SCD and Therapeutic Hypothermia Ruchika Husa MD OSU



- Slides: 62
SCD and Therapeutic Hypothermia Ruchika Husa, MD OSU Wexner Medical Center
Clinical Vignette • Young female found down by coworker in the UCSD temporary office building. • No bystander CPR upon code teams arrival. • pulseless, non-responsive. 2
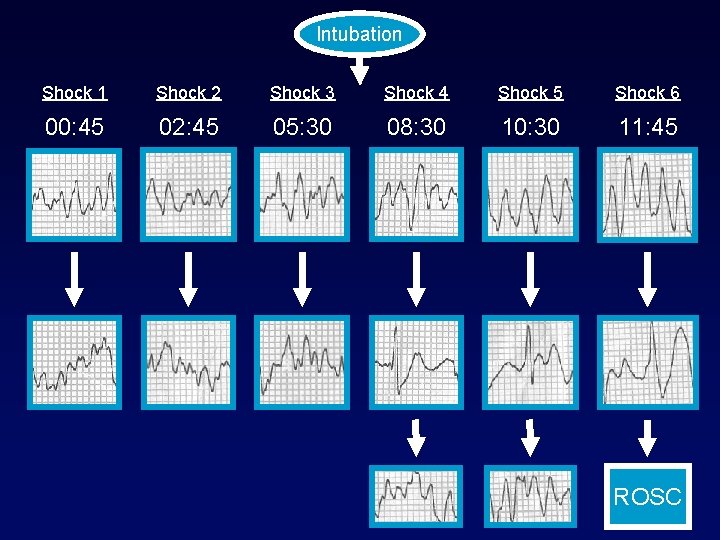
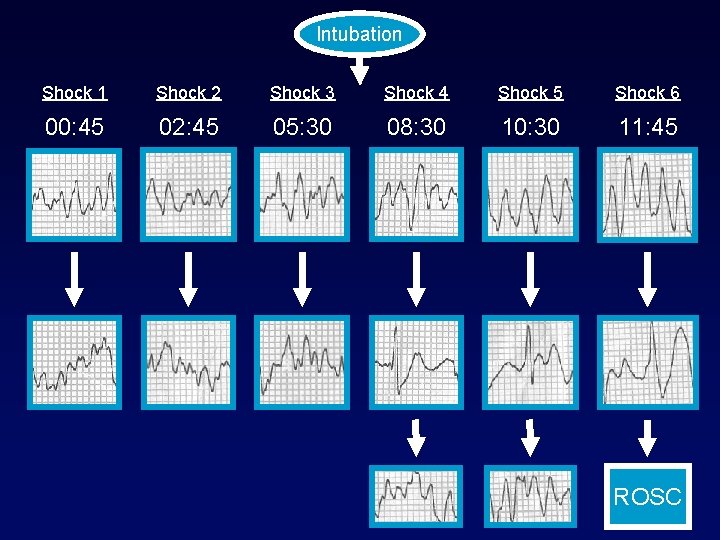
Intubation Shock 1 Shock 2 Shock 3 Shock 4 Shock 5 Shock 6 00: 45 02: 45 05: 30 08: 30 10: 30 11: 45 ROSC
Post Resuscitation • Cooled. Full neurologic recovery. • No baseline ECG abnormalities. • Cardiac MRI without anatomic abnormalities. • ICD and discharge after 12 days. 4
Objectives • Evidence behind therapeutic hypothermia • Patient selection • Methods of cooling • Timing of cooling • Degree of hypothermia • Duration of hypothermia

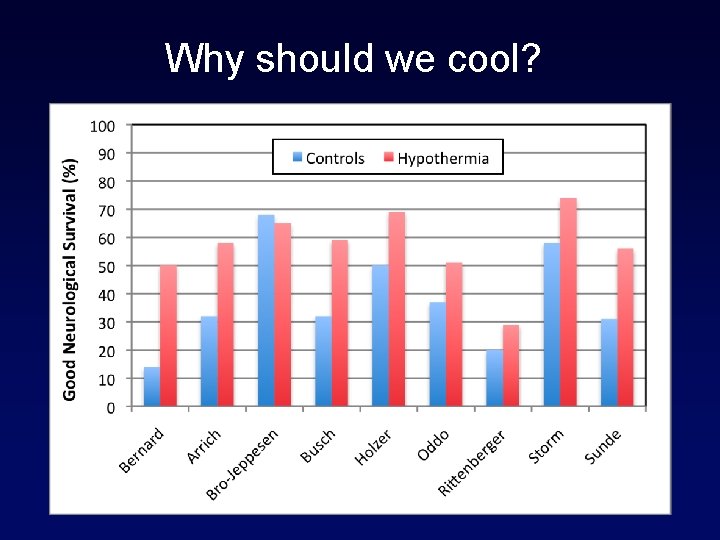
Why should we cool?
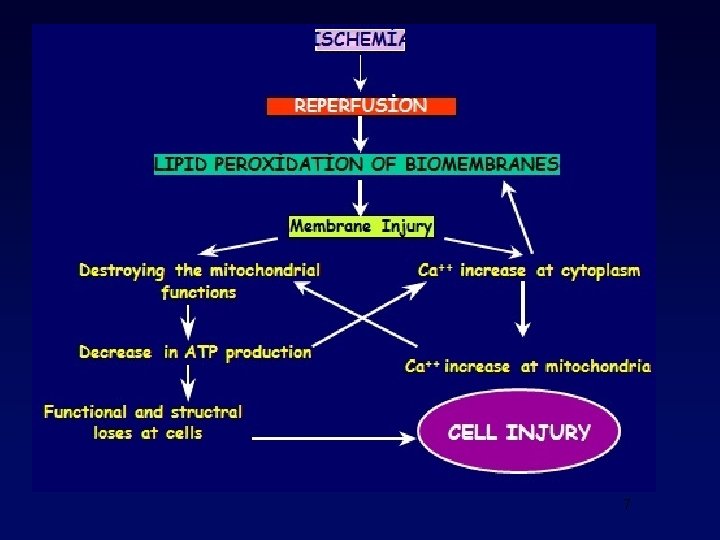
7
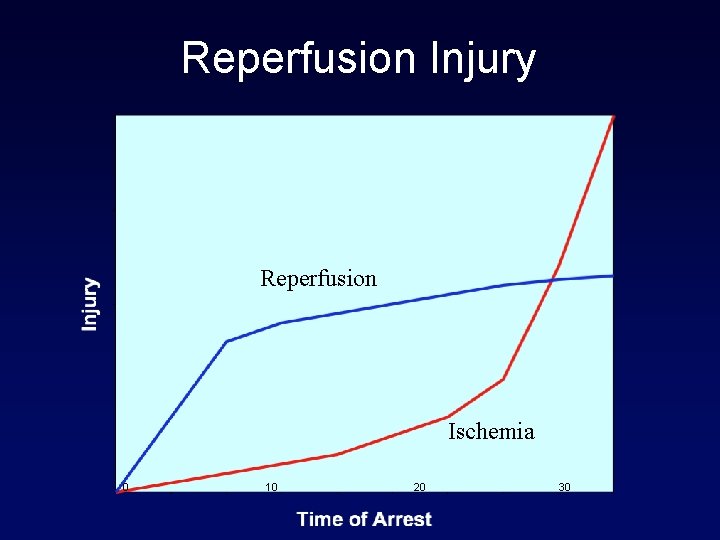
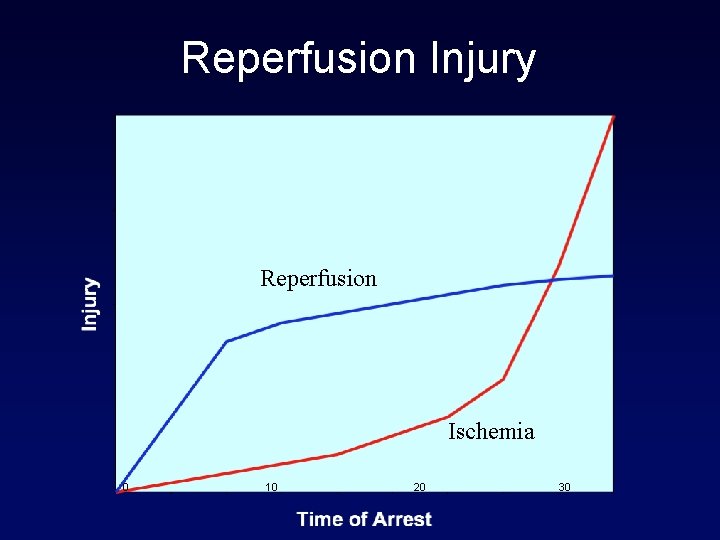
Reperfusion Injury Reperfusion Ischemia 0 10 20 30
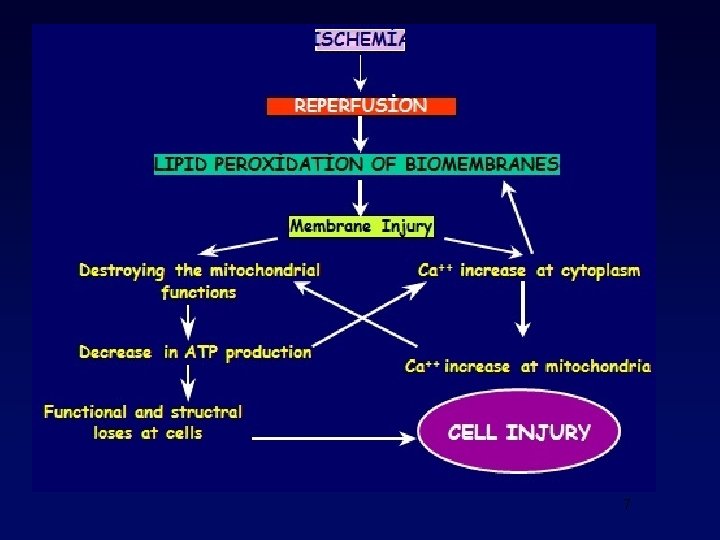
Why should we cool? • Reperfusion injury • Necrosis/apoptosis • Inflammation • Reactive oxygen species • Improved defibrillation • B-blocker effect?
Historic perspective • Open heart surgeries: moderate hypothermia (28 C to 32 C) used since the 1950 s to protect the brain during intra-op global ischemia. • Successful use of hypothermia after SCD described in 1950 s but subsequently abandoned due to lack of evidence. 10
Cont. • Guideline 2000 for CPR and Emergency Cardiovascular care did not include therapeutic hypothermia after arrest. • In 2002 the results of 2 prospective randomized trials lead to addition of this recommendation to the guidelines. 11
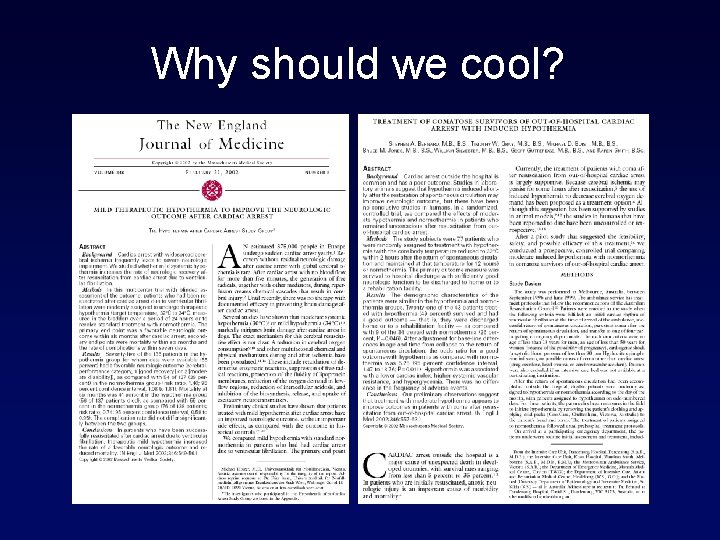
Why should we cool?
