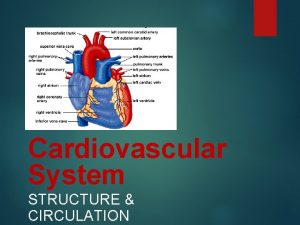
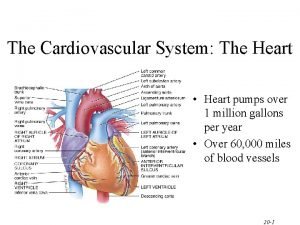
The Cardiovascular System The Heart The Cardiovascular System
- Slides: 47
The Cardiovascular System The Heart
The Cardiovascular System • A closed system of the heart and blood vessels – The heart pumps blood – Blood vessels allow blood to circulate to all parts of the body • The functions of the cardiovascular system – To deliver oxygen and nutrients to cells and tissues – To remove carbon dioxide and other waste products from cells and tissues
The Heart • Location – Thorax between the lungs in the inferior mediastinum • About the size of your fist
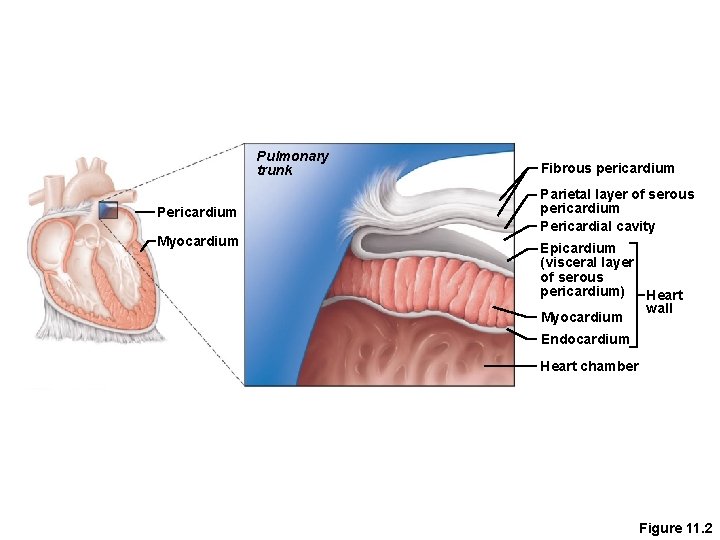
• The Heart: Coverings Pericardium—a double-walled sac – Serous fluid fills the space between the layers of pericardium
• The Heart: Heart Wall Three layers – Epicardium • Outside layer • Connective tissue layer – Myocardium • Middle layer • Mostly cardiac muscle – Endocardium • Inner layer • Endothelium
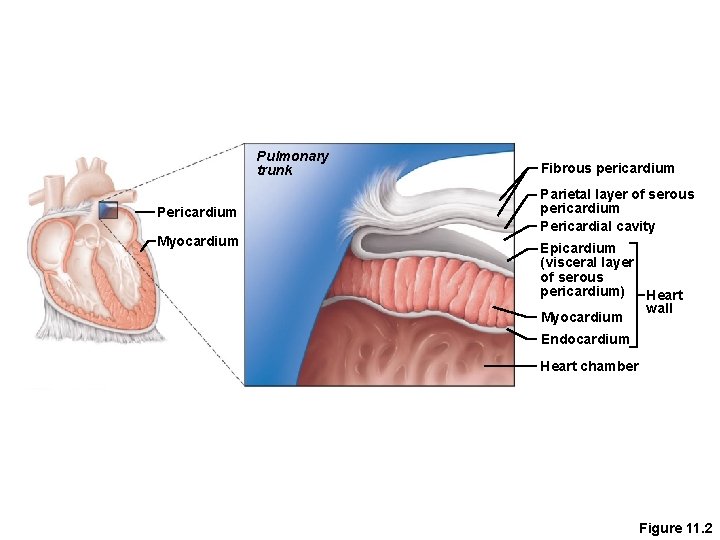
Pulmonary trunk Pericardium Myocardium Fibrous pericardium Parietal layer of serous pericardium Pericardial cavity Epicardium (visceral layer of serous pericardium) Heart wall Myocardium Endocardium Heart chamber Figure 11. 2
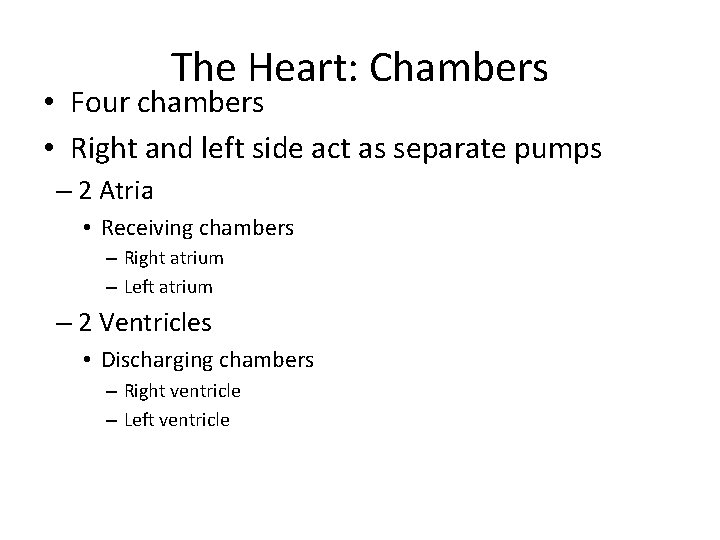
The Heart: Chambers • Four chambers • Right and left side act as separate pumps – 2 Atria • Receiving chambers – Right atrium – Left atrium – 2 Ventricles • Discharging chambers – Right ventricle – Left ventricle
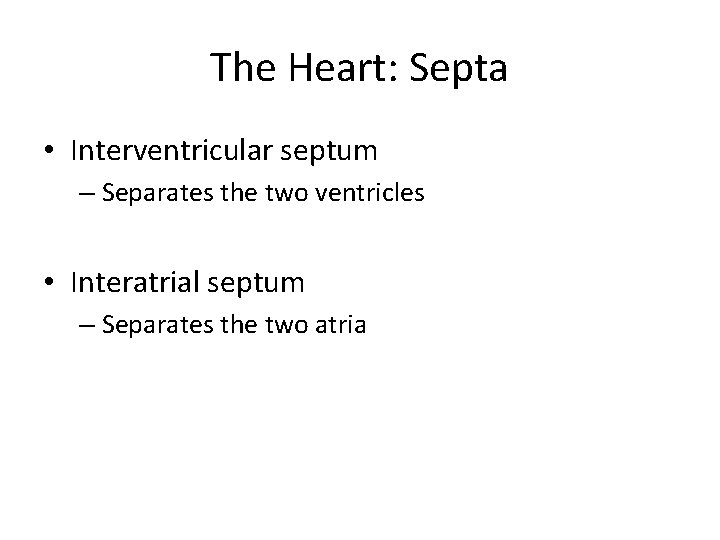
The Heart: Septa • Interventricular septum – Separates the two ventricles • Interatrial septum – Separates the two atria
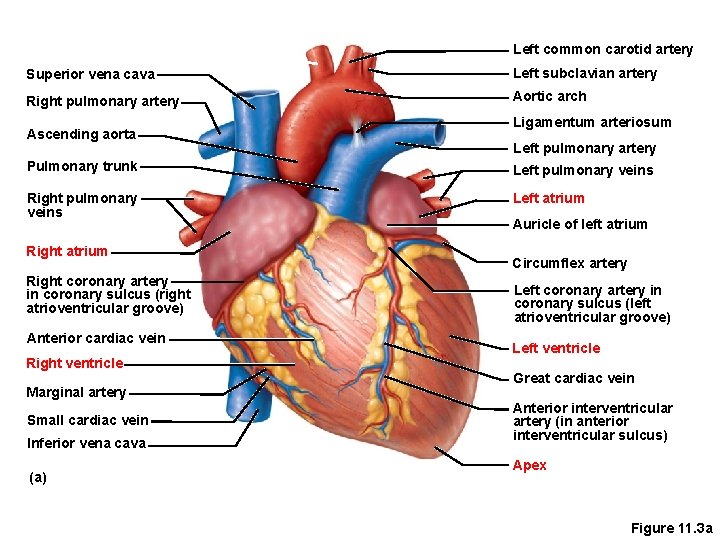
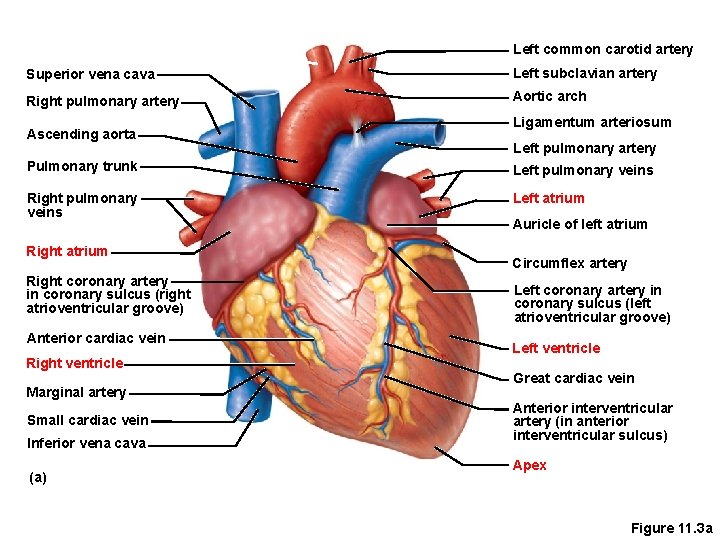
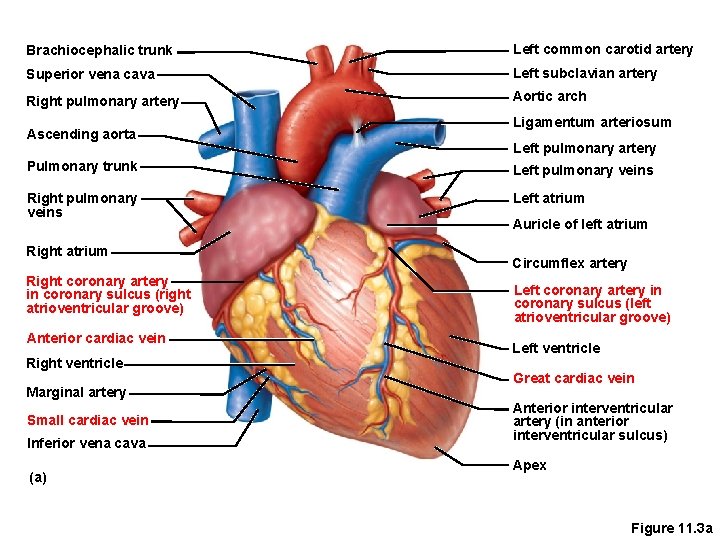
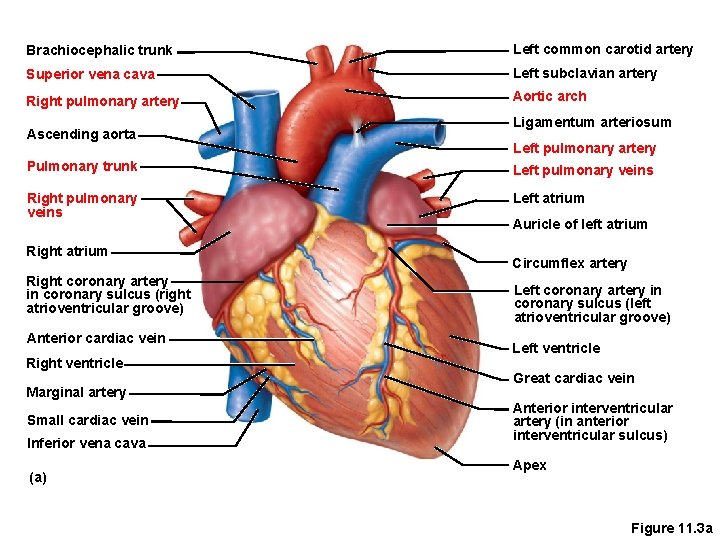
Left common carotid artery Superior vena cava Left subclavian artery Right pulmonary artery Aortic arch Ascending aorta Ligamentum arteriosum Left pulmonary artery Pulmonary trunk Left pulmonary veins Right pulmonary veins Left atrium Right coronary artery in coronary sulcus (right atrioventricular groove) Anterior cardiac vein Right ventricle Marginal artery Small cardiac vein Inferior vena cava (a) Auricle of left atrium Circumflex artery Left coronary artery in coronary sulcus (left atrioventricular groove) Left ventricle Great cardiac vein Anterior interventricular artery (in anterior interventricular sulcus) Apex Figure 11. 3 a
