Stroke Carla Kreft ND LAc MSOM What is





- Slides: 77
Stroke Carla Kreft ND LAc MSOM
What is a Stroke? • Short version: – Circulation to the brain is cut off, – the neurons are deprived of oxygen, – the neurons die – The person is left with symptoms that correspond to the area of the brain that died.
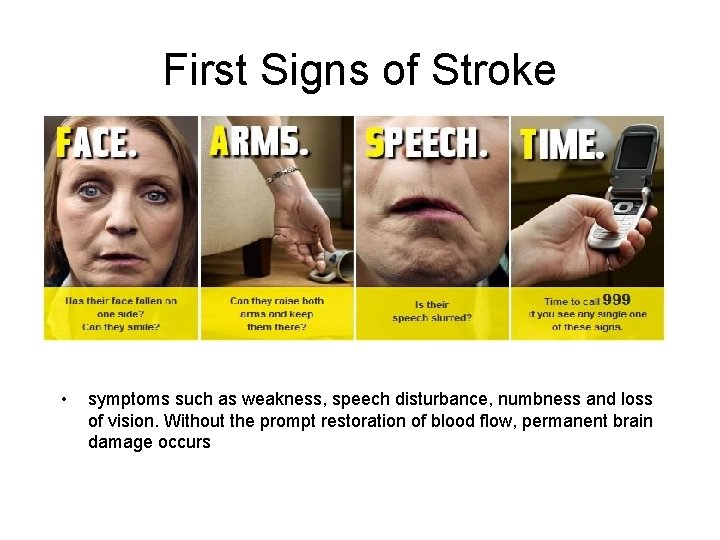
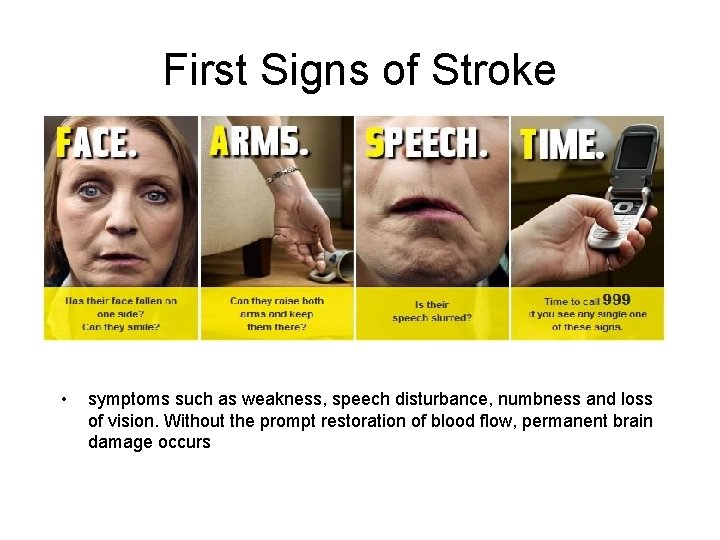
First Signs of Stroke • symptoms such as weakness, speech disturbance, numbness and loss of vision. Without the prompt restoration of blood flow, permanent brain damage occurs
Symptoms of a Stroke • • Abnormal sense of taste Change in alertness (level of consciousness) • – – – Apathetic, withdrawn – Sleepy, lethargic, stuporous – Unconscious, comatose • • • Difficulty speaking or understanding • speech • Difficulty swallowing Difficulty writing or reading Headache – May occur when lying flat – May awaken patient from sleep – May increase with change in position – May increase with bending, straining, and coughing • • Loss of coordination Loss of balance Movement changes • Difficulty moving any body part Hand tremor Loss of fine motor skills Weakness of any body part Nausea, vomiting Seizure Sensation changes – – Abnormal sensations Decreased sensation Facial paralysis Numbness or tingling Vision changes – Any change in vision – Decreased vision, loss of all or part of vision – Double vision – Eyelid drooping – Pupils different size – Uncontrollable eye movements
Blood Circulation from the Heart TO the Brain • Aorta > Brachiocephalic, Common Carotid, Subclavian > Internal Carotid & Vertebral Artery
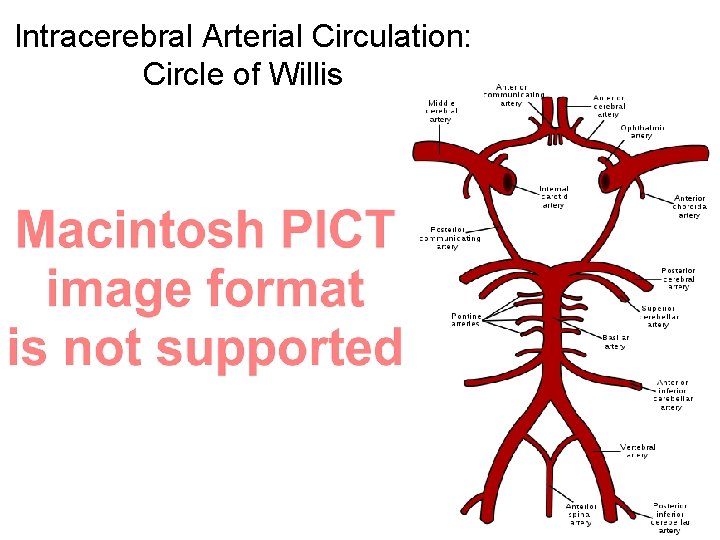
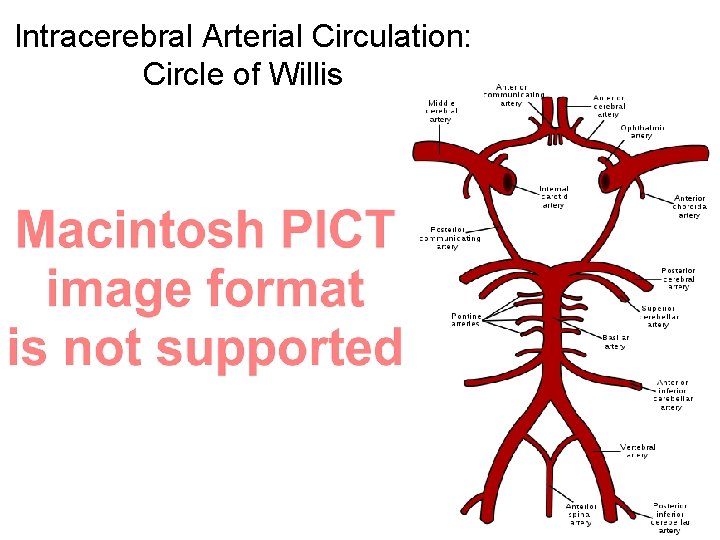
Intracerebral Arterial Circulation: Circle of Willis
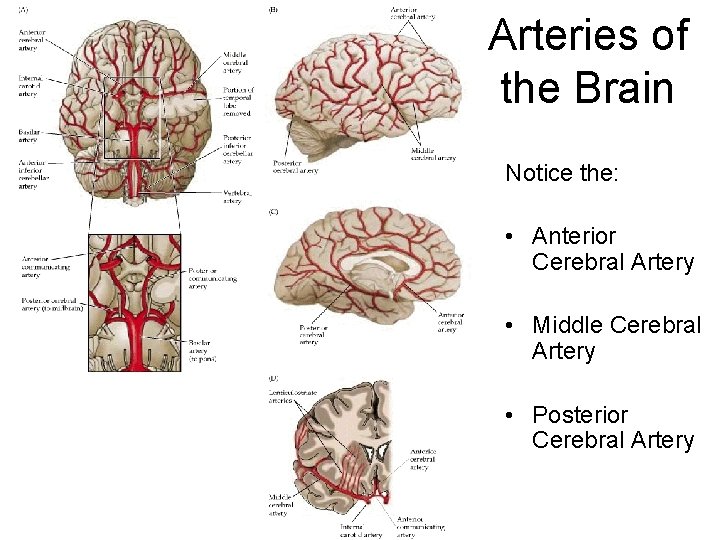
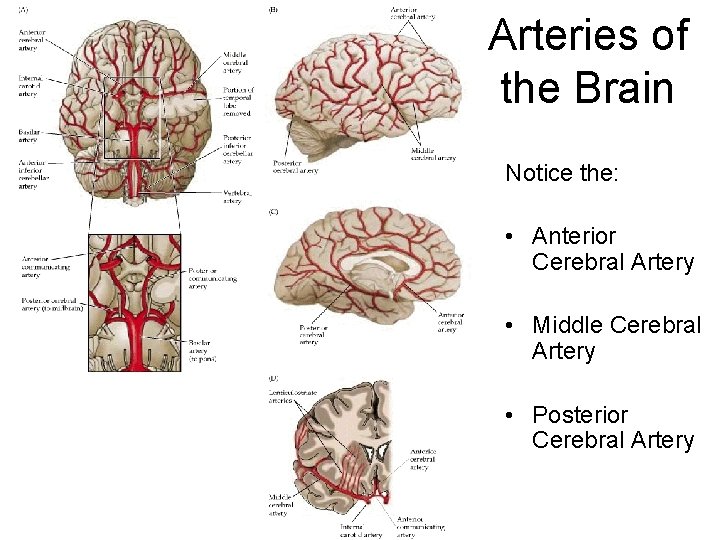
Arteries of the Brain Notice the: • Anterior Cerebral Artery • Middle Cerebral Artery • Posterior Cerebral Artery
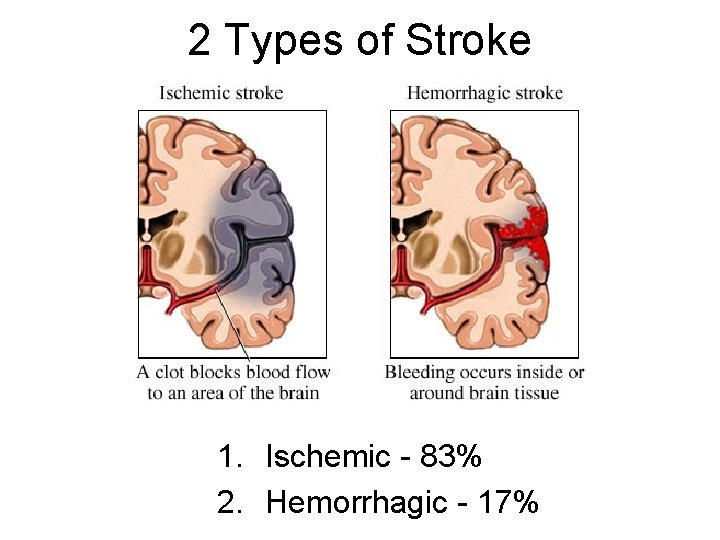
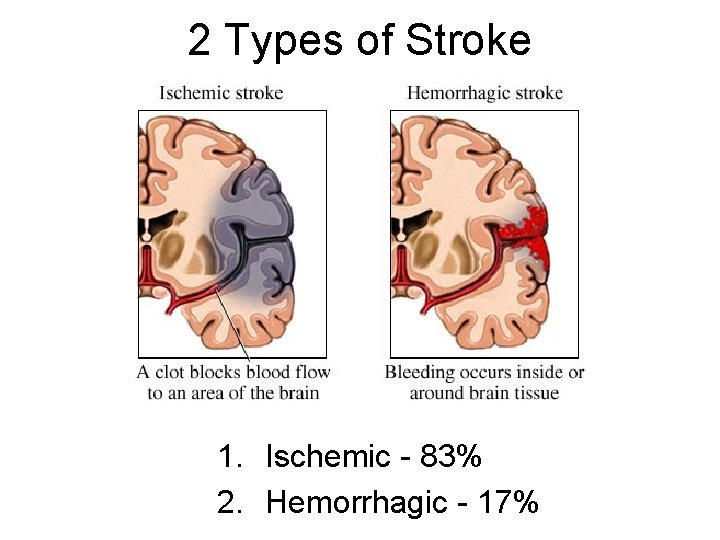
2 Types of Stroke 1. Ischemic - 83% 2. Hemorrhagic - 17%
Stroke Mortality • 30 day mortality rates among people 45 - 64 yo – Ischemic stroke: 8%- 12% – Hemorrhagic strokes 37% - 38% • Stroke is the 4 th leading cause of death in the USA
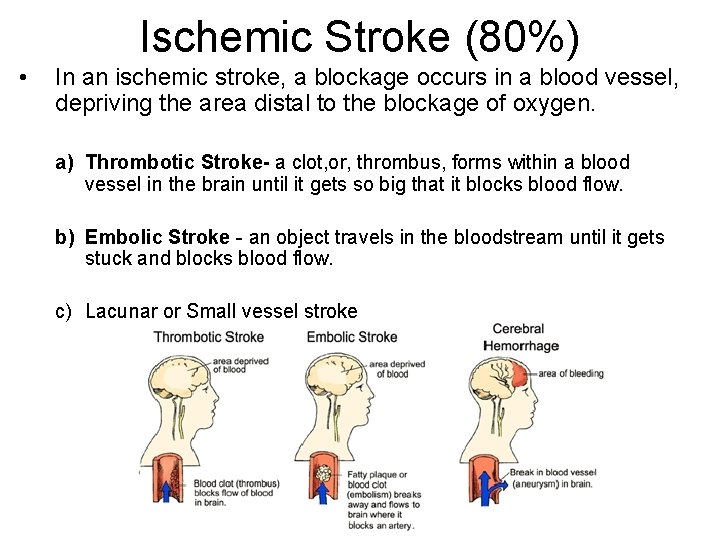
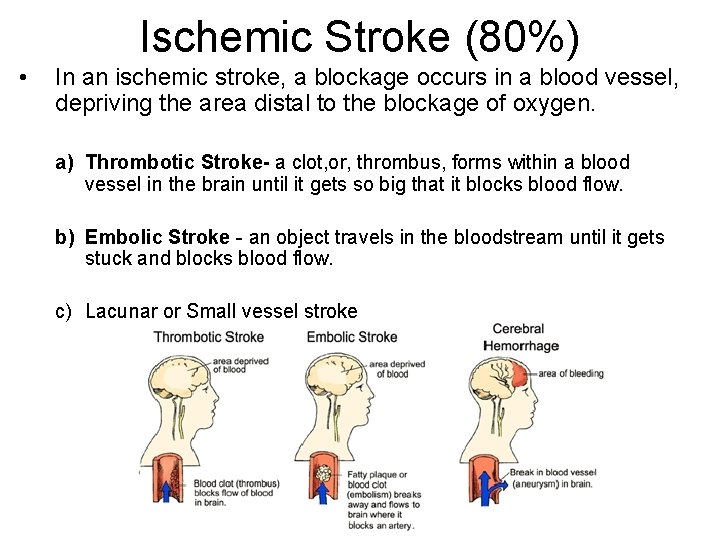
Ischemic Stroke (80%) • In an ischemic stroke, a blockage occurs in a blood vessel, depriving the area distal to the blockage of oxygen. a) Thrombotic Stroke- a clot, or, thrombus, forms within a blood vessel in the brain until it gets so big that it blocks blood flow. b) Embolic Stroke - an object travels in the bloodstream until it gets stuck and blocks blood flow. c) Lacunar or Small vessel stroke
Thrombotic Strokes • Thrombi are blood clots. They frequently form within an unhealthy, atherosclerotic vessel, on top of an atheroma. They can impede blood flow if they get too large (atherothrombotic stroke). • Atheromas, or, fatty plaques, can occur in any major cerebral artery and are common at areas of turbulent flow, particularly at the carotid bifurcation. If the cap on the atheroma ruptures or ulcerates, it causes thrombus formation.
Atherosclerosis • excess LDL passes through endothelial cells to tunica media. • Becomes oxidized & toxic. • Macrophages try to remove it & become foam cells • Dead macrophage lipids create a lipid core • A cap of collagen & elastin covers the plaque • If it is unstable, the plaque ruptures due to turbulent flow of blood & a thrombus forms
Less Common Causes of Thrombosis (clotting) Include: • Vascular inflammation from disorders such as: – acute or chronic meningitis – vasculitic disorders – syphilis • Dissection of intracranial arteries or the aorta (leads to clot formation at site) • Hypercoagulability disorders eg – Antiphospholipid syndrome – Hyperhomocysteinemia • Hyperviscosity disorders eg: – – polycythemia thrombocytosis hemoglobinopathies plasma cell disorders • Rare disorders eg: – moya disease Binswanger's disease • Older oral contraceptive formulations increase risk of thrombosis • FYI: Thrombi tend to occur during the night and thus are first noticed on awakening
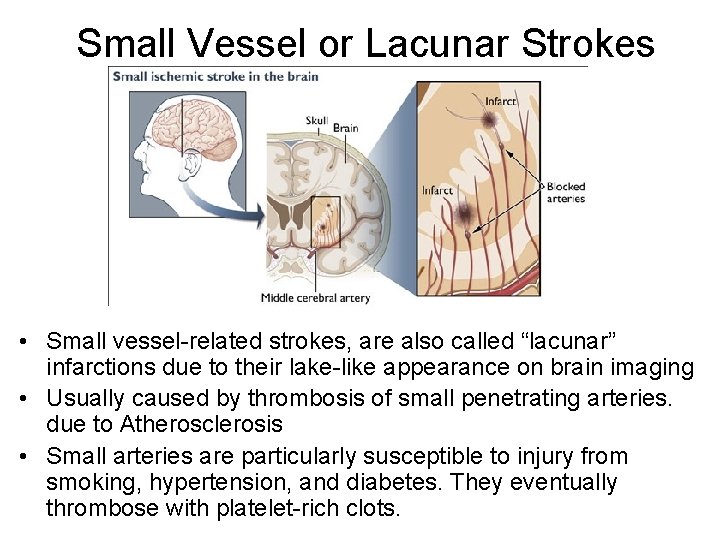
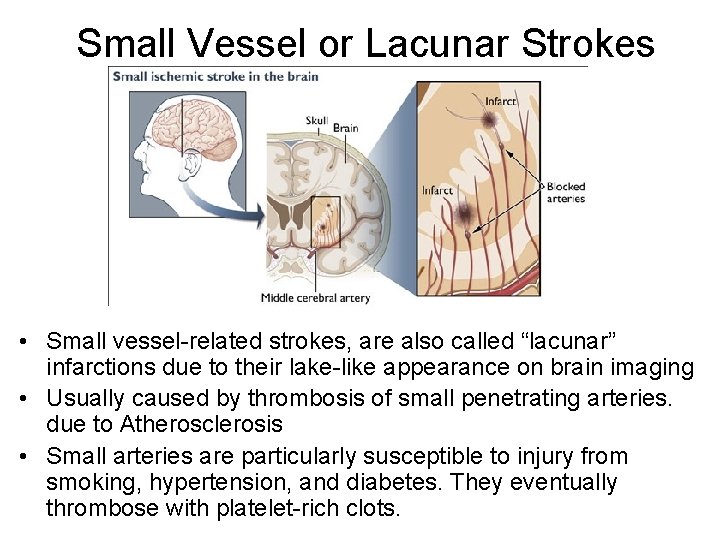
Small Vessel or Lacunar Strokes • Small vessel-related strokes, are also called “lacunar” infarctions due to their lake-like appearance on brain imaging • Usually caused by thrombosis of small penetrating arteries. due to Atherosclerosis • Small arteries are particularly susceptible to injury from smoking, hypertension, and diabetes. They eventually thrombose with platelet-rich clots.