• Entry criteria: witnessed cardiac arrest with first resuscitation attempt 5 -15 min after collapse, ROSC (<60 from collapse), persistent coma, VF. • Exclusion criteria: severe cardiogenic shock, hypotension (SBP <90 mm. Hg), persistent arrhythmias, primary coagulopathy. • Approximately 92% of screened participants were excluded. 13
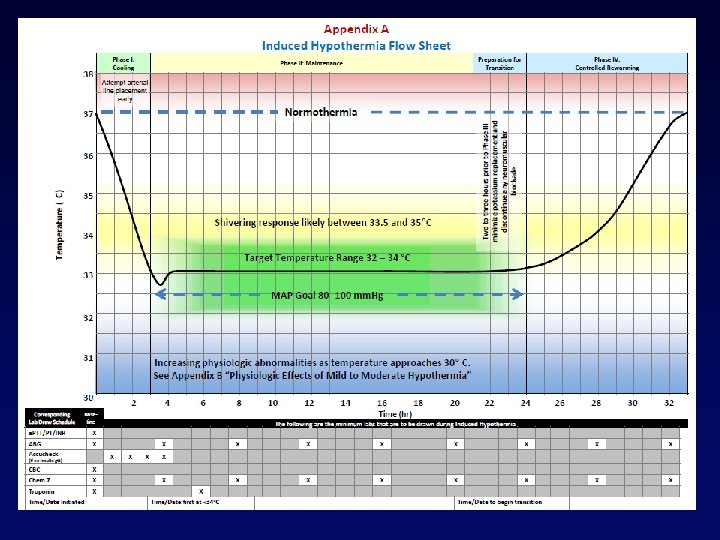
PROTOCOL • In European study, patients were cooled using a special mattress and ice packs. Target temp 32℃ to 34℃ for 24 hours. Rewarming over 8 hours. • Australian study used cold packs in the field. Target temp 33℃ for 12 hours. Rewarming over 6 hours. 14
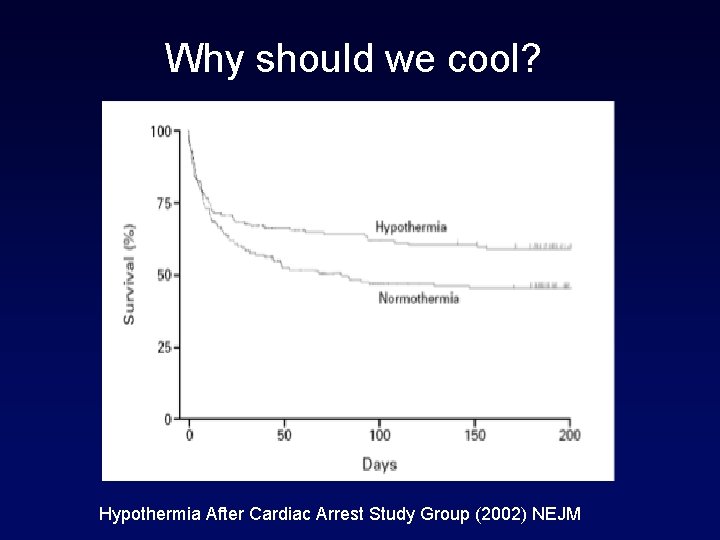
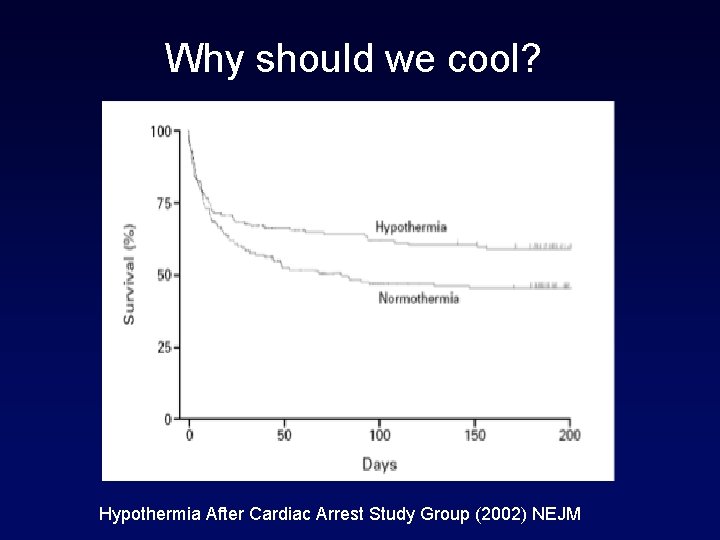
Why should we cool? Hypothermia After Cardiac Arrest Study Group (2002) NEJM
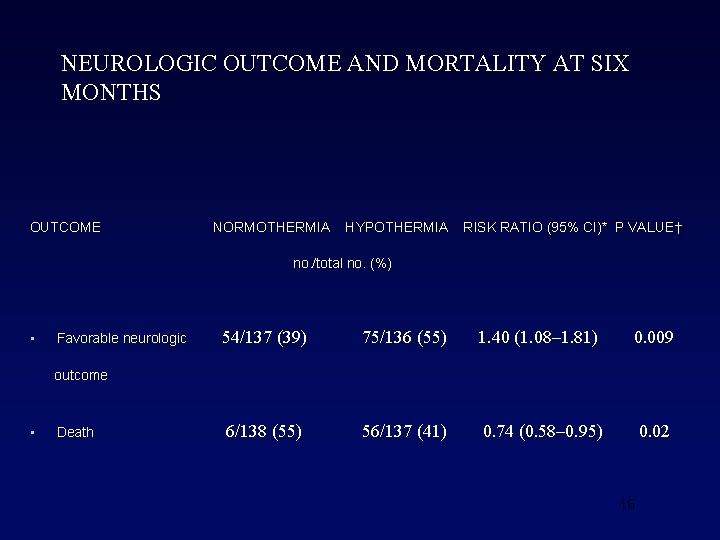
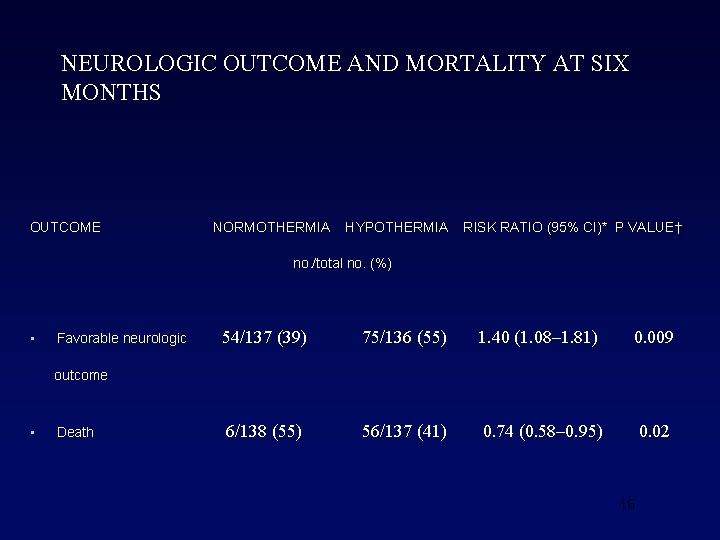
NEUROLOGIC OUTCOME AND MORTALITY AT SIX MONTHS OUTCOME NORMOTHERMIA HYPOTHERMIA RISK RATIO (95% CI)* P VALUE† no. /total no. (%) • Favorable neurologic 54/137 (39) 75/136 (55) 1. 40 (1. 08– 1. 81) 0. 009 6/138 (55) 56/137 (41) 0. 74 (0. 58– 0. 95) 0. 02 outcome • Death 16
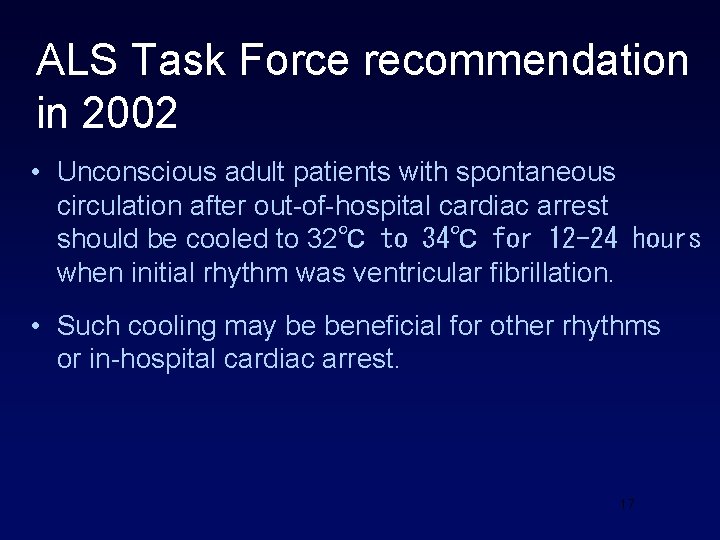
ALS Task Force recommendation in 2002 • Unconscious adult patients with spontaneous circulation after out-of-hospital cardiac arrest should be cooled to 32℃ to 34℃ for 12 -24 hours when initial rhythm was ventricular fibrillation. • Such cooling may be beneficial for other rhythms or in-hospital cardiac arrest. 17
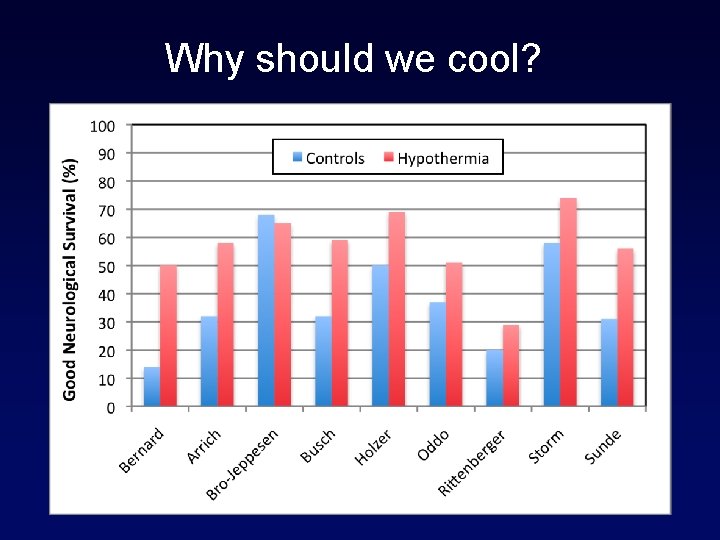
Why should we cool?
Post-Arrest Care • Cooling • Emergency PCI • Good ICU care • Rehab?
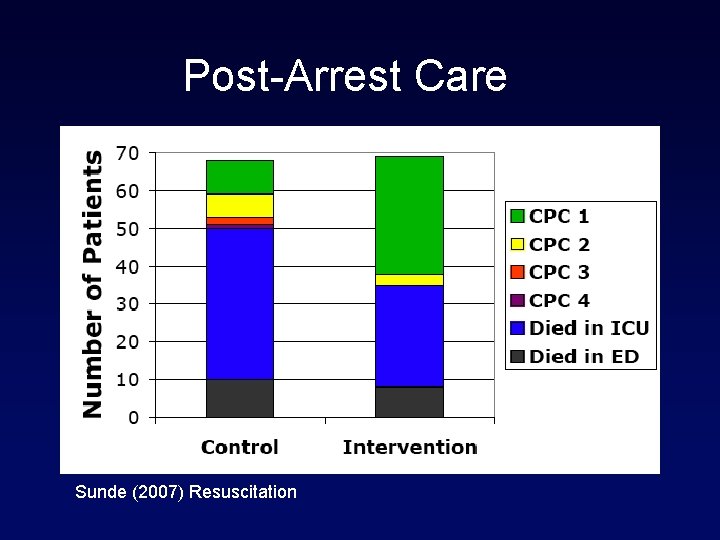
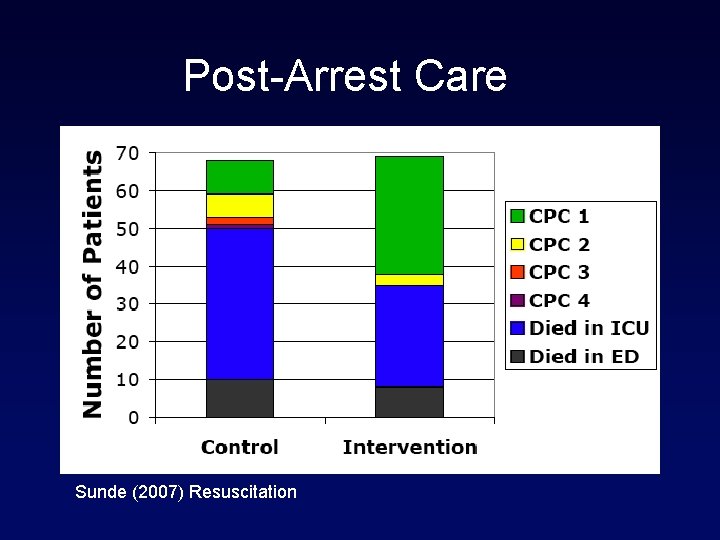
Post-Arrest Care Sunde (2007) Resuscitation
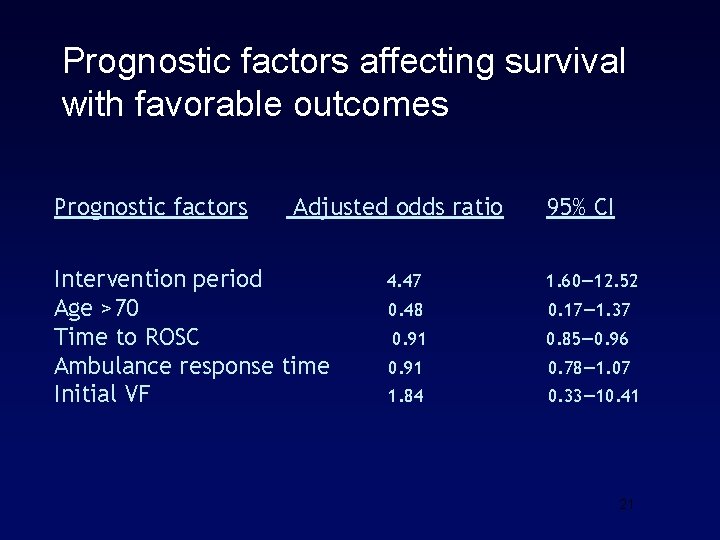
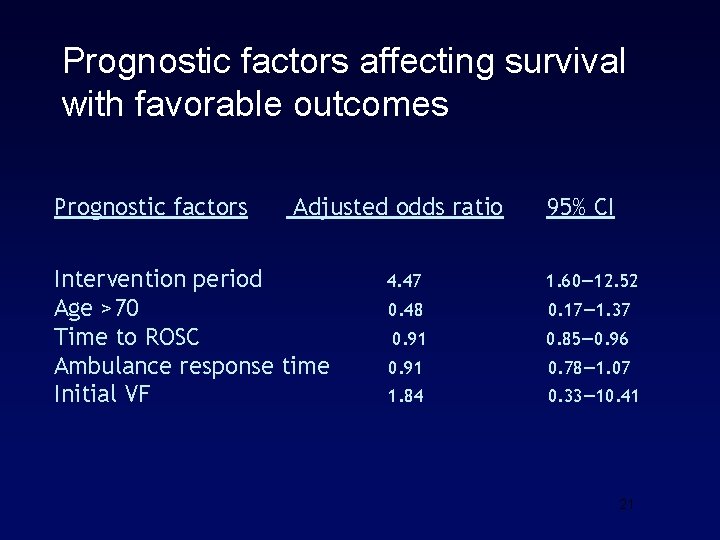
Prognostic factors affecting survival with favorable outcomes Prognostic factors Adjusted odds ratio Intervention period Age >70 Time to ROSC Ambulance response time Initial VF 95% CI 4. 47 1. 60— 12. 52 0. 48 0. 17— 1. 37 0. 91 0. 85— 0. 96 0. 91 0. 78— 1. 07 1. 84 0. 33— 10. 41 21
Post-Arrest Care
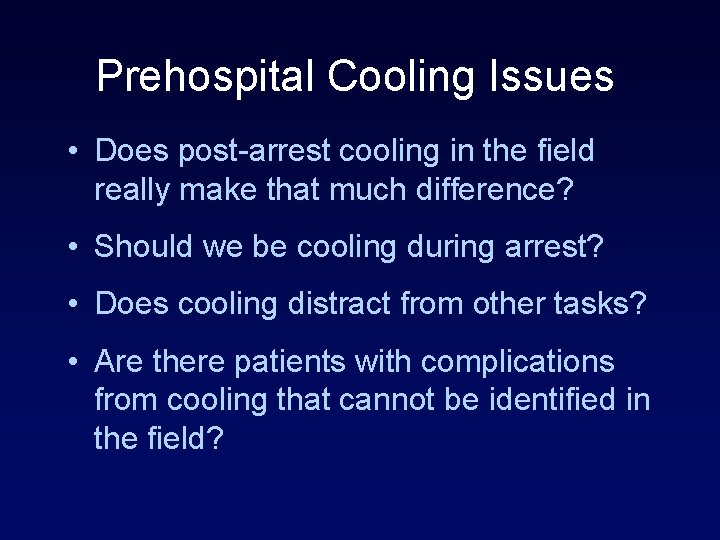
Prehospital Cooling Issues • Does post-arrest cooling in the field really make that much difference? • Should we be cooling during arrest? • Does cooling distract from other tasks? • Are there patients with complications from cooling that cannot be identified in the field?
