Thyroid Gland Hypothyroidism Hyperthyroidism Dr Zahoor 1 Thyroid









- Slides: 46
Thyroid Gland Hypothyroidism & Hyperthyroidism Dr. Zahoor 1
Thyroid Gland The metabolism of Virtually all nucleated cells of many tissues in the body is controlled by thyroid hormone Over activity (Hyperthyroidism) and under activity (Hypothyroidism) of the gland are most common of all endocrine problems 2
Thyroid Gland Anatomy: It has two lateral lobes connected by Isthmus It moves on swallowing as it is attached to thyroid cartilage and trachea Embryologically it originates from the base of the tongue and then descends therefore sometimes remnants of thyroid can be found at the base of tongue (Lingual thyroid) 3
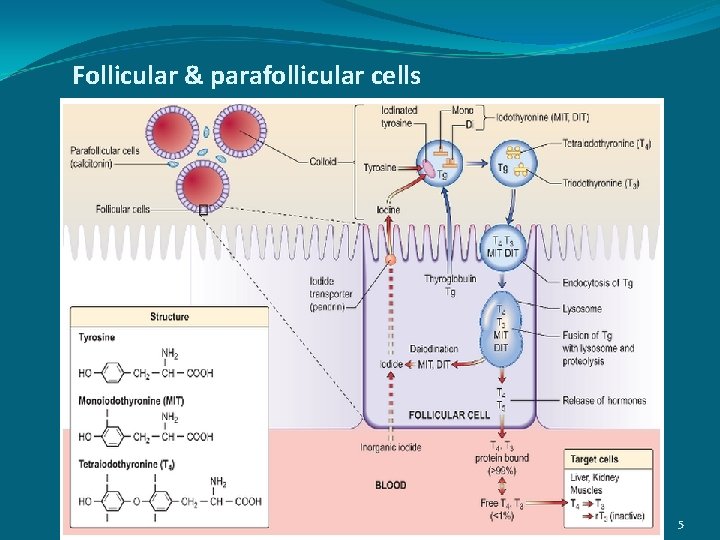
Thyroid Gland Anatomy: Thyroid gland has follicles lined by cuboidal epithelial cells. Inside the follicle is colloid (Iodinated glycoprotein Thyroglobulin) which is synthesized by follicular cells. Each follicle is surrounded by basement membrane, between follicular cells there are parafollicular cells containing calcitonin secreting C cells 4
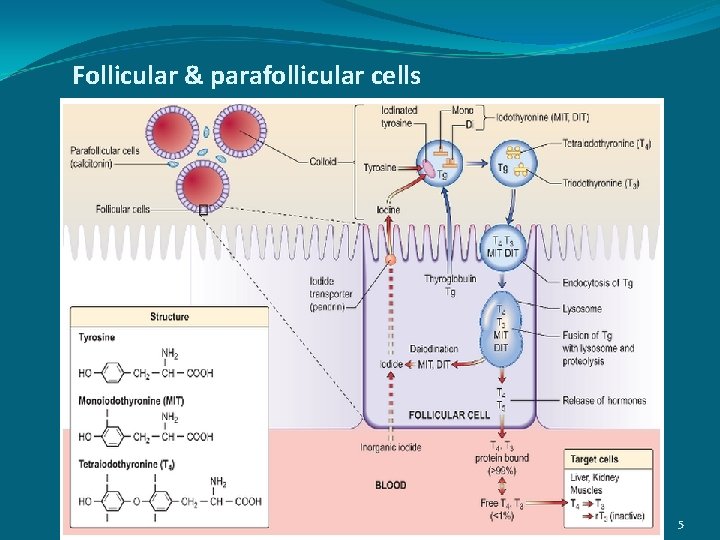
Follicular & parafollicular cells 5
Thyroid Gland Physiology: Thyroid gland synthesizes two hormones T 3 – Triiodothyronin: acts at Cellular level T 4 - L – Thyroxin: which is prehormone More T 4 is produced than T 3 in thyroid but T 4 is converted to T 3 in periphery 6
Thyroid Gland Physiology: In Plasma more than 99% of T 4 and T 3 is bound to protein (Thyroxin Binding Globulin TBG, Thyroid Binding Pre. Albumin TBPA) and Albumin 7
