Smallpox l Most devastating infectious disease in history



- Slides: 70
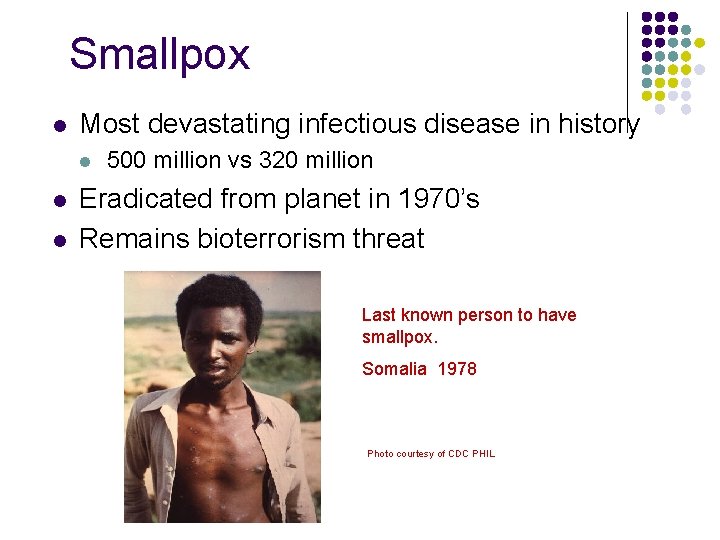
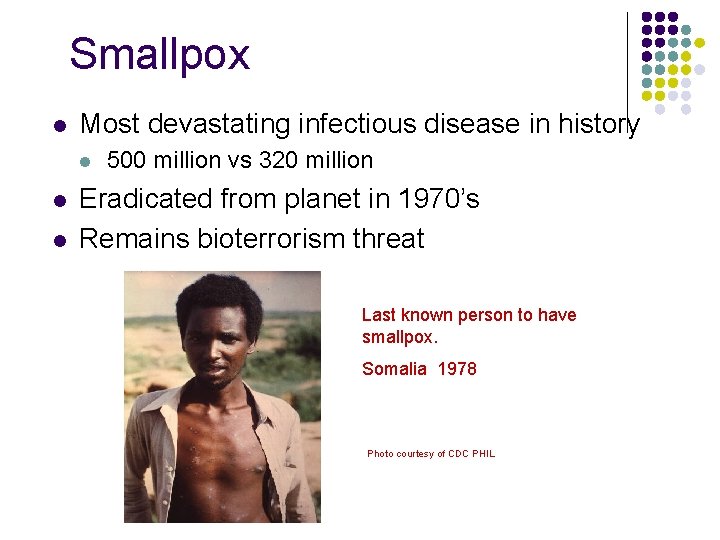
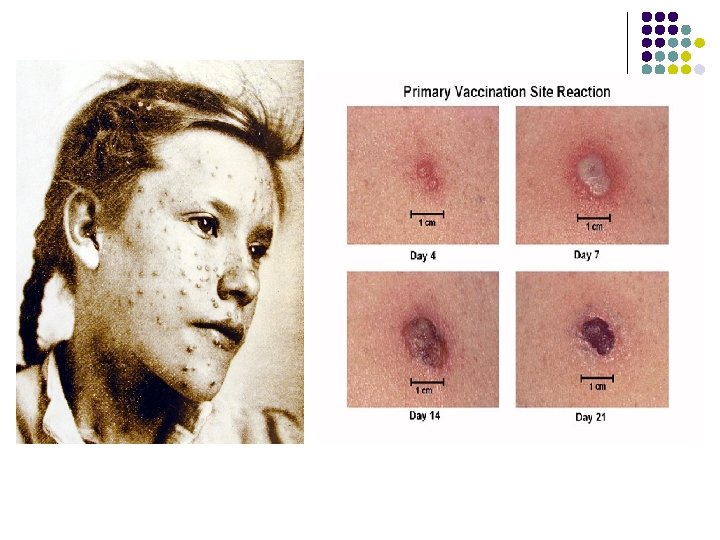
Smallpox l Most devastating infectious disease in history l l l 500 million vs 320 million Eradicated from planet in 1970’s Remains bioterrorism threat Last known person to have smallpox. Somalia 1978 Photo courtesy of CDC PHIL
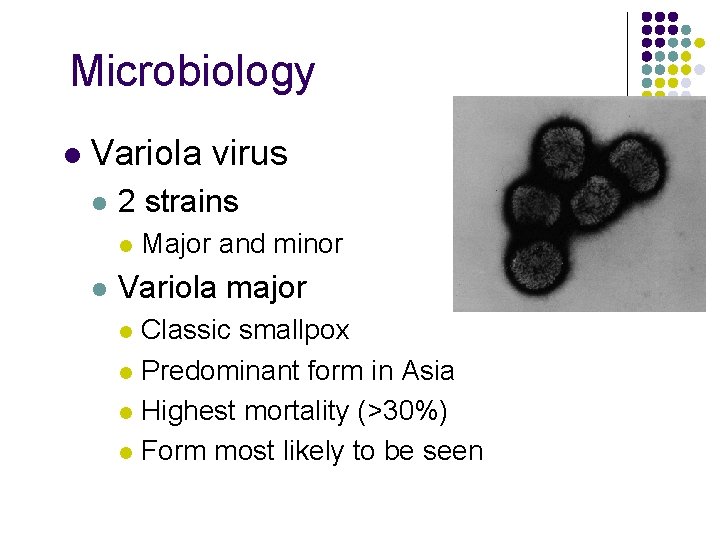
Microbiology l Variola virus l 2 strains l l Major and minor Variola major Classic smallpox l Predominant form in Asia l Highest mortality (>30%) l Form most likely to be seen l
Microbiology l Variola minor l Milder disease l Less morbidity/mortality (< 1%) Less severe prodrome and rash l Predominant form in N. America l
Diagnosis Base on signs and symptoms l Notify Local Health Department l l Suspicious cases
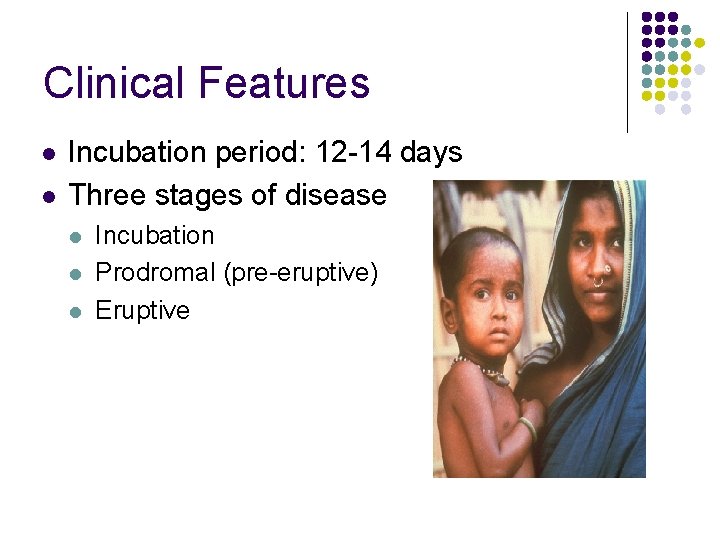
Clinical Features l l Incubation period: 12 -14 days Three stages of disease l l l Incubation Prodromal (pre-eruptive) Eruptive Photo courtesy of CDC PHIL
Clinical Features l Prodromal Stage l Common symptoms l l Occasional symptoms l l High fever, prostration, low back myalgias, HA Vomiting, abdominal pain, delirium Duration typically 3 -5 days l l Mucosal lesions appear at end of prodromal stage Onset of infectiousness
Clinical Features l Eruptive Stage (Rash) l Characteristic rash Centrifugal (in order of appearance & severity) l Lesions all in same stage of maturation l Initially oral mucosa l Head, face l Forearms, hands, palms l Legs, soles, +/- trunk l
