The Urinary System also known as The Excretory





















- Slides: 93
The Urinary System also known as The Excretory System
Function
Function - To remove waste products that have accumulated in blood. - Maintain the p. H of blood at about 7. 2 - Produce the hormone erythropoeietin (EPO).
The Urinary System • Cells produce water and carbon dioxide as byproducts of metabolic breakdown of sugars, fats, and proteins. • Chemical groups such as nitrogen, sulfur, and phosphorous must be stripped from the large molecules, to which they were formerly attached, as part of preparing them for energy conversion.
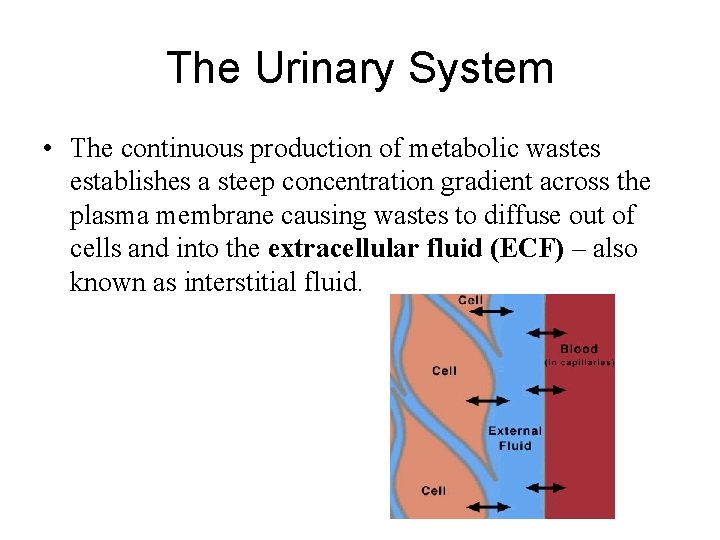
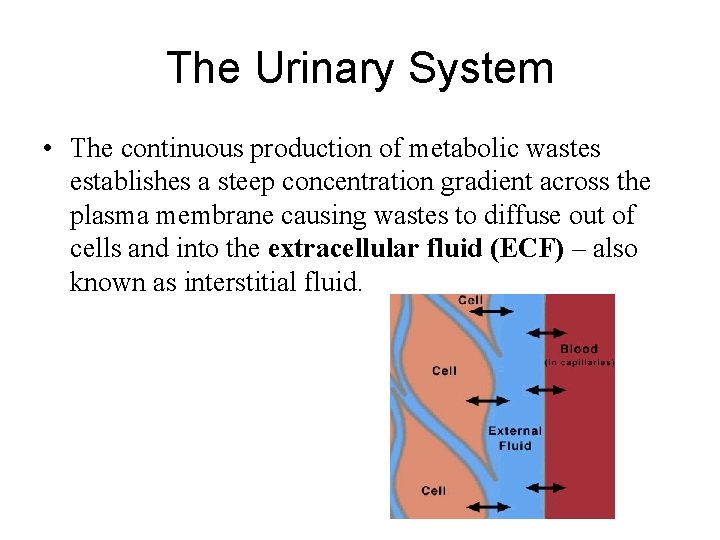
The Urinary System • The continuous production of metabolic wastes establishes a steep concentration gradient across the plasma membrane causing wastes to diffuse out of cells and into the extracellular fluid (ECF) – also known as interstitial fluid.

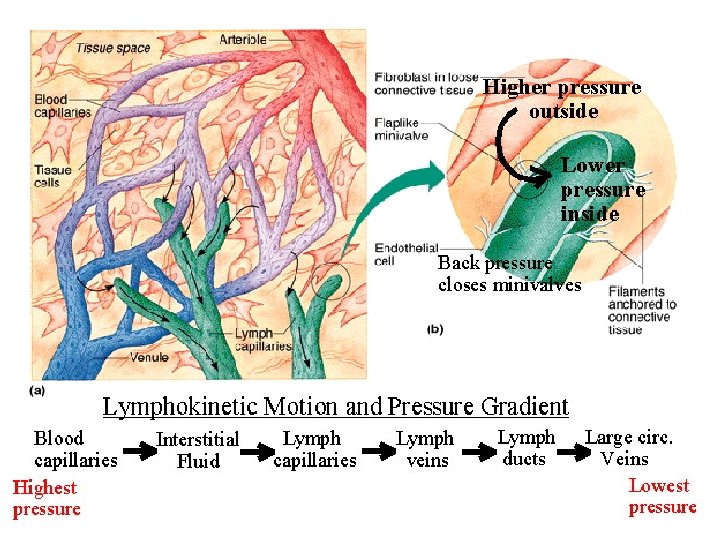
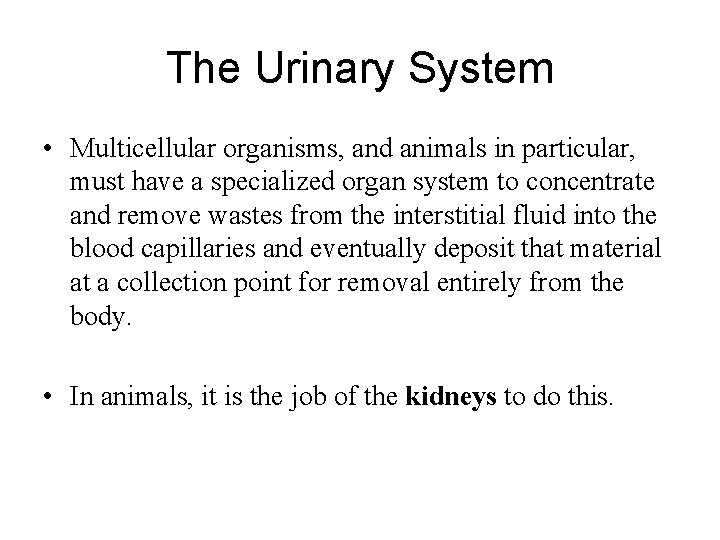
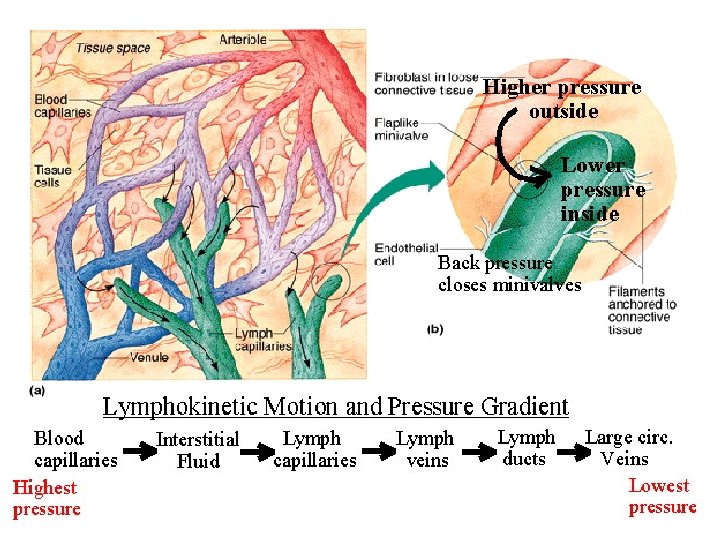
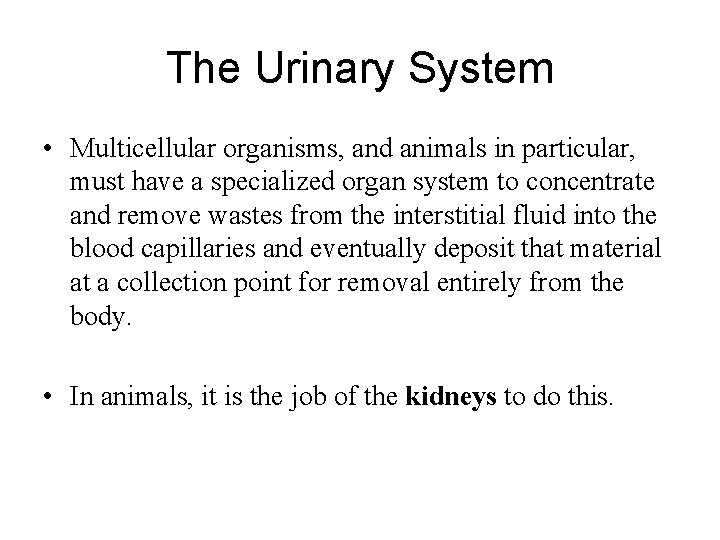
The Urinary System • Multicellular organisms, and animals in particular, must have a specialized organ system to concentrate and remove wastes from the interstitial fluid into the blood capillaries and eventually deposit that material at a collection point for removal entirely from the body. • In animals, it is the job of the kidneys to do this.
Homeostatic Functions • In addition to filtering blood to remove toxic waste products, the kidneys also control water balance, p. H, and levels of sodium, potassium, bicarbonate, and calcium ions in the blood. • They also secrete a hormone (erythropoietin – EPO) that stimulates red blood cell production and activate vitamin D production in the skin.