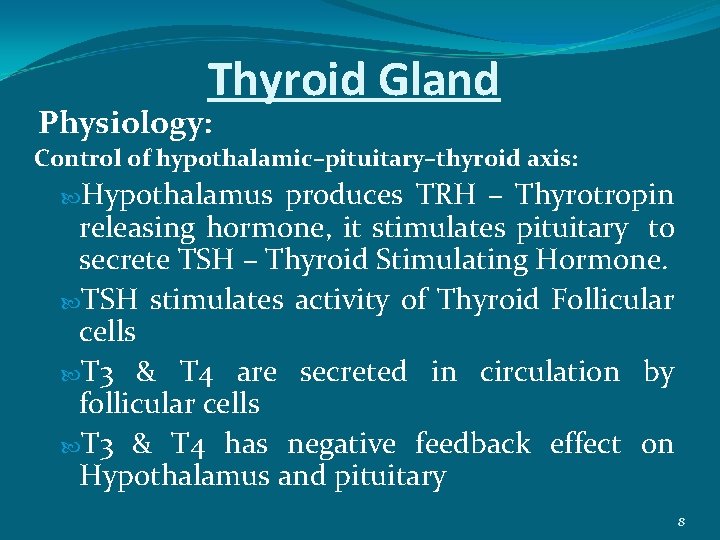
Thyroid Gland Physiology: Control of hypothalamic–pituitary–thyroid axis: Hypothalamus produces TRH – Thyrotropin releasing hormone, it stimulates pituitary to secrete TSH – Thyroid Stimulating Hormone. TSH stimulates activity of Thyroid Follicular cells T 3 & T 4 are secreted in circulation by follicular cells T 3 & T 4 has negative feedback effect on Hypothalamus and pituitary 8
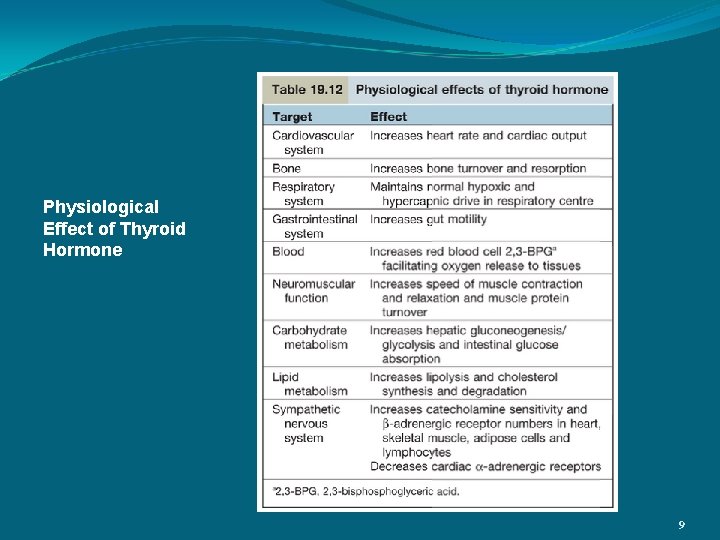
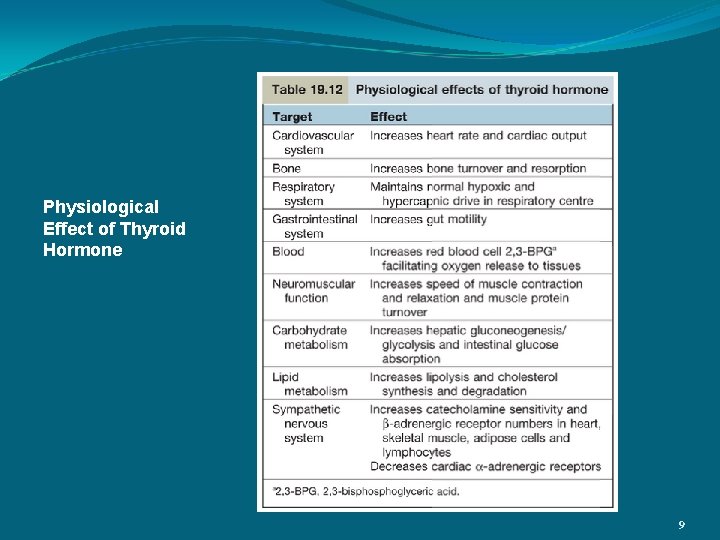
Physiological Effect of Thyroid Hormone 9
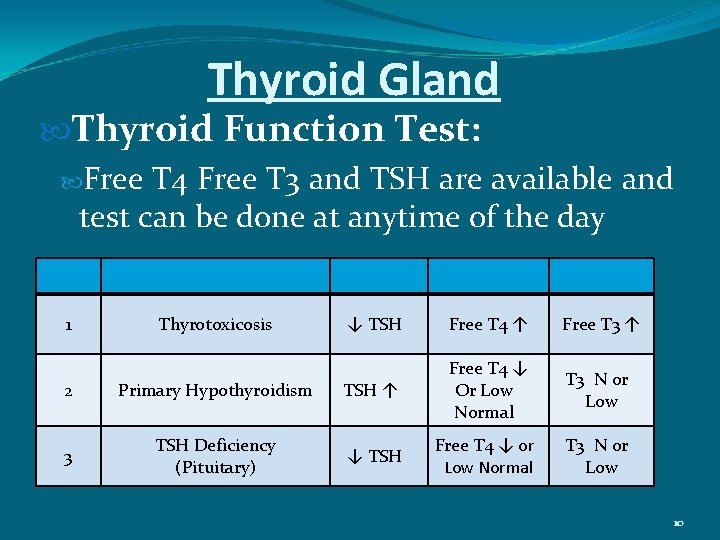
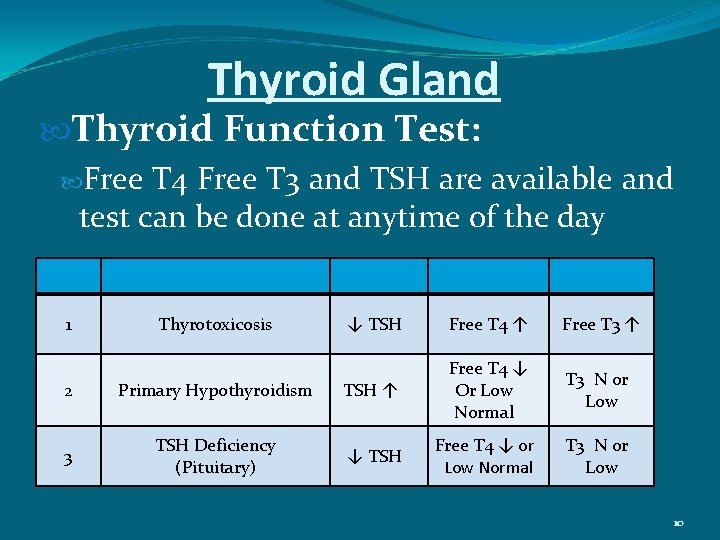
Thyroid Gland Thyroid Function Test: Free T 4 Free T 3 and TSH are available and test can be done at anytime of the day 1 Thyrotoxicosis ↓ TSH Free T 4 ↑ Free T 3 ↑ T 3 N or Low 2 Primary Hypothyroidism TSH ↑ Free T 4 ↓ Or Low Normal 3 TSH Deficiency (Pituitary) ↓ TSH Free T 4 ↓ or Low Normal 10

HYPOTHYROIDSM 11
Hypothyroidism It is usually primary due to disease of thyroid, but may be secondary to hypothalamic – pituitary disease (decreased TSH drive) It is more common in females 12
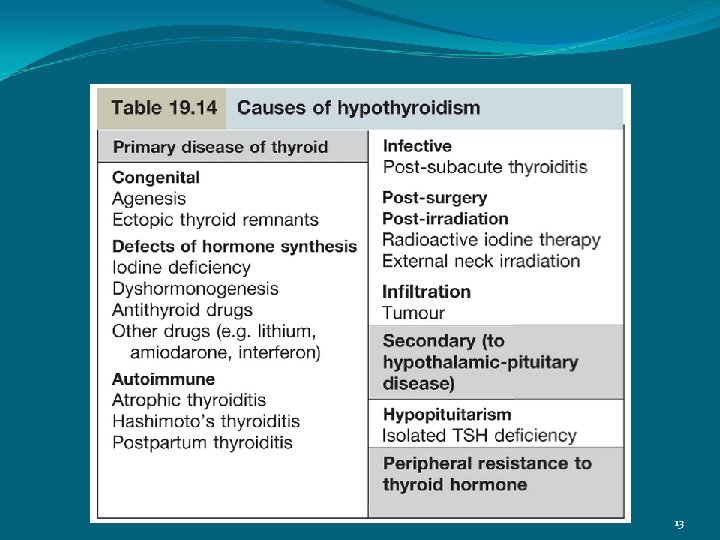
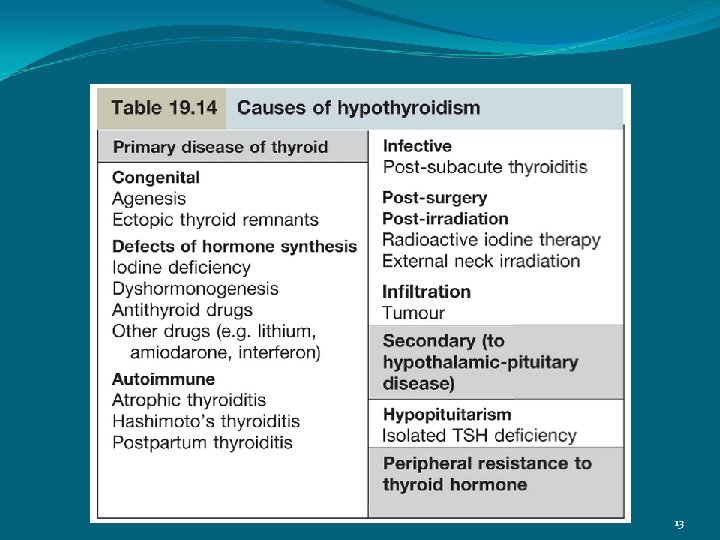
13
Hypothyroidism Autoimmune Hypothyroidism It is most common cause and associated with antithyroid antibodies It is six time more common in females It has association with other autoimmune diseases e. g. pernicious anemia, Vitiligo etc. 14