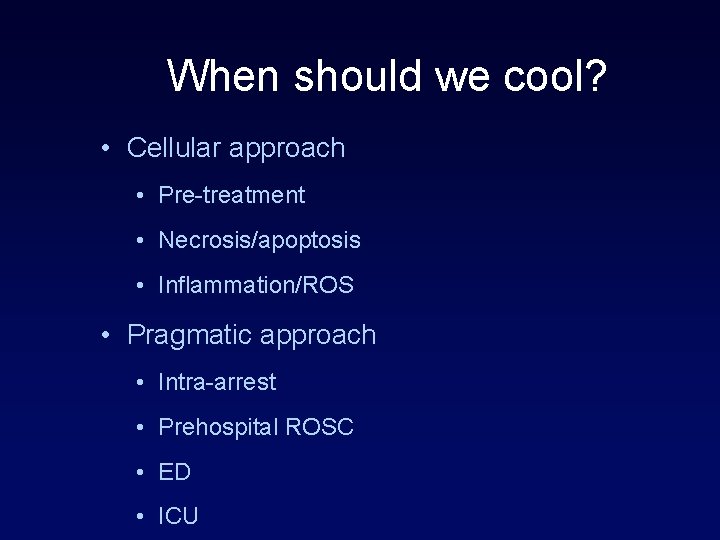
When should we cool? • Cellular approach • Pre-treatment • Necrosis/apoptosis • Inflammation/ROS • Pragmatic approach • Intra-arrest • Prehospital ROSC • ED • ICU
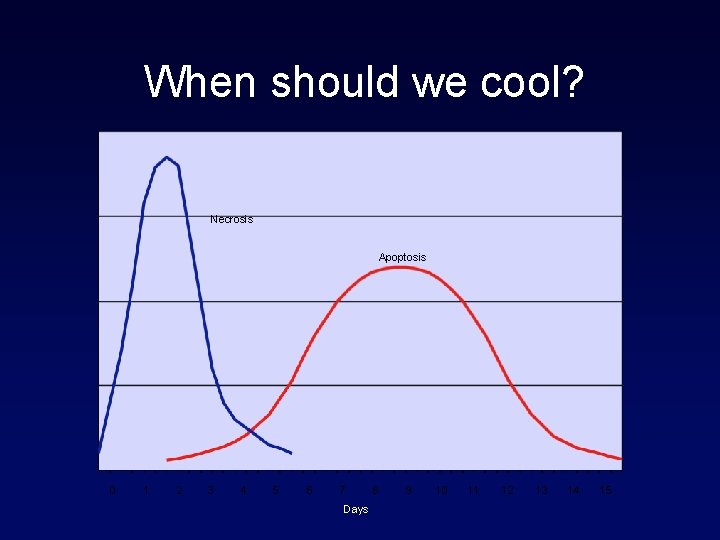
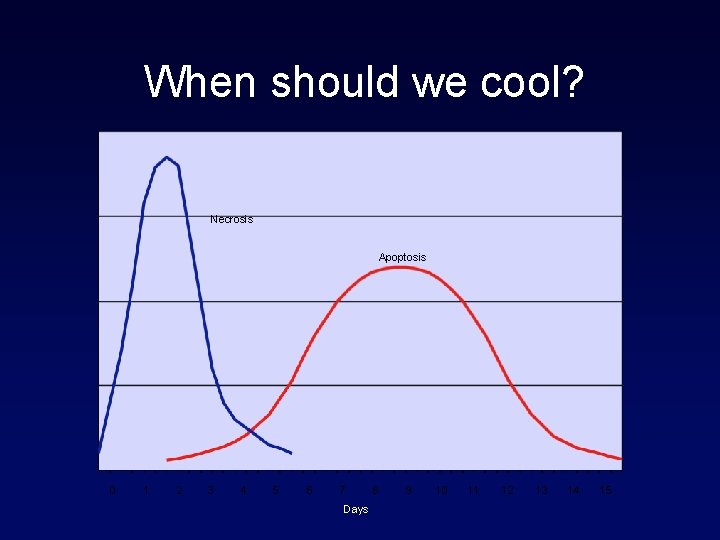
When should we cool? Necrosis Apoptosis 0 1 2 3 4 5 6 7 Days 8 9 10 11 12 13 14 15
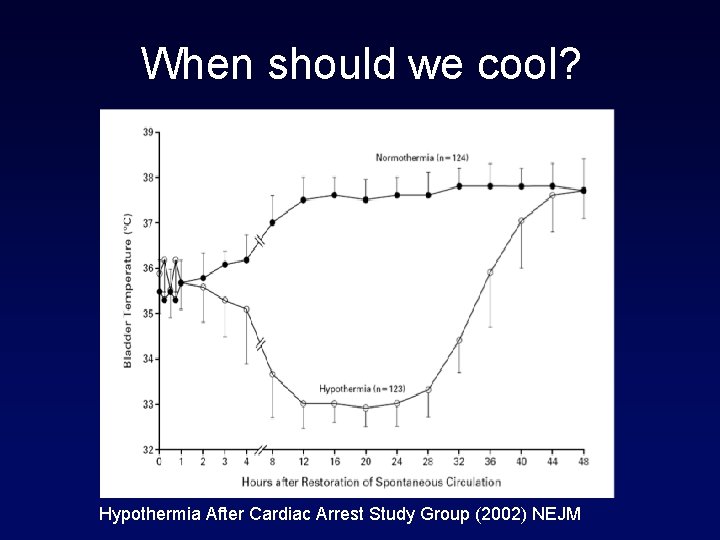
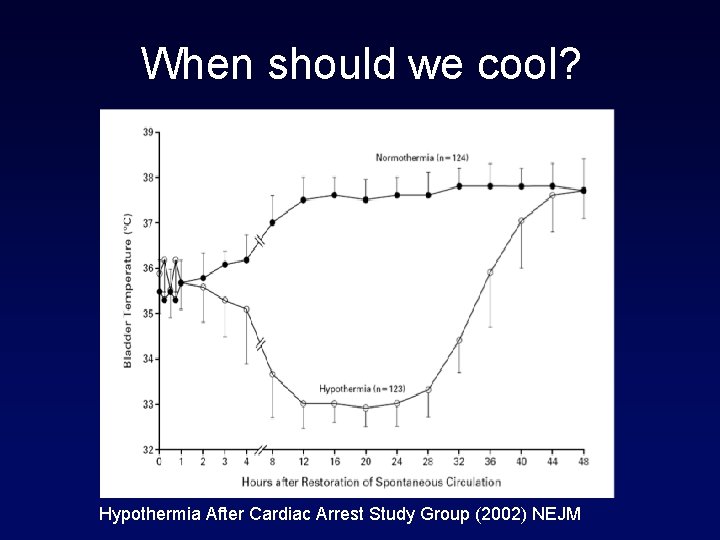
When should we cool? Hypothermia After Cardiac Arrest Study Group (2002) NEJM
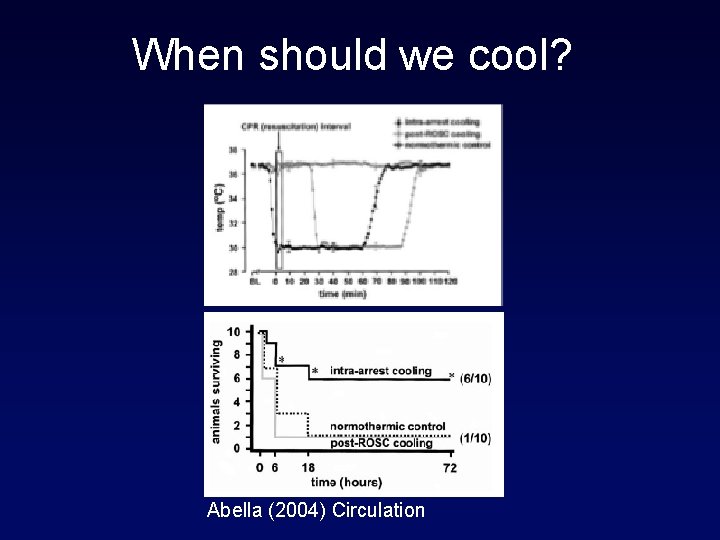
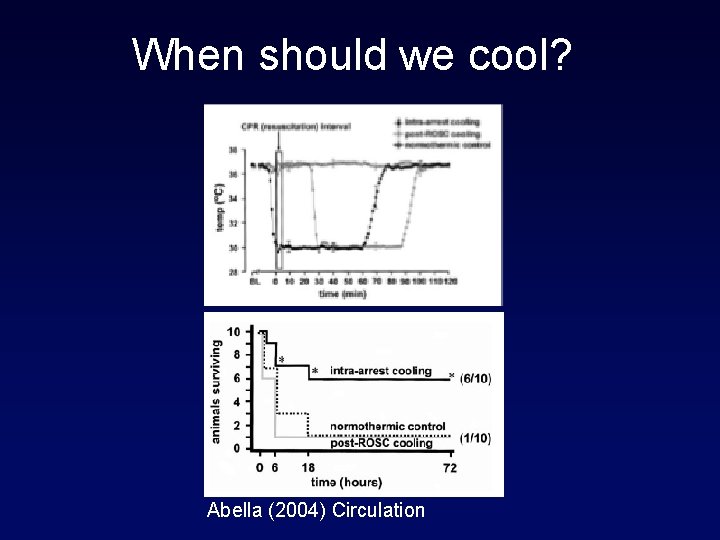
When should we cool? Abella (2004) Circulation
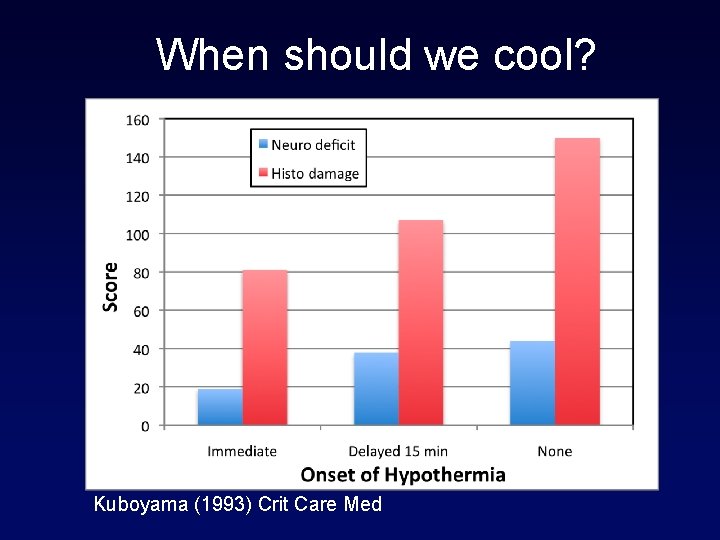
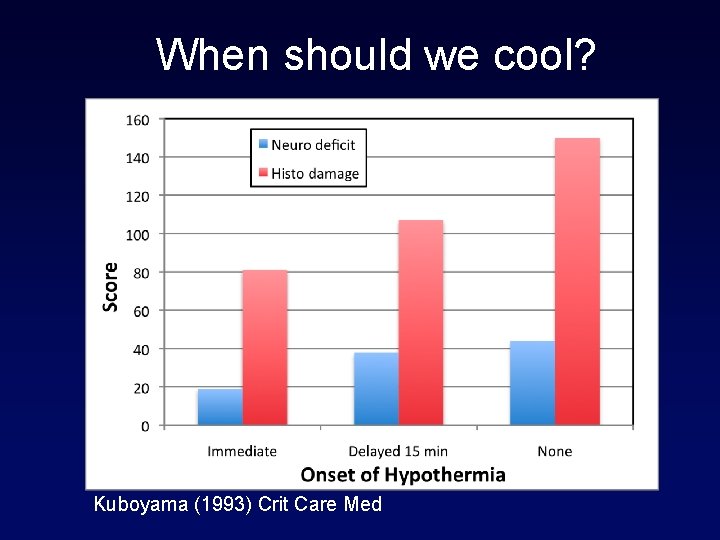
When should we cool? Kuboyama (1993) Crit Care Med
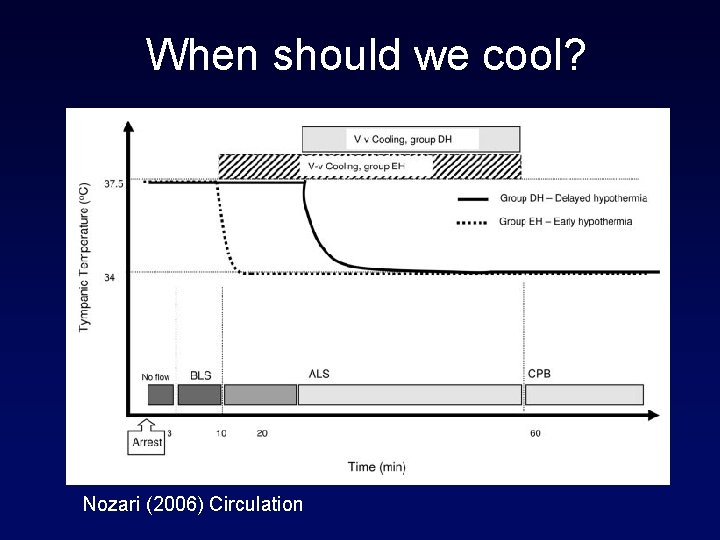
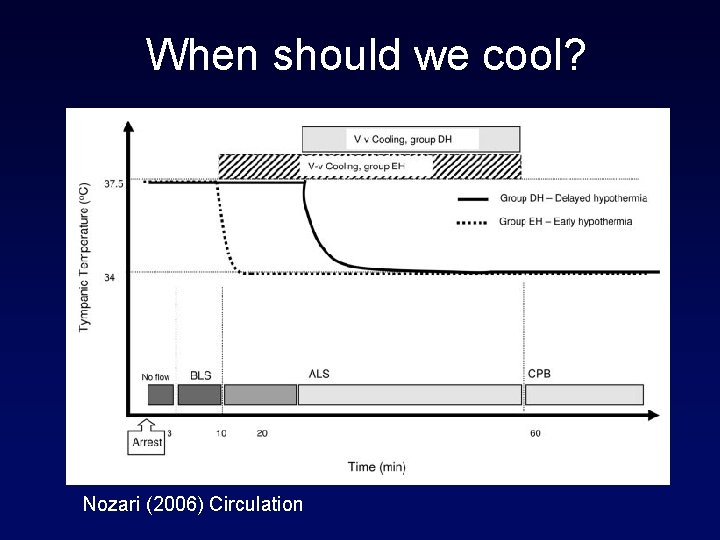
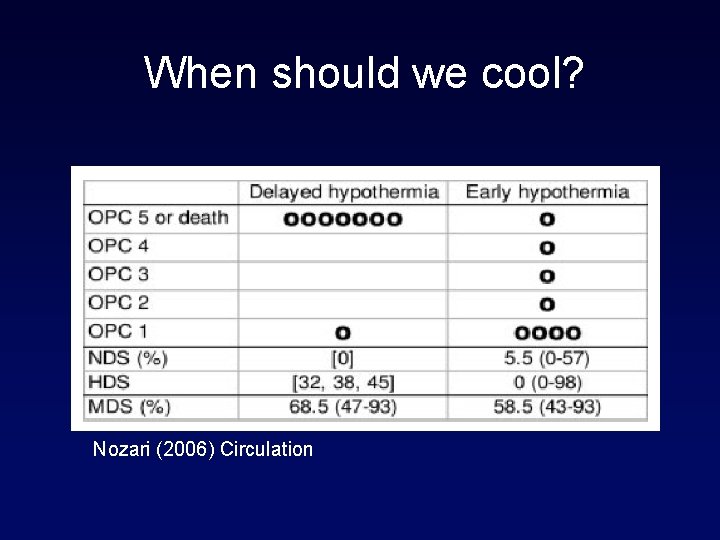
When should we cool? Nozari (2006) Circulation
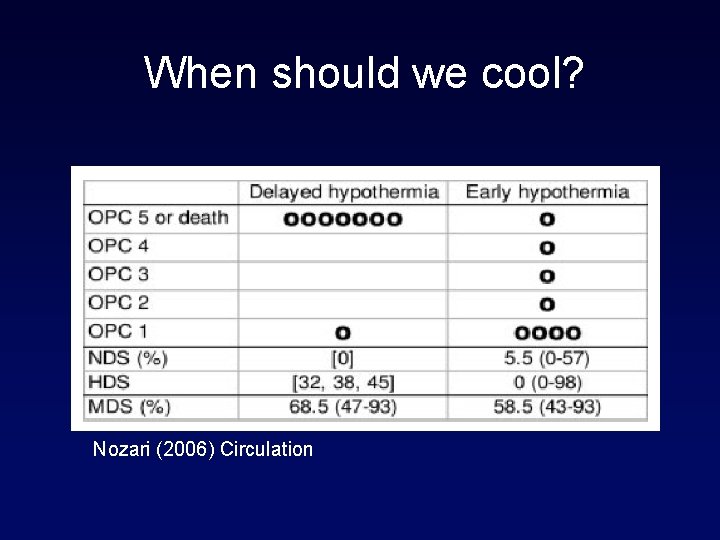
When should we cool? Nozari (2006) Circulation
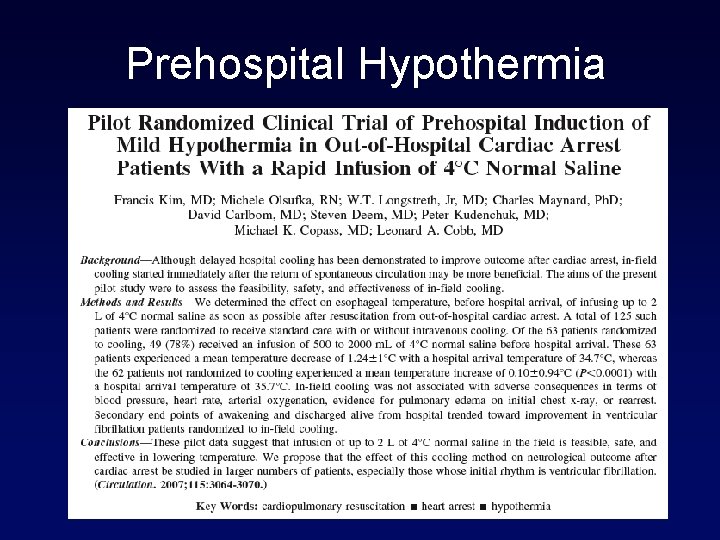
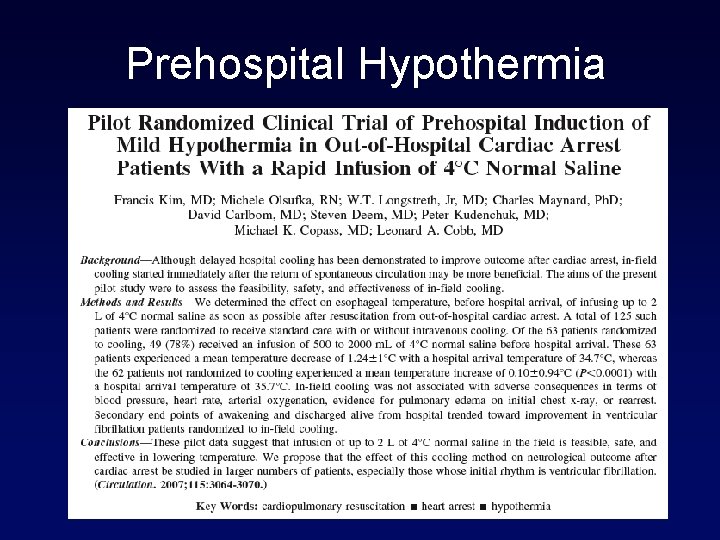
Prehospital Hypothermia
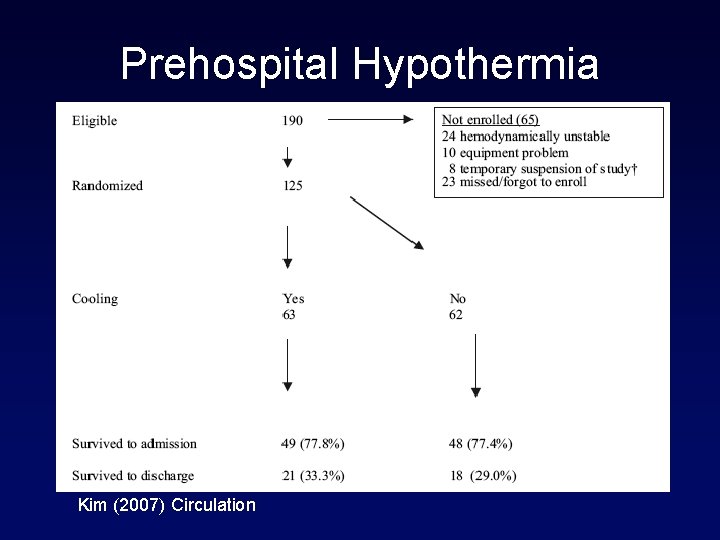