Structures
Gross Anatomy Organs
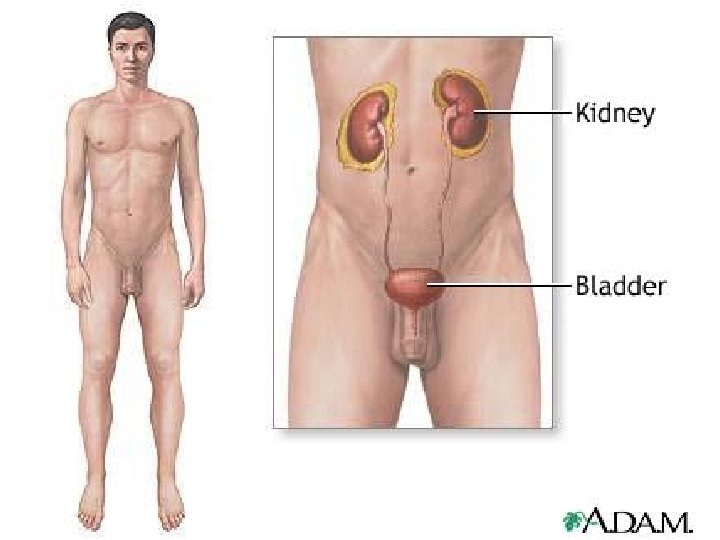
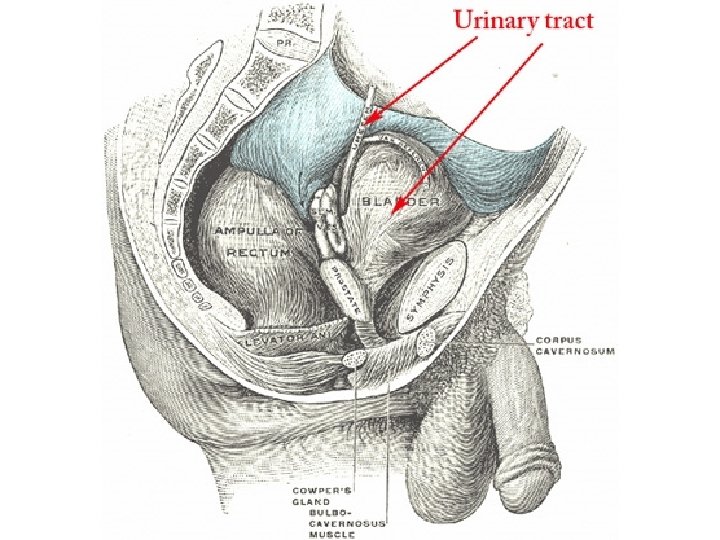
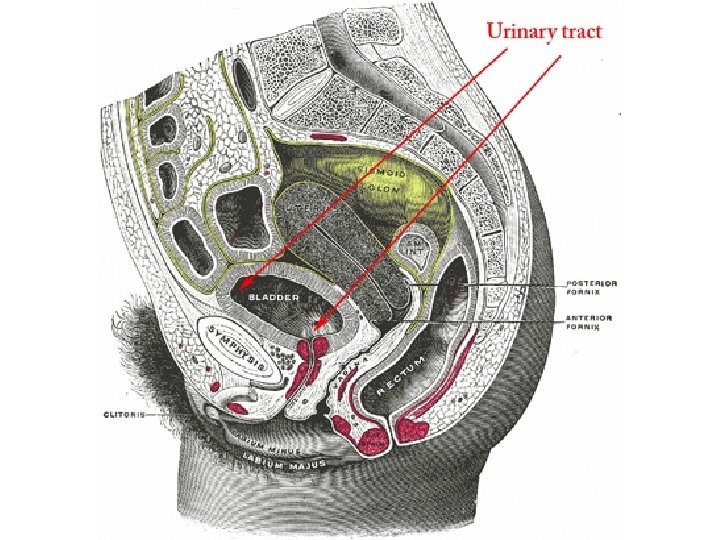
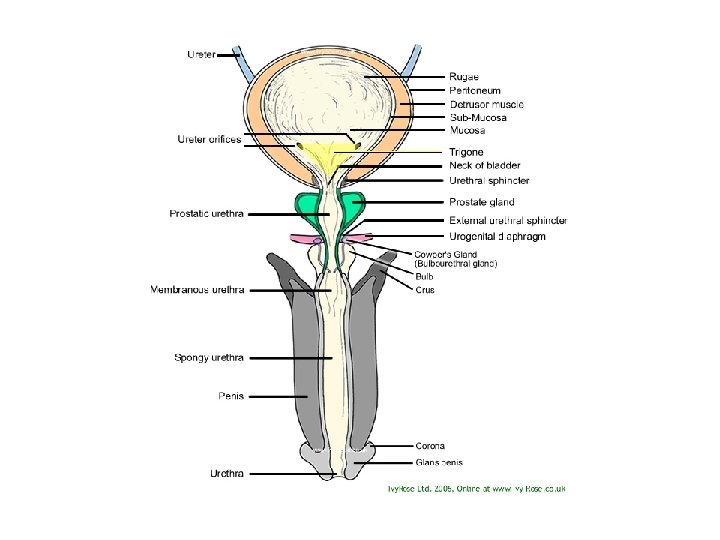
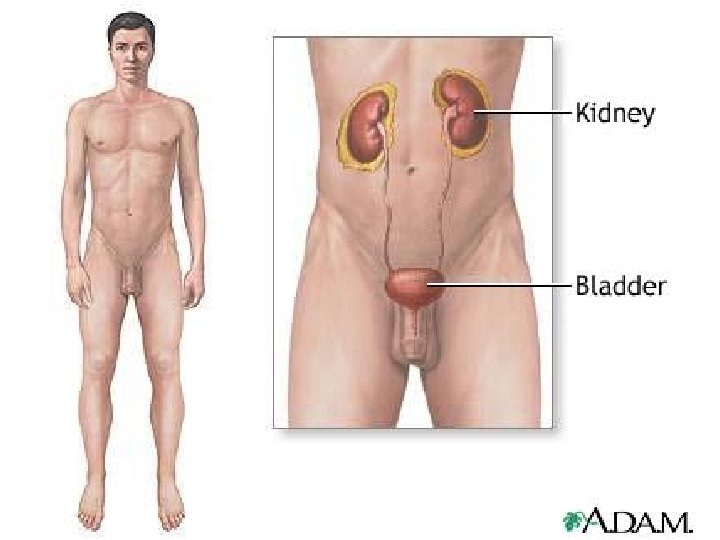
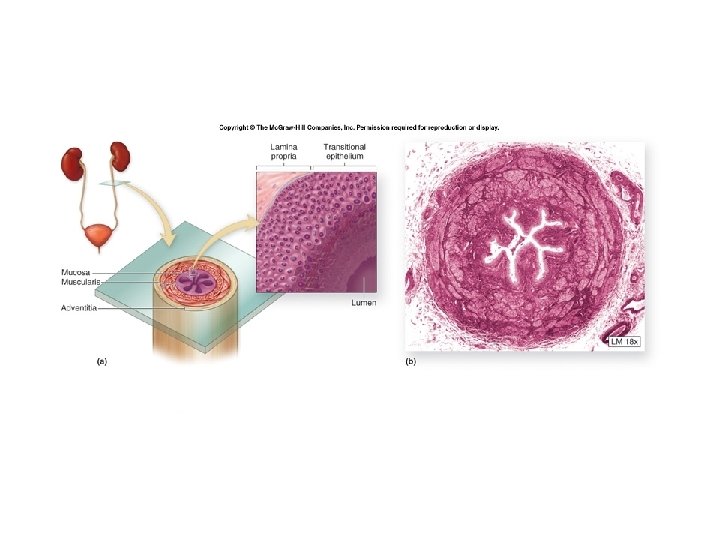
The Urinary System • The urinary system is composed of the following organs; – two kidneys, – two ureters, – one urinary bladder and – one urethra.




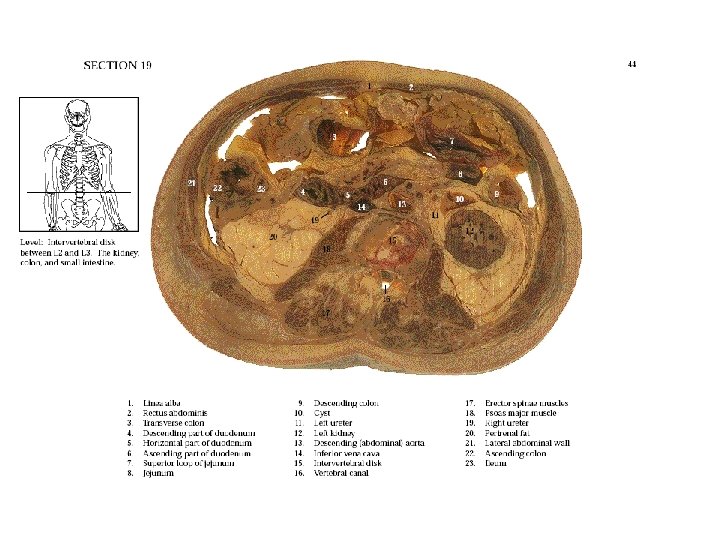
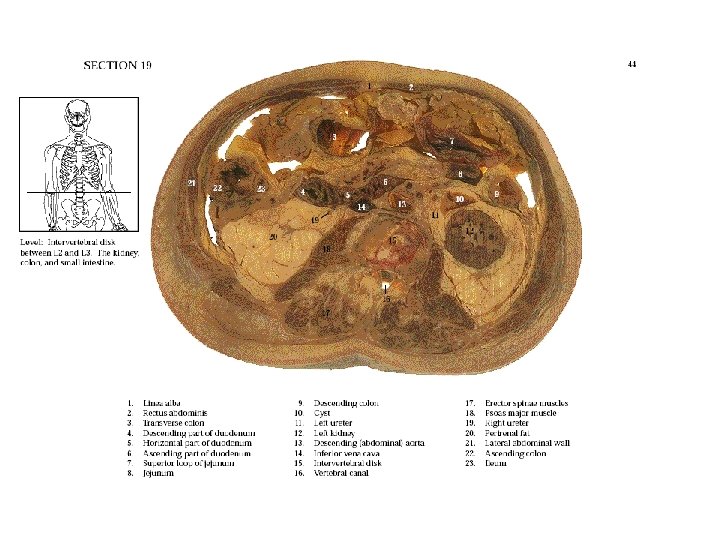
Gross Anatomy • The following is a series of cross sections through a human cadaver showing the placement of organs in the body. • Look for the excretory system organs!