Hypothyroidism Hashimotos Thyroiditis This is a form of autoimmune thyroiditis, more common in females and occurs in late middle age Causes atrophic changes and regeneration leading to goiter formation TPO ( Thyroid per oxidase) antibodies are present in high titer (> 1000 IU/L) Patient may be hypothyroid or Euthyroid, though they may go through initial toxic phase Levothyroxin is given when patient is hypothyroid 15

Hypothyroidism Post Partum Thyroiditis This is transient phenomena, observed after pregnancy It may cause Hyperthyroidism, Hypothyroidism It is due to result of modifications to the immune system in pregnancy It is usually self limiting or leads to hypothyroidism 16

Defects of Thyroid Hormone Synthesis Iodine Deficiency Iodine is required for synthesis of T 3 & T 4 We take iodine in diet, if deficient than people get goiter ( due to TSH stimulation) Patient may be euthyroid or hypothyroid Iodine deficiency is problem in many countries e. g. Netherlands, India, Asia, Africa, Russia Efforts are made to prevent iodine deficiency by adding iodine in common salt. 17
Defects of Thyroid Hormone Synthesis Dyshormonogenesis Rare condition, due to genetic defect in the synthesis of thyroid hormone Patient develops hypothyroidism with goiter Note—Some people have Genetic defect causing sensorineural deafness due to mutation at chromosome 7, they have goiter( hypothyroid) also and this condition is called Pendred Syndrome 18
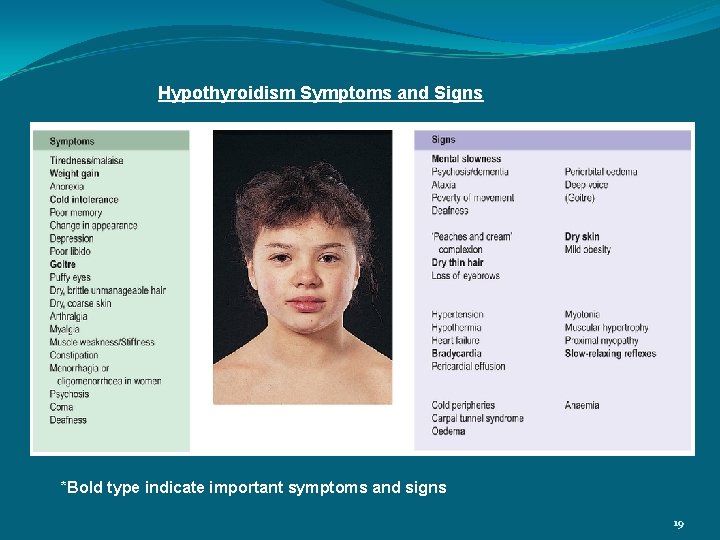
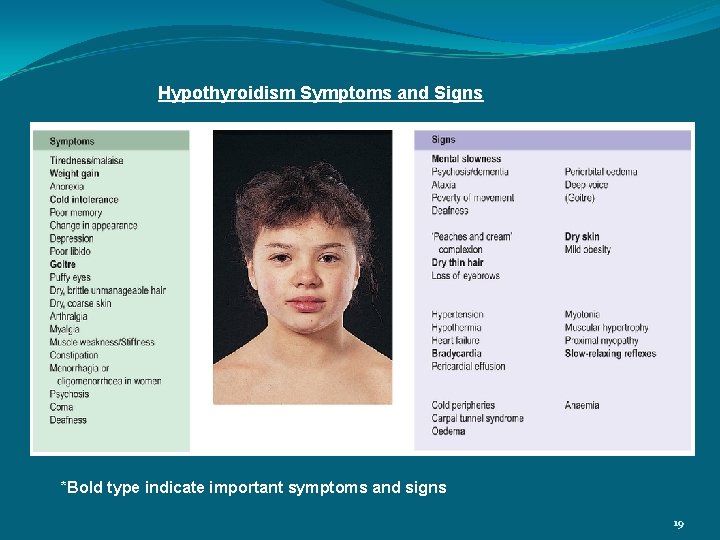
Hypothyroidism Symptoms and Signs *Bold type indicate important symptoms and signs 19