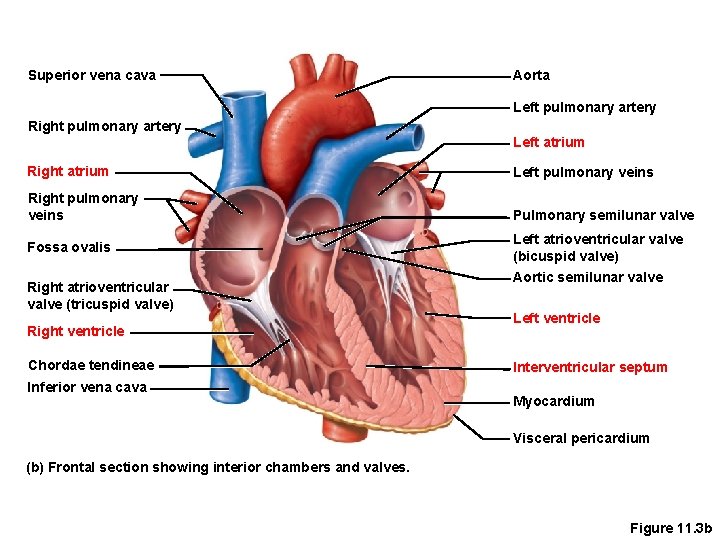
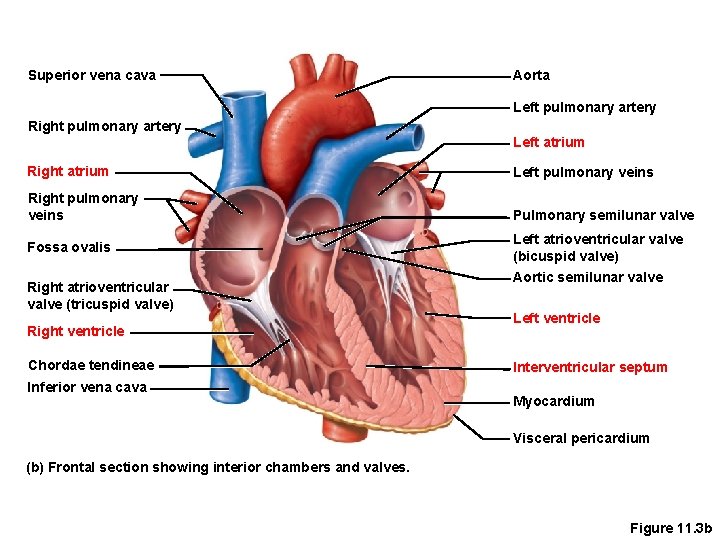
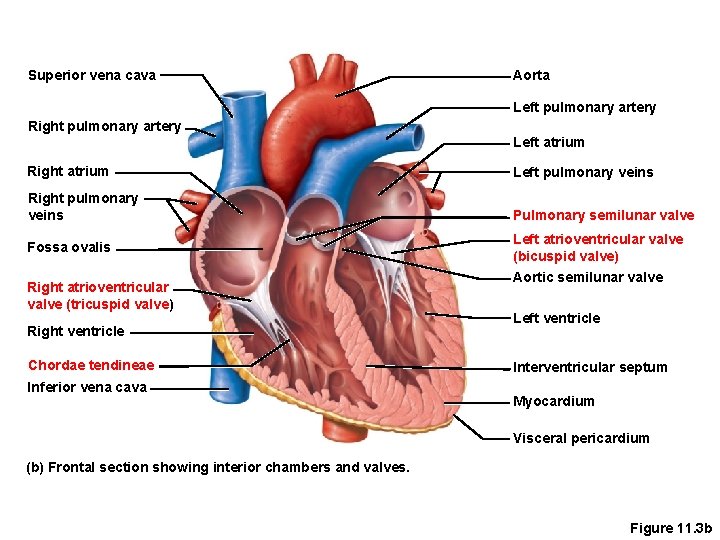
Superior vena cava Aorta Left pulmonary artery Right pulmonary artery Left atrium Right atrium Left pulmonary veins Right pulmonary veins Pulmonary semilunar valve Fossa ovalis Right atrioventricular valve (tricuspid valve) Right ventricle Chordae tendineae Inferior vena cava Left atrioventricular valve (bicuspid valve) Aortic semilunar valve Left ventricle Interventricular septum Myocardium Visceral pericardium (b) Frontal section showing interior chambers and valves. Figure 11. 3 b
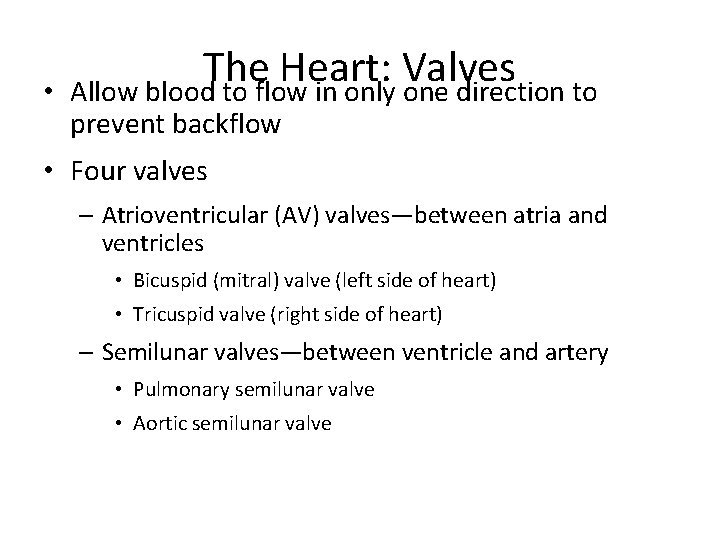
• The Heart: Valves Allow blood to flow in only one direction to prevent backflow • Four valves – Atrioventricular (AV) valves—between atria and ventricles • Bicuspid (mitral) valve (left side of heart) • Tricuspid valve (right side of heart) – Semilunar valves—between ventricle and artery • Pulmonary semilunar valve • Aortic semilunar valve
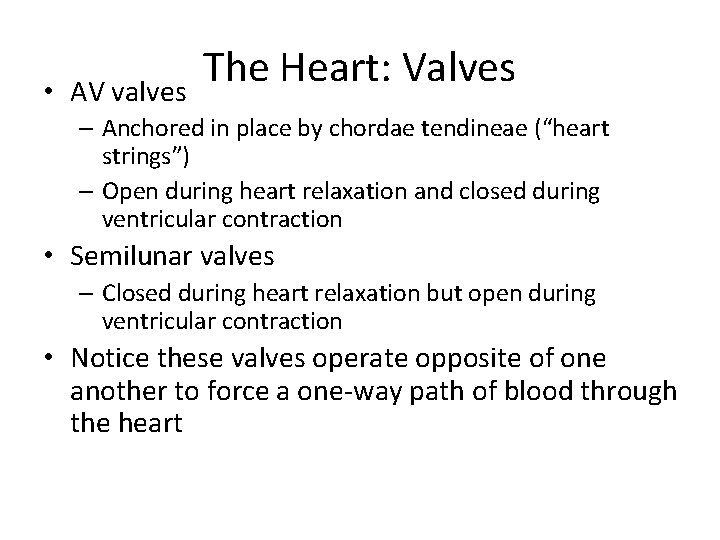
• AV valves The Heart: Valves – Anchored in place by chordae tendineae (“heart strings”) – Open during heart relaxation and closed during ventricular contraction • Semilunar valves – Closed during heart relaxation but open during ventricular contraction • Notice these valves operate opposite of one another to force a one-way path of blood through the heart
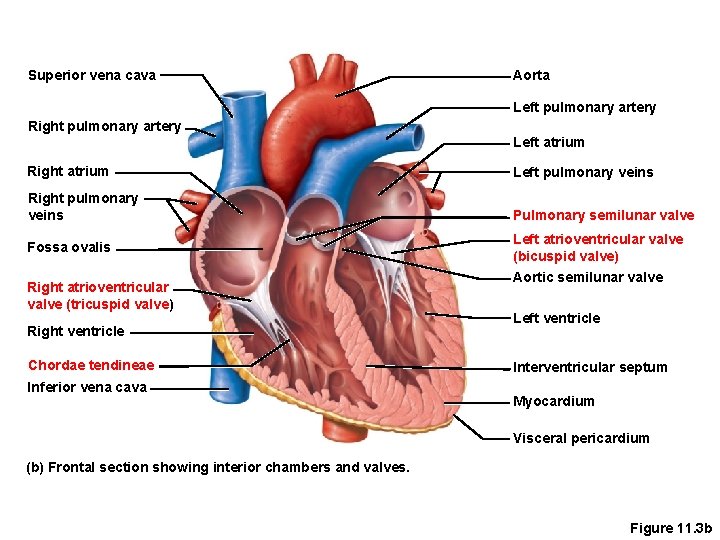
Superior vena cava Aorta Left pulmonary artery Right pulmonary artery Left atrium Right atrium Left pulmonary veins Right pulmonary veins Pulmonary semilunar valve Fossa ovalis Right atrioventricular valve (tricuspid valve) Right ventricle Chordae tendineae Inferior vena cava Left atrioventricular valve (bicuspid valve) Aortic semilunar valve Left ventricle Interventricular septum Myocardium Visceral pericardium (b) Frontal section showing interior chambers and valves. Figure 11. 3 b
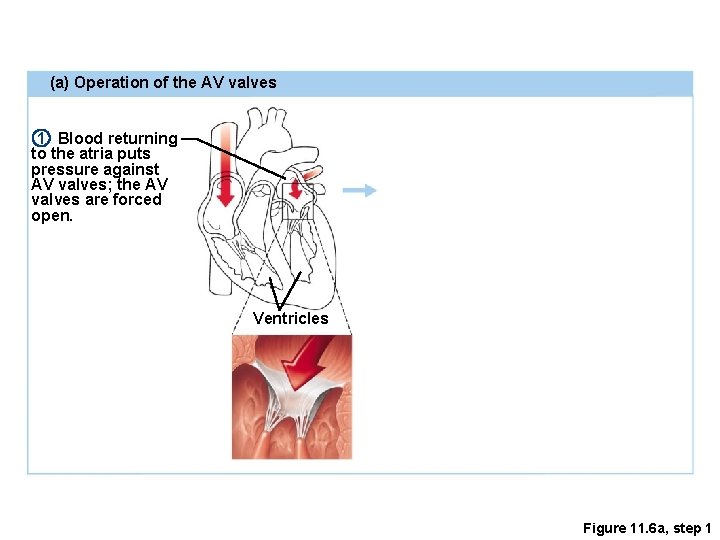
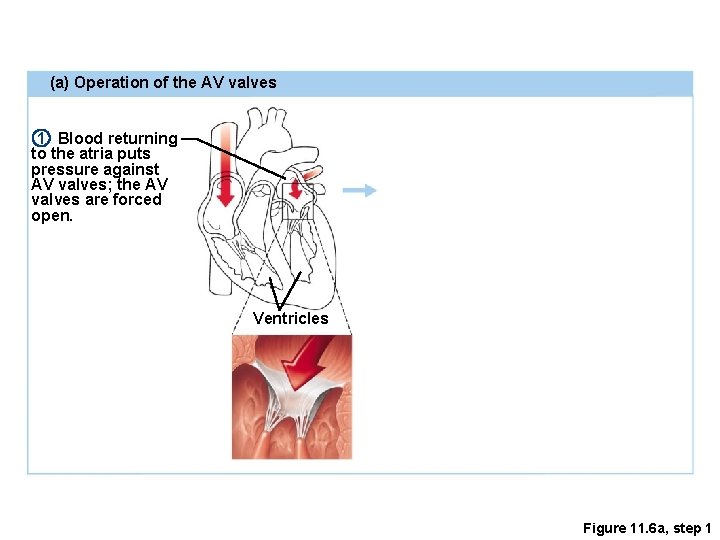
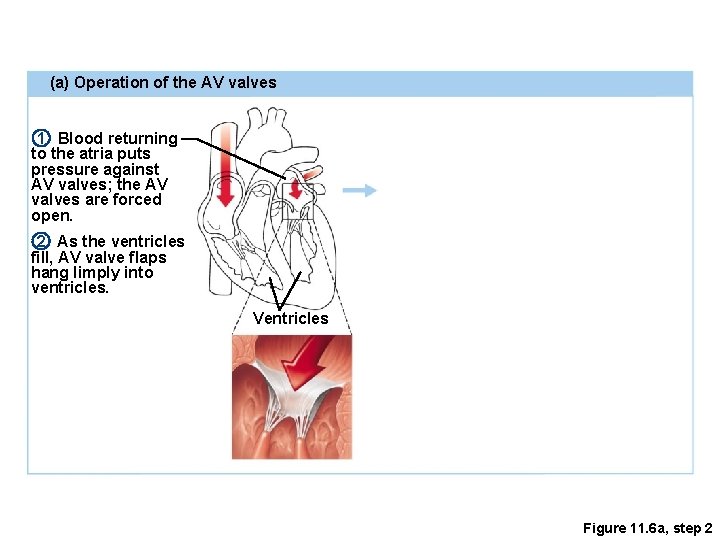
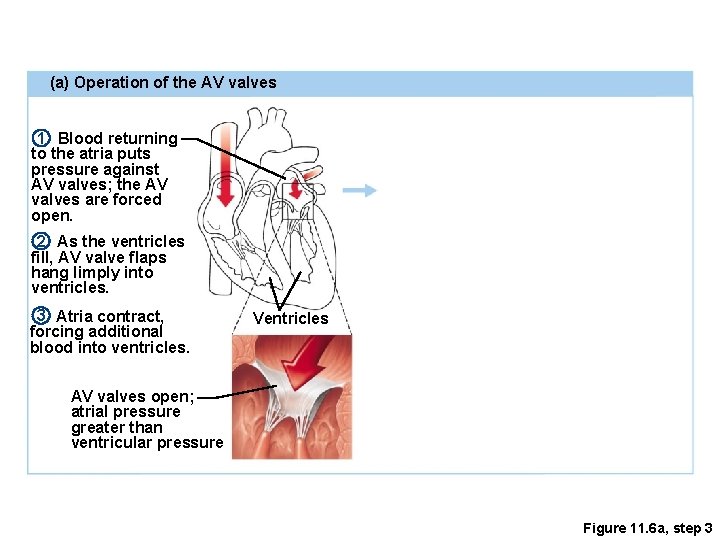
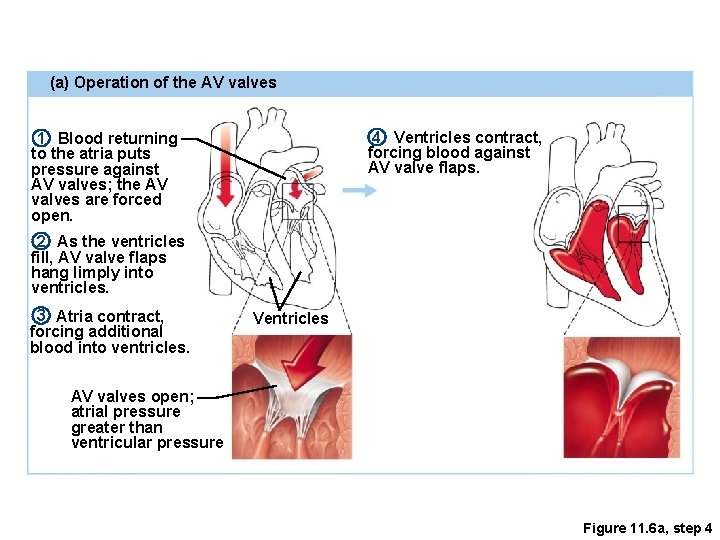
