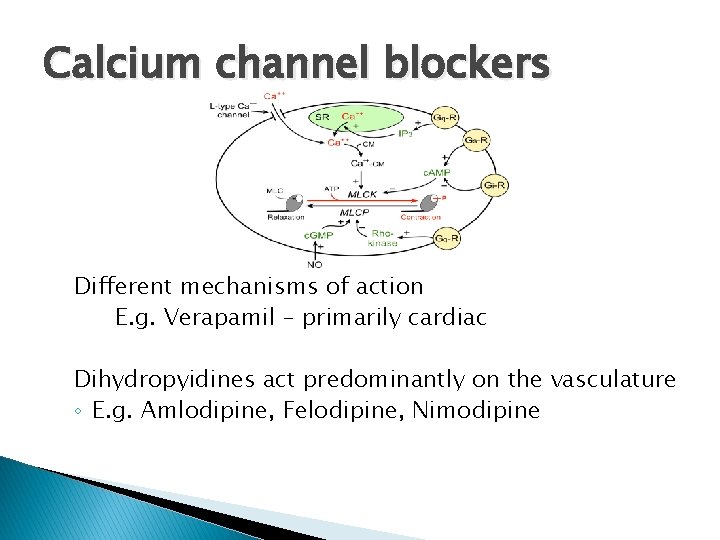
Calcium channel blockers Different mechanisms of action E. g. Verapamil – primarily cardiac Dihydropyidines act predominantly on the vasculature ◦ E. g. Amlodipine, Felodipine, Nimodipine
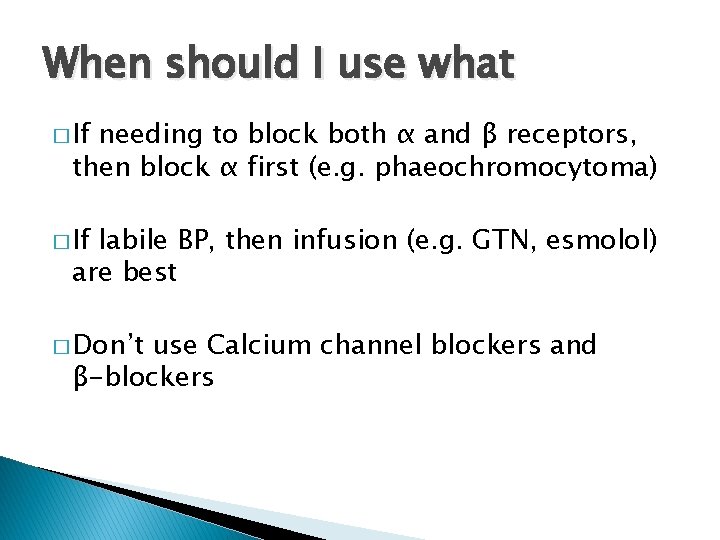
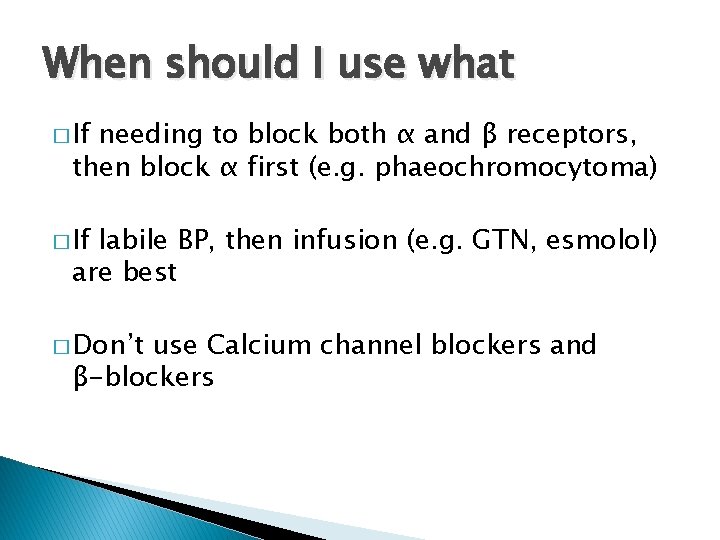
When should I use what � If needing to block both α and β receptors, then block α first (e. g. phaeochromocytoma) � If labile BP, then infusion (e. g. GTN, esmolol) are best � Don’t use Calcium channel blockers and β-blockers
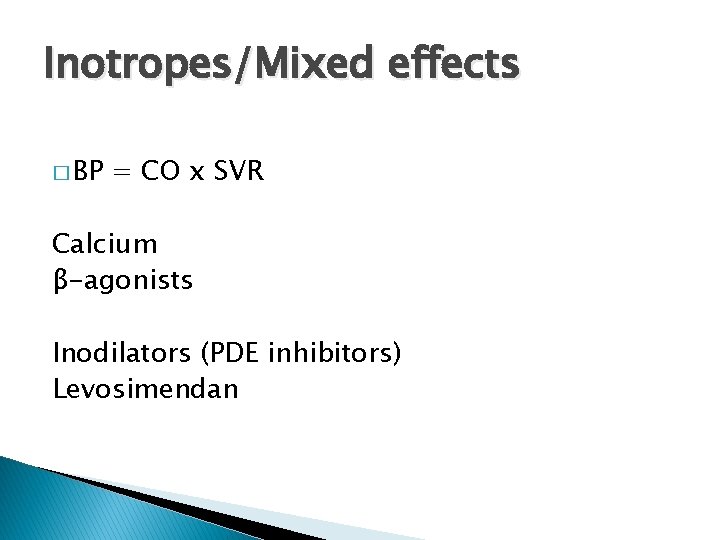
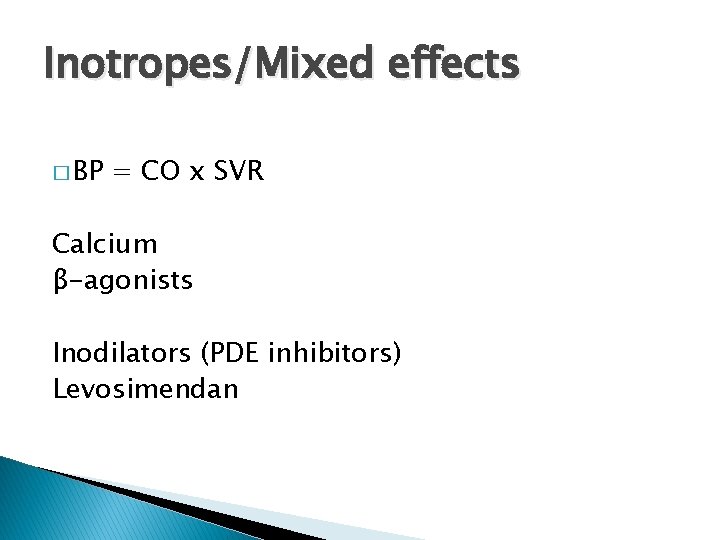
Inotropes/Mixed effects � BP = CO x SVR Calcium β-agonists Inodilators (PDE inhibitors) Levosimendan
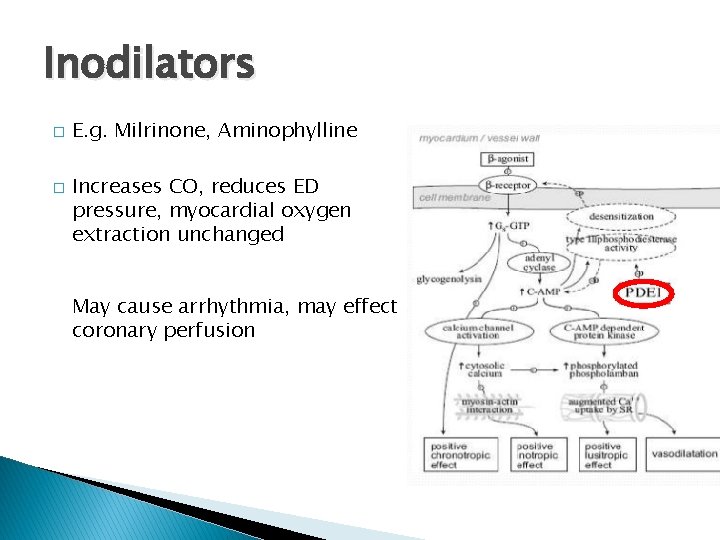
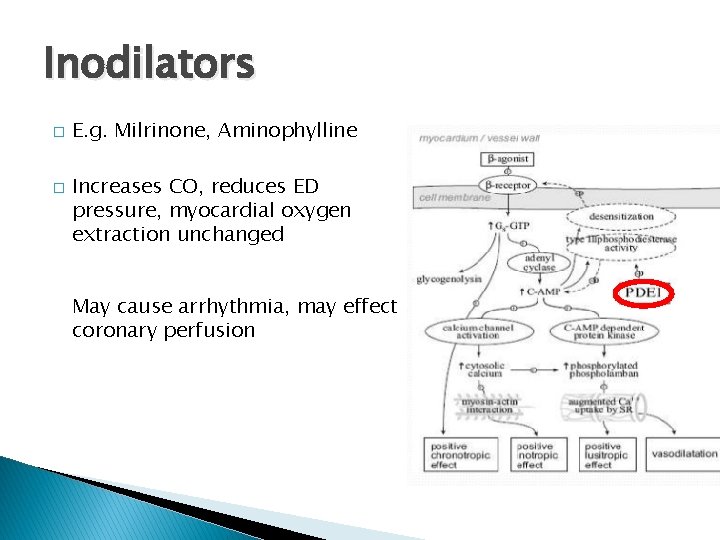
Inodilators � � E. g. Milrinone, Aminophylline Increases CO, reduces ED pressure, myocardial oxygen extraction unchanged May cause arrhythmia, may effect coronary perfusion
Levosimendan � Calcium sensitising agent ◦ Originally used for heart failure ◦ Currently being investigated in sepsis � Single � Trial infusion 7 days effect results suggest it’s not effective….
Pulmonary circulation p. BP = CO x PVR
Pulmonary hypertension � Characterised pressure by high pulmonary artery ◦ Variety of causes � Pulmonary hypertension ◦ Many different causes �Require investigation at specialist centre (Sheffield) ◦ Less production of NO and Prostacyclin

The same approach – different drugs � Prostanoids � PDE (Iloprost) V – Inhibitors (Sildenafil) � Endothelin antagonists (Bosentan)
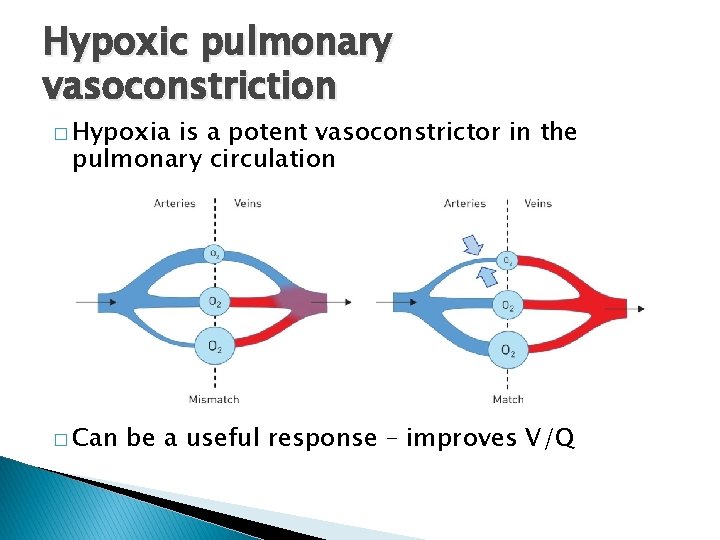
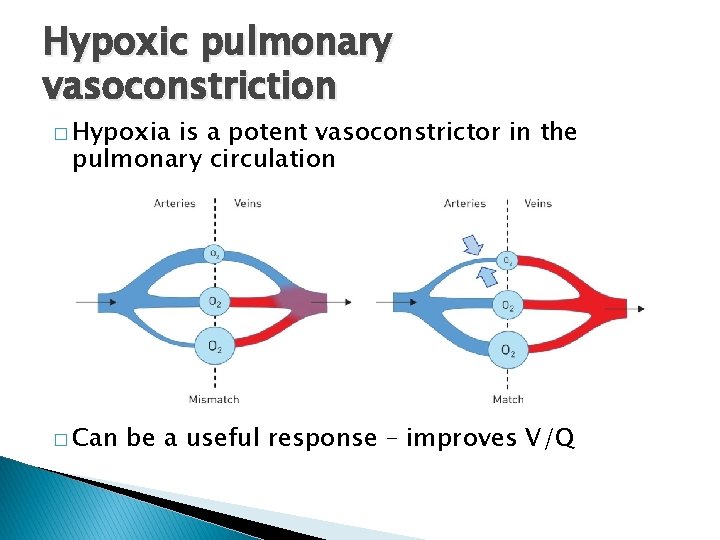
Hypoxic pulmonary vasoconstriction � Hypoxia is a potent vasoconstrictor in the pulmonary circulation � Can be a useful response – improves V/Q
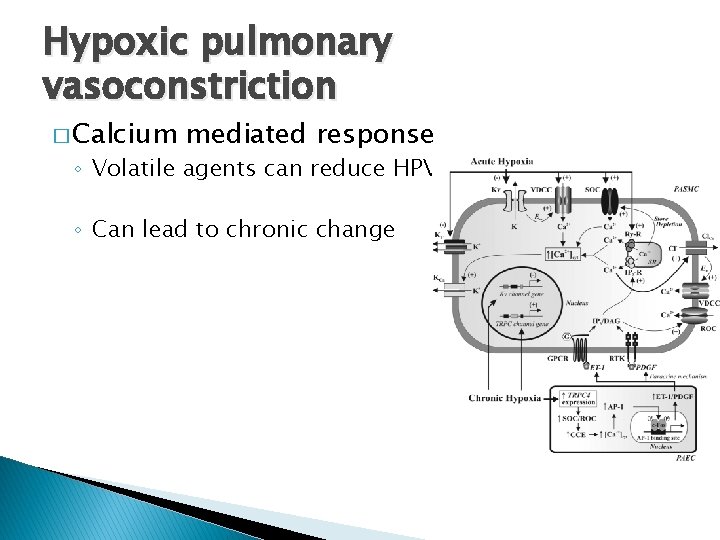
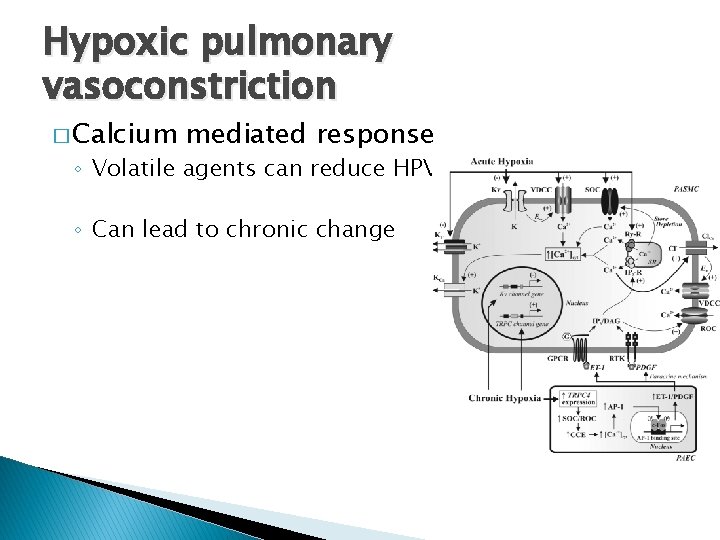
Hypoxic pulmonary vasoconstriction � Calcium mediated response ◦ Volatile agents can reduce HPV ◦ Can lead to chronic change
Summary � Most vasoactive drugs act to directly or indirectly alter calcium �A variety of different receptors – usually GPCR � Many drugs have both vasoactive and inotropic effects � Pulmonary and systemic circulations respond to different drugs. .