Complications l l Disfiguring pock marks Encephalitis Secondary bacterial infections Conjunctivitis or blindness
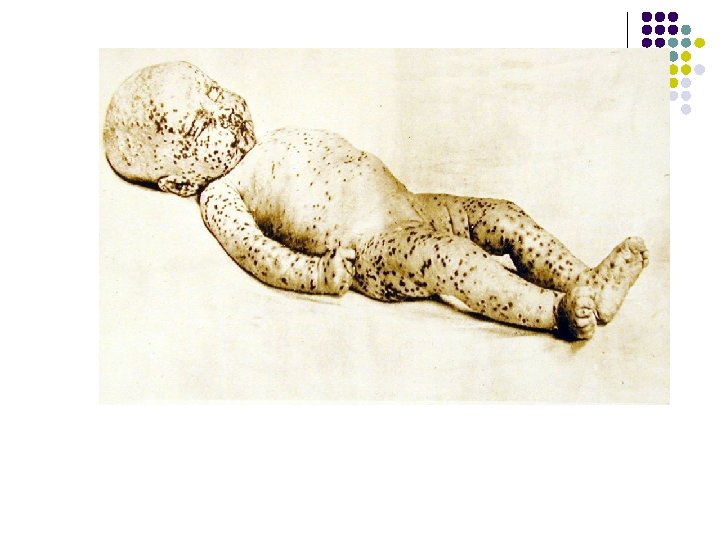
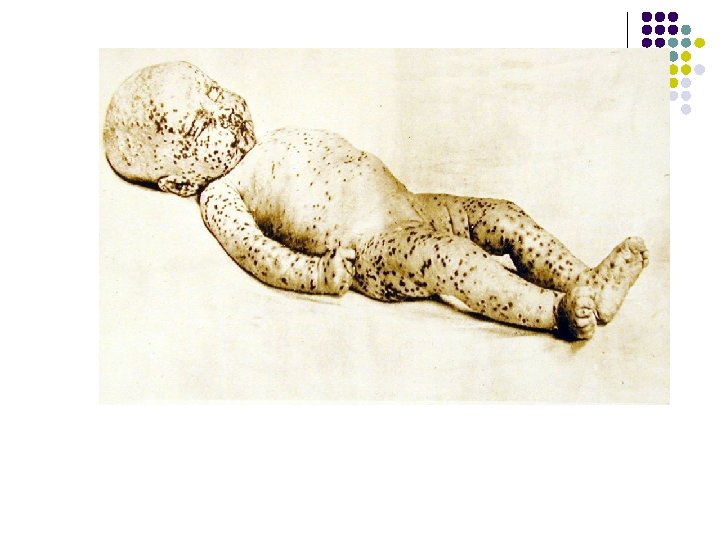
Classic Centrifugal Rash of Smallpox Involving Face and Extremities, Photo courtesy of National Archives Including the Soles.
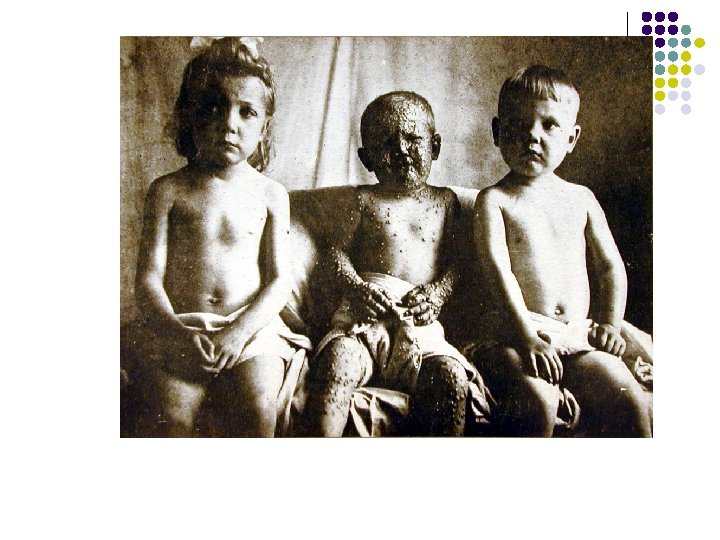
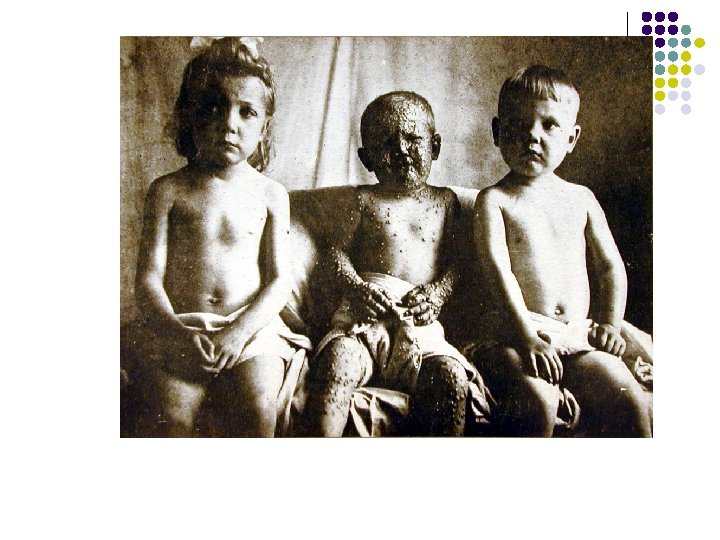
Classic Centrifugal Rash of Smallpox Involving Face and Extremities. Photo courtesy of National Archives
Classic Smallpox Rash, Demonstrating Same Development Stage (Pustular) of All Lesions in a Region Photo courtesy of National Archives
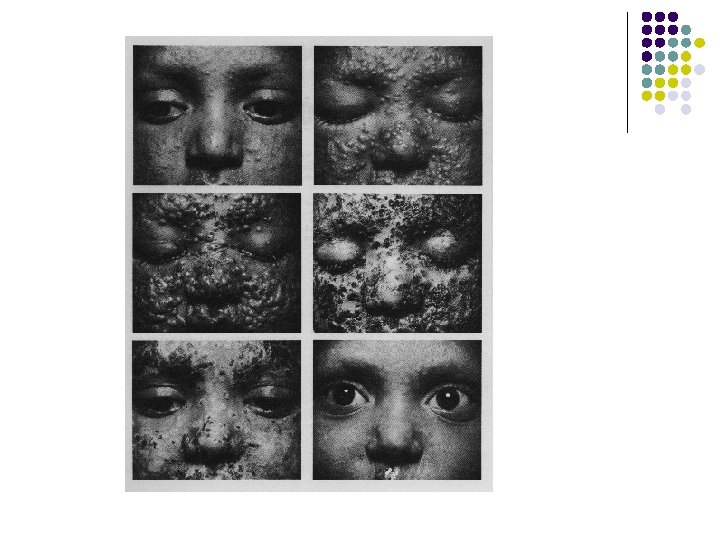
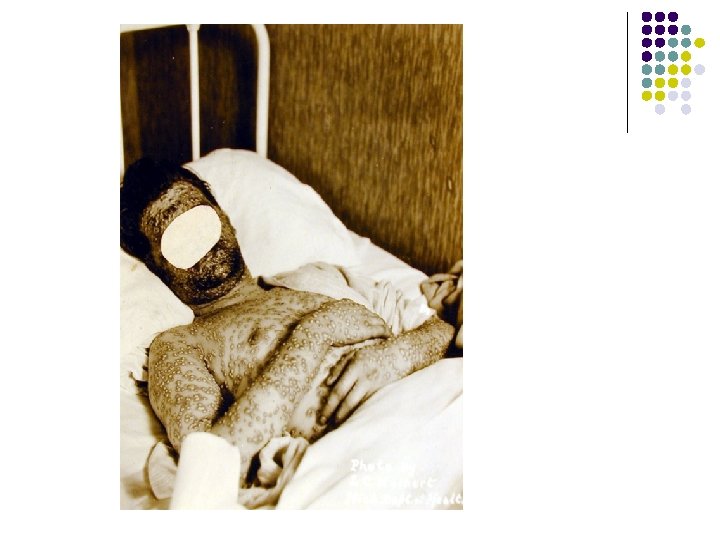
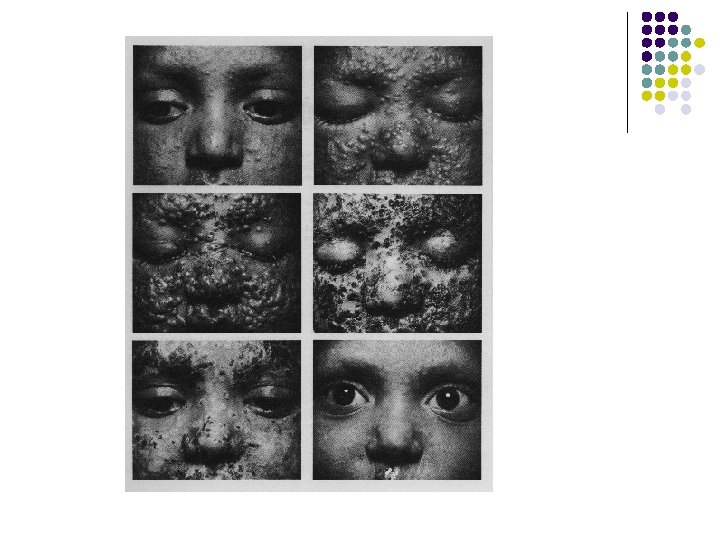
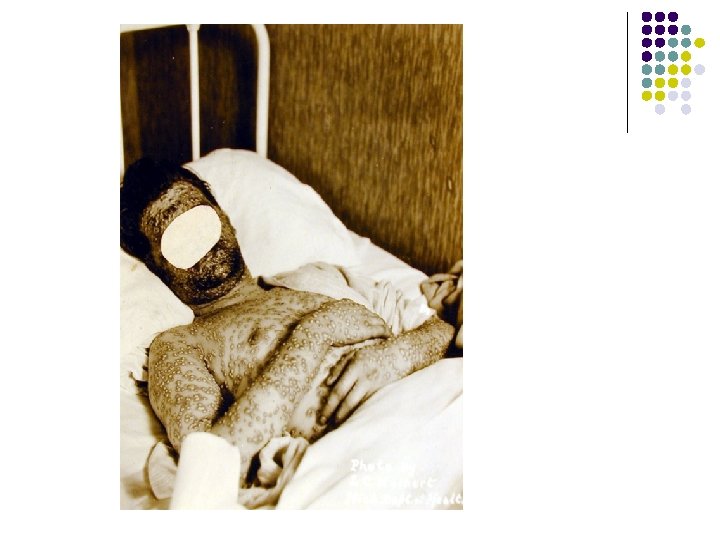
Progression of Smallpox Lesions in Semiconfluent Case Patient Who Survived. Demonstrates Vesicles, Pustules, Scabs Then Scars.
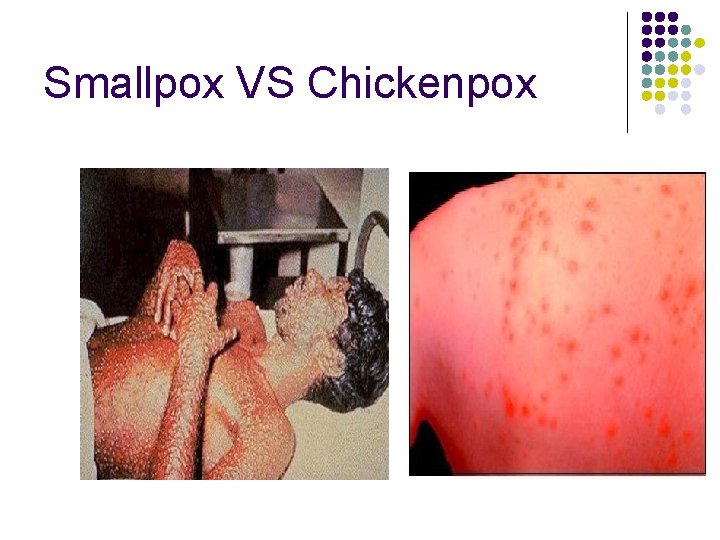
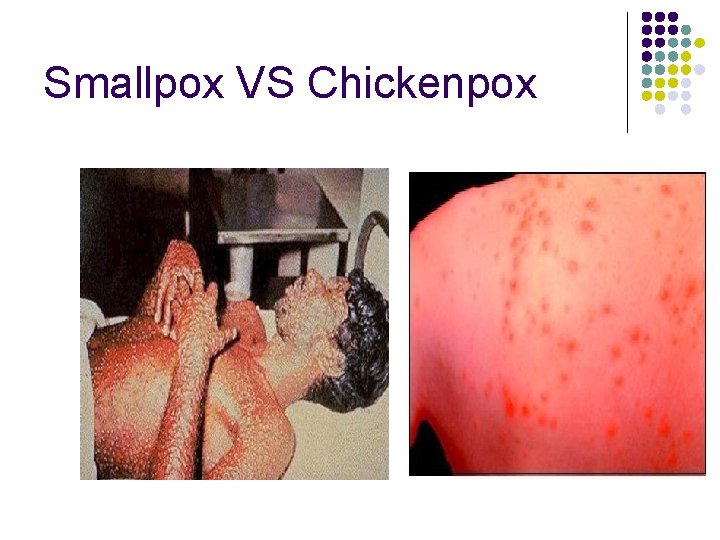
Smallpox VS Chickenpox Photo courtesy of CDC PHIL
Infection Control l Highly infectious l l Droplet, aerosol or clothing Transmission slower and less likely than with measles or chickenpox Attack rate 25 -40% 3 -4 secondary cases/primary case Photo courtesy of National Library of Medicine and WHO l 10– 20 not uncommon
Infection Control l Airborne and Contact Precautions l l l Monitor contacts 17 days l l Negative pressure or HEPA-filtered room N-95 mask Gown and gloves D/C when all scabs separate Isolate febrile contacts Home isolation Photo courtesy of National Library of Medicine
