STD 101 for Clinicians Sexually Transmitted Diseases Part

- Slides: 63
STD 101 for Clinicians Sexually Transmitted Diseases Part 2 Edward L. Goodman, MD February 9, 2004 1
STD 101 for Clinicians Background Information 2
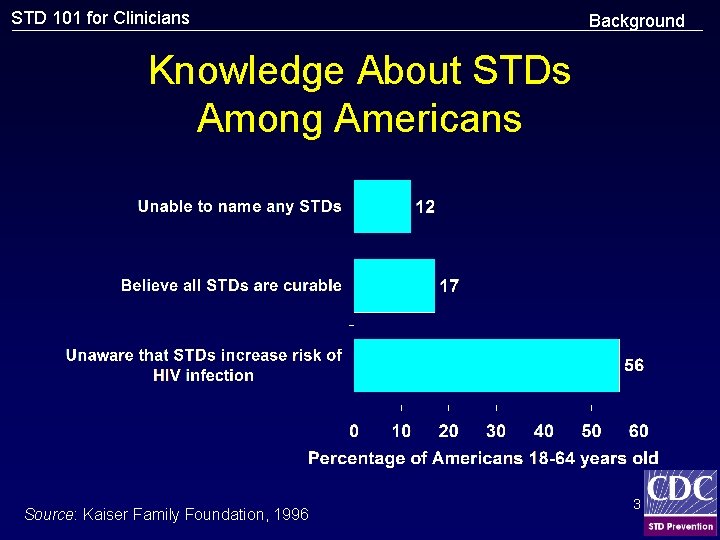
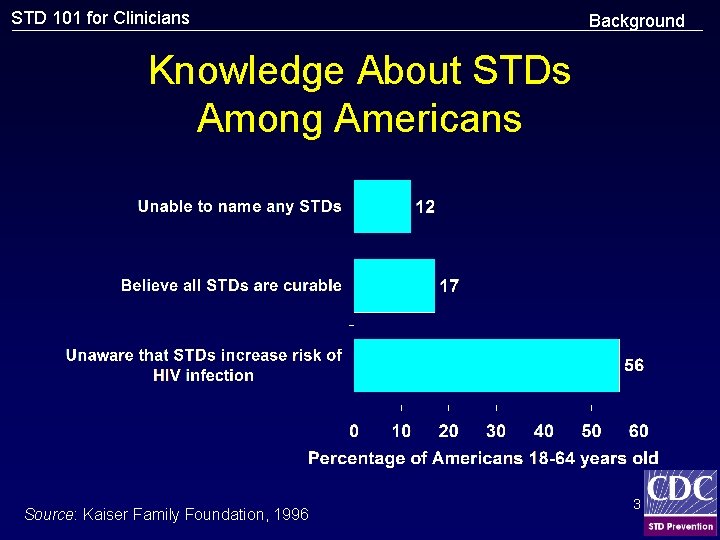
STD 101 for Clinicians Background Knowledge About STDs Among Americans Source: Kaiser Family Foundation, 1996 3
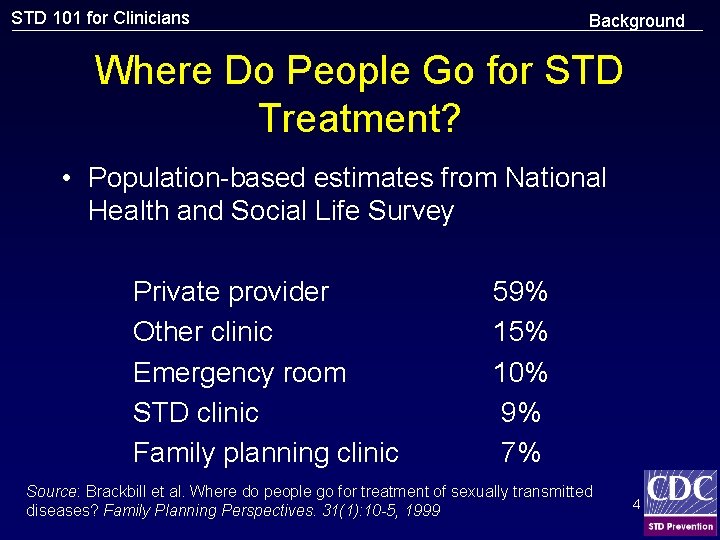
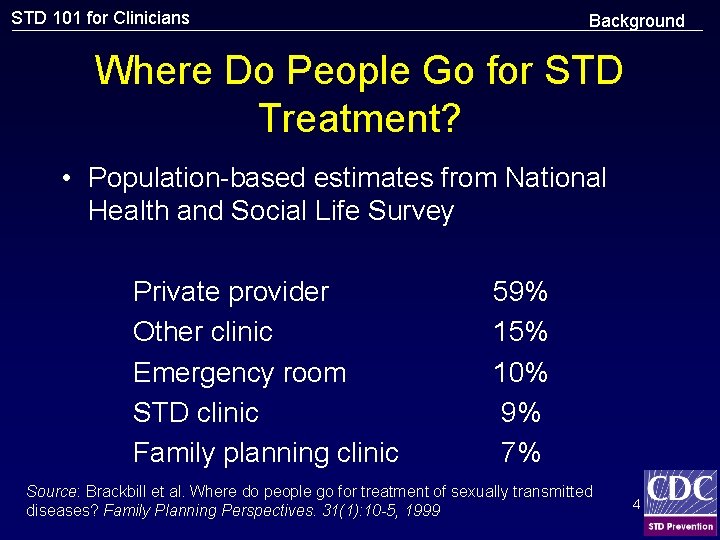
STD 101 for Clinicians Background Where Do People Go for STD Treatment? • Population-based estimates from National Health and Social Life Survey Private provider Other clinic Emergency room STD clinic Family planning clinic 59% 15% 10% 9% 7% Source: Brackbill et al. Where do people go for treatment of sexually transmitted diseases? Family Planning Perspectives. 31(1): 10 -5, 1999 4
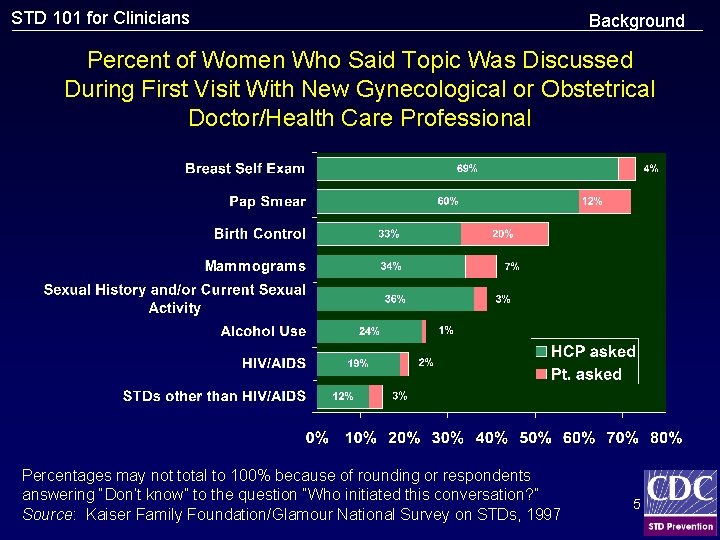
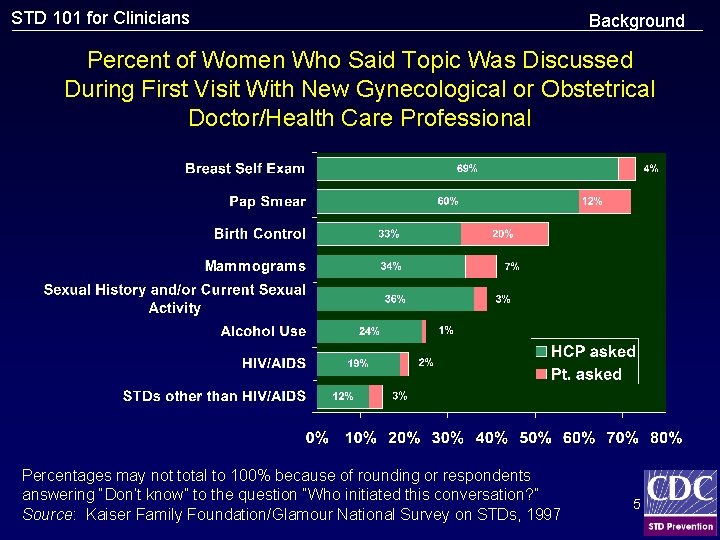
STD 101 for Clinicians Background Percent of Women Who Said Topic Was Discussed During First Visit With New Gynecological or Obstetrical Doctor/Health Care Professional Percentages may not total to 100% because of rounding or respondents answering “Don’t know” to the question “Who initiated this conversation? ” Source: Kaiser Family Foundation/Glamour National Survey on STDs, 1997 5
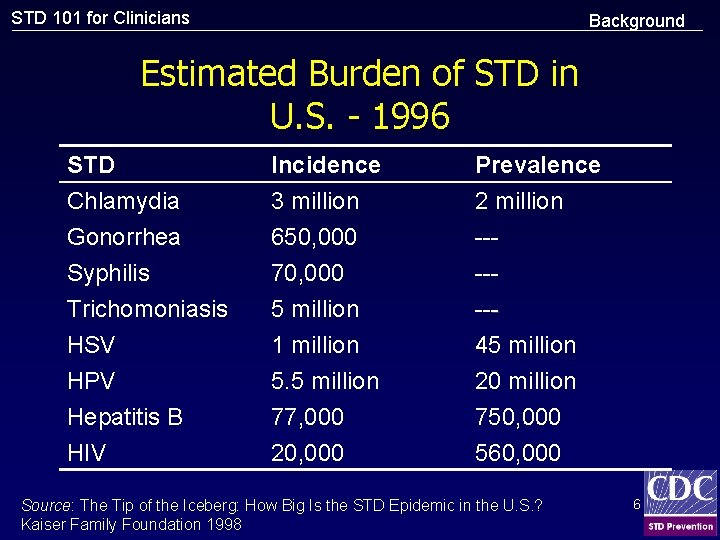
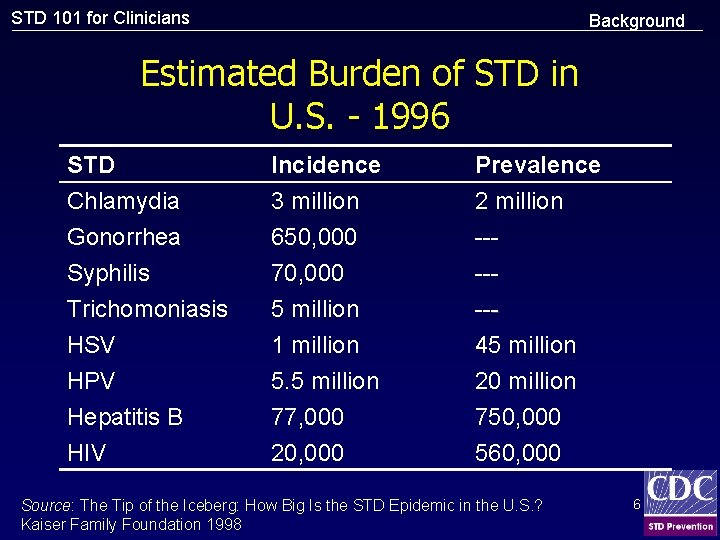
STD 101 for Clinicians Background Estimated Burden of STD in U. S. - 1996 STD Chlamydia Gonorrhea Syphilis Incidence 3 million 650, 000 70, 000 Prevalence 2 million ----- Trichomoniasis HSV HPV Hepatitis B HIV 5 million 1 million 5. 5 million 77, 000 20, 000 --45 million 20 million 750, 000 560, 000 Source: The Tip of the Iceberg: How Big Is the STD Epidemic in the U. S. ? Kaiser Family Foundation 1998 6
STD 101 for Clinicians Background “. . . the scope and impact of the STD epidemic are under-appreciated and the STD epidemic is largely hidden from public discourse. ” IOM Report 1997 7
STD 101 for Clinicians STD Prevention and Control • Education and counseling to reduce risk of STD acquisition • Detection of asymptomatic and/or symptomatic persons unlikely to seek evaluation • Effective diagnosis and treatment • Evaluation, treatment, and counseling of sexual partners • Preexposure vaccination--hepatitis A, B 8