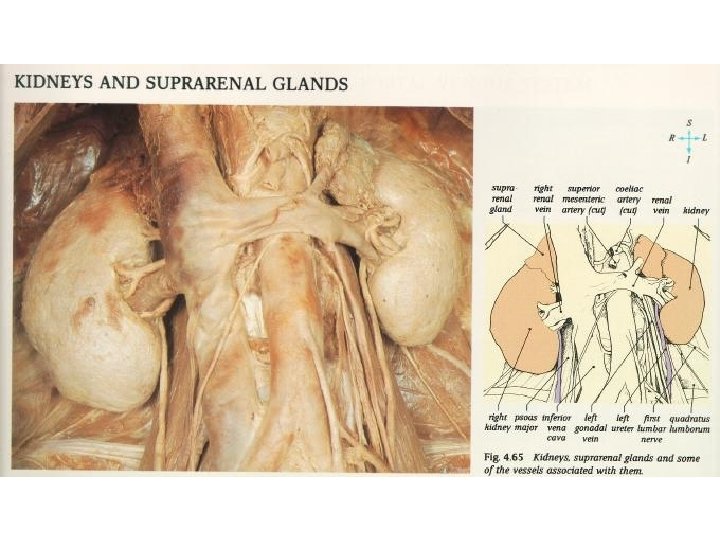
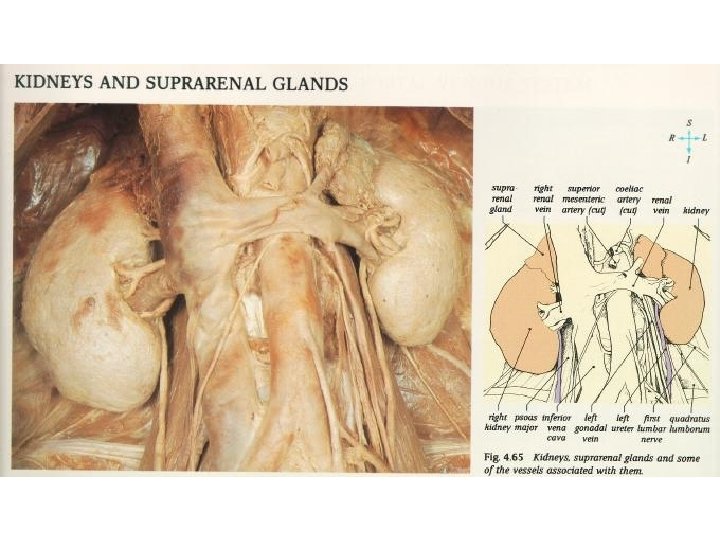
The Kidneys
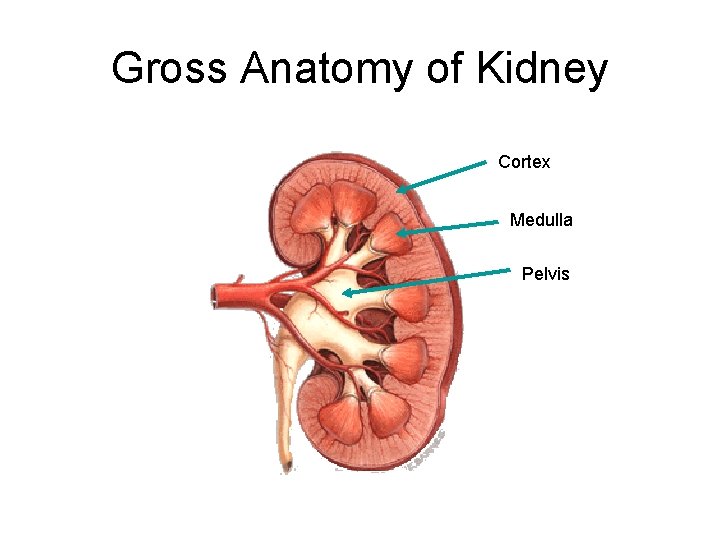
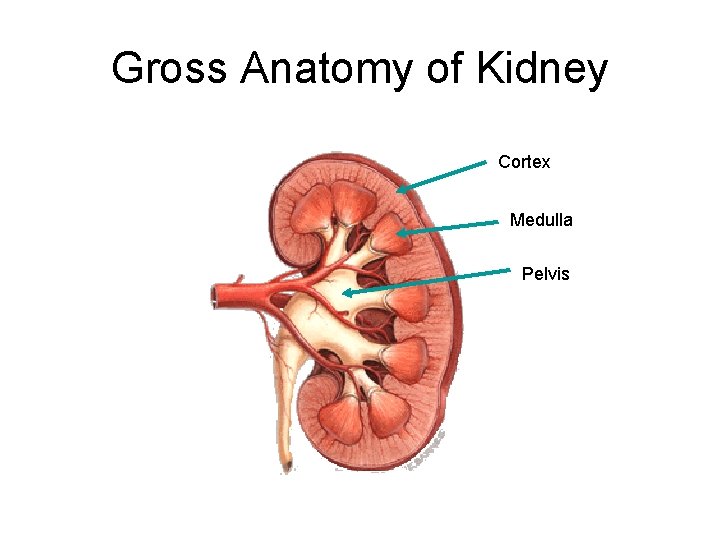
Gross Anatomy of Kidney Cortex Medulla Pelvis
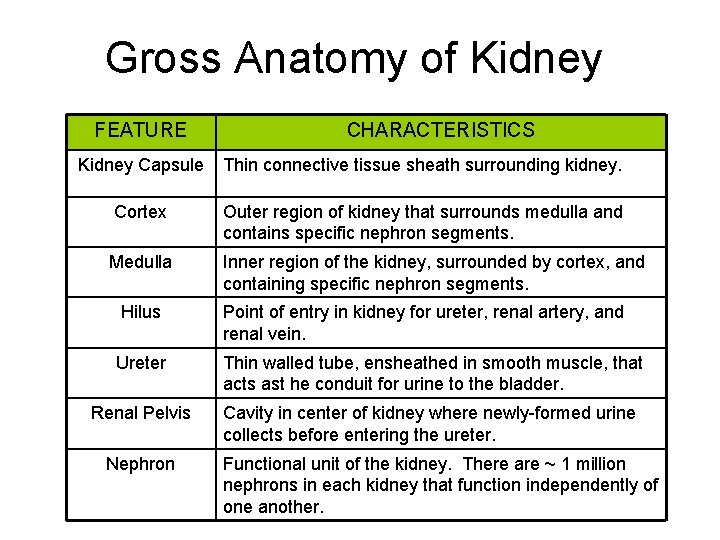
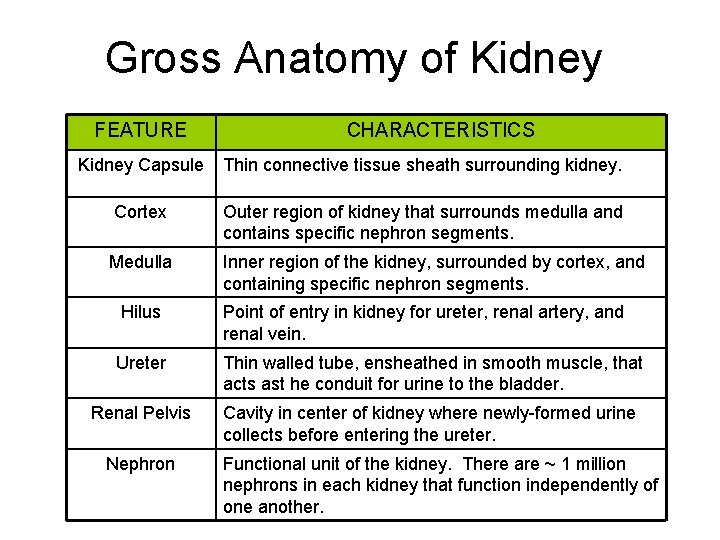
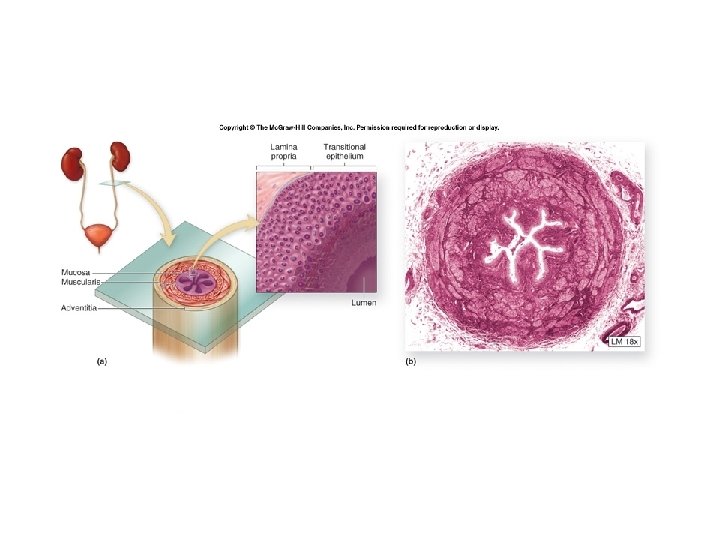
Gross Anatomy of Kidney FEATURE CHARACTERISTICS Kidney Capsule Thin connective tissue sheath surrounding kidney. Cortex Outer region of kidney that surrounds medulla and contains specific nephron segments. Medulla Inner region of the kidney, surrounded by cortex, and containing specific nephron segments. Hilus Point of entry in kidney for ureter, renal artery, and renal vein. Ureter Thin walled tube, ensheathed in smooth muscle, that acts ast he conduit for urine to the bladder. Renal Pelvis Cavity in center of kidney where newly-formed urine collects before entering the ureter. Nephron Functional unit of the kidney. There are ~ 1 million nephrons in each kidney that function independently of one another.