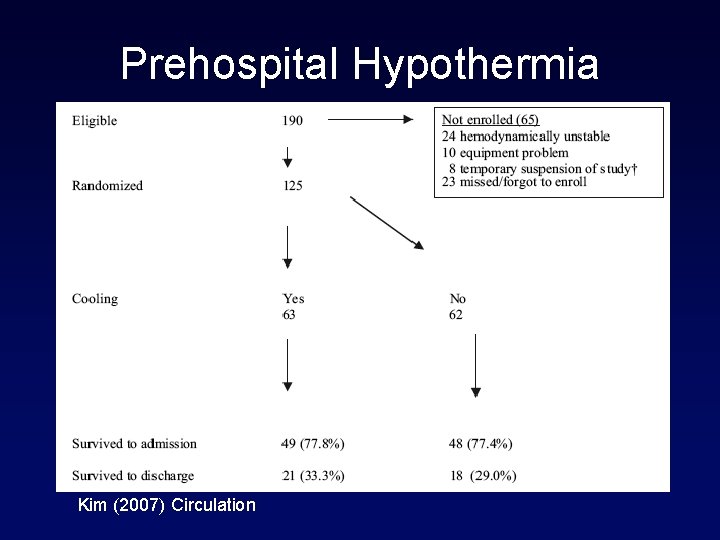
Prehospital Hypothermia Kim (2007) Circulation
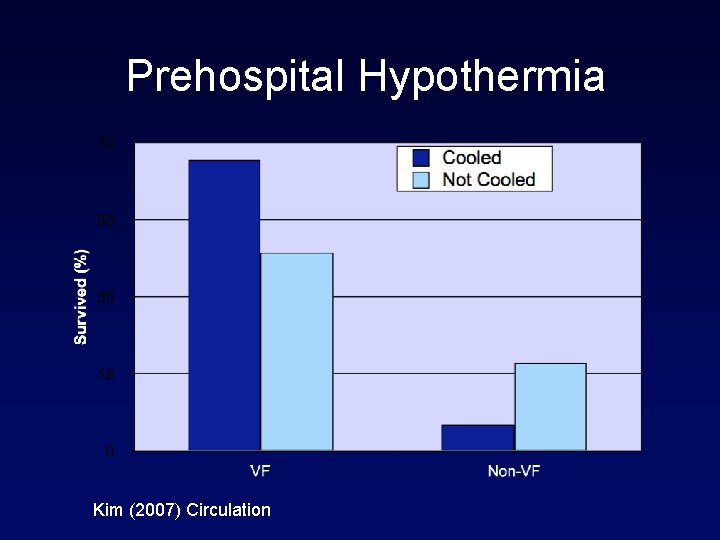
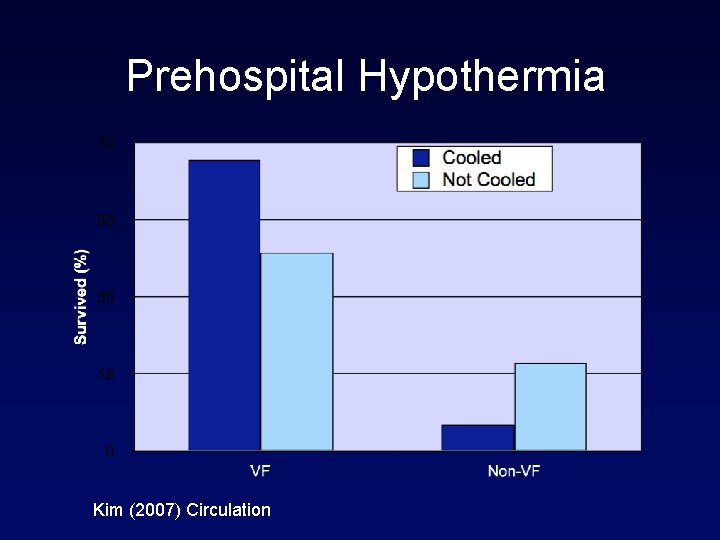
Prehospital Hypothermia Kim (2007) Circulation
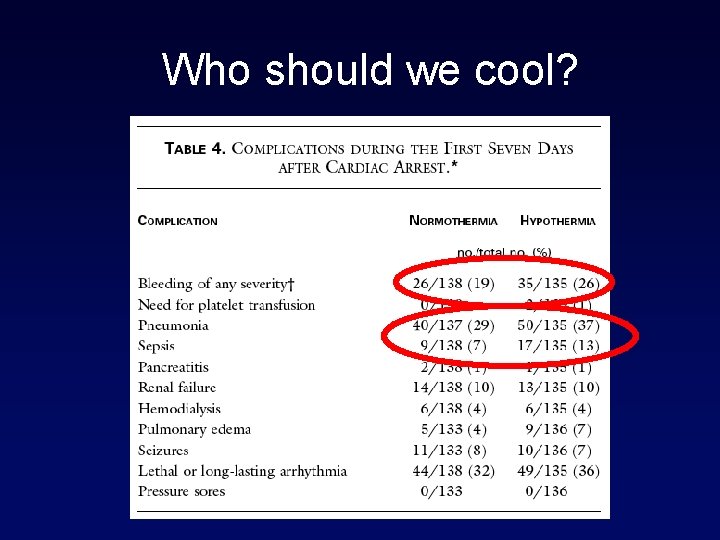
Who should we cool? • All arrest victims? • Brain doesn’t know the rhythm • Only ventricular fibrillation? • Evidence-based approach • Non-VF patients? • Infection • CHF • Bleeding
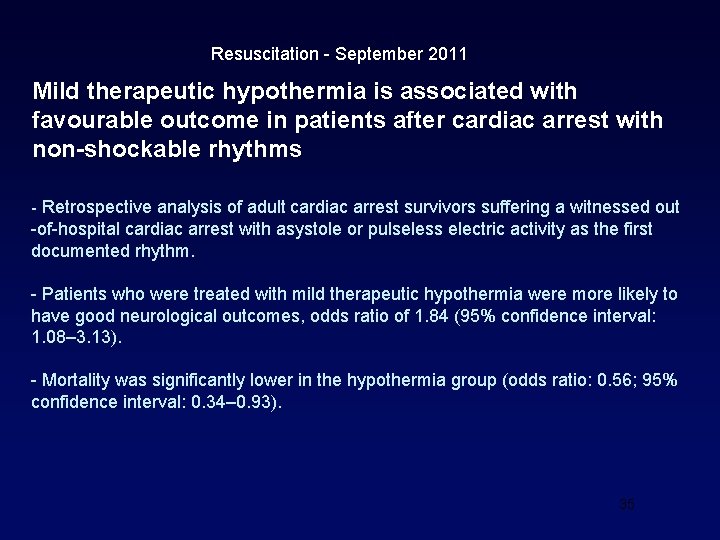
Resuscitation - September 2011 Mild therapeutic hypothermia is associated with favourable outcome in patients after cardiac arrest with non-shockable rhythms - Retrospective analysis of adult cardiac arrest survivors suffering a witnessed out -of-hospital cardiac arrest with asystole or pulseless electric activity as the first documented rhythm. - Patients who were treated with mild therapeutic hypothermia were more likely to have good neurological outcomes, odds ratio of 1. 84 (95% confidence interval: 1. 08– 3. 13). - Mortality was significantly lower in the hypothermia group (odds ratio: 0. 56; 95% confidence interval: 0. 34– 0. 93). 35