(a) Operation of the AV valves 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. Ventricles Figure 11. 6 a, step 1
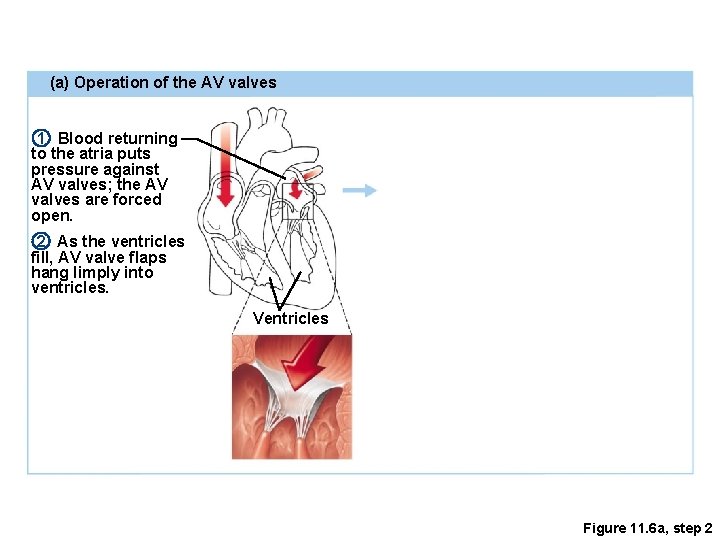
(a) Operation of the AV valves 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. 2 As the ventricles fill, AV valve flaps hang limply into ventricles. Ventricles Figure 11. 6 a, step 2
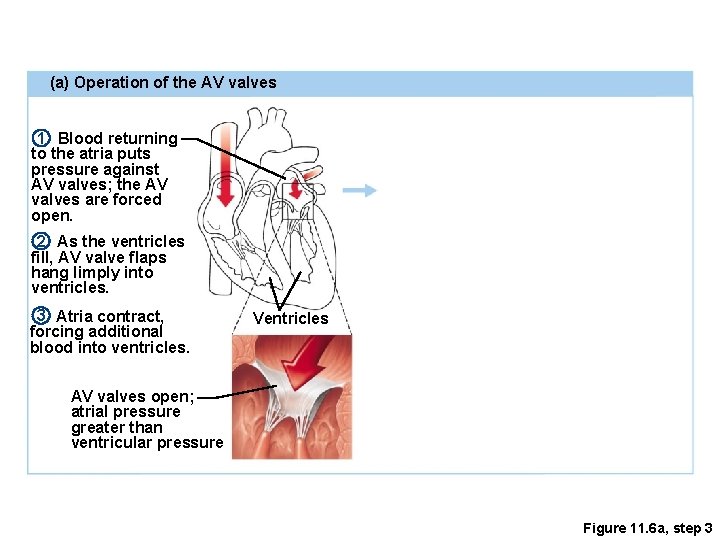
(a) Operation of the AV valves 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. 2 As the ventricles fill, AV valve flaps hang limply into ventricles. 3 Atria contract, forcing additional blood into ventricles. Ventricles AV valves open; atrial pressure greater than ventricular pressure Figure 11. 6 a, step 3
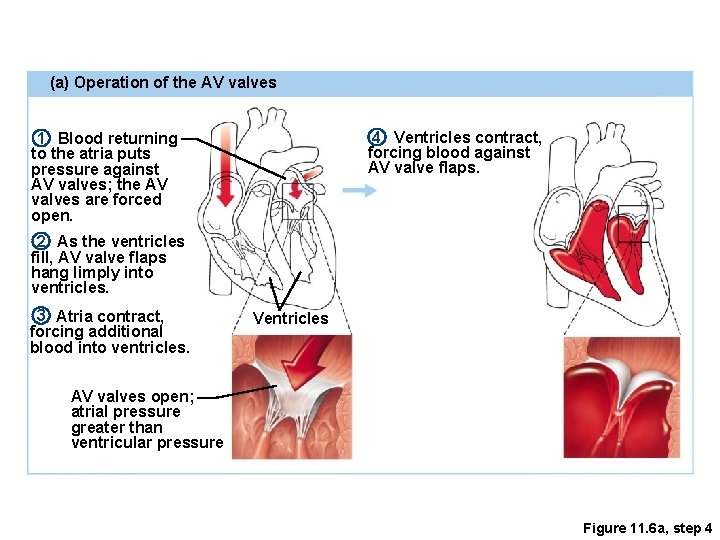
(a) Operation of the AV valves 4 Ventricles contract, forcing blood against AV valve flaps. 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. 2 As the ventricles fill, AV valve flaps hang limply into ventricles. 3 Atria contract, forcing additional blood into ventricles. Ventricles AV valves open; atrial pressure greater than ventricular pressure Figure 11. 6 a, step 4
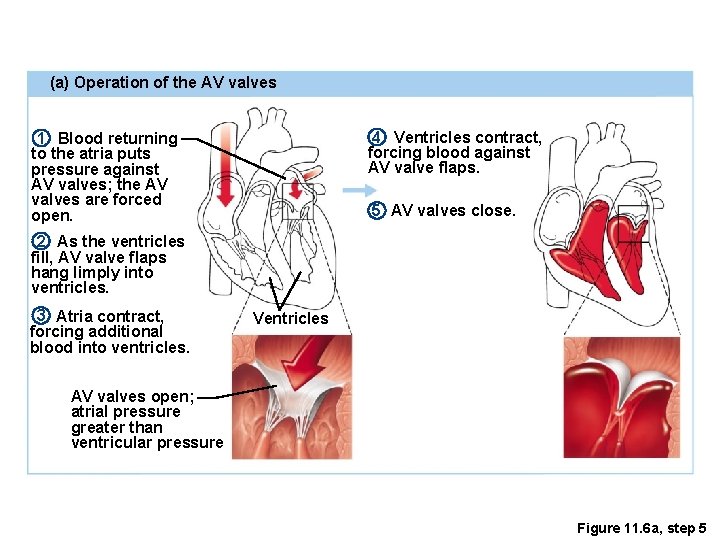
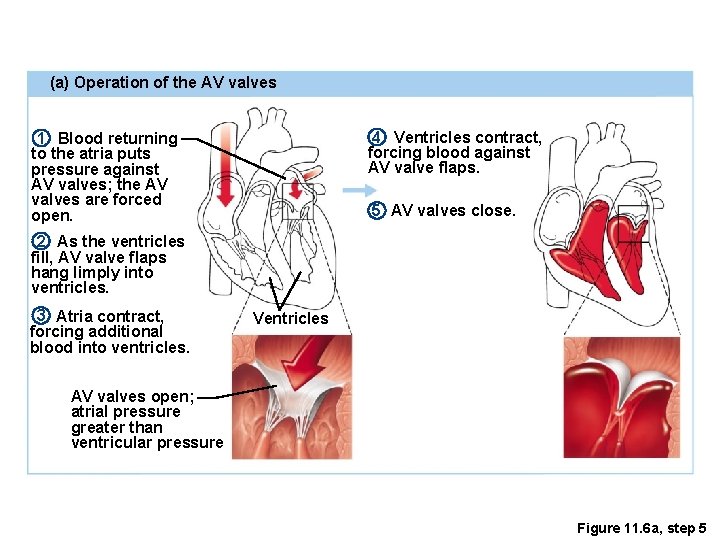
(a) Operation of the AV valves 4 Ventricles contract, forcing blood against AV valve flaps. 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. 5 AV valves close. 2 As the ventricles fill, AV valve flaps hang limply into ventricles. 3 Atria contract, forcing additional blood into ventricles. Ventricles AV valves open; atrial pressure greater than ventricular pressure Figure 11. 6 a, step 5
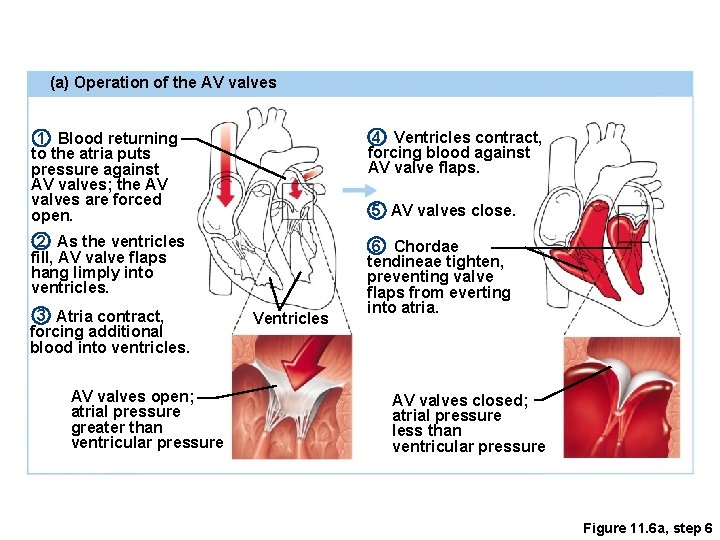
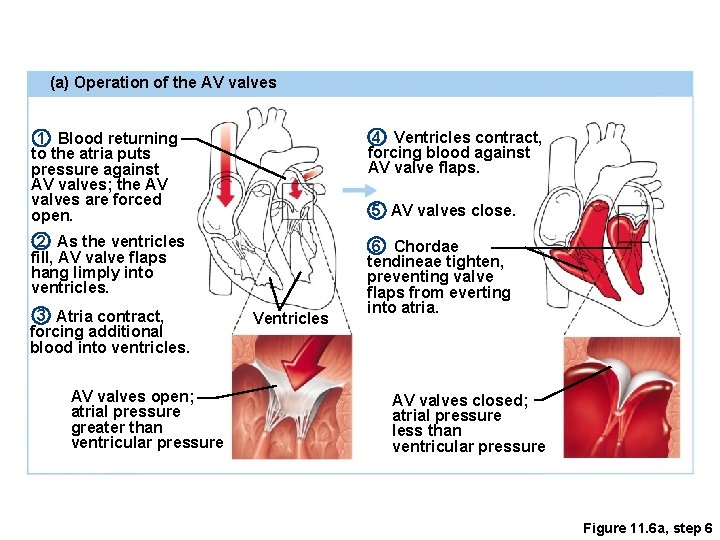
(a) Operation of the AV valves 1 Blood returning to the atria puts pressure against AV valves; the AV valves are forced open. 4 Ventricles contract, forcing blood against AV valve flaps. 2 As the ventricles fill, AV valve flaps hang limply into ventricles. 6 Chordae tendineae tighten, preventing valve flaps from everting into atria. 3 Atria contract, forcing additional blood into ventricles. AV valves open; atrial pressure greater than ventricular pressure 5 AV valves close. Ventricles AV valves closed; atrial pressure less than ventricular pressure Figure 11. 6 a, step 6
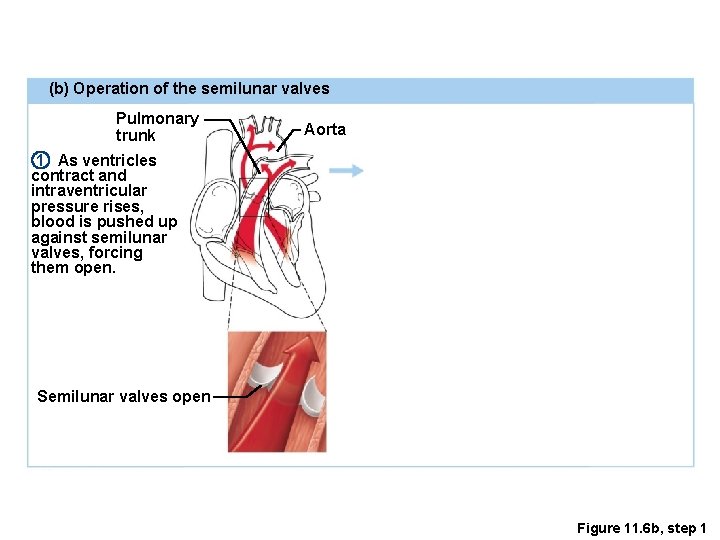
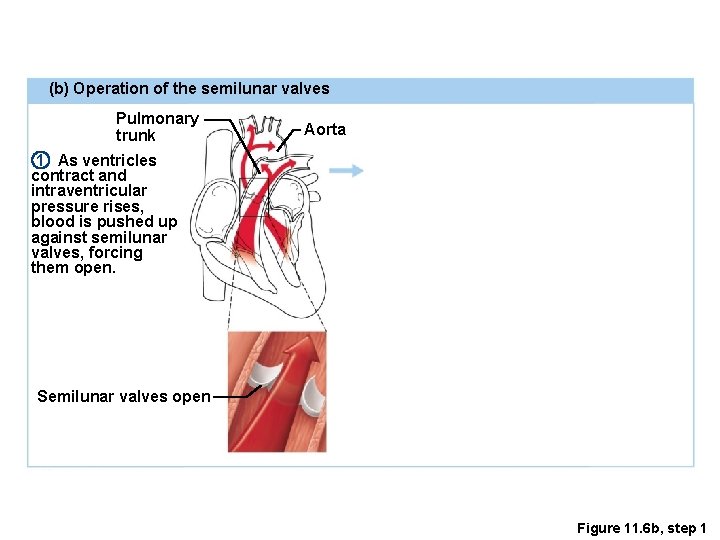
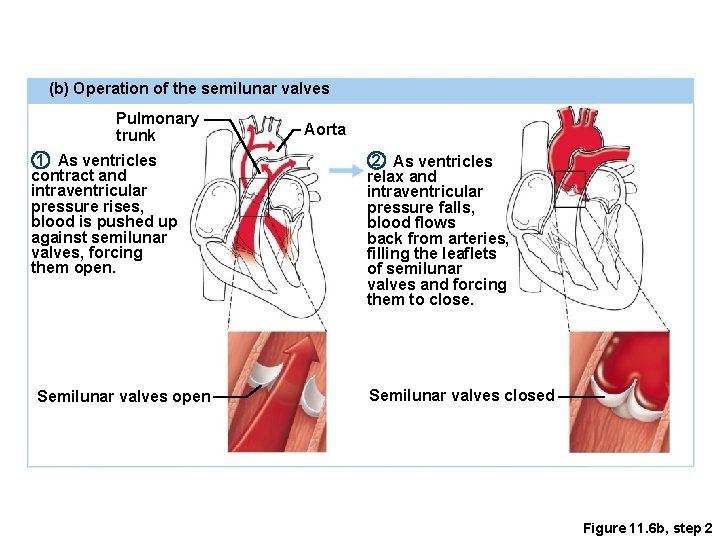