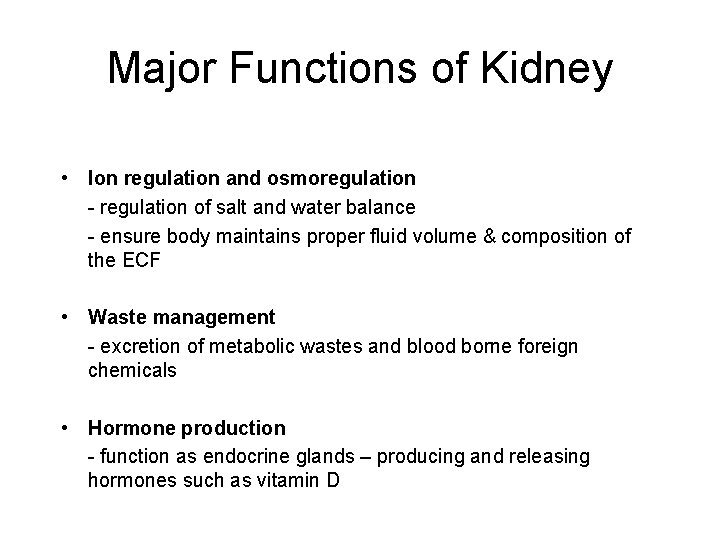
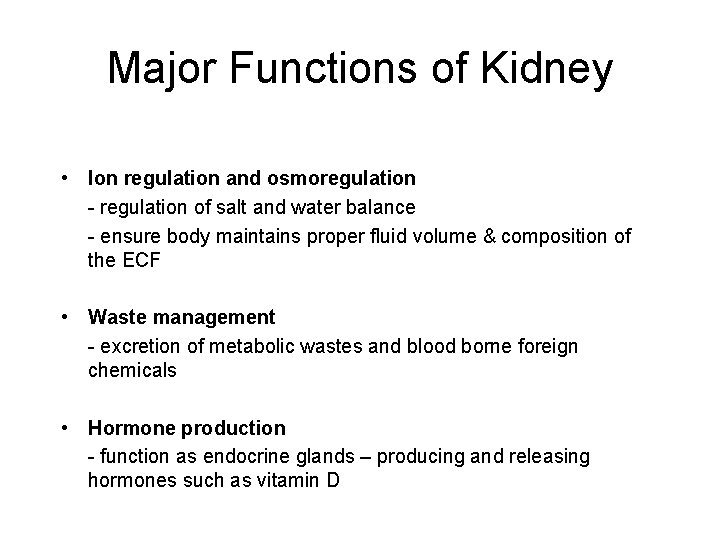
Major Functions of Kidney • Ion regulation and osmoregulation - regulation of salt and water balance - ensure body maintains proper fluid volume & composition of the ECF • Waste management - excretion of metabolic wastes and blood borne foreign chemicals • Hormone production - function as endocrine glands – producing and releasing hormones such as vitamin D
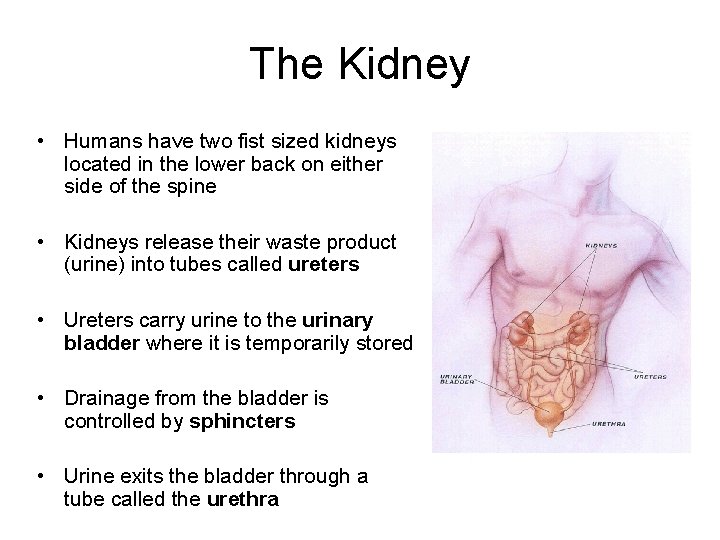
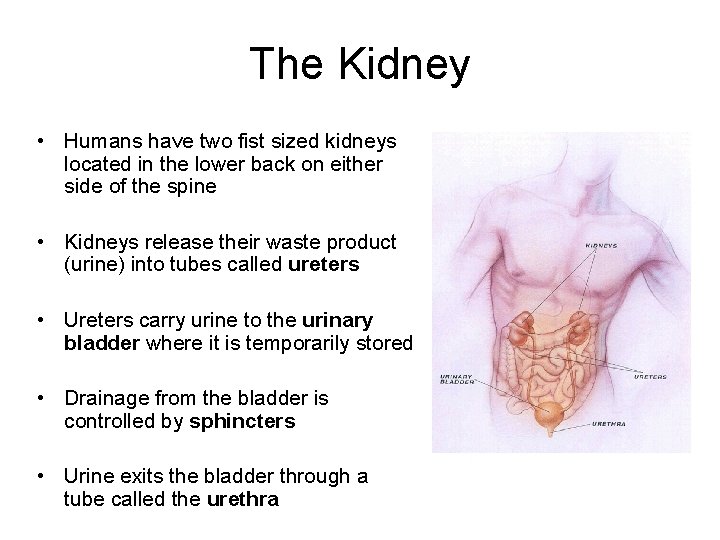
The Kidney • Humans have two fist sized kidneys located in the lower back on either side of the spine • Kidneys release their waste product (urine) into tubes called ureters • Ureters carry urine to the urinary bladder where it is temporarily stored • Drainage from the bladder is controlled by sphincters • Urine exits the bladder through a tube called the urethra
Excretion of Cellular Waste The main metabolic waste products all have nitrogen as a major component. - Urea - Uric Acid - Creatinine
Urea • Produced in the liver from the breakdown of excess amino acids that are the building blocks of proteins • Amine group (NH 2) is removed to release the rest of the amino acid molecule – which can then be converted into carbohydrates or fats • The amine group can combine with a hydrogen ion to form toxic ammonia • Ammonia is transformed in the liver into less toxic urea before being released into the bloodstream
Uric Acid and Creatinine • Uric Acid is usually produced by the breakdown of nucleic acids such as DNA and RNA • Creatinine is a waste product of muscle action
