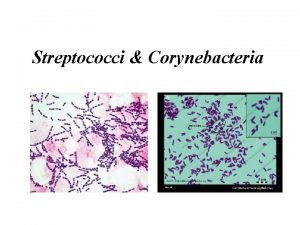
STREPTOCOCCI Streptococci Family Streptococcaceae Streptos means twisted and






























- Slides: 72

STREPTOCOCCI
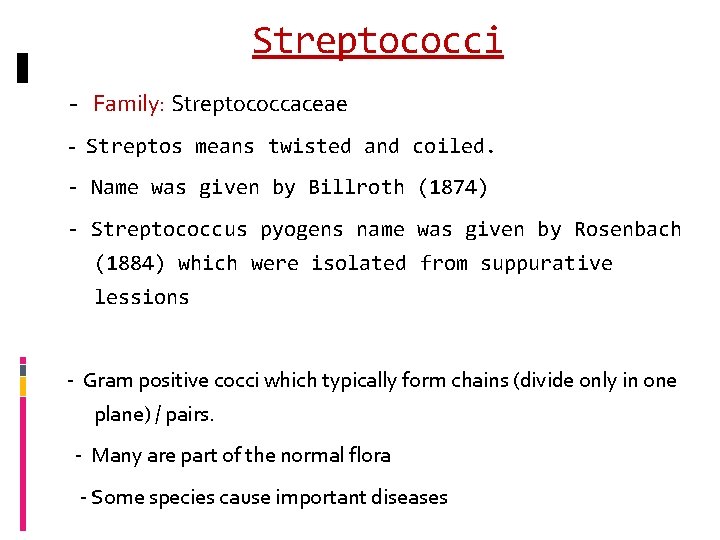
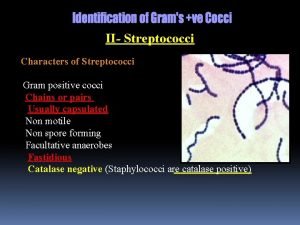
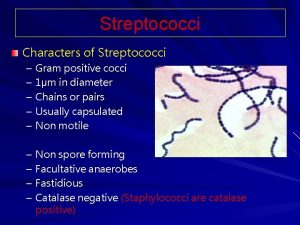
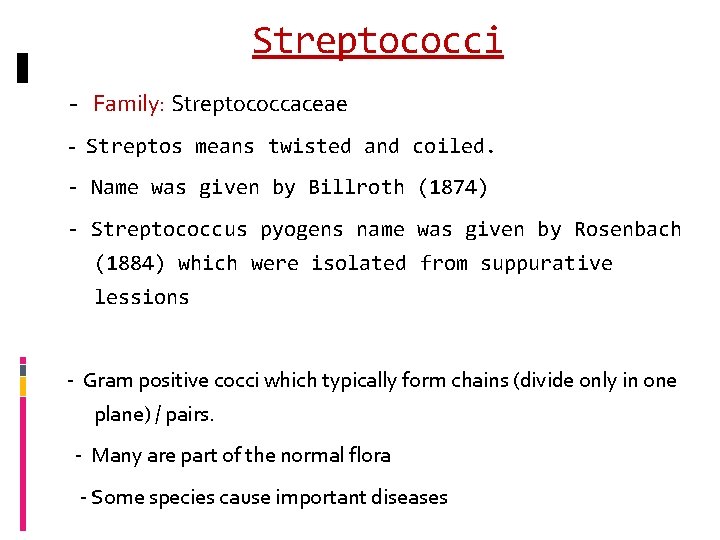
Streptococci - Family: Streptococcaceae - Streptos means twisted and coiled. - Name was given by Billroth (1874) - Streptococcus pyogens name was given by Rosenbach (1884) which were isolated from suppurative lessions - Gram positive cocci which typically form chains (divide only in one plane) / pairs. - Many are part of the normal flora - Some species cause important diseases

Classification is based on multiple criteria 1. Their Oxygen requirement 2. Hemolytic pattern on Sheep blood agar 3. Antigenic characteristics 4. Biochemical properties

Streptococci O 2 requirement Aerobes, Obligate anaerobes Facultative anaerobes 1. Alpha hemolytic Partial hemolysis (Greenish discoloration) Eg: Viridans Streptococci, Eg: Peptostreptococcus 2. Beta hemolytic Complete hemolysis (Clear zone) 3. Non hemolytic Eg: Enterococcus
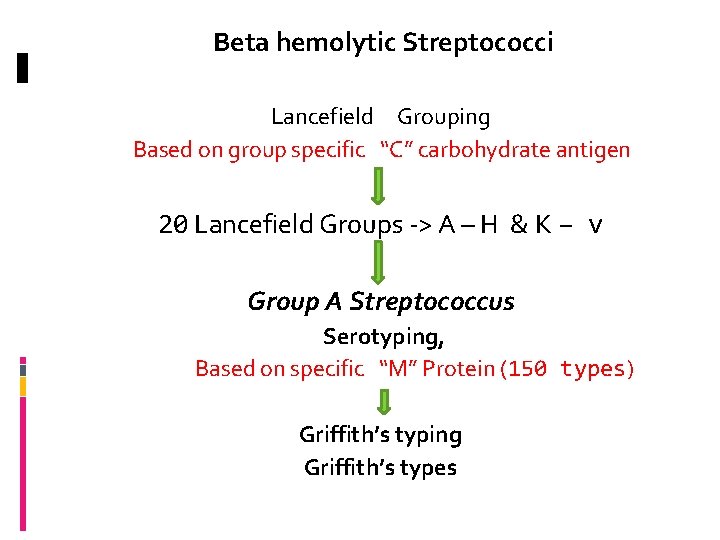
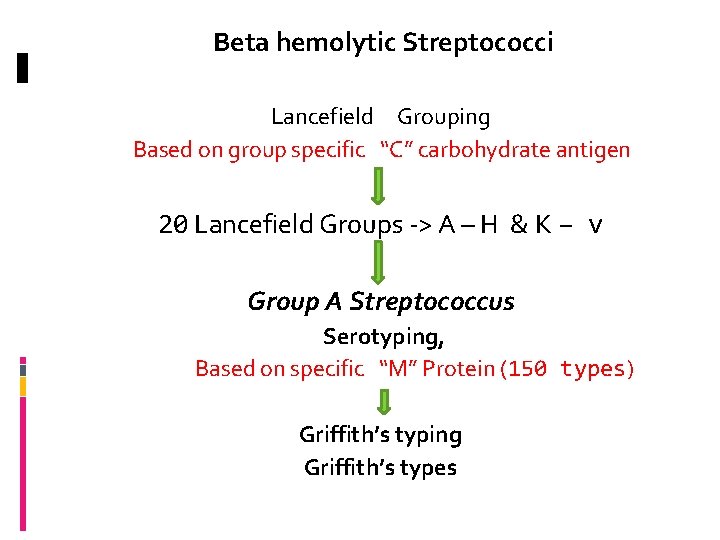
Beta hemolytic Streptococci Lancefield Grouping Based on group specific “C” carbohydrate antigen 20 Lancefield Groups -> A – H & K – v Group A Streptococcus Serotyping, Based on specific “M” Protein (150 types) Griffith’s typing Griffith’s types