STD 101 for Clinicians Prevention Messages • Prevention messages tailored to the client’s personal risk; interactive counseling approaches are effective • Despite adolescents greater risk of STDs, providers often fail to inquire about sexual behavior, assess risk, counsel about risk reduction, screen for asx infection • Specific actions necessary to avoid acquisition or transmission of STDs • Clients seeking evaluation or treatment for STDs should be informed which specific tests will be performed 9
STD 101 for Clinicians Prevention Methods Male Condoms • Consistent/correct use of latex condoms are effective in preventing sexual transmission of HIV infection and can reduce risk of other STDs • Likely to be more effective in prevention of infections transmitted by fluids from mucosal surfaces (GC, CT, trichomonas, HIV) than those transmitted by skin-skin contact (HSV, HPV, syphilis, chancroid) 10
STD 101 for Clinicians Prevention Methods Spermicides • N-9 vaginal spermicides are not effective in preventing CT, GC, or HIV infection • Frequent use of spermicides/N-9 have been associated with genital lesions • Spermicides alone are not recommended for STD/HIV prevention • N-9 should not be used a microbicide or lubricant during anal intercourse 11
STD 101 for Clinicians MSM • STD/HIV sexual risk assessment and clientcentered prevention counseling • Annual STD screening for MSM at risk -HIV and syphilis serology -Urethral cx or NAAT, GC/CT -Pharyngeal cx, GC (oro-genital) -Rectal cx, GC/CT (receptive anal IC) 12
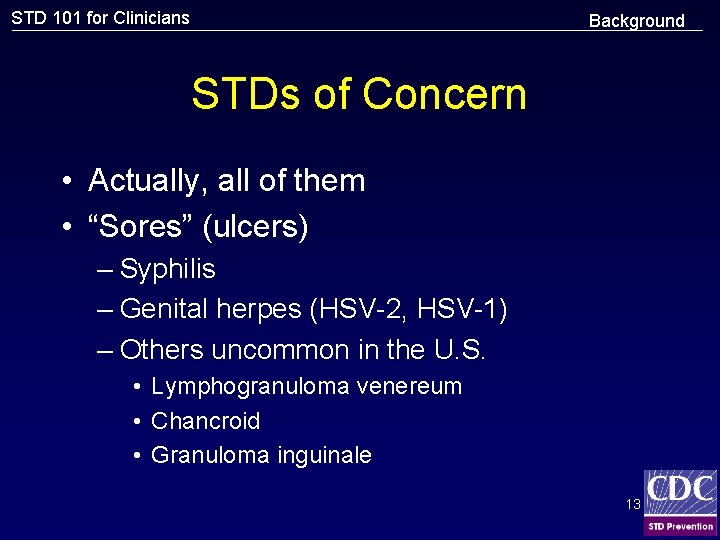
STD 101 for Clinicians Background STDs of Concern • Actually, all of them • “Sores” (ulcers) – Syphilis – Genital herpes (HSV-2, HSV-1) – Others uncommon in the U. S. • Lymphogranuloma venereum • Chancroid • Granuloma inguinale 13
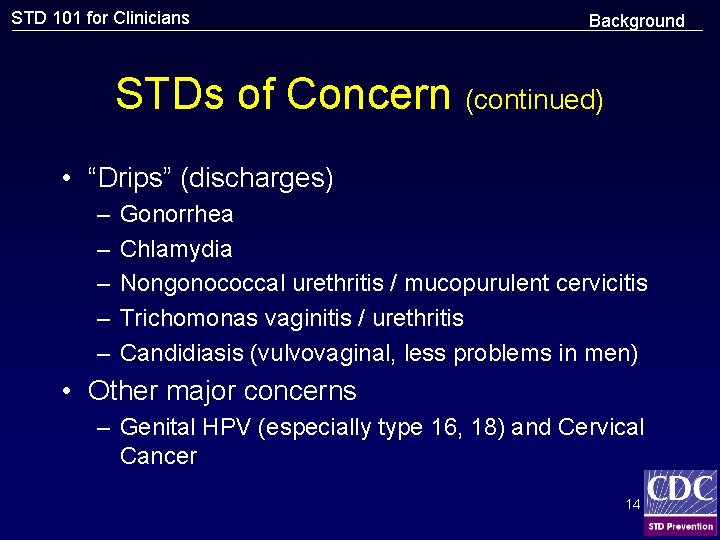
STD 101 for Clinicians Background STDs of Concern (continued) • “Drips” (discharges) – – – Gonorrhea Chlamydia Nongonococcal urethritis / mucopurulent cervicitis Trichomonas vaginitis / urethritis Candidiasis (vulvovaginal, less problems in men) • Other major concerns – Genital HPV (especially type 16, 18) and Cervical Cancer 14
STD 101 for Clinicians “Drips” Gonorrhea Nongonococcal urethritis Chlamydia Mucopurulent cervicitis Trichomonas vaginitis and urethritis Candidiasis 15
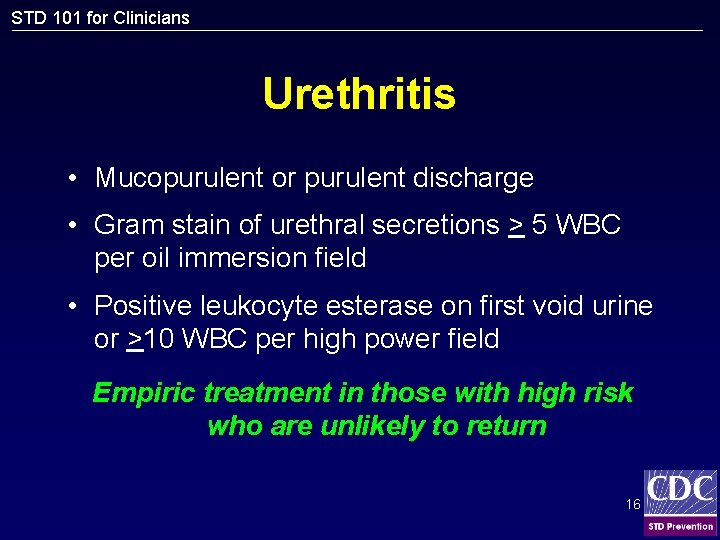
STD 101 for Clinicians Urethritis • Mucopurulent or purulent discharge • Gram stain of urethral secretions > 5 WBC per oil immersion field • Positive leukocyte esterase on first void urine or >10 WBC per high power field Empiric treatment in those with high risk who are unlikely to return 16
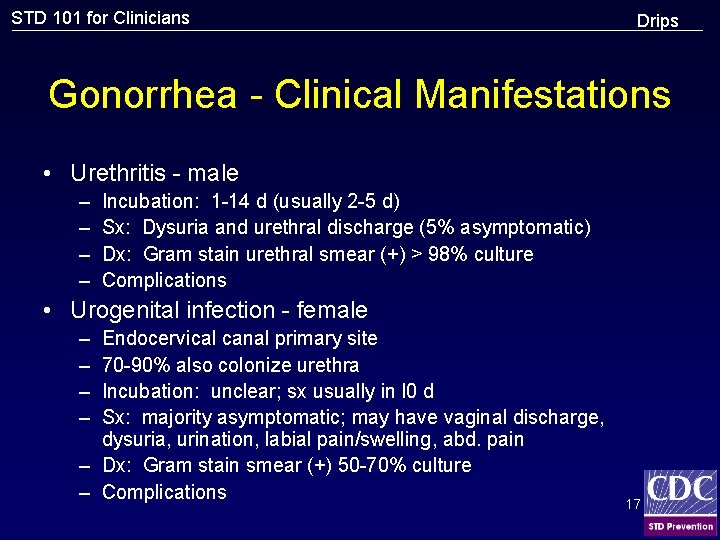
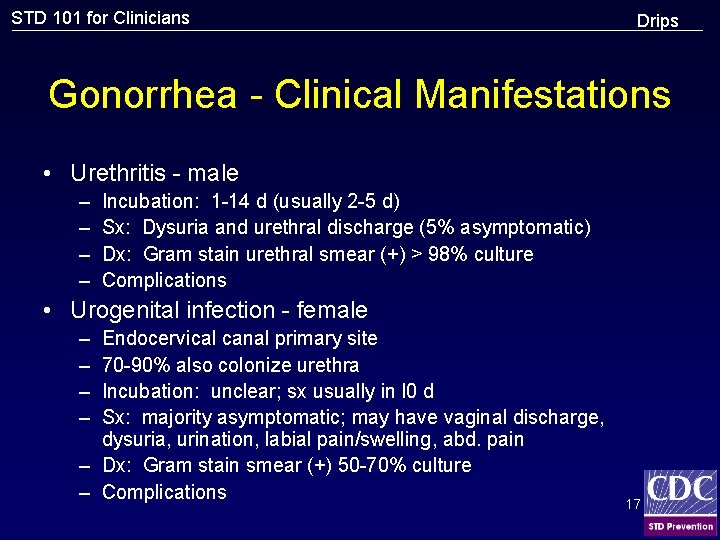