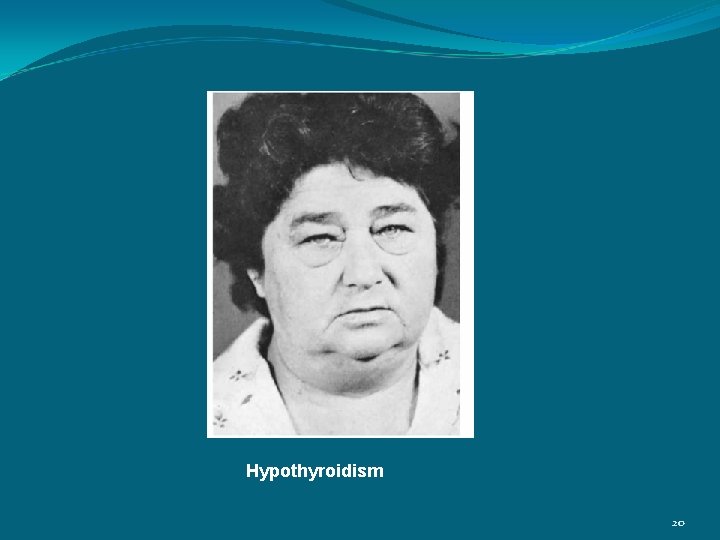
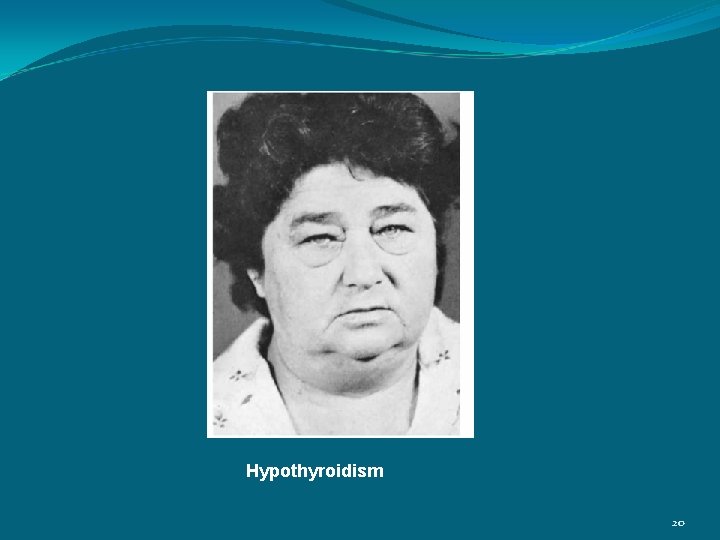
Hypothyroidism 20
Hypothyroidism Myxoedema: It refers to Hypothyroidism plus accumulation of mucopolysaccharide in subcutaneous tissue Patient is slow, thick skin, dry hair, deep voice, weight gain, cold intolerance, bradycardia, constipation 21
Hypothyroidism Children with Hypothyroidism: Have slow growth velocity Have poor school performance Young Females with Hypothyroidism should be excluded in all women with Oligomenorrhoea, amenorrhoea, menorrhagia, infertility, Hyperprolactinimia 22
Hypothyroidism Investigations: Serum Free T 3, Free T 4 and TSH High TSH confirms primary Hypothyroidism, free T 4 is low Other investigations: Anemia – usually normocytic normochromic But may be Macrocytic (due to associated Pernicious anemia ) Microcytic – in women due to menorrhagia 23
Hypothyroidism Other Investigations: Increase serum creatinine Kinase – with associated Myopathy Hypercholesterolemia and hypertriglyceridaemia Hyponatremia – due to increase ADH 24
Hypothyroidism Treatment: Thyroxin – T 4 is given for life Dose 100 Micrgram daily for young patients, 50 microgram for small, old patient to be increased to 100 microgram after 2 – 4 days If patient has IHD start with 25 Microgram daily and increase dose at 3 – 4 week interval ( monitor by serial ECG) Aim of treatment is to restore T 4 & TSH within normal range Improvement on T 4 takes 2 weeks or more and resolution of symptoms takes about 6 months 25