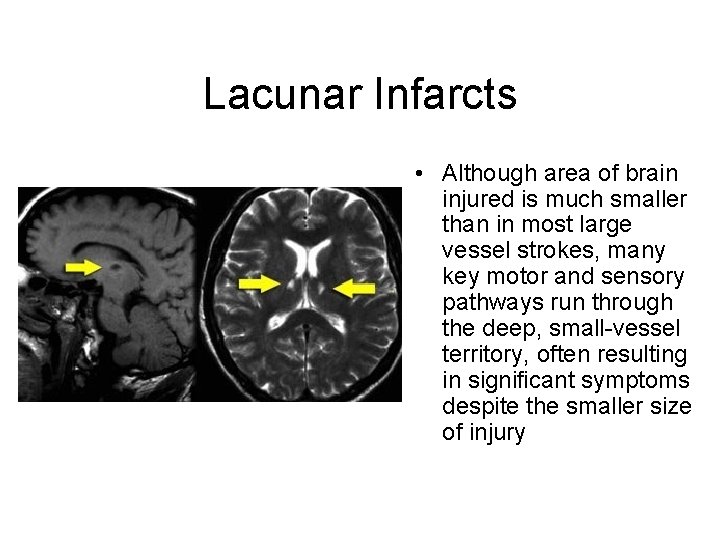
Lacunar Infarcts • Although area of brain injured is much smaller than in most large vessel strokes, many key motor and sensory pathways run through the deep, small-vessel territory, often resulting in significant symptoms despite the smaller size of injury
Embolic Stroke Emboli commonly originate from: 1. Ulcerated plaques at the carotid bifurcation in the neck or the aortic arch 2. Cardiac thrombi, (cardioembolic stroke) especially in the following conditions: – Atrial fibrillation (15 -20% of ischemic strokes yearly) – Rheumatic heart disease (usually mitral stenosis) – Post-Myocardial Infarction – Vegetations on heart valves from bacterial or non-bacterial endocarditis – Prosthetic heart valves
Other sources of Emboli • Clots that form and dislodge after open-heart surgery or other invasive cardiovascular procedures eg, catheterization • Rarely, emboli consist of: – Fat (from fractured long bones), – Air (in decompression sickness) – Venous clots that pass from the right to the left side of the heart through a patent foramen ovale with shunt (paradoxical emboli). • Rarely, thrombosis of the subclavian artery results in embolic stroke in the vertebral artery or its branches.
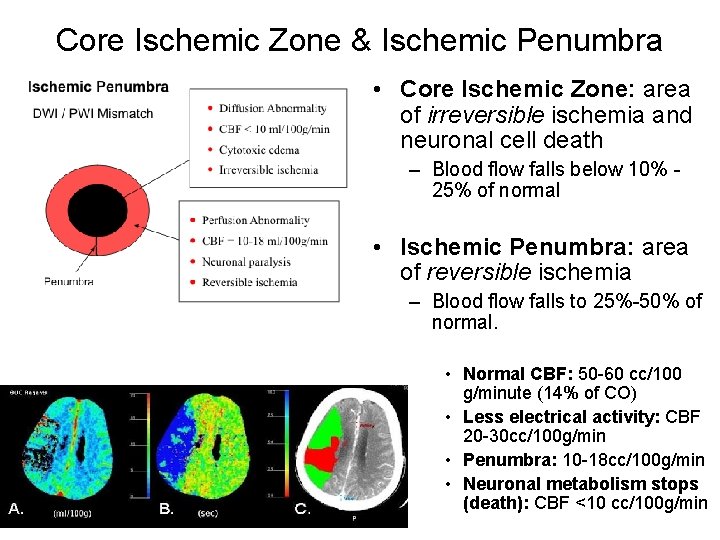
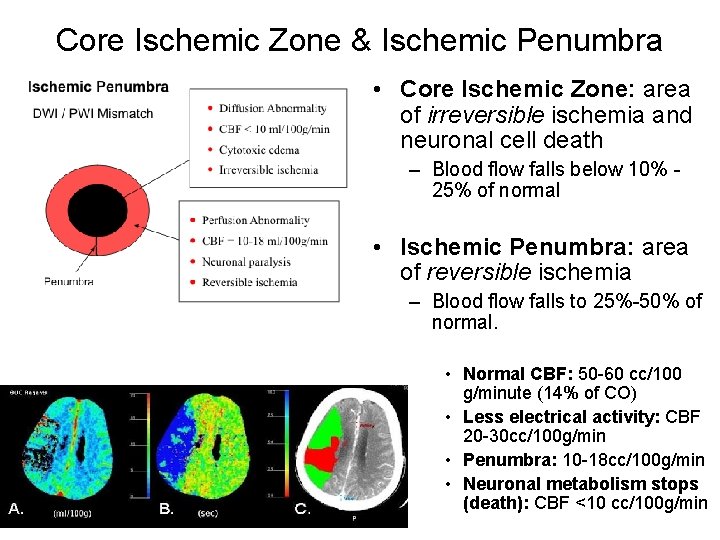
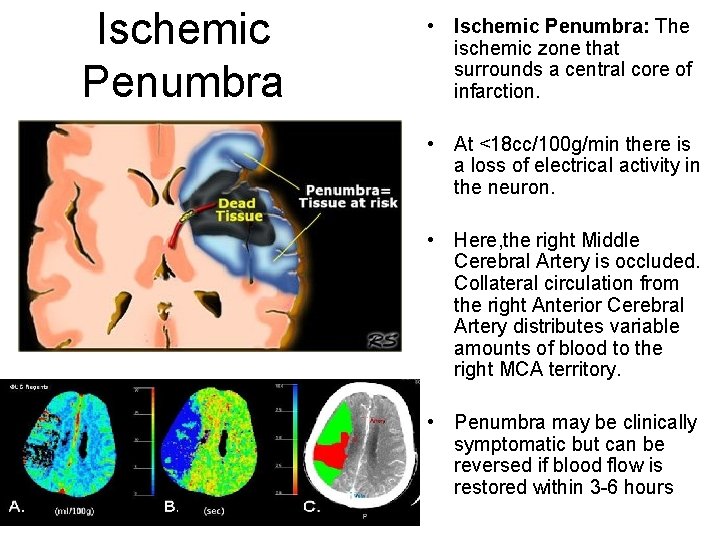
Core Ischemic Zone & Ischemic Penumbra • Core Ischemic Zone: area of irreversible ischemia and neuronal cell death – Blood flow falls below 10% 25% of normal • Ischemic Penumbra: area of reversible ischemia – Blood flow falls to 25%-50% of normal. • Normal CBF: 50 -60 cc/100 g/minute (14% of CO) • Less electrical activity: CBF 20 -30 cc/100 g/min • Penumbra: 10 -18 cc/100 g/min • Neuronal metabolism stops (death): CBF <10 cc/100 g/min
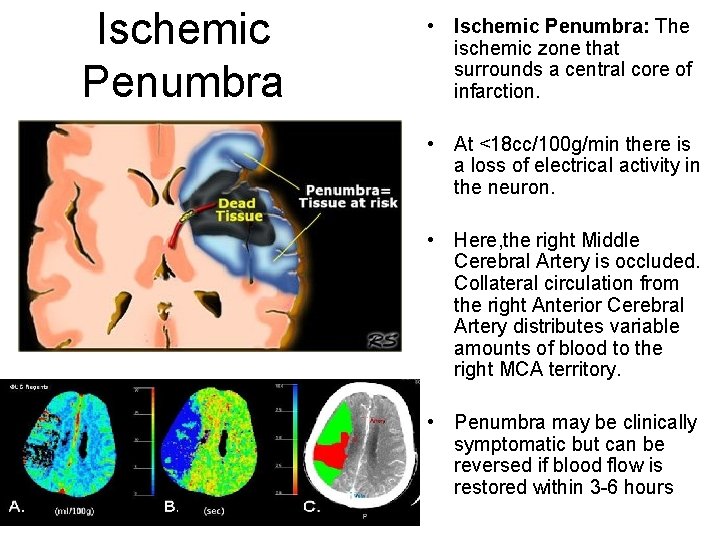
Ischemic Penumbra • Ischemic Penumbra: The ischemic zone that surrounds a central core of infarction. • At <18 cc/100 g/min there is a loss of electrical activity in the neuron. • Here, the right Middle Cerebral Artery is occluded. Collateral circulation from the right Anterior Cerebral Artery distributes variable amounts of blood to the right MCA territory. • Penumbra may be clinically symptomatic but can be reversed if blood flow is restored within 3 -6 hours
Window of Opportunity • Viability of brain tissue is preserved if perfusion is restored within a critical time period (2 to 4 hours)
The Neuron • • Resting Membrane Potential (Na+ outside, K+ inside. -55 m. V) Stimulus - causes Na+ channels to open Threshold - cell membrane depolarizes to +35 m. V Action Potential (+20 -50 m. V) Propagation (Na+ rushes into neuron along axon) • Neurotransmitter release at axon terminals into synapse • Repolarization - Na channels close, K+ channels open, K+ rushes out of cell • Na+/ K+ pump restores Na to outside of cell & K+ to inside of cell
Aerobic & Anaerobic Respiration • In the presence of oxygen, a cell (neuron) makes 36 ATP from 1 glucose via citric acid cycle & oxidative phosphorylation • In the absence of oxygen, the cell can only make 2 ATP via glycolysis, or fermentation
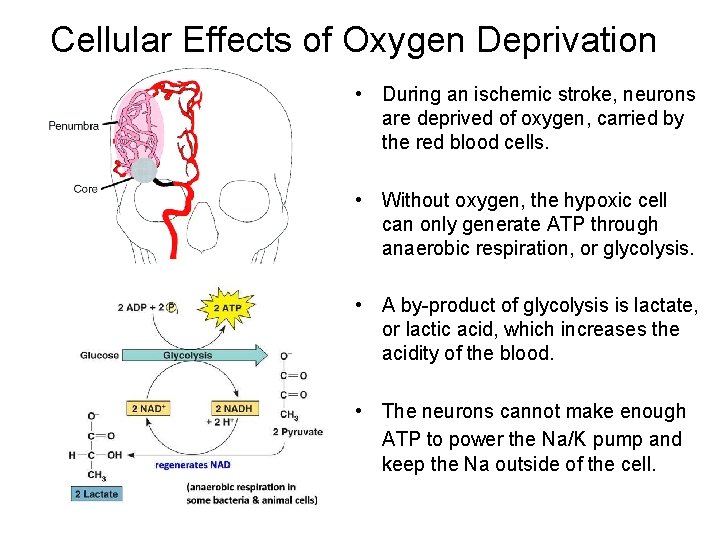
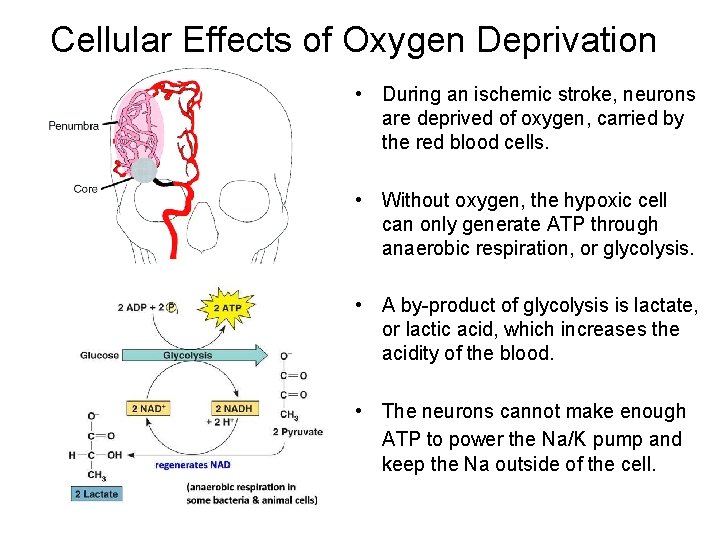
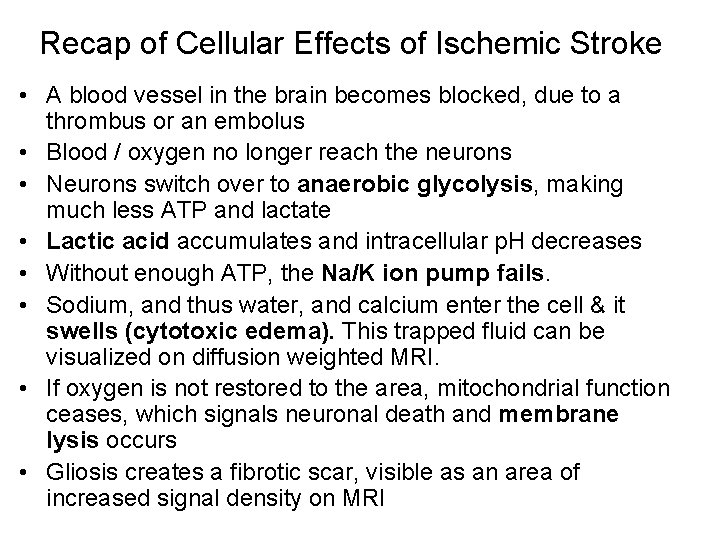
Cellular Effects of Oxygen Deprivation • During an ischemic stroke, neurons are deprived of oxygen, carried by the red blood cells. • Without oxygen, the hypoxic cell can only generate ATP through anaerobic respiration, or glycolysis. • A by-product of glycolysis is lactate, or lactic acid, which increases the acidity of the blood. • The neurons cannot make enough ATP to power the Na/K pump and keep the Na outside of the cell.
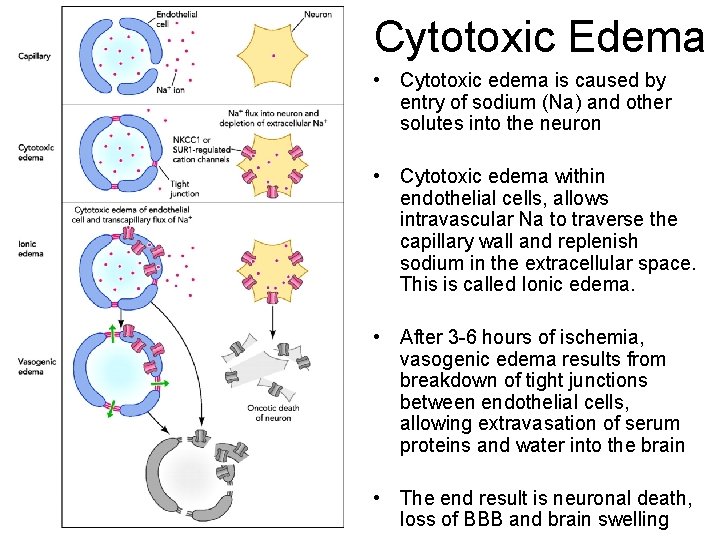
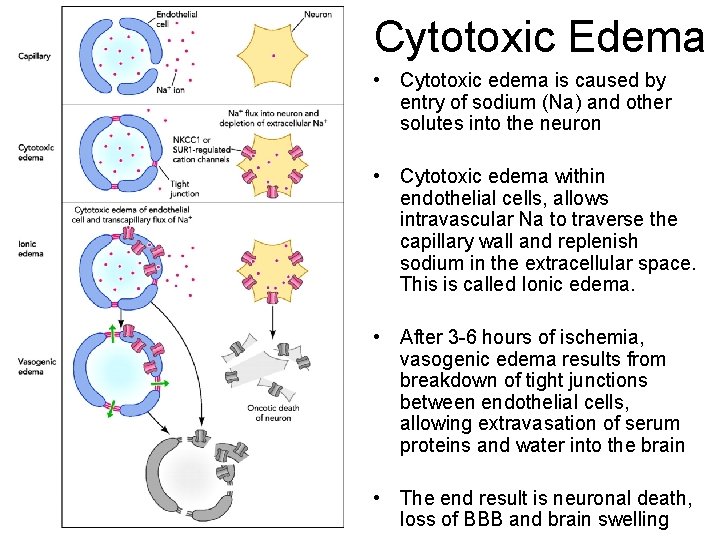
Cytotoxic Edema • Cytotoxic edema is caused by entry of sodium (Na) and other solutes into the neuron • Cytotoxic edema within endothelial cells, allows intravascular Na to traverse the capillary wall and replenish sodium in the extracellular space. This is called Ionic edema. • After 3 -6 hours of ischemia, vasogenic edema results from breakdown of tight junctions between endothelial cells, allowing extravasation of serum proteins and water into the brain • The end result is neuronal death, loss of BBB and brain swelling

Cytotoxic Edema • Cytotoxic edema is reversible at the stage where the Na/K pump is dysfunctional from lack of O 2 & ATP • When organelles like mitochondria become damaged, it the degeneration can no longer be reversed. • The area becomes edematous and ultimately fibrosed
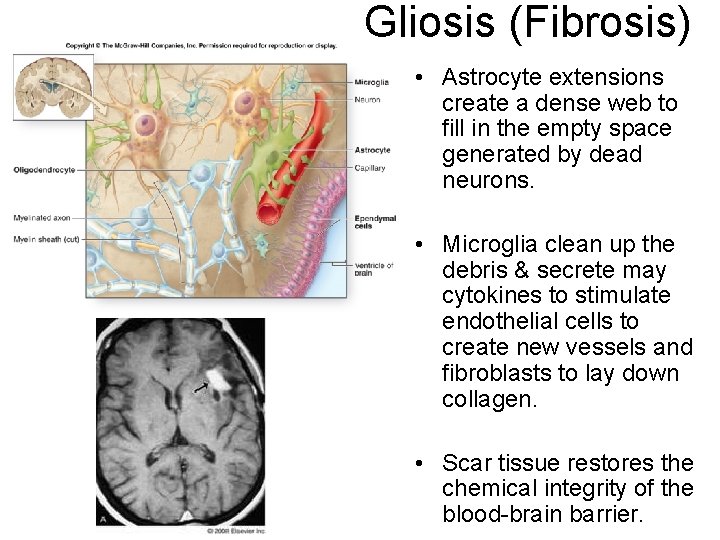
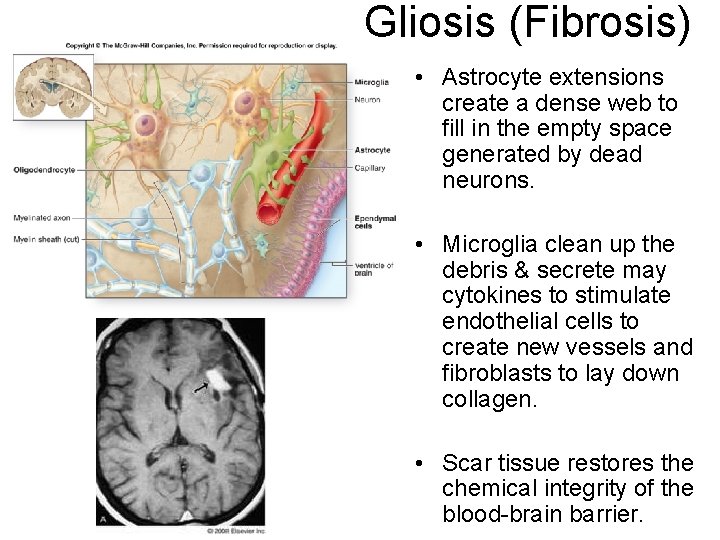
Gliosis (Fibrosis) • Astrocyte extensions create a dense web to fill in the empty space generated by dead neurons. • Microglia clean up the debris & secrete may cytokines to stimulate endothelial cells to create new vessels and fibroblasts to lay down collagen. • Scar tissue restores the chemical integrity of the blood-brain barrier.