Practicalities……
Practicalities � Treat the right thing… � When and which one should I start? � How much is too much? � Starting � What adjuncts and other drugs else should I do…
![Distributive shock DO 2 CO1 34 x Hb x Sp O 2 Distributive shock DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) +](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-39.jpg)
Distributive shock DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) + (Pa. O 2 x 0. 023)] BP = CO x SVR
Distributive shock � Causes: ◦ ◦ ◦ Sepsis Burns Pancreatitis Anaphylaxis CNS (spinal injury) Adrenal insufficiency
Distributive shock � Fix ◦ ◦ ◦ the underlying problem Sepsis – Source control Burns – Burns management + grafting Pancreatitis – Organ support +/- intervention Anaphylaxis – Specific management CNS (spinal injury) – Sheffield protocol Adrenal insufficiency - Steroids
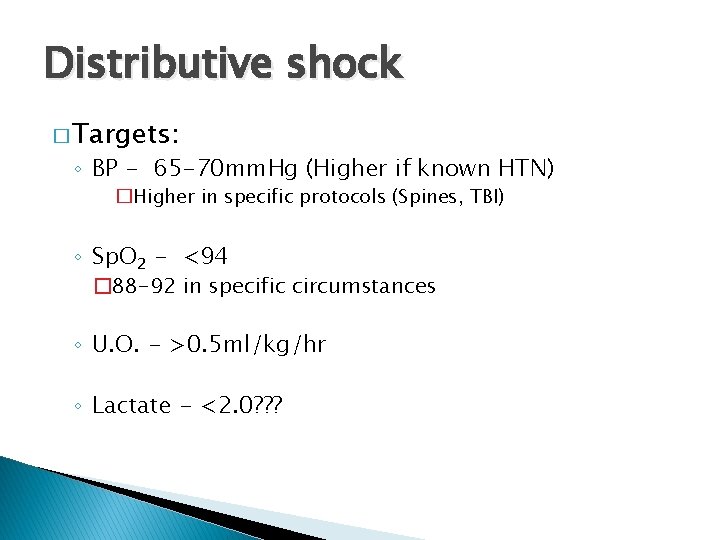
Distributive shock � Targets: ◦ BP ◦ Sp. O 2 ◦ U. O. ◦ Lactate
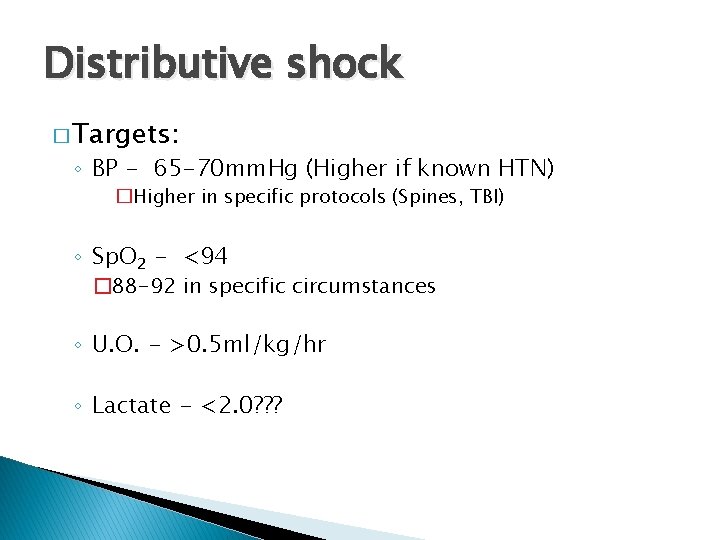
Distributive shock � Targets: ◦ BP - 65 -70 mm. Hg (Higher if known HTN) �Higher in specific protocols (Spines, TBI) ◦ Sp. O 2 - <94 � 88 -92 in specific circumstances ◦ U. O. - >0. 5 ml/kg/hr ◦ Lactate - <2. 0? ? ?
Distributive shock � When should I start something?
Distributive shock � When should I start something? ◦ Adequately fluid resuscitated? ◦ Signs of inadequate end organ perfusion? ◦ Low BP?
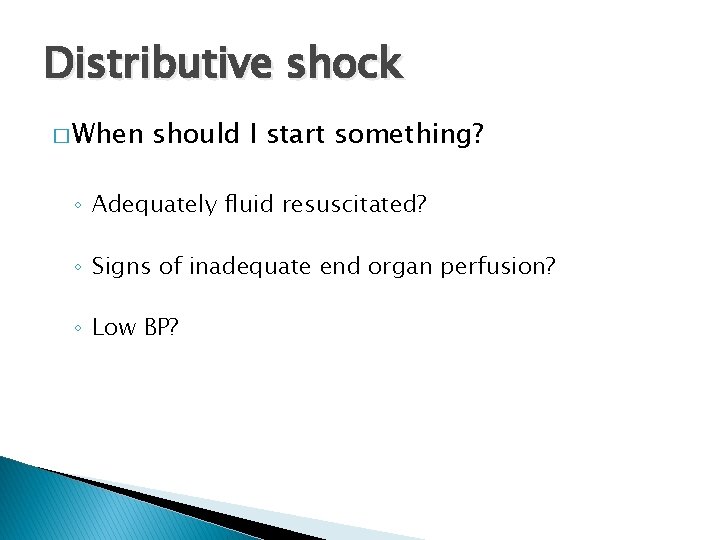
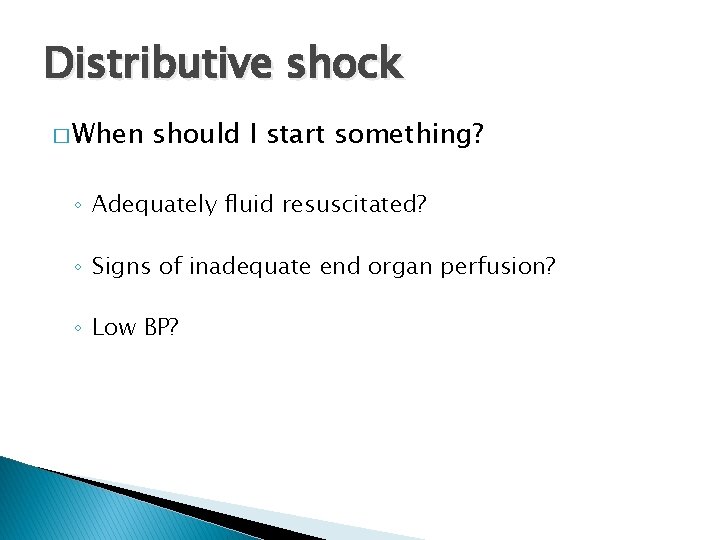
Distributive shock � What to start? BP = CO x SVR

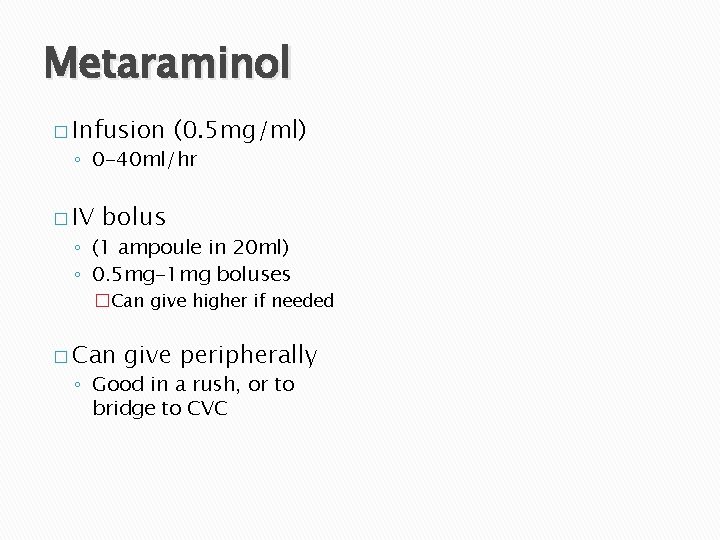
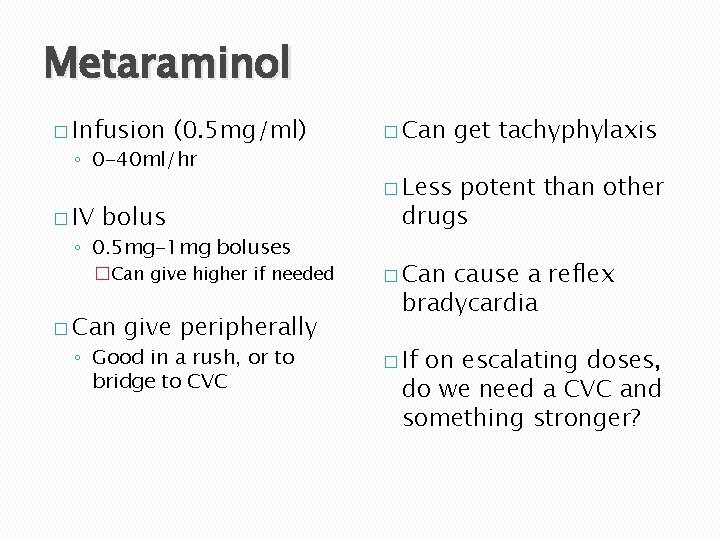
Metaraminol
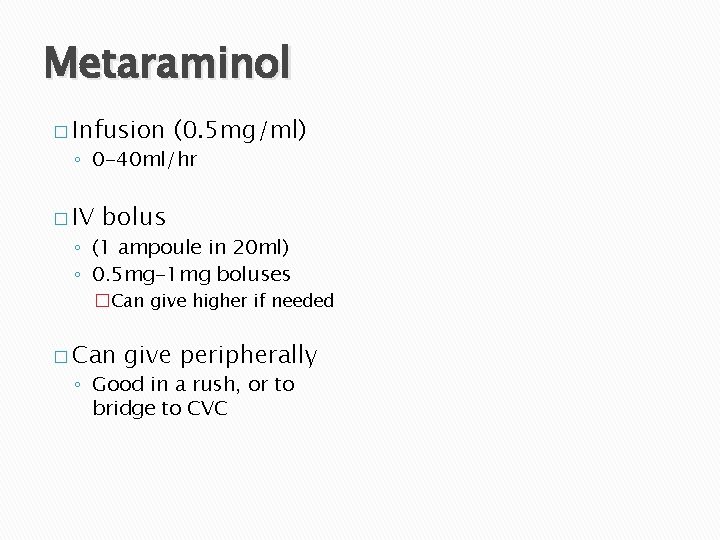
Metaraminol � Infusion (0. 5 mg/ml) ◦ 0 -40 ml/hr � IV bolus ◦ (1 ampoule in 20 ml) ◦ 0. 5 mg-1 mg boluses �Can give higher if needed � Can give peripherally ◦ Good in a rush, or to bridge to CVC
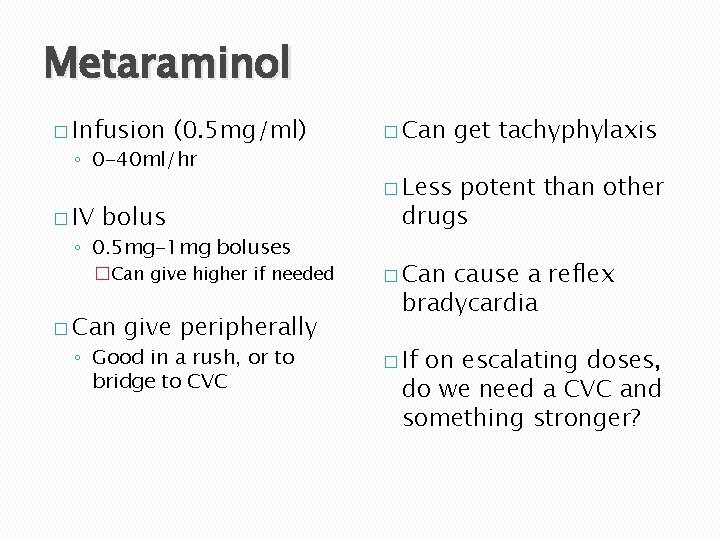
Metaraminol � Infusion (0. 5 mg/ml) ◦ 0 -40 ml/hr � IV bolus ◦ 0. 5 mg-1 mg boluses �Can give higher if needed � Can give peripherally ◦ Good in a rush, or to bridge to CVC � Can get tachyphylaxis � Less potent than other drugs � Can cause a reflex bradycardia � If on escalating doses, do we need a CVC and something stronger?