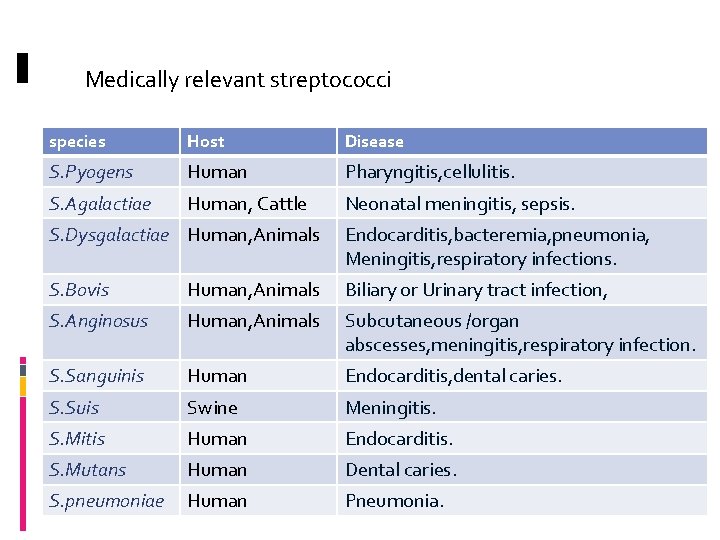
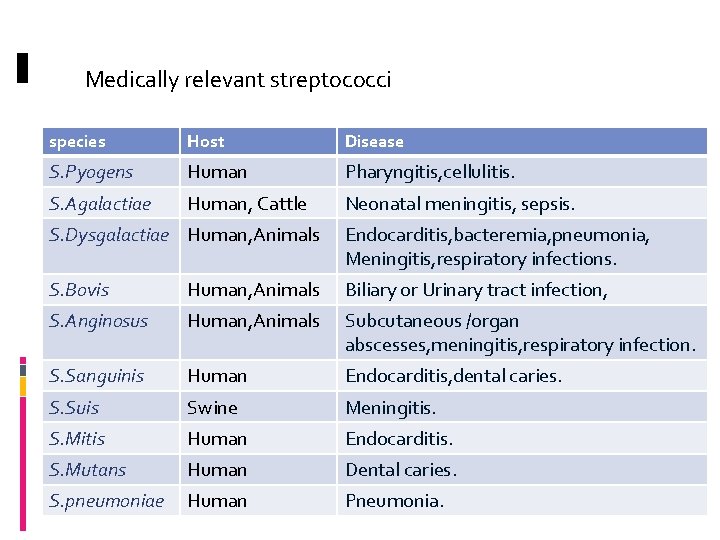
Medically relevant streptococci species Host Disease S. Pyogens Human Pharyngitis, cellulitis. S. Agalactiae Human, Cattle Neonatal meningitis, sepsis. S. Dysgalactiae Human, Animals Endocarditis, bacteremia, pneumonia, Meningitis, respiratory infections. S. Bovis Human, Animals Biliary or Urinary tract infection, S. Anginosus Human, Animals Subcutaneous /organ abscesses, meningitis, respiratory infection. S. Sanguinis Human Endocarditis, dental caries. S. Suis Swine Meningitis. S. Mitis Human Endocarditis. S. Mutans Human Dental caries. S. pneumoniae Human Pneumonia.
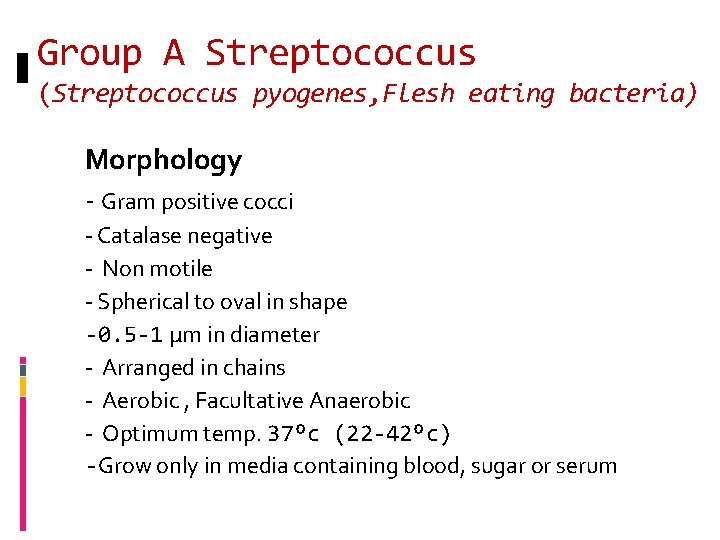
Group A Streptococcus (Streptococcus pyogenes, Flesh eating bacteria) Morphology - Gram positive cocci - Catalase negative - Non motile - Spherical to oval in shape -0. 5 -1 µm in diameter - Arranged in chains - Aerobic , Facultative Anaerobic - Optimum temp. 37⁰c (22 -42⁰c) -Grow only in media containing blood, sugar or serum