Infection Control l Disposal of linens/laundry l l Dispose in biohazard containers Autoclave before laundering Launder in hot water & bleach Cremation recommended for casualties
Treatment l l No known antiviral tx Offer supportive therapy l l l Electrolyte and volume repletion Hemodynamic support o known antiviral tx AB’s for bacterial infections Photo courtesy of National Archives
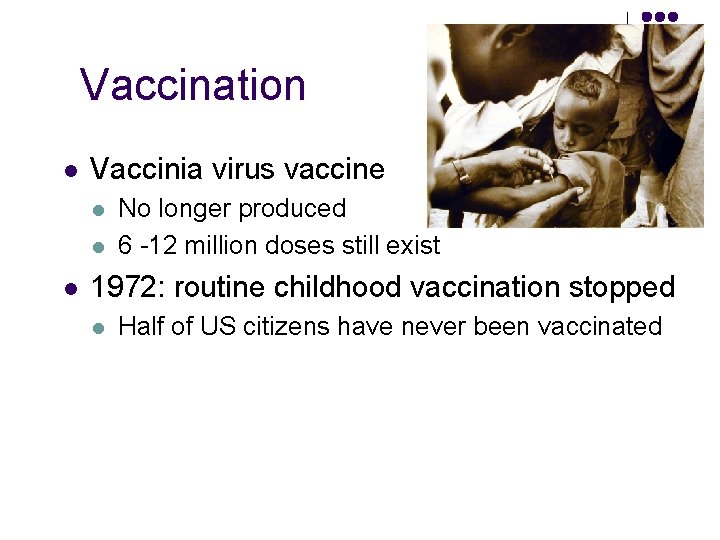
Vaccination l Vaccinia virus vaccine l l l No longer produced 6 -12 million doses still exist Photo courtesy of National Archives 1972: routine childhood vaccination stopped l Half of US citizens have never been vaccinated
Vaccination l Immunity lasts 3 -5 years: l l l Partial immunity Booster Prior infection = lifelong immunity
Adverse Reactions Related to Vaccination l Adverse reactions l l l Generalized vaccinia Encephalitis Give VIG to high risk groups l l Immunocompromised Eczema or chronic skin disorder Children < 1 yr old Pregnant women
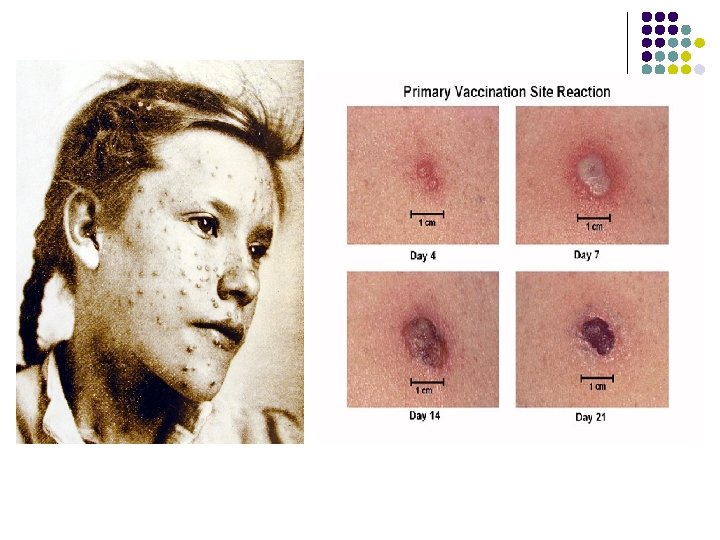
Photo courtesy of National Archives Photo courtesy of CDC

Photo courtesy of CDC
Post Exposure Prophylaxis l Exposure l l Inhalation during initial release, household or face to face contact, or direct contact with contaminated linens or lab specimens from known case Vaccination l l Within 3 -5 days of exposure All household or close contacts, hospital employees, hospitalized patients (at the same time as the infected patient), lab employees and mortuary employees