STD 101 for Clinicians Drips Gonorrhea - Clinical Manifestations • Urethritis - male – – Incubation: 1 -14 d (usually 2 -5 d) Sx: Dysuria and urethral discharge (5% asymptomatic) Dx: Gram stain urethral smear (+) > 98% culture Complications • Urogenital infection - female – – Endocervical canal primary site 70 -90% also colonize urethra Incubation: unclear; sx usually in l 0 d Sx: majority asymptomatic; may have vaginal discharge, dysuria, urination, labial pain/swelling, abd. pain – Dx: Gram stain smear (+) 50 -70% culture – Complications 17
STD 101 for Clinicians Gonorrhea Epidemiology of Gonorrhea • Proportion of gonococcal infections caused by resistant organisms is increasing • Incidence remains high in some groups defined by geography, age and race/ethnicity, or sexual orientation • Gonorrhea associated with increased susceptibility to HIV infection 18
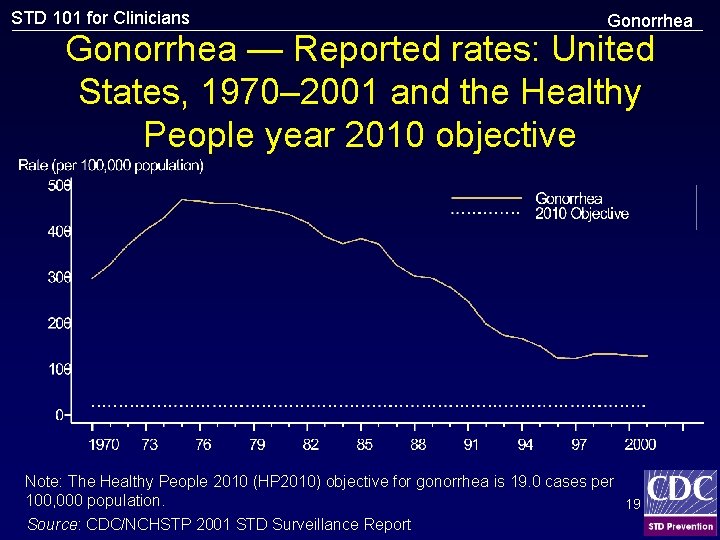
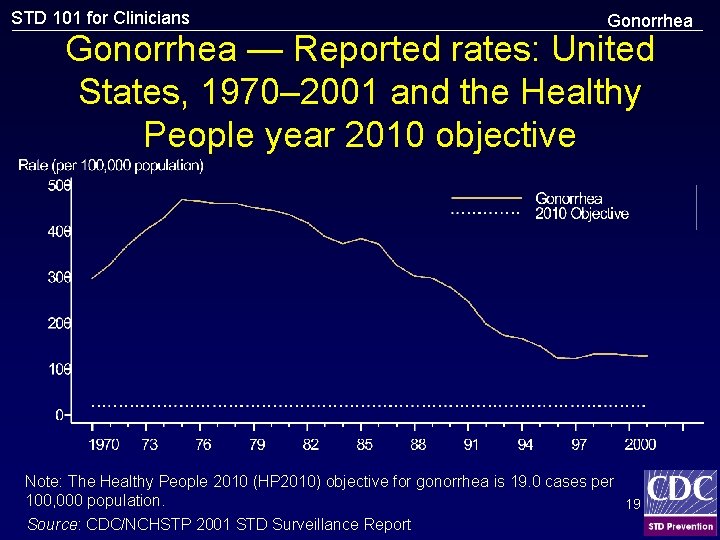
STD 101 for Clinicians Gonorrhea — Reported rates: United States, 1970– 2001 and the Healthy People year 2010 objective Note: The Healthy People 2010 (HP 2010) objective for gonorrhea is 19. 0 cases per 100, 000 population. 19 Source: CDC/NCHSTP 2001 STD Surveillance Report
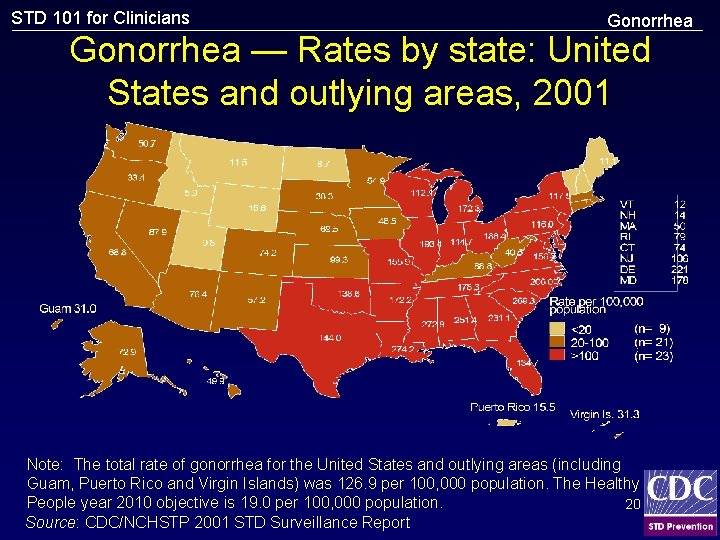
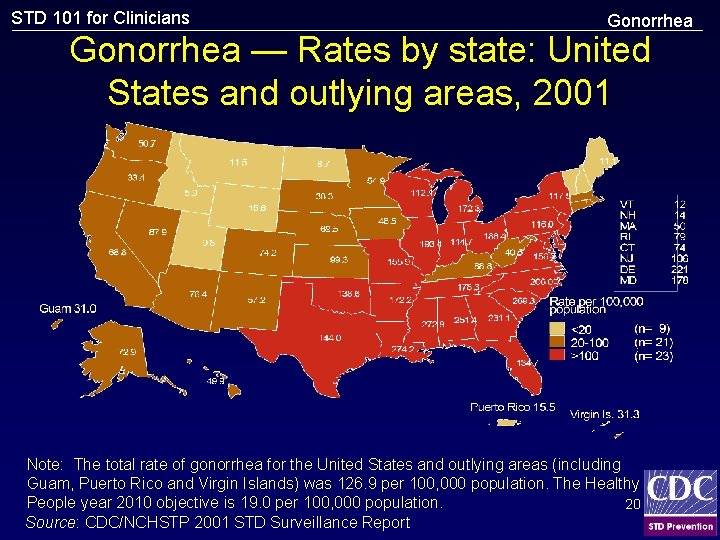
STD 101 for Clinicians Gonorrhea — Rates by state: United States and outlying areas, 2001 Note: The total rate of gonorrhea for the United States and outlying areas (including Guam, Puerto Rico and Virgin Islands) was 126. 9 per 100, 000 population. The Healthy People year 2010 objective is 19. 0 per 100, 000 population. 20 Source: CDC/NCHSTP 2001 STD Surveillance Report
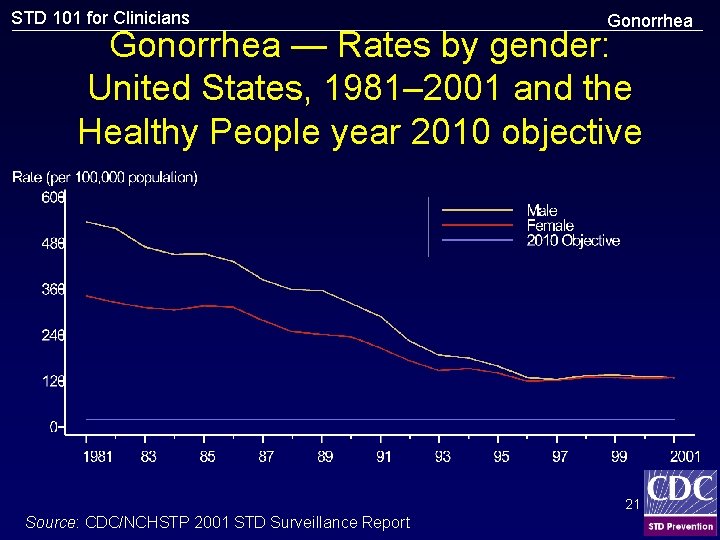
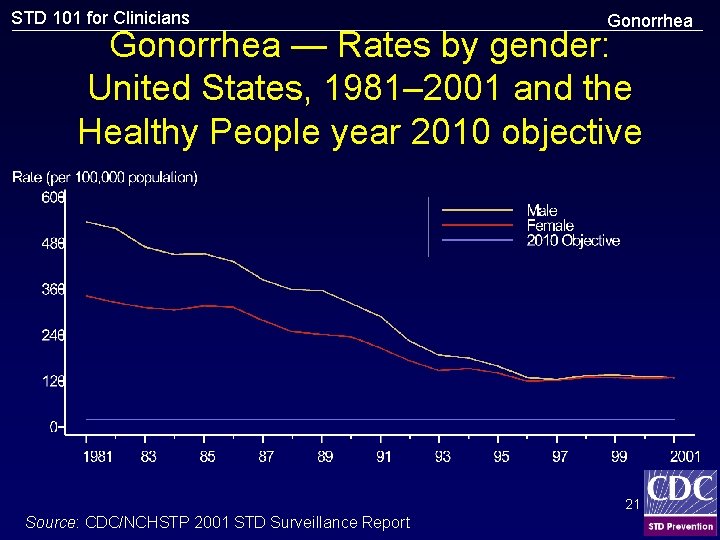
STD 101 for Clinicians Gonorrhea — Rates by gender: United States, 1981– 2001 and the Healthy People year 2010 objective 21 Source: CDC/NCHSTP 2001 STD Surveillance Report
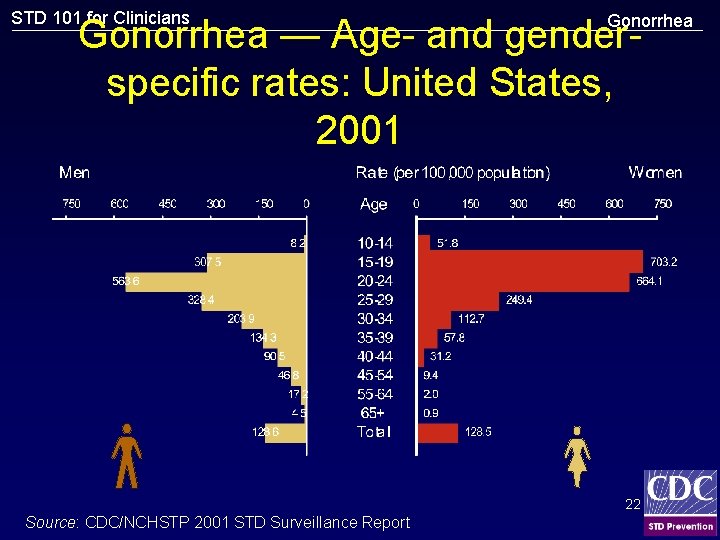
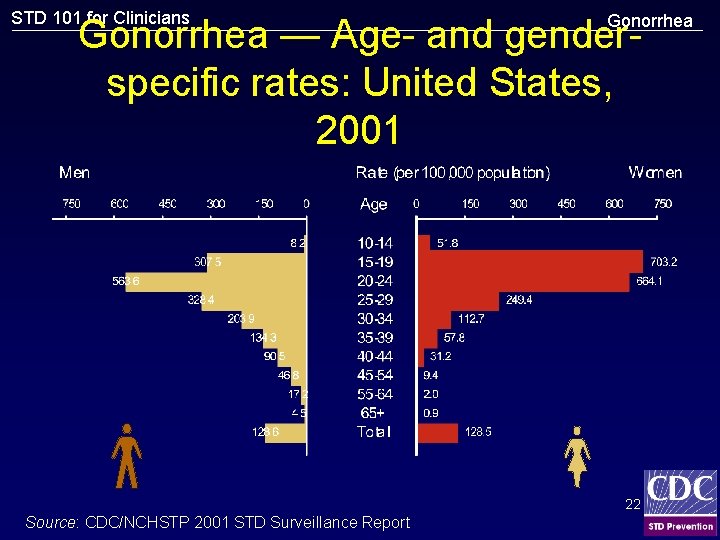
STD 101 for Clinicians Gonorrhea — Age- and genderspecific rates: United States, 2001 22 Source: CDC/NCHSTP 2001 STD Surveillance Report
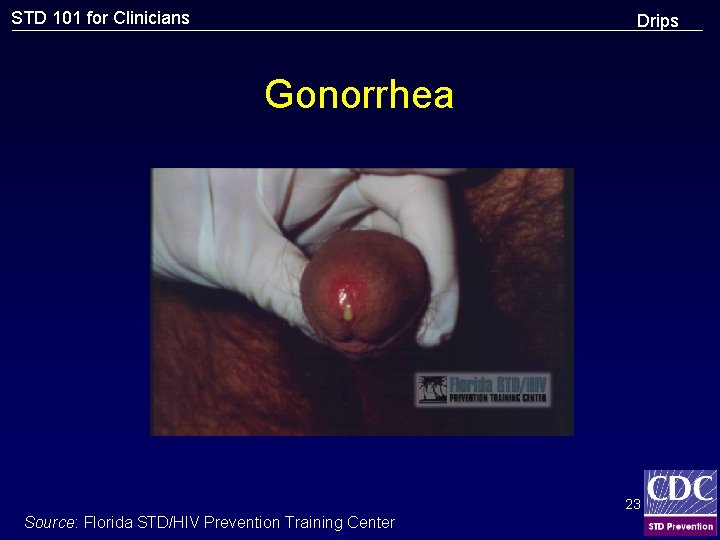
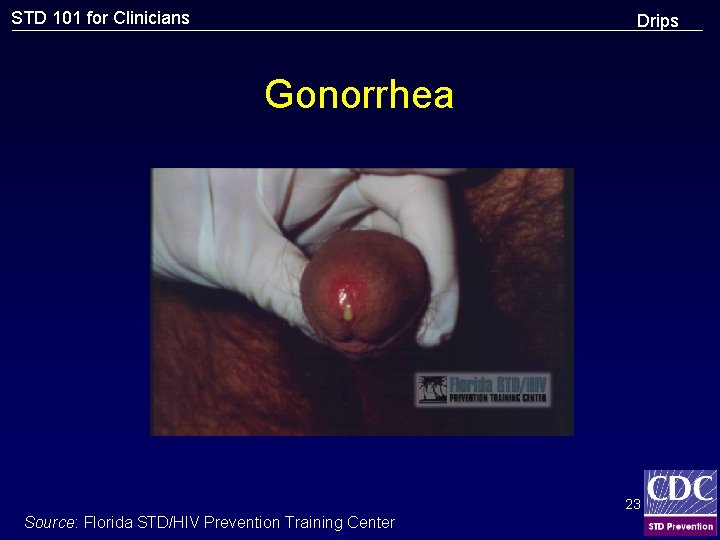
STD 101 for Clinicians Drips Gonorrhea 23 Source: Florida STD/HIV Prevention Training Center
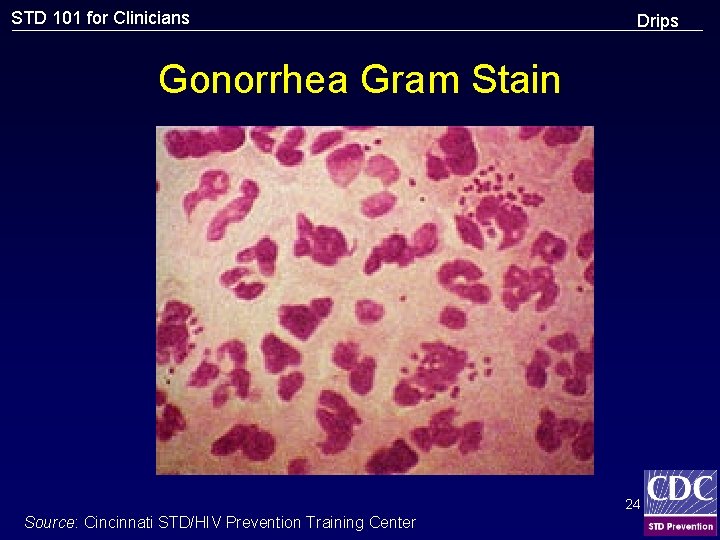
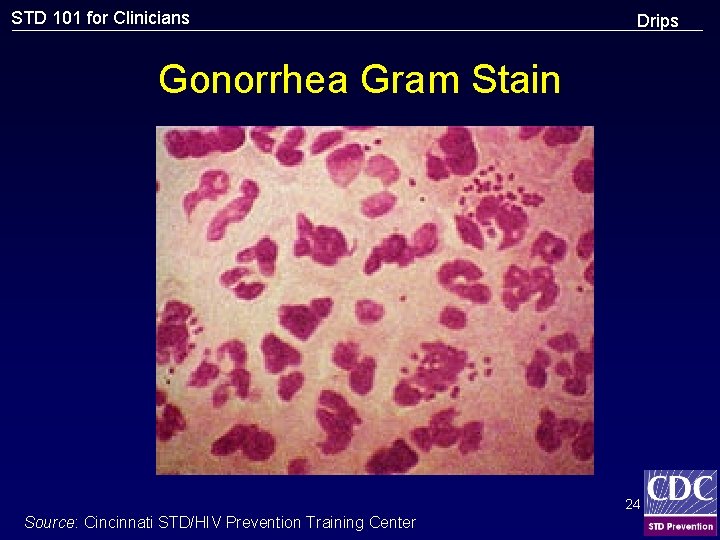
STD 101 for Clinicians Drips Gonorrhea Gram Stain 24 Source: Cincinnati STD/HIV Prevention Training Center
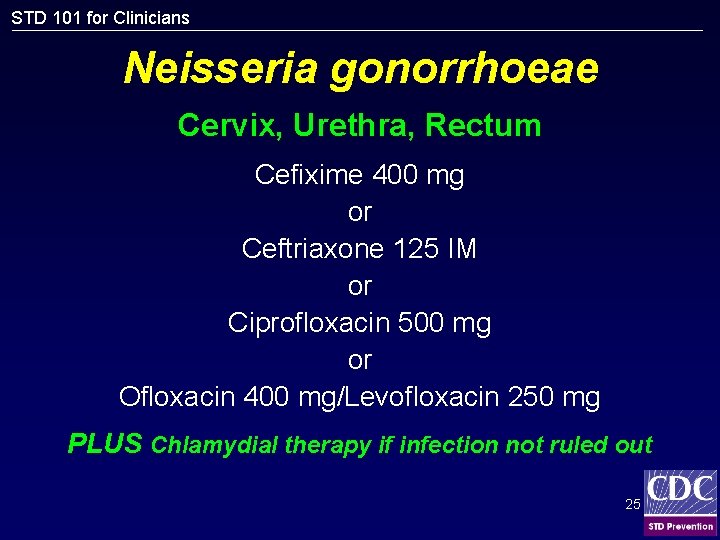