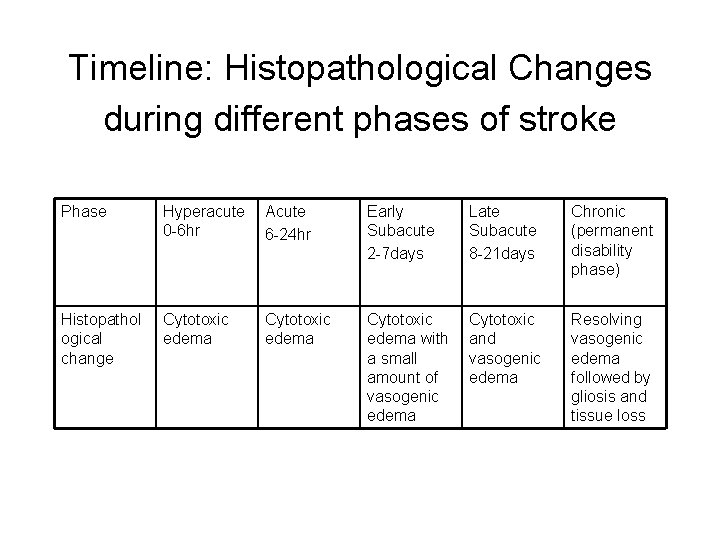
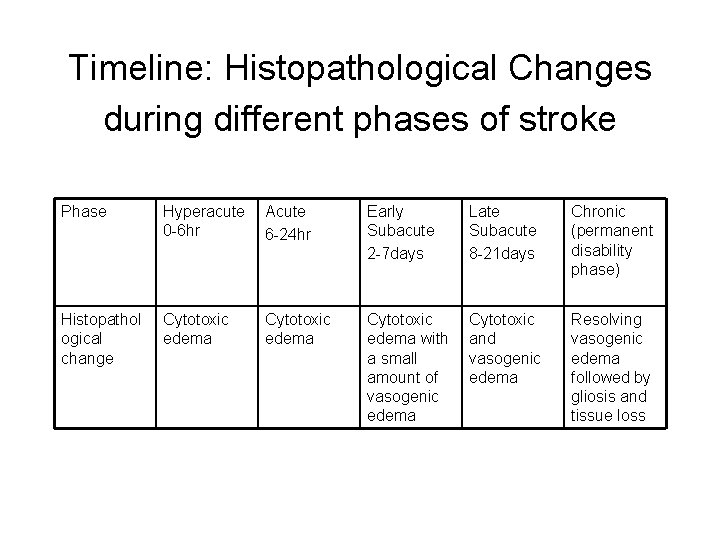
Timeline: Histopathological Changes during different phases of stroke Phase Hyperacute 0 -6 hr Acute 6 -24 hr Early Subacute 2 -7 days Late Subacute 8 -21 days Chronic (permanent disability phase) Histopathol ogical change Cytotoxic edema with a small amount of vasogenic edema Cytotoxic and vasogenic edema Resolving vasogenic edema followed by gliosis and tissue loss
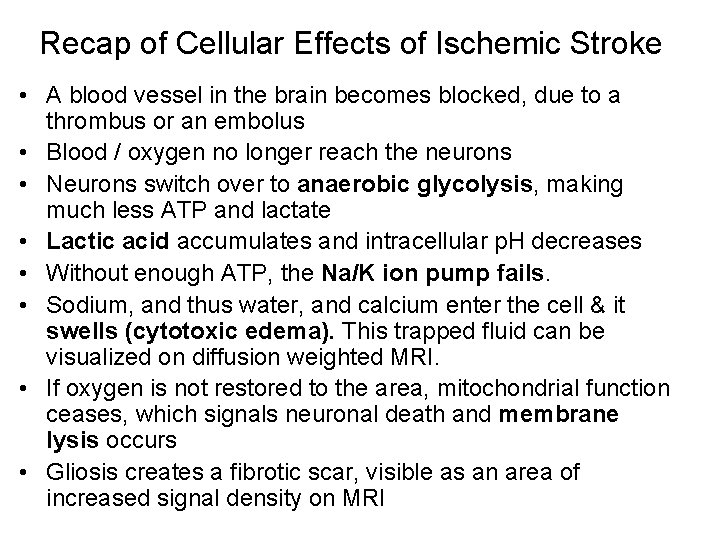
Recap of Cellular Effects of Ischemic Stroke • A blood vessel in the brain becomes blocked, due to a thrombus or an embolus • Blood / oxygen no longer reach the neurons • Neurons switch over to anaerobic glycolysis, making much less ATP and lactate • Lactic acid accumulates and intracellular p. H decreases • Without enough ATP, the Na/K ion pump fails. • Sodium, and thus water, and calcium enter the cell & it swells (cytotoxic edema). This trapped fluid can be visualized on diffusion weighted MRI. • If oxygen is not restored to the area, mitochondrial function ceases, which signals neuronal death and membrane lysis occurs • Gliosis creates a fibrotic scar, visible as an area of increased signal density on MRI
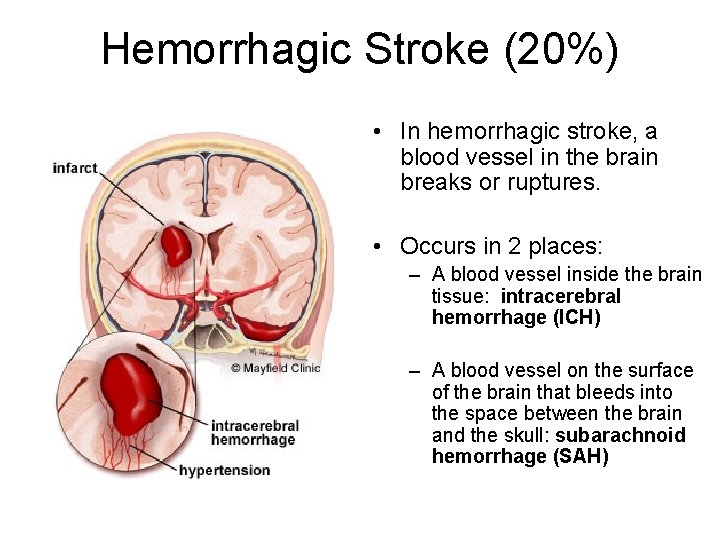
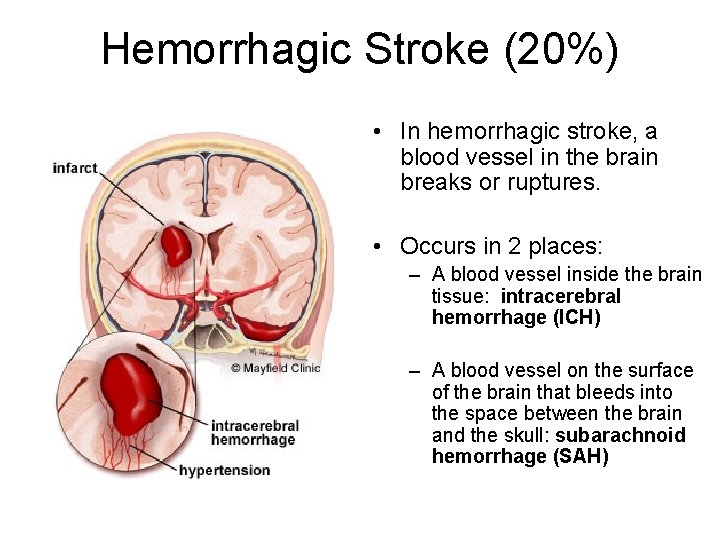
Hemorrhagic Stroke (20%) • In hemorrhagic stroke, a blood vessel in the brain breaks or ruptures. • Occurs in 2 places: – A blood vessel inside the brain tissue: intracerebral hemorrhage (ICH) – A blood vessel on the surface of the brain that bleeds into the space between the brain and the skull: subarachnoid hemorrhage (SAH)
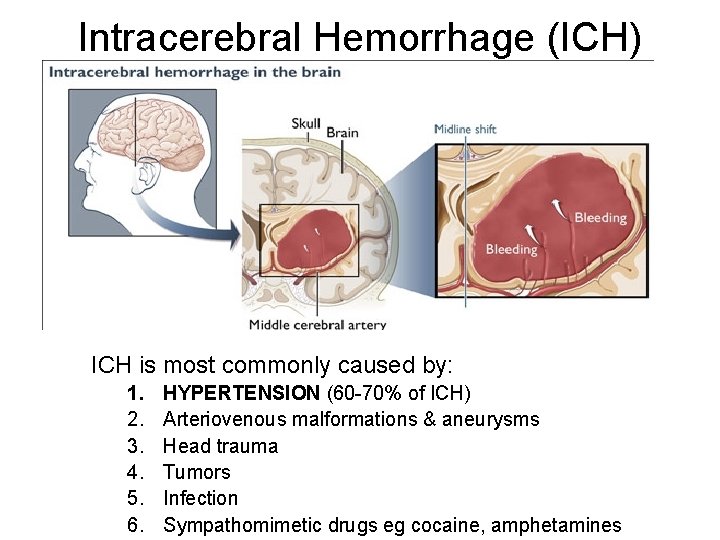
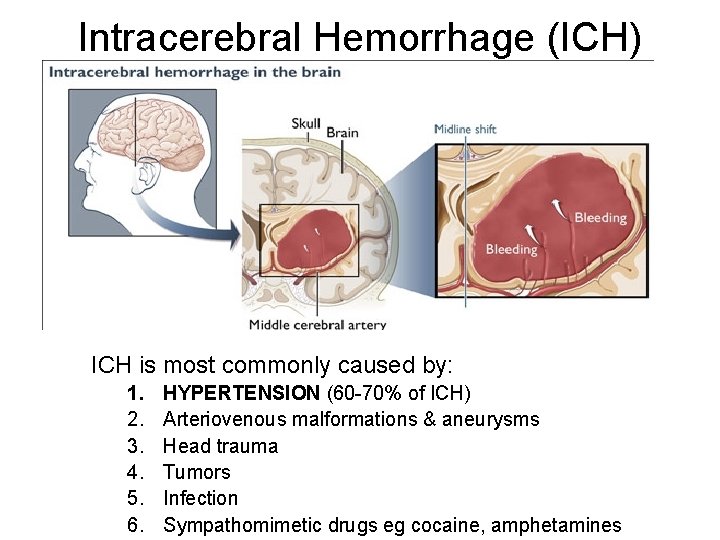
Intracerebral Hemorrhage (ICH) ICH is most commonly caused by: 1. 2. 3. 4. 5. 6. HYPERTENSION (60 -70% of ICH) Arteriovenous malformations & aneurysms Head trauma Tumors Infection Sympathomimetic drugs eg cocaine, amphetamines
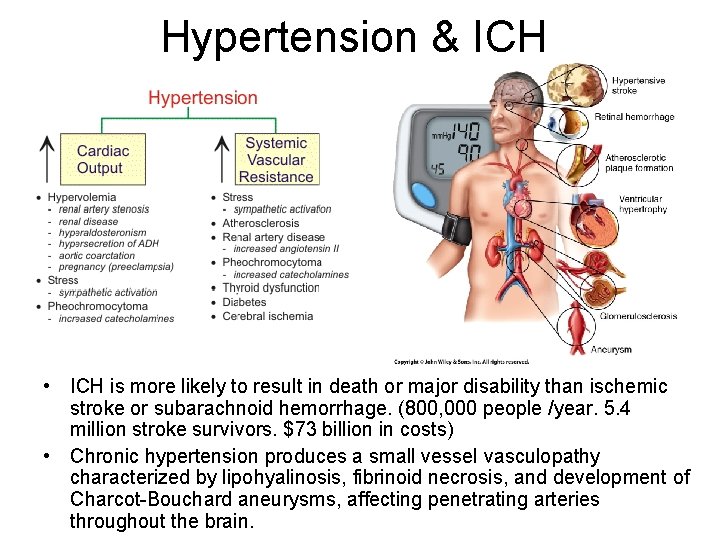
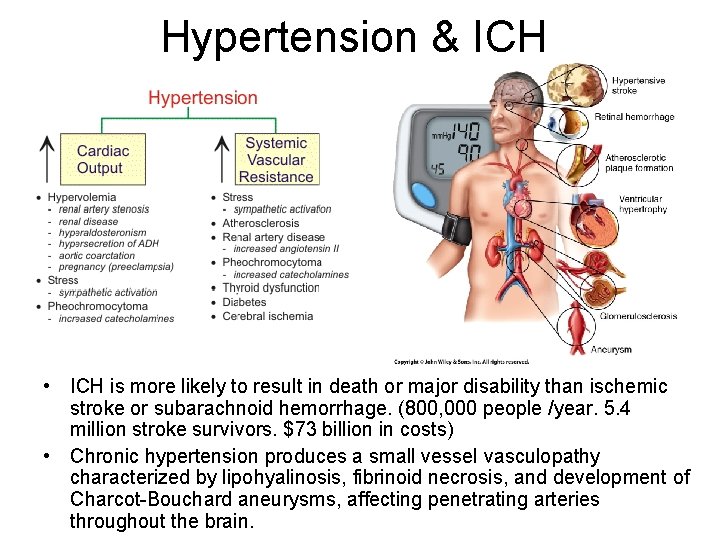
Hypertension & ICH • ICH is more likely to result in death or major disability than ischemic stroke or subarachnoid hemorrhage. (800, 000 people /year. 5. 4 million stroke survivors. $73 billion in costs) • Chronic hypertension produces a small vessel vasculopathy characterized by lipohyalinosis, fibrinoid necrosis, and development of Charcot-Bouchard aneurysms, affecting penetrating arteries throughout the brain.