Decontamination l l Virus inactivated within 2 days Buildings l l Not needed Standard hospital disinfectants l Photo courtesy of National Archives Bleach also effective, but should only be used if you run out of standard disinfectants

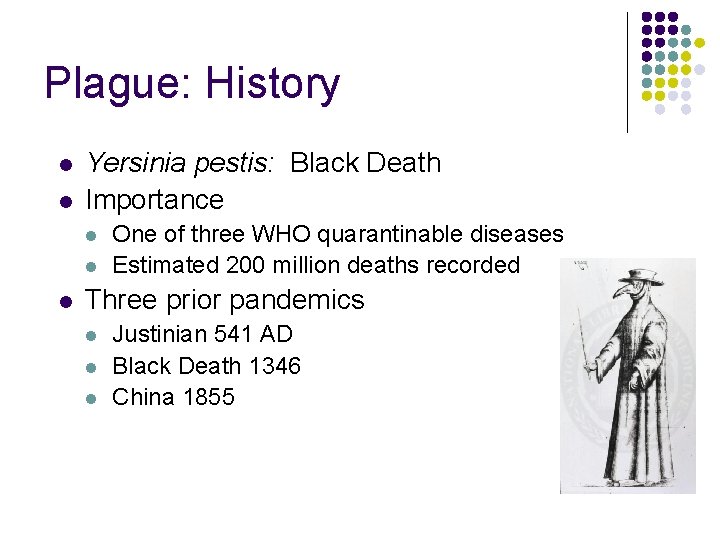
Plague: History l l Yersinia pestis: Black Death Importance l l l One of three WHO quarantinable diseases Estimated 200 million deaths recorded Three prior pandemics l l l Justinian 541 AD Black Death 1346 China 1855 Plague Doctor wearing protective clothing Image: National Library of Medicine
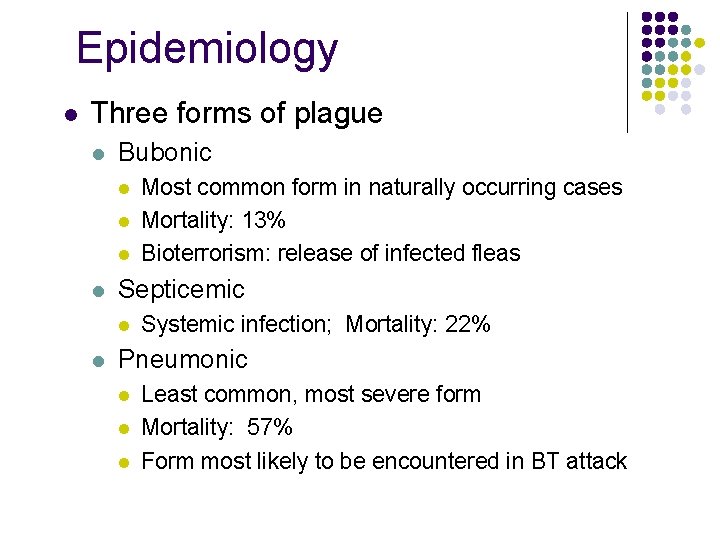
Epidemiology l Three forms of plague l Bubonic l l Septicemic l l Most common form in naturally occurring cases Mortality: 13% Bioterrorism: release of infected fleas Systemic infection; Mortality: 22% Pneumonic l l l Least common, most severe form Mortality: 57% Form most likely to be encountered in BT attack
When to Suspect Bioterrorism Attack Using Plague l Report suspected intentional release: l l l Human cases occur in non-endemic areas Cases occur in persons without risk factors Human cases occur in the absence of rodent cases
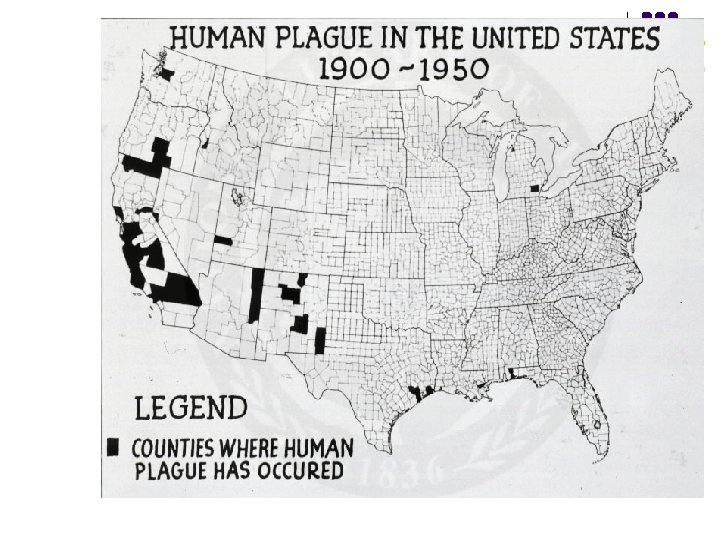
Photo courtesy of National Library of Medicine
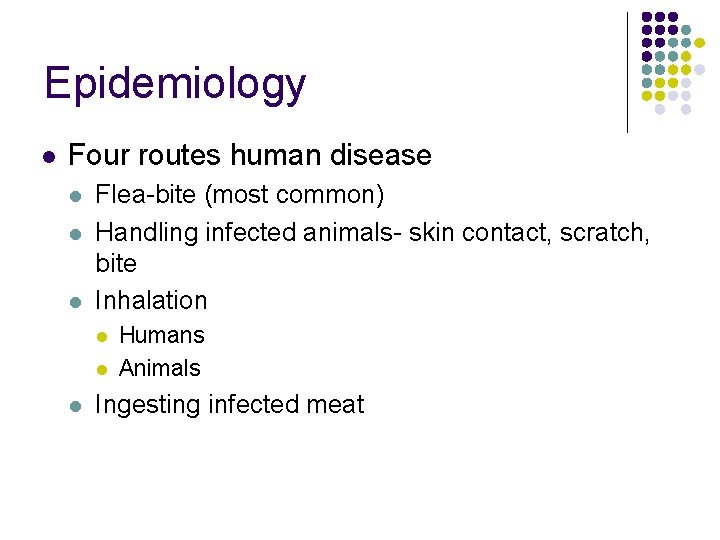
Epidemiology l Four routes human disease l l l Flea-bite (most common) Handling infected animals- skin contact, scratch, bite Inhalation l l l Humans Animals Ingesting infected meat