The Kidney • The human kidneys: – are two bean-shaped organs, one on each side of the backbone. – Represent about 0. 5% of the total weight of the body, – but receive 20– 25% of the total arterial blood pumped by the heart. – Each contains from one to two million nephrons.



The Ureters
The Urinary Bladder

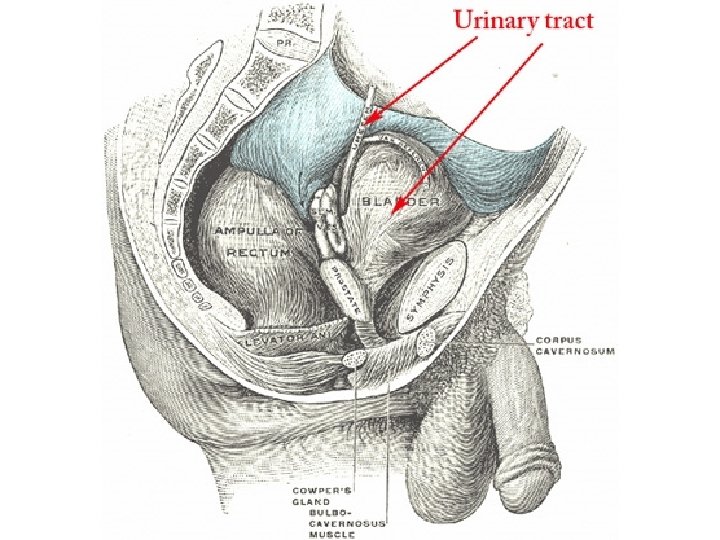
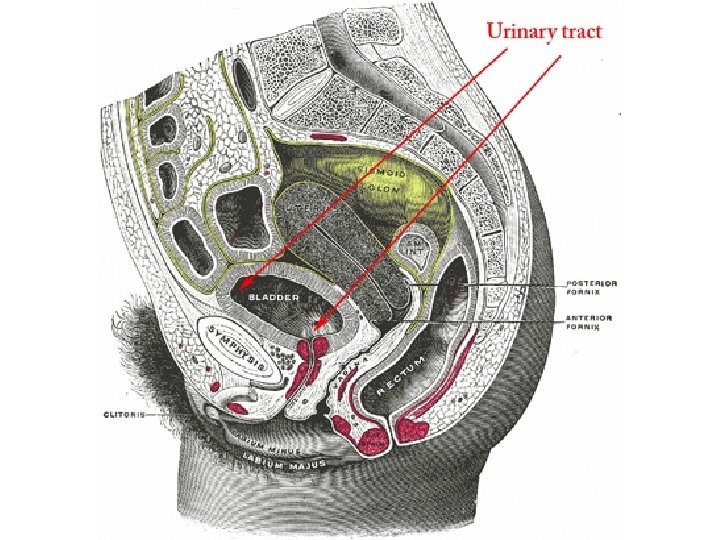
The Urethra
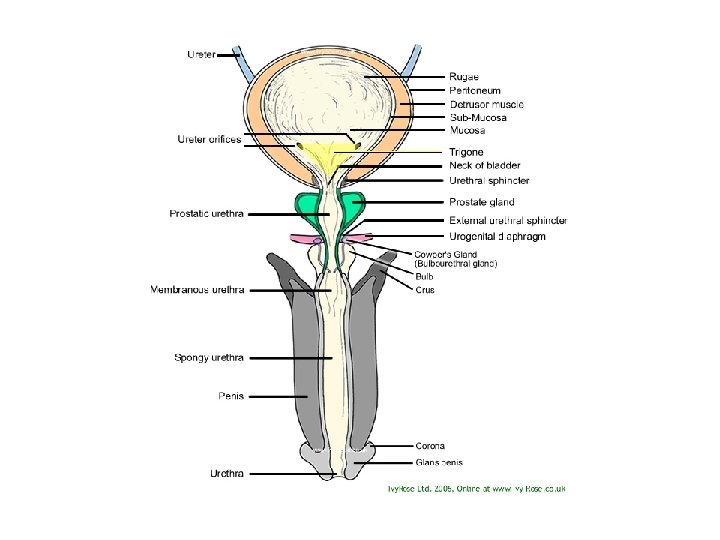
Micturition Reflex • This animation shows how urination, medically referred to as micturition, is accomplished. http: //highered. mcgrawhill. com/sites/0072495855/student_view 0/chapter 27/animati on__micturition_reflex. html
Microanatomy Microscopic Structures
The Nephron Structure

Nephrons • The kidney is composed of one million to two million nephrons. • It is in the nephrons that the blood is cleaned of its waste products: – Water, minerals, uric acid, glucose, protein, lipids, bilirubin (breakdown product of erythrocytes), alkaline phosphatase, etc…
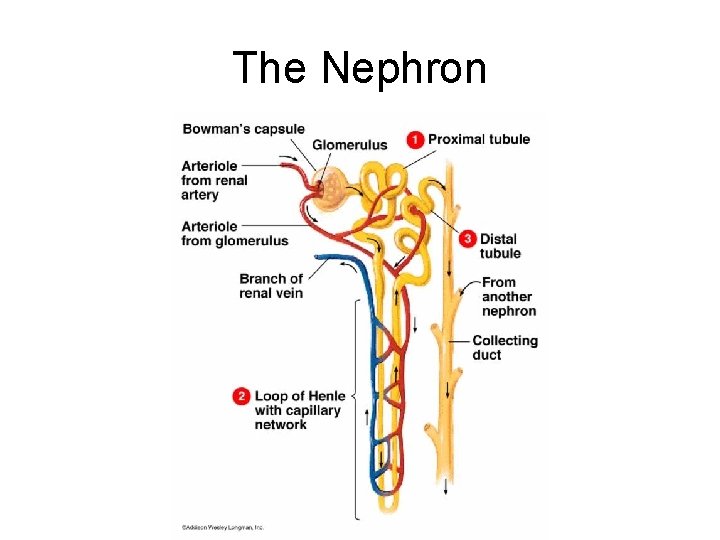
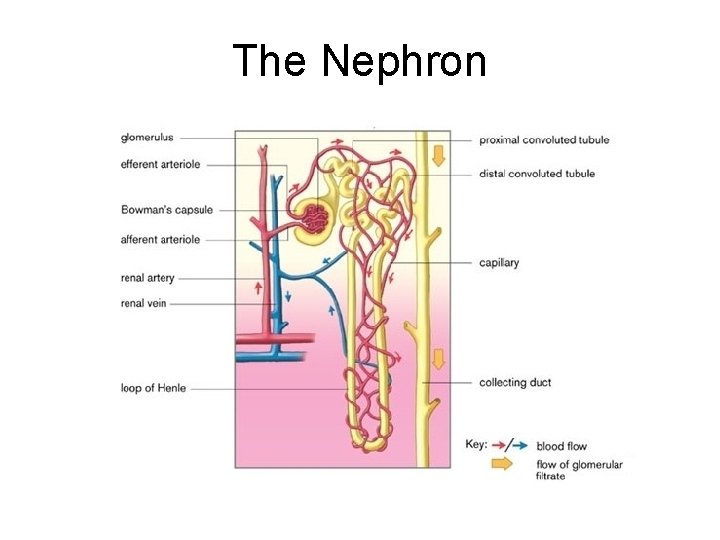
The Nephron • The tubes of the nephron are surrounded by cells, and a network of blood vessels spreads throughout the tissue • By controlling what enters or leaves the nephrons, the kidneys keep the levels of water, ions, and other materials in our body fluids relatively constant
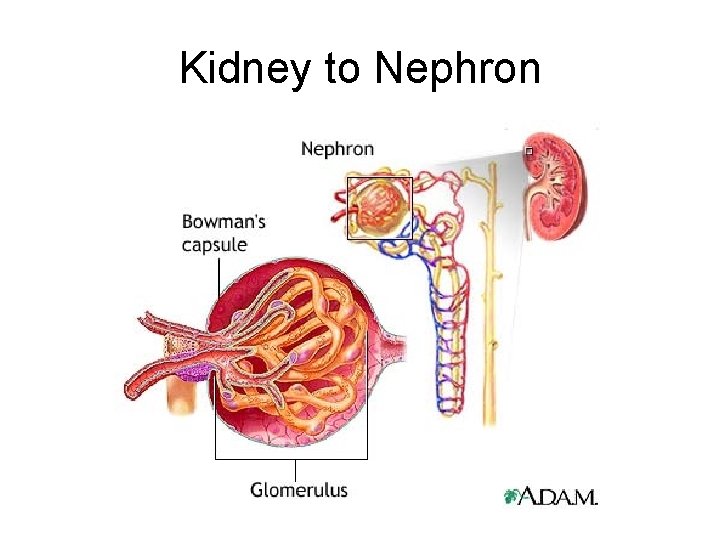
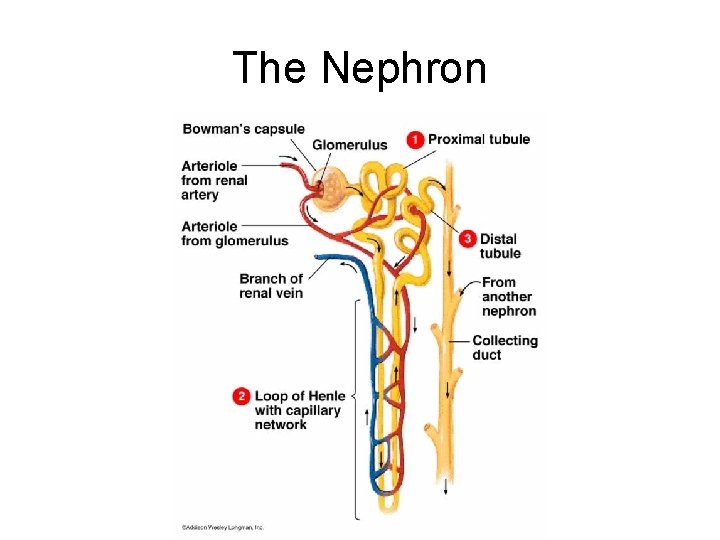
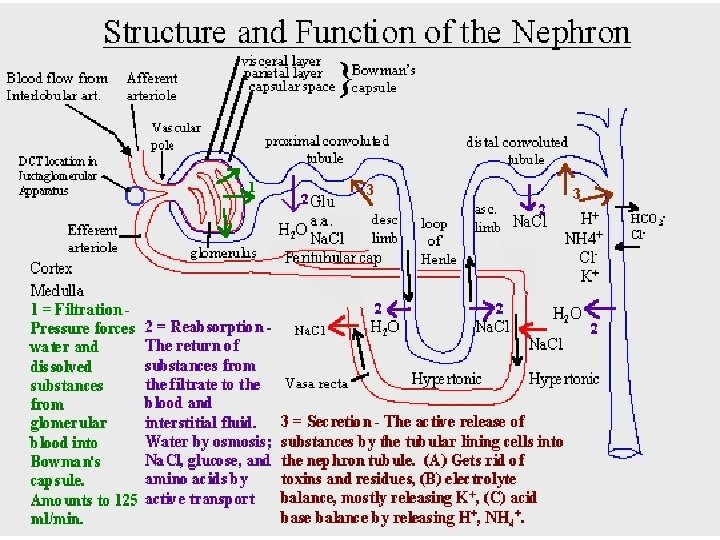
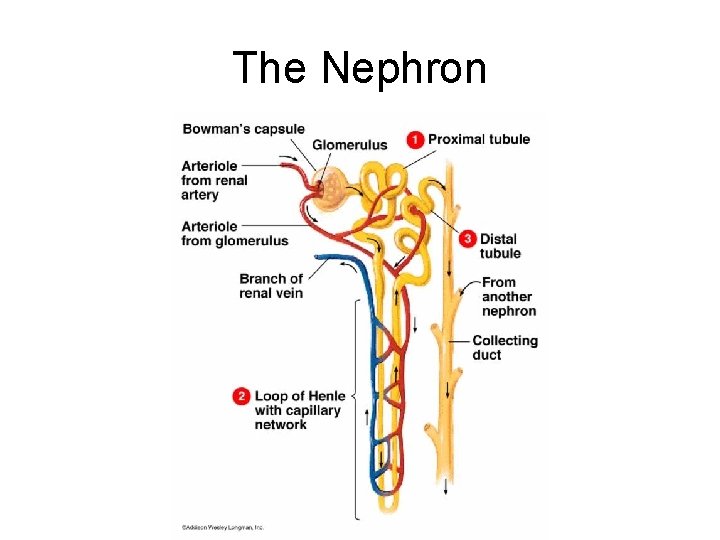