Bacterial virulence factors: Virulence factors of Streptococcus pyogenes may be divided into two categories – - Cellular virulence factors - Extracellular virulence factors
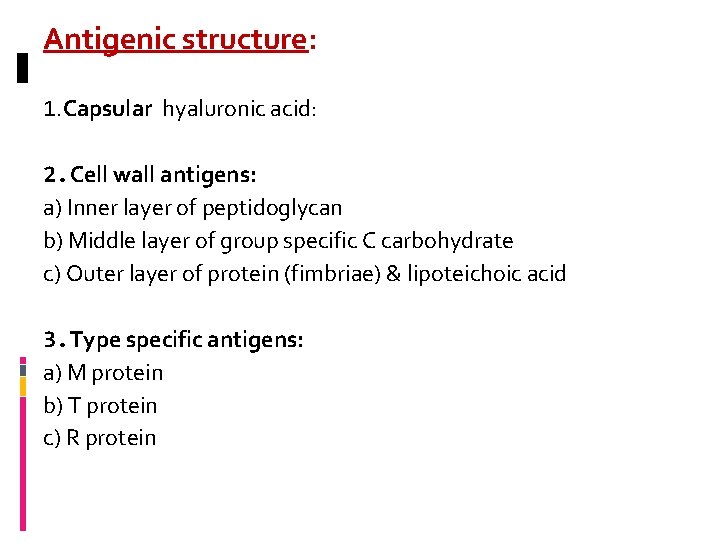
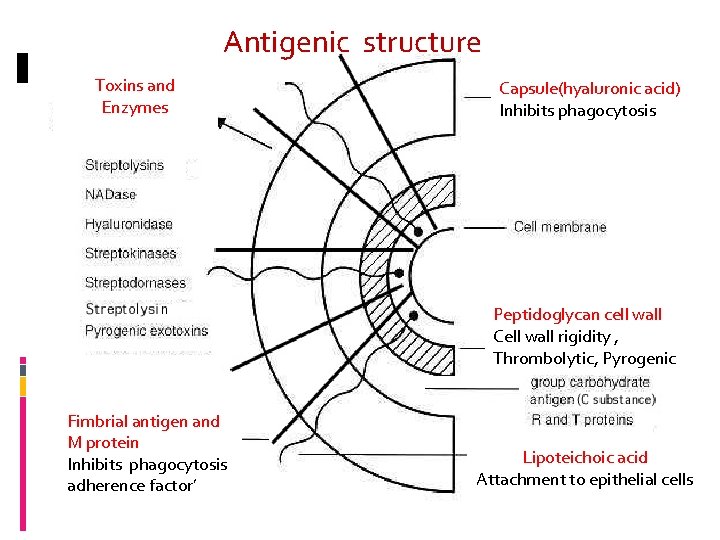
Antigenic structure: 1. Capsular hyaluronic acid: 2. Cell wall antigens: a) Inner layer of peptidoglycan b) Middle layer of group specific C carbohydrate c) Outer layer of protein (fimbriae) & lipoteichoic acid 3. Type specific antigens: a) M protein b) T protein c) R protein
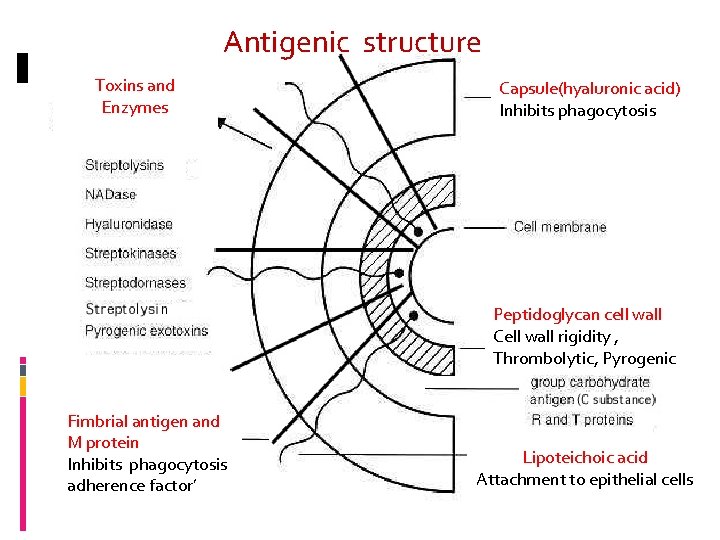
Antigenic structure Toxins and Enzymes Capsule(hyaluronic acid) Inhibits phagocytosis Peptidoglycan cell wall Cell wall rigidity , Thrombolytic, Pyrogenic Fimbrial antigen and M protein Inhibits phagocytosis adherence factor’ Lipoteichoic acid Attachment to epithelial cells