(b) Operation of the semilunar valves Pulmonary trunk Aorta 1 As ventricles contract and intraventricular pressure rises, blood is pushed up against semilunar valves, forcing them open. Semilunar valves open Figure 11. 6 b, step 1
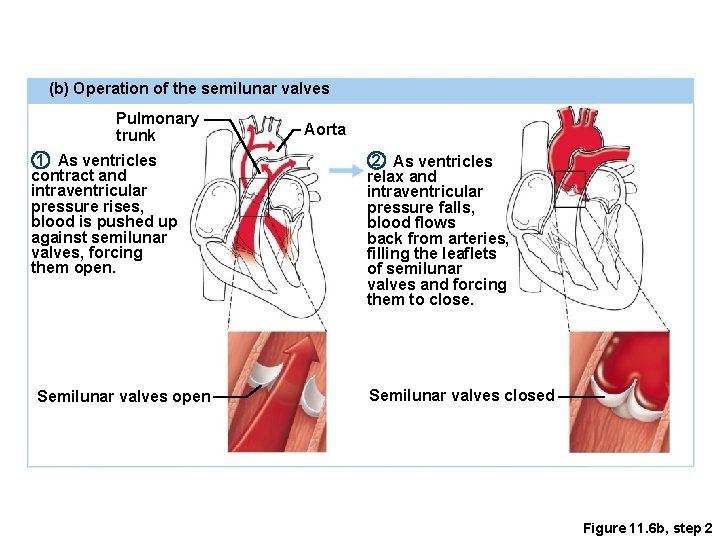
(b) Operation of the semilunar valves Pulmonary trunk 1 As ventricles contract and intraventricular pressure rises, blood is pushed up against semilunar valves, forcing them open. Semilunar valves open Aorta 2 As ventricles relax and intraventricular pressure falls, blood flows back from arteries, filling the leaflets of semilunar valves and forcing them to close. Semilunar valves closed Figure 11. 6 b, step 2
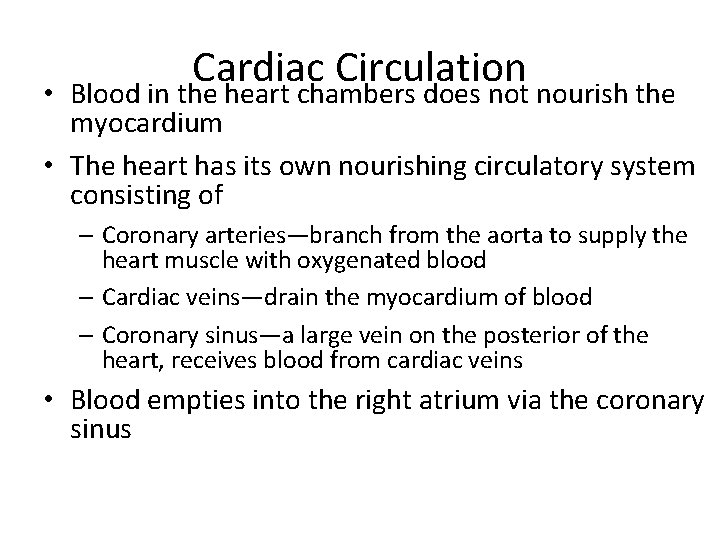
• Cardiac Circulation Blood in the heart chambers does not nourish the myocardium • The heart has its own nourishing circulatory system consisting of – Coronary arteries—branch from the aorta to supply the heart muscle with oxygenated blood – Cardiac veins—drain the myocardium of blood – Coronary sinus—a large vein on the posterior of the heart, receives blood from cardiac veins • Blood empties into the right atrium via the coronary sinus
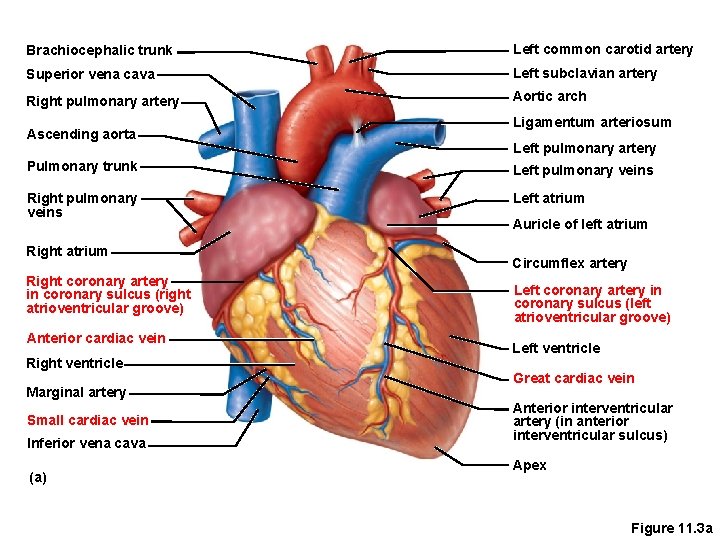
Brachiocephalic trunk Left common carotid artery Superior vena cava Left subclavian artery Right pulmonary artery Aortic arch Ascending aorta Ligamentum arteriosum Left pulmonary artery Pulmonary trunk Left pulmonary veins Right pulmonary veins Left atrium Right coronary artery in coronary sulcus (right atrioventricular groove) Anterior cardiac vein Right ventricle Marginal artery Small cardiac vein Inferior vena cava (a) Auricle of left atrium Circumflex artery Left coronary artery in coronary sulcus (left atrioventricular groove) Left ventricle Great cardiac vein Anterior interventricular artery (in anterior interventricular sulcus) Apex Figure 11. 3 a
The Heart: Associated Great Vessels • Arteries – Leave the Heart – Aorta • Leaves left ventricle – Pulmonary arteries • Leave right ventricle
The Heart: Associated Great Vessels • Veins – Return to the Heart – Superior and inferior venae cava • Enter right atrium – Pulmonary veins (four) • Enter left atrium
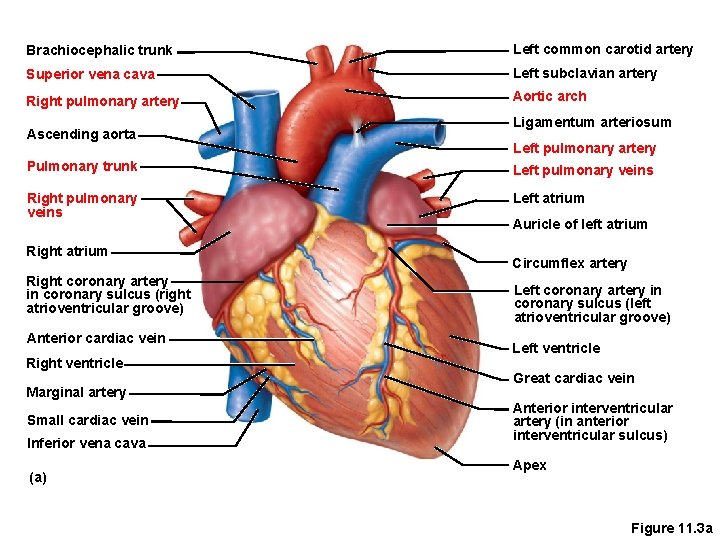