Plague l Early diagnosis essential l l Presumptive diagnosis l l Without treatment, death within 2 -3 days Symptoms; obtain culture specimens and send to reference lab Definitive diagnosis l Positive blood, sputum or bubo aspirate culture
Clinical Features l l Incubation period: 2 -4 days Early symptoms l Flu-like symptoms l l l Fever Chills Body aches Weakness WBC’s Headache
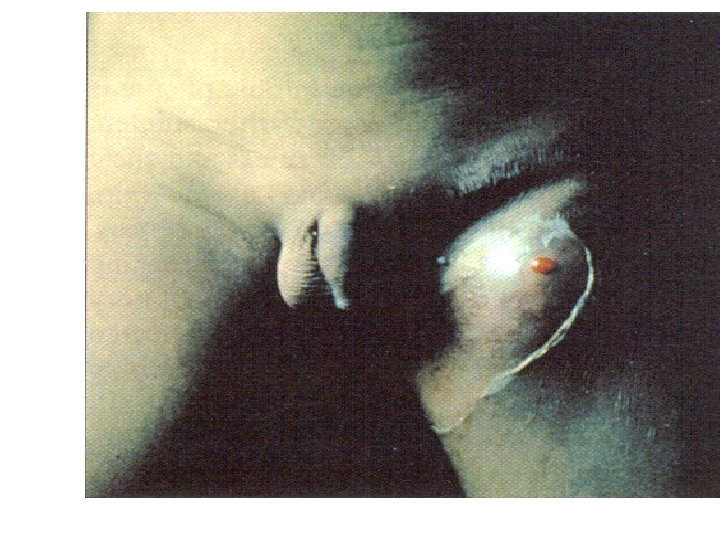
Clinical Features l Bubonic l Buboes l Enlarged tender lymph nodes l Usually unilateral l Usually inguinal/femoral in adults l Cervical/submaxillary more common in age < 10
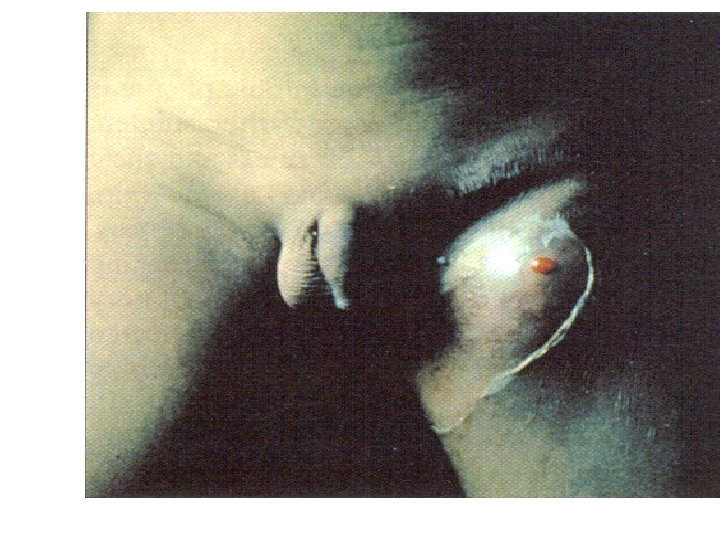
Image: Armstrong & Cohen
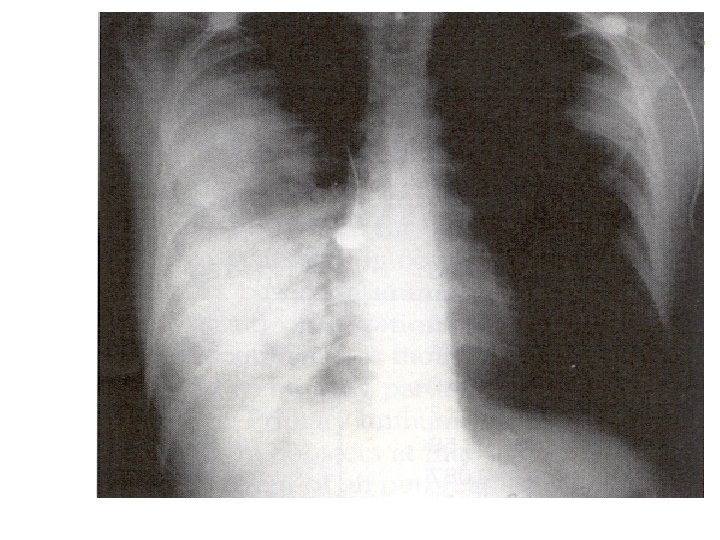
Clinical Features l Pnuemonic l Primary l l Inhalation Secondary (bubonic) l Spread to lungs § l Presents like typical pneumonia l l l Interstitial pattern initially CXR: usually patchy bilateral infiltrates, consolidation Hemoptysis Mortality nearly 100%
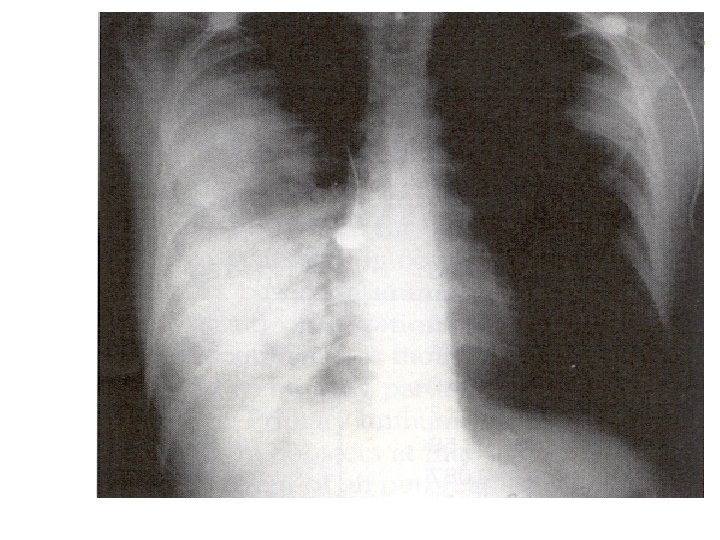
Image: Armstrong & Cohen
Infection Control l Bubonic or Septicemic: l l Standard precautions Contact precautions l l If bubo is draining Pneumonic plague: l l Droplet isolation (D/C 48 hours) Do not discontinue isolation until patient is clinically improving l Antibiotic resistant strain is possible
Infection Control l All forms of plague: l Avoid surgery or other aerosol-generating procedures (including autopsies) l Wear N-95 masks and perform procedure in negative pressure room
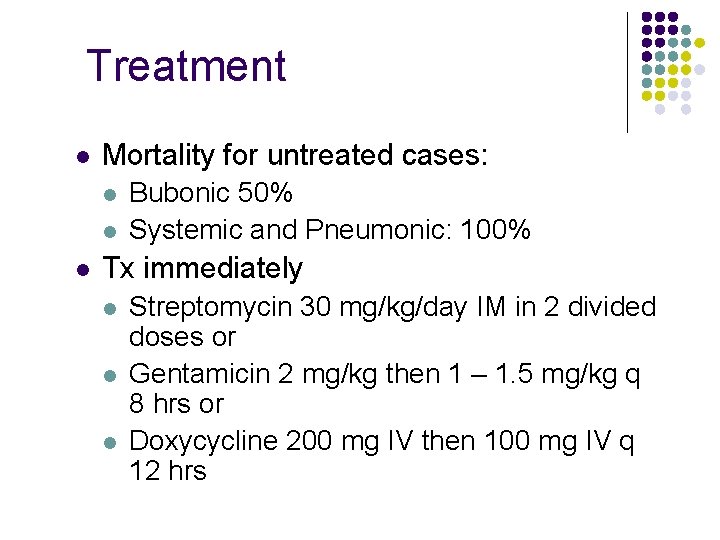