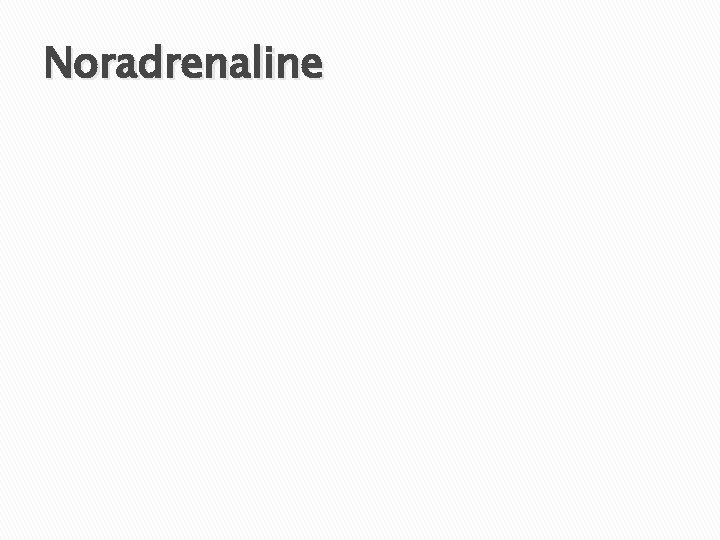
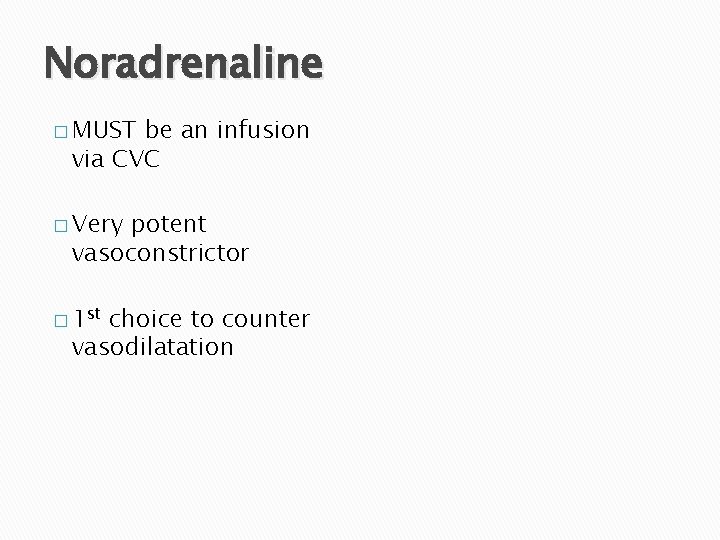
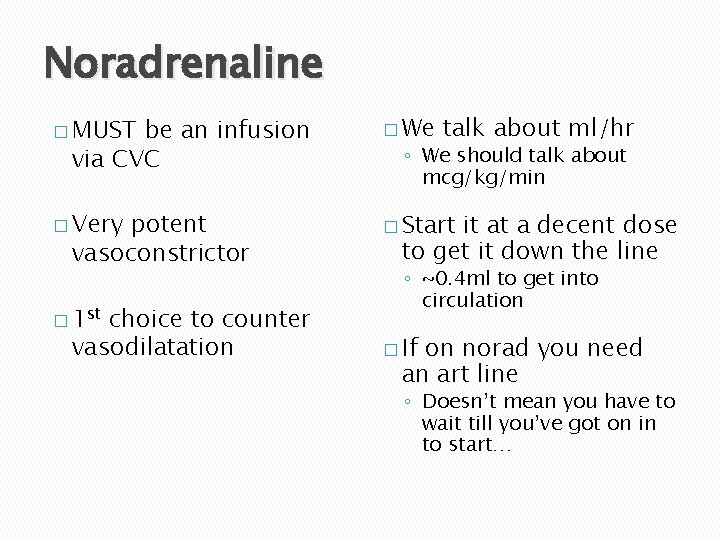
Noradrenaline
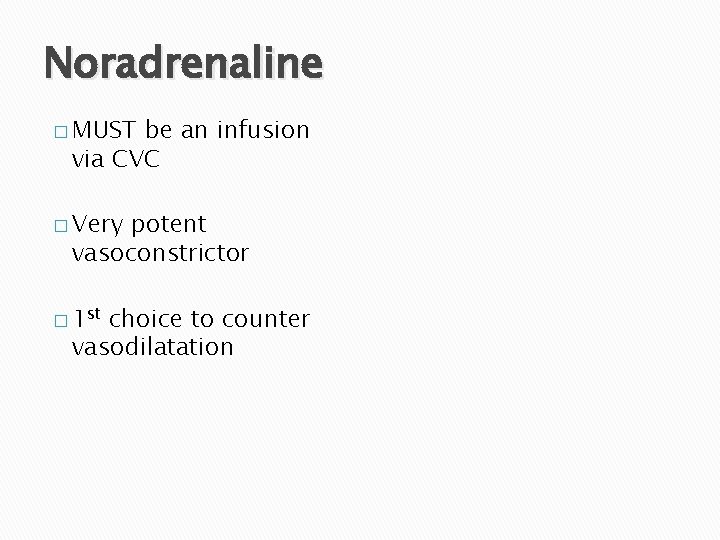
Noradrenaline � MUST be an infusion via CVC � Very potent vasoconstrictor � 1 st choice to counter vasodilatation
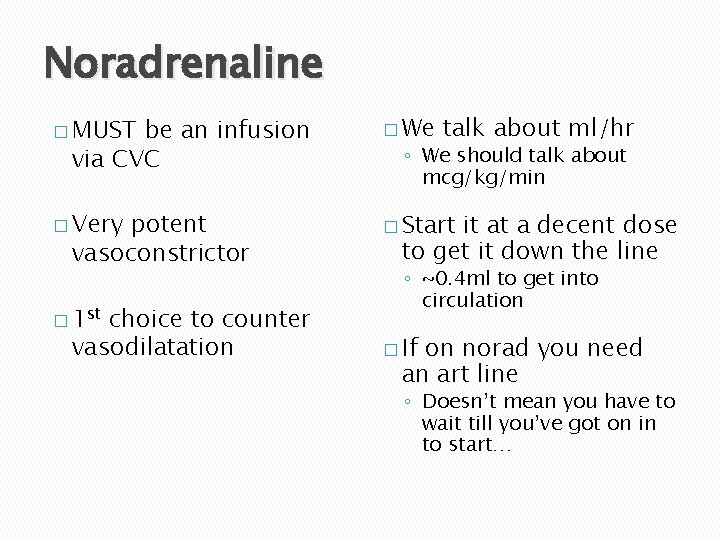
Noradrenaline � MUST � We � Very � Start be an infusion via CVC potent vasoconstrictor � 1 st choice to counter vasodilatation talk about ml/hr ◦ We should talk about mcg/kg/min it at a decent dose to get it down the line ◦ ~0. 4 ml to get into circulation � If on norad you need an art line ◦ Doesn’t mean you have to wait till you’ve got on in to start…
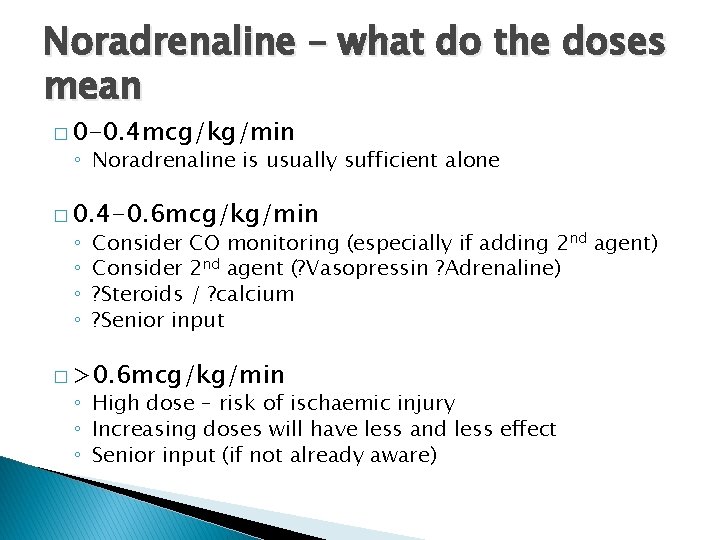
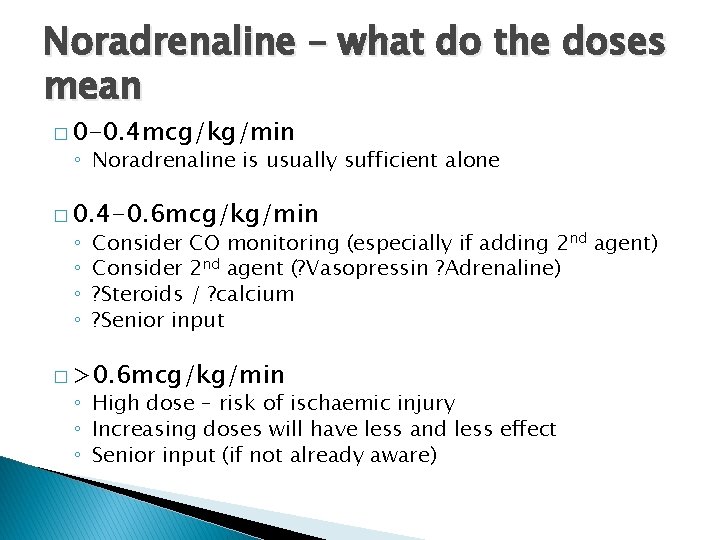
Noradrenaline – what do the doses mean � 0 -0. 4 mcg/kg/min ◦ Noradrenaline is usually sufficient alone � 0. 4 -0. 6 mcg/kg/min ◦ ◦ Consider CO monitoring (especially if adding 2 nd agent) Consider 2 nd agent (? Vasopressin ? Adrenaline) ? Steroids / ? calcium ? Senior input � >0. 6 mcg/kg/min ◦ High dose – risk of ischaemic injury ◦ Increasing doses will have less and less effect ◦ Senior input (if not already aware)
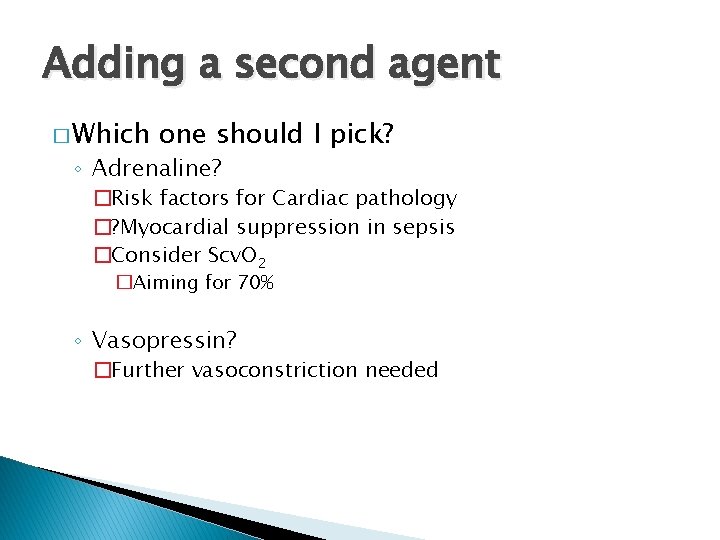
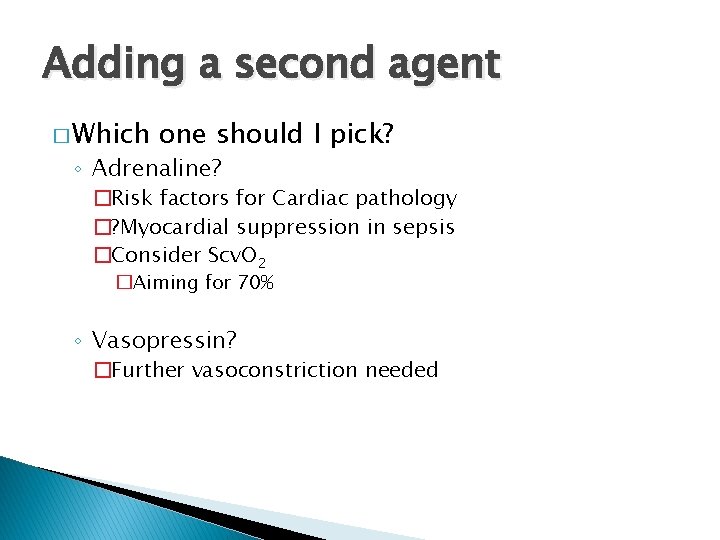
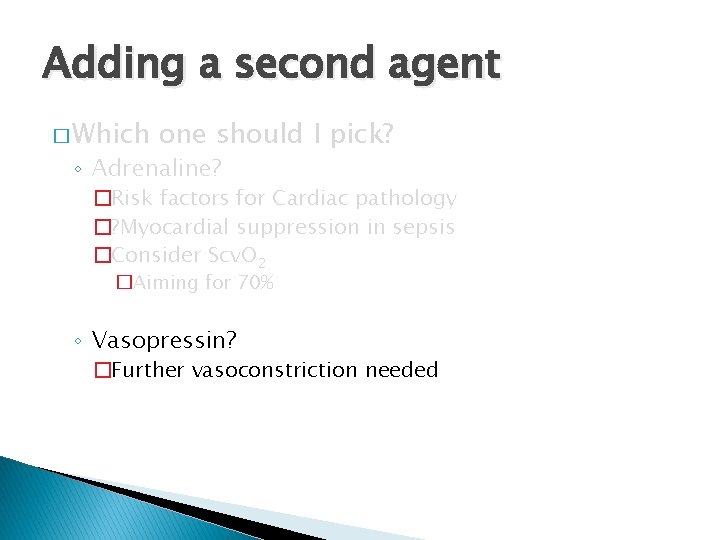
Adding a second agent � Which one should I pick? ◦ Adrenaline? �Risk factors for Cardiac pathology �? Myocardial suppression in sepsis �Consider Scv. O 2 �Aiming for 70% ◦ Vasopressin? �Further vasoconstriction needed
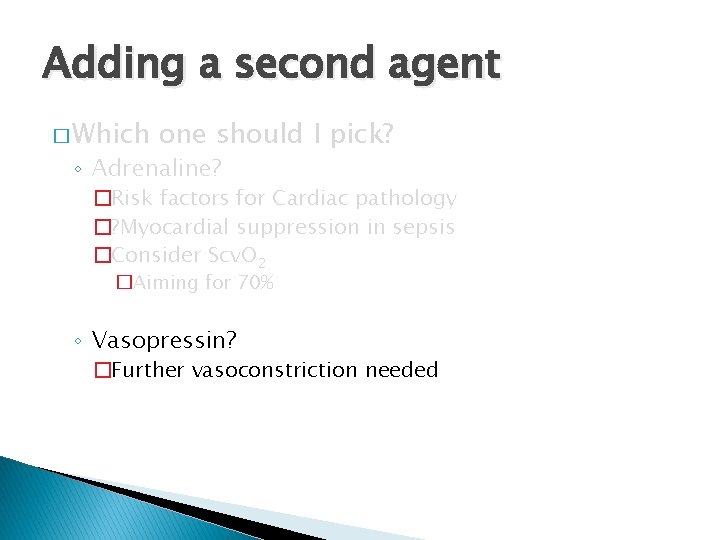
Adding a second agent � Which one should I pick? ◦ Adrenaline? �Risk factors for Cardiac pathology �? Myocardial suppression in sepsis �Consider Scv. O 2 �Aiming for 70% ◦ Vasopressin? �Further vasoconstriction needed
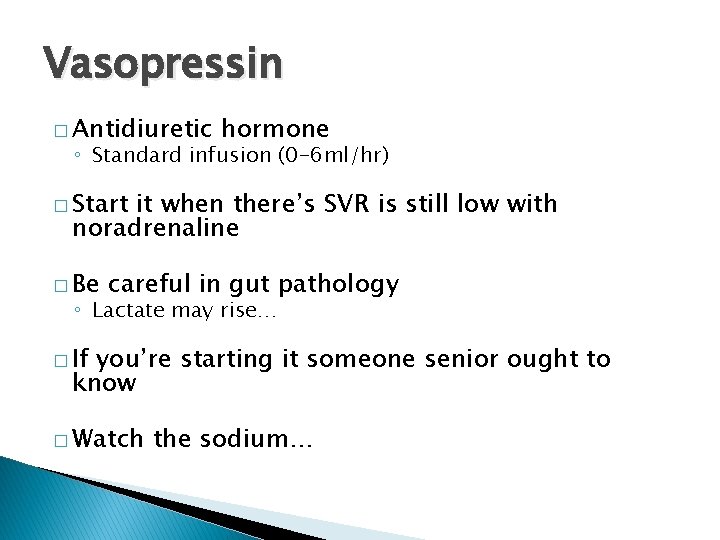