Brachiocephalic trunk Left common carotid artery Superior vena cava Left subclavian artery Right pulmonary artery Aortic arch Ascending aorta Ligamentum arteriosum Left pulmonary artery Pulmonary trunk Left pulmonary veins Right pulmonary veins Left atrium Right coronary artery in coronary sulcus (right atrioventricular groove) Anterior cardiac vein Right ventricle Marginal artery Small cardiac vein Inferior vena cava (a) Auricle of left atrium Circumflex artery Left coronary artery in coronary sulcus (left atrioventricular groove) Left ventricle Great cardiac vein Anterior interventricular artery (in anterior interventricular sulcus) Apex Figure 11. 3 a
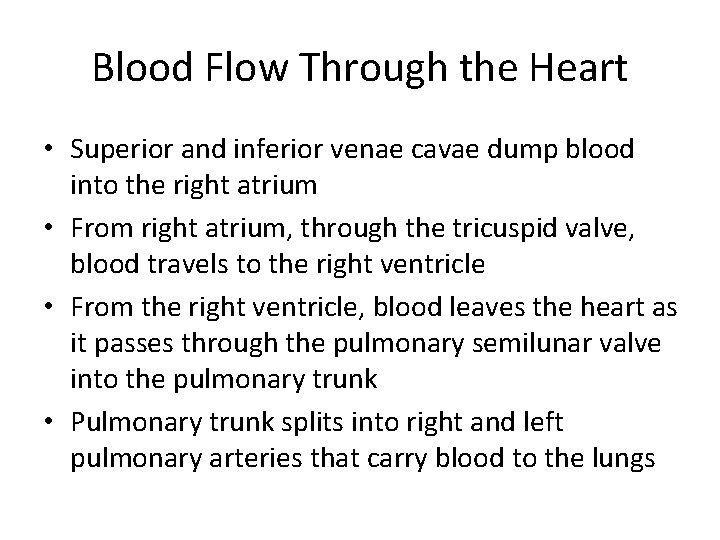
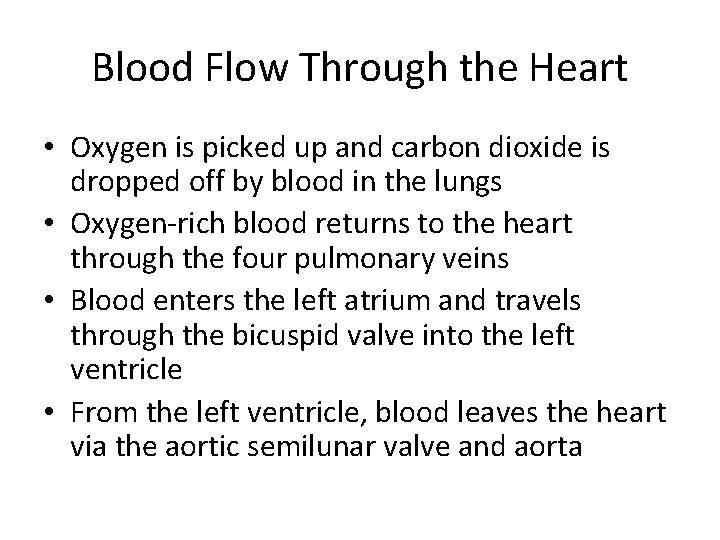
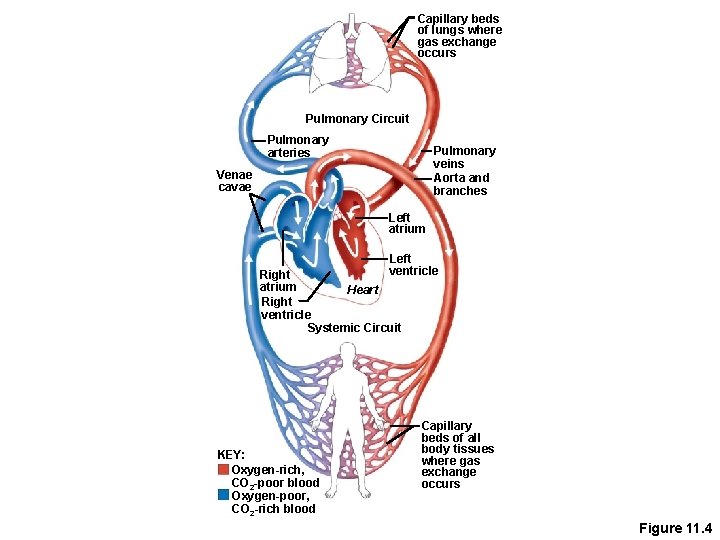
Blood Flow Through the Heart • Superior and inferior venae cavae dump blood into the right atrium • From right atrium, through the tricuspid valve, blood travels to the right ventricle • From the right ventricle, blood leaves the heart as it passes through the pulmonary semilunar valve into the pulmonary trunk • Pulmonary trunk splits into right and left pulmonary arteries that carry blood to the lungs
Blood Flow Through the Heart • Oxygen is picked up and carbon dioxide is dropped off by blood in the lungs • Oxygen-rich blood returns to the heart through the four pulmonary veins • Blood enters the left atrium and travels through the bicuspid valve into the left ventricle • From the left ventricle, blood leaves the heart via the aortic semilunar valve and aorta
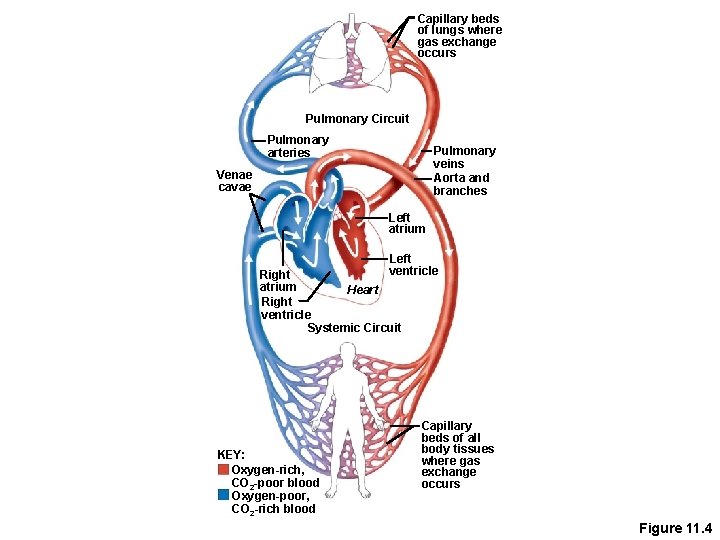
Capillary beds of lungs where gas exchange occurs Pulmonary Circuit Pulmonary arteries Pulmonary veins Aorta and branches Venae cavae Left atrium Left ventricle Right atrium Heart Right ventricle Systemic Circuit KEY: Oxygen-rich, CO 2 -poor blood Oxygen-poor, CO 2 -rich blood Capillary beds of all body tissues where gas exchange occurs Figure 11. 4
The Heart: Conduction System • Autorhythmic fibers – Heart muscle cells contract, without nerve impulses, in a regular, continuous way – Only about 1% of cardiac muscle fibers become autorhythmic fibers
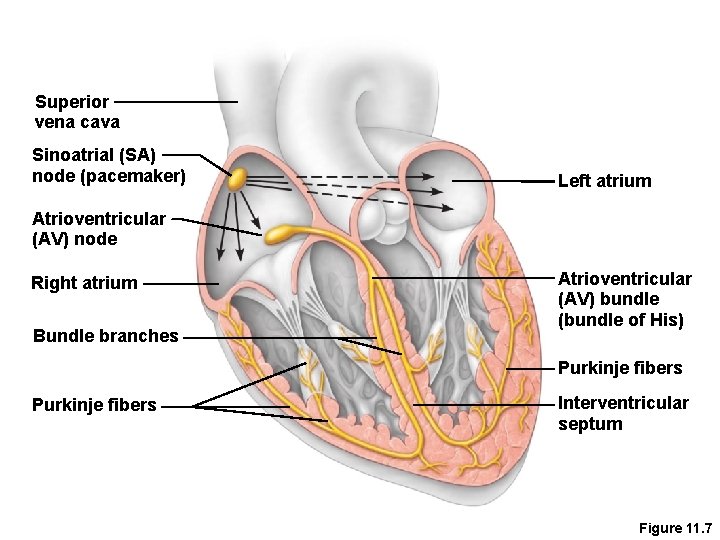
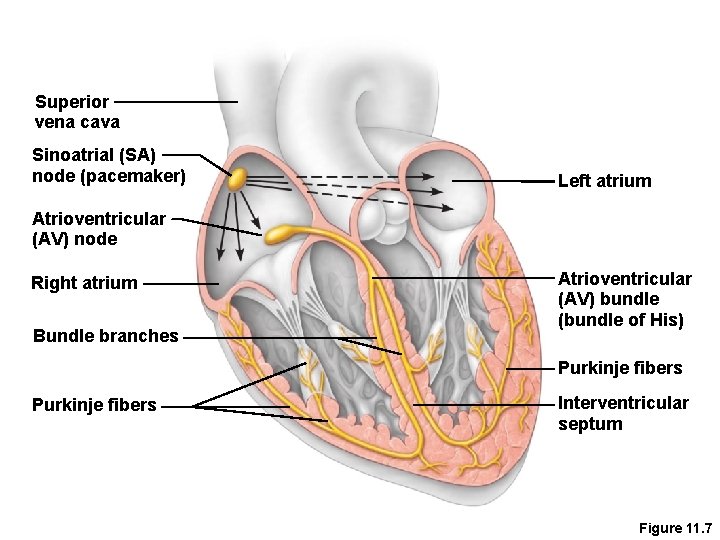