Resuscitation - February 2012 Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms? : A systematic review and meta-analysis of randomized and non-randomized studies. • TH is associated with reduced in-hospital mortality for adults patients resuscitated from non-shockable CA. • However, most of the studies had substantial risks of bias and quality of evidence was very low. • Further high quality randomized clinical trials would confirm the actual benefit of TH in this population. 36
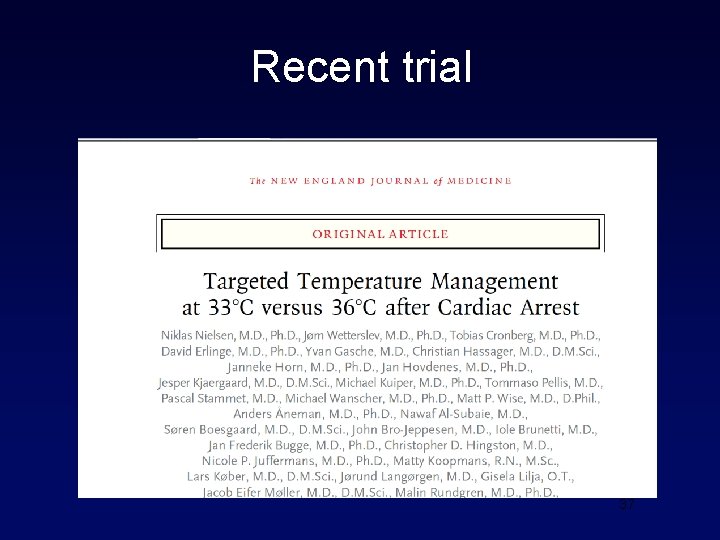
Recent trial 37
Trial design • Randomized 950 unconscious adults after out-ofhospital cardiac arrest of presumed cardiac cause (irrespective of initial rhythm) to targeted temperature management at either 33°C or 36°C. • The primary outcome was all-cause mortality through the end of the trial. • Secondary outcomes included a composite of poor neurologic function or death at 180 days 38
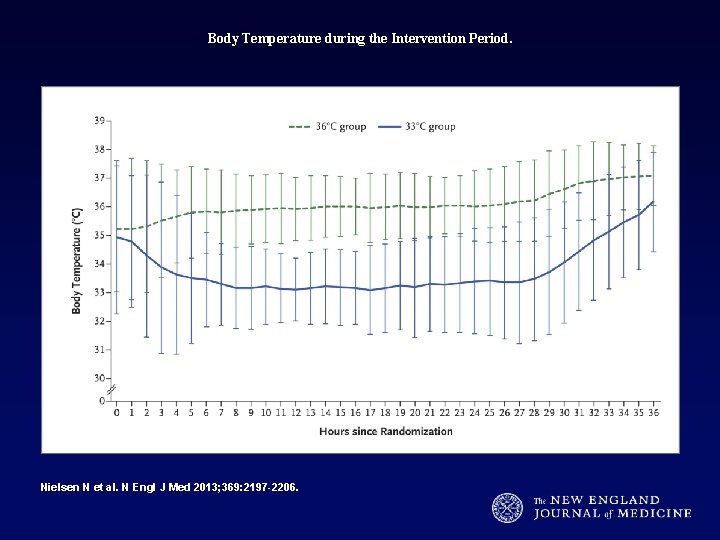
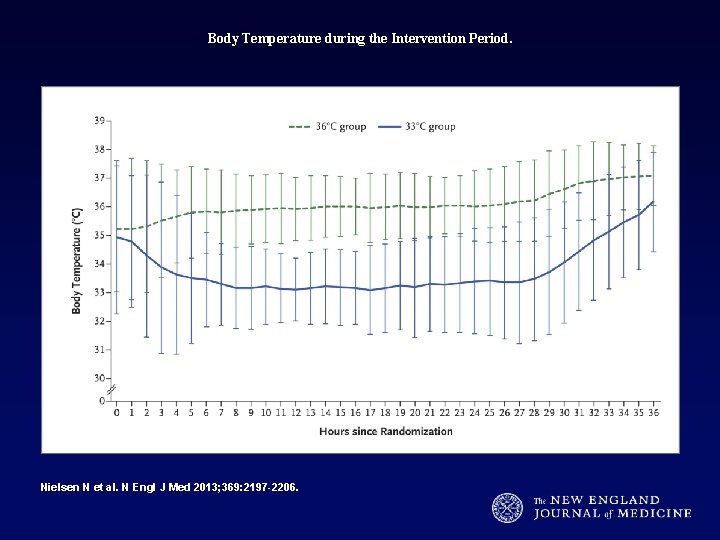
Body Temperature during the Intervention Period. Nielsen N et al. N Engl J Med 2013; 369: 2197 -2206.
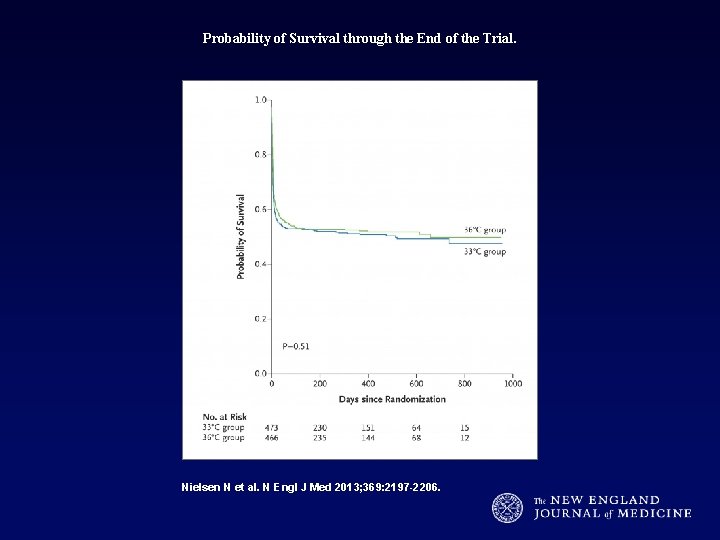
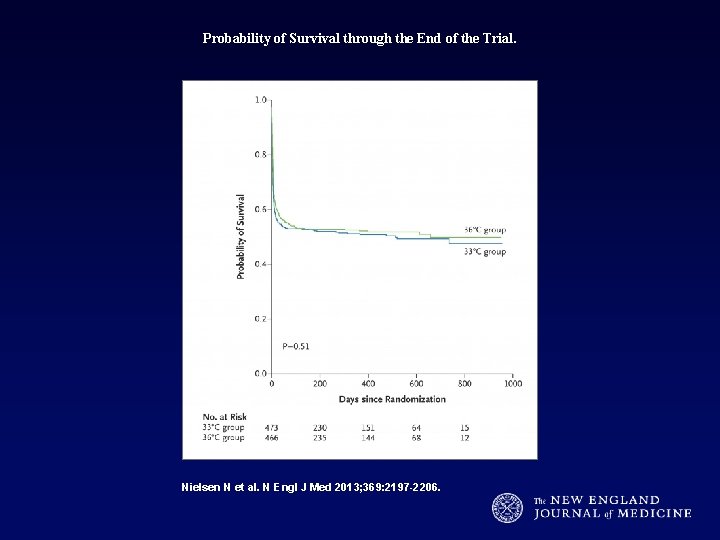
Probability of Survival through the End of the Trial. Nielsen N et al. N Engl J Med 2013; 369: 2197 -2206.