Hypothyroidism Treatment for Myxoedema: It is severe hypothyroidism and patient may present with confusion or even COMA Myxoedema Coma is very rare, hypothermia is often present and patient may have severe cardiac failure, pericardial effusion, hypoventilation, hypoglycemia, hyponatremia Mortality is high 26
Hypothyroidism Treatment for Myxoedema: T 3 orally or IV 2. 5 -5 microgram 8 hourly O 2 Hydrocortisone 100 mg IV 8 Hourly Glucose infusion Gradual rewarming 27
HYPERTHYROIDISM 28
Hyperthyroidism (Thyrotoxicosis) is common, affecting 2 -5% of all females Female-Male ratio 5: 1 Age 20 -40 years More than 99% cases are caused by intrinsic thyroid disease, pituitary cause is extremely rare 29

30

Graves Disease This is most common cause of hyperthyroidism and is due to autoimmune process Ig. G antibodies bind to TSH receptors in the thyroid and stimulate thyroid hormone production (Ig. G behaves like TSH) TSH receptor antibodies (TSHR – Ab antibodies) are specific for Graves Disease is associated with autoimmune disorders such as pernicious anemia, Vitiligo and myasthenia gravis 31
Other Causes of Hyperthyroidism/Thyrotoxicosis Solitary toxic adenoma/nodule It is cause of 5% cases of hyperthyroidism usually remit after antithyroid drugs Toxic multinodular goitre Commonly occurs in older woman Anti thyroid drugs control hyperthyroidism 32
Other Causes of Hyperthyroidism/Thyrotoxicosis De Quervain’s thyroditis This is transient hyperthyroidism due to inflammatory process, probably viral in origin There is fever, maliase, pain in the neck, tachycardia and local thyroid tenderness Thyroid function test show - Hyperthyroidism - Increased ESR 33