The Heart: Conduction System • Special tissue sets the pace – Sinoatrial node = SA node (“pacemaker”), is in the right atrium – Atrioventricular node = AV node, is at the junction of the atria and ventricles – Atrioventricular bundle = AV bundle (bundle of His), is in the interventricular septum – Bundle branches are in the interventricular septum – Purkinje fibers spread within the ventricle wall muscles
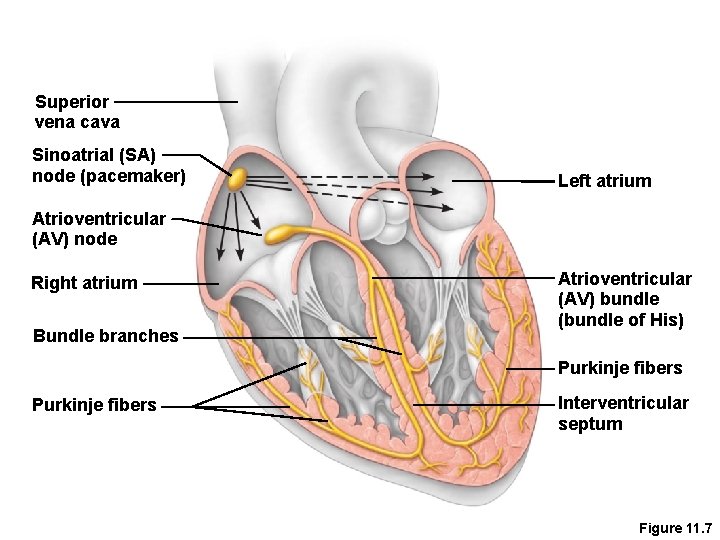
Superior vena cava Sinoatrial (SA) node (pacemaker) Left atrium Atrioventricular (AV) node Right atrium Bundle branches Atrioventricular (AV) bundle (bundle of His) Purkinje fibers Interventricular septum Figure 11. 7
Heart Contractions • Contraction is initiated by the sinoatrial node (SA node) • Force cardiac muscle depolarization in one direction—from atria to ventricles
Heart Contractions • Once SA node starts the heartbeat – Impulse spreads to the AV node – Then the atria contract • At the AV node, the impulse passes through the AV bundle, bundle branches, and Purkinje fibers • Blood is ejected from the ventricles to the aorta and pulmonary trunk as the ventricles contract
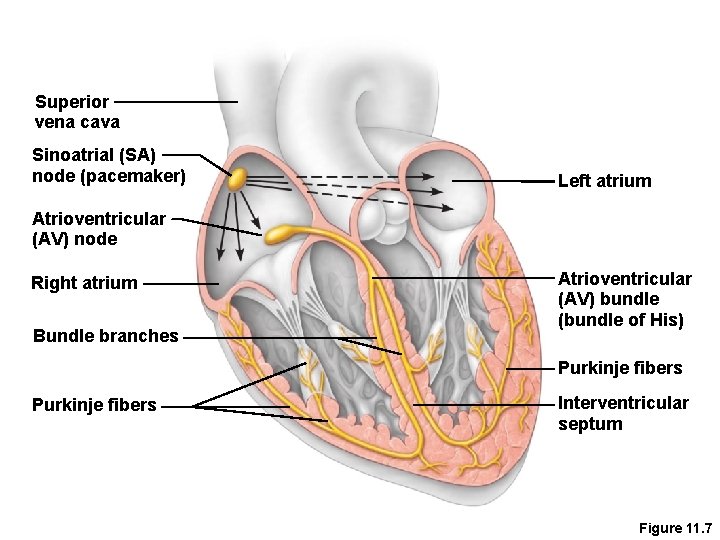
Superior vena cava Sinoatrial (SA) node (pacemaker) Left atrium Atrioventricular (AV) node Right atrium Bundle branches Atrioventricular (AV) bundle (bundle of His) Purkinje fibers Interventricular septum Figure 11. 7
Heart Contractions • Homeostatic imbalance – Heart block—damaged AV node releases them from control of the SA node; results in a slower heart rate as ventricles contract at their own rate – Ischemia—lack of adequate oxygen supply to heart muscle – Fibrillation—a rapid, uncoordinated shuddering of the heart muscle
Heart Contractions • Homeostatic imbalance (continued) – Tachycardia—rapid heart rate over 100 beats per minute – Bradycardia—slow heart rate less than 60 beats per minutes
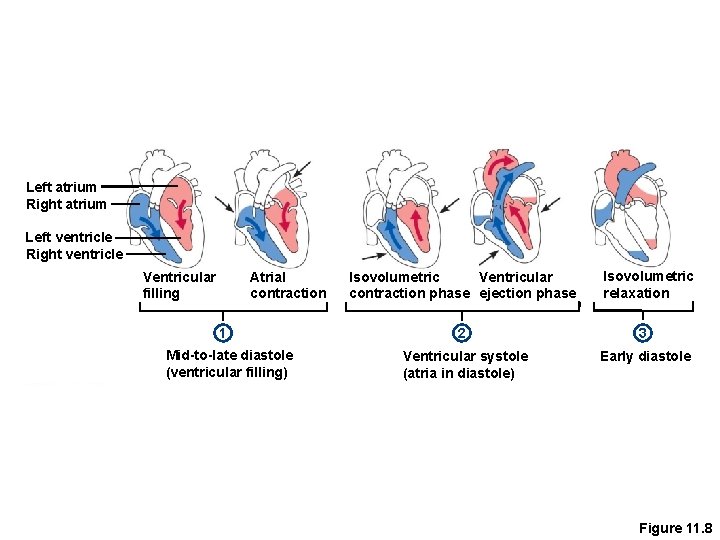
The Heart: Cardiac Cycle & Heart Sounds • • Atria contract simultaneously Atria relax, then ventricles contract Systole = contraction Diastole = relaxation
The Heart: Cardiac Cycle & Heart Sounds • Cardiac cycle—events of one complete heart beat – Mid-to-late diastole • Pressure in heart is low • Blood flows from passively into the atria and into ventricles • Semilunar valves are closed • Atrioventricular valves are open • Atria contract and force blood into ventricles