STD 101 for Clinicians Neisseria gonorrhoeae Cervix, Urethra, Rectum Cefixime 400 mg or Ceftriaxone 125 IM or Ciprofloxacin 500 mg or Ofloxacin 400 mg/Levofloxacin 250 mg PLUS Chlamydial therapy if infection not ruled out 25
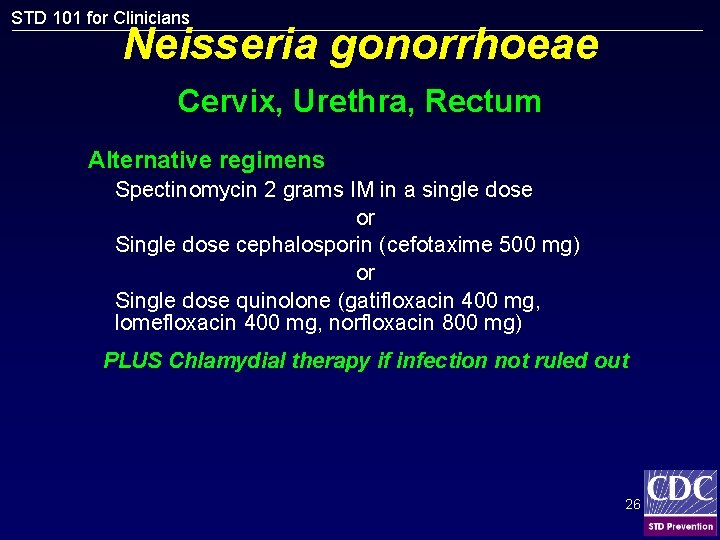
STD 101 for Clinicians Neisseria gonorrhoeae Cervix, Urethra, Rectum Alternative regimens Spectinomycin 2 grams IM in a single dose or Single dose cephalosporin (cefotaxime 500 mg) or Single dose quinolone (gatifloxacin 400 mg, lomefloxacin 400 mg, norfloxacin 800 mg) PLUS Chlamydial therapy if infection not ruled out 26
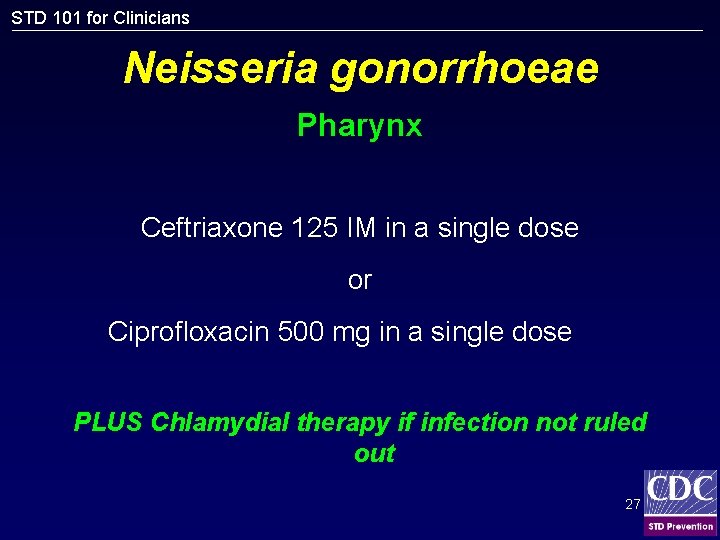
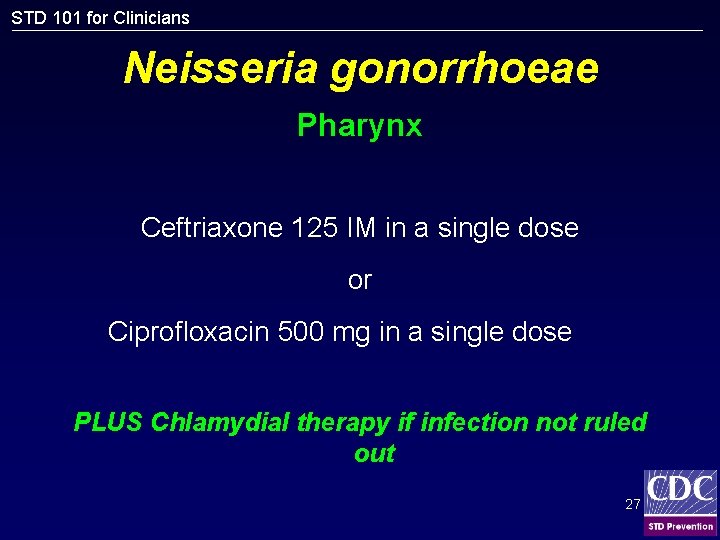
STD 101 for Clinicians Neisseria gonorrhoeae Pharynx Ceftriaxone 125 IM in a single dose or Ciprofloxacin 500 mg in a single dose PLUS Chlamydial therapy if infection not ruled out 27
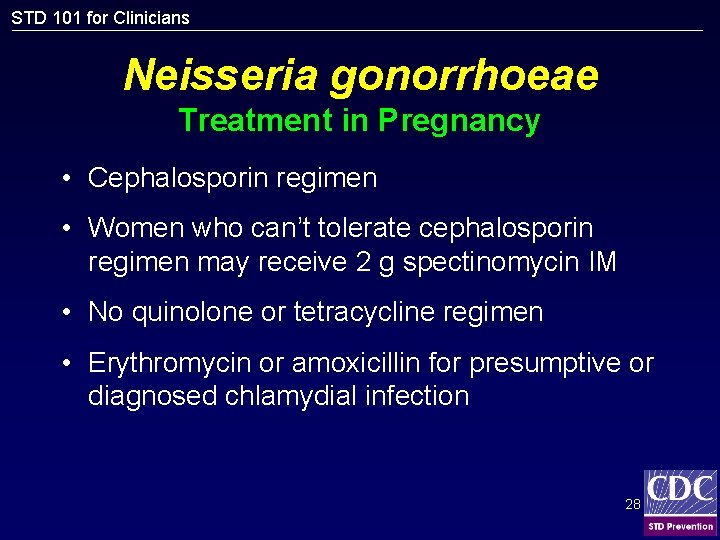
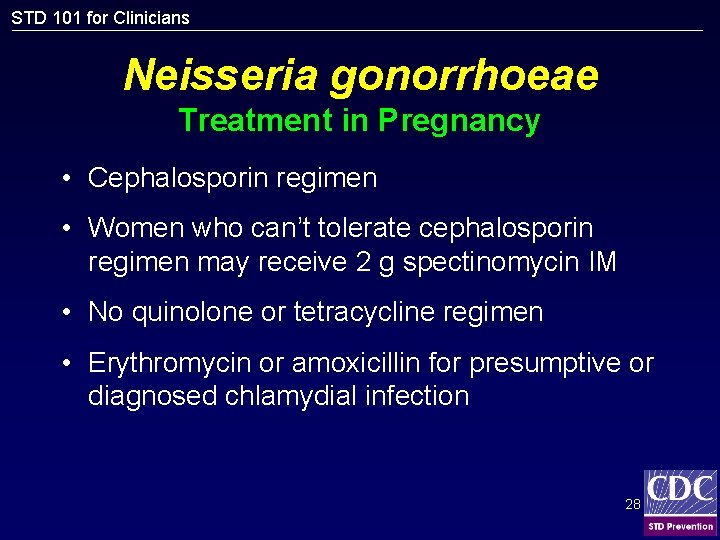
STD 101 for Clinicians Neisseria gonorrhoeae Treatment in Pregnancy • Cephalosporin regimen • Women who can’t tolerate cephalosporin regimen may receive 2 g spectinomycin IM • No quinolone or tetracycline regimen • Erythromycin or amoxicillin for presumptive or diagnosed chlamydial infection 28
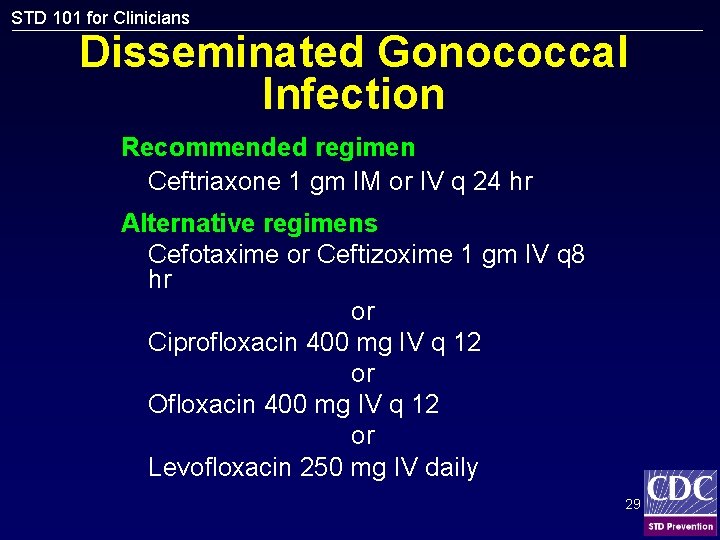
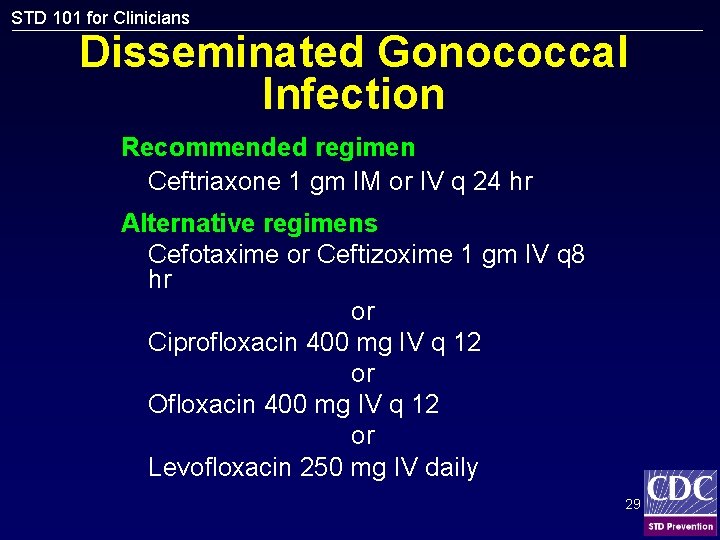
STD 101 for Clinicians Disseminated Gonococcal Infection Recommended regimen Ceftriaxone 1 gm IM or IV q 24 hr Alternative regimens Cefotaxime or Ceftizoxime 1 gm IV q 8 hr or Ciprofloxacin 400 mg IV q 12 or Ofloxacin 400 mg IV q 12 or Levofloxacin 250 mg IV daily 29
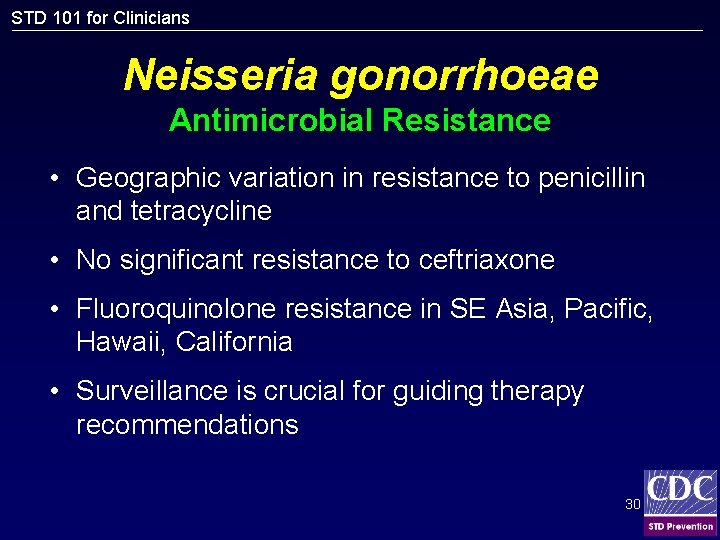
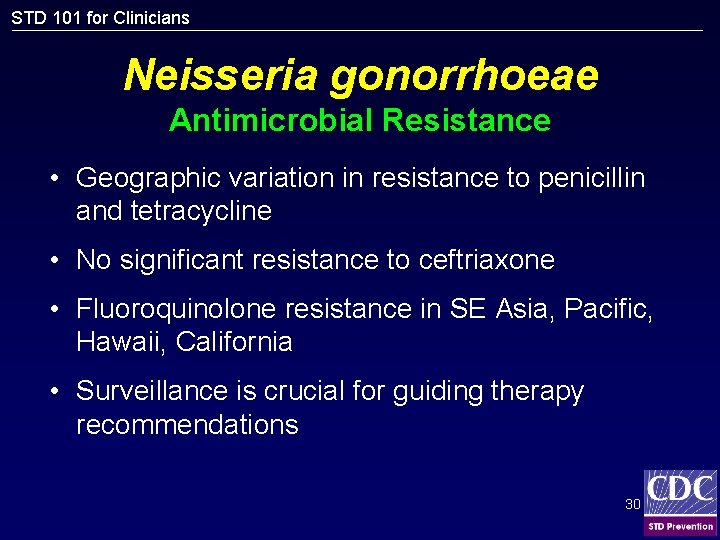
STD 101 for Clinicians Neisseria gonorrhoeae Antimicrobial Resistance • Geographic variation in resistance to penicillin and tetracycline • No significant resistance to ceftriaxone • Fluoroquinolone resistance in SE Asia, Pacific, Hawaii, California • Surveillance is crucial for guiding therapy recommendations 30
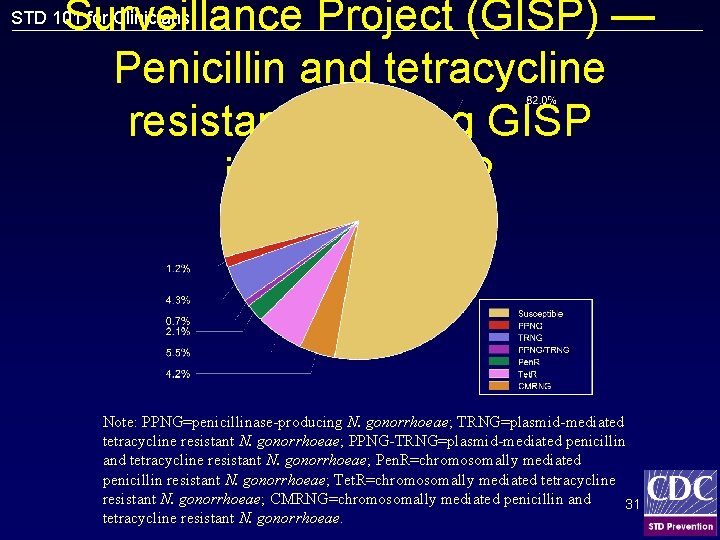
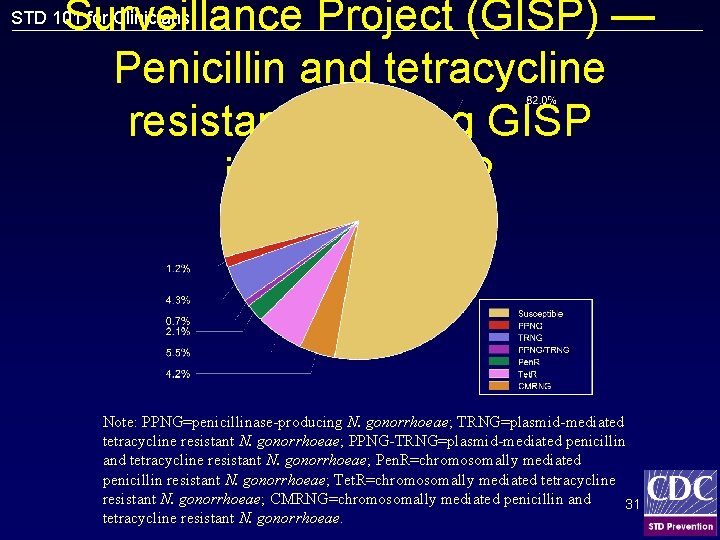
Surveillance Project (GISP) — Penicillin and tetracycline resistance among GISP isolates, 2002 STD 101 for Clinicians Note: PPNG=penicillinase-producing N. gonorrhoeae; TRNG=plasmid-mediated tetracycline resistant N. gonorrhoeae; PPNG-TRNG=plasmid-mediated penicillin and tetracycline resistant N. gonorrhoeae; Pen. R=chromosomally mediated penicillin resistant N. gonorrhoeae; Tet. R=chromosomally mediated tetracycline resistant N. gonorrhoeae; CMRNG=chromosomally mediated penicillin and 31 tetracycline resistant N. gonorrhoeae.