Treatment l Mortality for untreated cases: l l l Bubonic 50% Systemic and Pneumonic: 100% Tx immediately l l l Streptomycin 30 mg/kg/day IM in 2 divided doses or Gentamicin 2 mg/kg then 1 – 1. 5 mg/kg q 8 hrs or Doxycycline 200 mg IV then 100 mg IV q 12 hrs
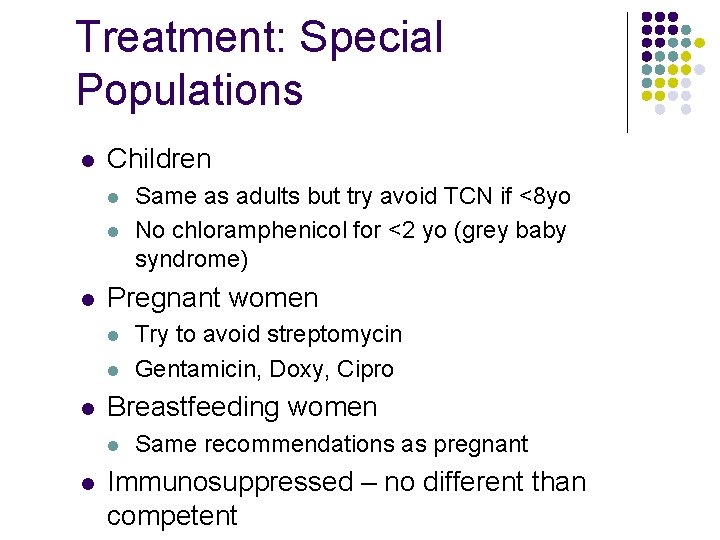
Treatment: Special Populations l Children l l l Pregnant women l l l Try to avoid streptomycin Gentamicin, Doxy, Cipro Breastfeeding women l l Same as adults but try avoid TCN if <8 yo No chloramphenicol for <2 yo (grey baby syndrome) Same recommendations as pregnant Immunosuppressed – no different than competent
Vaccination l Bubonic plague vaccine no longer available l No vaccine against pneumonic plague
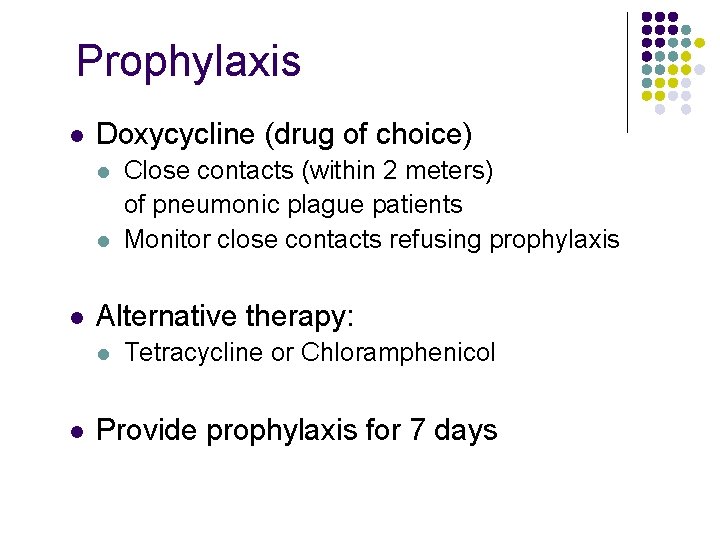
Prophylaxis l Doxycycline (drug of choice) l l l Alternative therapy: l l Close contacts (within 2 meters) of pneumonic plague patients Monitor close contacts refusing prophylaxis Tetracycline or Chloramphenicol Provide prophylaxis for 7 days
Decontamination l l Viable for only 1 hr as an aerosol Sunlight, heat or lack of host kills bacteria Environmental decontamination unnecessary Standard hospital-approved disinfectants

What is cholera? l l l Intestinal infection Severe diarrhea Caused by cholera toxin of bacterium, Vibrio cholera
V. cholerae l l l Grows in salt and fresh water Can survive and multiply in brackish water by infecting copepods Has over 150 identified serotypes based on Oantigen Only O 1 and O 139 are toxigenic and cause Cholera disease 2 categories of O 1 serotypes – Classical and El Tor