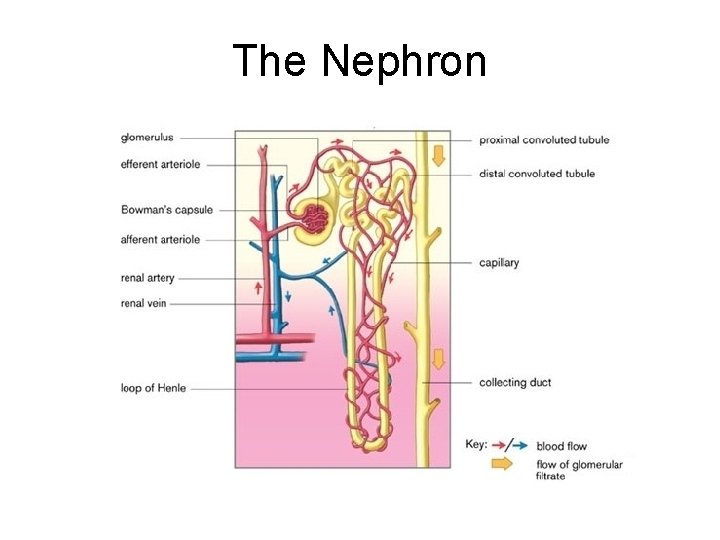
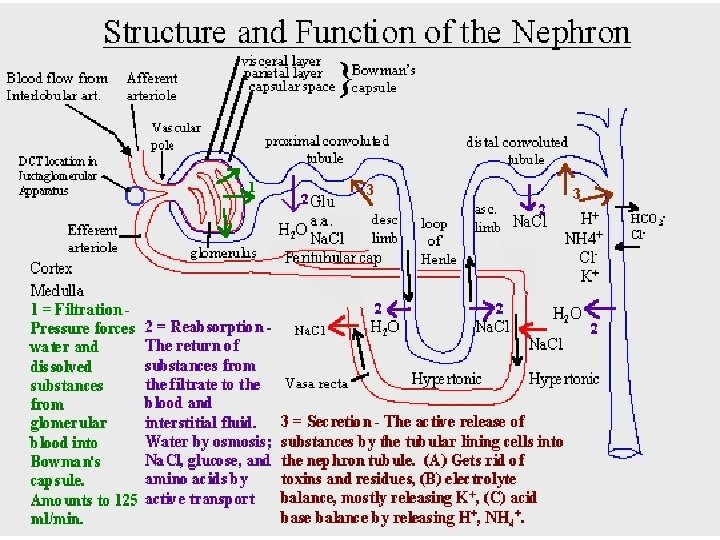
The Nephron Each nephron consists of five parts: - Bowman’s Capsule and Glomerulus - Proximal Convoluted Tubule - Loop of Henle (ascending & descending) - Distal Convoluted Tubule - Collecting Duct
The Nephron
The Nephron
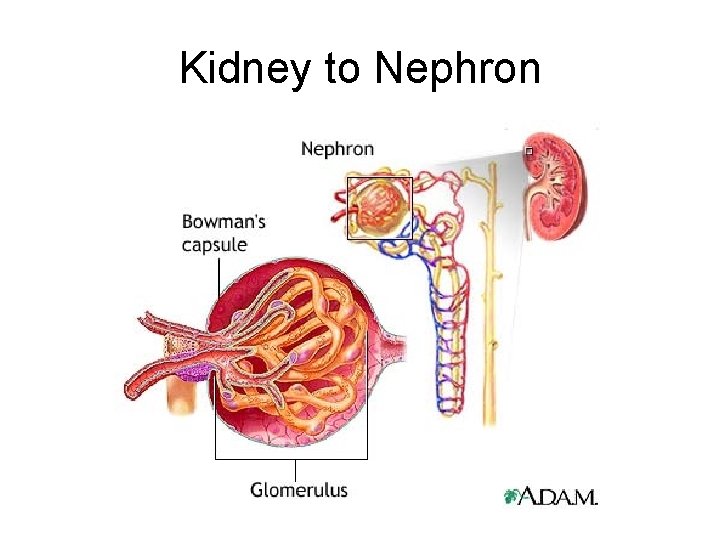
Kidney to Nephron
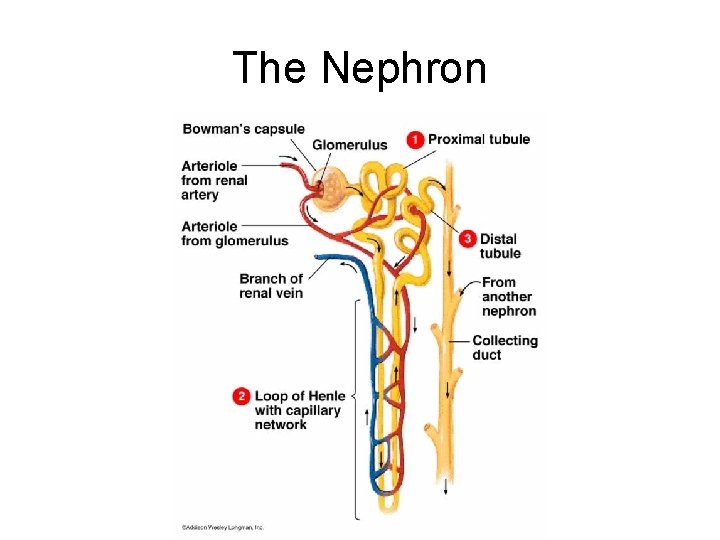
The Nephron
The Nephron Function
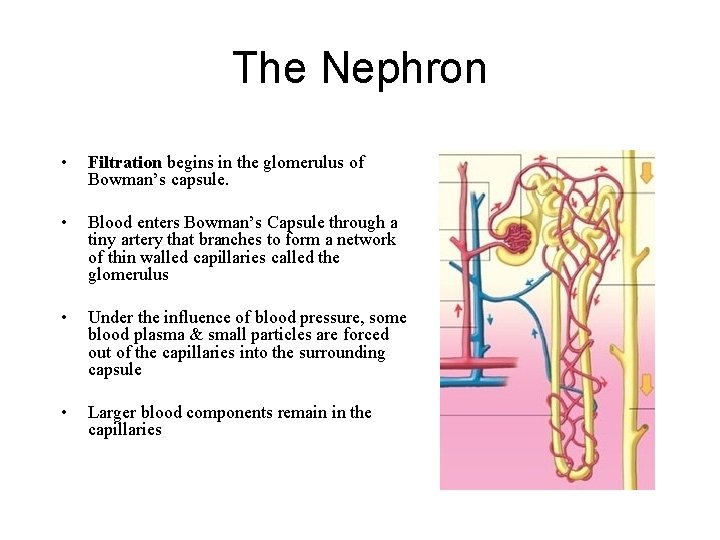
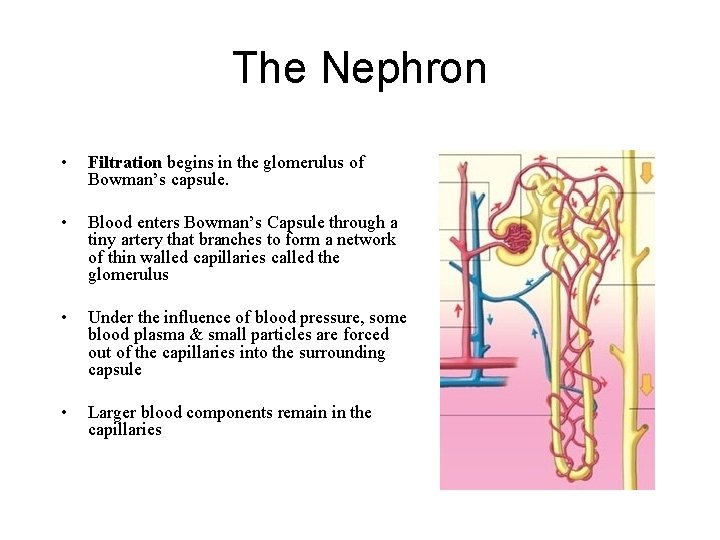
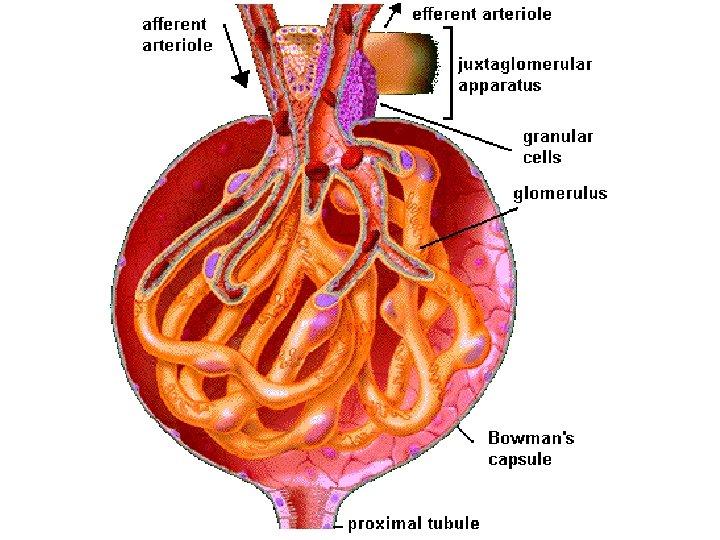
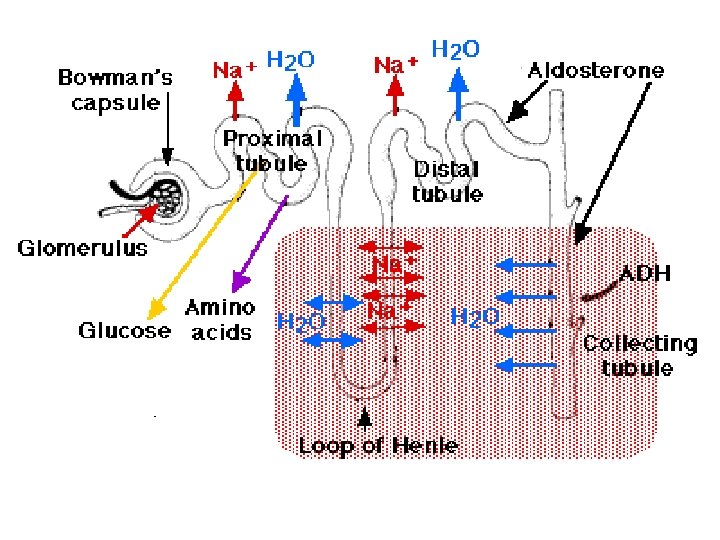
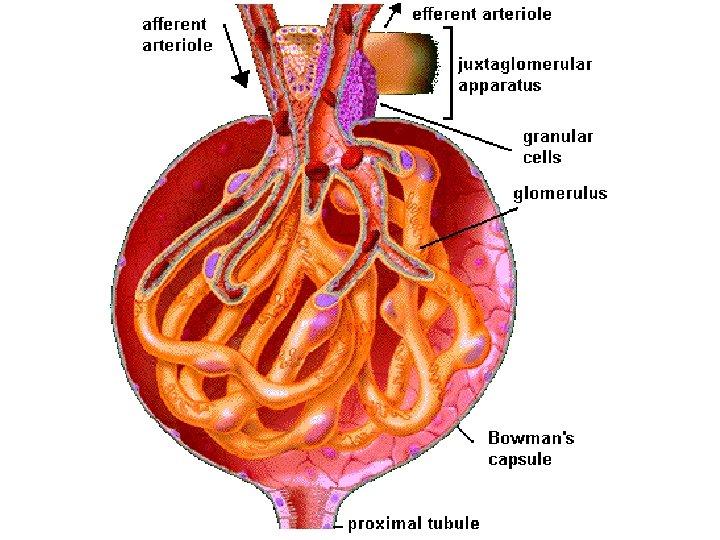
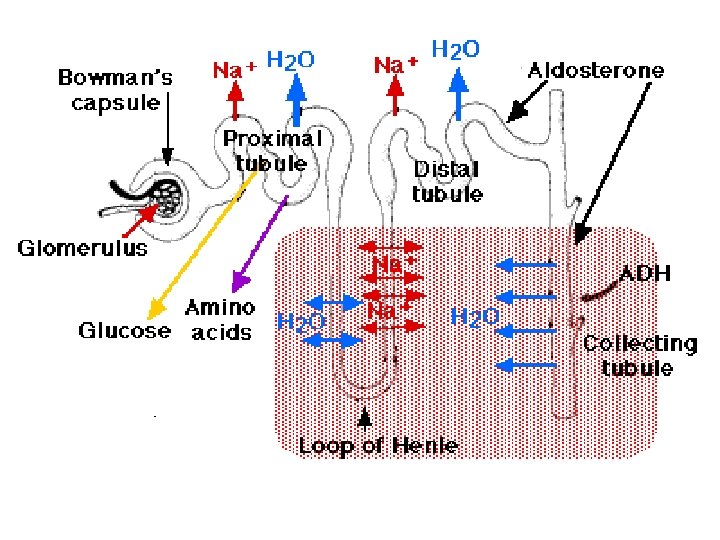
The Nephron • Filtration begins in the glomerulus of Bowman’s capsule. • Blood enters Bowman’s Capsule through a tiny artery that branches to form a network of thin walled capillaries called the glomerulus • Under the influence of blood pressure, some blood plasma & small particles are forced out of the capillaries into the surrounding capsule • Larger blood components remain in the capillaries
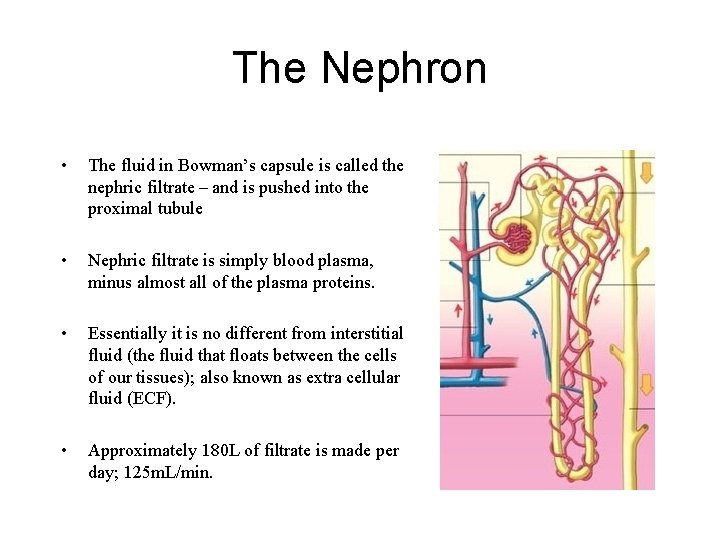
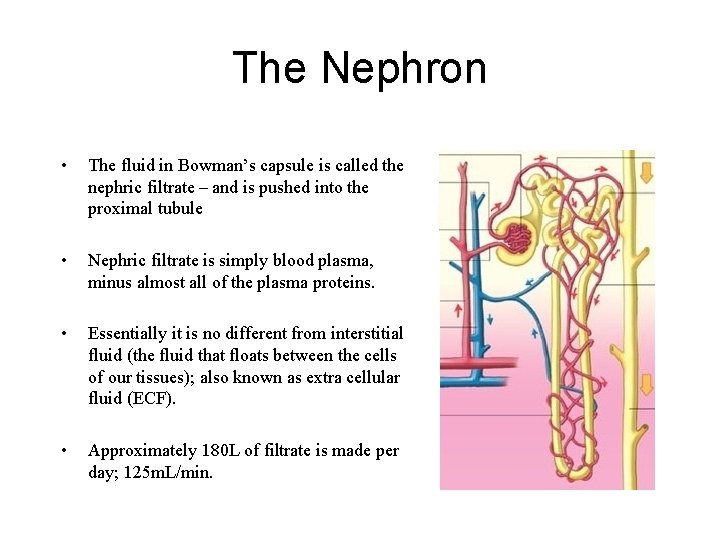
The Nephron • The fluid in Bowman’s capsule is called the nephric filtrate – and is pushed into the proximal tubule • Nephric filtrate is simply blood plasma, minus almost all of the plasma proteins. • Essentially it is no different from interstitial fluid (the fluid that floats between the cells of our tissues); also known as extra cellular fluid (ECF). • Approximately 180 L of filtrate is made per day; 125 m. L/min.