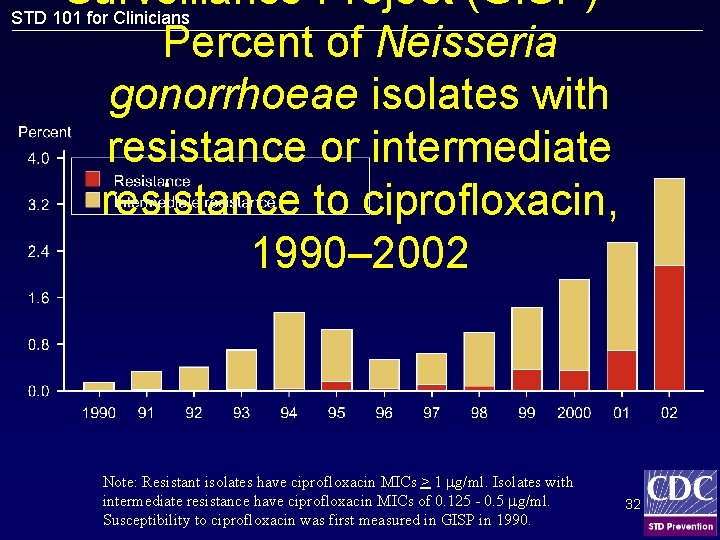
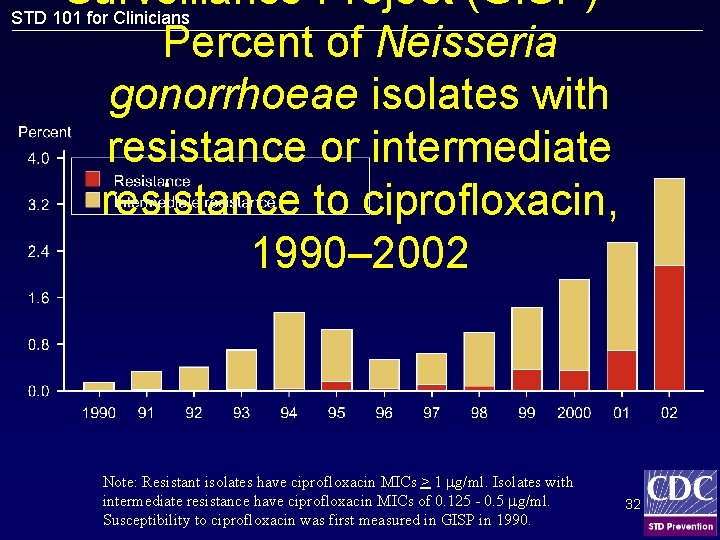
Surveillance Project (GISP) — STD 101 for Clinicians Percent of Neisseria gonorrhoeae isolates with resistance or intermediate resistance to ciprofloxacin, 1990– 2002 Note: Resistant isolates have ciprofloxacin MICs > 1 g/ml. Isolates with intermediate resistance have ciprofloxacin MICs of 0. 125 - 0. 5 g/ml. Susceptibility to ciprofloxacin was first measured in GISP in 1990. 32
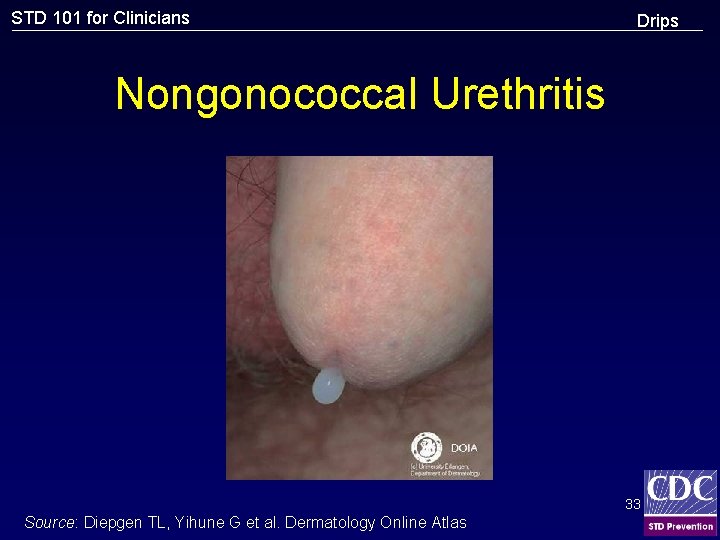
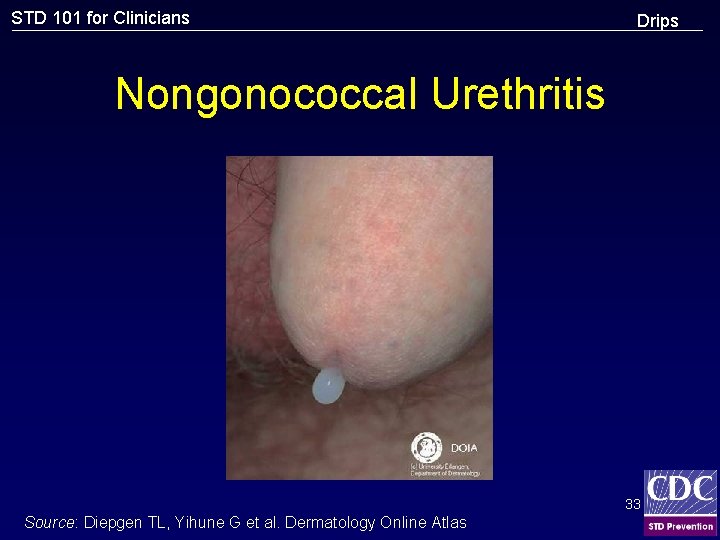
STD 101 for Clinicians Drips Nongonococcal Urethritis 33 Source: Diepgen TL, Yihune G et al. Dermatology Online Atlas
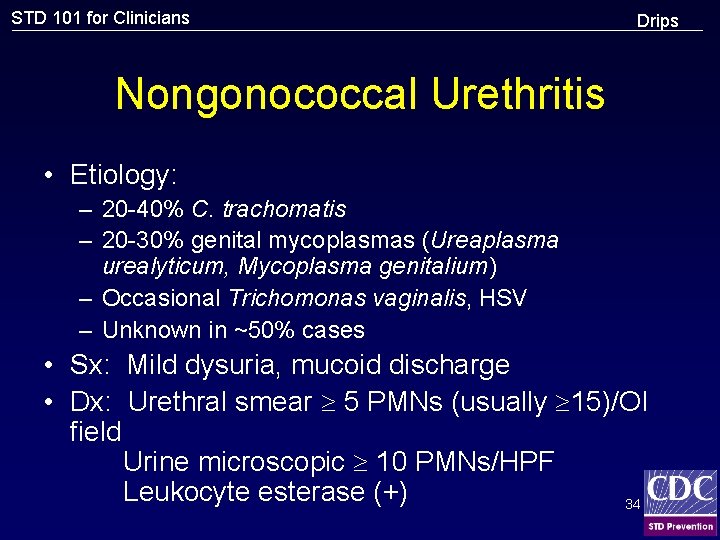
STD 101 for Clinicians Drips Nongonococcal Urethritis • Etiology: – 20 -40% C. trachomatis – 20 -30% genital mycoplasmas (Ureaplasma urealyticum, Mycoplasma genitalium) – Occasional Trichomonas vaginalis, HSV – Unknown in ~50% cases • Sx: Mild dysuria, mucoid discharge • Dx: Urethral smear 5 PMNs (usually 15)/OI field Urine microscopic 10 PMNs/HPF Leukocyte esterase (+) 34
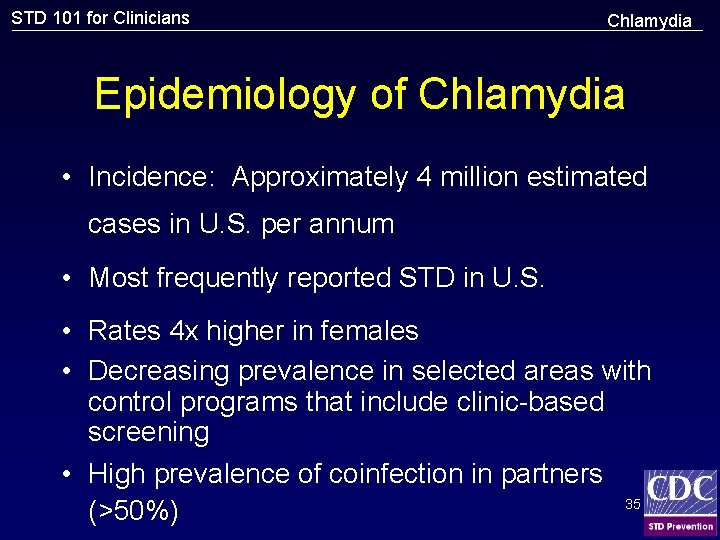
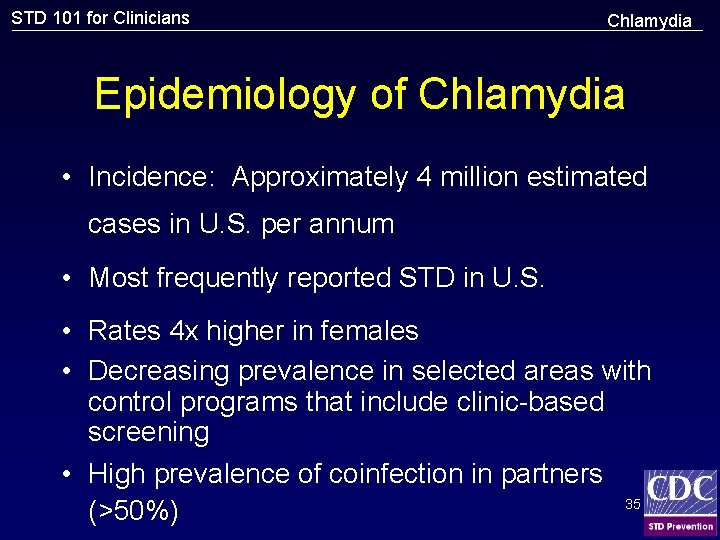
STD 101 for Clinicians Chlamydia Epidemiology of Chlamydia • Incidence: Approximately 4 million estimated cases in U. S. per annum • Most frequently reported STD in U. S. • Rates 4 x higher in females • Decreasing prevalence in selected areas with control programs that include clinic-based screening • High prevalence of coinfection in partners 35 (>50%)
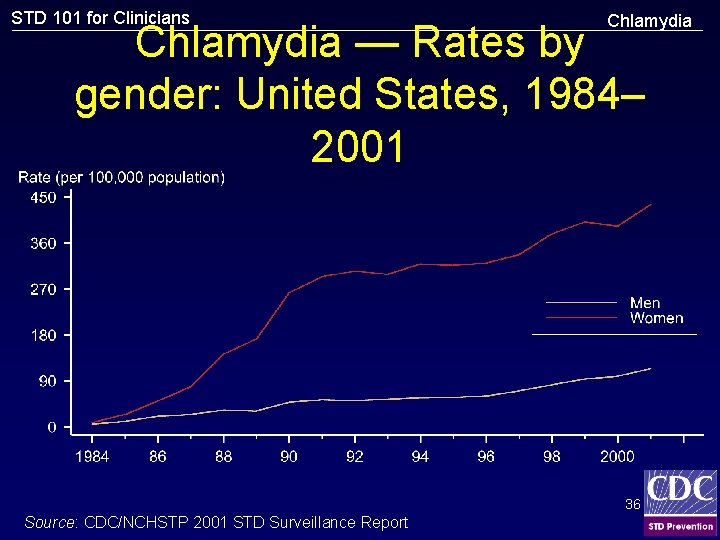
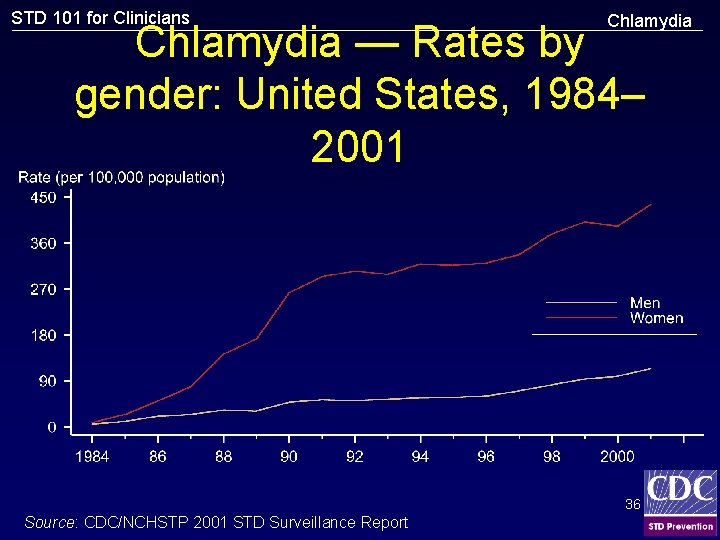
STD 101 for Clinicians Chlamydia — Rates by gender: United States, 1984– 2001 36 Source: CDC/NCHSTP 2001 STD Surveillance Report
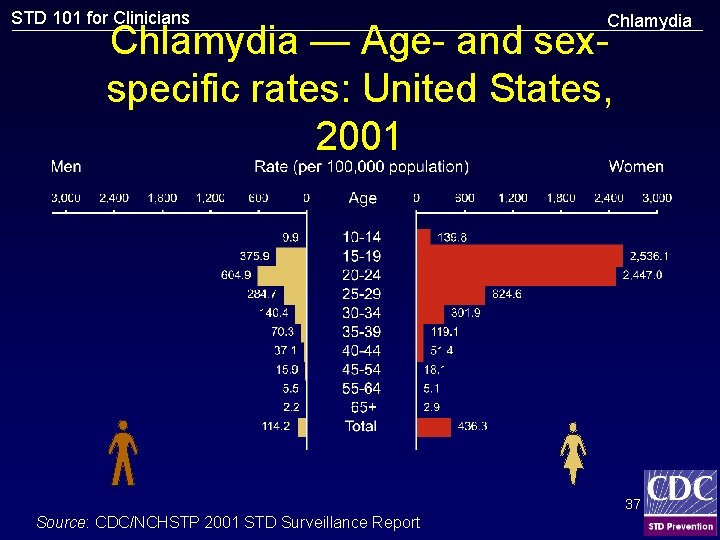
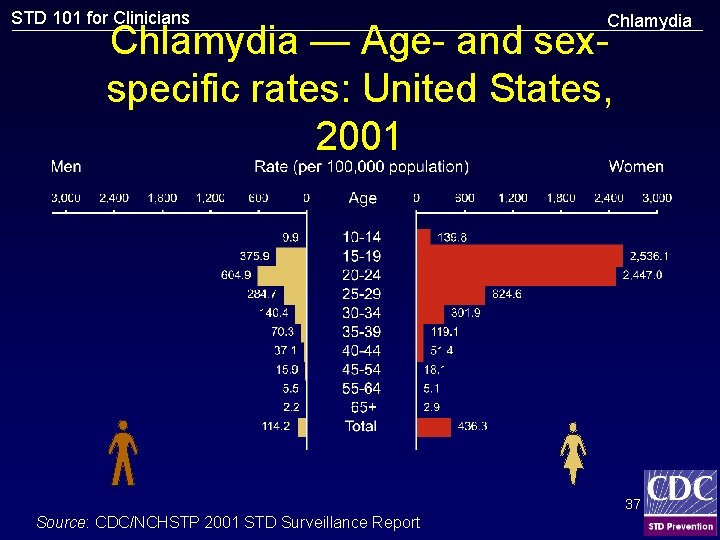
STD 101 for Clinicians Chlamydia — Age- and sexspecific rates: United States, 2001 37 Source: CDC/NCHSTP 2001 STD Surveillance Report
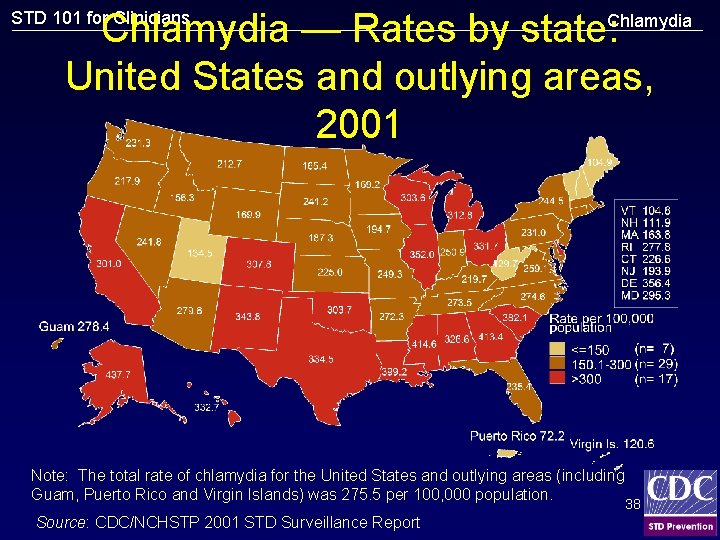
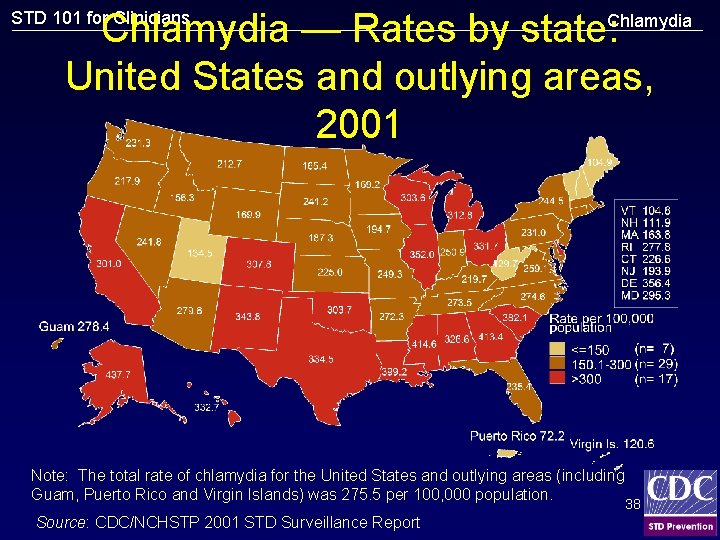
Chlamydia — Rates by state: United States and outlying areas, 2001 STD 101 for Clinicians Chlamydia Note: The total rate of chlamydia for the United States and outlying areas (including Guam, Puerto Rico and Virgin Islands) was 275. 5 per 100, 000 population. Source: CDC/NCHSTP 2001 STD Surveillance Report 38
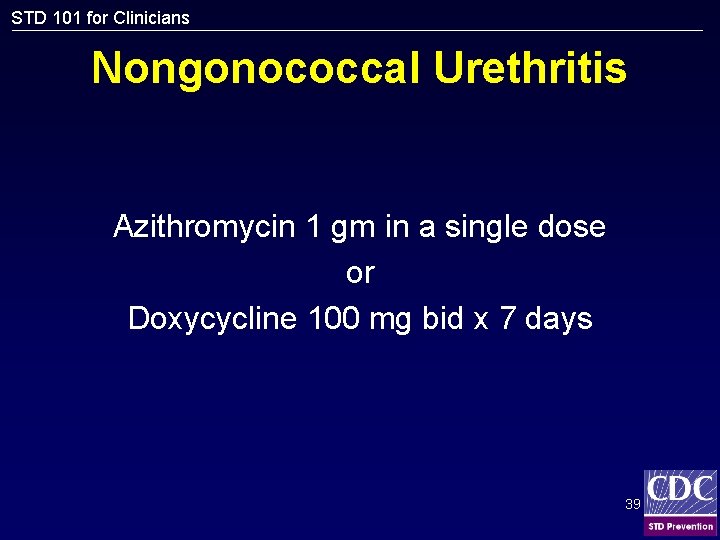
STD 101 for Clinicians Nongonococcal Urethritis Azithromycin 1 gm in a single dose or Doxycycline 100 mg bid x 7 days 39
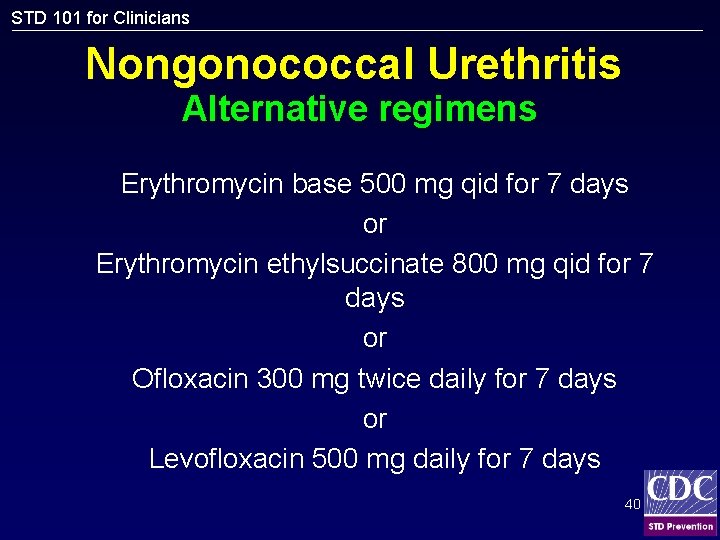