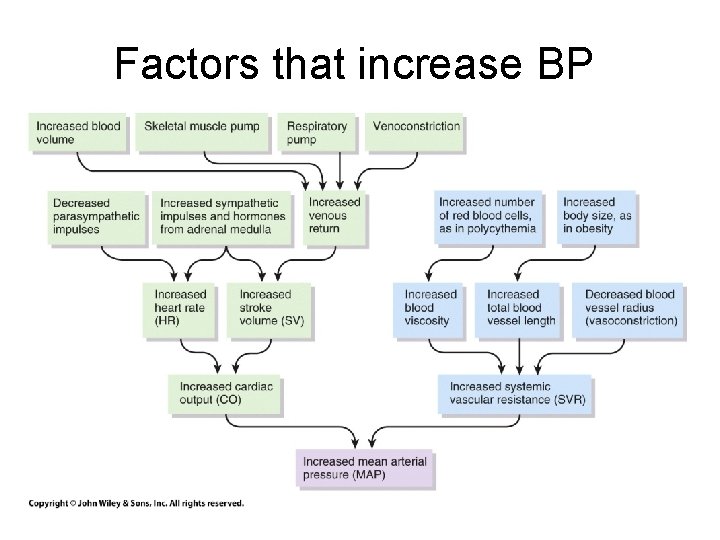
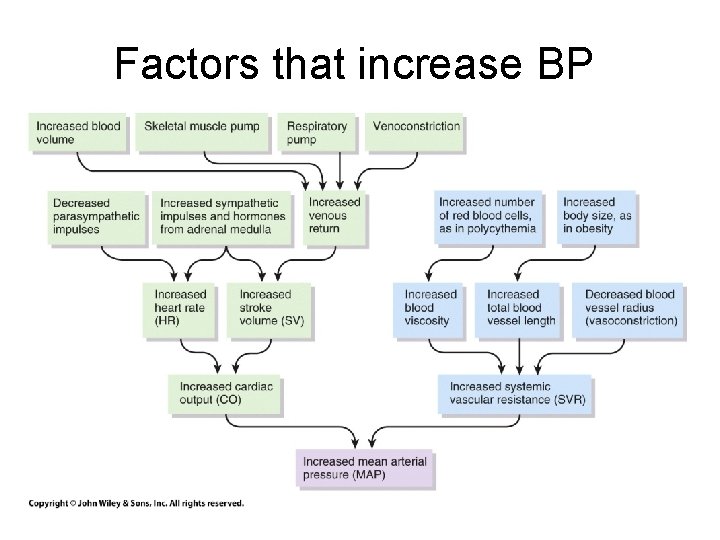
Factors that increase BP
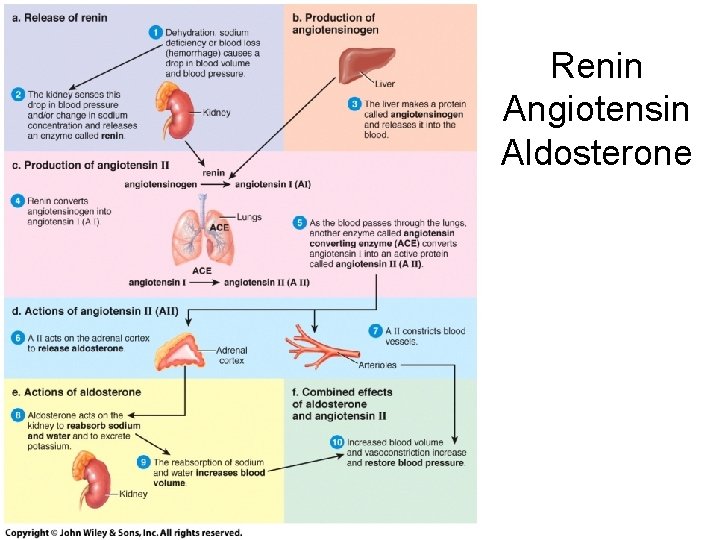
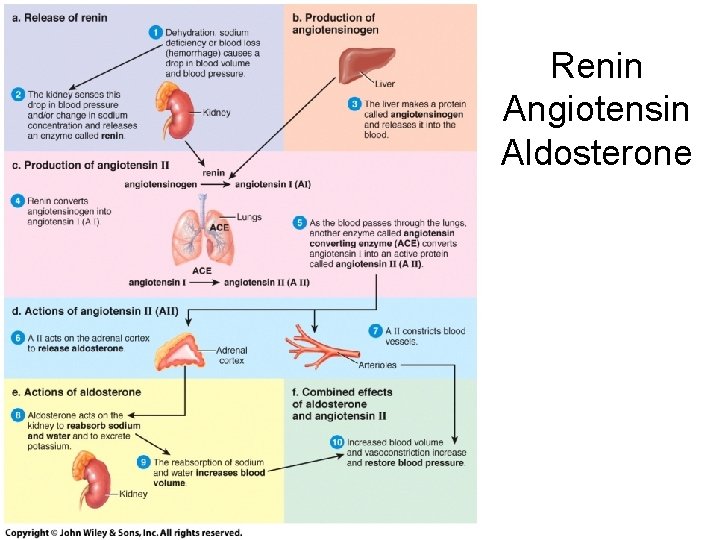
Renin Angiotensin Aldosterone
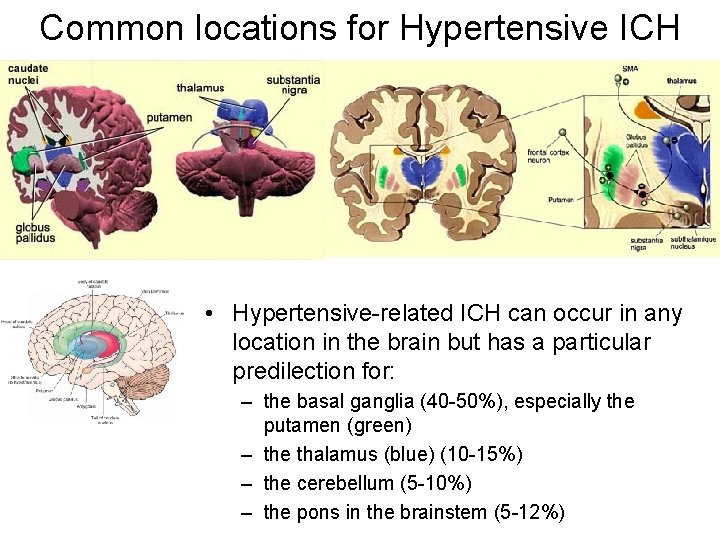
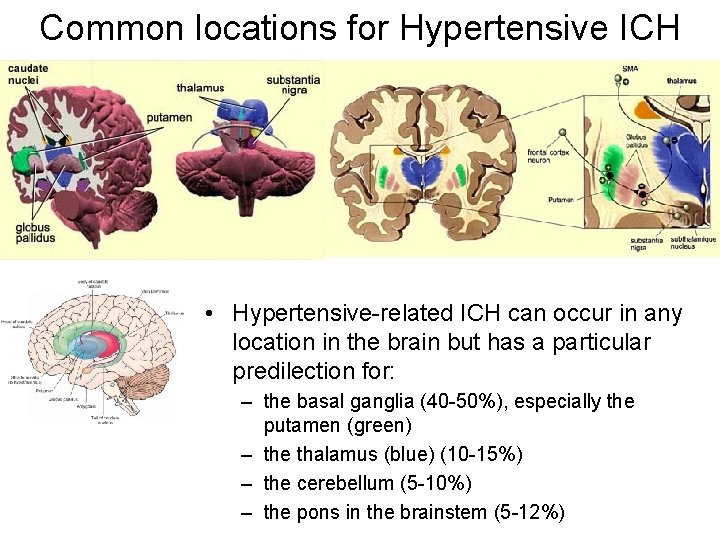
Common locations for Hypertensive ICH • Hypertensive-related ICH can occur in any location in the brain but has a particular predilection for: – the basal ganglia (40 -50%), especially the putamen (green) – the thalamus (blue) (10 -15%) – the cerebellum (5 -10%) – the pons in the brainstem (5 -12%)
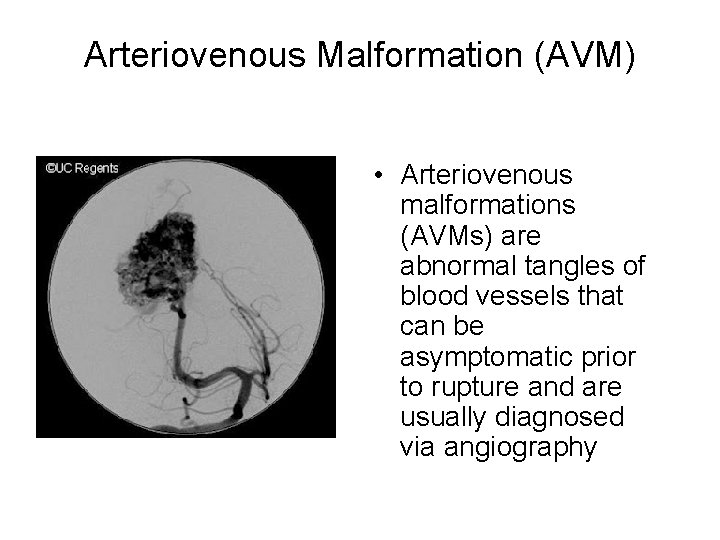
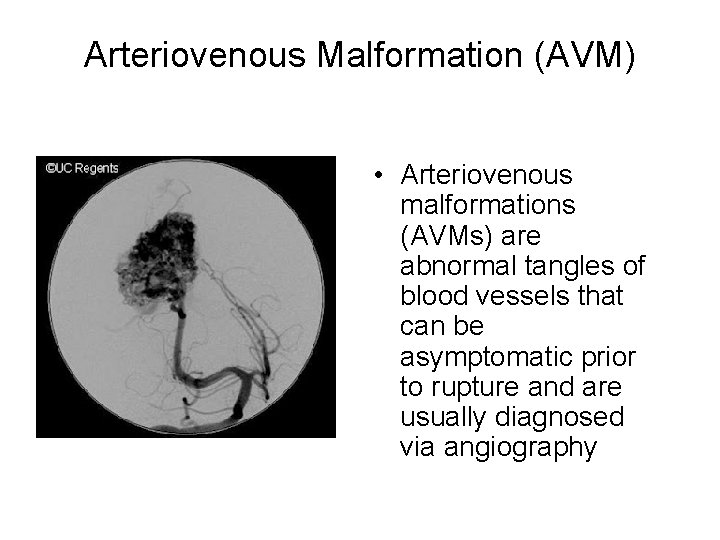
Arteriovenous Malformation (AVM) • Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels that can be asymptomatic prior to rupture and are usually diagnosed via angiography
Less common causes of ICH • Amyloid Angiopathy deposition of an abnormal protein weakens blood vessel walls. usually a disease of the elderly • Coagulopathy - increased bleeding tendency. from disorders such as liver disease, malignancy, or blood thinning medications • Ischemic stroke with secondary hemorrhage • Vasculitis -Inflammatory disorders involving the blood vessels of the
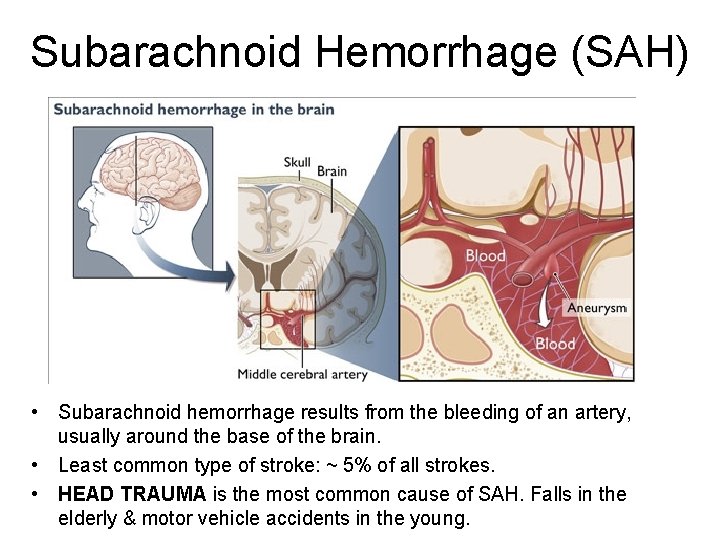
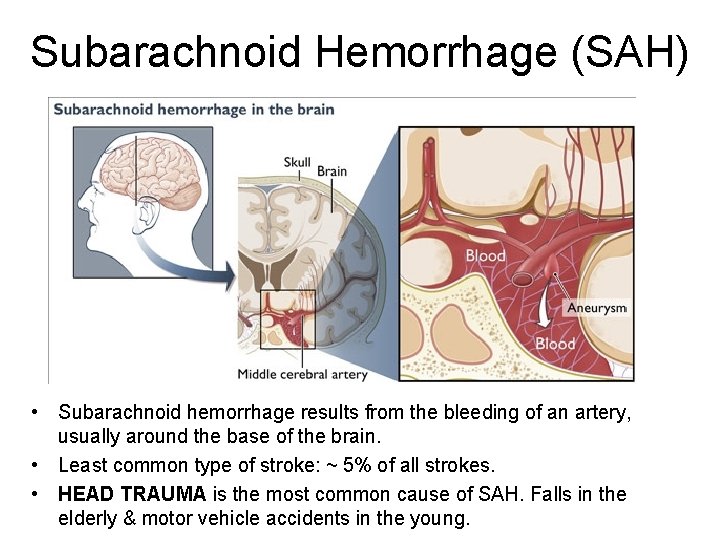
Subarachnoid Hemorrhage (SAH) • Subarachnoid hemorrhage results from the bleeding of an artery, usually around the base of the brain. • Least common type of stroke: ~ 5% of all strokes. • HEAD TRAUMA is the most common cause of SAH. Falls in the elderly & motor vehicle accidents in the young.
Traumatic SAH • Traumatic brain injury results from an external force hitting the head at high velocity which causes the brain to hit the inside of the skull, damaging blood vessels in the subarachnoid space. • This can be life threatening if the intracranial pressure exceeds the mean arterial blood pressure
Aneurysm • 80% of non-traumatic subarachnoid hemorrhage results from a ruptured berry ANEURYSM. • Aneurysms are defects in blood vessels thought to expand as a result of hydrostatic pressure from pulsatile blood flow and blood turbulence, which is greatest at the arterial bifurcations
Other Causes of SAH • Trauma is the most common. Usually falls in the elderly & motor vehicle accidents in the young • Ruptured Berry Aneurysm 80% of non traumatic SAH Other causes: • Bleeding from an arteriovenous malformation (AVM) • Bleeding from a cerebral aneurysm • Bleeding disorder • Use of blood thinners
Risks & Symptoms for SAH Risk Factors for SAH • • high blood pressure cigarette smoking oral contraceptives pregnancy and child birth cocaine abuse aneurysm fibromuscular dysplasia (FMD) and other connective tissue disorders • history of polycystic kidney disease (from htn) Symptoms of SAH • Main symptom is a severe headache that starts suddenly and is often worse near the back of the head. Patients often describe it as the "worst headache ever” • Blood throughout the subarachnoid space, causes headache and neck stiffness • Raised intracranial pressure, causes possibility of depressed conscious level, headache, vomiting, papilloedema
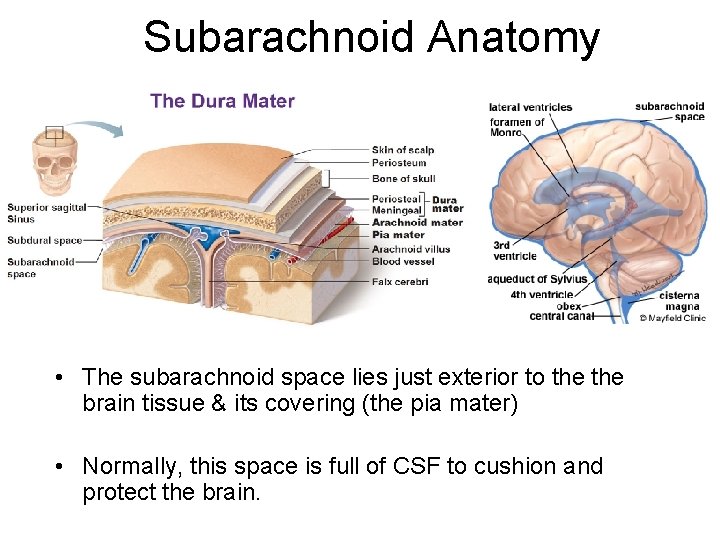
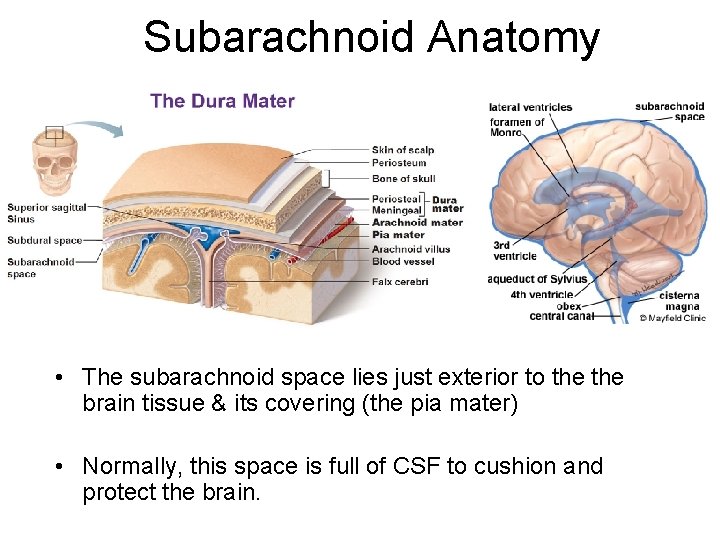
Subarachnoid Anatomy • The subarachnoid space lies just exterior to the brain tissue & its covering (the pia mater) • Normally, this space is full of CSF to cushion and protect the brain.