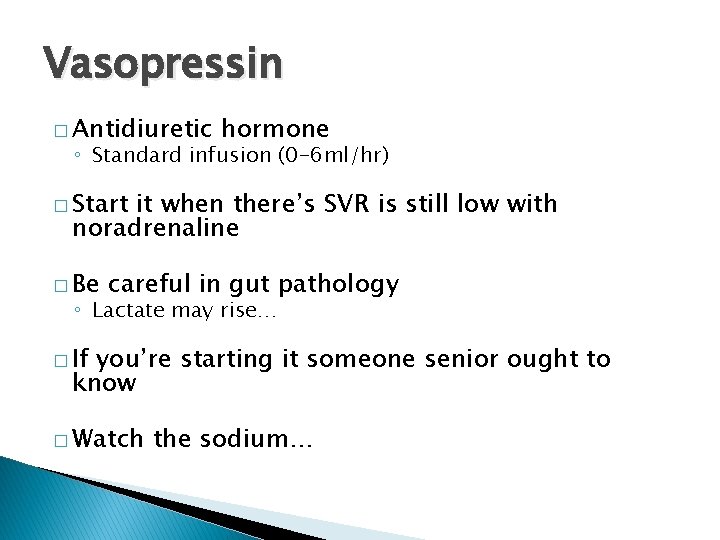
Vasopressin � Antidiuretic hormone ◦ Standard infusion (0 -6 ml/hr) � Start it when there’s SVR is still low with noradrenaline � Be careful in gut pathology ◦ Lactate may rise… � If you’re starting it someone senior ought to know � Watch the sodium…
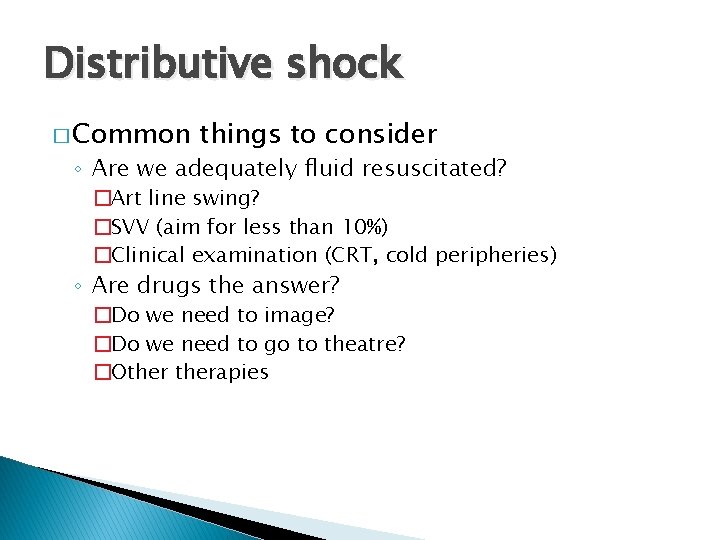
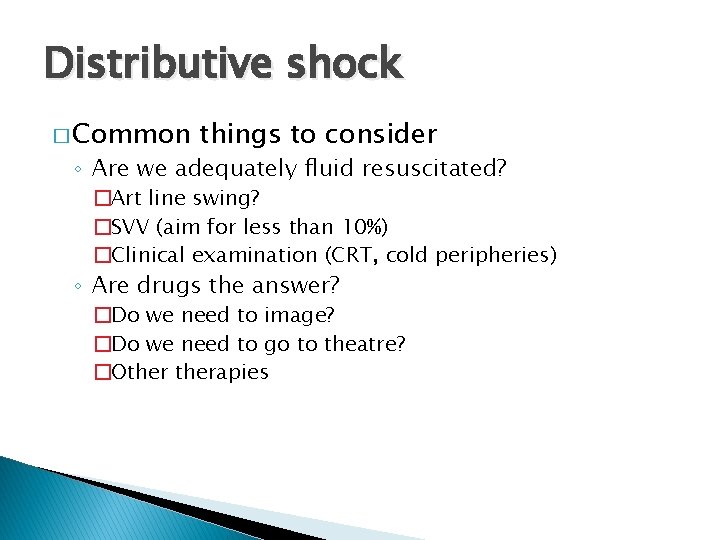
Distributive shock � Common things to consider ◦ Are we adequately fluid resuscitated? �Art line swing? �SVV (aim for less than 10%) �Clinical examination (CRT, cold peripheries) ◦ Are drugs the answer? �Do we need to image? �Do we need to go to theatre? �Otherapies
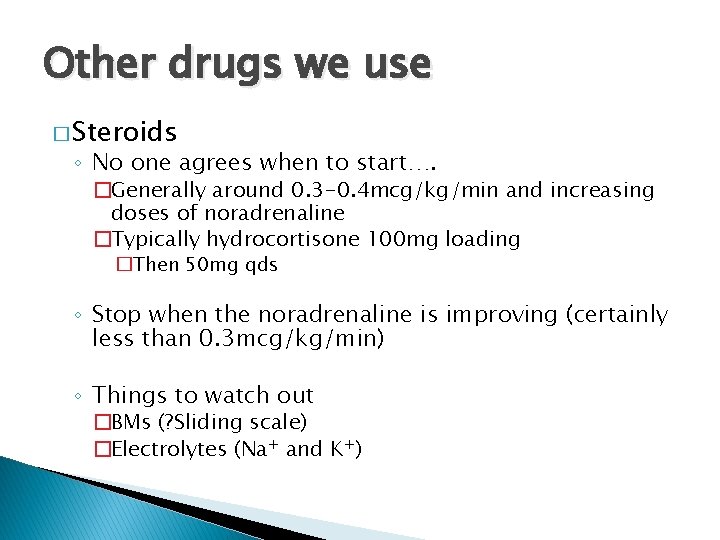
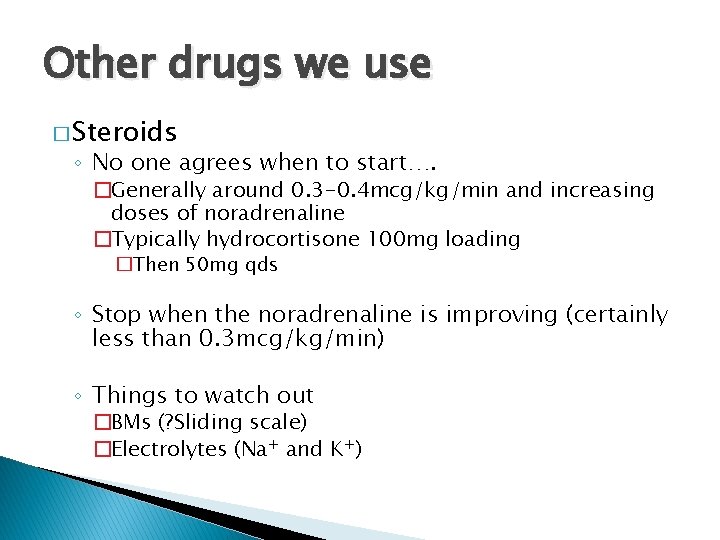
Other drugs we use � Steroids ◦ No one agrees when to start…. �Generally around 0. 3 -0. 4 mcg/kg/min and increasing doses of noradrenaline �Typically hydrocortisone 100 mg loading �Then 50 mg qds ◦ Stop when the noradrenaline is improving (certainly less than 0. 3 mcg/kg/min) ◦ Things to watch out �BMs (? Sliding scale) �Electrolytes (Na+ and K+)
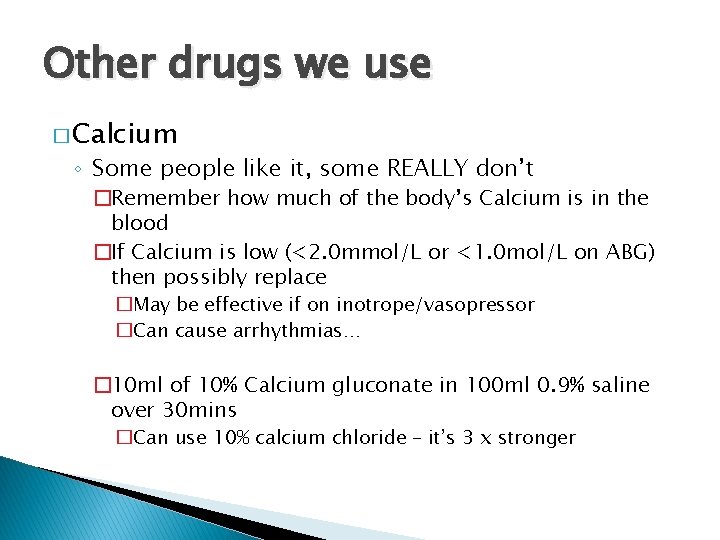
Other drugs we use � Calcium ◦ Some people like it, some REALLY don’t �Remember how much of the body’s Calcium is in the blood �If Calcium is low (<2. 0 mmol/L or <1. 0 mol/L on ABG) then possibly replace �May be effective if on inotrope/vasopressor �Can cause arrhythmias… � 10 ml of 10% Calcium gluconate in 100 ml 0. 9% saline over 30 mins �Can use 10% calcium chloride – it’s 3 x stronger
A few quirks of distributive shock � Burns ◦ Noradrenaline can be used ◦ Vasoconstriction affects the skin before most other sites � Anaphylaxis ◦ Adrenaline is the key… �Mast cell stabilisation…. �Can help with diagnosis (HR will decrease…)
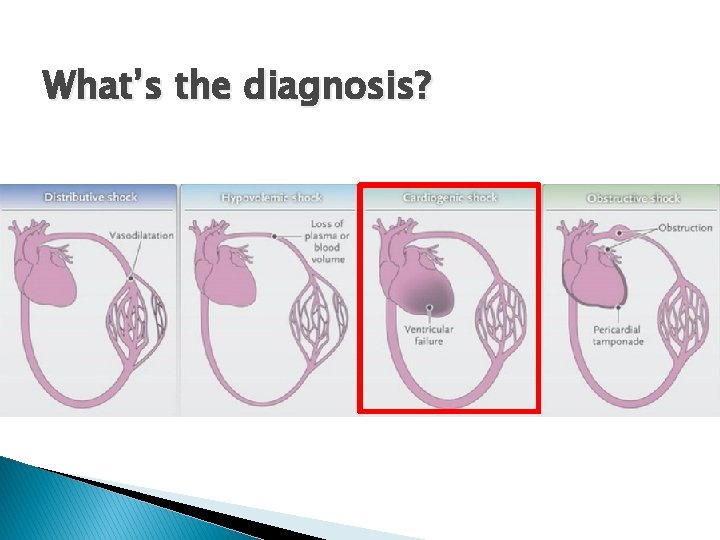
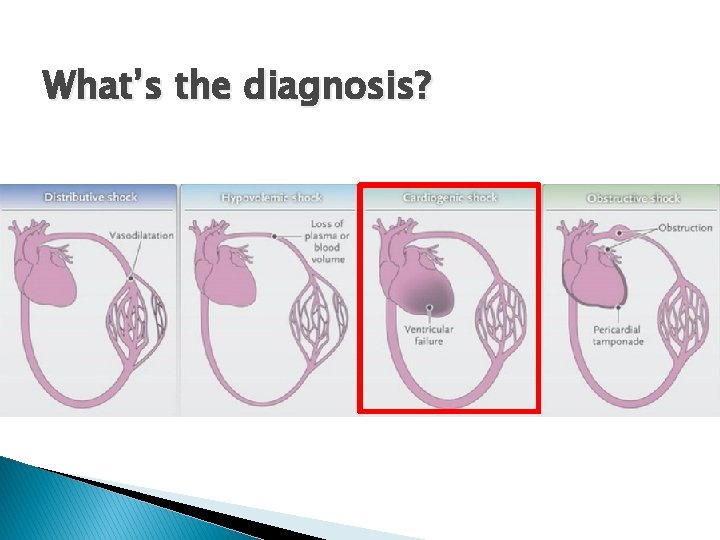
What’s the diagnosis?