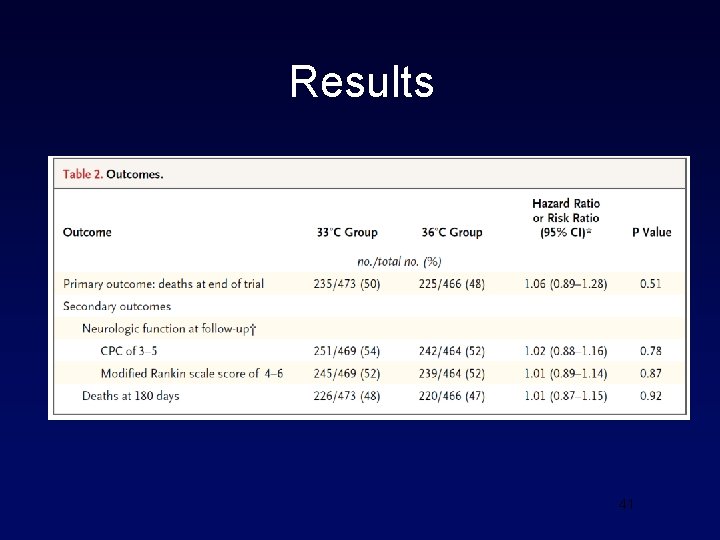
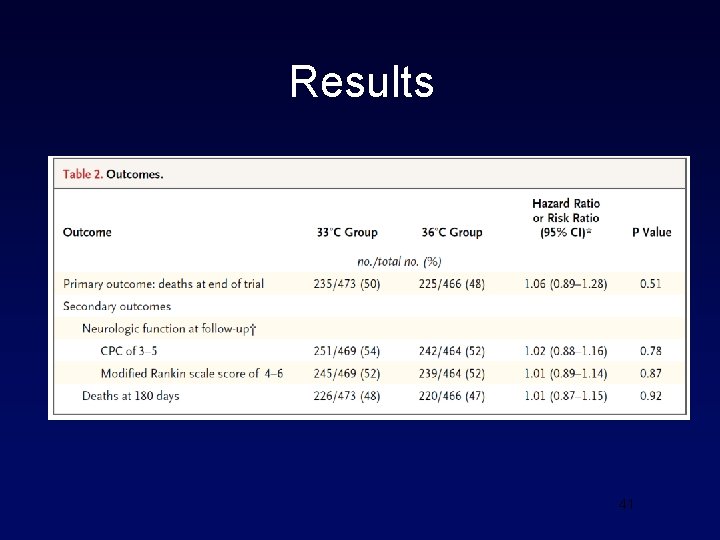
Results 41
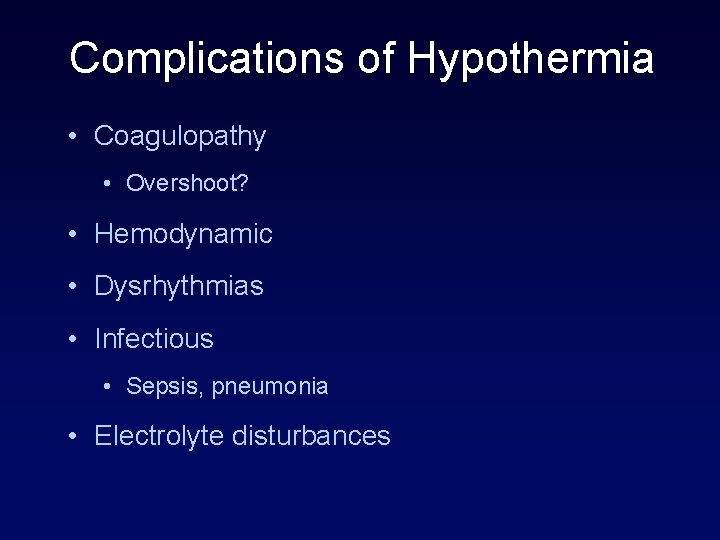
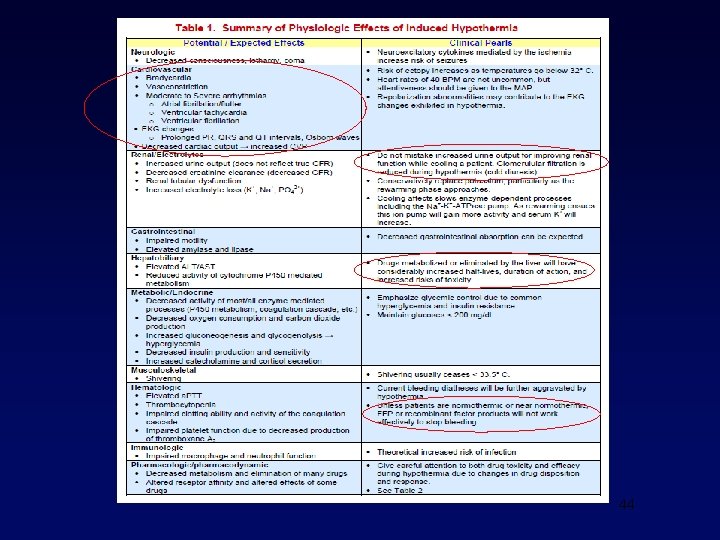
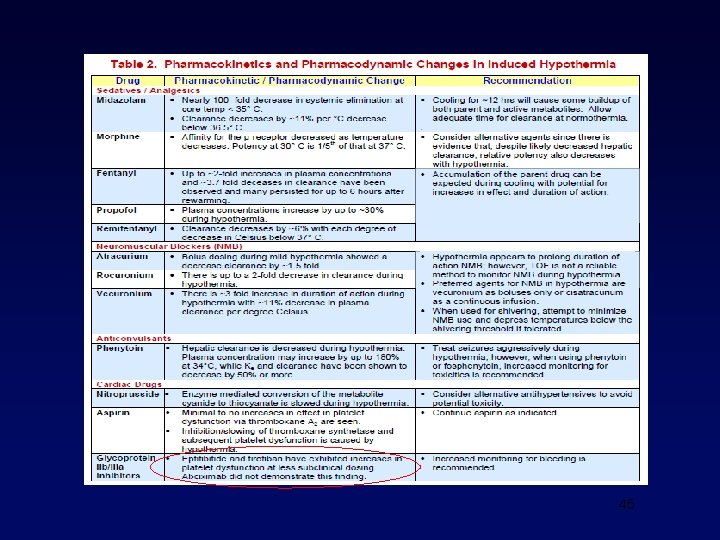
Complications of Hypothermia • Coagulopathy • Overshoot? • Hemodynamic • Dysrhythmias • Infectious • Sepsis, pneumonia • Electrolyte disturbances
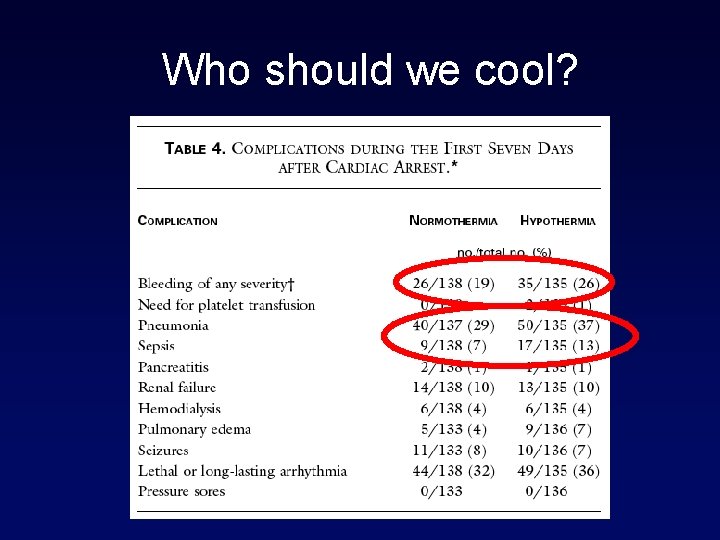
Who should we cool?
44
45
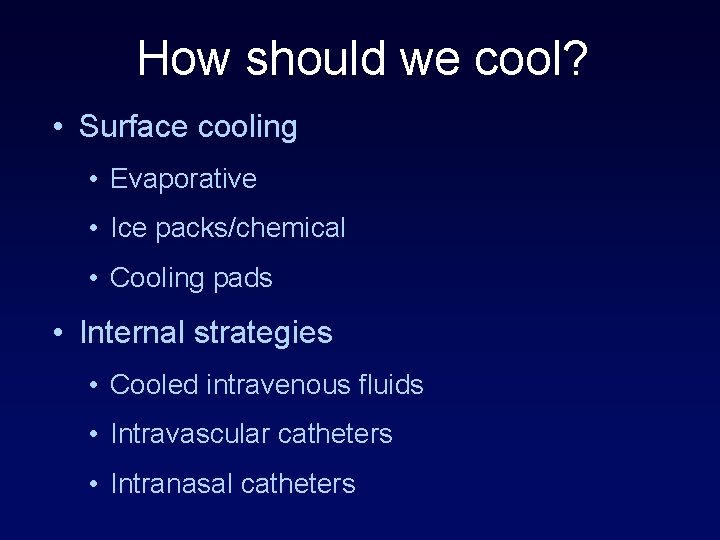
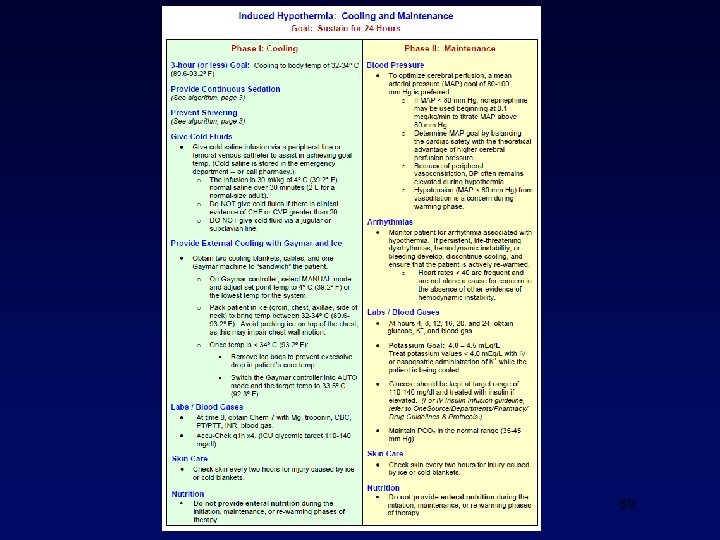
How should we cool? • Surface cooling • Evaporative • Ice packs/chemical • Cooling pads • Internal strategies • Cooled intravenous fluids • Intravascular catheters • Intranasal catheters
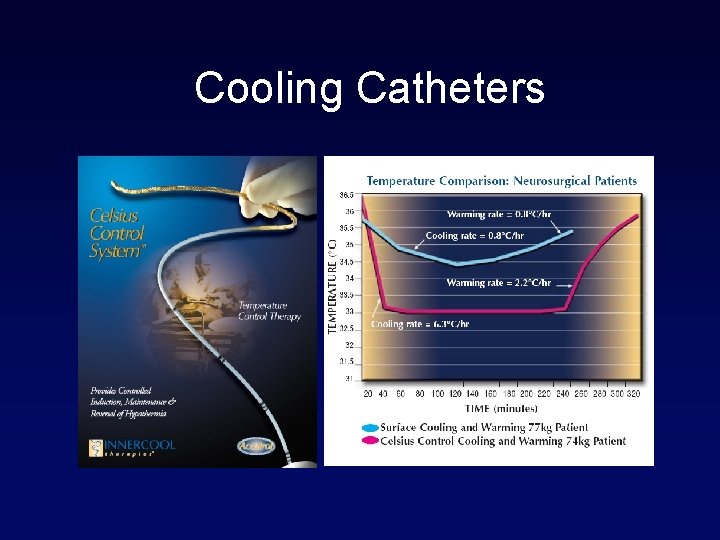
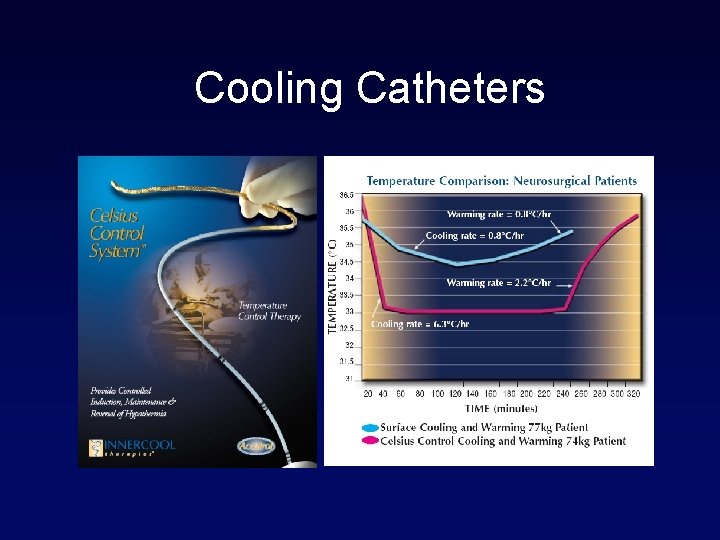
Cooling Catheters

Surface Cooling
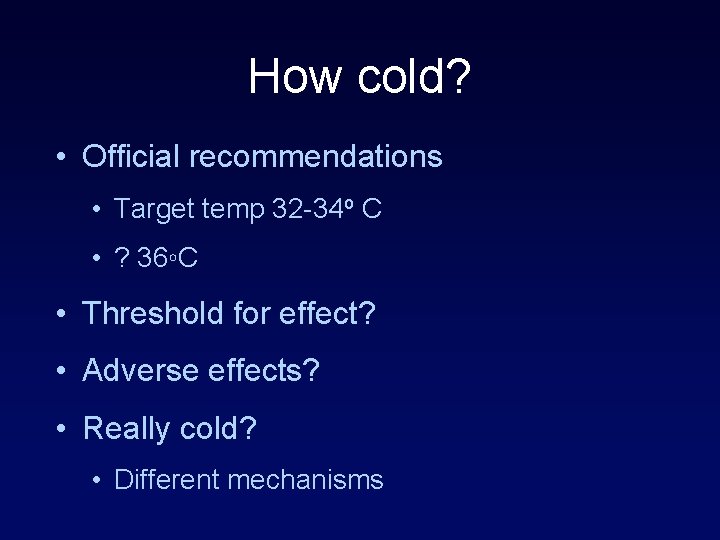
How cold? • Official recommendations • Target temp 32 -34 o C • ? 36◦C • Threshold for effect? • Adverse effects? • Really cold? • Different mechanisms

50
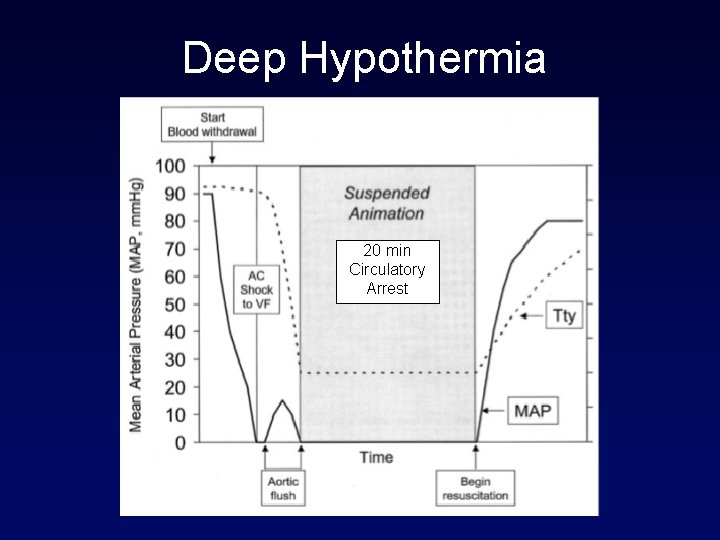
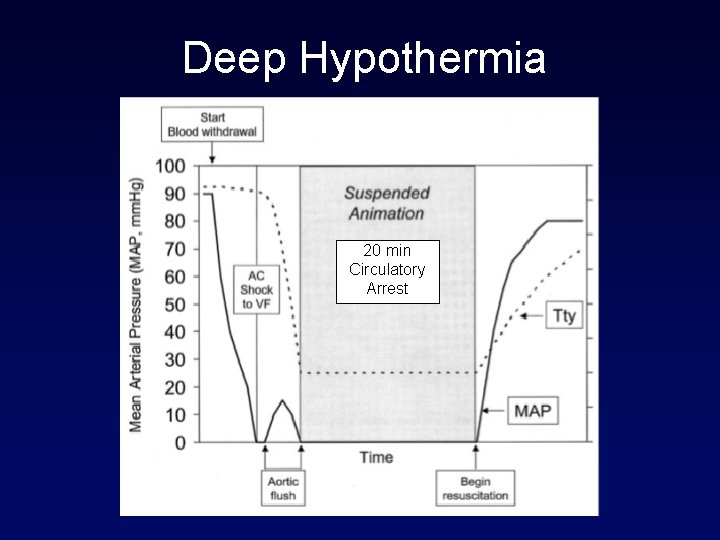
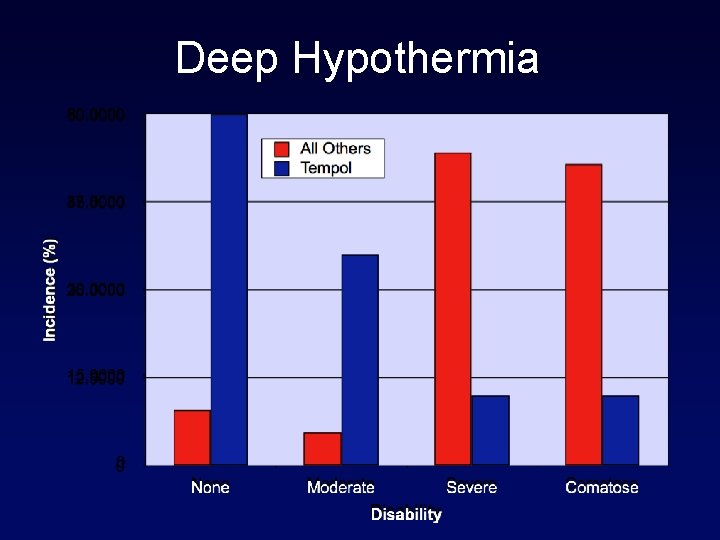
Deep Hypothermia 20 min Circulatory Arrest
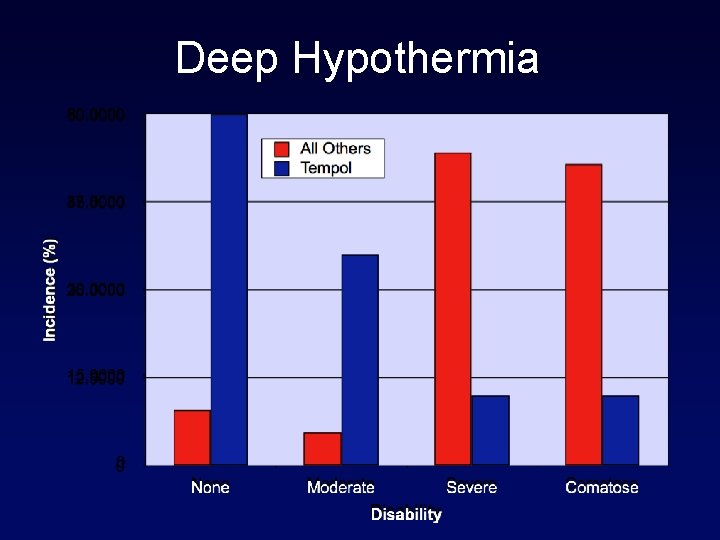
Deep Hypothermia
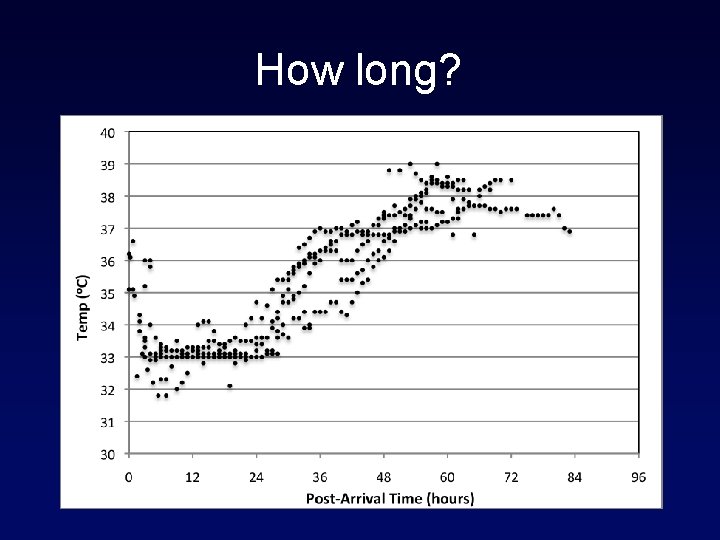
How long? • Official recommendations • Inflammatory pattern • Peak at 72 hours • Customized • Depth and duration
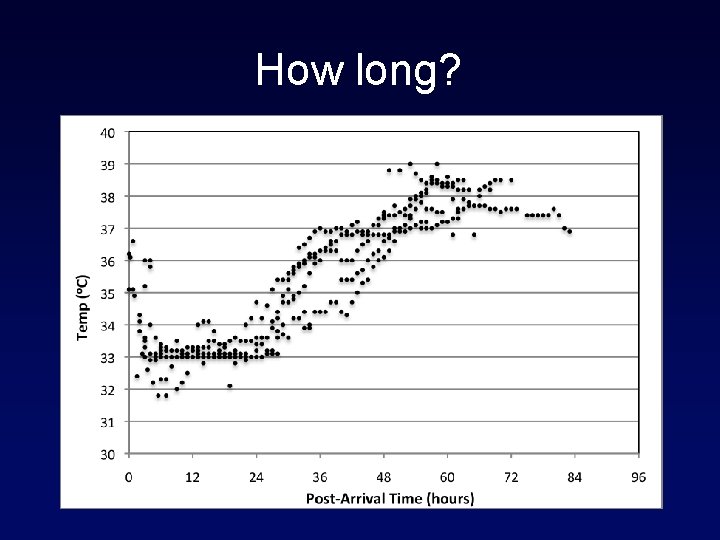
How long?
Assessing neurologic recovery • New thoughts on longer waiting time prior to withdrawal of care. 55
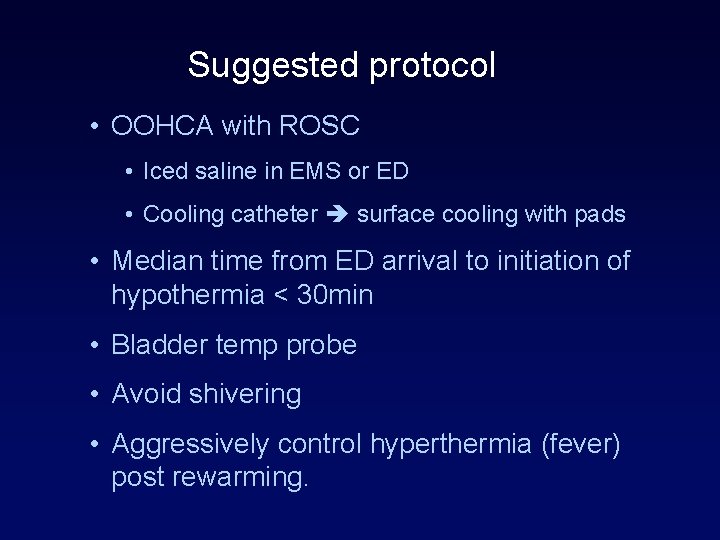
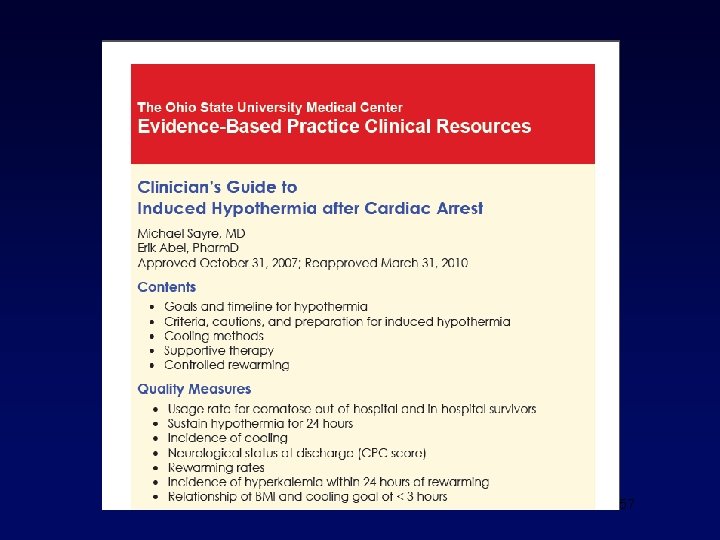
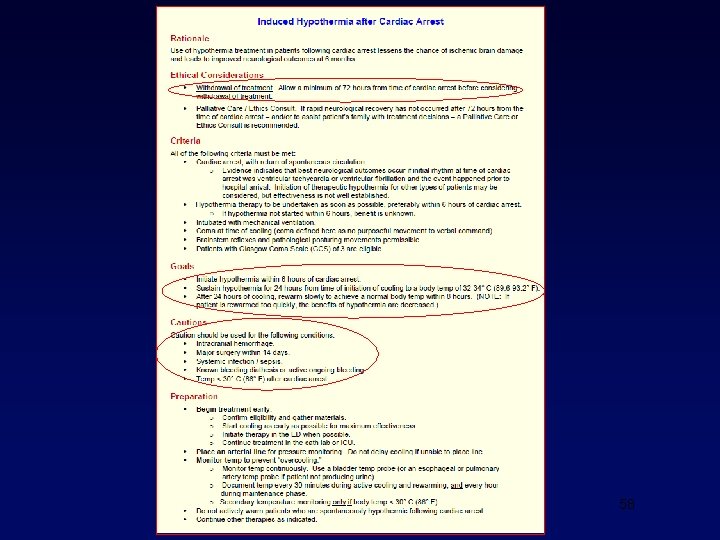
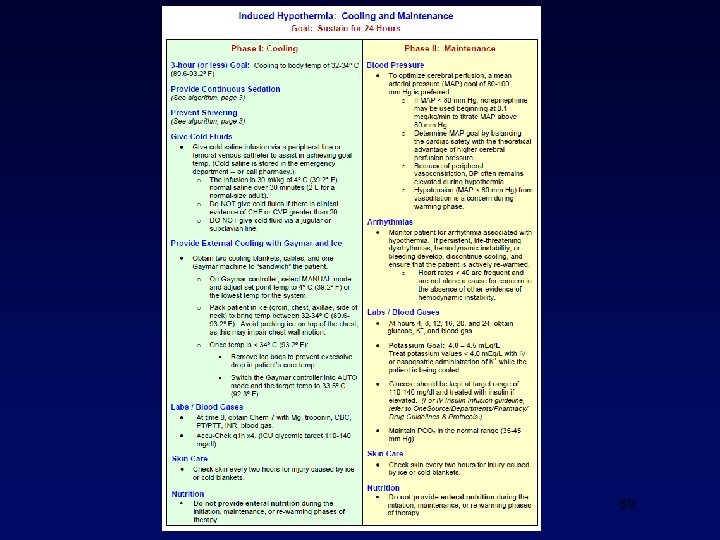
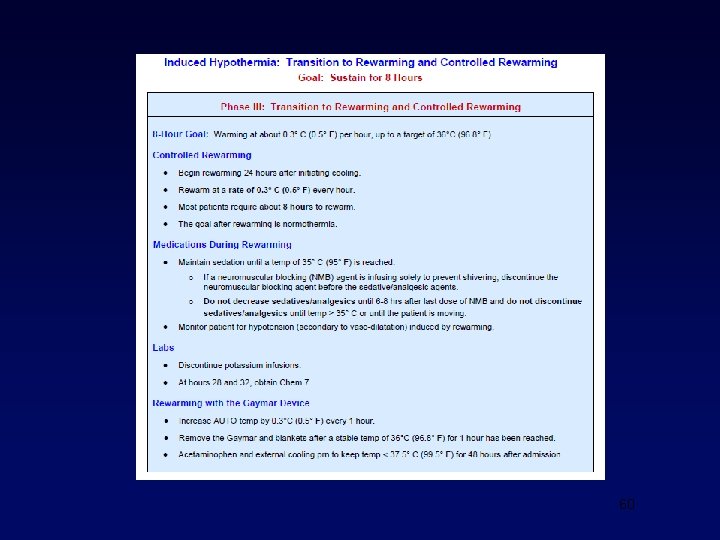
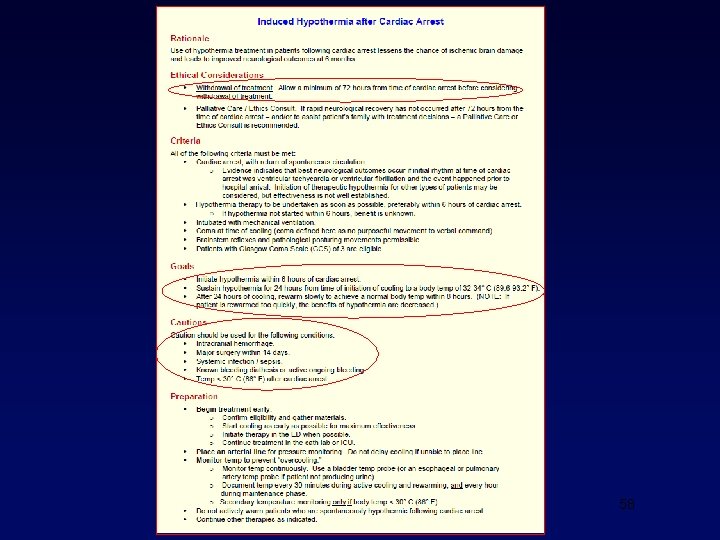
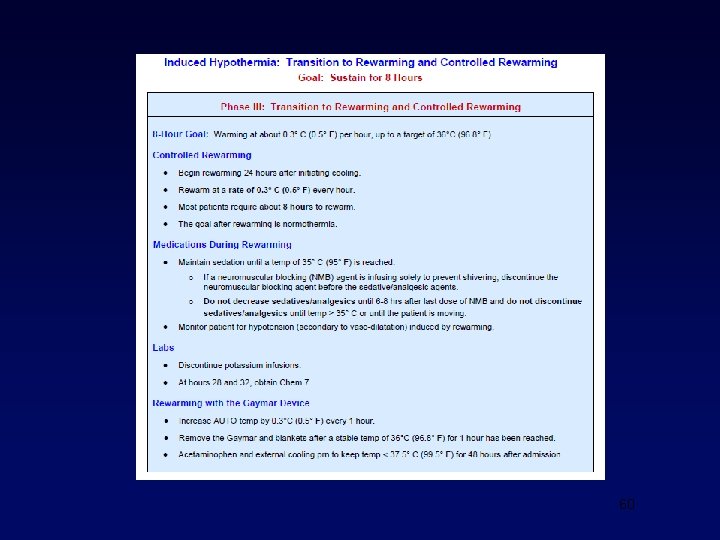
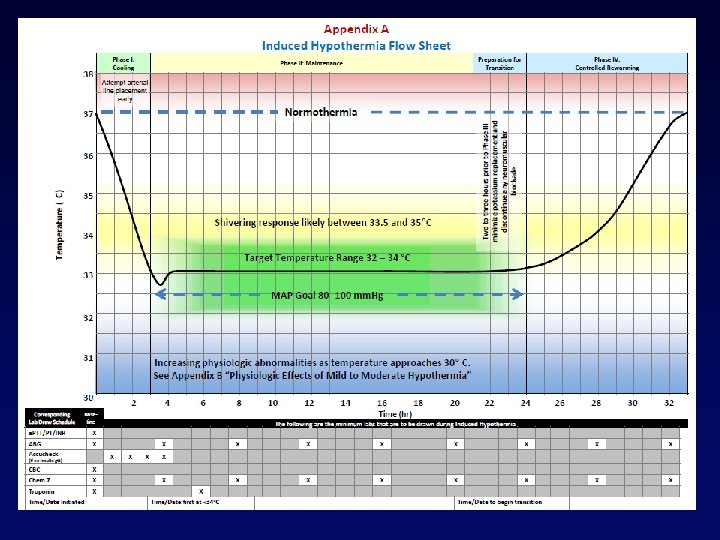