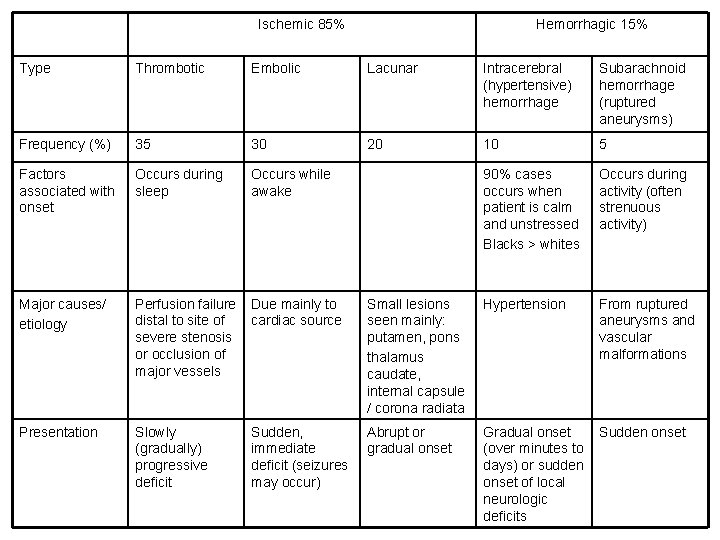
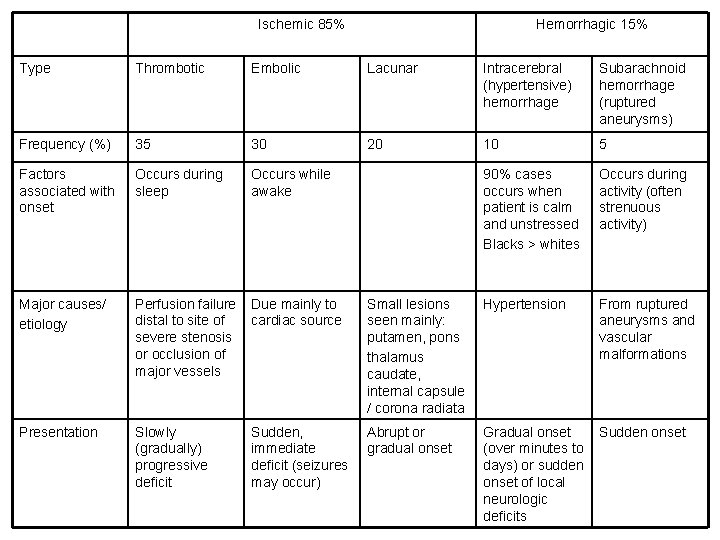
Ischemic 85% Hemorrhagic 15% Type Thrombotic Embolic Lacunar Intracerebral (hypertensive) hemorrhage Subarachnoid hemorrhage (ruptured aneurysms) Frequency (%) 35 30 20 10 5 Factors associated with onset Occurs during sleep Occurs while awake 90% cases occurs when patient is calm and unstressed Blacks > whites Occurs during activity (often strenuous activity) Major causes/ etiology Perfusion failure distal to site of severe stenosis or occlusion of major vessels Due mainly to cardiac source Small lesions seen mainly: putamen, pons thalamus caudate, internal capsule / corona radiata Hypertension From ruptured aneurysms and vascular malformations Presentation Slowly (gradually) progressive deficit Sudden, immediate deficit (seizures may occur) Abrupt or gradual onset Gradual onset (over minutes to days) or sudden onset of local neurologic deficits Sudden onset
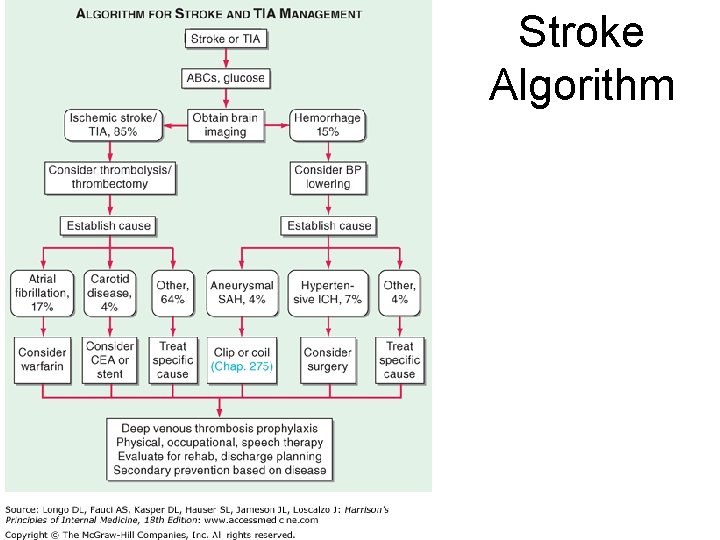
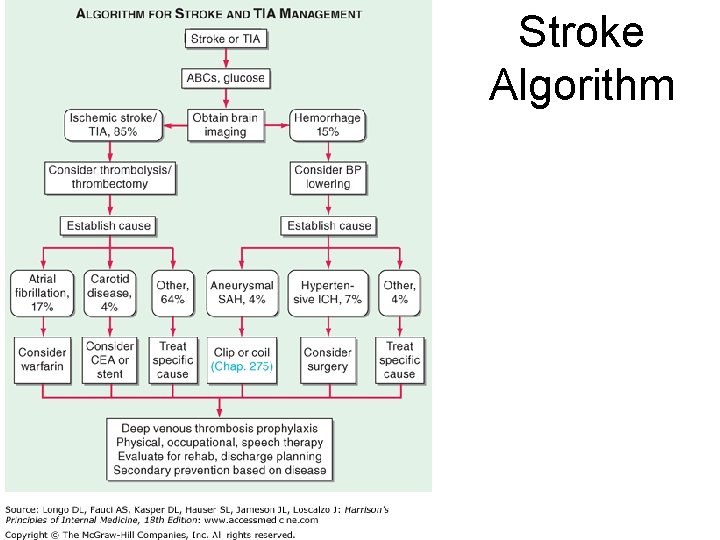
Stroke Algorithm

Diagnosis: Neurological exam Is it a stroke? • Stroke can be clinically diagnosis based on history and physical examination (NIH Stroke Scale evaluation). • http: //www. strokecenter. org/professionals/strok e-diagnosis/stroke-assessment-scalesoverview/ for complete chart evaluation tools LOOKING FOR SIGNS OF THESE AND MORE: • Aphasia: total or partial loss of ability to understand or use words - trouble finding words or unable to speak. problems understanding what others are saying or trouble with reading, writing or math. may have trouble talking yet understand what others say. • Apraxia: inability to control muscles making uncoordinated and jerky movements • Dysarthria: loss of control of muscles in face & mouth - voice may sound slurred, muffled, hoarse. mouth may droop on one side of face from muscle weakness. • Dysphagia: difficulty swallowing • Paralysis: loss of muscle function and sensation • Hemiparesis: weakness of muscles on one side of the body. • Hemianopia: loss of sight in half of visual field


Stroke Syndromes • The “hallmark” of an acute stroke is the sudden onset of focal neurologic dysfunction, corresponding to a distinct vascular territory. • A careful history and neurologic examination can often localize the region of brain dysfunction
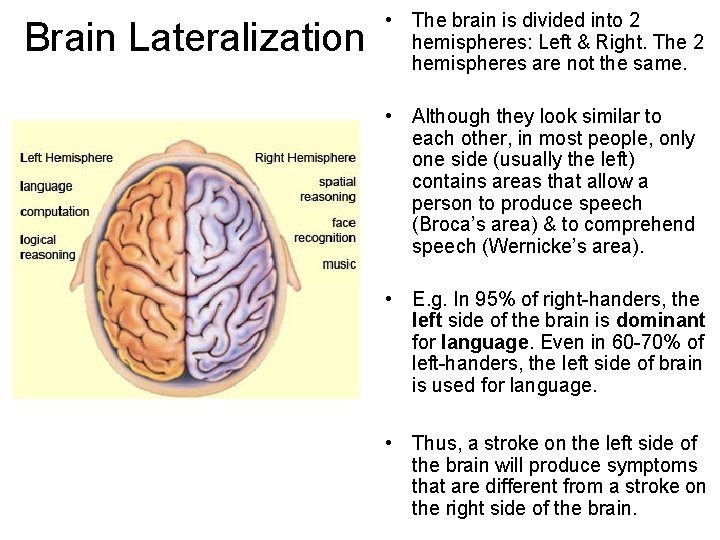
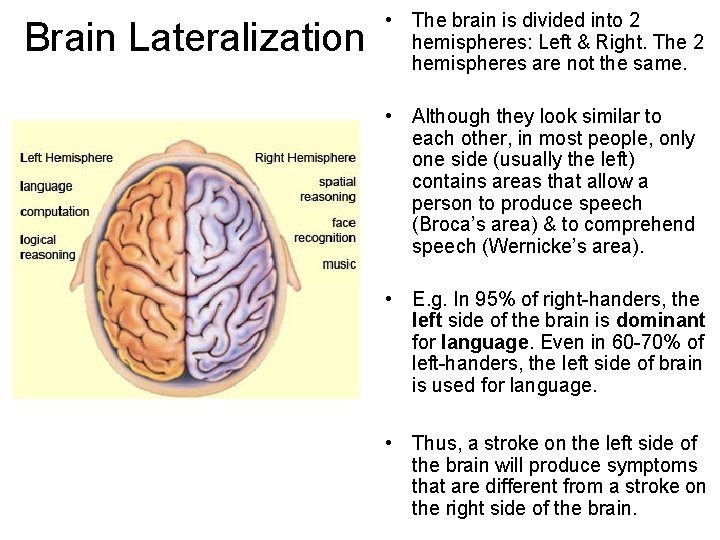
Brain Lateralization • The brain is divided into 2 hemispheres: Left & Right. The 2 hemispheres are not the same. • Although they look similar to each other, in most people, only one side (usually the left) contains areas that allow a person to produce speech (Broca’s area) & to comprehend speech (Wernicke’s area). • E. g. In 95% of right-handers, the left side of the brain is dominant for language. Even in 60 -70% of left-handers, the left side of brain is used for language. • Thus, a stroke on the left side of the brain will produce symptoms that are different from a stroke on the right side of the brain.
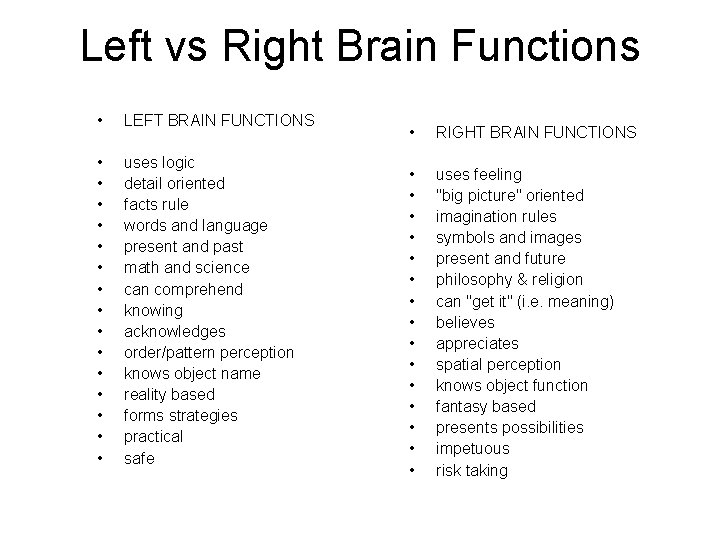
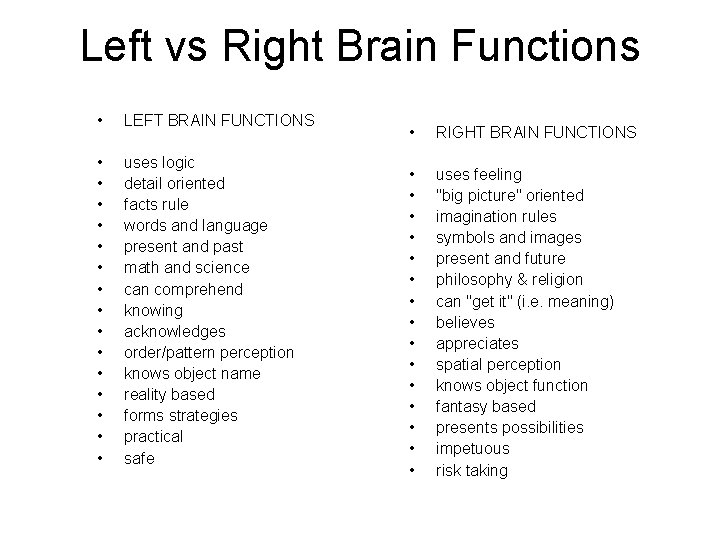
Left vs Right Brain Functions • LEFT BRAIN FUNCTIONS • • • • uses logic detail oriented facts rule words and language present and past math and science can comprehend knowing acknowledges order/pattern perception knows object name reality based forms strategies practical safe • RIGHT BRAIN FUNCTIONS • • • • uses feeling "big picture" oriented imagination rules symbols and images present and future philosophy & religion can "get it" (i. e. meaning) believes appreciates spatial perception knows object function fantasy based presents possibilities impetuous risk taking
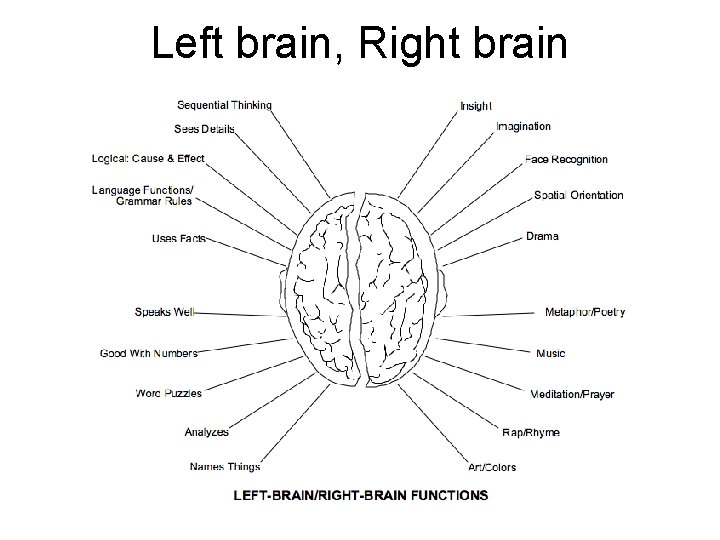
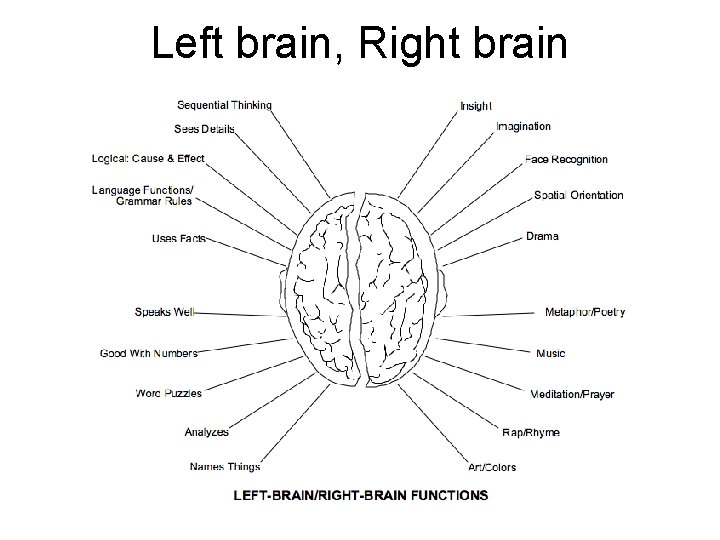
Left brain, Right brain
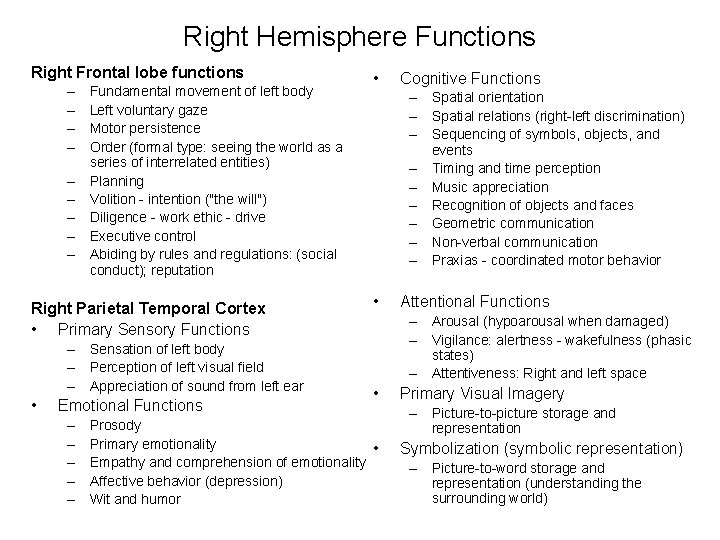
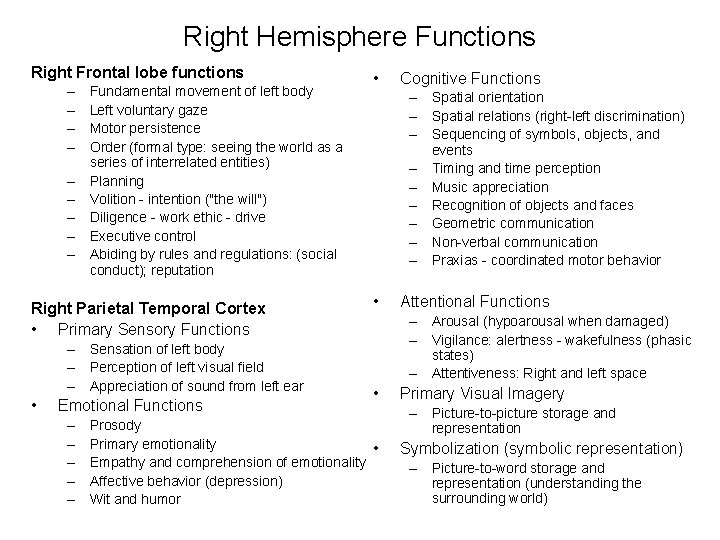
Right Hemisphere Functions Right Frontal lobe functions – – – – – Fundamental movement of left body Left voluntary gaze Motor persistence Order (formal type: seeing the world as a series of interrelated entities) Planning Volition - intention ("the will") Diligence - work ethic - drive Executive control Abiding by rules and regulations: (social conduct); reputation Right Parietal Temporal Cortex • Primary Sensory Functions – Sensation of left body – Perception of left visual field – Appreciation of sound from left ear • Emotional Functions – – – • Cognitive Functions – Spatial orientation – Spatial relations (right-left discrimination) – Sequencing of symbols, objects, and events – Timing and time perception – Music appreciation – Recognition of objects and faces – Geometric communication – Non-verbal communication – Praxias - coordinated motor behavior • Attentional Functions – Arousal (hypoarousal when damaged) – Vigilance: alertness - wakefulness (phasic states) – Attentiveness: Right and left space • Prosody Primary emotionality • Empathy and comprehension of emotionality Affective behavior (depression) Wit and humor Primary Visual Imagery – Picture-to-picture storage and representation Symbolization (symbolic representation) – Picture-to-word storage and representation (understanding the surrounding world)
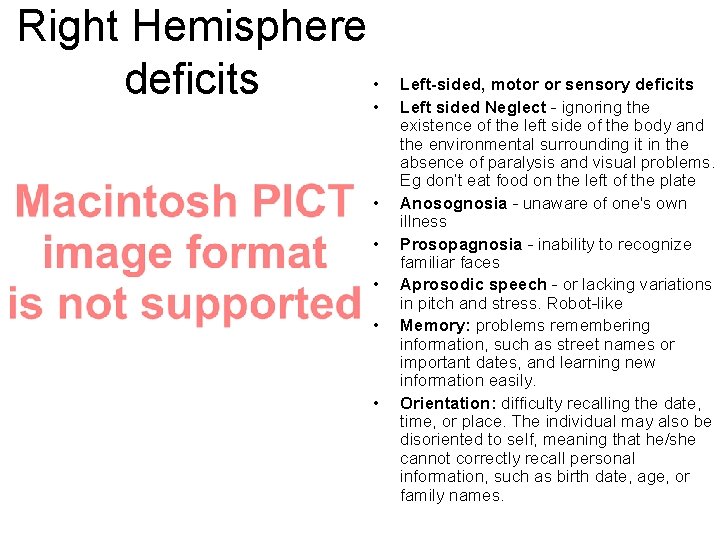
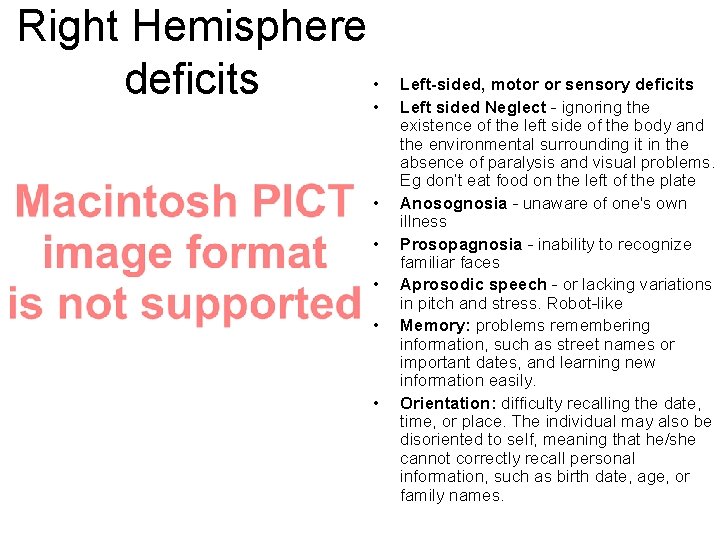
Right Hemisphere deficits • • Left-sided, motor or sensory deficits Left sided Neglect - ignoring the existence of the left side of the body and the environmental surrounding it in the absence of paralysis and visual problems. Eg don’t eat food on the left of the plate Anosognosia - unaware of one's own illness Prosopagnosia - inability to recognize familiar faces Aprosodic speech - or lacking variations in pitch and stress. Robot-like Memory: problems remembering information, such as street names or important dates, and learning new information easily. Orientation: difficulty recalling the date, time, or place. The individual may also be disoriented to self, meaning that he/she cannot correctly recall personal information, such as birth date, age, or family names.