The Heart: Cardiac Cycle & Heart Sounds – Ventricular systole • Blood pressure builds before ventricle contracts • Atrioventricular valves close causes first heart sound, “lub” • Semilunar valves open as blood pushes against them • Blood travels out of the ventricles through pulmonary trunk and aorta • Atria are relaxed
The Heart: Cardiac Cycle & Heart Sounds – Early diastole – Second heart sound is heard as semilunar valves close, causing “dup” sound – At the end of systole, all four valves are briefly closed at the same time • Atria finish refilling as pressure in the heart drops • Ventricular pressure is low • Atrioventricular valves open
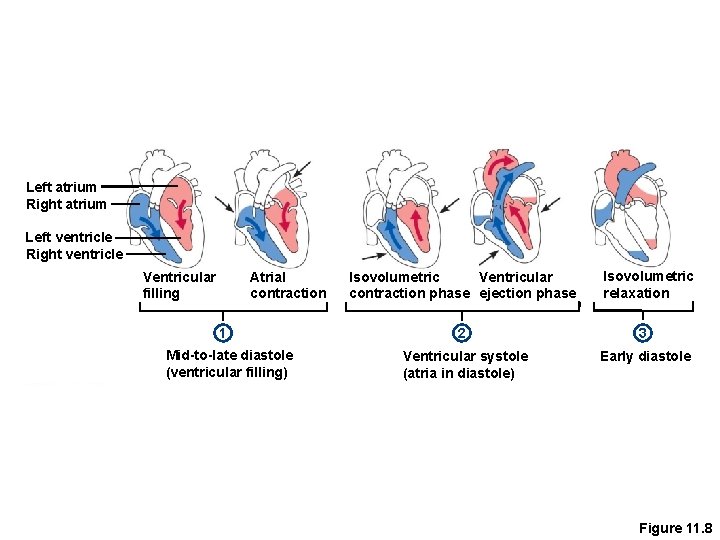
Left atrium Right atrium Left ventricle Right ventricle Ventricular filling Atrial contraction 1 Mid-to-late diastole (ventricular filling) Ventricular Isovolumetric contraction phase ejection phase Isovolumetric relaxation 2 3 Ventricular systole (atria in diastole) Early diastole Figure 11. 8
The Heart: Cardiac Output • Cardiac output (CO) – Amount of blood pumped by each side (ventricle) of the heart in one minute • Stroke volume (SV) – Volume of blood pumped by each ventricle in one contraction (each heartbeat) – Usually remains relatively constant – About 70 m. L of blood is pumped out of the left ventricle with each heartbeat • Heart rate (HR) – Typically 75 beats per minute
The Heart: Cardiac Output CO = HR SV CO = HR (75 beats/min) SV (70 m. L/beat) CO = 5250 m. L/min Starling’s law of the heart—the more the cardiac muscle is stretched, the stronger the contraction • Changing heart rate is the most common way to change cardiac output • •
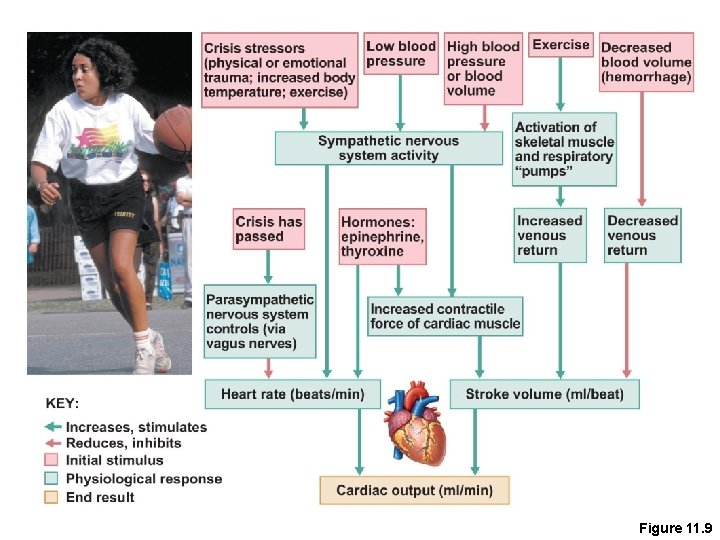
The Heart: Regulation of Heart Rate • Increased heart rate – Sympathetic nervous system • Crisis • Low blood pressure – Hormones • Epinephrine • Thyroxine – Exercise – Decreased blood volume
The Heart: Regulation of Heart Rate • Decreased heart rate – Parasympathetic nervous system – High blood pressure or blood volume
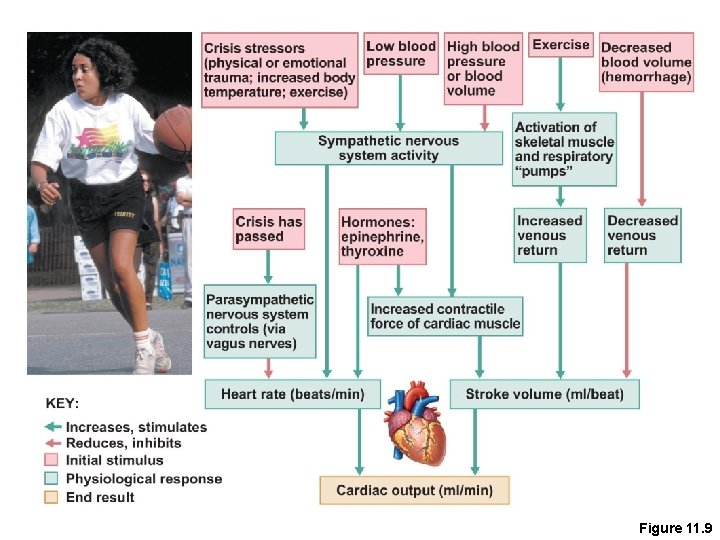
Figure 11. 9
 Chapter 19 the cardiovascular system blood vessels
Chapter 19 the cardiovascular system blood vessels What makes up the cardiovascular system
What makes up the cardiovascular system Pithed rat model
Pithed rat model Its tubular dude
Its tubular dude Coronary circulation of heart
Coronary circulation of heart Cengage chapter 5
Cengage chapter 5 Figure 11-9 is a diagram of the hepatic portal circulation