Cross reacting Antigens Various streptococcal Ags have similarity to different host tissues Capsular hyaluronic acid <–> human synovial fluid Cell wall M protein <–> myocardium Cytoplasmic membrane antigen <–> vascular intima These antigenic cross reactions may be responsible for the non-suppurative complications of group A Streptococcal infections.
Extracellular Virulence Factors Toxins Pyrogenic exotoxins (erythrogenic toxins) A, B, C -> Highly antigenic ü Pyrogenic – induce fever ü Responsible for skin rashes in scarlet fever ü Superantigens, responsible for streptococcal SSS ü Have ability to alter lymphocytic activity

2. Streptolysins ü Hemolysins of Group A streptococcus ü Two types – Streptolysin ‘O’ - Streptolysin ‘S’
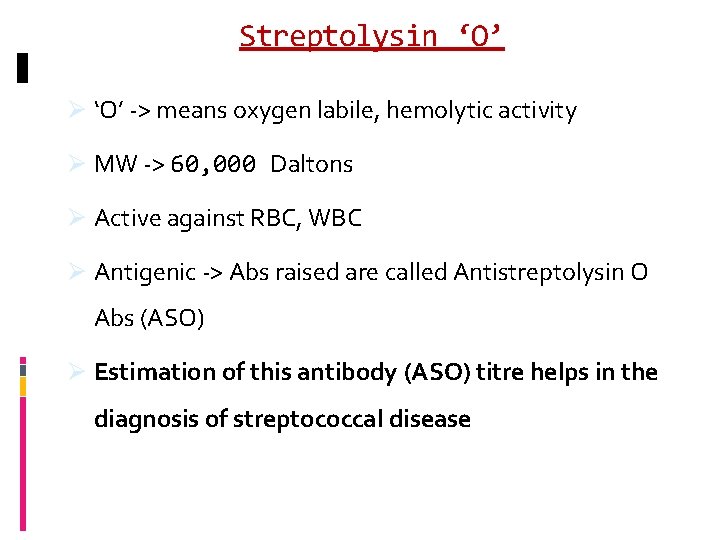
Streptolysin ‘O’ Ø ‘O’ -> means oxygen labile, hemolytic activity Ø MW -> 60, 000 Daltons Ø Active against RBC, WBC Ø Antigenic -> Abs raised are called Antistreptolysin O Abs (ASO) Ø Estimation of this antibody (ASO) titre helps in the diagnosis of streptococcal disease
Streptolysin ‘S’ Ø It is oxygen stable Ø Active against RBC, WBC, Platelets Ø Responsible for the Beta hemolysis seen around the colonies on the surface of blood agar Ø Has nephrotoxic activity

B. Enzymes of Str. pyogenes Streptokinase ü Can digest fibrin clots ( plaminogen in to plasmin) ü Helps in Streptococcal infections by breaking down the fibrin barrier around the lesions and facilitating the spread of infection. ü Practical use – given IV for treatment of pulmonary emboli; coronary artery/venous thromboses

Streptodornase (Streptococcal DNAse) Released by dead host cells. Responsible for the decrease in viscosity of purulent pus. Responsible for the serous nature of exudate in streptococcal infection. Help in spread of lesion. Mixture of streptokinase/streptodornase Practical use: in enzymatic debridement of necrotized tissues & empyemas. – facilitates early recovery of infected tissue

Hyaluronidase -> Spreading factor’ Ø Degrades hyaluronic acid , – it facilitates the rapid spread of Str. pyogenes in skin infection
Streptococcus pyogenes infections Pathogenesis Source: a) Patients with skin lesions; respiratory secretions of sore throat cases b) Carriers Mode of infection: Ø Direct/Indirect contact or inhalation
Diseases: attributable to streptococcus group A Diseases caused by S. pyogens is studied under 2 groups 1. Suppurative infections 2. Non suppurative complications

Suppurative infections: Pyogenic infections. Spreads locally, along lymphatics and through the blood stream. A) Respiratory infections - Tonsillitis - Pharyngitis - Otitis media -Mastoiditis -Quinsy - Ludwig’s angina - Rarely it may cause pneumonia & meningitis - Scarlet fever (sore throat & skin rash)

Tonsillitis Otitis media Pharyngitis Mastoiditis

Quinsy Skin rashes in Scarlet fever Ludwig’s angina

B) Skin infections: - Infection of wounds & burns - Impetigo - Erysipelas C) Soft tissue infections: - Cellulitis - Necrotising fasciitis
Soft tissue infections with some M types of strains may sometime cause toxic shock syndrome resembling staphylococcal TSS. D) Genital Infections: -Puerperal sepsis E) Other suppurative infections: - Pyemia - Septicemia - Abscesses in internal organs such as brain, lungs, liver and kidney.
2. Non suppurative complications: It is also called as post streptococcal complications Non suppurative complications of S. pyogens occur 1 -4 weeks after the acute infection. The organism may not be detectable when these complications set in.
These complications are believed to be the result of hypersensitivity to some streptococcal components. The complications are- 1. Acute rheumatic fever 2. Acute glomerulonephritis
Acute rheumatic fever: It occurs after (1 -4 weeks ) repeated sore throat caused by S. pyogens. Mechanism of pathogenesis: Primary infection antibodies produced against some streptococcal antigen. Similarity with cardiac tissue antigen Antibodies will cross react with cardiac tissue antigen causing destruction. Leads to clinical symptoms such as Aschoff’s nodules, carditis, fever and malaise.
Acute glomerulonephritis: It follows about 3 weeks after skin infection caused by S. pyogens nephritogenic types. (M types 49, 55, 59, 61) Mechanism of pathogenesis: Antibodies will be produced against cell membrane antigen. These antibodies cross react with glomerular basement membrane antigen causing Complement mediated damage. Leads clinical symptoms such as proteinuria, haematuria & hypertension.