STD 101 for Clinicians Nongonococcal Urethritis Alternative regimens Erythromycin base 500 mg qid for 7 days or Erythromycin ethylsuccinate 800 mg qid for 7 days or Ofloxacin 300 mg twice daily for 7 days or Levofloxacin 500 mg daily for 7 days 40

STD 101 for Clinicians Recurrent/Persistent Urethritis • Objective signs of urethritis • Re-treat with initial regimen if non-compliant or re-exposure occurs • Intraurethral culture for trichomonas • Effective regimens not identified in those with persistent symptoms without signs 41
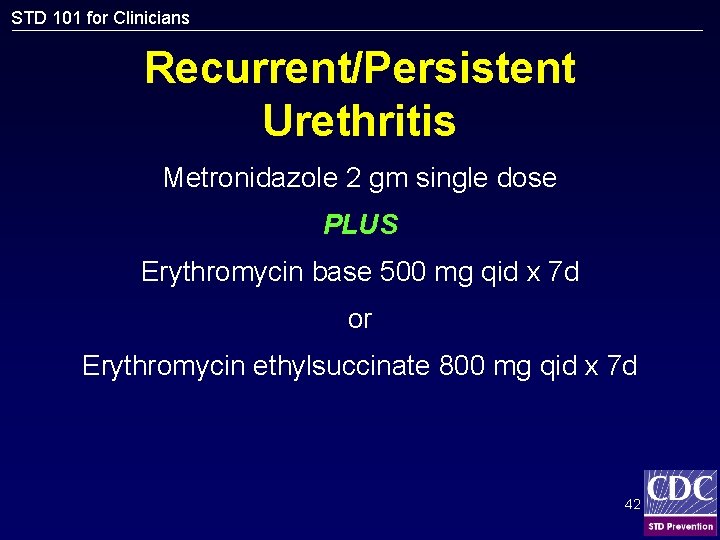
STD 101 for Clinicians Recurrent/Persistent Urethritis Metronidazole 2 gm single dose PLUS Erythromycin base 500 mg qid x 7 d or Erythromycin ethylsuccinate 800 mg qid x 7 d 42
STD 101 for Clinicians Drips Chlamydia trachomatis • More than three million new cases annually • Responsible for causing cervicitis, urethritis, proctitis, lymphogranuloma venereum, and pelvic inflammatory disease • Direct and indirect cost of chlamydial infections run into billions of dollars • Potential to transmit to newborn during delivery – Conjunctivitis, pneumonia 43
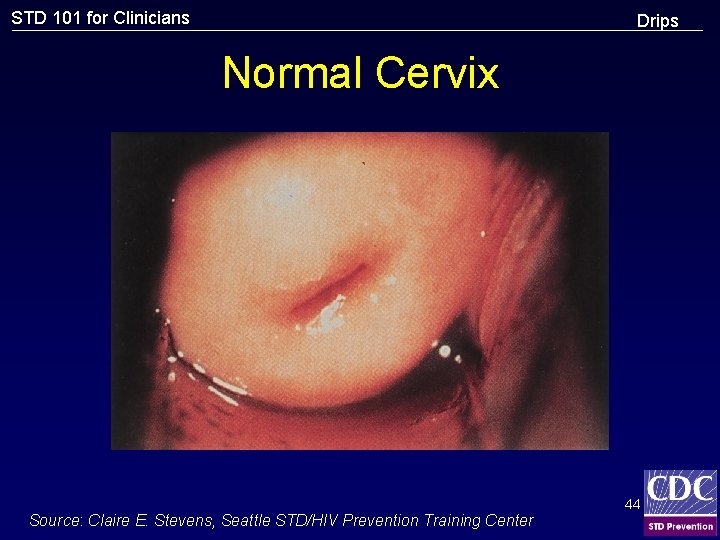
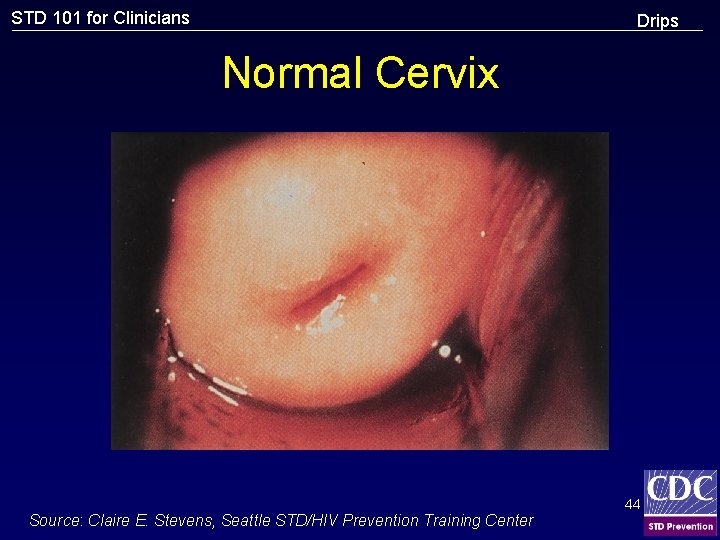
STD 101 for Clinicians Drips Normal Cervix Source: Claire E. Stevens, Seattle STD/HIV Prevention Training Center 44
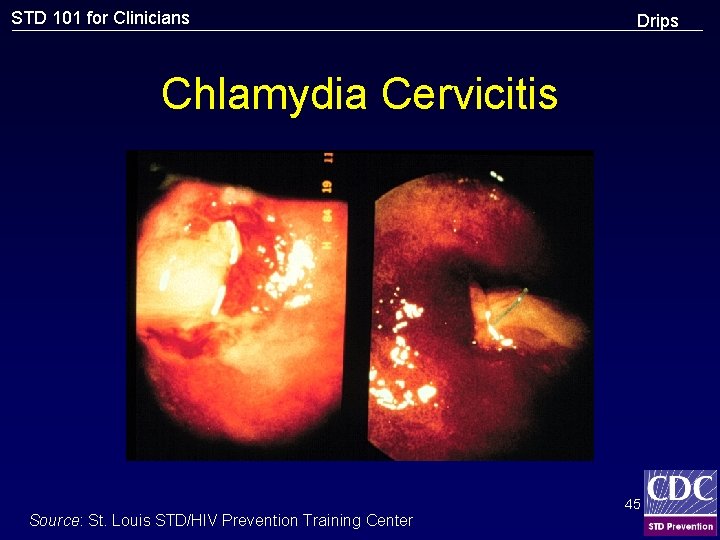
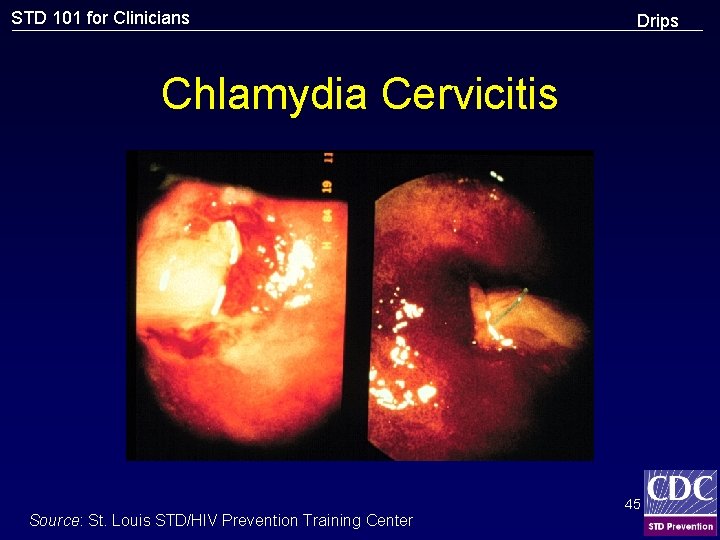
STD 101 for Clinicians Drips Chlamydia Cervicitis Source: St. Louis STD/HIV Prevention Training Center 45
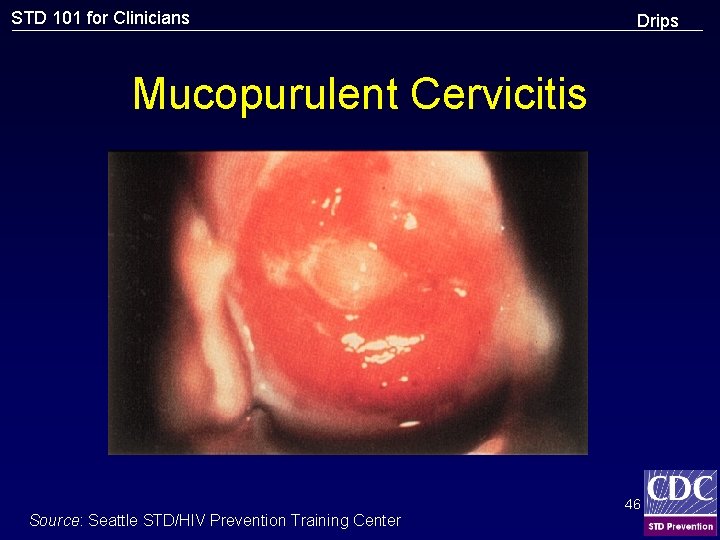
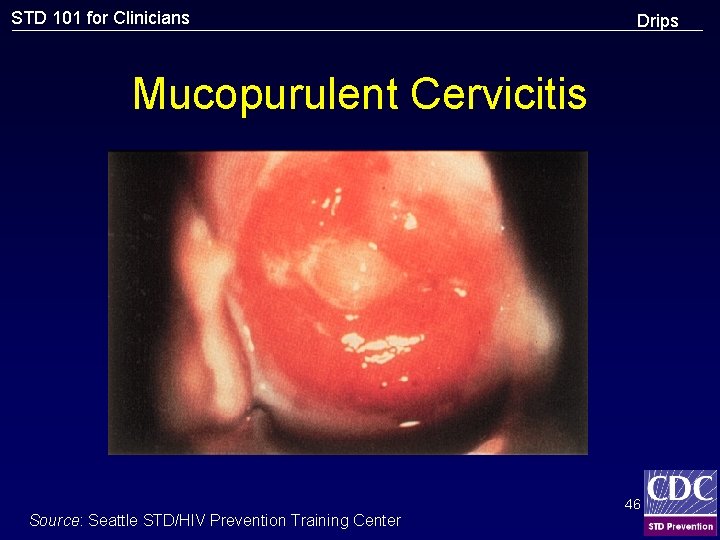
STD 101 for Clinicians Drips Mucopurulent Cervicitis Source: Seattle STD/HIV Prevention Training Center 46
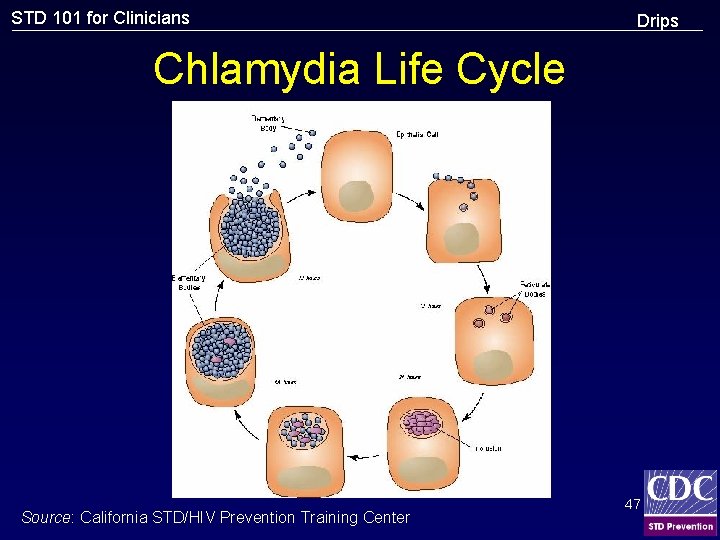
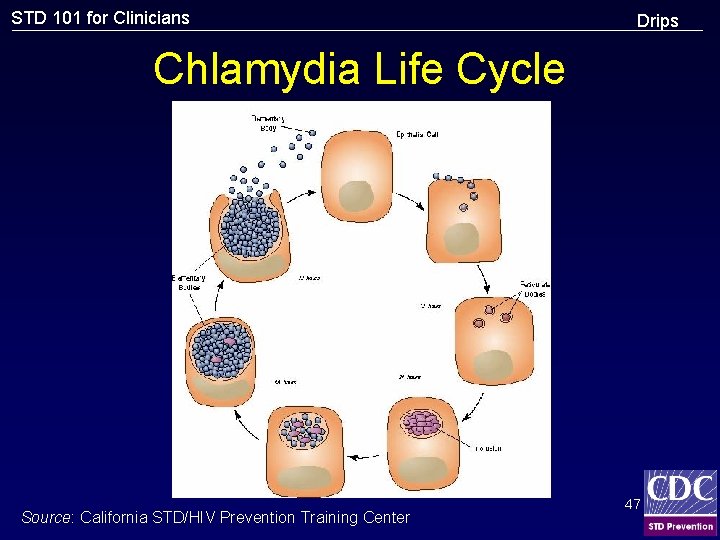
STD 101 for Clinicians Drips Chlamydia Life Cycle Source: California STD/HIV Prevention Training Center 47
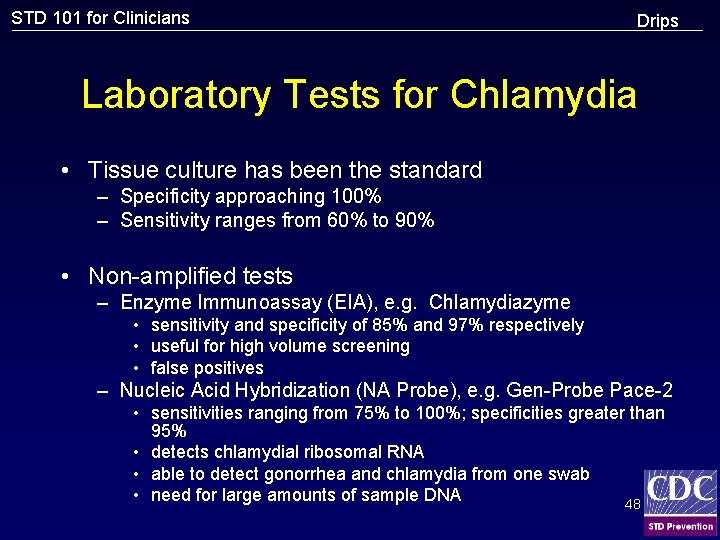
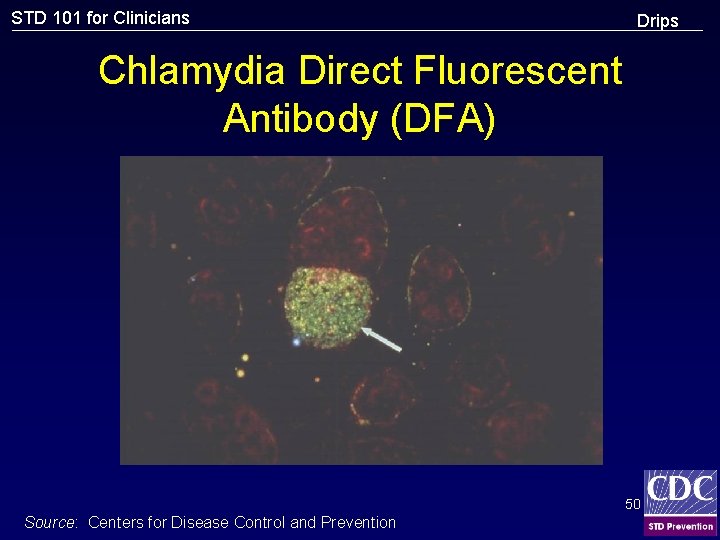
STD 101 for Clinicians Drips Laboratory Tests for Chlamydia • Tissue culture has been the standard – Specificity approaching 100% – Sensitivity ranges from 60% to 90% • Non-amplified tests – Enzyme Immunoassay (EIA), e. g. Chlamydiazyme • sensitivity and specificity of 85% and 97% respectively • useful for high volume screening • false positives – Nucleic Acid Hybridization (NA Probe), e. g. Gen-Probe Pace-2 • sensitivities ranging from 75% to 100%; specificities greater than 95% • detects chlamydial ribosomal RNA • able to detect gonorrhea and chlamydia from one swab • need for large amounts of sample DNA 48