Cholera l l A life-threatening secretory diarrhea induced by enterotoxin secreted by V. cholerae Water-borne illness caused by ingesting water/food contaminated by copepods infected by V. cholerae An enterotoxic enteropathy (a non-invasive diarrheal disease) A major epidemic disease
V. cholerae l l l Transmitted by fecal-oral route Endemic in areas of poor sanitation (India and Bangladesh ) May persist in shellfish or plankton 7 pandemics since 1817 – first 6 from Classical strains, 7 th from El Tor 1993: Cholera in Bengal caused by O 139 – may be cause of 8 th pandemic
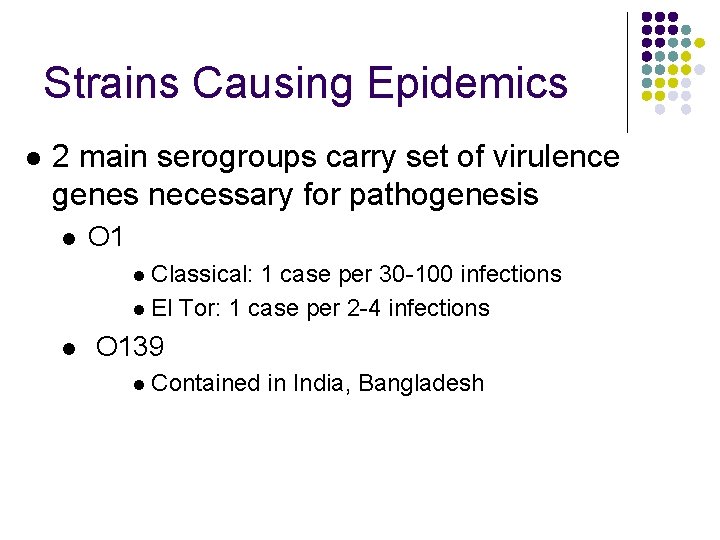
Strains Causing Epidemics l 2 main serogroups carry set of virulence genes necessary for pathogenesis l O 1 l Classical: 1 case per 30 -100 infections l El Tor: 1 case per 2 -4 infections l O 139 l Contained in India, Bangladesh
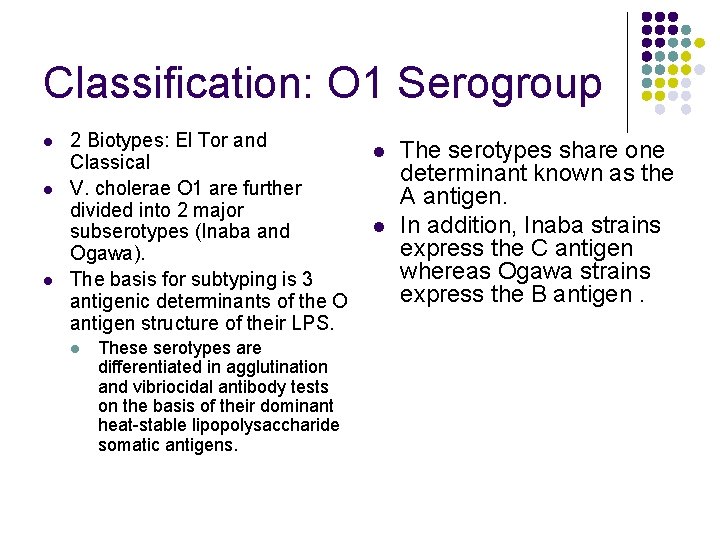
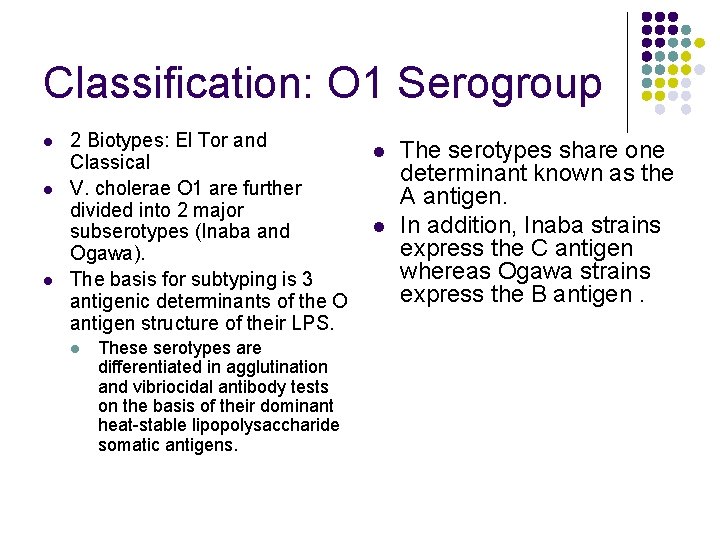
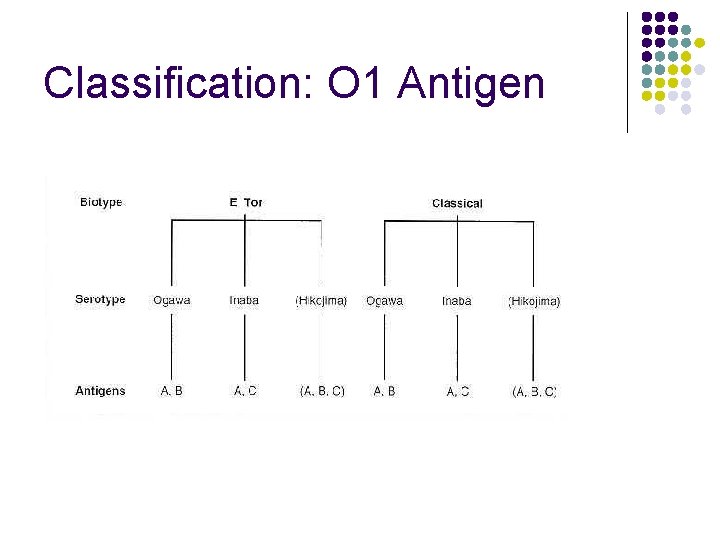
Classification: O 1 Serogroup l l l 2 Biotypes: El Tor and l Classical V. cholerae O 1 are further divided into 2 major l subserotypes (Inaba and Ogawa). The basis for subtyping is 3 antigenic determinants of the O antigen structure of their LPS. l These serotypes are differentiated in agglutination and vibriocidal antibody tests on the basis of their dominant heat-stable lipopolysaccharide somatic antigens. The serotypes share one determinant known as the A antigen. In addition, Inaba strains express the C antigen whereas Ogawa strains express the B antigen.