Comparison of Acute Rheumatic Fever and Acute Glomerulonephritis Features ARF AGN 1 o site of infection Throat Skin or throat Prior sensitization Essential Not required Serotypes responsible Any Nephritogenic M types 49, 55, 59 – 61 Immune response Marked Moderate Complement level Unaffected Lowered Repeated attack Common Absent Course Progressive or static Spontaneous resolution Prognosis Variable Good Penicillin prophylaxis Essential Not indicated


Lab diagnosis Specimen – Collection depends on type of disease ü Throat swab, ü pus, ü exudates, fluids ü necrotic tissue –> for culture ü Serum -> for serology
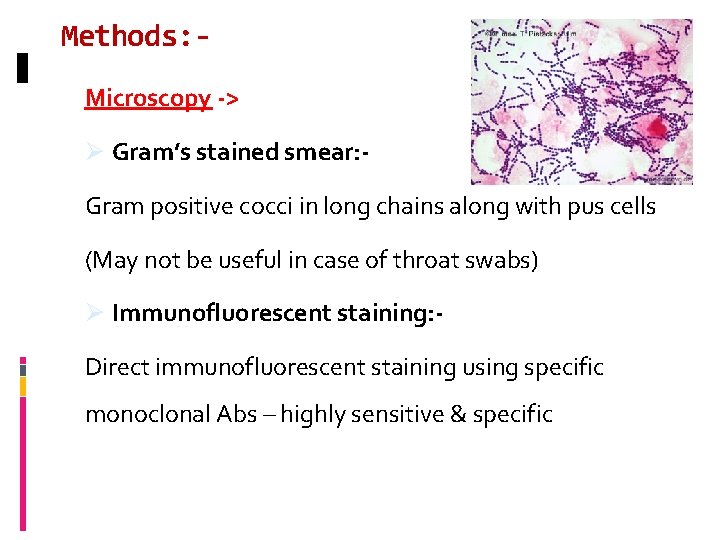
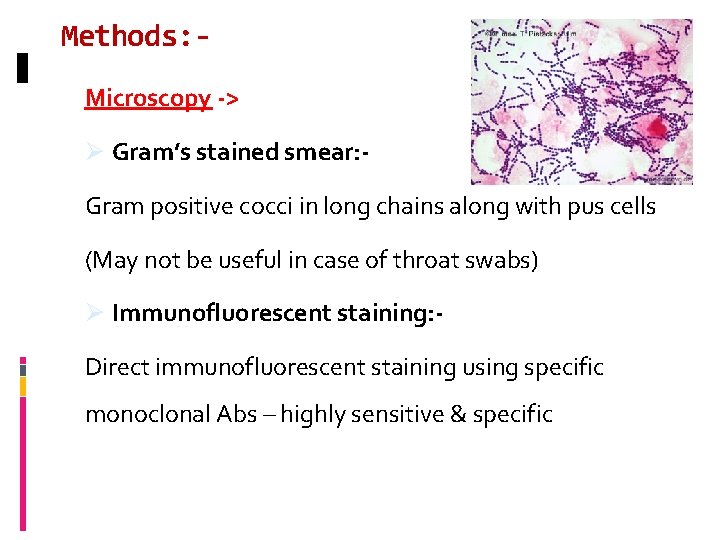
Methods: Microscopy -> Ø Gram’s stained smear: - Gram positive cocci in long chains along with pus cells (May not be useful in case of throat swabs) Ø Immunofluorescent staining: - Direct immunofluorescent staining using specific monoclonal Abs – highly sensitive & specific

Culture -> ü Specimen should be immediately processed ü Transport media – Pike’s / Stuart’s media used if delay in processing ü Routine media used – Sheep Blood agar; Thioglycollate medium ü Incubated for 24 -48 hrs at 37 o C in 5 -10% CO 2

Identification of Isolate -> ü Beta hemolytic colonies ü Gram positive cocci in chains ü Catalase test negative ü Isolate is susceptible to bacitracin ü Grouping (Lancefield) is done by Co-agglutination test to detect ‘Group A Streptococci’
Serology Rise in titre of Abs to many Group A Streptococcal Ags may be demonstrated. 1. Antistreptolysin O (ASO) test: Ø A serological test used to detect ASO Abs present in patient’s serum Ø A passive latex agglutination test Ø ASO titre of more than 200 units is indicative of recent streptococcal infection
Ø May also indicate an exaggerated immune response to an earlier exposure (ARF) Ø Useful in the diagnosis of ARF but not in AGN as titre is low (usually occurs as a result of skin infection and being oxygen labile toxin, Ab will not be produced in high titre)
Other serological tests - 2. Antistreptodornase (Anti. DNAse) test 3. Antihyaluronidase test 4. Antistreptokinase test

Treatment ü Penicillin G is the drug of choice. ü Patients allergic to penicillin: erythromycin / cephalexin may be used. ü All acute infections should be treated, as antimicrobials have no effect on already established ARF & AGN ü Long term Penicillin therapy for ARF patients to prevent recurrence of infection

THANKS
GROUP B STREPTOCOCCUS (STREPTOCOCCUS AGALACTIAE)
Streptococcus agalactiae It is part of the normal flora of the female genital tract (5 – 20% of women) Human pathogenecity Neonatal infections Infections in adults

Neonatal infections A. Early onset disease ü Seen at birth or within 7 days of birth ü Source of infection mothers birth canal ü Predisposing factors Prolonged labor PROM Premature child Low birth weight ü Manifestations Septicemia, meningitis, pneumonia

B. Late onset disease ü Occurs after first week of life ü Source hospital staff, environment. ü Manifestation o Sepsis with /without meningitis o Respiratory tract infection