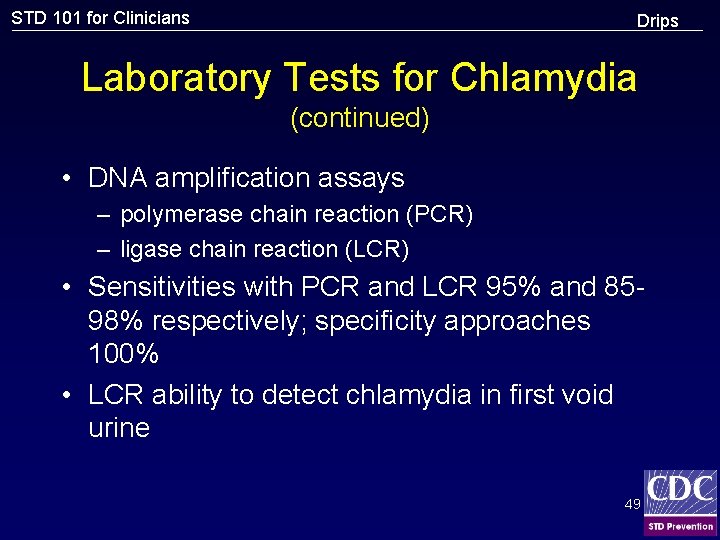
STD 101 for Clinicians Drips Laboratory Tests for Chlamydia (continued) • DNA amplification assays – polymerase chain reaction (PCR) – ligase chain reaction (LCR) • Sensitivities with PCR and LCR 95% and 8598% respectively; specificity approaches 100% • LCR ability to detect chlamydia in first void urine 49
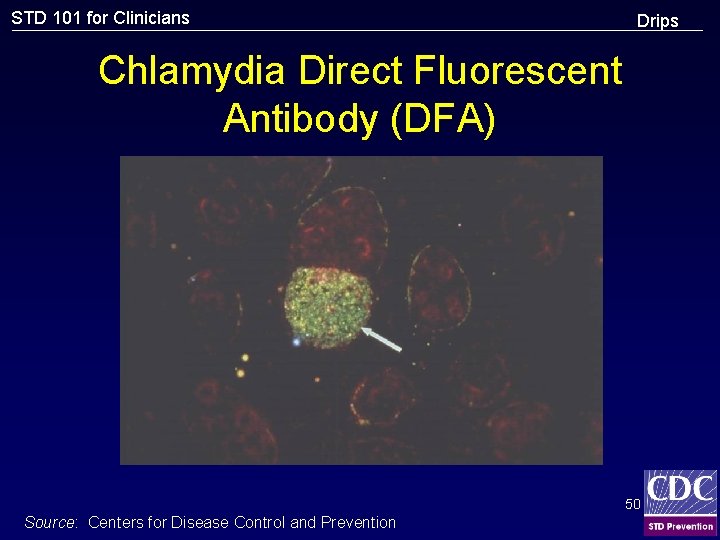
STD 101 for Clinicians Drips Chlamydia Direct Fluorescent Antibody (DFA) 50 Source: Centers for Disease Control and Prevention
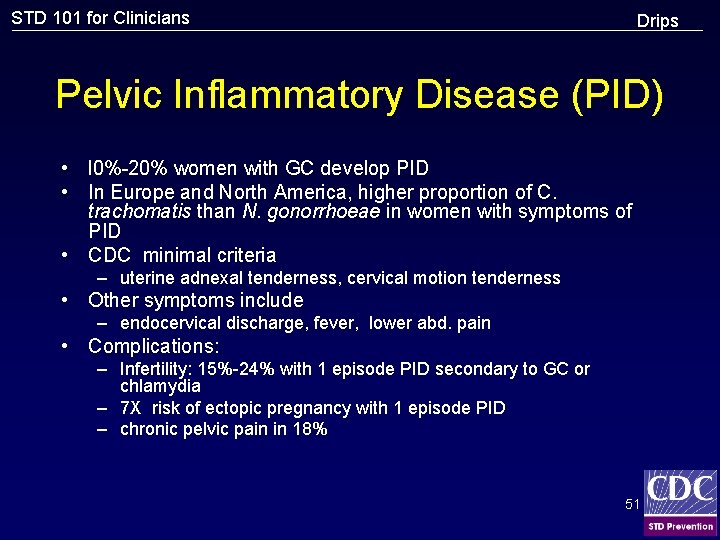
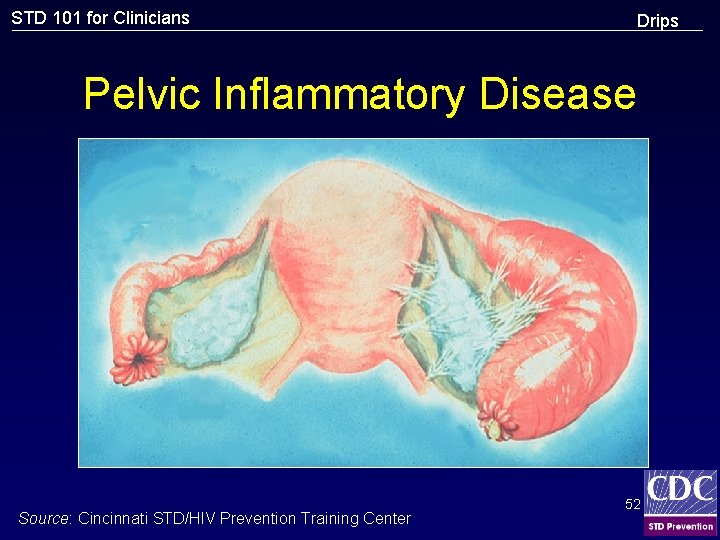
STD 101 for Clinicians Drips Pelvic Inflammatory Disease (PID) • l 0%-20% women with GC develop PID • In Europe and North America, higher proportion of C. trachomatis than N. gonorrhoeae in women with symptoms of PID • CDC minimal criteria – uterine adnexal tenderness, cervical motion tenderness • Other symptoms include – endocervical discharge, fever, lower abd. pain • Complications: – Infertility: 15%-24% with 1 episode PID secondary to GC or chlamydia – 7 X risk of ectopic pregnancy with 1 episode PID – chronic pelvic pain in 18% 51
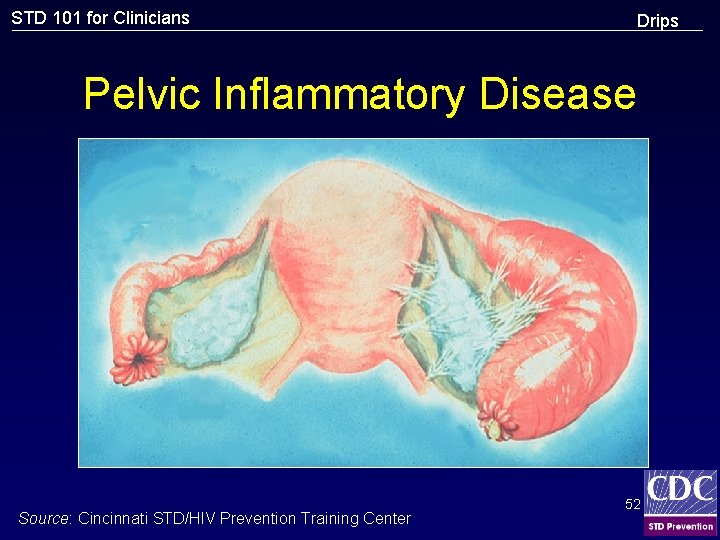
STD 101 for Clinicians Drips Pelvic Inflammatory Disease Source: Cincinnati STD/HIV Prevention Training Center 52
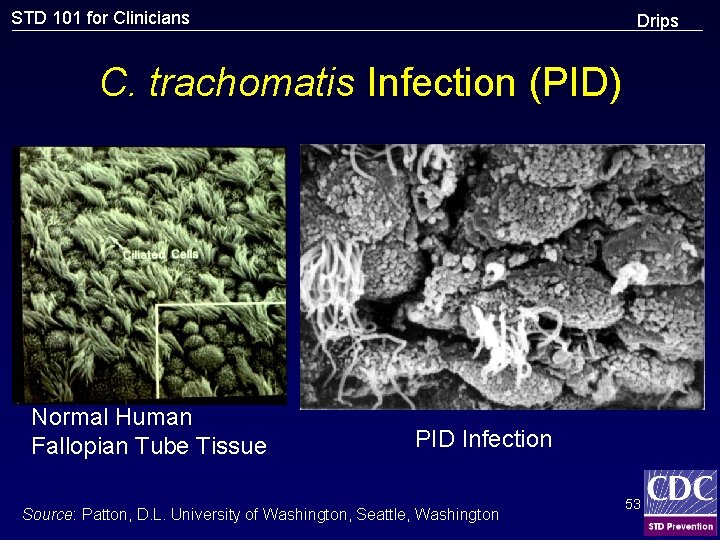
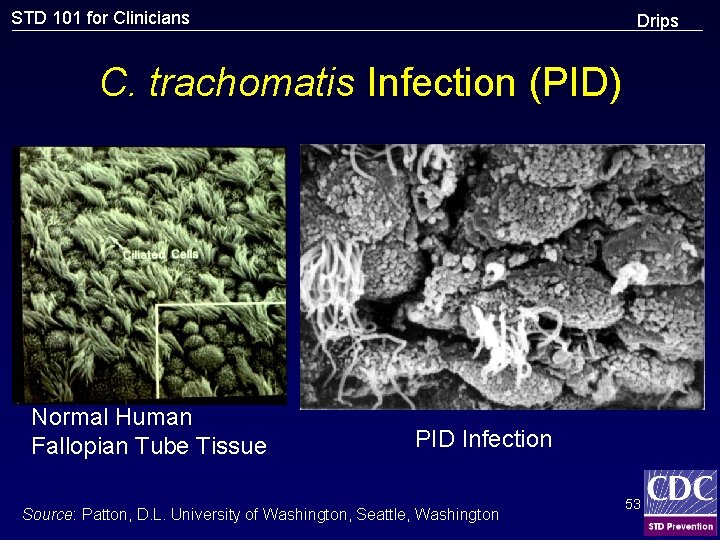
STD 101 for Clinicians Drips C. trachomatis Infection (PID) Normal Human Fallopian Tube Tissue PID Infection Source: Patton, D. L. University of Washington, Seattle, Washington 53
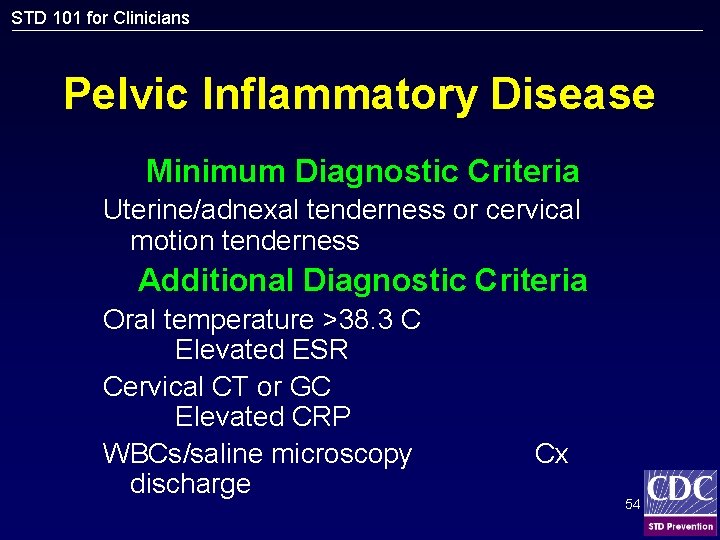
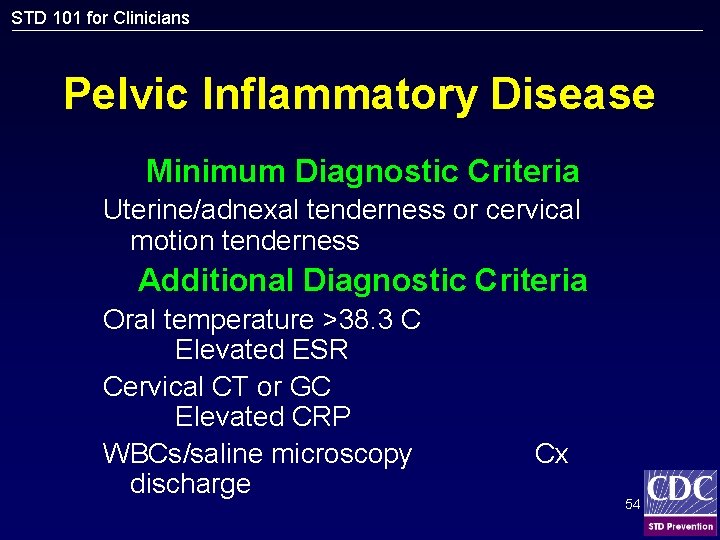
STD 101 for Clinicians Pelvic Inflammatory Disease Minimum Diagnostic Criteria Uterine/adnexal tenderness or cervical motion tenderness Additional Diagnostic Criteria Oral temperature >38. 3 C Elevated ESR Cervical CT or GC Elevated CRP WBCs/saline microscopy discharge Cx 54
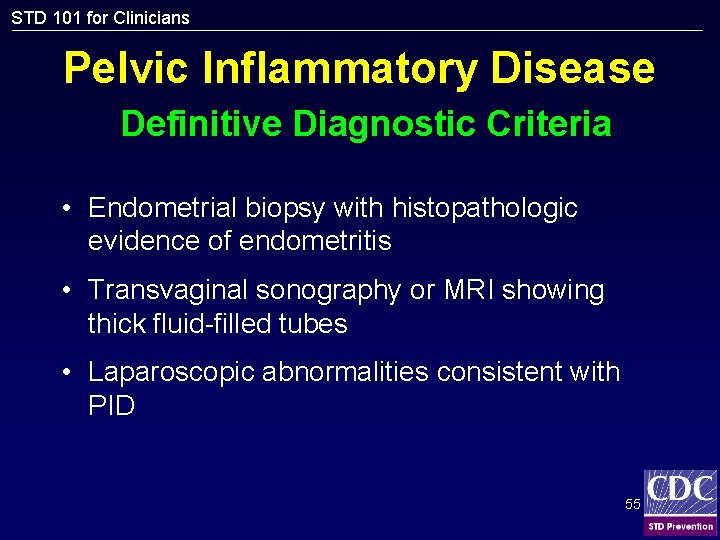
STD 101 for Clinicians Pelvic Inflammatory Disease Definitive Diagnostic Criteria • Endometrial biopsy with histopathologic evidence of endometritis • Transvaginal sonography or MRI showing thick fluid-filled tubes • Laparoscopic abnormalities consistent with PID 55
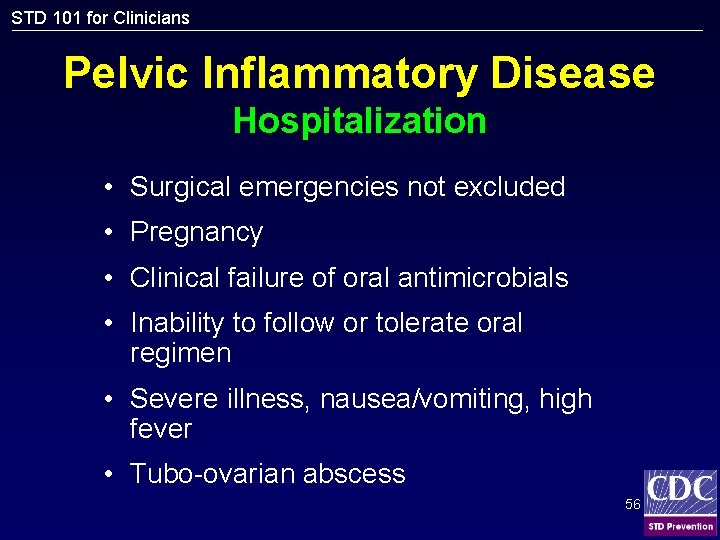
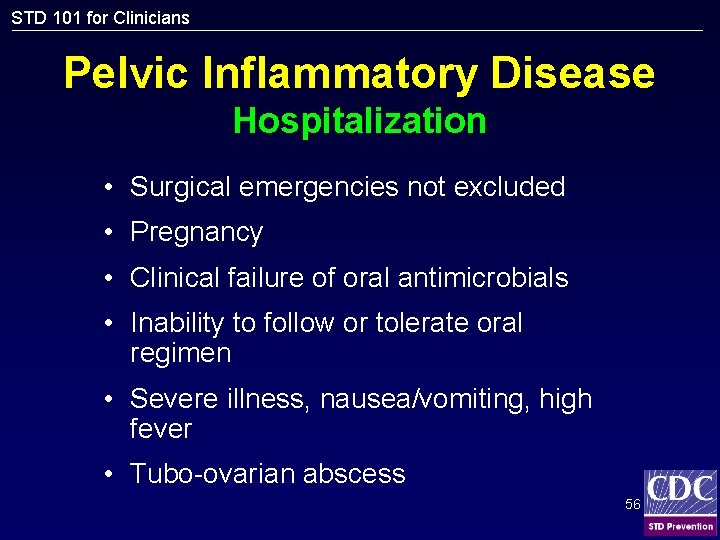
STD 101 for Clinicians Pelvic Inflammatory Disease Hospitalization • Surgical emergencies not excluded • Pregnancy • Clinical failure of oral antimicrobials • Inability to follow or tolerate oral regimen • Severe illness, nausea/vomiting, high fever • Tubo-ovarian abscess 56