Figure 11-9 is a diagram of the hepatic portal circulation Chapter 11 the cardiovascular system figure 11-10 answers
Chapter 11 the cardiovascular system figure 11-10 answers Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Tissues in circulatory system
Tissues in circulatory system Hypertensive atherosclerotic cardiovascular disease
Hypertensive atherosclerotic cardiovascular disease Introduction of heart
Introduction of heart Stent placement
Stent placement Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 13 cardiovascular system
Chapter 13 cardiovascular system Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 The cardiovascular system includes the
The cardiovascular system includes the Major arteries
Major arteries Venule
Venule Cardiac dullness
Cardiac dullness Sheep heart labeled
Sheep heart labeled Heart 2 heart
Heart 2 heart Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Maniobra de pachon
Maniobra de pachon Rias de hipertension arterial
Rias de hipertension arterial Fresenius national cardiovascular partners
Fresenius national cardiovascular partners When does stroke volume increase
When does stroke volume increase Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Chapter 25 assessment of cardiovascular function
Chapter 25 assessment of cardiovascular function American board of cardiovascular medicine
American board of cardiovascular medicine Advanced cardiovascular life support
Advanced cardiovascular life support Centro cardiovascular
Centro cardiovascular Características de los vasos sanguíneos
Características de los vasos sanguíneos Cardiovascular research institute basel
Cardiovascular research institute basel What are the components of fitness?
What are the components of fitness? Salud cardiovascular
Salud cardiovascular Mapeh grade 7 physical fitness
Mapeh grade 7 physical fitness Salud cardiovascular
Salud cardiovascular Estratificacion de riesgo cardiovascular acsm
Estratificacion de riesgo cardiovascular acsm Fitness chapter 7
Fitness chapter 7 Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Cardiovascular drugs
Cardiovascular drugs Glandula que produce insulina
Glandula que produce insulina Sistema cardiovascular
Sistema cardiovascular Pequena circulação e grande circulação
Pequena circulação e grande circulação