Suggested protocol • OOHCA with ROSC • Iced saline in EMS or ED • Cooling catheter surface cooling with pads • Median time from ED arrival to initiation of hypothermia < 30 min • Bladder temp probe • Avoid shivering • Aggressively control hyperthermia (fever) post rewarming.
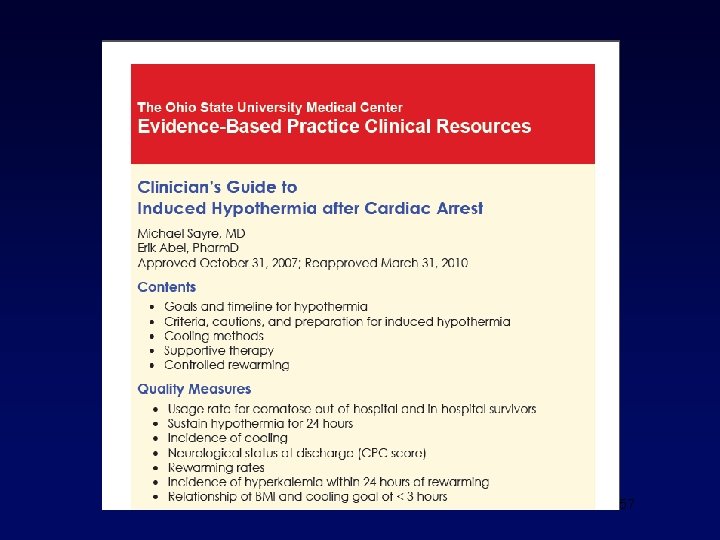
57
58
59
60
61
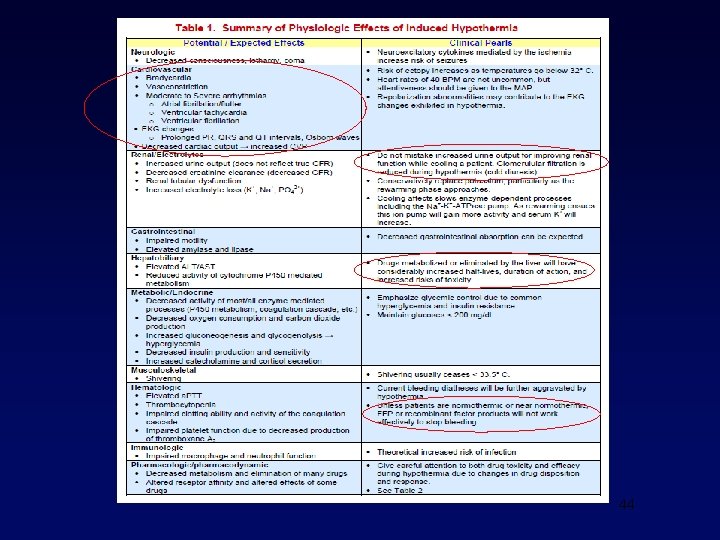
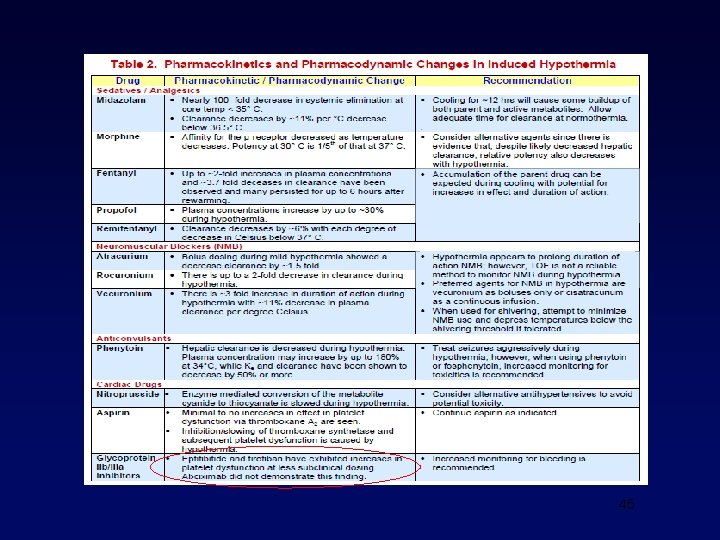
Parting Thoughts • More patients should be closely monitored for hyperthermia • The complications of hypothermia should be anticipated, not avoided • Future research may help clarify the optimal “dose” and duration of hypothermia
 Osu
Osu Dr ruchika husa
Dr ruchika husa Warning light
Warning light Stfc scd
Stfc scd Frostbite vs trench foot
Frostbite vs trench foot Temperature hypothermia
Temperature hypothermia Hypothermia suffix
Hypothermia suffix Slovo nadřazené ke slovu slepice husa kachna
Slovo nadřazené ke slovu slepice husa kachna Skloňovanie kobyla
Skloňovanie kobyla Ujo vzor
Ujo vzor Fürj kakas felismerése
Fürj kakas felismerése Husa býložravec
Husa býložravec čím se živí husa
čím se živí husa Husa domácí samec
Husa domácí samec Petr husa
Petr husa Jaakko husa
Jaakko husa Tuluská husa
Tuluská husa Milieu therapy introduction
Milieu therapy introduction Therapeutic class and pharmacologic class
Therapeutic class and pharmacologic class Association for applied and therapeutic humor
Association for applied and therapeutic humor Osu ehs training
Osu ehs training Osu oil and gas accounting conference
Osu oil and gas accounting conference Osu military
Osu military Osu environmental health and safety
Osu environmental health and safety Osu parking and transportation
Osu parking and transportation Therapeutic orientations
Therapeutic orientations Therapeutic feeding center adalah
Therapeutic feeding center adalah Therapeutic exercise chapter 1 mcqs
Therapeutic exercise chapter 1 mcqs Therapeutic equipments
Therapeutic equipments Therapeutic drift