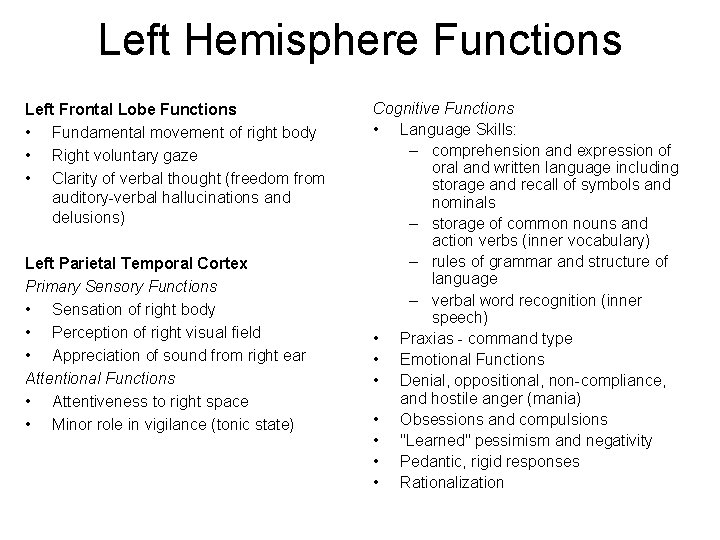
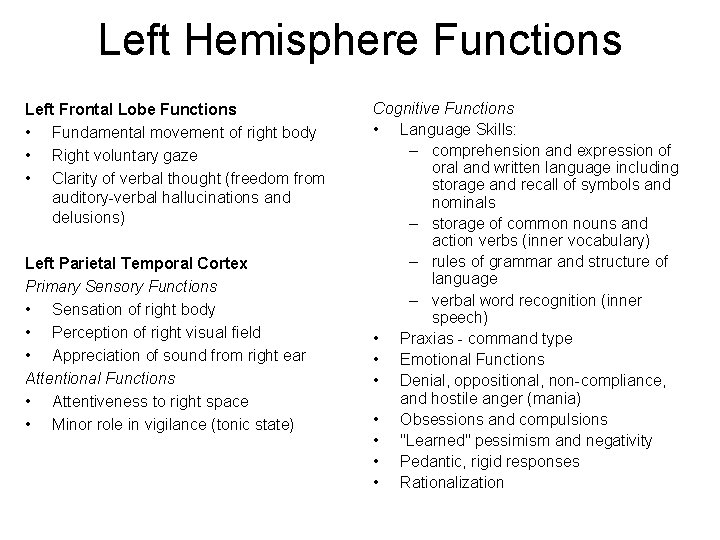
Left Hemisphere Functions Left Frontal Lobe Functions • Fundamental movement of right body • Right voluntary gaze • Clarity of verbal thought (freedom from auditory-verbal hallucinations and delusions) Left Parietal Temporal Cortex Primary Sensory Functions • Sensation of right body • Perception of right visual field • Appreciation of sound from right ear Attentional Functions • Attentiveness to right space • Minor role in vigilance (tonic state) Cognitive Functions • Language Skills: – comprehension and expression of oral and written language including storage and recall of symbols and nominals – storage of common nouns and action verbs (inner vocabulary) – rules of grammar and structure of language – verbal word recognition (inner speech) • Praxias - command type • Emotional Functions • Denial, oppositional, non-compliance, and hostile anger (mania) • Obsessions and compulsions • "Learned" pessimism and negativity • Pedantic, rigid responses • Rationalization
Left Hemisphere Deficits • • Right hemiplegia Aphasia: aphasia can affect auditory comprehension, oral expression, reading and writing – Wernicke’s aphasia: ‘cocktail hour speech’. long, grammatically well formed, utterances that contain almost no meaning. – Broca’s aphasia: Sentence length is short. Speech is labored and slow. impaired word finding – difficulty in learning new information and problems in conceptualizing and generalizing – develop a slow and cautious behavioral style
Now you know which side the lesion is on, but which artery was affected?
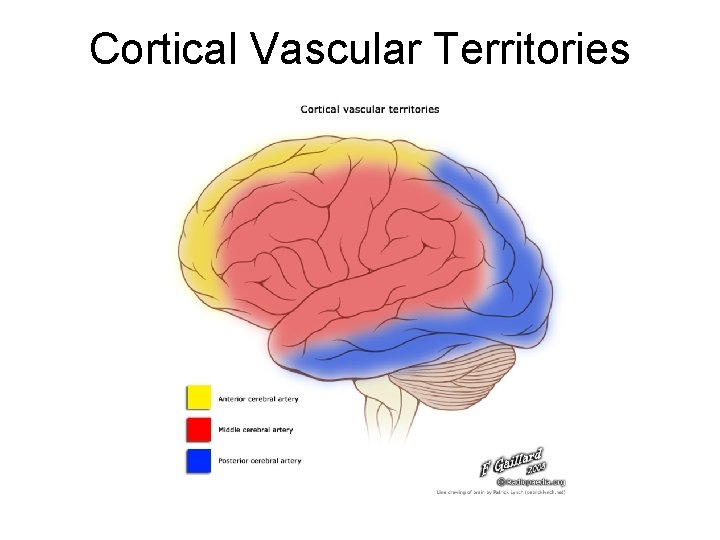
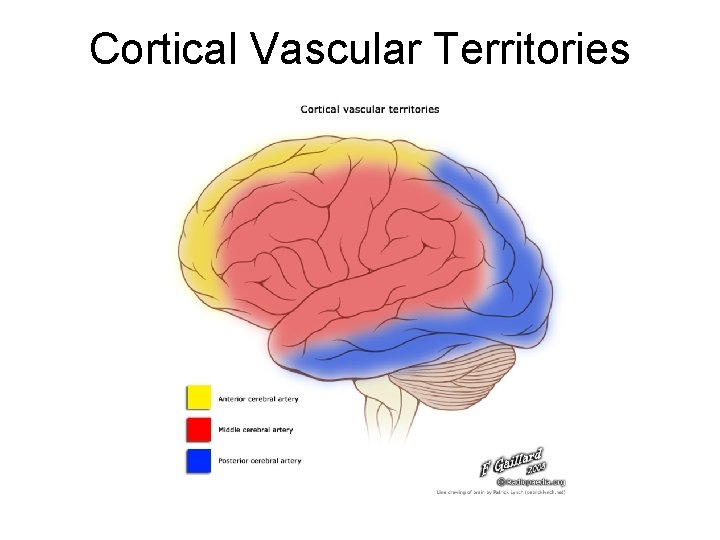
Cortical Vascular Territories
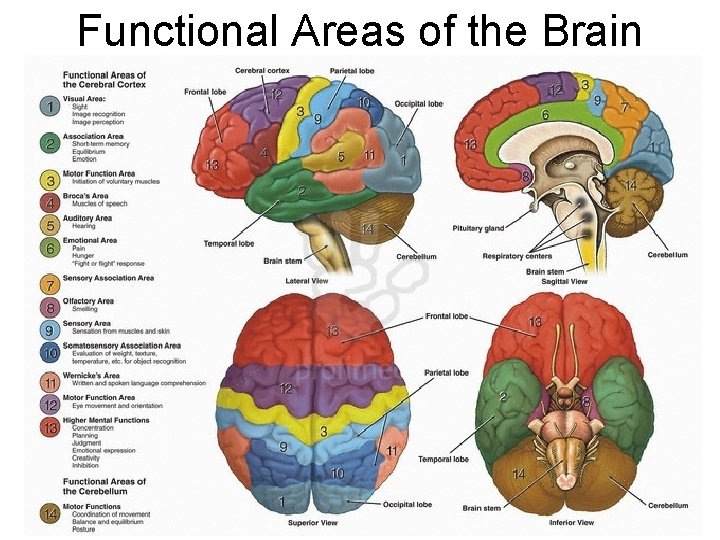
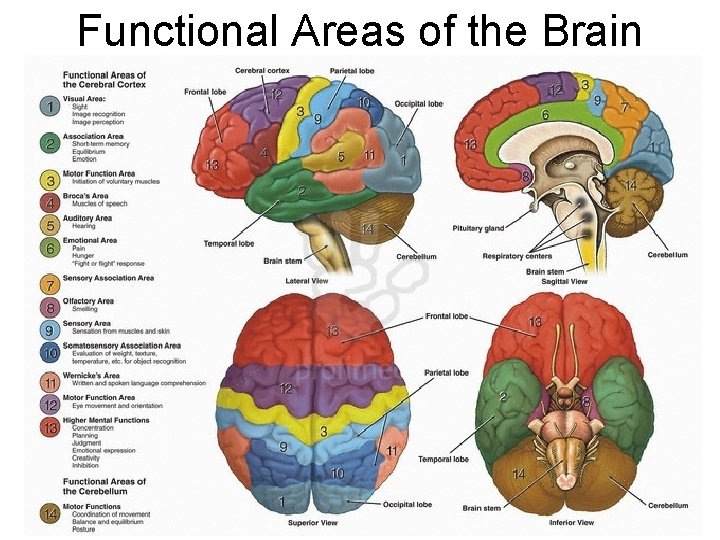
Functional Areas of the Brain
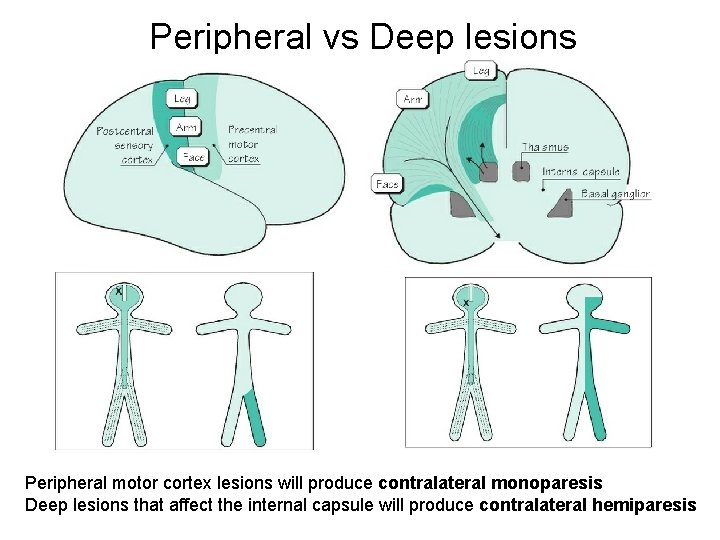
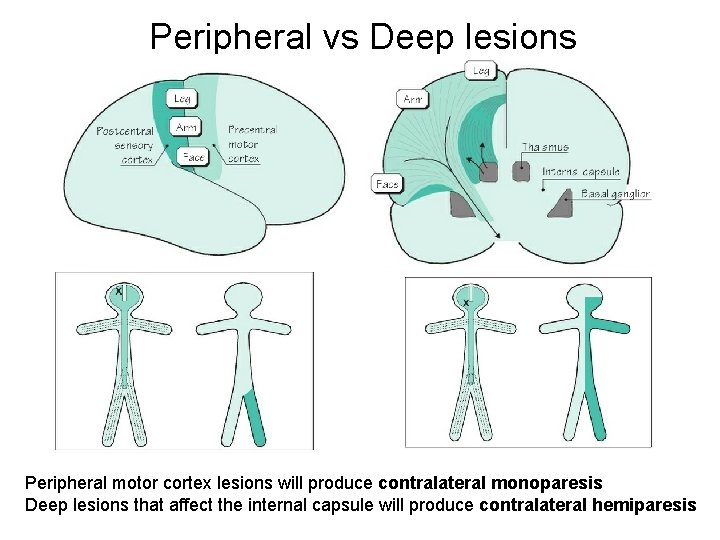
Peripheral vs Deep lesions Peripheral motor cortex lesions will produce contralateral monoparesis Deep lesions that affect the internal capsule will produce contralateral hemiparesis
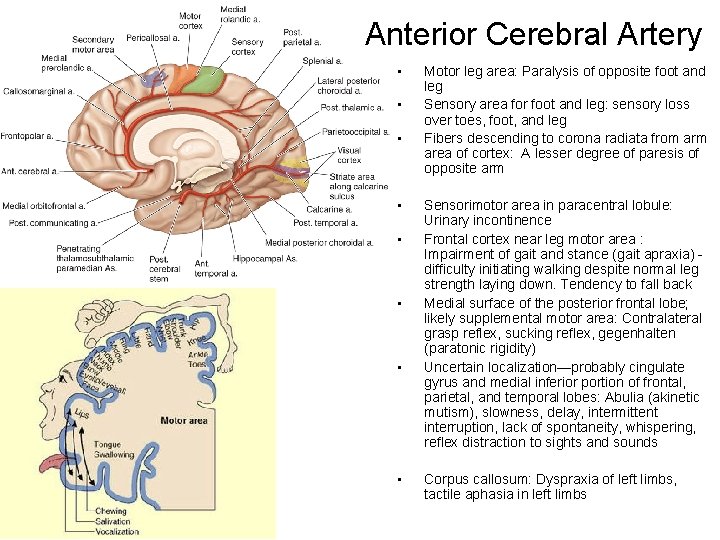
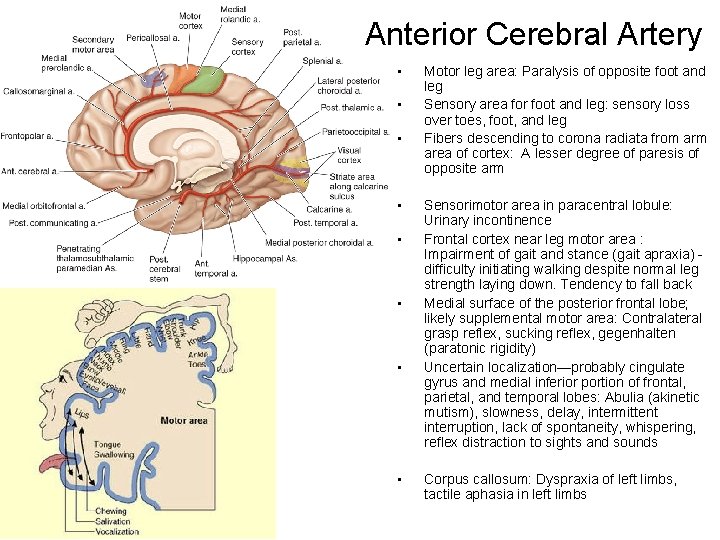
Anterior Cerebral Artery • • Motor leg area: Paralysis of opposite foot and leg Sensory area for foot and leg: sensory loss over toes, foot, and leg Fibers descending to corona radiata from area of cortex: A lesser degree of paresis of opposite arm Sensorimotor area in paracentral lobule: Urinary incontinence Frontal cortex near leg motor area : Impairment of gait and stance (gait apraxia) difficulty initiating walking despite normal leg strength laying down. Tendency to fall back Medial surface of the posterior frontal lobe; likely supplemental motor area: Contralateral grasp reflex, sucking reflex, gegenhalten (paratonic rigidity) Uncertain localization—probably cingulate gyrus and medial inferior portion of frontal, parietal, and temporal lobes: Abulia (akinetic mutism), slowness, delay, intermittent interruption, lack of spontaneity, whispering, reflex distraction to sights and sounds Corpus callosum: Dyspraxia of left limbs, tactile aphasia in left limbs
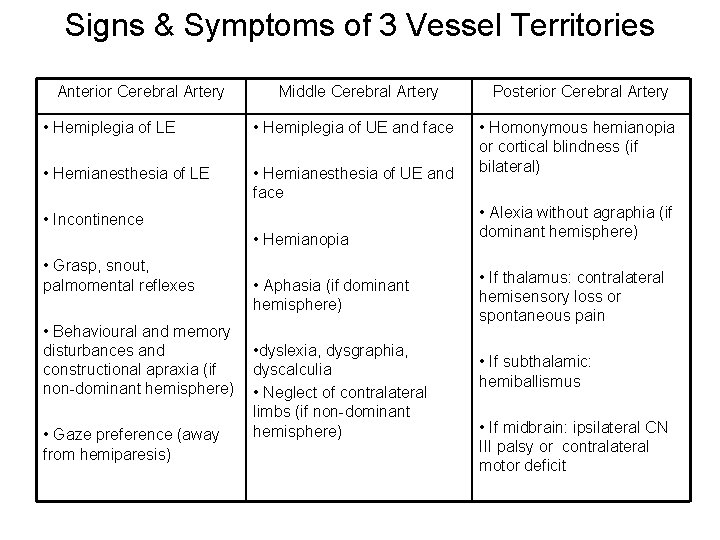
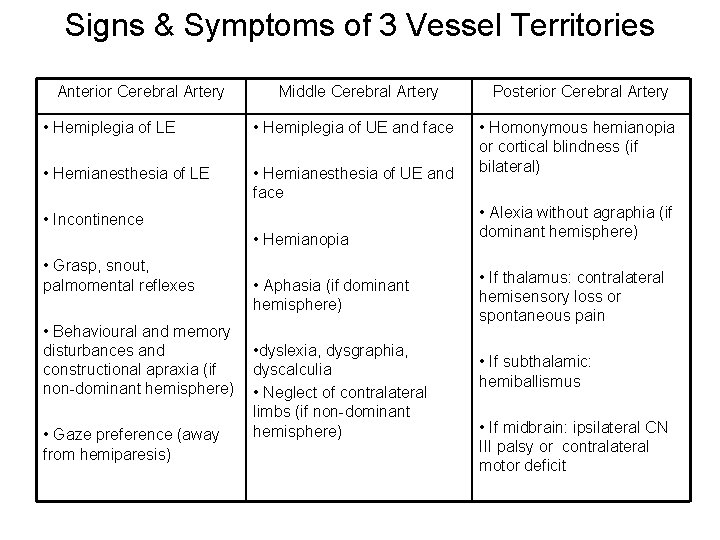
Signs & Symptoms of 3 Vessel Territories Anterior Cerebral Artery Middle Cerebral Artery • Hemiplegia of LE • Hemiplegia of UE and face • Hemianesthesia of LE • Hemianesthesia of UE and face • Incontinence • Hemianopia • Grasp, snout, palmomental reflexes • Behavioural and memory disturbances and constructional apraxia (if non-dominant hemisphere) • Gaze preference (away from hemiparesis) • Aphasia (if dominant hemisphere) • dyslexia, dysgraphia, dyscalculia • Neglect of contralateral limbs (if non-dominant hemisphere) Posterior Cerebral Artery • Homonymous hemianopia or cortical blindness (if bilateral) • Alexia without agraphia (if dominant hemisphere) • If thalamus: contralateral hemisensory loss or spontaneous pain • If subthalamic: hemiballismus • If midbrain: ipsilateral CN III palsy or contralateral motor deficit
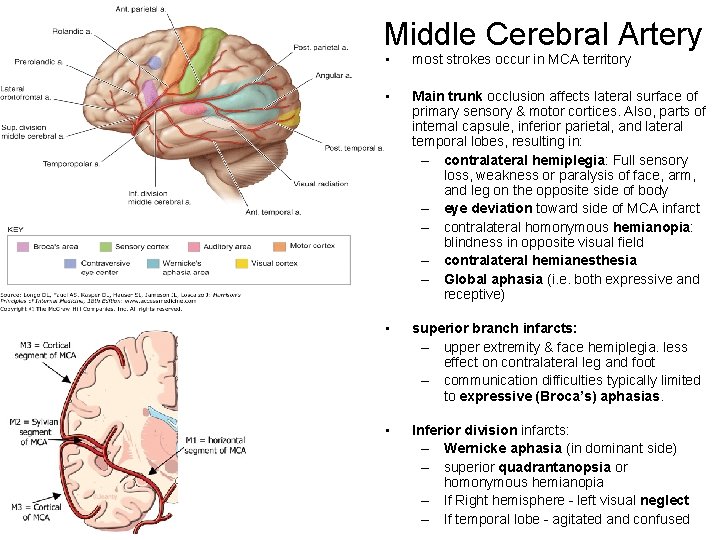