Cardiogenic shock � What’s the underlying cause? ◦ Acute Heart failure �MI? �Cardiomyopathy? �Is it obstructive?
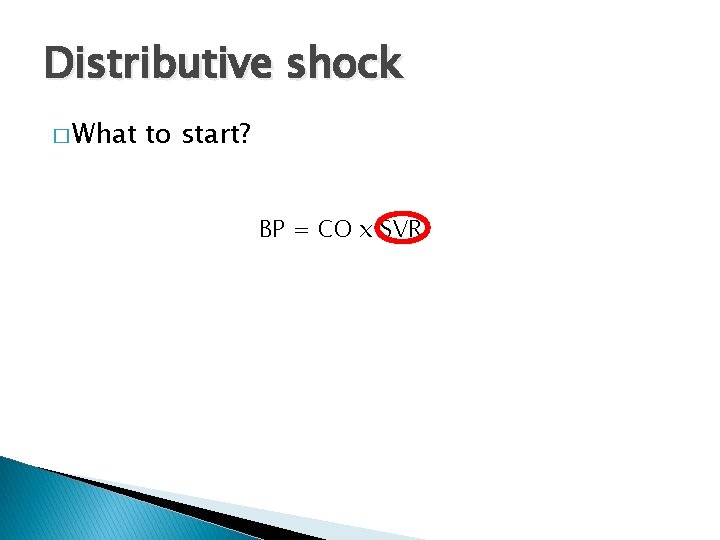
![Maintaining delivery of oxygen DO 2 CO1 34 x Hb x Sp O 2 Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2](https://slidetodoc.com/presentation_image_h/33c2284fde6bd1b5deb56e1fb964076b/image-63.jpg)
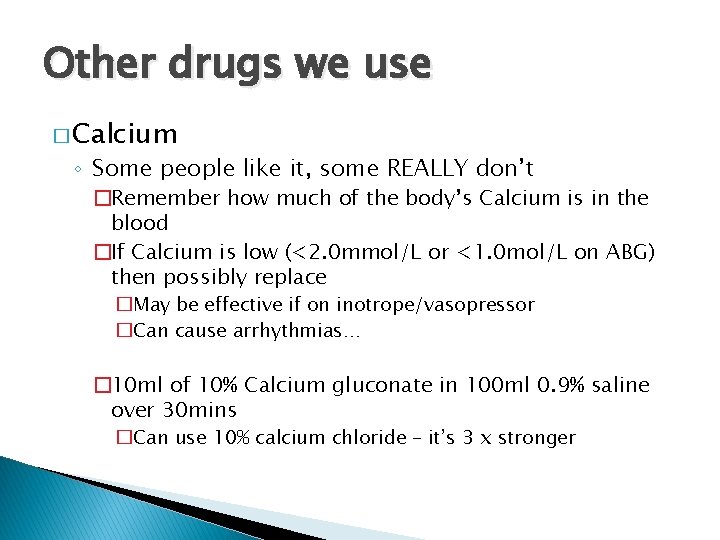
Maintaining delivery of oxygen DO 2 =CO[(1. 34 x [Hb] x Sp. O 2 ) + (Pa. O 2 x 0. 023)] BP = CO x SVR
Cardiogenic shock �A fine balance…… ◦ A failing heart should not be unduly stressed ◦ CO should meet the bodies needs…… � Adrenaline or Dobutamine (or GTN)
Which drug to start… � Dobutamine ◦ Can reduce LV afterload in systolic failure � Can be used peripherally � Typical doses 2. 520 mcg/kg/min
Which drug to start… � Dobutamine ◦ Can reduce LV afterload in systolic failure � Can be used peripherally � Typical doses 2. 520 mcg/kg/min � In acute heart failure can increase mortality � Can cause a tachycardia. . � In our units we don’t use it very often at all…
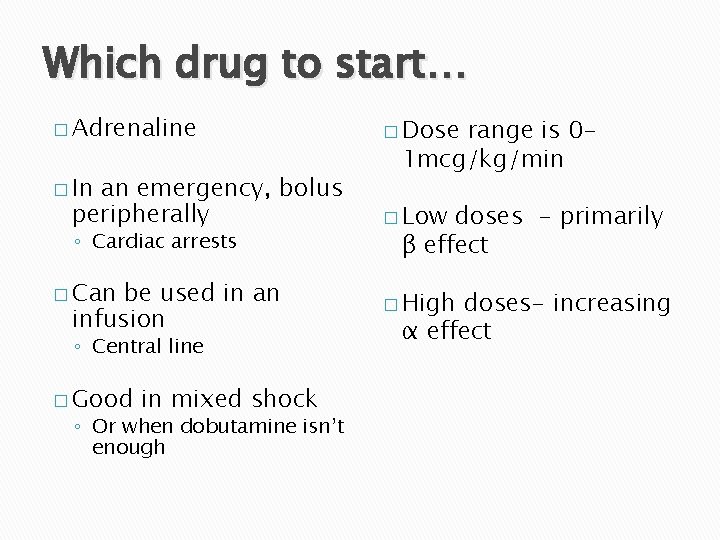
Which drug to start… � Adrenaline � In an emergency, bolus peripherally ◦ Cardiac arrests � Can be used in an infusion ◦ Central line � Good in mixed shock ◦ Or when dobutamine isnt enough
Which drug to start… � Adrenaline � Lactate � In � Tachycardia an emergency, bolus peripherally ◦ Cardiac arrests � Can be used in an infusion ◦ Central line � Good in mixed shock ◦ Or when dobutamine isn’t enough acidosis ◦ Often limits dose � May BP cause a DROP in ◦ Vasodilatation � Can � If cause arrhythmias it doesn’t work…
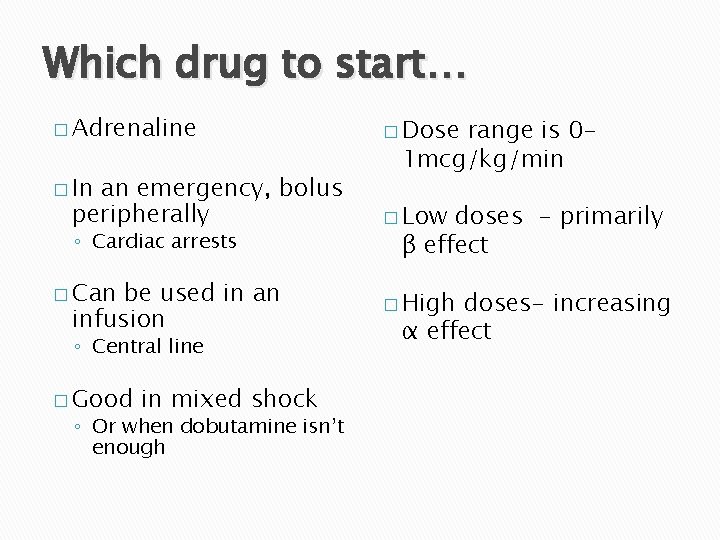
Which drug to start… � Adrenaline � In an emergency, bolus peripherally ◦ Cardiac arrests � Can be used in an infusion ◦ Central line � Good in mixed shock ◦ Or when dobutamine isn’t enough � Dose range is 01 mcg/kg/min � Low doses - primarily β effect � High doses- increasing α effect
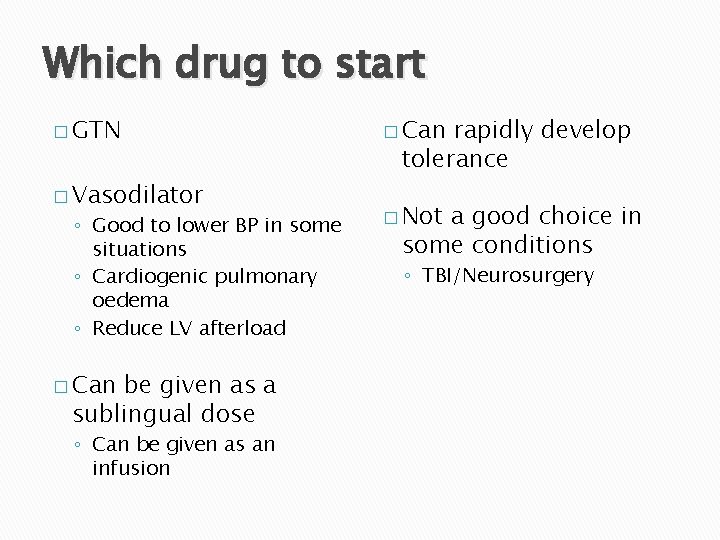
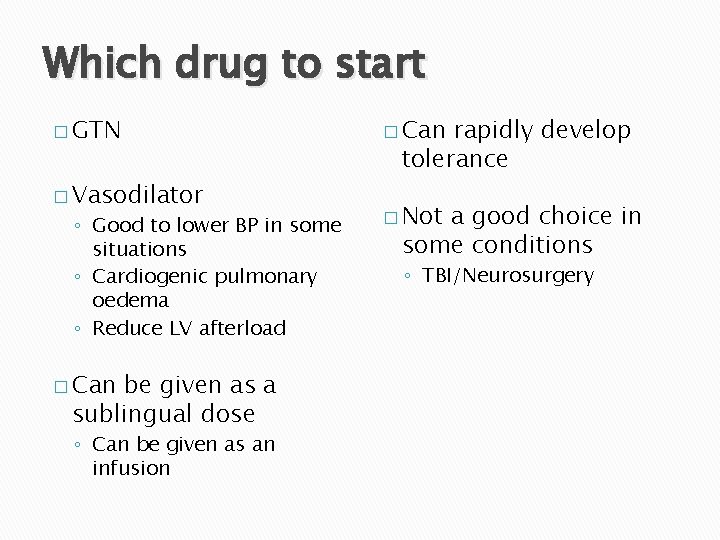
Which drug to start � GTN � Vasodilator ◦ Good to lower BP in some situations ◦ Cardiogenic pulmonary oedema ◦ Reduce LV afterload � Can be given as a sublingual dose ◦ Can be given as an infusion � Can rapidly develop tolerance � Not a good choice in some conditions ◦ TBI/Neurosurgery
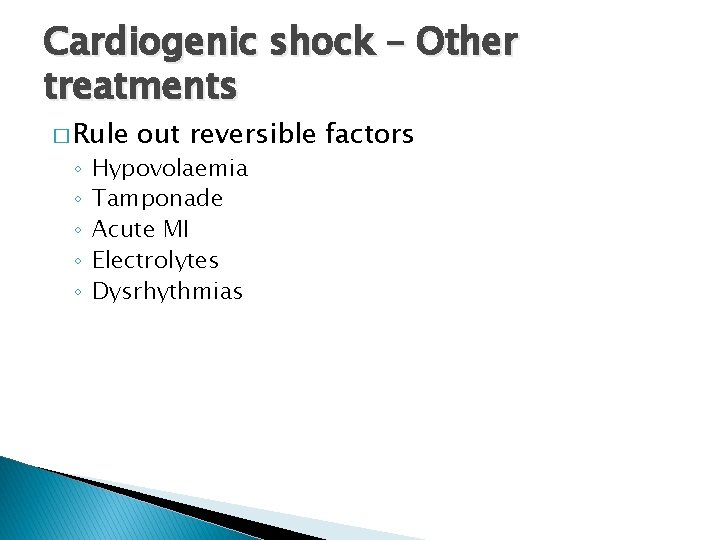
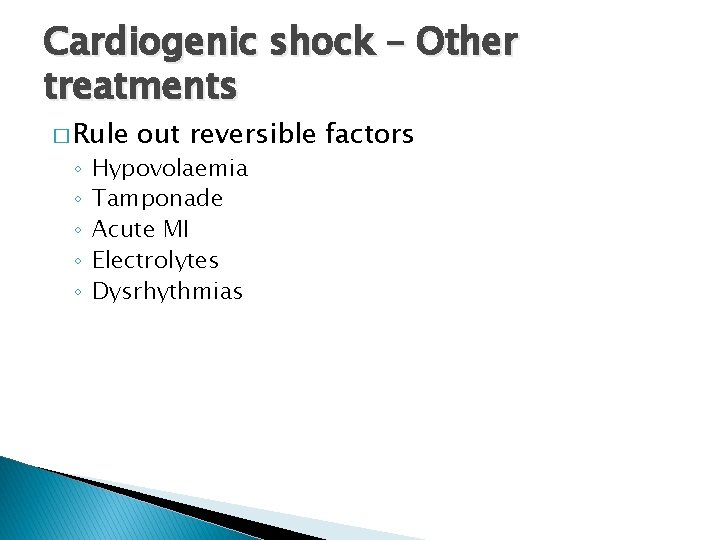
Cardiogenic shock – Other treatments � Rule ◦ ◦ ◦ out reversible factors Hypovolaemia Tamponade Acute MI Electrolytes Dysrhythmias
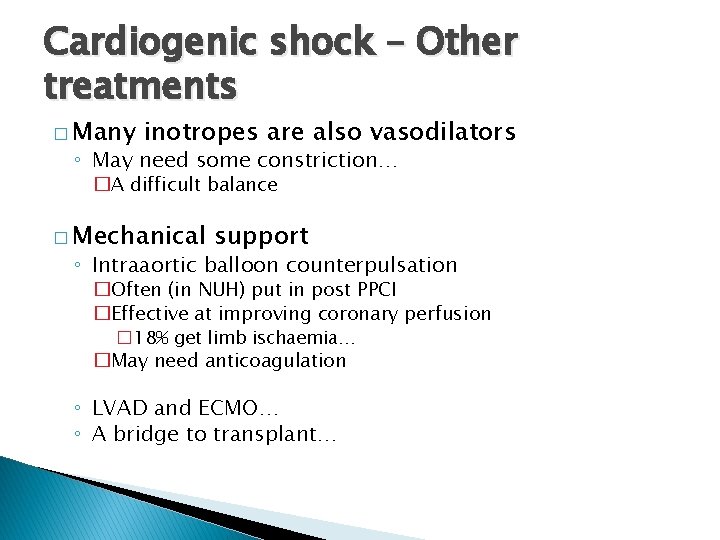
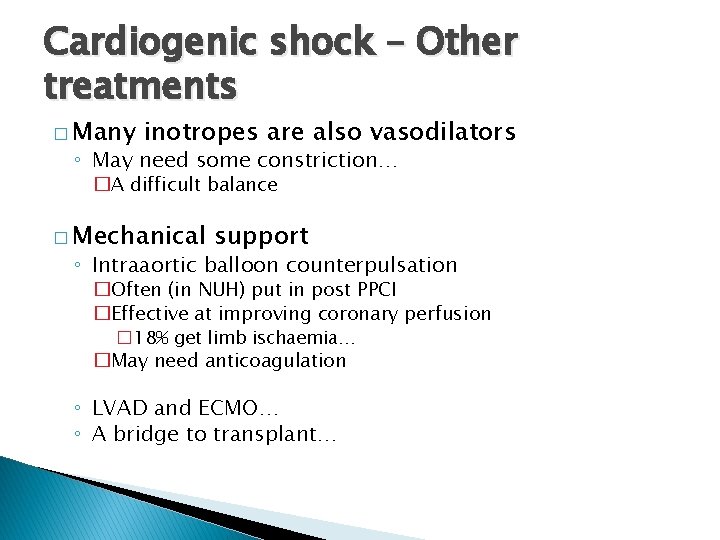
Cardiogenic shock – Other treatments � Many inotropes are also vasodilators ◦ May need some constriction… �A difficult balance � Mechanical support ◦ Intraaortic balloon counterpulsation �Often (in NUH) put in post PPCI �Effective at improving coronary perfusion � 18% get limb ischaemia… �May need anticoagulation ◦ LVAD and ECMO… ◦ A bridge to transplant…
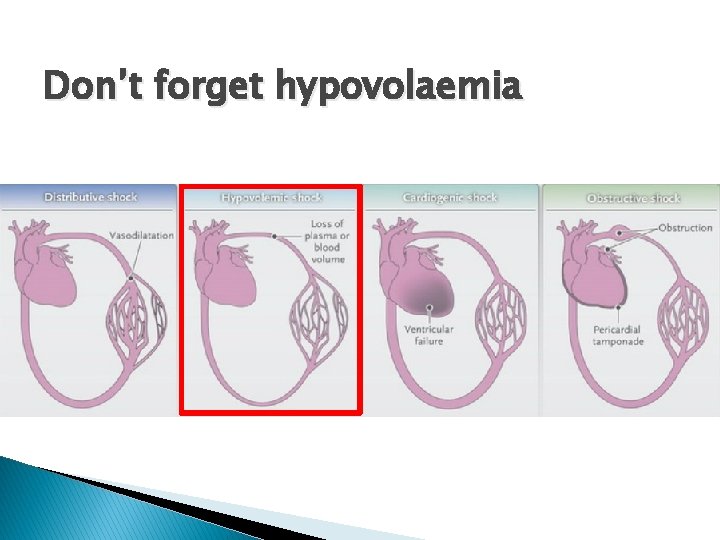
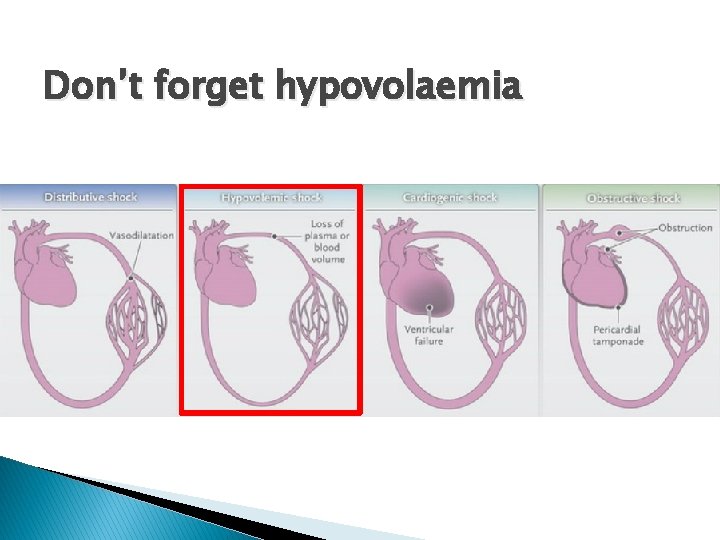
Don’t forget hypovolaemia