Therapeutic drift Introduction of therapeutic communication
Introduction of therapeutic communication What is the triangle of care
What is the triangle of care Therapeutic story writing starters
Therapeutic story writing starters What are the principles of therapeutic communication
What are the principles of therapeutic communication Principle of therapeutic exercise
Principle of therapeutic exercise Efficacy definition pharmacology
Efficacy definition pharmacology High therapeutic index
High therapeutic index Therapeutic index
Therapeutic index Classification of therapeutic exercise
Classification of therapeutic exercise Therapeutic relationship model
Therapeutic relationship model Therapeutic services pathway
Therapeutic services pathway Reproductive cloning process
Reproductive cloning process Multicultural therapeutic communication skills
Multicultural therapeutic communication skills Career cluster define
Career cluster define Why is a high therapeutic index better
Why is a high therapeutic index better Narrow therapeutic index drugs
Narrow therapeutic index drugs Define therapeutic environment
Define therapeutic environment Sepacto
Sepacto Non therapeutic
Non therapeutic Pharmacology introduction
Pharmacology introduction What is habilitative exercise?
What is habilitative exercise? Kelly chaplin
Kelly chaplin Therapeutic drift
Therapeutic drift Therapeutic communication types
Therapeutic communication types Therapeutic window
Therapeutic window Ichaemic
Ichaemic Chapter 4 therapeutic communication skills
Chapter 4 therapeutic communication skills Therapeutic recreation program sydney
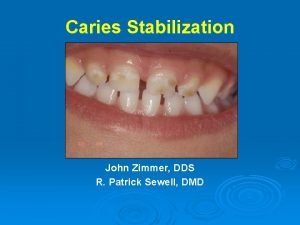
Therapeutic recreation program sydney Caries stabilization
Caries stabilization Btpb repertory rubrics
Btpb repertory rubrics Roger verbeeck
Roger verbeeck Therapeutic window
Therapeutic window Intentional relationship model
Intentional relationship model