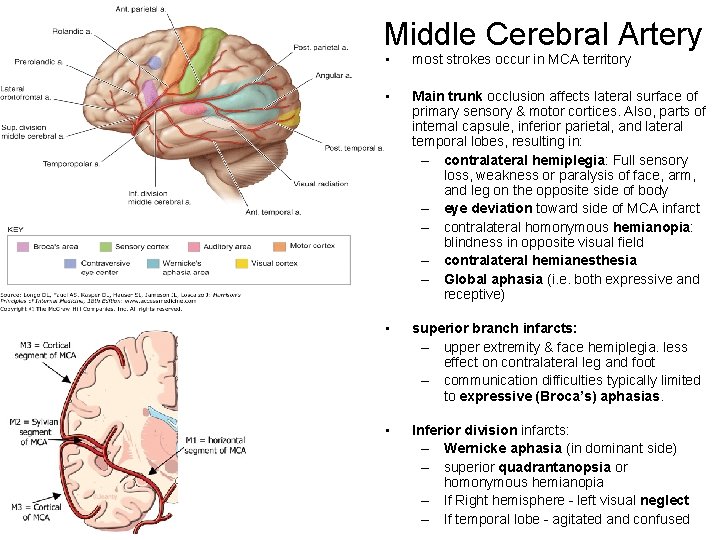
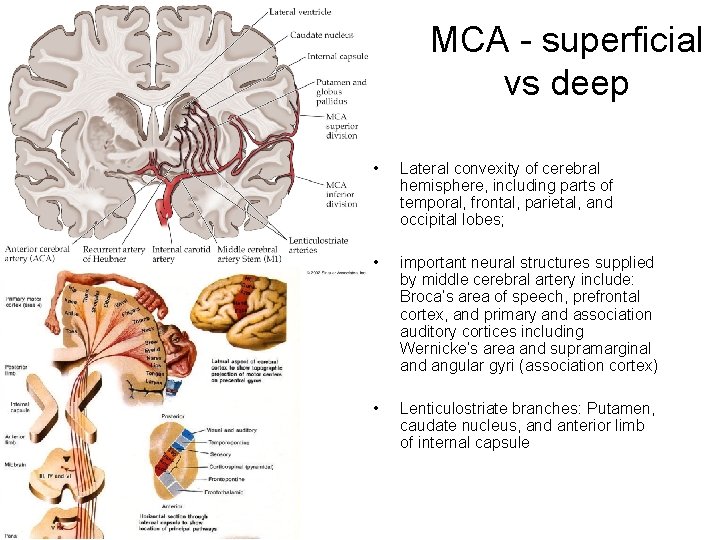
Middle Cerebral Artery • most strokes occur in MCA territory • Main trunk occlusion affects lateral surface of primary sensory & motor cortices. Also, parts of internal capsule, inferior parietal, and lateral temporal lobes, resulting in: – contralateral hemiplegia: Full sensory loss, weakness or paralysis of face, arm, and leg on the opposite side of body – eye deviation toward side of MCA infarct – contralateral homonymous hemianopia: blindness in opposite visual field – contralateral hemianesthesia – Global aphasia (i. e. both expressive and receptive) • superior branch infarcts: – upper extremity & face hemiplegia. less effect on contralateral leg and foot – communication difficulties typically limited to expressive (Broca’s) aphasias. • Inferior division infarcts: – Wernicke aphasia (in dominant side) – superior quadrantanopsia or homonymous hemianopia – If Right hemisphere - left visual neglect – If temporal lobe - agitated and confused

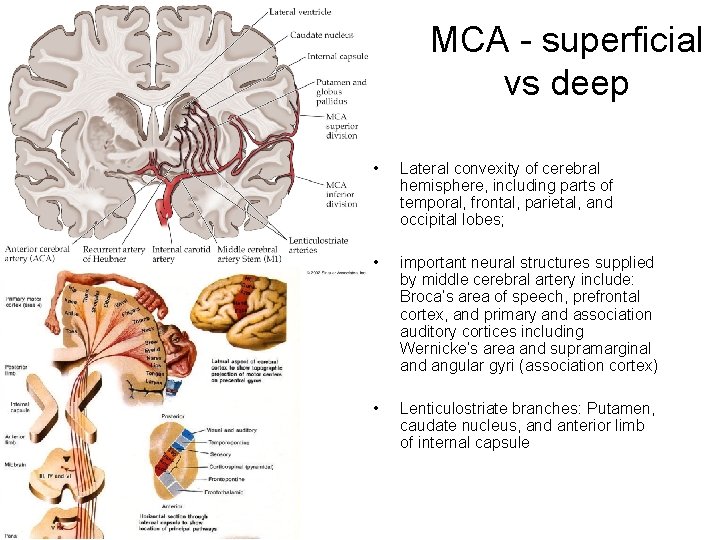
MCA - superficial vs deep • Lateral convexity of cerebral hemisphere, including parts of temporal, frontal, parietal, and occipital lobes; • important neural structures supplied by middle cerebral artery include: Broca’s area of speech, prefrontal cortex, and primary and association auditory cortices including Wernicke’s area and supramarginal and angular gyri (association cortex) • Lenticulostriate branches: Putamen, caudate nucleus, and anterior limb of internal capsule
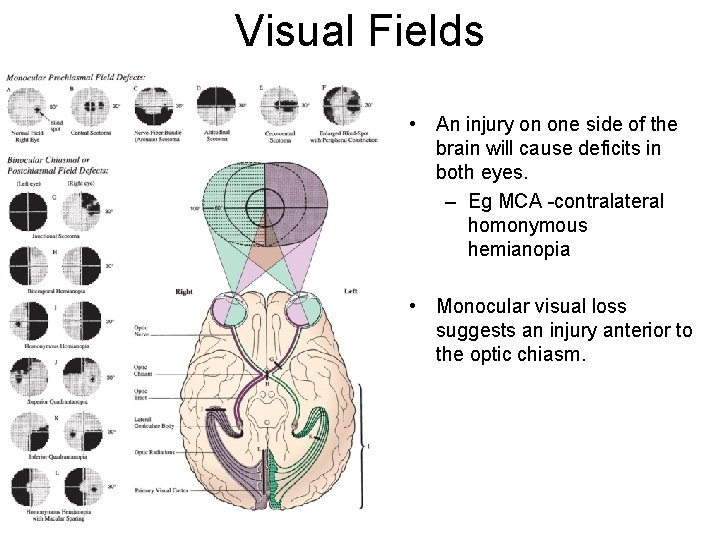
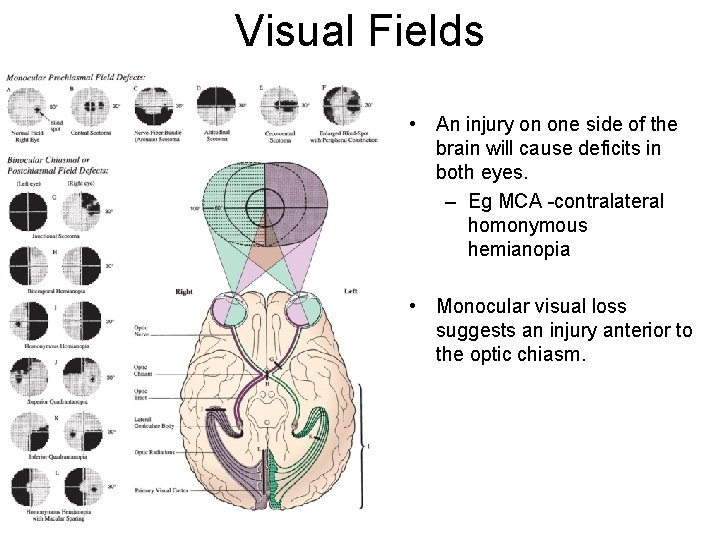
Visual Fields • An injury on one side of the brain will cause deficits in both eyes. – Eg MCA -contralateral homonymous hemianopia • Monocular visual loss suggests an injury anterior to the optic chiasm.
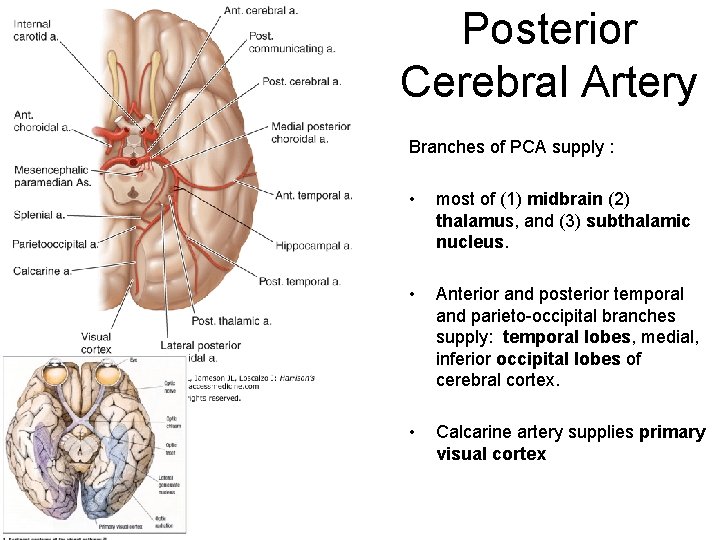
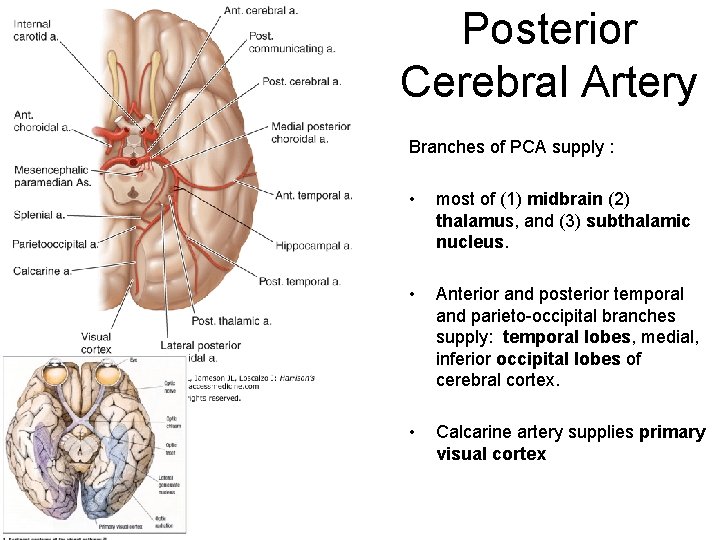
Posterior Cerebral Artery Branches of PCA supply : • most of (1) midbrain (2) thalamus, and (3) subthalamic nucleus. • Anterior and posterior temporal and parieto-occipital branches supply: temporal lobes, medial, inferior occipital lobes of cerebral cortex. • Calcarine artery supplies primary visual cortex
Posterior Cerebral Artery Stroke Symptoms Mostly eye symptoms: • sudden onset of bilateral signs, including ptosis, pupillary asymmetry or lack of reaction to light, and somnolence. • Visual field loss • Visual agnosia • Prosopagnosia- inability to recognize faces • Palinopsia (afterimage), micropsia (objects seem smaller), and macropsia (objects seem bigger • Disorders of reading (Alexia without Agraphia) • Disorders of color vision • Memory impairment • Motor dysfunction especially hemiballisumus • Paramedian thalamic infarction
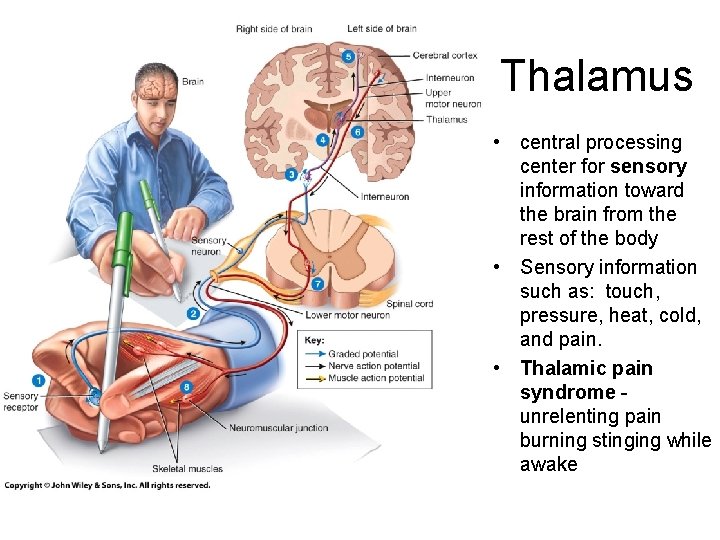
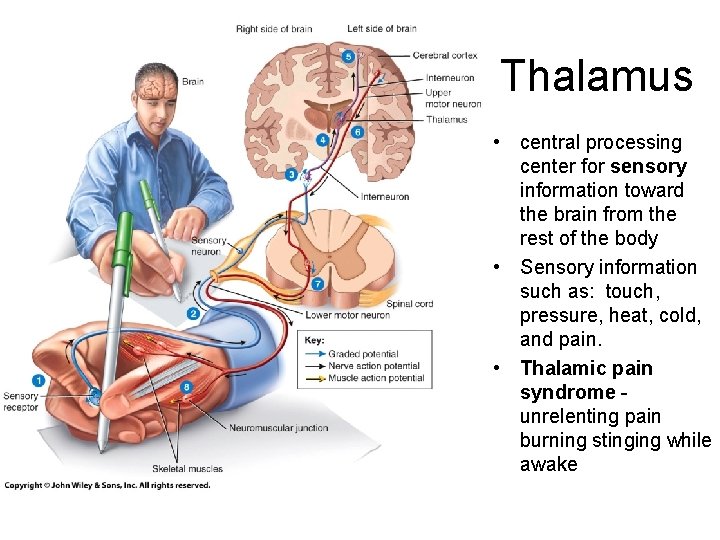
Thalamus • central processing center for sensory information toward the brain from the rest of the body • Sensory information such as: touch, pressure, heat, cold, and pain. • Thalamic pain syndrome unrelenting pain burning stinging while awake
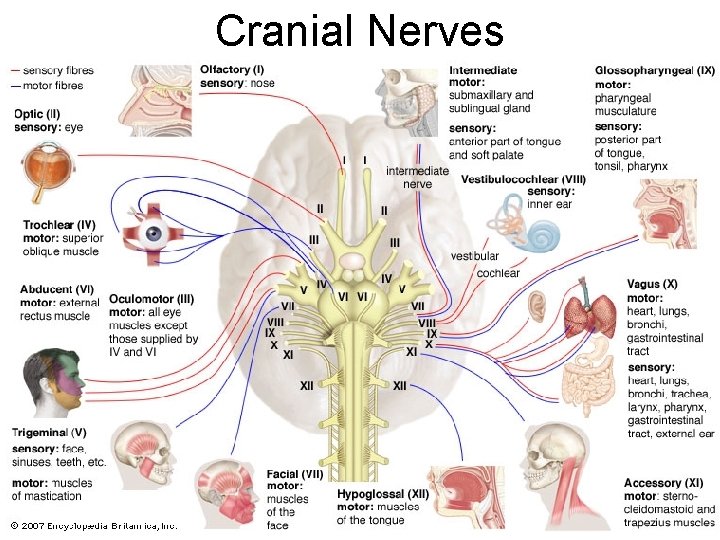
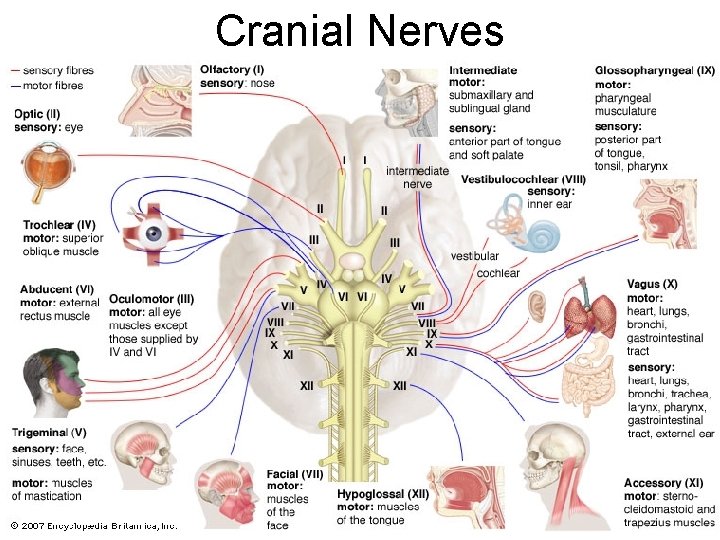
Cranial Nerves
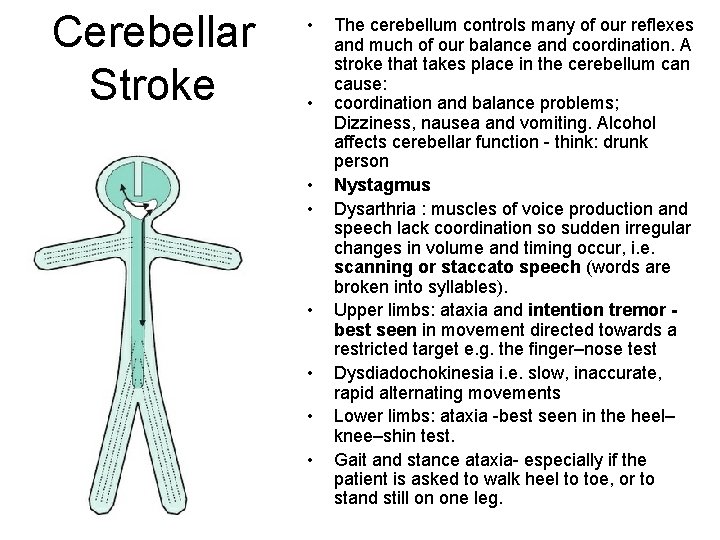
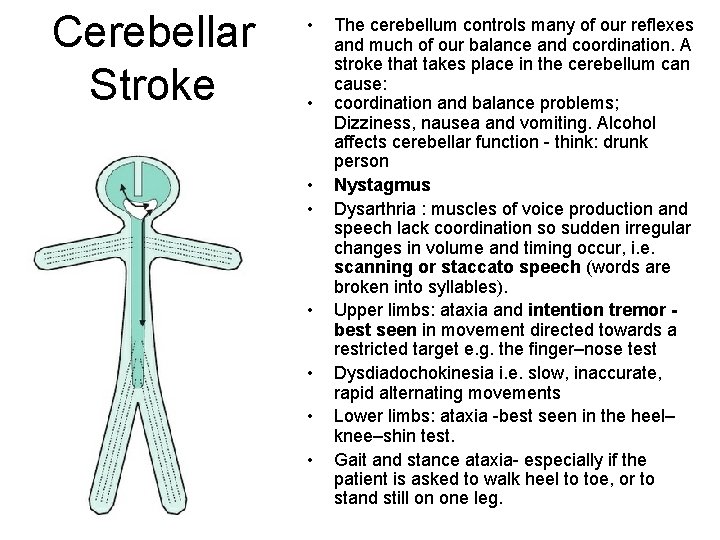
Cerebellar Stroke • • The cerebellum controls many of our reflexes and much of our balance and coordination. A stroke that takes place in the cerebellum can cause: coordination and balance problems; Dizziness, nausea and vomiting. Alcohol affects cerebellar function - think: drunk person Nystagmus Dysarthria : muscles of voice production and speech lack coordination so sudden irregular changes in volume and timing occur, i. e. scanning or staccato speech (words are broken into syllables). Upper limbs: ataxia and intention tremor best seen in movement directed towards a restricted target e. g. the finger–nose test Dysdiadochokinesia i. e. slow, inaccurate, rapid alternating movements Lower limbs: ataxia -best seen in the heel– knee–shin test. Gait and stance ataxia- especially if the patient is asked to walk heel to toe, or to stand still on one leg.