Hypovolaemia � Common in many pathologies ◦ If you’re underfilled… �You can’t squeeze an underfilled circulation �You can’t pump blood you don’t have � Consider hypovolaemia and fluid resuscitation in all forms of shock… ◦ Fluid therapy is a different talk…
Summary � Make sure you’ve got the right diagnosis � Drugs work better if your well filled � In distributive shock � In cardiogenic shock ◦ Noradrenaline then Vasopressin (or Adrenaline) ◦ Remember adjuncts ◦ Adrenaline is often the answer ◦ Mechanical therapies may be needed
A case study
Case �A 65 year old presents having fallen over in her garden 24 hours beforehand… she has a painful rapidly advancing cellulitis on her right leg � PMH ◦ Mild asthma ◦ HTN
Case � Pre-morbid state ◦ Lives independently ◦ ET – Unlimited � NKDA � Meds ◦ Amlodipine
Case � BP 80/50 � HR 120 � Sp. O 2 95% on 24% O 2 � RR 30 � Temp 38. 5 o. C � VBG ◦ p. H 7. 32 ◦ BE -3. 0 ◦ Lac 2. 0

Case � Treatments so far?
Case � Treatments ◦ ◦ ◦ so far Oxygen IV Access IV antibiotics 5 L Crystalloid Paracetamol Clexane…
Case � You 1) 2) 3) are asked to see the patient… What further history would you like? What further investigations should be performed What is your management plan….
On going management � Seen by plastics ◦ Make stab incisions – no fat necrosis ◦ Recommend conservative management with Abx � Any ◦ ◦ further specialist opinions Where should the patient be admitted? What investigations are needed? What treatments are needed? What procedures are needed?
Initial critical care management � Admitted to Critical care ◦ Art line inserted �BP 70/50, HR 130 ◦ CVC inserted Catheterised 60 ml urine (not passed urine in the 6 hours prior to admission to crit care ABG (on 40% O 2) p. H 7. 32, p. CO 2 3. 2, p. O 2 10. 2, HCO 3 - 12
Further management � 4 litres of crystalloid given in AICU ◦ U. O. remains <10 ml/hr ◦ Noradrenaline started (0. 15 mcg/kg/min) ◦ Further fluid boluses � D/W micro ◦ Fluclox and Clinda ◦ IVIg � Repeat ABG (60% O 2) � Patient looks ‘tired’ ◦ p. H 7. 25, p. CO 2 5. 2, p. O 2 8. 2, HCO 3 9, Lactate 5. 3 ◦ GCS now 13/15 (E 3 V 4 M 6)
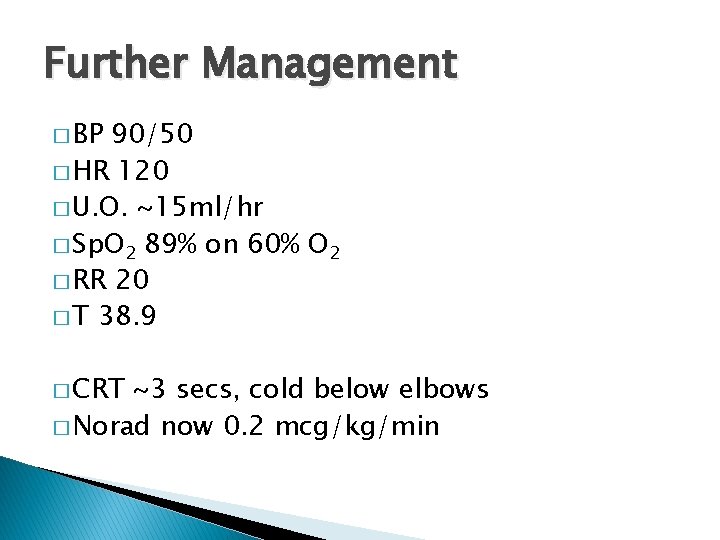
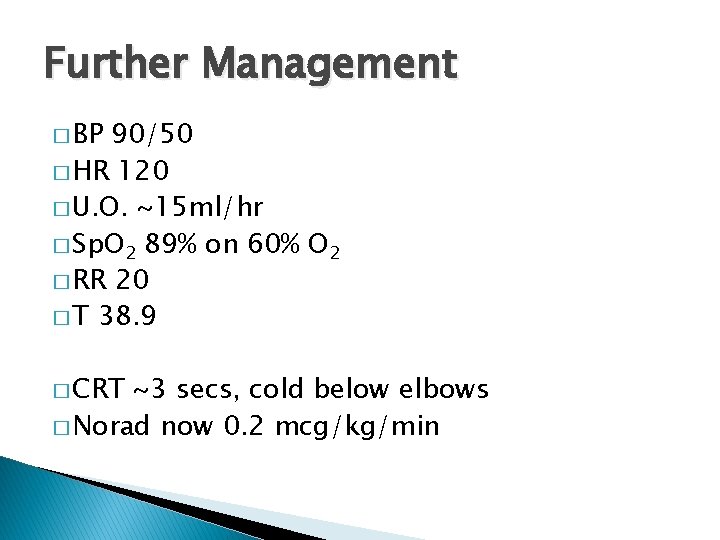
Further Management � BP 90/50 � HR 120 � U. O. ~15 ml/hr � Sp. O 2 89% on 60% O 2 � RR 20 � T 38. 9 � CRT ~3 secs, cold below elbows � Norad now 0. 2 mcg/kg/min
Next steps � What are your management priorities?
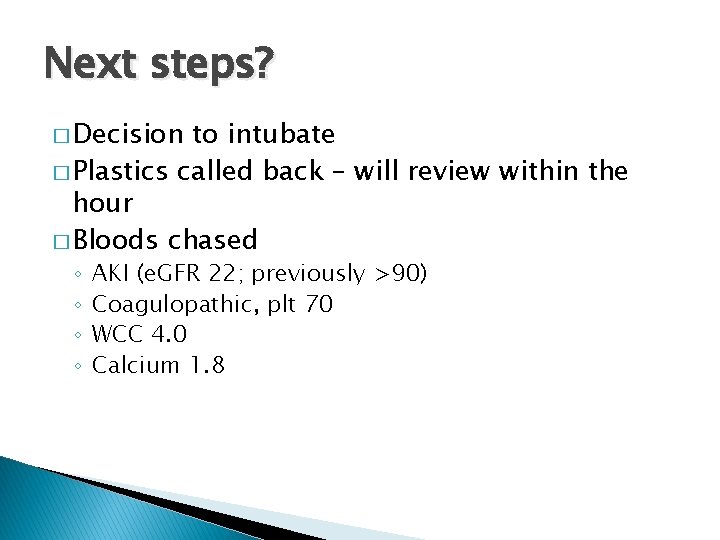
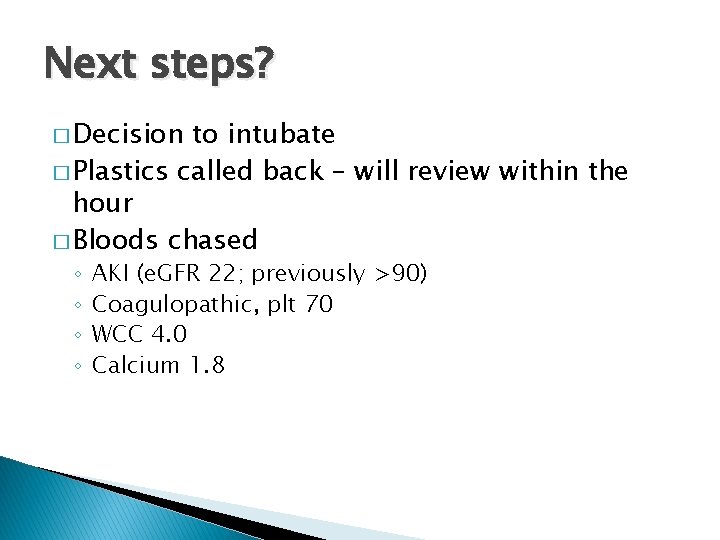
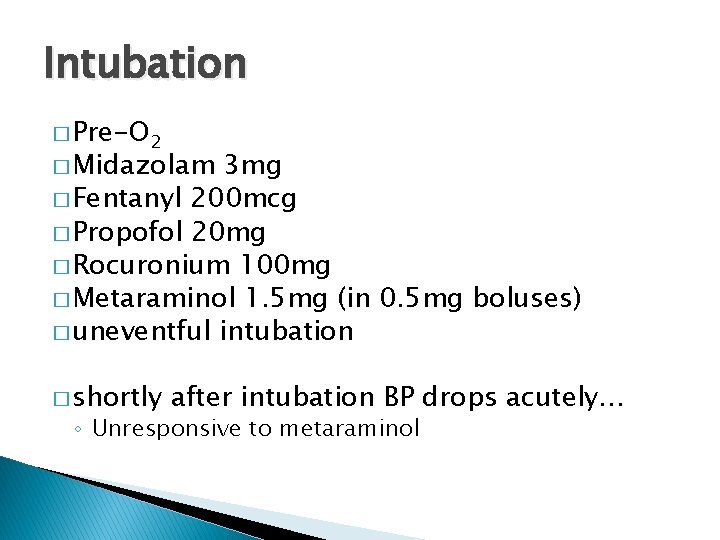
Next steps? � Decision to intubate � Plastics called back – will review within the hour � Bloods chased ◦ ◦ AKI (e. GFR 22; previously >90) Coagulopathic, plt 70 WCC 4. 0 Calcium 1. 8
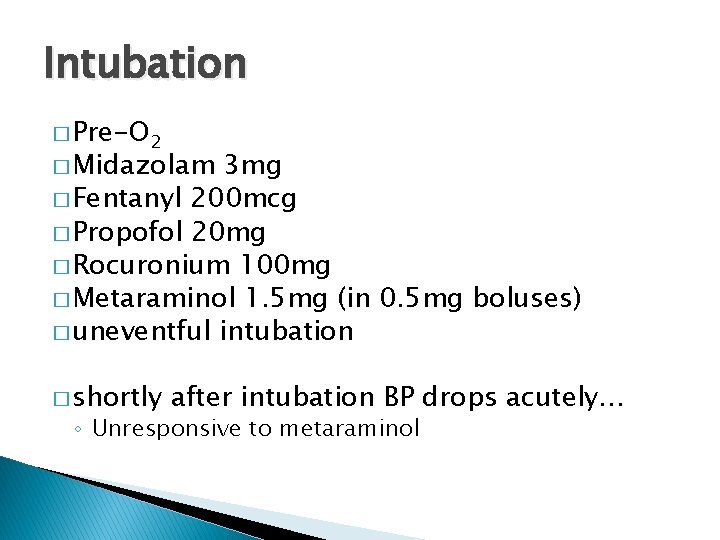
Intubation � Pre-O 2 � Midazolam 3 mg � Fentanyl 200 mcg � Propofol 20 mg � Rocuronium 100 mg � Metaraminol 1. 5 mg (in 0. 5 mg boluses) � uneventful intubation � shortly after intubation BP drops acutely… ◦ Unresponsive to metaraminol
Intubation � Hypotensive… ◦ 1) Why? ◦ 2) What are your immediate management steps? � What additional monitoring would you like?