Adult infections 1. In women Ø Abortion Ø Chorioamnionitis Ø Post partum sepsis 2. In debilitated individuals Ø Septicemia Ø Meningitis Ø Endocarditis
Lab diagnosis 1. Specimen -> CSF, Blood, Exudates 2. Cultured onto -> Sheep Blood Agar 3. Incubated at -> 37 o C for up to 48 hrs 4. Isolate identified by -> a) Beta hemolysis on blood agar b) Gram stained smear – Gram positive cocci in chains c) Ability to hydrolyze Hippurate d) CAMP test: positive
Christie Atkins Munch Petersen Test (CAMP Test) Test used to identify Group B Streptococci Principle Enhancement of β hemolysis of S. aureus by a soluble protein (CAMP factor) produced by Strep. Agalactiae Observation Arrow head hemolysis is seen in-between the two streaks of growth

S. Agalactiae Group B Enhancement of β hemolysis S. aureus S. Pyogens Group A

Treatment Penicillin is the drug of choice
GROUP D STREPTOCOCCUS (ENTEROCOCCI / NON-ENTEROCOCCI)
Enterococci previously classified under group D. Contain Group ‘D’ Ag. In 1984 enterococcus was reclassified to a separate genus. Entererococci are a part of normal intestinal flora of humans and animals. Enterococci poses a major therapeutic challenges.

Presently there are 16 species in the genus. Enterococcus faecalis and Enterococcus faecium is most often enterococcus isolated from human sources. o other species include: - observed occasionally ü Enterococcus durans ü Enterococcus avium ü Enterococcus casseliflavis ü Enterococcus gallinarum ü Enterococcus raffinosus
Biochemical characteristics: Facultative anaerobic ü Ability to survive in 40% bile ü Grow in medium with 6. 5% Na. Cl ü Bile-Esculin hydrolysis test – Positive ü Heat resistant (tolerate heat of 60 o. C for 30 min) ü May be non-hemolytic or alpha hemolytic
Pathogenesis and clinical disease Enterococci are commensal organisms. Not having potent toxin or well defined virulance factors. Greatest significance is in their resistance to many commonly used antibiotics (oxacillin, cephalosporins) or acquisition of resistant genes (aminoglycoside, vancomycin).
Source & mode of infection: 1. Endogenous-from colonized site. 2. Exogenous-through direct or indirect contact.
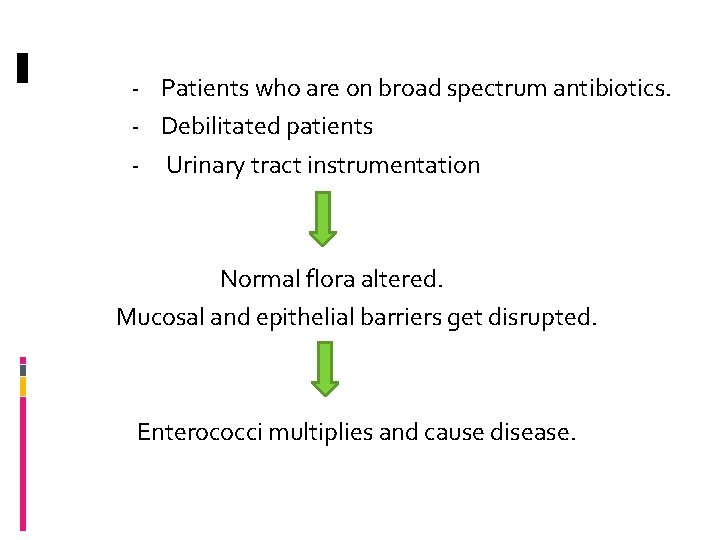
- Patients who are on broad spectrum antibiotics. - Debilitated patients - Urinary tract instrumentation Normal flora altered. Mucosal and epithelial barriers get disrupted. Enterococci multiplies and cause disease.

Frequent cause of nosocomial infection and may cause - Urinary tract infection. - Nosocomial Bacteremia. - Wound infection. - Intra-abdominal abscess. - Sub-acute bacterial endocarditis 10 -20 % of bacterial endocarditis on both native valve and prosthetic valves. - Enterococci meningitis in some underlying disease.
2. Nonenterococci (Group D Streptococci) -> o Contain Group ‘D’ Ag Important species: ü Streptococcus bovis ü Streptococcus equinus May be non-hemolytic or alpha hemolytic o Streptococcus bovis -> has been isolated from blood (septicemia) in patients with colon carcinoma.
Lab diagnosis Specimens –> Urine, pus, blood Microscopy -> Gram stain: Gram positive oval cocci arranged in pairs at an angle to each other Culture –> Ø Blood agar - non-hemolytic / α hemolytic Ø Mac. Conkey’s agar - magenta pink coloured colonies