Other Causes of Hyperthyroidism/Thyrotoxicosis De Quervain’s thyroditis Thyroid function test show (cont) - Thyroid uptake show suppression of uptake in acute phase due to follicular damage - Hypothyroidism, usually transient, may follow after few weeks Treatment of acute phase - Aspirin - Predinisolone 34
Other Causes of Hyperthyroidism/Thyrotoxicosis Amiodarone – induced thyrotoxicosis (AIT) Amiodarone is anti arrhythmic drug – class 111 and causes hyperthyroidism 35

Symptoms and Signs of Hyperthyroidism *Bold type indicate important symptoms and signs 36
Clinical Features of Hyperthyroidism The eye signs of lid lag and stare May occur with hyperthyroidism of any cause Graves dermopathy Pretibial myxoedema – is in filtration of the skin on the shin Thyroid Acropachy – very rare and consist of clubbing, swollen fingers and periosteal new bone formation 37

Clinical Features of Hyperthyroidism (cont) Atrial Fibrillation in the elderly Is frequent presentation Children with hyperthyroidism May present – excessive height, hyperactivity 38

Pretibial myxoedema in Hyperthyroidism 39
Differential Diagnosis Anxiety (Sympathetic Stimulation) There is tachycardia, tremor, but cold clammy hand In hyperthyroidism, there is tachycardia , tremor, warm hands, eye signs, diffused goitre, weight loss despite increase appetide 40