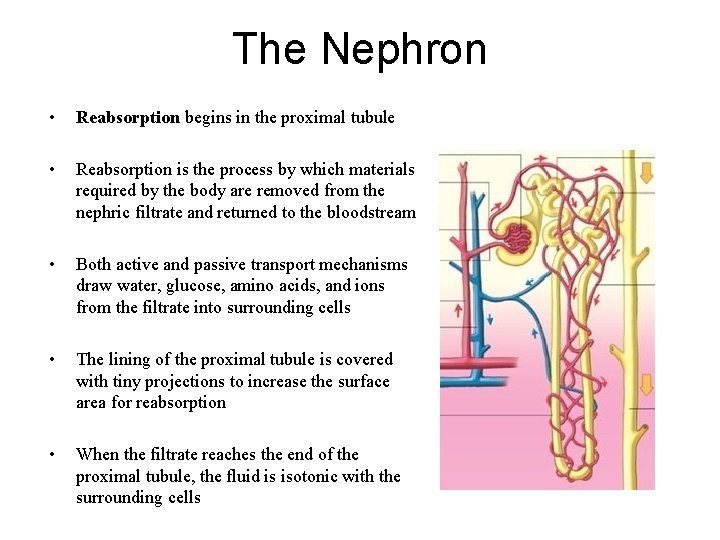
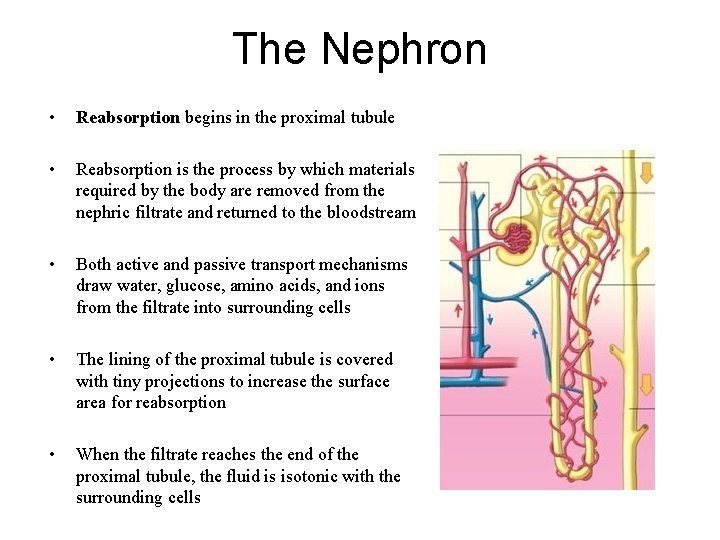
The Nephron • Reabsorption begins in the proximal tubule • Reabsorption is the process by which materials required by the body are removed from the nephric filtrate and returned to the bloodstream • Both active and passive transport mechanisms draw water, glucose, amino acids, and ions from the filtrate into surrounding cells • The lining of the proximal tubule is covered with tiny projections to increase the surface area for reabsorption • When the filtrate reaches the end of the proximal tubule, the fluid is isotonic with the surrounding cells
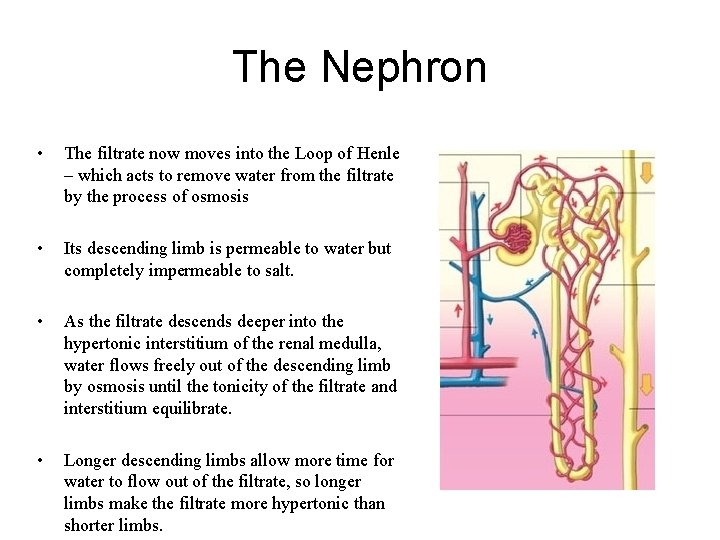
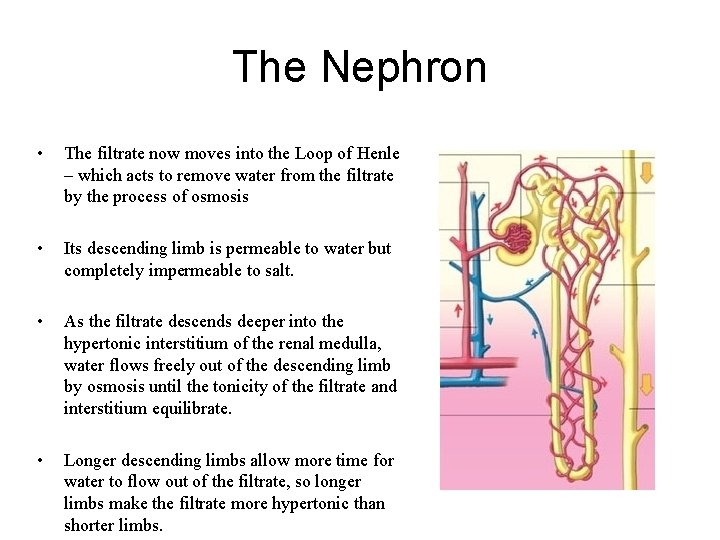
The Nephron • The filtrate now moves into the Loop of Henle – which acts to remove water from the filtrate by the process of osmosis • Its descending limb is permeable to water but completely impermeable to salt. • As the filtrate descends deeper into the hypertonic interstitium of the renal medulla, water flows freely out of the descending limb by osmosis until the tonicity of the filtrate and interstitium equilibrate. • Longer descending limbs allow more time for water to flow out of the filtrate, so longer limbs make the filtrate more hypertonic than shorter limbs.
The Nephron • Unlike the descending limb, the ascending limb of Henle's loop is impermeable to water, a critical feature of the countercurrent exchange mechanism employed by the loop. • The ascending limb actively pumps sodium out of the filtrate, generating the hypertonic interstitium that drives countercurrent exchange. • In passing through the ascending limb, the filtrate grows hypotonic since it has lost much of its sodium content. This hypotonic filtrate is passed to the distal convoluted tubule in the renal cortex.
The Nephron • Chloride ions follow the sodium ions because of electrical attraction • Also, as the water concentration in the filtrate decreases, the chloride ion concentration in the filtrate increases • This results in the diffusion of even more chloride ions out of the ascending loop
The Nephron • Secretion begins in the distal convoluted tubule. • It is the release by active transport of substances into the filtrate. It is accomplished by the tubular lining cells. • It is done for three purposes: – Removal of toxins, vitamins, hormones and drugs. – Electrolyte balance. – Acid-base balance
The Nephron • The fluid from a number of nephrons moves from the distal tubules into a common collecting duct • The permeability of the distal tubule and collecting duct is under hormonal control • Antidiuretic hormone (ADH) is secreted by the anterior pituitary gland increases the permeability of the distal tubule and collecting duct • ADH allows more water to be removed from the filtrate when the body needs to conserve water
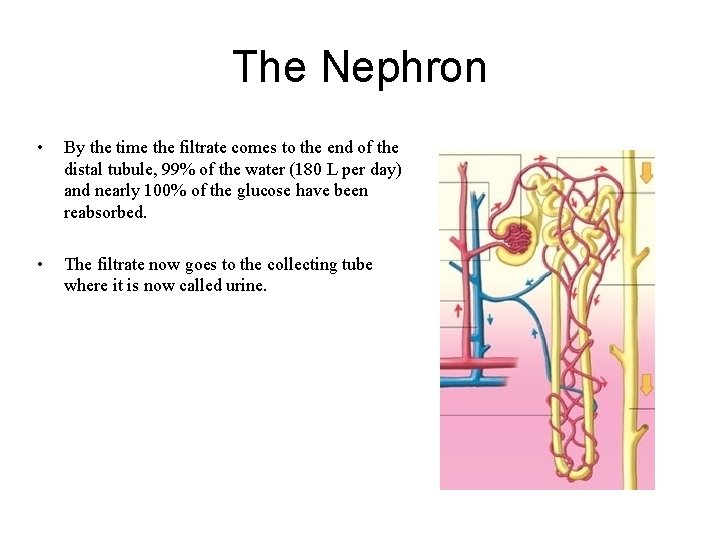
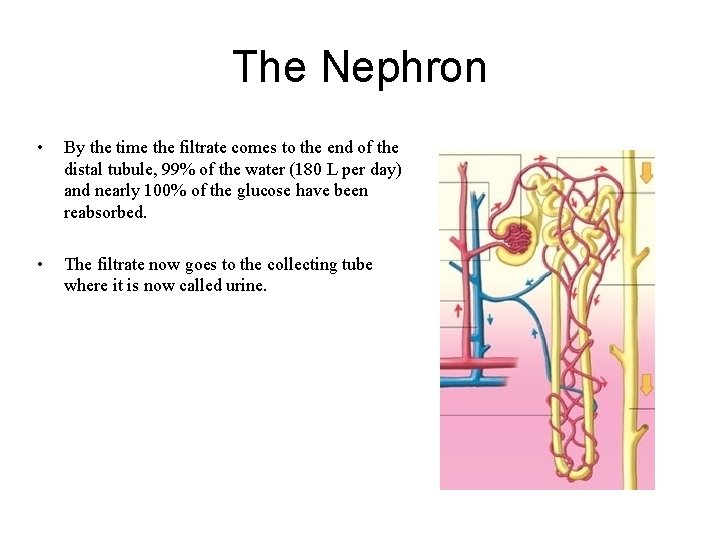
The Nephron • By the time the filtrate comes to the end of the distal tubule, 99% of the water (180 L per day) and nearly 100% of the glucose have been reabsorbed. • The filtrate now goes to the collecting tube where it is now called urine.


Control of Urine Output
Urine Output • The permeability of the distal and collecting tubes is controlled by a hormone called anti-diuretic hormone (ADH); also known as vasopressin. • When it enters the kidney, ADH makes the walls of the renal tubules and collecting ducts more permeable to water, so that more water is reabsorbed into the bloodstream. Less urine is formed, more water is retained. • Alcohol and caffeine block the release of ADH leading to low permeability and therefore increased urine production.
Kidneys & Blood p. H
Blood p. H • Blood p. H should be around 7. 4. • This is maintained by active transport of H+ out of the blood into the nephric filtrate. • Urine p. H can vary from 4. 5 to 8. 0; normal urine p. H is 6. 0.