Ø Growth on Bile Esculin agar – Positive

Drug resistance in vancomycin Isolation of enterococci resistant to multiple antibiotics has increasingly common in hospital setting. Clonal spread is the dominant factor in the dissemination of multi drug resistant enterococci. Enterococci have both an intrinsic and acquired resistance to antibiotics
Mechanism Beta lactam antibiotics : lactams. PBPs with low binding affinity for ẞ Trimethoprim / Sulfamethoxazole : inhibition of folate synthesis. Intrinsically resistant to: Pencillinase resistant pencillins, Cphalosporins, Nalidixic acid, Aztreonam, Macrolides, and low levels of clindamycin and amino glycosides.
Acquired resistance Includes resistance to penicillin by Beta lactamases, chlorophenicol, tetracyclines, rifampin, fluoroquinolones, aminoglycosides and vancomycin. Resistance to glycopeptides is mediated by vancomycin resistance Van operon. Carried chromosomally or extra chromosomally on a plasmid
Van operon consists of Van. S –Van R, in which 9 variant genes have been identified Van A, van B , van C, van D , van E, van G , van L, van M , van N Genes responsible for intrinsic or acquired vancomycin resistance results in peptide to which vancomycin cannot bind. TREATMENT OF VRE Combining various beta lactam antibiotics with Daptomycin may result in synergy.
THE VIRIDANS STREPTOCOCCI
The Viridans Streptococci Viridis (green) v A heterogeneous group of streptococci which cannot be grouped under Lancefield's classification. v Part of the normal flora of the oral cavity and upper respiratory tract. v Mostly alpha hemolytic (greenish color ‘viridans’). v Insoluble in bile v Resistant to ‘Optochin’
v Important species ü Streptococcus mitis ü Streptococcus mutans ü Streptococcus sanguis ü Streptococcus salivarius
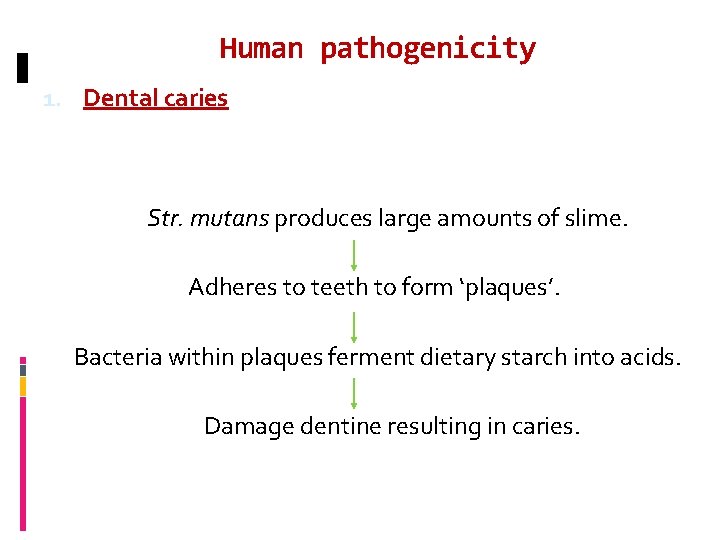
Human pathogenicity 1. Dental caries Str. mutans produces large amounts of slime. Adheres to teeth to form ‘plaques’. Bacteria within plaques ferment dietary starch into acids. Damage dentine resulting in caries.
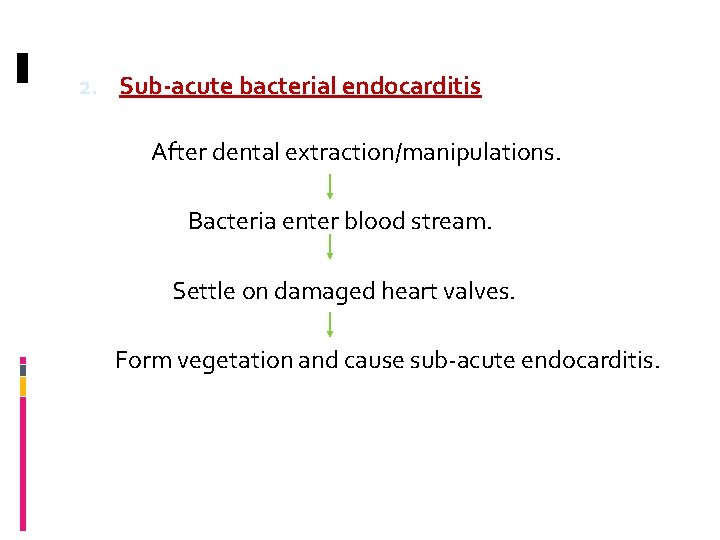
2. Sub-acute bacterial endocarditis After dental extraction/manipulations. Bacteria enter blood stream. Settle on damaged heart valves. Form vegetation and cause sub-acute endocarditis.
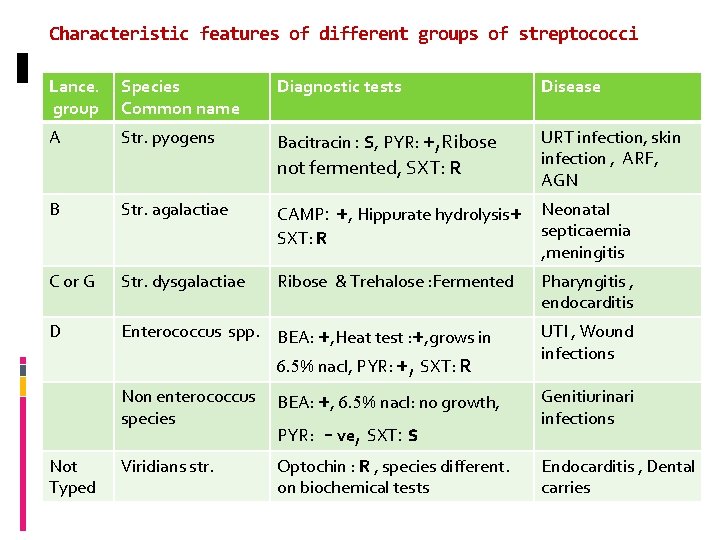
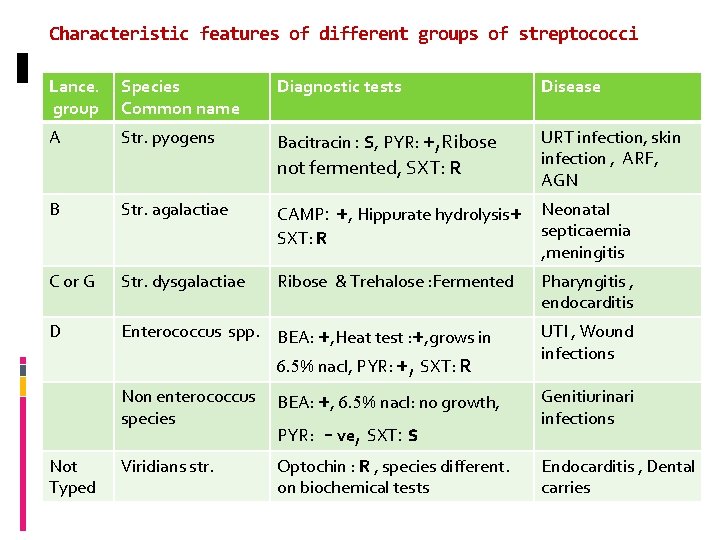
Characteristic features of different groups of streptococci Lance. group Species Common name Diagnostic tests Disease A Str. pyogens Bacitracin : S, PYR: +, Ribose not fermented, SXT: R URT infection, skin infection , ARF, AGN B Str. agalactiae CAMP: +, Hippurate hydrolysis+ SXT: R Neonatal septicaemia , meningitis C or G Str. dysgalactiae Ribose & Trehalose : Fermented Pharyngitis , endocarditis D Enterococcus spp. BEA: +, Heat test : +, grows in 6. 5% nacl, PYR: +, SXT: R Not Typed Non enterococcus species BEA: +, 6. 5% nacl: no growth, Viridians str. Optochin : R , species different. on biochemical tests PYR: - ve, SXT: s UTI , Wound infections Genitiurinari infections Endocarditis , Dental carries
 Eritrojenik toksin
Eritrojenik toksin Streptos
Streptos Streptococcacea
Streptococcacea Familia streptococcaceae
Familia streptococcaceae Disque optochine
Disque optochine Micrococcaceae e streptococcaceae
Micrococcaceae e streptococcaceae Lancefield classification of streptococci
Lancefield classification of streptococci Lancefield classification of streptococci
Lancefield classification of streptococci Lancefield grouping of streptococcus
Lancefield grouping of streptococcus Lancefield grouping of streptococcus