Brain Stem Stroke • • vertebrobasilar territory Strokes here are especially devastating - controls all our involuntary, "lifesupport" functions, eg breathing rate, blood pressure, heartbeat. also controls eye movements, hearing, speech and swallowing. Since impulses generated in the brain's hemispheres must travel through the brain stem on their way to arms and legs, patients with a brain stem stroke may also develop paralysis in one or both sides of the body. cranial nerves – Diplopia, gaze palsies, nystagmus, vertigo, dysarthria and dysphagia (sometimes hemispheric if patient hemiplegic) , other cranial nerve palsies (III -XII)
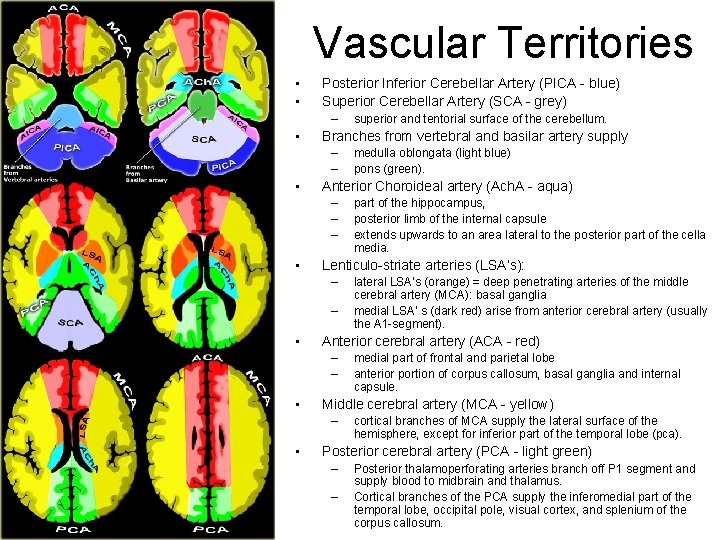
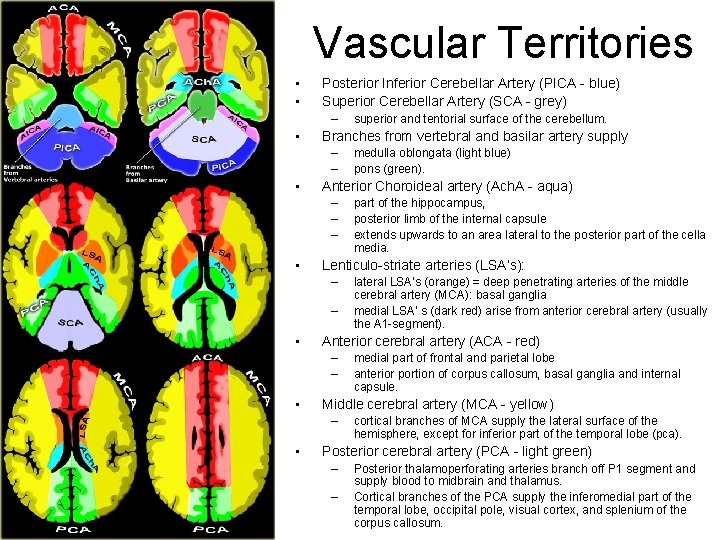
Vascular Territories • • Posterior Inferior Cerebellar Artery (PICA - blue) Superior Cerebellar Artery (SCA - grey) – • Branches from vertebral and basilar artery supply – – • – medial part of frontal and parietal lobe anterior portion of corpus callosum, basal ganglia and internal capsule. Middle cerebral artery (MCA - yellow) – • lateral LSA’s (orange) = deep penetrating arteries of the middle cerebral artery (MCA): basal ganglia medial LSA' s (dark red) arise from anterior cerebral artery (usually the A 1 -segment). Anterior cerebral artery (ACA - red) – – • part of the hippocampus, posterior limb of the internal capsule extends upwards to an area lateral to the posterior part of the cella media. Lenticulo-striate arteries (LSA’s): – • medulla oblongata (light blue) pons (green). Anterior Choroideal artery (Ach. A - aqua) – – – • superior and tentorial surface of the cerebellum. cortical branches of MCA supply the lateral surface of the hemisphere, except for inferior part of the temporal lobe (pca). Posterior cerebral artery (PCA - light green) – – Posterior thalamoperforating arteries branch off P 1 segment and supply blood to midbrain and thalamus. Cortical branches of the PCA supply the inferomedial part of the temporal lobe, occipital pole, visual cortex, and splenium of the corpus callosum.
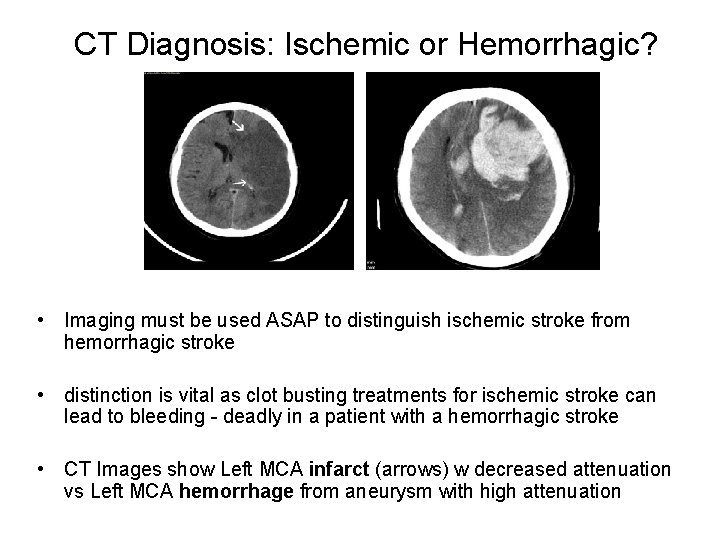
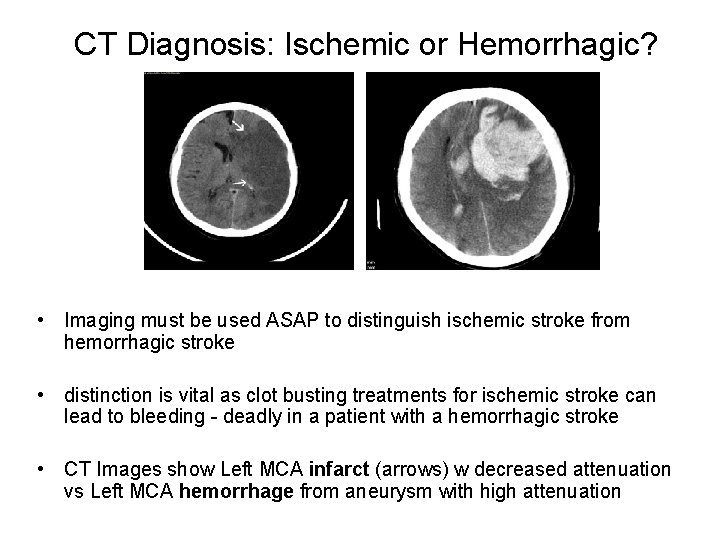
CT Diagnosis: Ischemic or Hemorrhagic? • Imaging must be used ASAP to distinguish ischemic stroke from hemorrhagic stroke • distinction is vital as clot busting treatments for ischemic stroke can lead to bleeding - deadly in a patient with a hemorrhagic stroke • CT Images show Left MCA infarct (arrows) w decreased attenuation vs Left MCA hemorrhage from aneurysm with high attenuation
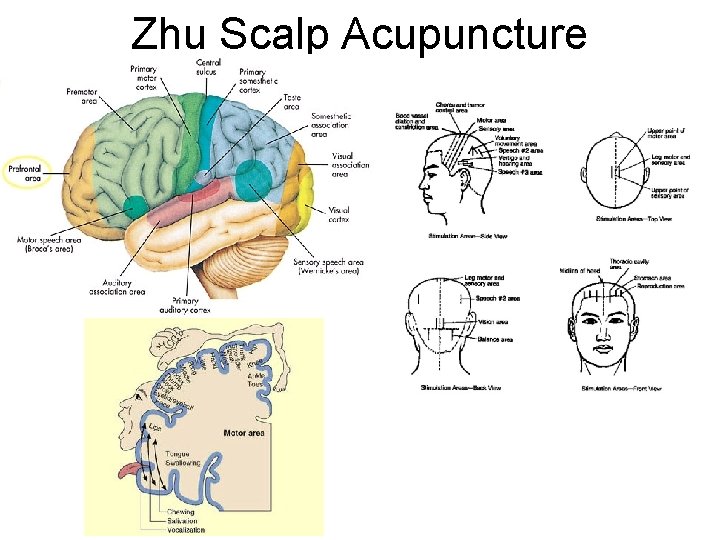
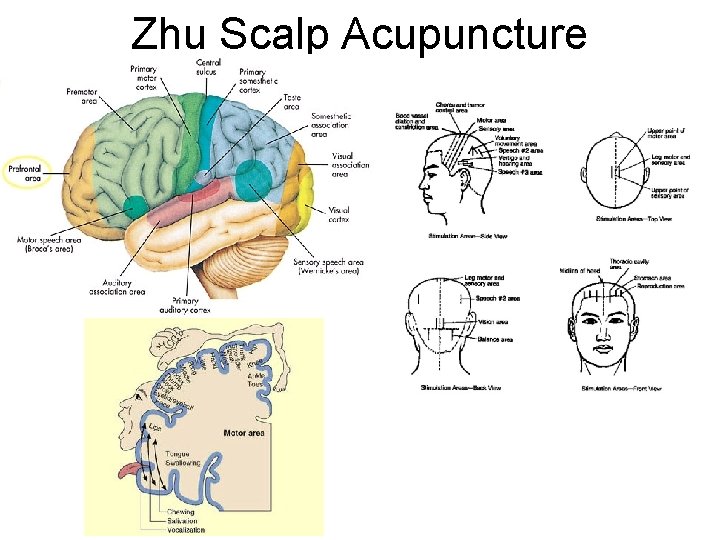
Zhu Scalp Acupuncture
TREATMENT • Once the site of blockage within the artery is located, several strategies can be employed to restore blood flow to the blocked vessel • Strategies include – – snaring the clot and pulling it out of the body removing the clot by suction stenting an artery open breaking down the clot with t. PA delivered directly to the clot – Carotid endarterectomy – Using one or more of these strategies, in the majority of cases, it is possible to restore blood flow and limit brain damage.
Treatment of ischemic stroke • intravenous “clot busting” drug TPA to restore blood flow. Patients failing to improve after this treatment or patients not able to safely receive the drug are considered for an emergent angiogram procedure. • • • Time Elapsed Since Patient Last Seen Normal: 0 -3 (or 0 -4. 5) Hours : intravenous t-PA 0 -6 Hours : intra-arterial t-PA* 0 -8 Hours : Mechanical Embolectomy t-PA= tissue plasminogen activator
Charts & Graphs Online • Brain Structure & Functions: http: //www. waiting. com/brainfunction. html • Brain functions & deficits http: //www. neuroskills. com/brain-injury/brainfunction. php • • Arteries of the Brain & area supplied: http: //what-when-how. com/neuroscience/blood-supply-of-the-centralnervous-system-gross-anatomy-of-the-brain-part-2/ • Aphasia and Apraxia at a Glance http: //www. csuchico. edu/~pmccaffrey/CMSD 636 Study. Guide. pdf
Select glossary • • • adiadochokinesia (syn: dysdiadocchokinesia) - Inability to perform rapidly alternating movements, that is to stop a movement and follow it with another in an opposite direction. agnosia -a loss of ability to recognize objects, people, sounds, shapes, or smells; that is, the inability to attach appropriate meaning to objective sense-data. It usually is used when the primary sense organ involved is not impaired. agraphia - Inability to express thought in written language (usually not due to mechanical disfunction akinesia (syn: dyskinesia) - Unresponsiveness, with extreme reluctance to perform elementary motor activities. A form of apraxia. alalia - Loss of ability to speak. alexia - Loss of the ability to understand written language, i. e. , to read. A subform of dyslexia. amnesia (syn: dysmnesia) - Total or partial loss of memory. aphasia (syn: dysphasis) - This is the general term that literally means "no speech. " It refers to any impairment of the ability to use and/or understand words and can be used to describe loss of one or more of the following abilities: ability to speak; ability to write; understand speech; understand written words. Major subcategories include: Broca's aphasia, in which one can comprehend speech, but not produce it; and, Wernicke's aphasia in which one can produce speech but not comprehend speech. aphonia (dysphonia) - Loss of ability to speak; inability to produce speech sounds. Distinguished from the motor defect called dysarthria, which is imperfect articulation of speech due to disturbances of muscular control. apraxia (syn: dyspraxia)- Difficulty in performing a learned movement or coordinated motor activity even though understanding, motor function coordination, and sensation are intact. Specific apraxias may be limited to a certain group of functions, such as inability to construct a simple structure from blocks, or inability to dress oneself. Related to akinesia. aprosodia (syn: amelodia)- Absence of normal variations of pitch, rhythm and stress in speech. . ataxia - Poor coordination and unsteadiness due to failure to regulate the body's posture, and strength and direction of limb movements. Often a consequence of a disorder in the cerebellum.