Intubation � Hypotensive… ◦ 1) Why? ◦ 2) What are your immediate management steps? � What ◦ ◦ additional monitoring would you like? Art line – no swing. . Negative straight leg raise CO monitoring PAFC? ?
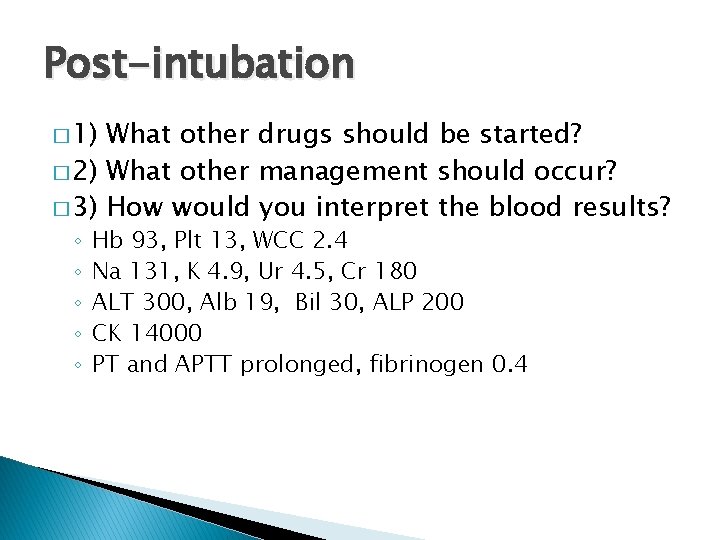
Post-intubation � 2 Litres of fluid given stat � Noradrenaline increased to 0. 7 mcg/kg/min � Vas cath inserted � Reassessed � BP 100/50 mm. Hg, HR 110 � No change with fluid bolus � Lactate 8. 2 on gas � U. O. ~15 ml/hr � Sp. O 2 ~92%
Post-intubation � Further investigations � Nurses report rapid progression of erythema ◦ Scv. O 2 52% ◦ Micro contact AICU – Gram +ve cocci in blood cultures. . ◦ Pathology phone – Coagulatopathic, plt 13. .
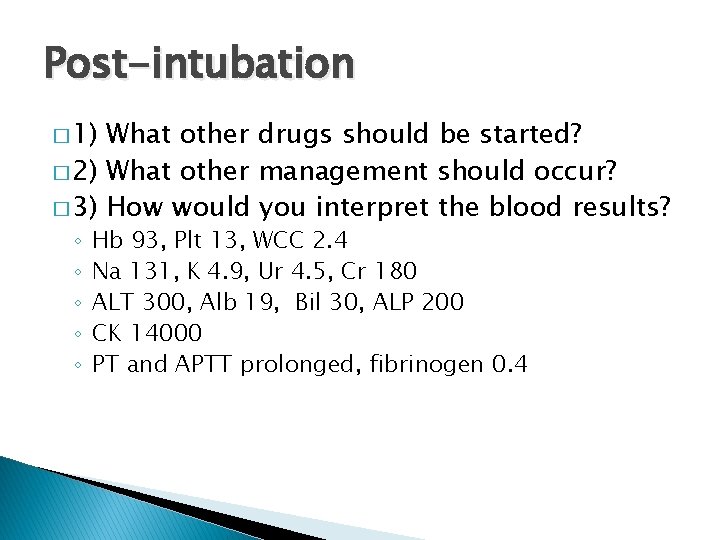
Post-intubation � 1) What other drugs should be started? � 2) What other management should occur? � 3) How would you interpret the blood results? ◦ ◦ ◦ Hb 93, Plt 13, WCC 2. 4 Na 131, K 4. 9, Ur 4. 5, Cr 180 ALT 300, Alb 19, Bil 30, ALP 200 CK 14000 PT and APTT prolonged, fibrinogen 0. 4
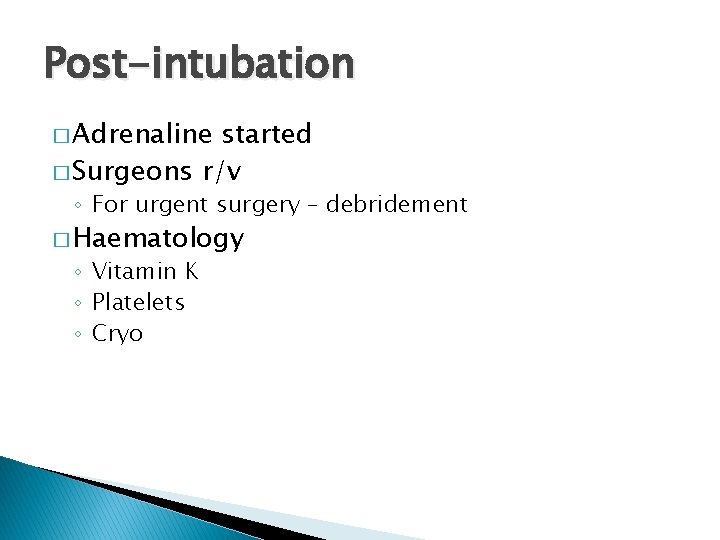
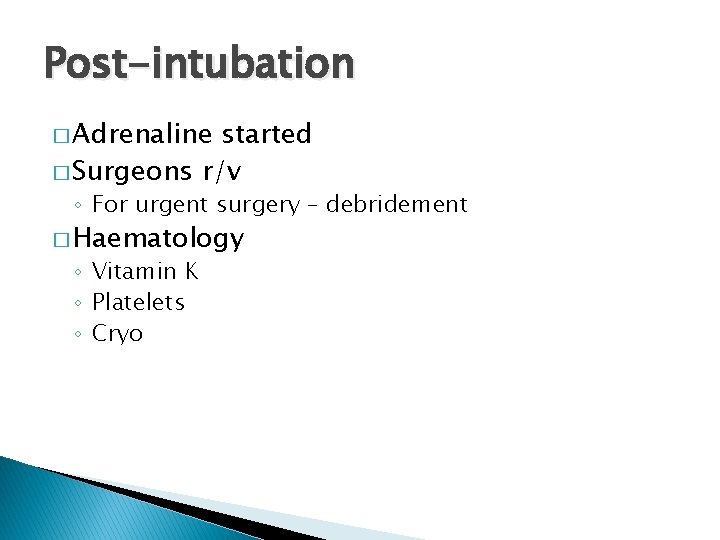
Post-intubation � Adrenaline started � Surgeons r/v ◦ For urgent surgery – debridement � Haematology ◦ Vitamin K ◦ Platelets ◦ Cryo

Theatre � Necrosed fat throughout leg � Debrided ankle to hip � In theatre lactate climbs to 14 � 10 L of crystalloid in theatre � Given hydrocortisone � FICE echo in theatre ◦ Mildly impaired LV function ◦ Well filled
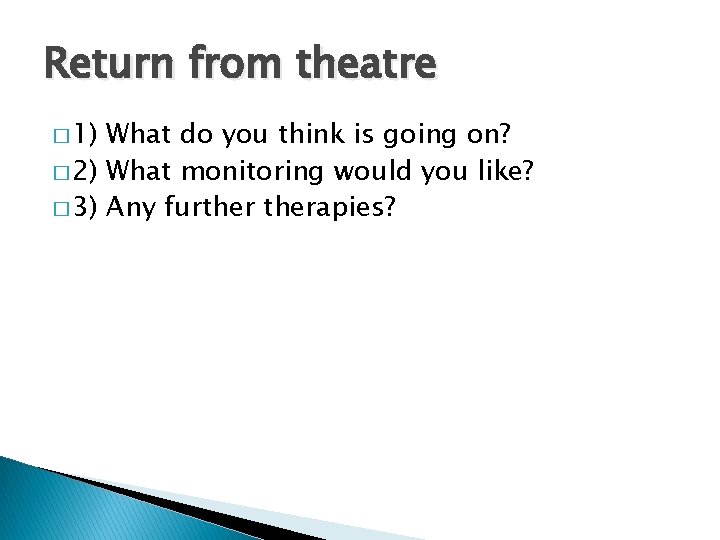
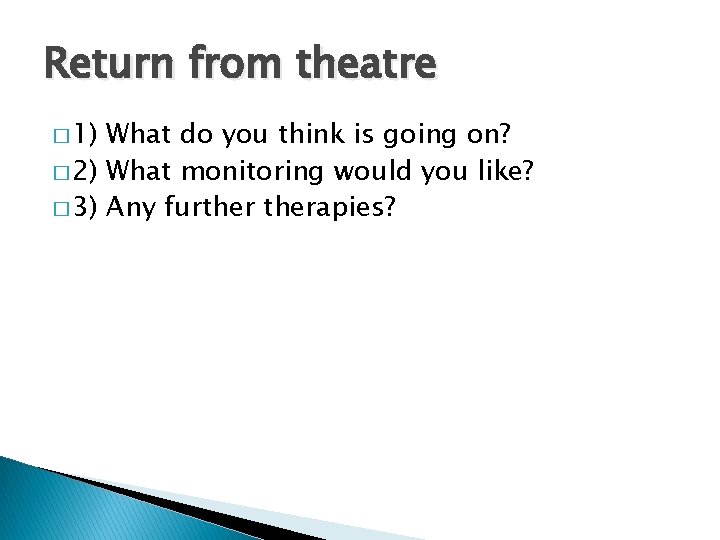
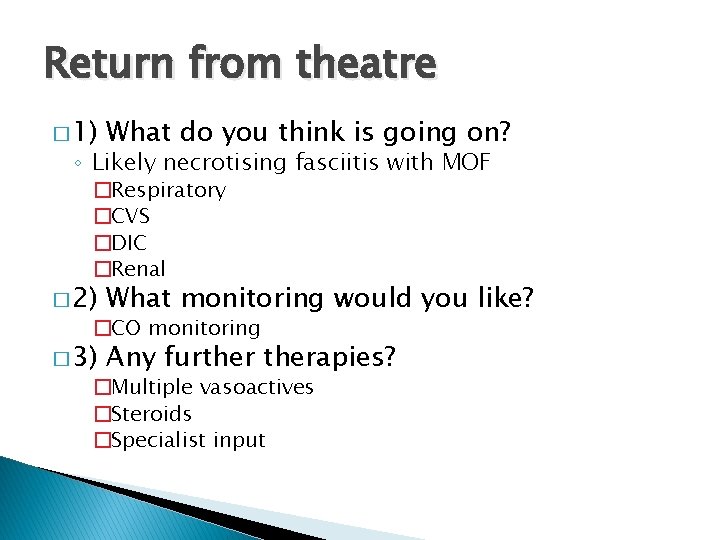
Return from theatre � 1) What do you think is going on? � 2) What monitoring would you like? � 3) Any furtherapies?