Lancefield grouping of streptococcus Viridans streptococci
Viridans streptococci The night of the scorpion
The night of the scorpion Twisted beta sheet
Twisted beta sheet Twisted shoulder joint
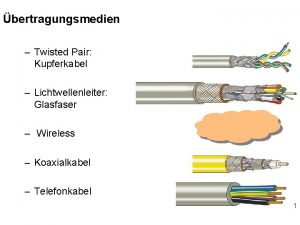
Twisted shoulder joint Schlitzkabel
Schlitzkabel A flag wags like a fishhook there in the sky
A flag wags like a fishhook there in the sky Thomas dark universe
Thomas dark universe Glasfaser koaxialkabel
Glasfaser koaxialkabel Genetics a twisted tale
Genetics a twisted tale Preparation of forcemeat
Preparation of forcemeat Twisted tetris
Twisted tetris Spiral wound heat exchanger
Spiral wound heat exchanger Composition of egg
Composition of egg 3 bit twisted ring counter
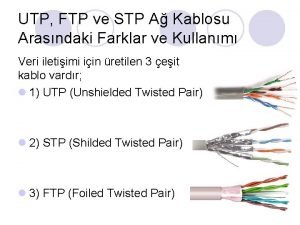
3 bit twisted ring counter Foiled twisted pair
Foiled twisted pair Twisted mp3
Twisted mp3 Twisted universe
Twisted universe Twisted pair cable application
Twisted pair cable application Twisted ankle
Twisted ankle Twisted laurie halse anderson summary
Twisted laurie halse anderson summary Gambar kabel twisted pair
Gambar kabel twisted pair Twisted greenlet
Twisted greenlet Themes in speak by laurie halse anderson
Themes in speak by laurie halse anderson Cosh-101
Cosh-101 G.hn over twisted pair
G.hn over twisted pair Coaxial cable twisted pair fiber optic
Coaxial cable twisted pair fiber optic Poly means many and gon means
Poly means many and gon means Meta and morph means
Meta and morph means Biodiversity and conservation
Biodiversity and conservation Meta means morphe means
Meta means morphe means Father and mother love
Father and mother love Life bio
Life bio Conjugal family
Conjugal family Carbon family
Carbon family Characteristics of single parent family
Characteristics of single parent family Family and morale welfare and recreation
Family and morale welfare and recreation Your favourite means of transport
Your favourite means of transport What means compare and contrast
What means compare and contrast Semasiology examples
Semasiology examples Syntactical expressive means
Syntactical expressive means Venn diagram of cardinal and cedar waxwing
Venn diagram of cardinal and cedar waxwing Expressive means and stylistic devices difference
Expressive means and stylistic devices difference Branches of stylistics
Branches of stylistics Bios logos meaning
Bios logos meaning What does this symbol mean
What does this symbol mean Means and extremes of proportions
Means and extremes of proportions Similarity and proportions
Similarity and proportions White suggests treachery suspiciousness and craftiness
White suggests treachery suspiciousness and craftiness Anthropos logos
Anthropos logos Principles of active supervision
Principles of active supervision Ratio theorem
Ratio theorem Service honor justice logo
Service honor justice logo The suffix in the terms comatose and grandiose means
The suffix in the terms comatose and grandiose means Means and extremes
Means and extremes Ap statistics rules for means and variances
Ap statistics rules for means and variances Rules for means and variances
Rules for means and variances Means and extremes
Means and extremes Refers to the loyalty and devotion to a nation
Refers to the loyalty and devotion to a nation Graphon stylistic device
Graphon stylistic device Means acquiring goods and or services
Means acquiring goods and or services Udl action and expression
Udl action and expression Four score and seven years ago
Four score and seven years ago Art appreciation description
Art appreciation description