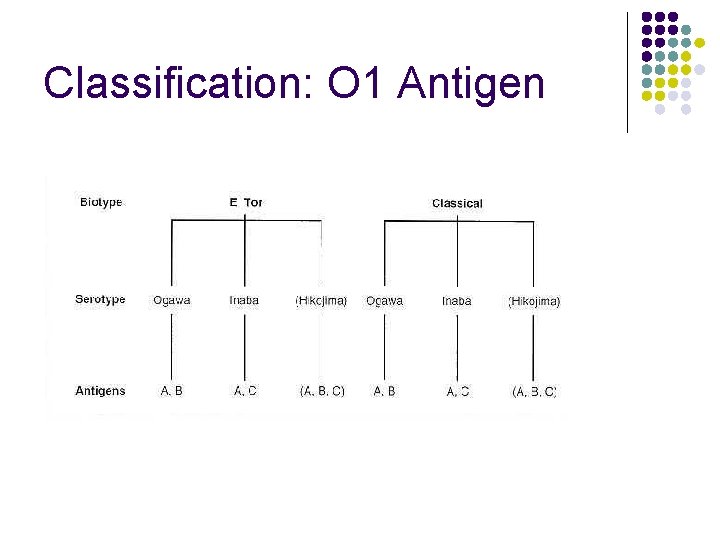
Classification: O 1 Antigen
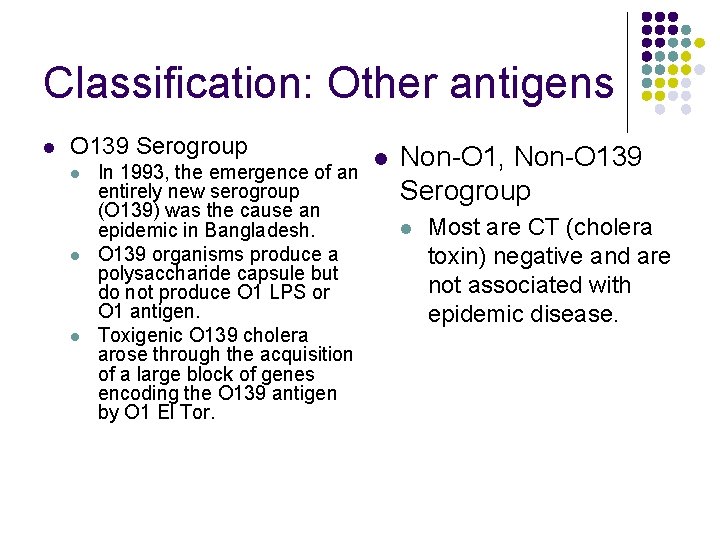
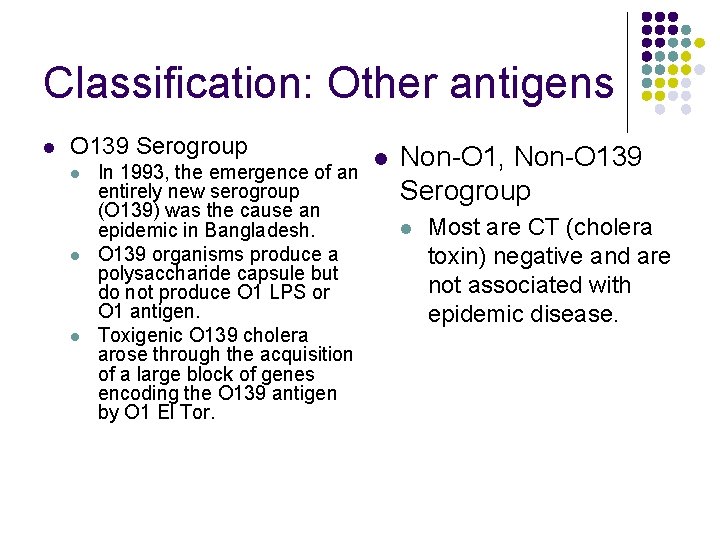
Classification: Other antigens l O 139 Serogroup l l l In 1993, the emergence of an entirely new serogroup (O 139) was the cause an epidemic in Bangladesh. O 139 organisms produce a polysaccharide capsule but do not produce O 1 LPS or O 1 antigen. Toxigenic O 139 cholera arose through the acquisition of a large block of genes encoding the O 139 antigen by O 1 El Tor. l Non-O 1, Non-O 139 Serogroup l Most are CT (cholera toxin) negative and are not associated with epidemic disease.
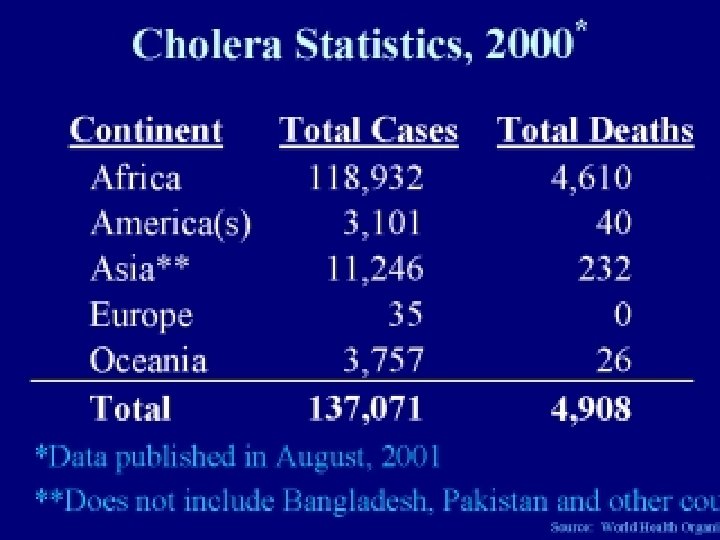
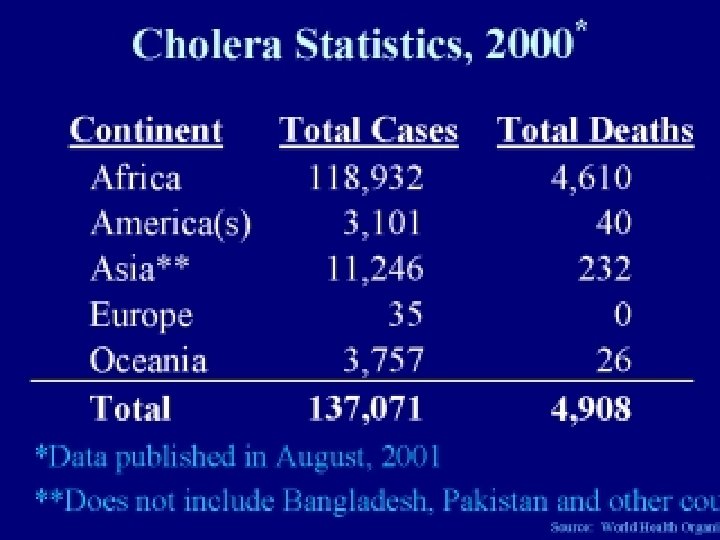
Epidemiology l l l Responsible for seven global pandemics over the past two centuries Common in India, Sub-Saharan Africa, Southern Asia Very rare in industrialized countries
Transmission l Contaminated food or water l l l Inadequate sewage treatment Lack of water treatment Improperly cooked shellfish l Transmission by casual contact unlikely
Epidemics l l l Fecal-oral transmission Feces of infected person contaminates water supply Resulting diarrhea makes it easy for bacteria to spread in unsanitary conditions
People Most at Risk l People with low gastric acid levels l Children: 10 x more susceptible than adults l Elderly l Blood types l O>> B > AB
Period of Communicability l l During acute stage A few days after recovery By end of week, 70% of patients non-infectious By end of third week, 98% non-infectious
Incubation l l l Ranges from a few hours to 5 days Average is 1 -3 days Shorter incubation period: l High gastric p. H (from use of antacids) l Consumption of high dosage of cholera
How Does Cholera Toxin Work? l l l Inactivates GTPase function of G-protein coupled receptors in intestinal cells G proteins stuck in “On” position 100 fold increase in c. AMP Activation of ion channels Ions flow out and water follows
Infectious Dose l l 106 -1011 colony-forming units Why such a high dosage? l Series of changes as moves from aquatic environment to intestine § l l Temperature, acidity Acidic environment of stomach Intestinal environment § § Bile salts, organic acids, complement inhibit bacteria growth Must penetrate mucous lining of intestinal epithelial cells
Symptoms l l Occur 2 -3 days after consumption of contaminated food/water Usually mild, or no symptoms at all l 75% asymptomatic 20% mild disease 2 -5% severe l Vomiting l Cramps Watery diarrhea (1 L/hour) Without treatment, death in 18 hours-several days l l
Cholera Gravis l l More severe symptoms Rapid loss of body fluids l l l 6 liters/hour 107 vibrios/m. L Rapidly lose more than 10% of bodyweight Dehydration and shock Death within 12 hours or less Death can occur within 2 -3 hours
Consequences of Severe Dehydration l l l Intravascular volume depletion Severe metabolic acidosis Hypokalemia Cardiac and renal failure Sunken eyes, decreased skin turgor Almost no urine production
Mortality Rate l l l Causes 120, 000 deaths/year worldwide With prompt rehydration: <1% Without treatment: 50%-60%