Blood p. H • Respiratory system works together with kidney to control blood p. H. • There are buffers in our blood that control blood p. H. • H+ + HCO 31 - H 2 CO 3 H 2 O + CO 2
Blood p. H • H+ + HCO 31 - • Breathing rate will affect the equilibria of the reactions above. • High rate of breathing will shift reactions to the right and increase p. H. Low rate of breathing will shift reactions to the left and increase p. H. • H 2 CO 3 H 2 O + CO 2
Diseases of the Excretory System
Diseases Some diseases of the Excretory System are… • • • Gout Kidney stones Urinary Tract Infections (UTI) Diabetes insipidus Liddle’s syndrome (the following descriptions come from Wikipedia)
Gout (also called metabolic arthritis) is a disease due to an inborn disorder of the uric acid metabolism. In this condition monosodium urate crystals are deposited on the articular cartilage of joints and in the particular tissue like tendons. This provokes an inflammatory reaction of these tissues. These deposits often increase in size and burst through the skin to form sinuses discharging a chalky white material. Normally, the human bloodstream only carries small amounts of uric acid. However, if the blood has an elevated concentration of uric acid, uric acid crystals are deposited in the cartilage and tissue surrounding joints. Elevated blood levels of uric acid can also result in uric kidney stones.

Gout
Kidney stones, also known as nephrolithiasis, urolithiasis or renal calculi, are solid concretions (crystal aggregations) of dissolved minerals in urine found inside the kidneys or ureters. They vary in size from as small as a grain of sand to as large as a grapefruit. Kidney stones typically leave the body in the urine stream; if they grow relatively large before passing (on the order of at least 2 -3 millimeters), obstruction of a ureter and distention with urine can cause severe pain most commonly felt in the flank, lower abdomen and groin. Such pain, called renal colic, often comes in waves and can be particularly severe. Nausea is associated with this particular pain primarily due to the embyrological association of the kidneys and the intestinal tract. Recurrence rates are estimated at about 10% per year. Kidney stones are totally unrelated to gallstones. http: //www. youtube. com/watch? v=Yev. E 6 r. YV 2 MA http: //www. youtube. com/watch? v=4 UM 90 Rx. Vbno&NR=1

Kidney Stones
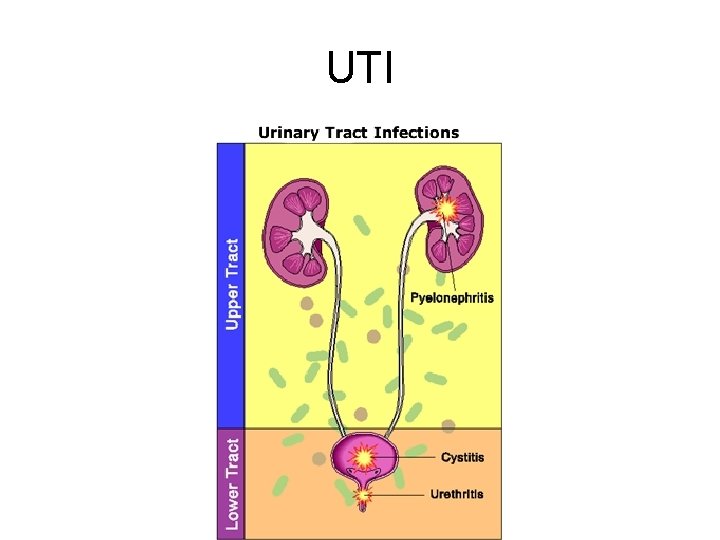
A urinary tract infection (UTI) is a bacterial infection that affects any part of the urinary tract. Although urine contains a variety of fluids, salts, and waste products, it usually does not have bacteria in it. When bacteria get into the bladder or kidney and multiply in the urine, they cause a UTI. The most common type of UTI is a bladder infection which is also often called cystitis. Another kind of UTI is a kidney infection, known as pyelonephritis, and is much more serious. Although they cause discomfort, urinary tract infections are usually quickly and easily treated by seeing a doctor promptly.
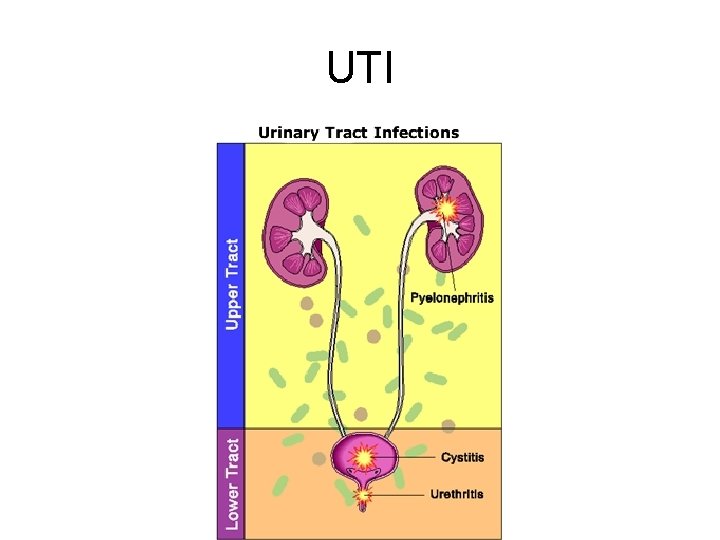
UTI
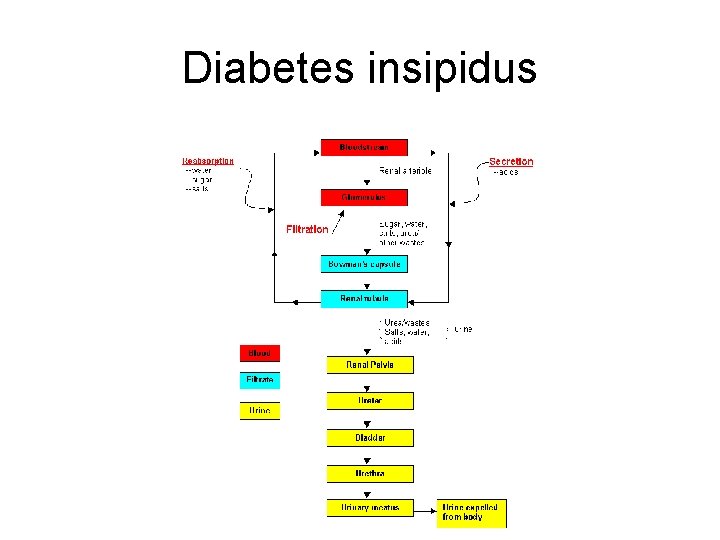
Diabetes insipidus (DI) is a disease characterized by excretion of large amounts of severely diluted urine, which cannot be reduced when fluid intake is reduced. It denotes inability of the kidney to concentrate urine. DI is caused by a deficiency of antidiuretic hormone (ADH), or by an insensitivity of the kidneys to that hormone.
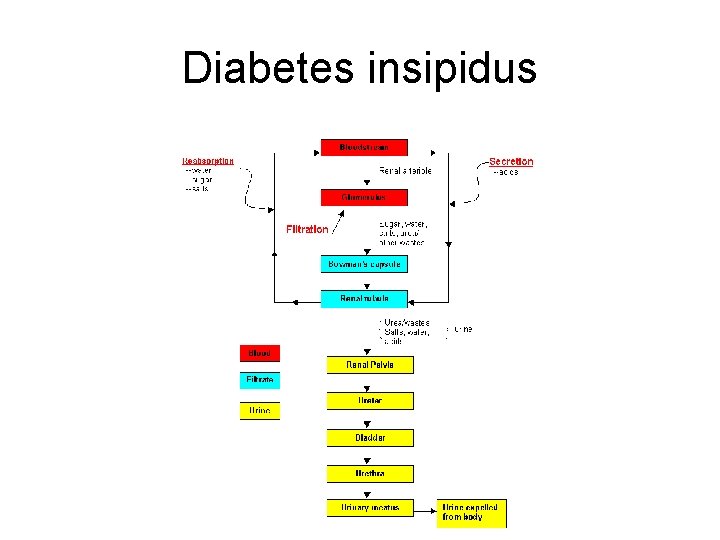
Diabetes insipidus
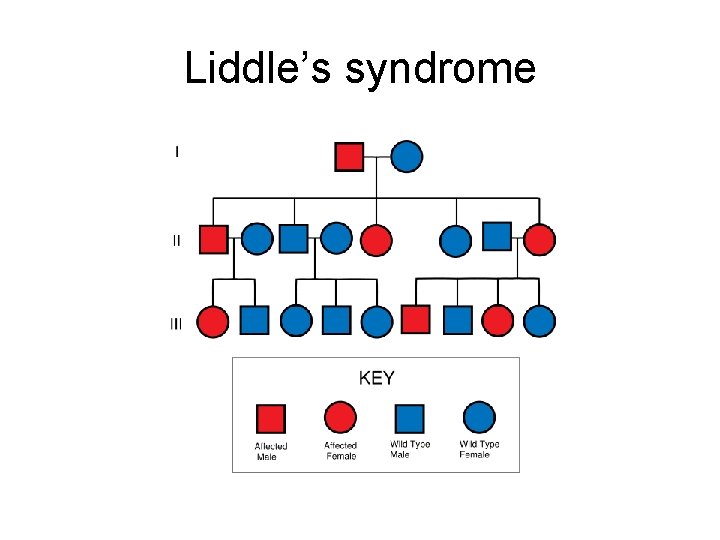
Liddle’s syndrome is caused by a single mutant allele (therefore the syndrome is inherited as a dominant trait) encoding the aldosterone-activated sodium channel in the collecting tubules. The defective channel is always "on" so too much Na+ is reabsorbed and too little is excreted. Where Na+ goes, water goes. The resulting elevated osmotic pressure of the blood produces hypertension (high blood pressure).
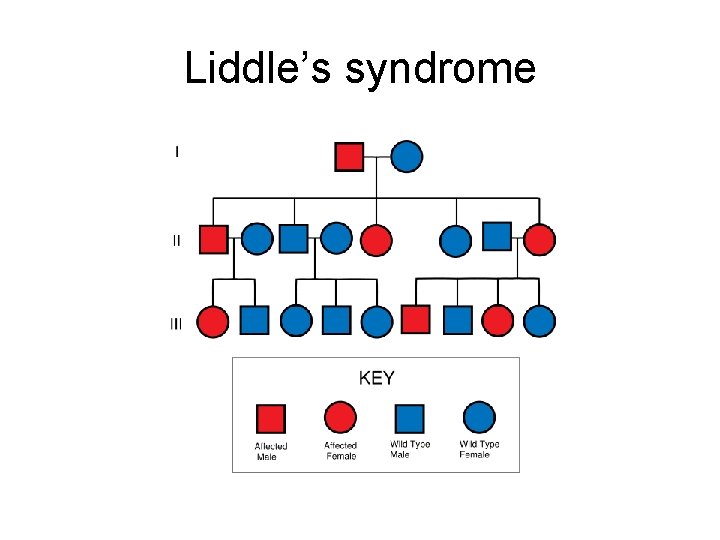
Liddle’s syndrome
The Excretory System also known as The Urinary System THE END