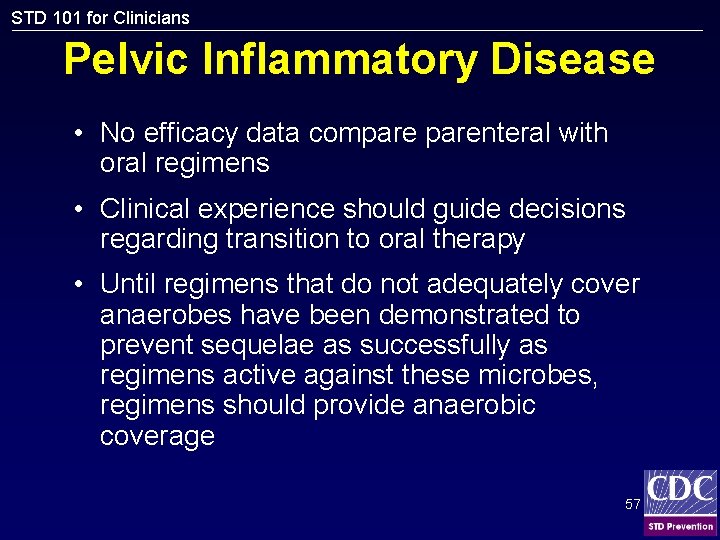
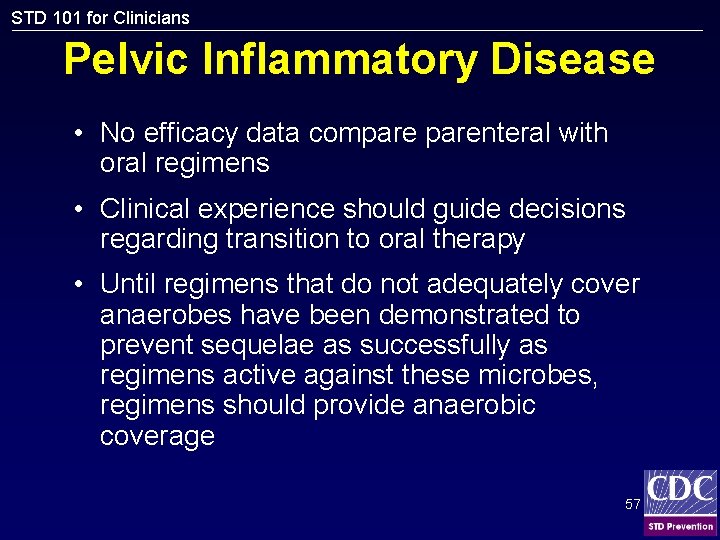
STD 101 for Clinicians Pelvic Inflammatory Disease • No efficacy data comparenteral with oral regimens • Clinical experience should guide decisions regarding transition to oral therapy • Until regimens that do not adequately cover anaerobes have been demonstrated to prevent sequelae as successfully as regimens active against these microbes, regimens should provide anaerobic coverage 57
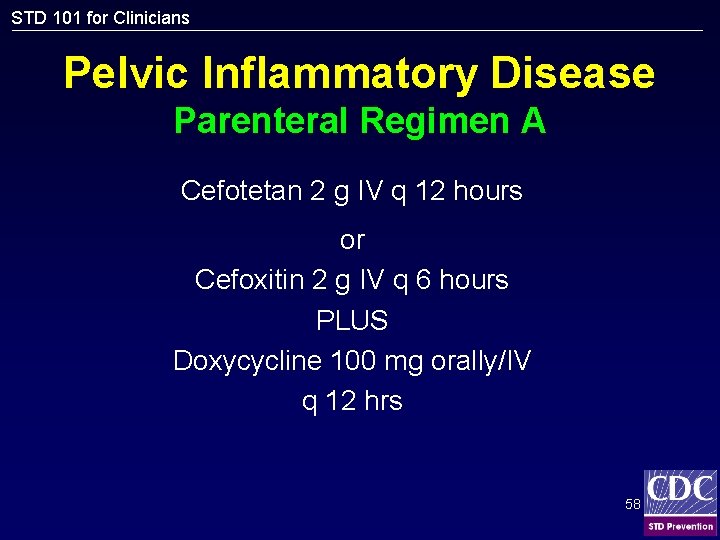
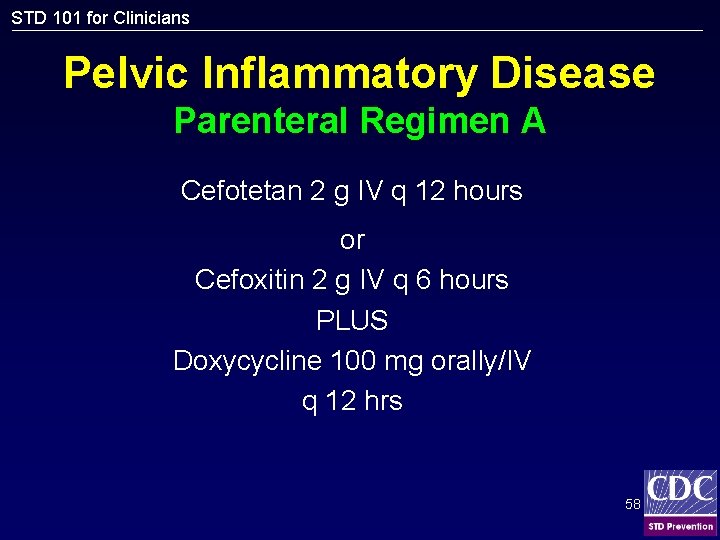
STD 101 for Clinicians Pelvic Inflammatory Disease Parenteral Regimen A Cefotetan 2 g IV q 12 hours or Cefoxitin 2 g IV q 6 hours PLUS Doxycycline 100 mg orally/IV q 12 hrs 58
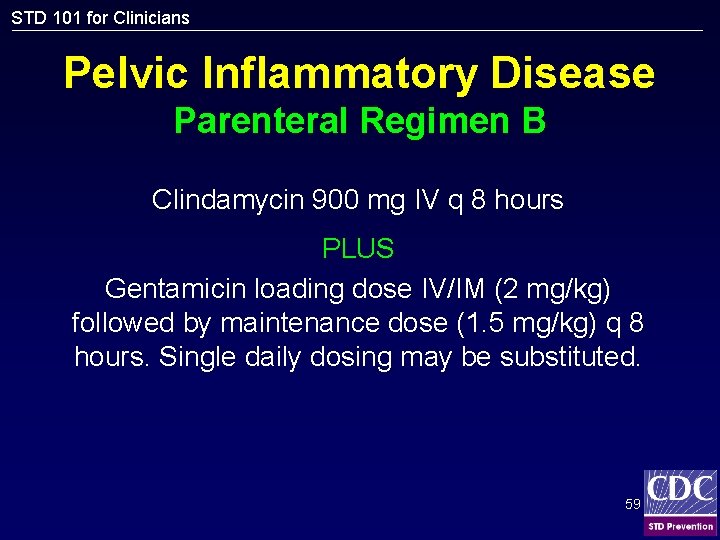
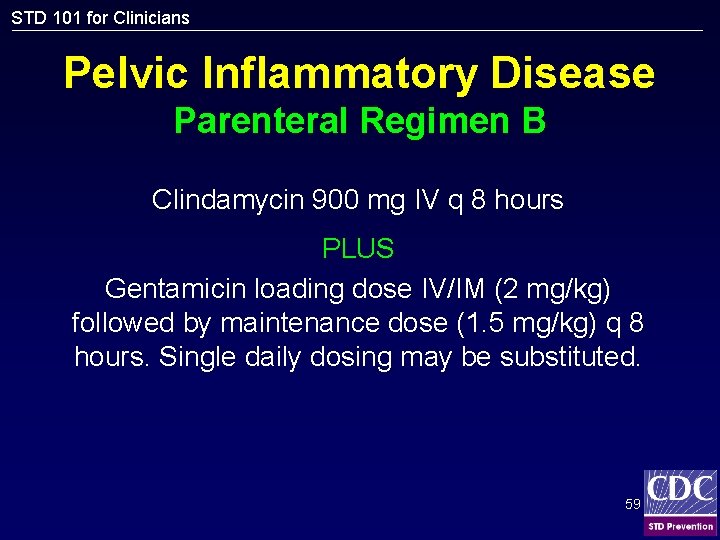
STD 101 for Clinicians Pelvic Inflammatory Disease Parenteral Regimen B Clindamycin 900 mg IV q 8 hours PLUS Gentamicin loading dose IV/IM (2 mg/kg) followed by maintenance dose (1. 5 mg/kg) q 8 hours. Single daily dosing may be substituted. 59
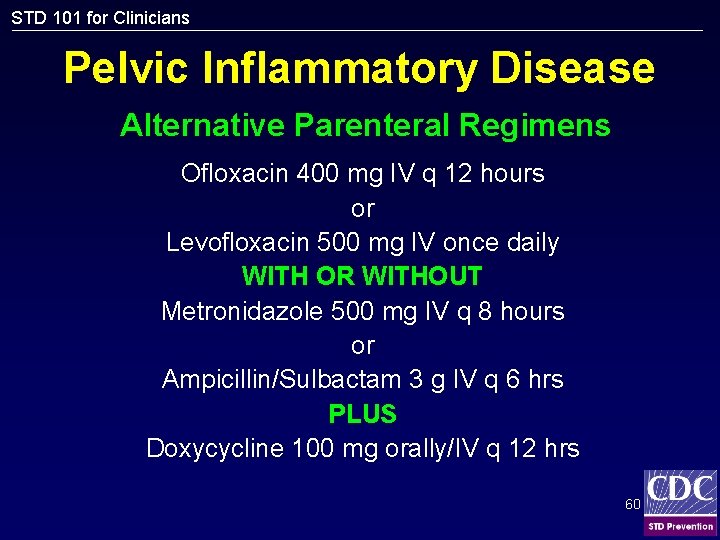
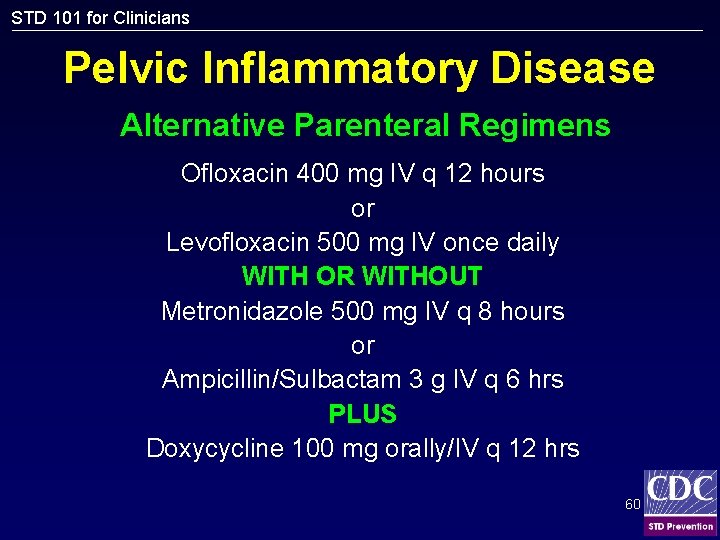
STD 101 for Clinicians Pelvic Inflammatory Disease Alternative Parenteral Regimens Ofloxacin 400 mg IV q 12 hours or Levofloxacin 500 mg IV once daily WITH OR WITHOUT Metronidazole 500 mg IV q 8 hours or Ampicillin/Sulbactam 3 g IV q 6 hrs PLUS Doxycycline 100 mg orally/IV q 12 hrs 60
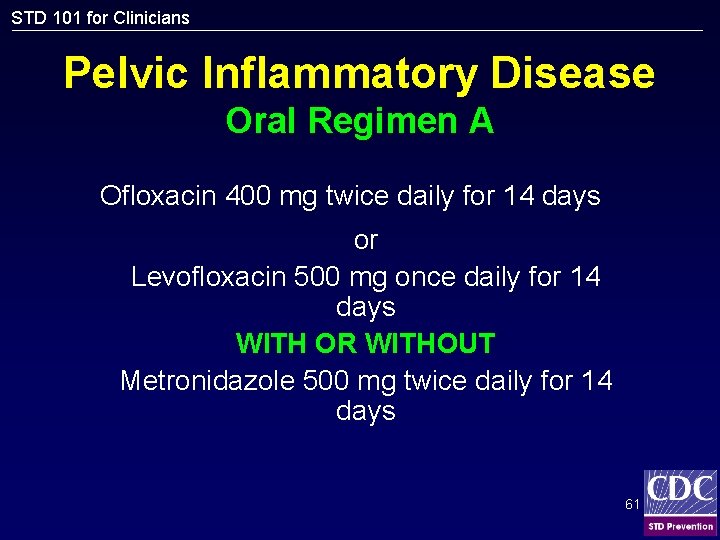
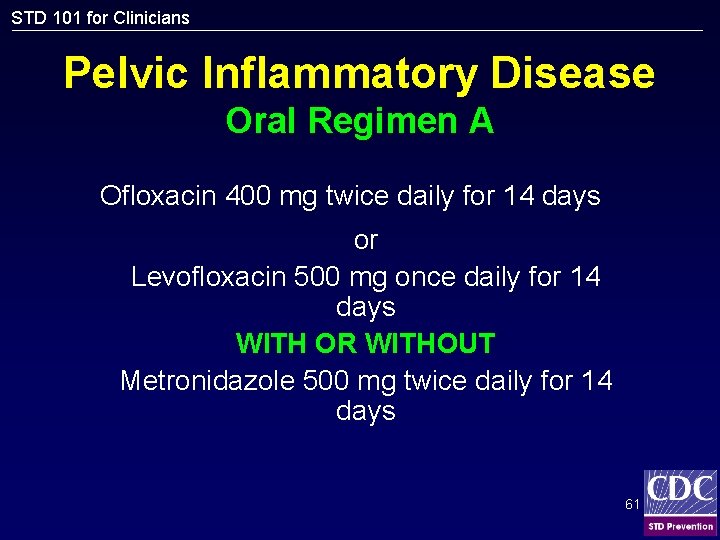
STD 101 for Clinicians Pelvic Inflammatory Disease Oral Regimen A Ofloxacin 400 mg twice daily for 14 days or Levofloxacin 500 mg once daily for 14 days WITH OR WITHOUT Metronidazole 500 mg twice daily for 14 days 61
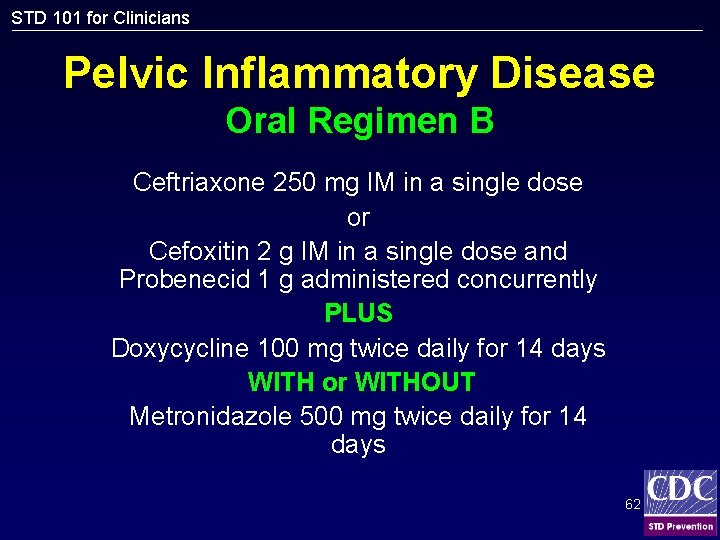
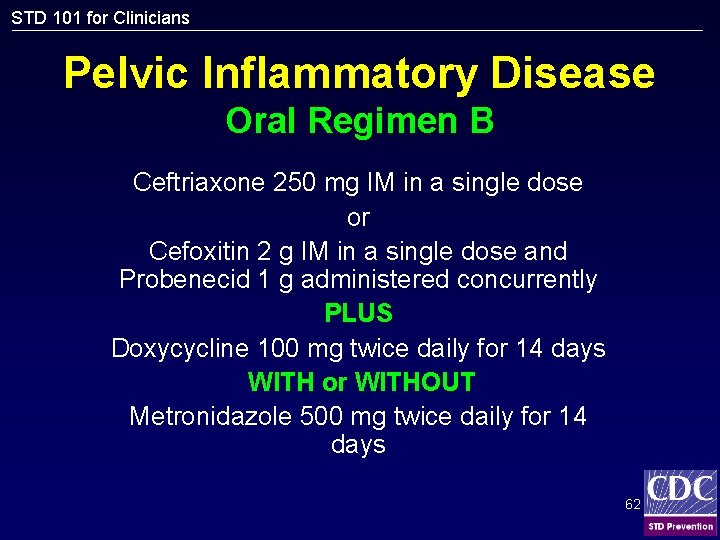
STD 101 for Clinicians Pelvic Inflammatory Disease Oral Regimen B Ceftriaxone 250 mg IM in a single dose or Cefoxitin 2 g IM in a single dose and Probenecid 1 g administered concurrently PLUS Doxycycline 100 mg twice daily for 14 days WITH or WITHOUT Metronidazole 500 mg twice daily for 14 days 62
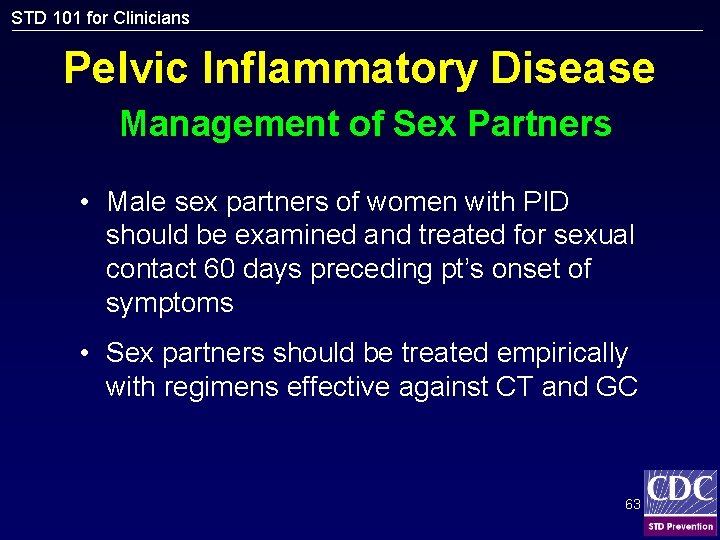
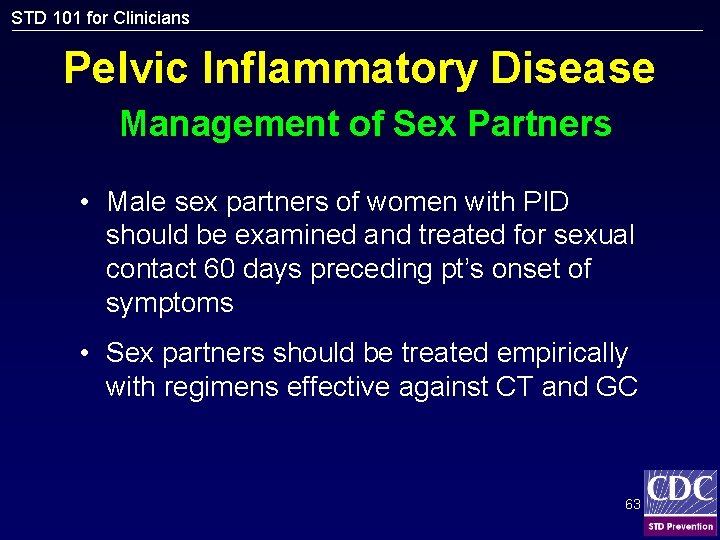
STD 101 for Clinicians Pelvic Inflammatory Disease Management of Sex Partners • Male sex partners of women with PID should be examined and treated for sexual contact 60 days preceding pt’s onset of symptoms • Sex partners should be treated empirically with regimens effective against CT and GC 63