Hyperthyroidism Investigations Serum TSH is suppressed, free T 4 or T 3 are raised Thyroid per oxidase (TPO) and thyroglobulin antibodies are present in most cases of Graves disease Thyroid stimulating immunoglobulin (TSI) are present in Graves disease 41
Hyperthyroidism Treatment Three options are available 1. Anti thyroid drugs 2. Radio active iodine 3. Surgery 1. Anti thyroid drugs Carbimazole – 20 -40 mg/day 8 hourly or single dose Propylthioracial (PTU) – 100 -200 mg 8 hourly They inhibit the formation of thyroid hormones Propranolol (Beta Blocker) is used for symptomatic relief 42
Hyperthyroidism Treatment Side effects of drugs Carbimazole – rash, nausea, vomiting, arthralgia, agranulocytosis, jaundice PTU – rash, nausea, vomiting, agranulocytosis NOTE – As agranulocytosis is the side effect, therefore, patient is advised if he has sore throat, he should report to hospital for investigation 43
Hyperthyroidism Treatment (cont) 2. Radioactive Iodine – 131 Iodine Can be given to all patients Is contraindicated in pregnancy and during breast feeding 3. Surgery Subtotal thyroidectomy/thyroidectamy Side effects – laryngeal nerve palsy occur in 1% Transient hypocalcemia up to 10% Permanent hypoparathyroidism < 1% 44

Hyperthyroidism in Pregnancy During pregnancy Propylthioracial (PTU) is preferred because there are reports of congenital abnormalities with Carbimazole TSI – thyroid stimulating immunoglobulin cross the placenta and stimulate fetal thyroid Carbimazole and PTU cross the placenta T 4 (Thyroxin) very poorly crosses the placenta If necessary surgery can be performed in second semester of the pregnancy 45
Thank you 46