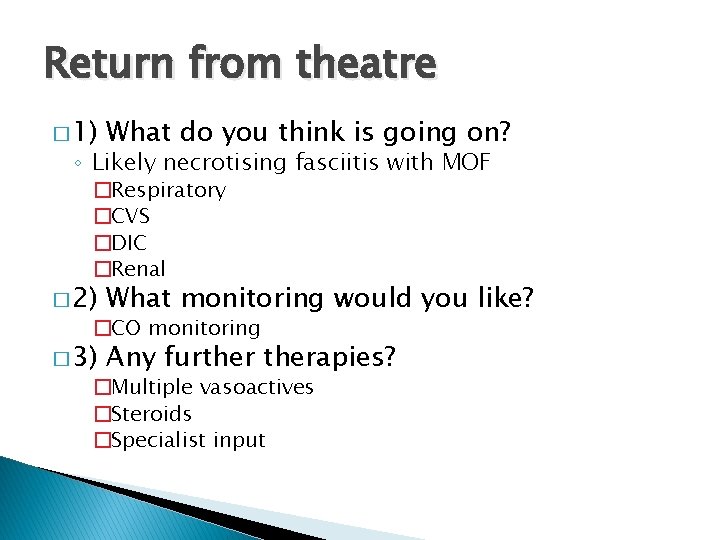
Return from theatre � 1) What do you think is going on? ◦ Likely necrotising fasciitis with MOF �Respiratory �CVS �DIC �Renal � 2) What monitoring would you like? � 3) Any furtherapies? �CO monitoring �Multiple vasoactives �Steroids �Specialist input
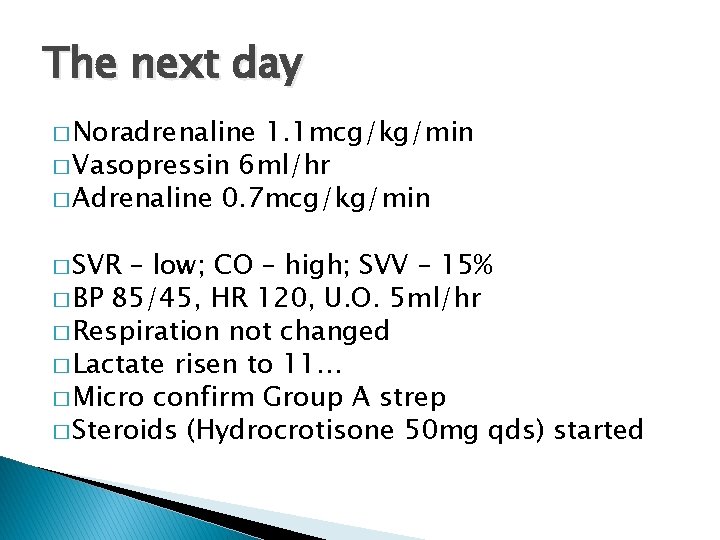
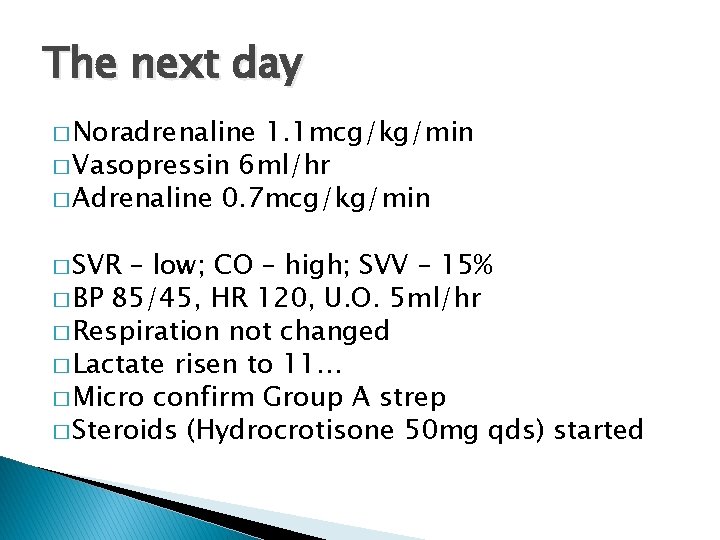
The next day � Noradrenaline 1. 1 mcg/kg/min � Vasopressin 6 ml/hr � Adrenaline 0. 7 mcg/kg/min � SVR – low; CO – high; SVV – 15% � BP 85/45, HR 120, U. O. 5 ml/hr � Respiration not changed � Lactate risen to 11… � Micro confirm Group A strep � Steroids (Hydrocrotisone 50 mg qds) started
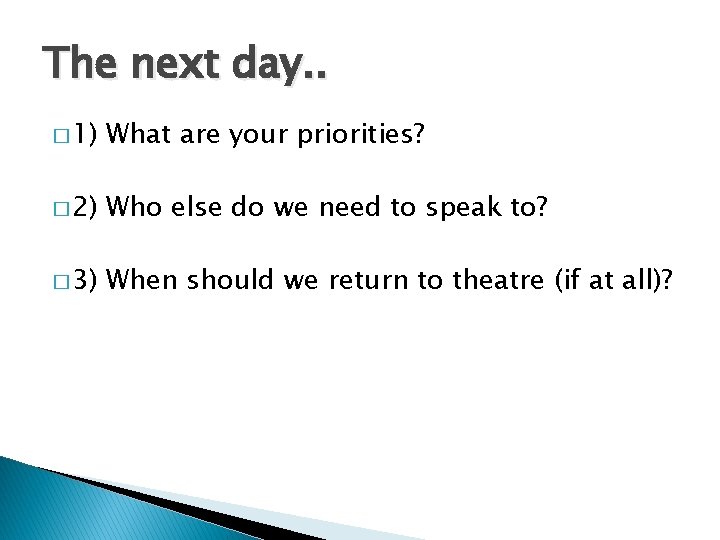
The next day. . � 1) What are your priorities? � 2) Who else do we need to speak to? � 3) When should we return to theatre (if at all)?
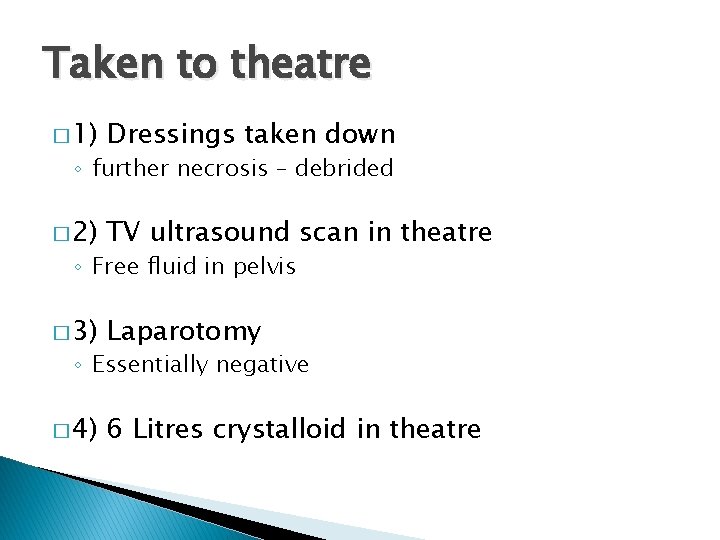
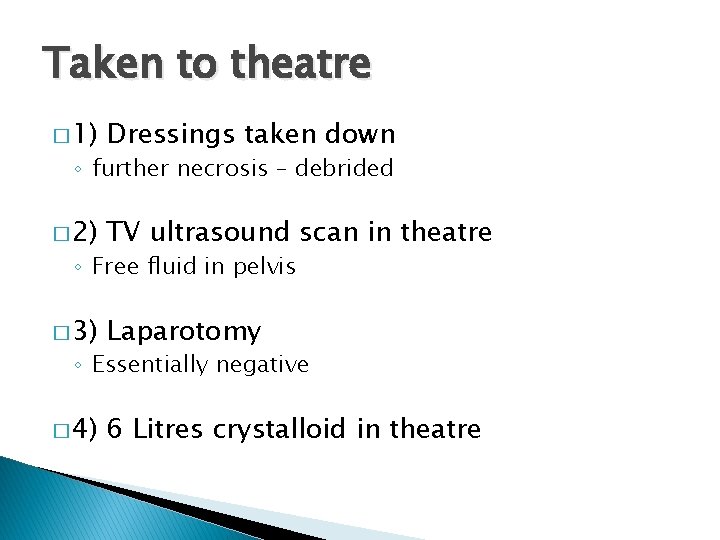
Taken to theatre � 1) Dressings taken down � 2) TV ultrasound scan in theatre � 3) Laparotomy � 4) 6 Litres crystalloid in theatre ◦ further necrosis – debrided ◦ Free fluid in pelvis ◦ Essentially negative
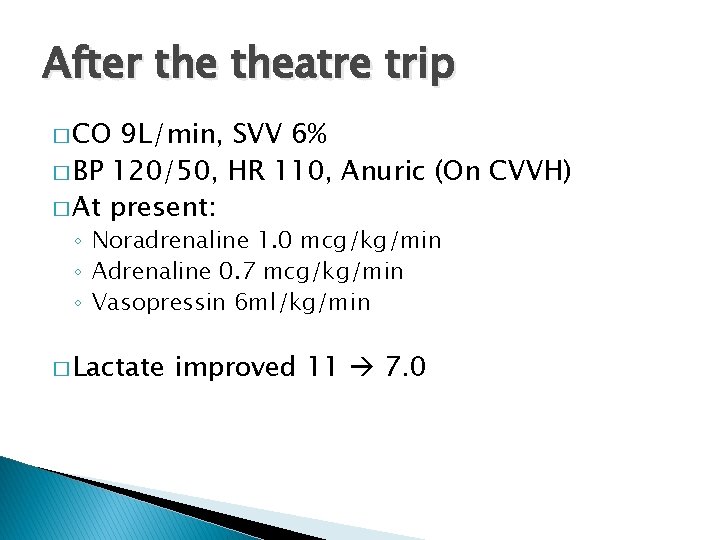
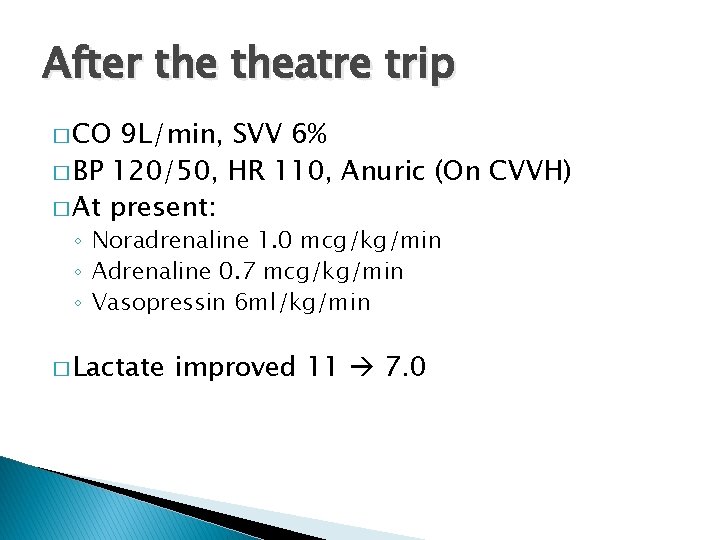
After theatre trip � CO 9 L/min, SVV 6% � BP 120/50, HR 110, Anuric (On CVVH) � At present: ◦ Noradrenaline 1. 0 mcg/kg/min ◦ Adrenaline 0. 7 mcg/kg/min ◦ Vasopressin 6 ml/kg/min � Lactate improved 11 7. 0
after theatre… � Which infusion should we reduce first? � What should we tell the family? � What would you expect to see on an ECHO?
3 days later � CVS stable � Inotropes/vasopressors weaning � Remains sedated and ventilated � Steroids stopped
Longer term ICM management � Weaning inotropes/vasopressin � Transferred to city hospital ◦ When should you transfer the transfer? ◦ Who should go?
Further progress � 6 further trips (debridements and SSG) � Tracheostomy � Ongoing CVVH � Discharged to Gillies ward 2 months after � Discharged home 3 months after admission
Questions. .
 Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Semi critical instruments in dentistry
Semi critical instruments in dentistry Local hormone
Local hormone Amine vasopressive exemple
Amine vasopressive exemple Mrc senior clinical fellowship
Mrc senior clinical fellowship Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Schooltool lyons
Schooltool lyons Robert lyons photographer
Robert lyons photographer Shante lyons
Shante lyons Adn
Adn Lyons ferry hatchery
Lyons ferry hatchery Tori lyons
Tori lyons Mrs lyons quotes
Mrs lyons quotes Infinite campus lths
Infinite campus lths Clarissa lyons
Clarissa lyons Ispic
Ispic Words to describe mrs lyons
Words to describe mrs lyons Critical reading meaning
Critical reading meaning Fellow lpkia
Fellow lpkia Odd fellow medlemsregister
Odd fellow medlemsregister Ieee fellow nomination
Ieee fellow nomination Importance of fellow customers in service delivery
Importance of fellow customers in service delivery Ieee fellow requirements
Ieee fellow requirements What is a technical fellow at microsoft
What is a technical fellow at microsoft Cisco fellow
Cisco fellow Fellow lpkia
Fellow lpkia Poor little black fellow summary
Poor little black fellow summary Mun sample
Mun sample Asme fellow nomination
Asme fellow nomination Odd fellow orden
Odd fellow orden Nhmrc emerging leadership fellow
Nhmrc emerging leadership fellow Little fellow
Little fellow Welcome phones
Welcome phones Ian karlin
Ian karlin Ian munro waterloo
Ian munro waterloo Ian mundy
Ian mundy Stanford wireless communication
Stanford wireless communication Red reflex absent causes
Red reflex absent causes Inżynieria oprogramowania ian sommerville
Inżynieria oprogramowania ian sommerville Ian giddy
Ian giddy Suffixes ian
Suffixes ian Ian gover
Ian gover Ian coddington
Ian coddington Simple aspect example
Simple aspect example Lindsay semler
Lindsay semler Ian devine accountant
Ian devine accountant Ian williams darlington borough council
Ian williams darlington borough council Mungol
Mungol Engineering software products ian sommerville
Engineering software products ian sommerville Ian fairlie
Ian fairlie Ian utting
Ian utting Ian jones bournemouth university
Ian jones bournemouth university Gans goodfellow
Gans goodfellow Ian harnarine
Ian harnarine Help2rent southwark
Help2rent southwark Ian lindsley
Ian lindsley Ian endres
Ian endres Ian
Ian A mcpherson pro reunion
A mcpherson pro reunion Ian mcdonald liverpool
Ian mcdonald liverpool Ian smales
Ian smales Audrey proulx
Audrey proulx Calptotectin
Calptotectin Ian sandford
Ian sandford Thinking history ian dawson
Thinking history ian dawson Ian brown oxford
Ian brown oxford Professor ian wilcox
Professor ian wilcox Ian gilham
Ian gilham Ian hembry
Ian hembry Stefanie molin
Stefanie molin Ian giddy
Ian giddy Ian karlin
Ian karlin Ian giddy
Ian giddy Thinkinghistory.co.uk
Thinkinghistory.co.uk Ian coddington
Ian coddington Geometry bootcamp 2019 answers
Geometry bootcamp 2019 answers Ian j goodfellow
Ian j goodfellow Ian crotty
Ian crotty Ian foster university of chicago
Ian foster university of chicago Ian giddy
Ian giddy Ian joesbury
Ian joesbury Cgan
Cgan Ian milborrow pwc
Ian milborrow pwc Ian gent
Ian gent Ian yen
Ian yen Ian mitchell ubc
Ian mitchell ubc Ian gallimore
Ian gallimore Rich picture
Rich picture Ian 345216_2004
Ian 345216_2004 Ian tibbetts
Ian tibbetts Buying american
Buying american Ian winship
Ian winship Ian boersma
Ian boersma Ian lindsley
Ian lindsley Ian woolford
Ian woolford Ian thurgood
Ian thurgood Ian hetherington death
Ian hetherington death Ian proulx
Ian proulx Meeting point
Meeting point Ian dykes
Ian dykes Novel definition
Novel definition Ian tombleson
Ian tombleson Ian scott international
Ian scott international Ian colebourne
Ian colebourne Ian giddy
Ian giddy Ian viney
Ian viney Cuando teresa regresa a casa por la tarde
Cuando teresa regresa a casa por la tarde Ian lously
Ian lously